User login
SERMs revisited: Can they improve menopausal care?
Selective estrogen receptor modulators (SERMs) are unique synthetic compounds that bind to the estrogen receptor and initiate either estrogenic agonistic or antagonistic activity, depending on the confirmational change they produce on binding to the receptor. Many SERMs have come to market, others have not. Unlike estrogens, which regardless of dose or route of administration all carry risks as a boxed warning on the label, referred to as class labeling,1 various SERMs exert various effects in some tissues (uterus, vagina) while they have apparent class properties in others (bone, breast).2
The first SERM, for all practical purposes, was tamoxifen (although clomiphene citrate is often considered a SERM). Tamoxifen was approved by the US Food and Drug Administration (FDA) in 1978 for the treatment of breast cancer and, subsequently, for breast cancer risk reduction. It became the most widely prescribed anticancer drug worldwide.
Subsequently, when data showed that tamoxifen could produce a small number of endometrial cancers and a larger number of endometrial polyps,3,4 there was renewed interest in raloxifene. In preclinical animal studies, raloxifene behaved differently than tamoxifen in the uterus. After clinical trials with raloxifene showed uterine safety,5 the drug was FDA approved for prevention of osteoporosis in 1997, for treatment of osteoporosis in 1999, and for breast cancer risk reduction in 2009. Most clinicians are familiar with these 2 SERMs, which have been in clinical use for more than 4 and 2 decades, respectively.
Ospemifene: A third-generation SERM and its indications
Hormone deficiency from menopause causes vulvovaginal and urogenital changes as well as a multitude of symptoms and signs, including vulvar and vaginal thinning, loss of rugal folds, diminished elasticity, increased pH, and most notably dyspareunia. The nomenclature that previously described vulvovaginal atrophy (VVA) has been expanded to include genitourinary syndrome of menopause (GSM).6 Unfortunately, many health care providers do not ask patients about GSM symptoms, and few women report their symptoms to their clinician.7 Furthermore, although low-dose local estrogens applied vaginally have been the mainstay of therapy for VVA/GSM, only 7% of symptomatic women use any pharmacologic agent,8 mainly because of fear of estrogens due to the class labeling mentioned above.
Ospemifene, a newer SERM, improved superficial cells and reduced parabasal cells as seen on a maturation index compared with placebo, according to results of multiple phase 3 clinical trials9,10; it also lowered vaginal pH and improved most bothersome symptoms (original studies were for dyspareunia). As a result, the FDA approved ospemifene for treatment of moderate to severe dyspareunia from VVA of menopause.
Subsequent studies allowed for a broadened indication to include treatment of moderate to severe dryness due to menopause.11 The ospemifene label contains a boxed warning that states, “In the endometrium, [ospemifene] has estrogen agonistic effects.”12 Although ospemifene is not an estrogen (it’s a SERM), the label goes on to state, “There is an increased risk of endometrial cancer in a woman with a uterus who uses unopposed estrogens.” This statement caused The Medical Letter to initially suggest that patients who receive ospemifene also should receive a progestational agent—a suggestion they later retracted.13,14
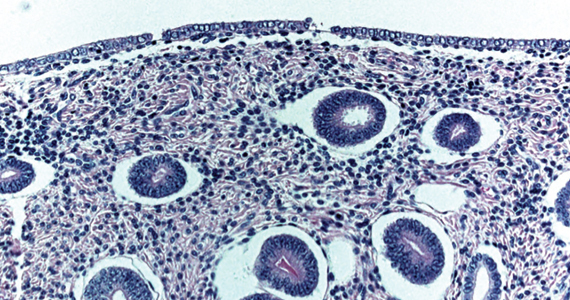
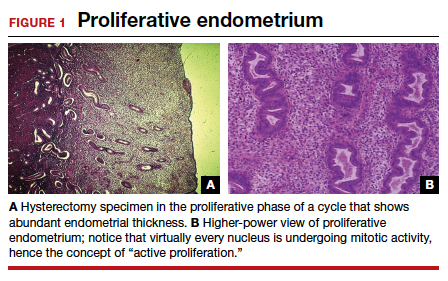
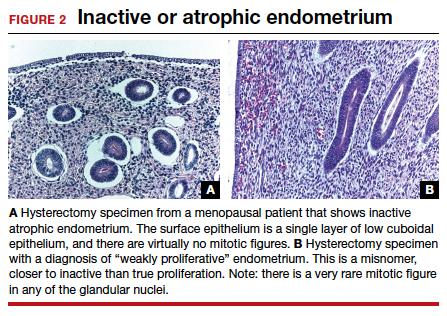
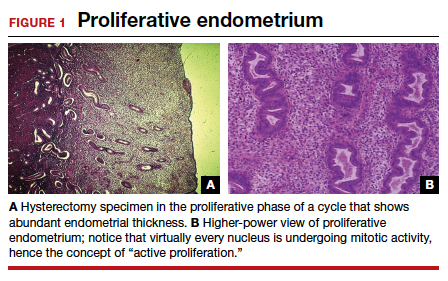
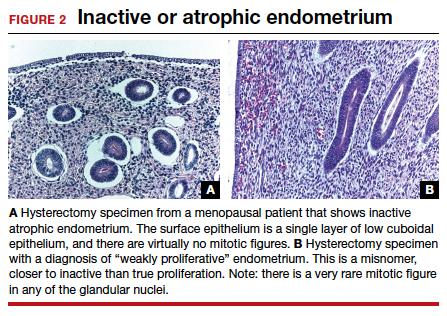
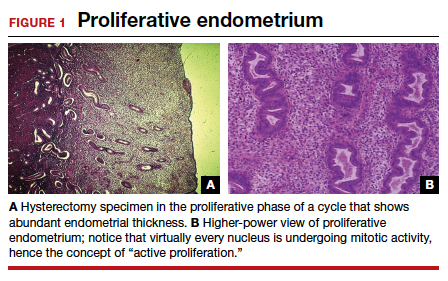
To understand why the ospemifene labeling might be worded in such a way, one must review the data regarding the poorly named entity “weakly proliferative endometrium.” The package labeling combines any proliferative endometrium (“weakly” plus “actively” plus “disordered”) that occurred in the clinical trial. Thus, 86.1 per 1,000 of the ospemifene-treated patients (vs 13.3 per 1,000 of those taking placebo) had any one of the proliferative types. The problem is that “actively proliferative” endometrial glands will have mitotic activity in virtually every nucleus of the gland as well as abundant glandular progression (FIGURE 1), whereas “weakly proliferative” is actually closer to inactive or atrophic endometrium with an occasional mitotic figure in only a few nuclei of each gland (FIGURE 2).
In addition, at 1 year, the incidence of active proliferation with ospemifene was 1%.15 In examining the uterine safety study for raloxifene, both doses of that agent had an active proliferation incidence of 3% at 1 year.5 Furthermore, that study had an estrogen-only arm in which, at end point, the incidence of endometrial proliferation was 39%, and hyperplasia, 23%!5 It therefore is evident that, in the endometrium, ospemifene is much more like the SERM raloxifene than it is like estrogen. The American College of Obstetricians and Gynecologists (ACOG) endorsed ospemifene (level A evidence) as a first-line therapy for dyspareunia, noting absent endometrial stimulation.16
Continue to: Ospemifene effects on breast and bone...
Ospemifene effects on breast and bone
Although ospemifene is approved for treatment of moderate to severe VVA/GSM, it has other SERM effects typical of its class. The label currently states that ospemifene “has not been adequately studied in women with breast cancer; therefore, it should not be used in women with known or suspected breast cancer.”12 We know that tamoxifen reduced breast cancer 49% in high-risk women in the Breast Cancer Prevention Trial (BCPT).17 We also know that in the Multiple Outcomes of Raloxifene Evaluation (MORE) trial, raloxifene reduced breast cancer 77% in osteoporotic women,18 and in the Study of Tamoxifen and Raloxifene (STAR) trial, it performed virtually identically to tamoxifen in breast cancer prevention.19 Previous studies demonstrated that ospemifene inhibits breast cancer cell growth in in vitro cultures as well as in animal studies20 and inhibits proliferation of human breast tissue epithelial cells,21 with breast effects similar to those seen with tamoxifen and raloxifene.
Thus, although one would not choose ospemifene as a primary treatment or risk-reducing agent for a patient with breast cancer, the direction of its activity in breast tissue is indisputable and is likely the reason that in the European Union (unlike in the United States) it is approved to treat dyspareunia from VVA/GSM in women with a prior history of breast cancer.
Virtually all SERMs have estrogen agonistic activity in bone. Bone is a dynamic organ, constantly being laid down and taken away (resorption). Estrogen and SERMs are potent antiresorptives in bone metabolism. Ospemifene effectively reduced bone loss in ovariectomized rats, with activity comparable to that of estradiol and raloxifene.22 Clinical data from 3 phase 1 or 2 clinical trials found that ospemifene 60 mg/day had a positive effect on biochemical markers for bone turnover in healthy postmenopausal women, with significant improvements relative to placebo and effects comparable to those of raloxifene.23 Actual fracture or bone mineral density (BMD) data in postmenopausal women are lacking, but there is a good correlation between biochemical markers for bone turnover and the occurrence of fracture.24 Once again, women who need treatment for osteoporosis should not be treated primarily with ospemifene, but women who use ospemifene for dyspareunia can expect positive activity on bone metabolism.
Clinical application
Ospemifene is an oral SERM approved for the treatment of moderate to severe dyspareunia as well as dryness from VVA due to menopause. In addition, it appears one can safely surmise that the direction of ospemifene’s activity in bone and breast is virtually indisputable. The magnitude of that activity, however, is unstudied. Therefore, in selecting an agent to treat women with dyspareunia or vaginal dryness from VVA of menopause, determining any potential add-on benefit for that particular patient in either bone and/or breast is clinically appropriate.
The SERM bazedoxifene
A meta-analysis of 4 randomized, placebo-controlled trials showed that another SERM, bazedoxifene, can significantly decrease the incidence of vertebral fracture in postmenopausal women at follow-up of 3 and 7 years.25 That meta-analysis also confirmed the long-term favorable safety and tolerability of bazedoxifene, with no increase in adverse events, serious adverse events, myocardial infarction, stroke, venous thromboembolic events, or breast carcinoma in patients using bazedoxifene. However, bazedoxifene use did result in an increased incidence of hot flushes and leg cramps across 7 years.25 Bazedoxifene is available in a 20-mg dose for treatment of postmenopausal osteoporosis in Israel and a number of European Union countries.
Continue to: Enter the concept of tissue-selective estrogen complex (TSEC)...
Enter the concept of tissue-selective estrogen complex (TSEC)
Some postmenopausal women are extremely intolerant of any progestogen added to estrogen therapy to confer endometrial protection in those with a uterus. According to the results of a clinical trial of postmenopausal women, bazedoxifene is the only SERM shown to decrease endometrial thickness compared with placebo.26 This is the basis for thinking that perhaps a SERM like bazedoxifene, instead of a progestogen, could be used to confer endometrial protection.
A further consideration comes out of the evaluation of data derived from the 2 arms of the Women’s Health Initiative (WHI).27 In the arm that combined conjugated estrogen with medroxyprogesterone acetate through 11.3 years, there was a 25% increase in the incidence of invasive breast cancer, which was statistically significant. Contrast that with the arm in hysterectomized women who received only conjugated estrogen (often inaccurately referred to as the “estrogen only” arm of the WHI). In that study arm, the relative risk of invasive breast cancer was reduced 23%, also statistically significant. Thus, the culprit in the breast cancer incidence difference in these 2 arms appears to be the addition of the progestogen medroxyprogesterone acetate.27
Since the progestogen was used only for endometrial protection, could such endometrial protection be provided by a SERM like bazedoxifene? Preclinical trials showed that a combination of bazedoxifene and conjugated estrogen (in various estrogen doses) resulted in uterine wet weight in an ovariectomized rat model that was no different than that with placebo.28
In terms of effects on breast, preclinical models showed that conjugated estrogen use resulted in less mammary duct elongation and end bud proliferation than estradiol by itself, and that the combination of conjugated estrogen and bazedoxifene resulted in mammary duct elongation and end bud proliferation that was similar to that in the ovariectomized animals and considerably less than a combination of estradiol with bazedoxifene.29
Five phase 3 studies known as the SMART (Selective estrogens, Menopause, And Response to Therapy) trials were then conducted. Collectively, these studies examined the frequency and severity of vasomotor symptoms (VMS), BMD, bone turnover markers, lipid profiles, sleep, quality of life, breast density, and endometrial safety with conjugated estrogen/bazedoxifene treatment.30 Based on these trials with more than 7,500 women, in 2013 the FDA approved a compound of conjugated estrogen 0.45 mg and bazedoxifene 20 mg (Duavee in the United States and Duavive outside the United States).
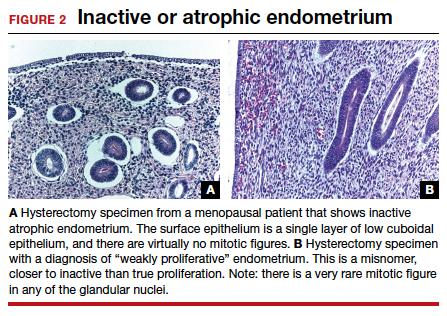
The incidence of endometrial hyperplasia at 12 months was consistently less than 1%, which is the FDA guidance for approval of hormone therapies. The incidence of bleeding or spotting with conjugated estrogen/bazedoxifene (FIGURE 3) in each 4-week interval over 12 months mirror-imaged that of placebo and ranged from 3.9% in the first 4-week interval to 1.7% in the last 4 weeks, compared with conjugated estrogen 0.45 mg/medroxyprogesterone acetate 1.5 mg, which had a 20.8% incidence of bleeding or spotting in the first 4-week interval and was still at an 8.8% incidence in the last 4 weeks.31 This is extremely relevant in clinical practice. There was no difference from placebo in breast cancer incidence, breast pain or tenderness, abnormal mammograms, or breast density at month 12.32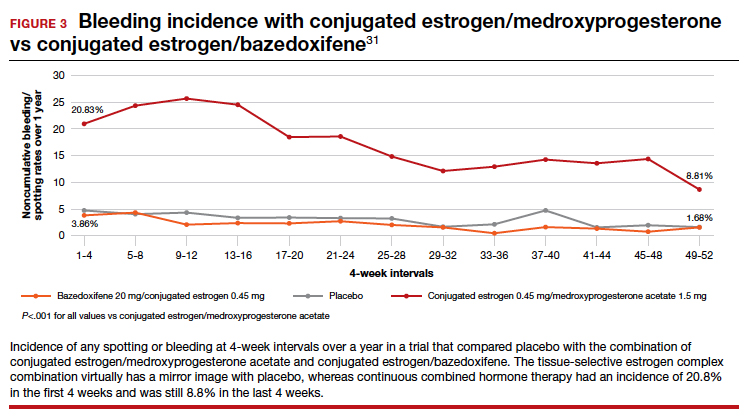
In terms of frequency of VMS, there was a 74% reduction from baseline at 12 weeks compared with placebo (P<.001), as well as a 37% reduction in the VMS severity score (P<.001).32 Statistically significant improvements occurred in lumbar spine and hip BMD (P<.01) for women who were 1 to 5 years since menopause as well as for those who were more than 5 years since menopause.33
Packaging issue puts TSEC on back order
In May 2020, Pfizer voluntarily recalled its conjugated estrogen/bazedoxifene product after identifying a “flaw in the drug’s foil laminate pouch that introduced oxygen and lowered the dissolution rate of active pharmaceutical ingredient bazedoxifene acetate.”34 The manufacturer then wrote a letter to health care professionals in September 2021 stating, “Duavee continues to be out of stock due to an unexpected and complex packaging issue, resulting in manufacturing delays. This has nothing to do with the safety or quality of the product itself but could affect product stability throughout its shelf life… Given regulatory approval timelines for any new packaging, it is unlikely that Duavee will return to stock in 2022.”35
Other TSECs?
The conjugated estrogen/bazedoxifene combination is the first FDA-approved TSEC. Other attempts have been made to achieve similar results with combined raloxifene and 17β-estradiol.36 That study was meant to be a 52-week treatment trial with either raloxifene 60 mg alone or in combination with 17β-estradiol 1 mg per day to assess effects on VMS and endometrial safety. The study was stopped early because signs of endometrial stimulation were observed in the raloxifene plus estradiol group. Thus, one cannot combine any estrogen with any SERM and assume similar results.
Clinical application
The combination of conjugated estrogen/bazedoxifene is approved for treatment of VMS of menopause as well as prevention of osteoporosis. Although it is not approved for treatment of moderate to severe VVA, in younger women who initiate treatment it should prevent the development of moderate to severe symptoms of VVA.
Finally, this drug should be protective of the breast. Conjugated estrogen has clearly shown a reduction in breast cancer incidence and mortality, and bazedoxifene is a SERM. All SERMs have, as a class effect, been shown to be antiestrogens in breast tissue, and abundant preclinical data point in that direction.
This combination of conjugated estrogen/bazedoxifene, when it is once again clinically available, may well provide a new paradigm of hormone therapy that is progestogen free and has a benefit/risk ratio that tilts toward its benefits.
Potential for wider therapeutic benefits
Newer SERMs like ospemifene, approved for treatment of VVA/GSM, and bazedoxifene/conjugated estrogen combination, approved for treatment of VMS and prevention of bone loss, have other beneficial properties that can and should result in their more widespread use. ●
- Stuenkel CA. More evidence why the product labeling for low-dose vaginal estrogen should be changed? Menopause. 2018;25:4-6.
- Goldstein SR. Not all SERMs are created equal. Menopause. 2006;13:325-327.
- Neven P, De Muylder X, Van Belle Y, et al. Hysteroscopic follow-up during tamoxifen treatment. Eur J Obstet Gynecol Reprod Biol. 1990;35:235-238.
- Schwartz LB, Snyder J, Horan C, et al. The use of transvaginal ultrasound and saline infusion sonohysterography for the evaluation of asymptomatic postmenopausal breast cancer patients on tamoxifen. Ultrasound Obstet Gynecol. 1998;11:48-53.
- Goldstein SR, Scheele WH, Rajagopalan SK, et al. A 12-month comparative study of raloxifene, estrogen, and placebo on the postmenopausal endometrium. Obstet Gynecol. 2000;95:95-103.
- Portman DJ, Gass MLS. Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21:1063-1068.
- Parish SJ, Nappi RE, Krychman ML, et al. Impact of vulvovaginal health on postmenopausal women: a review of surveys on symptoms of vulvovaginal atrophy. Int J Womens Health. 2013;5:437-447.
- Kingsberg SA, Krychman M, Graham S, et al. The Women’s EMPOWER Survey: identifying women’s perceptions on vulvar and vaginal atrophy and its treatment. J Sex Med. 2017;14:413-424.
- Bachmann GA, Komi JO; Ospemifene Study Group. Ospemifene effectively treats vulvovaginal atrophy in postmenopausal women: results from a pivotal phase 3 study. Menopause. 2010;17:480-486.
- Portman DJ, Bachmann GA, Simon JA; Ospemifene Study Group. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause. 2013;20:623-630.
- Archer DF, Goldstein SR, Simon JA, et al. Efficacy and safety of ospemifene in postmenopausal women with moderateto-severe vaginal dryness: a phase 3, randomized, doubleblind, placebo-controlled, multicenter trial. Menopause. 2019;26:611-621.
- Osphena. Package insert. Shionogi Inc; 2018.
- Ospemifene (Osphena) for dyspareunia. Med Lett Drugs Ther. 2013;55:55-56.
- Addendum: Ospemifene (Osphena) for dyspareunia (Med Lett Drugs Ther 2013;55:55). Med Lett Drugs Ther. 2013;55:84.
- Goldstein SR, Bachmann G, Lin V, et al. Endometrial safety profile of ospemifene 60 mg when used for long-term treatment of vulvar and vaginal atrophy for up to 1 year. Abstract. Climacteric. 2011;14(suppl 1):S57.
- ACOG practice bulletin no. 141: management of menopausal symptoms. Obstet Gynecol. 2014;123:202-216.
- Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371-1388.
- Cummings SR, Eckert S, Krueger KA, et al. The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple Outcomes of Raloxifene Evaluation. JAMA. 1999;281:2189-2197.
- Vogel VG, Costantino JP, Wickerham DL, et al; National Surgical Adjuvant Breast and Bowel Project (NSABP). Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295:2727-2741.
- Qu Q, Zheng H, Dahllund J, et al. Selective estrogenic effects of a novel triphenylethylene compound, FC1271a, on bone, cholesterol level, and reproductive tissues in intact and ovariectomized rats. Endocrinology. 2000;141:809-820.
- Eigeliene N, Kangas L, Hellmer C, et al. Effects of ospemifene, a novel selective estrogen-receptor modulator, on human breast tissue ex vivo. Menopause. 2016;23:719-730.
- Kangas L, Unkila M. Tissue selectivity of ospemifene: pharmacologic profile and clinical implications. Steroids. 2013;78:1273-1280.
- Constantine GD, Kagan R, Miller PD. Effects of ospemifene on bone parameters including clinical biomarkers in postmenopausal women. Menopause. 2016;23:638-644.
- Gerdhem P, Ivaska KK, Alatalo SL, et al. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res. 2004;19:386-393.
- Peng L, Luo Q, Lu H. Efficacy and safety of bazedoxifene in postmenopausal women with osteoporosis: a systematic review and meta-analysis. Medicine. 2017;96(49):e8659.
- Ronkin S, Northington R, Baracat E, et al. Endometrial effects of bazedoxifene acetate, a novel selective estrogen receptor modulator, in postmenopausal women. Obstet Gynecol. 2005;105:1397-1404.
- Anderson GL, Chlebowski RT, Aragaki AK, et al. Conjugated equine oestrogen and breast cancer incidence and mortality in postmenopausal women with hysterectomy: extended follow-up of the Women’s Health Initiative randomized placebo-controlled trial. Lancet Oncol. 2012;13:476-486.
- Kharode Y, Bodine PV, Miller CP, et al. The pairing of a selective estrogen receptor modulator, bazedoxifene, with conjugated estrogens as a new paradigm for the treatment of menopausal symptoms and osteoporosis prevention. Endocrinology. 2008;149:6084-6091.
- Song Y, Santen RJ, Wang JP, et al. Effects of the conjugated equine estrogen/bazedoxifene tissue-selective estrogen complex (TSEC) on mammary gland and breast cancer in mice. Endocrinology. 2012;153:5706-5715.
- Umland EM, Karel L, Santoro N. Bazedoxifene and conjugated equine estrogen: a combination product for the management of vasomotor symptoms and osteoporosis prevention associated with menopause. Pharmacotherapy. 2016;36:548-561.
- Kagan R, Goldstein SR, Pickar JH, et al. Patient considerations in the management of menopausal symptoms: role of conjugated estrogens with bazedoxifene. Ther Clin Risk Manag. 2016;12:549–562.
- Pinkerton JV, Harvey JA, Pan K, et al. Breast effects of bazedoxifene-conjugated estrogens: a randomized controlled trial. Obstet Gynecol. 2013;121:959-968.
- Lindsay R, Gallagher JC, Kagan R, et al. Efficacy of tissue-selective estrogen complex of bazedoxifene/ conjugated estrogens for osteoporosis prevention in at-risk postmenopausal women. Fertil Steril. 2009;92:1045-1052.
- Fierce Pharma. Pfizer continues recalls of menopause drug Duavee on faulty packaging concerns. https:// www.fiercepharma.com/manufacturing/pfizer-recallsmenopause-drug-duavive-uk-due-to-faulty-packagingworries. June 9, 2020. Accessed February 8, 2022.
- Pfizer. Letter to health care provider. Subject: Duavee (conjugated estrogens/bazedoxifene) extended drug shortage. September 10, 2021.
- Stovall DW, Utian WH, Gass MLS, et al. The effects of combined raloxifene and oral estrogen on vasomotor symptoms and endometrial safety. Menopause. 2007; 14(3 pt 1):510-517.
Selective estrogen receptor modulators (SERMs) are unique synthetic compounds that bind to the estrogen receptor and initiate either estrogenic agonistic or antagonistic activity, depending on the confirmational change they produce on binding to the receptor. Many SERMs have come to market, others have not. Unlike estrogens, which regardless of dose or route of administration all carry risks as a boxed warning on the label, referred to as class labeling,1 various SERMs exert various effects in some tissues (uterus, vagina) while they have apparent class properties in others (bone, breast).2
The first SERM, for all practical purposes, was tamoxifen (although clomiphene citrate is often considered a SERM). Tamoxifen was approved by the US Food and Drug Administration (FDA) in 1978 for the treatment of breast cancer and, subsequently, for breast cancer risk reduction. It became the most widely prescribed anticancer drug worldwide.
Subsequently, when data showed that tamoxifen could produce a small number of endometrial cancers and a larger number of endometrial polyps,3,4 there was renewed interest in raloxifene. In preclinical animal studies, raloxifene behaved differently than tamoxifen in the uterus. After clinical trials with raloxifene showed uterine safety,5 the drug was FDA approved for prevention of osteoporosis in 1997, for treatment of osteoporosis in 1999, and for breast cancer risk reduction in 2009. Most clinicians are familiar with these 2 SERMs, which have been in clinical use for more than 4 and 2 decades, respectively.
Ospemifene: A third-generation SERM and its indications
Hormone deficiency from menopause causes vulvovaginal and urogenital changes as well as a multitude of symptoms and signs, including vulvar and vaginal thinning, loss of rugal folds, diminished elasticity, increased pH, and most notably dyspareunia. The nomenclature that previously described vulvovaginal atrophy (VVA) has been expanded to include genitourinary syndrome of menopause (GSM).6 Unfortunately, many health care providers do not ask patients about GSM symptoms, and few women report their symptoms to their clinician.7 Furthermore, although low-dose local estrogens applied vaginally have been the mainstay of therapy for VVA/GSM, only 7% of symptomatic women use any pharmacologic agent,8 mainly because of fear of estrogens due to the class labeling mentioned above.
Ospemifene, a newer SERM, improved superficial cells and reduced parabasal cells as seen on a maturation index compared with placebo, according to results of multiple phase 3 clinical trials9,10; it also lowered vaginal pH and improved most bothersome symptoms (original studies were for dyspareunia). As a result, the FDA approved ospemifene for treatment of moderate to severe dyspareunia from VVA of menopause.
Subsequent studies allowed for a broadened indication to include treatment of moderate to severe dryness due to menopause.11 The ospemifene label contains a boxed warning that states, “In the endometrium, [ospemifene] has estrogen agonistic effects.”12 Although ospemifene is not an estrogen (it’s a SERM), the label goes on to state, “There is an increased risk of endometrial cancer in a woman with a uterus who uses unopposed estrogens.” This statement caused The Medical Letter to initially suggest that patients who receive ospemifene also should receive a progestational agent—a suggestion they later retracted.13,14
To understand why the ospemifene labeling might be worded in such a way, one must review the data regarding the poorly named entity “weakly proliferative endometrium.” The package labeling combines any proliferative endometrium (“weakly” plus “actively” plus “disordered”) that occurred in the clinical trial. Thus, 86.1 per 1,000 of the ospemifene-treated patients (vs 13.3 per 1,000 of those taking placebo) had any one of the proliferative types. The problem is that “actively proliferative” endometrial glands will have mitotic activity in virtually every nucleus of the gland as well as abundant glandular progression (FIGURE 1), whereas “weakly proliferative” is actually closer to inactive or atrophic endometrium with an occasional mitotic figure in only a few nuclei of each gland (FIGURE 2).
In addition, at 1 year, the incidence of active proliferation with ospemifene was 1%.15 In examining the uterine safety study for raloxifene, both doses of that agent had an active proliferation incidence of 3% at 1 year.5 Furthermore, that study had an estrogen-only arm in which, at end point, the incidence of endometrial proliferation was 39%, and hyperplasia, 23%!5 It therefore is evident that, in the endometrium, ospemifene is much more like the SERM raloxifene than it is like estrogen. The American College of Obstetricians and Gynecologists (ACOG) endorsed ospemifene (level A evidence) as a first-line therapy for dyspareunia, noting absent endometrial stimulation.16
Continue to: Ospemifene effects on breast and bone...
Ospemifene effects on breast and bone
Although ospemifene is approved for treatment of moderate to severe VVA/GSM, it has other SERM effects typical of its class. The label currently states that ospemifene “has not been adequately studied in women with breast cancer; therefore, it should not be used in women with known or suspected breast cancer.”12 We know that tamoxifen reduced breast cancer 49% in high-risk women in the Breast Cancer Prevention Trial (BCPT).17 We also know that in the Multiple Outcomes of Raloxifene Evaluation (MORE) trial, raloxifene reduced breast cancer 77% in osteoporotic women,18 and in the Study of Tamoxifen and Raloxifene (STAR) trial, it performed virtually identically to tamoxifen in breast cancer prevention.19 Previous studies demonstrated that ospemifene inhibits breast cancer cell growth in in vitro cultures as well as in animal studies20 and inhibits proliferation of human breast tissue epithelial cells,21 with breast effects similar to those seen with tamoxifen and raloxifene.
Thus, although one would not choose ospemifene as a primary treatment or risk-reducing agent for a patient with breast cancer, the direction of its activity in breast tissue is indisputable and is likely the reason that in the European Union (unlike in the United States) it is approved to treat dyspareunia from VVA/GSM in women with a prior history of breast cancer.
Virtually all SERMs have estrogen agonistic activity in bone. Bone is a dynamic organ, constantly being laid down and taken away (resorption). Estrogen and SERMs are potent antiresorptives in bone metabolism. Ospemifene effectively reduced bone loss in ovariectomized rats, with activity comparable to that of estradiol and raloxifene.22 Clinical data from 3 phase 1 or 2 clinical trials found that ospemifene 60 mg/day had a positive effect on biochemical markers for bone turnover in healthy postmenopausal women, with significant improvements relative to placebo and effects comparable to those of raloxifene.23 Actual fracture or bone mineral density (BMD) data in postmenopausal women are lacking, but there is a good correlation between biochemical markers for bone turnover and the occurrence of fracture.24 Once again, women who need treatment for osteoporosis should not be treated primarily with ospemifene, but women who use ospemifene for dyspareunia can expect positive activity on bone metabolism.
Clinical application
Ospemifene is an oral SERM approved for the treatment of moderate to severe dyspareunia as well as dryness from VVA due to menopause. In addition, it appears one can safely surmise that the direction of ospemifene’s activity in bone and breast is virtually indisputable. The magnitude of that activity, however, is unstudied. Therefore, in selecting an agent to treat women with dyspareunia or vaginal dryness from VVA of menopause, determining any potential add-on benefit for that particular patient in either bone and/or breast is clinically appropriate.
The SERM bazedoxifene
A meta-analysis of 4 randomized, placebo-controlled trials showed that another SERM, bazedoxifene, can significantly decrease the incidence of vertebral fracture in postmenopausal women at follow-up of 3 and 7 years.25 That meta-analysis also confirmed the long-term favorable safety and tolerability of bazedoxifene, with no increase in adverse events, serious adverse events, myocardial infarction, stroke, venous thromboembolic events, or breast carcinoma in patients using bazedoxifene. However, bazedoxifene use did result in an increased incidence of hot flushes and leg cramps across 7 years.25 Bazedoxifene is available in a 20-mg dose for treatment of postmenopausal osteoporosis in Israel and a number of European Union countries.
Continue to: Enter the concept of tissue-selective estrogen complex (TSEC)...
Enter the concept of tissue-selective estrogen complex (TSEC)
Some postmenopausal women are extremely intolerant of any progestogen added to estrogen therapy to confer endometrial protection in those with a uterus. According to the results of a clinical trial of postmenopausal women, bazedoxifene is the only SERM shown to decrease endometrial thickness compared with placebo.26 This is the basis for thinking that perhaps a SERM like bazedoxifene, instead of a progestogen, could be used to confer endometrial protection.
A further consideration comes out of the evaluation of data derived from the 2 arms of the Women’s Health Initiative (WHI).27 In the arm that combined conjugated estrogen with medroxyprogesterone acetate through 11.3 years, there was a 25% increase in the incidence of invasive breast cancer, which was statistically significant. Contrast that with the arm in hysterectomized women who received only conjugated estrogen (often inaccurately referred to as the “estrogen only” arm of the WHI). In that study arm, the relative risk of invasive breast cancer was reduced 23%, also statistically significant. Thus, the culprit in the breast cancer incidence difference in these 2 arms appears to be the addition of the progestogen medroxyprogesterone acetate.27
Since the progestogen was used only for endometrial protection, could such endometrial protection be provided by a SERM like bazedoxifene? Preclinical trials showed that a combination of bazedoxifene and conjugated estrogen (in various estrogen doses) resulted in uterine wet weight in an ovariectomized rat model that was no different than that with placebo.28
In terms of effects on breast, preclinical models showed that conjugated estrogen use resulted in less mammary duct elongation and end bud proliferation than estradiol by itself, and that the combination of conjugated estrogen and bazedoxifene resulted in mammary duct elongation and end bud proliferation that was similar to that in the ovariectomized animals and considerably less than a combination of estradiol with bazedoxifene.29
Five phase 3 studies known as the SMART (Selective estrogens, Menopause, And Response to Therapy) trials were then conducted. Collectively, these studies examined the frequency and severity of vasomotor symptoms (VMS), BMD, bone turnover markers, lipid profiles, sleep, quality of life, breast density, and endometrial safety with conjugated estrogen/bazedoxifene treatment.30 Based on these trials with more than 7,500 women, in 2013 the FDA approved a compound of conjugated estrogen 0.45 mg and bazedoxifene 20 mg (Duavee in the United States and Duavive outside the United States).
The incidence of endometrial hyperplasia at 12 months was consistently less than 1%, which is the FDA guidance for approval of hormone therapies. The incidence of bleeding or spotting with conjugated estrogen/bazedoxifene (FIGURE 3) in each 4-week interval over 12 months mirror-imaged that of placebo and ranged from 3.9% in the first 4-week interval to 1.7% in the last 4 weeks, compared with conjugated estrogen 0.45 mg/medroxyprogesterone acetate 1.5 mg, which had a 20.8% incidence of bleeding or spotting in the first 4-week interval and was still at an 8.8% incidence in the last 4 weeks.31 This is extremely relevant in clinical practice. There was no difference from placebo in breast cancer incidence, breast pain or tenderness, abnormal mammograms, or breast density at month 12.32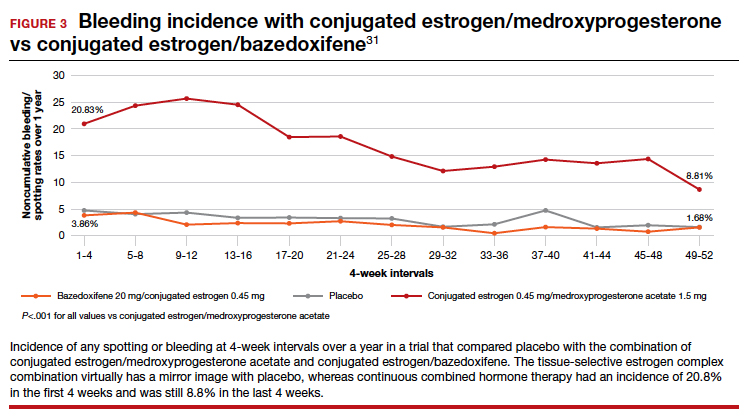
In terms of frequency of VMS, there was a 74% reduction from baseline at 12 weeks compared with placebo (P<.001), as well as a 37% reduction in the VMS severity score (P<.001).32 Statistically significant improvements occurred in lumbar spine and hip BMD (P<.01) for women who were 1 to 5 years since menopause as well as for those who were more than 5 years since menopause.33
Packaging issue puts TSEC on back order
In May 2020, Pfizer voluntarily recalled its conjugated estrogen/bazedoxifene product after identifying a “flaw in the drug’s foil laminate pouch that introduced oxygen and lowered the dissolution rate of active pharmaceutical ingredient bazedoxifene acetate.”34 The manufacturer then wrote a letter to health care professionals in September 2021 stating, “Duavee continues to be out of stock due to an unexpected and complex packaging issue, resulting in manufacturing delays. This has nothing to do with the safety or quality of the product itself but could affect product stability throughout its shelf life… Given regulatory approval timelines for any new packaging, it is unlikely that Duavee will return to stock in 2022.”35
Other TSECs?
The conjugated estrogen/bazedoxifene combination is the first FDA-approved TSEC. Other attempts have been made to achieve similar results with combined raloxifene and 17β-estradiol.36 That study was meant to be a 52-week treatment trial with either raloxifene 60 mg alone or in combination with 17β-estradiol 1 mg per day to assess effects on VMS and endometrial safety. The study was stopped early because signs of endometrial stimulation were observed in the raloxifene plus estradiol group. Thus, one cannot combine any estrogen with any SERM and assume similar results.
Clinical application
The combination of conjugated estrogen/bazedoxifene is approved for treatment of VMS of menopause as well as prevention of osteoporosis. Although it is not approved for treatment of moderate to severe VVA, in younger women who initiate treatment it should prevent the development of moderate to severe symptoms of VVA.
Finally, this drug should be protective of the breast. Conjugated estrogen has clearly shown a reduction in breast cancer incidence and mortality, and bazedoxifene is a SERM. All SERMs have, as a class effect, been shown to be antiestrogens in breast tissue, and abundant preclinical data point in that direction.
This combination of conjugated estrogen/bazedoxifene, when it is once again clinically available, may well provide a new paradigm of hormone therapy that is progestogen free and has a benefit/risk ratio that tilts toward its benefits.
Potential for wider therapeutic benefits
Newer SERMs like ospemifene, approved for treatment of VVA/GSM, and bazedoxifene/conjugated estrogen combination, approved for treatment of VMS and prevention of bone loss, have other beneficial properties that can and should result in their more widespread use. ●
Selective estrogen receptor modulators (SERMs) are unique synthetic compounds that bind to the estrogen receptor and initiate either estrogenic agonistic or antagonistic activity, depending on the confirmational change they produce on binding to the receptor. Many SERMs have come to market, others have not. Unlike estrogens, which regardless of dose or route of administration all carry risks as a boxed warning on the label, referred to as class labeling,1 various SERMs exert various effects in some tissues (uterus, vagina) while they have apparent class properties in others (bone, breast).2
The first SERM, for all practical purposes, was tamoxifen (although clomiphene citrate is often considered a SERM). Tamoxifen was approved by the US Food and Drug Administration (FDA) in 1978 for the treatment of breast cancer and, subsequently, for breast cancer risk reduction. It became the most widely prescribed anticancer drug worldwide.
Subsequently, when data showed that tamoxifen could produce a small number of endometrial cancers and a larger number of endometrial polyps,3,4 there was renewed interest in raloxifene. In preclinical animal studies, raloxifene behaved differently than tamoxifen in the uterus. After clinical trials with raloxifene showed uterine safety,5 the drug was FDA approved for prevention of osteoporosis in 1997, for treatment of osteoporosis in 1999, and for breast cancer risk reduction in 2009. Most clinicians are familiar with these 2 SERMs, which have been in clinical use for more than 4 and 2 decades, respectively.
Ospemifene: A third-generation SERM and its indications
Hormone deficiency from menopause causes vulvovaginal and urogenital changes as well as a multitude of symptoms and signs, including vulvar and vaginal thinning, loss of rugal folds, diminished elasticity, increased pH, and most notably dyspareunia. The nomenclature that previously described vulvovaginal atrophy (VVA) has been expanded to include genitourinary syndrome of menopause (GSM).6 Unfortunately, many health care providers do not ask patients about GSM symptoms, and few women report their symptoms to their clinician.7 Furthermore, although low-dose local estrogens applied vaginally have been the mainstay of therapy for VVA/GSM, only 7% of symptomatic women use any pharmacologic agent,8 mainly because of fear of estrogens due to the class labeling mentioned above.
Ospemifene, a newer SERM, improved superficial cells and reduced parabasal cells as seen on a maturation index compared with placebo, according to results of multiple phase 3 clinical trials9,10; it also lowered vaginal pH and improved most bothersome symptoms (original studies were for dyspareunia). As a result, the FDA approved ospemifene for treatment of moderate to severe dyspareunia from VVA of menopause.
Subsequent studies allowed for a broadened indication to include treatment of moderate to severe dryness due to menopause.11 The ospemifene label contains a boxed warning that states, “In the endometrium, [ospemifene] has estrogen agonistic effects.”12 Although ospemifene is not an estrogen (it’s a SERM), the label goes on to state, “There is an increased risk of endometrial cancer in a woman with a uterus who uses unopposed estrogens.” This statement caused The Medical Letter to initially suggest that patients who receive ospemifene also should receive a progestational agent—a suggestion they later retracted.13,14
To understand why the ospemifene labeling might be worded in such a way, one must review the data regarding the poorly named entity “weakly proliferative endometrium.” The package labeling combines any proliferative endometrium (“weakly” plus “actively” plus “disordered”) that occurred in the clinical trial. Thus, 86.1 per 1,000 of the ospemifene-treated patients (vs 13.3 per 1,000 of those taking placebo) had any one of the proliferative types. The problem is that “actively proliferative” endometrial glands will have mitotic activity in virtually every nucleus of the gland as well as abundant glandular progression (FIGURE 1), whereas “weakly proliferative” is actually closer to inactive or atrophic endometrium with an occasional mitotic figure in only a few nuclei of each gland (FIGURE 2).
In addition, at 1 year, the incidence of active proliferation with ospemifene was 1%.15 In examining the uterine safety study for raloxifene, both doses of that agent had an active proliferation incidence of 3% at 1 year.5 Furthermore, that study had an estrogen-only arm in which, at end point, the incidence of endometrial proliferation was 39%, and hyperplasia, 23%!5 It therefore is evident that, in the endometrium, ospemifene is much more like the SERM raloxifene than it is like estrogen. The American College of Obstetricians and Gynecologists (ACOG) endorsed ospemifene (level A evidence) as a first-line therapy for dyspareunia, noting absent endometrial stimulation.16
Continue to: Ospemifene effects on breast and bone...
Ospemifene effects on breast and bone
Although ospemifene is approved for treatment of moderate to severe VVA/GSM, it has other SERM effects typical of its class. The label currently states that ospemifene “has not been adequately studied in women with breast cancer; therefore, it should not be used in women with known or suspected breast cancer.”12 We know that tamoxifen reduced breast cancer 49% in high-risk women in the Breast Cancer Prevention Trial (BCPT).17 We also know that in the Multiple Outcomes of Raloxifene Evaluation (MORE) trial, raloxifene reduced breast cancer 77% in osteoporotic women,18 and in the Study of Tamoxifen and Raloxifene (STAR) trial, it performed virtually identically to tamoxifen in breast cancer prevention.19 Previous studies demonstrated that ospemifene inhibits breast cancer cell growth in in vitro cultures as well as in animal studies20 and inhibits proliferation of human breast tissue epithelial cells,21 with breast effects similar to those seen with tamoxifen and raloxifene.
Thus, although one would not choose ospemifene as a primary treatment or risk-reducing agent for a patient with breast cancer, the direction of its activity in breast tissue is indisputable and is likely the reason that in the European Union (unlike in the United States) it is approved to treat dyspareunia from VVA/GSM in women with a prior history of breast cancer.
Virtually all SERMs have estrogen agonistic activity in bone. Bone is a dynamic organ, constantly being laid down and taken away (resorption). Estrogen and SERMs are potent antiresorptives in bone metabolism. Ospemifene effectively reduced bone loss in ovariectomized rats, with activity comparable to that of estradiol and raloxifene.22 Clinical data from 3 phase 1 or 2 clinical trials found that ospemifene 60 mg/day had a positive effect on biochemical markers for bone turnover in healthy postmenopausal women, with significant improvements relative to placebo and effects comparable to those of raloxifene.23 Actual fracture or bone mineral density (BMD) data in postmenopausal women are lacking, but there is a good correlation between biochemical markers for bone turnover and the occurrence of fracture.24 Once again, women who need treatment for osteoporosis should not be treated primarily with ospemifene, but women who use ospemifene for dyspareunia can expect positive activity on bone metabolism.
Clinical application
Ospemifene is an oral SERM approved for the treatment of moderate to severe dyspareunia as well as dryness from VVA due to menopause. In addition, it appears one can safely surmise that the direction of ospemifene’s activity in bone and breast is virtually indisputable. The magnitude of that activity, however, is unstudied. Therefore, in selecting an agent to treat women with dyspareunia or vaginal dryness from VVA of menopause, determining any potential add-on benefit for that particular patient in either bone and/or breast is clinically appropriate.
The SERM bazedoxifene
A meta-analysis of 4 randomized, placebo-controlled trials showed that another SERM, bazedoxifene, can significantly decrease the incidence of vertebral fracture in postmenopausal women at follow-up of 3 and 7 years.25 That meta-analysis also confirmed the long-term favorable safety and tolerability of bazedoxifene, with no increase in adverse events, serious adverse events, myocardial infarction, stroke, venous thromboembolic events, or breast carcinoma in patients using bazedoxifene. However, bazedoxifene use did result in an increased incidence of hot flushes and leg cramps across 7 years.25 Bazedoxifene is available in a 20-mg dose for treatment of postmenopausal osteoporosis in Israel and a number of European Union countries.
Continue to: Enter the concept of tissue-selective estrogen complex (TSEC)...
Enter the concept of tissue-selective estrogen complex (TSEC)
Some postmenopausal women are extremely intolerant of any progestogen added to estrogen therapy to confer endometrial protection in those with a uterus. According to the results of a clinical trial of postmenopausal women, bazedoxifene is the only SERM shown to decrease endometrial thickness compared with placebo.26 This is the basis for thinking that perhaps a SERM like bazedoxifene, instead of a progestogen, could be used to confer endometrial protection.
A further consideration comes out of the evaluation of data derived from the 2 arms of the Women’s Health Initiative (WHI).27 In the arm that combined conjugated estrogen with medroxyprogesterone acetate through 11.3 years, there was a 25% increase in the incidence of invasive breast cancer, which was statistically significant. Contrast that with the arm in hysterectomized women who received only conjugated estrogen (often inaccurately referred to as the “estrogen only” arm of the WHI). In that study arm, the relative risk of invasive breast cancer was reduced 23%, also statistically significant. Thus, the culprit in the breast cancer incidence difference in these 2 arms appears to be the addition of the progestogen medroxyprogesterone acetate.27
Since the progestogen was used only for endometrial protection, could such endometrial protection be provided by a SERM like bazedoxifene? Preclinical trials showed that a combination of bazedoxifene and conjugated estrogen (in various estrogen doses) resulted in uterine wet weight in an ovariectomized rat model that was no different than that with placebo.28
In terms of effects on breast, preclinical models showed that conjugated estrogen use resulted in less mammary duct elongation and end bud proliferation than estradiol by itself, and that the combination of conjugated estrogen and bazedoxifene resulted in mammary duct elongation and end bud proliferation that was similar to that in the ovariectomized animals and considerably less than a combination of estradiol with bazedoxifene.29
Five phase 3 studies known as the SMART (Selective estrogens, Menopause, And Response to Therapy) trials were then conducted. Collectively, these studies examined the frequency and severity of vasomotor symptoms (VMS), BMD, bone turnover markers, lipid profiles, sleep, quality of life, breast density, and endometrial safety with conjugated estrogen/bazedoxifene treatment.30 Based on these trials with more than 7,500 women, in 2013 the FDA approved a compound of conjugated estrogen 0.45 mg and bazedoxifene 20 mg (Duavee in the United States and Duavive outside the United States).
The incidence of endometrial hyperplasia at 12 months was consistently less than 1%, which is the FDA guidance for approval of hormone therapies. The incidence of bleeding or spotting with conjugated estrogen/bazedoxifene (FIGURE 3) in each 4-week interval over 12 months mirror-imaged that of placebo and ranged from 3.9% in the first 4-week interval to 1.7% in the last 4 weeks, compared with conjugated estrogen 0.45 mg/medroxyprogesterone acetate 1.5 mg, which had a 20.8% incidence of bleeding or spotting in the first 4-week interval and was still at an 8.8% incidence in the last 4 weeks.31 This is extremely relevant in clinical practice. There was no difference from placebo in breast cancer incidence, breast pain or tenderness, abnormal mammograms, or breast density at month 12.32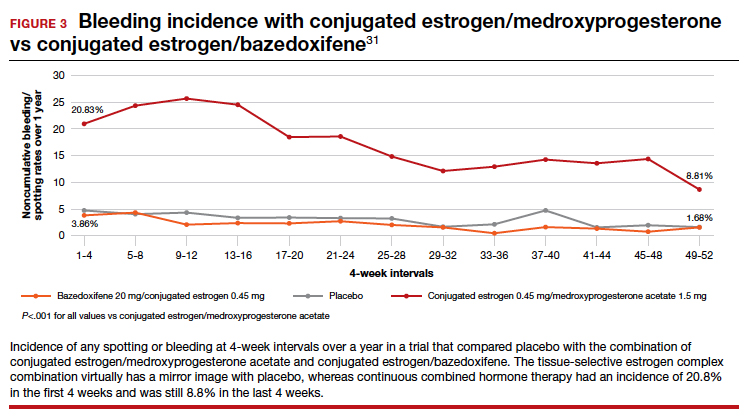
In terms of frequency of VMS, there was a 74% reduction from baseline at 12 weeks compared with placebo (P<.001), as well as a 37% reduction in the VMS severity score (P<.001).32 Statistically significant improvements occurred in lumbar spine and hip BMD (P<.01) for women who were 1 to 5 years since menopause as well as for those who were more than 5 years since menopause.33
Packaging issue puts TSEC on back order
In May 2020, Pfizer voluntarily recalled its conjugated estrogen/bazedoxifene product after identifying a “flaw in the drug’s foil laminate pouch that introduced oxygen and lowered the dissolution rate of active pharmaceutical ingredient bazedoxifene acetate.”34 The manufacturer then wrote a letter to health care professionals in September 2021 stating, “Duavee continues to be out of stock due to an unexpected and complex packaging issue, resulting in manufacturing delays. This has nothing to do with the safety or quality of the product itself but could affect product stability throughout its shelf life… Given regulatory approval timelines for any new packaging, it is unlikely that Duavee will return to stock in 2022.”35
Other TSECs?
The conjugated estrogen/bazedoxifene combination is the first FDA-approved TSEC. Other attempts have been made to achieve similar results with combined raloxifene and 17β-estradiol.36 That study was meant to be a 52-week treatment trial with either raloxifene 60 mg alone or in combination with 17β-estradiol 1 mg per day to assess effects on VMS and endometrial safety. The study was stopped early because signs of endometrial stimulation were observed in the raloxifene plus estradiol group. Thus, one cannot combine any estrogen with any SERM and assume similar results.
Clinical application
The combination of conjugated estrogen/bazedoxifene is approved for treatment of VMS of menopause as well as prevention of osteoporosis. Although it is not approved for treatment of moderate to severe VVA, in younger women who initiate treatment it should prevent the development of moderate to severe symptoms of VVA.
Finally, this drug should be protective of the breast. Conjugated estrogen has clearly shown a reduction in breast cancer incidence and mortality, and bazedoxifene is a SERM. All SERMs have, as a class effect, been shown to be antiestrogens in breast tissue, and abundant preclinical data point in that direction.
This combination of conjugated estrogen/bazedoxifene, when it is once again clinically available, may well provide a new paradigm of hormone therapy that is progestogen free and has a benefit/risk ratio that tilts toward its benefits.
Potential for wider therapeutic benefits
Newer SERMs like ospemifene, approved for treatment of VVA/GSM, and bazedoxifene/conjugated estrogen combination, approved for treatment of VMS and prevention of bone loss, have other beneficial properties that can and should result in their more widespread use. ●
- Stuenkel CA. More evidence why the product labeling for low-dose vaginal estrogen should be changed? Menopause. 2018;25:4-6.
- Goldstein SR. Not all SERMs are created equal. Menopause. 2006;13:325-327.
- Neven P, De Muylder X, Van Belle Y, et al. Hysteroscopic follow-up during tamoxifen treatment. Eur J Obstet Gynecol Reprod Biol. 1990;35:235-238.
- Schwartz LB, Snyder J, Horan C, et al. The use of transvaginal ultrasound and saline infusion sonohysterography for the evaluation of asymptomatic postmenopausal breast cancer patients on tamoxifen. Ultrasound Obstet Gynecol. 1998;11:48-53.
- Goldstein SR, Scheele WH, Rajagopalan SK, et al. A 12-month comparative study of raloxifene, estrogen, and placebo on the postmenopausal endometrium. Obstet Gynecol. 2000;95:95-103.
- Portman DJ, Gass MLS. Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21:1063-1068.
- Parish SJ, Nappi RE, Krychman ML, et al. Impact of vulvovaginal health on postmenopausal women: a review of surveys on symptoms of vulvovaginal atrophy. Int J Womens Health. 2013;5:437-447.
- Kingsberg SA, Krychman M, Graham S, et al. The Women’s EMPOWER Survey: identifying women’s perceptions on vulvar and vaginal atrophy and its treatment. J Sex Med. 2017;14:413-424.
- Bachmann GA, Komi JO; Ospemifene Study Group. Ospemifene effectively treats vulvovaginal atrophy in postmenopausal women: results from a pivotal phase 3 study. Menopause. 2010;17:480-486.
- Portman DJ, Bachmann GA, Simon JA; Ospemifene Study Group. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause. 2013;20:623-630.
- Archer DF, Goldstein SR, Simon JA, et al. Efficacy and safety of ospemifene in postmenopausal women with moderateto-severe vaginal dryness: a phase 3, randomized, doubleblind, placebo-controlled, multicenter trial. Menopause. 2019;26:611-621.
- Osphena. Package insert. Shionogi Inc; 2018.
- Ospemifene (Osphena) for dyspareunia. Med Lett Drugs Ther. 2013;55:55-56.
- Addendum: Ospemifene (Osphena) for dyspareunia (Med Lett Drugs Ther 2013;55:55). Med Lett Drugs Ther. 2013;55:84.
- Goldstein SR, Bachmann G, Lin V, et al. Endometrial safety profile of ospemifene 60 mg when used for long-term treatment of vulvar and vaginal atrophy for up to 1 year. Abstract. Climacteric. 2011;14(suppl 1):S57.
- ACOG practice bulletin no. 141: management of menopausal symptoms. Obstet Gynecol. 2014;123:202-216.
- Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371-1388.
- Cummings SR, Eckert S, Krueger KA, et al. The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple Outcomes of Raloxifene Evaluation. JAMA. 1999;281:2189-2197.
- Vogel VG, Costantino JP, Wickerham DL, et al; National Surgical Adjuvant Breast and Bowel Project (NSABP). Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295:2727-2741.
- Qu Q, Zheng H, Dahllund J, et al. Selective estrogenic effects of a novel triphenylethylene compound, FC1271a, on bone, cholesterol level, and reproductive tissues in intact and ovariectomized rats. Endocrinology. 2000;141:809-820.
- Eigeliene N, Kangas L, Hellmer C, et al. Effects of ospemifene, a novel selective estrogen-receptor modulator, on human breast tissue ex vivo. Menopause. 2016;23:719-730.
- Kangas L, Unkila M. Tissue selectivity of ospemifene: pharmacologic profile and clinical implications. Steroids. 2013;78:1273-1280.
- Constantine GD, Kagan R, Miller PD. Effects of ospemifene on bone parameters including clinical biomarkers in postmenopausal women. Menopause. 2016;23:638-644.
- Gerdhem P, Ivaska KK, Alatalo SL, et al. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res. 2004;19:386-393.
- Peng L, Luo Q, Lu H. Efficacy and safety of bazedoxifene in postmenopausal women with osteoporosis: a systematic review and meta-analysis. Medicine. 2017;96(49):e8659.
- Ronkin S, Northington R, Baracat E, et al. Endometrial effects of bazedoxifene acetate, a novel selective estrogen receptor modulator, in postmenopausal women. Obstet Gynecol. 2005;105:1397-1404.
- Anderson GL, Chlebowski RT, Aragaki AK, et al. Conjugated equine oestrogen and breast cancer incidence and mortality in postmenopausal women with hysterectomy: extended follow-up of the Women’s Health Initiative randomized placebo-controlled trial. Lancet Oncol. 2012;13:476-486.
- Kharode Y, Bodine PV, Miller CP, et al. The pairing of a selective estrogen receptor modulator, bazedoxifene, with conjugated estrogens as a new paradigm for the treatment of menopausal symptoms and osteoporosis prevention. Endocrinology. 2008;149:6084-6091.
- Song Y, Santen RJ, Wang JP, et al. Effects of the conjugated equine estrogen/bazedoxifene tissue-selective estrogen complex (TSEC) on mammary gland and breast cancer in mice. Endocrinology. 2012;153:5706-5715.
- Umland EM, Karel L, Santoro N. Bazedoxifene and conjugated equine estrogen: a combination product for the management of vasomotor symptoms and osteoporosis prevention associated with menopause. Pharmacotherapy. 2016;36:548-561.
- Kagan R, Goldstein SR, Pickar JH, et al. Patient considerations in the management of menopausal symptoms: role of conjugated estrogens with bazedoxifene. Ther Clin Risk Manag. 2016;12:549–562.
- Pinkerton JV, Harvey JA, Pan K, et al. Breast effects of bazedoxifene-conjugated estrogens: a randomized controlled trial. Obstet Gynecol. 2013;121:959-968.
- Lindsay R, Gallagher JC, Kagan R, et al. Efficacy of tissue-selective estrogen complex of bazedoxifene/ conjugated estrogens for osteoporosis prevention in at-risk postmenopausal women. Fertil Steril. 2009;92:1045-1052.
- Fierce Pharma. Pfizer continues recalls of menopause drug Duavee on faulty packaging concerns. https:// www.fiercepharma.com/manufacturing/pfizer-recallsmenopause-drug-duavive-uk-due-to-faulty-packagingworries. June 9, 2020. Accessed February 8, 2022.
- Pfizer. Letter to health care provider. Subject: Duavee (conjugated estrogens/bazedoxifene) extended drug shortage. September 10, 2021.
- Stovall DW, Utian WH, Gass MLS, et al. The effects of combined raloxifene and oral estrogen on vasomotor symptoms and endometrial safety. Menopause. 2007; 14(3 pt 1):510-517.
- Stuenkel CA. More evidence why the product labeling for low-dose vaginal estrogen should be changed? Menopause. 2018;25:4-6.
- Goldstein SR. Not all SERMs are created equal. Menopause. 2006;13:325-327.
- Neven P, De Muylder X, Van Belle Y, et al. Hysteroscopic follow-up during tamoxifen treatment. Eur J Obstet Gynecol Reprod Biol. 1990;35:235-238.
- Schwartz LB, Snyder J, Horan C, et al. The use of transvaginal ultrasound and saline infusion sonohysterography for the evaluation of asymptomatic postmenopausal breast cancer patients on tamoxifen. Ultrasound Obstet Gynecol. 1998;11:48-53.
- Goldstein SR, Scheele WH, Rajagopalan SK, et al. A 12-month comparative study of raloxifene, estrogen, and placebo on the postmenopausal endometrium. Obstet Gynecol. 2000;95:95-103.
- Portman DJ, Gass MLS. Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21:1063-1068.
- Parish SJ, Nappi RE, Krychman ML, et al. Impact of vulvovaginal health on postmenopausal women: a review of surveys on symptoms of vulvovaginal atrophy. Int J Womens Health. 2013;5:437-447.
- Kingsberg SA, Krychman M, Graham S, et al. The Women’s EMPOWER Survey: identifying women’s perceptions on vulvar and vaginal atrophy and its treatment. J Sex Med. 2017;14:413-424.
- Bachmann GA, Komi JO; Ospemifene Study Group. Ospemifene effectively treats vulvovaginal atrophy in postmenopausal women: results from a pivotal phase 3 study. Menopause. 2010;17:480-486.
- Portman DJ, Bachmann GA, Simon JA; Ospemifene Study Group. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause. 2013;20:623-630.
- Archer DF, Goldstein SR, Simon JA, et al. Efficacy and safety of ospemifene in postmenopausal women with moderateto-severe vaginal dryness: a phase 3, randomized, doubleblind, placebo-controlled, multicenter trial. Menopause. 2019;26:611-621.
- Osphena. Package insert. Shionogi Inc; 2018.
- Ospemifene (Osphena) for dyspareunia. Med Lett Drugs Ther. 2013;55:55-56.
- Addendum: Ospemifene (Osphena) for dyspareunia (Med Lett Drugs Ther 2013;55:55). Med Lett Drugs Ther. 2013;55:84.
- Goldstein SR, Bachmann G, Lin V, et al. Endometrial safety profile of ospemifene 60 mg when used for long-term treatment of vulvar and vaginal atrophy for up to 1 year. Abstract. Climacteric. 2011;14(suppl 1):S57.
- ACOG practice bulletin no. 141: management of menopausal symptoms. Obstet Gynecol. 2014;123:202-216.
- Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371-1388.
- Cummings SR, Eckert S, Krueger KA, et al. The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple Outcomes of Raloxifene Evaluation. JAMA. 1999;281:2189-2197.
- Vogel VG, Costantino JP, Wickerham DL, et al; National Surgical Adjuvant Breast and Bowel Project (NSABP). Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295:2727-2741.
- Qu Q, Zheng H, Dahllund J, et al. Selective estrogenic effects of a novel triphenylethylene compound, FC1271a, on bone, cholesterol level, and reproductive tissues in intact and ovariectomized rats. Endocrinology. 2000;141:809-820.
- Eigeliene N, Kangas L, Hellmer C, et al. Effects of ospemifene, a novel selective estrogen-receptor modulator, on human breast tissue ex vivo. Menopause. 2016;23:719-730.
- Kangas L, Unkila M. Tissue selectivity of ospemifene: pharmacologic profile and clinical implications. Steroids. 2013;78:1273-1280.
- Constantine GD, Kagan R, Miller PD. Effects of ospemifene on bone parameters including clinical biomarkers in postmenopausal women. Menopause. 2016;23:638-644.
- Gerdhem P, Ivaska KK, Alatalo SL, et al. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res. 2004;19:386-393.
- Peng L, Luo Q, Lu H. Efficacy and safety of bazedoxifene in postmenopausal women with osteoporosis: a systematic review and meta-analysis. Medicine. 2017;96(49):e8659.
- Ronkin S, Northington R, Baracat E, et al. Endometrial effects of bazedoxifene acetate, a novel selective estrogen receptor modulator, in postmenopausal women. Obstet Gynecol. 2005;105:1397-1404.
- Anderson GL, Chlebowski RT, Aragaki AK, et al. Conjugated equine oestrogen and breast cancer incidence and mortality in postmenopausal women with hysterectomy: extended follow-up of the Women’s Health Initiative randomized placebo-controlled trial. Lancet Oncol. 2012;13:476-486.
- Kharode Y, Bodine PV, Miller CP, et al. The pairing of a selective estrogen receptor modulator, bazedoxifene, with conjugated estrogens as a new paradigm for the treatment of menopausal symptoms and osteoporosis prevention. Endocrinology. 2008;149:6084-6091.
- Song Y, Santen RJ, Wang JP, et al. Effects of the conjugated equine estrogen/bazedoxifene tissue-selective estrogen complex (TSEC) on mammary gland and breast cancer in mice. Endocrinology. 2012;153:5706-5715.
- Umland EM, Karel L, Santoro N. Bazedoxifene and conjugated equine estrogen: a combination product for the management of vasomotor symptoms and osteoporosis prevention associated with menopause. Pharmacotherapy. 2016;36:548-561.
- Kagan R, Goldstein SR, Pickar JH, et al. Patient considerations in the management of menopausal symptoms: role of conjugated estrogens with bazedoxifene. Ther Clin Risk Manag. 2016;12:549–562.
- Pinkerton JV, Harvey JA, Pan K, et al. Breast effects of bazedoxifene-conjugated estrogens: a randomized controlled trial. Obstet Gynecol. 2013;121:959-968.
- Lindsay R, Gallagher JC, Kagan R, et al. Efficacy of tissue-selective estrogen complex of bazedoxifene/ conjugated estrogens for osteoporosis prevention in at-risk postmenopausal women. Fertil Steril. 2009;92:1045-1052.
- Fierce Pharma. Pfizer continues recalls of menopause drug Duavee on faulty packaging concerns. https:// www.fiercepharma.com/manufacturing/pfizer-recallsmenopause-drug-duavive-uk-due-to-faulty-packagingworries. June 9, 2020. Accessed February 8, 2022.
- Pfizer. Letter to health care provider. Subject: Duavee (conjugated estrogens/bazedoxifene) extended drug shortage. September 10, 2021.
- Stovall DW, Utian WH, Gass MLS, et al. The effects of combined raloxifene and oral estrogen on vasomotor symptoms and endometrial safety. Menopause. 2007; 14(3 pt 1):510-517.
What placental mechanisms protect the fetus from harm in the setting of maternal COVID-19 infection?
Taglauer ES, Wachman EM, Juttukonda L, et al. Acute severe acute respiratory syndrome coronavirus 2 infection in pregnancy is associated with placental angiotensin-converting enzyme 2 shedding. Am J Pathol. 2022;192:595-603. doi.org/10.1016/j.ajpath.2021.12.011
EXPERT COMMENTARY
Although transmission of SARS-CoV-2 virus from an infected mother to her fetus is rare, placental infection with SARS-CoV-2 can occur and has been observed in association with placental damage and adverse pregnancy outcomes, including stillbirth.1 Understanding what mechanisms of defense protect the placenta and fetus from direct SARS-CoV-2 infection at the maternal-fetal interface, as well as the factors that might disturb or enhance that protection, is critical to gaining a deeper understanding of the potential impact of maternal COVID-19 on fetal well-being.
Details of the study
In a cohort of 24 pregnant individuals, Taglauer and colleagues investigated levels of placental angiotensin-converting enzyme (ACE)-2, placental ADAM17 (a disintegrin and metalloprotease domain 17) activity, and maternal serum soluble ACE2 in samples obtained at delivery from individuals with a history of second trimester COVID-19 infection, early third trimester COVID-19 infection, and no history of COVID-19 infection.
Results. Maternal COVID-19 infection in the early third trimester of pregnancy resulted in lower ACE2 protein levels in the placenta at delivery, higher ACE2 gene expression, and an increase in ADAM17 activity, compared with infection in the second trimester of pregnancy and compared with noninfected controls.
The authors postulated that increased ADAM17 activity—the enzyme responsible for ACE2 cleavage and shedding—may be responsible for lower ACE2 protein levels. Soluble ACE2 levels in maternal blood at delivery were increased in individuals with third trimester COVID-19 infection, although the source of soluble ACE2 (placental or otherwise) could not be determined with the methods employed. Levels of placental estrogen were no different between groups, which suggests that estrogen is not responsible for the observed differences.
Study strengths and limitations
ACE2 is the main receptor for the SARS-CoV-2 virus and facilitates viral entry into the cell.2 Placental villous cells that are in direct contact with maternal blood express the ACE2 protein, rendering them potentially vulnerable to SARS-CoV-2 infection.3 In this study, the authors observed lower placental ACE2 protein in term placentas from recent (early third trimester) but not remote (second trimester) maternal SARS-CoV-2 infection, arguably the result of the observed increase in ADAM17 cleavage activity. Prior studies have shown conflicting results, with equal or higher ACE2 levels noted in the setting of maternal COVID-19 infection, which may be related to differences in COVID-19 disease severity, gestational age of infection, and/or fetal sex in these cohorts.4-6
The concept that increased placental ACE2 shedding represents a protective defense mechanism that might last weeks beyond the acute infectious period is intriguing, but it requires further study. Observed differences in third but not second trimester COVID-19 infections could indicate either 1) an effect of maternal COVID-19 infection that lasts for several weeks but eventually normalizes over time, in the case of a remote infection; or 2) that second trimester maternal COVID-19 infection does not have the same pronounced effect on ACE2 levels as does third trimester infection. Observational studies of the human placenta are not able to answer this question, as directly sampling the placenta at the time of the exposure (or repeated sampling over time) in ongoing pregnancies is neither practical nor ethical. Further studies using animal or cellular models of SARS-CoV-2 infection in pregnancy may be necessary to fully understand the clinical relevance of these findings.
The study by Taglauer and colleagues provides a compelling argument for exploring how immune defenses at the maternal-fetal interface evolve over time and vary by trimester of exposure. ●
As the number of pregnancies exposed to COVID-19 continues to grow worldwide, how immune defenses at the maternal-fetal interface protect against fetal infection remains an important area of investigation.
LYDIA L. SHOOK, MD
- Pregnant people are at increased risk of more severe COVID-19 illness.
- The risk of stillbirth is 2- to 4-fold higher in women with COVID-19 infection during pregnancy.1
- COVID-19 vaccination is recommended for all people who are pregnant, lactating, or considering pregnancy.
- Pregnant and recently pregnant people up to 6 weeks postpartum should receive a third “booster” dose of a COVID-19 mRNA vaccine following completion of their initial COVID-19 vaccine or vaccine series.
- The mRNA COVID-19 vaccines are preferred over the Johnson & Johnson/Janssen COVID-19 vaccine for pregnant and lactating individuals for primary series and booster vaccination.
- Completion of a 2-dose mRNA COVID-19 vaccination series during pregnancy might help prevent COVID-19 hospitalization among infants <6 months.2
aVaccine recommendations adapted from: ACOG practice advisory: COVID-19 vaccination considerations for obstetric-gynecologic care. Last updated March 2, 2022. https://www.acog.org/clinical/ clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetricgynecologic-care. Accessed March 21, 2022.
References
1. DeSisto CL, Wallace B, Simeone RM, et al. Risk for stillbirth among women with and without COVID-19 at delivery hospitalization—United States, March 2020–September 2021. MMWR Morbid Mortal Wkly Rep. 2021;70:1640-1645.
2. Halasa NB, Olson SM, Staat MA, et al; Overcoming COVID-19 Investigators; Overcoming COVID-19 Network. Effectiveness of maternal vaccination with mRNA COVID-19 vaccine during pregnancy against COVID-19–associated hospitalization in infants aged <6 months—17 states, July 2021–January 2022. MMWR Morbid Mortal Wkly Rep. 2022;71:264-270.
- Schwartz DA, Avvad-Portari E, Babál, et al. Placental tissue destruction and insufficiency from COVID-19 causes stillbirth and neonatal death from hypoxic-ischemic injury: a study of 68 cases with SARS-CoV-2 placentitis from 12 countries. Arch Pathol Lab Med. February 10, 2022. doi:10.5858/arpa.2022- 0029-SA.
- Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181: 271-280.e8.
- Hecht JL, Quade B, Deshpande V, et al. SARS-CoV-2 can infect the placenta and is not associated with specific placental histopathology: a series of 19 placentas from COVID-19- positive mothers. Mod Pathol. 2020;33:2092-2103.
- Mourad M, Jacob T, Sadovsky E, et al. Placental response to maternal SARS-CoV-2 infection. Sci Rep. 2021;11:14390.
- Lu-Culligan A, Chavan AR, Vijayakumar P, et al. Maternal respiratory SARS-CoV-2 infection in pregnancy is associated with a robust inflammatory response at the maternal-fetal interface. Med (N Y). 2021;2:591-610.e10.
- Shook LL, Bordt EA, Meinsohn MC, et al. Placental expression of ACE2 and TMPRSS2 in maternal severe acute respiratory syndrome coronavirus 2 infection: are placental defenses mediated by fetal sex? J Infect Dis. 2021;224(suppl 6):S659.
Taglauer ES, Wachman EM, Juttukonda L, et al. Acute severe acute respiratory syndrome coronavirus 2 infection in pregnancy is associated with placental angiotensin-converting enzyme 2 shedding. Am J Pathol. 2022;192:595-603. doi.org/10.1016/j.ajpath.2021.12.011
EXPERT COMMENTARY
Although transmission of SARS-CoV-2 virus from an infected mother to her fetus is rare, placental infection with SARS-CoV-2 can occur and has been observed in association with placental damage and adverse pregnancy outcomes, including stillbirth.1 Understanding what mechanisms of defense protect the placenta and fetus from direct SARS-CoV-2 infection at the maternal-fetal interface, as well as the factors that might disturb or enhance that protection, is critical to gaining a deeper understanding of the potential impact of maternal COVID-19 on fetal well-being.
Details of the study
In a cohort of 24 pregnant individuals, Taglauer and colleagues investigated levels of placental angiotensin-converting enzyme (ACE)-2, placental ADAM17 (a disintegrin and metalloprotease domain 17) activity, and maternal serum soluble ACE2 in samples obtained at delivery from individuals with a history of second trimester COVID-19 infection, early third trimester COVID-19 infection, and no history of COVID-19 infection.
Results. Maternal COVID-19 infection in the early third trimester of pregnancy resulted in lower ACE2 protein levels in the placenta at delivery, higher ACE2 gene expression, and an increase in ADAM17 activity, compared with infection in the second trimester of pregnancy and compared with noninfected controls.
The authors postulated that increased ADAM17 activity—the enzyme responsible for ACE2 cleavage and shedding—may be responsible for lower ACE2 protein levels. Soluble ACE2 levels in maternal blood at delivery were increased in individuals with third trimester COVID-19 infection, although the source of soluble ACE2 (placental or otherwise) could not be determined with the methods employed. Levels of placental estrogen were no different between groups, which suggests that estrogen is not responsible for the observed differences.
Study strengths and limitations
ACE2 is the main receptor for the SARS-CoV-2 virus and facilitates viral entry into the cell.2 Placental villous cells that are in direct contact with maternal blood express the ACE2 protein, rendering them potentially vulnerable to SARS-CoV-2 infection.3 In this study, the authors observed lower placental ACE2 protein in term placentas from recent (early third trimester) but not remote (second trimester) maternal SARS-CoV-2 infection, arguably the result of the observed increase in ADAM17 cleavage activity. Prior studies have shown conflicting results, with equal or higher ACE2 levels noted in the setting of maternal COVID-19 infection, which may be related to differences in COVID-19 disease severity, gestational age of infection, and/or fetal sex in these cohorts.4-6
The concept that increased placental ACE2 shedding represents a protective defense mechanism that might last weeks beyond the acute infectious period is intriguing, but it requires further study. Observed differences in third but not second trimester COVID-19 infections could indicate either 1) an effect of maternal COVID-19 infection that lasts for several weeks but eventually normalizes over time, in the case of a remote infection; or 2) that second trimester maternal COVID-19 infection does not have the same pronounced effect on ACE2 levels as does third trimester infection. Observational studies of the human placenta are not able to answer this question, as directly sampling the placenta at the time of the exposure (or repeated sampling over time) in ongoing pregnancies is neither practical nor ethical. Further studies using animal or cellular models of SARS-CoV-2 infection in pregnancy may be necessary to fully understand the clinical relevance of these findings.
The study by Taglauer and colleagues provides a compelling argument for exploring how immune defenses at the maternal-fetal interface evolve over time and vary by trimester of exposure. ●
As the number of pregnancies exposed to COVID-19 continues to grow worldwide, how immune defenses at the maternal-fetal interface protect against fetal infection remains an important area of investigation.
LYDIA L. SHOOK, MD
- Pregnant people are at increased risk of more severe COVID-19 illness.
- The risk of stillbirth is 2- to 4-fold higher in women with COVID-19 infection during pregnancy.1
- COVID-19 vaccination is recommended for all people who are pregnant, lactating, or considering pregnancy.
- Pregnant and recently pregnant people up to 6 weeks postpartum should receive a third “booster” dose of a COVID-19 mRNA vaccine following completion of their initial COVID-19 vaccine or vaccine series.
- The mRNA COVID-19 vaccines are preferred over the Johnson & Johnson/Janssen COVID-19 vaccine for pregnant and lactating individuals for primary series and booster vaccination.
- Completion of a 2-dose mRNA COVID-19 vaccination series during pregnancy might help prevent COVID-19 hospitalization among infants <6 months.2
aVaccine recommendations adapted from: ACOG practice advisory: COVID-19 vaccination considerations for obstetric-gynecologic care. Last updated March 2, 2022. https://www.acog.org/clinical/ clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetricgynecologic-care. Accessed March 21, 2022.
References
1. DeSisto CL, Wallace B, Simeone RM, et al. Risk for stillbirth among women with and without COVID-19 at delivery hospitalization—United States, March 2020–September 2021. MMWR Morbid Mortal Wkly Rep. 2021;70:1640-1645.
2. Halasa NB, Olson SM, Staat MA, et al; Overcoming COVID-19 Investigators; Overcoming COVID-19 Network. Effectiveness of maternal vaccination with mRNA COVID-19 vaccine during pregnancy against COVID-19–associated hospitalization in infants aged <6 months—17 states, July 2021–January 2022. MMWR Morbid Mortal Wkly Rep. 2022;71:264-270.
Taglauer ES, Wachman EM, Juttukonda L, et al. Acute severe acute respiratory syndrome coronavirus 2 infection in pregnancy is associated with placental angiotensin-converting enzyme 2 shedding. Am J Pathol. 2022;192:595-603. doi.org/10.1016/j.ajpath.2021.12.011
EXPERT COMMENTARY
Although transmission of SARS-CoV-2 virus from an infected mother to her fetus is rare, placental infection with SARS-CoV-2 can occur and has been observed in association with placental damage and adverse pregnancy outcomes, including stillbirth.1 Understanding what mechanisms of defense protect the placenta and fetus from direct SARS-CoV-2 infection at the maternal-fetal interface, as well as the factors that might disturb or enhance that protection, is critical to gaining a deeper understanding of the potential impact of maternal COVID-19 on fetal well-being.
Details of the study
In a cohort of 24 pregnant individuals, Taglauer and colleagues investigated levels of placental angiotensin-converting enzyme (ACE)-2, placental ADAM17 (a disintegrin and metalloprotease domain 17) activity, and maternal serum soluble ACE2 in samples obtained at delivery from individuals with a history of second trimester COVID-19 infection, early third trimester COVID-19 infection, and no history of COVID-19 infection.
Results. Maternal COVID-19 infection in the early third trimester of pregnancy resulted in lower ACE2 protein levels in the placenta at delivery, higher ACE2 gene expression, and an increase in ADAM17 activity, compared with infection in the second trimester of pregnancy and compared with noninfected controls.
The authors postulated that increased ADAM17 activity—the enzyme responsible for ACE2 cleavage and shedding—may be responsible for lower ACE2 protein levels. Soluble ACE2 levels in maternal blood at delivery were increased in individuals with third trimester COVID-19 infection, although the source of soluble ACE2 (placental or otherwise) could not be determined with the methods employed. Levels of placental estrogen were no different between groups, which suggests that estrogen is not responsible for the observed differences.
Study strengths and limitations
ACE2 is the main receptor for the SARS-CoV-2 virus and facilitates viral entry into the cell.2 Placental villous cells that are in direct contact with maternal blood express the ACE2 protein, rendering them potentially vulnerable to SARS-CoV-2 infection.3 In this study, the authors observed lower placental ACE2 protein in term placentas from recent (early third trimester) but not remote (second trimester) maternal SARS-CoV-2 infection, arguably the result of the observed increase in ADAM17 cleavage activity. Prior studies have shown conflicting results, with equal or higher ACE2 levels noted in the setting of maternal COVID-19 infection, which may be related to differences in COVID-19 disease severity, gestational age of infection, and/or fetal sex in these cohorts.4-6
The concept that increased placental ACE2 shedding represents a protective defense mechanism that might last weeks beyond the acute infectious period is intriguing, but it requires further study. Observed differences in third but not second trimester COVID-19 infections could indicate either 1) an effect of maternal COVID-19 infection that lasts for several weeks but eventually normalizes over time, in the case of a remote infection; or 2) that second trimester maternal COVID-19 infection does not have the same pronounced effect on ACE2 levels as does third trimester infection. Observational studies of the human placenta are not able to answer this question, as directly sampling the placenta at the time of the exposure (or repeated sampling over time) in ongoing pregnancies is neither practical nor ethical. Further studies using animal or cellular models of SARS-CoV-2 infection in pregnancy may be necessary to fully understand the clinical relevance of these findings.
The study by Taglauer and colleagues provides a compelling argument for exploring how immune defenses at the maternal-fetal interface evolve over time and vary by trimester of exposure. ●
As the number of pregnancies exposed to COVID-19 continues to grow worldwide, how immune defenses at the maternal-fetal interface protect against fetal infection remains an important area of investigation.
LYDIA L. SHOOK, MD
- Pregnant people are at increased risk of more severe COVID-19 illness.
- The risk of stillbirth is 2- to 4-fold higher in women with COVID-19 infection during pregnancy.1
- COVID-19 vaccination is recommended for all people who are pregnant, lactating, or considering pregnancy.
- Pregnant and recently pregnant people up to 6 weeks postpartum should receive a third “booster” dose of a COVID-19 mRNA vaccine following completion of their initial COVID-19 vaccine or vaccine series.
- The mRNA COVID-19 vaccines are preferred over the Johnson & Johnson/Janssen COVID-19 vaccine for pregnant and lactating individuals for primary series and booster vaccination.
- Completion of a 2-dose mRNA COVID-19 vaccination series during pregnancy might help prevent COVID-19 hospitalization among infants <6 months.2
aVaccine recommendations adapted from: ACOG practice advisory: COVID-19 vaccination considerations for obstetric-gynecologic care. Last updated March 2, 2022. https://www.acog.org/clinical/ clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetricgynecologic-care. Accessed March 21, 2022.
References
1. DeSisto CL, Wallace B, Simeone RM, et al. Risk for stillbirth among women with and without COVID-19 at delivery hospitalization—United States, March 2020–September 2021. MMWR Morbid Mortal Wkly Rep. 2021;70:1640-1645.
2. Halasa NB, Olson SM, Staat MA, et al; Overcoming COVID-19 Investigators; Overcoming COVID-19 Network. Effectiveness of maternal vaccination with mRNA COVID-19 vaccine during pregnancy against COVID-19–associated hospitalization in infants aged <6 months—17 states, July 2021–January 2022. MMWR Morbid Mortal Wkly Rep. 2022;71:264-270.
- Schwartz DA, Avvad-Portari E, Babál, et al. Placental tissue destruction and insufficiency from COVID-19 causes stillbirth and neonatal death from hypoxic-ischemic injury: a study of 68 cases with SARS-CoV-2 placentitis from 12 countries. Arch Pathol Lab Med. February 10, 2022. doi:10.5858/arpa.2022- 0029-SA.
- Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181: 271-280.e8.
- Hecht JL, Quade B, Deshpande V, et al. SARS-CoV-2 can infect the placenta and is not associated with specific placental histopathology: a series of 19 placentas from COVID-19- positive mothers. Mod Pathol. 2020;33:2092-2103.
- Mourad M, Jacob T, Sadovsky E, et al. Placental response to maternal SARS-CoV-2 infection. Sci Rep. 2021;11:14390.
- Lu-Culligan A, Chavan AR, Vijayakumar P, et al. Maternal respiratory SARS-CoV-2 infection in pregnancy is associated with a robust inflammatory response at the maternal-fetal interface. Med (N Y). 2021;2:591-610.e10.
- Shook LL, Bordt EA, Meinsohn MC, et al. Placental expression of ACE2 and TMPRSS2 in maternal severe acute respiratory syndrome coronavirus 2 infection: are placental defenses mediated by fetal sex? J Infect Dis. 2021;224(suppl 6):S659.
- Schwartz DA, Avvad-Portari E, Babál, et al. Placental tissue destruction and insufficiency from COVID-19 causes stillbirth and neonatal death from hypoxic-ischemic injury: a study of 68 cases with SARS-CoV-2 placentitis from 12 countries. Arch Pathol Lab Med. February 10, 2022. doi:10.5858/arpa.2022- 0029-SA.
- Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181: 271-280.e8.
- Hecht JL, Quade B, Deshpande V, et al. SARS-CoV-2 can infect the placenta and is not associated with specific placental histopathology: a series of 19 placentas from COVID-19- positive mothers. Mod Pathol. 2020;33:2092-2103.
- Mourad M, Jacob T, Sadovsky E, et al. Placental response to maternal SARS-CoV-2 infection. Sci Rep. 2021;11:14390.
- Lu-Culligan A, Chavan AR, Vijayakumar P, et al. Maternal respiratory SARS-CoV-2 infection in pregnancy is associated with a robust inflammatory response at the maternal-fetal interface. Med (N Y). 2021;2:591-610.e10.
- Shook LL, Bordt EA, Meinsohn MC, et al. Placental expression of ACE2 and TMPRSS2 in maternal severe acute respiratory syndrome coronavirus 2 infection: are placental defenses mediated by fetal sex? J Infect Dis. 2021;224(suppl 6):S659.
Transgender youth: Bringing evidence to the political debates
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
Metacognitive training an effective, durable treatment for schizophrenia
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.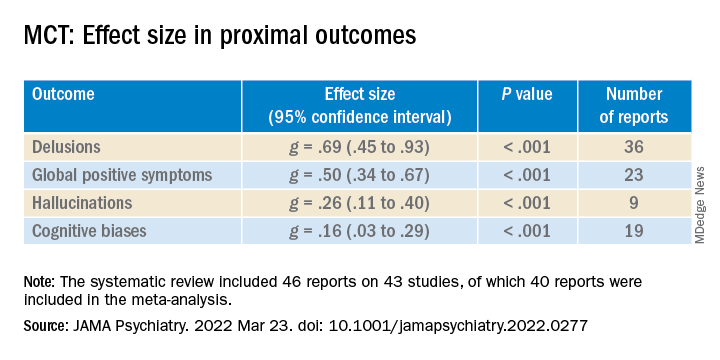
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).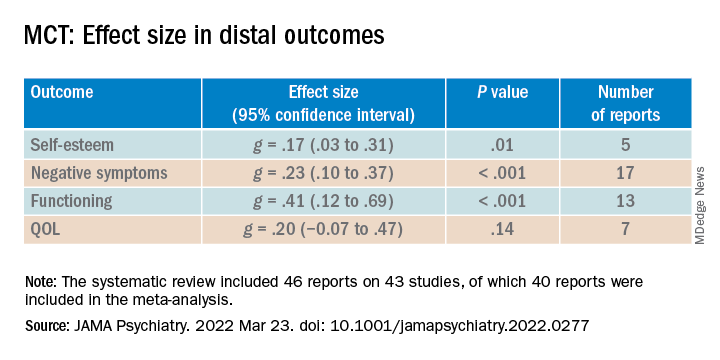
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.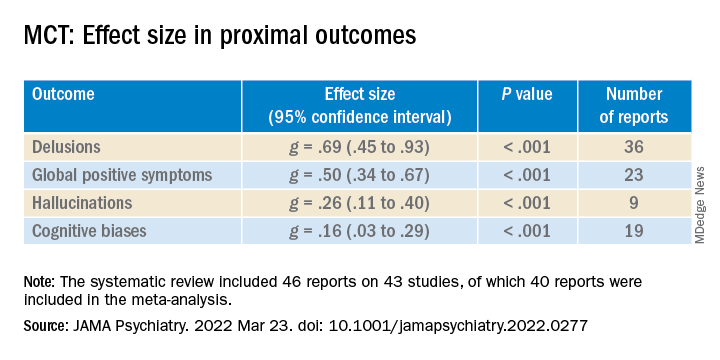
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).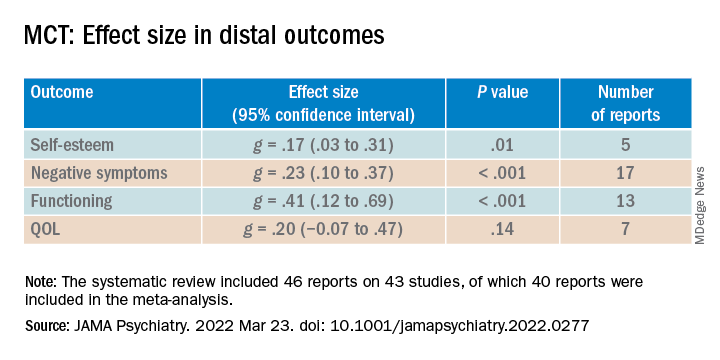
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.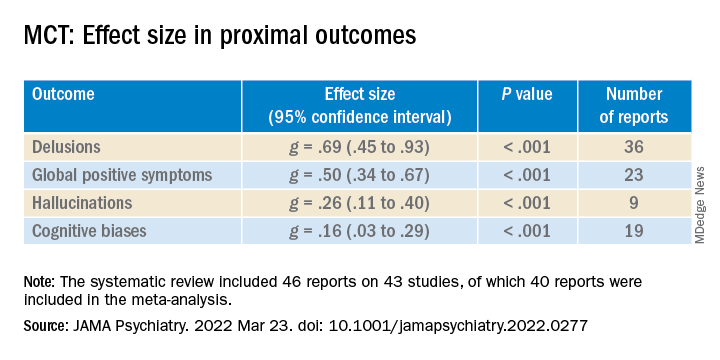
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).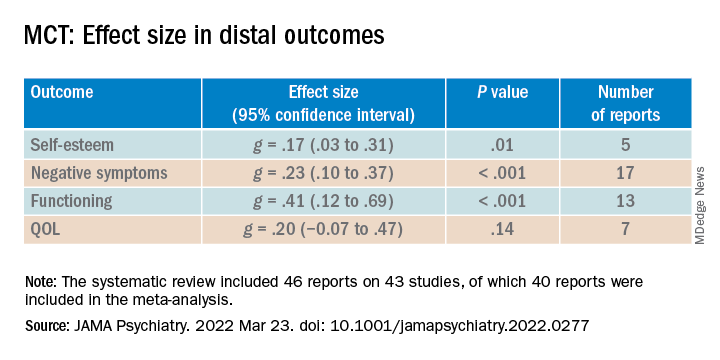
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Developing and Measuring Effectiveness of a Distance Learning Dermatology Course: A Prospective Observational Study
Medical education has seen major changes over the last decade. The allotted time for preclinical education has decreased from 24 months to 18 months or less at most institutions, with an increased focus on content associated with health care delivery and health system science.1,2 Many schools now include at least some blended learning with online delivery of preclinical education.3 On the other hand, the clinical portion of medical education has remained largely unchanged prior to the COVID-19 pandemic, with the apprenticeship framework allowing the experienced physician to observe, mentor, and pass on practical knowledge so that the apprentice can one day gain independence after demonstrating adequate proficiency.4
With respect to dermatology education, skin disorders are in the top 5 reported reasons for visits to primary care5; however, a 2009 survey found that only 0.24% to 0.30% of medical schools’ curricula are spent on dermatology.6 Moreover, one institution found that fourth-year medical students received an average of 46.6% on a 15-item quiz designed to assess the ability to diagnose and treat common dermatologic conditions, and within that same cohort, 87.6% of students felt that they received inadequate training in dermatology during medical school.7
COVID-19 caused an unprecedented paradigm shift when medical schools throughout the country, including our own, canceled clinical rotations at the end of March 2020 to protect students and control the spread of infection. To enable clinical and preclinical learning to continue, institutions around the globe turned to either online learning or participation in telehealth as a substitute for clinical rotations.8-10 At the Uniformed Services University of the Health Sciences (Bethesda, Maryland), one of the many online clinical courses offered included a distance learning (DL) dermatology course. Herein, we describe the results of a prospective study evaluating short-term information recall and comprehension as well as students’ confidence in their ability to apply course objectives over 3 months of an online DL dermatology course.
Methods
Between April and July 2020, 14 students at the Uniformed Services University of the Health Sciences (Table 1) enrolled in 1 of 3 four-week DL dermatology classes. The students independently completed the Basic Dermatology Curriculum, a set of online modules with demonstrated efficacy from the American Academy of Dermatology, over 4 weeks.11 Additionally, students were instructed to review an hour of clinical dermatology images daily from online dermatology atlases and e-books accessed through our medical school’s virtual library. Optional Free Open Access Meducation resources also were provided. The course syllabus provided the students with clear expectations, links to the resources, and a recommended daily schedule.
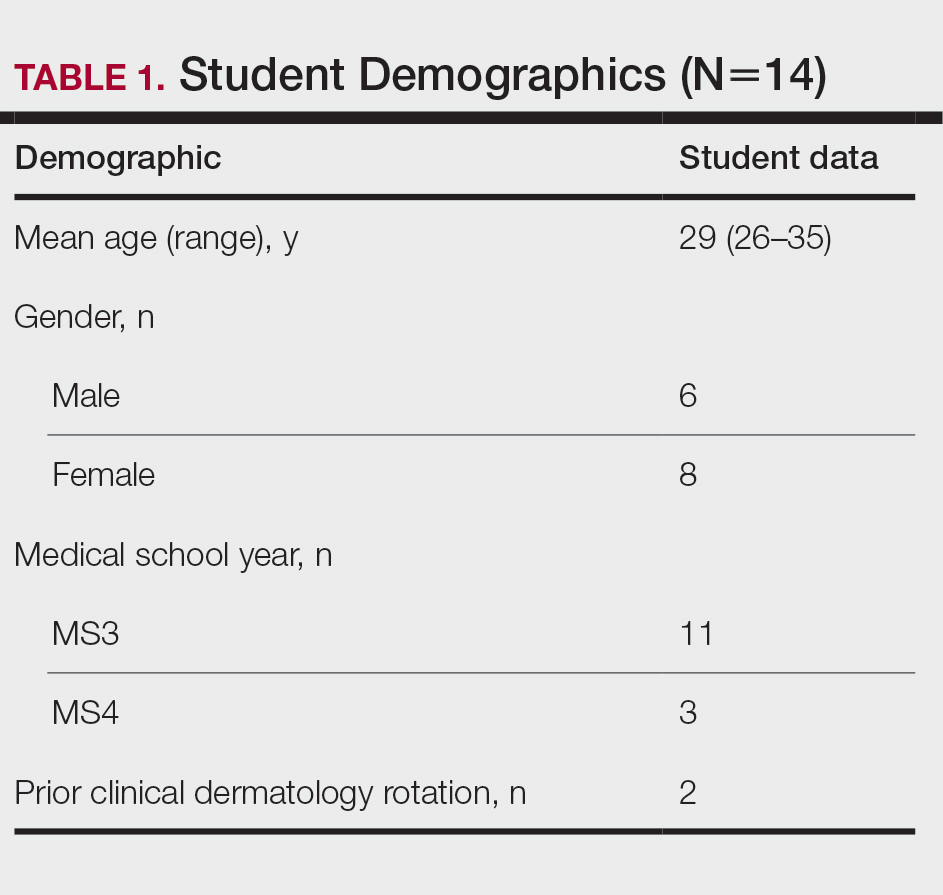
An online video conferencing platform was utilized for an orientation session and 4 subsequent weekly 1.5-hour virtual meetings. The weekly DL meetings focused on a discussion of clinical images pertinent to the American Academy of Dermatology modules covered for the week. These interactive analytic sessions were referred to as Clinpic sessions. With instructor guidance, the students learned to describe images, and they provided differential diagnoses, workup, and treatments for various skin diseases. The virtual meetings included supplemental lectures detailing the use of teledermatology and laser therapy in the Military Health System and a journal review on the cutaneous manifestations of COVID-19.
A 40-question, image-based pretest and posttest utilized during clinical rotations evaluated knowledge recall and comprehension. A precourse and postcourse survey using a 5-point Likert scale (1=not confident; 5=extremely confident) assessed students’ confidence levels across course objectives: general knowledge of dermatology, working knowledge of teledermatology, ability to accurately describe skin lesions, generate sound differential diagnoses, and formulate a reasonable treatment plan. Statistical analysis was performed using free online statistical software at statskingdom.com.12
Results
All 14 student enrollees completed the precourse and postcourse tests and surveys. Pretest and posttest scores followed a normal distribution and therefore met criteria for utilization of a parametric test. The precourse test average of 67% (range, 40%–90%) improved to 84% postcourse (range, 70%–98%; P<.001; 95% CI, 11-23 by paired t test). Not surprisingly, the 2 students who had completed a dermatology rotation had higher average pretest and posttest scores (pretest, 87%; posttest, 94%). Students’ confidence with the course objectives were mostly at the somewhat confident level on the 5-point Likert scale precourse survey. By the end of the course, student survey responses increased to confident and very confident levels, corresponding to an overall improvement of 1.3 points (P<.001 by paired t test)(Table 2) when the mean of the survey results was aggregated across every question. Instructor evaluation of student performance mirrored student assessments.
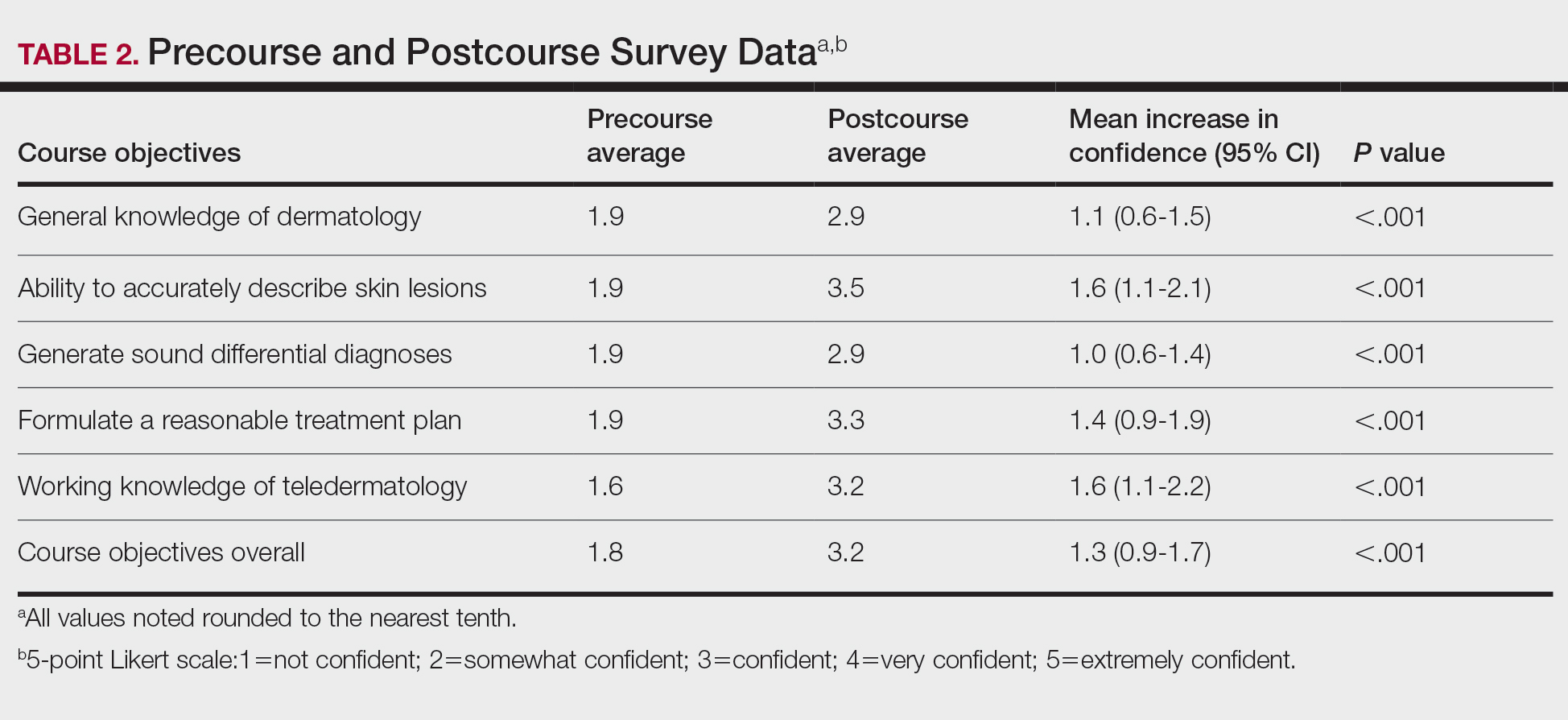
Comment
The DL dermatology course succeeded in helping the enrolled students attain course objectives and offered a reasonable solution when in-person interaction was restricted. The students in the DL course made notable improvements in their dermatology knowledge and improved their communication, diagnosis, and management skills. Although a blended dermatology curriculum with e-learning combined with clinical experience has been shown to increase knowledge acquisition,13,14 our results suggest that an online-only program also can increase comprehension as well as students’ confidence in their abilities.
A major challenge for the DL course was the lack of opportunity to perform common dermatology procedures. The addition of a hands-on skin procedure module would have been a great supplement to the course but was not possible due to social distancing guidelines during the COVID-19 pandemic. The small sample size and voluntary enrollment were limitations to this study.
Conclusion
Although the traditional dermatology rotation remains the gold standard for clinical instruction, a well-organized DL teaching environment allowed for a more controlled learning experience with a broader coverage of topics to include potentially greater exposure to rare skin disorders not typically encountered in everyday practice. A DL dermatology course may serve as an enduring curriculum for those who wish to learn dermatology more broadly and are not interested in performing skin procedures or direct patient exposure (eg, those pursuing non–primary care specialties, pathology, or radiology). It also may be attractive to students who have had a prior clinical dermatology rotation and desire a different learning experience with a wide coverage of topics.
Acknowledgments—The authors thank Thomas Darling, MD, PhD (Bethesda, Maryland), for coining the term Clinpic and providing critical feedback throughout the course. The authors also thank Sorana Raiciulescu, MS (Bethesda, Maryland), for assistance with the statistical analysis.
- Emanuel EJ. The inevitable reimagining of medical education. JAMA. 2020;323:1127-1128.
- Skochelak SE, Stack SJ. Creating the medical schools of the future. Acad Med. 2017;92:16-19.
- Vallée A, Blacher J, Cariou A, et al. Blended learning compared to traditional learning in medical education: systematic review and meta-analysis. J Med Internet Res. 2020;22:E16504.
- Rangachari D, Brown LE, Kern DE, et al. Clinical coaching: evolving the apprenticeship model for modern housestaff. Med Teach. 2017;39:780-782.
- Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Can Fam Physician. 2018;64:832-840.
- McCleskey PE, Gilson RT, DeVillez RL. Medical student core curriculum in dermatology survey. J Am Acad Dermatol. 2009;61:30-35.e4.
- Ulman CA, Binder SB, Borges NJ. Assessment of medical students’ proficiency in dermatology: are medical students adequately prepared to diagnose and treat common dermatologic conditions in the United States? J Educ Eval Health Prof. 2015;12:18.
- Loh TY, Hsiao JL, Shi VY. COVID-19 and its effect on medical student education in dermatology. J Am Acad Dermatol. 2020;83:E163-E164.
- Hilburg R, Patel N, Ambruso S, et al. Medical education during the coronavirus disease-2019 pandemic: learning from a distance. Adv Chronic Kidney Dis. 2020;27:412-417.
- Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323:2131-2132.
- McCleskey PE. Clinic teaching made easy: a prospective study of the American Academy of Dermatology core curriculum in primary care learners. J Am Acad Dermatol. 2013;69:273-279.e1.
- Paired T Test calculator. Statistics Kingdom website. Accessed February 7, 2022. http://www.statskingdom.com/160MeanT2pair.html
- Fransen F, Martens H, Nagtzaam I, et al. Use of e-learning in clinical clerkships: effects on acquisition of dermatological knowledge and learning processes. Int J Med Educ. 2018;9:11-17.
- Silva CS, Souza MB, Silva Filho RS, et al. E-learning program for medical students in dermatology. Clinics. 2011;66:619-622.
Medical education has seen major changes over the last decade. The allotted time for preclinical education has decreased from 24 months to 18 months or less at most institutions, with an increased focus on content associated with health care delivery and health system science.1,2 Many schools now include at least some blended learning with online delivery of preclinical education.3 On the other hand, the clinical portion of medical education has remained largely unchanged prior to the COVID-19 pandemic, with the apprenticeship framework allowing the experienced physician to observe, mentor, and pass on practical knowledge so that the apprentice can one day gain independence after demonstrating adequate proficiency.4
With respect to dermatology education, skin disorders are in the top 5 reported reasons for visits to primary care5; however, a 2009 survey found that only 0.24% to 0.30% of medical schools’ curricula are spent on dermatology.6 Moreover, one institution found that fourth-year medical students received an average of 46.6% on a 15-item quiz designed to assess the ability to diagnose and treat common dermatologic conditions, and within that same cohort, 87.6% of students felt that they received inadequate training in dermatology during medical school.7
COVID-19 caused an unprecedented paradigm shift when medical schools throughout the country, including our own, canceled clinical rotations at the end of March 2020 to protect students and control the spread of infection. To enable clinical and preclinical learning to continue, institutions around the globe turned to either online learning or participation in telehealth as a substitute for clinical rotations.8-10 At the Uniformed Services University of the Health Sciences (Bethesda, Maryland), one of the many online clinical courses offered included a distance learning (DL) dermatology course. Herein, we describe the results of a prospective study evaluating short-term information recall and comprehension as well as students’ confidence in their ability to apply course objectives over 3 months of an online DL dermatology course.
Methods
Between April and July 2020, 14 students at the Uniformed Services University of the Health Sciences (Table 1) enrolled in 1 of 3 four-week DL dermatology classes. The students independently completed the Basic Dermatology Curriculum, a set of online modules with demonstrated efficacy from the American Academy of Dermatology, over 4 weeks.11 Additionally, students were instructed to review an hour of clinical dermatology images daily from online dermatology atlases and e-books accessed through our medical school’s virtual library. Optional Free Open Access Meducation resources also were provided. The course syllabus provided the students with clear expectations, links to the resources, and a recommended daily schedule.
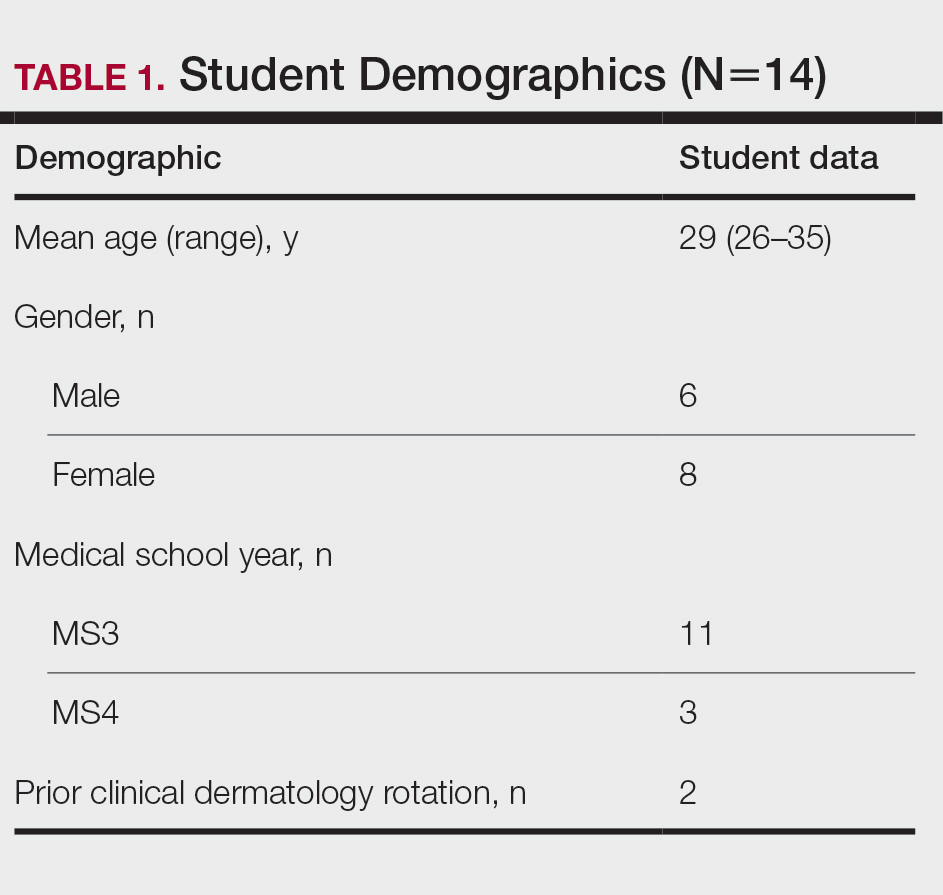
An online video conferencing platform was utilized for an orientation session and 4 subsequent weekly 1.5-hour virtual meetings. The weekly DL meetings focused on a discussion of clinical images pertinent to the American Academy of Dermatology modules covered for the week. These interactive analytic sessions were referred to as Clinpic sessions. With instructor guidance, the students learned to describe images, and they provided differential diagnoses, workup, and treatments for various skin diseases. The virtual meetings included supplemental lectures detailing the use of teledermatology and laser therapy in the Military Health System and a journal review on the cutaneous manifestations of COVID-19.
A 40-question, image-based pretest and posttest utilized during clinical rotations evaluated knowledge recall and comprehension. A precourse and postcourse survey using a 5-point Likert scale (1=not confident; 5=extremely confident) assessed students’ confidence levels across course objectives: general knowledge of dermatology, working knowledge of teledermatology, ability to accurately describe skin lesions, generate sound differential diagnoses, and formulate a reasonable treatment plan. Statistical analysis was performed using free online statistical software at statskingdom.com.12
Results
All 14 student enrollees completed the precourse and postcourse tests and surveys. Pretest and posttest scores followed a normal distribution and therefore met criteria for utilization of a parametric test. The precourse test average of 67% (range, 40%–90%) improved to 84% postcourse (range, 70%–98%; P<.001; 95% CI, 11-23 by paired t test). Not surprisingly, the 2 students who had completed a dermatology rotation had higher average pretest and posttest scores (pretest, 87%; posttest, 94%). Students’ confidence with the course objectives were mostly at the somewhat confident level on the 5-point Likert scale precourse survey. By the end of the course, student survey responses increased to confident and very confident levels, corresponding to an overall improvement of 1.3 points (P<.001 by paired t test)(Table 2) when the mean of the survey results was aggregated across every question. Instructor evaluation of student performance mirrored student assessments.
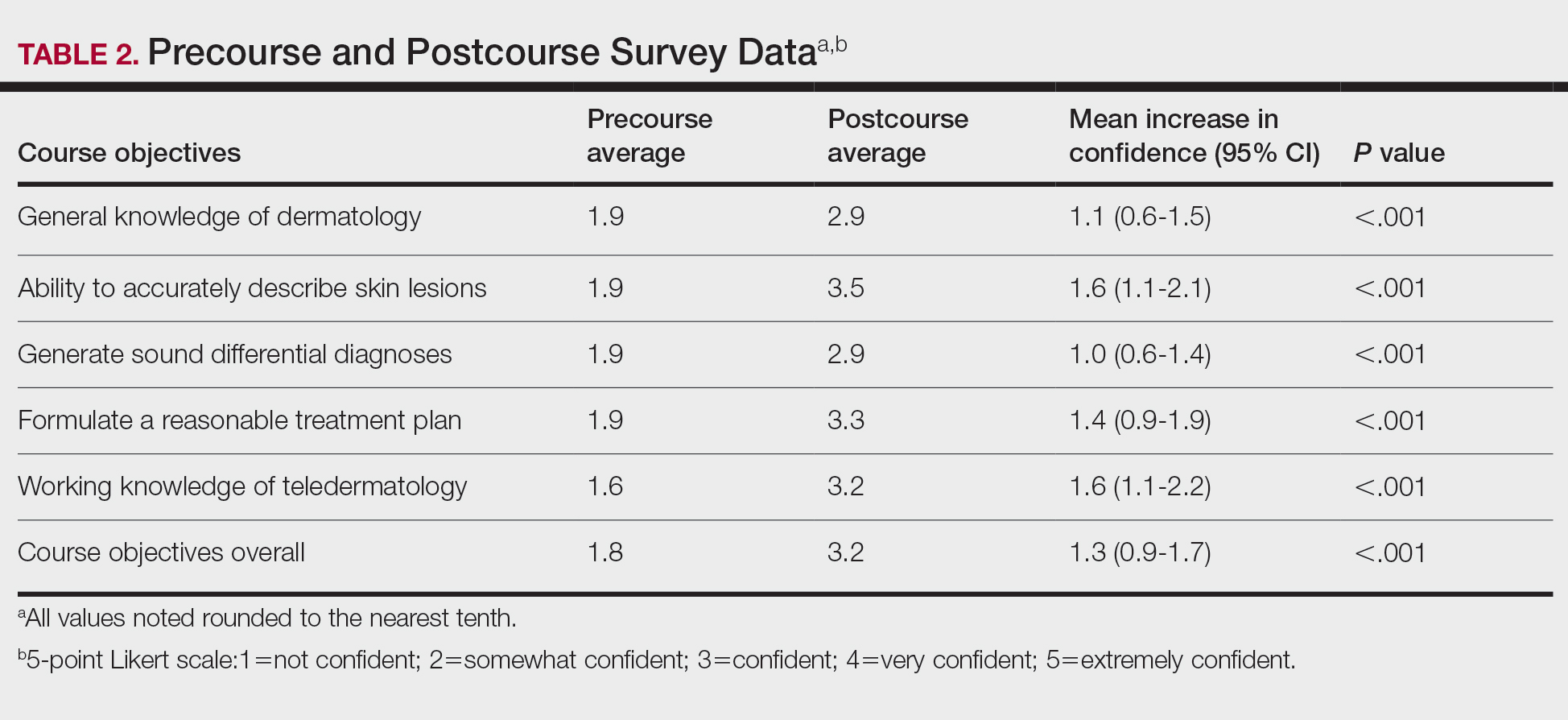
Comment
The DL dermatology course succeeded in helping the enrolled students attain course objectives and offered a reasonable solution when in-person interaction was restricted. The students in the DL course made notable improvements in their dermatology knowledge and improved their communication, diagnosis, and management skills. Although a blended dermatology curriculum with e-learning combined with clinical experience has been shown to increase knowledge acquisition,13,14 our results suggest that an online-only program also can increase comprehension as well as students’ confidence in their abilities.
A major challenge for the DL course was the lack of opportunity to perform common dermatology procedures. The addition of a hands-on skin procedure module would have been a great supplement to the course but was not possible due to social distancing guidelines during the COVID-19 pandemic. The small sample size and voluntary enrollment were limitations to this study.
Conclusion
Although the traditional dermatology rotation remains the gold standard for clinical instruction, a well-organized DL teaching environment allowed for a more controlled learning experience with a broader coverage of topics to include potentially greater exposure to rare skin disorders not typically encountered in everyday practice. A DL dermatology course may serve as an enduring curriculum for those who wish to learn dermatology more broadly and are not interested in performing skin procedures or direct patient exposure (eg, those pursuing non–primary care specialties, pathology, or radiology). It also may be attractive to students who have had a prior clinical dermatology rotation and desire a different learning experience with a wide coverage of topics.
Acknowledgments—The authors thank Thomas Darling, MD, PhD (Bethesda, Maryland), for coining the term Clinpic and providing critical feedback throughout the course. The authors also thank Sorana Raiciulescu, MS (Bethesda, Maryland), for assistance with the statistical analysis.
Medical education has seen major changes over the last decade. The allotted time for preclinical education has decreased from 24 months to 18 months or less at most institutions, with an increased focus on content associated with health care delivery and health system science.1,2 Many schools now include at least some blended learning with online delivery of preclinical education.3 On the other hand, the clinical portion of medical education has remained largely unchanged prior to the COVID-19 pandemic, with the apprenticeship framework allowing the experienced physician to observe, mentor, and pass on practical knowledge so that the apprentice can one day gain independence after demonstrating adequate proficiency.4
With respect to dermatology education, skin disorders are in the top 5 reported reasons for visits to primary care5; however, a 2009 survey found that only 0.24% to 0.30% of medical schools’ curricula are spent on dermatology.6 Moreover, one institution found that fourth-year medical students received an average of 46.6% on a 15-item quiz designed to assess the ability to diagnose and treat common dermatologic conditions, and within that same cohort, 87.6% of students felt that they received inadequate training in dermatology during medical school.7
COVID-19 caused an unprecedented paradigm shift when medical schools throughout the country, including our own, canceled clinical rotations at the end of March 2020 to protect students and control the spread of infection. To enable clinical and preclinical learning to continue, institutions around the globe turned to either online learning or participation in telehealth as a substitute for clinical rotations.8-10 At the Uniformed Services University of the Health Sciences (Bethesda, Maryland), one of the many online clinical courses offered included a distance learning (DL) dermatology course. Herein, we describe the results of a prospective study evaluating short-term information recall and comprehension as well as students’ confidence in their ability to apply course objectives over 3 months of an online DL dermatology course.
Methods
Between April and July 2020, 14 students at the Uniformed Services University of the Health Sciences (Table 1) enrolled in 1 of 3 four-week DL dermatology classes. The students independently completed the Basic Dermatology Curriculum, a set of online modules with demonstrated efficacy from the American Academy of Dermatology, over 4 weeks.11 Additionally, students were instructed to review an hour of clinical dermatology images daily from online dermatology atlases and e-books accessed through our medical school’s virtual library. Optional Free Open Access Meducation resources also were provided. The course syllabus provided the students with clear expectations, links to the resources, and a recommended daily schedule.
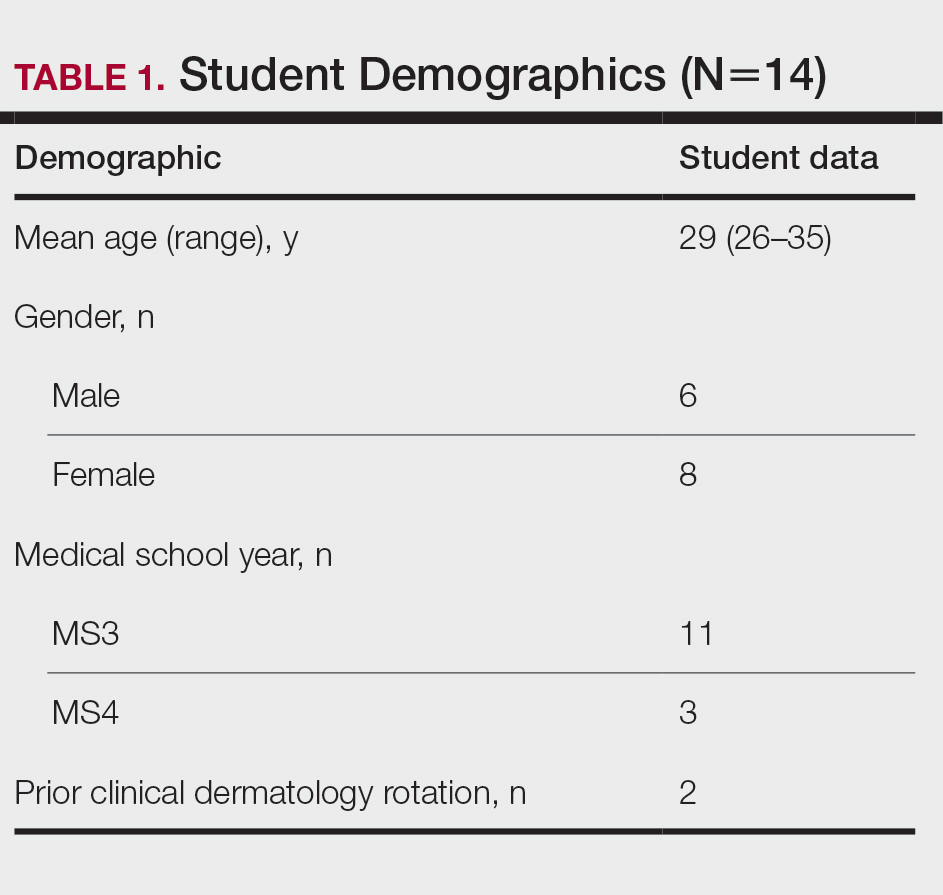
An online video conferencing platform was utilized for an orientation session and 4 subsequent weekly 1.5-hour virtual meetings. The weekly DL meetings focused on a discussion of clinical images pertinent to the American Academy of Dermatology modules covered for the week. These interactive analytic sessions were referred to as Clinpic sessions. With instructor guidance, the students learned to describe images, and they provided differential diagnoses, workup, and treatments for various skin diseases. The virtual meetings included supplemental lectures detailing the use of teledermatology and laser therapy in the Military Health System and a journal review on the cutaneous manifestations of COVID-19.
A 40-question, image-based pretest and posttest utilized during clinical rotations evaluated knowledge recall and comprehension. A precourse and postcourse survey using a 5-point Likert scale (1=not confident; 5=extremely confident) assessed students’ confidence levels across course objectives: general knowledge of dermatology, working knowledge of teledermatology, ability to accurately describe skin lesions, generate sound differential diagnoses, and formulate a reasonable treatment plan. Statistical analysis was performed using free online statistical software at statskingdom.com.12
Results
All 14 student enrollees completed the precourse and postcourse tests and surveys. Pretest and posttest scores followed a normal distribution and therefore met criteria for utilization of a parametric test. The precourse test average of 67% (range, 40%–90%) improved to 84% postcourse (range, 70%–98%; P<.001; 95% CI, 11-23 by paired t test). Not surprisingly, the 2 students who had completed a dermatology rotation had higher average pretest and posttest scores (pretest, 87%; posttest, 94%). Students’ confidence with the course objectives were mostly at the somewhat confident level on the 5-point Likert scale precourse survey. By the end of the course, student survey responses increased to confident and very confident levels, corresponding to an overall improvement of 1.3 points (P<.001 by paired t test)(Table 2) when the mean of the survey results was aggregated across every question. Instructor evaluation of student performance mirrored student assessments.
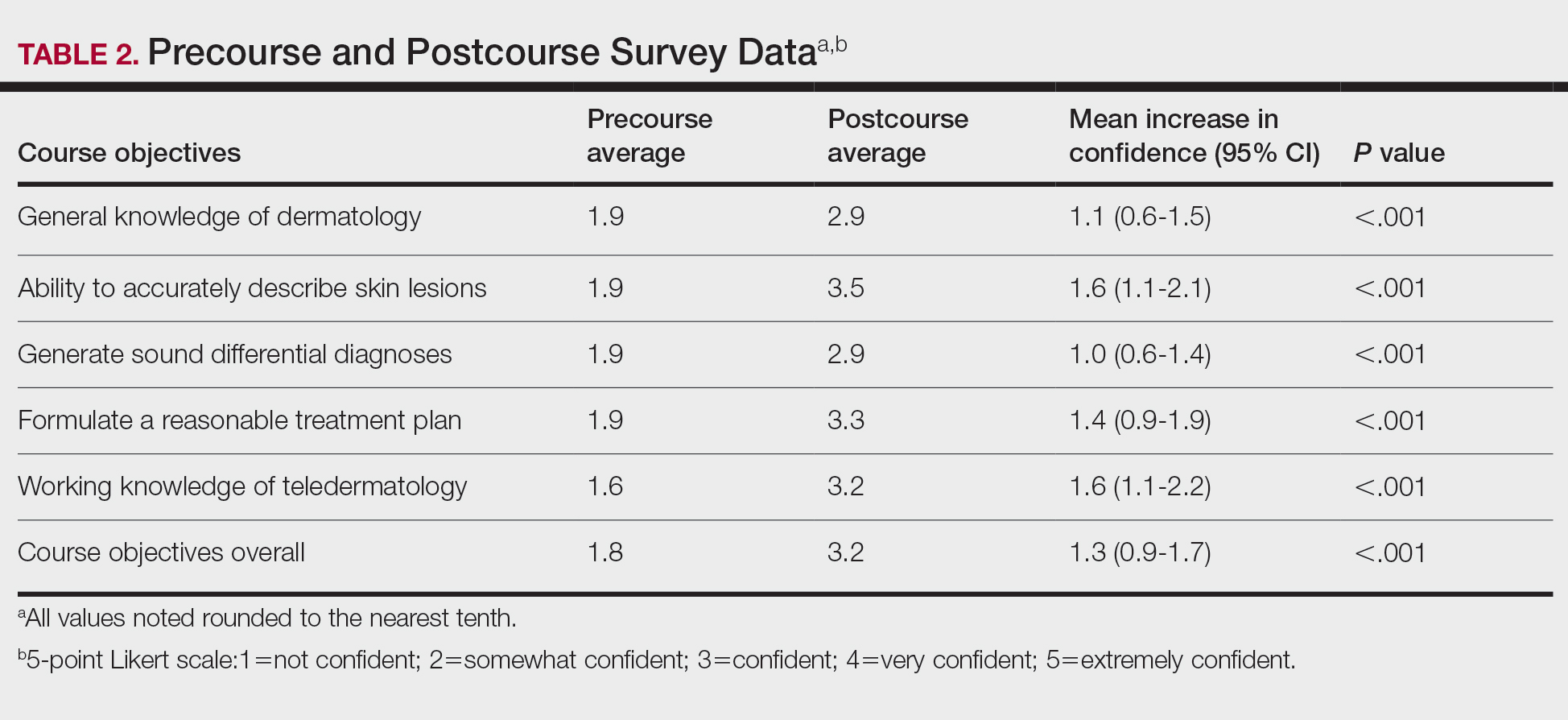
Comment
The DL dermatology course succeeded in helping the enrolled students attain course objectives and offered a reasonable solution when in-person interaction was restricted. The students in the DL course made notable improvements in their dermatology knowledge and improved their communication, diagnosis, and management skills. Although a blended dermatology curriculum with e-learning combined with clinical experience has been shown to increase knowledge acquisition,13,14 our results suggest that an online-only program also can increase comprehension as well as students’ confidence in their abilities.
A major challenge for the DL course was the lack of opportunity to perform common dermatology procedures. The addition of a hands-on skin procedure module would have been a great supplement to the course but was not possible due to social distancing guidelines during the COVID-19 pandemic. The small sample size and voluntary enrollment were limitations to this study.
Conclusion
Although the traditional dermatology rotation remains the gold standard for clinical instruction, a well-organized DL teaching environment allowed for a more controlled learning experience with a broader coverage of topics to include potentially greater exposure to rare skin disorders not typically encountered in everyday practice. A DL dermatology course may serve as an enduring curriculum for those who wish to learn dermatology more broadly and are not interested in performing skin procedures or direct patient exposure (eg, those pursuing non–primary care specialties, pathology, or radiology). It also may be attractive to students who have had a prior clinical dermatology rotation and desire a different learning experience with a wide coverage of topics.
Acknowledgments—The authors thank Thomas Darling, MD, PhD (Bethesda, Maryland), for coining the term Clinpic and providing critical feedback throughout the course. The authors also thank Sorana Raiciulescu, MS (Bethesda, Maryland), for assistance with the statistical analysis.
- Emanuel EJ. The inevitable reimagining of medical education. JAMA. 2020;323:1127-1128.
- Skochelak SE, Stack SJ. Creating the medical schools of the future. Acad Med. 2017;92:16-19.
- Vallée A, Blacher J, Cariou A, et al. Blended learning compared to traditional learning in medical education: systematic review and meta-analysis. J Med Internet Res. 2020;22:E16504.
- Rangachari D, Brown LE, Kern DE, et al. Clinical coaching: evolving the apprenticeship model for modern housestaff. Med Teach. 2017;39:780-782.
- Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Can Fam Physician. 2018;64:832-840.
- McCleskey PE, Gilson RT, DeVillez RL. Medical student core curriculum in dermatology survey. J Am Acad Dermatol. 2009;61:30-35.e4.
- Ulman CA, Binder SB, Borges NJ. Assessment of medical students’ proficiency in dermatology: are medical students adequately prepared to diagnose and treat common dermatologic conditions in the United States? J Educ Eval Health Prof. 2015;12:18.
- Loh TY, Hsiao JL, Shi VY. COVID-19 and its effect on medical student education in dermatology. J Am Acad Dermatol. 2020;83:E163-E164.
- Hilburg R, Patel N, Ambruso S, et al. Medical education during the coronavirus disease-2019 pandemic: learning from a distance. Adv Chronic Kidney Dis. 2020;27:412-417.
- Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323:2131-2132.
- McCleskey PE. Clinic teaching made easy: a prospective study of the American Academy of Dermatology core curriculum in primary care learners. J Am Acad Dermatol. 2013;69:273-279.e1.
- Paired T Test calculator. Statistics Kingdom website. Accessed February 7, 2022. http://www.statskingdom.com/160MeanT2pair.html
- Fransen F, Martens H, Nagtzaam I, et al. Use of e-learning in clinical clerkships: effects on acquisition of dermatological knowledge and learning processes. Int J Med Educ. 2018;9:11-17.
- Silva CS, Souza MB, Silva Filho RS, et al. E-learning program for medical students in dermatology. Clinics. 2011;66:619-622.
- Emanuel EJ. The inevitable reimagining of medical education. JAMA. 2020;323:1127-1128.
- Skochelak SE, Stack SJ. Creating the medical schools of the future. Acad Med. 2017;92:16-19.
- Vallée A, Blacher J, Cariou A, et al. Blended learning compared to traditional learning in medical education: systematic review and meta-analysis. J Med Internet Res. 2020;22:E16504.
- Rangachari D, Brown LE, Kern DE, et al. Clinical coaching: evolving the apprenticeship model for modern housestaff. Med Teach. 2017;39:780-782.
- Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Can Fam Physician. 2018;64:832-840.
- McCleskey PE, Gilson RT, DeVillez RL. Medical student core curriculum in dermatology survey. J Am Acad Dermatol. 2009;61:30-35.e4.
- Ulman CA, Binder SB, Borges NJ. Assessment of medical students’ proficiency in dermatology: are medical students adequately prepared to diagnose and treat common dermatologic conditions in the United States? J Educ Eval Health Prof. 2015;12:18.
- Loh TY, Hsiao JL, Shi VY. COVID-19 and its effect on medical student education in dermatology. J Am Acad Dermatol. 2020;83:E163-E164.
- Hilburg R, Patel N, Ambruso S, et al. Medical education during the coronavirus disease-2019 pandemic: learning from a distance. Adv Chronic Kidney Dis. 2020;27:412-417.
- Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323:2131-2132.
- McCleskey PE. Clinic teaching made easy: a prospective study of the American Academy of Dermatology core curriculum in primary care learners. J Am Acad Dermatol. 2013;69:273-279.e1.
- Paired T Test calculator. Statistics Kingdom website. Accessed February 7, 2022. http://www.statskingdom.com/160MeanT2pair.html
- Fransen F, Martens H, Nagtzaam I, et al. Use of e-learning in clinical clerkships: effects on acquisition of dermatological knowledge and learning processes. Int J Med Educ. 2018;9:11-17.
- Silva CS, Souza MB, Silva Filho RS, et al. E-learning program for medical students in dermatology. Clinics. 2011;66:619-622.
Practice Points
- An e-learning distance learning (DL) dermatology course can substantially improve clinically relevant skills and knowledge in dermatology.
- A DL dermatology course may serve as an alternative to clinical rotations for those who wish to learn dermatology more broadly and are not interested in performing skin procedures or direct patient exposure.
Study: Physical fitness in children linked with concentration, quality of life
The findings of the German study involving more than 6,500 kids emphasize the importance of cardiorespiratory health in childhood, and support physical fitness initiatives in schools, according to lead author Katharina Köble, MSc, of the Technical University of Munich (Germany), and colleagues.
“Recent studies show that only a few children meet the recommendations of physical activity,” the investigators wrote in Journal of Clinical Medicine.
While the health benefits of physical activity are clearly documented, Ms. Köble and colleagues noted that typical measures of activity, such as accelerometers or self-reported questionnaires, are suboptimal research tools.
“Physical fitness is a more objective parameter to quantify when evaluating health promotion,” the investigators wrote. “Furthermore, cardiorespiratory fitness as part of physical fitness is more strongly related to risk factors of cardiovascular disease than physical activity.”
According to the investigators, physical fitness has also been linked with better concentration and HRQOL, but never in the same population of children.
The new study aimed to address this knowledge gap by assessing 6,533 healthy children aged 6-10 years, approximately half boys and half girls. Associations between physical fitness, concentration, and HRQOL were evaluated using multiple linear regression analysis in participants aged 9-10 years.
Physical fitness was measured using a series of challenges, including curl-ups (pull-ups with palms facing body), push-ups, standing long jump, handgrip strength measurement, and Progressive Aerobic Cardiovascular Endurance Run (PACER). Performing the multistage shuttle run, PACER, “requires participants to maintain the pace set by an audio signal, which progressively increases the intensity every minute.” Results of the PACER test were used to estimate VO2max.
Concentration was measured using the d2-R test, “a paper-pencil cancellation test, where subjects have to cross out all ‘d’ letters with two dashes under a time limit.”
HRQOL was evaluated with the KINDL questionnaire, which covers emotional well-being, physical well-being, everyday functioning (school), friends, family, and self-esteem.
Analysis showed that physical fitness improved with age (P < .001), except for VO2max in girls (P = .129). Concentration also improved with age (P < .001), while HRQOL did not (P = .179).
Among children aged 9-10 years, VO2max scores were strongly associated with both HRQOL (P < .001) and concentration (P < .001).
“VO2max was found to be one of the main factors influencing concentration levels and HRQOL dimensions in primary school children,” the investigators wrote. “Physical fitness, especially cardiorespiratory performance, should therefore be promoted more specifically in school settings to support the promotion of an overall healthy lifestyle in children and adolescents.”
Findings are having a real-word impact, according to researcher
In an interview, Ms. Köble noted that the findings are already having a real-world impact.
“We continued data assessment in the long-term and specifically adapted prevention programs in school to the needs of the school children we identified in our study,” she said. “Schools are partially offering specific movement and nutrition classes now.”
In addition, Ms. Köble and colleagues plan on educating teachers about the “urgent need for sufficient physical activity.”
“Academic performance should be considered as an additional health factor in future studies, as well as screen time and eating patterns, as all those variables showed interactions with physical fitness and concentration. In a subanalysis, we showed that children with better physical fitness and concentration values were those who usually went to higher education secondary schools,” they wrote.
VO2max did not correlate with BMI
Gregory Weaver, MD, a pediatrician at Cleveland Clinic Children’s, voiced some concerns about the reliability of the findings. He noted that VO2max did not correlate with body mass index or other measures of physical fitness, and that using the PACER test to estimate VO2max may have skewed the association between physical fitness and concentration.
“It is quite conceivable that children who can maintain the focus to perform maximally on this test will also do well on other tests of attention/concentration,” Dr. Weaver said. “Most children I know would have a very difficult time performing a physical fitness test which requires them to match a recorded pace that slowly increases overtime. I’m not an expert in the area, but it is my understanding that usually VO2max tests involve a treadmill which allows investigators to have complete control over pace.”
Dr. Weaver concluded that more work is needed to determine if physical fitness interventions can have a positive impact on HRQOL and concentration.
“I think the authors of this study attempted to ask an important question about the possible association between physical fitness and concentration among school aged children,” Dr. Weaver said in an interview. “But what is even more vital are studies demonstrating that a change in modifiable health factors like nutrition, physical fitness, or the built environment can improve quality of life. I was hoping the authors would show that an improvement in VO2max over time resulted in an improvement in concentration. Frustratingly, that is not what this article demonstrates.”
The investigators and Dr. Weaver reported no conflicts of interest.
The findings of the German study involving more than 6,500 kids emphasize the importance of cardiorespiratory health in childhood, and support physical fitness initiatives in schools, according to lead author Katharina Köble, MSc, of the Technical University of Munich (Germany), and colleagues.
“Recent studies show that only a few children meet the recommendations of physical activity,” the investigators wrote in Journal of Clinical Medicine.
While the health benefits of physical activity are clearly documented, Ms. Köble and colleagues noted that typical measures of activity, such as accelerometers or self-reported questionnaires, are suboptimal research tools.
“Physical fitness is a more objective parameter to quantify when evaluating health promotion,” the investigators wrote. “Furthermore, cardiorespiratory fitness as part of physical fitness is more strongly related to risk factors of cardiovascular disease than physical activity.”
According to the investigators, physical fitness has also been linked with better concentration and HRQOL, but never in the same population of children.
The new study aimed to address this knowledge gap by assessing 6,533 healthy children aged 6-10 years, approximately half boys and half girls. Associations between physical fitness, concentration, and HRQOL were evaluated using multiple linear regression analysis in participants aged 9-10 years.
Physical fitness was measured using a series of challenges, including curl-ups (pull-ups with palms facing body), push-ups, standing long jump, handgrip strength measurement, and Progressive Aerobic Cardiovascular Endurance Run (PACER). Performing the multistage shuttle run, PACER, “requires participants to maintain the pace set by an audio signal, which progressively increases the intensity every minute.” Results of the PACER test were used to estimate VO2max.
Concentration was measured using the d2-R test, “a paper-pencil cancellation test, where subjects have to cross out all ‘d’ letters with two dashes under a time limit.”
HRQOL was evaluated with the KINDL questionnaire, which covers emotional well-being, physical well-being, everyday functioning (school), friends, family, and self-esteem.
Analysis showed that physical fitness improved with age (P < .001), except for VO2max in girls (P = .129). Concentration also improved with age (P < .001), while HRQOL did not (P = .179).
Among children aged 9-10 years, VO2max scores were strongly associated with both HRQOL (P < .001) and concentration (P < .001).
“VO2max was found to be one of the main factors influencing concentration levels and HRQOL dimensions in primary school children,” the investigators wrote. “Physical fitness, especially cardiorespiratory performance, should therefore be promoted more specifically in school settings to support the promotion of an overall healthy lifestyle in children and adolescents.”
Findings are having a real-word impact, according to researcher
In an interview, Ms. Köble noted that the findings are already having a real-world impact.
“We continued data assessment in the long-term and specifically adapted prevention programs in school to the needs of the school children we identified in our study,” she said. “Schools are partially offering specific movement and nutrition classes now.”
In addition, Ms. Köble and colleagues plan on educating teachers about the “urgent need for sufficient physical activity.”
“Academic performance should be considered as an additional health factor in future studies, as well as screen time and eating patterns, as all those variables showed interactions with physical fitness and concentration. In a subanalysis, we showed that children with better physical fitness and concentration values were those who usually went to higher education secondary schools,” they wrote.
VO2max did not correlate with BMI
Gregory Weaver, MD, a pediatrician at Cleveland Clinic Children’s, voiced some concerns about the reliability of the findings. He noted that VO2max did not correlate with body mass index or other measures of physical fitness, and that using the PACER test to estimate VO2max may have skewed the association between physical fitness and concentration.
“It is quite conceivable that children who can maintain the focus to perform maximally on this test will also do well on other tests of attention/concentration,” Dr. Weaver said. “Most children I know would have a very difficult time performing a physical fitness test which requires them to match a recorded pace that slowly increases overtime. I’m not an expert in the area, but it is my understanding that usually VO2max tests involve a treadmill which allows investigators to have complete control over pace.”
Dr. Weaver concluded that more work is needed to determine if physical fitness interventions can have a positive impact on HRQOL and concentration.
“I think the authors of this study attempted to ask an important question about the possible association between physical fitness and concentration among school aged children,” Dr. Weaver said in an interview. “But what is even more vital are studies demonstrating that a change in modifiable health factors like nutrition, physical fitness, or the built environment can improve quality of life. I was hoping the authors would show that an improvement in VO2max over time resulted in an improvement in concentration. Frustratingly, that is not what this article demonstrates.”
The investigators and Dr. Weaver reported no conflicts of interest.
The findings of the German study involving more than 6,500 kids emphasize the importance of cardiorespiratory health in childhood, and support physical fitness initiatives in schools, according to lead author Katharina Köble, MSc, of the Technical University of Munich (Germany), and colleagues.
“Recent studies show that only a few children meet the recommendations of physical activity,” the investigators wrote in Journal of Clinical Medicine.
While the health benefits of physical activity are clearly documented, Ms. Köble and colleagues noted that typical measures of activity, such as accelerometers or self-reported questionnaires, are suboptimal research tools.
“Physical fitness is a more objective parameter to quantify when evaluating health promotion,” the investigators wrote. “Furthermore, cardiorespiratory fitness as part of physical fitness is more strongly related to risk factors of cardiovascular disease than physical activity.”
According to the investigators, physical fitness has also been linked with better concentration and HRQOL, but never in the same population of children.
The new study aimed to address this knowledge gap by assessing 6,533 healthy children aged 6-10 years, approximately half boys and half girls. Associations between physical fitness, concentration, and HRQOL were evaluated using multiple linear regression analysis in participants aged 9-10 years.
Physical fitness was measured using a series of challenges, including curl-ups (pull-ups with palms facing body), push-ups, standing long jump, handgrip strength measurement, and Progressive Aerobic Cardiovascular Endurance Run (PACER). Performing the multistage shuttle run, PACER, “requires participants to maintain the pace set by an audio signal, which progressively increases the intensity every minute.” Results of the PACER test were used to estimate VO2max.
Concentration was measured using the d2-R test, “a paper-pencil cancellation test, where subjects have to cross out all ‘d’ letters with two dashes under a time limit.”
HRQOL was evaluated with the KINDL questionnaire, which covers emotional well-being, physical well-being, everyday functioning (school), friends, family, and self-esteem.
Analysis showed that physical fitness improved with age (P < .001), except for VO2max in girls (P = .129). Concentration also improved with age (P < .001), while HRQOL did not (P = .179).
Among children aged 9-10 years, VO2max scores were strongly associated with both HRQOL (P < .001) and concentration (P < .001).
“VO2max was found to be one of the main factors influencing concentration levels and HRQOL dimensions in primary school children,” the investigators wrote. “Physical fitness, especially cardiorespiratory performance, should therefore be promoted more specifically in school settings to support the promotion of an overall healthy lifestyle in children and adolescents.”
Findings are having a real-word impact, according to researcher
In an interview, Ms. Köble noted that the findings are already having a real-world impact.
“We continued data assessment in the long-term and specifically adapted prevention programs in school to the needs of the school children we identified in our study,” she said. “Schools are partially offering specific movement and nutrition classes now.”
In addition, Ms. Köble and colleagues plan on educating teachers about the “urgent need for sufficient physical activity.”
“Academic performance should be considered as an additional health factor in future studies, as well as screen time and eating patterns, as all those variables showed interactions with physical fitness and concentration. In a subanalysis, we showed that children with better physical fitness and concentration values were those who usually went to higher education secondary schools,” they wrote.
VO2max did not correlate with BMI
Gregory Weaver, MD, a pediatrician at Cleveland Clinic Children’s, voiced some concerns about the reliability of the findings. He noted that VO2max did not correlate with body mass index or other measures of physical fitness, and that using the PACER test to estimate VO2max may have skewed the association between physical fitness and concentration.
“It is quite conceivable that children who can maintain the focus to perform maximally on this test will also do well on other tests of attention/concentration,” Dr. Weaver said. “Most children I know would have a very difficult time performing a physical fitness test which requires them to match a recorded pace that slowly increases overtime. I’m not an expert in the area, but it is my understanding that usually VO2max tests involve a treadmill which allows investigators to have complete control over pace.”
Dr. Weaver concluded that more work is needed to determine if physical fitness interventions can have a positive impact on HRQOL and concentration.
“I think the authors of this study attempted to ask an important question about the possible association between physical fitness and concentration among school aged children,” Dr. Weaver said in an interview. “But what is even more vital are studies demonstrating that a change in modifiable health factors like nutrition, physical fitness, or the built environment can improve quality of life. I was hoping the authors would show that an improvement in VO2max over time resulted in an improvement in concentration. Frustratingly, that is not what this article demonstrates.”
The investigators and Dr. Weaver reported no conflicts of interest.
FROM THE JOURNAL OF CLINICAL MEDICINE
Lung cancer in 2030: Expand genotyping
In recent years, –both of which have led to improved survival rates. But what will lung cancer look like in 2030?
Pasi A. Janne, MD, PhD, of the Dana-Farber Cancer Institute, Boston, hopes to see improved access to tumor and blood-based genotyping.
Dr. Janne, who serves as director of the Lowe Center for Thoracic Oncology at Dana-Farber, gave a keynote presentation at the 2022 European Lung Cancer Congress, where he highlighted the need to broaden the scope of targeted therapies, make “great drugs work even better,” improve the ability to treat patients based on risk level, and expand the use of targeted therapies in the adjuvant and neoadjuvant setting to make significant progress in the treatment lung cancer treatment in coming years.
Genotyping is underutilized, he said. A 2019 multicenter study reported at the annual meeting of the American Society of Clinical Oncology showed that only 54% of 1,203 patients underwent testing for EGFR mutations, 22% were tested for EGFR, ALK, ROS1, and BRAF mutations, and only 7% were tested for all biomarkers recommended by National Comprehensive Cancer Network guidelines at the time.
That study also showed that only 45% of patients received biomarker-driven treatment, even when driver mutations were detected.
“Immunotherapy was often prescribed instead of targeted therapy, even when molecular results were available,” Dr. Janne said.
Another study, reported at the 2021 ASCO annual meeting, showed some improvement in testing rates, but still, only 37% of patients were tested for all biomarkers as recommended.
Racial disparities in testing have also been observed. Bruno and colleagues found that any next-generation sequencing was performed in 50.1% of White patients, compared with 39.8% of black patients, and NGS prior to first-line therapy was performed in 35.5% and 25.8%, respectively.
The study, also reported at ASCO in 2021, showed that trial participation was observed among 3.9% of White patients and 1.9% of Black patients.
“The studies really highlight the need for increased testing rates and appropriate utilization of testing results to deliver optimal care to our patients with advanced lung cancer. We have a long way to go. To live the promise and appreciate the promise of precision therapy ... we need to be able to offer this testing to all of our patients with lung cancer,” he said.
Dr. Janne reported relationships with numerous pharmaceutical companies, including consulting, research support and stock ownership. He also receives postmarketing royalties from Dana-Farber Cancer Institute–owned intellectual property on EGFR mutations.
In recent years, –both of which have led to improved survival rates. But what will lung cancer look like in 2030?
Pasi A. Janne, MD, PhD, of the Dana-Farber Cancer Institute, Boston, hopes to see improved access to tumor and blood-based genotyping.
Dr. Janne, who serves as director of the Lowe Center for Thoracic Oncology at Dana-Farber, gave a keynote presentation at the 2022 European Lung Cancer Congress, where he highlighted the need to broaden the scope of targeted therapies, make “great drugs work even better,” improve the ability to treat patients based on risk level, and expand the use of targeted therapies in the adjuvant and neoadjuvant setting to make significant progress in the treatment lung cancer treatment in coming years.
Genotyping is underutilized, he said. A 2019 multicenter study reported at the annual meeting of the American Society of Clinical Oncology showed that only 54% of 1,203 patients underwent testing for EGFR mutations, 22% were tested for EGFR, ALK, ROS1, and BRAF mutations, and only 7% were tested for all biomarkers recommended by National Comprehensive Cancer Network guidelines at the time.
That study also showed that only 45% of patients received biomarker-driven treatment, even when driver mutations were detected.
“Immunotherapy was often prescribed instead of targeted therapy, even when molecular results were available,” Dr. Janne said.
Another study, reported at the 2021 ASCO annual meeting, showed some improvement in testing rates, but still, only 37% of patients were tested for all biomarkers as recommended.
Racial disparities in testing have also been observed. Bruno and colleagues found that any next-generation sequencing was performed in 50.1% of White patients, compared with 39.8% of black patients, and NGS prior to first-line therapy was performed in 35.5% and 25.8%, respectively.
The study, also reported at ASCO in 2021, showed that trial participation was observed among 3.9% of White patients and 1.9% of Black patients.
“The studies really highlight the need for increased testing rates and appropriate utilization of testing results to deliver optimal care to our patients with advanced lung cancer. We have a long way to go. To live the promise and appreciate the promise of precision therapy ... we need to be able to offer this testing to all of our patients with lung cancer,” he said.
Dr. Janne reported relationships with numerous pharmaceutical companies, including consulting, research support and stock ownership. He also receives postmarketing royalties from Dana-Farber Cancer Institute–owned intellectual property on EGFR mutations.
In recent years, –both of which have led to improved survival rates. But what will lung cancer look like in 2030?
Pasi A. Janne, MD, PhD, of the Dana-Farber Cancer Institute, Boston, hopes to see improved access to tumor and blood-based genotyping.
Dr. Janne, who serves as director of the Lowe Center for Thoracic Oncology at Dana-Farber, gave a keynote presentation at the 2022 European Lung Cancer Congress, where he highlighted the need to broaden the scope of targeted therapies, make “great drugs work even better,” improve the ability to treat patients based on risk level, and expand the use of targeted therapies in the adjuvant and neoadjuvant setting to make significant progress in the treatment lung cancer treatment in coming years.
Genotyping is underutilized, he said. A 2019 multicenter study reported at the annual meeting of the American Society of Clinical Oncology showed that only 54% of 1,203 patients underwent testing for EGFR mutations, 22% were tested for EGFR, ALK, ROS1, and BRAF mutations, and only 7% were tested for all biomarkers recommended by National Comprehensive Cancer Network guidelines at the time.
That study also showed that only 45% of patients received biomarker-driven treatment, even when driver mutations were detected.
“Immunotherapy was often prescribed instead of targeted therapy, even when molecular results were available,” Dr. Janne said.
Another study, reported at the 2021 ASCO annual meeting, showed some improvement in testing rates, but still, only 37% of patients were tested for all biomarkers as recommended.
Racial disparities in testing have also been observed. Bruno and colleagues found that any next-generation sequencing was performed in 50.1% of White patients, compared with 39.8% of black patients, and NGS prior to first-line therapy was performed in 35.5% and 25.8%, respectively.
The study, also reported at ASCO in 2021, showed that trial participation was observed among 3.9% of White patients and 1.9% of Black patients.
“The studies really highlight the need for increased testing rates and appropriate utilization of testing results to deliver optimal care to our patients with advanced lung cancer. We have a long way to go. To live the promise and appreciate the promise of precision therapy ... we need to be able to offer this testing to all of our patients with lung cancer,” he said.
Dr. Janne reported relationships with numerous pharmaceutical companies, including consulting, research support and stock ownership. He also receives postmarketing royalties from Dana-Farber Cancer Institute–owned intellectual property on EGFR mutations.
FROM ELCC 2022
Weighing the complexity of pathological response in lung cancer
studies, but much work remains to be done, said William D. Travis, MD, director of thoracic pathology at Memorial Sloan Kettering Cancer Center, New York.
In a keynote address at the 2022 European Lung Cancer Conference, Dr. Travis highlighted advances in the use of pathological response in this setting and outlined areas that need refinement. “Pathologic response after preoperative therapy is important because the extent of pathologic response strongly correlates with improved overall survival, and it is reflective of neoadjuvant therapy. The degree of response is associated with the degree of benefit in survival, and it’s being used as a surrogate for survival in phase 2 and 3 neoadjuvant clinical trials.”
In fact, multiple studies have demonstrated that non–small cell lung cancer patients with 10% or less viable residual tumor after treatment have improved overall survival and disease-free survival, compared with patients who have more residual tumor, he explained.
Recent studies have demonstrated the value of pathological response as an endpoint in the neoadjuvant therapy and molecular targeted therapy setting, he said, citing a study published in the Journal of Clinical Oncology that showed major pathological response rates of 14%-45% and pathological complete response rates up to 29% in patients treated with single-agent checkpoint inhibition.
In the CheckMate 816 trial, both major pathologic response and pathological complete response were significantly higher in patients treated with combination nivolumab and chemotherapy, compared with those treated with chemotherapy alone (37% vs. 8.9% and 24% vs. 2%, respectively).
“This high rate of responses with combined immunotherapy and chemotherapy is quite exciting,” he said.
Dr. Travis also stressed the importance of consulting the current International Association for the Study of Lung Cancer Recommendations for Pathologic Assessment of Lung Cancer Resection Specimens After Neoadjuvant Therapy.
He highlighted several key points regarding pathological response in lung cancer:
- Major pathological response (MPR) is calculated as the estimated size of viable tumor divided by the size of the tumor bed.
- Optimal cutoffs for determining MPR is currently 10%, but recent data suggest that in the conventional chemotherapy setting this may vary by tumor histology, with much higher cutoffs of about 65% for adenocarcinoma.
- Estimating the amount of viable tumor is “quite complicated and requires quite a number of steps,” and one the most important steps is “for the surgeon to the pathologist know that given specimen is from a patient who received neoadjuvant therapy.”
- Determining the border of the tumor bed can be challenging, therefore “resection specimens after neoadjuvant therapy should be sampled to optimize comprehensive gross and histologic assessment of the lung tumor bed for pathologic response ... as outlined in the guidelines.”
- The IASLC panel determined that having a single approach for estimating treatment effect would be best, despite the different therapy types and combinations used, but “it is recognized that there may be certain types of features that need to be addressed,” such as immune cell infiltrates in pats who received immunotherapy.
- The recommendations provide specific guidance for measuring tumor size for staging, including for special circumstances.
As for future direction, Dr. Travis said, “one question is how to assess treatment effect in lymph node samples.
“This is done for lymph nodes in breast cancer but not in lung cancer. We need system[s] for lung cancer.”
Good “infrastructure for pathology departments” is needed to support clinical trials, he said, noting that the team at Memorial Sloan Kettering Cancer Center includes physician assistants, tissue procurement staff, frozen section techs, research fellows, and research assistants.
Future work should also aim to standardize pathology assessment for clinical trials, improve the current recommendations, make use of new technology like artificial intelligence, optimize banking protocols and special techniques, and identify radiologic-pathological correlations, he said.
He added that “IASLC is promoting the design and implementation of an international database to collect uniformly clinical and pathologic information with the ultimate goal of fostering collaboration and to facilitate the identification of surrogate endpoints of long-term survival.”
Dr. Travis is a nonpaid pathology consultant for the LCMC3 and LCMC4 trials.
studies, but much work remains to be done, said William D. Travis, MD, director of thoracic pathology at Memorial Sloan Kettering Cancer Center, New York.
In a keynote address at the 2022 European Lung Cancer Conference, Dr. Travis highlighted advances in the use of pathological response in this setting and outlined areas that need refinement. “Pathologic response after preoperative therapy is important because the extent of pathologic response strongly correlates with improved overall survival, and it is reflective of neoadjuvant therapy. The degree of response is associated with the degree of benefit in survival, and it’s being used as a surrogate for survival in phase 2 and 3 neoadjuvant clinical trials.”
In fact, multiple studies have demonstrated that non–small cell lung cancer patients with 10% or less viable residual tumor after treatment have improved overall survival and disease-free survival, compared with patients who have more residual tumor, he explained.
Recent studies have demonstrated the value of pathological response as an endpoint in the neoadjuvant therapy and molecular targeted therapy setting, he said, citing a study published in the Journal of Clinical Oncology that showed major pathological response rates of 14%-45% and pathological complete response rates up to 29% in patients treated with single-agent checkpoint inhibition.
In the CheckMate 816 trial, both major pathologic response and pathological complete response were significantly higher in patients treated with combination nivolumab and chemotherapy, compared with those treated with chemotherapy alone (37% vs. 8.9% and 24% vs. 2%, respectively).
“This high rate of responses with combined immunotherapy and chemotherapy is quite exciting,” he said.
Dr. Travis also stressed the importance of consulting the current International Association for the Study of Lung Cancer Recommendations for Pathologic Assessment of Lung Cancer Resection Specimens After Neoadjuvant Therapy.
He highlighted several key points regarding pathological response in lung cancer:
- Major pathological response (MPR) is calculated as the estimated size of viable tumor divided by the size of the tumor bed.
- Optimal cutoffs for determining MPR is currently 10%, but recent data suggest that in the conventional chemotherapy setting this may vary by tumor histology, with much higher cutoffs of about 65% for adenocarcinoma.
- Estimating the amount of viable tumor is “quite complicated and requires quite a number of steps,” and one the most important steps is “for the surgeon to the pathologist know that given specimen is from a patient who received neoadjuvant therapy.”
- Determining the border of the tumor bed can be challenging, therefore “resection specimens after neoadjuvant therapy should be sampled to optimize comprehensive gross and histologic assessment of the lung tumor bed for pathologic response ... as outlined in the guidelines.”
- The IASLC panel determined that having a single approach for estimating treatment effect would be best, despite the different therapy types and combinations used, but “it is recognized that there may be certain types of features that need to be addressed,” such as immune cell infiltrates in pats who received immunotherapy.
- The recommendations provide specific guidance for measuring tumor size for staging, including for special circumstances.
As for future direction, Dr. Travis said, “one question is how to assess treatment effect in lymph node samples.
“This is done for lymph nodes in breast cancer but not in lung cancer. We need system[s] for lung cancer.”
Good “infrastructure for pathology departments” is needed to support clinical trials, he said, noting that the team at Memorial Sloan Kettering Cancer Center includes physician assistants, tissue procurement staff, frozen section techs, research fellows, and research assistants.
Future work should also aim to standardize pathology assessment for clinical trials, improve the current recommendations, make use of new technology like artificial intelligence, optimize banking protocols and special techniques, and identify radiologic-pathological correlations, he said.
He added that “IASLC is promoting the design and implementation of an international database to collect uniformly clinical and pathologic information with the ultimate goal of fostering collaboration and to facilitate the identification of surrogate endpoints of long-term survival.”
Dr. Travis is a nonpaid pathology consultant for the LCMC3 and LCMC4 trials.
studies, but much work remains to be done, said William D. Travis, MD, director of thoracic pathology at Memorial Sloan Kettering Cancer Center, New York.
In a keynote address at the 2022 European Lung Cancer Conference, Dr. Travis highlighted advances in the use of pathological response in this setting and outlined areas that need refinement. “Pathologic response after preoperative therapy is important because the extent of pathologic response strongly correlates with improved overall survival, and it is reflective of neoadjuvant therapy. The degree of response is associated with the degree of benefit in survival, and it’s being used as a surrogate for survival in phase 2 and 3 neoadjuvant clinical trials.”
In fact, multiple studies have demonstrated that non–small cell lung cancer patients with 10% or less viable residual tumor after treatment have improved overall survival and disease-free survival, compared with patients who have more residual tumor, he explained.
Recent studies have demonstrated the value of pathological response as an endpoint in the neoadjuvant therapy and molecular targeted therapy setting, he said, citing a study published in the Journal of Clinical Oncology that showed major pathological response rates of 14%-45% and pathological complete response rates up to 29% in patients treated with single-agent checkpoint inhibition.
In the CheckMate 816 trial, both major pathologic response and pathological complete response were significantly higher in patients treated with combination nivolumab and chemotherapy, compared with those treated with chemotherapy alone (37% vs. 8.9% and 24% vs. 2%, respectively).
“This high rate of responses with combined immunotherapy and chemotherapy is quite exciting,” he said.
Dr. Travis also stressed the importance of consulting the current International Association for the Study of Lung Cancer Recommendations for Pathologic Assessment of Lung Cancer Resection Specimens After Neoadjuvant Therapy.
He highlighted several key points regarding pathological response in lung cancer:
- Major pathological response (MPR) is calculated as the estimated size of viable tumor divided by the size of the tumor bed.
- Optimal cutoffs for determining MPR is currently 10%, but recent data suggest that in the conventional chemotherapy setting this may vary by tumor histology, with much higher cutoffs of about 65% for adenocarcinoma.
- Estimating the amount of viable tumor is “quite complicated and requires quite a number of steps,” and one the most important steps is “for the surgeon to the pathologist know that given specimen is from a patient who received neoadjuvant therapy.”
- Determining the border of the tumor bed can be challenging, therefore “resection specimens after neoadjuvant therapy should be sampled to optimize comprehensive gross and histologic assessment of the lung tumor bed for pathologic response ... as outlined in the guidelines.”
- The IASLC panel determined that having a single approach for estimating treatment effect would be best, despite the different therapy types and combinations used, but “it is recognized that there may be certain types of features that need to be addressed,” such as immune cell infiltrates in pats who received immunotherapy.
- The recommendations provide specific guidance for measuring tumor size for staging, including for special circumstances.
As for future direction, Dr. Travis said, “one question is how to assess treatment effect in lymph node samples.
“This is done for lymph nodes in breast cancer but not in lung cancer. We need system[s] for lung cancer.”
Good “infrastructure for pathology departments” is needed to support clinical trials, he said, noting that the team at Memorial Sloan Kettering Cancer Center includes physician assistants, tissue procurement staff, frozen section techs, research fellows, and research assistants.
Future work should also aim to standardize pathology assessment for clinical trials, improve the current recommendations, make use of new technology like artificial intelligence, optimize banking protocols and special techniques, and identify radiologic-pathological correlations, he said.
He added that “IASLC is promoting the design and implementation of an international database to collect uniformly clinical and pathologic information with the ultimate goal of fostering collaboration and to facilitate the identification of surrogate endpoints of long-term survival.”
Dr. Travis is a nonpaid pathology consultant for the LCMC3 and LCMC4 trials.
FROM ELCC 2022
FDA: Switch to disposable duodenoscope models
Health care facilities and providers should complete the transition to fully disposable duodenoscopes and those with disposable components, the U.S. Food and Drug Administration announced this week after an analysis of postmarket surveillance studies was completed.
The FDA’s directive updates its April 2020 recommendations on the subject. It cites concerns about cleaning fixed endcap duodenoscopes and the increasing availability of models that eliminate the need for reprocessing.
The announcement highlighted the potential for a dramatic difference in between-patient contamination risk, reducing it “by half or more as compared to reusable, or fixed endcaps.”
“Interim results from one duodenoscope model with a removable component show a contamination rate of just 0.5%, as compared to older duodenoscope models which had contamination rates as high as 6%,” the FDA writes.
Duodenoscopes are used in more than 500,000 procedures each year in the United States and are key in assessing and treating diseases and conditions of the pancreas and bile ducts.
Upgrade to new models to decrease infections
Manufacturers no longer market fixed endcap models in the United States, but some health care facilities continue to use them. The FDA recommends that all fixed endcap models be replaced.
The FDA says some manufacturers are offering replacement programs to upgrade to a model with a disposable component at no cost.
Two fully disposable models and five with disposable components have been cleared by the FDA. (One model is no longer marketed and thus not listed here.)
Fully Disposable:
Ambu Innovation GmbH, Duodenoscope model aScope Duodeno
Boston Scientific Corporation, EXALT Model D Single-Use Duodenoscope
Disposable Components:
Fujifilm Corporation, Duodenoscope model ED-580XT
Olympus Medical Systems, Evis Exera III Duodenovideoscope Olympus TJF-Q190V
Pentax Medical, Duodenoscope model ED34-i10T2
Pentax Medical, Duodenoscope model ED32-i10
Additionally, the failure to correctly reprocess a duodenoscope could result in tissue or fluid from one patient transferring to a subsequent patient.
“In rare cases, this can lead to patient-to-patient disease transmission,” the FDA says.
Postmarket surveillance studies
In 2015, the FDA ordered three manufacturers of reusable devices (Fujifilm, Olympus, and Pentax) to conduct postmarket surveillance studies to determine contamination rates after reprocessing.
In 2019, the FDA also ordered postmarket surveillance studies to the makers of duodenoscopes with disposable endcaps to verify that the new designs reduce the contamination rate.
The final results of the fixed endcap design indicate that contamination rates were as high as 6.6% with high-concern organisms after contamination. High-concern organisms are those more often associated with disease, such as E coli and Pseudomonas contamination.
“As a result, Pentax and Olympus are withdrawing their fixed endcap duodenoscopes from the market, and Fujifilm has completed withdrawal of its fixed endcap duodenoscope,” the FDA writes.
Studies are not yet complete for duodenoscopes with removable components. As of August 12, 2021, the Fujifilm ED-580XT duodenoscope with a removable cap had 57% of the samples required. Interim results indicate that no samples tested positive for enough low-concern organisms to indicate a reprocessing failure, and only 0.5% tested positive for high-concern organisms.
In addition to the contamination risk sampling, each manufacturer was ordered to do postmarket surveillance studies to evaluate whether staff could understand and follow the manufacturer’s reprocessing instructions in real-world health care settings.
According to the FDA, the results showed that users frequently had difficulty understanding and following the manufacturers’ instructions and were not able to successfully complete reprocessing with the older models.
However, the newer models had high user success rates for understanding instructions and correctly performing reprocessing tasks, the FDA says.
A version of this article first appeared on Medscape.com.
Health care facilities and providers should complete the transition to fully disposable duodenoscopes and those with disposable components, the U.S. Food and Drug Administration announced this week after an analysis of postmarket surveillance studies was completed.
The FDA’s directive updates its April 2020 recommendations on the subject. It cites concerns about cleaning fixed endcap duodenoscopes and the increasing availability of models that eliminate the need for reprocessing.
The announcement highlighted the potential for a dramatic difference in between-patient contamination risk, reducing it “by half or more as compared to reusable, or fixed endcaps.”
“Interim results from one duodenoscope model with a removable component show a contamination rate of just 0.5%, as compared to older duodenoscope models which had contamination rates as high as 6%,” the FDA writes.
Duodenoscopes are used in more than 500,000 procedures each year in the United States and are key in assessing and treating diseases and conditions of the pancreas and bile ducts.
Upgrade to new models to decrease infections
Manufacturers no longer market fixed endcap models in the United States, but some health care facilities continue to use them. The FDA recommends that all fixed endcap models be replaced.
The FDA says some manufacturers are offering replacement programs to upgrade to a model with a disposable component at no cost.
Two fully disposable models and five with disposable components have been cleared by the FDA. (One model is no longer marketed and thus not listed here.)
Fully Disposable:
Ambu Innovation GmbH, Duodenoscope model aScope Duodeno
Boston Scientific Corporation, EXALT Model D Single-Use Duodenoscope
Disposable Components:
Fujifilm Corporation, Duodenoscope model ED-580XT
Olympus Medical Systems, Evis Exera III Duodenovideoscope Olympus TJF-Q190V
Pentax Medical, Duodenoscope model ED34-i10T2
Pentax Medical, Duodenoscope model ED32-i10
Additionally, the failure to correctly reprocess a duodenoscope could result in tissue or fluid from one patient transferring to a subsequent patient.
“In rare cases, this can lead to patient-to-patient disease transmission,” the FDA says.
Postmarket surveillance studies
In 2015, the FDA ordered three manufacturers of reusable devices (Fujifilm, Olympus, and Pentax) to conduct postmarket surveillance studies to determine contamination rates after reprocessing.
In 2019, the FDA also ordered postmarket surveillance studies to the makers of duodenoscopes with disposable endcaps to verify that the new designs reduce the contamination rate.
The final results of the fixed endcap design indicate that contamination rates were as high as 6.6% with high-concern organisms after contamination. High-concern organisms are those more often associated with disease, such as E coli and Pseudomonas contamination.
“As a result, Pentax and Olympus are withdrawing their fixed endcap duodenoscopes from the market, and Fujifilm has completed withdrawal of its fixed endcap duodenoscope,” the FDA writes.
Studies are not yet complete for duodenoscopes with removable components. As of August 12, 2021, the Fujifilm ED-580XT duodenoscope with a removable cap had 57% of the samples required. Interim results indicate that no samples tested positive for enough low-concern organisms to indicate a reprocessing failure, and only 0.5% tested positive for high-concern organisms.
In addition to the contamination risk sampling, each manufacturer was ordered to do postmarket surveillance studies to evaluate whether staff could understand and follow the manufacturer’s reprocessing instructions in real-world health care settings.
According to the FDA, the results showed that users frequently had difficulty understanding and following the manufacturers’ instructions and were not able to successfully complete reprocessing with the older models.
However, the newer models had high user success rates for understanding instructions and correctly performing reprocessing tasks, the FDA says.
A version of this article first appeared on Medscape.com.
Health care facilities and providers should complete the transition to fully disposable duodenoscopes and those with disposable components, the U.S. Food and Drug Administration announced this week after an analysis of postmarket surveillance studies was completed.
The FDA’s directive updates its April 2020 recommendations on the subject. It cites concerns about cleaning fixed endcap duodenoscopes and the increasing availability of models that eliminate the need for reprocessing.
The announcement highlighted the potential for a dramatic difference in between-patient contamination risk, reducing it “by half or more as compared to reusable, or fixed endcaps.”
“Interim results from one duodenoscope model with a removable component show a contamination rate of just 0.5%, as compared to older duodenoscope models which had contamination rates as high as 6%,” the FDA writes.
Duodenoscopes are used in more than 500,000 procedures each year in the United States and are key in assessing and treating diseases and conditions of the pancreas and bile ducts.
Upgrade to new models to decrease infections
Manufacturers no longer market fixed endcap models in the United States, but some health care facilities continue to use them. The FDA recommends that all fixed endcap models be replaced.
The FDA says some manufacturers are offering replacement programs to upgrade to a model with a disposable component at no cost.
Two fully disposable models and five with disposable components have been cleared by the FDA. (One model is no longer marketed and thus not listed here.)
Fully Disposable:
Ambu Innovation GmbH, Duodenoscope model aScope Duodeno
Boston Scientific Corporation, EXALT Model D Single-Use Duodenoscope
Disposable Components:
Fujifilm Corporation, Duodenoscope model ED-580XT
Olympus Medical Systems, Evis Exera III Duodenovideoscope Olympus TJF-Q190V
Pentax Medical, Duodenoscope model ED34-i10T2
Pentax Medical, Duodenoscope model ED32-i10
Additionally, the failure to correctly reprocess a duodenoscope could result in tissue or fluid from one patient transferring to a subsequent patient.
“In rare cases, this can lead to patient-to-patient disease transmission,” the FDA says.
Postmarket surveillance studies
In 2015, the FDA ordered three manufacturers of reusable devices (Fujifilm, Olympus, and Pentax) to conduct postmarket surveillance studies to determine contamination rates after reprocessing.
In 2019, the FDA also ordered postmarket surveillance studies to the makers of duodenoscopes with disposable endcaps to verify that the new designs reduce the contamination rate.
The final results of the fixed endcap design indicate that contamination rates were as high as 6.6% with high-concern organisms after contamination. High-concern organisms are those more often associated with disease, such as E coli and Pseudomonas contamination.
“As a result, Pentax and Olympus are withdrawing their fixed endcap duodenoscopes from the market, and Fujifilm has completed withdrawal of its fixed endcap duodenoscope,” the FDA writes.
Studies are not yet complete for duodenoscopes with removable components. As of August 12, 2021, the Fujifilm ED-580XT duodenoscope with a removable cap had 57% of the samples required. Interim results indicate that no samples tested positive for enough low-concern organisms to indicate a reprocessing failure, and only 0.5% tested positive for high-concern organisms.
In addition to the contamination risk sampling, each manufacturer was ordered to do postmarket surveillance studies to evaluate whether staff could understand and follow the manufacturer’s reprocessing instructions in real-world health care settings.
According to the FDA, the results showed that users frequently had difficulty understanding and following the manufacturers’ instructions and were not able to successfully complete reprocessing with the older models.
However, the newer models had high user success rates for understanding instructions and correctly performing reprocessing tasks, the FDA says.
A version of this article first appeared on Medscape.com.
Hospitalists and PCPs crave greater communication
Hospitalists and PCPs want more dialogue while patients are in the hospital in order to coordinate and personalize care, according to data collected at Beth Israel Deaconess Medical Center, Boston. The results were presented at the annual meeting of the Society of General Internal Medicine.
“I think a major takeaway is that both hospitalists and primary care doctors agree that it’s important for primary care doctors to be involved in a patient’s hospitalization. They both identified a value that PCPs can bring to the table,” coresearcher Kristen Flint, MD, a primary care resident, told this news organization.
A majority in both camps reported that communication with the other party occurred in less than 25% of cases, whereas ideally it would happen half of the time. Dr. Flint noted that communication tools differ among hospitals, limiting the applicability of the findings.
The research team surveyed 39 hospitalists and 28 PCPs employed by the medical center during the first half of 2021. They also interviewed six hospitalists as they admitted and discharged patients.
The hospitalist movement, which took hold in response to cost and efficiency demands of managed care, led to the start of inpatient specialists, thereby reducing the need for PCPs to commute between their offices and the hospital to care for patients in both settings.
Primary care involvement is important during hospitalization
In the Beth Israel Deaconess survey, four out of five hospitalists and three-quarters of PCPs agreed that primary care involvement is still important during hospitalization, most critically during discharge and admission. Hospitalists reported that PCPs provide valuable data about a patient’s medical status, social supports, mental health, and goals for care. They also said having such data helps to boost patient trust and improve the quality of inpatient care.
“Most projects around communication between inpatient and outpatient doctors have really focused on the time of discharge,” when clinicians identify what care a patient will need after they leave the hospital, Dr. Flint said. “But we found that both sides felt increased communication at time of admission would also be beneficial.”
The biggest barrier for PCPs, cited by 82% of respondents, was lack of time. Hospitalists’ top impediment was being unable to find contact information for the other party, which was cited by 79% of these survey participants.
Hospitalists operate ‘in a very stressful environment’
The Beth Israel Deaconess research “documents what has largely been suspected,” said primary care general internist Allan Goroll, MD.
Dr. Goroll, a professor of medicine at Harvard Medical School, Boston, said in an interview that hospitalists operate “in a very stressful environment.”
“They [hospitalists] appreciate accurate information about a patient’s recent medical history, test results, and responses to treatment as well as a briefing on patient values and preferences, family dynamics, and priorities for the admission. It makes for a safer, more personalized, and more efficient hospital admission,” said Dr. Goroll, who was not involved in the research.
In a 2015 article in the New England Journal of Medicine, Dr. Goroll and Daniel Hunt, MD, director of hospital medicine at Emory University, Atlanta, proposed a collaborative model in which PCPs visit hospitalized patients and serve as consultants to inpatient staff. Dr. Goroll said Massachusetts General Hospital in Boston, where he practices, initiated a study of that approach, but it was interrupted by the pandemic.
“As limited time is the most often cited barrier to communication, future interventions such as asynchronous forms of communication between the two groups should be considered,” the researchers wrote in the NEJM perspective.
To narrow the gap, Beth Israel Deaconess will study converting an admission notification letter sent to PCPs into a two-way communication tool in which PCPs can insert patient information, Dr. Flint said.
Dr. Flint and Dr. Goroll have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hospitalists and PCPs want more dialogue while patients are in the hospital in order to coordinate and personalize care, according to data collected at Beth Israel Deaconess Medical Center, Boston. The results were presented at the annual meeting of the Society of General Internal Medicine.
“I think a major takeaway is that both hospitalists and primary care doctors agree that it’s important for primary care doctors to be involved in a patient’s hospitalization. They both identified a value that PCPs can bring to the table,” coresearcher Kristen Flint, MD, a primary care resident, told this news organization.
A majority in both camps reported that communication with the other party occurred in less than 25% of cases, whereas ideally it would happen half of the time. Dr. Flint noted that communication tools differ among hospitals, limiting the applicability of the findings.
The research team surveyed 39 hospitalists and 28 PCPs employed by the medical center during the first half of 2021. They also interviewed six hospitalists as they admitted and discharged patients.
The hospitalist movement, which took hold in response to cost and efficiency demands of managed care, led to the start of inpatient specialists, thereby reducing the need for PCPs to commute between their offices and the hospital to care for patients in both settings.
Primary care involvement is important during hospitalization
In the Beth Israel Deaconess survey, four out of five hospitalists and three-quarters of PCPs agreed that primary care involvement is still important during hospitalization, most critically during discharge and admission. Hospitalists reported that PCPs provide valuable data about a patient’s medical status, social supports, mental health, and goals for care. They also said having such data helps to boost patient trust and improve the quality of inpatient care.
“Most projects around communication between inpatient and outpatient doctors have really focused on the time of discharge,” when clinicians identify what care a patient will need after they leave the hospital, Dr. Flint said. “But we found that both sides felt increased communication at time of admission would also be beneficial.”
The biggest barrier for PCPs, cited by 82% of respondents, was lack of time. Hospitalists’ top impediment was being unable to find contact information for the other party, which was cited by 79% of these survey participants.
Hospitalists operate ‘in a very stressful environment’
The Beth Israel Deaconess research “documents what has largely been suspected,” said primary care general internist Allan Goroll, MD.
Dr. Goroll, a professor of medicine at Harvard Medical School, Boston, said in an interview that hospitalists operate “in a very stressful environment.”
“They [hospitalists] appreciate accurate information about a patient’s recent medical history, test results, and responses to treatment as well as a briefing on patient values and preferences, family dynamics, and priorities for the admission. It makes for a safer, more personalized, and more efficient hospital admission,” said Dr. Goroll, who was not involved in the research.
In a 2015 article in the New England Journal of Medicine, Dr. Goroll and Daniel Hunt, MD, director of hospital medicine at Emory University, Atlanta, proposed a collaborative model in which PCPs visit hospitalized patients and serve as consultants to inpatient staff. Dr. Goroll said Massachusetts General Hospital in Boston, where he practices, initiated a study of that approach, but it was interrupted by the pandemic.
“As limited time is the most often cited barrier to communication, future interventions such as asynchronous forms of communication between the two groups should be considered,” the researchers wrote in the NEJM perspective.
To narrow the gap, Beth Israel Deaconess will study converting an admission notification letter sent to PCPs into a two-way communication tool in which PCPs can insert patient information, Dr. Flint said.
Dr. Flint and Dr. Goroll have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hospitalists and PCPs want more dialogue while patients are in the hospital in order to coordinate and personalize care, according to data collected at Beth Israel Deaconess Medical Center, Boston. The results were presented at the annual meeting of the Society of General Internal Medicine.
“I think a major takeaway is that both hospitalists and primary care doctors agree that it’s important for primary care doctors to be involved in a patient’s hospitalization. They both identified a value that PCPs can bring to the table,” coresearcher Kristen Flint, MD, a primary care resident, told this news organization.
A majority in both camps reported that communication with the other party occurred in less than 25% of cases, whereas ideally it would happen half of the time. Dr. Flint noted that communication tools differ among hospitals, limiting the applicability of the findings.
The research team surveyed 39 hospitalists and 28 PCPs employed by the medical center during the first half of 2021. They also interviewed six hospitalists as they admitted and discharged patients.
The hospitalist movement, which took hold in response to cost and efficiency demands of managed care, led to the start of inpatient specialists, thereby reducing the need for PCPs to commute between their offices and the hospital to care for patients in both settings.
Primary care involvement is important during hospitalization
In the Beth Israel Deaconess survey, four out of five hospitalists and three-quarters of PCPs agreed that primary care involvement is still important during hospitalization, most critically during discharge and admission. Hospitalists reported that PCPs provide valuable data about a patient’s medical status, social supports, mental health, and goals for care. They also said having such data helps to boost patient trust and improve the quality of inpatient care.
“Most projects around communication between inpatient and outpatient doctors have really focused on the time of discharge,” when clinicians identify what care a patient will need after they leave the hospital, Dr. Flint said. “But we found that both sides felt increased communication at time of admission would also be beneficial.”
The biggest barrier for PCPs, cited by 82% of respondents, was lack of time. Hospitalists’ top impediment was being unable to find contact information for the other party, which was cited by 79% of these survey participants.
Hospitalists operate ‘in a very stressful environment’
The Beth Israel Deaconess research “documents what has largely been suspected,” said primary care general internist Allan Goroll, MD.
Dr. Goroll, a professor of medicine at Harvard Medical School, Boston, said in an interview that hospitalists operate “in a very stressful environment.”
“They [hospitalists] appreciate accurate information about a patient’s recent medical history, test results, and responses to treatment as well as a briefing on patient values and preferences, family dynamics, and priorities for the admission. It makes for a safer, more personalized, and more efficient hospital admission,” said Dr. Goroll, who was not involved in the research.
In a 2015 article in the New England Journal of Medicine, Dr. Goroll and Daniel Hunt, MD, director of hospital medicine at Emory University, Atlanta, proposed a collaborative model in which PCPs visit hospitalized patients and serve as consultants to inpatient staff. Dr. Goroll said Massachusetts General Hospital in Boston, where he practices, initiated a study of that approach, but it was interrupted by the pandemic.
“As limited time is the most often cited barrier to communication, future interventions such as asynchronous forms of communication between the two groups should be considered,” the researchers wrote in the NEJM perspective.
To narrow the gap, Beth Israel Deaconess will study converting an admission notification letter sent to PCPs into a two-way communication tool in which PCPs can insert patient information, Dr. Flint said.
Dr. Flint and Dr. Goroll have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SGIM 2022