User login
Deadly Marburg virus found in West Africa
Marburg virus has been found in fruit bats in Sierra Leone, marking the first appearance of the deadly, Ebola-like virus in West Africa, the Centers for Disease Control and Prevention (CDC) is reporting.
Five Egyptian rousette fruit bats found in three different districts tested positive for infection with Marburg virus, a cousin to Ebola that can cause a hemorrhagic fever with case fatality rates up to 90%, according to CDC.
While no confirmed cases of Marburg infection have been reported in Sierra Leone, the presence of virus in these bats indicates that people nearby may be at risk, according to scientists.
“We have known for a long time that rousette bats, which carry Marburg virus in other parts of Africa, also live in West Africa, so it’s not surprising that we’d find the virus in bats there,” CDC ecologist Jonathan S. Towner, PhD, said in a news release.
The Egyptian rousette bat (Rousettus aegyptiacus) is the natural reservoir for Marburg, shedding the virus in saliva, urine, and feces while feeding on fruit. People and are exposed to the virus when they eat contaminated fruit or capture bats for food, according to the CDC.
The most recent Marburg virus outbreak, which occurred in Uganda in 2017, was the 12th reported outbreak linked to Africa, according to the agency. The largest and deadliest outbreak occurred in 2005 in Angola, infecting 252 people, of whom 90% died.
Testing of the Marburg-positive bats revealed genetically diverse strains, suggesting the virus has been present in Sierra Leone bat colonies for many years, the agency said. Two of the four Marburg virus strains identified in the Sierra Leone bats were genetically similar to the strain implicated in the Angola outbreak.
Egyptian fruit bats are in fact common throughout Africa, living in caves or underground mines. Marburg-positive bats have been found in sub-Saharan Africa, according to researchers, mainly in Uganda and the Democratic Republic of Congo.
Colonies of Egyptian fruit bats can number more than 100,000 animals in eastern and central Africa, while in Sierra Leone, colonies are much smaller, which may explain the lack of Marburg virus disease outbreaks in that country, CDC said.
Discovery of Marburg virus in Sierra Leone was the result of two projects, one led by the CDC and Njala University in Freetown, Sierra Leone, and the other by the University of California, Davis, and the University of Makeni, Sierra Leone, which was funded by the United States Agency for International Development (USAID).
“This discovery is an excellent example of how our work can identify a threat and help us warn people of the risk before they get sick.” Dr. Towner said in the news release.
The two projects began in 2016 after the large Ebola outbreak in West Africa with the aim of identifying the reservoir of Ebola, according to CDC.
SOURCES: U.S. Department of Health and Human Services CDC Newsroom and Centers for Disease Control and Prevention (Marburg Virus).
Marburg virus has been found in fruit bats in Sierra Leone, marking the first appearance of the deadly, Ebola-like virus in West Africa, the Centers for Disease Control and Prevention (CDC) is reporting.
Five Egyptian rousette fruit bats found in three different districts tested positive for infection with Marburg virus, a cousin to Ebola that can cause a hemorrhagic fever with case fatality rates up to 90%, according to CDC.
While no confirmed cases of Marburg infection have been reported in Sierra Leone, the presence of virus in these bats indicates that people nearby may be at risk, according to scientists.
“We have known for a long time that rousette bats, which carry Marburg virus in other parts of Africa, also live in West Africa, so it’s not surprising that we’d find the virus in bats there,” CDC ecologist Jonathan S. Towner, PhD, said in a news release.
The Egyptian rousette bat (Rousettus aegyptiacus) is the natural reservoir for Marburg, shedding the virus in saliva, urine, and feces while feeding on fruit. People and are exposed to the virus when they eat contaminated fruit or capture bats for food, according to the CDC.
The most recent Marburg virus outbreak, which occurred in Uganda in 2017, was the 12th reported outbreak linked to Africa, according to the agency. The largest and deadliest outbreak occurred in 2005 in Angola, infecting 252 people, of whom 90% died.
Testing of the Marburg-positive bats revealed genetically diverse strains, suggesting the virus has been present in Sierra Leone bat colonies for many years, the agency said. Two of the four Marburg virus strains identified in the Sierra Leone bats were genetically similar to the strain implicated in the Angola outbreak.
Egyptian fruit bats are in fact common throughout Africa, living in caves or underground mines. Marburg-positive bats have been found in sub-Saharan Africa, according to researchers, mainly in Uganda and the Democratic Republic of Congo.
Colonies of Egyptian fruit bats can number more than 100,000 animals in eastern and central Africa, while in Sierra Leone, colonies are much smaller, which may explain the lack of Marburg virus disease outbreaks in that country, CDC said.
Discovery of Marburg virus in Sierra Leone was the result of two projects, one led by the CDC and Njala University in Freetown, Sierra Leone, and the other by the University of California, Davis, and the University of Makeni, Sierra Leone, which was funded by the United States Agency for International Development (USAID).
“This discovery is an excellent example of how our work can identify a threat and help us warn people of the risk before they get sick.” Dr. Towner said in the news release.
The two projects began in 2016 after the large Ebola outbreak in West Africa with the aim of identifying the reservoir of Ebola, according to CDC.
SOURCES: U.S. Department of Health and Human Services CDC Newsroom and Centers for Disease Control and Prevention (Marburg Virus).
Marburg virus has been found in fruit bats in Sierra Leone, marking the first appearance of the deadly, Ebola-like virus in West Africa, the Centers for Disease Control and Prevention (CDC) is reporting.
Five Egyptian rousette fruit bats found in three different districts tested positive for infection with Marburg virus, a cousin to Ebola that can cause a hemorrhagic fever with case fatality rates up to 90%, according to CDC.
While no confirmed cases of Marburg infection have been reported in Sierra Leone, the presence of virus in these bats indicates that people nearby may be at risk, according to scientists.
“We have known for a long time that rousette bats, which carry Marburg virus in other parts of Africa, also live in West Africa, so it’s not surprising that we’d find the virus in bats there,” CDC ecologist Jonathan S. Towner, PhD, said in a news release.
The Egyptian rousette bat (Rousettus aegyptiacus) is the natural reservoir for Marburg, shedding the virus in saliva, urine, and feces while feeding on fruit. People and are exposed to the virus when they eat contaminated fruit or capture bats for food, according to the CDC.
The most recent Marburg virus outbreak, which occurred in Uganda in 2017, was the 12th reported outbreak linked to Africa, according to the agency. The largest and deadliest outbreak occurred in 2005 in Angola, infecting 252 people, of whom 90% died.
Testing of the Marburg-positive bats revealed genetically diverse strains, suggesting the virus has been present in Sierra Leone bat colonies for many years, the agency said. Two of the four Marburg virus strains identified in the Sierra Leone bats were genetically similar to the strain implicated in the Angola outbreak.
Egyptian fruit bats are in fact common throughout Africa, living in caves or underground mines. Marburg-positive bats have been found in sub-Saharan Africa, according to researchers, mainly in Uganda and the Democratic Republic of Congo.
Colonies of Egyptian fruit bats can number more than 100,000 animals in eastern and central Africa, while in Sierra Leone, colonies are much smaller, which may explain the lack of Marburg virus disease outbreaks in that country, CDC said.
Discovery of Marburg virus in Sierra Leone was the result of two projects, one led by the CDC and Njala University in Freetown, Sierra Leone, and the other by the University of California, Davis, and the University of Makeni, Sierra Leone, which was funded by the United States Agency for International Development (USAID).
“This discovery is an excellent example of how our work can identify a threat and help us warn people of the risk before they get sick.” Dr. Towner said in the news release.
The two projects began in 2016 after the large Ebola outbreak in West Africa with the aim of identifying the reservoir of Ebola, according to CDC.
SOURCES: U.S. Department of Health and Human Services CDC Newsroom and Centers for Disease Control and Prevention (Marburg Virus).
FROM THE CENTERS FOR DISEASE CONTROL AND PREVENTION
Healthcare.gov activity surged in last week of open enrollment
A surge in activity during the last week of open enrollment at Healthcare.gov more than doubled the number of plans selected for the season, according to the Centers for Medicare & Medicaid Services.
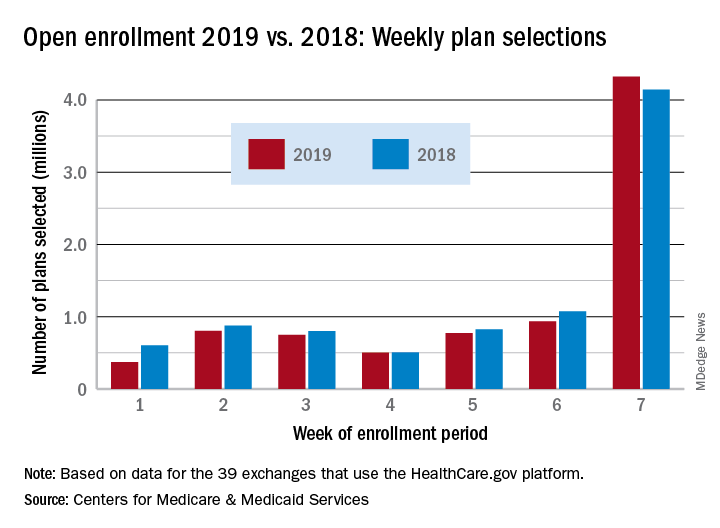
Over 4.32 million plans were selected during week 7 (Dec. 9-15) of enrollment for the 2019 coverage year, exceeding the 4.13 million selected over the previous 6 weeks and bringing the total to 8.45 million, the CMS reported. During week 6 (Dec. 3-9), which was previously the busiest week of the year, 943,000 plans were selected by residents of the 39 states that use the Healthcare.gov platform.
This year’s week 7 total also topped the comparable number from last year’s enrollment period for the first time and closed the gap in cumulative selections from 11.7% after 6 weeks to 4.2%. Last year, a total of 8.82 million plans were selected for the 2018 coverage year, CMS said, while also noting that the data for this year “are preliminary and do not represent final 2019 Exchange Open Enrollment figures.”
CMS Administrator Seema Verma addressed the drop from 2018 to 2019: “With the lowest unemployment rate in 50 years, it’s possible that more Americans have employer based coverage, and don’t need exchange plans.” The CMS also estimated that “approximately 100,000 current exchange enrollees in Virginia will be eligible for” Medicaid now that the state has expanded its Medicaid population.
A surge in activity during the last week of open enrollment at Healthcare.gov more than doubled the number of plans selected for the season, according to the Centers for Medicare & Medicaid Services.
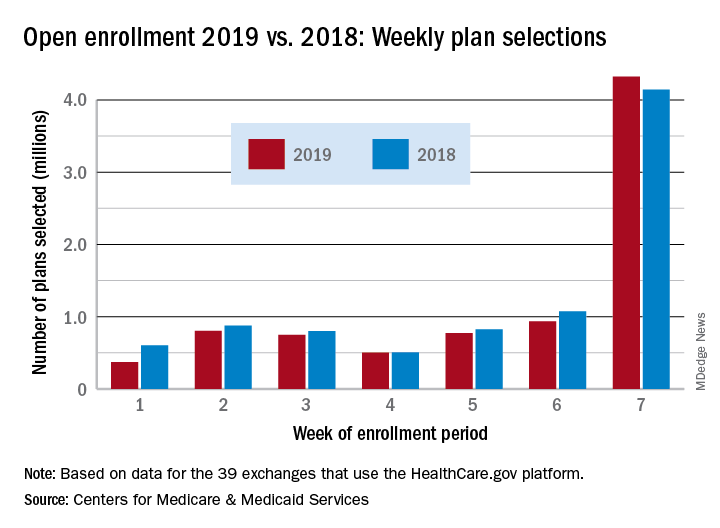
Over 4.32 million plans were selected during week 7 (Dec. 9-15) of enrollment for the 2019 coverage year, exceeding the 4.13 million selected over the previous 6 weeks and bringing the total to 8.45 million, the CMS reported. During week 6 (Dec. 3-9), which was previously the busiest week of the year, 943,000 plans were selected by residents of the 39 states that use the Healthcare.gov platform.
This year’s week 7 total also topped the comparable number from last year’s enrollment period for the first time and closed the gap in cumulative selections from 11.7% after 6 weeks to 4.2%. Last year, a total of 8.82 million plans were selected for the 2018 coverage year, CMS said, while also noting that the data for this year “are preliminary and do not represent final 2019 Exchange Open Enrollment figures.”
CMS Administrator Seema Verma addressed the drop from 2018 to 2019: “With the lowest unemployment rate in 50 years, it’s possible that more Americans have employer based coverage, and don’t need exchange plans.” The CMS also estimated that “approximately 100,000 current exchange enrollees in Virginia will be eligible for” Medicaid now that the state has expanded its Medicaid population.
A surge in activity during the last week of open enrollment at Healthcare.gov more than doubled the number of plans selected for the season, according to the Centers for Medicare & Medicaid Services.
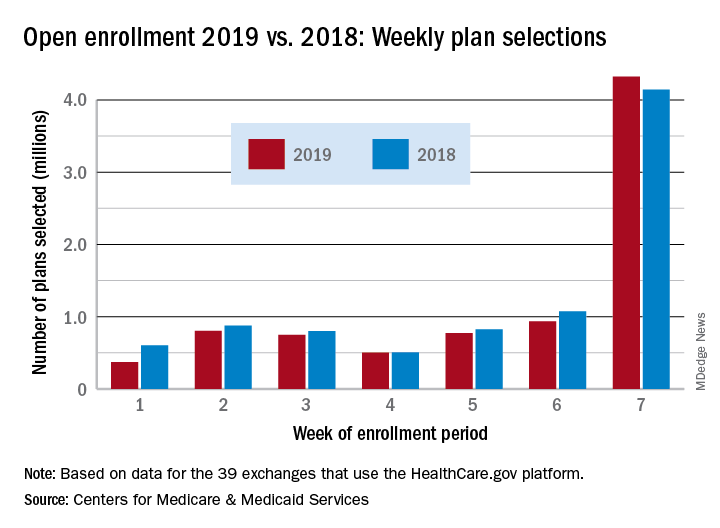
Over 4.32 million plans were selected during week 7 (Dec. 9-15) of enrollment for the 2019 coverage year, exceeding the 4.13 million selected over the previous 6 weeks and bringing the total to 8.45 million, the CMS reported. During week 6 (Dec. 3-9), which was previously the busiest week of the year, 943,000 plans were selected by residents of the 39 states that use the Healthcare.gov platform.
This year’s week 7 total also topped the comparable number from last year’s enrollment period for the first time and closed the gap in cumulative selections from 11.7% after 6 weeks to 4.2%. Last year, a total of 8.82 million plans were selected for the 2018 coverage year, CMS said, while also noting that the data for this year “are preliminary and do not represent final 2019 Exchange Open Enrollment figures.”
CMS Administrator Seema Verma addressed the drop from 2018 to 2019: “With the lowest unemployment rate in 50 years, it’s possible that more Americans have employer based coverage, and don’t need exchange plans.” The CMS also estimated that “approximately 100,000 current exchange enrollees in Virginia will be eligible for” Medicaid now that the state has expanded its Medicaid population.
Next legal ruling on ACA could come on New Year’s Eve
As Democratic governors scramble to appeal a Dec. 14 ruling that essentially struck down the Affordable Care Act, a reprieve keeping the law intact could come by the end of the year.
The ACA remains in effect until Dec. 31 after Judge Reed O’Connor of the U.S. District Court for the Northern District of Texas ruled that the 2017 tax law that zeroed out penalties beginning in 2019 for not carrying health insurance effectively rendered the entire ACA unconstitutional.
On Dec. 17, a group of Democratic attorneys general “asked Judge O’Connor to clarify that his ruling does not presently affect any rights or responsibilities under the ACA until appellate review is complete, or alternatively to stay his ruling,” Timothy S. Jost, emeritus professor at the Washington and Lee School of Law, in Lexington, Va., said during a Dec. 18 press teleconference hosted by the Commonwealth Fund. “They also asked him to certify the case for an immediate appeal and to do so by the end of this week.”
Mr. Jost noted that Judge O’Connor asked the plaintiffs and the U.S. Department of Health & Human Services to respond to this request by Dec. 21.
“I expect him to rule, probably, on New Year’s Eve on what happens next,” Mr. Jost said.
If Judge O’Connor refuses to stay his order, the group of Democratic attorneys general is expected to appeal to the Fifth Circuit Court of Appeals for such a stay, Mr. Jost said. He noted that the Fifth Circuit is one of the more conservative courts – with five Trump administration appointees and five judges appointed by previous Democratic administrations.
In general, Mr. Jost said that he does not expect Judge O’Connor’s ruling to stand.
“The decision is so clearly wrong, however, that I believe there is a good chance that it will be reversed,” he said. “If the Fifth Circuit does, I think it is very unlikely the Supreme Court take the case.” He added that if the Fifth Circuit upholds Judge O’Connor’s ruling, the court would take the case and “very likely reverse at least 5-4 and quite possibly 6-3 on at least the issue of severability.”
Mr. Jost added that he expects the case to drag into 2020 and possibly 2021.
Democrats – with their new majority in the House of Representatives – are likely to intervene legislatively in early in 2019 but are unlikely to be successful at getting the Republican-led Senate to pass “feel-good” legislation that would protect those with preexisting conditions, something Mr. Jost said “cannot be re-created” short of reenacting the entire ACA given the complex processes and subsidies that make coverage of preexisting conditions possible.
Both chambers of Congress could work together on something as simple as reinstating the penalty – even if it were set at just $1 – to coming up with something more comprehensive, but that would be extremely challenging to make happen and to get President Trump to sign off on, he said.
As Democratic governors scramble to appeal a Dec. 14 ruling that essentially struck down the Affordable Care Act, a reprieve keeping the law intact could come by the end of the year.
The ACA remains in effect until Dec. 31 after Judge Reed O’Connor of the U.S. District Court for the Northern District of Texas ruled that the 2017 tax law that zeroed out penalties beginning in 2019 for not carrying health insurance effectively rendered the entire ACA unconstitutional.
On Dec. 17, a group of Democratic attorneys general “asked Judge O’Connor to clarify that his ruling does not presently affect any rights or responsibilities under the ACA until appellate review is complete, or alternatively to stay his ruling,” Timothy S. Jost, emeritus professor at the Washington and Lee School of Law, in Lexington, Va., said during a Dec. 18 press teleconference hosted by the Commonwealth Fund. “They also asked him to certify the case for an immediate appeal and to do so by the end of this week.”
Mr. Jost noted that Judge O’Connor asked the plaintiffs and the U.S. Department of Health & Human Services to respond to this request by Dec. 21.
“I expect him to rule, probably, on New Year’s Eve on what happens next,” Mr. Jost said.
If Judge O’Connor refuses to stay his order, the group of Democratic attorneys general is expected to appeal to the Fifth Circuit Court of Appeals for such a stay, Mr. Jost said. He noted that the Fifth Circuit is one of the more conservative courts – with five Trump administration appointees and five judges appointed by previous Democratic administrations.
In general, Mr. Jost said that he does not expect Judge O’Connor’s ruling to stand.
“The decision is so clearly wrong, however, that I believe there is a good chance that it will be reversed,” he said. “If the Fifth Circuit does, I think it is very unlikely the Supreme Court take the case.” He added that if the Fifth Circuit upholds Judge O’Connor’s ruling, the court would take the case and “very likely reverse at least 5-4 and quite possibly 6-3 on at least the issue of severability.”
Mr. Jost added that he expects the case to drag into 2020 and possibly 2021.
Democrats – with their new majority in the House of Representatives – are likely to intervene legislatively in early in 2019 but are unlikely to be successful at getting the Republican-led Senate to pass “feel-good” legislation that would protect those with preexisting conditions, something Mr. Jost said “cannot be re-created” short of reenacting the entire ACA given the complex processes and subsidies that make coverage of preexisting conditions possible.
Both chambers of Congress could work together on something as simple as reinstating the penalty – even if it were set at just $1 – to coming up with something more comprehensive, but that would be extremely challenging to make happen and to get President Trump to sign off on, he said.
As Democratic governors scramble to appeal a Dec. 14 ruling that essentially struck down the Affordable Care Act, a reprieve keeping the law intact could come by the end of the year.
The ACA remains in effect until Dec. 31 after Judge Reed O’Connor of the U.S. District Court for the Northern District of Texas ruled that the 2017 tax law that zeroed out penalties beginning in 2019 for not carrying health insurance effectively rendered the entire ACA unconstitutional.
On Dec. 17, a group of Democratic attorneys general “asked Judge O’Connor to clarify that his ruling does not presently affect any rights or responsibilities under the ACA until appellate review is complete, or alternatively to stay his ruling,” Timothy S. Jost, emeritus professor at the Washington and Lee School of Law, in Lexington, Va., said during a Dec. 18 press teleconference hosted by the Commonwealth Fund. “They also asked him to certify the case for an immediate appeal and to do so by the end of this week.”
Mr. Jost noted that Judge O’Connor asked the plaintiffs and the U.S. Department of Health & Human Services to respond to this request by Dec. 21.
“I expect him to rule, probably, on New Year’s Eve on what happens next,” Mr. Jost said.
If Judge O’Connor refuses to stay his order, the group of Democratic attorneys general is expected to appeal to the Fifth Circuit Court of Appeals for such a stay, Mr. Jost said. He noted that the Fifth Circuit is one of the more conservative courts – with five Trump administration appointees and five judges appointed by previous Democratic administrations.
In general, Mr. Jost said that he does not expect Judge O’Connor’s ruling to stand.
“The decision is so clearly wrong, however, that I believe there is a good chance that it will be reversed,” he said. “If the Fifth Circuit does, I think it is very unlikely the Supreme Court take the case.” He added that if the Fifth Circuit upholds Judge O’Connor’s ruling, the court would take the case and “very likely reverse at least 5-4 and quite possibly 6-3 on at least the issue of severability.”
Mr. Jost added that he expects the case to drag into 2020 and possibly 2021.
Democrats – with their new majority in the House of Representatives – are likely to intervene legislatively in early in 2019 but are unlikely to be successful at getting the Republican-led Senate to pass “feel-good” legislation that would protect those with preexisting conditions, something Mr. Jost said “cannot be re-created” short of reenacting the entire ACA given the complex processes and subsidies that make coverage of preexisting conditions possible.
Both chambers of Congress could work together on something as simple as reinstating the penalty – even if it were set at just $1 – to coming up with something more comprehensive, but that would be extremely challenging to make happen and to get President Trump to sign off on, he said.
Is an IUD a good contraceptive choice for a never sexually active teen?
Expert Commentary
Data demonstrate efficacy and safety of the IUD in adolescents. In addition, IUDs (particularly the levonorgestrel-containing IUD) have many noncontraceptive benefits. There is still reluctance, however, among clinicians to use IUDs in adolescents. In a sample of fellows of the American College of Obstetricians and Gynecologists, only 43% considered adolescents appropriate candidates for use of an IUD.1
Study details
In this retrospective chart review, Kebodeaux and Schwartz sought to compare successful IUD insertion rates on first attempt in 120 sexually active (SA) and 82 never sexually active (NSA) adolescents. The IUD type used for all women was the 52-mg levonorgestrel IUD (Mirena), except for 3 copper IUDs (Paragard) used in the SA group. The primary indications for IUD use were contraception (85.2%) in the SA group and abnormal uterine bleeding (43.9%) and menstrual suppression (24.4%) in the NSA group.
In the NSA group, 82.9% of adolescents had had some type of prior treatment affecting the menstrual cycle, compared with 60.9% in the SA group (P = .001).
Non–office insertion. Either a sedation unit or operating room was utilized in 5.5% of the IUD insertions in the SA group and 47.6% of the NSA group. Among the 39 adolescents in the NSA group undergoing non–office insertion, 19 (48.7%) had special needs (learning or intellectual disabilities, autism/autism spectrum, or physical disabilities, such as cerebral palsy). Only 1 adolescent with special needs in the NSA group had an office insertion compared with 5 out of 6 in the SA group.
The performance of another procedure other than the IUD insertion (including diagnostic laparoscopy and hymenectomy) was common among adolescents undergoing procedures in the sedation unit or operating room who did not have special needs. It is also important to note that adolescents with special needs were routinely offered insertion under anesthesia while SA adolescents were offered insertion under anesthesia only if they were undergoing another procedure as well.
Study strengths and weaknesses
The study’s strengths include IUD insertions performed at a children’s hospital by providers with experience working with adolescent populations. This likely accounts for the high rates of “tolerance of the procedure well” (93.8% in the SA group vs 81.7% in the NSA group; P = .006). The study also included a patient population—adolescents with special needs—that has not been studied relative to IUD use previously.
A significant weakness of the study, however, is that there are no long-term follow-up data, particularly related to continuation rates.
These study findings provides further support to combat the myth that adolescents, particularly if nulliparous or not sexually active, are not suitable candidates for IUD use. However, if they have never been sexually active or have special needs, IUD insertion under sedation or in an operating room may be necessary. It is also likely that selection of the IUD as an option by an adolescent and overall tolerance of the insertion procedure requires providers with experience in caring for adolescents as well as providers possessing good counseling skills.
—Ronald T. Burkman, MD
1. Luchowski AT, Anderson BL, Power ML, Reglan GB, Espey E, Shulkin J. Obstetrician-gynecologists and contraception: practice and opinions about the use of IUDs in nulliparous women, adolescents and other patient populations. Contraception. 2014;89:572-577.
Expert Commentary
Data demonstrate efficacy and safety of the IUD in adolescents. In addition, IUDs (particularly the levonorgestrel-containing IUD) have many noncontraceptive benefits. There is still reluctance, however, among clinicians to use IUDs in adolescents. In a sample of fellows of the American College of Obstetricians and Gynecologists, only 43% considered adolescents appropriate candidates for use of an IUD.1
Study details
In this retrospective chart review, Kebodeaux and Schwartz sought to compare successful IUD insertion rates on first attempt in 120 sexually active (SA) and 82 never sexually active (NSA) adolescents. The IUD type used for all women was the 52-mg levonorgestrel IUD (Mirena), except for 3 copper IUDs (Paragard) used in the SA group. The primary indications for IUD use were contraception (85.2%) in the SA group and abnormal uterine bleeding (43.9%) and menstrual suppression (24.4%) in the NSA group.
In the NSA group, 82.9% of adolescents had had some type of prior treatment affecting the menstrual cycle, compared with 60.9% in the SA group (P = .001).
Non–office insertion. Either a sedation unit or operating room was utilized in 5.5% of the IUD insertions in the SA group and 47.6% of the NSA group. Among the 39 adolescents in the NSA group undergoing non–office insertion, 19 (48.7%) had special needs (learning or intellectual disabilities, autism/autism spectrum, or physical disabilities, such as cerebral palsy). Only 1 adolescent with special needs in the NSA group had an office insertion compared with 5 out of 6 in the SA group.
The performance of another procedure other than the IUD insertion (including diagnostic laparoscopy and hymenectomy) was common among adolescents undergoing procedures in the sedation unit or operating room who did not have special needs. It is also important to note that adolescents with special needs were routinely offered insertion under anesthesia while SA adolescents were offered insertion under anesthesia only if they were undergoing another procedure as well.
Study strengths and weaknesses
The study’s strengths include IUD insertions performed at a children’s hospital by providers with experience working with adolescent populations. This likely accounts for the high rates of “tolerance of the procedure well” (93.8% in the SA group vs 81.7% in the NSA group; P = .006). The study also included a patient population—adolescents with special needs—that has not been studied relative to IUD use previously.
A significant weakness of the study, however, is that there are no long-term follow-up data, particularly related to continuation rates.
These study findings provides further support to combat the myth that adolescents, particularly if nulliparous or not sexually active, are not suitable candidates for IUD use. However, if they have never been sexually active or have special needs, IUD insertion under sedation or in an operating room may be necessary. It is also likely that selection of the IUD as an option by an adolescent and overall tolerance of the insertion procedure requires providers with experience in caring for adolescents as well as providers possessing good counseling skills.
—Ronald T. Burkman, MD
Expert Commentary
Data demonstrate efficacy and safety of the IUD in adolescents. In addition, IUDs (particularly the levonorgestrel-containing IUD) have many noncontraceptive benefits. There is still reluctance, however, among clinicians to use IUDs in adolescents. In a sample of fellows of the American College of Obstetricians and Gynecologists, only 43% considered adolescents appropriate candidates for use of an IUD.1
Study details
In this retrospective chart review, Kebodeaux and Schwartz sought to compare successful IUD insertion rates on first attempt in 120 sexually active (SA) and 82 never sexually active (NSA) adolescents. The IUD type used for all women was the 52-mg levonorgestrel IUD (Mirena), except for 3 copper IUDs (Paragard) used in the SA group. The primary indications for IUD use were contraception (85.2%) in the SA group and abnormal uterine bleeding (43.9%) and menstrual suppression (24.4%) in the NSA group.
In the NSA group, 82.9% of adolescents had had some type of prior treatment affecting the menstrual cycle, compared with 60.9% in the SA group (P = .001).
Non–office insertion. Either a sedation unit or operating room was utilized in 5.5% of the IUD insertions in the SA group and 47.6% of the NSA group. Among the 39 adolescents in the NSA group undergoing non–office insertion, 19 (48.7%) had special needs (learning or intellectual disabilities, autism/autism spectrum, or physical disabilities, such as cerebral palsy). Only 1 adolescent with special needs in the NSA group had an office insertion compared with 5 out of 6 in the SA group.
The performance of another procedure other than the IUD insertion (including diagnostic laparoscopy and hymenectomy) was common among adolescents undergoing procedures in the sedation unit or operating room who did not have special needs. It is also important to note that adolescents with special needs were routinely offered insertion under anesthesia while SA adolescents were offered insertion under anesthesia only if they were undergoing another procedure as well.
Study strengths and weaknesses
The study’s strengths include IUD insertions performed at a children’s hospital by providers with experience working with adolescent populations. This likely accounts for the high rates of “tolerance of the procedure well” (93.8% in the SA group vs 81.7% in the NSA group; P = .006). The study also included a patient population—adolescents with special needs—that has not been studied relative to IUD use previously.
A significant weakness of the study, however, is that there are no long-term follow-up data, particularly related to continuation rates.
These study findings provides further support to combat the myth that adolescents, particularly if nulliparous or not sexually active, are not suitable candidates for IUD use. However, if they have never been sexually active or have special needs, IUD insertion under sedation or in an operating room may be necessary. It is also likely that selection of the IUD as an option by an adolescent and overall tolerance of the insertion procedure requires providers with experience in caring for adolescents as well as providers possessing good counseling skills.
—Ronald T. Burkman, MD
1. Luchowski AT, Anderson BL, Power ML, Reglan GB, Espey E, Shulkin J. Obstetrician-gynecologists and contraception: practice and opinions about the use of IUDs in nulliparous women, adolescents and other patient populations. Contraception. 2014;89:572-577.
1. Luchowski AT, Anderson BL, Power ML, Reglan GB, Espey E, Shulkin J. Obstetrician-gynecologists and contraception: practice and opinions about the use of IUDs in nulliparous women, adolescents and other patient populations. Contraception. 2014;89:572-577.
Hippocampal abnormalities seen in epilepsy subtypes may be congenital
NEW ORLEANS – , although to a lesser extent, based on findings from two studies presented at the annual meeting of the American Epilepsy Society.
While the studies suggest an imaging endophenotype associated with these disorders, it’s unclear if a larger degree of abnormality causes disease manifestation, or whether there are other predisposing actors at work.
“What our study tells us is that hippocampal abnormalities can occur in the absence of seizure,” Marian Galovic, MD, said in an interview. “It may be that, in some cases, hippocampal abnormalities could be the cause, rather than the consequence, of seizures.”
Dr. Galovic of University College London was on hand to discuss the work of his colleague, Lili Long, MD, PhD, of the Xiangya Hospital of Central South University, Changsha, China. Visa issues prevented her from attending the meeting.
The study included 18 sibling pairs in which the affected siblings had sporadic, nonlesional temporal lobe epilepsy (TLE), involving the right lobe in 12 and the left in 6. The patients, siblings, and 18 healthy, age-matched controls underwent clinical, electrophysiologic, and high-resolution structural neuroimaging.
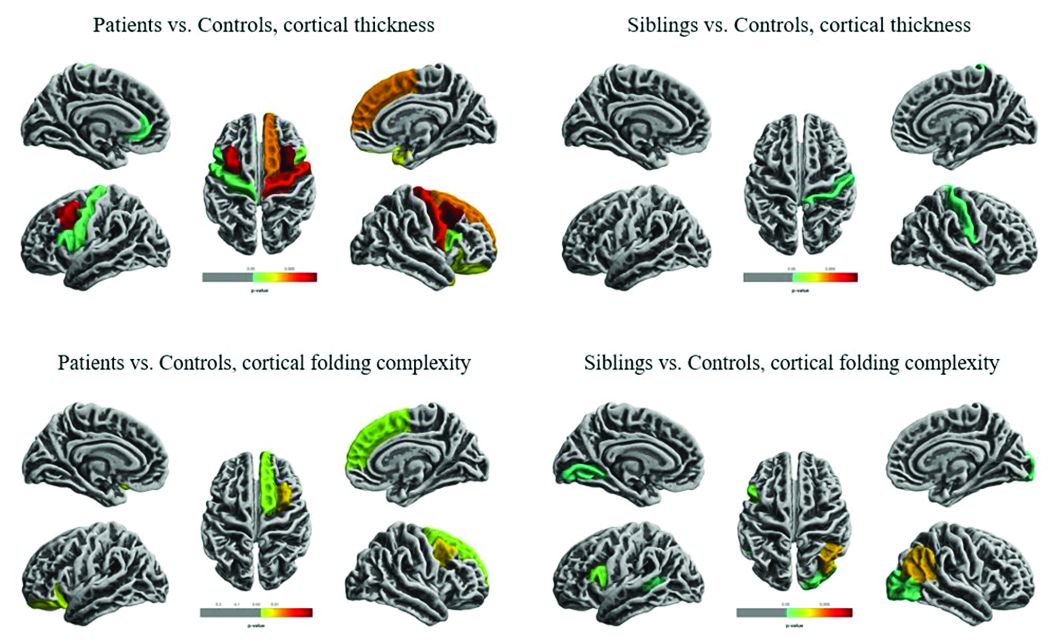
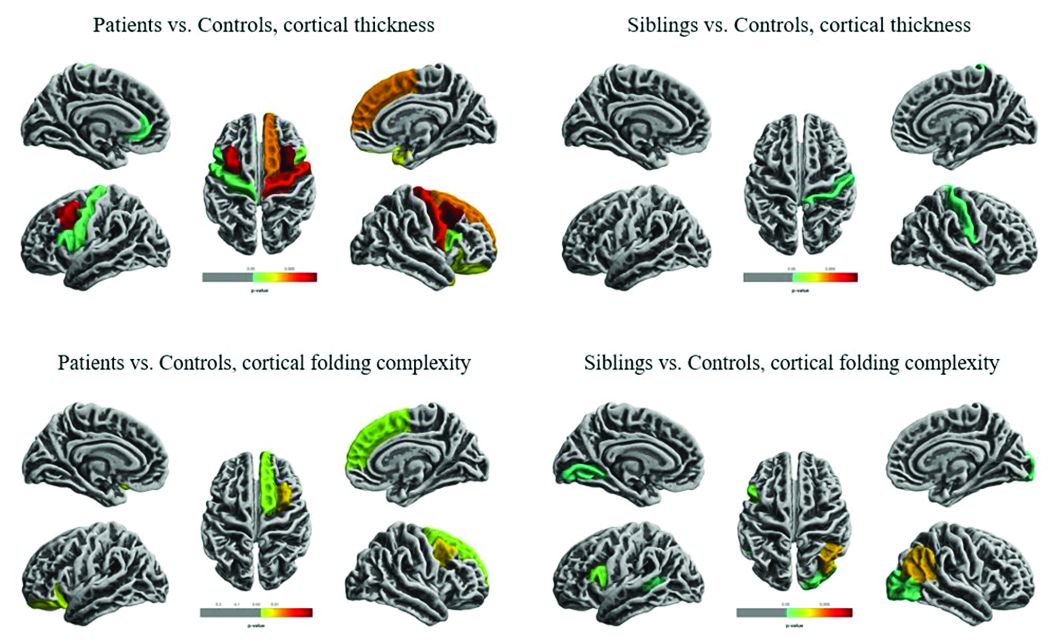
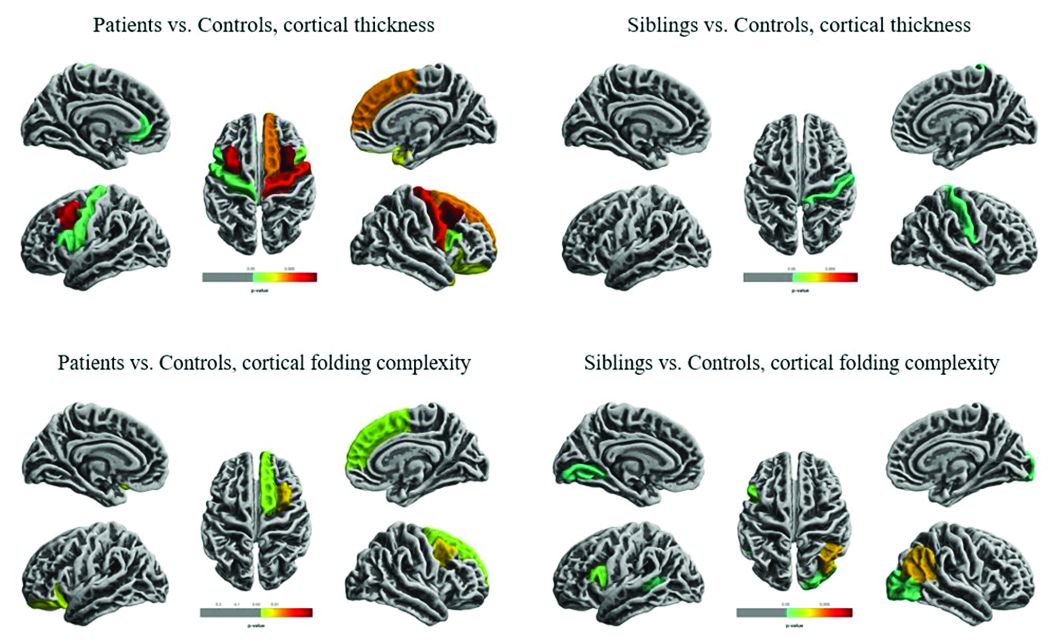
The researchers compared overall hippocampal volumes between groups and determined the subregional extent of hippocampal abnormalities using shape analysis. They also looked at whole-brain differences in cortical thickness and folding complexity.
As expected, median hippocampal volumes were largest in the healthy controls (left = 2.82 mL, right = 2.94 mL), and smallest in patients. Patients with left TLE had a median left hippocampal volume of 2.23 mL, while those with right TLE had a median right hippocampal volume of 1.92 mL.
However, volume in the unaffected siblings was a surprise. Like the patients, these subjects also had significant reductions in hippocampal volume when compared with controls (left = 2.47 mL, right = 2.65 mL). “The atrophy was relatively similar in siblings and patients, although not as pronounced in siblings,” Dr. Galovic said. “It was mostly unilateral in the siblings and bilateral in the patients, but it was still more pronounced on the side where the epilepsy of the affected sibling was coming from.”
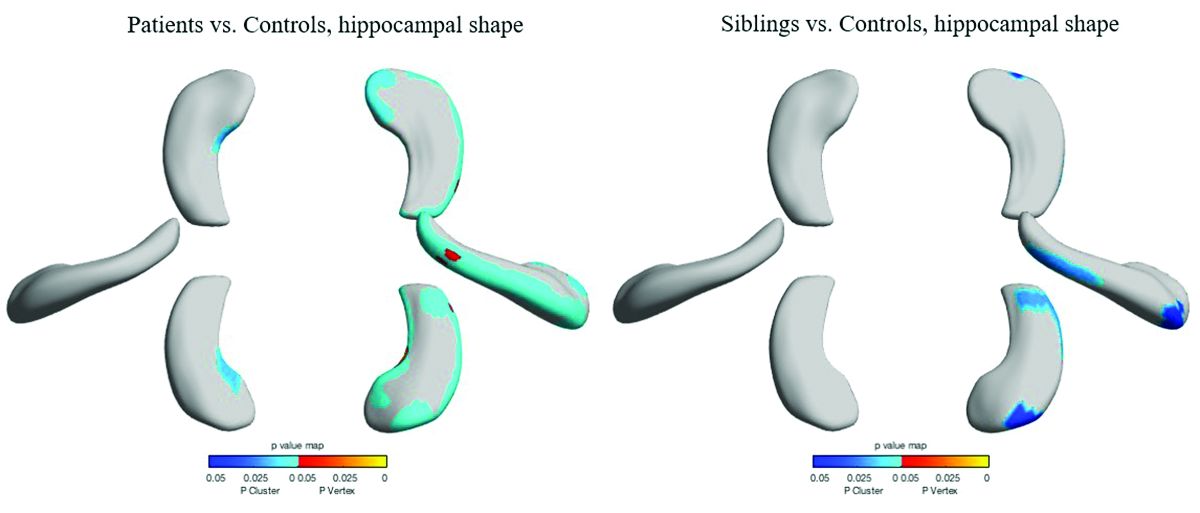
Patients and siblings also shared morphologic variations of the hippocampus, with atrophy more pronounced on the right than the left. The right lateral body and anterior head of the hippocampus were most affected, Dr. Galovic said, with reductions in the right cornu ammonis 1 subfield and subiculum.
Widespread cortical thinning was present in patients, including the pericentral, frontal, and temporal areas. Unaffected siblings also showed cortical thinning, but this was mostly restricted to the right postcentral gyrus. Patients and siblings also demonstrated increased cortical folding complexity, but in different areas: predominantly frontal in patients, but predominantly parieto-occipital in siblings. Both were significantly different than healthy control subjects.
The study didn’t examine any association with memory, which is often impaired in patients with TLE. However, Dr. Galovic said, “We have just submitted for publication a study in which we did find an association between focal hippocampal atrophy and memory performance.”
A different study by a team at University College London looked at hippocampal structure and function in patients with juvenile myoclonic epilepsy (JME) and their unaffected siblings. The imaging study, lead by Lorenzo Caciagli, MD, of the university comprised 37 patients with JME, 16 unaffected siblings, and 20 healthy controls. It employed multimodal MRI and neuropsychological measures to examine the form and function of the mesiotemporal lobe.
The subjects were matched for age, sex, handedness, and hemispheric dominance, which was assessed with language lateralization indices. This measures the number of active voxels on functional MRI, showing which hemisphere is dominant for language.
Both patients and their siblings showed reductions in left hippocampal volume on the order of 5%-8%, significantly smaller than the volumes seen in healthy controls. About half of patients and half of siblings also showed either unilateral or bilateral hippocampal malrotation. This was present in just 15% of controls, another significant difference. The structural differences weren’t associated with seizure control or age at disease onset, or with any impairments in verbal or visual memory. But when the investigators performed functional mapping, they found unusual patterns of hippocampal activation in both patients and siblings, pointing to a dysfunction of verbal encoding. In patients, there appeared to be distinct patterns of underactivation along the hippocampal long axis, regardless of whether malrotation was present. But among patients who had malrotation, the left posterior hippocampus showed more activation during visual memory.
The team concluded that the hippocampal abnormalities in volume, shape, and positioning in patients with JME and their siblings are related to functional reorganization. The abnormalities probably occur during prenatal neurodevelopment, they noted.
“Cosegregation of imaging patterns in patients and their siblings is suggestive of genetic imaging phenotypes, and independent of disease activity,” Dr. Caciagli and his coinvestigators wrote in their abstract.
Funding for the TLE study came from the National Natural Science Foundation of China, the Ministry of Science and Technology of China, and Xiangya Hospital. Funding for the JME study came from a variety of U.K. charities and government agencies.
SOURCES: Long L et al. AES 2018, Abstract 2.183; Caciagli L et al. AES 2018, Abstract 2.166.
NEW ORLEANS – , although to a lesser extent, based on findings from two studies presented at the annual meeting of the American Epilepsy Society.
While the studies suggest an imaging endophenotype associated with these disorders, it’s unclear if a larger degree of abnormality causes disease manifestation, or whether there are other predisposing actors at work.
“What our study tells us is that hippocampal abnormalities can occur in the absence of seizure,” Marian Galovic, MD, said in an interview. “It may be that, in some cases, hippocampal abnormalities could be the cause, rather than the consequence, of seizures.”
Dr. Galovic of University College London was on hand to discuss the work of his colleague, Lili Long, MD, PhD, of the Xiangya Hospital of Central South University, Changsha, China. Visa issues prevented her from attending the meeting.
The study included 18 sibling pairs in which the affected siblings had sporadic, nonlesional temporal lobe epilepsy (TLE), involving the right lobe in 12 and the left in 6. The patients, siblings, and 18 healthy, age-matched controls underwent clinical, electrophysiologic, and high-resolution structural neuroimaging.
The researchers compared overall hippocampal volumes between groups and determined the subregional extent of hippocampal abnormalities using shape analysis. They also looked at whole-brain differences in cortical thickness and folding complexity.
As expected, median hippocampal volumes were largest in the healthy controls (left = 2.82 mL, right = 2.94 mL), and smallest in patients. Patients with left TLE had a median left hippocampal volume of 2.23 mL, while those with right TLE had a median right hippocampal volume of 1.92 mL.
However, volume in the unaffected siblings was a surprise. Like the patients, these subjects also had significant reductions in hippocampal volume when compared with controls (left = 2.47 mL, right = 2.65 mL). “The atrophy was relatively similar in siblings and patients, although not as pronounced in siblings,” Dr. Galovic said. “It was mostly unilateral in the siblings and bilateral in the patients, but it was still more pronounced on the side where the epilepsy of the affected sibling was coming from.”
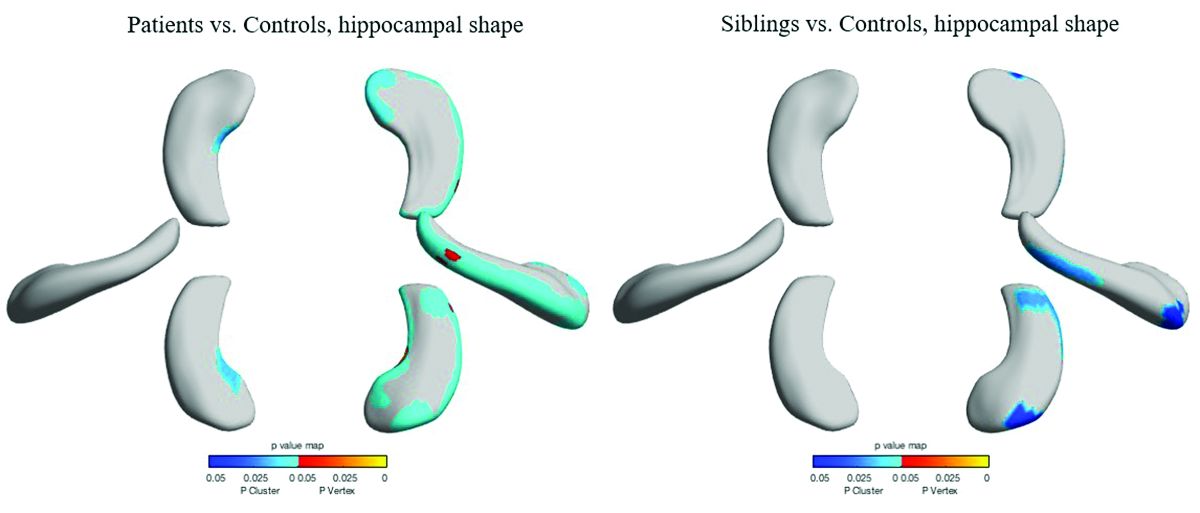
Patients and siblings also shared morphologic variations of the hippocampus, with atrophy more pronounced on the right than the left. The right lateral body and anterior head of the hippocampus were most affected, Dr. Galovic said, with reductions in the right cornu ammonis 1 subfield and subiculum.
Widespread cortical thinning was present in patients, including the pericentral, frontal, and temporal areas. Unaffected siblings also showed cortical thinning, but this was mostly restricted to the right postcentral gyrus. Patients and siblings also demonstrated increased cortical folding complexity, but in different areas: predominantly frontal in patients, but predominantly parieto-occipital in siblings. Both were significantly different than healthy control subjects.
The study didn’t examine any association with memory, which is often impaired in patients with TLE. However, Dr. Galovic said, “We have just submitted for publication a study in which we did find an association between focal hippocampal atrophy and memory performance.”
A different study by a team at University College London looked at hippocampal structure and function in patients with juvenile myoclonic epilepsy (JME) and their unaffected siblings. The imaging study, lead by Lorenzo Caciagli, MD, of the university comprised 37 patients with JME, 16 unaffected siblings, and 20 healthy controls. It employed multimodal MRI and neuropsychological measures to examine the form and function of the mesiotemporal lobe.
The subjects were matched for age, sex, handedness, and hemispheric dominance, which was assessed with language lateralization indices. This measures the number of active voxels on functional MRI, showing which hemisphere is dominant for language.
Both patients and their siblings showed reductions in left hippocampal volume on the order of 5%-8%, significantly smaller than the volumes seen in healthy controls. About half of patients and half of siblings also showed either unilateral or bilateral hippocampal malrotation. This was present in just 15% of controls, another significant difference. The structural differences weren’t associated with seizure control or age at disease onset, or with any impairments in verbal or visual memory. But when the investigators performed functional mapping, they found unusual patterns of hippocampal activation in both patients and siblings, pointing to a dysfunction of verbal encoding. In patients, there appeared to be distinct patterns of underactivation along the hippocampal long axis, regardless of whether malrotation was present. But among patients who had malrotation, the left posterior hippocampus showed more activation during visual memory.
The team concluded that the hippocampal abnormalities in volume, shape, and positioning in patients with JME and their siblings are related to functional reorganization. The abnormalities probably occur during prenatal neurodevelopment, they noted.
“Cosegregation of imaging patterns in patients and their siblings is suggestive of genetic imaging phenotypes, and independent of disease activity,” Dr. Caciagli and his coinvestigators wrote in their abstract.
Funding for the TLE study came from the National Natural Science Foundation of China, the Ministry of Science and Technology of China, and Xiangya Hospital. Funding for the JME study came from a variety of U.K. charities and government agencies.
SOURCES: Long L et al. AES 2018, Abstract 2.183; Caciagli L et al. AES 2018, Abstract 2.166.
NEW ORLEANS – , although to a lesser extent, based on findings from two studies presented at the annual meeting of the American Epilepsy Society.
While the studies suggest an imaging endophenotype associated with these disorders, it’s unclear if a larger degree of abnormality causes disease manifestation, or whether there are other predisposing actors at work.
“What our study tells us is that hippocampal abnormalities can occur in the absence of seizure,” Marian Galovic, MD, said in an interview. “It may be that, in some cases, hippocampal abnormalities could be the cause, rather than the consequence, of seizures.”
Dr. Galovic of University College London was on hand to discuss the work of his colleague, Lili Long, MD, PhD, of the Xiangya Hospital of Central South University, Changsha, China. Visa issues prevented her from attending the meeting.
The study included 18 sibling pairs in which the affected siblings had sporadic, nonlesional temporal lobe epilepsy (TLE), involving the right lobe in 12 and the left in 6. The patients, siblings, and 18 healthy, age-matched controls underwent clinical, electrophysiologic, and high-resolution structural neuroimaging.
The researchers compared overall hippocampal volumes between groups and determined the subregional extent of hippocampal abnormalities using shape analysis. They also looked at whole-brain differences in cortical thickness and folding complexity.
As expected, median hippocampal volumes were largest in the healthy controls (left = 2.82 mL, right = 2.94 mL), and smallest in patients. Patients with left TLE had a median left hippocampal volume of 2.23 mL, while those with right TLE had a median right hippocampal volume of 1.92 mL.
However, volume in the unaffected siblings was a surprise. Like the patients, these subjects also had significant reductions in hippocampal volume when compared with controls (left = 2.47 mL, right = 2.65 mL). “The atrophy was relatively similar in siblings and patients, although not as pronounced in siblings,” Dr. Galovic said. “It was mostly unilateral in the siblings and bilateral in the patients, but it was still more pronounced on the side where the epilepsy of the affected sibling was coming from.”
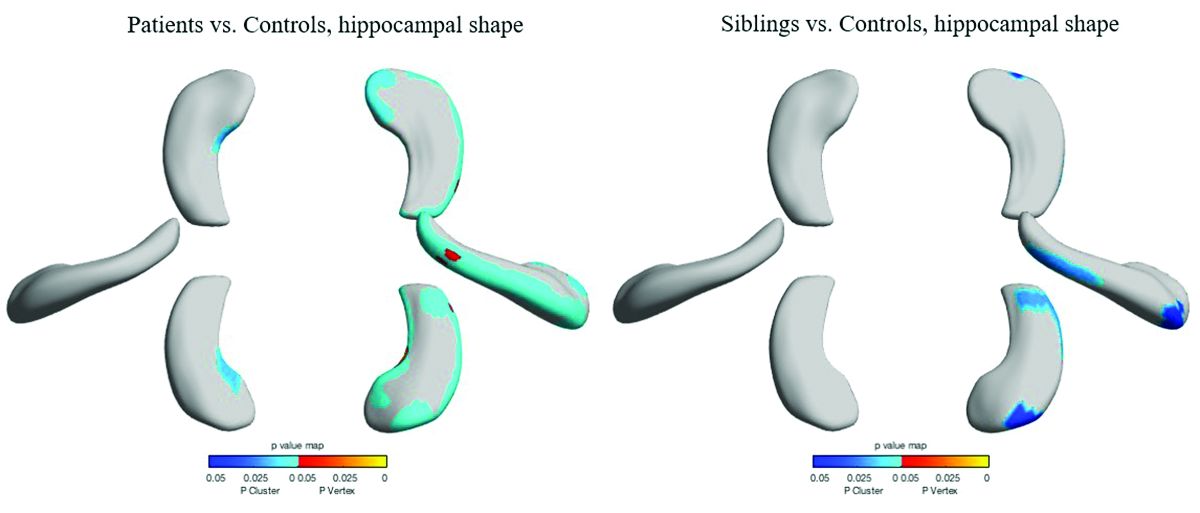
Patients and siblings also shared morphologic variations of the hippocampus, with atrophy more pronounced on the right than the left. The right lateral body and anterior head of the hippocampus were most affected, Dr. Galovic said, with reductions in the right cornu ammonis 1 subfield and subiculum.
Widespread cortical thinning was present in patients, including the pericentral, frontal, and temporal areas. Unaffected siblings also showed cortical thinning, but this was mostly restricted to the right postcentral gyrus. Patients and siblings also demonstrated increased cortical folding complexity, but in different areas: predominantly frontal in patients, but predominantly parieto-occipital in siblings. Both were significantly different than healthy control subjects.
The study didn’t examine any association with memory, which is often impaired in patients with TLE. However, Dr. Galovic said, “We have just submitted for publication a study in which we did find an association between focal hippocampal atrophy and memory performance.”
A different study by a team at University College London looked at hippocampal structure and function in patients with juvenile myoclonic epilepsy (JME) and their unaffected siblings. The imaging study, lead by Lorenzo Caciagli, MD, of the university comprised 37 patients with JME, 16 unaffected siblings, and 20 healthy controls. It employed multimodal MRI and neuropsychological measures to examine the form and function of the mesiotemporal lobe.
The subjects were matched for age, sex, handedness, and hemispheric dominance, which was assessed with language lateralization indices. This measures the number of active voxels on functional MRI, showing which hemisphere is dominant for language.
Both patients and their siblings showed reductions in left hippocampal volume on the order of 5%-8%, significantly smaller than the volumes seen in healthy controls. About half of patients and half of siblings also showed either unilateral or bilateral hippocampal malrotation. This was present in just 15% of controls, another significant difference. The structural differences weren’t associated with seizure control or age at disease onset, or with any impairments in verbal or visual memory. But when the investigators performed functional mapping, they found unusual patterns of hippocampal activation in both patients and siblings, pointing to a dysfunction of verbal encoding. In patients, there appeared to be distinct patterns of underactivation along the hippocampal long axis, regardless of whether malrotation was present. But among patients who had malrotation, the left posterior hippocampus showed more activation during visual memory.
The team concluded that the hippocampal abnormalities in volume, shape, and positioning in patients with JME and their siblings are related to functional reorganization. The abnormalities probably occur during prenatal neurodevelopment, they noted.
“Cosegregation of imaging patterns in patients and their siblings is suggestive of genetic imaging phenotypes, and independent of disease activity,” Dr. Caciagli and his coinvestigators wrote in their abstract.
Funding for the TLE study came from the National Natural Science Foundation of China, the Ministry of Science and Technology of China, and Xiangya Hospital. Funding for the JME study came from a variety of U.K. charities and government agencies.
SOURCES: Long L et al. AES 2018, Abstract 2.183; Caciagli L et al. AES 2018, Abstract 2.166.
REPORTING FROM AES 2018
ECHELON-2: BV-CHP boosts survival in PTCL
SAN DIEGO – A newly approved treatment regimen provides a survival benefit over standard therapy for patients with CD30-positive peripheral T-cell lymphomas (PTCLs), according to new research presented at the annual meeting of the American Society of Hematology.
In the ECHELON-2 trial, patients who received brentuximab vedotin (BV) plus cyclophosphamide, doxorubicin, and prednisone (CHP) had superior progression-free survival (PFS) and overall survival (OS), compared with patients who received standard treatment with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).
These results supported the recent U.S. approval of BV in combination with CHP for adults with previously untreated, systemic anaplastic large cell lymphoma or other CD30-expressing PTCLs.
“ECHELON-2 is the first prospective trial in peripheral T-cell lymphoma to show an overall survival benefit over CHOP,” said Steven M. Horwitz, MD, of Memorial Sloan Kettering Cancer Center, with locations in New York and New Jersey.
Dr. Horwitz presented data from this trial at the ASH meeting. Results were simultaneously published in the Lancet (2018 Dec 3. doi: 10.1016/S0140-6736[18]32984-2).
ECHELON-2 (NCT01777152) enrolled 452 patients with previously untreated, CD30-positive PTCL. Subtypes included ALK-positive or ALK-negative systemic anaplastic large-cell lymphoma, PTCL not otherwise specified, angioimmunoblastic T-cell lymphoma, enteropathy-associated T-cell lymphoma, and adult T-cell leukemia/lymphoma.
Patients were randomized to receive BV-CHP plus placebo (n = 226) or CHOP plus placebo (n = 226) every 3 weeks for six to eight cycles.
At baseline, the median age was 58 in the BV-CHP arm and the CHOP arm. The majority of patients were male – 59% in the BV-CHP arm and 67% in the CHOP arm – and most patients had stage III/IV disease, 81% and 80%, respectively.
In all, 89% of patients in the BV-CHP arm and 81% in the CHOP arm completed six or more cycles of their assigned treatment.
The overall response rate was 83% in the BV-CHP arm and 72% in the CHOP arm (P = .0032). The complete response rates were 68% and 56%, respectively (P = .0066).
At a median follow-up of 36.2 months, the median PFS was 48.2 months in the BV-CHP arm and 20.8 months in the CHOP arm. The rate of death or progression was 42% in the BV-CHP arm and 55% in the CHOP arm (hazard ratio = 0.71, P = .011).
At a median follow-up of 42.1 months, the median OS was not reached in either treatment arm. The rate of death was 23% in the BV-CHP arm and 32% in the CHOP arm (HR = 0.66, P = .0244).
Dr. Horwitz noted that this study was not powered to determine differences in PFS or OS by PTCL subtypes.
BV-CHP had a safety profile comparable with that of CHOP, Dr. Horwitz said.
The rate of adverse events (AEs) was 99% in the BV-CHP arm and 98% in the CHOP arm. Grade 3 or higher AEs occurred in 66% and 65% of patients, respectively. Serious AEs occurred in 39% and 38%, respectively.
Three percent of patients in the BV-CHP arm and 4% of those in the CHOP arm had fatal AEs.
The study was funded by Seattle Genetics, Millennium Pharmaceuticals, and the National Institutes of Health. Dr. Horwitz reported relationships with Seattle Genetics, Millennium Pharmaceuticals, and other companies.
SOURCE: Horwitz S et al. ASH 2018, Abstract 997.
SAN DIEGO – A newly approved treatment regimen provides a survival benefit over standard therapy for patients with CD30-positive peripheral T-cell lymphomas (PTCLs), according to new research presented at the annual meeting of the American Society of Hematology.
In the ECHELON-2 trial, patients who received brentuximab vedotin (BV) plus cyclophosphamide, doxorubicin, and prednisone (CHP) had superior progression-free survival (PFS) and overall survival (OS), compared with patients who received standard treatment with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).
These results supported the recent U.S. approval of BV in combination with CHP for adults with previously untreated, systemic anaplastic large cell lymphoma or other CD30-expressing PTCLs.
“ECHELON-2 is the first prospective trial in peripheral T-cell lymphoma to show an overall survival benefit over CHOP,” said Steven M. Horwitz, MD, of Memorial Sloan Kettering Cancer Center, with locations in New York and New Jersey.
Dr. Horwitz presented data from this trial at the ASH meeting. Results were simultaneously published in the Lancet (2018 Dec 3. doi: 10.1016/S0140-6736[18]32984-2).
ECHELON-2 (NCT01777152) enrolled 452 patients with previously untreated, CD30-positive PTCL. Subtypes included ALK-positive or ALK-negative systemic anaplastic large-cell lymphoma, PTCL not otherwise specified, angioimmunoblastic T-cell lymphoma, enteropathy-associated T-cell lymphoma, and adult T-cell leukemia/lymphoma.
Patients were randomized to receive BV-CHP plus placebo (n = 226) or CHOP plus placebo (n = 226) every 3 weeks for six to eight cycles.
At baseline, the median age was 58 in the BV-CHP arm and the CHOP arm. The majority of patients were male – 59% in the BV-CHP arm and 67% in the CHOP arm – and most patients had stage III/IV disease, 81% and 80%, respectively.
In all, 89% of patients in the BV-CHP arm and 81% in the CHOP arm completed six or more cycles of their assigned treatment.
The overall response rate was 83% in the BV-CHP arm and 72% in the CHOP arm (P = .0032). The complete response rates were 68% and 56%, respectively (P = .0066).
At a median follow-up of 36.2 months, the median PFS was 48.2 months in the BV-CHP arm and 20.8 months in the CHOP arm. The rate of death or progression was 42% in the BV-CHP arm and 55% in the CHOP arm (hazard ratio = 0.71, P = .011).
At a median follow-up of 42.1 months, the median OS was not reached in either treatment arm. The rate of death was 23% in the BV-CHP arm and 32% in the CHOP arm (HR = 0.66, P = .0244).
Dr. Horwitz noted that this study was not powered to determine differences in PFS or OS by PTCL subtypes.
BV-CHP had a safety profile comparable with that of CHOP, Dr. Horwitz said.
The rate of adverse events (AEs) was 99% in the BV-CHP arm and 98% in the CHOP arm. Grade 3 or higher AEs occurred in 66% and 65% of patients, respectively. Serious AEs occurred in 39% and 38%, respectively.
Three percent of patients in the BV-CHP arm and 4% of those in the CHOP arm had fatal AEs.
The study was funded by Seattle Genetics, Millennium Pharmaceuticals, and the National Institutes of Health. Dr. Horwitz reported relationships with Seattle Genetics, Millennium Pharmaceuticals, and other companies.
SOURCE: Horwitz S et al. ASH 2018, Abstract 997.
SAN DIEGO – A newly approved treatment regimen provides a survival benefit over standard therapy for patients with CD30-positive peripheral T-cell lymphomas (PTCLs), according to new research presented at the annual meeting of the American Society of Hematology.
In the ECHELON-2 trial, patients who received brentuximab vedotin (BV) plus cyclophosphamide, doxorubicin, and prednisone (CHP) had superior progression-free survival (PFS) and overall survival (OS), compared with patients who received standard treatment with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).
These results supported the recent U.S. approval of BV in combination with CHP for adults with previously untreated, systemic anaplastic large cell lymphoma or other CD30-expressing PTCLs.
“ECHELON-2 is the first prospective trial in peripheral T-cell lymphoma to show an overall survival benefit over CHOP,” said Steven M. Horwitz, MD, of Memorial Sloan Kettering Cancer Center, with locations in New York and New Jersey.
Dr. Horwitz presented data from this trial at the ASH meeting. Results were simultaneously published in the Lancet (2018 Dec 3. doi: 10.1016/S0140-6736[18]32984-2).
ECHELON-2 (NCT01777152) enrolled 452 patients with previously untreated, CD30-positive PTCL. Subtypes included ALK-positive or ALK-negative systemic anaplastic large-cell lymphoma, PTCL not otherwise specified, angioimmunoblastic T-cell lymphoma, enteropathy-associated T-cell lymphoma, and adult T-cell leukemia/lymphoma.
Patients were randomized to receive BV-CHP plus placebo (n = 226) or CHOP plus placebo (n = 226) every 3 weeks for six to eight cycles.
At baseline, the median age was 58 in the BV-CHP arm and the CHOP arm. The majority of patients were male – 59% in the BV-CHP arm and 67% in the CHOP arm – and most patients had stage III/IV disease, 81% and 80%, respectively.
In all, 89% of patients in the BV-CHP arm and 81% in the CHOP arm completed six or more cycles of their assigned treatment.
The overall response rate was 83% in the BV-CHP arm and 72% in the CHOP arm (P = .0032). The complete response rates were 68% and 56%, respectively (P = .0066).
At a median follow-up of 36.2 months, the median PFS was 48.2 months in the BV-CHP arm and 20.8 months in the CHOP arm. The rate of death or progression was 42% in the BV-CHP arm and 55% in the CHOP arm (hazard ratio = 0.71, P = .011).
At a median follow-up of 42.1 months, the median OS was not reached in either treatment arm. The rate of death was 23% in the BV-CHP arm and 32% in the CHOP arm (HR = 0.66, P = .0244).
Dr. Horwitz noted that this study was not powered to determine differences in PFS or OS by PTCL subtypes.
BV-CHP had a safety profile comparable with that of CHOP, Dr. Horwitz said.
The rate of adverse events (AEs) was 99% in the BV-CHP arm and 98% in the CHOP arm. Grade 3 or higher AEs occurred in 66% and 65% of patients, respectively. Serious AEs occurred in 39% and 38%, respectively.
Three percent of patients in the BV-CHP arm and 4% of those in the CHOP arm had fatal AEs.
The study was funded by Seattle Genetics, Millennium Pharmaceuticals, and the National Institutes of Health. Dr. Horwitz reported relationships with Seattle Genetics, Millennium Pharmaceuticals, and other companies.
SOURCE: Horwitz S et al. ASH 2018, Abstract 997.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: The rate of death or progression was 42% in the BV-CHP arm and 55% in the CHOP arm (hazard ratio = 0.71, P = .011), while the rate of death alone was 23% and 32%, respectively (HR = 0.66, P = .0244).
Study details: A phase 3 trial of 452 patients with peripheral T-cell lymphoma.
Disclosures: The study was funded by Seattle Genetics, Millennium Pharmaceuticals, and the National Institutes of Health. Dr. Horwitz reported relationships with Seattle Genetics, Millennium Pharmaceuticals, and other companies.
Source: Horwitz S et al. ASH 2018, Abstract 997.
GO-8: Early promise for novel FVIII variant in hemophilia A
SAN DIEGO – A novel human factor VIII variant shows promise for the treatment of severe hemophilia A, according to preliminary findings from the ongoing Gene Therapy for Hemophilia A (GO-8) phase 1/2 dose-escalation study.
A single peripheral vein infusion of the factor VIII (FVIII) variant resulted in FVIII activity levels of about 6% versus levels of no more than 1% of normal at study entry in the first four patients, Pratima Chowdary, MD, reported at the annual meeting of the American Society of Hematology.
The variant, known as scAAV2/8-LP1-hFIXco, is being investigated for safety and efficacy in the GO-8 investigator-led, open-label, nonrandomized trial at a low, mid, and high dose (2 x 1011 vector genomes/kg, 6 x 1011 vector genomes/kg, and 2 x 1012 vector genomes/kg), said Dr. Chowdary, a consultant hematologist at Royal Free Hospital London.
The main study period is 6 months and 15 years of follow-up are offered.
The first patient received the low dose and achieved FVIII of about 6% within 1 week. That level persisted for about 6 weeks when the patient developed a transaminitis, which promptly responded to steroids.
His steady-state FVIII within a few weeks was 7% by one-stage assay and about 3% by chromogenic assay, Dr. Chowdary said.
The remaining patients received the mid dose and also achieved FVIII levels of about 6% within a week. Patient 2 started on prophylactic steroids at week 6, per protocol, and did not experience transaminitis, but also had no increase in FVIII level, compared with the low-dose patient, which may be explained by the potential drug half-life, she noted.
Patient 3 reached a FVIII level of about 30% by week 4. He developed transaminitis at that time, which was about 2 weeks before planned prophylactic drug administration, but the transaminitis was controlled by steroids over a period of about 8-10 weeks.
“His steady-state FVIII level by one stage was 34% and by chromogenic assay was 17%. He has not had any bleeds since his gene transfer and has not required any FVIII concentrate either,” she said.
Patient 4 reached a FVIII level of about 40% by week 4. He was given prophylactic steroids at that time because of the occurrence of transaminitis at week 4 in Patient 3.
The patient developed transaminitis during steroid taper about 4 weeks later, perhaps because of the rapid taper, Dr. Chowdary said, adding that the transaminitis was well controlled with steroids, but follow-up in this patient has only been about 12 weeks.
“The characteristics of FVIII expression in this patient are very similar to the previous patient. ... We suspect he will have a steady-state level of about 30%,” she said. “Again, he’s had no bleeds since his gene transfer and has not required any FVIII concentrate.”
The single infusion of this novel vector was well tolerated in each patient, with no evidence of infusion-related reactions, neutralizing anti-FVIII antibodies, or vector-related adverse events.
“The transgene expression was achieved in all patients and at both vector dosages,” Dr. Chowdary said. “What is very important is that the levels of less than 10% had only a modest impact on the bleed rates and FVIII usage, whereas an expression of more than 10% resulted in zero bleeds and the patient did not require any additional FVIII treatment.”
The data are “encouraging,” she said. “We look forward to escalating the dose in the next patient.”
Dr. Chowdary reported financial relationships with Bayer, CSL Behring, Baxalta, Baxter, Biogen, Freeline, Novo Nordisk, Pfizer, Roche, Shire, and SOBI.
SOURCE: Chowdary P et al. ASH 2018, Abstract 489.
SAN DIEGO – A novel human factor VIII variant shows promise for the treatment of severe hemophilia A, according to preliminary findings from the ongoing Gene Therapy for Hemophilia A (GO-8) phase 1/2 dose-escalation study.
A single peripheral vein infusion of the factor VIII (FVIII) variant resulted in FVIII activity levels of about 6% versus levels of no more than 1% of normal at study entry in the first four patients, Pratima Chowdary, MD, reported at the annual meeting of the American Society of Hematology.
The variant, known as scAAV2/8-LP1-hFIXco, is being investigated for safety and efficacy in the GO-8 investigator-led, open-label, nonrandomized trial at a low, mid, and high dose (2 x 1011 vector genomes/kg, 6 x 1011 vector genomes/kg, and 2 x 1012 vector genomes/kg), said Dr. Chowdary, a consultant hematologist at Royal Free Hospital London.
The main study period is 6 months and 15 years of follow-up are offered.
The first patient received the low dose and achieved FVIII of about 6% within 1 week. That level persisted for about 6 weeks when the patient developed a transaminitis, which promptly responded to steroids.
His steady-state FVIII within a few weeks was 7% by one-stage assay and about 3% by chromogenic assay, Dr. Chowdary said.
The remaining patients received the mid dose and also achieved FVIII levels of about 6% within a week. Patient 2 started on prophylactic steroids at week 6, per protocol, and did not experience transaminitis, but also had no increase in FVIII level, compared with the low-dose patient, which may be explained by the potential drug half-life, she noted.
Patient 3 reached a FVIII level of about 30% by week 4. He developed transaminitis at that time, which was about 2 weeks before planned prophylactic drug administration, but the transaminitis was controlled by steroids over a period of about 8-10 weeks.
“His steady-state FVIII level by one stage was 34% and by chromogenic assay was 17%. He has not had any bleeds since his gene transfer and has not required any FVIII concentrate either,” she said.
Patient 4 reached a FVIII level of about 40% by week 4. He was given prophylactic steroids at that time because of the occurrence of transaminitis at week 4 in Patient 3.
The patient developed transaminitis during steroid taper about 4 weeks later, perhaps because of the rapid taper, Dr. Chowdary said, adding that the transaminitis was well controlled with steroids, but follow-up in this patient has only been about 12 weeks.
“The characteristics of FVIII expression in this patient are very similar to the previous patient. ... We suspect he will have a steady-state level of about 30%,” she said. “Again, he’s had no bleeds since his gene transfer and has not required any FVIII concentrate.”
The single infusion of this novel vector was well tolerated in each patient, with no evidence of infusion-related reactions, neutralizing anti-FVIII antibodies, or vector-related adverse events.
“The transgene expression was achieved in all patients and at both vector dosages,” Dr. Chowdary said. “What is very important is that the levels of less than 10% had only a modest impact on the bleed rates and FVIII usage, whereas an expression of more than 10% resulted in zero bleeds and the patient did not require any additional FVIII treatment.”
The data are “encouraging,” she said. “We look forward to escalating the dose in the next patient.”
Dr. Chowdary reported financial relationships with Bayer, CSL Behring, Baxalta, Baxter, Biogen, Freeline, Novo Nordisk, Pfizer, Roche, Shire, and SOBI.
SOURCE: Chowdary P et al. ASH 2018, Abstract 489.
SAN DIEGO – A novel human factor VIII variant shows promise for the treatment of severe hemophilia A, according to preliminary findings from the ongoing Gene Therapy for Hemophilia A (GO-8) phase 1/2 dose-escalation study.
A single peripheral vein infusion of the factor VIII (FVIII) variant resulted in FVIII activity levels of about 6% versus levels of no more than 1% of normal at study entry in the first four patients, Pratima Chowdary, MD, reported at the annual meeting of the American Society of Hematology.
The variant, known as scAAV2/8-LP1-hFIXco, is being investigated for safety and efficacy in the GO-8 investigator-led, open-label, nonrandomized trial at a low, mid, and high dose (2 x 1011 vector genomes/kg, 6 x 1011 vector genomes/kg, and 2 x 1012 vector genomes/kg), said Dr. Chowdary, a consultant hematologist at Royal Free Hospital London.
The main study period is 6 months and 15 years of follow-up are offered.
The first patient received the low dose and achieved FVIII of about 6% within 1 week. That level persisted for about 6 weeks when the patient developed a transaminitis, which promptly responded to steroids.
His steady-state FVIII within a few weeks was 7% by one-stage assay and about 3% by chromogenic assay, Dr. Chowdary said.
The remaining patients received the mid dose and also achieved FVIII levels of about 6% within a week. Patient 2 started on prophylactic steroids at week 6, per protocol, and did not experience transaminitis, but also had no increase in FVIII level, compared with the low-dose patient, which may be explained by the potential drug half-life, she noted.
Patient 3 reached a FVIII level of about 30% by week 4. He developed transaminitis at that time, which was about 2 weeks before planned prophylactic drug administration, but the transaminitis was controlled by steroids over a period of about 8-10 weeks.
“His steady-state FVIII level by one stage was 34% and by chromogenic assay was 17%. He has not had any bleeds since his gene transfer and has not required any FVIII concentrate either,” she said.
Patient 4 reached a FVIII level of about 40% by week 4. He was given prophylactic steroids at that time because of the occurrence of transaminitis at week 4 in Patient 3.
The patient developed transaminitis during steroid taper about 4 weeks later, perhaps because of the rapid taper, Dr. Chowdary said, adding that the transaminitis was well controlled with steroids, but follow-up in this patient has only been about 12 weeks.
“The characteristics of FVIII expression in this patient are very similar to the previous patient. ... We suspect he will have a steady-state level of about 30%,” she said. “Again, he’s had no bleeds since his gene transfer and has not required any FVIII concentrate.”
The single infusion of this novel vector was well tolerated in each patient, with no evidence of infusion-related reactions, neutralizing anti-FVIII antibodies, or vector-related adverse events.
“The transgene expression was achieved in all patients and at both vector dosages,” Dr. Chowdary said. “What is very important is that the levels of less than 10% had only a modest impact on the bleed rates and FVIII usage, whereas an expression of more than 10% resulted in zero bleeds and the patient did not require any additional FVIII treatment.”
The data are “encouraging,” she said. “We look forward to escalating the dose in the next patient.”
Dr. Chowdary reported financial relationships with Bayer, CSL Behring, Baxalta, Baxter, Biogen, Freeline, Novo Nordisk, Pfizer, Roche, Shire, and SOBI.
SOURCE: Chowdary P et al. ASH 2018, Abstract 489.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: A single infusion of the factor VIII variant resulted in activity levels of about 6%, compared with 1% or less at baseline.
Study details: The findings were from the first four patients in a phase 1/2 dose-escalation study.
Disclosures: Dr. Chowdary reported financial relationships with Bayer, CSL Behring, Baxalta, Baxter, Biogen, Freeline, Novo Nordisk, Pfizer, Roche, Shire, and SOBI.
Source: Chowdary P et al. ASH 2018, Abstract 489.
Pembrolizumab approved for Merkel cell carcinoma
The Food and Drug Administration has , specifically for recurrent locally advanced or metastatic disease.
In a nonrandomized, open-label trial of 50 patients with recurrent locally advanced or metastatic Merkel cell carcinoma who had not received systemic treatment for the advanced disease, the overall response rate was 56% with a complete response rate of 24%; median response duration was not reached. But responses lasting more than 6 months were achieved by 96% and more than 12 months by 54%. The most common adverse reactions included fatigue, musculoskeletal pain, and decreased appetite.
Because it is an accelerated approval, “continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials,” according to the FDA press release announcing the approval.
Pembrolizumab is a programmed death receptor-1 (PD-1)-blocking antibody that was previously approved for treatment of unresectable or metastatic melanoma.
More about the latest approval, as well as full prescribing information, can be found on the FDA’s website.
The Food and Drug Administration has , specifically for recurrent locally advanced or metastatic disease.
In a nonrandomized, open-label trial of 50 patients with recurrent locally advanced or metastatic Merkel cell carcinoma who had not received systemic treatment for the advanced disease, the overall response rate was 56% with a complete response rate of 24%; median response duration was not reached. But responses lasting more than 6 months were achieved by 96% and more than 12 months by 54%. The most common adverse reactions included fatigue, musculoskeletal pain, and decreased appetite.
Because it is an accelerated approval, “continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials,” according to the FDA press release announcing the approval.
Pembrolizumab is a programmed death receptor-1 (PD-1)-blocking antibody that was previously approved for treatment of unresectable or metastatic melanoma.
More about the latest approval, as well as full prescribing information, can be found on the FDA’s website.
The Food and Drug Administration has , specifically for recurrent locally advanced or metastatic disease.
In a nonrandomized, open-label trial of 50 patients with recurrent locally advanced or metastatic Merkel cell carcinoma who had not received systemic treatment for the advanced disease, the overall response rate was 56% with a complete response rate of 24%; median response duration was not reached. But responses lasting more than 6 months were achieved by 96% and more than 12 months by 54%. The most common adverse reactions included fatigue, musculoskeletal pain, and decreased appetite.
Because it is an accelerated approval, “continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials,” according to the FDA press release announcing the approval.
Pembrolizumab is a programmed death receptor-1 (PD-1)-blocking antibody that was previously approved for treatment of unresectable or metastatic melanoma.
More about the latest approval, as well as full prescribing information, can be found on the FDA’s website.
Measuring the Impact of Developmental Encephalopathic Epilepsy
Developmental encephalopathic epilepsies (DEEs) are responsible for a disproportionate number of cases of drug resistance, early deaths, and disability, according to researchers from Northwestern-Feinberg School of Medicine and Yale School of Medicine.
- An analysis of 613 pediatric patients from the Connecticut Study of Epilepsy allowed researchers to classify patients into specific epilepsy syndromes and to reclassify them over a period of 9 years.
- Among these children, 58 were found to have DEEs (9.4%).
- DEEs were more resistant to drug therapy than other epilepsies (71% vs 18%), more likely to cause intellectual disability (84% vs 11%), and more likely to cause death (21% vs <1%).
- The analysis also revealed changes from the initial epilepsy diagnosis over time, eg, Lennox-Gastaut syndrome was initially diagnosed in only 4 children but by the end of 9 years, 22 had received the diagnosis.
Berg AT, Levy SR, Testa FM. Evolution and course of early life developmental encephalopathic epilepsies: Focus on Lennox‐Gastaut syndrome. Epilepsia. 2018;59:2096-2105.
Developmental encephalopathic epilepsies (DEEs) are responsible for a disproportionate number of cases of drug resistance, early deaths, and disability, according to researchers from Northwestern-Feinberg School of Medicine and Yale School of Medicine.
- An analysis of 613 pediatric patients from the Connecticut Study of Epilepsy allowed researchers to classify patients into specific epilepsy syndromes and to reclassify them over a period of 9 years.
- Among these children, 58 were found to have DEEs (9.4%).
- DEEs were more resistant to drug therapy than other epilepsies (71% vs 18%), more likely to cause intellectual disability (84% vs 11%), and more likely to cause death (21% vs <1%).
- The analysis also revealed changes from the initial epilepsy diagnosis over time, eg, Lennox-Gastaut syndrome was initially diagnosed in only 4 children but by the end of 9 years, 22 had received the diagnosis.
Berg AT, Levy SR, Testa FM. Evolution and course of early life developmental encephalopathic epilepsies: Focus on Lennox‐Gastaut syndrome. Epilepsia. 2018;59:2096-2105.
Developmental encephalopathic epilepsies (DEEs) are responsible for a disproportionate number of cases of drug resistance, early deaths, and disability, according to researchers from Northwestern-Feinberg School of Medicine and Yale School of Medicine.
- An analysis of 613 pediatric patients from the Connecticut Study of Epilepsy allowed researchers to classify patients into specific epilepsy syndromes and to reclassify them over a period of 9 years.
- Among these children, 58 were found to have DEEs (9.4%).
- DEEs were more resistant to drug therapy than other epilepsies (71% vs 18%), more likely to cause intellectual disability (84% vs 11%), and more likely to cause death (21% vs <1%).
- The analysis also revealed changes from the initial epilepsy diagnosis over time, eg, Lennox-Gastaut syndrome was initially diagnosed in only 4 children but by the end of 9 years, 22 had received the diagnosis.
Berg AT, Levy SR, Testa FM. Evolution and course of early life developmental encephalopathic epilepsies: Focus on Lennox‐Gastaut syndrome. Epilepsia. 2018;59:2096-2105.
Infraslow Envelope Analysis Holds Promise in Predicting Seizures
Analyzing infraslow amplitude modulations may help clinicians better understand changes in intracranial EEG readings over the long-term and help researchers develop better algorithms to forecast the onset of seizures, according to a report published in Epilepsia.
- Investigators from Yale-New Haven Hospital collected intracranial EEG readings from 13 adult patients with medically refractory epilepsy.
- To derive infraslow envelope correlations, they estimated magnitude-squared coherence at <0.15 Hz of EEG frequency band power time series for all electrode contact pairs.
- Infraslow envelope magnitude-squared coherence increased significantly after patients had their antiepileptic drugs tapered; it also increased at night and decreased during the day.
Joshi RB, Duckrow RB, Goncharova II, et al. Seizure susceptibility and infraslow modulatory activity in the intracranial electroencephalogram. Epilepsia. 2018;59:2075-2085.
Analyzing infraslow amplitude modulations may help clinicians better understand changes in intracranial EEG readings over the long-term and help researchers develop better algorithms to forecast the onset of seizures, according to a report published in Epilepsia.
- Investigators from Yale-New Haven Hospital collected intracranial EEG readings from 13 adult patients with medically refractory epilepsy.
- To derive infraslow envelope correlations, they estimated magnitude-squared coherence at <0.15 Hz of EEG frequency band power time series for all electrode contact pairs.
- Infraslow envelope magnitude-squared coherence increased significantly after patients had their antiepileptic drugs tapered; it also increased at night and decreased during the day.
Joshi RB, Duckrow RB, Goncharova II, et al. Seizure susceptibility and infraslow modulatory activity in the intracranial electroencephalogram. Epilepsia. 2018;59:2075-2085.
Analyzing infraslow amplitude modulations may help clinicians better understand changes in intracranial EEG readings over the long-term and help researchers develop better algorithms to forecast the onset of seizures, according to a report published in Epilepsia.
- Investigators from Yale-New Haven Hospital collected intracranial EEG readings from 13 adult patients with medically refractory epilepsy.
- To derive infraslow envelope correlations, they estimated magnitude-squared coherence at <0.15 Hz of EEG frequency band power time series for all electrode contact pairs.
- Infraslow envelope magnitude-squared coherence increased significantly after patients had their antiepileptic drugs tapered; it also increased at night and decreased during the day.
Joshi RB, Duckrow RB, Goncharova II, et al. Seizure susceptibility and infraslow modulatory activity in the intracranial electroencephalogram. Epilepsia. 2018;59:2075-2085.






