User login
Well tolerated with promising responses in ALL/LL: Venetoclax plus navitoclax plus chemotherapy
In heavily pretreated pediatric patients with relapsed or refractory acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), venetoclax plus navitoclax with chemotherapy was well tolerated with promising responses, according to results of a phase 1 trial. Delayed count recovery, however, stated lead author Jeffrey E. Rubnitz, MD, PhD, St. Jude’s Children’s Research Hospital, Memphis, remained a key safety concern.
Unmet medical need
Despite intensive chemotherapy and novel therapeutics, Dr. Rubnitz said in a virtual oral presentation at the annual meeting of the American Society of Hematology, patients with relapsed or refractory ALL and LL have a poor prognosis and represent an unmet medical need. Venetoclax, a potent, highly selective oral B-cell lymphoma 2 inhibitor, and navitoclax, an oral BCL-2, BCL-XL, and BCL-W inhibitor, directly bind their BCL-2 family member targets to promote apoptosis. In ALL preclinical models, venetoclax and navitoclax have demonstrated antileukemic effects, which suggests dependence on BCL-2 family members. Venetoclax efficacy associated with BCL-2 family inhibition may be potentiated and dose-limiting thrombocytopenia associated with standard-dose navitoclax monotherapy may be avoided by adding venetoclax to low-dose navitoclax. Previous reports of an ongoing phase 1, multicenter, open-label, dose-escalation study in an adult and pediatric population (NCT03181126), Dr. Rubnitz noted, showed the venetoclax/navitoclax/chemotherapy combination to be well tolerated with promising response rates. In the current report, Dr. Rubnitz presented data on the safety, tolerability, pharmacokinetics, and antitumor activity of the triplet regimen in the subgroup of pediatric patients.
The study included pediatric patients (ages, 4-18 years and weight ≥20 kg) receiving venetoclax (weight-adjusted equivalent of 400 mg daily) and navitoclax at three dose levels (25, 50, 100 mg) for patients weighing ≥45 kg and two dose levels (25, 50 mg) for patients weighing <45 kg. At investigator’s discretion, patients could receive chemotherapy (polyethylene glycosylated–asparaginase, vincristine, and dexamethasone). The primary outcomes were safety (including incidence of dose-limiting toxicities and adverse events) and pharmacokinetics. A safety expansion cohort assessed a 21-day dosing schedule of venetoclax at 400 mg followed by 7 days off plus navitoclax at 50 mg (patients ≥45 kg) or 25 mg (patients <45 kg).
Investigators enrolled 18 patients <18 years (median age, 10 years; range, 6-16; 56% male), with 12 in the dose-escalation cohort and 6 in the safety-expansion cohort. Three patients had prior chimeric antigen receptor (CAR) T treatment and four had received prior stem cell transplantation. In the overall cohort, B-cell ALL was most common (n = 13, 72%), with T-cell ALL (n = 3, 17%) and LL (n = 2, 11%) following. The median number of prior therapies was 2 (range 1-6). All patients received chemotherapy.
Grade 3-4 adverse events
Venetoclax-related grade 3-4 adverse events occurred in 56% of patients. Similarly, navitoclax-related grade 3-4 events were reported in 56% of patients. Navitoclax dose-limiting toxicities occurred in two patients (11%), delayed count recovery on 25 mg and sepsis on 50 mg. No grade 5 adverse events and tumor lysis syndrome were reported.
Among secondary endpoint efficacy parameters, complete responses, CRs with incomplete marrow recovery (CRi) and CRs without platelet recovery (CRp) combined occurred in 62% of B-ALL patients (8/13), 33% of T-cell ALL patients (1/3) and in 50% of LL patients (1/2). Separately, CRs/CRis/CRps occurred in 33%/22%/0% of all patients, respectively.
Subsequently, 5 of 18 (28%) of patients proceeded to stem cell transplantation and 3 (17%) to CAR T. Eight patients (44%) died from disease progression.
BH3 profiling
BH3 profiling revealed that at baseline, patients with B-cell ALL had more diversity in BCL-2 and BCL-XL dependency than did patients with T-cell ALL or early T-cell precursor ALL. The fact that responses were observed in patients who were BCL-2 or BCL-XL dependent, Dr. Rubnitz said, supports the use of venetoclax plus navitoclax in these patients. Analysis of these results led to a recommended phase 2 dose for pediatric patients of 400 mg venetoclax with 25 mg navitoclax (for patients weighing <45 kg) or 50 mg navitoclax (for patients weighing 45 kg or more).
Dr. Rubnitz concluded: “Venetoclax plus navitoclax plus chemotherapy was well tolerated in pediatric patients with relapsed/refractory ALL or LL, with promising response rates observed in a heavily pretreated pediatric population.”
Asked whether the combination might be used also before the refractory setting, in a minimal residual disease (MRD) setting, Dr. Rubnitz replied: “We have a lot of safety data on venetoclax but very little on navitoclax. The next trial, being developed by Seth Karol, MD, will include relapsed patients. MRD-positive patients will also be eligible for enrollment.” To a further question as to whether guiding titration via BH3 profiling would lead to improved outcomes, Dr. Rubnitz said, “I think BH3 profiling can be used to identify which patients will respond to these drugs, but we are still a long way from using it for titrating the doses and dose ratios for the two drugs.”
Dr. Rubnitz disclosed research funding from AbbVie.
SOURCE: Rubnitz JE et al. ASH 2020, Abstract 466.
In heavily pretreated pediatric patients with relapsed or refractory acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), venetoclax plus navitoclax with chemotherapy was well tolerated with promising responses, according to results of a phase 1 trial. Delayed count recovery, however, stated lead author Jeffrey E. Rubnitz, MD, PhD, St. Jude’s Children’s Research Hospital, Memphis, remained a key safety concern.
Unmet medical need
Despite intensive chemotherapy and novel therapeutics, Dr. Rubnitz said in a virtual oral presentation at the annual meeting of the American Society of Hematology, patients with relapsed or refractory ALL and LL have a poor prognosis and represent an unmet medical need. Venetoclax, a potent, highly selective oral B-cell lymphoma 2 inhibitor, and navitoclax, an oral BCL-2, BCL-XL, and BCL-W inhibitor, directly bind their BCL-2 family member targets to promote apoptosis. In ALL preclinical models, venetoclax and navitoclax have demonstrated antileukemic effects, which suggests dependence on BCL-2 family members. Venetoclax efficacy associated with BCL-2 family inhibition may be potentiated and dose-limiting thrombocytopenia associated with standard-dose navitoclax monotherapy may be avoided by adding venetoclax to low-dose navitoclax. Previous reports of an ongoing phase 1, multicenter, open-label, dose-escalation study in an adult and pediatric population (NCT03181126), Dr. Rubnitz noted, showed the venetoclax/navitoclax/chemotherapy combination to be well tolerated with promising response rates. In the current report, Dr. Rubnitz presented data on the safety, tolerability, pharmacokinetics, and antitumor activity of the triplet regimen in the subgroup of pediatric patients.
The study included pediatric patients (ages, 4-18 years and weight ≥20 kg) receiving venetoclax (weight-adjusted equivalent of 400 mg daily) and navitoclax at three dose levels (25, 50, 100 mg) for patients weighing ≥45 kg and two dose levels (25, 50 mg) for patients weighing <45 kg. At investigator’s discretion, patients could receive chemotherapy (polyethylene glycosylated–asparaginase, vincristine, and dexamethasone). The primary outcomes were safety (including incidence of dose-limiting toxicities and adverse events) and pharmacokinetics. A safety expansion cohort assessed a 21-day dosing schedule of venetoclax at 400 mg followed by 7 days off plus navitoclax at 50 mg (patients ≥45 kg) or 25 mg (patients <45 kg).
Investigators enrolled 18 patients <18 years (median age, 10 years; range, 6-16; 56% male), with 12 in the dose-escalation cohort and 6 in the safety-expansion cohort. Three patients had prior chimeric antigen receptor (CAR) T treatment and four had received prior stem cell transplantation. In the overall cohort, B-cell ALL was most common (n = 13, 72%), with T-cell ALL (n = 3, 17%) and LL (n = 2, 11%) following. The median number of prior therapies was 2 (range 1-6). All patients received chemotherapy.
Grade 3-4 adverse events
Venetoclax-related grade 3-4 adverse events occurred in 56% of patients. Similarly, navitoclax-related grade 3-4 events were reported in 56% of patients. Navitoclax dose-limiting toxicities occurred in two patients (11%), delayed count recovery on 25 mg and sepsis on 50 mg. No grade 5 adverse events and tumor lysis syndrome were reported.
Among secondary endpoint efficacy parameters, complete responses, CRs with incomplete marrow recovery (CRi) and CRs without platelet recovery (CRp) combined occurred in 62% of B-ALL patients (8/13), 33% of T-cell ALL patients (1/3) and in 50% of LL patients (1/2). Separately, CRs/CRis/CRps occurred in 33%/22%/0% of all patients, respectively.
Subsequently, 5 of 18 (28%) of patients proceeded to stem cell transplantation and 3 (17%) to CAR T. Eight patients (44%) died from disease progression.
BH3 profiling
BH3 profiling revealed that at baseline, patients with B-cell ALL had more diversity in BCL-2 and BCL-XL dependency than did patients with T-cell ALL or early T-cell precursor ALL. The fact that responses were observed in patients who were BCL-2 or BCL-XL dependent, Dr. Rubnitz said, supports the use of venetoclax plus navitoclax in these patients. Analysis of these results led to a recommended phase 2 dose for pediatric patients of 400 mg venetoclax with 25 mg navitoclax (for patients weighing <45 kg) or 50 mg navitoclax (for patients weighing 45 kg or more).
Dr. Rubnitz concluded: “Venetoclax plus navitoclax plus chemotherapy was well tolerated in pediatric patients with relapsed/refractory ALL or LL, with promising response rates observed in a heavily pretreated pediatric population.”
Asked whether the combination might be used also before the refractory setting, in a minimal residual disease (MRD) setting, Dr. Rubnitz replied: “We have a lot of safety data on venetoclax but very little on navitoclax. The next trial, being developed by Seth Karol, MD, will include relapsed patients. MRD-positive patients will also be eligible for enrollment.” To a further question as to whether guiding titration via BH3 profiling would lead to improved outcomes, Dr. Rubnitz said, “I think BH3 profiling can be used to identify which patients will respond to these drugs, but we are still a long way from using it for titrating the doses and dose ratios for the two drugs.”
Dr. Rubnitz disclosed research funding from AbbVie.
SOURCE: Rubnitz JE et al. ASH 2020, Abstract 466.
In heavily pretreated pediatric patients with relapsed or refractory acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), venetoclax plus navitoclax with chemotherapy was well tolerated with promising responses, according to results of a phase 1 trial. Delayed count recovery, however, stated lead author Jeffrey E. Rubnitz, MD, PhD, St. Jude’s Children’s Research Hospital, Memphis, remained a key safety concern.
Unmet medical need
Despite intensive chemotherapy and novel therapeutics, Dr. Rubnitz said in a virtual oral presentation at the annual meeting of the American Society of Hematology, patients with relapsed or refractory ALL and LL have a poor prognosis and represent an unmet medical need. Venetoclax, a potent, highly selective oral B-cell lymphoma 2 inhibitor, and navitoclax, an oral BCL-2, BCL-XL, and BCL-W inhibitor, directly bind their BCL-2 family member targets to promote apoptosis. In ALL preclinical models, venetoclax and navitoclax have demonstrated antileukemic effects, which suggests dependence on BCL-2 family members. Venetoclax efficacy associated with BCL-2 family inhibition may be potentiated and dose-limiting thrombocytopenia associated with standard-dose navitoclax monotherapy may be avoided by adding venetoclax to low-dose navitoclax. Previous reports of an ongoing phase 1, multicenter, open-label, dose-escalation study in an adult and pediatric population (NCT03181126), Dr. Rubnitz noted, showed the venetoclax/navitoclax/chemotherapy combination to be well tolerated with promising response rates. In the current report, Dr. Rubnitz presented data on the safety, tolerability, pharmacokinetics, and antitumor activity of the triplet regimen in the subgroup of pediatric patients.
The study included pediatric patients (ages, 4-18 years and weight ≥20 kg) receiving venetoclax (weight-adjusted equivalent of 400 mg daily) and navitoclax at three dose levels (25, 50, 100 mg) for patients weighing ≥45 kg and two dose levels (25, 50 mg) for patients weighing <45 kg. At investigator’s discretion, patients could receive chemotherapy (polyethylene glycosylated–asparaginase, vincristine, and dexamethasone). The primary outcomes were safety (including incidence of dose-limiting toxicities and adverse events) and pharmacokinetics. A safety expansion cohort assessed a 21-day dosing schedule of venetoclax at 400 mg followed by 7 days off plus navitoclax at 50 mg (patients ≥45 kg) or 25 mg (patients <45 kg).
Investigators enrolled 18 patients <18 years (median age, 10 years; range, 6-16; 56% male), with 12 in the dose-escalation cohort and 6 in the safety-expansion cohort. Three patients had prior chimeric antigen receptor (CAR) T treatment and four had received prior stem cell transplantation. In the overall cohort, B-cell ALL was most common (n = 13, 72%), with T-cell ALL (n = 3, 17%) and LL (n = 2, 11%) following. The median number of prior therapies was 2 (range 1-6). All patients received chemotherapy.
Grade 3-4 adverse events
Venetoclax-related grade 3-4 adverse events occurred in 56% of patients. Similarly, navitoclax-related grade 3-4 events were reported in 56% of patients. Navitoclax dose-limiting toxicities occurred in two patients (11%), delayed count recovery on 25 mg and sepsis on 50 mg. No grade 5 adverse events and tumor lysis syndrome were reported.
Among secondary endpoint efficacy parameters, complete responses, CRs with incomplete marrow recovery (CRi) and CRs without platelet recovery (CRp) combined occurred in 62% of B-ALL patients (8/13), 33% of T-cell ALL patients (1/3) and in 50% of LL patients (1/2). Separately, CRs/CRis/CRps occurred in 33%/22%/0% of all patients, respectively.
Subsequently, 5 of 18 (28%) of patients proceeded to stem cell transplantation and 3 (17%) to CAR T. Eight patients (44%) died from disease progression.
BH3 profiling
BH3 profiling revealed that at baseline, patients with B-cell ALL had more diversity in BCL-2 and BCL-XL dependency than did patients with T-cell ALL or early T-cell precursor ALL. The fact that responses were observed in patients who were BCL-2 or BCL-XL dependent, Dr. Rubnitz said, supports the use of venetoclax plus navitoclax in these patients. Analysis of these results led to a recommended phase 2 dose for pediatric patients of 400 mg venetoclax with 25 mg navitoclax (for patients weighing <45 kg) or 50 mg navitoclax (for patients weighing 45 kg or more).
Dr. Rubnitz concluded: “Venetoclax plus navitoclax plus chemotherapy was well tolerated in pediatric patients with relapsed/refractory ALL or LL, with promising response rates observed in a heavily pretreated pediatric population.”
Asked whether the combination might be used also before the refractory setting, in a minimal residual disease (MRD) setting, Dr. Rubnitz replied: “We have a lot of safety data on venetoclax but very little on navitoclax. The next trial, being developed by Seth Karol, MD, will include relapsed patients. MRD-positive patients will also be eligible for enrollment.” To a further question as to whether guiding titration via BH3 profiling would lead to improved outcomes, Dr. Rubnitz said, “I think BH3 profiling can be used to identify which patients will respond to these drugs, but we are still a long way from using it for titrating the doses and dose ratios for the two drugs.”
Dr. Rubnitz disclosed research funding from AbbVie.
SOURCE: Rubnitz JE et al. ASH 2020, Abstract 466.
FROM ASH 2020
FDA clears first OTC rapid at-home COVID diagnostic test
The Food and Drug Administration has issued an emergency-use authorization (EUA) for the first COVID-19 diagnostic test that can be completed at home without a prescription.
Authorization of the Ellume COVID-19 Home Test is “a major milestone in diagnostic testing for COVID-19,” FDA Commissioner Stephen M. Hahn, MD, said in a news release.
“By authorizing a test for over-the-counter use, the FDA allows it to be sold in places like drug stores, where a patient can buy it, swab their nose, run the test, and find out their results in as little as 20 minutes,” said Dr. Hahn.
The Ellume COVID-19 Home Test is a rapid antigen test that detects fragments of the SARS-CoV-2 virus from a nasal swab sample taken from anyone aged 2 years and older, including those not showing any symptoms.
In testing, the Ellume COVID-19 Home Test correctly identified 96% of positive samples and 100% of negative samples in individuals with symptoms.
In people without symptoms, the test correctly identified 91% of positive samples and 96% of negative samples, the FDA said.
The test includes a sterile nasal swab, a dropper, processing fluid, and a Bluetooth-connected analyzer for use with an app on the user’s smartphone. The sample is analyzed and results are automatically transmitted to the user’s smartphone.
“The Ellume COVID-19 home test’s core technology combines ultra-sensitive optics, electronics, and proprietary software to leverage best-in-class digital immunoassay technology with next-generation multi-quantum dot fluorescence technology,” the company said in a news release.
The mobile app requires individuals to input their ZIP code and date of birth, with optional fields including name and email address. The app automatically reports the results as appropriate to public health authorities to monitor disease prevalence.
Ellume expects to produce more than 3 million tests in January 2021. The company said the test will cost around $30.
FDA authorization of this first fully at-home nonprescription COVID-19 diagnostic test follows last month’s EUA for the first prescription COVID-19 test for home use, as reported this news organization.
Since the start of the pandemic, the FDA has authorized more than 225 diagnostic tests for COVID-19, including more than 25 tests that allow for home collection of samples, which are then sent to a lab for testing.
“As we continue to authorize additional tests for home use, we are helping expand Americans’ access to testing, reducing the burden on laboratories and test supplies, and giving Americans more testing options from the comfort and safety of their own homes,” Dr. Hahn said.
“This test, like other antigen tests, is less sensitive and less specific than typical molecular tests run in a lab,” said Jeffrey Shuren, MD, JD, director of FDA’s Center for Devices and Radiological Health, in the release. “However, the fact that it can be used completely at home and return results quickly means that it can play an important role in response to the pandemic.”
As with other antigen tests, a small percentage of positive and negative results from the Ellume test may be false. In patients without symptoms, positive results should be treated as presumptively positive until confirmed by another test as soon as possible, the FDA advised.
This is especially true if there are fewer infections in a particular community, as false-positive results can be more common when antigen tests are used in populations where there is a low prevalence of COVID-19, the agency said.
Because all tests can give false-negative and false-positive results, individuals with positive results should self-isolate and seek additional care from their health care provider.
Individuals who test negative and have symptoms of COVID-19 should follow up with their health care provider, as negative results don’t preclude an individual from SARS-CoV-2 infection.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has issued an emergency-use authorization (EUA) for the first COVID-19 diagnostic test that can be completed at home without a prescription.
Authorization of the Ellume COVID-19 Home Test is “a major milestone in diagnostic testing for COVID-19,” FDA Commissioner Stephen M. Hahn, MD, said in a news release.
“By authorizing a test for over-the-counter use, the FDA allows it to be sold in places like drug stores, where a patient can buy it, swab their nose, run the test, and find out their results in as little as 20 minutes,” said Dr. Hahn.
The Ellume COVID-19 Home Test is a rapid antigen test that detects fragments of the SARS-CoV-2 virus from a nasal swab sample taken from anyone aged 2 years and older, including those not showing any symptoms.
In testing, the Ellume COVID-19 Home Test correctly identified 96% of positive samples and 100% of negative samples in individuals with symptoms.
In people without symptoms, the test correctly identified 91% of positive samples and 96% of negative samples, the FDA said.
The test includes a sterile nasal swab, a dropper, processing fluid, and a Bluetooth-connected analyzer for use with an app on the user’s smartphone. The sample is analyzed and results are automatically transmitted to the user’s smartphone.
“The Ellume COVID-19 home test’s core technology combines ultra-sensitive optics, electronics, and proprietary software to leverage best-in-class digital immunoassay technology with next-generation multi-quantum dot fluorescence technology,” the company said in a news release.
The mobile app requires individuals to input their ZIP code and date of birth, with optional fields including name and email address. The app automatically reports the results as appropriate to public health authorities to monitor disease prevalence.
Ellume expects to produce more than 3 million tests in January 2021. The company said the test will cost around $30.
FDA authorization of this first fully at-home nonprescription COVID-19 diagnostic test follows last month’s EUA for the first prescription COVID-19 test for home use, as reported this news organization.
Since the start of the pandemic, the FDA has authorized more than 225 diagnostic tests for COVID-19, including more than 25 tests that allow for home collection of samples, which are then sent to a lab for testing.
“As we continue to authorize additional tests for home use, we are helping expand Americans’ access to testing, reducing the burden on laboratories and test supplies, and giving Americans more testing options from the comfort and safety of their own homes,” Dr. Hahn said.
“This test, like other antigen tests, is less sensitive and less specific than typical molecular tests run in a lab,” said Jeffrey Shuren, MD, JD, director of FDA’s Center for Devices and Radiological Health, in the release. “However, the fact that it can be used completely at home and return results quickly means that it can play an important role in response to the pandemic.”
As with other antigen tests, a small percentage of positive and negative results from the Ellume test may be false. In patients without symptoms, positive results should be treated as presumptively positive until confirmed by another test as soon as possible, the FDA advised.
This is especially true if there are fewer infections in a particular community, as false-positive results can be more common when antigen tests are used in populations where there is a low prevalence of COVID-19, the agency said.
Because all tests can give false-negative and false-positive results, individuals with positive results should self-isolate and seek additional care from their health care provider.
Individuals who test negative and have symptoms of COVID-19 should follow up with their health care provider, as negative results don’t preclude an individual from SARS-CoV-2 infection.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has issued an emergency-use authorization (EUA) for the first COVID-19 diagnostic test that can be completed at home without a prescription.
Authorization of the Ellume COVID-19 Home Test is “a major milestone in diagnostic testing for COVID-19,” FDA Commissioner Stephen M. Hahn, MD, said in a news release.
“By authorizing a test for over-the-counter use, the FDA allows it to be sold in places like drug stores, where a patient can buy it, swab their nose, run the test, and find out their results in as little as 20 minutes,” said Dr. Hahn.
The Ellume COVID-19 Home Test is a rapid antigen test that detects fragments of the SARS-CoV-2 virus from a nasal swab sample taken from anyone aged 2 years and older, including those not showing any symptoms.
In testing, the Ellume COVID-19 Home Test correctly identified 96% of positive samples and 100% of negative samples in individuals with symptoms.
In people without symptoms, the test correctly identified 91% of positive samples and 96% of negative samples, the FDA said.
The test includes a sterile nasal swab, a dropper, processing fluid, and a Bluetooth-connected analyzer for use with an app on the user’s smartphone. The sample is analyzed and results are automatically transmitted to the user’s smartphone.
“The Ellume COVID-19 home test’s core technology combines ultra-sensitive optics, electronics, and proprietary software to leverage best-in-class digital immunoassay technology with next-generation multi-quantum dot fluorescence technology,” the company said in a news release.
The mobile app requires individuals to input their ZIP code and date of birth, with optional fields including name and email address. The app automatically reports the results as appropriate to public health authorities to monitor disease prevalence.
Ellume expects to produce more than 3 million tests in January 2021. The company said the test will cost around $30.
FDA authorization of this first fully at-home nonprescription COVID-19 diagnostic test follows last month’s EUA for the first prescription COVID-19 test for home use, as reported this news organization.
Since the start of the pandemic, the FDA has authorized more than 225 diagnostic tests for COVID-19, including more than 25 tests that allow for home collection of samples, which are then sent to a lab for testing.
“As we continue to authorize additional tests for home use, we are helping expand Americans’ access to testing, reducing the burden on laboratories and test supplies, and giving Americans more testing options from the comfort and safety of their own homes,” Dr. Hahn said.
“This test, like other antigen tests, is less sensitive and less specific than typical molecular tests run in a lab,” said Jeffrey Shuren, MD, JD, director of FDA’s Center for Devices and Radiological Health, in the release. “However, the fact that it can be used completely at home and return results quickly means that it can play an important role in response to the pandemic.”
As with other antigen tests, a small percentage of positive and negative results from the Ellume test may be false. In patients without symptoms, positive results should be treated as presumptively positive until confirmed by another test as soon as possible, the FDA advised.
This is especially true if there are fewer infections in a particular community, as false-positive results can be more common when antigen tests are used in populations where there is a low prevalence of COVID-19, the agency said.
Because all tests can give false-negative and false-positive results, individuals with positive results should self-isolate and seek additional care from their health care provider.
Individuals who test negative and have symptoms of COVID-19 should follow up with their health care provider, as negative results don’t preclude an individual from SARS-CoV-2 infection.
A version of this article first appeared on Medscape.com.
Nobel laureates on their hunt for the cure
Researchers have worked at record-breaking speed to not only identify and characterize the novel coronavirus, but also to develop potential vaccines; it is a race that another trio of scientists, awarded the 2020 Nobel Prize in Medicine, know well after their own decades-long marathon to crack the code of hepatitis C.
The RNA virus vexed researchers like Harvey J. Alter, MD; Michael Houghton, PhD; and Charles M. Rice, PhD, for years. Unlike today’s parallel sequencing and polymerase chain reaction, screening at the time was tedious and painstaking. But they were all in for some big highs, some dead-ends, and a little inspiration by way of author Lewis Carroll.
“Our undertaking was a success,” Dr. Alter said in an interview, “because everyone got on board.” Investigators, the Food and Drug Administration, and blood banks all worked together. It was a national effort, he added.
The Laureates will share the $1 million prize that recognizes their achievement. This is the second time that scientists who have devoted their time to the pursuit of viral hepatitis have been honored.
Two main types of infectious hepatitis were identified in the 1940s. The first, hepatitis A, is transmitted by polluted water or food and generally has little long-term effect on the patient. The second, transmitted through blood and other bodily fluids, is a much more serious threat.
In the 1960s, Baruch Blumberg, MD, ascertained that blood-borne hepatitis was caused by an insidious virus – hepatitis B – which silently causes liver complications in otherwise healthy people years after infection. Dr. Blumberg’s discovery led to the development of diagnostic tests and an effective vaccine; he was awarded the Nobel Prize in Physiology or Medicine in 1976.
At that time, Dr. Alter was working at the National Institutes of Health in Bethesda, Md., studying the occurrence of hepatitis in patients who had received blood transfusions. Globally, blood-borne hepatitis was causing more than a million deaths each year.
When screening began in 1969 to prevent people with hepatitis A or hepatitis B from donating blood, many recipients were spared from developing liver inflammation after transfusion. However, some people were still getting sick and researchers began to suspect that something dubbed “non-A, non-B” was lurking in donated blood.
As scientists were tracking it down in the micro world, public health officials and others tried to block the presumed virus in the macro world. In the United States, this meant changing blood-donation practices. When it became clear that as many as one in five transfusion recipients developed hepatitis, probably as the result of a virus, the blood donation system switched from being a paid enterprise to a volunteer activity.
It was anticipated that this would eliminate one source of the virus – users of street drugs – and it did; rates of transmission after transfusion dropped by half. By the 1980s, researchers had figured out that donors carrying the mysterious pathogen often had elevated levels of antibodies to the hepatitis B virus or elevated levels of ALT. Blood banks then began testing prospective donors and cut the incidence of non-A, non-B hepatitis by another half.
When Dr. Alter and his team got to work studying chimpanzees, they were able to confirm that the non-A, non-B agent was transmittable by blood transfusion. But the next step proved insurmountable. “People knew what the virus would look like if we found it, but we couldn’t find it,” Dr. Alter said.
“Then Chiron came along and cloned it,” he recounts.
The tiny start-up company was housed in a few rented rooms in an abandoned plant in Emeryville, Calif. This is where Nobel Laureate Dr. Houghton and coworkers Qui-Lim Choo, PhD, and George Kuo, PhD, spent 7 years chasing the mystery pathogen. When every traditional method to pin it down failed, the team tried some nontraditional approaches.
They found success when they painstakingly cloned genomic fragments from the blood of an infected chimpanzee and then screened this library using serum isolated from affected patients. The hope was that antibodies in the serum samples would stick to the viral genetic material and create a signpost indicating its presence.
This “fishing expedition” was disappointing at first, said Dr. Choo, now vice president of research at Nansha Biologics Limited in Hong Kong. “We didn’t catch any fish.”
He likened the pursuit, which took place under growing pressure from upper management, to that in “The Imitation Game,” the film that depicted Alan Turing’s effort to decrypt German intelligence messages for the British government during World War II.
The effort wasn’t working out and the team was down. So to keep spirits up, Dr. Kuo shared a snippet of the Lewis Carroll poem “The Hunting of the Snark.” It just happened to encapsulate the frustrations of their pursuit while also encouraging perseverance: “For the Snark’s a peculiar creature, that won’t / Be caught in a commonplace way. / Do all that you know, and try all that you don’t: / Not a chance must be wasted today!”
Those words motivated the team to keep going, to try different approaches and, ultimately, to find the hepatitis C virus, said Dr. Kuo, now retired.
During the tedious process of screening millions of clones, Dr. Choo spotted a single likely area on one of the plates that his “gut feeling” told him would contain the viral material. And it did. The pathogen – RNA packed in a lipid coat – was a member of the Flaviviridae family.
In 1989, the team reported that they’d identified a new flavivirus associated with posttransfusion hepatitis, and published their findings in Science. Later that year, an antibody test for it was described in Science by the team, which included Dr. Alter.
The success was a “fantastic feeling,” mused Dr. Houghton, now a virologist at the University of Alberta, Edmonton. “I’ve often said that, from 1989 to 1991, I was high just on the discovery.” After that, “researchers and the pharmaceutical industry did a great job coming up with really effective antivirals.”
“Mike, with his team, took 7 years to get this tiny little piece of viral genome, which reacted with convalescent patient serum, and used that to build up the sequence. That’s where I come into it,” said Dr. Rice, professor of virology at Rockefeller University, New York, and the third scientist in the Nobel Prize–winning trio.
The next step was to confirm that this was causing the hepatitis in patients who received blood transfusions. Over the course of several years, Dr. Rice and colleagues at the Washington University, St. Louis, engineered a version of the virus that retained its replicating capacity and injected it into chimpanzees. The animals developed hepatitis, confirming that this flavivirus was indeed the cause. More than 8 years after the virus was identified, scientists had proof of its infectiousness.
“We finally knew the structure of the viral genome,” said Dr. Rice. “We showed that the sequence was sufficient to initiate infection and cause disease.”
Those findings, published in 1997 in Science, were the key final step in the search for a molecular target for therapies and, maybe someday, a vaccine.
For the first time in history, hepatitis C can now be cured, raising hopes that the virus will be eradicated from the world population. But obstacles remain as the World Health Organization works toward its goal of eliminating hepatitis C–related disease by 2030.
Rates have actually risen in the United States as the opioid epidemic has taken hold because the virus is common in people who use street drugs and are at increased risk for behaviors that lead to transmission.
The prevalence of chronic hepatitis C now hovers around 1%. In 2019, it affected an estimated 3.8 million Americans, and more than 39,000 people died of hepatitis C–related causes. Of all deaths from liver cancer in 2019, 39% were attributable to hepatitis C.
This “silent killer” can take years to develop, which dampens the sense of immediacy to help, said Jean-Michel Piedagnel, director of the Drugs for Neglected Diseases nonprofit initiative.
People infected with hepatitis C are often part of marginalized groups. There isn’t typically a common demographic factor to unite them in advocacy.
And even though treatment can cost as little as $200 in countries where generic drugs are available, money can still be an issue, Mr. Piedagnel pointed out.
The COVID-19 response shows how quickly health systems can evolve in a crisis and adapt. “If there is political will, means can be found, said Cary James, CEO at the World Hepatitis Alliance.
The incredible speed of vaccine development for SARS-CoV-2 has impressed the Nobel Laureates, who have yet to see a vaccine for hepatitis C.
Dr. Houghton said he hopes this momentum will perpetuate new emergency filings for hepatitis C vaccines.
If even a tiny fraction of the money that’s gone into COVID-19 were used, Dr. Rice pointed out, “we’d have a hep C vaccine by now.”
A version of this article first appeared on Medscape.com
Researchers have worked at record-breaking speed to not only identify and characterize the novel coronavirus, but also to develop potential vaccines; it is a race that another trio of scientists, awarded the 2020 Nobel Prize in Medicine, know well after their own decades-long marathon to crack the code of hepatitis C.
The RNA virus vexed researchers like Harvey J. Alter, MD; Michael Houghton, PhD; and Charles M. Rice, PhD, for years. Unlike today’s parallel sequencing and polymerase chain reaction, screening at the time was tedious and painstaking. But they were all in for some big highs, some dead-ends, and a little inspiration by way of author Lewis Carroll.
“Our undertaking was a success,” Dr. Alter said in an interview, “because everyone got on board.” Investigators, the Food and Drug Administration, and blood banks all worked together. It was a national effort, he added.
The Laureates will share the $1 million prize that recognizes their achievement. This is the second time that scientists who have devoted their time to the pursuit of viral hepatitis have been honored.
Two main types of infectious hepatitis were identified in the 1940s. The first, hepatitis A, is transmitted by polluted water or food and generally has little long-term effect on the patient. The second, transmitted through blood and other bodily fluids, is a much more serious threat.
In the 1960s, Baruch Blumberg, MD, ascertained that blood-borne hepatitis was caused by an insidious virus – hepatitis B – which silently causes liver complications in otherwise healthy people years after infection. Dr. Blumberg’s discovery led to the development of diagnostic tests and an effective vaccine; he was awarded the Nobel Prize in Physiology or Medicine in 1976.
At that time, Dr. Alter was working at the National Institutes of Health in Bethesda, Md., studying the occurrence of hepatitis in patients who had received blood transfusions. Globally, blood-borne hepatitis was causing more than a million deaths each year.
When screening began in 1969 to prevent people with hepatitis A or hepatitis B from donating blood, many recipients were spared from developing liver inflammation after transfusion. However, some people were still getting sick and researchers began to suspect that something dubbed “non-A, non-B” was lurking in donated blood.
As scientists were tracking it down in the micro world, public health officials and others tried to block the presumed virus in the macro world. In the United States, this meant changing blood-donation practices. When it became clear that as many as one in five transfusion recipients developed hepatitis, probably as the result of a virus, the blood donation system switched from being a paid enterprise to a volunteer activity.
It was anticipated that this would eliminate one source of the virus – users of street drugs – and it did; rates of transmission after transfusion dropped by half. By the 1980s, researchers had figured out that donors carrying the mysterious pathogen often had elevated levels of antibodies to the hepatitis B virus or elevated levels of ALT. Blood banks then began testing prospective donors and cut the incidence of non-A, non-B hepatitis by another half.
When Dr. Alter and his team got to work studying chimpanzees, they were able to confirm that the non-A, non-B agent was transmittable by blood transfusion. But the next step proved insurmountable. “People knew what the virus would look like if we found it, but we couldn’t find it,” Dr. Alter said.
“Then Chiron came along and cloned it,” he recounts.
The tiny start-up company was housed in a few rented rooms in an abandoned plant in Emeryville, Calif. This is where Nobel Laureate Dr. Houghton and coworkers Qui-Lim Choo, PhD, and George Kuo, PhD, spent 7 years chasing the mystery pathogen. When every traditional method to pin it down failed, the team tried some nontraditional approaches.
They found success when they painstakingly cloned genomic fragments from the blood of an infected chimpanzee and then screened this library using serum isolated from affected patients. The hope was that antibodies in the serum samples would stick to the viral genetic material and create a signpost indicating its presence.
This “fishing expedition” was disappointing at first, said Dr. Choo, now vice president of research at Nansha Biologics Limited in Hong Kong. “We didn’t catch any fish.”
He likened the pursuit, which took place under growing pressure from upper management, to that in “The Imitation Game,” the film that depicted Alan Turing’s effort to decrypt German intelligence messages for the British government during World War II.
The effort wasn’t working out and the team was down. So to keep spirits up, Dr. Kuo shared a snippet of the Lewis Carroll poem “The Hunting of the Snark.” It just happened to encapsulate the frustrations of their pursuit while also encouraging perseverance: “For the Snark’s a peculiar creature, that won’t / Be caught in a commonplace way. / Do all that you know, and try all that you don’t: / Not a chance must be wasted today!”
Those words motivated the team to keep going, to try different approaches and, ultimately, to find the hepatitis C virus, said Dr. Kuo, now retired.
During the tedious process of screening millions of clones, Dr. Choo spotted a single likely area on one of the plates that his “gut feeling” told him would contain the viral material. And it did. The pathogen – RNA packed in a lipid coat – was a member of the Flaviviridae family.
In 1989, the team reported that they’d identified a new flavivirus associated with posttransfusion hepatitis, and published their findings in Science. Later that year, an antibody test for it was described in Science by the team, which included Dr. Alter.
The success was a “fantastic feeling,” mused Dr. Houghton, now a virologist at the University of Alberta, Edmonton. “I’ve often said that, from 1989 to 1991, I was high just on the discovery.” After that, “researchers and the pharmaceutical industry did a great job coming up with really effective antivirals.”
“Mike, with his team, took 7 years to get this tiny little piece of viral genome, which reacted with convalescent patient serum, and used that to build up the sequence. That’s where I come into it,” said Dr. Rice, professor of virology at Rockefeller University, New York, and the third scientist in the Nobel Prize–winning trio.
The next step was to confirm that this was causing the hepatitis in patients who received blood transfusions. Over the course of several years, Dr. Rice and colleagues at the Washington University, St. Louis, engineered a version of the virus that retained its replicating capacity and injected it into chimpanzees. The animals developed hepatitis, confirming that this flavivirus was indeed the cause. More than 8 years after the virus was identified, scientists had proof of its infectiousness.
“We finally knew the structure of the viral genome,” said Dr. Rice. “We showed that the sequence was sufficient to initiate infection and cause disease.”
Those findings, published in 1997 in Science, were the key final step in the search for a molecular target for therapies and, maybe someday, a vaccine.
For the first time in history, hepatitis C can now be cured, raising hopes that the virus will be eradicated from the world population. But obstacles remain as the World Health Organization works toward its goal of eliminating hepatitis C–related disease by 2030.
Rates have actually risen in the United States as the opioid epidemic has taken hold because the virus is common in people who use street drugs and are at increased risk for behaviors that lead to transmission.
The prevalence of chronic hepatitis C now hovers around 1%. In 2019, it affected an estimated 3.8 million Americans, and more than 39,000 people died of hepatitis C–related causes. Of all deaths from liver cancer in 2019, 39% were attributable to hepatitis C.
This “silent killer” can take years to develop, which dampens the sense of immediacy to help, said Jean-Michel Piedagnel, director of the Drugs for Neglected Diseases nonprofit initiative.
People infected with hepatitis C are often part of marginalized groups. There isn’t typically a common demographic factor to unite them in advocacy.
And even though treatment can cost as little as $200 in countries where generic drugs are available, money can still be an issue, Mr. Piedagnel pointed out.
The COVID-19 response shows how quickly health systems can evolve in a crisis and adapt. “If there is political will, means can be found, said Cary James, CEO at the World Hepatitis Alliance.
The incredible speed of vaccine development for SARS-CoV-2 has impressed the Nobel Laureates, who have yet to see a vaccine for hepatitis C.
Dr. Houghton said he hopes this momentum will perpetuate new emergency filings for hepatitis C vaccines.
If even a tiny fraction of the money that’s gone into COVID-19 were used, Dr. Rice pointed out, “we’d have a hep C vaccine by now.”
A version of this article first appeared on Medscape.com
Researchers have worked at record-breaking speed to not only identify and characterize the novel coronavirus, but also to develop potential vaccines; it is a race that another trio of scientists, awarded the 2020 Nobel Prize in Medicine, know well after their own decades-long marathon to crack the code of hepatitis C.
The RNA virus vexed researchers like Harvey J. Alter, MD; Michael Houghton, PhD; and Charles M. Rice, PhD, for years. Unlike today’s parallel sequencing and polymerase chain reaction, screening at the time was tedious and painstaking. But they were all in for some big highs, some dead-ends, and a little inspiration by way of author Lewis Carroll.
“Our undertaking was a success,” Dr. Alter said in an interview, “because everyone got on board.” Investigators, the Food and Drug Administration, and blood banks all worked together. It was a national effort, he added.
The Laureates will share the $1 million prize that recognizes their achievement. This is the second time that scientists who have devoted their time to the pursuit of viral hepatitis have been honored.
Two main types of infectious hepatitis were identified in the 1940s. The first, hepatitis A, is transmitted by polluted water or food and generally has little long-term effect on the patient. The second, transmitted through blood and other bodily fluids, is a much more serious threat.
In the 1960s, Baruch Blumberg, MD, ascertained that blood-borne hepatitis was caused by an insidious virus – hepatitis B – which silently causes liver complications in otherwise healthy people years after infection. Dr. Blumberg’s discovery led to the development of diagnostic tests and an effective vaccine; he was awarded the Nobel Prize in Physiology or Medicine in 1976.
At that time, Dr. Alter was working at the National Institutes of Health in Bethesda, Md., studying the occurrence of hepatitis in patients who had received blood transfusions. Globally, blood-borne hepatitis was causing more than a million deaths each year.
When screening began in 1969 to prevent people with hepatitis A or hepatitis B from donating blood, many recipients were spared from developing liver inflammation after transfusion. However, some people were still getting sick and researchers began to suspect that something dubbed “non-A, non-B” was lurking in donated blood.
As scientists were tracking it down in the micro world, public health officials and others tried to block the presumed virus in the macro world. In the United States, this meant changing blood-donation practices. When it became clear that as many as one in five transfusion recipients developed hepatitis, probably as the result of a virus, the blood donation system switched from being a paid enterprise to a volunteer activity.
It was anticipated that this would eliminate one source of the virus – users of street drugs – and it did; rates of transmission after transfusion dropped by half. By the 1980s, researchers had figured out that donors carrying the mysterious pathogen often had elevated levels of antibodies to the hepatitis B virus or elevated levels of ALT. Blood banks then began testing prospective donors and cut the incidence of non-A, non-B hepatitis by another half.
When Dr. Alter and his team got to work studying chimpanzees, they were able to confirm that the non-A, non-B agent was transmittable by blood transfusion. But the next step proved insurmountable. “People knew what the virus would look like if we found it, but we couldn’t find it,” Dr. Alter said.
“Then Chiron came along and cloned it,” he recounts.
The tiny start-up company was housed in a few rented rooms in an abandoned plant in Emeryville, Calif. This is where Nobel Laureate Dr. Houghton and coworkers Qui-Lim Choo, PhD, and George Kuo, PhD, spent 7 years chasing the mystery pathogen. When every traditional method to pin it down failed, the team tried some nontraditional approaches.
They found success when they painstakingly cloned genomic fragments from the blood of an infected chimpanzee and then screened this library using serum isolated from affected patients. The hope was that antibodies in the serum samples would stick to the viral genetic material and create a signpost indicating its presence.
This “fishing expedition” was disappointing at first, said Dr. Choo, now vice president of research at Nansha Biologics Limited in Hong Kong. “We didn’t catch any fish.”
He likened the pursuit, which took place under growing pressure from upper management, to that in “The Imitation Game,” the film that depicted Alan Turing’s effort to decrypt German intelligence messages for the British government during World War II.
The effort wasn’t working out and the team was down. So to keep spirits up, Dr. Kuo shared a snippet of the Lewis Carroll poem “The Hunting of the Snark.” It just happened to encapsulate the frustrations of their pursuit while also encouraging perseverance: “For the Snark’s a peculiar creature, that won’t / Be caught in a commonplace way. / Do all that you know, and try all that you don’t: / Not a chance must be wasted today!”
Those words motivated the team to keep going, to try different approaches and, ultimately, to find the hepatitis C virus, said Dr. Kuo, now retired.
During the tedious process of screening millions of clones, Dr. Choo spotted a single likely area on one of the plates that his “gut feeling” told him would contain the viral material. And it did. The pathogen – RNA packed in a lipid coat – was a member of the Flaviviridae family.
In 1989, the team reported that they’d identified a new flavivirus associated with posttransfusion hepatitis, and published their findings in Science. Later that year, an antibody test for it was described in Science by the team, which included Dr. Alter.
The success was a “fantastic feeling,” mused Dr. Houghton, now a virologist at the University of Alberta, Edmonton. “I’ve often said that, from 1989 to 1991, I was high just on the discovery.” After that, “researchers and the pharmaceutical industry did a great job coming up with really effective antivirals.”
“Mike, with his team, took 7 years to get this tiny little piece of viral genome, which reacted with convalescent patient serum, and used that to build up the sequence. That’s where I come into it,” said Dr. Rice, professor of virology at Rockefeller University, New York, and the third scientist in the Nobel Prize–winning trio.
The next step was to confirm that this was causing the hepatitis in patients who received blood transfusions. Over the course of several years, Dr. Rice and colleagues at the Washington University, St. Louis, engineered a version of the virus that retained its replicating capacity and injected it into chimpanzees. The animals developed hepatitis, confirming that this flavivirus was indeed the cause. More than 8 years after the virus was identified, scientists had proof of its infectiousness.
“We finally knew the structure of the viral genome,” said Dr. Rice. “We showed that the sequence was sufficient to initiate infection and cause disease.”
Those findings, published in 1997 in Science, were the key final step in the search for a molecular target for therapies and, maybe someday, a vaccine.
For the first time in history, hepatitis C can now be cured, raising hopes that the virus will be eradicated from the world population. But obstacles remain as the World Health Organization works toward its goal of eliminating hepatitis C–related disease by 2030.
Rates have actually risen in the United States as the opioid epidemic has taken hold because the virus is common in people who use street drugs and are at increased risk for behaviors that lead to transmission.
The prevalence of chronic hepatitis C now hovers around 1%. In 2019, it affected an estimated 3.8 million Americans, and more than 39,000 people died of hepatitis C–related causes. Of all deaths from liver cancer in 2019, 39% were attributable to hepatitis C.
This “silent killer” can take years to develop, which dampens the sense of immediacy to help, said Jean-Michel Piedagnel, director of the Drugs for Neglected Diseases nonprofit initiative.
People infected with hepatitis C are often part of marginalized groups. There isn’t typically a common demographic factor to unite them in advocacy.
And even though treatment can cost as little as $200 in countries where generic drugs are available, money can still be an issue, Mr. Piedagnel pointed out.
The COVID-19 response shows how quickly health systems can evolve in a crisis and adapt. “If there is political will, means can be found, said Cary James, CEO at the World Hepatitis Alliance.
The incredible speed of vaccine development for SARS-CoV-2 has impressed the Nobel Laureates, who have yet to see a vaccine for hepatitis C.
Dr. Houghton said he hopes this momentum will perpetuate new emergency filings for hepatitis C vaccines.
If even a tiny fraction of the money that’s gone into COVID-19 were used, Dr. Rice pointed out, “we’d have a hep C vaccine by now.”
A version of this article first appeared on Medscape.com
Can patients record office visits?
Recently I posted a simple question on several social media pages and internet blogs populated exclusively by board-certified dermatologists and dermatologic surgeons: How would you respond to a patient asking (or demanding) to record all or part of their office visit? (Or, if you have encountered such a situation, how did you respond?)
The question was simple, but the answers were somewhat complicated.
First, I noticed a fundamental misunderstanding of applicable laws: Many practitioners apparently believe that taping or recording a private conversation is per se illegal. Perhaps they are conflating with wiretapping laws, which don’t apply in this situation. HIPAA laws don’t apply either, because the patient, by definition, is waiving the right to privacy by initiating the recording in the first place.
In fact, and only 11 states (California, Florida, Illinois, Maryland, Massachusetts, Michigan, Montana, New Hampshire, Oregon, Pennsylvania, and Washington) require the consent of both parties. All other states and territories actually allow it even if one party has not given consent. And some patients don’t ask permission at all; they just do it.
Another misconception was the perceived frequency of such situations. Recordings of conversations in the doctor’s office are by no means rare. A 2014 survey in the United Kingdom revealed that 15% of the public had secretly recorded a clinic visit, and a further 11% were aware of someone else doing the same, a topic discussed by a Dartmouth group in the Aug. 8, 2017, issue of JAMA.
In general, younger respondents to my (admittedly unscientific) informal survey tended to be less receptive to being recorded. “I do not allow recordings by patients because I can’t control how they may be used later and it’s just creepy,” wrote one. “It just seems a strange way to begin a trusting, transparent patient/doctor relationship … this is not Instagram.”
“I will sometimes let them take a photo of a specimen or a defect but I don’t allow recording,” wrote another. “Same reasons; creepy and out of my control. I worry about it happening surreptitiously, but what can you do?”
You can proactively prohibit all office recordings by posting a “no recording” sign in your waiting room in the name of confidentiality and privacy. Should a patient initiate a covert recording anyway, you have the option of terminating the visit with a warning that a repeat attempt will result in discharge. If you practice in one of the 39 one-party states, the recording would still be admissible, but your notice gives your attorney an argument – specifically, that the patient made the recording after being expressly directed not to do so – if anyone ever tries to use the recording against you, or without your permission.
Older, more experienced practitioners in the survey tended to be more sanguine about recordings. “I have allowed patients to record all or parts of the visit,” wrote one. “I even allowed a patient to film a [liposuction] procedure. My decision … was that the patient might think I had something to hide, which I [did not].”
Another reported, “I have no problem with patients or family recording office visits or procedures. When someone is recording a procedure, I have no problem ignoring them.”
“We don’t have anything to hide, after all,” affirmed another. “In the era of telemedicine, many things can be recorded, even without permission.”
Several other veteran practitioners summarized my own philosophy on the subject: Patients have a right to record visits in my state (New Jersey), whether I like it or not, so I simply assume I’m being recorded during every visit, and conduct myself accordingly.
Risk managers and malpractice carriers are divided on recordings. At one neurology clinic in Arizona, patients are routinely offered videos of their visits, and clinicians who participate in these recordings receive a 10% reduction in the cost of their medical defense and extra liability coverage. There are clear advantages to having a permanent record of a doctor’s professional opinion. Other carriers are not as supportive, discouraging their insureds from allowing recordings to be made.
In the end, like it or not, recordings are here to stay, and the omnipresence of modern communications devices such as smartphones, tablets, etc., will only increase their prevalence. My advice: Familiarize yourself with the laws in your state, and never say anything during an office visit that you would not stand behind, if it ever turns out to have been recorded.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Recently I posted a simple question on several social media pages and internet blogs populated exclusively by board-certified dermatologists and dermatologic surgeons: How would you respond to a patient asking (or demanding) to record all or part of their office visit? (Or, if you have encountered such a situation, how did you respond?)
The question was simple, but the answers were somewhat complicated.
First, I noticed a fundamental misunderstanding of applicable laws: Many practitioners apparently believe that taping or recording a private conversation is per se illegal. Perhaps they are conflating with wiretapping laws, which don’t apply in this situation. HIPAA laws don’t apply either, because the patient, by definition, is waiving the right to privacy by initiating the recording in the first place.
In fact, and only 11 states (California, Florida, Illinois, Maryland, Massachusetts, Michigan, Montana, New Hampshire, Oregon, Pennsylvania, and Washington) require the consent of both parties. All other states and territories actually allow it even if one party has not given consent. And some patients don’t ask permission at all; they just do it.
Another misconception was the perceived frequency of such situations. Recordings of conversations in the doctor’s office are by no means rare. A 2014 survey in the United Kingdom revealed that 15% of the public had secretly recorded a clinic visit, and a further 11% were aware of someone else doing the same, a topic discussed by a Dartmouth group in the Aug. 8, 2017, issue of JAMA.
In general, younger respondents to my (admittedly unscientific) informal survey tended to be less receptive to being recorded. “I do not allow recordings by patients because I can’t control how they may be used later and it’s just creepy,” wrote one. “It just seems a strange way to begin a trusting, transparent patient/doctor relationship … this is not Instagram.”
“I will sometimes let them take a photo of a specimen or a defect but I don’t allow recording,” wrote another. “Same reasons; creepy and out of my control. I worry about it happening surreptitiously, but what can you do?”
You can proactively prohibit all office recordings by posting a “no recording” sign in your waiting room in the name of confidentiality and privacy. Should a patient initiate a covert recording anyway, you have the option of terminating the visit with a warning that a repeat attempt will result in discharge. If you practice in one of the 39 one-party states, the recording would still be admissible, but your notice gives your attorney an argument – specifically, that the patient made the recording after being expressly directed not to do so – if anyone ever tries to use the recording against you, or without your permission.
Older, more experienced practitioners in the survey tended to be more sanguine about recordings. “I have allowed patients to record all or parts of the visit,” wrote one. “I even allowed a patient to film a [liposuction] procedure. My decision … was that the patient might think I had something to hide, which I [did not].”
Another reported, “I have no problem with patients or family recording office visits or procedures. When someone is recording a procedure, I have no problem ignoring them.”
“We don’t have anything to hide, after all,” affirmed another. “In the era of telemedicine, many things can be recorded, even without permission.”
Several other veteran practitioners summarized my own philosophy on the subject: Patients have a right to record visits in my state (New Jersey), whether I like it or not, so I simply assume I’m being recorded during every visit, and conduct myself accordingly.
Risk managers and malpractice carriers are divided on recordings. At one neurology clinic in Arizona, patients are routinely offered videos of their visits, and clinicians who participate in these recordings receive a 10% reduction in the cost of their medical defense and extra liability coverage. There are clear advantages to having a permanent record of a doctor’s professional opinion. Other carriers are not as supportive, discouraging their insureds from allowing recordings to be made.
In the end, like it or not, recordings are here to stay, and the omnipresence of modern communications devices such as smartphones, tablets, etc., will only increase their prevalence. My advice: Familiarize yourself with the laws in your state, and never say anything during an office visit that you would not stand behind, if it ever turns out to have been recorded.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Recently I posted a simple question on several social media pages and internet blogs populated exclusively by board-certified dermatologists and dermatologic surgeons: How would you respond to a patient asking (or demanding) to record all or part of their office visit? (Or, if you have encountered such a situation, how did you respond?)
The question was simple, but the answers were somewhat complicated.
First, I noticed a fundamental misunderstanding of applicable laws: Many practitioners apparently believe that taping or recording a private conversation is per se illegal. Perhaps they are conflating with wiretapping laws, which don’t apply in this situation. HIPAA laws don’t apply either, because the patient, by definition, is waiving the right to privacy by initiating the recording in the first place.
In fact, and only 11 states (California, Florida, Illinois, Maryland, Massachusetts, Michigan, Montana, New Hampshire, Oregon, Pennsylvania, and Washington) require the consent of both parties. All other states and territories actually allow it even if one party has not given consent. And some patients don’t ask permission at all; they just do it.
Another misconception was the perceived frequency of such situations. Recordings of conversations in the doctor’s office are by no means rare. A 2014 survey in the United Kingdom revealed that 15% of the public had secretly recorded a clinic visit, and a further 11% were aware of someone else doing the same, a topic discussed by a Dartmouth group in the Aug. 8, 2017, issue of JAMA.
In general, younger respondents to my (admittedly unscientific) informal survey tended to be less receptive to being recorded. “I do not allow recordings by patients because I can’t control how they may be used later and it’s just creepy,” wrote one. “It just seems a strange way to begin a trusting, transparent patient/doctor relationship … this is not Instagram.”
“I will sometimes let them take a photo of a specimen or a defect but I don’t allow recording,” wrote another. “Same reasons; creepy and out of my control. I worry about it happening surreptitiously, but what can you do?”
You can proactively prohibit all office recordings by posting a “no recording” sign in your waiting room in the name of confidentiality and privacy. Should a patient initiate a covert recording anyway, you have the option of terminating the visit with a warning that a repeat attempt will result in discharge. If you practice in one of the 39 one-party states, the recording would still be admissible, but your notice gives your attorney an argument – specifically, that the patient made the recording after being expressly directed not to do so – if anyone ever tries to use the recording against you, or without your permission.
Older, more experienced practitioners in the survey tended to be more sanguine about recordings. “I have allowed patients to record all or parts of the visit,” wrote one. “I even allowed a patient to film a [liposuction] procedure. My decision … was that the patient might think I had something to hide, which I [did not].”
Another reported, “I have no problem with patients or family recording office visits or procedures. When someone is recording a procedure, I have no problem ignoring them.”
“We don’t have anything to hide, after all,” affirmed another. “In the era of telemedicine, many things can be recorded, even without permission.”
Several other veteran practitioners summarized my own philosophy on the subject: Patients have a right to record visits in my state (New Jersey), whether I like it or not, so I simply assume I’m being recorded during every visit, and conduct myself accordingly.
Risk managers and malpractice carriers are divided on recordings. At one neurology clinic in Arizona, patients are routinely offered videos of their visits, and clinicians who participate in these recordings receive a 10% reduction in the cost of their medical defense and extra liability coverage. There are clear advantages to having a permanent record of a doctor’s professional opinion. Other carriers are not as supportive, discouraging their insureds from allowing recordings to be made.
In the end, like it or not, recordings are here to stay, and the omnipresence of modern communications devices such as smartphones, tablets, etc., will only increase their prevalence. My advice: Familiarize yourself with the laws in your state, and never say anything during an office visit that you would not stand behind, if it ever turns out to have been recorded.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Endocrine societies push back on discriminatory transgender health policies
Science should be the cornerstone for health policy, and decisions on medical care of transgender and gender-diverse (TGD) individuals should be between a patient and their doctor.
That’s according to a joint policy statement from the Endocrine Society and Pediatric Endocrine Society published in the Journal of Clinical Endocrinology & Metabolism expressing concern about recent proposed legislation that would limit access to medical care for TGD individuals.
“The main emphasis is that we are simply medical people trying to be conservative and science driven in the care of our patients,” Joshua D. Safer, MD, coauthor and executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System, and professor of medicine at Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Why the health care for a particular group of people should be considered political is a mystery to me.”
TGD individuals have seen a recent uptick in efforts to limit or restrict their access to medical care at the federal and state levels. In June 2020, the Department of Health & Human Services finalized a revision to Section 1557 of the Affordable Care Act, rolling back a 2016 rule that determined the phrase “on the basis of sex” included nondiscrimination based on a person’s sex and gender identity. The Endocrine Society opposed this rule revision, arguing that it would allow “providers to deny care to TGD persons as well as discourage patients from seeking routine and gender-affirming care or reporting discrimination.”
Over a dozen U.S. states have introduced proposed legislation concerning medical care of TGD individuals that contain erroneous and misleading information. Proposed laws in Alabama, Missouri, and Texas, for example, would prohibit any use of medical treatments for minors for the purpose of gender-affirming medical care, including “gonadotropin-releasing hormone agonist therapy for pubertal suppression and gender-affirming hormonal therapy,” the authors of the joint statement wrote. In some cases, medical professionals who provide medical care for TGD patients could face criminal charges.
Outside the United States, three High Court judges in the United Kingdom recently ruled that minors aged under 16 years could not legally consent to pubertal suppression. “The recent U.K. court decision could be very disruptive because it would raise a barrier to transgender children receiving puberty blockers at exactly the ages that puberty blockers would be typically used,” Dr. Safer said.
Misleading characterizations of gender-affirming medical care for TGD individuals have also been spread to the general public. A recent Republican primary ballot proposition in Texas asked whether the state should ban “chemical castration, puberty blockers, cross-sex hormones, and genital mutilation surgery on all minor children for transition purposes,” falsely asserting that “Texas children as young as 3 are being transitioned from their biological sex to the opposite sex,” referencing a high-profile custody battle of a transgender child in Texas.
There are several tiers of misinformation that exist within these statements, Dr. Safer noted. “Some statements have suggested that gender-affirming treatment for young children can include hormone therapy or even surgery. Of course, there are no medical treatments for transgender and gender-diverse children prior to puberty.”
For adolescents aged under 18 years, Endocrine Society guidelines released in 2017 state that pubertal suppression is fully reversible and “offered to adolescents who meet diagnostic and treatment criteria, and are requesting care, for gender dysphoria/gender incongruence after they exhibit physical changes of puberty,” Dr. Safer and coauthors wrote in the joint policy statement. Other, more permanent – but still partially reversible – treatments such as hormone therapy are available as options for adolescents with confirmed and persistent gender dysphoria/gender incongruence, after meeting with a team of medical and mental health professionals and giving informed consent, according to the guidelines.
Dr. Safer expressed surprise at the opposition to puberty blockers in proposed state legislation. “Puberty blockers are the conservative option so that we can avoid permanent changes while thoughtful decisions are being made by our adolescent patients with their families and health care providers,” he said.
The perception that puberty blockers will lead to hormone therapy is another misunderstanding and source of misinformation, Dr. Safer explained.
“The fear is that these data suggest that puberty blockers are a ‘gateway drug’ of some sort. But that is false. The reason that most adolescents who take puberty blockers go on to hormone therapy is because most of the adolescents who are identified in our conservative systems are actually transgender and interested in more gender-affirming care as they age,” he said.
Effects of discrimination on TGD persons
Many of these proposed state bills have not advanced through state legislatures, but a few – such as the proposed laws in Alabama, Missouri, and Texas – are still currently under consideration.
“In the United States, most recent efforts to single out transgender and gender-diverse people for discrimination in health care have failed. However, the demonization of trans people and attempts to disrupt care have been the source of much stress among our patients,” Dr. Safer said.
Restricting access to health care has “multiple implications” for TGD patients. “In the era when we did not provide care to transgender youth, we had a situation where approximately 40% of transgender people had considered suicide in their lives,” Dr. Safer said. In contrast, having access to these treatments has been shown to improve mental health outcomes in these patients, according to an Endocrine Society position statement.
The purpose of earlier interventions such as puberty blockers is to allow an adolescent to “explore options and live in the experienced gender before making a decision to proceed with gender-affirming hormone therapy,” the authors of the Endocrine Society and Pediatric Endocrine Society joint statement said.
Blocking access to puberty blockers, on the other hand, forces transgender youth to experience a puberty that doesn’t match their gender identity, Dr. Safer noted. “The puberty will include permanent changes which will then have to be reversed with surgery. Why would we intentionally allow that to happen?”
Dr. Safer reported that his spouse is an employee of Parexel. Dr. Tangpricha is the current president of the World Association for Transgender Health and a board member of the American Association of Clinical Endocrinology. The other authors reported no relevant conflicts of interests.
SOURCE: Safer JD et al. J Clin Endocrinol Metab. 2020. doi: 10.1210/clinem/dgaa816.
Science should be the cornerstone for health policy, and decisions on medical care of transgender and gender-diverse (TGD) individuals should be between a patient and their doctor.
That’s according to a joint policy statement from the Endocrine Society and Pediatric Endocrine Society published in the Journal of Clinical Endocrinology & Metabolism expressing concern about recent proposed legislation that would limit access to medical care for TGD individuals.
“The main emphasis is that we are simply medical people trying to be conservative and science driven in the care of our patients,” Joshua D. Safer, MD, coauthor and executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System, and professor of medicine at Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Why the health care for a particular group of people should be considered political is a mystery to me.”
TGD individuals have seen a recent uptick in efforts to limit or restrict their access to medical care at the federal and state levels. In June 2020, the Department of Health & Human Services finalized a revision to Section 1557 of the Affordable Care Act, rolling back a 2016 rule that determined the phrase “on the basis of sex” included nondiscrimination based on a person’s sex and gender identity. The Endocrine Society opposed this rule revision, arguing that it would allow “providers to deny care to TGD persons as well as discourage patients from seeking routine and gender-affirming care or reporting discrimination.”
Over a dozen U.S. states have introduced proposed legislation concerning medical care of TGD individuals that contain erroneous and misleading information. Proposed laws in Alabama, Missouri, and Texas, for example, would prohibit any use of medical treatments for minors for the purpose of gender-affirming medical care, including “gonadotropin-releasing hormone agonist therapy for pubertal suppression and gender-affirming hormonal therapy,” the authors of the joint statement wrote. In some cases, medical professionals who provide medical care for TGD patients could face criminal charges.
Outside the United States, three High Court judges in the United Kingdom recently ruled that minors aged under 16 years could not legally consent to pubertal suppression. “The recent U.K. court decision could be very disruptive because it would raise a barrier to transgender children receiving puberty blockers at exactly the ages that puberty blockers would be typically used,” Dr. Safer said.
Misleading characterizations of gender-affirming medical care for TGD individuals have also been spread to the general public. A recent Republican primary ballot proposition in Texas asked whether the state should ban “chemical castration, puberty blockers, cross-sex hormones, and genital mutilation surgery on all minor children for transition purposes,” falsely asserting that “Texas children as young as 3 are being transitioned from their biological sex to the opposite sex,” referencing a high-profile custody battle of a transgender child in Texas.
There are several tiers of misinformation that exist within these statements, Dr. Safer noted. “Some statements have suggested that gender-affirming treatment for young children can include hormone therapy or even surgery. Of course, there are no medical treatments for transgender and gender-diverse children prior to puberty.”
For adolescents aged under 18 years, Endocrine Society guidelines released in 2017 state that pubertal suppression is fully reversible and “offered to adolescents who meet diagnostic and treatment criteria, and are requesting care, for gender dysphoria/gender incongruence after they exhibit physical changes of puberty,” Dr. Safer and coauthors wrote in the joint policy statement. Other, more permanent – but still partially reversible – treatments such as hormone therapy are available as options for adolescents with confirmed and persistent gender dysphoria/gender incongruence, after meeting with a team of medical and mental health professionals and giving informed consent, according to the guidelines.
Dr. Safer expressed surprise at the opposition to puberty blockers in proposed state legislation. “Puberty blockers are the conservative option so that we can avoid permanent changes while thoughtful decisions are being made by our adolescent patients with their families and health care providers,” he said.
The perception that puberty blockers will lead to hormone therapy is another misunderstanding and source of misinformation, Dr. Safer explained.
“The fear is that these data suggest that puberty blockers are a ‘gateway drug’ of some sort. But that is false. The reason that most adolescents who take puberty blockers go on to hormone therapy is because most of the adolescents who are identified in our conservative systems are actually transgender and interested in more gender-affirming care as they age,” he said.
Effects of discrimination on TGD persons
Many of these proposed state bills have not advanced through state legislatures, but a few – such as the proposed laws in Alabama, Missouri, and Texas – are still currently under consideration.
“In the United States, most recent efforts to single out transgender and gender-diverse people for discrimination in health care have failed. However, the demonization of trans people and attempts to disrupt care have been the source of much stress among our patients,” Dr. Safer said.
Restricting access to health care has “multiple implications” for TGD patients. “In the era when we did not provide care to transgender youth, we had a situation where approximately 40% of transgender people had considered suicide in their lives,” Dr. Safer said. In contrast, having access to these treatments has been shown to improve mental health outcomes in these patients, according to an Endocrine Society position statement.
The purpose of earlier interventions such as puberty blockers is to allow an adolescent to “explore options and live in the experienced gender before making a decision to proceed with gender-affirming hormone therapy,” the authors of the Endocrine Society and Pediatric Endocrine Society joint statement said.
Blocking access to puberty blockers, on the other hand, forces transgender youth to experience a puberty that doesn’t match their gender identity, Dr. Safer noted. “The puberty will include permanent changes which will then have to be reversed with surgery. Why would we intentionally allow that to happen?”
Dr. Safer reported that his spouse is an employee of Parexel. Dr. Tangpricha is the current president of the World Association for Transgender Health and a board member of the American Association of Clinical Endocrinology. The other authors reported no relevant conflicts of interests.
SOURCE: Safer JD et al. J Clin Endocrinol Metab. 2020. doi: 10.1210/clinem/dgaa816.
Science should be the cornerstone for health policy, and decisions on medical care of transgender and gender-diverse (TGD) individuals should be between a patient and their doctor.
That’s according to a joint policy statement from the Endocrine Society and Pediatric Endocrine Society published in the Journal of Clinical Endocrinology & Metabolism expressing concern about recent proposed legislation that would limit access to medical care for TGD individuals.
“The main emphasis is that we are simply medical people trying to be conservative and science driven in the care of our patients,” Joshua D. Safer, MD, coauthor and executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System, and professor of medicine at Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Why the health care for a particular group of people should be considered political is a mystery to me.”
TGD individuals have seen a recent uptick in efforts to limit or restrict their access to medical care at the federal and state levels. In June 2020, the Department of Health & Human Services finalized a revision to Section 1557 of the Affordable Care Act, rolling back a 2016 rule that determined the phrase “on the basis of sex” included nondiscrimination based on a person’s sex and gender identity. The Endocrine Society opposed this rule revision, arguing that it would allow “providers to deny care to TGD persons as well as discourage patients from seeking routine and gender-affirming care or reporting discrimination.”
Over a dozen U.S. states have introduced proposed legislation concerning medical care of TGD individuals that contain erroneous and misleading information. Proposed laws in Alabama, Missouri, and Texas, for example, would prohibit any use of medical treatments for minors for the purpose of gender-affirming medical care, including “gonadotropin-releasing hormone agonist therapy for pubertal suppression and gender-affirming hormonal therapy,” the authors of the joint statement wrote. In some cases, medical professionals who provide medical care for TGD patients could face criminal charges.
Outside the United States, three High Court judges in the United Kingdom recently ruled that minors aged under 16 years could not legally consent to pubertal suppression. “The recent U.K. court decision could be very disruptive because it would raise a barrier to transgender children receiving puberty blockers at exactly the ages that puberty blockers would be typically used,” Dr. Safer said.
Misleading characterizations of gender-affirming medical care for TGD individuals have also been spread to the general public. A recent Republican primary ballot proposition in Texas asked whether the state should ban “chemical castration, puberty blockers, cross-sex hormones, and genital mutilation surgery on all minor children for transition purposes,” falsely asserting that “Texas children as young as 3 are being transitioned from their biological sex to the opposite sex,” referencing a high-profile custody battle of a transgender child in Texas.
There are several tiers of misinformation that exist within these statements, Dr. Safer noted. “Some statements have suggested that gender-affirming treatment for young children can include hormone therapy or even surgery. Of course, there are no medical treatments for transgender and gender-diverse children prior to puberty.”
For adolescents aged under 18 years, Endocrine Society guidelines released in 2017 state that pubertal suppression is fully reversible and “offered to adolescents who meet diagnostic and treatment criteria, and are requesting care, for gender dysphoria/gender incongruence after they exhibit physical changes of puberty,” Dr. Safer and coauthors wrote in the joint policy statement. Other, more permanent – but still partially reversible – treatments such as hormone therapy are available as options for adolescents with confirmed and persistent gender dysphoria/gender incongruence, after meeting with a team of medical and mental health professionals and giving informed consent, according to the guidelines.
Dr. Safer expressed surprise at the opposition to puberty blockers in proposed state legislation. “Puberty blockers are the conservative option so that we can avoid permanent changes while thoughtful decisions are being made by our adolescent patients with their families and health care providers,” he said.
The perception that puberty blockers will lead to hormone therapy is another misunderstanding and source of misinformation, Dr. Safer explained.
“The fear is that these data suggest that puberty blockers are a ‘gateway drug’ of some sort. But that is false. The reason that most adolescents who take puberty blockers go on to hormone therapy is because most of the adolescents who are identified in our conservative systems are actually transgender and interested in more gender-affirming care as they age,” he said.
Effects of discrimination on TGD persons
Many of these proposed state bills have not advanced through state legislatures, but a few – such as the proposed laws in Alabama, Missouri, and Texas – are still currently under consideration.
“In the United States, most recent efforts to single out transgender and gender-diverse people for discrimination in health care have failed. However, the demonization of trans people and attempts to disrupt care have been the source of much stress among our patients,” Dr. Safer said.
Restricting access to health care has “multiple implications” for TGD patients. “In the era when we did not provide care to transgender youth, we had a situation where approximately 40% of transgender people had considered suicide in their lives,” Dr. Safer said. In contrast, having access to these treatments has been shown to improve mental health outcomes in these patients, according to an Endocrine Society position statement.
The purpose of earlier interventions such as puberty blockers is to allow an adolescent to “explore options and live in the experienced gender before making a decision to proceed with gender-affirming hormone therapy,” the authors of the Endocrine Society and Pediatric Endocrine Society joint statement said.
Blocking access to puberty blockers, on the other hand, forces transgender youth to experience a puberty that doesn’t match their gender identity, Dr. Safer noted. “The puberty will include permanent changes which will then have to be reversed with surgery. Why would we intentionally allow that to happen?”
Dr. Safer reported that his spouse is an employee of Parexel. Dr. Tangpricha is the current president of the World Association for Transgender Health and a board member of the American Association of Clinical Endocrinology. The other authors reported no relevant conflicts of interests.
SOURCE: Safer JD et al. J Clin Endocrinol Metab. 2020. doi: 10.1210/clinem/dgaa816.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
Beware a pair of dermatologic emergencies in children
in a presentation at MedscapeLive’s virtual Women’s & Pediatric Dermatology Seminar.
Eczema herpeticum is a condition in which a herpes simplex virus (HSV-1 or HSV-2) is superimposed over preexisting eczema. “The infection may be primary and sustained from a close contact or result in some of our older patients from reactivation and spread through autoinoculation,” said Dr. Hightower, of Rady Children’s Hospital and the University of California, both in San Diego.
Signs, he said, include acute worsening of atopic dermatitis with new-onset vesicles, pustules, and “punched-out” hemorrhagic crusted erosions. “Presentation ranges from mild to transient to life threatening.”
Potential complications include meningitis, encephalitis, hepatitis, and chronic conjunctivitis. “That’s why immediate ophthalmological evaluation is needed when there’s involvement on the face near the eye,” he said.
As for management and care, “where I have concern for HSV patients, I get HSV [polymerase chain reaction] as well as a bacterial culture,” he said. But even before the results are available, empiric treatment with acyclovir can be appropriate. “It’s got to be systemic for these kids with severe involvement,” he said, and they should also be started on medication for staphylococci and streptococci.
During his presentation, Dr. Hightower also highlighted staphylococcal scalded skin syndrome. Patients with the disease commonly have concurrent skin pain (which can appear to be fussiness), fever, irritability, malaise, and poor feeding. Examination may reveal widespread erythema with accentuation at folds/peeling at hands and large sheets of superficial peeling scale with diffuse erythema.
Widespread skin involvement “results not from the presence of staph throughout the skin, but the exotoxin that it produces that becomes systemic,” he said. “Clinical diagnosis is supported by presence of S. aureus on bacterial culture, but the presence of staph is not necessary to make the diagnosis. When in doubt, histopathology is helpful. But again, it’s not necessary to make the diagnosis.”
Cases can be managed with a first- or second-generation cephalosporin, he said. Alternative therapies include antistaphylococcus penicillinase-resistant penicillins (oxacillin or nafcillin) or vancomycin.
While Dr. Hightower doesn’t use clindamycin in these patients, he said it’s an option that some dermatologists consider because of its antistaphylococcus activity. “Historically, people thought it may decrease exotoxin production. The big concern if you are going to use clindamycin is that there are high rates of community resistance,” he said. “So you want to be careful that you know your resistance patterns wherever you are. Follow up on culture to make sure that you have adequate coverage for the bug that the kiddo in front of you has.”
Dr. Hightower reported no relevant disclosures. MedscapeLive and this news organization are owned by the same parent company.
in a presentation at MedscapeLive’s virtual Women’s & Pediatric Dermatology Seminar.
Eczema herpeticum is a condition in which a herpes simplex virus (HSV-1 or HSV-2) is superimposed over preexisting eczema. “The infection may be primary and sustained from a close contact or result in some of our older patients from reactivation and spread through autoinoculation,” said Dr. Hightower, of Rady Children’s Hospital and the University of California, both in San Diego.
Signs, he said, include acute worsening of atopic dermatitis with new-onset vesicles, pustules, and “punched-out” hemorrhagic crusted erosions. “Presentation ranges from mild to transient to life threatening.”
Potential complications include meningitis, encephalitis, hepatitis, and chronic conjunctivitis. “That’s why immediate ophthalmological evaluation is needed when there’s involvement on the face near the eye,” he said.
As for management and care, “where I have concern for HSV patients, I get HSV [polymerase chain reaction] as well as a bacterial culture,” he said. But even before the results are available, empiric treatment with acyclovir can be appropriate. “It’s got to be systemic for these kids with severe involvement,” he said, and they should also be started on medication for staphylococci and streptococci.
During his presentation, Dr. Hightower also highlighted staphylococcal scalded skin syndrome. Patients with the disease commonly have concurrent skin pain (which can appear to be fussiness), fever, irritability, malaise, and poor feeding. Examination may reveal widespread erythema with accentuation at folds/peeling at hands and large sheets of superficial peeling scale with diffuse erythema.
Widespread skin involvement “results not from the presence of staph throughout the skin, but the exotoxin that it produces that becomes systemic,” he said. “Clinical diagnosis is supported by presence of S. aureus on bacterial culture, but the presence of staph is not necessary to make the diagnosis. When in doubt, histopathology is helpful. But again, it’s not necessary to make the diagnosis.”
Cases can be managed with a first- or second-generation cephalosporin, he said. Alternative therapies include antistaphylococcus penicillinase-resistant penicillins (oxacillin or nafcillin) or vancomycin.
While Dr. Hightower doesn’t use clindamycin in these patients, he said it’s an option that some dermatologists consider because of its antistaphylococcus activity. “Historically, people thought it may decrease exotoxin production. The big concern if you are going to use clindamycin is that there are high rates of community resistance,” he said. “So you want to be careful that you know your resistance patterns wherever you are. Follow up on culture to make sure that you have adequate coverage for the bug that the kiddo in front of you has.”
Dr. Hightower reported no relevant disclosures. MedscapeLive and this news organization are owned by the same parent company.
in a presentation at MedscapeLive’s virtual Women’s & Pediatric Dermatology Seminar.
Eczema herpeticum is a condition in which a herpes simplex virus (HSV-1 or HSV-2) is superimposed over preexisting eczema. “The infection may be primary and sustained from a close contact or result in some of our older patients from reactivation and spread through autoinoculation,” said Dr. Hightower, of Rady Children’s Hospital and the University of California, both in San Diego.
Signs, he said, include acute worsening of atopic dermatitis with new-onset vesicles, pustules, and “punched-out” hemorrhagic crusted erosions. “Presentation ranges from mild to transient to life threatening.”
Potential complications include meningitis, encephalitis, hepatitis, and chronic conjunctivitis. “That’s why immediate ophthalmological evaluation is needed when there’s involvement on the face near the eye,” he said.
As for management and care, “where I have concern for HSV patients, I get HSV [polymerase chain reaction] as well as a bacterial culture,” he said. But even before the results are available, empiric treatment with acyclovir can be appropriate. “It’s got to be systemic for these kids with severe involvement,” he said, and they should also be started on medication for staphylococci and streptococci.
During his presentation, Dr. Hightower also highlighted staphylococcal scalded skin syndrome. Patients with the disease commonly have concurrent skin pain (which can appear to be fussiness), fever, irritability, malaise, and poor feeding. Examination may reveal widespread erythema with accentuation at folds/peeling at hands and large sheets of superficial peeling scale with diffuse erythema.
Widespread skin involvement “results not from the presence of staph throughout the skin, but the exotoxin that it produces that becomes systemic,” he said. “Clinical diagnosis is supported by presence of S. aureus on bacterial culture, but the presence of staph is not necessary to make the diagnosis. When in doubt, histopathology is helpful. But again, it’s not necessary to make the diagnosis.”
Cases can be managed with a first- or second-generation cephalosporin, he said. Alternative therapies include antistaphylococcus penicillinase-resistant penicillins (oxacillin or nafcillin) or vancomycin.
While Dr. Hightower doesn’t use clindamycin in these patients, he said it’s an option that some dermatologists consider because of its antistaphylococcus activity. “Historically, people thought it may decrease exotoxin production. The big concern if you are going to use clindamycin is that there are high rates of community resistance,” he said. “So you want to be careful that you know your resistance patterns wherever you are. Follow up on culture to make sure that you have adequate coverage for the bug that the kiddo in front of you has.”
Dr. Hightower reported no relevant disclosures. MedscapeLive and this news organization are owned by the same parent company.
FROM MEDSCAPELIVE WOMEN’S & PEDIATRIC DERMATOLOGY SEMINAR
Six big changes coming for office-visit coding
Betsy Nicoletti, MS, a nationally recognized coding expert, will take your coding questions via email and provide guidance on how to code properly to maximize reimbursement. Have a question about coding? Send it to [email protected].
thanks to the American Medical Association.
The first major changes to the definitions for E/M services will be in effect as of Jan. 1, 2021, with all payers expected to adopt these new guidelines. In particular, the AMA has revised the definitions for E/M codes 99202-99215 in the Current Procedural Terminology (CPT) 2021 codebook. The existing guidelines were developed in 1995 and 1997 and remain in effect for all other E/M services determined by history, exam, and medical decision-making (MDM).
What do the new changes mean to you? In 2021, for new and established office and other outpatient services reported with codes 99202-99215, a clinician may select the code on the basis of time or MDM.
There are three elements in MDM, and two of three are required. These elements are the number and complexity of problems addressed, amount and/or complexity of data to be reviewed and analyzed, and risk of complications and/or morbidity or mortality of patient management.
Make sure you familiarize yourself with these six big changes. It may take a bit of time to integrate these new processes into your daily routine, but wrapping your head around them as soon as possible can help boost your bottom line:
1. History and exam don’t count toward level of service
Physicians, advanced practice registered nurses, and physician assistants won’t use history or exam to select what level of code to bill for office visits 99202-99215, as they did in the past. They need only document a medically appropriate history and exam. The history may be obtained by staff members and reviewed by the billing practitioner.
While specific history and exam requirements disappear for office visit codes, they remain for all other types of visits, selected on the basis of history, exam, and MDM, such as hospital services, nursing facility services, and home and domiciliary care. So, say goodbye to “all other systems reviewed and negative” in office notes, but keep it handy for those other E/M codes.
2. All time spent caring for the patient on a particular day counts
This includes all time spent on the day of service, including preparing to see the patient, seeing the patient, phone calls or other work done after the visit (if not billed with a care management or other CPT code), and documenting in the medical record. The AMA developed new guidelines for using time for office and other outpatient services. For codes 99202-99215, count all of the face-to-face and non–face-to-face time spent by the billing clinician on the day of the visit. Counseling does not need to be more than 50% of the total time.
Do not include any staff time or time spent on any days before or after the visit. This allows clinicians to capture the work when a significant amount of it takes place before or after the visit with the patient, and to bill for it on the day of the visit.
According to the 2021 CPT codebook, physician or other qualified health care professional time includes the following activities:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
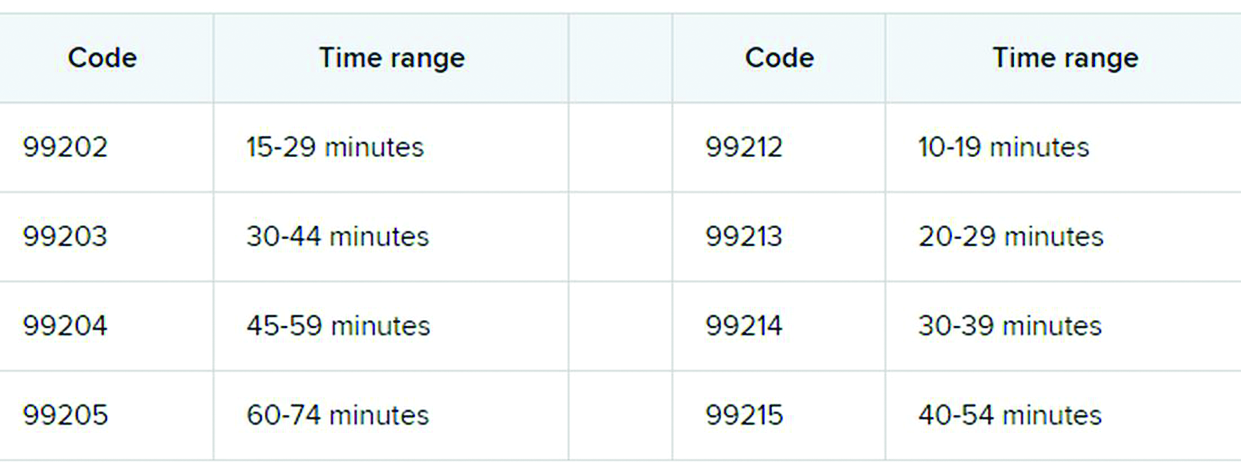
3. Soon to be gone: ‘new to the examiner’ and ‘workup planned’
The current guidelines don’t differentiate between a new problem to the clinician or an established problem to the clinician. So it doesn’t matter whether you’re hearing about a particular problem for the first time or the fifth time. The new office and outpatient services guidelines define problems only as they relate to the patient. For example, when selecting a level of service, a chronic problem with a mild exacerbation is the same level whether it’s the primary care physician seeing the patient for the 10th time to help manage her diabetes or the endocrinologist seeing the patient for the first time.
In the current guidelines (1995 and 1997), additional weight is given in selecting the level of MDM for a problem that’s new to the examiner with a workup planned, yet when the diagnostic test couldn’t be completed at the visit. This concept is gone from element of number and complexity of new problems. Ordering diagnostic tests is part of the second element, the amount and/or complexity of data to be reviewed.
4. Different guidelines if you need a history from a parent or other source
The new guidelines recognize the additional work required by the clinician when the patient is unable to give a history or when the practitioner doesn’t find the history to be reliable.
For example, in the case of a baby or child who is unable to give a history, the parent counts as an “independent historian,” according to the new guidelines. Likewise, for a patient with dementia, the caregiver counts as a historian. Note, however, that the criteria is not met simply because the patient is accompanied by another person. The additional weight in selecting the level of service is based on the patient being unable to give a reliable history.
Bottom line: In cases where patients are unable to communicate clearly, physicians or other providers should document the necessity of getting a complete history and who provided it.
5. A new spin on social determinants of health (SDoH)
In the risk of morbidity and/or mortality element, conditions described as “social determinants of health” are considered moderate complexity. SDoH are social and environmental factors that affect a patient’s health and medical outcomes. These include homelessness, inability to afford medications, food insecurity, and occupational exposure to risk factors. These circumstances are reported with codes in categories Z55-Z65.
In the past, physicians often documented this information in their office notes but rarely added a diagnosis code that described the patient’s situation. The ICD-10-CM code set includes codes that describe these factors. Using them allows the practice to track patients who have increased needs, and it communicates to payers the complexity of caring for these patients.
6. Risks related to surgery are defined
The current guidelines assign different levels of risk to minor and major surgery. They also include differentiation for “minor surgery with no identified risk factors,” “minor surgery with identified risk factors,” “elective major surgery with no identified risk factors,” and “elective major surgery with identified risk factors.” The old guidelines didn’t state whether the risk factors pertained to the patient – such as smoking, heart disease, or high body mass index – or to the procedure itself.
The new guidelines specifically say that it’s both. In the risk column, “decision regarding minor surgery with identified patient or procedure risk factors” and “decision regarding elective major surgery without patient or procedure risk factors” are both considered moderate. “Decision regarding elective major surgery with identified patient or procedure risk factors” and “decision regarding emergency major surgery” are in the high complexity column for risk.
Keep in mind that two of three elements are required: the number and complexity of problems, amount of data, and morbidity/mortality risk. Risk of morbidity/mortality alone doesn’t count as the basis for selecting the code. Of course, when surgeons see this, they ask, “What major procedures don’t have identified risk factors?”
Note, too, that these new CPT guidelines do not define the terms “minor” and “major” surgery. For payment reasons related to the postop period, the Centers for Medicare & Medicaid Services defines minor surgery as a procedure with 0-10 global days and a major surgery as a procedure with 90 global days. However, there are many procedures with 0 global days (endoscopy, cardiac catheterization) that are not minor procedures. Hopefully, the AMA will clarify this in 2021.
What’s the take-away for clinicians?
There are sure to be shifts in coding patterns based on these new guidelines. Some specialties will find that not being able to select a service based on history and exam alone will lower the level of service for which they can bill. Some practices, on the other hand, will be able to code for more high-level visits, without the need for a complete review of systems or a comprehensive exam.
The biggest challenge will be for practices that provide services both in the hospital and in the office, because they’ll have to use both sets of guidelines, depending on which type of service they’re performing.
For more details on what’s coming your way beginning on New Year’s Day, you may want to read the 16-page AMA document .
A version of this article first appeared on Medscape.com.
Betsy Nicoletti, MS, a nationally recognized coding expert, will take your coding questions via email and provide guidance on how to code properly to maximize reimbursement. Have a question about coding? Send it to [email protected].
thanks to the American Medical Association.
The first major changes to the definitions for E/M services will be in effect as of Jan. 1, 2021, with all payers expected to adopt these new guidelines. In particular, the AMA has revised the definitions for E/M codes 99202-99215 in the Current Procedural Terminology (CPT) 2021 codebook. The existing guidelines were developed in 1995 and 1997 and remain in effect for all other E/M services determined by history, exam, and medical decision-making (MDM).
What do the new changes mean to you? In 2021, for new and established office and other outpatient services reported with codes 99202-99215, a clinician may select the code on the basis of time or MDM.
There are three elements in MDM, and two of three are required. These elements are the number and complexity of problems addressed, amount and/or complexity of data to be reviewed and analyzed, and risk of complications and/or morbidity or mortality of patient management.
Make sure you familiarize yourself with these six big changes. It may take a bit of time to integrate these new processes into your daily routine, but wrapping your head around them as soon as possible can help boost your bottom line:
1. History and exam don’t count toward level of service
Physicians, advanced practice registered nurses, and physician assistants won’t use history or exam to select what level of code to bill for office visits 99202-99215, as they did in the past. They need only document a medically appropriate history and exam. The history may be obtained by staff members and reviewed by the billing practitioner.
While specific history and exam requirements disappear for office visit codes, they remain for all other types of visits, selected on the basis of history, exam, and MDM, such as hospital services, nursing facility services, and home and domiciliary care. So, say goodbye to “all other systems reviewed and negative” in office notes, but keep it handy for those other E/M codes.
2. All time spent caring for the patient on a particular day counts
This includes all time spent on the day of service, including preparing to see the patient, seeing the patient, phone calls or other work done after the visit (if not billed with a care management or other CPT code), and documenting in the medical record. The AMA developed new guidelines for using time for office and other outpatient services. For codes 99202-99215, count all of the face-to-face and non–face-to-face time spent by the billing clinician on the day of the visit. Counseling does not need to be more than 50% of the total time.
Do not include any staff time or time spent on any days before or after the visit. This allows clinicians to capture the work when a significant amount of it takes place before or after the visit with the patient, and to bill for it on the day of the visit.
According to the 2021 CPT codebook, physician or other qualified health care professional time includes the following activities:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
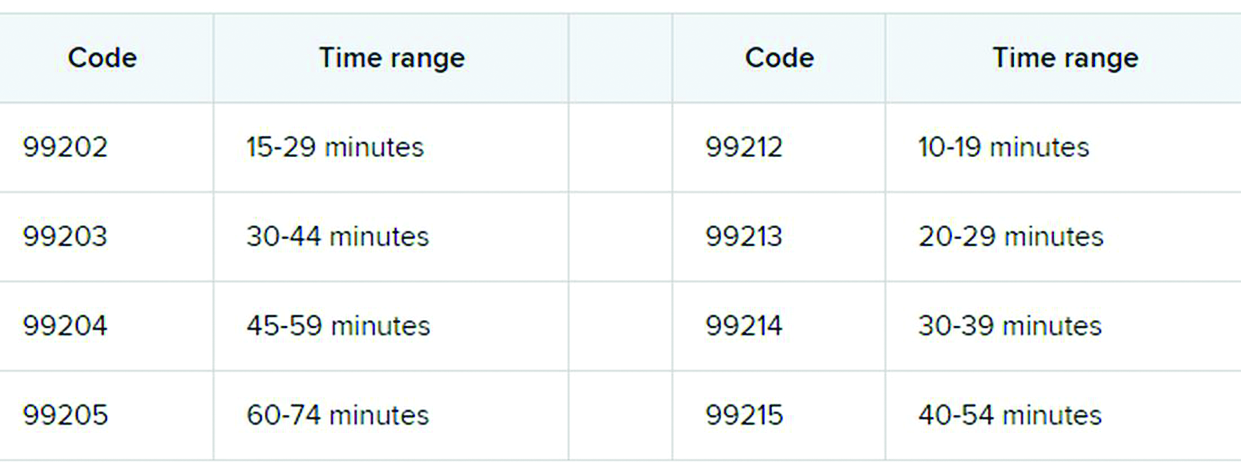
3. Soon to be gone: ‘new to the examiner’ and ‘workup planned’
The current guidelines don’t differentiate between a new problem to the clinician or an established problem to the clinician. So it doesn’t matter whether you’re hearing about a particular problem for the first time or the fifth time. The new office and outpatient services guidelines define problems only as they relate to the patient. For example, when selecting a level of service, a chronic problem with a mild exacerbation is the same level whether it’s the primary care physician seeing the patient for the 10th time to help manage her diabetes or the endocrinologist seeing the patient for the first time.
In the current guidelines (1995 and 1997), additional weight is given in selecting the level of MDM for a problem that’s new to the examiner with a workup planned, yet when the diagnostic test couldn’t be completed at the visit. This concept is gone from element of number and complexity of new problems. Ordering diagnostic tests is part of the second element, the amount and/or complexity of data to be reviewed.
4. Different guidelines if you need a history from a parent or other source
The new guidelines recognize the additional work required by the clinician when the patient is unable to give a history or when the practitioner doesn’t find the history to be reliable.
For example, in the case of a baby or child who is unable to give a history, the parent counts as an “independent historian,” according to the new guidelines. Likewise, for a patient with dementia, the caregiver counts as a historian. Note, however, that the criteria is not met simply because the patient is accompanied by another person. The additional weight in selecting the level of service is based on the patient being unable to give a reliable history.
Bottom line: In cases where patients are unable to communicate clearly, physicians or other providers should document the necessity of getting a complete history and who provided it.
5. A new spin on social determinants of health (SDoH)
In the risk of morbidity and/or mortality element, conditions described as “social determinants of health” are considered moderate complexity. SDoH are social and environmental factors that affect a patient’s health and medical outcomes. These include homelessness, inability to afford medications, food insecurity, and occupational exposure to risk factors. These circumstances are reported with codes in categories Z55-Z65.
In the past, physicians often documented this information in their office notes but rarely added a diagnosis code that described the patient’s situation. The ICD-10-CM code set includes codes that describe these factors. Using them allows the practice to track patients who have increased needs, and it communicates to payers the complexity of caring for these patients.
6. Risks related to surgery are defined
The current guidelines assign different levels of risk to minor and major surgery. They also include differentiation for “minor surgery with no identified risk factors,” “minor surgery with identified risk factors,” “elective major surgery with no identified risk factors,” and “elective major surgery with identified risk factors.” The old guidelines didn’t state whether the risk factors pertained to the patient – such as smoking, heart disease, or high body mass index – or to the procedure itself.
The new guidelines specifically say that it’s both. In the risk column, “decision regarding minor surgery with identified patient or procedure risk factors” and “decision regarding elective major surgery without patient or procedure risk factors” are both considered moderate. “Decision regarding elective major surgery with identified patient or procedure risk factors” and “decision regarding emergency major surgery” are in the high complexity column for risk.
Keep in mind that two of three elements are required: the number and complexity of problems, amount of data, and morbidity/mortality risk. Risk of morbidity/mortality alone doesn’t count as the basis for selecting the code. Of course, when surgeons see this, they ask, “What major procedures don’t have identified risk factors?”
Note, too, that these new CPT guidelines do not define the terms “minor” and “major” surgery. For payment reasons related to the postop period, the Centers for Medicare & Medicaid Services defines minor surgery as a procedure with 0-10 global days and a major surgery as a procedure with 90 global days. However, there are many procedures with 0 global days (endoscopy, cardiac catheterization) that are not minor procedures. Hopefully, the AMA will clarify this in 2021.
What’s the take-away for clinicians?
There are sure to be shifts in coding patterns based on these new guidelines. Some specialties will find that not being able to select a service based on history and exam alone will lower the level of service for which they can bill. Some practices, on the other hand, will be able to code for more high-level visits, without the need for a complete review of systems or a comprehensive exam.
The biggest challenge will be for practices that provide services both in the hospital and in the office, because they’ll have to use both sets of guidelines, depending on which type of service they’re performing.
For more details on what’s coming your way beginning on New Year’s Day, you may want to read the 16-page AMA document .
A version of this article first appeared on Medscape.com.
Betsy Nicoletti, MS, a nationally recognized coding expert, will take your coding questions via email and provide guidance on how to code properly to maximize reimbursement. Have a question about coding? Send it to [email protected].
thanks to the American Medical Association.
The first major changes to the definitions for E/M services will be in effect as of Jan. 1, 2021, with all payers expected to adopt these new guidelines. In particular, the AMA has revised the definitions for E/M codes 99202-99215 in the Current Procedural Terminology (CPT) 2021 codebook. The existing guidelines were developed in 1995 and 1997 and remain in effect for all other E/M services determined by history, exam, and medical decision-making (MDM).
What do the new changes mean to you? In 2021, for new and established office and other outpatient services reported with codes 99202-99215, a clinician may select the code on the basis of time or MDM.
There are three elements in MDM, and two of three are required. These elements are the number and complexity of problems addressed, amount and/or complexity of data to be reviewed and analyzed, and risk of complications and/or morbidity or mortality of patient management.
Make sure you familiarize yourself with these six big changes. It may take a bit of time to integrate these new processes into your daily routine, but wrapping your head around them as soon as possible can help boost your bottom line:
1. History and exam don’t count toward level of service
Physicians, advanced practice registered nurses, and physician assistants won’t use history or exam to select what level of code to bill for office visits 99202-99215, as they did in the past. They need only document a medically appropriate history and exam. The history may be obtained by staff members and reviewed by the billing practitioner.
While specific history and exam requirements disappear for office visit codes, they remain for all other types of visits, selected on the basis of history, exam, and MDM, such as hospital services, nursing facility services, and home and domiciliary care. So, say goodbye to “all other systems reviewed and negative” in office notes, but keep it handy for those other E/M codes.
2. All time spent caring for the patient on a particular day counts
This includes all time spent on the day of service, including preparing to see the patient, seeing the patient, phone calls or other work done after the visit (if not billed with a care management or other CPT code), and documenting in the medical record. The AMA developed new guidelines for using time for office and other outpatient services. For codes 99202-99215, count all of the face-to-face and non–face-to-face time spent by the billing clinician on the day of the visit. Counseling does not need to be more than 50% of the total time.
Do not include any staff time or time spent on any days before or after the visit. This allows clinicians to capture the work when a significant amount of it takes place before or after the visit with the patient, and to bill for it on the day of the visit.
According to the 2021 CPT codebook, physician or other qualified health care professional time includes the following activities:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
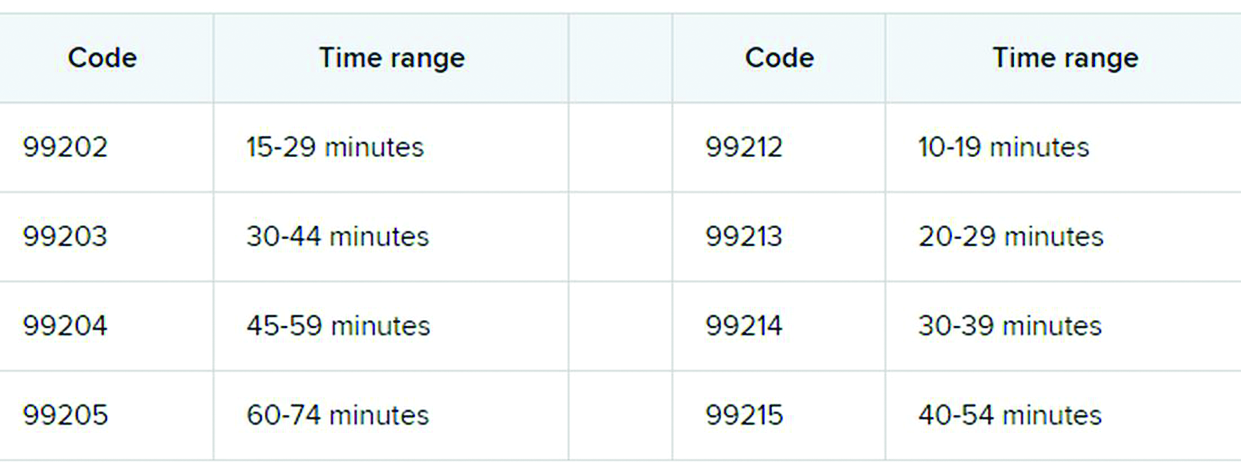
3. Soon to be gone: ‘new to the examiner’ and ‘workup planned’
The current guidelines don’t differentiate between a new problem to the clinician or an established problem to the clinician. So it doesn’t matter whether you’re hearing about a particular problem for the first time or the fifth time. The new office and outpatient services guidelines define problems only as they relate to the patient. For example, when selecting a level of service, a chronic problem with a mild exacerbation is the same level whether it’s the primary care physician seeing the patient for the 10th time to help manage her diabetes or the endocrinologist seeing the patient for the first time.
In the current guidelines (1995 and 1997), additional weight is given in selecting the level of MDM for a problem that’s new to the examiner with a workup planned, yet when the diagnostic test couldn’t be completed at the visit. This concept is gone from element of number and complexity of new problems. Ordering diagnostic tests is part of the second element, the amount and/or complexity of data to be reviewed.
4. Different guidelines if you need a history from a parent or other source
The new guidelines recognize the additional work required by the clinician when the patient is unable to give a history or when the practitioner doesn’t find the history to be reliable.
For example, in the case of a baby or child who is unable to give a history, the parent counts as an “independent historian,” according to the new guidelines. Likewise, for a patient with dementia, the caregiver counts as a historian. Note, however, that the criteria is not met simply because the patient is accompanied by another person. The additional weight in selecting the level of service is based on the patient being unable to give a reliable history.
Bottom line: In cases where patients are unable to communicate clearly, physicians or other providers should document the necessity of getting a complete history and who provided it.
5. A new spin on social determinants of health (SDoH)
In the risk of morbidity and/or mortality element, conditions described as “social determinants of health” are considered moderate complexity. SDoH are social and environmental factors that affect a patient’s health and medical outcomes. These include homelessness, inability to afford medications, food insecurity, and occupational exposure to risk factors. These circumstances are reported with codes in categories Z55-Z65.
In the past, physicians often documented this information in their office notes but rarely added a diagnosis code that described the patient’s situation. The ICD-10-CM code set includes codes that describe these factors. Using them allows the practice to track patients who have increased needs, and it communicates to payers the complexity of caring for these patients.
6. Risks related to surgery are defined
The current guidelines assign different levels of risk to minor and major surgery. They also include differentiation for “minor surgery with no identified risk factors,” “minor surgery with identified risk factors,” “elective major surgery with no identified risk factors,” and “elective major surgery with identified risk factors.” The old guidelines didn’t state whether the risk factors pertained to the patient – such as smoking, heart disease, or high body mass index – or to the procedure itself.
The new guidelines specifically say that it’s both. In the risk column, “decision regarding minor surgery with identified patient or procedure risk factors” and “decision regarding elective major surgery without patient or procedure risk factors” are both considered moderate. “Decision regarding elective major surgery with identified patient or procedure risk factors” and “decision regarding emergency major surgery” are in the high complexity column for risk.
Keep in mind that two of three elements are required: the number and complexity of problems, amount of data, and morbidity/mortality risk. Risk of morbidity/mortality alone doesn’t count as the basis for selecting the code. Of course, when surgeons see this, they ask, “What major procedures don’t have identified risk factors?”
Note, too, that these new CPT guidelines do not define the terms “minor” and “major” surgery. For payment reasons related to the postop period, the Centers for Medicare & Medicaid Services defines minor surgery as a procedure with 0-10 global days and a major surgery as a procedure with 90 global days. However, there are many procedures with 0 global days (endoscopy, cardiac catheterization) that are not minor procedures. Hopefully, the AMA will clarify this in 2021.
What’s the take-away for clinicians?
There are sure to be shifts in coding patterns based on these new guidelines. Some specialties will find that not being able to select a service based on history and exam alone will lower the level of service for which they can bill. Some practices, on the other hand, will be able to code for more high-level visits, without the need for a complete review of systems or a comprehensive exam.
The biggest challenge will be for practices that provide services both in the hospital and in the office, because they’ll have to use both sets of guidelines, depending on which type of service they’re performing.
For more details on what’s coming your way beginning on New Year’s Day, you may want to read the 16-page AMA document .
A version of this article first appeared on Medscape.com.
FDA panel supports expanded HF role for sacubitril/valsartan
UPDATED DECEMBER 17
A panel of federal advisers on Tuesday effectively backed a bid to expand approval of sacubitril/valsartan for use in a form of heart failure for which there is not yet an approved medication.
The U.S. Food and Drug Administration asked its Cardiovascular and Renal Drugs Advisory Committee to broadly consider whether new analyses of data from the PARAGON-HF trial, combined with other information, could support use of sacubitril/valsartan (Entresto, Novartis) in heart failure with preserved ejection fraction (HFpEF).
The advisory committee voted 12-1 on this question, which can be seen as a marker for an expanded approval: “Does PARAGON-HF, perhaps supported by previous studies, provide sufficient evidence to support any indication?”
The dissenting vote was cast by the panel’s chairperson, Julia B. Lewis, MD, a professor of medicine from Vanderbilt University. In explaining her vote, Dr. Lewis cited concerns about expanding use of the drug, which has a potential for hypotension. But she noted that the rest of the panelists were “impressed by the totality of the evidence” presented, including a willingness to take a new look at the PARAGON-HF trial. This study was perceived at first pass as having failed to prove a benefit for people with HFpEF.
The 2019 initial unveiling of the PARAGON-HF results had dampened hopes for an evidence-based drug therapy for HFpEF. Patients treated with the first-of-its-kind renin-angiotensin system (RAS) inhibitor, compared with those who received standard valsartan, had 13% fewer heart failure hospitalizations or cardiovascular (CV) deaths over an average of about 3 years, but the difference missed significance at a P value of .059.
“Everybody agreed that the P value of .05 was not written in stone,” Dr. Lewis said in summarizing the panelists’ views on the voting question.
At the FDA’s request, the panel also addressed several other questions without voting on them. The agency asked the panel to describe the patient population for whom an expanded approval would be appropriate. The FDA initially approved sacubitril/valsartan in 2015 to reduce the risk of cardiovascular death and hospitalization for heart failure in patients with chronic heart failure (NYHA Class II-IV) and reduced ejection fraction.
Novartis in April submitted an application to the FDA, seeking to expand the use of sacubitril/valsartan from the currently approved indication for the treatment of chronic heart failure (CHF) patients with reduced ejection fraction (HFrEF) to include what the company terms “the adjacent population of patients with preserved ejection fraction (HFpEF) who have a left ventricular ejection fraction (LVEF) below normal.” The American Society of Echocardiography and European Association of Cardiovascular Imaging define normal LVEF and normal range (±2 standard deviations) as 62% (range, 52%-72%) in men and 64% (range, 54%-74%) in women, Novartis said in its briefing materials for the meeting.
FDA panelist Christopher M. O’Connor, MD, for example, suggested that an expanded approval could allow for use of sacubitril/valsartan for the reduction of heart failure or hospitalization in patients with mildly reduced ejection fraction as defined by greater than 45% through 55%. FDA panelist C. Noel Bairey Merz, MD, director of the Barbra Streisand Women’s Heart Center at Cedars-Sinai Medical Center in Los Angeles, suggested extending this to 57% to acknowledge the higher threshold for women.
Another FDA panelist, Steven E. Nissen, MD, of the Cleveland Clinic, argued against use of imprecise terms in defining an expanded patient population for sacubitril/valsartan. If used in the right patient population, the drug could provide a benefit for people who have active heart failure with symptoms, including preventing hospitalizations and renal disease, he said.
“If you are symptomatic with a syndrome that’s consistent with heart failure and you have an ejection fraction below the lower limits of normal, I believe it’s in the public interest for you to get sacubitril/valsartan,” Dr. Nissen said.
The FDA usually follows the advice of its panels, but is not obligated to. But in this case, the agency staff were clearly seeking a path for an expanded approval of sacubitril/valsartan.
Challenging a standard
The FDA had encouraged Novartis to submit the supplementary application for the HFpEF indication and even suggested some of the post-hoc analyses, the agency staff said in a briefing document for the meeting.
PARAGON-HF illustrated some of the agency’s concerns about missed opportunities in general in large research trials. Some events of interest in studies may be miscounted due to a lack of information such as a requirement for the presence of physical examination findings that are not documented in the patient’s dossier, the FDA staff said.
“We would like to consider giving ‘partial credit’ to events based on the level of evidence provided, e.g., use of an ordinal variable rather than a dichotomous ‘yes’ or ‘no,’ ” the staff said in the briefing document.
At the panel meeting, Norman Stockbridge, MD, PhD, director of the Division of Cardiology and Nephrology in the FDA’s Center for Drug Evaluation and Research, told the panelists there is no basis in law for setting a P value of .05 as the benchmark on whether to declare a trial a success or failure.
“I wanted to take a few minutes and make sure that you on the committee understands what flexibility you have in addressing the case study in question,” Dr. Stockbridge said at the start of the meeting.
He then reviewed cases where the FDA had approved claims for cardiac medicines that had not shown desired results in key tests. These include approval of enalapril for use in asymptomatic left ventricular dysfunction on the basis of the SOLVD-Prevention trial, approval of digoxin for heart failure on the basis of the DIG study, and approval of carvedilol for reduced ejection fraction following myocardial infarction on
the basis of the CAPRICORN study, Dr. Stockbridge said.
In reviewing the data for sacubitril/valsartan, FDA staff noted a similarity between investigator-reported and adjudicated results, Stockbridge said.
“This suggested that there were events that did not need all evidentiary criteria as qualified events, but likely were nonetheless,” he said. “This is an example of dichotomization of events being wasteful of information.”
Post-hoc exploratory analyses in PARAGON-HF were able to meet the commonly used standard, according to the FDA briefing document. Among the key findings of these analyses were:
- An analysis of investigator-reported events for the primary composite endpoint of total hospitalizations for heart failure (HHF) and cardiovascular (CV) death demonstrated a rate ratio (RR) of 0.84 (95% confidence interval 0.74- 0.97; P = .01).
- Investigator-reported events added 226 and 290 HHF events but decreased CV death by 56 and 58 events in the sacubitril/valsartan and valsartan arms, respectively. Hence, a net 170 and 232 events were added to the clinical endpoint committee–reported primary composite endpoint leading to a P value of .01, without a significant change in RR.
- Analysis of investigator-reported expanded primary composite endpoint events including total HHF, urgent HF visits, and CV death demonstrated a RR of 0.83 (95% CI, 0.73-0.95; P = .006. There were 136 and 173 investigator-reported urgent HF events in sacubitril/valsartan and valsartan arms, respectively.
Opening a floodgate?
Cynthia L. Chauhan, MSW, of Wichita, Kansas, who served as the consumer representative on the panel, questioned whether a decision to revisit the data on PARAGON-HF might lead drugmakers to seek to repurpose other failed trials.
“Are we opening any kind of floodgate for other researchers to go back and see this is an invitation to try to, for want of a better term, back-door their way into some approvals?” Ms. Chauhan asked.
Dr. Nissen assured her that this concern was valid and would be considered. The goal would be to allow some flexibility in cases that merit further consideration, while preventing companies from data mining until they find some evidence to support an FDA application, he said.
Re-analyzing trials “should be done carefully, conservatively, and only when it really is compelling that the public interest supports it,” Dr. Nissen stressed.
Panelists reported no conflicts of interest related to the topic of the meeting.
UPDATED DECEMBER 17
A panel of federal advisers on Tuesday effectively backed a bid to expand approval of sacubitril/valsartan for use in a form of heart failure for which there is not yet an approved medication.
The U.S. Food and Drug Administration asked its Cardiovascular and Renal Drugs Advisory Committee to broadly consider whether new analyses of data from the PARAGON-HF trial, combined with other information, could support use of sacubitril/valsartan (Entresto, Novartis) in heart failure with preserved ejection fraction (HFpEF).
The advisory committee voted 12-1 on this question, which can be seen as a marker for an expanded approval: “Does PARAGON-HF, perhaps supported by previous studies, provide sufficient evidence to support any indication?”
The dissenting vote was cast by the panel’s chairperson, Julia B. Lewis, MD, a professor of medicine from Vanderbilt University. In explaining her vote, Dr. Lewis cited concerns about expanding use of the drug, which has a potential for hypotension. But she noted that the rest of the panelists were “impressed by the totality of the evidence” presented, including a willingness to take a new look at the PARAGON-HF trial. This study was perceived at first pass as having failed to prove a benefit for people with HFpEF.
The 2019 initial unveiling of the PARAGON-HF results had dampened hopes for an evidence-based drug therapy for HFpEF. Patients treated with the first-of-its-kind renin-angiotensin system (RAS) inhibitor, compared with those who received standard valsartan, had 13% fewer heart failure hospitalizations or cardiovascular (CV) deaths over an average of about 3 years, but the difference missed significance at a P value of .059.
“Everybody agreed that the P value of .05 was not written in stone,” Dr. Lewis said in summarizing the panelists’ views on the voting question.
At the FDA’s request, the panel also addressed several other questions without voting on them. The agency asked the panel to describe the patient population for whom an expanded approval would be appropriate. The FDA initially approved sacubitril/valsartan in 2015 to reduce the risk of cardiovascular death and hospitalization for heart failure in patients with chronic heart failure (NYHA Class II-IV) and reduced ejection fraction.
Novartis in April submitted an application to the FDA, seeking to expand the use of sacubitril/valsartan from the currently approved indication for the treatment of chronic heart failure (CHF) patients with reduced ejection fraction (HFrEF) to include what the company terms “the adjacent population of patients with preserved ejection fraction (HFpEF) who have a left ventricular ejection fraction (LVEF) below normal.” The American Society of Echocardiography and European Association of Cardiovascular Imaging define normal LVEF and normal range (±2 standard deviations) as 62% (range, 52%-72%) in men and 64% (range, 54%-74%) in women, Novartis said in its briefing materials for the meeting.
FDA panelist Christopher M. O’Connor, MD, for example, suggested that an expanded approval could allow for use of sacubitril/valsartan for the reduction of heart failure or hospitalization in patients with mildly reduced ejection fraction as defined by greater than 45% through 55%. FDA panelist C. Noel Bairey Merz, MD, director of the Barbra Streisand Women’s Heart Center at Cedars-Sinai Medical Center in Los Angeles, suggested extending this to 57% to acknowledge the higher threshold for women.
Another FDA panelist, Steven E. Nissen, MD, of the Cleveland Clinic, argued against use of imprecise terms in defining an expanded patient population for sacubitril/valsartan. If used in the right patient population, the drug could provide a benefit for people who have active heart failure with symptoms, including preventing hospitalizations and renal disease, he said.
“If you are symptomatic with a syndrome that’s consistent with heart failure and you have an ejection fraction below the lower limits of normal, I believe it’s in the public interest for you to get sacubitril/valsartan,” Dr. Nissen said.
The FDA usually follows the advice of its panels, but is not obligated to. But in this case, the agency staff were clearly seeking a path for an expanded approval of sacubitril/valsartan.
Challenging a standard
The FDA had encouraged Novartis to submit the supplementary application for the HFpEF indication and even suggested some of the post-hoc analyses, the agency staff said in a briefing document for the meeting.
PARAGON-HF illustrated some of the agency’s concerns about missed opportunities in general in large research trials. Some events of interest in studies may be miscounted due to a lack of information such as a requirement for the presence of physical examination findings that are not documented in the patient’s dossier, the FDA staff said.
“We would like to consider giving ‘partial credit’ to events based on the level of evidence provided, e.g., use of an ordinal variable rather than a dichotomous ‘yes’ or ‘no,’ ” the staff said in the briefing document.
At the panel meeting, Norman Stockbridge, MD, PhD, director of the Division of Cardiology and Nephrology in the FDA’s Center for Drug Evaluation and Research, told the panelists there is no basis in law for setting a P value of .05 as the benchmark on whether to declare a trial a success or failure.
“I wanted to take a few minutes and make sure that you on the committee understands what flexibility you have in addressing the case study in question,” Dr. Stockbridge said at the start of the meeting.
He then reviewed cases where the FDA had approved claims for cardiac medicines that had not shown desired results in key tests. These include approval of enalapril for use in asymptomatic left ventricular dysfunction on the basis of the SOLVD-Prevention trial, approval of digoxin for heart failure on the basis of the DIG study, and approval of carvedilol for reduced ejection fraction following myocardial infarction on
the basis of the CAPRICORN study, Dr. Stockbridge said.
In reviewing the data for sacubitril/valsartan, FDA staff noted a similarity between investigator-reported and adjudicated results, Stockbridge said.
“This suggested that there were events that did not need all evidentiary criteria as qualified events, but likely were nonetheless,” he said. “This is an example of dichotomization of events being wasteful of information.”
Post-hoc exploratory analyses in PARAGON-HF were able to meet the commonly used standard, according to the FDA briefing document. Among the key findings of these analyses were:
- An analysis of investigator-reported events for the primary composite endpoint of total hospitalizations for heart failure (HHF) and cardiovascular (CV) death demonstrated a rate ratio (RR) of 0.84 (95% confidence interval 0.74- 0.97; P = .01).
- Investigator-reported events added 226 and 290 HHF events but decreased CV death by 56 and 58 events in the sacubitril/valsartan and valsartan arms, respectively. Hence, a net 170 and 232 events were added to the clinical endpoint committee–reported primary composite endpoint leading to a P value of .01, without a significant change in RR.
- Analysis of investigator-reported expanded primary composite endpoint events including total HHF, urgent HF visits, and CV death demonstrated a RR of 0.83 (95% CI, 0.73-0.95; P = .006. There were 136 and 173 investigator-reported urgent HF events in sacubitril/valsartan and valsartan arms, respectively.
Opening a floodgate?
Cynthia L. Chauhan, MSW, of Wichita, Kansas, who served as the consumer representative on the panel, questioned whether a decision to revisit the data on PARAGON-HF might lead drugmakers to seek to repurpose other failed trials.
“Are we opening any kind of floodgate for other researchers to go back and see this is an invitation to try to, for want of a better term, back-door their way into some approvals?” Ms. Chauhan asked.
Dr. Nissen assured her that this concern was valid and would be considered. The goal would be to allow some flexibility in cases that merit further consideration, while preventing companies from data mining until they find some evidence to support an FDA application, he said.
Re-analyzing trials “should be done carefully, conservatively, and only when it really is compelling that the public interest supports it,” Dr. Nissen stressed.
Panelists reported no conflicts of interest related to the topic of the meeting.
UPDATED DECEMBER 17
A panel of federal advisers on Tuesday effectively backed a bid to expand approval of sacubitril/valsartan for use in a form of heart failure for which there is not yet an approved medication.
The U.S. Food and Drug Administration asked its Cardiovascular and Renal Drugs Advisory Committee to broadly consider whether new analyses of data from the PARAGON-HF trial, combined with other information, could support use of sacubitril/valsartan (Entresto, Novartis) in heart failure with preserved ejection fraction (HFpEF).
The advisory committee voted 12-1 on this question, which can be seen as a marker for an expanded approval: “Does PARAGON-HF, perhaps supported by previous studies, provide sufficient evidence to support any indication?”
The dissenting vote was cast by the panel’s chairperson, Julia B. Lewis, MD, a professor of medicine from Vanderbilt University. In explaining her vote, Dr. Lewis cited concerns about expanding use of the drug, which has a potential for hypotension. But she noted that the rest of the panelists were “impressed by the totality of the evidence” presented, including a willingness to take a new look at the PARAGON-HF trial. This study was perceived at first pass as having failed to prove a benefit for people with HFpEF.
The 2019 initial unveiling of the PARAGON-HF results had dampened hopes for an evidence-based drug therapy for HFpEF. Patients treated with the first-of-its-kind renin-angiotensin system (RAS) inhibitor, compared with those who received standard valsartan, had 13% fewer heart failure hospitalizations or cardiovascular (CV) deaths over an average of about 3 years, but the difference missed significance at a P value of .059.
“Everybody agreed that the P value of .05 was not written in stone,” Dr. Lewis said in summarizing the panelists’ views on the voting question.
At the FDA’s request, the panel also addressed several other questions without voting on them. The agency asked the panel to describe the patient population for whom an expanded approval would be appropriate. The FDA initially approved sacubitril/valsartan in 2015 to reduce the risk of cardiovascular death and hospitalization for heart failure in patients with chronic heart failure (NYHA Class II-IV) and reduced ejection fraction.
Novartis in April submitted an application to the FDA, seeking to expand the use of sacubitril/valsartan from the currently approved indication for the treatment of chronic heart failure (CHF) patients with reduced ejection fraction (HFrEF) to include what the company terms “the adjacent population of patients with preserved ejection fraction (HFpEF) who have a left ventricular ejection fraction (LVEF) below normal.” The American Society of Echocardiography and European Association of Cardiovascular Imaging define normal LVEF and normal range (±2 standard deviations) as 62% (range, 52%-72%) in men and 64% (range, 54%-74%) in women, Novartis said in its briefing materials for the meeting.
FDA panelist Christopher M. O’Connor, MD, for example, suggested that an expanded approval could allow for use of sacubitril/valsartan for the reduction of heart failure or hospitalization in patients with mildly reduced ejection fraction as defined by greater than 45% through 55%. FDA panelist C. Noel Bairey Merz, MD, director of the Barbra Streisand Women’s Heart Center at Cedars-Sinai Medical Center in Los Angeles, suggested extending this to 57% to acknowledge the higher threshold for women.
Another FDA panelist, Steven E. Nissen, MD, of the Cleveland Clinic, argued against use of imprecise terms in defining an expanded patient population for sacubitril/valsartan. If used in the right patient population, the drug could provide a benefit for people who have active heart failure with symptoms, including preventing hospitalizations and renal disease, he said.
“If you are symptomatic with a syndrome that’s consistent with heart failure and you have an ejection fraction below the lower limits of normal, I believe it’s in the public interest for you to get sacubitril/valsartan,” Dr. Nissen said.
The FDA usually follows the advice of its panels, but is not obligated to. But in this case, the agency staff were clearly seeking a path for an expanded approval of sacubitril/valsartan.
Challenging a standard
The FDA had encouraged Novartis to submit the supplementary application for the HFpEF indication and even suggested some of the post-hoc analyses, the agency staff said in a briefing document for the meeting.
PARAGON-HF illustrated some of the agency’s concerns about missed opportunities in general in large research trials. Some events of interest in studies may be miscounted due to a lack of information such as a requirement for the presence of physical examination findings that are not documented in the patient’s dossier, the FDA staff said.
“We would like to consider giving ‘partial credit’ to events based on the level of evidence provided, e.g., use of an ordinal variable rather than a dichotomous ‘yes’ or ‘no,’ ” the staff said in the briefing document.
At the panel meeting, Norman Stockbridge, MD, PhD, director of the Division of Cardiology and Nephrology in the FDA’s Center for Drug Evaluation and Research, told the panelists there is no basis in law for setting a P value of .05 as the benchmark on whether to declare a trial a success or failure.
“I wanted to take a few minutes and make sure that you on the committee understands what flexibility you have in addressing the case study in question,” Dr. Stockbridge said at the start of the meeting.
He then reviewed cases where the FDA had approved claims for cardiac medicines that had not shown desired results in key tests. These include approval of enalapril for use in asymptomatic left ventricular dysfunction on the basis of the SOLVD-Prevention trial, approval of digoxin for heart failure on the basis of the DIG study, and approval of carvedilol for reduced ejection fraction following myocardial infarction on
the basis of the CAPRICORN study, Dr. Stockbridge said.
In reviewing the data for sacubitril/valsartan, FDA staff noted a similarity between investigator-reported and adjudicated results, Stockbridge said.
“This suggested that there were events that did not need all evidentiary criteria as qualified events, but likely were nonetheless,” he said. “This is an example of dichotomization of events being wasteful of information.”
Post-hoc exploratory analyses in PARAGON-HF were able to meet the commonly used standard, according to the FDA briefing document. Among the key findings of these analyses were:
- An analysis of investigator-reported events for the primary composite endpoint of total hospitalizations for heart failure (HHF) and cardiovascular (CV) death demonstrated a rate ratio (RR) of 0.84 (95% confidence interval 0.74- 0.97; P = .01).
- Investigator-reported events added 226 and 290 HHF events but decreased CV death by 56 and 58 events in the sacubitril/valsartan and valsartan arms, respectively. Hence, a net 170 and 232 events were added to the clinical endpoint committee–reported primary composite endpoint leading to a P value of .01, without a significant change in RR.
- Analysis of investigator-reported expanded primary composite endpoint events including total HHF, urgent HF visits, and CV death demonstrated a RR of 0.83 (95% CI, 0.73-0.95; P = .006. There were 136 and 173 investigator-reported urgent HF events in sacubitril/valsartan and valsartan arms, respectively.
Opening a floodgate?
Cynthia L. Chauhan, MSW, of Wichita, Kansas, who served as the consumer representative on the panel, questioned whether a decision to revisit the data on PARAGON-HF might lead drugmakers to seek to repurpose other failed trials.
“Are we opening any kind of floodgate for other researchers to go back and see this is an invitation to try to, for want of a better term, back-door their way into some approvals?” Ms. Chauhan asked.
Dr. Nissen assured her that this concern was valid and would be considered. The goal would be to allow some flexibility in cases that merit further consideration, while preventing companies from data mining until they find some evidence to support an FDA application, he said.
Re-analyzing trials “should be done carefully, conservatively, and only when it really is compelling that the public interest supports it,” Dr. Nissen stressed.
Panelists reported no conflicts of interest related to the topic of the meeting.
Endocrine-disrupting plastics pose growing health threat
Many types of plastics pose an unrecognized threat to human health by leaching endocrine-disrupting chemicals, and a new report from the Endocrine Society and the International Pollutants Elimination Network presents their dangers and risks.
Written in a consumer-friendly form designed to guide public interest groups and policy makers, the report also can be used by clinicians to inform discussions with patients about the potential dangers of plastics and how they can reduce their exposure to endocrine-disrupting chemicals.
The report, Plastics, EDCs, & Health, defines endocrine-disrupting chemicals (EDCs) as “an exogenous chemical, or mixture of chemicals, that interferes with any aspect of hormone action.” Hormones in the body must be released at specific times, and therefore interference with their normal activity can have profound effects on health in areas including growth and reproductive development, according to the report.
The available data show “more and more information about the different chemicals and the different effects they are having,” said lead author, Jodi Flaws, PhD, of the University of Illinois at Urbana-Champaign, in a virtual press conference accompanying the release of the report.
Although numerous EDCs have been identified, a recent study suggested that many potentially dangerous chemical additives remain unknown because they are identified as confidential or simply not well described, the report authors said. In addition, creation of more plastic products will likely lead to increased exposure to EDCs and make health problems worse, said report coauthor Pauliina Damdimopoulou, PhD, of the Karolinska Institutet in Stockholm.
Lesser-known EDCs populate consumer products
Most consumers are aware of bisphenol A and phthalates as known EDCs, said Dr. Flaws, but the report identifies other lesser-known EDCs including per- and polyfluoroalkyl substances (PFAS), dioxins, flame retardants, and UV stabilizers.
For example, PFAS have been used for decades in a range of consumer products including stain resistant clothes, fast food wrappers, carpet and furniture treatments, cookware, and firefighting foams, according to the report. Consequently, PFAS have become common in many water sources including surface water, drinking water, and ground water because of how they are disposed. “Consumption of fish and other aquatic creatures caught in waterways contaminated with PFAS also poses heightened risks due to bioaccumulation of persistent chemicals in these animals,” the report authors noted. Human exposures to PFAS have been documented in urine, serum, plasma, placenta, umbilical cord, breast milk, and fetal tissues, they added.
Brominated flame retardants are another lesser-known EDC highlighted in the report. These chemical additives are used in plastics such as electronics cases to reduce the spread of fire, as well as in furniture foam and other building materials, the authors wrote. UV stabilizers, which also have been linked to health problems, often are used in manufacturing cars and other machinery.
Microplastics create large risk
Microplastics, defined as plastic particles less than 5 mm in diameter, are another source of exposure to EDCs that is not well publicized, according to the report. Plastic waste disposal often leads to the release of microplastics, which can infiltrate soil and water. Plastic waste is often dumped or burned; outdoor burning of plastic causes emission of dioxins into the air and ground.
“Not only do microplastics contain endogenous chemical additives, which are not bound to the microplastic and can leach out of the microplastic and expose the population, they can also bind and accumulate toxic chemicals from the surrounding environment such as sea water and sediment,” the report authors said.
Recycling is not an easy answer, either. Often more chemicals are created and released during the process of using plastics to make other plastics, according to the report.
Overall, more awareness of the potential for increased exposure to EDCs and support of strategies to seek out alternatives to hazardous chemicals is needed at the global level, the authors wrote. For example, the European Union has proposed a chemicals strategy that includes improved classification of EDCs and banning identified EDCs in consumer products.
New data support ongoing dangers
“It was important to produce the report at this time because several new studies came out on the effects of EDCs from plastics on human health,” Dr. Flaws said in an interview. “Further, there was not previously a single source that brought together all the information in a manner that was targeted towards the public, policy makers, and others,” she said.
Dr. Flaws said that what has surprised her most in the recent research is the fact that plastics contain such a range of chemicals and EDCs.
“A good take-home message [from the report] is that plastics can contain endocrine-disrupting chemicals that can interfere with normal hormones and lead to adverse health outcomes,” she said. “I suggest limiting the use of plastics as much as possible. I know this is very hard to do, so if someone needs to use plastic, they should not heat food or drink in plastic containers,” she emphasized. Individuals also can limit reuse of plastics over and over,” she said. “Heating and repeated use/washing often causes plastics to leach EDCs into food and drink that we then get into our bodies.”
Additional research is needed to understand the mechanisms by which EDCs from plastics cause damage, Dr. Flaws emphasized. “Given that it is not possible to eliminate plastics at this time, if we understood mechanisms of action, we could develop ways to prevent toxicity or treat EDC-induced adverse health outcomes,” she said. “We also need research designed to develop plastics or ‘green materials’ that do not contain endocrine disruptors and do not cause health problems or damage the environment,” she noted.
The report was produced as a joint effort of the Endocrine Society and International Pollutants Elimination Network. The report authors had no financial conflicts to disclose.
Many types of plastics pose an unrecognized threat to human health by leaching endocrine-disrupting chemicals, and a new report from the Endocrine Society and the International Pollutants Elimination Network presents their dangers and risks.
Written in a consumer-friendly form designed to guide public interest groups and policy makers, the report also can be used by clinicians to inform discussions with patients about the potential dangers of plastics and how they can reduce their exposure to endocrine-disrupting chemicals.
The report, Plastics, EDCs, & Health, defines endocrine-disrupting chemicals (EDCs) as “an exogenous chemical, or mixture of chemicals, that interferes with any aspect of hormone action.” Hormones in the body must be released at specific times, and therefore interference with their normal activity can have profound effects on health in areas including growth and reproductive development, according to the report.
The available data show “more and more information about the different chemicals and the different effects they are having,” said lead author, Jodi Flaws, PhD, of the University of Illinois at Urbana-Champaign, in a virtual press conference accompanying the release of the report.
Although numerous EDCs have been identified, a recent study suggested that many potentially dangerous chemical additives remain unknown because they are identified as confidential or simply not well described, the report authors said. In addition, creation of more plastic products will likely lead to increased exposure to EDCs and make health problems worse, said report coauthor Pauliina Damdimopoulou, PhD, of the Karolinska Institutet in Stockholm.
Lesser-known EDCs populate consumer products
Most consumers are aware of bisphenol A and phthalates as known EDCs, said Dr. Flaws, but the report identifies other lesser-known EDCs including per- and polyfluoroalkyl substances (PFAS), dioxins, flame retardants, and UV stabilizers.
For example, PFAS have been used for decades in a range of consumer products including stain resistant clothes, fast food wrappers, carpet and furniture treatments, cookware, and firefighting foams, according to the report. Consequently, PFAS have become common in many water sources including surface water, drinking water, and ground water because of how they are disposed. “Consumption of fish and other aquatic creatures caught in waterways contaminated with PFAS also poses heightened risks due to bioaccumulation of persistent chemicals in these animals,” the report authors noted. Human exposures to PFAS have been documented in urine, serum, plasma, placenta, umbilical cord, breast milk, and fetal tissues, they added.
Brominated flame retardants are another lesser-known EDC highlighted in the report. These chemical additives are used in plastics such as electronics cases to reduce the spread of fire, as well as in furniture foam and other building materials, the authors wrote. UV stabilizers, which also have been linked to health problems, often are used in manufacturing cars and other machinery.
Microplastics create large risk
Microplastics, defined as plastic particles less than 5 mm in diameter, are another source of exposure to EDCs that is not well publicized, according to the report. Plastic waste disposal often leads to the release of microplastics, which can infiltrate soil and water. Plastic waste is often dumped or burned; outdoor burning of plastic causes emission of dioxins into the air and ground.
“Not only do microplastics contain endogenous chemical additives, which are not bound to the microplastic and can leach out of the microplastic and expose the population, they can also bind and accumulate toxic chemicals from the surrounding environment such as sea water and sediment,” the report authors said.
Recycling is not an easy answer, either. Often more chemicals are created and released during the process of using plastics to make other plastics, according to the report.
Overall, more awareness of the potential for increased exposure to EDCs and support of strategies to seek out alternatives to hazardous chemicals is needed at the global level, the authors wrote. For example, the European Union has proposed a chemicals strategy that includes improved classification of EDCs and banning identified EDCs in consumer products.
New data support ongoing dangers
“It was important to produce the report at this time because several new studies came out on the effects of EDCs from plastics on human health,” Dr. Flaws said in an interview. “Further, there was not previously a single source that brought together all the information in a manner that was targeted towards the public, policy makers, and others,” she said.
Dr. Flaws said that what has surprised her most in the recent research is the fact that plastics contain such a range of chemicals and EDCs.
“A good take-home message [from the report] is that plastics can contain endocrine-disrupting chemicals that can interfere with normal hormones and lead to adverse health outcomes,” she said. “I suggest limiting the use of plastics as much as possible. I know this is very hard to do, so if someone needs to use plastic, they should not heat food or drink in plastic containers,” she emphasized. Individuals also can limit reuse of plastics over and over,” she said. “Heating and repeated use/washing often causes plastics to leach EDCs into food and drink that we then get into our bodies.”
Additional research is needed to understand the mechanisms by which EDCs from plastics cause damage, Dr. Flaws emphasized. “Given that it is not possible to eliminate plastics at this time, if we understood mechanisms of action, we could develop ways to prevent toxicity or treat EDC-induced adverse health outcomes,” she said. “We also need research designed to develop plastics or ‘green materials’ that do not contain endocrine disruptors and do not cause health problems or damage the environment,” she noted.
The report was produced as a joint effort of the Endocrine Society and International Pollutants Elimination Network. The report authors had no financial conflicts to disclose.
Many types of plastics pose an unrecognized threat to human health by leaching endocrine-disrupting chemicals, and a new report from the Endocrine Society and the International Pollutants Elimination Network presents their dangers and risks.
Written in a consumer-friendly form designed to guide public interest groups and policy makers, the report also can be used by clinicians to inform discussions with patients about the potential dangers of plastics and how they can reduce their exposure to endocrine-disrupting chemicals.
The report, Plastics, EDCs, & Health, defines endocrine-disrupting chemicals (EDCs) as “an exogenous chemical, or mixture of chemicals, that interferes with any aspect of hormone action.” Hormones in the body must be released at specific times, and therefore interference with their normal activity can have profound effects on health in areas including growth and reproductive development, according to the report.
The available data show “more and more information about the different chemicals and the different effects they are having,” said lead author, Jodi Flaws, PhD, of the University of Illinois at Urbana-Champaign, in a virtual press conference accompanying the release of the report.
Although numerous EDCs have been identified, a recent study suggested that many potentially dangerous chemical additives remain unknown because they are identified as confidential or simply not well described, the report authors said. In addition, creation of more plastic products will likely lead to increased exposure to EDCs and make health problems worse, said report coauthor Pauliina Damdimopoulou, PhD, of the Karolinska Institutet in Stockholm.
Lesser-known EDCs populate consumer products
Most consumers are aware of bisphenol A and phthalates as known EDCs, said Dr. Flaws, but the report identifies other lesser-known EDCs including per- and polyfluoroalkyl substances (PFAS), dioxins, flame retardants, and UV stabilizers.
For example, PFAS have been used for decades in a range of consumer products including stain resistant clothes, fast food wrappers, carpet and furniture treatments, cookware, and firefighting foams, according to the report. Consequently, PFAS have become common in many water sources including surface water, drinking water, and ground water because of how they are disposed. “Consumption of fish and other aquatic creatures caught in waterways contaminated with PFAS also poses heightened risks due to bioaccumulation of persistent chemicals in these animals,” the report authors noted. Human exposures to PFAS have been documented in urine, serum, plasma, placenta, umbilical cord, breast milk, and fetal tissues, they added.
Brominated flame retardants are another lesser-known EDC highlighted in the report. These chemical additives are used in plastics such as electronics cases to reduce the spread of fire, as well as in furniture foam and other building materials, the authors wrote. UV stabilizers, which also have been linked to health problems, often are used in manufacturing cars and other machinery.
Microplastics create large risk
Microplastics, defined as plastic particles less than 5 mm in diameter, are another source of exposure to EDCs that is not well publicized, according to the report. Plastic waste disposal often leads to the release of microplastics, which can infiltrate soil and water. Plastic waste is often dumped or burned; outdoor burning of plastic causes emission of dioxins into the air and ground.
“Not only do microplastics contain endogenous chemical additives, which are not bound to the microplastic and can leach out of the microplastic and expose the population, they can also bind and accumulate toxic chemicals from the surrounding environment such as sea water and sediment,” the report authors said.
Recycling is not an easy answer, either. Often more chemicals are created and released during the process of using plastics to make other plastics, according to the report.
Overall, more awareness of the potential for increased exposure to EDCs and support of strategies to seek out alternatives to hazardous chemicals is needed at the global level, the authors wrote. For example, the European Union has proposed a chemicals strategy that includes improved classification of EDCs and banning identified EDCs in consumer products.
New data support ongoing dangers
“It was important to produce the report at this time because several new studies came out on the effects of EDCs from plastics on human health,” Dr. Flaws said in an interview. “Further, there was not previously a single source that brought together all the information in a manner that was targeted towards the public, policy makers, and others,” she said.
Dr. Flaws said that what has surprised her most in the recent research is the fact that plastics contain such a range of chemicals and EDCs.
“A good take-home message [from the report] is that plastics can contain endocrine-disrupting chemicals that can interfere with normal hormones and lead to adverse health outcomes,” she said. “I suggest limiting the use of plastics as much as possible. I know this is very hard to do, so if someone needs to use plastic, they should not heat food or drink in plastic containers,” she emphasized. Individuals also can limit reuse of plastics over and over,” she said. “Heating and repeated use/washing often causes plastics to leach EDCs into food and drink that we then get into our bodies.”
Additional research is needed to understand the mechanisms by which EDCs from plastics cause damage, Dr. Flaws emphasized. “Given that it is not possible to eliminate plastics at this time, if we understood mechanisms of action, we could develop ways to prevent toxicity or treat EDC-induced adverse health outcomes,” she said. “We also need research designed to develop plastics or ‘green materials’ that do not contain endocrine disruptors and do not cause health problems or damage the environment,” she noted.
The report was produced as a joint effort of the Endocrine Society and International Pollutants Elimination Network. The report authors had no financial conflicts to disclose.
Liver injury linked to COVID-19–related coagulopathy
There is a link between liver injury and a tendency toward excessive clotting in patients with COVID-19, and the organ’s own blood vessels could be responsible, new research shows.
The effect of IL-6 on the liver sinusoidal endothelial cells lining the liver blood vessels creates a prothrombotic environment that includes the release of factor VIII, said investigator Matthew McConnell, MD, from the Yale University, New Haven, Conn.
Dr. McConnell presented the results at the virtual annual meeting of the American Association for the Study of Liver Diseases.
These associations offer insights into why COVID-19 patients with underlying liver disease can experience “devastating complications” related to improper blood vessel function in the organ, he added.
For their study, Dr. McConnell and colleagues analyzed data on ALT and hypercoagulability from 68 adults treated at the Yale–New Haven Hospital. The liver and coagulation tests were administered within 5 days of each other.
The team set the ALT cutoff for liver injury at three times the upper limit of normal. Patients with two or more parameters indicating excessive clotting were considered to have a hypercoagulable profile, which Dr. McConnell called “a signature clinical finding of COVID-19 infection.”
Patients with high levels of ALT also experienced elevations in clotting-related factors, such as fibrinogen levels and the activity of factor VIII and factor II. Furthermore, liver injury was significantly associated with hypercoagulability (P < .05).
Because COVID-19 is linked to the proinflammatory IL-6, the investigators examined how this cytokine and its receptor affect human liver sinusoidal cells. Cells exposed to IL-6 and its receptor pumped out factor VIII at levels that were significantly higher than in unexposed cells (P < .01). Exposed cells also produced significantly more von Willebrand factor (P < .05), another prothrombotic molecule, and showed increased expression of genes that induce the expression of factor VIII.There is utility in the findings beyond COVID-19, said Dr. McConnell. They provide “insights into complications of critical illness, in general, in the liver blood vessels” of patients with underlying liver disease.
Dr. McConnell has no conflicts.
For the latest clinical guidance, education, research, and physician resources about coronavirus, visit the AGA COVID-19 Resource Center at www.gastro.org/COVID.
A version of this article originally appeared on Medscape.com.
There is a link between liver injury and a tendency toward excessive clotting in patients with COVID-19, and the organ’s own blood vessels could be responsible, new research shows.
The effect of IL-6 on the liver sinusoidal endothelial cells lining the liver blood vessels creates a prothrombotic environment that includes the release of factor VIII, said investigator Matthew McConnell, MD, from the Yale University, New Haven, Conn.
Dr. McConnell presented the results at the virtual annual meeting of the American Association for the Study of Liver Diseases.
These associations offer insights into why COVID-19 patients with underlying liver disease can experience “devastating complications” related to improper blood vessel function in the organ, he added.
For their study, Dr. McConnell and colleagues analyzed data on ALT and hypercoagulability from 68 adults treated at the Yale–New Haven Hospital. The liver and coagulation tests were administered within 5 days of each other.
The team set the ALT cutoff for liver injury at three times the upper limit of normal. Patients with two or more parameters indicating excessive clotting were considered to have a hypercoagulable profile, which Dr. McConnell called “a signature clinical finding of COVID-19 infection.”
Patients with high levels of ALT also experienced elevations in clotting-related factors, such as fibrinogen levels and the activity of factor VIII and factor II. Furthermore, liver injury was significantly associated with hypercoagulability (P < .05).
Because COVID-19 is linked to the proinflammatory IL-6, the investigators examined how this cytokine and its receptor affect human liver sinusoidal cells. Cells exposed to IL-6 and its receptor pumped out factor VIII at levels that were significantly higher than in unexposed cells (P < .01). Exposed cells also produced significantly more von Willebrand factor (P < .05), another prothrombotic molecule, and showed increased expression of genes that induce the expression of factor VIII.There is utility in the findings beyond COVID-19, said Dr. McConnell. They provide “insights into complications of critical illness, in general, in the liver blood vessels” of patients with underlying liver disease.
Dr. McConnell has no conflicts.
For the latest clinical guidance, education, research, and physician resources about coronavirus, visit the AGA COVID-19 Resource Center at www.gastro.org/COVID.
A version of this article originally appeared on Medscape.com.
There is a link between liver injury and a tendency toward excessive clotting in patients with COVID-19, and the organ’s own blood vessels could be responsible, new research shows.
The effect of IL-6 on the liver sinusoidal endothelial cells lining the liver blood vessels creates a prothrombotic environment that includes the release of factor VIII, said investigator Matthew McConnell, MD, from the Yale University, New Haven, Conn.
Dr. McConnell presented the results at the virtual annual meeting of the American Association for the Study of Liver Diseases.
These associations offer insights into why COVID-19 patients with underlying liver disease can experience “devastating complications” related to improper blood vessel function in the organ, he added.
For their study, Dr. McConnell and colleagues analyzed data on ALT and hypercoagulability from 68 adults treated at the Yale–New Haven Hospital. The liver and coagulation tests were administered within 5 days of each other.
The team set the ALT cutoff for liver injury at three times the upper limit of normal. Patients with two or more parameters indicating excessive clotting were considered to have a hypercoagulable profile, which Dr. McConnell called “a signature clinical finding of COVID-19 infection.”
Patients with high levels of ALT also experienced elevations in clotting-related factors, such as fibrinogen levels and the activity of factor VIII and factor II. Furthermore, liver injury was significantly associated with hypercoagulability (P < .05).
Because COVID-19 is linked to the proinflammatory IL-6, the investigators examined how this cytokine and its receptor affect human liver sinusoidal cells. Cells exposed to IL-6 and its receptor pumped out factor VIII at levels that were significantly higher than in unexposed cells (P < .01). Exposed cells also produced significantly more von Willebrand factor (P < .05), another prothrombotic molecule, and showed increased expression of genes that induce the expression of factor VIII.There is utility in the findings beyond COVID-19, said Dr. McConnell. They provide “insights into complications of critical illness, in general, in the liver blood vessels” of patients with underlying liver disease.
Dr. McConnell has no conflicts.
For the latest clinical guidance, education, research, and physician resources about coronavirus, visit the AGA COVID-19 Resource Center at www.gastro.org/COVID.
A version of this article originally appeared on Medscape.com.