User login
A woman with scaling, and painful, crusted, erythematous papules and pustules on her face
Biopsy for this patient revealed folliculitis with Demodex mites visualized on histology. Direct immunofluorescence was negative. A KOH preparation was performed and was positive for large numbers of Demodex. Bacterial cultures were negative. The patient was started on a course of submicrobial doxycycline and ivermectin and showed marked improvement 1 month following treatment.
Demodex folliculorum and Demodex brevis (collectively referred to as Demodex) are microscopic parasitic mites that commonly live on human skin.1 Typically, the mite remains asymptomatic. However, in higher numbers, the infestation may cause dermatoses, called demodicosis. Lesions often present as itchy papules, pustules, and erythematous scaling on the face, ears, and scalp. Blepharitis may be present. Demodex folliculitis is more common in immunocompromised patients.2
Demodex may have a causative role in rosacea and present similarly, with a key difference being that Demodex-type rosacea is more scaly/dry and pustular than common rosacea.1 In Demodex folliculitis, bacterial cultures are often negative. A skin scraping for KOH will reveal increased mite colonization. The Demodex mite may also be seen in histologic slides.
Treatment of Demodex folliculitis includes crotamiton cream, permethrin cream, oral tetracyclines, topical or systemic metronidazole, and topical or oral ivermectin.
This case and photos were submitted by Susannah McClain, MD, Three Rivers Dermatology, Pittsburgh.
References
1. Rather PA and Hassan I. Indian J Dermatol. 2014 Jan;59(1):60-6.
2. Bachmeyer C and Moreno-Sabater A. CMAJ. 2017 Jun 26;189(25):E865.
Biopsy for this patient revealed folliculitis with Demodex mites visualized on histology. Direct immunofluorescence was negative. A KOH preparation was performed and was positive for large numbers of Demodex. Bacterial cultures were negative. The patient was started on a course of submicrobial doxycycline and ivermectin and showed marked improvement 1 month following treatment.
Demodex folliculorum and Demodex brevis (collectively referred to as Demodex) are microscopic parasitic mites that commonly live on human skin.1 Typically, the mite remains asymptomatic. However, in higher numbers, the infestation may cause dermatoses, called demodicosis. Lesions often present as itchy papules, pustules, and erythematous scaling on the face, ears, and scalp. Blepharitis may be present. Demodex folliculitis is more common in immunocompromised patients.2
Demodex may have a causative role in rosacea and present similarly, with a key difference being that Demodex-type rosacea is more scaly/dry and pustular than common rosacea.1 In Demodex folliculitis, bacterial cultures are often negative. A skin scraping for KOH will reveal increased mite colonization. The Demodex mite may also be seen in histologic slides.
Treatment of Demodex folliculitis includes crotamiton cream, permethrin cream, oral tetracyclines, topical or systemic metronidazole, and topical or oral ivermectin.
This case and photos were submitted by Susannah McClain, MD, Three Rivers Dermatology, Pittsburgh.
References
1. Rather PA and Hassan I. Indian J Dermatol. 2014 Jan;59(1):60-6.
2. Bachmeyer C and Moreno-Sabater A. CMAJ. 2017 Jun 26;189(25):E865.
Biopsy for this patient revealed folliculitis with Demodex mites visualized on histology. Direct immunofluorescence was negative. A KOH preparation was performed and was positive for large numbers of Demodex. Bacterial cultures were negative. The patient was started on a course of submicrobial doxycycline and ivermectin and showed marked improvement 1 month following treatment.
Demodex folliculorum and Demodex brevis (collectively referred to as Demodex) are microscopic parasitic mites that commonly live on human skin.1 Typically, the mite remains asymptomatic. However, in higher numbers, the infestation may cause dermatoses, called demodicosis. Lesions often present as itchy papules, pustules, and erythematous scaling on the face, ears, and scalp. Blepharitis may be present. Demodex folliculitis is more common in immunocompromised patients.2
Demodex may have a causative role in rosacea and present similarly, with a key difference being that Demodex-type rosacea is more scaly/dry and pustular than common rosacea.1 In Demodex folliculitis, bacterial cultures are often negative. A skin scraping for KOH will reveal increased mite colonization. The Demodex mite may also be seen in histologic slides.
Treatment of Demodex folliculitis includes crotamiton cream, permethrin cream, oral tetracyclines, topical or systemic metronidazole, and topical or oral ivermectin.
This case and photos were submitted by Susannah McClain, MD, Three Rivers Dermatology, Pittsburgh.
References
1. Rather PA and Hassan I. Indian J Dermatol. 2014 Jan;59(1):60-6.
2. Bachmeyer C and Moreno-Sabater A. CMAJ. 2017 Jun 26;189(25):E865.
Lesions in pelvis may be ‘tip of the iceberg’ in endometriosis
Recognizing the systemic effects of endometriosis may help doctors better understand the experiences of patients with the disease and guide the approach to diagnosis and treatment, according to the president of the American Society for Reproductive Medicine (ASRM).
, Hugh S. Taylor, MD, said at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
Its systemic manifestations may explain why women with endometriosis tend to have a lower body mass index, compared with women without the disease, Dr. Taylor said.
“Stem cells, microRNAs, and generalized inflammation are some of the mechanisms that mediate these long-range effects on distant organ systems,” he said.
Studies have indicated that lesions in the pelvis do not fully explain the disease, and investigators continue to elucidate how “endometriosis that we see in the pelvis is really just the tip of the iceberg,” said Dr. Taylor, chair of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn.
Pain, including dysmenorrhea, pelvic pain, and dyspareunia, “can be just as bad with ... stage 1 disease as it can be with stage 4 disease,” he said.
Some patients may not have pain, but have infertility. Other women are asymptomatic, and doctors find endometriosis incidentally.
One common definition of endometriosis – ectopic endometrial glands and stroma predominantly caused by retrograde menstruation – “probably overly simplifies this complex disease,” said Dr. Taylor, who reviewed the current understanding of endometriosis in an article in The Lancet. “The lesions in the pelvis are important. We see them. We treat them. But endometriosis has ... effects throughout the body.”
Dr. Taylor’s research group has shown that stem cells are a potential source of endometriosis. “There are cells from the endometriosis that can be found traveling in the circulation,” but their effects are unclear, he said.
Levels of several microRNAs may be increased or decreased in women with endometriosis, and these altered levels may induce the production of inflammatory cytokines. They also may serve as the basis of a blood test for endometriosis that could be ready for clinical use soon, Dr. Taylor said.
In a mouse model of endometriosis, the disease changes the electrophysiology of the brain and behavior. “We see changes in anxiety induced by endometriosis. We see changes in pain sensitivity induced by endometriosis. And we also see an increase in depression induced by endometriosis in this animal model,” Dr. Taylor said.
Although surgical therapy treats local disease, medical therapy may be needed to treat the systemic manifestations.
During a question-and-answer period after the presentation, Marcelle I. Cedars, MD, asked whether analgesic and hormonal management may be sufficient when a woman has suspected or laparoscopically diagnosed endometriosis and pain is the primary complaint.
“Given the understanding of endometriosis, how would you suggest approaching treatment?” asked Dr. Cedars, president elect of the ASRM and director of the division of reproductive endocrinology and infertility at the University of California, San Francisco.
Analgesic and hormonal therapies remain “the best treatments we have,” Dr. Taylor said. He starts treatment with an oral contraceptive and a nonsteroidal anti-inflammatory medication – “not only for pain relief but to tamp some of the inflammation associated with endometriosis,” he said. If an oral contraceptive does not work, a gonadotropin-releasing hormone antagonist typically is the next step.
Dr. Taylor has disclosed ties to Dot Lab and AbbVie. Dr. Cedars had no disclosures.
Recognizing the systemic effects of endometriosis may help doctors better understand the experiences of patients with the disease and guide the approach to diagnosis and treatment, according to the president of the American Society for Reproductive Medicine (ASRM).
, Hugh S. Taylor, MD, said at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
Its systemic manifestations may explain why women with endometriosis tend to have a lower body mass index, compared with women without the disease, Dr. Taylor said.
“Stem cells, microRNAs, and generalized inflammation are some of the mechanisms that mediate these long-range effects on distant organ systems,” he said.
Studies have indicated that lesions in the pelvis do not fully explain the disease, and investigators continue to elucidate how “endometriosis that we see in the pelvis is really just the tip of the iceberg,” said Dr. Taylor, chair of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn.
Pain, including dysmenorrhea, pelvic pain, and dyspareunia, “can be just as bad with ... stage 1 disease as it can be with stage 4 disease,” he said.
Some patients may not have pain, but have infertility. Other women are asymptomatic, and doctors find endometriosis incidentally.
One common definition of endometriosis – ectopic endometrial glands and stroma predominantly caused by retrograde menstruation – “probably overly simplifies this complex disease,” said Dr. Taylor, who reviewed the current understanding of endometriosis in an article in The Lancet. “The lesions in the pelvis are important. We see them. We treat them. But endometriosis has ... effects throughout the body.”
Dr. Taylor’s research group has shown that stem cells are a potential source of endometriosis. “There are cells from the endometriosis that can be found traveling in the circulation,” but their effects are unclear, he said.
Levels of several microRNAs may be increased or decreased in women with endometriosis, and these altered levels may induce the production of inflammatory cytokines. They also may serve as the basis of a blood test for endometriosis that could be ready for clinical use soon, Dr. Taylor said.
In a mouse model of endometriosis, the disease changes the electrophysiology of the brain and behavior. “We see changes in anxiety induced by endometriosis. We see changes in pain sensitivity induced by endometriosis. And we also see an increase in depression induced by endometriosis in this animal model,” Dr. Taylor said.
Although surgical therapy treats local disease, medical therapy may be needed to treat the systemic manifestations.
During a question-and-answer period after the presentation, Marcelle I. Cedars, MD, asked whether analgesic and hormonal management may be sufficient when a woman has suspected or laparoscopically diagnosed endometriosis and pain is the primary complaint.
“Given the understanding of endometriosis, how would you suggest approaching treatment?” asked Dr. Cedars, president elect of the ASRM and director of the division of reproductive endocrinology and infertility at the University of California, San Francisco.
Analgesic and hormonal therapies remain “the best treatments we have,” Dr. Taylor said. He starts treatment with an oral contraceptive and a nonsteroidal anti-inflammatory medication – “not only for pain relief but to tamp some of the inflammation associated with endometriosis,” he said. If an oral contraceptive does not work, a gonadotropin-releasing hormone antagonist typically is the next step.
Dr. Taylor has disclosed ties to Dot Lab and AbbVie. Dr. Cedars had no disclosures.
Recognizing the systemic effects of endometriosis may help doctors better understand the experiences of patients with the disease and guide the approach to diagnosis and treatment, according to the president of the American Society for Reproductive Medicine (ASRM).
, Hugh S. Taylor, MD, said at the 2021 virtual meeting of the American College of Obstetricians and Gynecologists.
Its systemic manifestations may explain why women with endometriosis tend to have a lower body mass index, compared with women without the disease, Dr. Taylor said.
“Stem cells, microRNAs, and generalized inflammation are some of the mechanisms that mediate these long-range effects on distant organ systems,” he said.
Studies have indicated that lesions in the pelvis do not fully explain the disease, and investigators continue to elucidate how “endometriosis that we see in the pelvis is really just the tip of the iceberg,” said Dr. Taylor, chair of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn.
Pain, including dysmenorrhea, pelvic pain, and dyspareunia, “can be just as bad with ... stage 1 disease as it can be with stage 4 disease,” he said.
Some patients may not have pain, but have infertility. Other women are asymptomatic, and doctors find endometriosis incidentally.
One common definition of endometriosis – ectopic endometrial glands and stroma predominantly caused by retrograde menstruation – “probably overly simplifies this complex disease,” said Dr. Taylor, who reviewed the current understanding of endometriosis in an article in The Lancet. “The lesions in the pelvis are important. We see them. We treat them. But endometriosis has ... effects throughout the body.”
Dr. Taylor’s research group has shown that stem cells are a potential source of endometriosis. “There are cells from the endometriosis that can be found traveling in the circulation,” but their effects are unclear, he said.
Levels of several microRNAs may be increased or decreased in women with endometriosis, and these altered levels may induce the production of inflammatory cytokines. They also may serve as the basis of a blood test for endometriosis that could be ready for clinical use soon, Dr. Taylor said.
In a mouse model of endometriosis, the disease changes the electrophysiology of the brain and behavior. “We see changes in anxiety induced by endometriosis. We see changes in pain sensitivity induced by endometriosis. And we also see an increase in depression induced by endometriosis in this animal model,” Dr. Taylor said.
Although surgical therapy treats local disease, medical therapy may be needed to treat the systemic manifestations.
During a question-and-answer period after the presentation, Marcelle I. Cedars, MD, asked whether analgesic and hormonal management may be sufficient when a woman has suspected or laparoscopically diagnosed endometriosis and pain is the primary complaint.
“Given the understanding of endometriosis, how would you suggest approaching treatment?” asked Dr. Cedars, president elect of the ASRM and director of the division of reproductive endocrinology and infertility at the University of California, San Francisco.
Analgesic and hormonal therapies remain “the best treatments we have,” Dr. Taylor said. He starts treatment with an oral contraceptive and a nonsteroidal anti-inflammatory medication – “not only for pain relief but to tamp some of the inflammation associated with endometriosis,” he said. If an oral contraceptive does not work, a gonadotropin-releasing hormone antagonist typically is the next step.
Dr. Taylor has disclosed ties to Dot Lab and AbbVie. Dr. Cedars had no disclosures.
FROM ACOG 2021
Procalcitonin-guided antibiotic stewardship for lower respiratory tract infection
Dynamics of the assay must be considered
Case
A 50-year-old female presents with 3 days of cough, subjective fevers, myalgias, and dyspnea. She feels she “may have caught something” while volunteering at a preschool. She has hypertension, congestive heart failure, and 20 pack-years of smoking. Chest x-ray shows bibasilar consolidation versus atelectasis. Vital signs are notable for an O2 saturation of 93%. White blood cell count and differential are normal. Procalcitonin level is 0.4 mcg/L.
Overview of the issue
Lower respiratory tract infections (LRTI) are common in the practice of hospital medicine; however, the primary symptoms of cough and dyspnea can be caused by a myriad of noninfectious conditions. Even when infection is suggested by the clinical presentation, the distinction between bacterial and viral etiologies can be challenging, complicating decisions about antibiotic use. Attention to antibiotic stewardship is a growing concern in U.S. hospitals, where the CDC estimates that as many as 50% of antibiotic orders are inappropriate or entirely unnecessary.1 Antibiotic overuse is a driver of multidrug-resistant organisms and increasing rates of Clostridium difficile infection. A diagnostic test to enhance physicians’ ability to target patients who would benefit from antibiotics could be a useful tool to combat the complications of antibiotic overuse. (See Figure 1.) 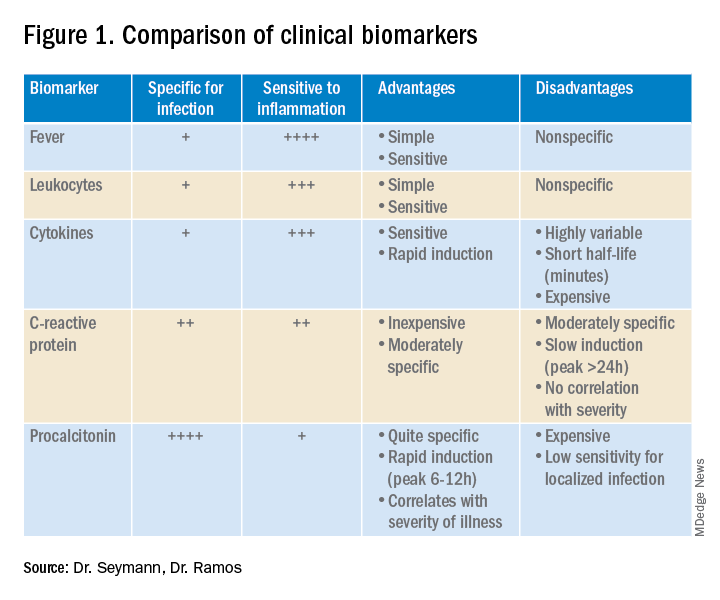
Procalcitonin is produced in the thyroidal C-cells as a prohormone which is processed intracellularly and secreted as calcitonin in response to serum calcium levels. However, intact procalcitonin protein can be secreted from many other tissues in the presence of cytokines such as interleukin 1-beta, tumor necrosis factor-alpha, and lipopolysaccharide, typically released in response to systemic bacterial infections. Conversely, cytokines present in acute viral illness (interferon-gamma) suppress procalcitonin release. This dichotomy presents an opportunity to use procalcitonin to differentiate bacterial from nonbacterial etiologies in various clinical scenarios including LRTI.
Overview of the data
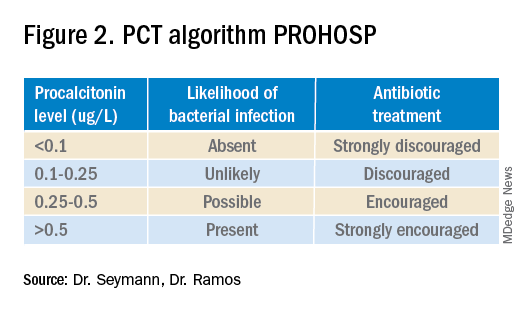
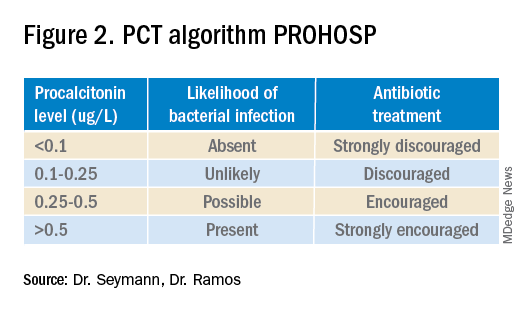
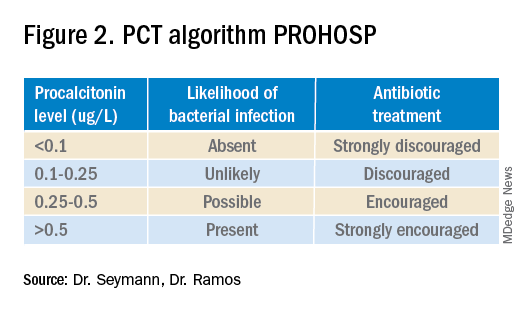
Multiple studies have demonstrated that procalcitonin can be safely used to guide antibiotic prescribing in patients with LRTI. The first large multicenter randomized controlled trial to address the topic was the Swiss PROHOSP study.2 Investigators randomized 1,359 patients hospitalized with LRTI to procalcitonin (PCT) guided therapy or guideline-based therapy. After an initial PCT level was measured, antibiotic prescribing in the PCT arm of the study was directed by a prespecified protocol; specifically, clinicians were discouraged from prescribing antibiotics in patients with PCT levels less than 0.25 mcg/L. (See Figure 2.)
For patients who were particularly ill or unstable at admission, the protocol allowed for antibiotics despite a low PCT level, but repeat measurement within 24 hours and accompanying treatment recommendations were reinforced with the treatment team. Clinicians caring for patients in the control arm were presented with condition-specific clinical practice guidelines to reinforce antibiotic choices. In both arms, the final decision on antibiotic treatment remained with the physician.
Results from the PROHOSP study showed no difference in the combined outcome of death, intensive care unit admission, or complications in the ensuing 30 days, but antibiotic use was significantly reduced. Mean antibiotic exposure dropped from 8.7 to 5.7 days, a reduction of 35%, with the largest decrease among patients with chronic obstructive pulmonary disease (COPD) and acute bronchitis. Antibiotic-related adverse effects fell by 8.2%. Strengths of the study included a very high rate of protocol compliance (90%) by the treating clinicians.
A systematic review of all available studies of procalcitonin-guided therapy for LRTI was published in 2018 and included 26 randomized controlled trials encompassing 6,708 patients in 12 countries. Findings confirmed an overall reduction of 2.4 days in antibiotic exposure, 6% reduction in antibiotic-related adverse effects, and importantly a 17% relative risk reduction in mortality.3
Similar benefits of PCT-guided therapy have been demonstrated even among severely ill patients. A meta-analysis including 523 patients with bacteremia noted mean reduction in antibiotic exposure of 2.86 days, without excess mortality.4 A second meta-analysis of 4,482 critically ill patients admitted to the ICU with sepsis demonstrated not only a reduction in antibiotic exposure, but in mortality as well. Despite a relatively small decrease in antibiotic duration of 1.19 days, the investigators found an 11% reduction in mortality (P = .03) in the PCT-guided group.5
One notable outlier among the many positive studies on PCT-guided antibiotic therapy is the 2018 PROACT study performed in U.S. hospitals over 4 years.6 Its design was similar to the PROHOSP study, however, in contrast to the majority of other trials, the investigators were unable to demonstrate a reduction in antibiotic exposure, leading them to conclude that PCT guidance may not be a useful tool for antibiotic stewardship.
Unfortunately, significant differences in the compliance with the study protocol (90% in PROHOSP vs. 63% in PROACT), and a much healthier patient population (91% of the patients had a PCT less than 0.25, and a majority of patients had asthma which is not normally treated with antibiotics) hamper the generalizability of the PROACT findings. Rather than indicating a failure of PCT, the findings of the study underscore the fact that the utility of any lab test is limited unless it is applied in an appropriate diagnostic setting.
For hospitalists, the most clinically useful role for PCT testing is to guide the duration of antibiotic therapy. Although the literature supports short-course antibiotic therapy in many common conditions seen by hospitalists (Table 1), data suggest overprescribing remains prevalent. Several recent studies targeting LRTI underscore this point.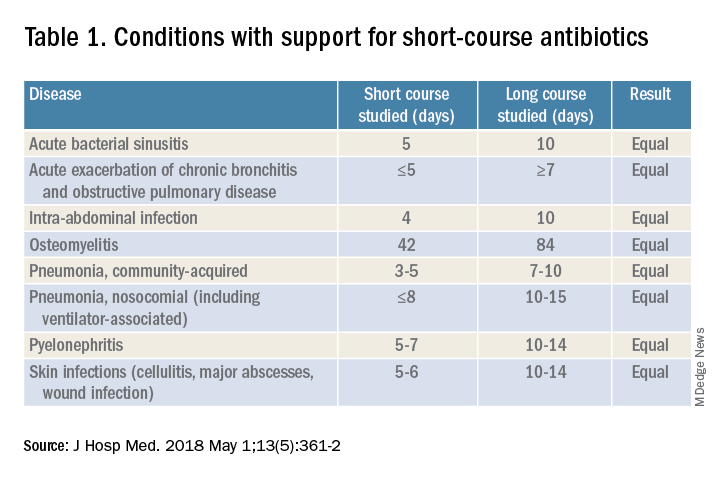
Despite guidelines advocating for treatment of uncomplicated community-acquired pneumonia (CAP) for no more than 5-7 days, two recent retrospective studies suggest most patients receive longer courses. A review of more than 150,000 patients across the United States with uncomplicated CAP documented a mean antibiotic duration of 9.5 days, with close to 70% of patients receiving more than 7 days of therapy.7 A multicenter study of CAP patients hospitalized in Michigan noted similar findings, with a mean 2-day excess duration of therapy or 2,526 excess days of treatment per 1,000 discharges.8 Though some who argue against procalcitonin’s utility cite the fact that existing guidelines already support short-course therapy, obviating the need for biomarker guidance, clinicians have not yet universally adopted this practice. Using a PCT algorithm can decrease duration of therapy and thereby reduce unnecessary antibiotic use. PCT levels less than 0.25 mcg/L support withholding or discontinuing antibiotics, or consideration of an alternative diagnosis.
The dynamics of the PCT assay must be considered in order to use it appropriately. Levels of PCT rise within 3-6 hours of infection, so patients presenting extremely early in the disease course may have falsely low levels. PCT levels correlate with severity of illness and should fall within 2-3 days of initiation of appropriate therapy. A repeat PCT in 2-3 days can be used to help time antibiotic cessation. Studies support stopping antibiotics in stable patients once the PCT level falls below 0.25 mcg/L or drops by 80% in patients with severe elevations. Lack of improvement suggests inadequate antibiotic therapy and is predictive of excess mortality.
Most drivers of false-positive PCT levels are rare and easily identifiable. (See Figure 3.) However, like troponin, patients with chronic kidney disease have delayed PCT clearance, so baseline levels may be about double the normal range. If a baseline is known, monitoring the rise and fall of PCT levels remains clinically useful in this population.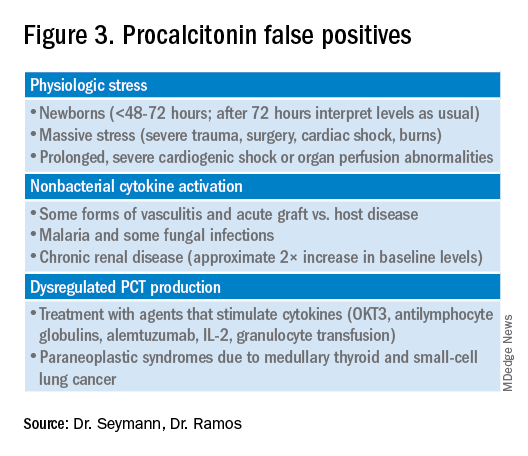
Application of data to case
In reviewing the case, the differential includes a viral upper respiratory infection, an acute exacerbation of COPD, decompensated heart failure, or bacterial pneumonia. The lab and imaging findings are nonspecific, but a PCT level less than 0.25 mcg/L raises concern for an acute bacterial pneumonia. Given that PCT levels rise in bacterial infection and are suppressed in viral infections, treating this patient with antibiotics seems prudent. In this case the relatively mild elevation suggests a less severe infection or a presentation early in the disease course. A repeat PCT in 2-3 days will guide timing for antibiotic cessation.
Bottom line
Thoughtful procalcitonin-guided antibiotic therapy for LRTI may further current antibiotic stewardship initiatives targeting reduction of inappropriate antimicrobial use, which may ultimately reduce rates of Clostridium difficile infections and the emergence of multidrug-resistant organisms.
Dr. Seymann and Dr. Ramos are clinical professors in the division of hospital medicine, department of medicine, at the University of California San Diego.
Key points
- Initial PCT level can help distinguish between viral and bacterial pneumonias.
- PCT levels rise in response to acute bacterial infections and are suppressed in viral infections.
- PCT levels below 0.25 mcg/L suggest that antibiotics can be safely withheld in otherwise stable patients.
- PCT levels correlate with severity of illness and prognosis.
- Rise of PCT is rapid (3-6 hours), and levels fall quickly with appropriate treatment (2-3 days).
- Serial PCT levels can be used to guide duration of antibiotic therapy.
References
1. CDC. Core elements of hospital antibiotic stewardship programs. Atlanta: U.S. Department of Health & Human Services. 2014. Available at www.cdc.gov/getsmart/healthcare/ implementation/core-elements.html.
2. Schuetz P et al. Effect of procalcitonin-based guidelines vs. standard guidelines on antibiotic use in lower respiratory tract infections: The ProHOSP randomized controlled trial. JAMA. 2009;302(10):1059-66. doi: 10.1001/jama.2009.1297.
3. Schuetz P et al. Effect of procalcitonin-guided antibiotic treatment on mortality in acute respiratory infections: A patient level meta-analysis. Lancet Infect Dis. 2018;18(1):95-107. doi: 10.1016/S1473-3099(17)30592-3.
4. Meier MA et al. Procalcitonin-guided antibiotic treatment in patients with positive blood cultures: A patient-level meta-analysis of randomized trials. Clin Infect Dis. 2019;69(3):388-96. doi: 10.1093/cid/ciy917.
5. Wirz Y et al. Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: A patient-level meta-analysis of randomized trials. Crit Care. 2018;22(1):191. doi: 10.1186/s13054-018-2125-7.
6. Huang DT et al. Procalcitonin-guided use of antibiotics for lower respiratory tract infection. N Engl J Med. 2018 Jul 19;379(3):236-49. doi: 10.1056/NEJMoa1802670.
7. Yi SH et al. Duration of antibiotic use among adults with uncomplicated community-acquired pneumonia requiring hospitalization in the United States. Clin Infect Dis. 2018;66(9):1333-41. doi: 10.1093/cid/cix986.
8. Vaughn V et al. Excess antibiotic treatment duration and adverse events in patients hospitalized with pneumonia: A multihospital cohort study. Ann Intern Med. 2019; 171(3):153-63. doi: 10.7326/M18-3640.
Quiz
1. A 57-year-old male is hospitalized for treatment of community-acquired pneumonia with IV azithromycin and ceftriaxone. PCT level on day 1 = 0.35 mcg/L. On day 4 of antibiotics the PCT level is 0.15 mcg/L. What should be done regarding the antibiotic course?
a. Continue antibiotics for a total course of 5 days.
b. Continue antibiotics for a total course of 7 days.
c. Stop antibiotics.
d. Continue antibiotics and repeat a PCT level the next day.
Answer: The best answer is c. Evidence suggests that 5 days of therapy is adequate treatment for uncomplicated community-acquired pneumonia. Procalcitonin-guided therapy allows for further tailoring of the regimen to the individual patient. Since this patient has clinically improved, and the PCT level is less than 0.25 mcg/L, it is reasonable to discontinue treatment and avoid unnecessary antibiotic days.
2. A 42-year-old female with known CKD stage 4 is hospitalized with suspected community-acquired pneumonia. Procalcitonin level is elevated at 0.6 mcg/L. How should the patient be treated?
a. Ignore the PCT as levels are falsely elevated due to CKD.
b. Treat with antibiotics for suspected community-acquired pneumonia.
c. Repeat PCT level in the morning.
d. Check a C-reactive protein level instead.
Answer: The best answer is b. Although decreased renal function can delay clearance of PCT, levels in CKD are typically about twice normal. In this case, when pneumonia is clinically suspected, the level of 0.6 mcg/L would correspond to a level of approximately 0.3 mcg/L and support a decision to treat with antibiotics.
3. A 36-year-old male develops sudden onset of dyspnea, cough, fever, and chills and proceeds rapidly to the emergency department. He is hypoxic, febrile, and has a leukocytosis. The PCT level is checked and found to be 0.2 mcg/L. Chest imaging shows a right middle lobe consolidation. How should the patient be treated?
a. Hold antibiotics.
b. Start antibiotic therapy.
c. Hold antibiotics and repeat PCT level in the morning.
Answer: The best answer is b. The clinical scenario suggests bacterial pneumonia. Given the sudden onset and early presentation to the ED, it is likely that the PCT level has not had time to peak. PCT levels typically begin to rise in 3-6 hours from the time of infection. Withholding antibiotics until the level exceeds 0.25 mcg/L would not be recommended when clinical judgment suggests otherwise.
4. Which of the following noninfectious scenarios does NOT cause an elevated PCT level?
a. Bone marrow transplant patient with acute graft versus host disease of the skin.
b. Patient presenting with paraneoplastic syndrome from small cell lung cancer.
c. Patient with cirrhosis presenting with hepatic encephalopathy.
d. Patient presenting with severe trauma from a motor vehicle accident.
Answer: The answer is c. Cirrhosis and/or hepatic encephalopathy does not cause a falsely elevated PCT level. Acute graft versus host disease, paraneoplastic syndrome from small cell lung cancer or medullary thyroid cancer, and massive stress such as severe trauma can cause elevations in PCT.
Additional reading
Spellberg B. The maturing antibiotic mantra: Shorter is still better. J Hosp Med. 2018;13:361-2. doi: 10.12788/jhm.2904.
Soni NJ et al. Procalcitonin-guided antibiotic therapy: A systematic review and meta-analysis. J Hosp Med. 2013;8:530-540. doi: 10.1002/jhm.2067.
Rhee C. Using procalcitonin to guide antibiotic therapy. Open Forum Infect Dis. 2017;4(1):ofw249. doi: 10.1093/ofid/ofw249.
Sager R et al. Procalcitonin-guided diagnosis and antibiotic stewardship revisited. BMC Med. 2017;15. doi: 10.1186/s12916-017-0795-7.
Dynamics of the assay must be considered
Dynamics of the assay must be considered
Case
A 50-year-old female presents with 3 days of cough, subjective fevers, myalgias, and dyspnea. She feels she “may have caught something” while volunteering at a preschool. She has hypertension, congestive heart failure, and 20 pack-years of smoking. Chest x-ray shows bibasilar consolidation versus atelectasis. Vital signs are notable for an O2 saturation of 93%. White blood cell count and differential are normal. Procalcitonin level is 0.4 mcg/L.
Overview of the issue
Lower respiratory tract infections (LRTI) are common in the practice of hospital medicine; however, the primary symptoms of cough and dyspnea can be caused by a myriad of noninfectious conditions. Even when infection is suggested by the clinical presentation, the distinction between bacterial and viral etiologies can be challenging, complicating decisions about antibiotic use. Attention to antibiotic stewardship is a growing concern in U.S. hospitals, where the CDC estimates that as many as 50% of antibiotic orders are inappropriate or entirely unnecessary.1 Antibiotic overuse is a driver of multidrug-resistant organisms and increasing rates of Clostridium difficile infection. A diagnostic test to enhance physicians’ ability to target patients who would benefit from antibiotics could be a useful tool to combat the complications of antibiotic overuse. (See Figure 1.) 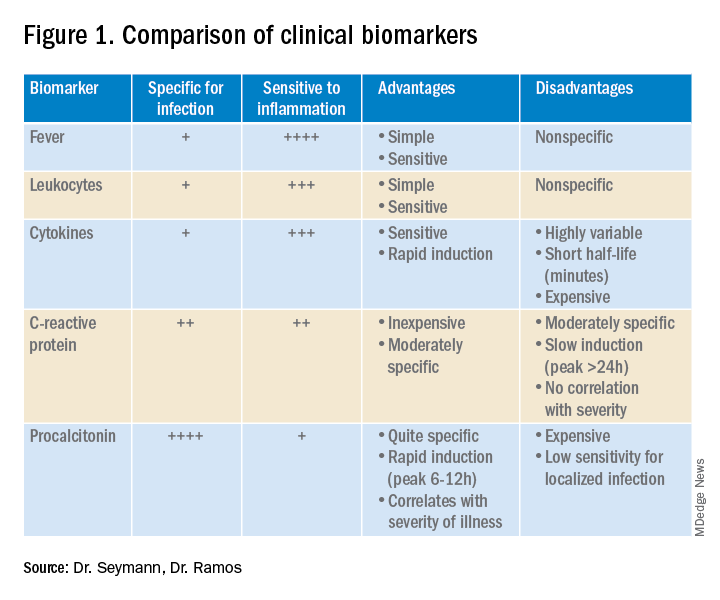
Procalcitonin is produced in the thyroidal C-cells as a prohormone which is processed intracellularly and secreted as calcitonin in response to serum calcium levels. However, intact procalcitonin protein can be secreted from many other tissues in the presence of cytokines such as interleukin 1-beta, tumor necrosis factor-alpha, and lipopolysaccharide, typically released in response to systemic bacterial infections. Conversely, cytokines present in acute viral illness (interferon-gamma) suppress procalcitonin release. This dichotomy presents an opportunity to use procalcitonin to differentiate bacterial from nonbacterial etiologies in various clinical scenarios including LRTI.
Overview of the data
Multiple studies have demonstrated that procalcitonin can be safely used to guide antibiotic prescribing in patients with LRTI. The first large multicenter randomized controlled trial to address the topic was the Swiss PROHOSP study.2 Investigators randomized 1,359 patients hospitalized with LRTI to procalcitonin (PCT) guided therapy or guideline-based therapy. After an initial PCT level was measured, antibiotic prescribing in the PCT arm of the study was directed by a prespecified protocol; specifically, clinicians were discouraged from prescribing antibiotics in patients with PCT levels less than 0.25 mcg/L. (See Figure 2.)
For patients who were particularly ill or unstable at admission, the protocol allowed for antibiotics despite a low PCT level, but repeat measurement within 24 hours and accompanying treatment recommendations were reinforced with the treatment team. Clinicians caring for patients in the control arm were presented with condition-specific clinical practice guidelines to reinforce antibiotic choices. In both arms, the final decision on antibiotic treatment remained with the physician.
Results from the PROHOSP study showed no difference in the combined outcome of death, intensive care unit admission, or complications in the ensuing 30 days, but antibiotic use was significantly reduced. Mean antibiotic exposure dropped from 8.7 to 5.7 days, a reduction of 35%, with the largest decrease among patients with chronic obstructive pulmonary disease (COPD) and acute bronchitis. Antibiotic-related adverse effects fell by 8.2%. Strengths of the study included a very high rate of protocol compliance (90%) by the treating clinicians.
A systematic review of all available studies of procalcitonin-guided therapy for LRTI was published in 2018 and included 26 randomized controlled trials encompassing 6,708 patients in 12 countries. Findings confirmed an overall reduction of 2.4 days in antibiotic exposure, 6% reduction in antibiotic-related adverse effects, and importantly a 17% relative risk reduction in mortality.3
Similar benefits of PCT-guided therapy have been demonstrated even among severely ill patients. A meta-analysis including 523 patients with bacteremia noted mean reduction in antibiotic exposure of 2.86 days, without excess mortality.4 A second meta-analysis of 4,482 critically ill patients admitted to the ICU with sepsis demonstrated not only a reduction in antibiotic exposure, but in mortality as well. Despite a relatively small decrease in antibiotic duration of 1.19 days, the investigators found an 11% reduction in mortality (P = .03) in the PCT-guided group.5
One notable outlier among the many positive studies on PCT-guided antibiotic therapy is the 2018 PROACT study performed in U.S. hospitals over 4 years.6 Its design was similar to the PROHOSP study, however, in contrast to the majority of other trials, the investigators were unable to demonstrate a reduction in antibiotic exposure, leading them to conclude that PCT guidance may not be a useful tool for antibiotic stewardship.
Unfortunately, significant differences in the compliance with the study protocol (90% in PROHOSP vs. 63% in PROACT), and a much healthier patient population (91% of the patients had a PCT less than 0.25, and a majority of patients had asthma which is not normally treated with antibiotics) hamper the generalizability of the PROACT findings. Rather than indicating a failure of PCT, the findings of the study underscore the fact that the utility of any lab test is limited unless it is applied in an appropriate diagnostic setting.
For hospitalists, the most clinically useful role for PCT testing is to guide the duration of antibiotic therapy. Although the literature supports short-course antibiotic therapy in many common conditions seen by hospitalists (Table 1), data suggest overprescribing remains prevalent. Several recent studies targeting LRTI underscore this point.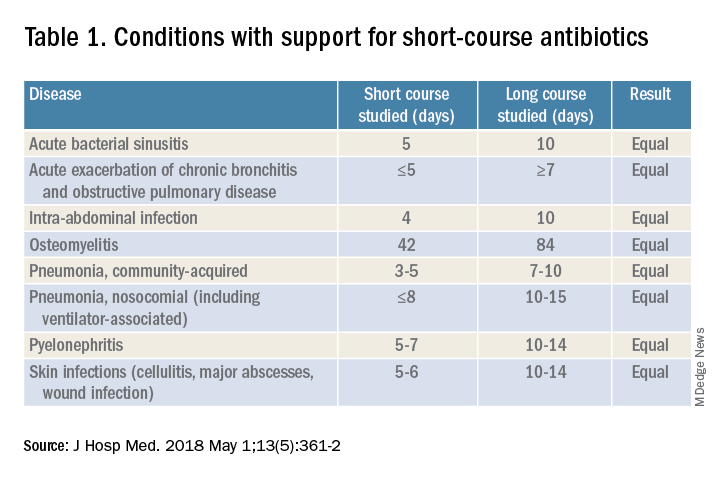
Despite guidelines advocating for treatment of uncomplicated community-acquired pneumonia (CAP) for no more than 5-7 days, two recent retrospective studies suggest most patients receive longer courses. A review of more than 150,000 patients across the United States with uncomplicated CAP documented a mean antibiotic duration of 9.5 days, with close to 70% of patients receiving more than 7 days of therapy.7 A multicenter study of CAP patients hospitalized in Michigan noted similar findings, with a mean 2-day excess duration of therapy or 2,526 excess days of treatment per 1,000 discharges.8 Though some who argue against procalcitonin’s utility cite the fact that existing guidelines already support short-course therapy, obviating the need for biomarker guidance, clinicians have not yet universally adopted this practice. Using a PCT algorithm can decrease duration of therapy and thereby reduce unnecessary antibiotic use. PCT levels less than 0.25 mcg/L support withholding or discontinuing antibiotics, or consideration of an alternative diagnosis.
The dynamics of the PCT assay must be considered in order to use it appropriately. Levels of PCT rise within 3-6 hours of infection, so patients presenting extremely early in the disease course may have falsely low levels. PCT levels correlate with severity of illness and should fall within 2-3 days of initiation of appropriate therapy. A repeat PCT in 2-3 days can be used to help time antibiotic cessation. Studies support stopping antibiotics in stable patients once the PCT level falls below 0.25 mcg/L or drops by 80% in patients with severe elevations. Lack of improvement suggests inadequate antibiotic therapy and is predictive of excess mortality.
Most drivers of false-positive PCT levels are rare and easily identifiable. (See Figure 3.) However, like troponin, patients with chronic kidney disease have delayed PCT clearance, so baseline levels may be about double the normal range. If a baseline is known, monitoring the rise and fall of PCT levels remains clinically useful in this population.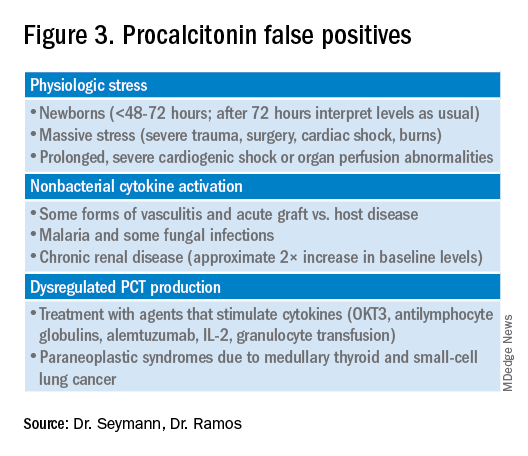
Application of data to case
In reviewing the case, the differential includes a viral upper respiratory infection, an acute exacerbation of COPD, decompensated heart failure, or bacterial pneumonia. The lab and imaging findings are nonspecific, but a PCT level less than 0.25 mcg/L raises concern for an acute bacterial pneumonia. Given that PCT levels rise in bacterial infection and are suppressed in viral infections, treating this patient with antibiotics seems prudent. In this case the relatively mild elevation suggests a less severe infection or a presentation early in the disease course. A repeat PCT in 2-3 days will guide timing for antibiotic cessation.
Bottom line
Thoughtful procalcitonin-guided antibiotic therapy for LRTI may further current antibiotic stewardship initiatives targeting reduction of inappropriate antimicrobial use, which may ultimately reduce rates of Clostridium difficile infections and the emergence of multidrug-resistant organisms.
Dr. Seymann and Dr. Ramos are clinical professors in the division of hospital medicine, department of medicine, at the University of California San Diego.
Key points
- Initial PCT level can help distinguish between viral and bacterial pneumonias.
- PCT levels rise in response to acute bacterial infections and are suppressed in viral infections.
- PCT levels below 0.25 mcg/L suggest that antibiotics can be safely withheld in otherwise stable patients.
- PCT levels correlate with severity of illness and prognosis.
- Rise of PCT is rapid (3-6 hours), and levels fall quickly with appropriate treatment (2-3 days).
- Serial PCT levels can be used to guide duration of antibiotic therapy.
References
1. CDC. Core elements of hospital antibiotic stewardship programs. Atlanta: U.S. Department of Health & Human Services. 2014. Available at www.cdc.gov/getsmart/healthcare/ implementation/core-elements.html.
2. Schuetz P et al. Effect of procalcitonin-based guidelines vs. standard guidelines on antibiotic use in lower respiratory tract infections: The ProHOSP randomized controlled trial. JAMA. 2009;302(10):1059-66. doi: 10.1001/jama.2009.1297.
3. Schuetz P et al. Effect of procalcitonin-guided antibiotic treatment on mortality in acute respiratory infections: A patient level meta-analysis. Lancet Infect Dis. 2018;18(1):95-107. doi: 10.1016/S1473-3099(17)30592-3.
4. Meier MA et al. Procalcitonin-guided antibiotic treatment in patients with positive blood cultures: A patient-level meta-analysis of randomized trials. Clin Infect Dis. 2019;69(3):388-96. doi: 10.1093/cid/ciy917.
5. Wirz Y et al. Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: A patient-level meta-analysis of randomized trials. Crit Care. 2018;22(1):191. doi: 10.1186/s13054-018-2125-7.
6. Huang DT et al. Procalcitonin-guided use of antibiotics for lower respiratory tract infection. N Engl J Med. 2018 Jul 19;379(3):236-49. doi: 10.1056/NEJMoa1802670.
7. Yi SH et al. Duration of antibiotic use among adults with uncomplicated community-acquired pneumonia requiring hospitalization in the United States. Clin Infect Dis. 2018;66(9):1333-41. doi: 10.1093/cid/cix986.
8. Vaughn V et al. Excess antibiotic treatment duration and adverse events in patients hospitalized with pneumonia: A multihospital cohort study. Ann Intern Med. 2019; 171(3):153-63. doi: 10.7326/M18-3640.
Quiz
1. A 57-year-old male is hospitalized for treatment of community-acquired pneumonia with IV azithromycin and ceftriaxone. PCT level on day 1 = 0.35 mcg/L. On day 4 of antibiotics the PCT level is 0.15 mcg/L. What should be done regarding the antibiotic course?
a. Continue antibiotics for a total course of 5 days.
b. Continue antibiotics for a total course of 7 days.
c. Stop antibiotics.
d. Continue antibiotics and repeat a PCT level the next day.
Answer: The best answer is c. Evidence suggests that 5 days of therapy is adequate treatment for uncomplicated community-acquired pneumonia. Procalcitonin-guided therapy allows for further tailoring of the regimen to the individual patient. Since this patient has clinically improved, and the PCT level is less than 0.25 mcg/L, it is reasonable to discontinue treatment and avoid unnecessary antibiotic days.
2. A 42-year-old female with known CKD stage 4 is hospitalized with suspected community-acquired pneumonia. Procalcitonin level is elevated at 0.6 mcg/L. How should the patient be treated?
a. Ignore the PCT as levels are falsely elevated due to CKD.
b. Treat with antibiotics for suspected community-acquired pneumonia.
c. Repeat PCT level in the morning.
d. Check a C-reactive protein level instead.
Answer: The best answer is b. Although decreased renal function can delay clearance of PCT, levels in CKD are typically about twice normal. In this case, when pneumonia is clinically suspected, the level of 0.6 mcg/L would correspond to a level of approximately 0.3 mcg/L and support a decision to treat with antibiotics.
3. A 36-year-old male develops sudden onset of dyspnea, cough, fever, and chills and proceeds rapidly to the emergency department. He is hypoxic, febrile, and has a leukocytosis. The PCT level is checked and found to be 0.2 mcg/L. Chest imaging shows a right middle lobe consolidation. How should the patient be treated?
a. Hold antibiotics.
b. Start antibiotic therapy.
c. Hold antibiotics and repeat PCT level in the morning.
Answer: The best answer is b. The clinical scenario suggests bacterial pneumonia. Given the sudden onset and early presentation to the ED, it is likely that the PCT level has not had time to peak. PCT levels typically begin to rise in 3-6 hours from the time of infection. Withholding antibiotics until the level exceeds 0.25 mcg/L would not be recommended when clinical judgment suggests otherwise.
4. Which of the following noninfectious scenarios does NOT cause an elevated PCT level?
a. Bone marrow transplant patient with acute graft versus host disease of the skin.
b. Patient presenting with paraneoplastic syndrome from small cell lung cancer.
c. Patient with cirrhosis presenting with hepatic encephalopathy.
d. Patient presenting with severe trauma from a motor vehicle accident.
Answer: The answer is c. Cirrhosis and/or hepatic encephalopathy does not cause a falsely elevated PCT level. Acute graft versus host disease, paraneoplastic syndrome from small cell lung cancer or medullary thyroid cancer, and massive stress such as severe trauma can cause elevations in PCT.
Additional reading
Spellberg B. The maturing antibiotic mantra: Shorter is still better. J Hosp Med. 2018;13:361-2. doi: 10.12788/jhm.2904.
Soni NJ et al. Procalcitonin-guided antibiotic therapy: A systematic review and meta-analysis. J Hosp Med. 2013;8:530-540. doi: 10.1002/jhm.2067.
Rhee C. Using procalcitonin to guide antibiotic therapy. Open Forum Infect Dis. 2017;4(1):ofw249. doi: 10.1093/ofid/ofw249.
Sager R et al. Procalcitonin-guided diagnosis and antibiotic stewardship revisited. BMC Med. 2017;15. doi: 10.1186/s12916-017-0795-7.
Case
A 50-year-old female presents with 3 days of cough, subjective fevers, myalgias, and dyspnea. She feels she “may have caught something” while volunteering at a preschool. She has hypertension, congestive heart failure, and 20 pack-years of smoking. Chest x-ray shows bibasilar consolidation versus atelectasis. Vital signs are notable for an O2 saturation of 93%. White blood cell count and differential are normal. Procalcitonin level is 0.4 mcg/L.
Overview of the issue
Lower respiratory tract infections (LRTI) are common in the practice of hospital medicine; however, the primary symptoms of cough and dyspnea can be caused by a myriad of noninfectious conditions. Even when infection is suggested by the clinical presentation, the distinction between bacterial and viral etiologies can be challenging, complicating decisions about antibiotic use. Attention to antibiotic stewardship is a growing concern in U.S. hospitals, where the CDC estimates that as many as 50% of antibiotic orders are inappropriate or entirely unnecessary.1 Antibiotic overuse is a driver of multidrug-resistant organisms and increasing rates of Clostridium difficile infection. A diagnostic test to enhance physicians’ ability to target patients who would benefit from antibiotics could be a useful tool to combat the complications of antibiotic overuse. (See Figure 1.) 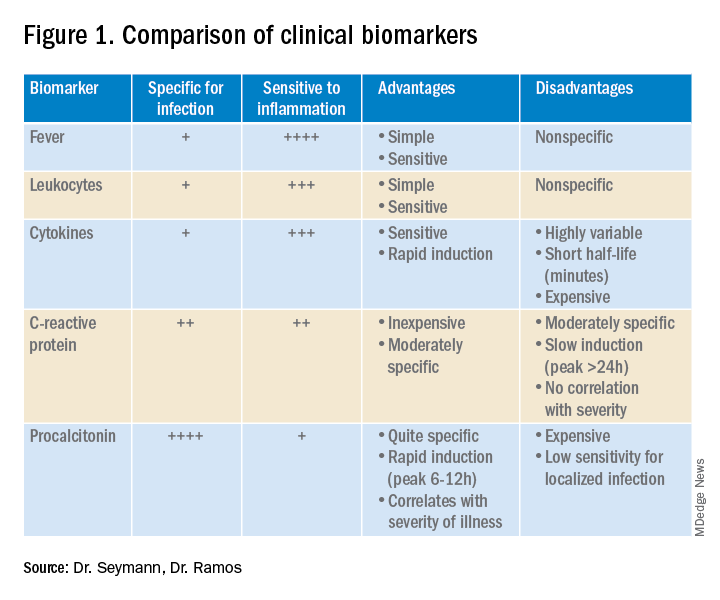
Procalcitonin is produced in the thyroidal C-cells as a prohormone which is processed intracellularly and secreted as calcitonin in response to serum calcium levels. However, intact procalcitonin protein can be secreted from many other tissues in the presence of cytokines such as interleukin 1-beta, tumor necrosis factor-alpha, and lipopolysaccharide, typically released in response to systemic bacterial infections. Conversely, cytokines present in acute viral illness (interferon-gamma) suppress procalcitonin release. This dichotomy presents an opportunity to use procalcitonin to differentiate bacterial from nonbacterial etiologies in various clinical scenarios including LRTI.
Overview of the data
Multiple studies have demonstrated that procalcitonin can be safely used to guide antibiotic prescribing in patients with LRTI. The first large multicenter randomized controlled trial to address the topic was the Swiss PROHOSP study.2 Investigators randomized 1,359 patients hospitalized with LRTI to procalcitonin (PCT) guided therapy or guideline-based therapy. After an initial PCT level was measured, antibiotic prescribing in the PCT arm of the study was directed by a prespecified protocol; specifically, clinicians were discouraged from prescribing antibiotics in patients with PCT levels less than 0.25 mcg/L. (See Figure 2.)
For patients who were particularly ill or unstable at admission, the protocol allowed for antibiotics despite a low PCT level, but repeat measurement within 24 hours and accompanying treatment recommendations were reinforced with the treatment team. Clinicians caring for patients in the control arm were presented with condition-specific clinical practice guidelines to reinforce antibiotic choices. In both arms, the final decision on antibiotic treatment remained with the physician.
Results from the PROHOSP study showed no difference in the combined outcome of death, intensive care unit admission, or complications in the ensuing 30 days, but antibiotic use was significantly reduced. Mean antibiotic exposure dropped from 8.7 to 5.7 days, a reduction of 35%, with the largest decrease among patients with chronic obstructive pulmonary disease (COPD) and acute bronchitis. Antibiotic-related adverse effects fell by 8.2%. Strengths of the study included a very high rate of protocol compliance (90%) by the treating clinicians.
A systematic review of all available studies of procalcitonin-guided therapy for LRTI was published in 2018 and included 26 randomized controlled trials encompassing 6,708 patients in 12 countries. Findings confirmed an overall reduction of 2.4 days in antibiotic exposure, 6% reduction in antibiotic-related adverse effects, and importantly a 17% relative risk reduction in mortality.3
Similar benefits of PCT-guided therapy have been demonstrated even among severely ill patients. A meta-analysis including 523 patients with bacteremia noted mean reduction in antibiotic exposure of 2.86 days, without excess mortality.4 A second meta-analysis of 4,482 critically ill patients admitted to the ICU with sepsis demonstrated not only a reduction in antibiotic exposure, but in mortality as well. Despite a relatively small decrease in antibiotic duration of 1.19 days, the investigators found an 11% reduction in mortality (P = .03) in the PCT-guided group.5
One notable outlier among the many positive studies on PCT-guided antibiotic therapy is the 2018 PROACT study performed in U.S. hospitals over 4 years.6 Its design was similar to the PROHOSP study, however, in contrast to the majority of other trials, the investigators were unable to demonstrate a reduction in antibiotic exposure, leading them to conclude that PCT guidance may not be a useful tool for antibiotic stewardship.
Unfortunately, significant differences in the compliance with the study protocol (90% in PROHOSP vs. 63% in PROACT), and a much healthier patient population (91% of the patients had a PCT less than 0.25, and a majority of patients had asthma which is not normally treated with antibiotics) hamper the generalizability of the PROACT findings. Rather than indicating a failure of PCT, the findings of the study underscore the fact that the utility of any lab test is limited unless it is applied in an appropriate diagnostic setting.
For hospitalists, the most clinically useful role for PCT testing is to guide the duration of antibiotic therapy. Although the literature supports short-course antibiotic therapy in many common conditions seen by hospitalists (Table 1), data suggest overprescribing remains prevalent. Several recent studies targeting LRTI underscore this point.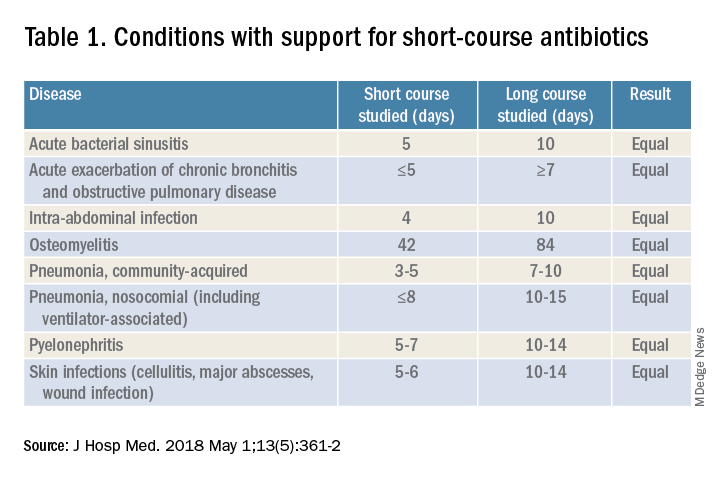
Despite guidelines advocating for treatment of uncomplicated community-acquired pneumonia (CAP) for no more than 5-7 days, two recent retrospective studies suggest most patients receive longer courses. A review of more than 150,000 patients across the United States with uncomplicated CAP documented a mean antibiotic duration of 9.5 days, with close to 70% of patients receiving more than 7 days of therapy.7 A multicenter study of CAP patients hospitalized in Michigan noted similar findings, with a mean 2-day excess duration of therapy or 2,526 excess days of treatment per 1,000 discharges.8 Though some who argue against procalcitonin’s utility cite the fact that existing guidelines already support short-course therapy, obviating the need for biomarker guidance, clinicians have not yet universally adopted this practice. Using a PCT algorithm can decrease duration of therapy and thereby reduce unnecessary antibiotic use. PCT levels less than 0.25 mcg/L support withholding or discontinuing antibiotics, or consideration of an alternative diagnosis.
The dynamics of the PCT assay must be considered in order to use it appropriately. Levels of PCT rise within 3-6 hours of infection, so patients presenting extremely early in the disease course may have falsely low levels. PCT levels correlate with severity of illness and should fall within 2-3 days of initiation of appropriate therapy. A repeat PCT in 2-3 days can be used to help time antibiotic cessation. Studies support stopping antibiotics in stable patients once the PCT level falls below 0.25 mcg/L or drops by 80% in patients with severe elevations. Lack of improvement suggests inadequate antibiotic therapy and is predictive of excess mortality.
Most drivers of false-positive PCT levels are rare and easily identifiable. (See Figure 3.) However, like troponin, patients with chronic kidney disease have delayed PCT clearance, so baseline levels may be about double the normal range. If a baseline is known, monitoring the rise and fall of PCT levels remains clinically useful in this population.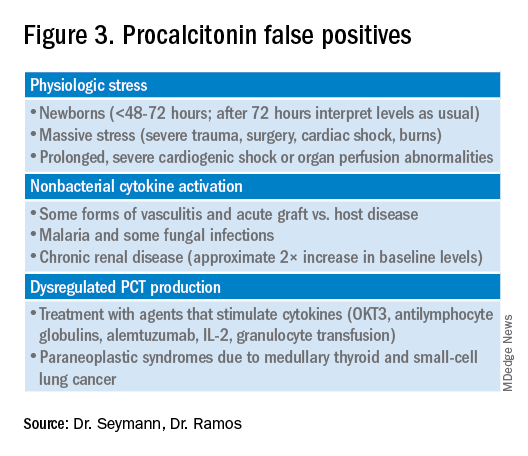
Application of data to case
In reviewing the case, the differential includes a viral upper respiratory infection, an acute exacerbation of COPD, decompensated heart failure, or bacterial pneumonia. The lab and imaging findings are nonspecific, but a PCT level less than 0.25 mcg/L raises concern for an acute bacterial pneumonia. Given that PCT levels rise in bacterial infection and are suppressed in viral infections, treating this patient with antibiotics seems prudent. In this case the relatively mild elevation suggests a less severe infection or a presentation early in the disease course. A repeat PCT in 2-3 days will guide timing for antibiotic cessation.
Bottom line
Thoughtful procalcitonin-guided antibiotic therapy for LRTI may further current antibiotic stewardship initiatives targeting reduction of inappropriate antimicrobial use, which may ultimately reduce rates of Clostridium difficile infections and the emergence of multidrug-resistant organisms.
Dr. Seymann and Dr. Ramos are clinical professors in the division of hospital medicine, department of medicine, at the University of California San Diego.
Key points
- Initial PCT level can help distinguish between viral and bacterial pneumonias.
- PCT levels rise in response to acute bacterial infections and are suppressed in viral infections.
- PCT levels below 0.25 mcg/L suggest that antibiotics can be safely withheld in otherwise stable patients.
- PCT levels correlate with severity of illness and prognosis.
- Rise of PCT is rapid (3-6 hours), and levels fall quickly with appropriate treatment (2-3 days).
- Serial PCT levels can be used to guide duration of antibiotic therapy.
References
1. CDC. Core elements of hospital antibiotic stewardship programs. Atlanta: U.S. Department of Health & Human Services. 2014. Available at www.cdc.gov/getsmart/healthcare/ implementation/core-elements.html.
2. Schuetz P et al. Effect of procalcitonin-based guidelines vs. standard guidelines on antibiotic use in lower respiratory tract infections: The ProHOSP randomized controlled trial. JAMA. 2009;302(10):1059-66. doi: 10.1001/jama.2009.1297.
3. Schuetz P et al. Effect of procalcitonin-guided antibiotic treatment on mortality in acute respiratory infections: A patient level meta-analysis. Lancet Infect Dis. 2018;18(1):95-107. doi: 10.1016/S1473-3099(17)30592-3.
4. Meier MA et al. Procalcitonin-guided antibiotic treatment in patients with positive blood cultures: A patient-level meta-analysis of randomized trials. Clin Infect Dis. 2019;69(3):388-96. doi: 10.1093/cid/ciy917.
5. Wirz Y et al. Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: A patient-level meta-analysis of randomized trials. Crit Care. 2018;22(1):191. doi: 10.1186/s13054-018-2125-7.
6. Huang DT et al. Procalcitonin-guided use of antibiotics for lower respiratory tract infection. N Engl J Med. 2018 Jul 19;379(3):236-49. doi: 10.1056/NEJMoa1802670.
7. Yi SH et al. Duration of antibiotic use among adults with uncomplicated community-acquired pneumonia requiring hospitalization in the United States. Clin Infect Dis. 2018;66(9):1333-41. doi: 10.1093/cid/cix986.
8. Vaughn V et al. Excess antibiotic treatment duration and adverse events in patients hospitalized with pneumonia: A multihospital cohort study. Ann Intern Med. 2019; 171(3):153-63. doi: 10.7326/M18-3640.
Quiz
1. A 57-year-old male is hospitalized for treatment of community-acquired pneumonia with IV azithromycin and ceftriaxone. PCT level on day 1 = 0.35 mcg/L. On day 4 of antibiotics the PCT level is 0.15 mcg/L. What should be done regarding the antibiotic course?
a. Continue antibiotics for a total course of 5 days.
b. Continue antibiotics for a total course of 7 days.
c. Stop antibiotics.
d. Continue antibiotics and repeat a PCT level the next day.
Answer: The best answer is c. Evidence suggests that 5 days of therapy is adequate treatment for uncomplicated community-acquired pneumonia. Procalcitonin-guided therapy allows for further tailoring of the regimen to the individual patient. Since this patient has clinically improved, and the PCT level is less than 0.25 mcg/L, it is reasonable to discontinue treatment and avoid unnecessary antibiotic days.
2. A 42-year-old female with known CKD stage 4 is hospitalized with suspected community-acquired pneumonia. Procalcitonin level is elevated at 0.6 mcg/L. How should the patient be treated?
a. Ignore the PCT as levels are falsely elevated due to CKD.
b. Treat with antibiotics for suspected community-acquired pneumonia.
c. Repeat PCT level in the morning.
d. Check a C-reactive protein level instead.
Answer: The best answer is b. Although decreased renal function can delay clearance of PCT, levels in CKD are typically about twice normal. In this case, when pneumonia is clinically suspected, the level of 0.6 mcg/L would correspond to a level of approximately 0.3 mcg/L and support a decision to treat with antibiotics.
3. A 36-year-old male develops sudden onset of dyspnea, cough, fever, and chills and proceeds rapidly to the emergency department. He is hypoxic, febrile, and has a leukocytosis. The PCT level is checked and found to be 0.2 mcg/L. Chest imaging shows a right middle lobe consolidation. How should the patient be treated?
a. Hold antibiotics.
b. Start antibiotic therapy.
c. Hold antibiotics and repeat PCT level in the morning.
Answer: The best answer is b. The clinical scenario suggests bacterial pneumonia. Given the sudden onset and early presentation to the ED, it is likely that the PCT level has not had time to peak. PCT levels typically begin to rise in 3-6 hours from the time of infection. Withholding antibiotics until the level exceeds 0.25 mcg/L would not be recommended when clinical judgment suggests otherwise.
4. Which of the following noninfectious scenarios does NOT cause an elevated PCT level?
a. Bone marrow transplant patient with acute graft versus host disease of the skin.
b. Patient presenting with paraneoplastic syndrome from small cell lung cancer.
c. Patient with cirrhosis presenting with hepatic encephalopathy.
d. Patient presenting with severe trauma from a motor vehicle accident.
Answer: The answer is c. Cirrhosis and/or hepatic encephalopathy does not cause a falsely elevated PCT level. Acute graft versus host disease, paraneoplastic syndrome from small cell lung cancer or medullary thyroid cancer, and massive stress such as severe trauma can cause elevations in PCT.
Additional reading
Spellberg B. The maturing antibiotic mantra: Shorter is still better. J Hosp Med. 2018;13:361-2. doi: 10.12788/jhm.2904.
Soni NJ et al. Procalcitonin-guided antibiotic therapy: A systematic review and meta-analysis. J Hosp Med. 2013;8:530-540. doi: 10.1002/jhm.2067.
Rhee C. Using procalcitonin to guide antibiotic therapy. Open Forum Infect Dis. 2017;4(1):ofw249. doi: 10.1093/ofid/ofw249.
Sager R et al. Procalcitonin-guided diagnosis and antibiotic stewardship revisited. BMC Med. 2017;15. doi: 10.1186/s12916-017-0795-7.
Ptosis after motorcycle accident
A 45-year-old woman visited the clinic 6 weeks after having a stroke while on her motorcycle, which resulted in a crash. She had not been wearing a helmet and was uncertain if she had sustained a head injury. She said that during the hospital stay following the accident, she was diagnosed as hypertensive; she denied any other significant prior medical history.
Following the crash, she said she’d been experiencing weakness in her right arm and leg and had been unable to open her right eye. When her right eye was opened manually, she said she had double vision and sensitivity to light.
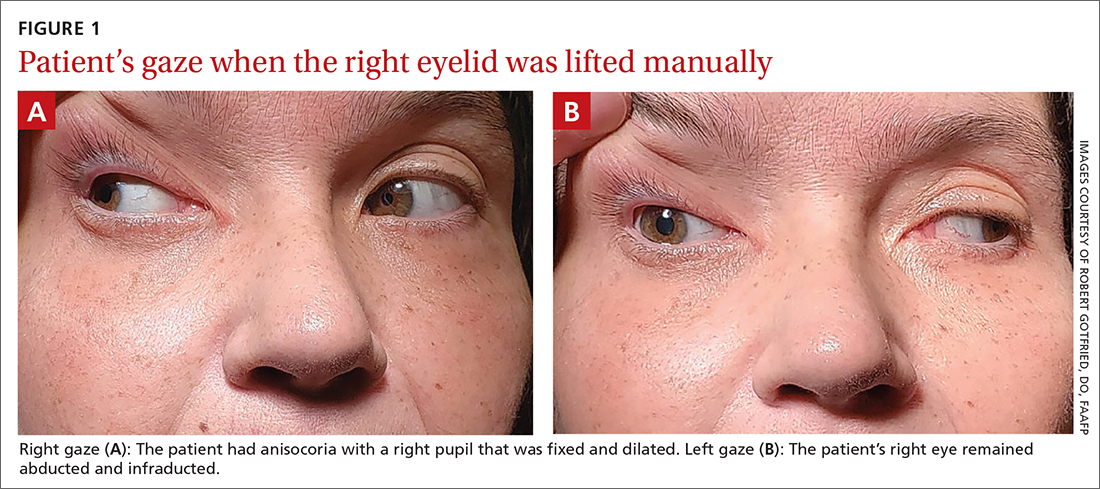
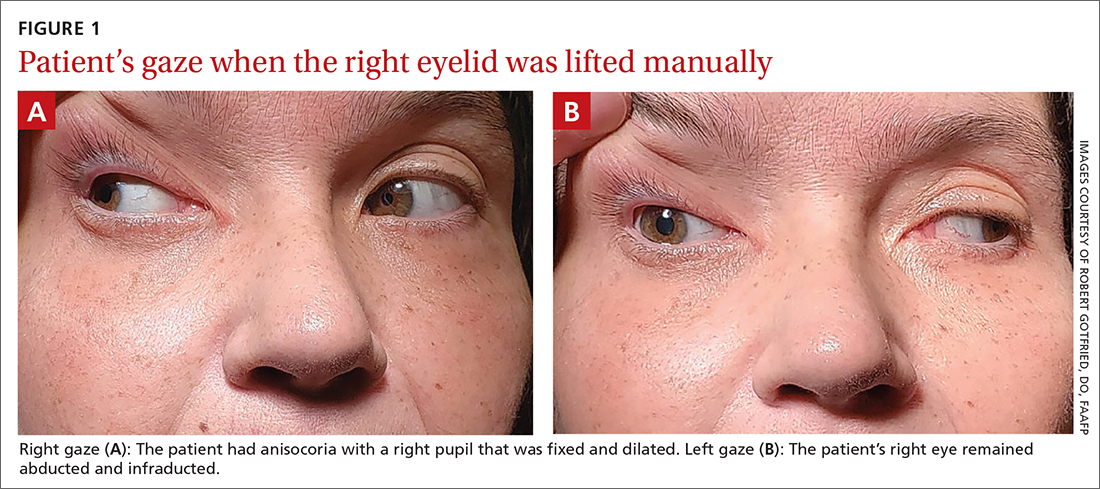
On exam, the patient had exotropia with hypotropia of her right eye. Additionally, she had anisocoria with an enlarged, nonreactive right pupil (FIGURE 1A). She was unable to adduct, supraduct, or infraduct her right eye (FIGURE 1B). Her cranial nerves were otherwise intact. On manual strength testing, she had 4/5 strength of both her right upper and lower extremities.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Third (oculomotor) nerve palsy
This patient had a complete third nerve palsy (TNP). This is defined as palsy involving all of the muscles innervated by the oculomotor nerve, with pupillary involvement.1 The oculomotor nerve supplies motor innervation to the levator palpebrae superioris, superior rectus, medial rectus, inferior rectus, and inferior oblique muscles and parasympathetic innervation to the pupillary constrictor and ciliary muscles.2 As a result, patients present with exotropia and hypotropia on exam with anisocoria. Diplopia, ptosis, and an enlarged pupil are classic symptoms of TNP.2
Computed tomography (CT) of the brain performed immediately after this patient’s accident demonstrated a 15-mm hemorrhage within the left basal ganglia with mild associated edema, and a small focus of hyperattenuation within the right aspect of the suprasellar cistern. There was no evidence of skull fracture. CT angiography (CTA) of the brain showed no evidence of aneurysm.
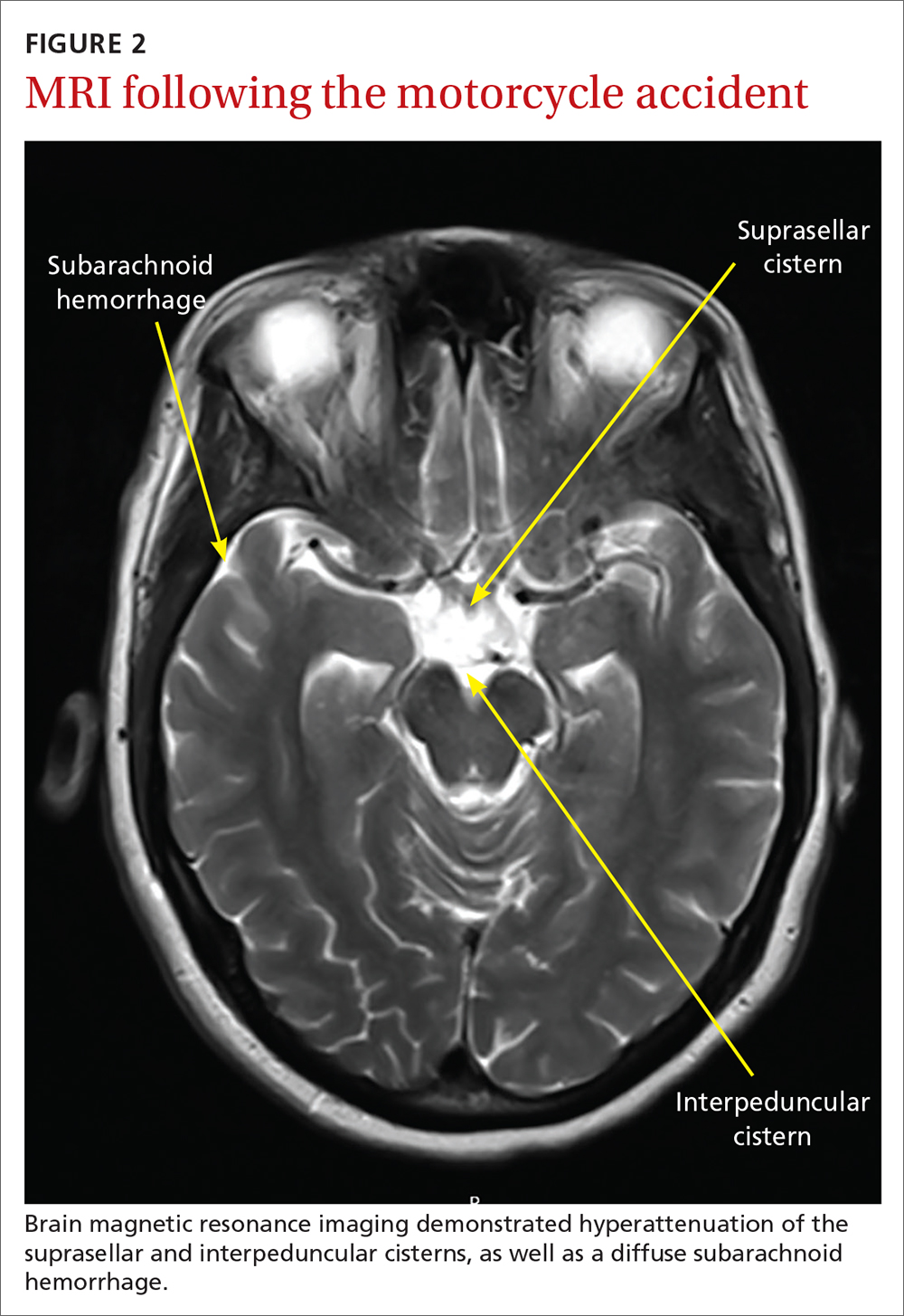
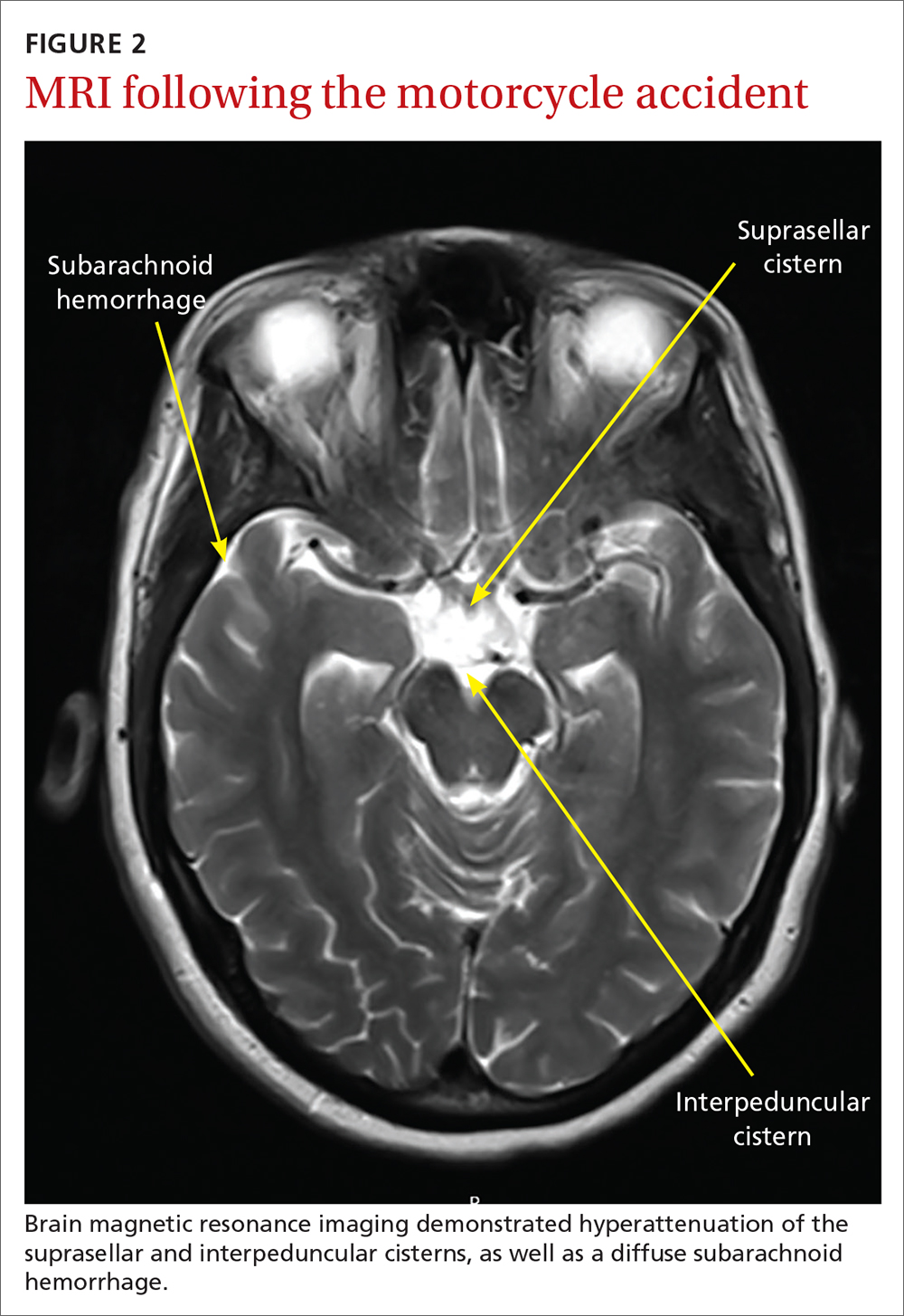
Several days later, magnetic resonance imaging (MRI) of the brain confirmed prior CT findings and revealed hemorrhagic contusions along the anterior and medial left temporal lobe. Additionally, the MRI showed subtle subdural hemorrhages along the midline falx and right parietal region, as well as diffuse subarachnoid hemorrhage around both hemispheres, the interpeduncular cistern, and the suprasellar cistern (FIGURE 2). The basal ganglia hemorrhage was believed to have been a result of uncontrolled hypertension. The hemorrhage was responsible for her right-sided weakness and was the presumed cause of the accident. The other findings were due to head trauma. Her TNP was most likely caused by both compression and irritation of the right oculomotor nerve.
An uncommon occurrence
A population-based study identified the annual incidence of TNP to be 4 per 100,000.1 The mean age of onset was 42 years. The incidence in patients older than 60 years was greater than the incidence in those younger than 60.2 Isolated TNP occurred in approximately 40% of cases.2
Complete TNP is typically indicative of compression of the ipsilateral third nerve.2 The most common region for third nerve injury is the subarachnoid space, where the oculomotor nerve is vulnerable to compression, often by an aneurysm arising from the junction of the internal carotid and posterior communicating arteries.3
Continue to: Incomplete TNP
Incomplete TNP is often microvascular in origin and requires evaluation for diabetes and hypertension. Microvascular TNP is frequently painful but usually self-resolves after 2 to 4 months.2 Giant cell arteritis may also cause an isolated, painful TNP.2
A varied differential diagnosis and a TNP link to COVID-19
The differential diagnosis for TNP includes the following:
Orbital apex injury is usually seen after high-energy craniofacial trauma.4 Orbital apex fractures present with different signs and symptoms, depending on the degree of injury to neural and vascular structures. Various syndromes come into play, the most common being superior orbital fissure syndrome, which is characterized by dysfunction of cranial nerves III, IV, V, and VI.4 Features include ophthalmoplegia, upper eyelid ptosis, a nonreactive dilated pupil, anesthesia over the ipsilateral forehead, loss of corneal reflex, orbital pain, and proptosis.4
In patients with suspected orbital apex fractures, it’s important to assess for the presence of an optic neuropathy, an evolving orbital compartment syndrome, or a ruptured globe, because these 3 things may demand acute intervention.4
Chronic progressive external ophthalmoplegia (CPEO) is a mitochondrial disorder characterized by a slow, progressive paralysis of the extraocular muscles.5 Patients usually experience bilateral, symmetrical, progressive ptosis, followed by ophthalmoparesis months to years later. Ciliary and iris muscles are not involved. CPEO often occurs with other systemic features of mitochondrial dysfunction that can cause significant morbidity and mortality.5
Continue to: Graves ophthalmopathy
Graves ophthalmopathy arises from soft-tissue enlargement in the orbit, leading to increased pressure within the bony cavity.6 Approximately 40% of patients with Graves ophthalmopathy present with restrictive extraocular myopathy; however > 90% have eyelid retraction, as opposed to ptosis.7
Guillain-Barré syndrome (GBS) is an acute, demyelinating immune-mediated polyneuropathy involving the spinal roots, peripheral nerves, and often the cranial nerves.8 The Miller Fisher variant of GBS is characterized by bilateral ophthalmoparesis, areflexia, and ataxia.8 At the early stage of illness, the presentation may be similar to TNP.8 Brain imaging is normal in patients with GBS; the diagnosis is established via characteristic electromyography and cerebrospinal fluid findings.8
Myasthenia gravis often manifests with variable ptosis associated with diplopia.9 Symptoms may be unilateral or bilateral. The ice-pack test has been identified as a simple, preliminary test for ocular myasthenia. The test involves the application of an ice-pack over the lids for 5 minutes. A 50% reduction in at least 1 component of ocular deviation is considered a positive response.10 Its specificity reportedly reaches 100%, with a sensitivity of 80%.10
COVID-19 infection may also include neurologic manifestations. There are an increasing number of case reports of central nervous system abnormalities including TNP.11,12
Trauma, tumors, or an aneurysm could be at work in TNP
TNP associated with trauma usually develops secondary to compression from an expanding hematoma, although it may also be a result of irritation of the nerve from blood in the subarachnoid space.13 Estimates of the incidence of TNP due to trauma range from 12% to 26% of cases.1,14 Vehicle-related injury is the most frequent cause of trauma-related TNP.14
Continue to: Pituitary tumors
Pituitary tumors most commonly involve the oculomotor nerve; 14% to 30% of pituitary tumors lead to TNP.13 Pituitary apoplexy secondary to infarction or hemorrhage is often associated with visual field defects and TNP.13
An underlying aneurysm manifests in a minority (10% to 15%) of patients presenting with TNP.3
Imaging is key to getting at the cause of TNP
The evaluation of patients presenting with acute TNP should be focused first on detecting an aneurysmal compressive lesion.3 CTA is the imaging modality of choice.
Once an aneurysm has been ruled out, the work-up should include a lumbar puncture and an erythrocyte sedimentation rate. Older patients should be assessed for conditions such as hypertension or diabetes that put them at risk for microvascular disease.3 If microvascular TNP is unlikely, MRI with MR angiography is recommended to exclude other potential etiologies of TNP.3 If the patient is younger than 50 years of age, consider potential infectious and inflammatory etiologies (eg, giant cell arteritis).3
Treatment options are varied
The treatment of patients with TNP is specific to the disease state. For those patients with vascular risk factors and a presumptive diagnosis of microvascular TNP, it is reasonable to observe the patient for 2 to 3 months.3 Antiplatelet therapy is usually initiated. Patching 1 eye is useful in alleviating diplopia, particularly in the short term. In most cases, deficits related to TNP resolve over weeks to months. Deficits that persist beyond 6 months may require surgical intervention.
Continue to: "The tip of the iceberg"
TNP: “The tip of the iceberg”
TNP may signal a neurologic emergency, such as an aneurysm, or other conditions such as pituitary disease or giant cell arteritis. Any patient presenting with acute onset of TNP should undergo a noninvasive neuroimaging study.3
Our patient was treated for hypertension; however, she was lost to follow-up.
1. Fang C, Leavitt JA, Hodge DO, et al. Incidence and etiologies of acquired third nerve palsy using a population-based method. JAMA Ophthalmol. 2017;135:23-28. doi: 10.1001/jamaophthalmol.2016.4456
2. Bruce BB, Biousse V, Newman NJ. Third nerve palsies. Semin Neurol. 2007;27:257-268. doi: 10.1055/s-2007-979681
3. Margolin E, Freund P. A review of third nerve palsies. Int Ophthalmol Clin. 2019;59:99-112. doi: 10.1097/IIO.0000000000000279
4. Linnau KF, Hallam DK, Lomoschitz FM, et al. Orbital apex injury: trauma at the junction between the face and the cranium. Eur J Radiol. 2003;48:5-16. doi: 10.1016/s0720-048x(03)00203-1
5. McClelland C, Manousakis G, Lee MS. Progressive external ophthalmoplegia. Curr Neurol Neurosci Rep. 2016;16:53. doi: 10.1007/s11910-016-0652-7
6. Bahn RS. Graves’ ophthalmopathy. N Engl J Med. 2010;362:726-738. doi: 10.1056/NEJMra0905750
7. Subetki I, Soewond P, Soebardi S, et al. Practical guidelines management of graves ophthalmopathy. Acta Med Indones. 2019;51:364-371.
8. Wijdicks EF, Klein CJ. Guillain-Barré syndrome. Mayo Clin Proc. 2017;92:467-479. doi: 10.1016/j.mayocp.2016.12.002
9. Beloor Suresh A, Asuncion RMD. Myasthenia Gravis. In: StatPearls [Internet]. StatPearls Publishing; 2021. Accessed April 26, 2021. www.ncbi.nlm.nih.gov/books/NBK559331/
10. Chatzistefanou KI, Kouris T, Iliakis E, et al. The ice pack test in the differential diagnosis of myasthenic diplopia. Ophthalmology. 2009;116:2236-2243. doi: 10.1016/j.ophtha.2009.04.039
11. Pascual-Prieto J, Narváez-Palazón C, Porta-Etessam J, et al. COVID-19 epidemic: should ophthalmologists be aware of oculomotor paresis? Arch Soc Esp Oftalmol. 2020;95:361-362. doi: 10.1016/j.oftal.2020.05.002
12. Collantes MEV, Espiritu AI, Sy MCC, et al. Neurological manifestations in COVID-19 infection: a systematic review and meta-analysis. Can J Neurol Sci. 2021;48:66-76. doi: 10.1017/cjn.2020.146
13. Raza HK, Chen H, Chansysouphanthong T, et al. The aetiologies of the unilateral oculomotor nerve palsy: a review of the literature. Somatosens Mot Res. 2018;35:229-239. doi :10.1080/08990220.2018.1547697
14. Keane J. Third nerve palsy: analysis of 1400 personally-examined inpatients. Can J Neurol Sci. 2010;37:662-670. doi: 10.1017/s0317167100010866
A 45-year-old woman visited the clinic 6 weeks after having a stroke while on her motorcycle, which resulted in a crash. She had not been wearing a helmet and was uncertain if she had sustained a head injury. She said that during the hospital stay following the accident, she was diagnosed as hypertensive; she denied any other significant prior medical history.
Following the crash, she said she’d been experiencing weakness in her right arm and leg and had been unable to open her right eye. When her right eye was opened manually, she said she had double vision and sensitivity to light.
On exam, the patient had exotropia with hypotropia of her right eye. Additionally, she had anisocoria with an enlarged, nonreactive right pupil (FIGURE 1A). She was unable to adduct, supraduct, or infraduct her right eye (FIGURE 1B). Her cranial nerves were otherwise intact. On manual strength testing, she had 4/5 strength of both her right upper and lower extremities.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Third (oculomotor) nerve palsy
This patient had a complete third nerve palsy (TNP). This is defined as palsy involving all of the muscles innervated by the oculomotor nerve, with pupillary involvement.1 The oculomotor nerve supplies motor innervation to the levator palpebrae superioris, superior rectus, medial rectus, inferior rectus, and inferior oblique muscles and parasympathetic innervation to the pupillary constrictor and ciliary muscles.2 As a result, patients present with exotropia and hypotropia on exam with anisocoria. Diplopia, ptosis, and an enlarged pupil are classic symptoms of TNP.2
Computed tomography (CT) of the brain performed immediately after this patient’s accident demonstrated a 15-mm hemorrhage within the left basal ganglia with mild associated edema, and a small focus of hyperattenuation within the right aspect of the suprasellar cistern. There was no evidence of skull fracture. CT angiography (CTA) of the brain showed no evidence of aneurysm.
Several days later, magnetic resonance imaging (MRI) of the brain confirmed prior CT findings and revealed hemorrhagic contusions along the anterior and medial left temporal lobe. Additionally, the MRI showed subtle subdural hemorrhages along the midline falx and right parietal region, as well as diffuse subarachnoid hemorrhage around both hemispheres, the interpeduncular cistern, and the suprasellar cistern (FIGURE 2). The basal ganglia hemorrhage was believed to have been a result of uncontrolled hypertension. The hemorrhage was responsible for her right-sided weakness and was the presumed cause of the accident. The other findings were due to head trauma. Her TNP was most likely caused by both compression and irritation of the right oculomotor nerve.
An uncommon occurrence
A population-based study identified the annual incidence of TNP to be 4 per 100,000.1 The mean age of onset was 42 years. The incidence in patients older than 60 years was greater than the incidence in those younger than 60.2 Isolated TNP occurred in approximately 40% of cases.2
Complete TNP is typically indicative of compression of the ipsilateral third nerve.2 The most common region for third nerve injury is the subarachnoid space, where the oculomotor nerve is vulnerable to compression, often by an aneurysm arising from the junction of the internal carotid and posterior communicating arteries.3
Continue to: Incomplete TNP
Incomplete TNP is often microvascular in origin and requires evaluation for diabetes and hypertension. Microvascular TNP is frequently painful but usually self-resolves after 2 to 4 months.2 Giant cell arteritis may also cause an isolated, painful TNP.2
A varied differential diagnosis and a TNP link to COVID-19
The differential diagnosis for TNP includes the following:
Orbital apex injury is usually seen after high-energy craniofacial trauma.4 Orbital apex fractures present with different signs and symptoms, depending on the degree of injury to neural and vascular structures. Various syndromes come into play, the most common being superior orbital fissure syndrome, which is characterized by dysfunction of cranial nerves III, IV, V, and VI.4 Features include ophthalmoplegia, upper eyelid ptosis, a nonreactive dilated pupil, anesthesia over the ipsilateral forehead, loss of corneal reflex, orbital pain, and proptosis.4
In patients with suspected orbital apex fractures, it’s important to assess for the presence of an optic neuropathy, an evolving orbital compartment syndrome, or a ruptured globe, because these 3 things may demand acute intervention.4
Chronic progressive external ophthalmoplegia (CPEO) is a mitochondrial disorder characterized by a slow, progressive paralysis of the extraocular muscles.5 Patients usually experience bilateral, symmetrical, progressive ptosis, followed by ophthalmoparesis months to years later. Ciliary and iris muscles are not involved. CPEO often occurs with other systemic features of mitochondrial dysfunction that can cause significant morbidity and mortality.5
Continue to: Graves ophthalmopathy
Graves ophthalmopathy arises from soft-tissue enlargement in the orbit, leading to increased pressure within the bony cavity.6 Approximately 40% of patients with Graves ophthalmopathy present with restrictive extraocular myopathy; however > 90% have eyelid retraction, as opposed to ptosis.7
Guillain-Barré syndrome (GBS) is an acute, demyelinating immune-mediated polyneuropathy involving the spinal roots, peripheral nerves, and often the cranial nerves.8 The Miller Fisher variant of GBS is characterized by bilateral ophthalmoparesis, areflexia, and ataxia.8 At the early stage of illness, the presentation may be similar to TNP.8 Brain imaging is normal in patients with GBS; the diagnosis is established via characteristic electromyography and cerebrospinal fluid findings.8
Myasthenia gravis often manifests with variable ptosis associated with diplopia.9 Symptoms may be unilateral or bilateral. The ice-pack test has been identified as a simple, preliminary test for ocular myasthenia. The test involves the application of an ice-pack over the lids for 5 minutes. A 50% reduction in at least 1 component of ocular deviation is considered a positive response.10 Its specificity reportedly reaches 100%, with a sensitivity of 80%.10
COVID-19 infection may also include neurologic manifestations. There are an increasing number of case reports of central nervous system abnormalities including TNP.11,12
Trauma, tumors, or an aneurysm could be at work in TNP
TNP associated with trauma usually develops secondary to compression from an expanding hematoma, although it may also be a result of irritation of the nerve from blood in the subarachnoid space.13 Estimates of the incidence of TNP due to trauma range from 12% to 26% of cases.1,14 Vehicle-related injury is the most frequent cause of trauma-related TNP.14
Continue to: Pituitary tumors
Pituitary tumors most commonly involve the oculomotor nerve; 14% to 30% of pituitary tumors lead to TNP.13 Pituitary apoplexy secondary to infarction or hemorrhage is often associated with visual field defects and TNP.13
An underlying aneurysm manifests in a minority (10% to 15%) of patients presenting with TNP.3
Imaging is key to getting at the cause of TNP
The evaluation of patients presenting with acute TNP should be focused first on detecting an aneurysmal compressive lesion.3 CTA is the imaging modality of choice.
Once an aneurysm has been ruled out, the work-up should include a lumbar puncture and an erythrocyte sedimentation rate. Older patients should be assessed for conditions such as hypertension or diabetes that put them at risk for microvascular disease.3 If microvascular TNP is unlikely, MRI with MR angiography is recommended to exclude other potential etiologies of TNP.3 If the patient is younger than 50 years of age, consider potential infectious and inflammatory etiologies (eg, giant cell arteritis).3
Treatment options are varied
The treatment of patients with TNP is specific to the disease state. For those patients with vascular risk factors and a presumptive diagnosis of microvascular TNP, it is reasonable to observe the patient for 2 to 3 months.3 Antiplatelet therapy is usually initiated. Patching 1 eye is useful in alleviating diplopia, particularly in the short term. In most cases, deficits related to TNP resolve over weeks to months. Deficits that persist beyond 6 months may require surgical intervention.
Continue to: "The tip of the iceberg"
TNP: “The tip of the iceberg”
TNP may signal a neurologic emergency, such as an aneurysm, or other conditions such as pituitary disease or giant cell arteritis. Any patient presenting with acute onset of TNP should undergo a noninvasive neuroimaging study.3
Our patient was treated for hypertension; however, she was lost to follow-up.
A 45-year-old woman visited the clinic 6 weeks after having a stroke while on her motorcycle, which resulted in a crash. She had not been wearing a helmet and was uncertain if she had sustained a head injury. She said that during the hospital stay following the accident, she was diagnosed as hypertensive; she denied any other significant prior medical history.
Following the crash, she said she’d been experiencing weakness in her right arm and leg and had been unable to open her right eye. When her right eye was opened manually, she said she had double vision and sensitivity to light.
On exam, the patient had exotropia with hypotropia of her right eye. Additionally, she had anisocoria with an enlarged, nonreactive right pupil (FIGURE 1A). She was unable to adduct, supraduct, or infraduct her right eye (FIGURE 1B). Her cranial nerves were otherwise intact. On manual strength testing, she had 4/5 strength of both her right upper and lower extremities.
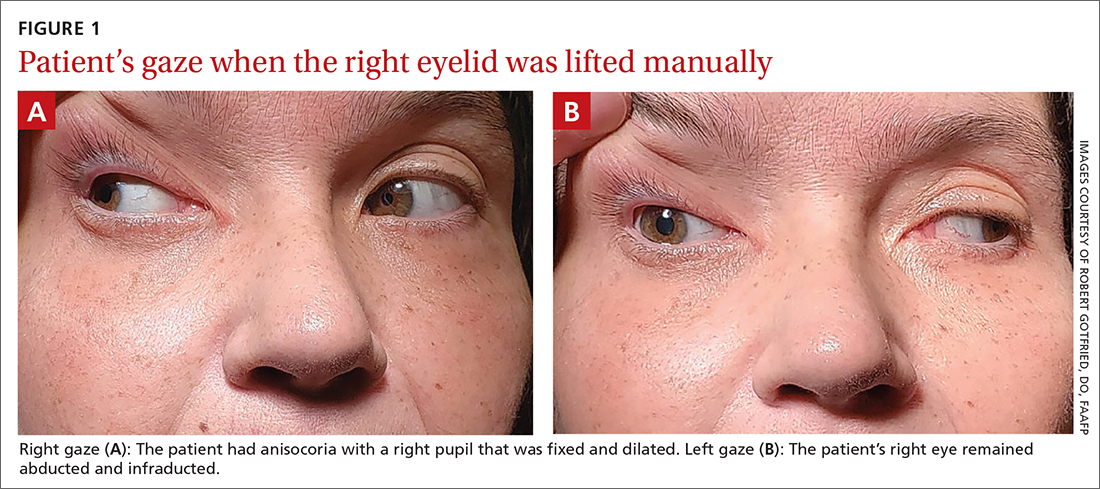
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Third (oculomotor) nerve palsy
This patient had a complete third nerve palsy (TNP). This is defined as palsy involving all of the muscles innervated by the oculomotor nerve, with pupillary involvement.1 The oculomotor nerve supplies motor innervation to the levator palpebrae superioris, superior rectus, medial rectus, inferior rectus, and inferior oblique muscles and parasympathetic innervation to the pupillary constrictor and ciliary muscles.2 As a result, patients present with exotropia and hypotropia on exam with anisocoria. Diplopia, ptosis, and an enlarged pupil are classic symptoms of TNP.2
Computed tomography (CT) of the brain performed immediately after this patient’s accident demonstrated a 15-mm hemorrhage within the left basal ganglia with mild associated edema, and a small focus of hyperattenuation within the right aspect of the suprasellar cistern. There was no evidence of skull fracture. CT angiography (CTA) of the brain showed no evidence of aneurysm.
Several days later, magnetic resonance imaging (MRI) of the brain confirmed prior CT findings and revealed hemorrhagic contusions along the anterior and medial left temporal lobe. Additionally, the MRI showed subtle subdural hemorrhages along the midline falx and right parietal region, as well as diffuse subarachnoid hemorrhage around both hemispheres, the interpeduncular cistern, and the suprasellar cistern (FIGURE 2). The basal ganglia hemorrhage was believed to have been a result of uncontrolled hypertension. The hemorrhage was responsible for her right-sided weakness and was the presumed cause of the accident. The other findings were due to head trauma. Her TNP was most likely caused by both compression and irritation of the right oculomotor nerve.
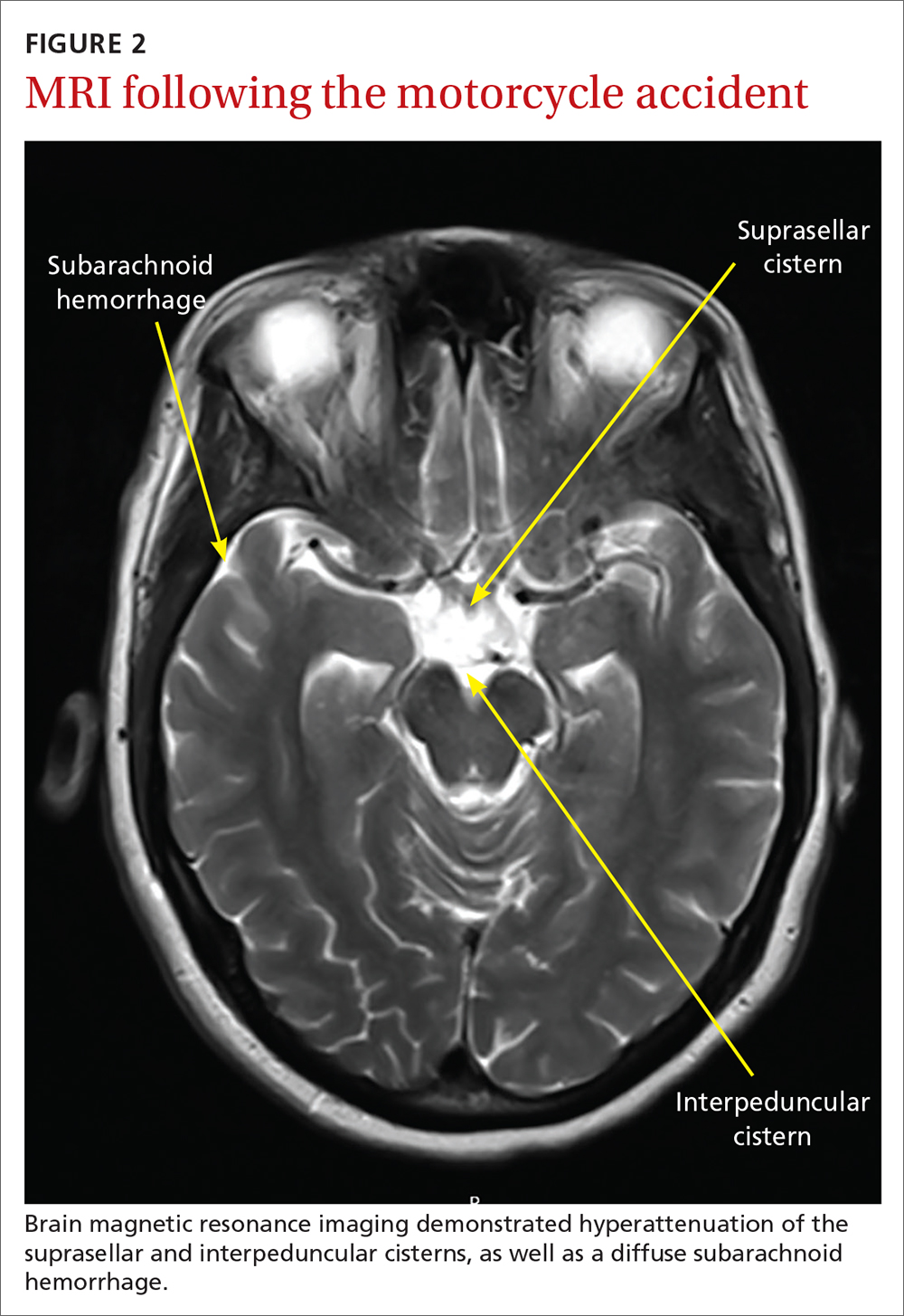
An uncommon occurrence
A population-based study identified the annual incidence of TNP to be 4 per 100,000.1 The mean age of onset was 42 years. The incidence in patients older than 60 years was greater than the incidence in those younger than 60.2 Isolated TNP occurred in approximately 40% of cases.2
Complete TNP is typically indicative of compression of the ipsilateral third nerve.2 The most common region for third nerve injury is the subarachnoid space, where the oculomotor nerve is vulnerable to compression, often by an aneurysm arising from the junction of the internal carotid and posterior communicating arteries.3
Continue to: Incomplete TNP
Incomplete TNP is often microvascular in origin and requires evaluation for diabetes and hypertension. Microvascular TNP is frequently painful but usually self-resolves after 2 to 4 months.2 Giant cell arteritis may also cause an isolated, painful TNP.2
A varied differential diagnosis and a TNP link to COVID-19
The differential diagnosis for TNP includes the following:
Orbital apex injury is usually seen after high-energy craniofacial trauma.4 Orbital apex fractures present with different signs and symptoms, depending on the degree of injury to neural and vascular structures. Various syndromes come into play, the most common being superior orbital fissure syndrome, which is characterized by dysfunction of cranial nerves III, IV, V, and VI.4 Features include ophthalmoplegia, upper eyelid ptosis, a nonreactive dilated pupil, anesthesia over the ipsilateral forehead, loss of corneal reflex, orbital pain, and proptosis.4
In patients with suspected orbital apex fractures, it’s important to assess for the presence of an optic neuropathy, an evolving orbital compartment syndrome, or a ruptured globe, because these 3 things may demand acute intervention.4
Chronic progressive external ophthalmoplegia (CPEO) is a mitochondrial disorder characterized by a slow, progressive paralysis of the extraocular muscles.5 Patients usually experience bilateral, symmetrical, progressive ptosis, followed by ophthalmoparesis months to years later. Ciliary and iris muscles are not involved. CPEO often occurs with other systemic features of mitochondrial dysfunction that can cause significant morbidity and mortality.5
Continue to: Graves ophthalmopathy
Graves ophthalmopathy arises from soft-tissue enlargement in the orbit, leading to increased pressure within the bony cavity.6 Approximately 40% of patients with Graves ophthalmopathy present with restrictive extraocular myopathy; however > 90% have eyelid retraction, as opposed to ptosis.7
Guillain-Barré syndrome (GBS) is an acute, demyelinating immune-mediated polyneuropathy involving the spinal roots, peripheral nerves, and often the cranial nerves.8 The Miller Fisher variant of GBS is characterized by bilateral ophthalmoparesis, areflexia, and ataxia.8 At the early stage of illness, the presentation may be similar to TNP.8 Brain imaging is normal in patients with GBS; the diagnosis is established via characteristic electromyography and cerebrospinal fluid findings.8
Myasthenia gravis often manifests with variable ptosis associated with diplopia.9 Symptoms may be unilateral or bilateral. The ice-pack test has been identified as a simple, preliminary test for ocular myasthenia. The test involves the application of an ice-pack over the lids for 5 minutes. A 50% reduction in at least 1 component of ocular deviation is considered a positive response.10 Its specificity reportedly reaches 100%, with a sensitivity of 80%.10
COVID-19 infection may also include neurologic manifestations. There are an increasing number of case reports of central nervous system abnormalities including TNP.11,12
Trauma, tumors, or an aneurysm could be at work in TNP
TNP associated with trauma usually develops secondary to compression from an expanding hematoma, although it may also be a result of irritation of the nerve from blood in the subarachnoid space.13 Estimates of the incidence of TNP due to trauma range from 12% to 26% of cases.1,14 Vehicle-related injury is the most frequent cause of trauma-related TNP.14
Continue to: Pituitary tumors
Pituitary tumors most commonly involve the oculomotor nerve; 14% to 30% of pituitary tumors lead to TNP.13 Pituitary apoplexy secondary to infarction or hemorrhage is often associated with visual field defects and TNP.13
An underlying aneurysm manifests in a minority (10% to 15%) of patients presenting with TNP.3
Imaging is key to getting at the cause of TNP
The evaluation of patients presenting with acute TNP should be focused first on detecting an aneurysmal compressive lesion.3 CTA is the imaging modality of choice.
Once an aneurysm has been ruled out, the work-up should include a lumbar puncture and an erythrocyte sedimentation rate. Older patients should be assessed for conditions such as hypertension or diabetes that put them at risk for microvascular disease.3 If microvascular TNP is unlikely, MRI with MR angiography is recommended to exclude other potential etiologies of TNP.3 If the patient is younger than 50 years of age, consider potential infectious and inflammatory etiologies (eg, giant cell arteritis).3
Treatment options are varied
The treatment of patients with TNP is specific to the disease state. For those patients with vascular risk factors and a presumptive diagnosis of microvascular TNP, it is reasonable to observe the patient for 2 to 3 months.3 Antiplatelet therapy is usually initiated. Patching 1 eye is useful in alleviating diplopia, particularly in the short term. In most cases, deficits related to TNP resolve over weeks to months. Deficits that persist beyond 6 months may require surgical intervention.
Continue to: "The tip of the iceberg"
TNP: “The tip of the iceberg”
TNP may signal a neurologic emergency, such as an aneurysm, or other conditions such as pituitary disease or giant cell arteritis. Any patient presenting with acute onset of TNP should undergo a noninvasive neuroimaging study.3
Our patient was treated for hypertension; however, she was lost to follow-up.
1. Fang C, Leavitt JA, Hodge DO, et al. Incidence and etiologies of acquired third nerve palsy using a population-based method. JAMA Ophthalmol. 2017;135:23-28. doi: 10.1001/jamaophthalmol.2016.4456
2. Bruce BB, Biousse V, Newman NJ. Third nerve palsies. Semin Neurol. 2007;27:257-268. doi: 10.1055/s-2007-979681
3. Margolin E, Freund P. A review of third nerve palsies. Int Ophthalmol Clin. 2019;59:99-112. doi: 10.1097/IIO.0000000000000279
4. Linnau KF, Hallam DK, Lomoschitz FM, et al. Orbital apex injury: trauma at the junction between the face and the cranium. Eur J Radiol. 2003;48:5-16. doi: 10.1016/s0720-048x(03)00203-1
5. McClelland C, Manousakis G, Lee MS. Progressive external ophthalmoplegia. Curr Neurol Neurosci Rep. 2016;16:53. doi: 10.1007/s11910-016-0652-7
6. Bahn RS. Graves’ ophthalmopathy. N Engl J Med. 2010;362:726-738. doi: 10.1056/NEJMra0905750
7. Subetki I, Soewond P, Soebardi S, et al. Practical guidelines management of graves ophthalmopathy. Acta Med Indones. 2019;51:364-371.
8. Wijdicks EF, Klein CJ. Guillain-Barré syndrome. Mayo Clin Proc. 2017;92:467-479. doi: 10.1016/j.mayocp.2016.12.002
9. Beloor Suresh A, Asuncion RMD. Myasthenia Gravis. In: StatPearls [Internet]. StatPearls Publishing; 2021. Accessed April 26, 2021. www.ncbi.nlm.nih.gov/books/NBK559331/
10. Chatzistefanou KI, Kouris T, Iliakis E, et al. The ice pack test in the differential diagnosis of myasthenic diplopia. Ophthalmology. 2009;116:2236-2243. doi: 10.1016/j.ophtha.2009.04.039
11. Pascual-Prieto J, Narváez-Palazón C, Porta-Etessam J, et al. COVID-19 epidemic: should ophthalmologists be aware of oculomotor paresis? Arch Soc Esp Oftalmol. 2020;95:361-362. doi: 10.1016/j.oftal.2020.05.002
12. Collantes MEV, Espiritu AI, Sy MCC, et al. Neurological manifestations in COVID-19 infection: a systematic review and meta-analysis. Can J Neurol Sci. 2021;48:66-76. doi: 10.1017/cjn.2020.146
13. Raza HK, Chen H, Chansysouphanthong T, et al. The aetiologies of the unilateral oculomotor nerve palsy: a review of the literature. Somatosens Mot Res. 2018;35:229-239. doi :10.1080/08990220.2018.1547697
14. Keane J. Third nerve palsy: analysis of 1400 personally-examined inpatients. Can J Neurol Sci. 2010;37:662-670. doi: 10.1017/s0317167100010866
1. Fang C, Leavitt JA, Hodge DO, et al. Incidence and etiologies of acquired third nerve palsy using a population-based method. JAMA Ophthalmol. 2017;135:23-28. doi: 10.1001/jamaophthalmol.2016.4456
2. Bruce BB, Biousse V, Newman NJ. Third nerve palsies. Semin Neurol. 2007;27:257-268. doi: 10.1055/s-2007-979681
3. Margolin E, Freund P. A review of third nerve palsies. Int Ophthalmol Clin. 2019;59:99-112. doi: 10.1097/IIO.0000000000000279
4. Linnau KF, Hallam DK, Lomoschitz FM, et al. Orbital apex injury: trauma at the junction between the face and the cranium. Eur J Radiol. 2003;48:5-16. doi: 10.1016/s0720-048x(03)00203-1
5. McClelland C, Manousakis G, Lee MS. Progressive external ophthalmoplegia. Curr Neurol Neurosci Rep. 2016;16:53. doi: 10.1007/s11910-016-0652-7
6. Bahn RS. Graves’ ophthalmopathy. N Engl J Med. 2010;362:726-738. doi: 10.1056/NEJMra0905750
7. Subetki I, Soewond P, Soebardi S, et al. Practical guidelines management of graves ophthalmopathy. Acta Med Indones. 2019;51:364-371.
8. Wijdicks EF, Klein CJ. Guillain-Barré syndrome. Mayo Clin Proc. 2017;92:467-479. doi: 10.1016/j.mayocp.2016.12.002
9. Beloor Suresh A, Asuncion RMD. Myasthenia Gravis. In: StatPearls [Internet]. StatPearls Publishing; 2021. Accessed April 26, 2021. www.ncbi.nlm.nih.gov/books/NBK559331/
10. Chatzistefanou KI, Kouris T, Iliakis E, et al. The ice pack test in the differential diagnosis of myasthenic diplopia. Ophthalmology. 2009;116:2236-2243. doi: 10.1016/j.ophtha.2009.04.039
11. Pascual-Prieto J, Narváez-Palazón C, Porta-Etessam J, et al. COVID-19 epidemic: should ophthalmologists be aware of oculomotor paresis? Arch Soc Esp Oftalmol. 2020;95:361-362. doi: 10.1016/j.oftal.2020.05.002
12. Collantes MEV, Espiritu AI, Sy MCC, et al. Neurological manifestations in COVID-19 infection: a systematic review and meta-analysis. Can J Neurol Sci. 2021;48:66-76. doi: 10.1017/cjn.2020.146
13. Raza HK, Chen H, Chansysouphanthong T, et al. The aetiologies of the unilateral oculomotor nerve palsy: a review of the literature. Somatosens Mot Res. 2018;35:229-239. doi :10.1080/08990220.2018.1547697
14. Keane J. Third nerve palsy: analysis of 1400 personally-examined inpatients. Can J Neurol Sci. 2010;37:662-670. doi: 10.1017/s0317167100010866
COVID-19 in children: Weekly cases drop to 6-month low
Just 1 week after it looked like the COVID-19 situation in children might be taking another turn for the worse, the number of new pediatric cases dropped to its lowest level since October, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
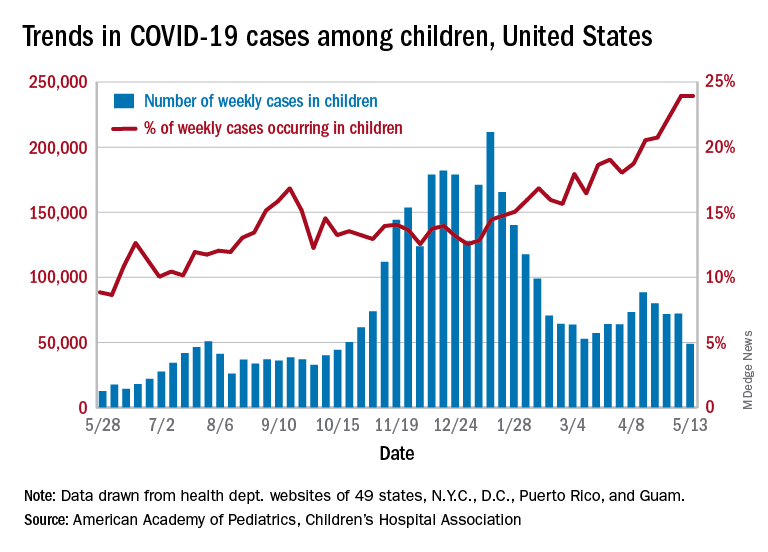
the AAP and CHA said in their weekly COVID-19 report. During the week of April 30 to May 6 – the same week Rhode Island reported a large backlog of cases and increased its total by 30% – the number of new cases went up slightly after 2 weeks of declines.
Other positive indicators come in the form of the proportion of cases occurring in children. The cumulative percentage of cases in children since the start of the pandemic remained at 14.0% for a second consecutive week, and the proportion of new cases in children held at 24.0% and did not increase for the first time in 6 weeks, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The total number of child COVID-19 cases reported in these jurisdictions is now up to 3.9 million, for a cumulative rate of 5,187 cases per 100,000 children in the United States. Among the states, total counts range from a low of 4,070 in Hawaii to 475,619 in California. Hawaii also has the lowest rate at 1,357 per 100,000 children, while the highest, 9,778 per 100,000, can be found in Rhode Island, the AAP and CHA said.
Deaths in children continue to accumulate at a relatively slow pace, with two more added during the week of May 7-13, bringing the total to 308 for the entire pandemic in 43 states, New York City, Puerto Rico, and Guam. Children’s share of the mortality burden is currently 0.06%, a figure that has not changed since mid-December, and the death rate for children with COVID-19 is 0.01%, according to the report.
Almost two-thirds (65%) of all deaths have occurred in just nine states – Arizona (31), California (21), Colorado (13), Georgia (10), Illinois (18), Maryland (10), Pennsylvania (10), Tennessee (10), and Texas (52) – and New York City (24), while eight states have not reported any deaths yet, the two groups said.
Just 1 week after it looked like the COVID-19 situation in children might be taking another turn for the worse, the number of new pediatric cases dropped to its lowest level since October, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
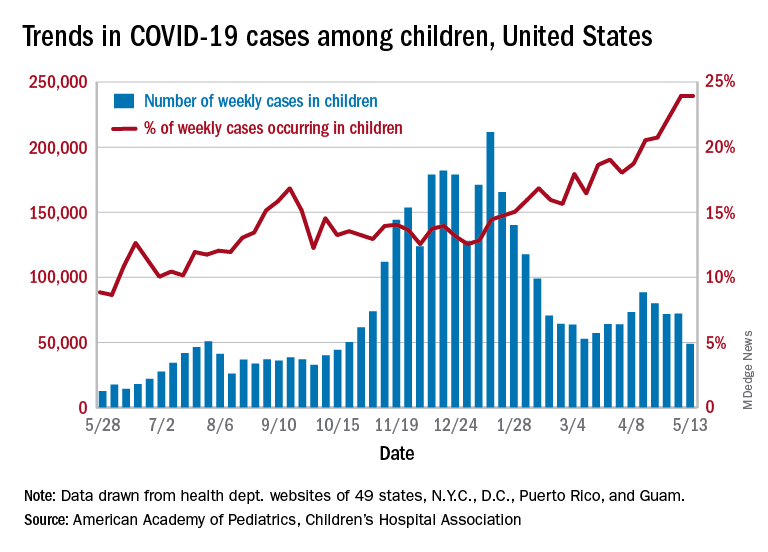
the AAP and CHA said in their weekly COVID-19 report. During the week of April 30 to May 6 – the same week Rhode Island reported a large backlog of cases and increased its total by 30% – the number of new cases went up slightly after 2 weeks of declines.
Other positive indicators come in the form of the proportion of cases occurring in children. The cumulative percentage of cases in children since the start of the pandemic remained at 14.0% for a second consecutive week, and the proportion of new cases in children held at 24.0% and did not increase for the first time in 6 weeks, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The total number of child COVID-19 cases reported in these jurisdictions is now up to 3.9 million, for a cumulative rate of 5,187 cases per 100,000 children in the United States. Among the states, total counts range from a low of 4,070 in Hawaii to 475,619 in California. Hawaii also has the lowest rate at 1,357 per 100,000 children, while the highest, 9,778 per 100,000, can be found in Rhode Island, the AAP and CHA said.
Deaths in children continue to accumulate at a relatively slow pace, with two more added during the week of May 7-13, bringing the total to 308 for the entire pandemic in 43 states, New York City, Puerto Rico, and Guam. Children’s share of the mortality burden is currently 0.06%, a figure that has not changed since mid-December, and the death rate for children with COVID-19 is 0.01%, according to the report.
Almost two-thirds (65%) of all deaths have occurred in just nine states – Arizona (31), California (21), Colorado (13), Georgia (10), Illinois (18), Maryland (10), Pennsylvania (10), Tennessee (10), and Texas (52) – and New York City (24), while eight states have not reported any deaths yet, the two groups said.
Just 1 week after it looked like the COVID-19 situation in children might be taking another turn for the worse, the number of new pediatric cases dropped to its lowest level since October, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
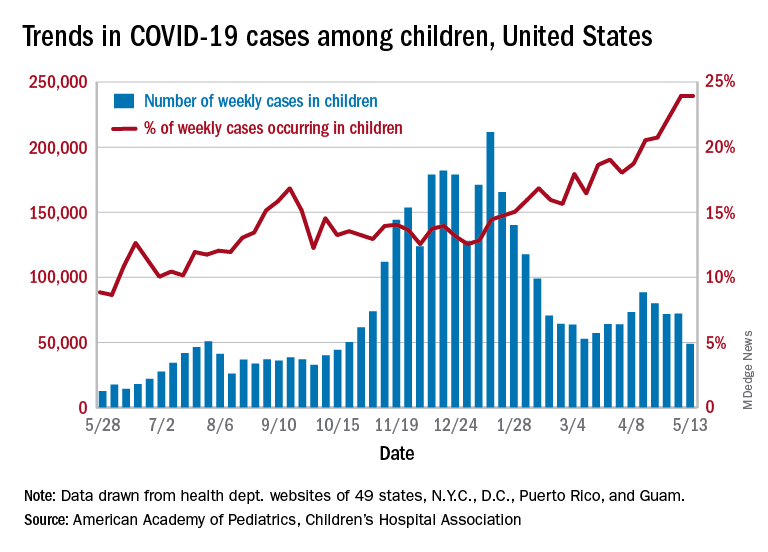
the AAP and CHA said in their weekly COVID-19 report. During the week of April 30 to May 6 – the same week Rhode Island reported a large backlog of cases and increased its total by 30% – the number of new cases went up slightly after 2 weeks of declines.
Other positive indicators come in the form of the proportion of cases occurring in children. The cumulative percentage of cases in children since the start of the pandemic remained at 14.0% for a second consecutive week, and the proportion of new cases in children held at 24.0% and did not increase for the first time in 6 weeks, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The total number of child COVID-19 cases reported in these jurisdictions is now up to 3.9 million, for a cumulative rate of 5,187 cases per 100,000 children in the United States. Among the states, total counts range from a low of 4,070 in Hawaii to 475,619 in California. Hawaii also has the lowest rate at 1,357 per 100,000 children, while the highest, 9,778 per 100,000, can be found in Rhode Island, the AAP and CHA said.
Deaths in children continue to accumulate at a relatively slow pace, with two more added during the week of May 7-13, bringing the total to 308 for the entire pandemic in 43 states, New York City, Puerto Rico, and Guam. Children’s share of the mortality burden is currently 0.06%, a figure that has not changed since mid-December, and the death rate for children with COVID-19 is 0.01%, according to the report.
Almost two-thirds (65%) of all deaths have occurred in just nine states – Arizona (31), California (21), Colorado (13), Georgia (10), Illinois (18), Maryland (10), Pennsylvania (10), Tennessee (10), and Texas (52) – and New York City (24), while eight states have not reported any deaths yet, the two groups said.
A guide to diagnosing and managing ascites in cirrhosis
Liver cirrhosis is implicated in 75% to 85% of ascites cases in the Western world, with heart failure or malignancy accounting for fewer cases.1 Among patients who have decompensated cirrhosis with ascites, annual mortality is 20%.2 Another study showed a 3-year survival rate after onset of ascites of only 56%.3 It is vital for primary care physicians (PCPs) to be alert for ascites not only in patients who have risk factors for chronic liver disease and cirrhosis—eg, a history of alcohol use disorder, chronic viral infections (hepatitis B and C), or metabolic syndrome—but also in patients with abnormal liver function tests and thrombocytopenia. In this review, we discuss the initial assessment of ascites and its long-term management, concentrating on the role of the PCP.
Pathophysiology: Vasodilation leads to a cascade
Splanchnic vasodilation is the main underlying event triggering a pathologic cascade that leads to the development of ascites.4 Initially portal hypertension in the setting of liver inflammation and fibrosis causes the release of inflammatory cytokines such as nitric oxide and carbon monoxide. This, in turn, causes the pathologic dilation of splanchnic circulation that decreases effective circulating volume. Activation of the sympathetic nervous system, vasopressin, and renin-angiotensin-aldosterone system (RAAS) then causes the proximal and distal tubules to increase renal absorption of sodium and water.5 The resulting volume overload further decreases the heart’s ability to maintain circulating volume, leading to increased activation of compensating symptoms. This vicious cycle eventually manifests as ascites.6
A complex interplay of cirrhosis-associated immune dysfunction (CAID), gut dysbiosis, and increased translocation of microorganisms into ascitic fluid is also an important aspect of the pathogenesis.7 CAID (FIGURE 1)7,8 is an immunodeficient state due to cirrhosis with reduced phagocytic activity by neutrophils and macrophages, T- and B-cell hypoproliferation, and reduced cytotoxicity of natural killer cells. In parallel, there is increased production of inflammatory cytokines due to the effects of damage-associated molecular patterns (DAMPs) from hepatocytes and pathogen-associated molecular patterns (PAMPs) from the gut microbiota on the immune system, which leads to many of the manifestations of decompensated cirrhosis including ascites.8
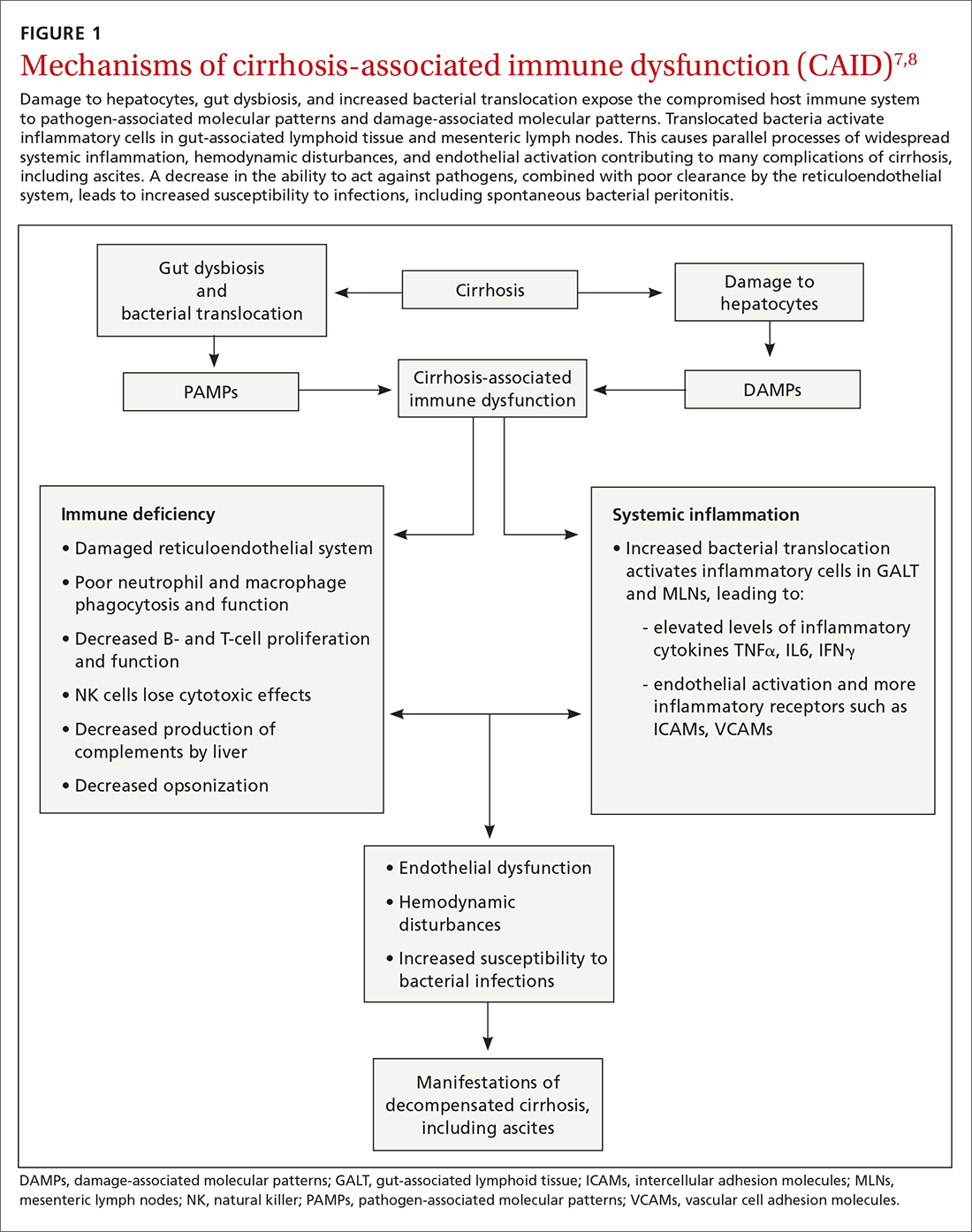
Key in on these elementsof the history and exam
Each step of the basic work-up for ascites provides opportunities to refine or redirect the diagnostic inquiry (TABLE).
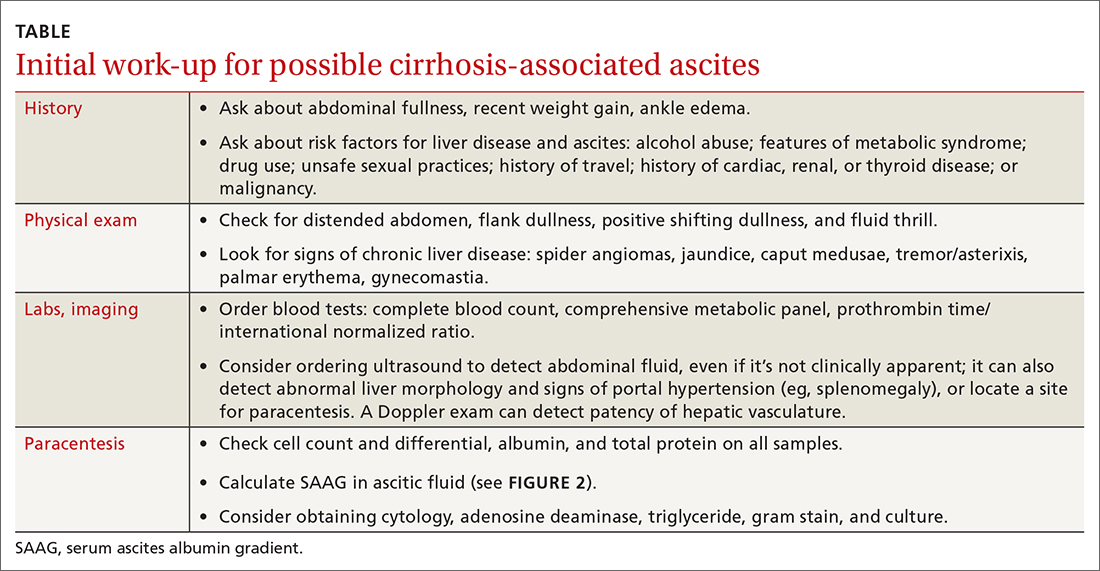
History
Generally, patients with ascites present with weight gain and symptoms of abdominal distension, such as early satiety, nausea, and vomiting. Besides cirrhosis, rule out other causes of ascites, as treatment differs based on the cause.9 Also ask about histories of cancer and cardiac, renal, or thyroid disease.10
Patients with ascites in the setting of liver disease usually are asymptomatic in its early stages. Common complaints are vague abdominal pain, generalized weakness, malaise, and fatigue.11 Ask patients about risk factors for liver disease such as obesity, diabetes, hypertension, alcohol use, unsafe sexual practices, recent travel, and needle sharing or drug use. Due to a strong association between obstructive sleep apnea and fatty liver disease, consider screening at-risk patients for sleep apnea.12
Physical exam
When there are risk factors for liver disease, examine the patient for stigmata of cirrhosis and ascites. Signs of liver disease, aside from ascites, may include spider angiomas on the upper trunk (33% of cirrhosis patients),13 gynecomastia (44% of cirrhosis patients),14 palmar erythema, jaundice, asterixis, and abdominal wall collaterals including caput medusa.15
Continue to: We suggest a systematic...
We suggest a systematic and targeted approach to using various physical exam maneuvers described in the literature. If the patient has a full/distended abdomen, percuss the flanks. If increased dullness at the flanks is detected, check for shifting dullness, which indicates at least 1500 mL of fluid in the abdomen.16 Keep in mind that a 10% chance of ascites exists even if shifting dullness is absent.17 Maneuvers such as the puddle sign and fluid thrill are less accurate than shifting dullness, which has 83% sensitivity and 56% specificity in detecting ascites.17 Patients with cirrhosis also have a high likelihood of complications from ascites such as inguinal, umbilical, and other hernias.
Diagnostic work-up includes blood tests and ultrasound
Blood tests. The initial work-up for ascites should include complete blood count, complete metabolic panel, and prothrombin time/international normalized ratio.18
Abdominal ultrasound is recommended as the first-line imaging test.19 Aside from detecting ascites, it can give an estimate of the volume of ascites and indicate whether it is amenable to paracentesis. A vascular exam added to the standard ultrasound can detect radiologic evidence of portal hypertension such as splenomegaly, portosystemic collaterals, splenorenal shunt, patency of the paraumbilical vein, and portal vein diameter. Patients with established cirrhosis also require abdominal ultrasound every 6 months to screen for hepatocellular cancer.20
Abdominal paracentesis is the cornerstone of ascites evaluation.21 It is indicated for every patient with new-onset ascites or for any patient with known ascites and clinical deterioration. Ascitic fluid analysis can be used to easily differentiate portal hypertension from other causes of ascites. It can also be used to rule out bacterial peritonitis. The recommended sites for evaluation are in the left lower quadrant, 3 cm cranially and 3 cm medially from the anterior superior iliac spine.22 A large cohort study showed that abdominal ultrasound-guided paracentesis reduced bleeding complications by 68% following the procedure and is strongly recommended (if available).23 Generally, paracentesis is a relatively safe procedure with a low risk of complications such as abdominal wall hematoma (1%), hemoperitoneum (< 0.1%), bowel perforation (< 0.1%), and infection (< 0.1%).24
Assess all ascitic fluid samples for color, consistency, cell count and differential, albumin, and total protein. These tests are usually sufficient to provide evidence regarding the cause of ascites. If there is suspicion of infection, order a gram stain and culture (80% sensitivity for detecting an infection if obtained prior to initiation of antibiotics)25 and glucose, lactate dehydrogenase (useful to differentiate primary from secondary bacterial peritonitis),26 and amylase tests. Other tests such as cytology, acid-fast bacilli smear and culture, and triglyceride level should only be obtained if specific conditions are suspected based on high pretest probabilities.
Continue to: Calculating serum ascites albumin gradient...
Calculating serum ascites albumin gradient (SAAG) is recommended as it has been shown to better characterize ascitic fluid than total protein-based tests.27 SAAG is calculated by subtracting the level of ascitic fluid albumin from serum albumin level (SAAG = serum albumin – ascitic fluid albumin). A SAAG ≥ 1.1 g/dL is consistent with portal hypertension,28 with approximately 97% accuracy.
After calculating SAAG, look at total protein levels in ascitic fluid. Total protein concentration ≥ 2.5 g/dL with SAAG ≥ 1.1 g/dL has a 78.3% diagnostic accuracy in determining heart failure as the cause of ascites, with a sensitivity of 53.3% and specificity of 86.7%.28 On the other hand, a value of total protein < 2.5 g/dL indicates cirrhosis, liver failure, or acute hepatitis as the cause of fluid build-up.29 Stepwise evaluation of SAAG and total protein and how they can point toward the most likely cause of ascites is presented in FIGURE 2.27-29
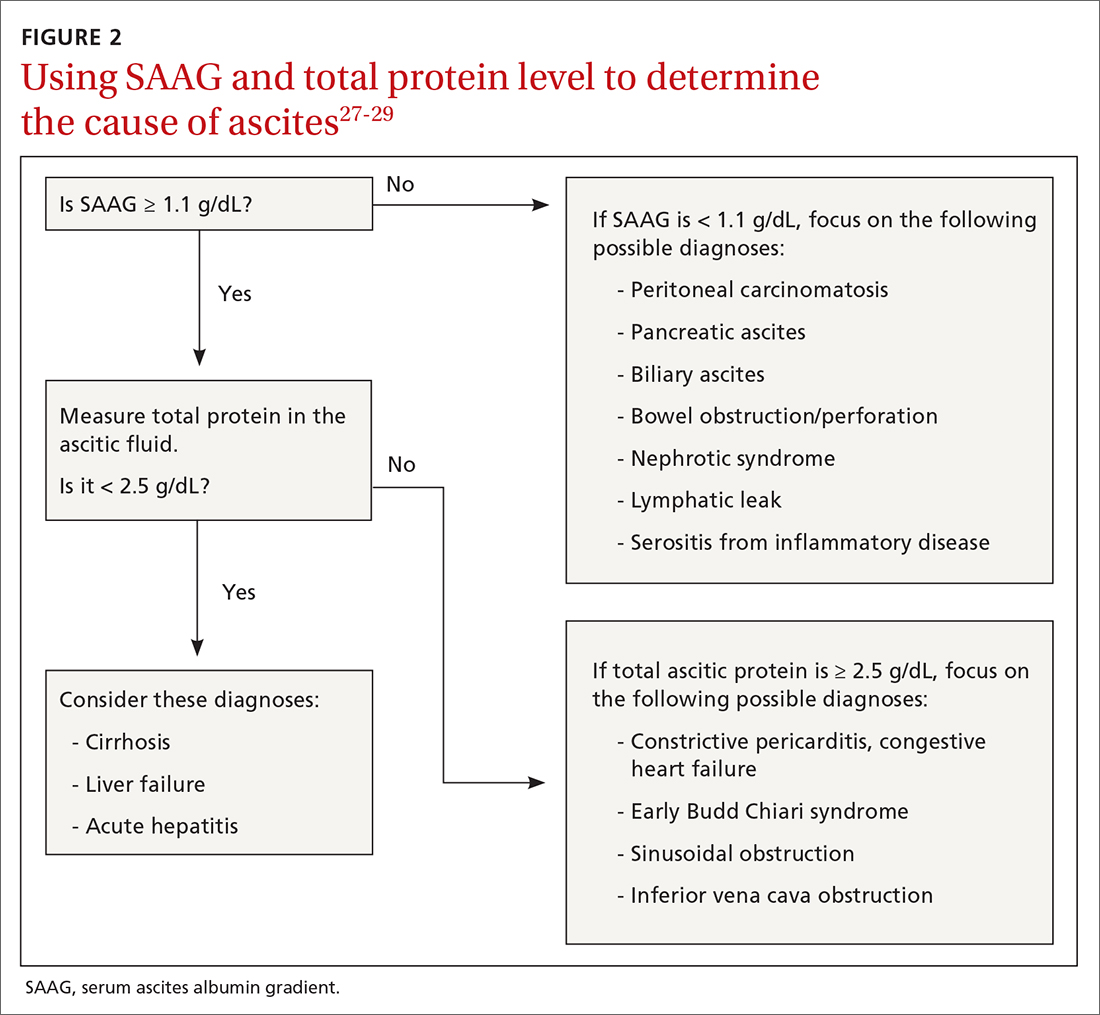
Management
Noninvasive measures
Sodium restriction. The aim of treatment for uncomplicated clinically apparent ascites is sodium restriction and removal of fluid from the body. Dietary salt restriction is complicated, and care should be taken to properly educate patients. Salt restriction advised in the literature has shifted from a strict measure of < 2 g/d30 to more moderate strategies (described below).18
The 2 main reasons for this easing of restriction are issues with patient compliance and concerns about adverse effects with aggressive salt-restricted diets. One study assessing patient compliance with a salt-restricted diet found that more than two-thirds of the patients were noncompliant,31 and 65% of the patients incorrectly assumed they were following the plan, which suggests poor dietary education.31 Of the group that was compliant, 20% actually decreased their caloric intake, which can be detrimental in liver disease.31 Concerns have been raised that aggressive salt restriction along with diuretic use can lead to diuretic-induced hyponatremia and renal failure.32 Current European Association for the Study of the Liver (EASL) guidelines recommend salt restriction to a more moderate degree (80-120 mmol/d of sodium). This is equivalent to 4.9-6.9 g of salt (1 tablespoon is roughly equivalent to 6 g or 104 mmol of sodium).18
Diuretics. Initiation and dosage of diuretic therapy is a matter of some controversy. Historically, simultaneous administration of a loop diuretic and mineralocorticoid receptor blocker were recommended: 40 mg furosemide and 100 mg spironolactone, keeping the ratio constant with any dosage increases. This was based on a randomized controlled trial (RCT) showing that the combined diuretic therapy effectively mobilized ascites in a shorter period of time and with less frequent adverse effects (eg, hyperkalemia) compared with initial monotherapy.33
Continue to: On the other hand...
On the other hand, another study with more stable patients and relatively normal renal function showed that starting with a mineralocorticoid receptor blocker alone with sequential dose increments had equivalent benefit with no increase in adverse effects.34 Since the patient population in this study was more in line with what a PCP might encounter, we recommend following this guideline initially and keeping a close watch on serum electrolytes.
Usual maximum doses are spironolactone 400 mg/d and furosemide 160 mg/d.21,35 Adequate weight loss for patients with diffuse edema is at least 1 kg/d, per EASL guidelines.36,37 However, this might not be practical in outpatient settings, and a more conservative target of 0.5 kg/d may be used for patients without significant edema.37
It is vital to get accurate daily weights and avoid excessive diuretic use, as it has been associated with intravascular volume depletion and acute kidney injury (25%), hyponatremia (28%),38,39 and hepatic encephalopathy (30%).40 Therefore, patients with acute kidney injury, hyponatremia, acute variceal hemorrhage, or infection should also have their diuretics held until their creatinine returns to baseline.
Invasive measures
Large-volume paracentesis. Patients with extensive and tense ascites should be treated initially with large-volume paracentesis, as this has been shown to predictably remove fluid more effectively than diuretics.38 This should be accompanied by albumin administration, 8 g for every liter of ascitic fluid removed if the total amount exceeds 5 L.41 Following large-volume paracentesis, manage patients with the standard salt restriction and diuretic regimen.38 Serial large-volume paracentesis is a temporary measure reserved for a select group of patients who are intolerant to diuretics and are not candidates for a shunt.
Transjugular intrahepatic portosystemic shunt (TIPS) is another option to control refractory ascites, but its benefit should be weighed against complications such as hepatic encephalopathy. An RCT found that TIPS with covered stents improved survival in patients with cirrhosis compared with regular large-volume paracentesis.42 Patients should be referred to hepatologists to make a determination about TIPS placement. Widely accepted contraindications for the placement of TIPS are decompensated cirrhosis (Child-Pugh > 11, model for end-stage liver disease [MELD] > 18), renal failure (serum creatinine > 3 mg/dL), heart failure, porto-pulmonary hypertension, and uncontrolled sepsis.43 Recurrent or persistent hepatic encephalopathy (West Haven grade ≥ 2) is also a contraindication. The West Haven scale is widely used to measure severity of hepatic encephalopathy, grading it from 1 to 4, with 1 being mild encephalopathy characterized by lack of awareness and shorter attention span, and 4 indicating unresponsiveness or coma.44
Continue to: How to manage refractory ascites
How to manage refractory ascites
Fragile patients are those with refractory ascites that is either unresponsive to standard salt restriction and maximum-dose diuretic therapy or that results in a re-accumulation of ascitic fluid soon after paracentesis.45 Specialist care is required to improve survival and quality of life for these patients. They should be referred to a hepatologist for consideration of TIPS placement or liver transplantation.18
Long-term use of albumin was tested in 2 trials for management of decompensated cirrhosis with ascites, yielding conflicting results. The ANSWER trial from Italy showed benefit with this treatment for prolonged survival.46 The other trial, from Spain, showed no benefit from albumin and midodrine administration for survival or for improving complications of cirrhosis.47 The contradictory results are likely due to heterogeneous populations in the 2 trials and differences in dose and duration of albumin administration. Hence, no clear recommendations can be made based on the available data; further research is needed.
Getting a handle on bacterial peritonitis
Bacterial peritonitis can be divided into spontaneous bacterial peritonitis (SBP) and secondary bacterial peritonitis. SBP is a common complication in patients with cirrhosis and occurs in around 16% of hospitalized patients, based on 1 study.48 SBP is defined as a polymorphonuclear leukocyte count ≥ 250 cells/μL in the absence of a surgically treatable source of infection.49 It is believed to be caused by bacterial translocation and is treated empirically with a third-generation cephalosporin. This treatment has been shown to be effective in 85% of patients.50
Patients with SBP are at a higher risk for renal impairment, likely resulting from increased cytokine production and decreased circulatory volume.51 Concomitant albumin administration has been shown to significantly improve outcomes and to reduce rates of hepatorenal syndrome in patients with serum creatinine > 1 mg/dL, blood urea nitrogen > 30 mg/dL, or total bilirubin > 4 mg/dL.52 The recommended amount of albumin is 1.5 g/kg given within 6 hours of SBP detection and repeat administration of 1 g/kg on Day 3.52
Guidelines from the American Association for the Study of Liver Diseases and from EASL recommend the long-term use of daily norfloxacin or trimethoprim-sulfamethoxazole as secondary prophylaxis in patients who have survived an episode of SBP.18
Continue to: Avoid these medications
Avoid these medications
Commonly used medications that should be avoided in patients with cirrhosis and ascites are angiotensin-converting enzyme inhibitors and angiotensin receptor blockers. These agents block the action of angiotensin, which is a vital vasoconstrictor, and thereby cause a drop in blood pressure. This has independently been associated with poor outcomes in patients with cirrhosis.37
Nonsteroidal anti-inflammatory drugs (NSAIDs) are also relatively contraindicated in cirrhosis, as they can affect kidney function, induce azotemia, and reduce kidney sodium excretion. NSAIDs induce vasoconstriction of afferent arterioles in the kidneys, leading to a decreased glomerular filtration rate, further activating RAAS and sympathetic drive. This leads to increased sodium and water retention and worsening ascites.54
Improve outcomes by circling in a hepatologist
PCPs can play a vital role in the prevention, treatment, surveillance, and home care of patients with cirrhosis who are at risk for ascites.55 Referral of patients with hepatic impairment manifesting as unexplained abnormal liver function tests, new-onset ascites, and/or image findings consistent with cirrhosis to a hepatologist at least once is recommended. Such referrals have been shown to be associated with a better overall outcome.56 Patients with known cirrhosis leading to ascites can generally be managed at home with the assistance of specialists and specialized nurses.35
In a study from the University of Michigan, 69% of patients with cirrhosis had at least 1 nonelective readmission; 14% of patients were readmitted within 1 week, and 37% within 1 month.57 These are staggering statistics that highlight the gaps in care coordination and management of patients with cirrhosis in the outpatient setting. PCPs can play a vital role in bridging this gap.
A promising framework is suggested by a study from Italy by Morando et al in 2013.58 The researchers assessed a specialized health care model for cirrhotic patients and showed significant improvement in health care cost, readmission rate, and overall mortality when compared with the existing model of outpatient care.58
Continue to: This was not a blinded study...
This was not a blinded study and there were concerns raised by the scientific community about its design. Because it was conducted in Italy, the results might not be fully applicable to the United States health care setting. However, it did show that better coordination of care leads to significantly better patient outcomes and reduces health care expenditure. Therefore, a more complete understanding of the disease process and latest literature by PCPs, communication with specialists, and comprehensive coordination of care by all parties involved is vital for the management of this patient population.
CORRESPONDENCE
Muhammad Salman Faisal, MD, Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, OH 44195; [email protected]
1. Runyon BA, Montano AA, Akriviadis EA, et al. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med. 1992;117:215-220.
2. D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-231.
3. Gordon FD. Ascites. Clin Liver Dis. 2012;16:285-299.
4. Schrier RW, Arroyo V, Bernardi M, et al. Peripheral arterial vasodilation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology. 1988;8:1151-1157.
5. Arroyo V, Terra C, Gines P. Advances in the pathogenesis and treatment of type-1 and type-2 hepatorenal syndrome. J Hepatol. 2007;46:935-946.
6. Bernardi M, Moreau R, Angeli P, et al. Mechanisms of decompensation and organ failure in cirrhosis: from peripheral arterial vasodilation to systemic inflammation hypothesis. J Hepatol. 2015;63:1272-1284.
7. Jalan R, Fernandez J, Wiest R, et al. Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol. 2014;60:1310-1324.
8. Albillos A, Lario M, Álvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol. 2014;61:1385-1396.
9. Oey RC, van Buuren HR, de Man RA. The diagnostic work-up in patients with ascites: current guidelines and future prospects. Neth J Med. 2016;74:330-335.
10. de Kerguenec C, Hillaire S, Molinié V, et al. Hepatic manifestations of hemophagocytic syndrome: a study of 30 cases. Am J Gastroenterol. 2001;96:852-857.
11. Milić S, Lulić D, Štimac D. Non-alcoholic fatty liver disease and obesity: biochemical, metabolic and clinical presentations. World J Gastroenterol. 2014;20:9330-9337.
12. Aron-Wisnewsky J, Clement K, Pépin J-L. Nonalcoholic fatty liver disease and obstructive sleep apnea. Metabolism. 2016;65:1124-1135.
13. Li CP, Lee FY, Hwang SJ, et al. Spider angiomas in patients with liver cirrhosis: role of alcoholism and impaired liver function. Scand J Gastroenterol. 1999;34:520-523.
14. Cavanaugh J. Gynecomastia and cirrhosis of the liver. Arch Intern Med. 1990;150:563-565.
15. Karnath B. Stigmata of chronic liver disease. Hosp Phys. 2003;7:14-16,28.
16. Schipper HG, Godfried MH. [Physical diagnosis--ascites]. Ned Tijdschr Geneeskd. 2001;145:260-264.
17. Cattau EL, Jr., Benjamin SB, Knuff TE, et al. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247:1164-1166.
18. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69:406-460.
19. Runyon BA, AASLD Practice Guidelines Committee. Management of adult patients with ascites due to cirrhosis: an update. Hepatology 2009;49:2087-2107.
20. EASL Clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236.
21. Runyon BA. Care of patients with ascites. New Engl J Med. 1994;330:337-342.
22. Sakai H, Sheer TA, Mendler MH, et al. Choosing the location for non-image guided abdominal paracentesis. Liver Int. 2005;25:984-986.
23. Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis. Chest. 2013;143:532-538.
24. Ennis J, Schultz G, Perera P, et al. Ultrasound for detection of ascites and for guidance of the paracentesis procedure: technique and review of the literature. Int J Clin Med. 2014;5:1277-1293.
25. Runyon BA, Canawati HN, Akriviadis EA. Optimization of ascitic fluid culture technique. Gastroenterology. 1988;95:1351-1355.
26. Akriviadis EA, Runyon BA. Utility of an algorithm in differentiating spontaneous from secondary bacterial peritonitis. Gastroenterology 1990;98:127-133.
27. Hoefs JC. Serum protein concentration and portal pressure determine the ascitic fluid protein concentration in patients with chronic liver disease. J Lab Clin Med. 1983;102:260-273.
28. Farias AQ, Silvestre OM, Garcia-Tsao G, et al. Serum B-type natriuretic peptide in the initial workup of patients with new onset ascites: a diagnostic accuracy study. Hepatology. 2014;59:1043-1051.
29. Gupta R, Misra SP, Dwivedi M, et al. Diagnosing ascites: value of ascitic fluid total protein, albumin, cholesterol, their ratios, serum-ascites albumin and cholesterol gradient. J Gastroenterol Hepatol. 1995;10:295-299.
30. Runyon BA. Management of adult patients with ascites due to cirrhosis: update 2012. AASLD Practice Guideline. Accessed April 28, 2021. www.aasld.org/sites/default/files/2019-06/AASLDPracticeGuidelineAsciteDuetoCirrhosisUpdate2012Edition4_.pdf
31. Morando F, Rosi S, Gola E, et al. Adherence to a moderate sodium restriction diet in outpatients with cirrhosis and ascites: a real-life cross-sectional study. Liver Int. 2015;35:1508-1515.
32. Bernardi M, Laffi G, Salvagnini M, et al. Efficacy and safety of the stepped care medical treatment of ascites in liver cirrhosis: a randomized controlled clinical trial comparing two diets with different sodium content. Liver. 1993;13:156-162.
33. Angeli P, Fasolato S, Mazza E, et al. Combined versus sequential diuretic treatment of ascites in non-azotaemic patients with cirrhosis: results of an open randomised clinical trial. Gut. 2010;59:98-104.
34. Santos J, Planas R, Pardo A, et al. Spironolactone alone or in combination with furosemide in the treatment of moderate ascites in nonazotemic cirrhosis. A randomized comparative study of efficacy and safety. J Hepatol. 2003;39:187–192.
35. Grattagliano I, Ubaldi E, Bonfrate L, et al. Management of liver cirrhosis between primary care and specialists. World J Gastroenterol. 2011;17:2273-2282.
36. Pockros PJ, Reynolds TB. Rapid diuresis in patients with ascites from chronic liver disease: the importance of peripheral edema. Gastroenterology. 1986;90:1827-1833.
37. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397-417.
38. Gines P, Arroyo V, Quintero E, et al. Comparison of paracentesis and diuretics in the treatment of cirrhotics with tense ascites. Results of a randomized study. Gastroenterology. 1987;93:234-241.
39. Salerno F, Badalamenti S, Incerti P, et al. Repeated paracentesis and i.v. albumin infusion to treat ‘tense’ ascites in cirrhotic patients. A safe alternative therapy. J Hepatol. 1987;5:102-108.
40. Sola R, Vila MC, Andreu M, et al. Total paracentesis with dextran 40 vs diuretics in the treatment of ascites in cirrhosis: a randomized controlled study. J Hepatol. 1994;20:282-288.
41. Bernardi M, Caraceni P, Navickis RJ, et al. Albumin infusion in patients undergoing large-volume paracentesis: a meta-analysis of randomized trials. Hepatology. 2012;55:1172-1181.
42. Bureau C, Thabut D, Oberti F, et al. Transjugular intrahepatic portosystemic shunts with covered stents increase transplant-free survival of patients with cirrhosis and recurrent ascites. Gastroenterology. 2017;152:157-163.
43. Fagiuoli S, Bruno R, Debernardi Venon W, et al. Consensus conference on TIPS management: techniques, indications, contraindications. Dig Liver Dis. 2017;49:121-137.
44. Ferenci P, Lockwood A, Mullen K, et al. Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716-721.
45. Salerno F, Guevara M, Bernardi M, et al. Refractory ascites: pathogenesis, definition and therapy of a severe complication in patients with cirrhosis. Liver Int. 2010;30:937-947.
46. Caraceni P, Riggio O, Angeli P, et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial. Lancet. 2018;391:2417-2429.
47. Solà E, Solé C, Simón-Talero M, et al. Midodrine and albumin for prevention of complications in patients with cirrhosis awaiting liver transplantation. A randomized placebo-controlled trial. J Hepatol. 2018;69:1250-1259.
48. Fasolato S, Angeli P, Dallagnese L, et al. Renal failure and bacterial infections in patients with cirrhosis: epidemiology and clinical features. Hepatology. 2007;45:223-229.
49. Hoefs JC, Canawati HN, Sapico FL, et al. Spontaneous bacterial peritonitis. Hepatology. 2007;2:399-407.
50. Felisart J, Rimola A, Arroyo V, et al. Cefotaxime is more effective than is ampicillin-tobramycin in cirrhotics with severe infections. Hepatology. 1985;5:457-462.
51. Lenz K, Kapral C, Gegenhuber A, et al. Systemic, renal, and hepatic hemodynamic derangement in cirrhotic patients with spontaneous bacterial peritonitis. Hepatology. 2004;39:865-866.
52. Sigal SH, Stanca CM, Fernandez J, et al. Restricted use of albumin for spontaneous bacterial peritonitis. Gut. 2007;56:597-599.
53. Fernández J, Navasa M, Planas R, et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology. 2007;133:818-824.
54. Boyer TD, Zia P, Reynolds TB. Effect of indomethacin and prostaglandin A1 on renal function and plasma renin activity in alcoholic liver disease. Gastroenterology. 1979;77:215-222.
55. Grattagliano I, Ubaldi E, Portincasa P, et al. Liver disease: early signs you may be missing. J Fam Pract. 2009;58:514-521.
56. Bini EJ, Weinshel EH, Generoso R, et al. Impact of gastroenterology consultation on the outcomes of patients admitted to the hospital with decompensated cirrhosis. Hepatology. 2001;34:1089-1095.
57. Volk ML, Tocco RS, Bazick J, et al. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107:247-252.
58. Morando F, Maresio G, Piano S, et al. How to improve care in outpatients with cirrhosis and ascites: a new model of care coordination by consultant hepatologists. J Hepatol. 2013;59:257-264.
Liver cirrhosis is implicated in 75% to 85% of ascites cases in the Western world, with heart failure or malignancy accounting for fewer cases.1 Among patients who have decompensated cirrhosis with ascites, annual mortality is 20%.2 Another study showed a 3-year survival rate after onset of ascites of only 56%.3 It is vital for primary care physicians (PCPs) to be alert for ascites not only in patients who have risk factors for chronic liver disease and cirrhosis—eg, a history of alcohol use disorder, chronic viral infections (hepatitis B and C), or metabolic syndrome—but also in patients with abnormal liver function tests and thrombocytopenia. In this review, we discuss the initial assessment of ascites and its long-term management, concentrating on the role of the PCP.
Pathophysiology: Vasodilation leads to a cascade
Splanchnic vasodilation is the main underlying event triggering a pathologic cascade that leads to the development of ascites.4 Initially portal hypertension in the setting of liver inflammation and fibrosis causes the release of inflammatory cytokines such as nitric oxide and carbon monoxide. This, in turn, causes the pathologic dilation of splanchnic circulation that decreases effective circulating volume. Activation of the sympathetic nervous system, vasopressin, and renin-angiotensin-aldosterone system (RAAS) then causes the proximal and distal tubules to increase renal absorption of sodium and water.5 The resulting volume overload further decreases the heart’s ability to maintain circulating volume, leading to increased activation of compensating symptoms. This vicious cycle eventually manifests as ascites.6
A complex interplay of cirrhosis-associated immune dysfunction (CAID), gut dysbiosis, and increased translocation of microorganisms into ascitic fluid is also an important aspect of the pathogenesis.7 CAID (FIGURE 1)7,8 is an immunodeficient state due to cirrhosis with reduced phagocytic activity by neutrophils and macrophages, T- and B-cell hypoproliferation, and reduced cytotoxicity of natural killer cells. In parallel, there is increased production of inflammatory cytokines due to the effects of damage-associated molecular patterns (DAMPs) from hepatocytes and pathogen-associated molecular patterns (PAMPs) from the gut microbiota on the immune system, which leads to many of the manifestations of decompensated cirrhosis including ascites.8
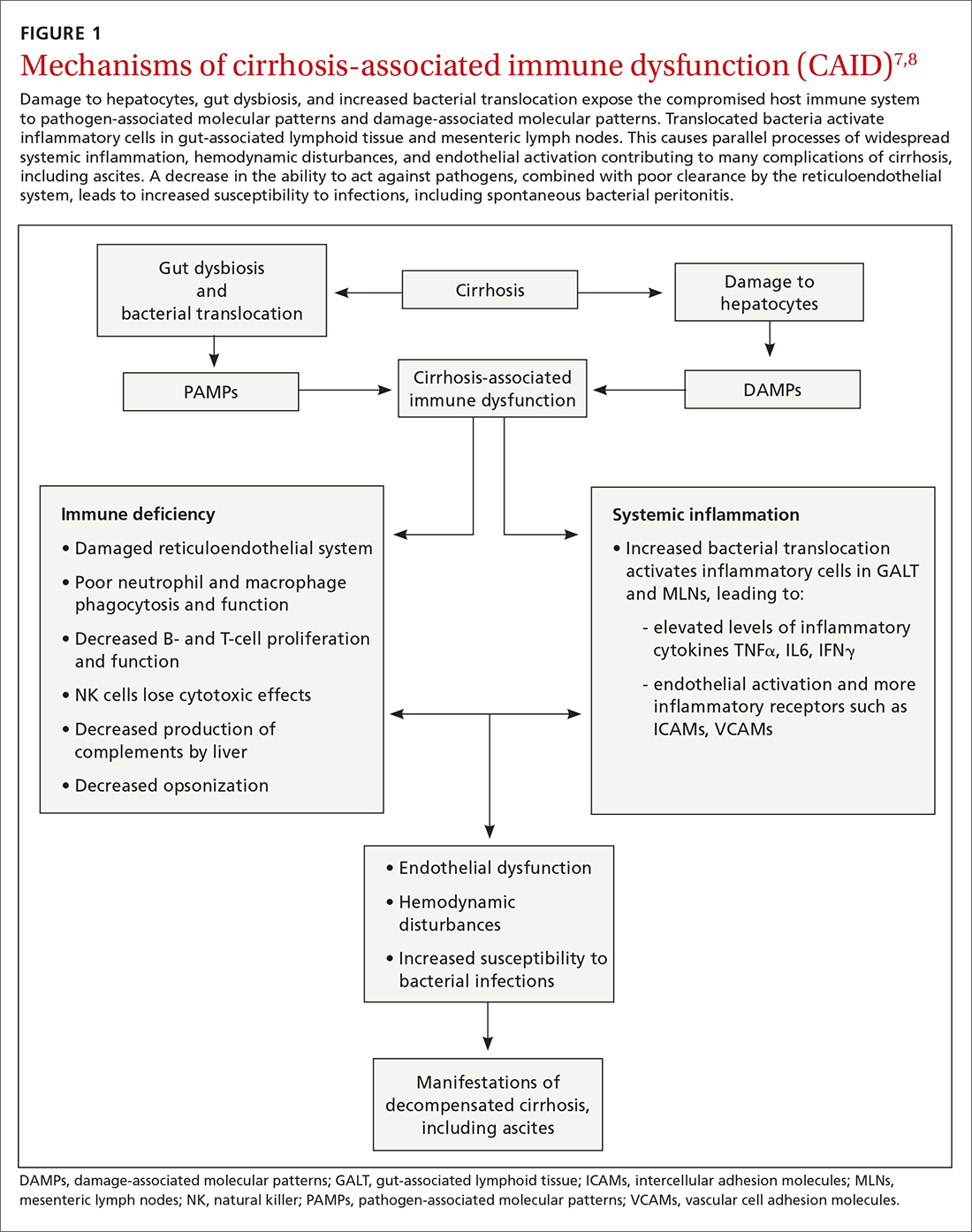
Key in on these elementsof the history and exam
Each step of the basic work-up for ascites provides opportunities to refine or redirect the diagnostic inquiry (TABLE).
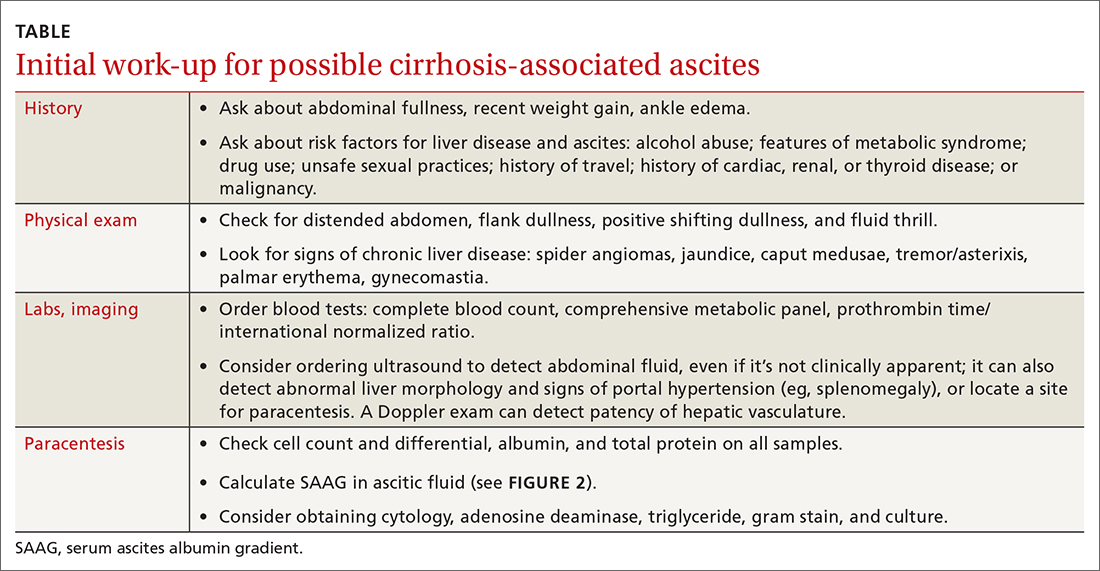
History
Generally, patients with ascites present with weight gain and symptoms of abdominal distension, such as early satiety, nausea, and vomiting. Besides cirrhosis, rule out other causes of ascites, as treatment differs based on the cause.9 Also ask about histories of cancer and cardiac, renal, or thyroid disease.10
Patients with ascites in the setting of liver disease usually are asymptomatic in its early stages. Common complaints are vague abdominal pain, generalized weakness, malaise, and fatigue.11 Ask patients about risk factors for liver disease such as obesity, diabetes, hypertension, alcohol use, unsafe sexual practices, recent travel, and needle sharing or drug use. Due to a strong association between obstructive sleep apnea and fatty liver disease, consider screening at-risk patients for sleep apnea.12
Physical exam
When there are risk factors for liver disease, examine the patient for stigmata of cirrhosis and ascites. Signs of liver disease, aside from ascites, may include spider angiomas on the upper trunk (33% of cirrhosis patients),13 gynecomastia (44% of cirrhosis patients),14 palmar erythema, jaundice, asterixis, and abdominal wall collaterals including caput medusa.15
Continue to: We suggest a systematic...
We suggest a systematic and targeted approach to using various physical exam maneuvers described in the literature. If the patient has a full/distended abdomen, percuss the flanks. If increased dullness at the flanks is detected, check for shifting dullness, which indicates at least 1500 mL of fluid in the abdomen.16 Keep in mind that a 10% chance of ascites exists even if shifting dullness is absent.17 Maneuvers such as the puddle sign and fluid thrill are less accurate than shifting dullness, which has 83% sensitivity and 56% specificity in detecting ascites.17 Patients with cirrhosis also have a high likelihood of complications from ascites such as inguinal, umbilical, and other hernias.
Diagnostic work-up includes blood tests and ultrasound
Blood tests. The initial work-up for ascites should include complete blood count, complete metabolic panel, and prothrombin time/international normalized ratio.18
Abdominal ultrasound is recommended as the first-line imaging test.19 Aside from detecting ascites, it can give an estimate of the volume of ascites and indicate whether it is amenable to paracentesis. A vascular exam added to the standard ultrasound can detect radiologic evidence of portal hypertension such as splenomegaly, portosystemic collaterals, splenorenal shunt, patency of the paraumbilical vein, and portal vein diameter. Patients with established cirrhosis also require abdominal ultrasound every 6 months to screen for hepatocellular cancer.20
Abdominal paracentesis is the cornerstone of ascites evaluation.21 It is indicated for every patient with new-onset ascites or for any patient with known ascites and clinical deterioration. Ascitic fluid analysis can be used to easily differentiate portal hypertension from other causes of ascites. It can also be used to rule out bacterial peritonitis. The recommended sites for evaluation are in the left lower quadrant, 3 cm cranially and 3 cm medially from the anterior superior iliac spine.22 A large cohort study showed that abdominal ultrasound-guided paracentesis reduced bleeding complications by 68% following the procedure and is strongly recommended (if available).23 Generally, paracentesis is a relatively safe procedure with a low risk of complications such as abdominal wall hematoma (1%), hemoperitoneum (< 0.1%), bowel perforation (< 0.1%), and infection (< 0.1%).24
Assess all ascitic fluid samples for color, consistency, cell count and differential, albumin, and total protein. These tests are usually sufficient to provide evidence regarding the cause of ascites. If there is suspicion of infection, order a gram stain and culture (80% sensitivity for detecting an infection if obtained prior to initiation of antibiotics)25 and glucose, lactate dehydrogenase (useful to differentiate primary from secondary bacterial peritonitis),26 and amylase tests. Other tests such as cytology, acid-fast bacilli smear and culture, and triglyceride level should only be obtained if specific conditions are suspected based on high pretest probabilities.
Continue to: Calculating serum ascites albumin gradient...
Calculating serum ascites albumin gradient (SAAG) is recommended as it has been shown to better characterize ascitic fluid than total protein-based tests.27 SAAG is calculated by subtracting the level of ascitic fluid albumin from serum albumin level (SAAG = serum albumin – ascitic fluid albumin). A SAAG ≥ 1.1 g/dL is consistent with portal hypertension,28 with approximately 97% accuracy.
After calculating SAAG, look at total protein levels in ascitic fluid. Total protein concentration ≥ 2.5 g/dL with SAAG ≥ 1.1 g/dL has a 78.3% diagnostic accuracy in determining heart failure as the cause of ascites, with a sensitivity of 53.3% and specificity of 86.7%.28 On the other hand, a value of total protein < 2.5 g/dL indicates cirrhosis, liver failure, or acute hepatitis as the cause of fluid build-up.29 Stepwise evaluation of SAAG and total protein and how they can point toward the most likely cause of ascites is presented in FIGURE 2.27-29
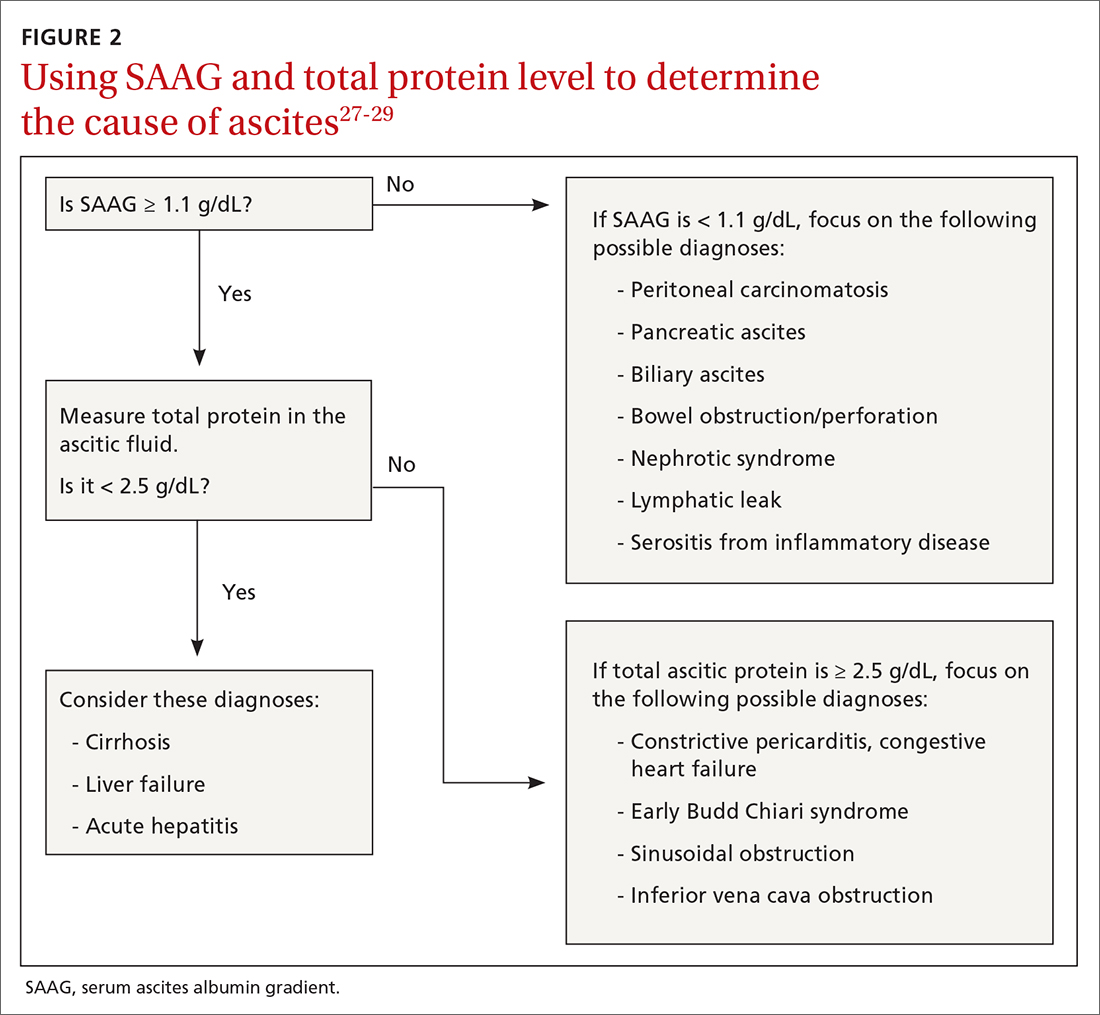
Management
Noninvasive measures
Sodium restriction. The aim of treatment for uncomplicated clinically apparent ascites is sodium restriction and removal of fluid from the body. Dietary salt restriction is complicated, and care should be taken to properly educate patients. Salt restriction advised in the literature has shifted from a strict measure of < 2 g/d30 to more moderate strategies (described below).18
The 2 main reasons for this easing of restriction are issues with patient compliance and concerns about adverse effects with aggressive salt-restricted diets. One study assessing patient compliance with a salt-restricted diet found that more than two-thirds of the patients were noncompliant,31 and 65% of the patients incorrectly assumed they were following the plan, which suggests poor dietary education.31 Of the group that was compliant, 20% actually decreased their caloric intake, which can be detrimental in liver disease.31 Concerns have been raised that aggressive salt restriction along with diuretic use can lead to diuretic-induced hyponatremia and renal failure.32 Current European Association for the Study of the Liver (EASL) guidelines recommend salt restriction to a more moderate degree (80-120 mmol/d of sodium). This is equivalent to 4.9-6.9 g of salt (1 tablespoon is roughly equivalent to 6 g or 104 mmol of sodium).18
Diuretics. Initiation and dosage of diuretic therapy is a matter of some controversy. Historically, simultaneous administration of a loop diuretic and mineralocorticoid receptor blocker were recommended: 40 mg furosemide and 100 mg spironolactone, keeping the ratio constant with any dosage increases. This was based on a randomized controlled trial (RCT) showing that the combined diuretic therapy effectively mobilized ascites in a shorter period of time and with less frequent adverse effects (eg, hyperkalemia) compared with initial monotherapy.33
Continue to: On the other hand...
On the other hand, another study with more stable patients and relatively normal renal function showed that starting with a mineralocorticoid receptor blocker alone with sequential dose increments had equivalent benefit with no increase in adverse effects.34 Since the patient population in this study was more in line with what a PCP might encounter, we recommend following this guideline initially and keeping a close watch on serum electrolytes.
Usual maximum doses are spironolactone 400 mg/d and furosemide 160 mg/d.21,35 Adequate weight loss for patients with diffuse edema is at least 1 kg/d, per EASL guidelines.36,37 However, this might not be practical in outpatient settings, and a more conservative target of 0.5 kg/d may be used for patients without significant edema.37
It is vital to get accurate daily weights and avoid excessive diuretic use, as it has been associated with intravascular volume depletion and acute kidney injury (25%), hyponatremia (28%),38,39 and hepatic encephalopathy (30%).40 Therefore, patients with acute kidney injury, hyponatremia, acute variceal hemorrhage, or infection should also have their diuretics held until their creatinine returns to baseline.
Invasive measures
Large-volume paracentesis. Patients with extensive and tense ascites should be treated initially with large-volume paracentesis, as this has been shown to predictably remove fluid more effectively than diuretics.38 This should be accompanied by albumin administration, 8 g for every liter of ascitic fluid removed if the total amount exceeds 5 L.41 Following large-volume paracentesis, manage patients with the standard salt restriction and diuretic regimen.38 Serial large-volume paracentesis is a temporary measure reserved for a select group of patients who are intolerant to diuretics and are not candidates for a shunt.
Transjugular intrahepatic portosystemic shunt (TIPS) is another option to control refractory ascites, but its benefit should be weighed against complications such as hepatic encephalopathy. An RCT found that TIPS with covered stents improved survival in patients with cirrhosis compared with regular large-volume paracentesis.42 Patients should be referred to hepatologists to make a determination about TIPS placement. Widely accepted contraindications for the placement of TIPS are decompensated cirrhosis (Child-Pugh > 11, model for end-stage liver disease [MELD] > 18), renal failure (serum creatinine > 3 mg/dL), heart failure, porto-pulmonary hypertension, and uncontrolled sepsis.43 Recurrent or persistent hepatic encephalopathy (West Haven grade ≥ 2) is also a contraindication. The West Haven scale is widely used to measure severity of hepatic encephalopathy, grading it from 1 to 4, with 1 being mild encephalopathy characterized by lack of awareness and shorter attention span, and 4 indicating unresponsiveness or coma.44
Continue to: How to manage refractory ascites
How to manage refractory ascites
Fragile patients are those with refractory ascites that is either unresponsive to standard salt restriction and maximum-dose diuretic therapy or that results in a re-accumulation of ascitic fluid soon after paracentesis.45 Specialist care is required to improve survival and quality of life for these patients. They should be referred to a hepatologist for consideration of TIPS placement or liver transplantation.18
Long-term use of albumin was tested in 2 trials for management of decompensated cirrhosis with ascites, yielding conflicting results. The ANSWER trial from Italy showed benefit with this treatment for prolonged survival.46 The other trial, from Spain, showed no benefit from albumin and midodrine administration for survival or for improving complications of cirrhosis.47 The contradictory results are likely due to heterogeneous populations in the 2 trials and differences in dose and duration of albumin administration. Hence, no clear recommendations can be made based on the available data; further research is needed.
Getting a handle on bacterial peritonitis
Bacterial peritonitis can be divided into spontaneous bacterial peritonitis (SBP) and secondary bacterial peritonitis. SBP is a common complication in patients with cirrhosis and occurs in around 16% of hospitalized patients, based on 1 study.48 SBP is defined as a polymorphonuclear leukocyte count ≥ 250 cells/μL in the absence of a surgically treatable source of infection.49 It is believed to be caused by bacterial translocation and is treated empirically with a third-generation cephalosporin. This treatment has been shown to be effective in 85% of patients.50
Patients with SBP are at a higher risk for renal impairment, likely resulting from increased cytokine production and decreased circulatory volume.51 Concomitant albumin administration has been shown to significantly improve outcomes and to reduce rates of hepatorenal syndrome in patients with serum creatinine > 1 mg/dL, blood urea nitrogen > 30 mg/dL, or total bilirubin > 4 mg/dL.52 The recommended amount of albumin is 1.5 g/kg given within 6 hours of SBP detection and repeat administration of 1 g/kg on Day 3.52
Guidelines from the American Association for the Study of Liver Diseases and from EASL recommend the long-term use of daily norfloxacin or trimethoprim-sulfamethoxazole as secondary prophylaxis in patients who have survived an episode of SBP.18
Continue to: Avoid these medications
Avoid these medications
Commonly used medications that should be avoided in patients with cirrhosis and ascites are angiotensin-converting enzyme inhibitors and angiotensin receptor blockers. These agents block the action of angiotensin, which is a vital vasoconstrictor, and thereby cause a drop in blood pressure. This has independently been associated with poor outcomes in patients with cirrhosis.37
Nonsteroidal anti-inflammatory drugs (NSAIDs) are also relatively contraindicated in cirrhosis, as they can affect kidney function, induce azotemia, and reduce kidney sodium excretion. NSAIDs induce vasoconstriction of afferent arterioles in the kidneys, leading to a decreased glomerular filtration rate, further activating RAAS and sympathetic drive. This leads to increased sodium and water retention and worsening ascites.54
Improve outcomes by circling in a hepatologist
PCPs can play a vital role in the prevention, treatment, surveillance, and home care of patients with cirrhosis who are at risk for ascites.55 Referral of patients with hepatic impairment manifesting as unexplained abnormal liver function tests, new-onset ascites, and/or image findings consistent with cirrhosis to a hepatologist at least once is recommended. Such referrals have been shown to be associated with a better overall outcome.56 Patients with known cirrhosis leading to ascites can generally be managed at home with the assistance of specialists and specialized nurses.35
In a study from the University of Michigan, 69% of patients with cirrhosis had at least 1 nonelective readmission; 14% of patients were readmitted within 1 week, and 37% within 1 month.57 These are staggering statistics that highlight the gaps in care coordination and management of patients with cirrhosis in the outpatient setting. PCPs can play a vital role in bridging this gap.
A promising framework is suggested by a study from Italy by Morando et al in 2013.58 The researchers assessed a specialized health care model for cirrhotic patients and showed significant improvement in health care cost, readmission rate, and overall mortality when compared with the existing model of outpatient care.58
Continue to: This was not a blinded study...
This was not a blinded study and there were concerns raised by the scientific community about its design. Because it was conducted in Italy, the results might not be fully applicable to the United States health care setting. However, it did show that better coordination of care leads to significantly better patient outcomes and reduces health care expenditure. Therefore, a more complete understanding of the disease process and latest literature by PCPs, communication with specialists, and comprehensive coordination of care by all parties involved is vital for the management of this patient population.
CORRESPONDENCE
Muhammad Salman Faisal, MD, Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, OH 44195; [email protected]
Liver cirrhosis is implicated in 75% to 85% of ascites cases in the Western world, with heart failure or malignancy accounting for fewer cases.1 Among patients who have decompensated cirrhosis with ascites, annual mortality is 20%.2 Another study showed a 3-year survival rate after onset of ascites of only 56%.3 It is vital for primary care physicians (PCPs) to be alert for ascites not only in patients who have risk factors for chronic liver disease and cirrhosis—eg, a history of alcohol use disorder, chronic viral infections (hepatitis B and C), or metabolic syndrome—but also in patients with abnormal liver function tests and thrombocytopenia. In this review, we discuss the initial assessment of ascites and its long-term management, concentrating on the role of the PCP.
Pathophysiology: Vasodilation leads to a cascade
Splanchnic vasodilation is the main underlying event triggering a pathologic cascade that leads to the development of ascites.4 Initially portal hypertension in the setting of liver inflammation and fibrosis causes the release of inflammatory cytokines such as nitric oxide and carbon monoxide. This, in turn, causes the pathologic dilation of splanchnic circulation that decreases effective circulating volume. Activation of the sympathetic nervous system, vasopressin, and renin-angiotensin-aldosterone system (RAAS) then causes the proximal and distal tubules to increase renal absorption of sodium and water.5 The resulting volume overload further decreases the heart’s ability to maintain circulating volume, leading to increased activation of compensating symptoms. This vicious cycle eventually manifests as ascites.6
A complex interplay of cirrhosis-associated immune dysfunction (CAID), gut dysbiosis, and increased translocation of microorganisms into ascitic fluid is also an important aspect of the pathogenesis.7 CAID (FIGURE 1)7,8 is an immunodeficient state due to cirrhosis with reduced phagocytic activity by neutrophils and macrophages, T- and B-cell hypoproliferation, and reduced cytotoxicity of natural killer cells. In parallel, there is increased production of inflammatory cytokines due to the effects of damage-associated molecular patterns (DAMPs) from hepatocytes and pathogen-associated molecular patterns (PAMPs) from the gut microbiota on the immune system, which leads to many of the manifestations of decompensated cirrhosis including ascites.8
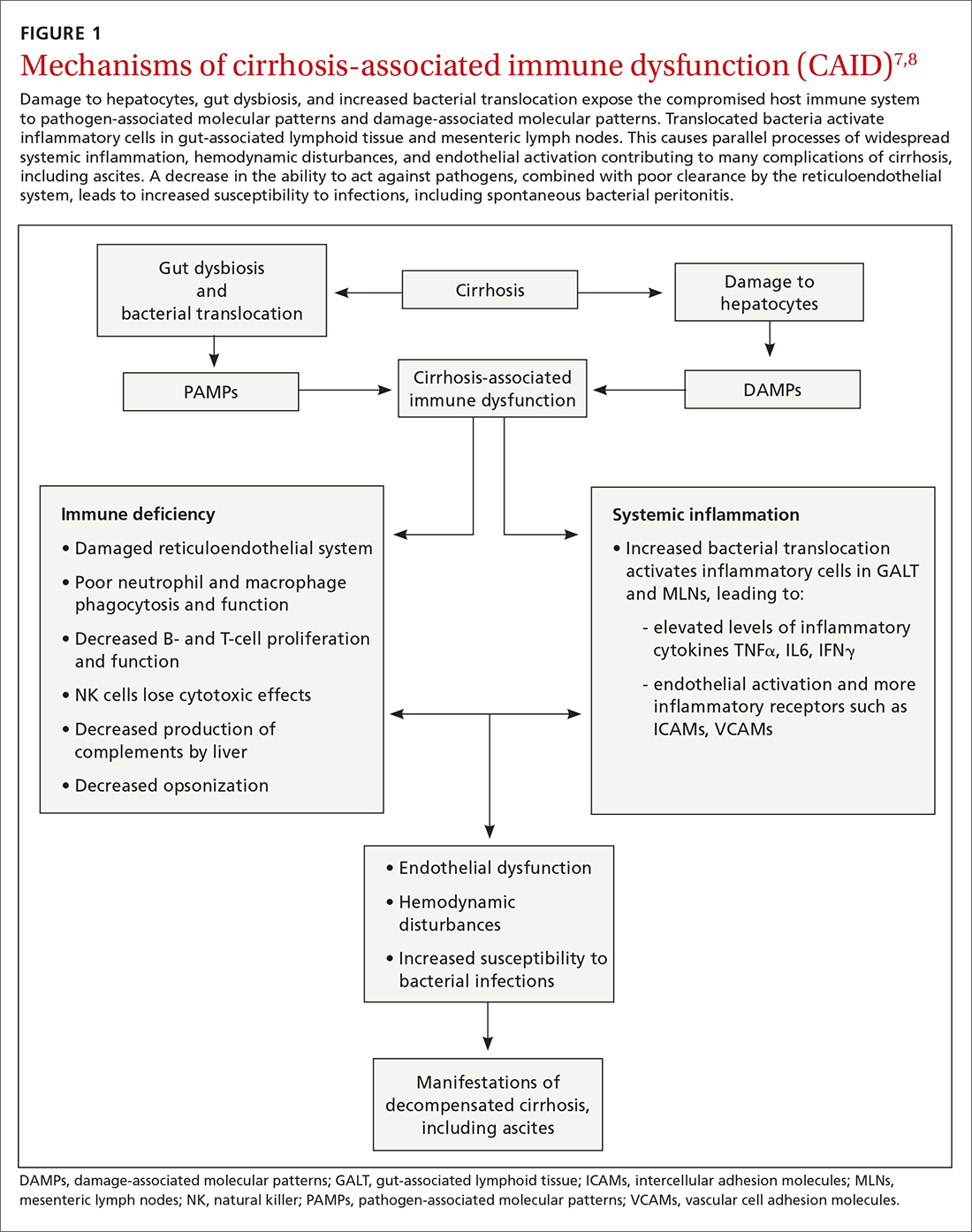
Key in on these elementsof the history and exam
Each step of the basic work-up for ascites provides opportunities to refine or redirect the diagnostic inquiry (TABLE).
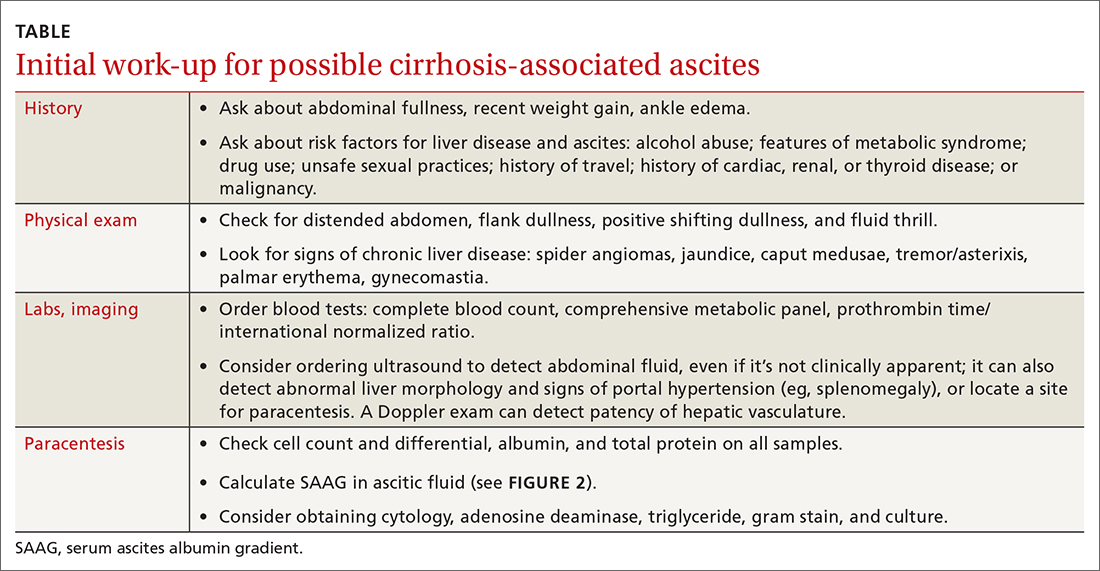
History
Generally, patients with ascites present with weight gain and symptoms of abdominal distension, such as early satiety, nausea, and vomiting. Besides cirrhosis, rule out other causes of ascites, as treatment differs based on the cause.9 Also ask about histories of cancer and cardiac, renal, or thyroid disease.10
Patients with ascites in the setting of liver disease usually are asymptomatic in its early stages. Common complaints are vague abdominal pain, generalized weakness, malaise, and fatigue.11 Ask patients about risk factors for liver disease such as obesity, diabetes, hypertension, alcohol use, unsafe sexual practices, recent travel, and needle sharing or drug use. Due to a strong association between obstructive sleep apnea and fatty liver disease, consider screening at-risk patients for sleep apnea.12
Physical exam
When there are risk factors for liver disease, examine the patient for stigmata of cirrhosis and ascites. Signs of liver disease, aside from ascites, may include spider angiomas on the upper trunk (33% of cirrhosis patients),13 gynecomastia (44% of cirrhosis patients),14 palmar erythema, jaundice, asterixis, and abdominal wall collaterals including caput medusa.15
Continue to: We suggest a systematic...
We suggest a systematic and targeted approach to using various physical exam maneuvers described in the literature. If the patient has a full/distended abdomen, percuss the flanks. If increased dullness at the flanks is detected, check for shifting dullness, which indicates at least 1500 mL of fluid in the abdomen.16 Keep in mind that a 10% chance of ascites exists even if shifting dullness is absent.17 Maneuvers such as the puddle sign and fluid thrill are less accurate than shifting dullness, which has 83% sensitivity and 56% specificity in detecting ascites.17 Patients with cirrhosis also have a high likelihood of complications from ascites such as inguinal, umbilical, and other hernias.
Diagnostic work-up includes blood tests and ultrasound
Blood tests. The initial work-up for ascites should include complete blood count, complete metabolic panel, and prothrombin time/international normalized ratio.18
Abdominal ultrasound is recommended as the first-line imaging test.19 Aside from detecting ascites, it can give an estimate of the volume of ascites and indicate whether it is amenable to paracentesis. A vascular exam added to the standard ultrasound can detect radiologic evidence of portal hypertension such as splenomegaly, portosystemic collaterals, splenorenal shunt, patency of the paraumbilical vein, and portal vein diameter. Patients with established cirrhosis also require abdominal ultrasound every 6 months to screen for hepatocellular cancer.20
Abdominal paracentesis is the cornerstone of ascites evaluation.21 It is indicated for every patient with new-onset ascites or for any patient with known ascites and clinical deterioration. Ascitic fluid analysis can be used to easily differentiate portal hypertension from other causes of ascites. It can also be used to rule out bacterial peritonitis. The recommended sites for evaluation are in the left lower quadrant, 3 cm cranially and 3 cm medially from the anterior superior iliac spine.22 A large cohort study showed that abdominal ultrasound-guided paracentesis reduced bleeding complications by 68% following the procedure and is strongly recommended (if available).23 Generally, paracentesis is a relatively safe procedure with a low risk of complications such as abdominal wall hematoma (1%), hemoperitoneum (< 0.1%), bowel perforation (< 0.1%), and infection (< 0.1%).24
Assess all ascitic fluid samples for color, consistency, cell count and differential, albumin, and total protein. These tests are usually sufficient to provide evidence regarding the cause of ascites. If there is suspicion of infection, order a gram stain and culture (80% sensitivity for detecting an infection if obtained prior to initiation of antibiotics)25 and glucose, lactate dehydrogenase (useful to differentiate primary from secondary bacterial peritonitis),26 and amylase tests. Other tests such as cytology, acid-fast bacilli smear and culture, and triglyceride level should only be obtained if specific conditions are suspected based on high pretest probabilities.
Continue to: Calculating serum ascites albumin gradient...
Calculating serum ascites albumin gradient (SAAG) is recommended as it has been shown to better characterize ascitic fluid than total protein-based tests.27 SAAG is calculated by subtracting the level of ascitic fluid albumin from serum albumin level (SAAG = serum albumin – ascitic fluid albumin). A SAAG ≥ 1.1 g/dL is consistent with portal hypertension,28 with approximately 97% accuracy.
After calculating SAAG, look at total protein levels in ascitic fluid. Total protein concentration ≥ 2.5 g/dL with SAAG ≥ 1.1 g/dL has a 78.3% diagnostic accuracy in determining heart failure as the cause of ascites, with a sensitivity of 53.3% and specificity of 86.7%.28 On the other hand, a value of total protein < 2.5 g/dL indicates cirrhosis, liver failure, or acute hepatitis as the cause of fluid build-up.29 Stepwise evaluation of SAAG and total protein and how they can point toward the most likely cause of ascites is presented in FIGURE 2.27-29
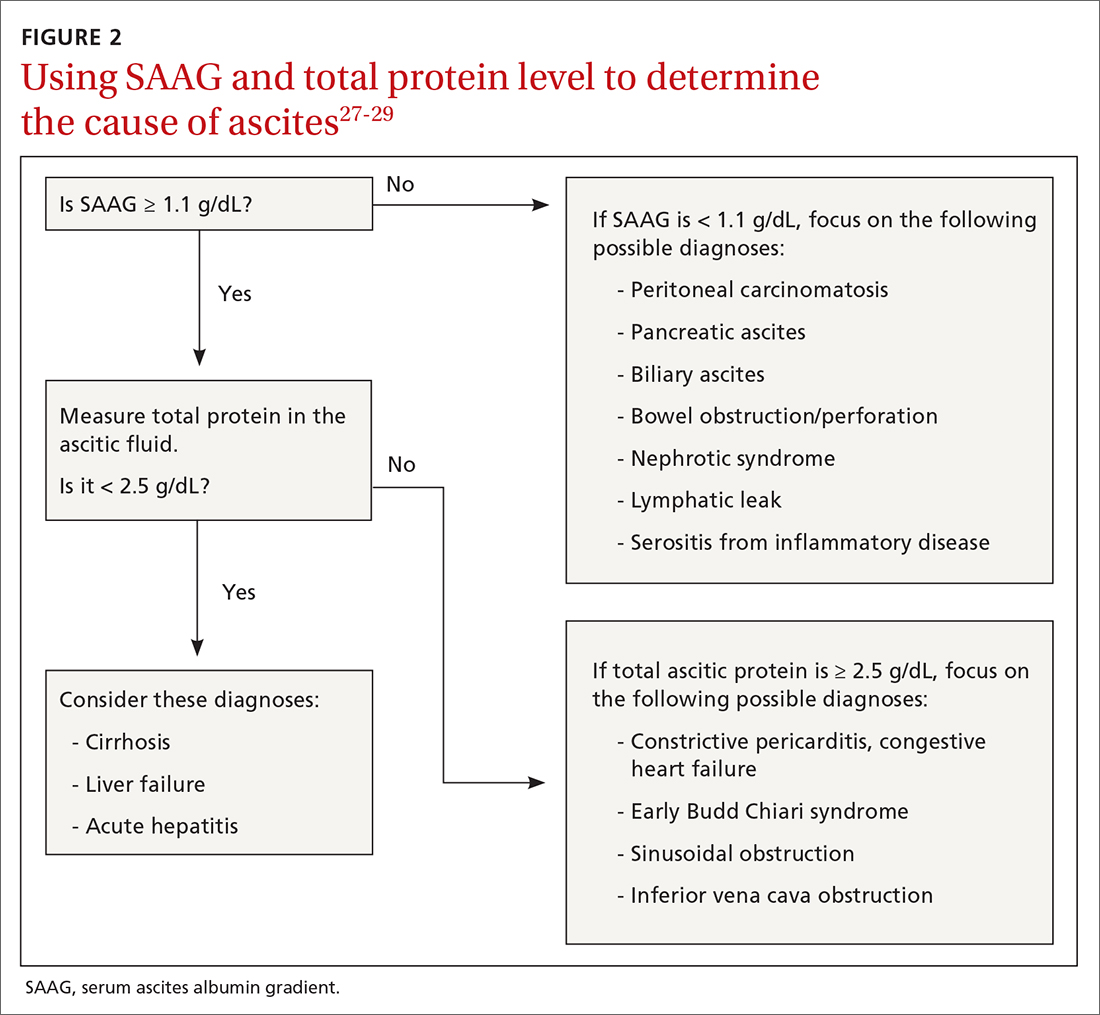
Management
Noninvasive measures
Sodium restriction. The aim of treatment for uncomplicated clinically apparent ascites is sodium restriction and removal of fluid from the body. Dietary salt restriction is complicated, and care should be taken to properly educate patients. Salt restriction advised in the literature has shifted from a strict measure of < 2 g/d30 to more moderate strategies (described below).18
The 2 main reasons for this easing of restriction are issues with patient compliance and concerns about adverse effects with aggressive salt-restricted diets. One study assessing patient compliance with a salt-restricted diet found that more than two-thirds of the patients were noncompliant,31 and 65% of the patients incorrectly assumed they were following the plan, which suggests poor dietary education.31 Of the group that was compliant, 20% actually decreased their caloric intake, which can be detrimental in liver disease.31 Concerns have been raised that aggressive salt restriction along with diuretic use can lead to diuretic-induced hyponatremia and renal failure.32 Current European Association for the Study of the Liver (EASL) guidelines recommend salt restriction to a more moderate degree (80-120 mmol/d of sodium). This is equivalent to 4.9-6.9 g of salt (1 tablespoon is roughly equivalent to 6 g or 104 mmol of sodium).18
Diuretics. Initiation and dosage of diuretic therapy is a matter of some controversy. Historically, simultaneous administration of a loop diuretic and mineralocorticoid receptor blocker were recommended: 40 mg furosemide and 100 mg spironolactone, keeping the ratio constant with any dosage increases. This was based on a randomized controlled trial (RCT) showing that the combined diuretic therapy effectively mobilized ascites in a shorter period of time and with less frequent adverse effects (eg, hyperkalemia) compared with initial monotherapy.33
Continue to: On the other hand...
On the other hand, another study with more stable patients and relatively normal renal function showed that starting with a mineralocorticoid receptor blocker alone with sequential dose increments had equivalent benefit with no increase in adverse effects.34 Since the patient population in this study was more in line with what a PCP might encounter, we recommend following this guideline initially and keeping a close watch on serum electrolytes.
Usual maximum doses are spironolactone 400 mg/d and furosemide 160 mg/d.21,35 Adequate weight loss for patients with diffuse edema is at least 1 kg/d, per EASL guidelines.36,37 However, this might not be practical in outpatient settings, and a more conservative target of 0.5 kg/d may be used for patients without significant edema.37
It is vital to get accurate daily weights and avoid excessive diuretic use, as it has been associated with intravascular volume depletion and acute kidney injury (25%), hyponatremia (28%),38,39 and hepatic encephalopathy (30%).40 Therefore, patients with acute kidney injury, hyponatremia, acute variceal hemorrhage, or infection should also have their diuretics held until their creatinine returns to baseline.
Invasive measures
Large-volume paracentesis. Patients with extensive and tense ascites should be treated initially with large-volume paracentesis, as this has been shown to predictably remove fluid more effectively than diuretics.38 This should be accompanied by albumin administration, 8 g for every liter of ascitic fluid removed if the total amount exceeds 5 L.41 Following large-volume paracentesis, manage patients with the standard salt restriction and diuretic regimen.38 Serial large-volume paracentesis is a temporary measure reserved for a select group of patients who are intolerant to diuretics and are not candidates for a shunt.
Transjugular intrahepatic portosystemic shunt (TIPS) is another option to control refractory ascites, but its benefit should be weighed against complications such as hepatic encephalopathy. An RCT found that TIPS with covered stents improved survival in patients with cirrhosis compared with regular large-volume paracentesis.42 Patients should be referred to hepatologists to make a determination about TIPS placement. Widely accepted contraindications for the placement of TIPS are decompensated cirrhosis (Child-Pugh > 11, model for end-stage liver disease [MELD] > 18), renal failure (serum creatinine > 3 mg/dL), heart failure, porto-pulmonary hypertension, and uncontrolled sepsis.43 Recurrent or persistent hepatic encephalopathy (West Haven grade ≥ 2) is also a contraindication. The West Haven scale is widely used to measure severity of hepatic encephalopathy, grading it from 1 to 4, with 1 being mild encephalopathy characterized by lack of awareness and shorter attention span, and 4 indicating unresponsiveness or coma.44
Continue to: How to manage refractory ascites
How to manage refractory ascites
Fragile patients are those with refractory ascites that is either unresponsive to standard salt restriction and maximum-dose diuretic therapy or that results in a re-accumulation of ascitic fluid soon after paracentesis.45 Specialist care is required to improve survival and quality of life for these patients. They should be referred to a hepatologist for consideration of TIPS placement or liver transplantation.18
Long-term use of albumin was tested in 2 trials for management of decompensated cirrhosis with ascites, yielding conflicting results. The ANSWER trial from Italy showed benefit with this treatment for prolonged survival.46 The other trial, from Spain, showed no benefit from albumin and midodrine administration for survival or for improving complications of cirrhosis.47 The contradictory results are likely due to heterogeneous populations in the 2 trials and differences in dose and duration of albumin administration. Hence, no clear recommendations can be made based on the available data; further research is needed.
Getting a handle on bacterial peritonitis
Bacterial peritonitis can be divided into spontaneous bacterial peritonitis (SBP) and secondary bacterial peritonitis. SBP is a common complication in patients with cirrhosis and occurs in around 16% of hospitalized patients, based on 1 study.48 SBP is defined as a polymorphonuclear leukocyte count ≥ 250 cells/μL in the absence of a surgically treatable source of infection.49 It is believed to be caused by bacterial translocation and is treated empirically with a third-generation cephalosporin. This treatment has been shown to be effective in 85% of patients.50
Patients with SBP are at a higher risk for renal impairment, likely resulting from increased cytokine production and decreased circulatory volume.51 Concomitant albumin administration has been shown to significantly improve outcomes and to reduce rates of hepatorenal syndrome in patients with serum creatinine > 1 mg/dL, blood urea nitrogen > 30 mg/dL, or total bilirubin > 4 mg/dL.52 The recommended amount of albumin is 1.5 g/kg given within 6 hours of SBP detection and repeat administration of 1 g/kg on Day 3.52
Guidelines from the American Association for the Study of Liver Diseases and from EASL recommend the long-term use of daily norfloxacin or trimethoprim-sulfamethoxazole as secondary prophylaxis in patients who have survived an episode of SBP.18
Continue to: Avoid these medications
Avoid these medications
Commonly used medications that should be avoided in patients with cirrhosis and ascites are angiotensin-converting enzyme inhibitors and angiotensin receptor blockers. These agents block the action of angiotensin, which is a vital vasoconstrictor, and thereby cause a drop in blood pressure. This has independently been associated with poor outcomes in patients with cirrhosis.37
Nonsteroidal anti-inflammatory drugs (NSAIDs) are also relatively contraindicated in cirrhosis, as they can affect kidney function, induce azotemia, and reduce kidney sodium excretion. NSAIDs induce vasoconstriction of afferent arterioles in the kidneys, leading to a decreased glomerular filtration rate, further activating RAAS and sympathetic drive. This leads to increased sodium and water retention and worsening ascites.54
Improve outcomes by circling in a hepatologist
PCPs can play a vital role in the prevention, treatment, surveillance, and home care of patients with cirrhosis who are at risk for ascites.55 Referral of patients with hepatic impairment manifesting as unexplained abnormal liver function tests, new-onset ascites, and/or image findings consistent with cirrhosis to a hepatologist at least once is recommended. Such referrals have been shown to be associated with a better overall outcome.56 Patients with known cirrhosis leading to ascites can generally be managed at home with the assistance of specialists and specialized nurses.35
In a study from the University of Michigan, 69% of patients with cirrhosis had at least 1 nonelective readmission; 14% of patients were readmitted within 1 week, and 37% within 1 month.57 These are staggering statistics that highlight the gaps in care coordination and management of patients with cirrhosis in the outpatient setting. PCPs can play a vital role in bridging this gap.
A promising framework is suggested by a study from Italy by Morando et al in 2013.58 The researchers assessed a specialized health care model for cirrhotic patients and showed significant improvement in health care cost, readmission rate, and overall mortality when compared with the existing model of outpatient care.58
Continue to: This was not a blinded study...
This was not a blinded study and there were concerns raised by the scientific community about its design. Because it was conducted in Italy, the results might not be fully applicable to the United States health care setting. However, it did show that better coordination of care leads to significantly better patient outcomes and reduces health care expenditure. Therefore, a more complete understanding of the disease process and latest literature by PCPs, communication with specialists, and comprehensive coordination of care by all parties involved is vital for the management of this patient population.
CORRESPONDENCE
Muhammad Salman Faisal, MD, Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, OH 44195; [email protected]
1. Runyon BA, Montano AA, Akriviadis EA, et al. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med. 1992;117:215-220.
2. D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-231.
3. Gordon FD. Ascites. Clin Liver Dis. 2012;16:285-299.
4. Schrier RW, Arroyo V, Bernardi M, et al. Peripheral arterial vasodilation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology. 1988;8:1151-1157.
5. Arroyo V, Terra C, Gines P. Advances in the pathogenesis and treatment of type-1 and type-2 hepatorenal syndrome. J Hepatol. 2007;46:935-946.
6. Bernardi M, Moreau R, Angeli P, et al. Mechanisms of decompensation and organ failure in cirrhosis: from peripheral arterial vasodilation to systemic inflammation hypothesis. J Hepatol. 2015;63:1272-1284.
7. Jalan R, Fernandez J, Wiest R, et al. Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol. 2014;60:1310-1324.
8. Albillos A, Lario M, Álvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol. 2014;61:1385-1396.
9. Oey RC, van Buuren HR, de Man RA. The diagnostic work-up in patients with ascites: current guidelines and future prospects. Neth J Med. 2016;74:330-335.
10. de Kerguenec C, Hillaire S, Molinié V, et al. Hepatic manifestations of hemophagocytic syndrome: a study of 30 cases. Am J Gastroenterol. 2001;96:852-857.
11. Milić S, Lulić D, Štimac D. Non-alcoholic fatty liver disease and obesity: biochemical, metabolic and clinical presentations. World J Gastroenterol. 2014;20:9330-9337.
12. Aron-Wisnewsky J, Clement K, Pépin J-L. Nonalcoholic fatty liver disease and obstructive sleep apnea. Metabolism. 2016;65:1124-1135.
13. Li CP, Lee FY, Hwang SJ, et al. Spider angiomas in patients with liver cirrhosis: role of alcoholism and impaired liver function. Scand J Gastroenterol. 1999;34:520-523.
14. Cavanaugh J. Gynecomastia and cirrhosis of the liver. Arch Intern Med. 1990;150:563-565.
15. Karnath B. Stigmata of chronic liver disease. Hosp Phys. 2003;7:14-16,28.
16. Schipper HG, Godfried MH. [Physical diagnosis--ascites]. Ned Tijdschr Geneeskd. 2001;145:260-264.
17. Cattau EL, Jr., Benjamin SB, Knuff TE, et al. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247:1164-1166.
18. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69:406-460.
19. Runyon BA, AASLD Practice Guidelines Committee. Management of adult patients with ascites due to cirrhosis: an update. Hepatology 2009;49:2087-2107.
20. EASL Clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236.
21. Runyon BA. Care of patients with ascites. New Engl J Med. 1994;330:337-342.
22. Sakai H, Sheer TA, Mendler MH, et al. Choosing the location for non-image guided abdominal paracentesis. Liver Int. 2005;25:984-986.
23. Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis. Chest. 2013;143:532-538.
24. Ennis J, Schultz G, Perera P, et al. Ultrasound for detection of ascites and for guidance of the paracentesis procedure: technique and review of the literature. Int J Clin Med. 2014;5:1277-1293.
25. Runyon BA, Canawati HN, Akriviadis EA. Optimization of ascitic fluid culture technique. Gastroenterology. 1988;95:1351-1355.
26. Akriviadis EA, Runyon BA. Utility of an algorithm in differentiating spontaneous from secondary bacterial peritonitis. Gastroenterology 1990;98:127-133.
27. Hoefs JC. Serum protein concentration and portal pressure determine the ascitic fluid protein concentration in patients with chronic liver disease. J Lab Clin Med. 1983;102:260-273.
28. Farias AQ, Silvestre OM, Garcia-Tsao G, et al. Serum B-type natriuretic peptide in the initial workup of patients with new onset ascites: a diagnostic accuracy study. Hepatology. 2014;59:1043-1051.
29. Gupta R, Misra SP, Dwivedi M, et al. Diagnosing ascites: value of ascitic fluid total protein, albumin, cholesterol, their ratios, serum-ascites albumin and cholesterol gradient. J Gastroenterol Hepatol. 1995;10:295-299.
30. Runyon BA. Management of adult patients with ascites due to cirrhosis: update 2012. AASLD Practice Guideline. Accessed April 28, 2021. www.aasld.org/sites/default/files/2019-06/AASLDPracticeGuidelineAsciteDuetoCirrhosisUpdate2012Edition4_.pdf
31. Morando F, Rosi S, Gola E, et al. Adherence to a moderate sodium restriction diet in outpatients with cirrhosis and ascites: a real-life cross-sectional study. Liver Int. 2015;35:1508-1515.
32. Bernardi M, Laffi G, Salvagnini M, et al. Efficacy and safety of the stepped care medical treatment of ascites in liver cirrhosis: a randomized controlled clinical trial comparing two diets with different sodium content. Liver. 1993;13:156-162.
33. Angeli P, Fasolato S, Mazza E, et al. Combined versus sequential diuretic treatment of ascites in non-azotaemic patients with cirrhosis: results of an open randomised clinical trial. Gut. 2010;59:98-104.
34. Santos J, Planas R, Pardo A, et al. Spironolactone alone or in combination with furosemide in the treatment of moderate ascites in nonazotemic cirrhosis. A randomized comparative study of efficacy and safety. J Hepatol. 2003;39:187–192.
35. Grattagliano I, Ubaldi E, Bonfrate L, et al. Management of liver cirrhosis between primary care and specialists. World J Gastroenterol. 2011;17:2273-2282.
36. Pockros PJ, Reynolds TB. Rapid diuresis in patients with ascites from chronic liver disease: the importance of peripheral edema. Gastroenterology. 1986;90:1827-1833.
37. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397-417.
38. Gines P, Arroyo V, Quintero E, et al. Comparison of paracentesis and diuretics in the treatment of cirrhotics with tense ascites. Results of a randomized study. Gastroenterology. 1987;93:234-241.
39. Salerno F, Badalamenti S, Incerti P, et al. Repeated paracentesis and i.v. albumin infusion to treat ‘tense’ ascites in cirrhotic patients. A safe alternative therapy. J Hepatol. 1987;5:102-108.
40. Sola R, Vila MC, Andreu M, et al. Total paracentesis with dextran 40 vs diuretics in the treatment of ascites in cirrhosis: a randomized controlled study. J Hepatol. 1994;20:282-288.
41. Bernardi M, Caraceni P, Navickis RJ, et al. Albumin infusion in patients undergoing large-volume paracentesis: a meta-analysis of randomized trials. Hepatology. 2012;55:1172-1181.
42. Bureau C, Thabut D, Oberti F, et al. Transjugular intrahepatic portosystemic shunts with covered stents increase transplant-free survival of patients with cirrhosis and recurrent ascites. Gastroenterology. 2017;152:157-163.
43. Fagiuoli S, Bruno R, Debernardi Venon W, et al. Consensus conference on TIPS management: techniques, indications, contraindications. Dig Liver Dis. 2017;49:121-137.
44. Ferenci P, Lockwood A, Mullen K, et al. Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716-721.
45. Salerno F, Guevara M, Bernardi M, et al. Refractory ascites: pathogenesis, definition and therapy of a severe complication in patients with cirrhosis. Liver Int. 2010;30:937-947.
46. Caraceni P, Riggio O, Angeli P, et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial. Lancet. 2018;391:2417-2429.
47. Solà E, Solé C, Simón-Talero M, et al. Midodrine and albumin for prevention of complications in patients with cirrhosis awaiting liver transplantation. A randomized placebo-controlled trial. J Hepatol. 2018;69:1250-1259.
48. Fasolato S, Angeli P, Dallagnese L, et al. Renal failure and bacterial infections in patients with cirrhosis: epidemiology and clinical features. Hepatology. 2007;45:223-229.
49. Hoefs JC, Canawati HN, Sapico FL, et al. Spontaneous bacterial peritonitis. Hepatology. 2007;2:399-407.
50. Felisart J, Rimola A, Arroyo V, et al. Cefotaxime is more effective than is ampicillin-tobramycin in cirrhotics with severe infections. Hepatology. 1985;5:457-462.
51. Lenz K, Kapral C, Gegenhuber A, et al. Systemic, renal, and hepatic hemodynamic derangement in cirrhotic patients with spontaneous bacterial peritonitis. Hepatology. 2004;39:865-866.
52. Sigal SH, Stanca CM, Fernandez J, et al. Restricted use of albumin for spontaneous bacterial peritonitis. Gut. 2007;56:597-599.
53. Fernández J, Navasa M, Planas R, et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology. 2007;133:818-824.
54. Boyer TD, Zia P, Reynolds TB. Effect of indomethacin and prostaglandin A1 on renal function and plasma renin activity in alcoholic liver disease. Gastroenterology. 1979;77:215-222.
55. Grattagliano I, Ubaldi E, Portincasa P, et al. Liver disease: early signs you may be missing. J Fam Pract. 2009;58:514-521.
56. Bini EJ, Weinshel EH, Generoso R, et al. Impact of gastroenterology consultation on the outcomes of patients admitted to the hospital with decompensated cirrhosis. Hepatology. 2001;34:1089-1095.
57. Volk ML, Tocco RS, Bazick J, et al. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107:247-252.
58. Morando F, Maresio G, Piano S, et al. How to improve care in outpatients with cirrhosis and ascites: a new model of care coordination by consultant hepatologists. J Hepatol. 2013;59:257-264.
1. Runyon BA, Montano AA, Akriviadis EA, et al. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med. 1992;117:215-220.
2. D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-231.
3. Gordon FD. Ascites. Clin Liver Dis. 2012;16:285-299.
4. Schrier RW, Arroyo V, Bernardi M, et al. Peripheral arterial vasodilation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology. 1988;8:1151-1157.
5. Arroyo V, Terra C, Gines P. Advances in the pathogenesis and treatment of type-1 and type-2 hepatorenal syndrome. J Hepatol. 2007;46:935-946.
6. Bernardi M, Moreau R, Angeli P, et al. Mechanisms of decompensation and organ failure in cirrhosis: from peripheral arterial vasodilation to systemic inflammation hypothesis. J Hepatol. 2015;63:1272-1284.
7. Jalan R, Fernandez J, Wiest R, et al. Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol. 2014;60:1310-1324.
8. Albillos A, Lario M, Álvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol. 2014;61:1385-1396.
9. Oey RC, van Buuren HR, de Man RA. The diagnostic work-up in patients with ascites: current guidelines and future prospects. Neth J Med. 2016;74:330-335.
10. de Kerguenec C, Hillaire S, Molinié V, et al. Hepatic manifestations of hemophagocytic syndrome: a study of 30 cases. Am J Gastroenterol. 2001;96:852-857.
11. Milić S, Lulić D, Štimac D. Non-alcoholic fatty liver disease and obesity: biochemical, metabolic and clinical presentations. World J Gastroenterol. 2014;20:9330-9337.
12. Aron-Wisnewsky J, Clement K, Pépin J-L. Nonalcoholic fatty liver disease and obstructive sleep apnea. Metabolism. 2016;65:1124-1135.
13. Li CP, Lee FY, Hwang SJ, et al. Spider angiomas in patients with liver cirrhosis: role of alcoholism and impaired liver function. Scand J Gastroenterol. 1999;34:520-523.
14. Cavanaugh J. Gynecomastia and cirrhosis of the liver. Arch Intern Med. 1990;150:563-565.
15. Karnath B. Stigmata of chronic liver disease. Hosp Phys. 2003;7:14-16,28.
16. Schipper HG, Godfried MH. [Physical diagnosis--ascites]. Ned Tijdschr Geneeskd. 2001;145:260-264.
17. Cattau EL, Jr., Benjamin SB, Knuff TE, et al. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247:1164-1166.
18. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69:406-460.
19. Runyon BA, AASLD Practice Guidelines Committee. Management of adult patients with ascites due to cirrhosis: an update. Hepatology 2009;49:2087-2107.
20. EASL Clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236.
21. Runyon BA. Care of patients with ascites. New Engl J Med. 1994;330:337-342.
22. Sakai H, Sheer TA, Mendler MH, et al. Choosing the location for non-image guided abdominal paracentesis. Liver Int. 2005;25:984-986.
23. Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis. Chest. 2013;143:532-538.
24. Ennis J, Schultz G, Perera P, et al. Ultrasound for detection of ascites and for guidance of the paracentesis procedure: technique and review of the literature. Int J Clin Med. 2014;5:1277-1293.
25. Runyon BA, Canawati HN, Akriviadis EA. Optimization of ascitic fluid culture technique. Gastroenterology. 1988;95:1351-1355.
26. Akriviadis EA, Runyon BA. Utility of an algorithm in differentiating spontaneous from secondary bacterial peritonitis. Gastroenterology 1990;98:127-133.
27. Hoefs JC. Serum protein concentration and portal pressure determine the ascitic fluid protein concentration in patients with chronic liver disease. J Lab Clin Med. 1983;102:260-273.
28. Farias AQ, Silvestre OM, Garcia-Tsao G, et al. Serum B-type natriuretic peptide in the initial workup of patients with new onset ascites: a diagnostic accuracy study. Hepatology. 2014;59:1043-1051.
29. Gupta R, Misra SP, Dwivedi M, et al. Diagnosing ascites: value of ascitic fluid total protein, albumin, cholesterol, their ratios, serum-ascites albumin and cholesterol gradient. J Gastroenterol Hepatol. 1995;10:295-299.
30. Runyon BA. Management of adult patients with ascites due to cirrhosis: update 2012. AASLD Practice Guideline. Accessed April 28, 2021. www.aasld.org/sites/default/files/2019-06/AASLDPracticeGuidelineAsciteDuetoCirrhosisUpdate2012Edition4_.pdf
31. Morando F, Rosi S, Gola E, et al. Adherence to a moderate sodium restriction diet in outpatients with cirrhosis and ascites: a real-life cross-sectional study. Liver Int. 2015;35:1508-1515.
32. Bernardi M, Laffi G, Salvagnini M, et al. Efficacy and safety of the stepped care medical treatment of ascites in liver cirrhosis: a randomized controlled clinical trial comparing two diets with different sodium content. Liver. 1993;13:156-162.
33. Angeli P, Fasolato S, Mazza E, et al. Combined versus sequential diuretic treatment of ascites in non-azotaemic patients with cirrhosis: results of an open randomised clinical trial. Gut. 2010;59:98-104.
34. Santos J, Planas R, Pardo A, et al. Spironolactone alone or in combination with furosemide in the treatment of moderate ascites in nonazotemic cirrhosis. A randomized comparative study of efficacy and safety. J Hepatol. 2003;39:187–192.
35. Grattagliano I, Ubaldi E, Bonfrate L, et al. Management of liver cirrhosis between primary care and specialists. World J Gastroenterol. 2011;17:2273-2282.
36. Pockros PJ, Reynolds TB. Rapid diuresis in patients with ascites from chronic liver disease: the importance of peripheral edema. Gastroenterology. 1986;90:1827-1833.
37. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397-417.
38. Gines P, Arroyo V, Quintero E, et al. Comparison of paracentesis and diuretics in the treatment of cirrhotics with tense ascites. Results of a randomized study. Gastroenterology. 1987;93:234-241.
39. Salerno F, Badalamenti S, Incerti P, et al. Repeated paracentesis and i.v. albumin infusion to treat ‘tense’ ascites in cirrhotic patients. A safe alternative therapy. J Hepatol. 1987;5:102-108.
40. Sola R, Vila MC, Andreu M, et al. Total paracentesis with dextran 40 vs diuretics in the treatment of ascites in cirrhosis: a randomized controlled study. J Hepatol. 1994;20:282-288.
41. Bernardi M, Caraceni P, Navickis RJ, et al. Albumin infusion in patients undergoing large-volume paracentesis: a meta-analysis of randomized trials. Hepatology. 2012;55:1172-1181.
42. Bureau C, Thabut D, Oberti F, et al. Transjugular intrahepatic portosystemic shunts with covered stents increase transplant-free survival of patients with cirrhosis and recurrent ascites. Gastroenterology. 2017;152:157-163.
43. Fagiuoli S, Bruno R, Debernardi Venon W, et al. Consensus conference on TIPS management: techniques, indications, contraindications. Dig Liver Dis. 2017;49:121-137.
44. Ferenci P, Lockwood A, Mullen K, et al. Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716-721.
45. Salerno F, Guevara M, Bernardi M, et al. Refractory ascites: pathogenesis, definition and therapy of a severe complication in patients with cirrhosis. Liver Int. 2010;30:937-947.
46. Caraceni P, Riggio O, Angeli P, et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial. Lancet. 2018;391:2417-2429.
47. Solà E, Solé C, Simón-Talero M, et al. Midodrine and albumin for prevention of complications in patients with cirrhosis awaiting liver transplantation. A randomized placebo-controlled trial. J Hepatol. 2018;69:1250-1259.
48. Fasolato S, Angeli P, Dallagnese L, et al. Renal failure and bacterial infections in patients with cirrhosis: epidemiology and clinical features. Hepatology. 2007;45:223-229.
49. Hoefs JC, Canawati HN, Sapico FL, et al. Spontaneous bacterial peritonitis. Hepatology. 2007;2:399-407.
50. Felisart J, Rimola A, Arroyo V, et al. Cefotaxime is more effective than is ampicillin-tobramycin in cirrhotics with severe infections. Hepatology. 1985;5:457-462.
51. Lenz K, Kapral C, Gegenhuber A, et al. Systemic, renal, and hepatic hemodynamic derangement in cirrhotic patients with spontaneous bacterial peritonitis. Hepatology. 2004;39:865-866.
52. Sigal SH, Stanca CM, Fernandez J, et al. Restricted use of albumin for spontaneous bacterial peritonitis. Gut. 2007;56:597-599.
53. Fernández J, Navasa M, Planas R, et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology. 2007;133:818-824.
54. Boyer TD, Zia P, Reynolds TB. Effect of indomethacin and prostaglandin A1 on renal function and plasma renin activity in alcoholic liver disease. Gastroenterology. 1979;77:215-222.
55. Grattagliano I, Ubaldi E, Portincasa P, et al. Liver disease: early signs you may be missing. J Fam Pract. 2009;58:514-521.
56. Bini EJ, Weinshel EH, Generoso R, et al. Impact of gastroenterology consultation on the outcomes of patients admitted to the hospital with decompensated cirrhosis. Hepatology. 2001;34:1089-1095.
57. Volk ML, Tocco RS, Bazick J, et al. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107:247-252.
58. Morando F, Maresio G, Piano S, et al. How to improve care in outpatients with cirrhosis and ascites: a new model of care coordination by consultant hepatologists. J Hepatol. 2013;59:257-264.
PRACTICE RECOMMENDATIONS
› Calculate the serum ascites albumin gradient and measure the total ascites protein level to distinguish cirrhotic ascites from that caused by heart failure or other disorders. C
› Recommend sodium restriction of 4.9-6.9 g for patients with established ascites secondary to cirrhosis. C
› Avoid giving angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and nonsteroidal anti-inflammatory drugs in cirrhosis. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Primary ovarian insufficiency requires long-term management of sequelae
Primary ovarian insufficiency is not your mother’s early menopause, according to Laurie McKenzie, MD, a reproductive endocrinologist and associate professor of ob.gyn. at the University of Texas MD Anderson Cancer Center with a joint appointment at Baylor College of Medicine, both in Houston.
Known previously as primary ovarian failure, the syndrome of primary ovarian insufficiency (POI) no longer refers to a failure in part because of the term’s negative connotations but mostly because it’s not precisely accurate, Dr. McKenzie told attendees at the 2021 annual meeting of the American College of Obstetricians and Gynecologists on May 1.
“Many of these women, especially early on in diagnosis, may be experiencing some intermittent ovarian function, so it may not be a complete failure of the ovaries,” Dr. McKenzie said.
Although the condition is not common, affecting about 1% of the female population, “it’s the kind of thing that when a gynecologist has someone who has this walk into their office, you really need to know how to address it because these women are understandably very distressed.” Lauren Streicher, MD, a clinical professor of obstetrics and gynecology at Northwestern University, Chicago, said in an interview after attending the talk.
Women who develop POI lose ovarian activity before age 40, characterized by menstrual disturbance with raised gonadotropins and low estradiol. Symptoms include the hot flushes and night sweats characteristic of estrogen deficiency as well as vaginal symptoms, including dyspareunia and dryness. Other symptoms can include sleep disturbance, mood changes, poor concentration, stiffness, dry eyes, altered urinary frequency, low libido, and lack of energy.
Dr. McKenzie urged doctors to ask women about their symptoms if they present with amenorrhea because young women with primary amenorrhea rarely experience symptoms at presentation, “implying that these symptoms are due to estrogen withdrawal rather than estrogen deficiency,” she said. Diagnosis involves confirmation of 4-6 months of amenorrhea or oligomenorrhea and two measurements of elevated follicle-stimulating hormone (FSH). Following this work-up, clinicians should seek the cause of the condition.
Etiology of POI and associated conditions
A wide range of conditions or genetic factors can cause POI or be more likely in patients with POI, Dr. McKenzie said. Many women diagnosed with POI have chromosomal abnormalities, and there is no cutoff for genetic testing, she said. Most of these genetic causes (94%) are X chromosome abnormalities, including Turners-associated dysmorphic features, gonadal dysgenesis, and FMR1 anomalies. Autosomal gene mutations could also play a role in POI.
Although women with the full FMR1 mutation (Fragile X syndrome) do not have an increased risk of POI, those with the premutation (55-200 repeats) have a 13%-26% increased risk of developing POI, albeit no increased risk of intellectual disability. About 0.8%-7.5% of women with sporadic POI and up to 13% of women with a family history of POI have this genetic anomaly.
Autoimmune conditions may also develop or be related to POI, including hypothyroidism and adrenal insufficiency, Dr. McKenzie said. About 20% of adults with POI will develop hypothyroidism, so testing every 1-2 years is reasonable, though no formal screening guidelines exist. In women whose cause of POI is unknown or in whom you suspect an immune disorder, clinicians may consider screening for 21OH-Ab or adrenocortical antibodies. Patients with a positive 21OH-Ab or adrenocortical antibodies test should be referred to an endocrinologist to test adrenal function and rule out Addison disease.
Though diabetes mellitus has been linked to POI, not enough evidence exists to recommend screening women with POI for diabetes. There’s similarly no indication for infection screening, but infections can cause POI. Mumps oophoritis, for example, accounts for 3%-7% of POI cases. Cancer therapy, including radiotherapy and chemotherapy, and surgical treatment for cancer can result in POI.
“Smoking, alcohol, nutrition, and exposure to endocrine disruptors are implicated as influencing the age of menopause but are not readily diagnosable causes of POI,” Dr. McKenzie said. “Although not proven to cause POI, cigarette smoking is toxic to the ovaries and has been linked to an earlier age at menopause.” Then there are many women whose cause of POI is unknown.
To take all these possibilities into account, Dr. McKenzie described the complete diagnostic work-up recommended by ACOG:
- Menstrual irregularity for at least 3-4 months
- Test FSH and estradiol
- Test hCG, TSH, and prolactin
- If diagnosis is confirmed, test karyotype, FMR1 premutation, adrenal antibodies, and a pelvic sonogram.
However, she added during the Q&A after her talk, she is not sure why a sonogram is recommended or what additional information it might provide.
Long-term consequences of POI
Dr McKenzie noted that one study found a 2-year reduction in life expectancy among women who developed menopause before age 40. The reduced life expectancy linked to untreated POI is primarily caused by cardiovascular disease, she said. Women who undergo menopause aged between 35 and 40 years have a 50% greater risk of death related to ischemic heart disease than those ages 49-51, after adjusting for other comorbidities and confounders.
“Women with primary ovarian insufficiency should be advised on how to reduce cardiovascular risk factors by not smoking, taking regular exercise, and maintaining a healthy weight,” Dr McKenzie said.
No interventions have been shown to increase ovarian activity
Though fertility is substantially reduced in women with POI, it may not be completely gone. Several studies have found pregnancy rates ranging from 1.5% to 4.8%, and one study found that 25% of women with idiopathic POI had some evidence of ovarian function. Clinicians should therefore recommend women with POI use contraception if they do not want to conceive. Egg donation is an option for preserving fertility in women with POI but only before POI is solidly established.
“No interventions have been reliably shown to increase ovarian activity and natural conception rates,” Dr. McKenzie said.
For women who survive childhood or adolescent cancer and become pregnant, no evidence has shown an increased risk of congenital anomalies, but risk of low birth weight is elevated in babies whose mothers received anthracyclines. Treatment with anthracyclines and mediastinal radiotherapy have also been linked with cardiomyopathy and heart failure, so an echocardiogram prior to pregnancy is indicated in women with exposure to these or high-dose cyclophosphamide.
Abdominopelvic radiotherapy, however, has been linked to poor uterine function with a greater risk of late miscarriage, prematurity, low birth weight, stillbirth, neonatal hemorrhage, and postpartum hemorrhage.
“Pregnancies in women with Turner syndrome are very high risk and may have a maternal mortality as high as 3.5%,” Dr. McKenzie said, so these pregnancies require involvement of a cardiologist.
Other sequelae of POI can include increased bone resorption, net loss of bone (2%-3% annually soon after menopause) and reduced bone mineral density. Women should be getting 1,000 mg/day of calcium and 800 IU/day of vitamin D, but bone screening remains controversial in the field. Finally, providers should not ignore psychosocial effects of POI, including grief, diminished self esteem, and sadness, even more so, potentially, among adolescents.
Treatment of POI
Managing POI involves a two-pronged strategy of providing enough estrogen (estradiol, ethinyl estradiol, or conjugated equine estrogens) to mimic normal physiology and enough progestogen (synthetic or progesterone) to protect the endometrium from the mitogenic effect of estrogen.
The two primary options are hormone therapy and combination oral contraceptives. Hormone therapy might allow ovulation and pregnancy in some women, but combination oral contraceptive may feel less stigmatized in those who are still young, albeit with a potential risk for venous thromboembolism.
Continuous treatment tends to be easier and can involve breakthrough bleeding in younger patients; in postmenopausal women, breast cancer risk is higher but endometrial cancer risk is lower. Cyclic treatment mimics the endometrium’s normal function, resulting in bleeding that may help some women feel more “normal” and aids in knowing about a pregnancy. Those wanting to avoid bleeds and use contraception can use the levonorgestrel IUD off label.
Dr. Streicher said in an interview, “Not only is it critically important to recognize [long-term consequences] in this small group of women, but the lessons learned from young women who go though menopause can absolutely be extrapolated to women who go through menopause at an appropriate time.”
Dr. McKenzie had no disclosures. Dr. Streicher has consulted for Astellas Pharma and Church & Dwight, and she owns investments in InControl Medical and Sermonix Pharmaceutical.
Primary ovarian insufficiency is not your mother’s early menopause, according to Laurie McKenzie, MD, a reproductive endocrinologist and associate professor of ob.gyn. at the University of Texas MD Anderson Cancer Center with a joint appointment at Baylor College of Medicine, both in Houston.
Known previously as primary ovarian failure, the syndrome of primary ovarian insufficiency (POI) no longer refers to a failure in part because of the term’s negative connotations but mostly because it’s not precisely accurate, Dr. McKenzie told attendees at the 2021 annual meeting of the American College of Obstetricians and Gynecologists on May 1.
“Many of these women, especially early on in diagnosis, may be experiencing some intermittent ovarian function, so it may not be a complete failure of the ovaries,” Dr. McKenzie said.
Although the condition is not common, affecting about 1% of the female population, “it’s the kind of thing that when a gynecologist has someone who has this walk into their office, you really need to know how to address it because these women are understandably very distressed.” Lauren Streicher, MD, a clinical professor of obstetrics and gynecology at Northwestern University, Chicago, said in an interview after attending the talk.
Women who develop POI lose ovarian activity before age 40, characterized by menstrual disturbance with raised gonadotropins and low estradiol. Symptoms include the hot flushes and night sweats characteristic of estrogen deficiency as well as vaginal symptoms, including dyspareunia and dryness. Other symptoms can include sleep disturbance, mood changes, poor concentration, stiffness, dry eyes, altered urinary frequency, low libido, and lack of energy.
Dr. McKenzie urged doctors to ask women about their symptoms if they present with amenorrhea because young women with primary amenorrhea rarely experience symptoms at presentation, “implying that these symptoms are due to estrogen withdrawal rather than estrogen deficiency,” she said. Diagnosis involves confirmation of 4-6 months of amenorrhea or oligomenorrhea and two measurements of elevated follicle-stimulating hormone (FSH). Following this work-up, clinicians should seek the cause of the condition.
Etiology of POI and associated conditions
A wide range of conditions or genetic factors can cause POI or be more likely in patients with POI, Dr. McKenzie said. Many women diagnosed with POI have chromosomal abnormalities, and there is no cutoff for genetic testing, she said. Most of these genetic causes (94%) are X chromosome abnormalities, including Turners-associated dysmorphic features, gonadal dysgenesis, and FMR1 anomalies. Autosomal gene mutations could also play a role in POI.
Although women with the full FMR1 mutation (Fragile X syndrome) do not have an increased risk of POI, those with the premutation (55-200 repeats) have a 13%-26% increased risk of developing POI, albeit no increased risk of intellectual disability. About 0.8%-7.5% of women with sporadic POI and up to 13% of women with a family history of POI have this genetic anomaly.
Autoimmune conditions may also develop or be related to POI, including hypothyroidism and adrenal insufficiency, Dr. McKenzie said. About 20% of adults with POI will develop hypothyroidism, so testing every 1-2 years is reasonable, though no formal screening guidelines exist. In women whose cause of POI is unknown or in whom you suspect an immune disorder, clinicians may consider screening for 21OH-Ab or adrenocortical antibodies. Patients with a positive 21OH-Ab or adrenocortical antibodies test should be referred to an endocrinologist to test adrenal function and rule out Addison disease.
Though diabetes mellitus has been linked to POI, not enough evidence exists to recommend screening women with POI for diabetes. There’s similarly no indication for infection screening, but infections can cause POI. Mumps oophoritis, for example, accounts for 3%-7% of POI cases. Cancer therapy, including radiotherapy and chemotherapy, and surgical treatment for cancer can result in POI.
“Smoking, alcohol, nutrition, and exposure to endocrine disruptors are implicated as influencing the age of menopause but are not readily diagnosable causes of POI,” Dr. McKenzie said. “Although not proven to cause POI, cigarette smoking is toxic to the ovaries and has been linked to an earlier age at menopause.” Then there are many women whose cause of POI is unknown.
To take all these possibilities into account, Dr. McKenzie described the complete diagnostic work-up recommended by ACOG:
- Menstrual irregularity for at least 3-4 months
- Test FSH and estradiol
- Test hCG, TSH, and prolactin
- If diagnosis is confirmed, test karyotype, FMR1 premutation, adrenal antibodies, and a pelvic sonogram.
However, she added during the Q&A after her talk, she is not sure why a sonogram is recommended or what additional information it might provide.
Long-term consequences of POI
Dr McKenzie noted that one study found a 2-year reduction in life expectancy among women who developed menopause before age 40. The reduced life expectancy linked to untreated POI is primarily caused by cardiovascular disease, she said. Women who undergo menopause aged between 35 and 40 years have a 50% greater risk of death related to ischemic heart disease than those ages 49-51, after adjusting for other comorbidities and confounders.
“Women with primary ovarian insufficiency should be advised on how to reduce cardiovascular risk factors by not smoking, taking regular exercise, and maintaining a healthy weight,” Dr McKenzie said.
No interventions have been shown to increase ovarian activity
Though fertility is substantially reduced in women with POI, it may not be completely gone. Several studies have found pregnancy rates ranging from 1.5% to 4.8%, and one study found that 25% of women with idiopathic POI had some evidence of ovarian function. Clinicians should therefore recommend women with POI use contraception if they do not want to conceive. Egg donation is an option for preserving fertility in women with POI but only before POI is solidly established.
“No interventions have been reliably shown to increase ovarian activity and natural conception rates,” Dr. McKenzie said.
For women who survive childhood or adolescent cancer and become pregnant, no evidence has shown an increased risk of congenital anomalies, but risk of low birth weight is elevated in babies whose mothers received anthracyclines. Treatment with anthracyclines and mediastinal radiotherapy have also been linked with cardiomyopathy and heart failure, so an echocardiogram prior to pregnancy is indicated in women with exposure to these or high-dose cyclophosphamide.
Abdominopelvic radiotherapy, however, has been linked to poor uterine function with a greater risk of late miscarriage, prematurity, low birth weight, stillbirth, neonatal hemorrhage, and postpartum hemorrhage.
“Pregnancies in women with Turner syndrome are very high risk and may have a maternal mortality as high as 3.5%,” Dr. McKenzie said, so these pregnancies require involvement of a cardiologist.
Other sequelae of POI can include increased bone resorption, net loss of bone (2%-3% annually soon after menopause) and reduced bone mineral density. Women should be getting 1,000 mg/day of calcium and 800 IU/day of vitamin D, but bone screening remains controversial in the field. Finally, providers should not ignore psychosocial effects of POI, including grief, diminished self esteem, and sadness, even more so, potentially, among adolescents.
Treatment of POI
Managing POI involves a two-pronged strategy of providing enough estrogen (estradiol, ethinyl estradiol, or conjugated equine estrogens) to mimic normal physiology and enough progestogen (synthetic or progesterone) to protect the endometrium from the mitogenic effect of estrogen.
The two primary options are hormone therapy and combination oral contraceptives. Hormone therapy might allow ovulation and pregnancy in some women, but combination oral contraceptive may feel less stigmatized in those who are still young, albeit with a potential risk for venous thromboembolism.
Continuous treatment tends to be easier and can involve breakthrough bleeding in younger patients; in postmenopausal women, breast cancer risk is higher but endometrial cancer risk is lower. Cyclic treatment mimics the endometrium’s normal function, resulting in bleeding that may help some women feel more “normal” and aids in knowing about a pregnancy. Those wanting to avoid bleeds and use contraception can use the levonorgestrel IUD off label.
Dr. Streicher said in an interview, “Not only is it critically important to recognize [long-term consequences] in this small group of women, but the lessons learned from young women who go though menopause can absolutely be extrapolated to women who go through menopause at an appropriate time.”
Dr. McKenzie had no disclosures. Dr. Streicher has consulted for Astellas Pharma and Church & Dwight, and she owns investments in InControl Medical and Sermonix Pharmaceutical.
Primary ovarian insufficiency is not your mother’s early menopause, according to Laurie McKenzie, MD, a reproductive endocrinologist and associate professor of ob.gyn. at the University of Texas MD Anderson Cancer Center with a joint appointment at Baylor College of Medicine, both in Houston.
Known previously as primary ovarian failure, the syndrome of primary ovarian insufficiency (POI) no longer refers to a failure in part because of the term’s negative connotations but mostly because it’s not precisely accurate, Dr. McKenzie told attendees at the 2021 annual meeting of the American College of Obstetricians and Gynecologists on May 1.
“Many of these women, especially early on in diagnosis, may be experiencing some intermittent ovarian function, so it may not be a complete failure of the ovaries,” Dr. McKenzie said.
Although the condition is not common, affecting about 1% of the female population, “it’s the kind of thing that when a gynecologist has someone who has this walk into their office, you really need to know how to address it because these women are understandably very distressed.” Lauren Streicher, MD, a clinical professor of obstetrics and gynecology at Northwestern University, Chicago, said in an interview after attending the talk.
Women who develop POI lose ovarian activity before age 40, characterized by menstrual disturbance with raised gonadotropins and low estradiol. Symptoms include the hot flushes and night sweats characteristic of estrogen deficiency as well as vaginal symptoms, including dyspareunia and dryness. Other symptoms can include sleep disturbance, mood changes, poor concentration, stiffness, dry eyes, altered urinary frequency, low libido, and lack of energy.
Dr. McKenzie urged doctors to ask women about their symptoms if they present with amenorrhea because young women with primary amenorrhea rarely experience symptoms at presentation, “implying that these symptoms are due to estrogen withdrawal rather than estrogen deficiency,” she said. Diagnosis involves confirmation of 4-6 months of amenorrhea or oligomenorrhea and two measurements of elevated follicle-stimulating hormone (FSH). Following this work-up, clinicians should seek the cause of the condition.
Etiology of POI and associated conditions
A wide range of conditions or genetic factors can cause POI or be more likely in patients with POI, Dr. McKenzie said. Many women diagnosed with POI have chromosomal abnormalities, and there is no cutoff for genetic testing, she said. Most of these genetic causes (94%) are X chromosome abnormalities, including Turners-associated dysmorphic features, gonadal dysgenesis, and FMR1 anomalies. Autosomal gene mutations could also play a role in POI.
Although women with the full FMR1 mutation (Fragile X syndrome) do not have an increased risk of POI, those with the premutation (55-200 repeats) have a 13%-26% increased risk of developing POI, albeit no increased risk of intellectual disability. About 0.8%-7.5% of women with sporadic POI and up to 13% of women with a family history of POI have this genetic anomaly.
Autoimmune conditions may also develop or be related to POI, including hypothyroidism and adrenal insufficiency, Dr. McKenzie said. About 20% of adults with POI will develop hypothyroidism, so testing every 1-2 years is reasonable, though no formal screening guidelines exist. In women whose cause of POI is unknown or in whom you suspect an immune disorder, clinicians may consider screening for 21OH-Ab or adrenocortical antibodies. Patients with a positive 21OH-Ab or adrenocortical antibodies test should be referred to an endocrinologist to test adrenal function and rule out Addison disease.
Though diabetes mellitus has been linked to POI, not enough evidence exists to recommend screening women with POI for diabetes. There’s similarly no indication for infection screening, but infections can cause POI. Mumps oophoritis, for example, accounts for 3%-7% of POI cases. Cancer therapy, including radiotherapy and chemotherapy, and surgical treatment for cancer can result in POI.
“Smoking, alcohol, nutrition, and exposure to endocrine disruptors are implicated as influencing the age of menopause but are not readily diagnosable causes of POI,” Dr. McKenzie said. “Although not proven to cause POI, cigarette smoking is toxic to the ovaries and has been linked to an earlier age at menopause.” Then there are many women whose cause of POI is unknown.
To take all these possibilities into account, Dr. McKenzie described the complete diagnostic work-up recommended by ACOG:
- Menstrual irregularity for at least 3-4 months
- Test FSH and estradiol
- Test hCG, TSH, and prolactin
- If diagnosis is confirmed, test karyotype, FMR1 premutation, adrenal antibodies, and a pelvic sonogram.
However, she added during the Q&A after her talk, she is not sure why a sonogram is recommended or what additional information it might provide.
Long-term consequences of POI
Dr McKenzie noted that one study found a 2-year reduction in life expectancy among women who developed menopause before age 40. The reduced life expectancy linked to untreated POI is primarily caused by cardiovascular disease, she said. Women who undergo menopause aged between 35 and 40 years have a 50% greater risk of death related to ischemic heart disease than those ages 49-51, after adjusting for other comorbidities and confounders.
“Women with primary ovarian insufficiency should be advised on how to reduce cardiovascular risk factors by not smoking, taking regular exercise, and maintaining a healthy weight,” Dr McKenzie said.
No interventions have been shown to increase ovarian activity
Though fertility is substantially reduced in women with POI, it may not be completely gone. Several studies have found pregnancy rates ranging from 1.5% to 4.8%, and one study found that 25% of women with idiopathic POI had some evidence of ovarian function. Clinicians should therefore recommend women with POI use contraception if they do not want to conceive. Egg donation is an option for preserving fertility in women with POI but only before POI is solidly established.
“No interventions have been reliably shown to increase ovarian activity and natural conception rates,” Dr. McKenzie said.
For women who survive childhood or adolescent cancer and become pregnant, no evidence has shown an increased risk of congenital anomalies, but risk of low birth weight is elevated in babies whose mothers received anthracyclines. Treatment with anthracyclines and mediastinal radiotherapy have also been linked with cardiomyopathy and heart failure, so an echocardiogram prior to pregnancy is indicated in women with exposure to these or high-dose cyclophosphamide.
Abdominopelvic radiotherapy, however, has been linked to poor uterine function with a greater risk of late miscarriage, prematurity, low birth weight, stillbirth, neonatal hemorrhage, and postpartum hemorrhage.
“Pregnancies in women with Turner syndrome are very high risk and may have a maternal mortality as high as 3.5%,” Dr. McKenzie said, so these pregnancies require involvement of a cardiologist.
Other sequelae of POI can include increased bone resorption, net loss of bone (2%-3% annually soon after menopause) and reduced bone mineral density. Women should be getting 1,000 mg/day of calcium and 800 IU/day of vitamin D, but bone screening remains controversial in the field. Finally, providers should not ignore psychosocial effects of POI, including grief, diminished self esteem, and sadness, even more so, potentially, among adolescents.
Treatment of POI
Managing POI involves a two-pronged strategy of providing enough estrogen (estradiol, ethinyl estradiol, or conjugated equine estrogens) to mimic normal physiology and enough progestogen (synthetic or progesterone) to protect the endometrium from the mitogenic effect of estrogen.
The two primary options are hormone therapy and combination oral contraceptives. Hormone therapy might allow ovulation and pregnancy in some women, but combination oral contraceptive may feel less stigmatized in those who are still young, albeit with a potential risk for venous thromboembolism.
Continuous treatment tends to be easier and can involve breakthrough bleeding in younger patients; in postmenopausal women, breast cancer risk is higher but endometrial cancer risk is lower. Cyclic treatment mimics the endometrium’s normal function, resulting in bleeding that may help some women feel more “normal” and aids in knowing about a pregnancy. Those wanting to avoid bleeds and use contraception can use the levonorgestrel IUD off label.
Dr. Streicher said in an interview, “Not only is it critically important to recognize [long-term consequences] in this small group of women, but the lessons learned from young women who go though menopause can absolutely be extrapolated to women who go through menopause at an appropriate time.”
Dr. McKenzie had no disclosures. Dr. Streicher has consulted for Astellas Pharma and Church & Dwight, and she owns investments in InControl Medical and Sermonix Pharmaceutical.
FROM ACOG 2021
Heavy cannabis use in pregnancy correlates with risks to infant
Cannabis use that interferes with a woman’s ability to function during pregnancy is a risk factor for severe health problems in the child, new research indicates.
Pregnant women with cannabis use disorder are more likely to have children with low birth weights and children who die within 1 year of birth, compared with matched controls, according to a study published online in Addiction.
The death rate among infants exposed to prenatal cannabis use disorder was 0.98%, compared with 0.75% among infants whose mothers did not have this diagnosis.
Cannabis use disorder during pregnancy “has increased dramatically in the past two decades,” but few studies have examined the health impacts on offspring, study author Yuyan Shi, PhD, said in an interview. “It is particularly concerning in states with cannabis legalization where cannabis is increasingly available.”
Dr. Shi, a researcher at the Herbert Wertheim School of Public Health and Human Longevity Science at the University of California, San Diego, and colleagues analyzed data from more than 4.8 million mothers who delivered a live singleton birth in California between 2001 and 2012 and their infants. They focused on 20,237 mothers who had a diagnosis of cannabis use disorder at delivery. The disorder is defined by continued use of the drug despite impairments in physical, psychological, and social functioning.
The researchers matched mothers with cannabis use disorder 1:2 to mothers who did not have this diagnosis. They aimed to balance factors such as maternal age, educational attainment, health insurance, physical and mental health conditions, prenatal care, and alcohol and opioid use disorder.
An increasingly common diagnosis
Over the study period, the rate of cannabis use disorder increased from 2.8 cases per 1,000 deliveries in 2001 to 6.9 cases per 1,000 deliveries in 2012.
Cannabis use disorder was associated with increased odds of preterm birth (odds ratio, 1.06), small for gestational age (OR, 1.13), low birth weight (OR, 1.13), and death within 1 year of birth (OR, 1.35), according to the researchers’ estimates. Cannabis use disorder was associated with lower odds of hospitalization within 1 year of birth, however (OR, 0.91).
“The most notable observation is that exposed infants were 35% more likely to die within 1 year of birth than unexposed infants,” Dr. Shi and colleagues wrote. More research is needed to understand the causes of death at different stages of infancy, they said.
The results “imply that cannabis use disorder screening as well as appropriate education, counseling, or referral to substance abuse treatment services should be encouraged among pregnant women,” Dr. Shi said.
The study does not establish that cannabis use disorder causes adverse effects, and it is not clear how the results might apply to mothers who use cannabis but do not meet diagnostic criteria for the disorder, the authors noted.
“Presumably the health consequences of mothers who use cannabis but do not meet the criteria ... are less severe than mothers with cannabis use disorder,” Dr. Shi said. “Unfortunately, no research has been conducted to test this hypothesis.”
Enough data to recommend abstaining
Many clinicians may not feel equipped to make a diagnosis of cannabis use disorder, said Jamie Lo, MD, assistant professor of obstetrics and gynecology at Oregon Health and Science University in Portland.
Although many clinicians ask patients about substance use in general, specifically screening for cannabis use is not necessarily routine practice. “I think people are starting to adopt that, but it probably will take a little bit of time,” Dr. Lo said.
Dr. Lo, who was not involved in the study, researches the effects of marijuana during pregnancy.
Confounding factors such as frequent co-use of tobacco have so far made it “difficult to suss out” whether observed effects are directly from cannabis use, other substances or exposures, or a combination, said Dr. Lo. The possibility that stigma may lead to inaccurate self-reporting poses another challenge. And the range of cannabis delivery devices further complicates matters.
“It is hard to compare smoking a bowl versus a joint versus using the oils or CBD or edibles,” Dr. Lo said. The data regarding cigarettes and alcohol are cleaner and more precise, in comparison.
Still, federal agencies and professional societies agree that “what we do know is enough to recommend that pregnant women abstain from using cannabis during pregnancy,” Dr. Lo said.
The National Institute on Drug Abuse, which funded the study, said the results add to the evidence that prenatal exposure to cannabis may be associated with poor birth outcomes and infant health.
“While we cannot establish that cannabis use caused negative outcomes in this study, these data reinforce the case for caution around using cannabis during pregnancy,” Nora D. Volkow, MD, the director of the agency, said in a news release.
“Careful analysis of data like these is one way we can responsibly study how cannabis use affects the developing child, all while a natural experiment is playing out across our country in places where cannabis is becoming widely available to pregnant consumers.”
The study authors and Dr. Lo had no disclosures.
Cannabis use that interferes with a woman’s ability to function during pregnancy is a risk factor for severe health problems in the child, new research indicates.
Pregnant women with cannabis use disorder are more likely to have children with low birth weights and children who die within 1 year of birth, compared with matched controls, according to a study published online in Addiction.
The death rate among infants exposed to prenatal cannabis use disorder was 0.98%, compared with 0.75% among infants whose mothers did not have this diagnosis.
Cannabis use disorder during pregnancy “has increased dramatically in the past two decades,” but few studies have examined the health impacts on offspring, study author Yuyan Shi, PhD, said in an interview. “It is particularly concerning in states with cannabis legalization where cannabis is increasingly available.”
Dr. Shi, a researcher at the Herbert Wertheim School of Public Health and Human Longevity Science at the University of California, San Diego, and colleagues analyzed data from more than 4.8 million mothers who delivered a live singleton birth in California between 2001 and 2012 and their infants. They focused on 20,237 mothers who had a diagnosis of cannabis use disorder at delivery. The disorder is defined by continued use of the drug despite impairments in physical, psychological, and social functioning.
The researchers matched mothers with cannabis use disorder 1:2 to mothers who did not have this diagnosis. They aimed to balance factors such as maternal age, educational attainment, health insurance, physical and mental health conditions, prenatal care, and alcohol and opioid use disorder.
An increasingly common diagnosis
Over the study period, the rate of cannabis use disorder increased from 2.8 cases per 1,000 deliveries in 2001 to 6.9 cases per 1,000 deliveries in 2012.
Cannabis use disorder was associated with increased odds of preterm birth (odds ratio, 1.06), small for gestational age (OR, 1.13), low birth weight (OR, 1.13), and death within 1 year of birth (OR, 1.35), according to the researchers’ estimates. Cannabis use disorder was associated with lower odds of hospitalization within 1 year of birth, however (OR, 0.91).
“The most notable observation is that exposed infants were 35% more likely to die within 1 year of birth than unexposed infants,” Dr. Shi and colleagues wrote. More research is needed to understand the causes of death at different stages of infancy, they said.
The results “imply that cannabis use disorder screening as well as appropriate education, counseling, or referral to substance abuse treatment services should be encouraged among pregnant women,” Dr. Shi said.
The study does not establish that cannabis use disorder causes adverse effects, and it is not clear how the results might apply to mothers who use cannabis but do not meet diagnostic criteria for the disorder, the authors noted.
“Presumably the health consequences of mothers who use cannabis but do not meet the criteria ... are less severe than mothers with cannabis use disorder,” Dr. Shi said. “Unfortunately, no research has been conducted to test this hypothesis.”
Enough data to recommend abstaining
Many clinicians may not feel equipped to make a diagnosis of cannabis use disorder, said Jamie Lo, MD, assistant professor of obstetrics and gynecology at Oregon Health and Science University in Portland.
Although many clinicians ask patients about substance use in general, specifically screening for cannabis use is not necessarily routine practice. “I think people are starting to adopt that, but it probably will take a little bit of time,” Dr. Lo said.
Dr. Lo, who was not involved in the study, researches the effects of marijuana during pregnancy.
Confounding factors such as frequent co-use of tobacco have so far made it “difficult to suss out” whether observed effects are directly from cannabis use, other substances or exposures, or a combination, said Dr. Lo. The possibility that stigma may lead to inaccurate self-reporting poses another challenge. And the range of cannabis delivery devices further complicates matters.
“It is hard to compare smoking a bowl versus a joint versus using the oils or CBD or edibles,” Dr. Lo said. The data regarding cigarettes and alcohol are cleaner and more precise, in comparison.
Still, federal agencies and professional societies agree that “what we do know is enough to recommend that pregnant women abstain from using cannabis during pregnancy,” Dr. Lo said.
The National Institute on Drug Abuse, which funded the study, said the results add to the evidence that prenatal exposure to cannabis may be associated with poor birth outcomes and infant health.
“While we cannot establish that cannabis use caused negative outcomes in this study, these data reinforce the case for caution around using cannabis during pregnancy,” Nora D. Volkow, MD, the director of the agency, said in a news release.
“Careful analysis of data like these is one way we can responsibly study how cannabis use affects the developing child, all while a natural experiment is playing out across our country in places where cannabis is becoming widely available to pregnant consumers.”
The study authors and Dr. Lo had no disclosures.
Cannabis use that interferes with a woman’s ability to function during pregnancy is a risk factor for severe health problems in the child, new research indicates.
Pregnant women with cannabis use disorder are more likely to have children with low birth weights and children who die within 1 year of birth, compared with matched controls, according to a study published online in Addiction.
The death rate among infants exposed to prenatal cannabis use disorder was 0.98%, compared with 0.75% among infants whose mothers did not have this diagnosis.
Cannabis use disorder during pregnancy “has increased dramatically in the past two decades,” but few studies have examined the health impacts on offspring, study author Yuyan Shi, PhD, said in an interview. “It is particularly concerning in states with cannabis legalization where cannabis is increasingly available.”
Dr. Shi, a researcher at the Herbert Wertheim School of Public Health and Human Longevity Science at the University of California, San Diego, and colleagues analyzed data from more than 4.8 million mothers who delivered a live singleton birth in California between 2001 and 2012 and their infants. They focused on 20,237 mothers who had a diagnosis of cannabis use disorder at delivery. The disorder is defined by continued use of the drug despite impairments in physical, psychological, and social functioning.
The researchers matched mothers with cannabis use disorder 1:2 to mothers who did not have this diagnosis. They aimed to balance factors such as maternal age, educational attainment, health insurance, physical and mental health conditions, prenatal care, and alcohol and opioid use disorder.
An increasingly common diagnosis
Over the study period, the rate of cannabis use disorder increased from 2.8 cases per 1,000 deliveries in 2001 to 6.9 cases per 1,000 deliveries in 2012.
Cannabis use disorder was associated with increased odds of preterm birth (odds ratio, 1.06), small for gestational age (OR, 1.13), low birth weight (OR, 1.13), and death within 1 year of birth (OR, 1.35), according to the researchers’ estimates. Cannabis use disorder was associated with lower odds of hospitalization within 1 year of birth, however (OR, 0.91).
“The most notable observation is that exposed infants were 35% more likely to die within 1 year of birth than unexposed infants,” Dr. Shi and colleagues wrote. More research is needed to understand the causes of death at different stages of infancy, they said.
The results “imply that cannabis use disorder screening as well as appropriate education, counseling, or referral to substance abuse treatment services should be encouraged among pregnant women,” Dr. Shi said.
The study does not establish that cannabis use disorder causes adverse effects, and it is not clear how the results might apply to mothers who use cannabis but do not meet diagnostic criteria for the disorder, the authors noted.
“Presumably the health consequences of mothers who use cannabis but do not meet the criteria ... are less severe than mothers with cannabis use disorder,” Dr. Shi said. “Unfortunately, no research has been conducted to test this hypothesis.”
Enough data to recommend abstaining
Many clinicians may not feel equipped to make a diagnosis of cannabis use disorder, said Jamie Lo, MD, assistant professor of obstetrics and gynecology at Oregon Health and Science University in Portland.
Although many clinicians ask patients about substance use in general, specifically screening for cannabis use is not necessarily routine practice. “I think people are starting to adopt that, but it probably will take a little bit of time,” Dr. Lo said.
Dr. Lo, who was not involved in the study, researches the effects of marijuana during pregnancy.
Confounding factors such as frequent co-use of tobacco have so far made it “difficult to suss out” whether observed effects are directly from cannabis use, other substances or exposures, or a combination, said Dr. Lo. The possibility that stigma may lead to inaccurate self-reporting poses another challenge. And the range of cannabis delivery devices further complicates matters.
“It is hard to compare smoking a bowl versus a joint versus using the oils or CBD or edibles,” Dr. Lo said. The data regarding cigarettes and alcohol are cleaner and more precise, in comparison.
Still, federal agencies and professional societies agree that “what we do know is enough to recommend that pregnant women abstain from using cannabis during pregnancy,” Dr. Lo said.
The National Institute on Drug Abuse, which funded the study, said the results add to the evidence that prenatal exposure to cannabis may be associated with poor birth outcomes and infant health.
“While we cannot establish that cannabis use caused negative outcomes in this study, these data reinforce the case for caution around using cannabis during pregnancy,” Nora D. Volkow, MD, the director of the agency, said in a news release.
“Careful analysis of data like these is one way we can responsibly study how cannabis use affects the developing child, all while a natural experiment is playing out across our country in places where cannabis is becoming widely available to pregnant consumers.”
The study authors and Dr. Lo had no disclosures.
The financial advantages of medical scribes extend beyond increased visits
ABSTRACT
Purpose Medical scribes are known to increase revenue by increasing visits to a medical practice. We examined whether medical scribes are associated with markers of financial benefit independent of increased visits.
Methods We conducted a pre- and post-observational study with a control group, examining changes in the percentage of visits (1) coded as level of service 4 or 5, (2) with at least 1 hierarchical condition category code billed, and (3) at which orders for 3 pay-for-performance quality measures (screening for breast, cervical, and colon cancer) were placed, if due. We looked at changes in outcomes among scribed providers and compared them to nonscribed providers. We used generalized estimating equations with robust standard errors to account for repeated measures and the hierarchical nature of the data, controlling for patient demographics.
Results We examined 41,371 visits to 17 scribed providers and 230,297 visits to 78 nonscribed providers. In adjusted analyses, and compared to nonscribed providers, scribes were associated with an increase of:
- Frutiger LT Std9.2 percentage points in level-of-service 4 or 5 billing (Frutiger LT StdP < .001)
- 3.6 percentage points in hierarchical condition category coding (Frutiger LT StdP < .001)
- 4.0 percentage points in breast cancer screening orders (Frutiger LT StdP = .01)
- 4.9 percentage points in colon cancer screening orders (Frutiger LT StdPFrutiger LT Std = .04).
Conclusions This study suggests that scribes are associated with financial benefit in addition to increased visit volume. Primary care practices should consider the financial benefit of scribes independent of their ability to add patient volume.
Increasingly, medical scribes are used in ambulatory care settings across the United States.1 Scribes are trained personnel who accompany providers during visits to provide documentation support and assist with other administrative tasks. They are associated with reduced documentation time for providers2-6 and improved provider satisfaction,7-11 without detriment to4-16 (or with possible improvement in17-20) patient satisfaction in ambulatory care settings. At the same time, concerns remain that using scribes might inhibit patient communication, harm clinical reasoning, reduce the effectiveness of clinical decision-support tools, and simply serve as a work-around to fixing inefficiencies in the electronic medical record (EMR).21-23
A driving force for the increased use of medical scribes is the expectation that they reduce the cost of providing care. Cost-efficiency is typically described as resulting from a reduction in physician time per patient seen, which allows increased patient volume and, in turn, drives increased physician productivity.2,8,10,18,24-27 Whether scribes result in cost savings remains unclear; some papers suggest that scribes are cost efficient in ambulatory care,2,10,18 while others have been unable to identify cost savings, particularly in primary care.4
One reason why scribes might not be associated with cost savings is that their financial benefit might be undercounted. Studies that focus on increased volume miss the opportunity to capture financial benefits conferred through mechanisms that are independent of seeing more patients:
- Scribes might help providers address and document more, and more complex, medical problems, allowing higher level-of-service (LOS) billing. For example, a provider chooses a lower LOS because they have insufficiently documented a visit to support a higher LOS; by assisting with documentation, the scribe might allow the provider to choose a higher LOS.
- Scribes might prompt a provider to use decision-support tools for risk coding (using appropriate medical codes to capture the patient’s level of medical complexity), thereby increasing reimbursement.
- Scribes might extend the time available during the visit for the provider to address pay-for-performance quality measures, such as cancer screening.
Continue to: Making visits count, not counting visits
Making visits count, not counting visits. In this study, we examined whether medical scribes in primary care are associated with improved markers of revenue that are independent of seeing more patients. Specifically, we examined whether scribes are associated with increased LOS coding, risk coding, and orders for pay-for-performance measures for all primary care visits and for nonpreventive primary care visits.
Methods
Design
This observational study compared the change in outcomes before implementation of scribes and during implementation of scribes, between scribed providers and nonscribed providers. We compared visits during the year prior to the implementation of scribes (July 2017–June 2018) with the year during their implementation (July 2018–2019).
The Cambridge Health Alliance Institutional Review Board considered this study exempt from review.
Setting
This study was conducted at a safety-net community academic health system that uses an EMR developed by Epic Systems [Verona, WI]. This EMR includes decision-support tools that prompt providers when pay-for-performance quality measures are due and when hierarchical condition category (HCC) codes—ie, specific diagnoses used by Medicare and other payers to reimburse providers for the complexity of their patients—might apply to the visit.
These EMR decision-support tools use algorithms that draw on age, gender, diagnoses that were billed previously or are on the problem list, laboratory findings, and prior imaging. They alert physicians when a patient is due for pay-for-performance quality measures, such as cancer screenings, and when HCC codes might be applicable.
Continue to: During the study period...
During the study period, the EMR decision-support tool for HCC coding underwent several changes designed to improve HCC coding. In addition, systematic changes to primary care visits took place, leading to an increase in the number of patients seen and screenings required.
Outcomes
We examined 2 categories of outcomes that confer financial benefit to many institutions: billing measures and pay-for-performance measures.
Billing measures included the percentage of visits (1) coded as LOS 4 or 5 and (2) with at least 1 HCC code billed (among those for which the decision-support tool identified at least 1 potential HCC code).
Pay-for-performance measures. We examined whether any of 3 pay-for-performance quality measures were addressed during the visit, selecting 3 that are commonly addressed by primary care providers (PCPs) and that require PCPs to sign an order for screening during a primary care visit: breast cancer (mammography order), cervical cancer (Papanicolaou smear order), and colon cancer (an order for fecal occult blood testing or colonoscopy).
Intervention
Scribes were employees of Cambridge Health Alliance who had recently graduated from college and were interested in a career as a health care professional. Scribes received 3 days of training on how to function effectively in their role; 1 day of training in EMR functionality; and 2 hours of training on decision-support tools for pay-for-performance quality measures and risk coding. Scribes continued learning on the job through feedback from supervising PCPs. Scribes documented patient encounters, recording histories and findings on the physical exam and transcribing discussion of treatment plans and the PCP’s instructions to patients.
Continue to: The 14 scribes worked with 17 physician...
The 14 scribes worked with 17 physician and nurse practitioner PCPs beginning in July 2018. Participation by PCPs was voluntary; they received no compensation for participating in the scribe program. PCPs were not required to see additional patients to participate. PCPs who chose to work with a scribe were similar to those who declined a scribe, as regards gender, race, type of provider (MD or NP), tenure at the institution, and percentage of time in clinical work (see Table W-1).
The control group comprised providers who elected not to work with a scribe but who worked in the same clinics as the intervention providers.
Scribes were assigned to a PCP based on availability during the PCP’s scheduled hours and worked with 1 PCP throughout the intervention (except for 1 PCP who worked with 2 scribes). All PCPs worked with their scribe(s) part time; on average, 49% of intervention PCPs’ visits were scribed.
Inclusion and exclusion criteria
Because the first year at an institution is a learning period for PCPs, we excluded those who worked at the institution for < 1 year before the start of the scribe program (n = 12). Based on the extensive clinical experience of 1 PCP (WA) with scribes, we excluded the first 200 visits or 6 weeks (whichever occurred first) with a scribe among all scribed providers, to account for an initial learning period (n = 2202, of 15,372 scribed visits [14%]). We also excluded 2 providers who left during the pre-intervention period or were in the intervention period for < 1 month.
To ensure that we captured visits to providers with clinically significant exposure to scribes, we required scribed providers to have ≥ 20% of their visits scribed during the intervention period. To minimize the potential for contamination, we excluded nonscribed visits to scribed providers during the intervention period (n = 2211), because such nonscribed visits were largely due to visits outside the scribe’s scheduled time.
Continue to: Analysis
Analysis
We compared demographic characteristics for patients and providers using the chi-square test for categorical variables and the t test for continuous variables. We compared the change in outcomes from before implementation of scribes to during implementation of scribes among scribed providers, compared to nonscribed providers, using generalized estimating equations with robust standard errors to account for repeated measures (ie, multiple visits by the same patients) and the hierarchical nature of the data (ie, patients nested within providers). We then recalculated these estimates, controlling for patient demographics (age, gender, race, and ethnicity). We repeated these analyses for patients presenting for nonpreventive visits.
Results
Visit characteristics
We examined 271,768 visits, including 41,371 visits to 17 scribed providers and 230,397 visits to 78 nonscribed providers (Table 1). Patients were most likely to be female, > 21 years of age, have English as their language of care, and be non-White. Most visits were by established patients and were nonpreventive.
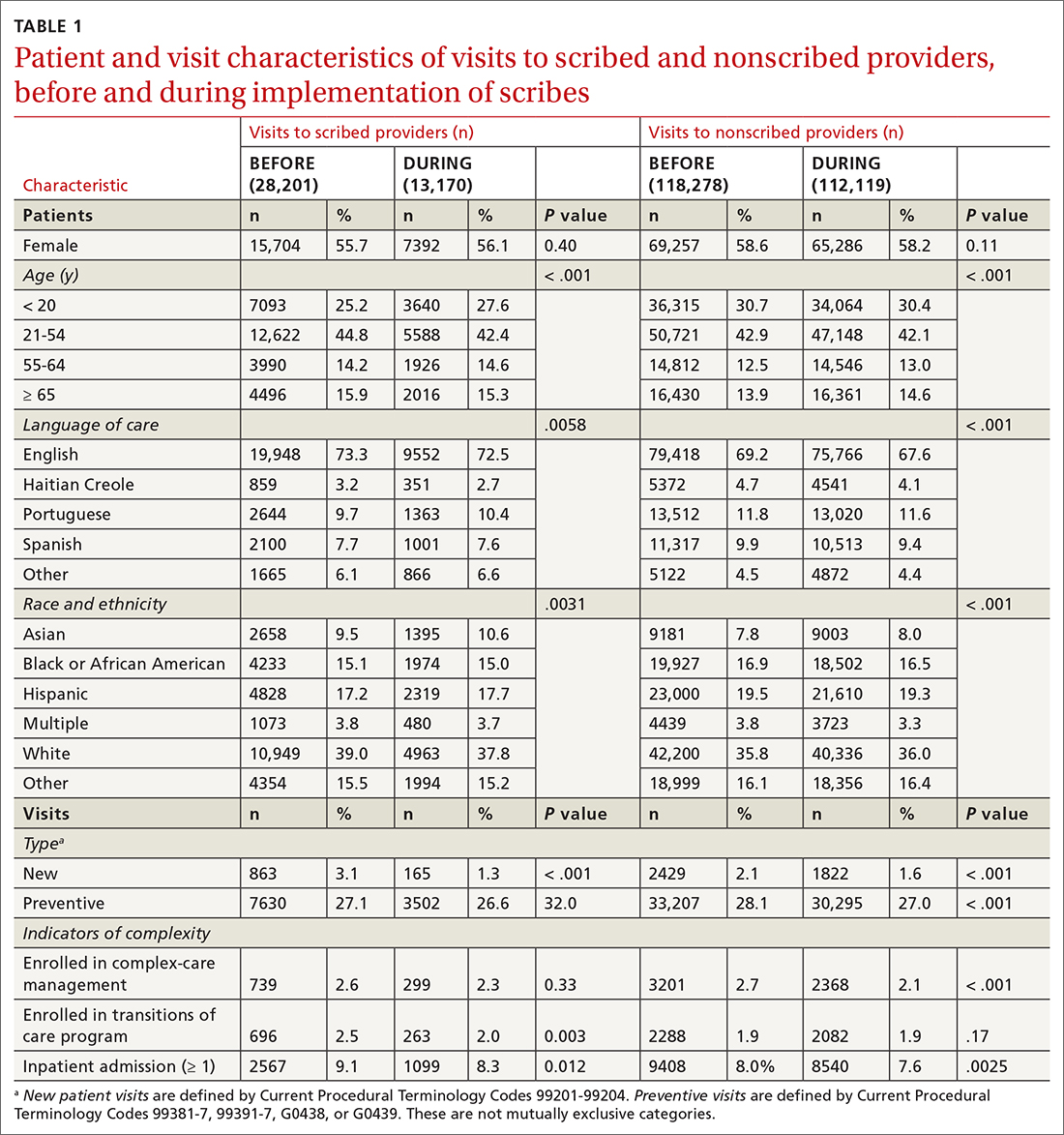
We noted no clinically significant differences in characteristics between visits with scribed providers and visits with nonscribed providers, and over time. Patient complexity measures, including care management enrollment and hospital admissions, were also similar between groups, and over time.
Billing measures
HCC coding. In 28.6% of visits, the decision-support tool identified at least 1 potential HCC code. Among these, the percentage of visits with at least 1 HCC code billed increased by 10.1 percentage points (from 3.9% before implementation of scribes to 14.0%) among scribed providers, compared to increasing by 6.5 percentage points (from 2.9% before implementation to 9.3%) among nonscribed providers (TABLE 2). Scribes were therefore associated with an additional 3.6 percentage-point increase in visits with at least 1 HCC code billed (P < .0001)—a difference that remained significant after adjusting for patient demographics (P < .0001).
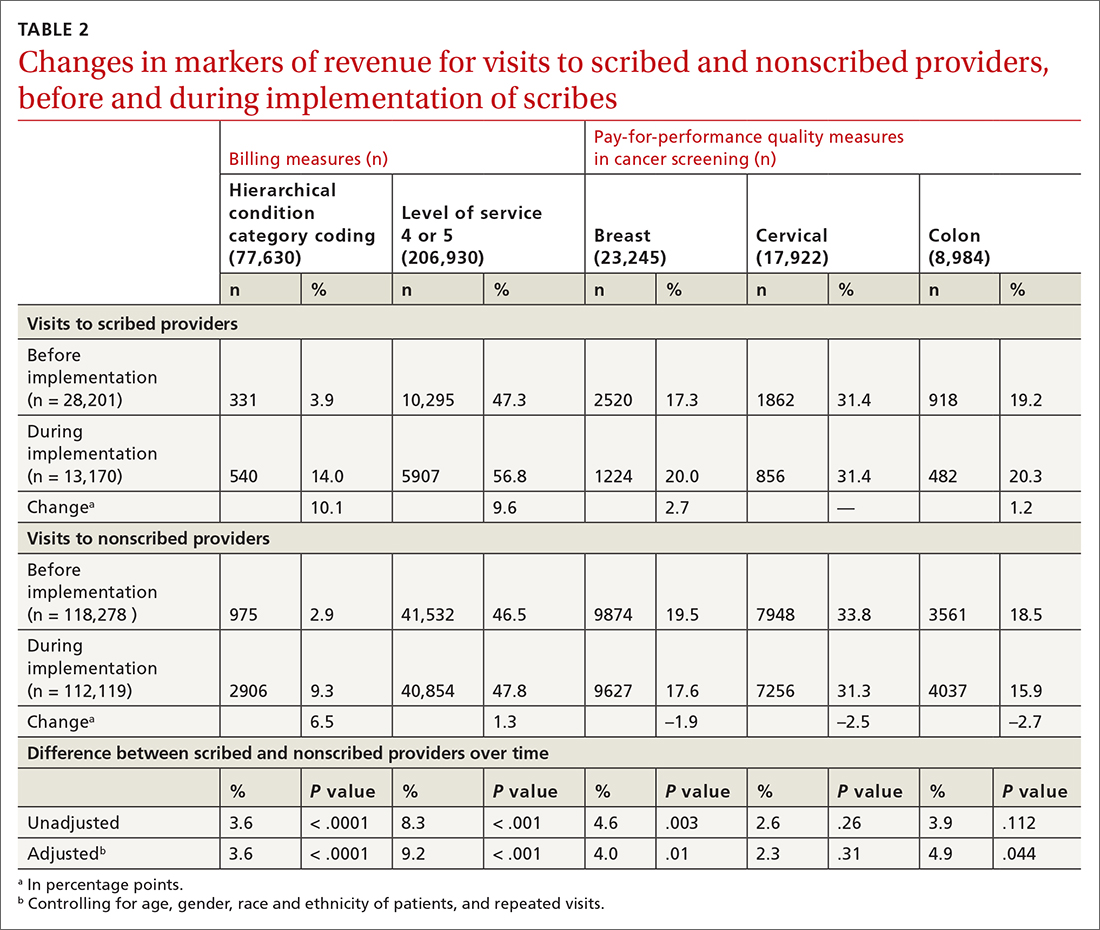
LOS coding. Scribed providers increased the number of visits billed as LOS 4 or 5 by 9.6 percentage points (from 47.3% before implementation to 56.8%); during the same period, nonscribed providers increased the number of visits billed as LOS 4 or 5 by 1.3 percentage points (from 46.5% before implementation to 47.8%) (TABLE 2). Scribes were therefore associated with an additional 8.3 percentage points in LOS 4 or 5 billing (P < .001) (TABLE 2). This difference remained significant after adjusting for patient demographics (P < .001).
Continue to: Pay-for-performance quality measures
Pay-for-performance quality measures
Breast cancer screening. Scribed providers increased the number of visits at which breast cancer screening was ordered by 2.7 percentage points (from 17.3% before implementation of scribes to 20.0%); during the same period, the number of visits at which breast cancer screening was ordered by nonscribed providers decreased by 1.9 percentage points (from 19.5% to 17.6%). Scribes were therefore associated with an increase of 4.6 percentage points in breast cancer screening orders, compared to nonscribed providers (P < .003) (TABLE 2). That difference remained significant after adjusting for patient demographics (P = .01).
Colon cancer screening. Similarly, scribed providers increased the number of visits at which colon cancer screening was ordered by 1.2 percentage points (from 19.2% before implementation of scribes to 20.3%); during the same period, the number of visits at which colon cancer screening was ordered by nonscribed providers decreased by 2.7 percentage points (from 18.5% to 15.9%) (P = .112). After adjusting for patient demographics, scribes were associated with an increase of 4.9 percentage points in colon cancer screening orders, compared to nonscribed providers (P = .044) (TABLE 2).
Cervical cancer screening. The rate at which cervical cancer screening was ordered did not change among scribed providers and decreased (by 2.5 percentage points) among nonscribed providers—a difference that was not statistically significant (P = .26).
Nonpreventive visits. Our findings overall did not change in analyses focused on nonpreventive visits, in which scribes were associated with an increase of 8.2 percentage points in LOS 4 or 5 billing (P < .001); an increase of 3.1 percentage points in HCC coding (P < .001); and an increase of 3.2 percentage points in breast cancer screening orders (P = .03) (TABLE 3). Although scribes were associated with an increase of 1.5 percentage points in cervical cancer screening orders and an increase of 3.1 percentage points in colon cancer screening orders, these increases did not reach statistical significance.
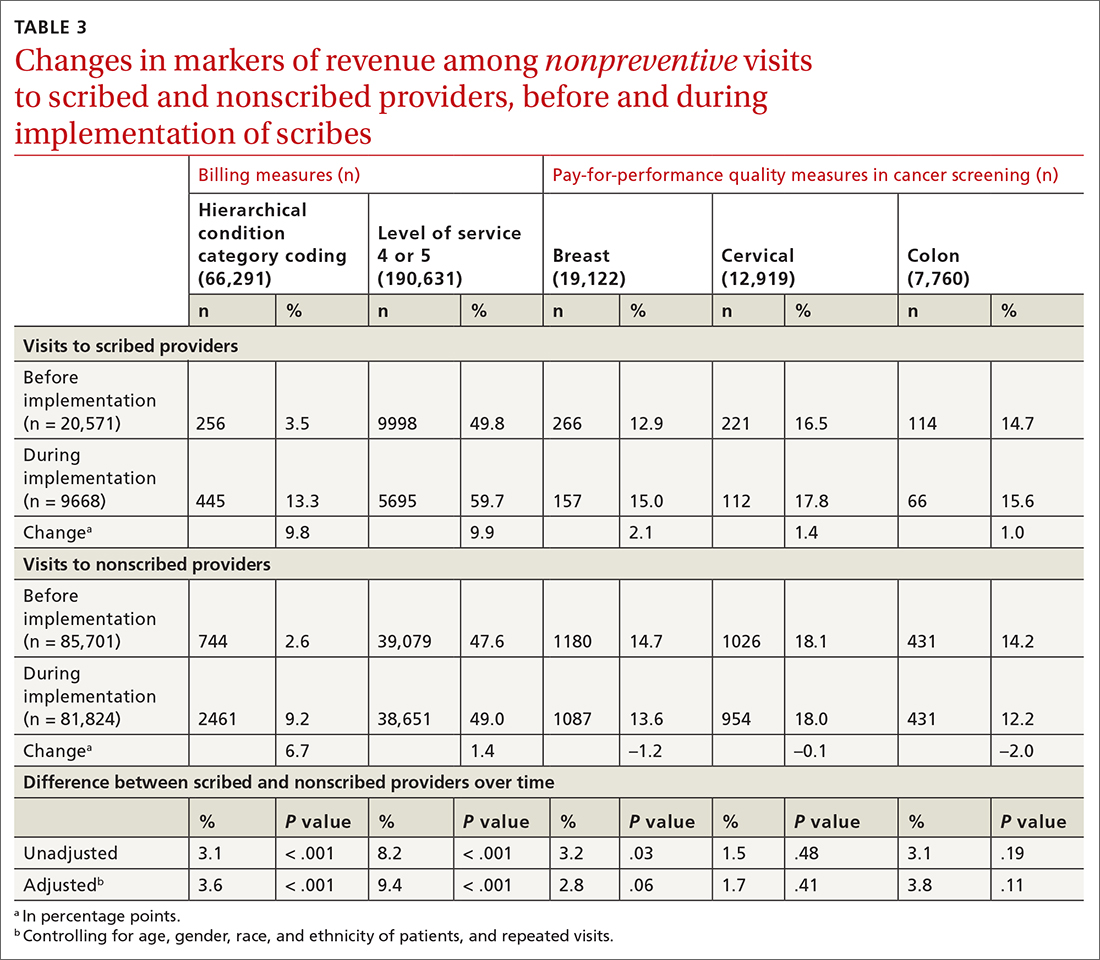
Discussion
We found that implementation of scribes is associated with (1) an increase in LOS coding and risk coding and (2) a higher frequency of addressing 2 of 3 pay-for-performance quality measures in primary care. In adjusted analyses in our study, and compared to nonscribed providers, scribes were associated with an additional 9.2 percentage points in LOS 4 or 5 billing; 3.6 percentage points in HCC coding; 4.0 percentage points in breast cancer screening orders; and 4.9 percentage points in colon cancer screening orders. Cervical cancer screening orders followed a similar pattern, with an increase of 2.3 percentage points in the adjusted screening order rate among scribed providers, compared to nonscribed providers, during implementation of scribes—although the increase was not significant. These findings did not change in analyses focused on nonpreventive visits.
Continue to: Our findings are consistent
Our findings are consistent with those of earlier studies. Prior examinations in ambulatory specialties found that scribes increased HCC coding,4 LOS billing,24 and pay-for-performance metrics.18 The only study to examine these areas in primary care found that scribes were associated with increased pay-for-performance measure documentation,20 a change that is necessary but insufficient to realize increased pay-for-performance revenue. Therefore, our study confirms, for the first time, that PCPs can better address pay-for-performance measures, LOS billing, and HCC coding when working with a scribe in primary care.
Demands on primary care visits are increasing.28 Physicians are required to provide more documentation; there is greater emphasis on PCPs meeting pay-for-performance measures; and there are more data in the EMR to review. In this context, addressing pay-for-performance measures and gaps in risk coding is likely to be increasingly challenging. Our study suggests that scribes might provide a mechanism to increase risk coding, LOS billing, and pay-for-performance measures, despite increased demands on primary care visits.
Increase in LOS billing. In the settings in which we work, a fee-for-service LOS 4 primary care visit generates, on average, $20 to $75 more in revenue than an LOS 3 visit. Using an average of $50 additional revenue for LOS 4 billing, we estimate that a full-time scribe is associated with roughly $7,000 in additional revenue annually. We arrived at this estimate using an average of 1500 visits at LOS ≤ 3 for every PCP full-time equivalent. A 9.2 percentage–point increase in LOS 4 billing would lead to roughly 140 additional LOS 4 visits, with each visit generating an additional $50 in revenue.
This analysis does not account for increased revenue associated with increased pay for HCC coding identified in our study.
Furthermore, in our conservative assumption, the entire increase in LOS billing was from level 3 to level 4; in fact, a small percentage of that increase would be from level 2 and another small percentage would be to level 5—both of which would generate additional revenue. Our assumption therefore underestimates the full financial value associated with scribes in the absence of increased patient volume. Nonetheless, the assumption suggests that increases in LOS billing offset a substantial percentage of a scribe’s salary.
Continue to: Limitations of this study
Limitations of this study. Our study should be interpreted in the context of several limitations:
- The study was conducted at 1 institution. Our findings might not be generalizable beyond this setting.
- The study measures the impact of scribes when providers work with scribes part time. Because providers who utilize a scribe for all, or nearly all, their visits are likely to use a scribe more efficiently, our study might underestimate the full impact of a scribe.
- In some settings, team members such as medical assistants are trained to assist with documentation and other responsibilities (such as closing care gaps) in addition to other patient care responsibilities.29-32 The extent to which our findings transfer to other models is unclear; studies comparing the impact of other models (which might provide even stronger outcomes) to the impact of medical scribes would be an interesting area for further research.
- In addition to the variability of models, there is likely variability in the quality and interactions of medical scribes, which might impact outcomes. We did not examine the qualities of scribes that led to outcomes in this study.
- We examined the impact of scribes on quality measure–ordering behaviors of providers, not on whether quality measures actually improved. Because scribes are associated with more face-to-face time with patients,27 they might allow for increased attention being paid by physicians to barriers to pay-for-performance measures (eg, patient education). This could increase the likelihood that patients complete a multitude of screenings, and thus improve adherence and follow-up. However, the impact of scribes on quality measures is a topic for future study.
Value beyond volume. Any limitations notwithstanding, our study suggests that scribes are associated with financial benefit in addition to the benefit of increased volume. Primary care practices should therefore consider the financial benefit of scribes independent of their ability to add patient volume. By recognizing this additive value, primary care practices might more fully capture the benefit of scribes, which might then allow practices to employ scribes with less demand to increase volume. This added support without increased volume would, in turn, likely reduce provider burnout (and the costly associated turnover) and increase patient satisfaction, leading to a synergistic financial benefit.
CORRESPONDENCE
Wayne Altman, MD, FAAFP, Tufts University School of Medicine, 200 Harrison Avenue, Boston, MA 02111; wayne. [email protected]
1. Gellert GA, Ramirez R, Webster SL. The rise of the medical scribe industry: implications for the advancement of electronic health records. JAMA. 2015;313:1315-1316. doi: 10.1001/jama.2014.1712
2. Cho J, Sanchez K, Ganor O, et al. Utilizing a physician scribe in a pediatric plastic surgical practice: a time-driven activity-based costing study. Plast Reconstr Surg Glob Open. 2019;7:e2460. doi: 10.1097/GOX.0000000000002460
3. Danak SU, Guetterman TC, Plegue MA, et al. Influence of scribes on patient-physician communication in primary care encounters: mixed methods study. JMIR Med Inform. 2019;7:e14797. doi: 10.2196/14797
4. Martel ML, Imdieke BH, Holm KM, et al. Developing a medical scribe program at an academic hospital: the Hennepin County Medical Center experience. Jt Comm J Qual Patient Saf. 2018;44:238-249. doi: 10.1016/j.jcjq.2018.01.001
5. Mishra P, Kiang JC, Grant RW. Association of medical scribes in primary care with physician workflow and patient experience. JAMA Intern Med. 2018;178:1467-1472. doi: 10.1001/ jamainternmed.2018.3956
6. Taylor KA, McQuilkin D, Hughes RG. Medical scribe impact on patient and provider experience. Mil Med. 2019;184:388-393. doi: 10.1093/milmed/usz030
7. Gidwani R, Nguyen C, Kofoed A, et al. Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: a randomized controlled trial. Ann Fam Med. 2017;15:427-433. doi: 10.1370/afm.2122.
8. Heckman J, Mukamal KJ, Christensen A, et al. Medical scribes, provider and patient experience, and patient throughput: a trial in an academic general internal medicine practice. J Gen Intern Med. 2019;35:770-774. doi: 10.1007/s11606-019-05352-5
9. Koshy S, Feustel PJ, Hong M, et al. Scribes in an ambulatory urology practice: patient and physician satisfaction. J Urol. 2010;184:258-262. doi: 10.1016/j.juro.2010.03.040
10. McCormick BJ, Deal A, Borawski KM, et al. Implementation of medical scribes in an academic urology practice: an analysis of productivity, revenue, and satisfaction. World J Urol. 2018;36:1691-1697. doi: 10.1007/s00345-018-2293-8
11. Pozdnyakova A, Laiteerapong N, Volerman A, et al. Impact of medical scribes on physician and patient satisfaction in primary care. J Gen Intern Med. Jul 2018;33:1109-1115. doi: 10.1007/ s11606-018-4434-6
12. Bank AJ, Obetz C, Konrardy A, et al. Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: a prospective study. Clinicoecon Outcomes Res. 2013;5:399-406. doi: 10.2147/CEOR.S49010
13. Danila MI, Melnick JA, Curtis JR, et al. Use of scribes for documentation assistance in rheumatology and endocrinology clinics: impact on clinic workflow and patient and physician satisfaction. J Clin Rheumatol. 2018;24:116-121. doi: 10.1097/ RHU.0000000000000620
14. Keefe KR, Levi JR, Brook CD. The impact of medical scribes on patient satisfaction in an academic otolaryngology clinic. Ann Otol Rhinol Laryngol. 2020;129:238-244. doi: 10.1177/0003489419884337
15. Lowry C, Orr K, Embry B, et al. Primary care scribes: writing a new story for safety net clinics. BMJ Open Qual. 2017;6:e000124. doi: 10.1136/bmjoq-2017-000124
16. Rohlfing ML, Keefe KR, Komshian SR, et al. Clinical scribes and their association with patient experience in the otolaryngology clinic. Laryngoscope. 2020;130:e134-e139. doi: 10.1002/ lary.28075
17. Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med. 2010;17:490-494. doi: 10.1111/j.1553- 2712.2010.00718.x
18. Ewelukwa O, Perez R, Carter LE, et al. Incorporation of scribes into the inflammatory bowel disease clinic improves quality of care and physician productivity. Inflamm Bowel Dis. 2018;24: 552-557. doi: 10.1093/ibd/izx078
19. Misra-Hebert AD, Yan C, Rothberg MB. Physician, scribe, and patient perspectives on clinical scribes in primary care. J Gen Intern Med. 2017;32:244. doi: 10.1007/s11606-016-3888-7
20. Platt J, Altman W. Can medical scribes improve quality measure documentation? J Fam Pract. Jun 2019;68:e1-e7.
21. Guglielmo WJ. What a scribe can do for you. Med Econ. Jan 6 2006;83:42,44-46.
22. Richmond M. Don’t use scribes for order entry. Emergency Medicine News. 2009;31:6-7. doi: 10.1097/01.EEM.0000360578.87654.cc
23. Schiff GD, Zucker L. Medical scribes: salvation for primary care or workaround for poor EMR usability? J Gen Intern Med. 2016;31:979-981. doi: 10.1007/s11606-016-3788-x
24. Bank AJ, Gage RM. Annual impact of scribes on physician productivity and revenue in a cardiology clinic. Clinicoecon Outcomes Res. 2015;7:489-495. doi: 10.2147/CEOR.S89329
25. Heaton HA, Castaneda-Guarderas A, Trotter ER, et al. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Am J Emerg Med. 2016;34:2018-2028. doi: 10.1016/j.ajem.2016.07.056
26. Earls ST, Savageau JA, Begley S, et al. Can scribes boost FPs’ efficiency and job satisfaction? J Fam Pract. 2017;66:206-214.
27. Zallman L, Finnegan K, Roll D, et al. Impact of medical scribes in primary care on productivity, face-to-face time, and patient comfort. J Am Board Fam Med. 2018;31:612-619. doi: 10.3122/ jabfm.2018.04.170325
28. Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23:2058-2065. doi: 10.1007/s11606- 008-0805-8
29. Ammann Howard K, Helé K, Salibi N, et al. Adapting the EHR scribe model to community health centers: the experience of Shasta Community Health Center’s pilot. Blue Shield of California Foundation; 2012. Accessed April 28, 2021. https:// blueshieldcafoundation.org/sites/default/files/publications/ downloadable/Shasta%20EHR%20Scribes%20Final%20Report.pdf
30. Anderson P, Halley MD. A new approach to making your doctor– nurse team more productive. Fam Pract Manag. 2008;15:35-40.
31. Blash L, Dower C, Chapman SA. University of Utah community clinics—medical assistant teams enhance patient-centered, physician-efficient care. Center for the Health Professions at UCSF; April 2011. Revised November 2011. Accessed April 28, 2021. https://healthforce.ucsf.edu/sites/healthforce.ucsf.edu/ files/publication-pdf/3.1%202011_04_University_of_Utah_Community_Clinics--Medical_Assistant_Teams_Enhance_PatientCentered_Physician-Efficient%20Care.pdf
32. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193. doi: 10.1001/ jamainternmed.2014.1315
ABSTRACT
Purpose Medical scribes are known to increase revenue by increasing visits to a medical practice. We examined whether medical scribes are associated with markers of financial benefit independent of increased visits.
Methods We conducted a pre- and post-observational study with a control group, examining changes in the percentage of visits (1) coded as level of service 4 or 5, (2) with at least 1 hierarchical condition category code billed, and (3) at which orders for 3 pay-for-performance quality measures (screening for breast, cervical, and colon cancer) were placed, if due. We looked at changes in outcomes among scribed providers and compared them to nonscribed providers. We used generalized estimating equations with robust standard errors to account for repeated measures and the hierarchical nature of the data, controlling for patient demographics.
Results We examined 41,371 visits to 17 scribed providers and 230,297 visits to 78 nonscribed providers. In adjusted analyses, and compared to nonscribed providers, scribes were associated with an increase of:
- Frutiger LT Std9.2 percentage points in level-of-service 4 or 5 billing (Frutiger LT StdP < .001)
- 3.6 percentage points in hierarchical condition category coding (Frutiger LT StdP < .001)
- 4.0 percentage points in breast cancer screening orders (Frutiger LT StdP = .01)
- 4.9 percentage points in colon cancer screening orders (Frutiger LT StdPFrutiger LT Std = .04).
Conclusions This study suggests that scribes are associated with financial benefit in addition to increased visit volume. Primary care practices should consider the financial benefit of scribes independent of their ability to add patient volume.
Increasingly, medical scribes are used in ambulatory care settings across the United States.1 Scribes are trained personnel who accompany providers during visits to provide documentation support and assist with other administrative tasks. They are associated with reduced documentation time for providers2-6 and improved provider satisfaction,7-11 without detriment to4-16 (or with possible improvement in17-20) patient satisfaction in ambulatory care settings. At the same time, concerns remain that using scribes might inhibit patient communication, harm clinical reasoning, reduce the effectiveness of clinical decision-support tools, and simply serve as a work-around to fixing inefficiencies in the electronic medical record (EMR).21-23
A driving force for the increased use of medical scribes is the expectation that they reduce the cost of providing care. Cost-efficiency is typically described as resulting from a reduction in physician time per patient seen, which allows increased patient volume and, in turn, drives increased physician productivity.2,8,10,18,24-27 Whether scribes result in cost savings remains unclear; some papers suggest that scribes are cost efficient in ambulatory care,2,10,18 while others have been unable to identify cost savings, particularly in primary care.4
One reason why scribes might not be associated with cost savings is that their financial benefit might be undercounted. Studies that focus on increased volume miss the opportunity to capture financial benefits conferred through mechanisms that are independent of seeing more patients:
- Scribes might help providers address and document more, and more complex, medical problems, allowing higher level-of-service (LOS) billing. For example, a provider chooses a lower LOS because they have insufficiently documented a visit to support a higher LOS; by assisting with documentation, the scribe might allow the provider to choose a higher LOS.
- Scribes might prompt a provider to use decision-support tools for risk coding (using appropriate medical codes to capture the patient’s level of medical complexity), thereby increasing reimbursement.
- Scribes might extend the time available during the visit for the provider to address pay-for-performance quality measures, such as cancer screening.
Continue to: Making visits count, not counting visits
Making visits count, not counting visits. In this study, we examined whether medical scribes in primary care are associated with improved markers of revenue that are independent of seeing more patients. Specifically, we examined whether scribes are associated with increased LOS coding, risk coding, and orders for pay-for-performance measures for all primary care visits and for nonpreventive primary care visits.
Methods
Design
This observational study compared the change in outcomes before implementation of scribes and during implementation of scribes, between scribed providers and nonscribed providers. We compared visits during the year prior to the implementation of scribes (July 2017–June 2018) with the year during their implementation (July 2018–2019).
The Cambridge Health Alliance Institutional Review Board considered this study exempt from review.
Setting
This study was conducted at a safety-net community academic health system that uses an EMR developed by Epic Systems [Verona, WI]. This EMR includes decision-support tools that prompt providers when pay-for-performance quality measures are due and when hierarchical condition category (HCC) codes—ie, specific diagnoses used by Medicare and other payers to reimburse providers for the complexity of their patients—might apply to the visit.
These EMR decision-support tools use algorithms that draw on age, gender, diagnoses that were billed previously or are on the problem list, laboratory findings, and prior imaging. They alert physicians when a patient is due for pay-for-performance quality measures, such as cancer screenings, and when HCC codes might be applicable.
Continue to: During the study period...
During the study period, the EMR decision-support tool for HCC coding underwent several changes designed to improve HCC coding. In addition, systematic changes to primary care visits took place, leading to an increase in the number of patients seen and screenings required.
Outcomes
We examined 2 categories of outcomes that confer financial benefit to many institutions: billing measures and pay-for-performance measures.
Billing measures included the percentage of visits (1) coded as LOS 4 or 5 and (2) with at least 1 HCC code billed (among those for which the decision-support tool identified at least 1 potential HCC code).
Pay-for-performance measures. We examined whether any of 3 pay-for-performance quality measures were addressed during the visit, selecting 3 that are commonly addressed by primary care providers (PCPs) and that require PCPs to sign an order for screening during a primary care visit: breast cancer (mammography order), cervical cancer (Papanicolaou smear order), and colon cancer (an order for fecal occult blood testing or colonoscopy).
Intervention
Scribes were employees of Cambridge Health Alliance who had recently graduated from college and were interested in a career as a health care professional. Scribes received 3 days of training on how to function effectively in their role; 1 day of training in EMR functionality; and 2 hours of training on decision-support tools for pay-for-performance quality measures and risk coding. Scribes continued learning on the job through feedback from supervising PCPs. Scribes documented patient encounters, recording histories and findings on the physical exam and transcribing discussion of treatment plans and the PCP’s instructions to patients.
Continue to: The 14 scribes worked with 17 physician...
The 14 scribes worked with 17 physician and nurse practitioner PCPs beginning in July 2018. Participation by PCPs was voluntary; they received no compensation for participating in the scribe program. PCPs were not required to see additional patients to participate. PCPs who chose to work with a scribe were similar to those who declined a scribe, as regards gender, race, type of provider (MD or NP), tenure at the institution, and percentage of time in clinical work (see Table W-1).
The control group comprised providers who elected not to work with a scribe but who worked in the same clinics as the intervention providers.
Scribes were assigned to a PCP based on availability during the PCP’s scheduled hours and worked with 1 PCP throughout the intervention (except for 1 PCP who worked with 2 scribes). All PCPs worked with their scribe(s) part time; on average, 49% of intervention PCPs’ visits were scribed.
Inclusion and exclusion criteria
Because the first year at an institution is a learning period for PCPs, we excluded those who worked at the institution for < 1 year before the start of the scribe program (n = 12). Based on the extensive clinical experience of 1 PCP (WA) with scribes, we excluded the first 200 visits or 6 weeks (whichever occurred first) with a scribe among all scribed providers, to account for an initial learning period (n = 2202, of 15,372 scribed visits [14%]). We also excluded 2 providers who left during the pre-intervention period or were in the intervention period for < 1 month.
To ensure that we captured visits to providers with clinically significant exposure to scribes, we required scribed providers to have ≥ 20% of their visits scribed during the intervention period. To minimize the potential for contamination, we excluded nonscribed visits to scribed providers during the intervention period (n = 2211), because such nonscribed visits were largely due to visits outside the scribe’s scheduled time.
Continue to: Analysis
Analysis
We compared demographic characteristics for patients and providers using the chi-square test for categorical variables and the t test for continuous variables. We compared the change in outcomes from before implementation of scribes to during implementation of scribes among scribed providers, compared to nonscribed providers, using generalized estimating equations with robust standard errors to account for repeated measures (ie, multiple visits by the same patients) and the hierarchical nature of the data (ie, patients nested within providers). We then recalculated these estimates, controlling for patient demographics (age, gender, race, and ethnicity). We repeated these analyses for patients presenting for nonpreventive visits.
Results
Visit characteristics
We examined 271,768 visits, including 41,371 visits to 17 scribed providers and 230,397 visits to 78 nonscribed providers (Table 1). Patients were most likely to be female, > 21 years of age, have English as their language of care, and be non-White. Most visits were by established patients and were nonpreventive.
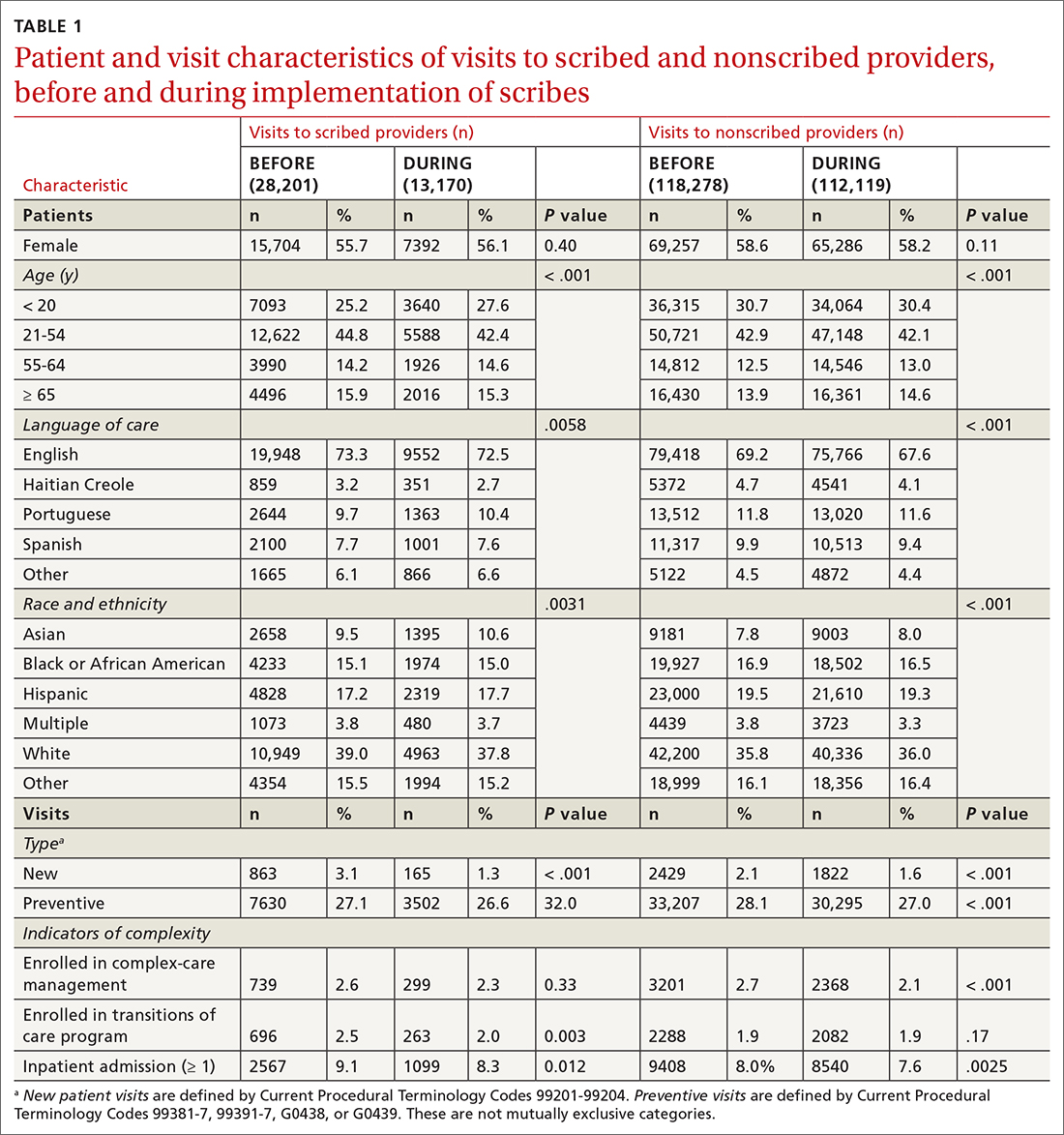
We noted no clinically significant differences in characteristics between visits with scribed providers and visits with nonscribed providers, and over time. Patient complexity measures, including care management enrollment and hospital admissions, were also similar between groups, and over time.
Billing measures
HCC coding. In 28.6% of visits, the decision-support tool identified at least 1 potential HCC code. Among these, the percentage of visits with at least 1 HCC code billed increased by 10.1 percentage points (from 3.9% before implementation of scribes to 14.0%) among scribed providers, compared to increasing by 6.5 percentage points (from 2.9% before implementation to 9.3%) among nonscribed providers (TABLE 2). Scribes were therefore associated with an additional 3.6 percentage-point increase in visits with at least 1 HCC code billed (P < .0001)—a difference that remained significant after adjusting for patient demographics (P < .0001).
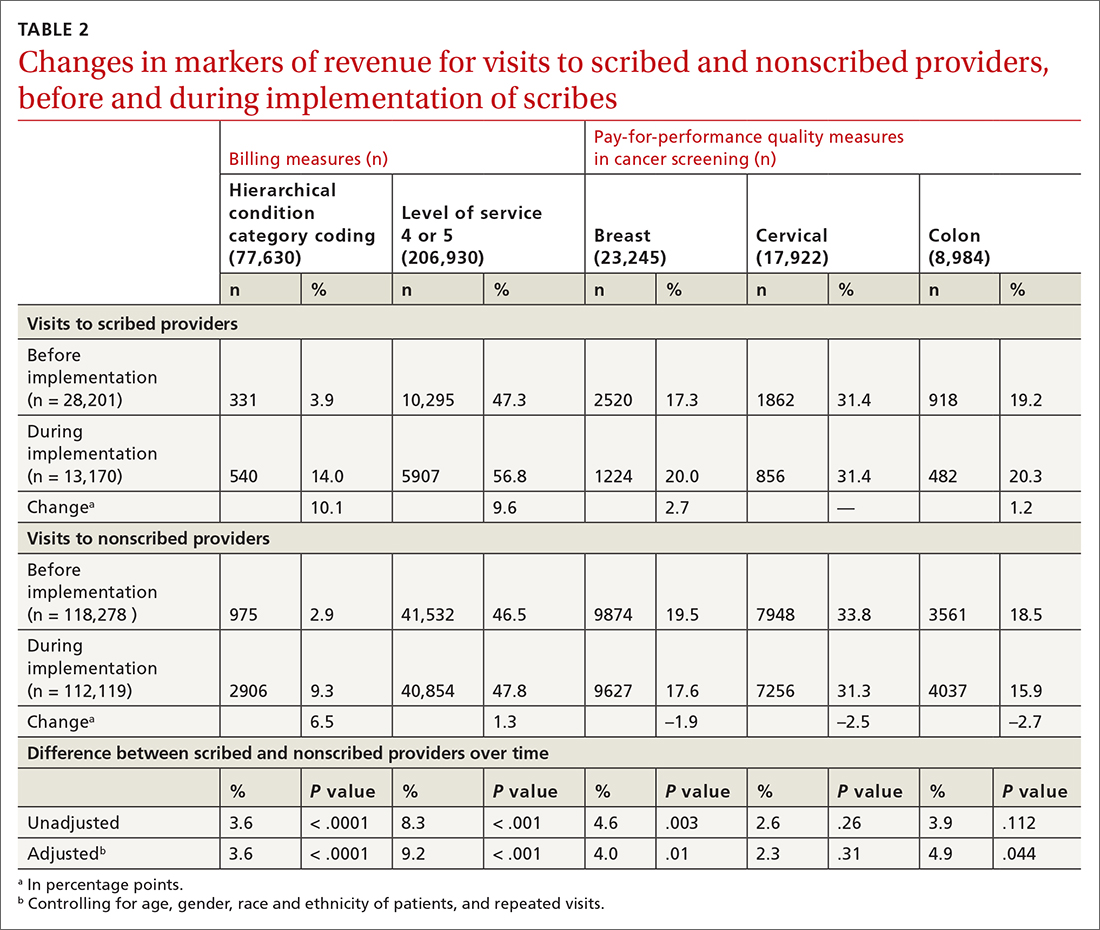
LOS coding. Scribed providers increased the number of visits billed as LOS 4 or 5 by 9.6 percentage points (from 47.3% before implementation to 56.8%); during the same period, nonscribed providers increased the number of visits billed as LOS 4 or 5 by 1.3 percentage points (from 46.5% before implementation to 47.8%) (TABLE 2). Scribes were therefore associated with an additional 8.3 percentage points in LOS 4 or 5 billing (P < .001) (TABLE 2). This difference remained significant after adjusting for patient demographics (P < .001).
Continue to: Pay-for-performance quality measures
Pay-for-performance quality measures
Breast cancer screening. Scribed providers increased the number of visits at which breast cancer screening was ordered by 2.7 percentage points (from 17.3% before implementation of scribes to 20.0%); during the same period, the number of visits at which breast cancer screening was ordered by nonscribed providers decreased by 1.9 percentage points (from 19.5% to 17.6%). Scribes were therefore associated with an increase of 4.6 percentage points in breast cancer screening orders, compared to nonscribed providers (P < .003) (TABLE 2). That difference remained significant after adjusting for patient demographics (P = .01).
Colon cancer screening. Similarly, scribed providers increased the number of visits at which colon cancer screening was ordered by 1.2 percentage points (from 19.2% before implementation of scribes to 20.3%); during the same period, the number of visits at which colon cancer screening was ordered by nonscribed providers decreased by 2.7 percentage points (from 18.5% to 15.9%) (P = .112). After adjusting for patient demographics, scribes were associated with an increase of 4.9 percentage points in colon cancer screening orders, compared to nonscribed providers (P = .044) (TABLE 2).
Cervical cancer screening. The rate at which cervical cancer screening was ordered did not change among scribed providers and decreased (by 2.5 percentage points) among nonscribed providers—a difference that was not statistically significant (P = .26).
Nonpreventive visits. Our findings overall did not change in analyses focused on nonpreventive visits, in which scribes were associated with an increase of 8.2 percentage points in LOS 4 or 5 billing (P < .001); an increase of 3.1 percentage points in HCC coding (P < .001); and an increase of 3.2 percentage points in breast cancer screening orders (P = .03) (TABLE 3). Although scribes were associated with an increase of 1.5 percentage points in cervical cancer screening orders and an increase of 3.1 percentage points in colon cancer screening orders, these increases did not reach statistical significance.
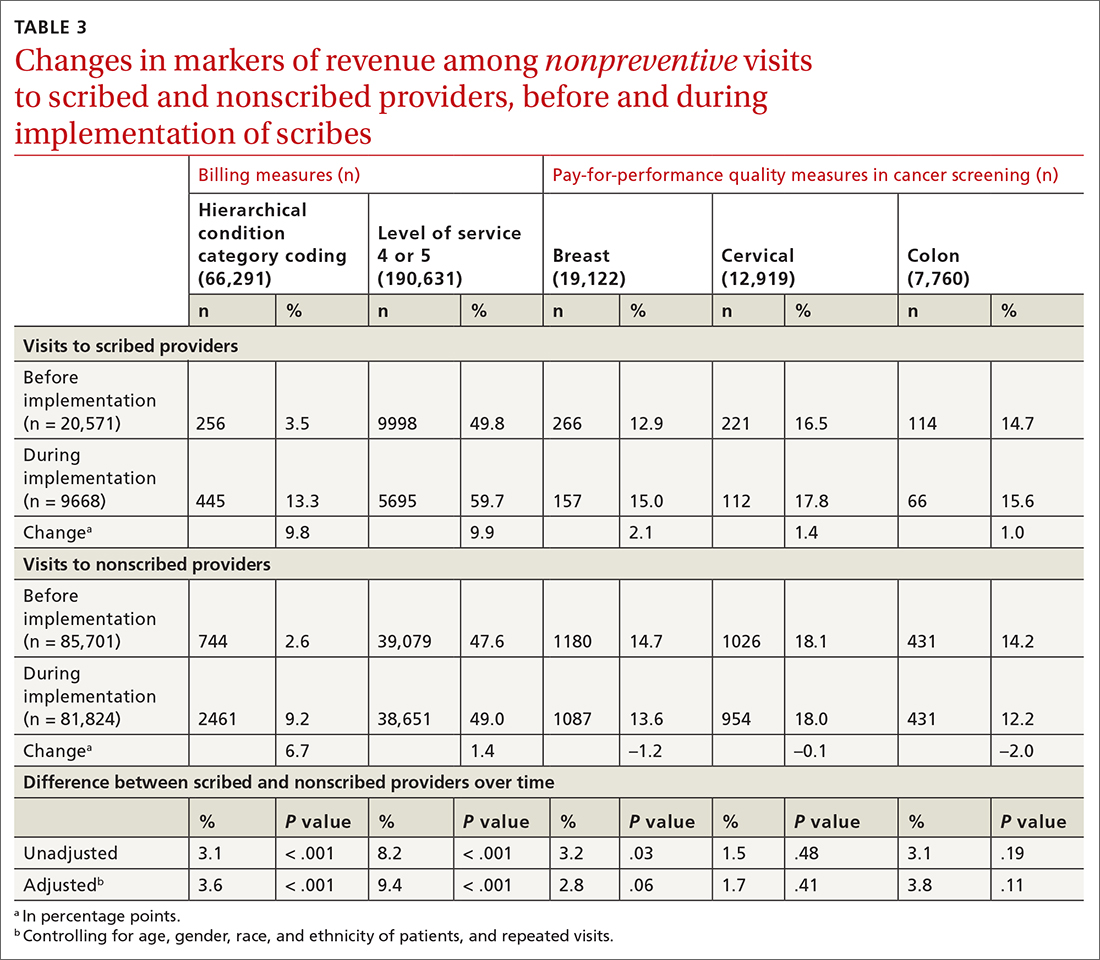
Discussion
We found that implementation of scribes is associated with (1) an increase in LOS coding and risk coding and (2) a higher frequency of addressing 2 of 3 pay-for-performance quality measures in primary care. In adjusted analyses in our study, and compared to nonscribed providers, scribes were associated with an additional 9.2 percentage points in LOS 4 or 5 billing; 3.6 percentage points in HCC coding; 4.0 percentage points in breast cancer screening orders; and 4.9 percentage points in colon cancer screening orders. Cervical cancer screening orders followed a similar pattern, with an increase of 2.3 percentage points in the adjusted screening order rate among scribed providers, compared to nonscribed providers, during implementation of scribes—although the increase was not significant. These findings did not change in analyses focused on nonpreventive visits.
Continue to: Our findings are consistent
Our findings are consistent with those of earlier studies. Prior examinations in ambulatory specialties found that scribes increased HCC coding,4 LOS billing,24 and pay-for-performance metrics.18 The only study to examine these areas in primary care found that scribes were associated with increased pay-for-performance measure documentation,20 a change that is necessary but insufficient to realize increased pay-for-performance revenue. Therefore, our study confirms, for the first time, that PCPs can better address pay-for-performance measures, LOS billing, and HCC coding when working with a scribe in primary care.
Demands on primary care visits are increasing.28 Physicians are required to provide more documentation; there is greater emphasis on PCPs meeting pay-for-performance measures; and there are more data in the EMR to review. In this context, addressing pay-for-performance measures and gaps in risk coding is likely to be increasingly challenging. Our study suggests that scribes might provide a mechanism to increase risk coding, LOS billing, and pay-for-performance measures, despite increased demands on primary care visits.
Increase in LOS billing. In the settings in which we work, a fee-for-service LOS 4 primary care visit generates, on average, $20 to $75 more in revenue than an LOS 3 visit. Using an average of $50 additional revenue for LOS 4 billing, we estimate that a full-time scribe is associated with roughly $7,000 in additional revenue annually. We arrived at this estimate using an average of 1500 visits at LOS ≤ 3 for every PCP full-time equivalent. A 9.2 percentage–point increase in LOS 4 billing would lead to roughly 140 additional LOS 4 visits, with each visit generating an additional $50 in revenue.
This analysis does not account for increased revenue associated with increased pay for HCC coding identified in our study.
Furthermore, in our conservative assumption, the entire increase in LOS billing was from level 3 to level 4; in fact, a small percentage of that increase would be from level 2 and another small percentage would be to level 5—both of which would generate additional revenue. Our assumption therefore underestimates the full financial value associated with scribes in the absence of increased patient volume. Nonetheless, the assumption suggests that increases in LOS billing offset a substantial percentage of a scribe’s salary.
Continue to: Limitations of this study
Limitations of this study. Our study should be interpreted in the context of several limitations:
- The study was conducted at 1 institution. Our findings might not be generalizable beyond this setting.
- The study measures the impact of scribes when providers work with scribes part time. Because providers who utilize a scribe for all, or nearly all, their visits are likely to use a scribe more efficiently, our study might underestimate the full impact of a scribe.
- In some settings, team members such as medical assistants are trained to assist with documentation and other responsibilities (such as closing care gaps) in addition to other patient care responsibilities.29-32 The extent to which our findings transfer to other models is unclear; studies comparing the impact of other models (which might provide even stronger outcomes) to the impact of medical scribes would be an interesting area for further research.
- In addition to the variability of models, there is likely variability in the quality and interactions of medical scribes, which might impact outcomes. We did not examine the qualities of scribes that led to outcomes in this study.
- We examined the impact of scribes on quality measure–ordering behaviors of providers, not on whether quality measures actually improved. Because scribes are associated with more face-to-face time with patients,27 they might allow for increased attention being paid by physicians to barriers to pay-for-performance measures (eg, patient education). This could increase the likelihood that patients complete a multitude of screenings, and thus improve adherence and follow-up. However, the impact of scribes on quality measures is a topic for future study.
Value beyond volume. Any limitations notwithstanding, our study suggests that scribes are associated with financial benefit in addition to the benefit of increased volume. Primary care practices should therefore consider the financial benefit of scribes independent of their ability to add patient volume. By recognizing this additive value, primary care practices might more fully capture the benefit of scribes, which might then allow practices to employ scribes with less demand to increase volume. This added support without increased volume would, in turn, likely reduce provider burnout (and the costly associated turnover) and increase patient satisfaction, leading to a synergistic financial benefit.
CORRESPONDENCE
Wayne Altman, MD, FAAFP, Tufts University School of Medicine, 200 Harrison Avenue, Boston, MA 02111; wayne. [email protected]
ABSTRACT
Purpose Medical scribes are known to increase revenue by increasing visits to a medical practice. We examined whether medical scribes are associated with markers of financial benefit independent of increased visits.
Methods We conducted a pre- and post-observational study with a control group, examining changes in the percentage of visits (1) coded as level of service 4 or 5, (2) with at least 1 hierarchical condition category code billed, and (3) at which orders for 3 pay-for-performance quality measures (screening for breast, cervical, and colon cancer) were placed, if due. We looked at changes in outcomes among scribed providers and compared them to nonscribed providers. We used generalized estimating equations with robust standard errors to account for repeated measures and the hierarchical nature of the data, controlling for patient demographics.
Results We examined 41,371 visits to 17 scribed providers and 230,297 visits to 78 nonscribed providers. In adjusted analyses, and compared to nonscribed providers, scribes were associated with an increase of:
- Frutiger LT Std9.2 percentage points in level-of-service 4 or 5 billing (Frutiger LT StdP < .001)
- 3.6 percentage points in hierarchical condition category coding (Frutiger LT StdP < .001)
- 4.0 percentage points in breast cancer screening orders (Frutiger LT StdP = .01)
- 4.9 percentage points in colon cancer screening orders (Frutiger LT StdPFrutiger LT Std = .04).
Conclusions This study suggests that scribes are associated with financial benefit in addition to increased visit volume. Primary care practices should consider the financial benefit of scribes independent of their ability to add patient volume.
Increasingly, medical scribes are used in ambulatory care settings across the United States.1 Scribes are trained personnel who accompany providers during visits to provide documentation support and assist with other administrative tasks. They are associated with reduced documentation time for providers2-6 and improved provider satisfaction,7-11 without detriment to4-16 (or with possible improvement in17-20) patient satisfaction in ambulatory care settings. At the same time, concerns remain that using scribes might inhibit patient communication, harm clinical reasoning, reduce the effectiveness of clinical decision-support tools, and simply serve as a work-around to fixing inefficiencies in the electronic medical record (EMR).21-23
A driving force for the increased use of medical scribes is the expectation that they reduce the cost of providing care. Cost-efficiency is typically described as resulting from a reduction in physician time per patient seen, which allows increased patient volume and, in turn, drives increased physician productivity.2,8,10,18,24-27 Whether scribes result in cost savings remains unclear; some papers suggest that scribes are cost efficient in ambulatory care,2,10,18 while others have been unable to identify cost savings, particularly in primary care.4
One reason why scribes might not be associated with cost savings is that their financial benefit might be undercounted. Studies that focus on increased volume miss the opportunity to capture financial benefits conferred through mechanisms that are independent of seeing more patients:
- Scribes might help providers address and document more, and more complex, medical problems, allowing higher level-of-service (LOS) billing. For example, a provider chooses a lower LOS because they have insufficiently documented a visit to support a higher LOS; by assisting with documentation, the scribe might allow the provider to choose a higher LOS.
- Scribes might prompt a provider to use decision-support tools for risk coding (using appropriate medical codes to capture the patient’s level of medical complexity), thereby increasing reimbursement.
- Scribes might extend the time available during the visit for the provider to address pay-for-performance quality measures, such as cancer screening.
Continue to: Making visits count, not counting visits
Making visits count, not counting visits. In this study, we examined whether medical scribes in primary care are associated with improved markers of revenue that are independent of seeing more patients. Specifically, we examined whether scribes are associated with increased LOS coding, risk coding, and orders for pay-for-performance measures for all primary care visits and for nonpreventive primary care visits.
Methods
Design
This observational study compared the change in outcomes before implementation of scribes and during implementation of scribes, between scribed providers and nonscribed providers. We compared visits during the year prior to the implementation of scribes (July 2017–June 2018) with the year during their implementation (July 2018–2019).
The Cambridge Health Alliance Institutional Review Board considered this study exempt from review.
Setting
This study was conducted at a safety-net community academic health system that uses an EMR developed by Epic Systems [Verona, WI]. This EMR includes decision-support tools that prompt providers when pay-for-performance quality measures are due and when hierarchical condition category (HCC) codes—ie, specific diagnoses used by Medicare and other payers to reimburse providers for the complexity of their patients—might apply to the visit.
These EMR decision-support tools use algorithms that draw on age, gender, diagnoses that were billed previously or are on the problem list, laboratory findings, and prior imaging. They alert physicians when a patient is due for pay-for-performance quality measures, such as cancer screenings, and when HCC codes might be applicable.
Continue to: During the study period...
During the study period, the EMR decision-support tool for HCC coding underwent several changes designed to improve HCC coding. In addition, systematic changes to primary care visits took place, leading to an increase in the number of patients seen and screenings required.
Outcomes
We examined 2 categories of outcomes that confer financial benefit to many institutions: billing measures and pay-for-performance measures.
Billing measures included the percentage of visits (1) coded as LOS 4 or 5 and (2) with at least 1 HCC code billed (among those for which the decision-support tool identified at least 1 potential HCC code).
Pay-for-performance measures. We examined whether any of 3 pay-for-performance quality measures were addressed during the visit, selecting 3 that are commonly addressed by primary care providers (PCPs) and that require PCPs to sign an order for screening during a primary care visit: breast cancer (mammography order), cervical cancer (Papanicolaou smear order), and colon cancer (an order for fecal occult blood testing or colonoscopy).
Intervention
Scribes were employees of Cambridge Health Alliance who had recently graduated from college and were interested in a career as a health care professional. Scribes received 3 days of training on how to function effectively in their role; 1 day of training in EMR functionality; and 2 hours of training on decision-support tools for pay-for-performance quality measures and risk coding. Scribes continued learning on the job through feedback from supervising PCPs. Scribes documented patient encounters, recording histories and findings on the physical exam and transcribing discussion of treatment plans and the PCP’s instructions to patients.
Continue to: The 14 scribes worked with 17 physician...
The 14 scribes worked with 17 physician and nurse practitioner PCPs beginning in July 2018. Participation by PCPs was voluntary; they received no compensation for participating in the scribe program. PCPs were not required to see additional patients to participate. PCPs who chose to work with a scribe were similar to those who declined a scribe, as regards gender, race, type of provider (MD or NP), tenure at the institution, and percentage of time in clinical work (see Table W-1).
The control group comprised providers who elected not to work with a scribe but who worked in the same clinics as the intervention providers.
Scribes were assigned to a PCP based on availability during the PCP’s scheduled hours and worked with 1 PCP throughout the intervention (except for 1 PCP who worked with 2 scribes). All PCPs worked with their scribe(s) part time; on average, 49% of intervention PCPs’ visits were scribed.
Inclusion and exclusion criteria
Because the first year at an institution is a learning period for PCPs, we excluded those who worked at the institution for < 1 year before the start of the scribe program (n = 12). Based on the extensive clinical experience of 1 PCP (WA) with scribes, we excluded the first 200 visits or 6 weeks (whichever occurred first) with a scribe among all scribed providers, to account for an initial learning period (n = 2202, of 15,372 scribed visits [14%]). We also excluded 2 providers who left during the pre-intervention period or were in the intervention period for < 1 month.
To ensure that we captured visits to providers with clinically significant exposure to scribes, we required scribed providers to have ≥ 20% of their visits scribed during the intervention period. To minimize the potential for contamination, we excluded nonscribed visits to scribed providers during the intervention period (n = 2211), because such nonscribed visits were largely due to visits outside the scribe’s scheduled time.
Continue to: Analysis
Analysis
We compared demographic characteristics for patients and providers using the chi-square test for categorical variables and the t test for continuous variables. We compared the change in outcomes from before implementation of scribes to during implementation of scribes among scribed providers, compared to nonscribed providers, using generalized estimating equations with robust standard errors to account for repeated measures (ie, multiple visits by the same patients) and the hierarchical nature of the data (ie, patients nested within providers). We then recalculated these estimates, controlling for patient demographics (age, gender, race, and ethnicity). We repeated these analyses for patients presenting for nonpreventive visits.
Results
Visit characteristics
We examined 271,768 visits, including 41,371 visits to 17 scribed providers and 230,397 visits to 78 nonscribed providers (Table 1). Patients were most likely to be female, > 21 years of age, have English as their language of care, and be non-White. Most visits were by established patients and were nonpreventive.
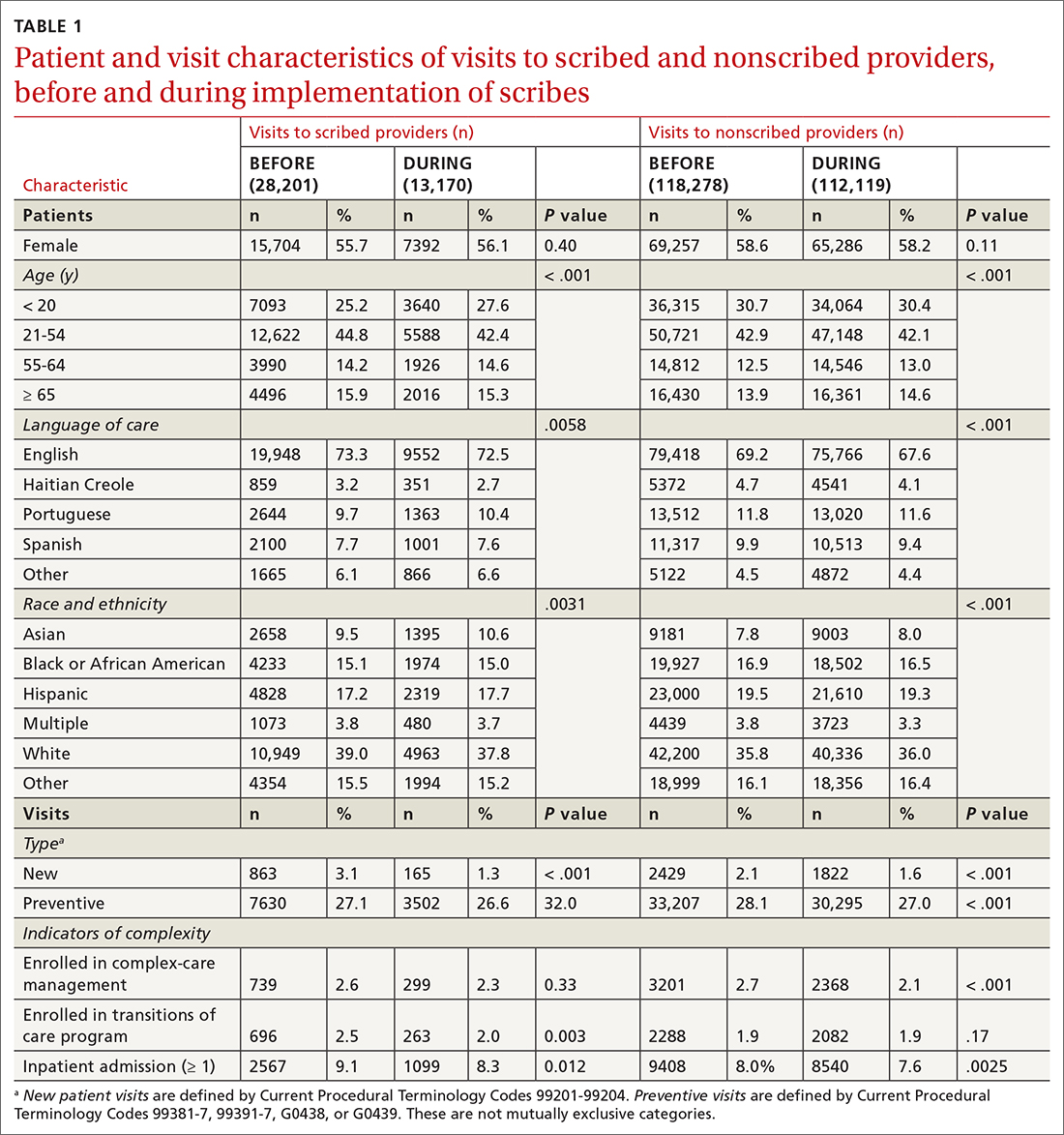
We noted no clinically significant differences in characteristics between visits with scribed providers and visits with nonscribed providers, and over time. Patient complexity measures, including care management enrollment and hospital admissions, were also similar between groups, and over time.
Billing measures
HCC coding. In 28.6% of visits, the decision-support tool identified at least 1 potential HCC code. Among these, the percentage of visits with at least 1 HCC code billed increased by 10.1 percentage points (from 3.9% before implementation of scribes to 14.0%) among scribed providers, compared to increasing by 6.5 percentage points (from 2.9% before implementation to 9.3%) among nonscribed providers (TABLE 2). Scribes were therefore associated with an additional 3.6 percentage-point increase in visits with at least 1 HCC code billed (P < .0001)—a difference that remained significant after adjusting for patient demographics (P < .0001).
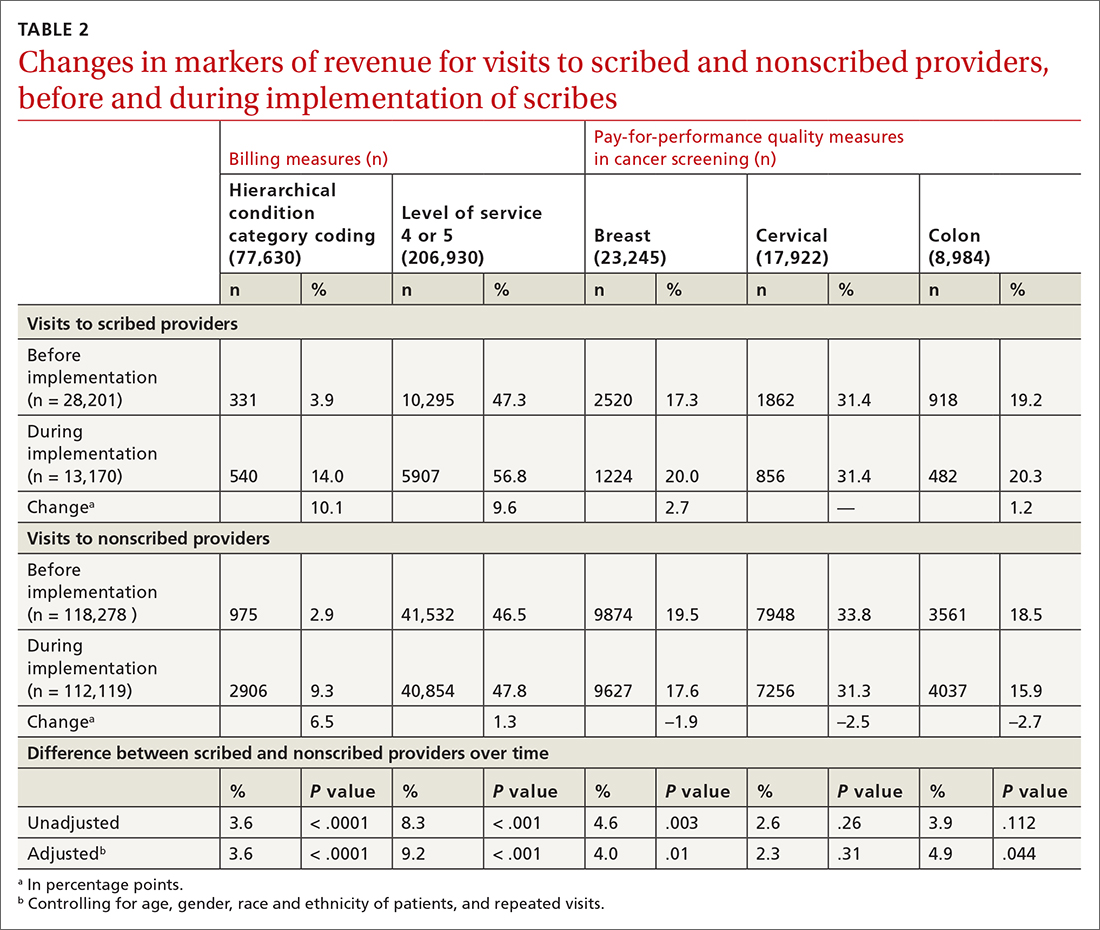
LOS coding. Scribed providers increased the number of visits billed as LOS 4 or 5 by 9.6 percentage points (from 47.3% before implementation to 56.8%); during the same period, nonscribed providers increased the number of visits billed as LOS 4 or 5 by 1.3 percentage points (from 46.5% before implementation to 47.8%) (TABLE 2). Scribes were therefore associated with an additional 8.3 percentage points in LOS 4 or 5 billing (P < .001) (TABLE 2). This difference remained significant after adjusting for patient demographics (P < .001).
Continue to: Pay-for-performance quality measures
Pay-for-performance quality measures
Breast cancer screening. Scribed providers increased the number of visits at which breast cancer screening was ordered by 2.7 percentage points (from 17.3% before implementation of scribes to 20.0%); during the same period, the number of visits at which breast cancer screening was ordered by nonscribed providers decreased by 1.9 percentage points (from 19.5% to 17.6%). Scribes were therefore associated with an increase of 4.6 percentage points in breast cancer screening orders, compared to nonscribed providers (P < .003) (TABLE 2). That difference remained significant after adjusting for patient demographics (P = .01).
Colon cancer screening. Similarly, scribed providers increased the number of visits at which colon cancer screening was ordered by 1.2 percentage points (from 19.2% before implementation of scribes to 20.3%); during the same period, the number of visits at which colon cancer screening was ordered by nonscribed providers decreased by 2.7 percentage points (from 18.5% to 15.9%) (P = .112). After adjusting for patient demographics, scribes were associated with an increase of 4.9 percentage points in colon cancer screening orders, compared to nonscribed providers (P = .044) (TABLE 2).
Cervical cancer screening. The rate at which cervical cancer screening was ordered did not change among scribed providers and decreased (by 2.5 percentage points) among nonscribed providers—a difference that was not statistically significant (P = .26).
Nonpreventive visits. Our findings overall did not change in analyses focused on nonpreventive visits, in which scribes were associated with an increase of 8.2 percentage points in LOS 4 or 5 billing (P < .001); an increase of 3.1 percentage points in HCC coding (P < .001); and an increase of 3.2 percentage points in breast cancer screening orders (P = .03) (TABLE 3). Although scribes were associated with an increase of 1.5 percentage points in cervical cancer screening orders and an increase of 3.1 percentage points in colon cancer screening orders, these increases did not reach statistical significance.
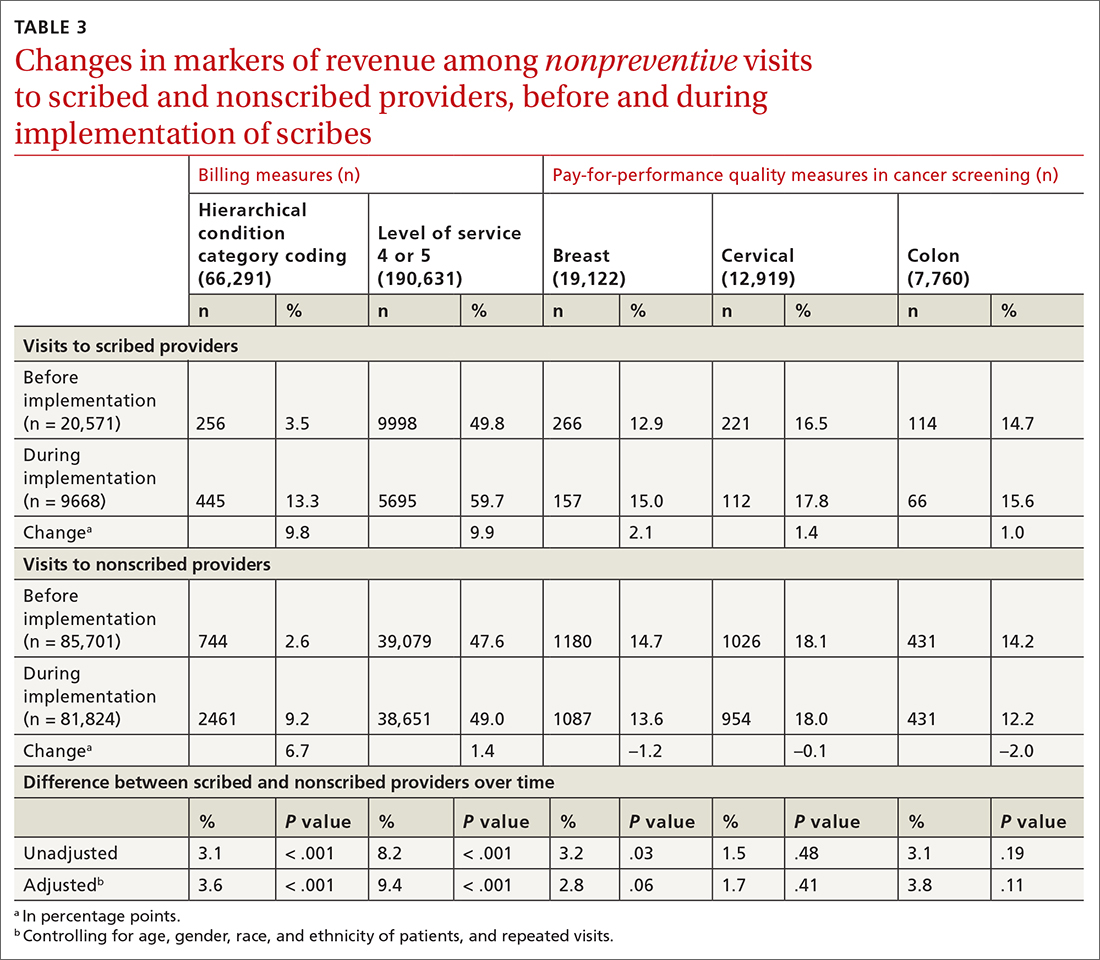
Discussion
We found that implementation of scribes is associated with (1) an increase in LOS coding and risk coding and (2) a higher frequency of addressing 2 of 3 pay-for-performance quality measures in primary care. In adjusted analyses in our study, and compared to nonscribed providers, scribes were associated with an additional 9.2 percentage points in LOS 4 or 5 billing; 3.6 percentage points in HCC coding; 4.0 percentage points in breast cancer screening orders; and 4.9 percentage points in colon cancer screening orders. Cervical cancer screening orders followed a similar pattern, with an increase of 2.3 percentage points in the adjusted screening order rate among scribed providers, compared to nonscribed providers, during implementation of scribes—although the increase was not significant. These findings did not change in analyses focused on nonpreventive visits.
Continue to: Our findings are consistent
Our findings are consistent with those of earlier studies. Prior examinations in ambulatory specialties found that scribes increased HCC coding,4 LOS billing,24 and pay-for-performance metrics.18 The only study to examine these areas in primary care found that scribes were associated with increased pay-for-performance measure documentation,20 a change that is necessary but insufficient to realize increased pay-for-performance revenue. Therefore, our study confirms, for the first time, that PCPs can better address pay-for-performance measures, LOS billing, and HCC coding when working with a scribe in primary care.
Demands on primary care visits are increasing.28 Physicians are required to provide more documentation; there is greater emphasis on PCPs meeting pay-for-performance measures; and there are more data in the EMR to review. In this context, addressing pay-for-performance measures and gaps in risk coding is likely to be increasingly challenging. Our study suggests that scribes might provide a mechanism to increase risk coding, LOS billing, and pay-for-performance measures, despite increased demands on primary care visits.
Increase in LOS billing. In the settings in which we work, a fee-for-service LOS 4 primary care visit generates, on average, $20 to $75 more in revenue than an LOS 3 visit. Using an average of $50 additional revenue for LOS 4 billing, we estimate that a full-time scribe is associated with roughly $7,000 in additional revenue annually. We arrived at this estimate using an average of 1500 visits at LOS ≤ 3 for every PCP full-time equivalent. A 9.2 percentage–point increase in LOS 4 billing would lead to roughly 140 additional LOS 4 visits, with each visit generating an additional $50 in revenue.
This analysis does not account for increased revenue associated with increased pay for HCC coding identified in our study.
Furthermore, in our conservative assumption, the entire increase in LOS billing was from level 3 to level 4; in fact, a small percentage of that increase would be from level 2 and another small percentage would be to level 5—both of which would generate additional revenue. Our assumption therefore underestimates the full financial value associated with scribes in the absence of increased patient volume. Nonetheless, the assumption suggests that increases in LOS billing offset a substantial percentage of a scribe’s salary.
Continue to: Limitations of this study
Limitations of this study. Our study should be interpreted in the context of several limitations:
- The study was conducted at 1 institution. Our findings might not be generalizable beyond this setting.
- The study measures the impact of scribes when providers work with scribes part time. Because providers who utilize a scribe for all, or nearly all, their visits are likely to use a scribe more efficiently, our study might underestimate the full impact of a scribe.
- In some settings, team members such as medical assistants are trained to assist with documentation and other responsibilities (such as closing care gaps) in addition to other patient care responsibilities.29-32 The extent to which our findings transfer to other models is unclear; studies comparing the impact of other models (which might provide even stronger outcomes) to the impact of medical scribes would be an interesting area for further research.
- In addition to the variability of models, there is likely variability in the quality and interactions of medical scribes, which might impact outcomes. We did not examine the qualities of scribes that led to outcomes in this study.
- We examined the impact of scribes on quality measure–ordering behaviors of providers, not on whether quality measures actually improved. Because scribes are associated with more face-to-face time with patients,27 they might allow for increased attention being paid by physicians to barriers to pay-for-performance measures (eg, patient education). This could increase the likelihood that patients complete a multitude of screenings, and thus improve adherence and follow-up. However, the impact of scribes on quality measures is a topic for future study.
Value beyond volume. Any limitations notwithstanding, our study suggests that scribes are associated with financial benefit in addition to the benefit of increased volume. Primary care practices should therefore consider the financial benefit of scribes independent of their ability to add patient volume. By recognizing this additive value, primary care practices might more fully capture the benefit of scribes, which might then allow practices to employ scribes with less demand to increase volume. This added support without increased volume would, in turn, likely reduce provider burnout (and the costly associated turnover) and increase patient satisfaction, leading to a synergistic financial benefit.
CORRESPONDENCE
Wayne Altman, MD, FAAFP, Tufts University School of Medicine, 200 Harrison Avenue, Boston, MA 02111; wayne. [email protected]
1. Gellert GA, Ramirez R, Webster SL. The rise of the medical scribe industry: implications for the advancement of electronic health records. JAMA. 2015;313:1315-1316. doi: 10.1001/jama.2014.1712
2. Cho J, Sanchez K, Ganor O, et al. Utilizing a physician scribe in a pediatric plastic surgical practice: a time-driven activity-based costing study. Plast Reconstr Surg Glob Open. 2019;7:e2460. doi: 10.1097/GOX.0000000000002460
3. Danak SU, Guetterman TC, Plegue MA, et al. Influence of scribes on patient-physician communication in primary care encounters: mixed methods study. JMIR Med Inform. 2019;7:e14797. doi: 10.2196/14797
4. Martel ML, Imdieke BH, Holm KM, et al. Developing a medical scribe program at an academic hospital: the Hennepin County Medical Center experience. Jt Comm J Qual Patient Saf. 2018;44:238-249. doi: 10.1016/j.jcjq.2018.01.001
5. Mishra P, Kiang JC, Grant RW. Association of medical scribes in primary care with physician workflow and patient experience. JAMA Intern Med. 2018;178:1467-1472. doi: 10.1001/ jamainternmed.2018.3956
6. Taylor KA, McQuilkin D, Hughes RG. Medical scribe impact on patient and provider experience. Mil Med. 2019;184:388-393. doi: 10.1093/milmed/usz030
7. Gidwani R, Nguyen C, Kofoed A, et al. Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: a randomized controlled trial. Ann Fam Med. 2017;15:427-433. doi: 10.1370/afm.2122.
8. Heckman J, Mukamal KJ, Christensen A, et al. Medical scribes, provider and patient experience, and patient throughput: a trial in an academic general internal medicine practice. J Gen Intern Med. 2019;35:770-774. doi: 10.1007/s11606-019-05352-5
9. Koshy S, Feustel PJ, Hong M, et al. Scribes in an ambulatory urology practice: patient and physician satisfaction. J Urol. 2010;184:258-262. doi: 10.1016/j.juro.2010.03.040
10. McCormick BJ, Deal A, Borawski KM, et al. Implementation of medical scribes in an academic urology practice: an analysis of productivity, revenue, and satisfaction. World J Urol. 2018;36:1691-1697. doi: 10.1007/s00345-018-2293-8
11. Pozdnyakova A, Laiteerapong N, Volerman A, et al. Impact of medical scribes on physician and patient satisfaction in primary care. J Gen Intern Med. Jul 2018;33:1109-1115. doi: 10.1007/ s11606-018-4434-6
12. Bank AJ, Obetz C, Konrardy A, et al. Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: a prospective study. Clinicoecon Outcomes Res. 2013;5:399-406. doi: 10.2147/CEOR.S49010
13. Danila MI, Melnick JA, Curtis JR, et al. Use of scribes for documentation assistance in rheumatology and endocrinology clinics: impact on clinic workflow and patient and physician satisfaction. J Clin Rheumatol. 2018;24:116-121. doi: 10.1097/ RHU.0000000000000620
14. Keefe KR, Levi JR, Brook CD. The impact of medical scribes on patient satisfaction in an academic otolaryngology clinic. Ann Otol Rhinol Laryngol. 2020;129:238-244. doi: 10.1177/0003489419884337
15. Lowry C, Orr K, Embry B, et al. Primary care scribes: writing a new story for safety net clinics. BMJ Open Qual. 2017;6:e000124. doi: 10.1136/bmjoq-2017-000124
16. Rohlfing ML, Keefe KR, Komshian SR, et al. Clinical scribes and their association with patient experience in the otolaryngology clinic. Laryngoscope. 2020;130:e134-e139. doi: 10.1002/ lary.28075
17. Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med. 2010;17:490-494. doi: 10.1111/j.1553- 2712.2010.00718.x
18. Ewelukwa O, Perez R, Carter LE, et al. Incorporation of scribes into the inflammatory bowel disease clinic improves quality of care and physician productivity. Inflamm Bowel Dis. 2018;24: 552-557. doi: 10.1093/ibd/izx078
19. Misra-Hebert AD, Yan C, Rothberg MB. Physician, scribe, and patient perspectives on clinical scribes in primary care. J Gen Intern Med. 2017;32:244. doi: 10.1007/s11606-016-3888-7
20. Platt J, Altman W. Can medical scribes improve quality measure documentation? J Fam Pract. Jun 2019;68:e1-e7.
21. Guglielmo WJ. What a scribe can do for you. Med Econ. Jan 6 2006;83:42,44-46.
22. Richmond M. Don’t use scribes for order entry. Emergency Medicine News. 2009;31:6-7. doi: 10.1097/01.EEM.0000360578.87654.cc
23. Schiff GD, Zucker L. Medical scribes: salvation for primary care or workaround for poor EMR usability? J Gen Intern Med. 2016;31:979-981. doi: 10.1007/s11606-016-3788-x
24. Bank AJ, Gage RM. Annual impact of scribes on physician productivity and revenue in a cardiology clinic. Clinicoecon Outcomes Res. 2015;7:489-495. doi: 10.2147/CEOR.S89329
25. Heaton HA, Castaneda-Guarderas A, Trotter ER, et al. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Am J Emerg Med. 2016;34:2018-2028. doi: 10.1016/j.ajem.2016.07.056
26. Earls ST, Savageau JA, Begley S, et al. Can scribes boost FPs’ efficiency and job satisfaction? J Fam Pract. 2017;66:206-214.
27. Zallman L, Finnegan K, Roll D, et al. Impact of medical scribes in primary care on productivity, face-to-face time, and patient comfort. J Am Board Fam Med. 2018;31:612-619. doi: 10.3122/ jabfm.2018.04.170325
28. Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23:2058-2065. doi: 10.1007/s11606- 008-0805-8
29. Ammann Howard K, Helé K, Salibi N, et al. Adapting the EHR scribe model to community health centers: the experience of Shasta Community Health Center’s pilot. Blue Shield of California Foundation; 2012. Accessed April 28, 2021. https:// blueshieldcafoundation.org/sites/default/files/publications/ downloadable/Shasta%20EHR%20Scribes%20Final%20Report.pdf
30. Anderson P, Halley MD. A new approach to making your doctor– nurse team more productive. Fam Pract Manag. 2008;15:35-40.
31. Blash L, Dower C, Chapman SA. University of Utah community clinics—medical assistant teams enhance patient-centered, physician-efficient care. Center for the Health Professions at UCSF; April 2011. Revised November 2011. Accessed April 28, 2021. https://healthforce.ucsf.edu/sites/healthforce.ucsf.edu/ files/publication-pdf/3.1%202011_04_University_of_Utah_Community_Clinics--Medical_Assistant_Teams_Enhance_PatientCentered_Physician-Efficient%20Care.pdf
32. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193. doi: 10.1001/ jamainternmed.2014.1315
1. Gellert GA, Ramirez R, Webster SL. The rise of the medical scribe industry: implications for the advancement of electronic health records. JAMA. 2015;313:1315-1316. doi: 10.1001/jama.2014.1712
2. Cho J, Sanchez K, Ganor O, et al. Utilizing a physician scribe in a pediatric plastic surgical practice: a time-driven activity-based costing study. Plast Reconstr Surg Glob Open. 2019;7:e2460. doi: 10.1097/GOX.0000000000002460
3. Danak SU, Guetterman TC, Plegue MA, et al. Influence of scribes on patient-physician communication in primary care encounters: mixed methods study. JMIR Med Inform. 2019;7:e14797. doi: 10.2196/14797
4. Martel ML, Imdieke BH, Holm KM, et al. Developing a medical scribe program at an academic hospital: the Hennepin County Medical Center experience. Jt Comm J Qual Patient Saf. 2018;44:238-249. doi: 10.1016/j.jcjq.2018.01.001
5. Mishra P, Kiang JC, Grant RW. Association of medical scribes in primary care with physician workflow and patient experience. JAMA Intern Med. 2018;178:1467-1472. doi: 10.1001/ jamainternmed.2018.3956
6. Taylor KA, McQuilkin D, Hughes RG. Medical scribe impact on patient and provider experience. Mil Med. 2019;184:388-393. doi: 10.1093/milmed/usz030
7. Gidwani R, Nguyen C, Kofoed A, et al. Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: a randomized controlled trial. Ann Fam Med. 2017;15:427-433. doi: 10.1370/afm.2122.
8. Heckman J, Mukamal KJ, Christensen A, et al. Medical scribes, provider and patient experience, and patient throughput: a trial in an academic general internal medicine practice. J Gen Intern Med. 2019;35:770-774. doi: 10.1007/s11606-019-05352-5
9. Koshy S, Feustel PJ, Hong M, et al. Scribes in an ambulatory urology practice: patient and physician satisfaction. J Urol. 2010;184:258-262. doi: 10.1016/j.juro.2010.03.040
10. McCormick BJ, Deal A, Borawski KM, et al. Implementation of medical scribes in an academic urology practice: an analysis of productivity, revenue, and satisfaction. World J Urol. 2018;36:1691-1697. doi: 10.1007/s00345-018-2293-8
11. Pozdnyakova A, Laiteerapong N, Volerman A, et al. Impact of medical scribes on physician and patient satisfaction in primary care. J Gen Intern Med. Jul 2018;33:1109-1115. doi: 10.1007/ s11606-018-4434-6
12. Bank AJ, Obetz C, Konrardy A, et al. Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: a prospective study. Clinicoecon Outcomes Res. 2013;5:399-406. doi: 10.2147/CEOR.S49010
13. Danila MI, Melnick JA, Curtis JR, et al. Use of scribes for documentation assistance in rheumatology and endocrinology clinics: impact on clinic workflow and patient and physician satisfaction. J Clin Rheumatol. 2018;24:116-121. doi: 10.1097/ RHU.0000000000000620
14. Keefe KR, Levi JR, Brook CD. The impact of medical scribes on patient satisfaction in an academic otolaryngology clinic. Ann Otol Rhinol Laryngol. 2020;129:238-244. doi: 10.1177/0003489419884337
15. Lowry C, Orr K, Embry B, et al. Primary care scribes: writing a new story for safety net clinics. BMJ Open Qual. 2017;6:e000124. doi: 10.1136/bmjoq-2017-000124
16. Rohlfing ML, Keefe KR, Komshian SR, et al. Clinical scribes and their association with patient experience in the otolaryngology clinic. Laryngoscope. 2020;130:e134-e139. doi: 10.1002/ lary.28075
17. Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med. 2010;17:490-494. doi: 10.1111/j.1553- 2712.2010.00718.x
18. Ewelukwa O, Perez R, Carter LE, et al. Incorporation of scribes into the inflammatory bowel disease clinic improves quality of care and physician productivity. Inflamm Bowel Dis. 2018;24: 552-557. doi: 10.1093/ibd/izx078
19. Misra-Hebert AD, Yan C, Rothberg MB. Physician, scribe, and patient perspectives on clinical scribes in primary care. J Gen Intern Med. 2017;32:244. doi: 10.1007/s11606-016-3888-7
20. Platt J, Altman W. Can medical scribes improve quality measure documentation? J Fam Pract. Jun 2019;68:e1-e7.
21. Guglielmo WJ. What a scribe can do for you. Med Econ. Jan 6 2006;83:42,44-46.
22. Richmond M. Don’t use scribes for order entry. Emergency Medicine News. 2009;31:6-7. doi: 10.1097/01.EEM.0000360578.87654.cc
23. Schiff GD, Zucker L. Medical scribes: salvation for primary care or workaround for poor EMR usability? J Gen Intern Med. 2016;31:979-981. doi: 10.1007/s11606-016-3788-x
24. Bank AJ, Gage RM. Annual impact of scribes on physician productivity and revenue in a cardiology clinic. Clinicoecon Outcomes Res. 2015;7:489-495. doi: 10.2147/CEOR.S89329
25. Heaton HA, Castaneda-Guarderas A, Trotter ER, et al. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Am J Emerg Med. 2016;34:2018-2028. doi: 10.1016/j.ajem.2016.07.056
26. Earls ST, Savageau JA, Begley S, et al. Can scribes boost FPs’ efficiency and job satisfaction? J Fam Pract. 2017;66:206-214.
27. Zallman L, Finnegan K, Roll D, et al. Impact of medical scribes in primary care on productivity, face-to-face time, and patient comfort. J Am Board Fam Med. 2018;31:612-619. doi: 10.3122/ jabfm.2018.04.170325
28. Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23:2058-2065. doi: 10.1007/s11606- 008-0805-8
29. Ammann Howard K, Helé K, Salibi N, et al. Adapting the EHR scribe model to community health centers: the experience of Shasta Community Health Center’s pilot. Blue Shield of California Foundation; 2012. Accessed April 28, 2021. https:// blueshieldcafoundation.org/sites/default/files/publications/ downloadable/Shasta%20EHR%20Scribes%20Final%20Report.pdf
30. Anderson P, Halley MD. A new approach to making your doctor– nurse team more productive. Fam Pract Manag. 2008;15:35-40.
31. Blash L, Dower C, Chapman SA. University of Utah community clinics—medical assistant teams enhance patient-centered, physician-efficient care. Center for the Health Professions at UCSF; April 2011. Revised November 2011. Accessed April 28, 2021. https://healthforce.ucsf.edu/sites/healthforce.ucsf.edu/ files/publication-pdf/3.1%202011_04_University_of_Utah_Community_Clinics--Medical_Assistant_Teams_Enhance_PatientCentered_Physician-Efficient%20Care.pdf
32. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193. doi: 10.1001/ jamainternmed.2014.1315
Dr. Fauci: Extraordinary challenges, scientific triumphs with COVID-19
“Vaccines have been the bright light of this extraordinary challenge that we’ve gone through,” said Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases.
In an address for the opening ceremony of the American Thoracic Society’s virtual international conference, Dr. Fauci emphasized the role of basic and clinical research and government support for science in helping turn the tide of the COVID-19 pandemic.
“A few weeks ago, I wrote an editorial in Science, because there was some misunderstanding about how and why we were able to go from a realization of a new pathogen in January of 2020, to getting doses of vaccines in the arms of individuals – a highly efficacious vaccine – 11 months later. Truly, an unprecedented accomplishment,” he said.
“But as I said in the editorial, the speed and efficiency with which these highly efficacious vaccines were developed, and their potential for saving millions of lives, are due to an extraordinary multidisciplinary effort, involving basic, preclinical, and clinical science that had been underway – out of the spotlight – for decades and decades before the unfolding of the COVID-19 pandemic, a fact that very few people really appreciate: namely, the importance of investment in biomedical research.”
The general addresses the troops
Perhaps no other audience is so well suited to receive Dr. Fauci’s speech as those who are currently attending (virtually) the ATS conference, including researchers who scrutinize the virus from every angle to describe its workings and identify its vulnerabilities, epidemiologists who study viral transmission and look for ways to thwart it, public health workers who fan out to communities across the country to push vaccine acceptance, and clinicians who specialize in critical care and pulmonary medicine, many of whom staff the respiratory floors and intensive care units where the most severely ill patients are treated.
Speaking about the lessons learned and challenges remaining from the COVID-19 pandemic, Dr. Fauci briefly reviewed the epidemiology, virology and transmission, diagnostics, and clinical course of SARS-CoV-2 infections and the therapeutics and vaccines for COVID-19.
Epidemiology
The pandemic began in December 2019 with recognition of a novel type of pneumonia in the Wuhan District of Central China, Dr. Fauci noted.
“Very quickly thereafter, in the first week of January 2020, the Chinese identified a new strain of coronavirus as [the] source of the outbreak. Fast forward to where we are right now: We have experienced and are experiencing the most devastating pandemic of a respiratory illness in the last 102 years, with already approximately 160 million individuals having been infected – and this is clearly a gross undercounting – and also 3.3 million deaths, again, very likely an undercounting,” he said.
According to the Centers for Disease Control and Prevention, as of May 9, 2021, there were approximately 32.5 million cases of COVID-19 and 578,520 deaths in the United States. Those cases and deaths occurred largely in three surges in the United States, in early spring, early summer, and late fall of 2020.
Virology and transmission
SARS-CoV-2 is a beta-coronavirus in the same subgenus as SARS-CoV-1 and some bat coronaviruses, Dr. Fauci explained. The viral genome is large, about 30,000 kilobases, and it has four structural proteins, most importantly the S or “spike” protein that allows the virus to attach to and fuse with cell membranes by binding to the ACE2 receptor on tissues in the upper and lower respiratory tract, gastrointestinal tract, cardiovascular system, and other organ systems.
The virus is transmitted mainly through exposure to respiratory droplets within 6 feet of an infected person, or sometimes through droplets or particles that remain in the air over time and various distances.
Contact with contaminated surfaces, once feared as a means of transmission, is now understood to be less common.
The virus has been detected in stool, blood, semen, and ocular secretions, although the role of transmission through these sources is still unknown.
“Some very interesting characteristics of this virus, really quite unique compared to other viruses, certainly other respiratory viruses, is [that] about a third to 40% of people who are infected never develop any symptoms,” Dr. Fauci said. “Importantly, and very problematic to what we do to contain it – particularly with regard to identification, isolation, and contract tracing – between 50% and 60% of the transmissions occur either from someone who will never develop symptoms, or someone in the presymptomatic phase of disease.”
The fundamentals of preventing acquisition and transmission are as familiar to most Americans now as the Pledge of Allegiance: universal mask wearing, physical distancing, avoiding crowds and congregate settings, preference for outdoor over indoor settings, and frequent hand washing, he noted.
Diagnostics
Tests for SARS-CoV-2 infection fall into three basic categories: molecular tests such as polymerase chain reaction (PCR) that are highly specific and highly sensitive for actual infections, antigen tests that detect the viral protein rather than the nucleic acids, and antibody tests to detect serum proteins made in response to viral infection.
Antigen testing is used largely for broader surveillance of groups of individuals to detect viral penetrance within that group, Dr. Fauci noted.
Clinical course
The clinical course of COVID-19 has some interesting characteristics but is not substantially different from a flu-like syndrome, Dr. Fauci said.
Symptoms and signs common to both types of infections include fever, cough, fatigue, anorexia, dyspnea, and myalgias, but the loss of smell and/or taste preceding the onset of respiratory symptoms is a unique feature of COVID-19.
Dr. Fauci cited data on more than 44,000 individuals with confirmed COVID-19 in China that showed that a large majority (81%) of cases were mild or moderate in nature, but 14% of patients experienced severe disease, and 5% were critically ill. The case-fatality rate in this study was 2.3%.
People at increased risk for severe disease include older adults and those of any age with certain comorbidities.
Manifestations of severe COVID-19 infections in adults can include neurological disorders, hyperinflammation, acute respiratory distress syndrome, cardiac dysfunction, hypercoagulability, and acute kidney injury.
In children, COVID-19 has been associated with a multisystem inflammatory syndrome (MIS-C) similar to Kawasaki disease.
In a substantial number of cases, the effects of COVID-19 can linger for 6 months or longer, Dr. Fauci said, pointing to a study from the University of Washington in Seattle.
Investigators there found that approximately 30% of patients enrolled at their center reported persistent symptoms for as long as 9 months after the initial illness, with fatigue as the most commonly reported symptom. One-third of outpatients with mild disease also reported persistent symptoms.
Therapeutics
Therapeutics that are either approved by the Food and Drug Administration, have emergency use authorization, or are in clinical trials for early or moderate disease include remdesivir (Veklury, Gilead Sciences), monoclonal antibodies, convalescent plasma, antiviral agents, hyperimmune globulin, anticoagulants, and immunomodulators.
Options for moderate to severe to advanced disease include dexamethasone, baricitinib (Olumiant, Eli Lilly and Company) plus remdesivir, and immunomodulators such as infliximab (Remicade, Janssen Biotech), and biosimilars.
Vaccines
Finally, Dr. Fauci reviewed the current state of vaccines, including the three with emergency use authorization from the FDA as of this writing: two nucleic acid, messenger RNA-based (mRNA) vaccines from Moderna and Pfizer/BioNTech, and an adenoviral vector-based vaccine from Johnson & Johnson.
Other vaccines in development or in use elsewhere in the world include recombinant protein and adjuvant approaches by GlaxoSmithKline and Sanofi (in a phase 2 clinical trial launched in February 2021) and by Novavax.
The three vaccines in use in the United States were highly efficacious in both clinical trials, with efficacy of about 95% for the mRNA vaccines and 67% for the Johnson & Johnson vaccine.
The real-world performance of these vaccines has been even more impressive, however.
For example, the Johnson & Johnson vaccine had 72% efficacy at preventing moderate to severe COVID 19 in the United States, 68% in Brazil, and 64% in South Africa, and 85% efficacy against severe disease across all regions studied, Dr. Fauci said.
He cited a study of 22,234 employees of the University of Texas Southwestern Medical Center in Dallas who were vaccinated under a program started on Dec. 15, 2020. The COVID-19 infection rate among these vaccinated employees was 0.05%.
Dr. Fauci recounted the experience in Israel, where the highly transmissible B.1.1.7 strain of SARS-CoV-2 is predominant. A chart of the progress shows clearly that as the vaccine doses delivered steadily increased, the number of COVID-19 cases began a precipitous decline.
Horse race
Fittingly for a speech presented on the day that the Preakness Stakes – the second leg in thoroughbred racing’s Triple Crown – was run, Dr. Fauci closed with a cartoon showing two racehorses, labeled “SARS-CoV-2” and “Vaccines,” nearly neck-and-neck, but with vaccines having a slight lead.
“We are in a race against the virus. The vaccines, and the virus: If we vaccinate the overwhelming proportion of our population, we will without a doubt be able to crush the outbreak in the same way as we have done with other viral-borne diseases like measles, smallpox, and polio.
“So, the message is: Get vaccinated,” he concluded.
“Vaccines have been the bright light of this extraordinary challenge that we’ve gone through,” said Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases.
In an address for the opening ceremony of the American Thoracic Society’s virtual international conference, Dr. Fauci emphasized the role of basic and clinical research and government support for science in helping turn the tide of the COVID-19 pandemic.
“A few weeks ago, I wrote an editorial in Science, because there was some misunderstanding about how and why we were able to go from a realization of a new pathogen in January of 2020, to getting doses of vaccines in the arms of individuals – a highly efficacious vaccine – 11 months later. Truly, an unprecedented accomplishment,” he said.
“But as I said in the editorial, the speed and efficiency with which these highly efficacious vaccines were developed, and their potential for saving millions of lives, are due to an extraordinary multidisciplinary effort, involving basic, preclinical, and clinical science that had been underway – out of the spotlight – for decades and decades before the unfolding of the COVID-19 pandemic, a fact that very few people really appreciate: namely, the importance of investment in biomedical research.”
The general addresses the troops
Perhaps no other audience is so well suited to receive Dr. Fauci’s speech as those who are currently attending (virtually) the ATS conference, including researchers who scrutinize the virus from every angle to describe its workings and identify its vulnerabilities, epidemiologists who study viral transmission and look for ways to thwart it, public health workers who fan out to communities across the country to push vaccine acceptance, and clinicians who specialize in critical care and pulmonary medicine, many of whom staff the respiratory floors and intensive care units where the most severely ill patients are treated.
Speaking about the lessons learned and challenges remaining from the COVID-19 pandemic, Dr. Fauci briefly reviewed the epidemiology, virology and transmission, diagnostics, and clinical course of SARS-CoV-2 infections and the therapeutics and vaccines for COVID-19.
Epidemiology
The pandemic began in December 2019 with recognition of a novel type of pneumonia in the Wuhan District of Central China, Dr. Fauci noted.
“Very quickly thereafter, in the first week of January 2020, the Chinese identified a new strain of coronavirus as [the] source of the outbreak. Fast forward to where we are right now: We have experienced and are experiencing the most devastating pandemic of a respiratory illness in the last 102 years, with already approximately 160 million individuals having been infected – and this is clearly a gross undercounting – and also 3.3 million deaths, again, very likely an undercounting,” he said.
According to the Centers for Disease Control and Prevention, as of May 9, 2021, there were approximately 32.5 million cases of COVID-19 and 578,520 deaths in the United States. Those cases and deaths occurred largely in three surges in the United States, in early spring, early summer, and late fall of 2020.
Virology and transmission
SARS-CoV-2 is a beta-coronavirus in the same subgenus as SARS-CoV-1 and some bat coronaviruses, Dr. Fauci explained. The viral genome is large, about 30,000 kilobases, and it has four structural proteins, most importantly the S or “spike” protein that allows the virus to attach to and fuse with cell membranes by binding to the ACE2 receptor on tissues in the upper and lower respiratory tract, gastrointestinal tract, cardiovascular system, and other organ systems.
The virus is transmitted mainly through exposure to respiratory droplets within 6 feet of an infected person, or sometimes through droplets or particles that remain in the air over time and various distances.
Contact with contaminated surfaces, once feared as a means of transmission, is now understood to be less common.
The virus has been detected in stool, blood, semen, and ocular secretions, although the role of transmission through these sources is still unknown.
“Some very interesting characteristics of this virus, really quite unique compared to other viruses, certainly other respiratory viruses, is [that] about a third to 40% of people who are infected never develop any symptoms,” Dr. Fauci said. “Importantly, and very problematic to what we do to contain it – particularly with regard to identification, isolation, and contract tracing – between 50% and 60% of the transmissions occur either from someone who will never develop symptoms, or someone in the presymptomatic phase of disease.”
The fundamentals of preventing acquisition and transmission are as familiar to most Americans now as the Pledge of Allegiance: universal mask wearing, physical distancing, avoiding crowds and congregate settings, preference for outdoor over indoor settings, and frequent hand washing, he noted.
Diagnostics
Tests for SARS-CoV-2 infection fall into three basic categories: molecular tests such as polymerase chain reaction (PCR) that are highly specific and highly sensitive for actual infections, antigen tests that detect the viral protein rather than the nucleic acids, and antibody tests to detect serum proteins made in response to viral infection.
Antigen testing is used largely for broader surveillance of groups of individuals to detect viral penetrance within that group, Dr. Fauci noted.
Clinical course
The clinical course of COVID-19 has some interesting characteristics but is not substantially different from a flu-like syndrome, Dr. Fauci said.
Symptoms and signs common to both types of infections include fever, cough, fatigue, anorexia, dyspnea, and myalgias, but the loss of smell and/or taste preceding the onset of respiratory symptoms is a unique feature of COVID-19.
Dr. Fauci cited data on more than 44,000 individuals with confirmed COVID-19 in China that showed that a large majority (81%) of cases were mild or moderate in nature, but 14% of patients experienced severe disease, and 5% were critically ill. The case-fatality rate in this study was 2.3%.
People at increased risk for severe disease include older adults and those of any age with certain comorbidities.
Manifestations of severe COVID-19 infections in adults can include neurological disorders, hyperinflammation, acute respiratory distress syndrome, cardiac dysfunction, hypercoagulability, and acute kidney injury.
In children, COVID-19 has been associated with a multisystem inflammatory syndrome (MIS-C) similar to Kawasaki disease.
In a substantial number of cases, the effects of COVID-19 can linger for 6 months or longer, Dr. Fauci said, pointing to a study from the University of Washington in Seattle.
Investigators there found that approximately 30% of patients enrolled at their center reported persistent symptoms for as long as 9 months after the initial illness, with fatigue as the most commonly reported symptom. One-third of outpatients with mild disease also reported persistent symptoms.
Therapeutics
Therapeutics that are either approved by the Food and Drug Administration, have emergency use authorization, or are in clinical trials for early or moderate disease include remdesivir (Veklury, Gilead Sciences), monoclonal antibodies, convalescent plasma, antiviral agents, hyperimmune globulin, anticoagulants, and immunomodulators.
Options for moderate to severe to advanced disease include dexamethasone, baricitinib (Olumiant, Eli Lilly and Company) plus remdesivir, and immunomodulators such as infliximab (Remicade, Janssen Biotech), and biosimilars.
Vaccines
Finally, Dr. Fauci reviewed the current state of vaccines, including the three with emergency use authorization from the FDA as of this writing: two nucleic acid, messenger RNA-based (mRNA) vaccines from Moderna and Pfizer/BioNTech, and an adenoviral vector-based vaccine from Johnson & Johnson.
Other vaccines in development or in use elsewhere in the world include recombinant protein and adjuvant approaches by GlaxoSmithKline and Sanofi (in a phase 2 clinical trial launched in February 2021) and by Novavax.
The three vaccines in use in the United States were highly efficacious in both clinical trials, with efficacy of about 95% for the mRNA vaccines and 67% for the Johnson & Johnson vaccine.
The real-world performance of these vaccines has been even more impressive, however.
For example, the Johnson & Johnson vaccine had 72% efficacy at preventing moderate to severe COVID 19 in the United States, 68% in Brazil, and 64% in South Africa, and 85% efficacy against severe disease across all regions studied, Dr. Fauci said.
He cited a study of 22,234 employees of the University of Texas Southwestern Medical Center in Dallas who were vaccinated under a program started on Dec. 15, 2020. The COVID-19 infection rate among these vaccinated employees was 0.05%.
Dr. Fauci recounted the experience in Israel, where the highly transmissible B.1.1.7 strain of SARS-CoV-2 is predominant. A chart of the progress shows clearly that as the vaccine doses delivered steadily increased, the number of COVID-19 cases began a precipitous decline.
Horse race
Fittingly for a speech presented on the day that the Preakness Stakes – the second leg in thoroughbred racing’s Triple Crown – was run, Dr. Fauci closed with a cartoon showing two racehorses, labeled “SARS-CoV-2” and “Vaccines,” nearly neck-and-neck, but with vaccines having a slight lead.
“We are in a race against the virus. The vaccines, and the virus: If we vaccinate the overwhelming proportion of our population, we will without a doubt be able to crush the outbreak in the same way as we have done with other viral-borne diseases like measles, smallpox, and polio.
“So, the message is: Get vaccinated,” he concluded.
“Vaccines have been the bright light of this extraordinary challenge that we’ve gone through,” said Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases.
In an address for the opening ceremony of the American Thoracic Society’s virtual international conference, Dr. Fauci emphasized the role of basic and clinical research and government support for science in helping turn the tide of the COVID-19 pandemic.
“A few weeks ago, I wrote an editorial in Science, because there was some misunderstanding about how and why we were able to go from a realization of a new pathogen in January of 2020, to getting doses of vaccines in the arms of individuals – a highly efficacious vaccine – 11 months later. Truly, an unprecedented accomplishment,” he said.
“But as I said in the editorial, the speed and efficiency with which these highly efficacious vaccines were developed, and their potential for saving millions of lives, are due to an extraordinary multidisciplinary effort, involving basic, preclinical, and clinical science that had been underway – out of the spotlight – for decades and decades before the unfolding of the COVID-19 pandemic, a fact that very few people really appreciate: namely, the importance of investment in biomedical research.”
The general addresses the troops
Perhaps no other audience is so well suited to receive Dr. Fauci’s speech as those who are currently attending (virtually) the ATS conference, including researchers who scrutinize the virus from every angle to describe its workings and identify its vulnerabilities, epidemiologists who study viral transmission and look for ways to thwart it, public health workers who fan out to communities across the country to push vaccine acceptance, and clinicians who specialize in critical care and pulmonary medicine, many of whom staff the respiratory floors and intensive care units where the most severely ill patients are treated.
Speaking about the lessons learned and challenges remaining from the COVID-19 pandemic, Dr. Fauci briefly reviewed the epidemiology, virology and transmission, diagnostics, and clinical course of SARS-CoV-2 infections and the therapeutics and vaccines for COVID-19.
Epidemiology
The pandemic began in December 2019 with recognition of a novel type of pneumonia in the Wuhan District of Central China, Dr. Fauci noted.
“Very quickly thereafter, in the first week of January 2020, the Chinese identified a new strain of coronavirus as [the] source of the outbreak. Fast forward to where we are right now: We have experienced and are experiencing the most devastating pandemic of a respiratory illness in the last 102 years, with already approximately 160 million individuals having been infected – and this is clearly a gross undercounting – and also 3.3 million deaths, again, very likely an undercounting,” he said.
According to the Centers for Disease Control and Prevention, as of May 9, 2021, there were approximately 32.5 million cases of COVID-19 and 578,520 deaths in the United States. Those cases and deaths occurred largely in three surges in the United States, in early spring, early summer, and late fall of 2020.
Virology and transmission
SARS-CoV-2 is a beta-coronavirus in the same subgenus as SARS-CoV-1 and some bat coronaviruses, Dr. Fauci explained. The viral genome is large, about 30,000 kilobases, and it has four structural proteins, most importantly the S or “spike” protein that allows the virus to attach to and fuse with cell membranes by binding to the ACE2 receptor on tissues in the upper and lower respiratory tract, gastrointestinal tract, cardiovascular system, and other organ systems.
The virus is transmitted mainly through exposure to respiratory droplets within 6 feet of an infected person, or sometimes through droplets or particles that remain in the air over time and various distances.
Contact with contaminated surfaces, once feared as a means of transmission, is now understood to be less common.
The virus has been detected in stool, blood, semen, and ocular secretions, although the role of transmission through these sources is still unknown.
“Some very interesting characteristics of this virus, really quite unique compared to other viruses, certainly other respiratory viruses, is [that] about a third to 40% of people who are infected never develop any symptoms,” Dr. Fauci said. “Importantly, and very problematic to what we do to contain it – particularly with regard to identification, isolation, and contract tracing – between 50% and 60% of the transmissions occur either from someone who will never develop symptoms, or someone in the presymptomatic phase of disease.”
The fundamentals of preventing acquisition and transmission are as familiar to most Americans now as the Pledge of Allegiance: universal mask wearing, physical distancing, avoiding crowds and congregate settings, preference for outdoor over indoor settings, and frequent hand washing, he noted.
Diagnostics
Tests for SARS-CoV-2 infection fall into three basic categories: molecular tests such as polymerase chain reaction (PCR) that are highly specific and highly sensitive for actual infections, antigen tests that detect the viral protein rather than the nucleic acids, and antibody tests to detect serum proteins made in response to viral infection.
Antigen testing is used largely for broader surveillance of groups of individuals to detect viral penetrance within that group, Dr. Fauci noted.
Clinical course
The clinical course of COVID-19 has some interesting characteristics but is not substantially different from a flu-like syndrome, Dr. Fauci said.
Symptoms and signs common to both types of infections include fever, cough, fatigue, anorexia, dyspnea, and myalgias, but the loss of smell and/or taste preceding the onset of respiratory symptoms is a unique feature of COVID-19.
Dr. Fauci cited data on more than 44,000 individuals with confirmed COVID-19 in China that showed that a large majority (81%) of cases were mild or moderate in nature, but 14% of patients experienced severe disease, and 5% were critically ill. The case-fatality rate in this study was 2.3%.
People at increased risk for severe disease include older adults and those of any age with certain comorbidities.
Manifestations of severe COVID-19 infections in adults can include neurological disorders, hyperinflammation, acute respiratory distress syndrome, cardiac dysfunction, hypercoagulability, and acute kidney injury.
In children, COVID-19 has been associated with a multisystem inflammatory syndrome (MIS-C) similar to Kawasaki disease.
In a substantial number of cases, the effects of COVID-19 can linger for 6 months or longer, Dr. Fauci said, pointing to a study from the University of Washington in Seattle.
Investigators there found that approximately 30% of patients enrolled at their center reported persistent symptoms for as long as 9 months after the initial illness, with fatigue as the most commonly reported symptom. One-third of outpatients with mild disease also reported persistent symptoms.
Therapeutics
Therapeutics that are either approved by the Food and Drug Administration, have emergency use authorization, or are in clinical trials for early or moderate disease include remdesivir (Veklury, Gilead Sciences), monoclonal antibodies, convalescent plasma, antiviral agents, hyperimmune globulin, anticoagulants, and immunomodulators.
Options for moderate to severe to advanced disease include dexamethasone, baricitinib (Olumiant, Eli Lilly and Company) plus remdesivir, and immunomodulators such as infliximab (Remicade, Janssen Biotech), and biosimilars.
Vaccines
Finally, Dr. Fauci reviewed the current state of vaccines, including the three with emergency use authorization from the FDA as of this writing: two nucleic acid, messenger RNA-based (mRNA) vaccines from Moderna and Pfizer/BioNTech, and an adenoviral vector-based vaccine from Johnson & Johnson.
Other vaccines in development or in use elsewhere in the world include recombinant protein and adjuvant approaches by GlaxoSmithKline and Sanofi (in a phase 2 clinical trial launched in February 2021) and by Novavax.
The three vaccines in use in the United States were highly efficacious in both clinical trials, with efficacy of about 95% for the mRNA vaccines and 67% for the Johnson & Johnson vaccine.
The real-world performance of these vaccines has been even more impressive, however.
For example, the Johnson & Johnson vaccine had 72% efficacy at preventing moderate to severe COVID 19 in the United States, 68% in Brazil, and 64% in South Africa, and 85% efficacy against severe disease across all regions studied, Dr. Fauci said.
He cited a study of 22,234 employees of the University of Texas Southwestern Medical Center in Dallas who were vaccinated under a program started on Dec. 15, 2020. The COVID-19 infection rate among these vaccinated employees was 0.05%.
Dr. Fauci recounted the experience in Israel, where the highly transmissible B.1.1.7 strain of SARS-CoV-2 is predominant. A chart of the progress shows clearly that as the vaccine doses delivered steadily increased, the number of COVID-19 cases began a precipitous decline.
Horse race
Fittingly for a speech presented on the day that the Preakness Stakes – the second leg in thoroughbred racing’s Triple Crown – was run, Dr. Fauci closed with a cartoon showing two racehorses, labeled “SARS-CoV-2” and “Vaccines,” nearly neck-and-neck, but with vaccines having a slight lead.
“We are in a race against the virus. The vaccines, and the virus: If we vaccinate the overwhelming proportion of our population, we will without a doubt be able to crush the outbreak in the same way as we have done with other viral-borne diseases like measles, smallpox, and polio.
“So, the message is: Get vaccinated,” he concluded.










