User login
Treatment includes surgery
Treatment includes surgery
Thank you for the great article about hidradenitis suppurativa. It was very informative as usual, but a little shortsighted. As ObGyns we tend not to focus so much on these dermatologic conditions. However, I think something very important is missing in the article. I do not see it mentioned that hidradenitis suppurativa is a type of acne, also called acne inversa. As such, it should be treated like acne, with special attention to diet with zero dairy products as a prevention measure. Also, metformin is very important, as noted in the article. Retinoids are also needed, maybe for years.
According to experts, the primary approach to this condition is surgical, with punch biopsies and unroofing of the lesions, with medical therapies as prevention strategies. Fortunately, special task forces are now tackling this condition, especially in Europe. I strongly recommend the book, Acne: Causes and Practical Management, by F. William Danby.
Ivan Valencia, MD
Quito, Ecuador
Dr. Barbieri responds
Dr. Valencia provides an important perspective on the surgical treatment of hidradenitis suppurativa (HS). I agree that surgery is an important treatment for Stage III HS, but nonsurgical approaches are preferred and often effective for Stage I HS, a stage most likely to be treated by a gynecologist.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Treatment includes surgery
Thank you for the great article about hidradenitis suppurativa. It was very informative as usual, but a little shortsighted. As ObGyns we tend not to focus so much on these dermatologic conditions. However, I think something very important is missing in the article. I do not see it mentioned that hidradenitis suppurativa is a type of acne, also called acne inversa. As such, it should be treated like acne, with special attention to diet with zero dairy products as a prevention measure. Also, metformin is very important, as noted in the article. Retinoids are also needed, maybe for years.
According to experts, the primary approach to this condition is surgical, with punch biopsies and unroofing of the lesions, with medical therapies as prevention strategies. Fortunately, special task forces are now tackling this condition, especially in Europe. I strongly recommend the book, Acne: Causes and Practical Management, by F. William Danby.
Ivan Valencia, MD
Quito, Ecuador
Dr. Barbieri responds
Dr. Valencia provides an important perspective on the surgical treatment of hidradenitis suppurativa (HS). I agree that surgery is an important treatment for Stage III HS, but nonsurgical approaches are preferred and often effective for Stage I HS, a stage most likely to be treated by a gynecologist.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Treatment includes surgery
Thank you for the great article about hidradenitis suppurativa. It was very informative as usual, but a little shortsighted. As ObGyns we tend not to focus so much on these dermatologic conditions. However, I think something very important is missing in the article. I do not see it mentioned that hidradenitis suppurativa is a type of acne, also called acne inversa. As such, it should be treated like acne, with special attention to diet with zero dairy products as a prevention measure. Also, metformin is very important, as noted in the article. Retinoids are also needed, maybe for years.
According to experts, the primary approach to this condition is surgical, with punch biopsies and unroofing of the lesions, with medical therapies as prevention strategies. Fortunately, special task forces are now tackling this condition, especially in Europe. I strongly recommend the book, Acne: Causes and Practical Management, by F. William Danby.
Ivan Valencia, MD
Quito, Ecuador
Dr. Barbieri responds
Dr. Valencia provides an important perspective on the surgical treatment of hidradenitis suppurativa (HS). I agree that surgery is an important treatment for Stage III HS, but nonsurgical approaches are preferred and often effective for Stage I HS, a stage most likely to be treated by a gynecologist.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Incision site for cesarean delivery is important in infection prevention
Incision site for cesarean delivery is important in infection prevention
Dr. Barbieri’s editorial very nicely explained strategies to reduce the risk of post–cesarean delivery surgical site infection (SSI). However, what was not mentioned, in my opinion, is the most important preventive strategy. Selecting the site for the initial skin incision plays a great role in whether or not the patient will develop an infection postoperatively.
Pfannenstiel incisions are popular because of their obvious cosmetic benefit. In nonemergent cesarean deliveries, most ObGyns try to use this incision. However, exactly where the incision is placed plays a large role in the genesis of a postoperative wound infection. The worst place for such incisions is in the crease above the pubis and below the panniculus. Invariably, this area remains moist and macerated, especially in obese patients, thus providing a fertile breeding ground for bacteria. This problem can be avoided by incising the skin approximately 2 cm cranial to and parallel to the aforementioned crease, provided that the panniculus is not too large. The point is that the incision should be placed in an area where it has a chance to stay dry.
Sometimes patients who are hugely obese require great creativity in the placement of their transverse skin incision. I recall one patient, pregnant with triplets, whose abdomen was so large that her umbilicus was over the region of the lower uterine segment when she was supine on the operating room table. Some would have lifted up her immense panniculus and placed the incision in the usual crease site. This would be problematic for obtaining adequate exposure to deliver the babies, and the risk of developing an incisional infection would be very high. Therefore, a transverse incision was made just below her umbilicus. The panniculus was a nonissue regarding gaining adequate exposure and, when closed, the incision remained completely dry and uninfected. The patient did extremely well postoperatively and had no infectious sequelae.
David L. Zisow, MD
Baltimore, Maryland
Extraperitoneal approach should be considered
I enjoyed the editorial on reducing surgical site infection, especially the references to the historical Halsted principles of surgery. “He was the first in this country to promulgate the philosophy of ‘safe’ surgery.”1 Regarding surgical principles of cesarean delivery, the pioneering German obstetricians in the 1930s were keenly aware that avoiding the peritoneal cavity was instrumental in reducing morbidity and mortality. They championed the safety of the extraperitoneal approach as the fundamental principle of cesarean delivery for maternal safety.2
I learned to embrace the principles of Kaboth while learning the technique in 1968–1972. Thus, for more than 30 years, I used the extraperitoneal approach to access the lower uterine segment, avoiding entrance into the abdominal cavity. My patients seemed to benefit. As the surgeon, I also benefited: with short operative delivery times, less postoperative pain and minor morbidities, fewer phone calls from nursing staff, and less difficulty for my patients. I had not contaminated the peritoneal cavity and avoided all those inherent problems. The decision to open the peritoneal cavity has not been subjected to the rigors of critical analysis.3 I think that Kaboth’s principles remain worthy of consideration even today.
Contemporary experiences in large populations such as in India and China that use the extraperitoneal cesarean approach seem to implicitly support Kaboth’s principles. However, in the milieu of evidence-based medicine, extraperitoneal cesarean delivery has not been adequately studied.4 Just maybe the extraperitoneal approach should be considered and understood as a primary surgical technique for cesarean deliveries; just maybe it deserves a historical asterisk alongside the Halsted dicta.
Hedric Hanson, MD
Anchorage, Alaska
Dr. Barbieri responds
I thank Drs. Zisow and Hanson for their great recommendations and clinical pearls. I agree with Dr. Zisow that I should have mentioned the importance of optimal placement of the transverse skin incision. Incision in a skin crease that is perpetually moist increases the risk for a postoperative complication. When the abdomen is prepped for surgery, the skin crease above the pubis appears to be very inviting for placement of the skin incision. Dr. Hanson highlights the important option of an extraperitoneal approach to cesarean delivery. I have not thought about using this approach since the mid-1980s. Dr. Hanson’s recommendation that a randomized trial be performed comparing the SSI rate and other outcomes for extraperitoneal and intraperitoneal cesarean delivery is a great idea.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Cameron JL. William Steward Halsted: our surgical heritage. Ann Surg. 1997;225(5):445–458.
- Kaboth G. Die Technik des extraperitonealen Entibindungschnittes. Zentralblatt fur Gynakologie.1934;58(6):310–311.
- Berghella V, Baxter JK Chauhan SP. Evidence-based surgery for cesarean section. Am J Obstet Gynecol. 2005;193(5):1607–1617.
- Hofmeyr GJ, Mathai M, Shah AN, Novikova N. Techniques for caesarean section. Cochrane Database Syst Rev. 2008; CD004662.
Incision site for cesarean delivery is important in infection prevention
Dr. Barbieri’s editorial very nicely explained strategies to reduce the risk of post–cesarean delivery surgical site infection (SSI). However, what was not mentioned, in my opinion, is the most important preventive strategy. Selecting the site for the initial skin incision plays a great role in whether or not the patient will develop an infection postoperatively.
Pfannenstiel incisions are popular because of their obvious cosmetic benefit. In nonemergent cesarean deliveries, most ObGyns try to use this incision. However, exactly where the incision is placed plays a large role in the genesis of a postoperative wound infection. The worst place for such incisions is in the crease above the pubis and below the panniculus. Invariably, this area remains moist and macerated, especially in obese patients, thus providing a fertile breeding ground for bacteria. This problem can be avoided by incising the skin approximately 2 cm cranial to and parallel to the aforementioned crease, provided that the panniculus is not too large. The point is that the incision should be placed in an area where it has a chance to stay dry.
Sometimes patients who are hugely obese require great creativity in the placement of their transverse skin incision. I recall one patient, pregnant with triplets, whose abdomen was so large that her umbilicus was over the region of the lower uterine segment when she was supine on the operating room table. Some would have lifted up her immense panniculus and placed the incision in the usual crease site. This would be problematic for obtaining adequate exposure to deliver the babies, and the risk of developing an incisional infection would be very high. Therefore, a transverse incision was made just below her umbilicus. The panniculus was a nonissue regarding gaining adequate exposure and, when closed, the incision remained completely dry and uninfected. The patient did extremely well postoperatively and had no infectious sequelae.
David L. Zisow, MD
Baltimore, Maryland
Extraperitoneal approach should be considered
I enjoyed the editorial on reducing surgical site infection, especially the references to the historical Halsted principles of surgery. “He was the first in this country to promulgate the philosophy of ‘safe’ surgery.”1 Regarding surgical principles of cesarean delivery, the pioneering German obstetricians in the 1930s were keenly aware that avoiding the peritoneal cavity was instrumental in reducing morbidity and mortality. They championed the safety of the extraperitoneal approach as the fundamental principle of cesarean delivery for maternal safety.2
I learned to embrace the principles of Kaboth while learning the technique in 1968–1972. Thus, for more than 30 years, I used the extraperitoneal approach to access the lower uterine segment, avoiding entrance into the abdominal cavity. My patients seemed to benefit. As the surgeon, I also benefited: with short operative delivery times, less postoperative pain and minor morbidities, fewer phone calls from nursing staff, and less difficulty for my patients. I had not contaminated the peritoneal cavity and avoided all those inherent problems. The decision to open the peritoneal cavity has not been subjected to the rigors of critical analysis.3 I think that Kaboth’s principles remain worthy of consideration even today.
Contemporary experiences in large populations such as in India and China that use the extraperitoneal cesarean approach seem to implicitly support Kaboth’s principles. However, in the milieu of evidence-based medicine, extraperitoneal cesarean delivery has not been adequately studied.4 Just maybe the extraperitoneal approach should be considered and understood as a primary surgical technique for cesarean deliveries; just maybe it deserves a historical asterisk alongside the Halsted dicta.
Hedric Hanson, MD
Anchorage, Alaska
Dr. Barbieri responds
I thank Drs. Zisow and Hanson for their great recommendations and clinical pearls. I agree with Dr. Zisow that I should have mentioned the importance of optimal placement of the transverse skin incision. Incision in a skin crease that is perpetually moist increases the risk for a postoperative complication. When the abdomen is prepped for surgery, the skin crease above the pubis appears to be very inviting for placement of the skin incision. Dr. Hanson highlights the important option of an extraperitoneal approach to cesarean delivery. I have not thought about using this approach since the mid-1980s. Dr. Hanson’s recommendation that a randomized trial be performed comparing the SSI rate and other outcomes for extraperitoneal and intraperitoneal cesarean delivery is a great idea.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Incision site for cesarean delivery is important in infection prevention
Dr. Barbieri’s editorial very nicely explained strategies to reduce the risk of post–cesarean delivery surgical site infection (SSI). However, what was not mentioned, in my opinion, is the most important preventive strategy. Selecting the site for the initial skin incision plays a great role in whether or not the patient will develop an infection postoperatively.
Pfannenstiel incisions are popular because of their obvious cosmetic benefit. In nonemergent cesarean deliveries, most ObGyns try to use this incision. However, exactly where the incision is placed plays a large role in the genesis of a postoperative wound infection. The worst place for such incisions is in the crease above the pubis and below the panniculus. Invariably, this area remains moist and macerated, especially in obese patients, thus providing a fertile breeding ground for bacteria. This problem can be avoided by incising the skin approximately 2 cm cranial to and parallel to the aforementioned crease, provided that the panniculus is not too large. The point is that the incision should be placed in an area where it has a chance to stay dry.
Sometimes patients who are hugely obese require great creativity in the placement of their transverse skin incision. I recall one patient, pregnant with triplets, whose abdomen was so large that her umbilicus was over the region of the lower uterine segment when she was supine on the operating room table. Some would have lifted up her immense panniculus and placed the incision in the usual crease site. This would be problematic for obtaining adequate exposure to deliver the babies, and the risk of developing an incisional infection would be very high. Therefore, a transverse incision was made just below her umbilicus. The panniculus was a nonissue regarding gaining adequate exposure and, when closed, the incision remained completely dry and uninfected. The patient did extremely well postoperatively and had no infectious sequelae.
David L. Zisow, MD
Baltimore, Maryland
Extraperitoneal approach should be considered
I enjoyed the editorial on reducing surgical site infection, especially the references to the historical Halsted principles of surgery. “He was the first in this country to promulgate the philosophy of ‘safe’ surgery.”1 Regarding surgical principles of cesarean delivery, the pioneering German obstetricians in the 1930s were keenly aware that avoiding the peritoneal cavity was instrumental in reducing morbidity and mortality. They championed the safety of the extraperitoneal approach as the fundamental principle of cesarean delivery for maternal safety.2
I learned to embrace the principles of Kaboth while learning the technique in 1968–1972. Thus, for more than 30 years, I used the extraperitoneal approach to access the lower uterine segment, avoiding entrance into the abdominal cavity. My patients seemed to benefit. As the surgeon, I also benefited: with short operative delivery times, less postoperative pain and minor morbidities, fewer phone calls from nursing staff, and less difficulty for my patients. I had not contaminated the peritoneal cavity and avoided all those inherent problems. The decision to open the peritoneal cavity has not been subjected to the rigors of critical analysis.3 I think that Kaboth’s principles remain worthy of consideration even today.
Contemporary experiences in large populations such as in India and China that use the extraperitoneal cesarean approach seem to implicitly support Kaboth’s principles. However, in the milieu of evidence-based medicine, extraperitoneal cesarean delivery has not been adequately studied.4 Just maybe the extraperitoneal approach should be considered and understood as a primary surgical technique for cesarean deliveries; just maybe it deserves a historical asterisk alongside the Halsted dicta.
Hedric Hanson, MD
Anchorage, Alaska
Dr. Barbieri responds
I thank Drs. Zisow and Hanson for their great recommendations and clinical pearls. I agree with Dr. Zisow that I should have mentioned the importance of optimal placement of the transverse skin incision. Incision in a skin crease that is perpetually moist increases the risk for a postoperative complication. When the abdomen is prepped for surgery, the skin crease above the pubis appears to be very inviting for placement of the skin incision. Dr. Hanson highlights the important option of an extraperitoneal approach to cesarean delivery. I have not thought about using this approach since the mid-1980s. Dr. Hanson’s recommendation that a randomized trial be performed comparing the SSI rate and other outcomes for extraperitoneal and intraperitoneal cesarean delivery is a great idea.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Cameron JL. William Steward Halsted: our surgical heritage. Ann Surg. 1997;225(5):445–458.
- Kaboth G. Die Technik des extraperitonealen Entibindungschnittes. Zentralblatt fur Gynakologie.1934;58(6):310–311.
- Berghella V, Baxter JK Chauhan SP. Evidence-based surgery for cesarean section. Am J Obstet Gynecol. 2005;193(5):1607–1617.
- Hofmeyr GJ, Mathai M, Shah AN, Novikova N. Techniques for caesarean section. Cochrane Database Syst Rev. 2008; CD004662.
- Cameron JL. William Steward Halsted: our surgical heritage. Ann Surg. 1997;225(5):445–458.
- Kaboth G. Die Technik des extraperitonealen Entibindungschnittes. Zentralblatt fur Gynakologie.1934;58(6):310–311.
- Berghella V, Baxter JK Chauhan SP. Evidence-based surgery for cesarean section. Am J Obstet Gynecol. 2005;193(5):1607–1617.
- Hofmeyr GJ, Mathai M, Shah AN, Novikova N. Techniques for caesarean section. Cochrane Database Syst Rev. 2008; CD004662.
Skip the catheter-directed thrombolytics
Background: Nearly half of all patients with proximal deep vein thrombosis (DVT) will develop postthrombotic syndrome at 2 years. Small trials have shown that the combination of catheter-directed delivery of thrombolytics, along with active mechanical clot removal, may prevent the postthrombotic syndrome.
Study design: Randomized, controlled trial.
Setting: Fifty-six clinical centers throughout the United States.
Synopsis: A total of 692 patients with symptomatic proximal DVT were randomized to receive either pharmacomechanical thrombolysis followed by anticoagulation or solely anticoagulation consistent with published guidelines. The primary outcome measured was the development of postthrombotic syndrome between 6 and 24 months. Over the 24 months that these patients were followed, 157 of 336 patients (47%) in the pharmacomechanical thrombolysis group and 171 of 355 patients (48%) in the control group developed postthrombotic syndrome (risk ratio, 0.96; 95% confidence interval, 0.82-1.11; P = .56). This result was consistent across predetermined subgroups.
Importantly, major bleeding within 10 days was more frequent in the pharmacomechanical thrombolysis group occurring in 6 of 336 patients (1.7%) versus 1 of 335 patients (0.3%) in the control group (P = .049). There was no significant difference in either recurrent venous thromboembolism at 24 months (12% in treatment group vs. 8% in control; P = .09) or deaths.
Of the 80 patients that did not present for follow-up postthrombotic syndrome assessments, two-thirds were in the control group, potentially leading to an underestimation of the effect of the intervention.
Bottom line: Pharmacomechanical catheter-directed thrombolysis does not reduce postthrombotic syndrome in proximal DVT and leads to an increased risk of major bleeding.
Citation: Vedantham S et al. Pharmacomechanical catheter-directed thrombolysis for deep-vein thrombosis. N Engl J Med. 2017 Dec 7;377(23):2240-52.
Dr. Scaletta is a hospitalist at Denver Health Medical Center and an assistant professor of medicine at the University of Colorado at Denver, Aurora.
Background: Nearly half of all patients with proximal deep vein thrombosis (DVT) will develop postthrombotic syndrome at 2 years. Small trials have shown that the combination of catheter-directed delivery of thrombolytics, along with active mechanical clot removal, may prevent the postthrombotic syndrome.
Study design: Randomized, controlled trial.
Setting: Fifty-six clinical centers throughout the United States.
Synopsis: A total of 692 patients with symptomatic proximal DVT were randomized to receive either pharmacomechanical thrombolysis followed by anticoagulation or solely anticoagulation consistent with published guidelines. The primary outcome measured was the development of postthrombotic syndrome between 6 and 24 months. Over the 24 months that these patients were followed, 157 of 336 patients (47%) in the pharmacomechanical thrombolysis group and 171 of 355 patients (48%) in the control group developed postthrombotic syndrome (risk ratio, 0.96; 95% confidence interval, 0.82-1.11; P = .56). This result was consistent across predetermined subgroups.
Importantly, major bleeding within 10 days was more frequent in the pharmacomechanical thrombolysis group occurring in 6 of 336 patients (1.7%) versus 1 of 335 patients (0.3%) in the control group (P = .049). There was no significant difference in either recurrent venous thromboembolism at 24 months (12% in treatment group vs. 8% in control; P = .09) or deaths.
Of the 80 patients that did not present for follow-up postthrombotic syndrome assessments, two-thirds were in the control group, potentially leading to an underestimation of the effect of the intervention.
Bottom line: Pharmacomechanical catheter-directed thrombolysis does not reduce postthrombotic syndrome in proximal DVT and leads to an increased risk of major bleeding.
Citation: Vedantham S et al. Pharmacomechanical catheter-directed thrombolysis for deep-vein thrombosis. N Engl J Med. 2017 Dec 7;377(23):2240-52.
Dr. Scaletta is a hospitalist at Denver Health Medical Center and an assistant professor of medicine at the University of Colorado at Denver, Aurora.
Background: Nearly half of all patients with proximal deep vein thrombosis (DVT) will develop postthrombotic syndrome at 2 years. Small trials have shown that the combination of catheter-directed delivery of thrombolytics, along with active mechanical clot removal, may prevent the postthrombotic syndrome.
Study design: Randomized, controlled trial.
Setting: Fifty-six clinical centers throughout the United States.
Synopsis: A total of 692 patients with symptomatic proximal DVT were randomized to receive either pharmacomechanical thrombolysis followed by anticoagulation or solely anticoagulation consistent with published guidelines. The primary outcome measured was the development of postthrombotic syndrome between 6 and 24 months. Over the 24 months that these patients were followed, 157 of 336 patients (47%) in the pharmacomechanical thrombolysis group and 171 of 355 patients (48%) in the control group developed postthrombotic syndrome (risk ratio, 0.96; 95% confidence interval, 0.82-1.11; P = .56). This result was consistent across predetermined subgroups.
Importantly, major bleeding within 10 days was more frequent in the pharmacomechanical thrombolysis group occurring in 6 of 336 patients (1.7%) versus 1 of 335 patients (0.3%) in the control group (P = .049). There was no significant difference in either recurrent venous thromboembolism at 24 months (12% in treatment group vs. 8% in control; P = .09) or deaths.
Of the 80 patients that did not present for follow-up postthrombotic syndrome assessments, two-thirds were in the control group, potentially leading to an underestimation of the effect of the intervention.
Bottom line: Pharmacomechanical catheter-directed thrombolysis does not reduce postthrombotic syndrome in proximal DVT and leads to an increased risk of major bleeding.
Citation: Vedantham S et al. Pharmacomechanical catheter-directed thrombolysis for deep-vein thrombosis. N Engl J Med. 2017 Dec 7;377(23):2240-52.
Dr. Scaletta is a hospitalist at Denver Health Medical Center and an assistant professor of medicine at the University of Colorado at Denver, Aurora.
Use of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes Worldwide
The majority of hospitalized patients worldwide have at least one peripheral intravenous catheter (PIVC),1 making PIVC insertion one of the most common clinical procedures. In the United States, physicians, advanced practitioners, and nurses insert over 300 million of these devices in hospitalized patients annually.2 Despite their prevalence, PIVCs are associated with high rates of complications, including insertion difficulty, phlebitis, infiltration, occlusion, dislodgment, and catheter-associated bloodstream infection (CABSI), known to increase morbidity and mortality risk.2-9 Up to 90% of PIVCs are prematurely removed owing to failure before planned replacement or before intravenous (IV) therapy completion.3-6,10-12
PIVC complication and failure commonly triggers insertion of a replacement device and can entail significant costs.2-4 One example is PIVC-related CABSI, where treatment costs have been estimated to be between US$35,000 and US$56,000 per patient.6,13 Another important consideration is the pain and anxiety experienced by patients who need a replacement device, particularly those with difficult vascular access, who may require multiple cannulation attempts to replace a PIVC.12,14-16 In developing nations, serious adverse events related to PIVCs are even more concerning, because hospital acquired infection rates and associated mortality are nearly 20 times greater than in developed nations.17
A number of evidence-based interventions have been suggested to reduce PIVC failure rates. In addition to optimal hand hygiene when inserting or accessing a PIVC to prevent infection,18 recommended interventions include placement of the PIVC in an area of non-flexion such as the forearm to provide stability for the device and to reduce patient discomfort, securing the PIVC to reduce movement of the catheter at the insertion site and within the blood vessel, and use of occlusive dressings that reduce the risk of external contamination of the PIVC site.11,19,20 Best practice guidelines also recommend the prompt removal of devices that are symptomatic (when phlebitis or other complications are suspected) and when the catheter is no longer required.21,22
Recent evidence has demonstrated that catheter size can have an impact on device survival rates. In adults, large-bore catheters of 18 gauge (G) or higher were found to have an increased rate of thrombosis, and smaller-bore catheters of 22G or lower (in adults) were found to have higher rates of dislodgment and occlusion/infiltration. The catheter size recommended for adults based on the latest evidence for most clinical applications is 20G.3,20,23,24 In addition, the documentation of insertion, maintenance, and removal of PIVCs in the medical record is a requirement in most healthcare facilities worldwide and is recommended by best practice guidelines; however, adherence remains a challenge.1,19
The concerning prevalence of PIVC-related complications and the lack of comparative data internationally on organizational compliance with best practice guidelines formed the rationale for this study. Our study aim was to describe the insertion characteristics, management practices, and outcomes of PIVCs internationally and to compare these variables to recommended best practice.
MATERIALS AND METHODS
Study Design and Participants
In this international cross-sectional study, we recruited hospitals through professional networks, including vascular access, infection prevention, safety and quality, nursing, and hospital associations (Appendix 2). Healthcare organizations, government health departments, and intravascular device suppliers were informed of the study and requested to further disseminate information through their networks. A study website was developed,25 and social media outlets, including Twitter®, LinkedIn®, and Facebook®, were used to promote the study.
Approval was granted by the Griffith University Human Research Ethics Committee in Australia (reference number NRS/34/13/HREC). In addition, evidence of study site and local institutional review board/ethics committee approval was required prior to study commencement. Each participating site agreed to follow the study protocol and signed an authorship agreement form. No financial support was provided to any site.
Hospitalized adult and pediatric patients with a PIVC in situ on the day of the study were eligible for inclusion. Sample size was determined by local capacity. Hospitals were encouraged to audit their entire institution if possible; however, data were accepted from as little as one ward. Data collectors comprised nurses and doctors with experience in PIVC assessment. They were briefed on the study protocol and data collection forms by the local site coordinator, and they were supported by an overall global coordinator. Clinicians assessed the PIVC insertion site and accessed hospital records to collect data related to PIVC insertion, concurrent medications, and IV fluid orders. Further clarification of data was obtained if necessary by the clinicians from the patients and treating staff. No identifiable patient information was collected.
Data Collection
To assess whether clinical facilities were following best practice recommendations, the study team developed three data collection forms to collect information regarding site characteristics (site questionnaire), track participant recruitment (screening log), and collect data regarding PIVC characteristics and management practices (case report form [CRF]). All forms were internally and externally validated following a pilot study involving 14 sites in 13 countries.1
The CRF included variables used to assess best practice interventions, such as catheter insertion characteristics (date and time, reason, location, profession of inserter, anatomical site of placement), catheter type (gauge, brand, and product), insertion site assessment (adverse symptoms, dressing type and integrity), and information related to the IV therapy (types of IV fluids and medications, flushing solutions). Idle PIVCs were defined as not being used for blood sampling or IV therapy in the preceding 24 h.
Data collection forms were translated into 15 languages by professional translators and back-translated for validity. Translation of some languages included additional rigor. For example, Spanish-speaking members from the Spanish mainland as well as from South America were employed so that appropriate synonyms were used to capture local terms and practice. Three options were provided for data entry: directly into a purpose-developed electronic database (Lime Survey® Project, Hamburg, Germany); on paper, then transcribed into the survey database at a later time by the hospital site; or paper entry then sent (via email or post) to the coordinating center for data entry. Once cleaned and collated, all data were provided to each participating hospital to confirm accuracy and for site use in local quality improvement processes. Data were collected between June 1, 2014 and July 31, 2015.
Statistical Analysis
All data management was undertaken using SAS statistical software (SAS Institute Inc., Cary NC, USA). Results are presented for eight geographical regions using descriptive statistics (frequencies, percentages, and 95% CIs) for the variables of interest. To assess trends in catheter dwell time and rates of phlebitis, Poisson regression was used. All analyses were undertaken using the R language for statistical analysis (R Core Team, Vienna, Austria). The (STROBE (Strengthening the Reporting of Observational Studies in Epidemiology statement) guidelines for cross-sectional studies were followed, and results are presented according to these recommendations.26
RESULTS
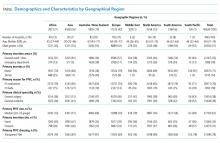
Of the 415 hospitals that participated in this study, 406 had patients with PIVCs on the day of the study (the others being small rural centers). Thus, a total of 40,620 PIVCs in 38,161 patients from 406 hospitals in 51 countries were assessed, with no more than 5% missing data for any CRF question. There were 2459 patients (6.1%) with two or more PIVCs concurrently in situ. The median patient age was 59 y (interquartile range [IQR], 37–74 y), and just over half were male (n = 20,550, 51%). Hospital size ranged from fewer than 10 beds to over 1,000 beds, and hospitals were located in rural, regional, and metropolitan districts. The majority of countries (n = 31, 61%) contributed multiple sites, the highest being Australia with 79 hospitals. Countries with the most PIVCs studied were Spain (n = 5,553, 14%) and the United States (n = 5,048, 12%).
General surgical (n = 15,616, 39%) and medical (n = 15,448, 38%) patients represented most of the population observed. PIVCs were inserted primarily in general wards or clinics (n = 22,167, 55%) or in emergency departments (n = 7,388, 18%; Table) and for the administration of IV medication (n = 28,571, 70%) and IV fluids (n = 7,093, 18%; Table).
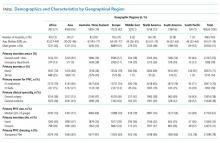
Globally, nurses were the primary PIVC inserters (n = 28,575, 71%); however, Australia/New Zealand had only 26% (n = 1,518) of PIVCs inserted by this group (Table). Only about one-third of PIVCs were placed in an area of non-flexion (forearm, n = 12,675, 31%, Table) the majority (n = 27,856, 69%) were placed in non-recommended anatomical sites (Figure 1). Most PIVCs were placed in the hand (n = 13,265, 32.7%) followed by the antecubital veins (n = 6176, 15.2%) and the wrist (n = 5,465, 13.5%). Site selection varied widely across the regions; 29% (n = 1686) of PIVCs in Australia/New Zealand were inserted into the antecubital veins, twice the study group average. Over half of the PIVCs inserted in the Middle East were placed in the hand (n = 295, 56%). This region also had the highest prevalence of devices placed in nonrecommended sites (n = 416, 79%; Figure 1).
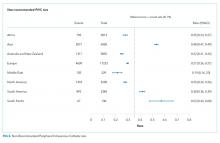
The majority of PIVCs (n = 27,192, 67%; Table) were of recommended size (20–22G); however, some devices were observed to be large (14–18G; n = 6,802, 17%) or small (24-26g; n = 4,869, 12%) in adults. In Asia, 41% (n = 2,617) of devices inserted were 24-26G, more than three times the global rate. Half of all devices in Asia (n = 3,077, 48%) and the South Pacific (n = 67, 52%) were of a size not recommended for routine IV therapy (Figure 2).
The primary dressing material used was a transparent dressing (n = 31,596, 77.8%; Table); however, nearly 1 in 5 dressings used had either nonsterile tape alone (n = 5,169, 13%; Appendix 4), or a sterile gauze and tape (n = 2,592, 6%; Appendix 4.1). We found a wide variation in the use of nonsterile tape, including 1 in every 3 devices in South America dressed with nonsterile tape (n = 714, 30%) and a larger proportion in Africa (n = 543, 19%) and Europe (n = 3,056, 18%). Nonsterile tape was rarely used in North America and Australia/New Zealand. Although most PIVC dressings were clean, dry, and intact (n = 31,786, 79%; Table), one-fifth overall were compromised (moist, soiled, and/or lifting off the skin). Compromised dressings (Appendix 4.2) were more prevalent in Australia/New Zealand (n = 1,448; 25%) and in Africa (n = 707, 25%) than elsewhere.
Ten percent of PIVCs (n = 4,204) had signs and/or symptoms suggestive of phlebitis (characterized by pain, redness and/or swelling at the insertion site; Appendix 4.3). The highest prevalence of phlebitis occurred in Asia (n = 1,021, 16%), Africa (n = 360, 13%), and South America (n = 284, 12%). Pain and/or redness were the most common phlebitis symptoms. We found no association between dwell time of PIVCs and phlebitis rates (P = .085). Phlebitis rates were 12% (Days 1-3; n = 15,625), 16% (Days 4-7; n = 3,348), 10% (Days 8-21; n = 457), and 13% (Day21+; n = 174). Nearly 10% (n = 3,879) of catheters were observed to have signs of malfunction such as blood in the infusion tubing, leaking at the insertion site, or dislodgment (Appendix 4.4).
We observed 14% (n = 5,796) of PIVCs to be idle (Appendix 4.5), defined as not used in the preceding 24 h. Nearly one-fourth of all devices in North America (n = 1,230, 23%) and Australia/New Zealand (n = 1,335, 23%) were idle. PIVC documentation in hospital records was also poor, nearly half of all PIVCs (n = 19,768, 49%) had no documented date and time of insertion. The poorest compliance was in Australia/New Zealand (n = 3,428, 59%; Appendix 4.6). We also observed that 1 in 10 PIVCs had no documentation regarding who inserted the PIVC (n = 3,905). Thirty-six percent of PIVCs (n = 14,787) had no documented assessment of the PIVC site on the day of review (Appendix 4.7), including over half of all PIVCs in Asia (n = 3,364, 52%). Overall, the median dwell at the time of assessment for PIVCs with insertion date/time documented was 1.5 d (IQR, 1.0–2.5 d).
DISCUSSION
This international assessment of more than 40,000 PIVCs in 51 countries provides great insight into device characteristics and variation in management practices. Predominantly, PIVCs were inserted by nurses in the general ward environment for IV medication. One in ten PIVCs had at least one symptom of phlebitis, one in ten were dysfunctional, one in five PIVC dressings were compromised, and one in six PIVCs had not been used in the preceding 24 h. Nearly half of the PIVCs audited had the insertion date and time missing.
Regional variation was found in the professions inserting PIVCs, as well as in anatomical placement. In Australia/New Zealand, the proportion of nurses inserting PIVCs was much lower than the study group average (26% vs 71%). Because these countries contributed a substantial number of hospitals to the study, this seems a representative finding and suggests a need for education targeted at nurses for PIVC insertion in this region. The veins in the forearm are recommended as optimal for PIVC insertion in adults, rather than areas of high flexion, because the forearm provides a wide surface area to secure and dress PIVCs. Forearm placement can reduce pain during catheter dwell as well as decrease the risk of accidental removal or occlusion.3,19,27 We found only one-third of PIVCs were placed in the forearm, with most placed in the hand, antecubital veins, or wrist. This highlights an inconsistency with published recommendations and suggests that additional training and technology are required so that staff can better identify and insert PIVCs in the forearm for other than very short-term (procedural) PIVCp;s.19
Phlebitis triggering PIVC failure remains a global clinical challenge with numerous phlebitis definitions and varied assessment techniques.10 The prevalence of phlebitis has been difficult to approximate with varying estimates and definitions in the literature; however, it remains a key predictor of PIVC failure.6,10 Identification of this complication and prompt removal of the device is critical for patient comfort and reducing CABSI risk.5,28 The overall prevalence of phlebitis signs or symptoms (defined in this study as having one or more signs of redness, swelling, or pain surrounding the insertion site) was just over 10%, with pain and/or redness being most prevalent. These compromised PIVCs had not been removed as is recommended for such complications.19,28 Considering that our study was a snapshot at only one time point, the per-catheter incidence of phlebitis would be even higher; interestingly, among PIVCs with a documented insertion date and time, we observed that dwell time did not influence phlebitis rates.
Another concern is that nearly 10% (n = 3,879) of PIVCs were malfunctioning (eg, leaking) but were still in place. To bring these problems into context, around 2 billion PIVCs are used annually worldwide; as a consequence, millions of patients suffer from painful or malfunctioning PIVCs staff had not responded.1,29 The placement of large-bore catheters, and smaller-gauge ones in adults, is known to increase the incidence of malfunction that leads to failure. There are a number of sound clinical reasons for the use of large-bore (eg, resuscitation and rapid fluid replacement) or small-bore (eg, difficult venous access with small superficial veins only visible and palpable) catheters. However, it would be expected that only a small proportion of patients would require these devices, and not one in three devices as we identified. This finding suggests that some PIVCs were inappropriate in size for general IV therapy and may reflect antiquated hospital policies for some clinical cohorts.30,31
Overall, transparent dressings were used to cover the PIVC, but a number of patients were observed to have a sterile gauze and tape dressing (n = 2,592, 6%). Although the latter is less common, both dressing approaches are recommended in clinical practice guidelines because there is a lack of high-quality evidence regarding which is superior.21,22,32 Of concern was the use of nonsterile tape to dress the PIVC (n = 5,169, 12.7%). We found the prevalence of nonsterile tape use to be higher in lower-resourced countries in South America (n = 714, 30%), Africa (n = 543, 19%) and Europe (n = 3,056, 18%) and this was likely related to institutional cost reduction practices.
This finding illustrates an important issue regarding proper PIVC care and management practices in developing nations. It is widely known that access to safe health care in lower-resourced nations is challenging and that rates of mortality related to healthcare-associated infections are much higher. Thus, the differences we found in PIVC management practices in these countries are not surprising.33,34 International health networks such as the Infection Control Africa Network, the International Federation of Infection Control, and the Centers for Disease Control and Prevention can have great influence on ministries of health and clinicians in these countries to develop coordinated efforts for safe and sustainable IV practices to reduce the burden of hospital-acquired infections and related morbidity and mortality.
We found that 14% of all PIVCs had no documented IV medication or IV fluid administered in the previous 24 h, strongly indicating that they were no longer needed. Australia/New Zealand, Europe, and North America were observed to have a higher prevalence of idle catheters than the remaining regions. This suggests that an opportunity exists to develop surveillance systems that better identify idle devices for prompt removal to reduce infection risk and patient discomfort. Several randomized controlled trials, a Cochrane review, and clinical practice guidelines recommend prompt removal of PIVCs when not required, if there are any complications, or if the PIVC was inserted urgently without an aseptic insertion technique.21,28,35,36 Idle PIVCs have been implicated in adverse patient outcomes, including phlebitis and CABSI.13,27
The substantial proportion of patients with a PIVC in this study who had no clinical indication for a PIVC, a symptomatic insertion site, malfunctioning catheter, and suboptimal dressing quality suggests the need for physicians, advanced practitioners, and nurses to adopt evidence-based PIVC insertion and maintenance bundles and supporting checklists to reduce the prevalence of PIVC complications.19,21,38-40 Recommended strategies for inclusion in PIVC maintenance bundles are prompt removal of symptomatic and/or idle catheters, hand hygiene prior to accessing the catheter, regular assessment of the device, and replacement of suboptimal dressings.41,42 This approach should be implemented across all clinical specialties involved in PIVC insertion and care.
Our study findings need to be considered within the context of some limitations. The cross-sectional design prevented follow-up of PIVCs until removal to collect outcomes, including subsequent PIVC complications and/or failure, following the study observation. Ideally, data collection could have included patient-level preferences for PIVC insertion, history of PIVC use and/or failure, the number of PIVC insertion attempts, and the number of PIVCs used during that hospitalization. However, a cohort study of this magnitude was not feasible, particularly because all sites contributed staff time to complete the data collection. Only half of all initially registered sites eventually participated in the study; reasons for not participating were cited as local workload constraints and/or difficulties in applying for local approvals. Although efforts to enroll hospitals worldwide were exhaustive, our sample was not randomly selected but relied on self-selection and so is not representative, particularly for countries that contributed only one hospital site. Caution is also required when comparing inter regional differences, particularly developing regions, because better-resourced/academic sites were possibly over represented in the sample. Nevertheless, PIVC variables differed significantly between participating hospitals, suggesting that the data represent a reasonable reflection of hospital variability.
CONCLUSIONS
On the basis of this international investigation, we report variations in the characteristics, management practices, and outcomes of PIVCs inserted in hospital patients from 51 countries. Many PIVCs were idle, symptomatic, had substandard dressings, and were inserted in suboptimal anatomical sites. Despite international best practice guidelines, a large number of patients had PIVCs that were already failing or at risk of complications, including infection. A stronger focus is needed on compliance with PIVC insertion and management guidelines; better surveillance of PIVC sites; and improved assessment, decision-making, and documentation.
Acknowledgements
We are extremely grateful to colleagues from across the globe who committed their time and effort to this study (for full details of countries and team members see Appendix 1).
1. Alexandrou E, Ray-Barruel G, Carr PJ, et al. International prevalence of the use of peripheral intravenous catheters. J Hosp Med. 2015;10(8):530-533. https:/doi.org/10.1002/jhm.2389
2. Zingg W, Pittet D. Peripheral venous catheters: an under-evaluated problem. Int J Antimicrob Agents. 2009;34(suppl 4):S38-S42. https:/ doi.org/10.1016/S0924-8579(09)70565-5
3. Wallis MC, McGrail MR, Webster J, Gowardman JR, Playford G, Rickard CM. Risk factors for PIV catheter failure: a multivariate analysis from a randomized control trial. Infect. Control Hosp Epidemiol. 2014;35(1):63-68. https:/doi.org/10.1086/674398.
4. Pujol M, Hornero A, Saballs M, et al. Clinical epidemiology and outcomes of peripheral venous catheter-related bloodstream infections at a university-affiliated hospital. J Hosp Infect. 2007;67(1):22-29.
5. Fakih MG, Jones K, Rey JE, et al. Sustained improvements in peripheral venous catheter care in non–intensive care units: a quasi-experimental controlled study of education and feedback. Infect. Control Hosp Epidemiol. 2012;33(5):449-455. https:/doi.org/10.1086/665322.
6. Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs. 2015;38(3):189-203. https:/ doi.org/10.1097/NAN.0000000000000100.
7. Austin ED, Sullivan SB, Whittier S, Lowy FD, Uhlemann AC. Peripheral intravenous catheter placement is an underrecognized source of Staphylococcus aureus bloodstream infection. Open Forum Infect Dis. 2016;3(2):ofw072. https:/ doi.org/10.1093/ofid/ofw072.
8. Stuart RL, Cameron D, Scott C, et al. Peripheral intravenous catheter-associated Staphylococcus aureus bacteraemia: more than 5 years of prospective data from two tertiary health services. Med J Aust. 2013;198(10):551-553.
9. Trinh TT, Chan PA, Edwards O, et al. Peripheral venous catheter-related Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol. 2011;32(6):579-583. https:/doi.org/10.1086/660099.
10. Ray Barruel G, Polit DF, Murfield JE, Rickard CM. Infusion phlebitis assessment measures: a systematic review. J Eval Clin Pract. 2014;20(2):191-202. https:/ doi.org/ 10.1111/jep.12107
11. Marsh N, Webster J, Flynn J, et al. Securement methods for peripheral venous catheters to prevent failure: a randomised controlled pilot trial. J Vasc Access. 2015;16(3):237-244. https:/doi.org /10.5301/jva.5000348.
12. Carr PJ, Higgins NS, Cooke ML, Rippey J, Rickard CM. Tools, clinical prediction rules, and algorithms for the insertion of peripheral intravenous catheters in adult hospitalized patients: a systematic scoping review of literature. J Hosp Med. 2017;12(10):851-858. https:/doi.org/ 10.12788/jhm.2836
13. Becerra MB, Shirley D, Safdar N. Prevalence, risk factors, and outcomes of idle intravenous catheters: An integrative review. Am J Infect Control. 2016;44(10):e167-e172. https:/ doi.org/10.1016/j.ajic.2016.03.073.
14. Robinson-Reilly M, Paliadelis P, Cruickshank M. Venous access: the patient experience. Support Care Cancer. 2016;24(3):1181-1187. https:/ doi.org/10.1007/s00520-015-2900-9.
15. Petroski A, Frisch A, Joseph N, Carlson JN. Predictors of difficult pediatric intravenous access in a community Emergency Department. J Vasc Access. 2015;16(6):521-526. https:/doi.org/10.5301/jva.5000411
16. Sou V, McManus C, Mifflin N, Frost SA, Ale J, Alexandrou E. A clinical pathway for the management of difficult venous access. BMC Nurs. 2017;16(1):64. https:/ doi.org/10.1186/s12912-017-0261-z
17. World Health Organization. Report on the burden of endemic health care-associated infection worldwide. Geneva2011. 9241501502.
18. Hirschmann H, Fux L, Podusel J, et al. The influence of hand hygiene prior to insertion of peripheral venous catheters on the frequency of complications. J Hosp Infect. 2001;49(3):199-203. https:/doi.org/10.1053/jhin.2001.1077
19. Gorski L, Hadaway L, Hagle M, McGoldrick M, Orr M, Doellman D. Infusion therapy standards of practice. J Infus Nurs. 2016;39(suppl 1):S1-S159.
20. Abolfotouh MA, Salam M, Bani-Mustafa Aa, White D, Balkhy HH. Prospective study of incidence and predictors of peripheral intravenous catheter-induced complications. Ther Clin Risk Manag. 2014;10:993. https://doi.org/10.2147/TCRM.S74685.
21. Loveday H, Wilson J, Pratt R, et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2014;86(suppl 1):S1-S70. https:/doi.org/10.1016/S0195-6701(13)60012-2.
22. O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162-e193. https:/doi.org/10.1093/cid/cir257
23. Cicolini G, Bonghi AP, Di Labio L, Di Mascio R. Position of peripheral venous cannulae and the incidence of thrombophlebitis: an observational study. J Adv Nurs. 2009;65(6):1268-1273. https:/doi.org/10.1111/j.1365-2648.2009.04980.x.
24. Marsh N, Webster J, Larson E, Cooke M, Mihala G, Rickard C. Observational study of peripheral intravenous catheter outcomes in adult hospitalized patients: a multivariable analysis of peripheral intravenous catheter failure. J Hosp Med. 2018;13(2):83-89. https:/doi.org/10.12788/jhm.2867.
25. One Million Global Catheters PIVC Worldwide Prevalence study. OMG study website http://www.omgpivc.org/. Accessed 23 March, 2017.
26. Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. https:/doi.org/ 10.1136/bmj.39335.541782.AD
27. Fields JM, Dean AJ, Todman RW, et al. The effect of vessel depth, diameter, and location on ultrasound-guided peripheral intravenous catheter longevity. Am J Emerg Med. 2012;30(7):1134-1140. https:/doi.org/10.1016/j.ajem.2011.07.027.
28. Patel SA, Alebich MM, Feldman LS. Choosing wisely: things we do for no reason. Routine replacement of peripheral intravenous catheters. J Hosp Med. 2017;12(1):42-45.
29. Newswire. Global Peripheral I.V. Catheter Market 2014 - 2018. New York, PR Newswire Assoc; 2014.
30. Webster J, Larsen E, Booker C, Laws J, Marsh N. Prophylactic insertion of large bore peripheral intravenous catheters in maternity patients for postpartum haemorrhage: A cohort study. Aust N Z J Obstet Gynaecol. 2017.https:/doi.org/10.1111/ajo.12759.
31. Rivera A, Strauss K, van Zundert A, Mortier E. Matching the peripheral intravenous catheter to the individual patient. Acta Anaesthesiol Belg. 2006;58(1):19.
32. Webster J, Gillies D, O’Riordan E, Sherriff KL, Rickard CM. Gauze and tape and transparent polyurethane dressings for central venous catheters. Cochrane Database Syst Rev. 2011;11:CD003827. https:/doi.org/10.1002/14651858.CD003827.pub2
33. Dieleman JL, Templin T, Sadat N, et al. National spending on health by source for 184 countries between 2013 and 2040. Lancet. 2016;387(10037):2521-2535. https:/ doi.org/10.1016/S0140-6736(16)30167-2.
34. Allegranzi B, Nejad SB, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377(9761):228-241. https:/ doi.org/10.1016/S0140-6736(10)61458-4.
35. Rickard CM, Webster J, Wallis MC, et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet. 2012;380(9847):1066-1074. https:/doi.org/10.1016/S0140-6736(12)61082-4.
36. Webster J, Osborne S, Rickard CM, New K. Clinically indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst Rev. 2015;8:CD007798. https://doi.org/10.1002/14651858.CD007798.pub4.
37. Yagnik L, Graves A, Thong K. Plastic in patient study: Prospective audit of adherence to peripheral intravenous cannula monitoring and documentation guidelines, with the aim of reducing future rates of intravenous cannula-related complications. Am J Infect Control. 2017;45(1):34-38. https:/doi.org/10.1016/j.ajic.2016.09.008.
38. Boyd S, Aggarwal I, Davey P, Logan M, Nathwani D. Peripheral intravenous catheters: the road to quality improvement and safer patient care. J Hosp Infect. 2011;77(1):37-41. https:/doi.org/10.1016/j.jhin.2010.09.011.
39. DeVries M, Valentine M, Mancos P. Protected clinical indication of peripheral intravenous lines: successful implementation. J Assoc Vasc Access. 2016;21(2):89-92. https://doi.org/10.1016/j.java.2016.03.001.
40. Rhodes D, Cheng A, McLellan S, et al. Reducing Staphylococcus aureus bloodstream infections associated with peripheral intravenous cannulae: successful implementation of a care bundle at a large Australian health service. J Hosp Infect. 2016;94(1):86-91. https:/doi.org/10.1016/j.jhin.2016.05.020.
41. Rinke ML, Chen AR, Bundy DG, et al. Implementation of a central line maintenance care bundle in hospitalized pediatric oncology patients. Pediatr. 2012;130(4):e996-e1004. https:/doi.org/10.1542/peds.2012-0295.
42. Marshall J, Mermel L, Fakih M, Hadaway L, Kallen A, O’Grady N. Strategies to prevent central line–associated bloodstream infections in acute care hospitals: 2014 update. Infect. Control Hosp Epidemiol. 2014;35(suppl 2):S89-107. https:/doi.org/10.1086/676533.
The majority of hospitalized patients worldwide have at least one peripheral intravenous catheter (PIVC),1 making PIVC insertion one of the most common clinical procedures. In the United States, physicians, advanced practitioners, and nurses insert over 300 million of these devices in hospitalized patients annually.2 Despite their prevalence, PIVCs are associated with high rates of complications, including insertion difficulty, phlebitis, infiltration, occlusion, dislodgment, and catheter-associated bloodstream infection (CABSI), known to increase morbidity and mortality risk.2-9 Up to 90% of PIVCs are prematurely removed owing to failure before planned replacement or before intravenous (IV) therapy completion.3-6,10-12
PIVC complication and failure commonly triggers insertion of a replacement device and can entail significant costs.2-4 One example is PIVC-related CABSI, where treatment costs have been estimated to be between US$35,000 and US$56,000 per patient.6,13 Another important consideration is the pain and anxiety experienced by patients who need a replacement device, particularly those with difficult vascular access, who may require multiple cannulation attempts to replace a PIVC.12,14-16 In developing nations, serious adverse events related to PIVCs are even more concerning, because hospital acquired infection rates and associated mortality are nearly 20 times greater than in developed nations.17
A number of evidence-based interventions have been suggested to reduce PIVC failure rates. In addition to optimal hand hygiene when inserting or accessing a PIVC to prevent infection,18 recommended interventions include placement of the PIVC in an area of non-flexion such as the forearm to provide stability for the device and to reduce patient discomfort, securing the PIVC to reduce movement of the catheter at the insertion site and within the blood vessel, and use of occlusive dressings that reduce the risk of external contamination of the PIVC site.11,19,20 Best practice guidelines also recommend the prompt removal of devices that are symptomatic (when phlebitis or other complications are suspected) and when the catheter is no longer required.21,22
Recent evidence has demonstrated that catheter size can have an impact on device survival rates. In adults, large-bore catheters of 18 gauge (G) or higher were found to have an increased rate of thrombosis, and smaller-bore catheters of 22G or lower (in adults) were found to have higher rates of dislodgment and occlusion/infiltration. The catheter size recommended for adults based on the latest evidence for most clinical applications is 20G.3,20,23,24 In addition, the documentation of insertion, maintenance, and removal of PIVCs in the medical record is a requirement in most healthcare facilities worldwide and is recommended by best practice guidelines; however, adherence remains a challenge.1,19
The concerning prevalence of PIVC-related complications and the lack of comparative data internationally on organizational compliance with best practice guidelines formed the rationale for this study. Our study aim was to describe the insertion characteristics, management practices, and outcomes of PIVCs internationally and to compare these variables to recommended best practice.
MATERIALS AND METHODS
Study Design and Participants
In this international cross-sectional study, we recruited hospitals through professional networks, including vascular access, infection prevention, safety and quality, nursing, and hospital associations (Appendix 2). Healthcare organizations, government health departments, and intravascular device suppliers were informed of the study and requested to further disseminate information through their networks. A study website was developed,25 and social media outlets, including Twitter®, LinkedIn®, and Facebook®, were used to promote the study.
Approval was granted by the Griffith University Human Research Ethics Committee in Australia (reference number NRS/34/13/HREC). In addition, evidence of study site and local institutional review board/ethics committee approval was required prior to study commencement. Each participating site agreed to follow the study protocol and signed an authorship agreement form. No financial support was provided to any site.
Hospitalized adult and pediatric patients with a PIVC in situ on the day of the study were eligible for inclusion. Sample size was determined by local capacity. Hospitals were encouraged to audit their entire institution if possible; however, data were accepted from as little as one ward. Data collectors comprised nurses and doctors with experience in PIVC assessment. They were briefed on the study protocol and data collection forms by the local site coordinator, and they were supported by an overall global coordinator. Clinicians assessed the PIVC insertion site and accessed hospital records to collect data related to PIVC insertion, concurrent medications, and IV fluid orders. Further clarification of data was obtained if necessary by the clinicians from the patients and treating staff. No identifiable patient information was collected.
Data Collection
To assess whether clinical facilities were following best practice recommendations, the study team developed three data collection forms to collect information regarding site characteristics (site questionnaire), track participant recruitment (screening log), and collect data regarding PIVC characteristics and management practices (case report form [CRF]). All forms were internally and externally validated following a pilot study involving 14 sites in 13 countries.1
The CRF included variables used to assess best practice interventions, such as catheter insertion characteristics (date and time, reason, location, profession of inserter, anatomical site of placement), catheter type (gauge, brand, and product), insertion site assessment (adverse symptoms, dressing type and integrity), and information related to the IV therapy (types of IV fluids and medications, flushing solutions). Idle PIVCs were defined as not being used for blood sampling or IV therapy in the preceding 24 h.
Data collection forms were translated into 15 languages by professional translators and back-translated for validity. Translation of some languages included additional rigor. For example, Spanish-speaking members from the Spanish mainland as well as from South America were employed so that appropriate synonyms were used to capture local terms and practice. Three options were provided for data entry: directly into a purpose-developed electronic database (Lime Survey® Project, Hamburg, Germany); on paper, then transcribed into the survey database at a later time by the hospital site; or paper entry then sent (via email or post) to the coordinating center for data entry. Once cleaned and collated, all data were provided to each participating hospital to confirm accuracy and for site use in local quality improvement processes. Data were collected between June 1, 2014 and July 31, 2015.
Statistical Analysis
All data management was undertaken using SAS statistical software (SAS Institute Inc., Cary NC, USA). Results are presented for eight geographical regions using descriptive statistics (frequencies, percentages, and 95% CIs) for the variables of interest. To assess trends in catheter dwell time and rates of phlebitis, Poisson regression was used. All analyses were undertaken using the R language for statistical analysis (R Core Team, Vienna, Austria). The (STROBE (Strengthening the Reporting of Observational Studies in Epidemiology statement) guidelines for cross-sectional studies were followed, and results are presented according to these recommendations.26
RESULTS
Of the 415 hospitals that participated in this study, 406 had patients with PIVCs on the day of the study (the others being small rural centers). Thus, a total of 40,620 PIVCs in 38,161 patients from 406 hospitals in 51 countries were assessed, with no more than 5% missing data for any CRF question. There were 2459 patients (6.1%) with two or more PIVCs concurrently in situ. The median patient age was 59 y (interquartile range [IQR], 37–74 y), and just over half were male (n = 20,550, 51%). Hospital size ranged from fewer than 10 beds to over 1,000 beds, and hospitals were located in rural, regional, and metropolitan districts. The majority of countries (n = 31, 61%) contributed multiple sites, the highest being Australia with 79 hospitals. Countries with the most PIVCs studied were Spain (n = 5,553, 14%) and the United States (n = 5,048, 12%).
General surgical (n = 15,616, 39%) and medical (n = 15,448, 38%) patients represented most of the population observed. PIVCs were inserted primarily in general wards or clinics (n = 22,167, 55%) or in emergency departments (n = 7,388, 18%; Table) and for the administration of IV medication (n = 28,571, 70%) and IV fluids (n = 7,093, 18%; Table).
Globally, nurses were the primary PIVC inserters (n = 28,575, 71%); however, Australia/New Zealand had only 26% (n = 1,518) of PIVCs inserted by this group (Table). Only about one-third of PIVCs were placed in an area of non-flexion (forearm, n = 12,675, 31%, Table) the majority (n = 27,856, 69%) were placed in non-recommended anatomical sites (Figure 1). Most PIVCs were placed in the hand (n = 13,265, 32.7%) followed by the antecubital veins (n = 6176, 15.2%) and the wrist (n = 5,465, 13.5%). Site selection varied widely across the regions; 29% (n = 1686) of PIVCs in Australia/New Zealand were inserted into the antecubital veins, twice the study group average. Over half of the PIVCs inserted in the Middle East were placed in the hand (n = 295, 56%). This region also had the highest prevalence of devices placed in nonrecommended sites (n = 416, 79%; Figure 1).
The majority of PIVCs (n = 27,192, 67%; Table) were of recommended size (20–22G); however, some devices were observed to be large (14–18G; n = 6,802, 17%) or small (24-26g; n = 4,869, 12%) in adults. In Asia, 41% (n = 2,617) of devices inserted were 24-26G, more than three times the global rate. Half of all devices in Asia (n = 3,077, 48%) and the South Pacific (n = 67, 52%) were of a size not recommended for routine IV therapy (Figure 2).
The primary dressing material used was a transparent dressing (n = 31,596, 77.8%; Table); however, nearly 1 in 5 dressings used had either nonsterile tape alone (n = 5,169, 13%; Appendix 4), or a sterile gauze and tape (n = 2,592, 6%; Appendix 4.1). We found a wide variation in the use of nonsterile tape, including 1 in every 3 devices in South America dressed with nonsterile tape (n = 714, 30%) and a larger proportion in Africa (n = 543, 19%) and Europe (n = 3,056, 18%). Nonsterile tape was rarely used in North America and Australia/New Zealand. Although most PIVC dressings were clean, dry, and intact (n = 31,786, 79%; Table), one-fifth overall were compromised (moist, soiled, and/or lifting off the skin). Compromised dressings (Appendix 4.2) were more prevalent in Australia/New Zealand (n = 1,448; 25%) and in Africa (n = 707, 25%) than elsewhere.
Ten percent of PIVCs (n = 4,204) had signs and/or symptoms suggestive of phlebitis (characterized by pain, redness and/or swelling at the insertion site; Appendix 4.3). The highest prevalence of phlebitis occurred in Asia (n = 1,021, 16%), Africa (n = 360, 13%), and South America (n = 284, 12%). Pain and/or redness were the most common phlebitis symptoms. We found no association between dwell time of PIVCs and phlebitis rates (P = .085). Phlebitis rates were 12% (Days 1-3; n = 15,625), 16% (Days 4-7; n = 3,348), 10% (Days 8-21; n = 457), and 13% (Day21+; n = 174). Nearly 10% (n = 3,879) of catheters were observed to have signs of malfunction such as blood in the infusion tubing, leaking at the insertion site, or dislodgment (Appendix 4.4).
We observed 14% (n = 5,796) of PIVCs to be idle (Appendix 4.5), defined as not used in the preceding 24 h. Nearly one-fourth of all devices in North America (n = 1,230, 23%) and Australia/New Zealand (n = 1,335, 23%) were idle. PIVC documentation in hospital records was also poor, nearly half of all PIVCs (n = 19,768, 49%) had no documented date and time of insertion. The poorest compliance was in Australia/New Zealand (n = 3,428, 59%; Appendix 4.6). We also observed that 1 in 10 PIVCs had no documentation regarding who inserted the PIVC (n = 3,905). Thirty-six percent of PIVCs (n = 14,787) had no documented assessment of the PIVC site on the day of review (Appendix 4.7), including over half of all PIVCs in Asia (n = 3,364, 52%). Overall, the median dwell at the time of assessment for PIVCs with insertion date/time documented was 1.5 d (IQR, 1.0–2.5 d).
DISCUSSION
This international assessment of more than 40,000 PIVCs in 51 countries provides great insight into device characteristics and variation in management practices. Predominantly, PIVCs were inserted by nurses in the general ward environment for IV medication. One in ten PIVCs had at least one symptom of phlebitis, one in ten were dysfunctional, one in five PIVC dressings were compromised, and one in six PIVCs had not been used in the preceding 24 h. Nearly half of the PIVCs audited had the insertion date and time missing.
Regional variation was found in the professions inserting PIVCs, as well as in anatomical placement. In Australia/New Zealand, the proportion of nurses inserting PIVCs was much lower than the study group average (26% vs 71%). Because these countries contributed a substantial number of hospitals to the study, this seems a representative finding and suggests a need for education targeted at nurses for PIVC insertion in this region. The veins in the forearm are recommended as optimal for PIVC insertion in adults, rather than areas of high flexion, because the forearm provides a wide surface area to secure and dress PIVCs. Forearm placement can reduce pain during catheter dwell as well as decrease the risk of accidental removal or occlusion.3,19,27 We found only one-third of PIVCs were placed in the forearm, with most placed in the hand, antecubital veins, or wrist. This highlights an inconsistency with published recommendations and suggests that additional training and technology are required so that staff can better identify and insert PIVCs in the forearm for other than very short-term (procedural) PIVCp;s.19
Phlebitis triggering PIVC failure remains a global clinical challenge with numerous phlebitis definitions and varied assessment techniques.10 The prevalence of phlebitis has been difficult to approximate with varying estimates and definitions in the literature; however, it remains a key predictor of PIVC failure.6,10 Identification of this complication and prompt removal of the device is critical for patient comfort and reducing CABSI risk.5,28 The overall prevalence of phlebitis signs or symptoms (defined in this study as having one or more signs of redness, swelling, or pain surrounding the insertion site) was just over 10%, with pain and/or redness being most prevalent. These compromised PIVCs had not been removed as is recommended for such complications.19,28 Considering that our study was a snapshot at only one time point, the per-catheter incidence of phlebitis would be even higher; interestingly, among PIVCs with a documented insertion date and time, we observed that dwell time did not influence phlebitis rates.
Another concern is that nearly 10% (n = 3,879) of PIVCs were malfunctioning (eg, leaking) but were still in place. To bring these problems into context, around 2 billion PIVCs are used annually worldwide; as a consequence, millions of patients suffer from painful or malfunctioning PIVCs staff had not responded.1,29 The placement of large-bore catheters, and smaller-gauge ones in adults, is known to increase the incidence of malfunction that leads to failure. There are a number of sound clinical reasons for the use of large-bore (eg, resuscitation and rapid fluid replacement) or small-bore (eg, difficult venous access with small superficial veins only visible and palpable) catheters. However, it would be expected that only a small proportion of patients would require these devices, and not one in three devices as we identified. This finding suggests that some PIVCs were inappropriate in size for general IV therapy and may reflect antiquated hospital policies for some clinical cohorts.30,31
Overall, transparent dressings were used to cover the PIVC, but a number of patients were observed to have a sterile gauze and tape dressing (n = 2,592, 6%). Although the latter is less common, both dressing approaches are recommended in clinical practice guidelines because there is a lack of high-quality evidence regarding which is superior.21,22,32 Of concern was the use of nonsterile tape to dress the PIVC (n = 5,169, 12.7%). We found the prevalence of nonsterile tape use to be higher in lower-resourced countries in South America (n = 714, 30%), Africa (n = 543, 19%) and Europe (n = 3,056, 18%) and this was likely related to institutional cost reduction practices.
This finding illustrates an important issue regarding proper PIVC care and management practices in developing nations. It is widely known that access to safe health care in lower-resourced nations is challenging and that rates of mortality related to healthcare-associated infections are much higher. Thus, the differences we found in PIVC management practices in these countries are not surprising.33,34 International health networks such as the Infection Control Africa Network, the International Federation of Infection Control, and the Centers for Disease Control and Prevention can have great influence on ministries of health and clinicians in these countries to develop coordinated efforts for safe and sustainable IV practices to reduce the burden of hospital-acquired infections and related morbidity and mortality.
We found that 14% of all PIVCs had no documented IV medication or IV fluid administered in the previous 24 h, strongly indicating that they were no longer needed. Australia/New Zealand, Europe, and North America were observed to have a higher prevalence of idle catheters than the remaining regions. This suggests that an opportunity exists to develop surveillance systems that better identify idle devices for prompt removal to reduce infection risk and patient discomfort. Several randomized controlled trials, a Cochrane review, and clinical practice guidelines recommend prompt removal of PIVCs when not required, if there are any complications, or if the PIVC was inserted urgently without an aseptic insertion technique.21,28,35,36 Idle PIVCs have been implicated in adverse patient outcomes, including phlebitis and CABSI.13,27
The substantial proportion of patients with a PIVC in this study who had no clinical indication for a PIVC, a symptomatic insertion site, malfunctioning catheter, and suboptimal dressing quality suggests the need for physicians, advanced practitioners, and nurses to adopt evidence-based PIVC insertion and maintenance bundles and supporting checklists to reduce the prevalence of PIVC complications.19,21,38-40 Recommended strategies for inclusion in PIVC maintenance bundles are prompt removal of symptomatic and/or idle catheters, hand hygiene prior to accessing the catheter, regular assessment of the device, and replacement of suboptimal dressings.41,42 This approach should be implemented across all clinical specialties involved in PIVC insertion and care.
Our study findings need to be considered within the context of some limitations. The cross-sectional design prevented follow-up of PIVCs until removal to collect outcomes, including subsequent PIVC complications and/or failure, following the study observation. Ideally, data collection could have included patient-level preferences for PIVC insertion, history of PIVC use and/or failure, the number of PIVC insertion attempts, and the number of PIVCs used during that hospitalization. However, a cohort study of this magnitude was not feasible, particularly because all sites contributed staff time to complete the data collection. Only half of all initially registered sites eventually participated in the study; reasons for not participating were cited as local workload constraints and/or difficulties in applying for local approvals. Although efforts to enroll hospitals worldwide were exhaustive, our sample was not randomly selected but relied on self-selection and so is not representative, particularly for countries that contributed only one hospital site. Caution is also required when comparing inter regional differences, particularly developing regions, because better-resourced/academic sites were possibly over represented in the sample. Nevertheless, PIVC variables differed significantly between participating hospitals, suggesting that the data represent a reasonable reflection of hospital variability.
CONCLUSIONS
On the basis of this international investigation, we report variations in the characteristics, management practices, and outcomes of PIVCs inserted in hospital patients from 51 countries. Many PIVCs were idle, symptomatic, had substandard dressings, and were inserted in suboptimal anatomical sites. Despite international best practice guidelines, a large number of patients had PIVCs that were already failing or at risk of complications, including infection. A stronger focus is needed on compliance with PIVC insertion and management guidelines; better surveillance of PIVC sites; and improved assessment, decision-making, and documentation.
Acknowledgements
We are extremely grateful to colleagues from across the globe who committed their time and effort to this study (for full details of countries and team members see Appendix 1).
The majority of hospitalized patients worldwide have at least one peripheral intravenous catheter (PIVC),1 making PIVC insertion one of the most common clinical procedures. In the United States, physicians, advanced practitioners, and nurses insert over 300 million of these devices in hospitalized patients annually.2 Despite their prevalence, PIVCs are associated with high rates of complications, including insertion difficulty, phlebitis, infiltration, occlusion, dislodgment, and catheter-associated bloodstream infection (CABSI), known to increase morbidity and mortality risk.2-9 Up to 90% of PIVCs are prematurely removed owing to failure before planned replacement or before intravenous (IV) therapy completion.3-6,10-12
PIVC complication and failure commonly triggers insertion of a replacement device and can entail significant costs.2-4 One example is PIVC-related CABSI, where treatment costs have been estimated to be between US$35,000 and US$56,000 per patient.6,13 Another important consideration is the pain and anxiety experienced by patients who need a replacement device, particularly those with difficult vascular access, who may require multiple cannulation attempts to replace a PIVC.12,14-16 In developing nations, serious adverse events related to PIVCs are even more concerning, because hospital acquired infection rates and associated mortality are nearly 20 times greater than in developed nations.17
A number of evidence-based interventions have been suggested to reduce PIVC failure rates. In addition to optimal hand hygiene when inserting or accessing a PIVC to prevent infection,18 recommended interventions include placement of the PIVC in an area of non-flexion such as the forearm to provide stability for the device and to reduce patient discomfort, securing the PIVC to reduce movement of the catheter at the insertion site and within the blood vessel, and use of occlusive dressings that reduce the risk of external contamination of the PIVC site.11,19,20 Best practice guidelines also recommend the prompt removal of devices that are symptomatic (when phlebitis or other complications are suspected) and when the catheter is no longer required.21,22
Recent evidence has demonstrated that catheter size can have an impact on device survival rates. In adults, large-bore catheters of 18 gauge (G) or higher were found to have an increased rate of thrombosis, and smaller-bore catheters of 22G or lower (in adults) were found to have higher rates of dislodgment and occlusion/infiltration. The catheter size recommended for adults based on the latest evidence for most clinical applications is 20G.3,20,23,24 In addition, the documentation of insertion, maintenance, and removal of PIVCs in the medical record is a requirement in most healthcare facilities worldwide and is recommended by best practice guidelines; however, adherence remains a challenge.1,19
The concerning prevalence of PIVC-related complications and the lack of comparative data internationally on organizational compliance with best practice guidelines formed the rationale for this study. Our study aim was to describe the insertion characteristics, management practices, and outcomes of PIVCs internationally and to compare these variables to recommended best practice.
MATERIALS AND METHODS
Study Design and Participants
In this international cross-sectional study, we recruited hospitals through professional networks, including vascular access, infection prevention, safety and quality, nursing, and hospital associations (Appendix 2). Healthcare organizations, government health departments, and intravascular device suppliers were informed of the study and requested to further disseminate information through their networks. A study website was developed,25 and social media outlets, including Twitter®, LinkedIn®, and Facebook®, were used to promote the study.
Approval was granted by the Griffith University Human Research Ethics Committee in Australia (reference number NRS/34/13/HREC). In addition, evidence of study site and local institutional review board/ethics committee approval was required prior to study commencement. Each participating site agreed to follow the study protocol and signed an authorship agreement form. No financial support was provided to any site.
Hospitalized adult and pediatric patients with a PIVC in situ on the day of the study were eligible for inclusion. Sample size was determined by local capacity. Hospitals were encouraged to audit their entire institution if possible; however, data were accepted from as little as one ward. Data collectors comprised nurses and doctors with experience in PIVC assessment. They were briefed on the study protocol and data collection forms by the local site coordinator, and they were supported by an overall global coordinator. Clinicians assessed the PIVC insertion site and accessed hospital records to collect data related to PIVC insertion, concurrent medications, and IV fluid orders. Further clarification of data was obtained if necessary by the clinicians from the patients and treating staff. No identifiable patient information was collected.
Data Collection
To assess whether clinical facilities were following best practice recommendations, the study team developed three data collection forms to collect information regarding site characteristics (site questionnaire), track participant recruitment (screening log), and collect data regarding PIVC characteristics and management practices (case report form [CRF]). All forms were internally and externally validated following a pilot study involving 14 sites in 13 countries.1
The CRF included variables used to assess best practice interventions, such as catheter insertion characteristics (date and time, reason, location, profession of inserter, anatomical site of placement), catheter type (gauge, brand, and product), insertion site assessment (adverse symptoms, dressing type and integrity), and information related to the IV therapy (types of IV fluids and medications, flushing solutions). Idle PIVCs were defined as not being used for blood sampling or IV therapy in the preceding 24 h.
Data collection forms were translated into 15 languages by professional translators and back-translated for validity. Translation of some languages included additional rigor. For example, Spanish-speaking members from the Spanish mainland as well as from South America were employed so that appropriate synonyms were used to capture local terms and practice. Three options were provided for data entry: directly into a purpose-developed electronic database (Lime Survey® Project, Hamburg, Germany); on paper, then transcribed into the survey database at a later time by the hospital site; or paper entry then sent (via email or post) to the coordinating center for data entry. Once cleaned and collated, all data were provided to each participating hospital to confirm accuracy and for site use in local quality improvement processes. Data were collected between June 1, 2014 and July 31, 2015.
Statistical Analysis
All data management was undertaken using SAS statistical software (SAS Institute Inc., Cary NC, USA). Results are presented for eight geographical regions using descriptive statistics (frequencies, percentages, and 95% CIs) for the variables of interest. To assess trends in catheter dwell time and rates of phlebitis, Poisson regression was used. All analyses were undertaken using the R language for statistical analysis (R Core Team, Vienna, Austria). The (STROBE (Strengthening the Reporting of Observational Studies in Epidemiology statement) guidelines for cross-sectional studies were followed, and results are presented according to these recommendations.26
RESULTS
Of the 415 hospitals that participated in this study, 406 had patients with PIVCs on the day of the study (the others being small rural centers). Thus, a total of 40,620 PIVCs in 38,161 patients from 406 hospitals in 51 countries were assessed, with no more than 5% missing data for any CRF question. There were 2459 patients (6.1%) with two or more PIVCs concurrently in situ. The median patient age was 59 y (interquartile range [IQR], 37–74 y), and just over half were male (n = 20,550, 51%). Hospital size ranged from fewer than 10 beds to over 1,000 beds, and hospitals were located in rural, regional, and metropolitan districts. The majority of countries (n = 31, 61%) contributed multiple sites, the highest being Australia with 79 hospitals. Countries with the most PIVCs studied were Spain (n = 5,553, 14%) and the United States (n = 5,048, 12%).
General surgical (n = 15,616, 39%) and medical (n = 15,448, 38%) patients represented most of the population observed. PIVCs were inserted primarily in general wards or clinics (n = 22,167, 55%) or in emergency departments (n = 7,388, 18%; Table) and for the administration of IV medication (n = 28,571, 70%) and IV fluids (n = 7,093, 18%; Table).
Globally, nurses were the primary PIVC inserters (n = 28,575, 71%); however, Australia/New Zealand had only 26% (n = 1,518) of PIVCs inserted by this group (Table). Only about one-third of PIVCs were placed in an area of non-flexion (forearm, n = 12,675, 31%, Table) the majority (n = 27,856, 69%) were placed in non-recommended anatomical sites (Figure 1). Most PIVCs were placed in the hand (n = 13,265, 32.7%) followed by the antecubital veins (n = 6176, 15.2%) and the wrist (n = 5,465, 13.5%). Site selection varied widely across the regions; 29% (n = 1686) of PIVCs in Australia/New Zealand were inserted into the antecubital veins, twice the study group average. Over half of the PIVCs inserted in the Middle East were placed in the hand (n = 295, 56%). This region also had the highest prevalence of devices placed in nonrecommended sites (n = 416, 79%; Figure 1).
The majority of PIVCs (n = 27,192, 67%; Table) were of recommended size (20–22G); however, some devices were observed to be large (14–18G; n = 6,802, 17%) or small (24-26g; n = 4,869, 12%) in adults. In Asia, 41% (n = 2,617) of devices inserted were 24-26G, more than three times the global rate. Half of all devices in Asia (n = 3,077, 48%) and the South Pacific (n = 67, 52%) were of a size not recommended for routine IV therapy (Figure 2).
The primary dressing material used was a transparent dressing (n = 31,596, 77.8%; Table); however, nearly 1 in 5 dressings used had either nonsterile tape alone (n = 5,169, 13%; Appendix 4), or a sterile gauze and tape (n = 2,592, 6%; Appendix 4.1). We found a wide variation in the use of nonsterile tape, including 1 in every 3 devices in South America dressed with nonsterile tape (n = 714, 30%) and a larger proportion in Africa (n = 543, 19%) and Europe (n = 3,056, 18%). Nonsterile tape was rarely used in North America and Australia/New Zealand. Although most PIVC dressings were clean, dry, and intact (n = 31,786, 79%; Table), one-fifth overall were compromised (moist, soiled, and/or lifting off the skin). Compromised dressings (Appendix 4.2) were more prevalent in Australia/New Zealand (n = 1,448; 25%) and in Africa (n = 707, 25%) than elsewhere.
Ten percent of PIVCs (n = 4,204) had signs and/or symptoms suggestive of phlebitis (characterized by pain, redness and/or swelling at the insertion site; Appendix 4.3). The highest prevalence of phlebitis occurred in Asia (n = 1,021, 16%), Africa (n = 360, 13%), and South America (n = 284, 12%). Pain and/or redness were the most common phlebitis symptoms. We found no association between dwell time of PIVCs and phlebitis rates (P = .085). Phlebitis rates were 12% (Days 1-3; n = 15,625), 16% (Days 4-7; n = 3,348), 10% (Days 8-21; n = 457), and 13% (Day21+; n = 174). Nearly 10% (n = 3,879) of catheters were observed to have signs of malfunction such as blood in the infusion tubing, leaking at the insertion site, or dislodgment (Appendix 4.4).
We observed 14% (n = 5,796) of PIVCs to be idle (Appendix 4.5), defined as not used in the preceding 24 h. Nearly one-fourth of all devices in North America (n = 1,230, 23%) and Australia/New Zealand (n = 1,335, 23%) were idle. PIVC documentation in hospital records was also poor, nearly half of all PIVCs (n = 19,768, 49%) had no documented date and time of insertion. The poorest compliance was in Australia/New Zealand (n = 3,428, 59%; Appendix 4.6). We also observed that 1 in 10 PIVCs had no documentation regarding who inserted the PIVC (n = 3,905). Thirty-six percent of PIVCs (n = 14,787) had no documented assessment of the PIVC site on the day of review (Appendix 4.7), including over half of all PIVCs in Asia (n = 3,364, 52%). Overall, the median dwell at the time of assessment for PIVCs with insertion date/time documented was 1.5 d (IQR, 1.0–2.5 d).
DISCUSSION
This international assessment of more than 40,000 PIVCs in 51 countries provides great insight into device characteristics and variation in management practices. Predominantly, PIVCs were inserted by nurses in the general ward environment for IV medication. One in ten PIVCs had at least one symptom of phlebitis, one in ten were dysfunctional, one in five PIVC dressings were compromised, and one in six PIVCs had not been used in the preceding 24 h. Nearly half of the PIVCs audited had the insertion date and time missing.
Regional variation was found in the professions inserting PIVCs, as well as in anatomical placement. In Australia/New Zealand, the proportion of nurses inserting PIVCs was much lower than the study group average (26% vs 71%). Because these countries contributed a substantial number of hospitals to the study, this seems a representative finding and suggests a need for education targeted at nurses for PIVC insertion in this region. The veins in the forearm are recommended as optimal for PIVC insertion in adults, rather than areas of high flexion, because the forearm provides a wide surface area to secure and dress PIVCs. Forearm placement can reduce pain during catheter dwell as well as decrease the risk of accidental removal or occlusion.3,19,27 We found only one-third of PIVCs were placed in the forearm, with most placed in the hand, antecubital veins, or wrist. This highlights an inconsistency with published recommendations and suggests that additional training and technology are required so that staff can better identify and insert PIVCs in the forearm for other than very short-term (procedural) PIVCp;s.19
Phlebitis triggering PIVC failure remains a global clinical challenge with numerous phlebitis definitions and varied assessment techniques.10 The prevalence of phlebitis has been difficult to approximate with varying estimates and definitions in the literature; however, it remains a key predictor of PIVC failure.6,10 Identification of this complication and prompt removal of the device is critical for patient comfort and reducing CABSI risk.5,28 The overall prevalence of phlebitis signs or symptoms (defined in this study as having one or more signs of redness, swelling, or pain surrounding the insertion site) was just over 10%, with pain and/or redness being most prevalent. These compromised PIVCs had not been removed as is recommended for such complications.19,28 Considering that our study was a snapshot at only one time point, the per-catheter incidence of phlebitis would be even higher; interestingly, among PIVCs with a documented insertion date and time, we observed that dwell time did not influence phlebitis rates.
Another concern is that nearly 10% (n = 3,879) of PIVCs were malfunctioning (eg, leaking) but were still in place. To bring these problems into context, around 2 billion PIVCs are used annually worldwide; as a consequence, millions of patients suffer from painful or malfunctioning PIVCs staff had not responded.1,29 The placement of large-bore catheters, and smaller-gauge ones in adults, is known to increase the incidence of malfunction that leads to failure. There are a number of sound clinical reasons for the use of large-bore (eg, resuscitation and rapid fluid replacement) or small-bore (eg, difficult venous access with small superficial veins only visible and palpable) catheters. However, it would be expected that only a small proportion of patients would require these devices, and not one in three devices as we identified. This finding suggests that some PIVCs were inappropriate in size for general IV therapy and may reflect antiquated hospital policies for some clinical cohorts.30,31
Overall, transparent dressings were used to cover the PIVC, but a number of patients were observed to have a sterile gauze and tape dressing (n = 2,592, 6%). Although the latter is less common, both dressing approaches are recommended in clinical practice guidelines because there is a lack of high-quality evidence regarding which is superior.21,22,32 Of concern was the use of nonsterile tape to dress the PIVC (n = 5,169, 12.7%). We found the prevalence of nonsterile tape use to be higher in lower-resourced countries in South America (n = 714, 30%), Africa (n = 543, 19%) and Europe (n = 3,056, 18%) and this was likely related to institutional cost reduction practices.
This finding illustrates an important issue regarding proper PIVC care and management practices in developing nations. It is widely known that access to safe health care in lower-resourced nations is challenging and that rates of mortality related to healthcare-associated infections are much higher. Thus, the differences we found in PIVC management practices in these countries are not surprising.33,34 International health networks such as the Infection Control Africa Network, the International Federation of Infection Control, and the Centers for Disease Control and Prevention can have great influence on ministries of health and clinicians in these countries to develop coordinated efforts for safe and sustainable IV practices to reduce the burden of hospital-acquired infections and related morbidity and mortality.
We found that 14% of all PIVCs had no documented IV medication or IV fluid administered in the previous 24 h, strongly indicating that they were no longer needed. Australia/New Zealand, Europe, and North America were observed to have a higher prevalence of idle catheters than the remaining regions. This suggests that an opportunity exists to develop surveillance systems that better identify idle devices for prompt removal to reduce infection risk and patient discomfort. Several randomized controlled trials, a Cochrane review, and clinical practice guidelines recommend prompt removal of PIVCs when not required, if there are any complications, or if the PIVC was inserted urgently without an aseptic insertion technique.21,28,35,36 Idle PIVCs have been implicated in adverse patient outcomes, including phlebitis and CABSI.13,27
The substantial proportion of patients with a PIVC in this study who had no clinical indication for a PIVC, a symptomatic insertion site, malfunctioning catheter, and suboptimal dressing quality suggests the need for physicians, advanced practitioners, and nurses to adopt evidence-based PIVC insertion and maintenance bundles and supporting checklists to reduce the prevalence of PIVC complications.19,21,38-40 Recommended strategies for inclusion in PIVC maintenance bundles are prompt removal of symptomatic and/or idle catheters, hand hygiene prior to accessing the catheter, regular assessment of the device, and replacement of suboptimal dressings.41,42 This approach should be implemented across all clinical specialties involved in PIVC insertion and care.
Our study findings need to be considered within the context of some limitations. The cross-sectional design prevented follow-up of PIVCs until removal to collect outcomes, including subsequent PIVC complications and/or failure, following the study observation. Ideally, data collection could have included patient-level preferences for PIVC insertion, history of PIVC use and/or failure, the number of PIVC insertion attempts, and the number of PIVCs used during that hospitalization. However, a cohort study of this magnitude was not feasible, particularly because all sites contributed staff time to complete the data collection. Only half of all initially registered sites eventually participated in the study; reasons for not participating were cited as local workload constraints and/or difficulties in applying for local approvals. Although efforts to enroll hospitals worldwide were exhaustive, our sample was not randomly selected but relied on self-selection and so is not representative, particularly for countries that contributed only one hospital site. Caution is also required when comparing inter regional differences, particularly developing regions, because better-resourced/academic sites were possibly over represented in the sample. Nevertheless, PIVC variables differed significantly between participating hospitals, suggesting that the data represent a reasonable reflection of hospital variability.
CONCLUSIONS
On the basis of this international investigation, we report variations in the characteristics, management practices, and outcomes of PIVCs inserted in hospital patients from 51 countries. Many PIVCs were idle, symptomatic, had substandard dressings, and were inserted in suboptimal anatomical sites. Despite international best practice guidelines, a large number of patients had PIVCs that were already failing or at risk of complications, including infection. A stronger focus is needed on compliance with PIVC insertion and management guidelines; better surveillance of PIVC sites; and improved assessment, decision-making, and documentation.
Acknowledgements
We are extremely grateful to colleagues from across the globe who committed their time and effort to this study (for full details of countries and team members see Appendix 1).
1. Alexandrou E, Ray-Barruel G, Carr PJ, et al. International prevalence of the use of peripheral intravenous catheters. J Hosp Med. 2015;10(8):530-533. https:/doi.org/10.1002/jhm.2389
2. Zingg W, Pittet D. Peripheral venous catheters: an under-evaluated problem. Int J Antimicrob Agents. 2009;34(suppl 4):S38-S42. https:/ doi.org/10.1016/S0924-8579(09)70565-5
3. Wallis MC, McGrail MR, Webster J, Gowardman JR, Playford G, Rickard CM. Risk factors for PIV catheter failure: a multivariate analysis from a randomized control trial. Infect. Control Hosp Epidemiol. 2014;35(1):63-68. https:/doi.org/10.1086/674398.
4. Pujol M, Hornero A, Saballs M, et al. Clinical epidemiology and outcomes of peripheral venous catheter-related bloodstream infections at a university-affiliated hospital. J Hosp Infect. 2007;67(1):22-29.
5. Fakih MG, Jones K, Rey JE, et al. Sustained improvements in peripheral venous catheter care in non–intensive care units: a quasi-experimental controlled study of education and feedback. Infect. Control Hosp Epidemiol. 2012;33(5):449-455. https:/doi.org/10.1086/665322.
6. Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs. 2015;38(3):189-203. https:/ doi.org/10.1097/NAN.0000000000000100.
7. Austin ED, Sullivan SB, Whittier S, Lowy FD, Uhlemann AC. Peripheral intravenous catheter placement is an underrecognized source of Staphylococcus aureus bloodstream infection. Open Forum Infect Dis. 2016;3(2):ofw072. https:/ doi.org/10.1093/ofid/ofw072.
8. Stuart RL, Cameron D, Scott C, et al. Peripheral intravenous catheter-associated Staphylococcus aureus bacteraemia: more than 5 years of prospective data from two tertiary health services. Med J Aust. 2013;198(10):551-553.
9. Trinh TT, Chan PA, Edwards O, et al. Peripheral venous catheter-related Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol. 2011;32(6):579-583. https:/doi.org/10.1086/660099.
10. Ray Barruel G, Polit DF, Murfield JE, Rickard CM. Infusion phlebitis assessment measures: a systematic review. J Eval Clin Pract. 2014;20(2):191-202. https:/ doi.org/ 10.1111/jep.12107
11. Marsh N, Webster J, Flynn J, et al. Securement methods for peripheral venous catheters to prevent failure: a randomised controlled pilot trial. J Vasc Access. 2015;16(3):237-244. https:/doi.org /10.5301/jva.5000348.
12. Carr PJ, Higgins NS, Cooke ML, Rippey J, Rickard CM. Tools, clinical prediction rules, and algorithms for the insertion of peripheral intravenous catheters in adult hospitalized patients: a systematic scoping review of literature. J Hosp Med. 2017;12(10):851-858. https:/doi.org/ 10.12788/jhm.2836
13. Becerra MB, Shirley D, Safdar N. Prevalence, risk factors, and outcomes of idle intravenous catheters: An integrative review. Am J Infect Control. 2016;44(10):e167-e172. https:/ doi.org/10.1016/j.ajic.2016.03.073.
14. Robinson-Reilly M, Paliadelis P, Cruickshank M. Venous access: the patient experience. Support Care Cancer. 2016;24(3):1181-1187. https:/ doi.org/10.1007/s00520-015-2900-9.
15. Petroski A, Frisch A, Joseph N, Carlson JN. Predictors of difficult pediatric intravenous access in a community Emergency Department. J Vasc Access. 2015;16(6):521-526. https:/doi.org/10.5301/jva.5000411
16. Sou V, McManus C, Mifflin N, Frost SA, Ale J, Alexandrou E. A clinical pathway for the management of difficult venous access. BMC Nurs. 2017;16(1):64. https:/ doi.org/10.1186/s12912-017-0261-z
17. World Health Organization. Report on the burden of endemic health care-associated infection worldwide. Geneva2011. 9241501502.
18. Hirschmann H, Fux L, Podusel J, et al. The influence of hand hygiene prior to insertion of peripheral venous catheters on the frequency of complications. J Hosp Infect. 2001;49(3):199-203. https:/doi.org/10.1053/jhin.2001.1077
19. Gorski L, Hadaway L, Hagle M, McGoldrick M, Orr M, Doellman D. Infusion therapy standards of practice. J Infus Nurs. 2016;39(suppl 1):S1-S159.
20. Abolfotouh MA, Salam M, Bani-Mustafa Aa, White D, Balkhy HH. Prospective study of incidence and predictors of peripheral intravenous catheter-induced complications. Ther Clin Risk Manag. 2014;10:993. https://doi.org/10.2147/TCRM.S74685.
21. Loveday H, Wilson J, Pratt R, et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2014;86(suppl 1):S1-S70. https:/doi.org/10.1016/S0195-6701(13)60012-2.
22. O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162-e193. https:/doi.org/10.1093/cid/cir257
23. Cicolini G, Bonghi AP, Di Labio L, Di Mascio R. Position of peripheral venous cannulae and the incidence of thrombophlebitis: an observational study. J Adv Nurs. 2009;65(6):1268-1273. https:/doi.org/10.1111/j.1365-2648.2009.04980.x.
24. Marsh N, Webster J, Larson E, Cooke M, Mihala G, Rickard C. Observational study of peripheral intravenous catheter outcomes in adult hospitalized patients: a multivariable analysis of peripheral intravenous catheter failure. J Hosp Med. 2018;13(2):83-89. https:/doi.org/10.12788/jhm.2867.
25. One Million Global Catheters PIVC Worldwide Prevalence study. OMG study website http://www.omgpivc.org/. Accessed 23 March, 2017.
26. Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. https:/doi.org/ 10.1136/bmj.39335.541782.AD
27. Fields JM, Dean AJ, Todman RW, et al. The effect of vessel depth, diameter, and location on ultrasound-guided peripheral intravenous catheter longevity. Am J Emerg Med. 2012;30(7):1134-1140. https:/doi.org/10.1016/j.ajem.2011.07.027.
28. Patel SA, Alebich MM, Feldman LS. Choosing wisely: things we do for no reason. Routine replacement of peripheral intravenous catheters. J Hosp Med. 2017;12(1):42-45.
29. Newswire. Global Peripheral I.V. Catheter Market 2014 - 2018. New York, PR Newswire Assoc; 2014.
30. Webster J, Larsen E, Booker C, Laws J, Marsh N. Prophylactic insertion of large bore peripheral intravenous catheters in maternity patients for postpartum haemorrhage: A cohort study. Aust N Z J Obstet Gynaecol. 2017.https:/doi.org/10.1111/ajo.12759.
31. Rivera A, Strauss K, van Zundert A, Mortier E. Matching the peripheral intravenous catheter to the individual patient. Acta Anaesthesiol Belg. 2006;58(1):19.
32. Webster J, Gillies D, O’Riordan E, Sherriff KL, Rickard CM. Gauze and tape and transparent polyurethane dressings for central venous catheters. Cochrane Database Syst Rev. 2011;11:CD003827. https:/doi.org/10.1002/14651858.CD003827.pub2
33. Dieleman JL, Templin T, Sadat N, et al. National spending on health by source for 184 countries between 2013 and 2040. Lancet. 2016;387(10037):2521-2535. https:/ doi.org/10.1016/S0140-6736(16)30167-2.
34. Allegranzi B, Nejad SB, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377(9761):228-241. https:/ doi.org/10.1016/S0140-6736(10)61458-4.
35. Rickard CM, Webster J, Wallis MC, et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet. 2012;380(9847):1066-1074. https:/doi.org/10.1016/S0140-6736(12)61082-4.
36. Webster J, Osborne S, Rickard CM, New K. Clinically indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst Rev. 2015;8:CD007798. https://doi.org/10.1002/14651858.CD007798.pub4.
37. Yagnik L, Graves A, Thong K. Plastic in patient study: Prospective audit of adherence to peripheral intravenous cannula monitoring and documentation guidelines, with the aim of reducing future rates of intravenous cannula-related complications. Am J Infect Control. 2017;45(1):34-38. https:/doi.org/10.1016/j.ajic.2016.09.008.
38. Boyd S, Aggarwal I, Davey P, Logan M, Nathwani D. Peripheral intravenous catheters: the road to quality improvement and safer patient care. J Hosp Infect. 2011;77(1):37-41. https:/doi.org/10.1016/j.jhin.2010.09.011.
39. DeVries M, Valentine M, Mancos P. Protected clinical indication of peripheral intravenous lines: successful implementation. J Assoc Vasc Access. 2016;21(2):89-92. https://doi.org/10.1016/j.java.2016.03.001.
40. Rhodes D, Cheng A, McLellan S, et al. Reducing Staphylococcus aureus bloodstream infections associated with peripheral intravenous cannulae: successful implementation of a care bundle at a large Australian health service. J Hosp Infect. 2016;94(1):86-91. https:/doi.org/10.1016/j.jhin.2016.05.020.
41. Rinke ML, Chen AR, Bundy DG, et al. Implementation of a central line maintenance care bundle in hospitalized pediatric oncology patients. Pediatr. 2012;130(4):e996-e1004. https:/doi.org/10.1542/peds.2012-0295.
42. Marshall J, Mermel L, Fakih M, Hadaway L, Kallen A, O’Grady N. Strategies to prevent central line–associated bloodstream infections in acute care hospitals: 2014 update. Infect. Control Hosp Epidemiol. 2014;35(suppl 2):S89-107. https:/doi.org/10.1086/676533.
1. Alexandrou E, Ray-Barruel G, Carr PJ, et al. International prevalence of the use of peripheral intravenous catheters. J Hosp Med. 2015;10(8):530-533. https:/doi.org/10.1002/jhm.2389
2. Zingg W, Pittet D. Peripheral venous catheters: an under-evaluated problem. Int J Antimicrob Agents. 2009;34(suppl 4):S38-S42. https:/ doi.org/10.1016/S0924-8579(09)70565-5
3. Wallis MC, McGrail MR, Webster J, Gowardman JR, Playford G, Rickard CM. Risk factors for PIV catheter failure: a multivariate analysis from a randomized control trial. Infect. Control Hosp Epidemiol. 2014;35(1):63-68. https:/doi.org/10.1086/674398.
4. Pujol M, Hornero A, Saballs M, et al. Clinical epidemiology and outcomes of peripheral venous catheter-related bloodstream infections at a university-affiliated hospital. J Hosp Infect. 2007;67(1):22-29.
5. Fakih MG, Jones K, Rey JE, et al. Sustained improvements in peripheral venous catheter care in non–intensive care units: a quasi-experimental controlled study of education and feedback. Infect. Control Hosp Epidemiol. 2012;33(5):449-455. https:/doi.org/10.1086/665322.
6. Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs. 2015;38(3):189-203. https:/ doi.org/10.1097/NAN.0000000000000100.
7. Austin ED, Sullivan SB, Whittier S, Lowy FD, Uhlemann AC. Peripheral intravenous catheter placement is an underrecognized source of Staphylococcus aureus bloodstream infection. Open Forum Infect Dis. 2016;3(2):ofw072. https:/ doi.org/10.1093/ofid/ofw072.
8. Stuart RL, Cameron D, Scott C, et al. Peripheral intravenous catheter-associated Staphylococcus aureus bacteraemia: more than 5 years of prospective data from two tertiary health services. Med J Aust. 2013;198(10):551-553.
9. Trinh TT, Chan PA, Edwards O, et al. Peripheral venous catheter-related Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol. 2011;32(6):579-583. https:/doi.org/10.1086/660099.
10. Ray Barruel G, Polit DF, Murfield JE, Rickard CM. Infusion phlebitis assessment measures: a systematic review. J Eval Clin Pract. 2014;20(2):191-202. https:/ doi.org/ 10.1111/jep.12107
11. Marsh N, Webster J, Flynn J, et al. Securement methods for peripheral venous catheters to prevent failure: a randomised controlled pilot trial. J Vasc Access. 2015;16(3):237-244. https:/doi.org /10.5301/jva.5000348.
12. Carr PJ, Higgins NS, Cooke ML, Rippey J, Rickard CM. Tools, clinical prediction rules, and algorithms for the insertion of peripheral intravenous catheters in adult hospitalized patients: a systematic scoping review of literature. J Hosp Med. 2017;12(10):851-858. https:/doi.org/ 10.12788/jhm.2836
13. Becerra MB, Shirley D, Safdar N. Prevalence, risk factors, and outcomes of idle intravenous catheters: An integrative review. Am J Infect Control. 2016;44(10):e167-e172. https:/ doi.org/10.1016/j.ajic.2016.03.073.
14. Robinson-Reilly M, Paliadelis P, Cruickshank M. Venous access: the patient experience. Support Care Cancer. 2016;24(3):1181-1187. https:/ doi.org/10.1007/s00520-015-2900-9.
15. Petroski A, Frisch A, Joseph N, Carlson JN. Predictors of difficult pediatric intravenous access in a community Emergency Department. J Vasc Access. 2015;16(6):521-526. https:/doi.org/10.5301/jva.5000411
16. Sou V, McManus C, Mifflin N, Frost SA, Ale J, Alexandrou E. A clinical pathway for the management of difficult venous access. BMC Nurs. 2017;16(1):64. https:/ doi.org/10.1186/s12912-017-0261-z
17. World Health Organization. Report on the burden of endemic health care-associated infection worldwide. Geneva2011. 9241501502.
18. Hirschmann H, Fux L, Podusel J, et al. The influence of hand hygiene prior to insertion of peripheral venous catheters on the frequency of complications. J Hosp Infect. 2001;49(3):199-203. https:/doi.org/10.1053/jhin.2001.1077
19. Gorski L, Hadaway L, Hagle M, McGoldrick M, Orr M, Doellman D. Infusion therapy standards of practice. J Infus Nurs. 2016;39(suppl 1):S1-S159.
20. Abolfotouh MA, Salam M, Bani-Mustafa Aa, White D, Balkhy HH. Prospective study of incidence and predictors of peripheral intravenous catheter-induced complications. Ther Clin Risk Manag. 2014;10:993. https://doi.org/10.2147/TCRM.S74685.
21. Loveday H, Wilson J, Pratt R, et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2014;86(suppl 1):S1-S70. https:/doi.org/10.1016/S0195-6701(13)60012-2.
22. O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162-e193. https:/doi.org/10.1093/cid/cir257
23. Cicolini G, Bonghi AP, Di Labio L, Di Mascio R. Position of peripheral venous cannulae and the incidence of thrombophlebitis: an observational study. J Adv Nurs. 2009;65(6):1268-1273. https:/doi.org/10.1111/j.1365-2648.2009.04980.x.
24. Marsh N, Webster J, Larson E, Cooke M, Mihala G, Rickard C. Observational study of peripheral intravenous catheter outcomes in adult hospitalized patients: a multivariable analysis of peripheral intravenous catheter failure. J Hosp Med. 2018;13(2):83-89. https:/doi.org/10.12788/jhm.2867.
25. One Million Global Catheters PIVC Worldwide Prevalence study. OMG study website http://www.omgpivc.org/. Accessed 23 March, 2017.
26. Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. https:/doi.org/ 10.1136/bmj.39335.541782.AD
27. Fields JM, Dean AJ, Todman RW, et al. The effect of vessel depth, diameter, and location on ultrasound-guided peripheral intravenous catheter longevity. Am J Emerg Med. 2012;30(7):1134-1140. https:/doi.org/10.1016/j.ajem.2011.07.027.
28. Patel SA, Alebich MM, Feldman LS. Choosing wisely: things we do for no reason. Routine replacement of peripheral intravenous catheters. J Hosp Med. 2017;12(1):42-45.
29. Newswire. Global Peripheral I.V. Catheter Market 2014 - 2018. New York, PR Newswire Assoc; 2014.
30. Webster J, Larsen E, Booker C, Laws J, Marsh N. Prophylactic insertion of large bore peripheral intravenous catheters in maternity patients for postpartum haemorrhage: A cohort study. Aust N Z J Obstet Gynaecol. 2017.https:/doi.org/10.1111/ajo.12759.
31. Rivera A, Strauss K, van Zundert A, Mortier E. Matching the peripheral intravenous catheter to the individual patient. Acta Anaesthesiol Belg. 2006;58(1):19.
32. Webster J, Gillies D, O’Riordan E, Sherriff KL, Rickard CM. Gauze and tape and transparent polyurethane dressings for central venous catheters. Cochrane Database Syst Rev. 2011;11:CD003827. https:/doi.org/10.1002/14651858.CD003827.pub2
33. Dieleman JL, Templin T, Sadat N, et al. National spending on health by source for 184 countries between 2013 and 2040. Lancet. 2016;387(10037):2521-2535. https:/ doi.org/10.1016/S0140-6736(16)30167-2.
34. Allegranzi B, Nejad SB, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377(9761):228-241. https:/ doi.org/10.1016/S0140-6736(10)61458-4.
35. Rickard CM, Webster J, Wallis MC, et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet. 2012;380(9847):1066-1074. https:/doi.org/10.1016/S0140-6736(12)61082-4.
36. Webster J, Osborne S, Rickard CM, New K. Clinically indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst Rev. 2015;8:CD007798. https://doi.org/10.1002/14651858.CD007798.pub4.
37. Yagnik L, Graves A, Thong K. Plastic in patient study: Prospective audit of adherence to peripheral intravenous cannula monitoring and documentation guidelines, with the aim of reducing future rates of intravenous cannula-related complications. Am J Infect Control. 2017;45(1):34-38. https:/doi.org/10.1016/j.ajic.2016.09.008.
38. Boyd S, Aggarwal I, Davey P, Logan M, Nathwani D. Peripheral intravenous catheters: the road to quality improvement and safer patient care. J Hosp Infect. 2011;77(1):37-41. https:/doi.org/10.1016/j.jhin.2010.09.011.
39. DeVries M, Valentine M, Mancos P. Protected clinical indication of peripheral intravenous lines: successful implementation. J Assoc Vasc Access. 2016;21(2):89-92. https://doi.org/10.1016/j.java.2016.03.001.
40. Rhodes D, Cheng A, McLellan S, et al. Reducing Staphylococcus aureus bloodstream infections associated with peripheral intravenous cannulae: successful implementation of a care bundle at a large Australian health service. J Hosp Infect. 2016;94(1):86-91. https:/doi.org/10.1016/j.jhin.2016.05.020.
41. Rinke ML, Chen AR, Bundy DG, et al. Implementation of a central line maintenance care bundle in hospitalized pediatric oncology patients. Pediatr. 2012;130(4):e996-e1004. https:/doi.org/10.1542/peds.2012-0295.
42. Marshall J, Mermel L, Fakih M, Hadaway L, Kallen A, O’Grady N. Strategies to prevent central line–associated bloodstream infections in acute care hospitals: 2014 update. Infect. Control Hosp Epidemiol. 2014;35(suppl 2):S89-107. https:/doi.org/10.1086/676533.
© 2018 Society of Hospital Medicine
New South Wales 2751, Australia; Telephone: + 612 9685 9506; Fax: + 612 9685 9023; E-mail: [email protected]
A New Target for a Flu Vaccine?
Seasonal flu vaccines mainly target an influenza surface protein called hemagglutinin (HA). But new research from National Institute of Health (NIH) studies suggest that it might be better to target a surface protein called neuraminidase (NA) for broader protection.
Researchers analyzed blood samples from people vaccinated against influenza and people who were diagnosed with the 2009 H1N1 virus or H3N2 viruses. The analyses indicated that influenza vaccines rarely induce NA-reactive antibodies, whereas natural influenza infection induces these types of antibodies at least as often as it induces HA-reactive antibodies, the researchers say.
Additional laboratory experiments showed the NA-reactive antibodies induced during natural flu infection were “broadly reactive,” meaning they could potentially protect against diverse strains. To test that theory, the researchers isolated NA-reactive monoclonal antibodies from the patients with H3N2 and H1N1, then administered 13 N2-reactive antibodies to mice and infected the mice with a different H3N2 virus strain. Eleven of the N2-reactive antibodies partially or fully protected the mice. In a similar test of N1-reactive antibodies versus H1N1 virus and H5N1-like virus, 4 of 8 antibodies completely protected against both strains.
Seasonal flu vaccines mainly target an influenza surface protein called hemagglutinin (HA). But new research from National Institute of Health (NIH) studies suggest that it might be better to target a surface protein called neuraminidase (NA) for broader protection.
Researchers analyzed blood samples from people vaccinated against influenza and people who were diagnosed with the 2009 H1N1 virus or H3N2 viruses. The analyses indicated that influenza vaccines rarely induce NA-reactive antibodies, whereas natural influenza infection induces these types of antibodies at least as often as it induces HA-reactive antibodies, the researchers say.
Additional laboratory experiments showed the NA-reactive antibodies induced during natural flu infection were “broadly reactive,” meaning they could potentially protect against diverse strains. To test that theory, the researchers isolated NA-reactive monoclonal antibodies from the patients with H3N2 and H1N1, then administered 13 N2-reactive antibodies to mice and infected the mice with a different H3N2 virus strain. Eleven of the N2-reactive antibodies partially or fully protected the mice. In a similar test of N1-reactive antibodies versus H1N1 virus and H5N1-like virus, 4 of 8 antibodies completely protected against both strains.
Seasonal flu vaccines mainly target an influenza surface protein called hemagglutinin (HA). But new research from National Institute of Health (NIH) studies suggest that it might be better to target a surface protein called neuraminidase (NA) for broader protection.
Researchers analyzed blood samples from people vaccinated against influenza and people who were diagnosed with the 2009 H1N1 virus or H3N2 viruses. The analyses indicated that influenza vaccines rarely induce NA-reactive antibodies, whereas natural influenza infection induces these types of antibodies at least as often as it induces HA-reactive antibodies, the researchers say.
Additional laboratory experiments showed the NA-reactive antibodies induced during natural flu infection were “broadly reactive,” meaning they could potentially protect against diverse strains. To test that theory, the researchers isolated NA-reactive monoclonal antibodies from the patients with H3N2 and H1N1, then administered 13 N2-reactive antibodies to mice and infected the mice with a different H3N2 virus strain. Eleven of the N2-reactive antibodies partially or fully protected the mice. In a similar test of N1-reactive antibodies versus H1N1 virus and H5N1-like virus, 4 of 8 antibodies completely protected against both strains.
Study of daratumamb with anti-PD-1 antibody in MM discontinued
Janssen is discontinuing the phase 1 MMY2036 study of daratumumab in combination with the anti PD-1 antibody JNJ-63723283 in patients with multiple myeloma (MM).
Janssen made the decision based on a Data Monitoring Committee review of Genmab’s phase 1b/2 study (LUC2001) of daratumumab plus the anti-PD-L1 antibody atezolizumab in non-small cell lung cancer (NSCLC).
Based on the DMC findings, Janssen also decided to discontinue its daratumumab-PD-1 combination study.
Janssen has an exclusive worldwide license from Genmab to develop, manufacture, and commercialize daratumumab.
In the planned review, the DMC determined there was no observed benefit within the daratumumab plus atezolizumab arm compared to the atezolizumab monotherapy arm. The DMC recommended termination of the NSCLC study.
The DMC also noted an increase in mortality-related events in the combination arm.
Janssen has informed health authorities about these events and has contacted its partner companies conducting daratumumab and anti-PD-1 combination studies to discuss ceasing enrollment and dosing of the combination while the data is being further investigated.
MMY2036 study (NCT03357952)
The randomized, multicenter, multiphase study was expected to enroll up to 386 patients with relapsed or refractory MM who had received at least 3 prior lines of therapy including a proteasome inhibitor (PI) and an immunomodulatory (IMiD) agent. Refractory patients had to be double refractory to both a PI and an IMiD.
The trial was to be conducted in 3 parts. Part 1 was to assess the safety of the combination of JNJ-63723283 and daratumumab. Part 2 was intended to compare the overall response rate in patients treated with the combination compared to those treated with daratumumab alone. And Part 3 was to compare progression-free survival between the 2 arms.
Daratumumab dose was planned to be 16 mg/kg weekly for 8 weeks, then once every other week for 16 weeks; then once every 4 weeks.
JNJ-63723283 dose was planned to be 240 milligrams IV fixed dose during week 1 on cycle 1 (28 days) day 2, cycle 1 day 15, then every 2 weeks thereafter.
The study was started in November 2017 and planned to be completed in December 2019.
In a news release, Genmab’s chief executive officer, Jan van de Winkel, PhD, expressed disappointment that the studies will be discontinued. He said Genmab “fully supports Janssen’s decision as patient safety is paramount in drug development. We look forward to gaining a better understanding of the data upon further analysis.”
Janssen is discontinuing the phase 1 MMY2036 study of daratumumab in combination with the anti PD-1 antibody JNJ-63723283 in patients with multiple myeloma (MM).
Janssen made the decision based on a Data Monitoring Committee review of Genmab’s phase 1b/2 study (LUC2001) of daratumumab plus the anti-PD-L1 antibody atezolizumab in non-small cell lung cancer (NSCLC).
Based on the DMC findings, Janssen also decided to discontinue its daratumumab-PD-1 combination study.
Janssen has an exclusive worldwide license from Genmab to develop, manufacture, and commercialize daratumumab.
In the planned review, the DMC determined there was no observed benefit within the daratumumab plus atezolizumab arm compared to the atezolizumab monotherapy arm. The DMC recommended termination of the NSCLC study.
The DMC also noted an increase in mortality-related events in the combination arm.
Janssen has informed health authorities about these events and has contacted its partner companies conducting daratumumab and anti-PD-1 combination studies to discuss ceasing enrollment and dosing of the combination while the data is being further investigated.
MMY2036 study (NCT03357952)
The randomized, multicenter, multiphase study was expected to enroll up to 386 patients with relapsed or refractory MM who had received at least 3 prior lines of therapy including a proteasome inhibitor (PI) and an immunomodulatory (IMiD) agent. Refractory patients had to be double refractory to both a PI and an IMiD.
The trial was to be conducted in 3 parts. Part 1 was to assess the safety of the combination of JNJ-63723283 and daratumumab. Part 2 was intended to compare the overall response rate in patients treated with the combination compared to those treated with daratumumab alone. And Part 3 was to compare progression-free survival between the 2 arms.
Daratumumab dose was planned to be 16 mg/kg weekly for 8 weeks, then once every other week for 16 weeks; then once every 4 weeks.
JNJ-63723283 dose was planned to be 240 milligrams IV fixed dose during week 1 on cycle 1 (28 days) day 2, cycle 1 day 15, then every 2 weeks thereafter.
The study was started in November 2017 and planned to be completed in December 2019.
In a news release, Genmab’s chief executive officer, Jan van de Winkel, PhD, expressed disappointment that the studies will be discontinued. He said Genmab “fully supports Janssen’s decision as patient safety is paramount in drug development. We look forward to gaining a better understanding of the data upon further analysis.”
Janssen is discontinuing the phase 1 MMY2036 study of daratumumab in combination with the anti PD-1 antibody JNJ-63723283 in patients with multiple myeloma (MM).
Janssen made the decision based on a Data Monitoring Committee review of Genmab’s phase 1b/2 study (LUC2001) of daratumumab plus the anti-PD-L1 antibody atezolizumab in non-small cell lung cancer (NSCLC).
Based on the DMC findings, Janssen also decided to discontinue its daratumumab-PD-1 combination study.
Janssen has an exclusive worldwide license from Genmab to develop, manufacture, and commercialize daratumumab.
In the planned review, the DMC determined there was no observed benefit within the daratumumab plus atezolizumab arm compared to the atezolizumab monotherapy arm. The DMC recommended termination of the NSCLC study.
The DMC also noted an increase in mortality-related events in the combination arm.
Janssen has informed health authorities about these events and has contacted its partner companies conducting daratumumab and anti-PD-1 combination studies to discuss ceasing enrollment and dosing of the combination while the data is being further investigated.
MMY2036 study (NCT03357952)
The randomized, multicenter, multiphase study was expected to enroll up to 386 patients with relapsed or refractory MM who had received at least 3 prior lines of therapy including a proteasome inhibitor (PI) and an immunomodulatory (IMiD) agent. Refractory patients had to be double refractory to both a PI and an IMiD.
The trial was to be conducted in 3 parts. Part 1 was to assess the safety of the combination of JNJ-63723283 and daratumumab. Part 2 was intended to compare the overall response rate in patients treated with the combination compared to those treated with daratumumab alone. And Part 3 was to compare progression-free survival between the 2 arms.
Daratumumab dose was planned to be 16 mg/kg weekly for 8 weeks, then once every other week for 16 weeks; then once every 4 weeks.
JNJ-63723283 dose was planned to be 240 milligrams IV fixed dose during week 1 on cycle 1 (28 days) day 2, cycle 1 day 15, then every 2 weeks thereafter.
The study was started in November 2017 and planned to be completed in December 2019.
In a news release, Genmab’s chief executive officer, Jan van de Winkel, PhD, expressed disappointment that the studies will be discontinued. He said Genmab “fully supports Janssen’s decision as patient safety is paramount in drug development. We look forward to gaining a better understanding of the data upon further analysis.”
FDA grants priority review to gilteritinib for R/R AML
The US Food and Drug Administration (FDA) has granted priority review to gilteritinib for the treatment of adult patients with relapsed or refractory (R/R) acute myeloid leukemia (AML) who have a FLT3 mutation.
At present, no FLT3-targeting agents are approved for the treatment of R/R FLT3-mutation-positive AML, according to Astellas, the developer of the drug.
The FDA previously granted gilteritinib orphan drug designation and fast track designation.
The European Commission (EC) also granted gilteritinib orphan designation and the Japan Ministry of Health, Labor and Welfare (MHLW) did likewise.
Gilteritinib has demonstrated inhibitory activity against FLT3 internal tandem duplication (ITD) and FLT tyrosine kinase domain (TKD) mutation. These 2 FLT3 mutations are present in approximately 1/3 of AML patients.
The priority review for the new drug application is based on the ongoing phase 3 ADMIRAL trial.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The goal date for a decision by the FDA is the end of November.
This open-label multicenter randomized study compares gilteritinib with salvage chemotherapy in adult patients with FLT3 mutations who are refractory to or have relapsed after first-line AML therapy.
The study has enrolled 371 patients with FLT3 mutations present in bone marrow or whole blood, as determined by a central lab.
Patients were randomized in a 2:1 ratio to receive gilteritinib (120 mg) or salvage chemotherapy.
Salvage chemotherapy could consist of low-dose cytarabine, azacitidine, MEC (mitoxantrone, etoposide, cytarabine) induction chemotherapy, or FLAG-IDA (fludarabine, cytarabine, and granulocyte colony-stimulating factor [G-CSF] with idarubicin) induction chemotherapy.
The primary endpoints of the study are overall survival and complete remission or complete remission with partial hematologic recovery.
Secondary endpoints include event-free survival, complete remission rate, leukemia-free survival, duration of remission, transplantation rate, fatigue inventory, among other outcomes.
The study is estimated to be completed in October for its primary endpoint and February 2020 for the entire study.
The US Food and Drug Administration (FDA) has granted priority review to gilteritinib for the treatment of adult patients with relapsed or refractory (R/R) acute myeloid leukemia (AML) who have a FLT3 mutation.
At present, no FLT3-targeting agents are approved for the treatment of R/R FLT3-mutation-positive AML, according to Astellas, the developer of the drug.
The FDA previously granted gilteritinib orphan drug designation and fast track designation.
The European Commission (EC) also granted gilteritinib orphan designation and the Japan Ministry of Health, Labor and Welfare (MHLW) did likewise.
Gilteritinib has demonstrated inhibitory activity against FLT3 internal tandem duplication (ITD) and FLT tyrosine kinase domain (TKD) mutation. These 2 FLT3 mutations are present in approximately 1/3 of AML patients.
The priority review for the new drug application is based on the ongoing phase 3 ADMIRAL trial.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The goal date for a decision by the FDA is the end of November.
This open-label multicenter randomized study compares gilteritinib with salvage chemotherapy in adult patients with FLT3 mutations who are refractory to or have relapsed after first-line AML therapy.
The study has enrolled 371 patients with FLT3 mutations present in bone marrow or whole blood, as determined by a central lab.
Patients were randomized in a 2:1 ratio to receive gilteritinib (120 mg) or salvage chemotherapy.
Salvage chemotherapy could consist of low-dose cytarabine, azacitidine, MEC (mitoxantrone, etoposide, cytarabine) induction chemotherapy, or FLAG-IDA (fludarabine, cytarabine, and granulocyte colony-stimulating factor [G-CSF] with idarubicin) induction chemotherapy.
The primary endpoints of the study are overall survival and complete remission or complete remission with partial hematologic recovery.
Secondary endpoints include event-free survival, complete remission rate, leukemia-free survival, duration of remission, transplantation rate, fatigue inventory, among other outcomes.
The study is estimated to be completed in October for its primary endpoint and February 2020 for the entire study.
The US Food and Drug Administration (FDA) has granted priority review to gilteritinib for the treatment of adult patients with relapsed or refractory (R/R) acute myeloid leukemia (AML) who have a FLT3 mutation.
At present, no FLT3-targeting agents are approved for the treatment of R/R FLT3-mutation-positive AML, according to Astellas, the developer of the drug.
The FDA previously granted gilteritinib orphan drug designation and fast track designation.
The European Commission (EC) also granted gilteritinib orphan designation and the Japan Ministry of Health, Labor and Welfare (MHLW) did likewise.
Gilteritinib has demonstrated inhibitory activity against FLT3 internal tandem duplication (ITD) and FLT tyrosine kinase domain (TKD) mutation. These 2 FLT3 mutations are present in approximately 1/3 of AML patients.
The priority review for the new drug application is based on the ongoing phase 3 ADMIRAL trial.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The goal date for a decision by the FDA is the end of November.
This open-label multicenter randomized study compares gilteritinib with salvage chemotherapy in adult patients with FLT3 mutations who are refractory to or have relapsed after first-line AML therapy.
The study has enrolled 371 patients with FLT3 mutations present in bone marrow or whole blood, as determined by a central lab.
Patients were randomized in a 2:1 ratio to receive gilteritinib (120 mg) or salvage chemotherapy.
Salvage chemotherapy could consist of low-dose cytarabine, azacitidine, MEC (mitoxantrone, etoposide, cytarabine) induction chemotherapy, or FLAG-IDA (fludarabine, cytarabine, and granulocyte colony-stimulating factor [G-CSF] with idarubicin) induction chemotherapy.
The primary endpoints of the study are overall survival and complete remission or complete remission with partial hematologic recovery.
Secondary endpoints include event-free survival, complete remission rate, leukemia-free survival, duration of remission, transplantation rate, fatigue inventory, among other outcomes.
The study is estimated to be completed in October for its primary endpoint and February 2020 for the entire study.
Inpatient Portals: The Questions that Remain
Personal health records (PHRs) are a broad group of applications “through which individuals can access, manage, and share their health information,” and are intended as a means to increase consumer health awareness, activation, safety, and self-efficacy.1 Patient portals—PHRs that are tethered to an electronic health record (EHR)—have expanded over the past decade, driven in part by the “Meaningful Use” EHR Incentive Program of the Centers for Medicare and Medicaid Services.2 This has been particularly true in the outpatient setting. Unfortunately, despite increased adoption and a large number of research studies, it is not clear whether outpatient portal use is associated with improved clinical outcomes.3
Both the use of portals in the inpatient setting and the research thereof are at a more nascent stage. In this issue of the Journal of Hospital Medicine, Kelly et al.4 provide a systematic review of the existing research on the implementation of inpatient portals. The authors identified 17 studies and categorized the papers’ findings into the following 3 themes: design, use and usability, and impact. Most of the studies elicited feedback from patients, caregivers, and/or providers – sometimes in multiple phases as portals were redesigned – allowing the authors to offer the following recommendations for inpatient portal design: portals should present timely information, include the care plan in ways patients can understand, and facilitate identification and communication with the care team.4 Most of the included studies focused on portal design and use, thereby limiting knowledge regarding impact on the outcomes portals are intended to target. All findings should be interpreted with caution, as many of the included studies were small and qualitative, most of them used convenience samples and subject-reported outcomes, and all were conducted at a single center. Many sites also used customized portals, thus limiting generalizability.
Participants often found portals to be useful, but this finding is of uncertain value in the absence of robust evidence on outcomes. In addition, providers included in the reviewed studies expressed concerns that have not yet been well studied, such as the potential impact of portals on workload and on patient anxiety. Some studies reported that provider concerns lessened following a portal rollout, but few studies evaluated physician input on features such as direct communication and test result reporting in active use. The outpatient portal literature suggests potential harm related to how results are delivered, thus placing importance on conducting additional inpatient studies. Patients value online access to their health information5 and in previous literature have indicated a preference for immediate access to results even if abnormal results would then be given without explanation.6 However, in a recent study, even normal findings delivered without context were a cause of negative emotions and increased calls to physicians.7 This effect could be more pronounced in inpatient settings, given the large volume of tests and abnormal results, the rapidly evolving treatment plans, and generally higher acuity and medical uncertainty.
This review and other current literature highlight challenges for vendors and hospitals. Vendors must ensure that patient health information is contextualized and delivered in a manner that meets individual learning styles.8 Patients and caregivers need clinical decision support to process today’s large amount of data, just as providers do. We must be careful not to implement patient portals in ways that increase cognitive load and generate anxiety and confusion. Hospitals have infrastructural challenges if portals are to be successful. Care provider information must be accurately registered in the EHR to route patient-to-provider communications, a difficult task across frequent handoffs and staffing changes.
We now have the beginnings of an informed vision for inpatient portal design. Future research and industry directions include greater exploration of recognized concerns and how to best reconcile these concerns with the benefits of portals espoused by consumer health advocates and experienced by patients, caregivers, and providers in the reviewed studies. Specifically, we need a better understanding of how best to incorporate inpatient portals into routine care delivery in ways that are useful to both patients and providers. We also need a better understanding of why patients opt out of portal use. Most of the studies to date report on the set of patients who decided to use the portals, leaving a knowledge gap in design and use implications for patients who opted out. Studies should include comparisons of patient outcomes between users and nonusers. Although inpatient portals show promise, many questions remain.
Disclosures
The authors declare no conflicts of interest.
1. Markle Foundation. Connecting Americans to their healthcare. Working group on policies for electronic information sharing between doctors and patients final report. https://www.markle.org/sites/default/files/CnctAmerHC_fullreport.pdf. Accessed February 18, 2018.
2. Centers for Medicare and Medicaid Services. Electronic health records (EHR) incentive programs. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms. Accessed February 18, 2018.
3. Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015;17(2):e44-e48. DOI:10.2196/jmir.3171. PubMed
4. Kelly MM, Coller RJ, Hoonakker PLT. Inpatient portals for hospitalized patients and caregivers: a systematic review. J Hosp Med. 2018;13(5):405-412.Published online first December 20, 2017. PubMed
5. Peacock S, Reddy A, Leveille SG, et al. Patient portals and personal health information online: perception, access, and use by US adults. J Am Med Inform Assoc. 2017;24(e1):e173-e177. DOI:10.1093/jamia/ocw095. PubMed
6. Johnson AJ, Easterling D, Nelson R, Chen MY, Frankel RM. Access to radiologic reports via a patient portal: clinical simulations to investigate patient preferences. JACR. 2012;9(4):256-263. DOI:10.1016/j.jacr.2011.12.023. PubMed
7. Giardina TD, Baldwin J, Nystrom DT, Sittig DF, Singh H. Patient perceptions of receiving test results via online portals: a mixed-methods study. J Am Med Inform Assoc. 2018;25(4)440-446. DOI:10.1093/jamia/ocx140. PubMed
8. Dalal AK, Bates DW, Collins S. Opportunities and challenges for improving the patient experience in the acute and post–acute care setting using patient portals: the patient’s perspective. J Hosp Med. 2017;12(12):1012-1016. DOI:10.12788/jhm.2860. PubMed
Personal health records (PHRs) are a broad group of applications “through which individuals can access, manage, and share their health information,” and are intended as a means to increase consumer health awareness, activation, safety, and self-efficacy.1 Patient portals—PHRs that are tethered to an electronic health record (EHR)—have expanded over the past decade, driven in part by the “Meaningful Use” EHR Incentive Program of the Centers for Medicare and Medicaid Services.2 This has been particularly true in the outpatient setting. Unfortunately, despite increased adoption and a large number of research studies, it is not clear whether outpatient portal use is associated with improved clinical outcomes.3
Both the use of portals in the inpatient setting and the research thereof are at a more nascent stage. In this issue of the Journal of Hospital Medicine, Kelly et al.4 provide a systematic review of the existing research on the implementation of inpatient portals. The authors identified 17 studies and categorized the papers’ findings into the following 3 themes: design, use and usability, and impact. Most of the studies elicited feedback from patients, caregivers, and/or providers – sometimes in multiple phases as portals were redesigned – allowing the authors to offer the following recommendations for inpatient portal design: portals should present timely information, include the care plan in ways patients can understand, and facilitate identification and communication with the care team.4 Most of the included studies focused on portal design and use, thereby limiting knowledge regarding impact on the outcomes portals are intended to target. All findings should be interpreted with caution, as many of the included studies were small and qualitative, most of them used convenience samples and subject-reported outcomes, and all were conducted at a single center. Many sites also used customized portals, thus limiting generalizability.
Participants often found portals to be useful, but this finding is of uncertain value in the absence of robust evidence on outcomes. In addition, providers included in the reviewed studies expressed concerns that have not yet been well studied, such as the potential impact of portals on workload and on patient anxiety. Some studies reported that provider concerns lessened following a portal rollout, but few studies evaluated physician input on features such as direct communication and test result reporting in active use. The outpatient portal literature suggests potential harm related to how results are delivered, thus placing importance on conducting additional inpatient studies. Patients value online access to their health information5 and in previous literature have indicated a preference for immediate access to results even if abnormal results would then be given without explanation.6 However, in a recent study, even normal findings delivered without context were a cause of negative emotions and increased calls to physicians.7 This effect could be more pronounced in inpatient settings, given the large volume of tests and abnormal results, the rapidly evolving treatment plans, and generally higher acuity and medical uncertainty.
This review and other current literature highlight challenges for vendors and hospitals. Vendors must ensure that patient health information is contextualized and delivered in a manner that meets individual learning styles.8 Patients and caregivers need clinical decision support to process today’s large amount of data, just as providers do. We must be careful not to implement patient portals in ways that increase cognitive load and generate anxiety and confusion. Hospitals have infrastructural challenges if portals are to be successful. Care provider information must be accurately registered in the EHR to route patient-to-provider communications, a difficult task across frequent handoffs and staffing changes.
We now have the beginnings of an informed vision for inpatient portal design. Future research and industry directions include greater exploration of recognized concerns and how to best reconcile these concerns with the benefits of portals espoused by consumer health advocates and experienced by patients, caregivers, and providers in the reviewed studies. Specifically, we need a better understanding of how best to incorporate inpatient portals into routine care delivery in ways that are useful to both patients and providers. We also need a better understanding of why patients opt out of portal use. Most of the studies to date report on the set of patients who decided to use the portals, leaving a knowledge gap in design and use implications for patients who opted out. Studies should include comparisons of patient outcomes between users and nonusers. Although inpatient portals show promise, many questions remain.
Disclosures
The authors declare no conflicts of interest.
Personal health records (PHRs) are a broad group of applications “through which individuals can access, manage, and share their health information,” and are intended as a means to increase consumer health awareness, activation, safety, and self-efficacy.1 Patient portals—PHRs that are tethered to an electronic health record (EHR)—have expanded over the past decade, driven in part by the “Meaningful Use” EHR Incentive Program of the Centers for Medicare and Medicaid Services.2 This has been particularly true in the outpatient setting. Unfortunately, despite increased adoption and a large number of research studies, it is not clear whether outpatient portal use is associated with improved clinical outcomes.3
Both the use of portals in the inpatient setting and the research thereof are at a more nascent stage. In this issue of the Journal of Hospital Medicine, Kelly et al.4 provide a systematic review of the existing research on the implementation of inpatient portals. The authors identified 17 studies and categorized the papers’ findings into the following 3 themes: design, use and usability, and impact. Most of the studies elicited feedback from patients, caregivers, and/or providers – sometimes in multiple phases as portals were redesigned – allowing the authors to offer the following recommendations for inpatient portal design: portals should present timely information, include the care plan in ways patients can understand, and facilitate identification and communication with the care team.4 Most of the included studies focused on portal design and use, thereby limiting knowledge regarding impact on the outcomes portals are intended to target. All findings should be interpreted with caution, as many of the included studies were small and qualitative, most of them used convenience samples and subject-reported outcomes, and all were conducted at a single center. Many sites also used customized portals, thus limiting generalizability.
Participants often found portals to be useful, but this finding is of uncertain value in the absence of robust evidence on outcomes. In addition, providers included in the reviewed studies expressed concerns that have not yet been well studied, such as the potential impact of portals on workload and on patient anxiety. Some studies reported that provider concerns lessened following a portal rollout, but few studies evaluated physician input on features such as direct communication and test result reporting in active use. The outpatient portal literature suggests potential harm related to how results are delivered, thus placing importance on conducting additional inpatient studies. Patients value online access to their health information5 and in previous literature have indicated a preference for immediate access to results even if abnormal results would then be given without explanation.6 However, in a recent study, even normal findings delivered without context were a cause of negative emotions and increased calls to physicians.7 This effect could be more pronounced in inpatient settings, given the large volume of tests and abnormal results, the rapidly evolving treatment plans, and generally higher acuity and medical uncertainty.
This review and other current literature highlight challenges for vendors and hospitals. Vendors must ensure that patient health information is contextualized and delivered in a manner that meets individual learning styles.8 Patients and caregivers need clinical decision support to process today’s large amount of data, just as providers do. We must be careful not to implement patient portals in ways that increase cognitive load and generate anxiety and confusion. Hospitals have infrastructural challenges if portals are to be successful. Care provider information must be accurately registered in the EHR to route patient-to-provider communications, a difficult task across frequent handoffs and staffing changes.
We now have the beginnings of an informed vision for inpatient portal design. Future research and industry directions include greater exploration of recognized concerns and how to best reconcile these concerns with the benefits of portals espoused by consumer health advocates and experienced by patients, caregivers, and providers in the reviewed studies. Specifically, we need a better understanding of how best to incorporate inpatient portals into routine care delivery in ways that are useful to both patients and providers. We also need a better understanding of why patients opt out of portal use. Most of the studies to date report on the set of patients who decided to use the portals, leaving a knowledge gap in design and use implications for patients who opted out. Studies should include comparisons of patient outcomes between users and nonusers. Although inpatient portals show promise, many questions remain.
Disclosures
The authors declare no conflicts of interest.
1. Markle Foundation. Connecting Americans to their healthcare. Working group on policies for electronic information sharing between doctors and patients final report. https://www.markle.org/sites/default/files/CnctAmerHC_fullreport.pdf. Accessed February 18, 2018.
2. Centers for Medicare and Medicaid Services. Electronic health records (EHR) incentive programs. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms. Accessed February 18, 2018.
3. Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015;17(2):e44-e48. DOI:10.2196/jmir.3171. PubMed
4. Kelly MM, Coller RJ, Hoonakker PLT. Inpatient portals for hospitalized patients and caregivers: a systematic review. J Hosp Med. 2018;13(5):405-412.Published online first December 20, 2017. PubMed
5. Peacock S, Reddy A, Leveille SG, et al. Patient portals and personal health information online: perception, access, and use by US adults. J Am Med Inform Assoc. 2017;24(e1):e173-e177. DOI:10.1093/jamia/ocw095. PubMed
6. Johnson AJ, Easterling D, Nelson R, Chen MY, Frankel RM. Access to radiologic reports via a patient portal: clinical simulations to investigate patient preferences. JACR. 2012;9(4):256-263. DOI:10.1016/j.jacr.2011.12.023. PubMed
7. Giardina TD, Baldwin J, Nystrom DT, Sittig DF, Singh H. Patient perceptions of receiving test results via online portals: a mixed-methods study. J Am Med Inform Assoc. 2018;25(4)440-446. DOI:10.1093/jamia/ocx140. PubMed
8. Dalal AK, Bates DW, Collins S. Opportunities and challenges for improving the patient experience in the acute and post–acute care setting using patient portals: the patient’s perspective. J Hosp Med. 2017;12(12):1012-1016. DOI:10.12788/jhm.2860. PubMed
1. Markle Foundation. Connecting Americans to their healthcare. Working group on policies for electronic information sharing between doctors and patients final report. https://www.markle.org/sites/default/files/CnctAmerHC_fullreport.pdf. Accessed February 18, 2018.
2. Centers for Medicare and Medicaid Services. Electronic health records (EHR) incentive programs. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms. Accessed February 18, 2018.
3. Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015;17(2):e44-e48. DOI:10.2196/jmir.3171. PubMed
4. Kelly MM, Coller RJ, Hoonakker PLT. Inpatient portals for hospitalized patients and caregivers: a systematic review. J Hosp Med. 2018;13(5):405-412.Published online first December 20, 2017. PubMed
5. Peacock S, Reddy A, Leveille SG, et al. Patient portals and personal health information online: perception, access, and use by US adults. J Am Med Inform Assoc. 2017;24(e1):e173-e177. DOI:10.1093/jamia/ocw095. PubMed
6. Johnson AJ, Easterling D, Nelson R, Chen MY, Frankel RM. Access to radiologic reports via a patient portal: clinical simulations to investigate patient preferences. JACR. 2012;9(4):256-263. DOI:10.1016/j.jacr.2011.12.023. PubMed
7. Giardina TD, Baldwin J, Nystrom DT, Sittig DF, Singh H. Patient perceptions of receiving test results via online portals: a mixed-methods study. J Am Med Inform Assoc. 2018;25(4)440-446. DOI:10.1093/jamia/ocx140. PubMed
8. Dalal AK, Bates DW, Collins S. Opportunities and challenges for improving the patient experience in the acute and post–acute care setting using patient portals: the patient’s perspective. J Hosp Med. 2017;12(12):1012-1016. DOI:10.12788/jhm.2860. PubMed
© 2018 Society of Hospital Medicine
Is it Time to Re-Examine the Physical Exam?
“Am I supposed to have such a hard time feeling the kidneys?” “I think I’m doing it wrong,” echoed another classmate. The frustration of these first-year students, who were already overwhelmed by the three pages of physical exam techniques that they were responsible for, became increasingly visible as they palpated the abdomens of their standardized patients. Then, they asked the dreaded question: “How often do you do this on real patients?”
When we teach first-year medical students the physical exam, these students are already aware that they have never observed physicians perform these maneuvers in their own medical care. “How come I’ve never seen my doctor do this before?” is a common question that we are often asked. We as faculty struggle with demonstrating and defending techniques that we hardly ever use given their variable utility in daily clinical practice. However, students are told that they must be familiar with the various “tools” in the repertoire, and they are led to believe that these skills will be a fundamental part of their future practice as physicians. Of course, when they begin their clerkships, the truth is revealed: the currency on the wards revolves around the computer. The experienced and passionate clinicians who may astonish them with the bedside exam are the exception and are hardly the rule.
In this issue of Journal of Hospital Medicine, Bergl et al.1 found that when medical students rotated on their internal medicine clerkship, patients were rarely examined during attending rounds and were even examined less often when these rounds were not at the bedside. Although the students themselves consistently incorporated the physical exam into patient assessments and presentations, neither their findings nor those of the residents were ever validated by the attending physician or by others. Notably, the physical exam did not influence clinical decision making as much as one might expect.
These findings should not come as a surprise. The current generation of residents and junior attendings today are more accustomed to emphasizing labs, imaging studies, pathology reports, and other data within the electronic health record (EHR) and with formulating initial plans before having met the patient.2 Physicians become uneasy when asked to decide without the reassurance of daily lab results, as if the information in the EHR is highly fundamental to patient care. Caring for the “iPatient” often trumps revisiting and reexamining the real patient.3 Medical teams are also bombarded with increasing demands for their attention and time and are pushed to expedite patient discharges while constantly responding to documentation queries in the EHR. Emphasis on patient throughput, quality metrics, and multidisciplinary communication is essential to provide effective patient care but often feels at odds with opportunities for bedside teaching.
Although discussions on these obstacles have increased in recent years, time-motion studies spanning decades and even preceding the duty-hours era have consistently shown that physicians reserve little time for physical examination and direct patient care.4 In other words, the challenges in bringing physicians to the bedside might have less to do with environmental barriers than we think.
Much of what we teach about physical diagnosis is imperfect,5 and the routine annual exam might well be eliminated given its low yield.6 Nevertheless, we cannot discount the importance of the physical exam in fostering the bond between the patient and the healthcare provider, particularly in patients with acute illnesses, and in making the interaction meaningful to the practitioner.
Many of us can easily recall embarrassing examples of obvious physical exam findings that were critical and overlooked with consequences – the missed incarcerated hernia in a patient labeled with gastritis and vomiting, or the patient with chest pain who had to undergo catheterization because the shingles rash was missed. The confidence in normal findings that might save a patient from unnecessary lab tests, imaging, or consultation is often not discussed. The burden is on us to retire maneuvers that have outlived their usefulness and to demonstrate to students the hazards and consequences of poor examination skills. We must also further what we know and understand about the physical exam as Osler, Laennec, and others before us once did. Point-of-care ultrasound is only one example of how innovation can bring trainees to the bedside, excite learners, engage patients, and affect care in a meaningful way while enhancing the nonultrasound-based skills of practitioners.7
It is promising that the students in this study consistently examined their patients each day. As future physicians, they can be very enthusiastic learners eager to apply the physical exam skills they have recently acquired during their early years of training. However, this excitement can taper off if not actively encouraged and reinforced, especially if role models are unintentionally sending the message that the physical exam does not matter or emphasizing exam maneuvers that do not serve a meaningful purpose. New technology will hopefully help us develop novel exam skills. If we can advance what we can diagnose at the bedside, students will remain motivated to improve and learn exam skills that truly affect patient-care decisions. After all, one day, they too will serve as role models for the next generation of physicians and hopefully will be the ones taking care of us at the bedside.
Disclosures
The authors declare no conflicts of interest.
1. Bergl PA, Taylor AC, Klumb J, et al. Teaching physical examination to medical students on inpatient medicine reams: A prospective mixed-methods descriptive study. J Hosp Med. 2018;13:399-402. PubMed
2. Chi J, Verghese A. Clinical education and the electronic health record: the flipped patient. JAMA. 2010;312(22):2331-2332. DOI: 10.1001/jama.2014.12820. PubMed
2. Verghese A. Culture shock—patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. DOI: 10.1056/NEJMp0807461 PubMed
3. Czernik Z, Lin CT. A piece of my mind. Time at the bedside (Computing). JAMA. 2016;315(22):2399-2400. DOI: 10.1001/jama.2016.1722 PubMed
5. Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548-551. DOI: 10.1056/NEJMp068013 PubMed
6. Mehrotra A, Prochazka A. Improving value in health care--against the annual physical. N Engl J Med. 2015;373(16):1485-1487. DOI: 10.1056/NEJMp1507485 PubMed
7. Kugler J. Price and the evolution of the physical examination. JAMA Cardiol. 2018. DOI: 10.1001/jamacardio.2018.0002. [Epub ahead of print] PubMed
“Am I supposed to have such a hard time feeling the kidneys?” “I think I’m doing it wrong,” echoed another classmate. The frustration of these first-year students, who were already overwhelmed by the three pages of physical exam techniques that they were responsible for, became increasingly visible as they palpated the abdomens of their standardized patients. Then, they asked the dreaded question: “How often do you do this on real patients?”
When we teach first-year medical students the physical exam, these students are already aware that they have never observed physicians perform these maneuvers in their own medical care. “How come I’ve never seen my doctor do this before?” is a common question that we are often asked. We as faculty struggle with demonstrating and defending techniques that we hardly ever use given their variable utility in daily clinical practice. However, students are told that they must be familiar with the various “tools” in the repertoire, and they are led to believe that these skills will be a fundamental part of their future practice as physicians. Of course, when they begin their clerkships, the truth is revealed: the currency on the wards revolves around the computer. The experienced and passionate clinicians who may astonish them with the bedside exam are the exception and are hardly the rule.
In this issue of Journal of Hospital Medicine, Bergl et al.1 found that when medical students rotated on their internal medicine clerkship, patients were rarely examined during attending rounds and were even examined less often when these rounds were not at the bedside. Although the students themselves consistently incorporated the physical exam into patient assessments and presentations, neither their findings nor those of the residents were ever validated by the attending physician or by others. Notably, the physical exam did not influence clinical decision making as much as one might expect.
These findings should not come as a surprise. The current generation of residents and junior attendings today are more accustomed to emphasizing labs, imaging studies, pathology reports, and other data within the electronic health record (EHR) and with formulating initial plans before having met the patient.2 Physicians become uneasy when asked to decide without the reassurance of daily lab results, as if the information in the EHR is highly fundamental to patient care. Caring for the “iPatient” often trumps revisiting and reexamining the real patient.3 Medical teams are also bombarded with increasing demands for their attention and time and are pushed to expedite patient discharges while constantly responding to documentation queries in the EHR. Emphasis on patient throughput, quality metrics, and multidisciplinary communication is essential to provide effective patient care but often feels at odds with opportunities for bedside teaching.
Although discussions on these obstacles have increased in recent years, time-motion studies spanning decades and even preceding the duty-hours era have consistently shown that physicians reserve little time for physical examination and direct patient care.4 In other words, the challenges in bringing physicians to the bedside might have less to do with environmental barriers than we think.
Much of what we teach about physical diagnosis is imperfect,5 and the routine annual exam might well be eliminated given its low yield.6 Nevertheless, we cannot discount the importance of the physical exam in fostering the bond between the patient and the healthcare provider, particularly in patients with acute illnesses, and in making the interaction meaningful to the practitioner.
Many of us can easily recall embarrassing examples of obvious physical exam findings that were critical and overlooked with consequences – the missed incarcerated hernia in a patient labeled with gastritis and vomiting, or the patient with chest pain who had to undergo catheterization because the shingles rash was missed. The confidence in normal findings that might save a patient from unnecessary lab tests, imaging, or consultation is often not discussed. The burden is on us to retire maneuvers that have outlived their usefulness and to demonstrate to students the hazards and consequences of poor examination skills. We must also further what we know and understand about the physical exam as Osler, Laennec, and others before us once did. Point-of-care ultrasound is only one example of how innovation can bring trainees to the bedside, excite learners, engage patients, and affect care in a meaningful way while enhancing the nonultrasound-based skills of practitioners.7
It is promising that the students in this study consistently examined their patients each day. As future physicians, they can be very enthusiastic learners eager to apply the physical exam skills they have recently acquired during their early years of training. However, this excitement can taper off if not actively encouraged and reinforced, especially if role models are unintentionally sending the message that the physical exam does not matter or emphasizing exam maneuvers that do not serve a meaningful purpose. New technology will hopefully help us develop novel exam skills. If we can advance what we can diagnose at the bedside, students will remain motivated to improve and learn exam skills that truly affect patient-care decisions. After all, one day, they too will serve as role models for the next generation of physicians and hopefully will be the ones taking care of us at the bedside.
Disclosures
The authors declare no conflicts of interest.
“Am I supposed to have such a hard time feeling the kidneys?” “I think I’m doing it wrong,” echoed another classmate. The frustration of these first-year students, who were already overwhelmed by the three pages of physical exam techniques that they were responsible for, became increasingly visible as they palpated the abdomens of their standardized patients. Then, they asked the dreaded question: “How often do you do this on real patients?”
When we teach first-year medical students the physical exam, these students are already aware that they have never observed physicians perform these maneuvers in their own medical care. “How come I’ve never seen my doctor do this before?” is a common question that we are often asked. We as faculty struggle with demonstrating and defending techniques that we hardly ever use given their variable utility in daily clinical practice. However, students are told that they must be familiar with the various “tools” in the repertoire, and they are led to believe that these skills will be a fundamental part of their future practice as physicians. Of course, when they begin their clerkships, the truth is revealed: the currency on the wards revolves around the computer. The experienced and passionate clinicians who may astonish them with the bedside exam are the exception and are hardly the rule.
In this issue of Journal of Hospital Medicine, Bergl et al.1 found that when medical students rotated on their internal medicine clerkship, patients were rarely examined during attending rounds and were even examined less often when these rounds were not at the bedside. Although the students themselves consistently incorporated the physical exam into patient assessments and presentations, neither their findings nor those of the residents were ever validated by the attending physician or by others. Notably, the physical exam did not influence clinical decision making as much as one might expect.
These findings should not come as a surprise. The current generation of residents and junior attendings today are more accustomed to emphasizing labs, imaging studies, pathology reports, and other data within the electronic health record (EHR) and with formulating initial plans before having met the patient.2 Physicians become uneasy when asked to decide without the reassurance of daily lab results, as if the information in the EHR is highly fundamental to patient care. Caring for the “iPatient” often trumps revisiting and reexamining the real patient.3 Medical teams are also bombarded with increasing demands for their attention and time and are pushed to expedite patient discharges while constantly responding to documentation queries in the EHR. Emphasis on patient throughput, quality metrics, and multidisciplinary communication is essential to provide effective patient care but often feels at odds with opportunities for bedside teaching.
Although discussions on these obstacles have increased in recent years, time-motion studies spanning decades and even preceding the duty-hours era have consistently shown that physicians reserve little time for physical examination and direct patient care.4 In other words, the challenges in bringing physicians to the bedside might have less to do with environmental barriers than we think.
Much of what we teach about physical diagnosis is imperfect,5 and the routine annual exam might well be eliminated given its low yield.6 Nevertheless, we cannot discount the importance of the physical exam in fostering the bond between the patient and the healthcare provider, particularly in patients with acute illnesses, and in making the interaction meaningful to the practitioner.
Many of us can easily recall embarrassing examples of obvious physical exam findings that were critical and overlooked with consequences – the missed incarcerated hernia in a patient labeled with gastritis and vomiting, or the patient with chest pain who had to undergo catheterization because the shingles rash was missed. The confidence in normal findings that might save a patient from unnecessary lab tests, imaging, or consultation is often not discussed. The burden is on us to retire maneuvers that have outlived their usefulness and to demonstrate to students the hazards and consequences of poor examination skills. We must also further what we know and understand about the physical exam as Osler, Laennec, and others before us once did. Point-of-care ultrasound is only one example of how innovation can bring trainees to the bedside, excite learners, engage patients, and affect care in a meaningful way while enhancing the nonultrasound-based skills of practitioners.7
It is promising that the students in this study consistently examined their patients each day. As future physicians, they can be very enthusiastic learners eager to apply the physical exam skills they have recently acquired during their early years of training. However, this excitement can taper off if not actively encouraged and reinforced, especially if role models are unintentionally sending the message that the physical exam does not matter or emphasizing exam maneuvers that do not serve a meaningful purpose. New technology will hopefully help us develop novel exam skills. If we can advance what we can diagnose at the bedside, students will remain motivated to improve and learn exam skills that truly affect patient-care decisions. After all, one day, they too will serve as role models for the next generation of physicians and hopefully will be the ones taking care of us at the bedside.
Disclosures
The authors declare no conflicts of interest.
1. Bergl PA, Taylor AC, Klumb J, et al. Teaching physical examination to medical students on inpatient medicine reams: A prospective mixed-methods descriptive study. J Hosp Med. 2018;13:399-402. PubMed
2. Chi J, Verghese A. Clinical education and the electronic health record: the flipped patient. JAMA. 2010;312(22):2331-2332. DOI: 10.1001/jama.2014.12820. PubMed
2. Verghese A. Culture shock—patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. DOI: 10.1056/NEJMp0807461 PubMed
3. Czernik Z, Lin CT. A piece of my mind. Time at the bedside (Computing). JAMA. 2016;315(22):2399-2400. DOI: 10.1001/jama.2016.1722 PubMed
5. Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548-551. DOI: 10.1056/NEJMp068013 PubMed
6. Mehrotra A, Prochazka A. Improving value in health care--against the annual physical. N Engl J Med. 2015;373(16):1485-1487. DOI: 10.1056/NEJMp1507485 PubMed
7. Kugler J. Price and the evolution of the physical examination. JAMA Cardiol. 2018. DOI: 10.1001/jamacardio.2018.0002. [Epub ahead of print] PubMed
1. Bergl PA, Taylor AC, Klumb J, et al. Teaching physical examination to medical students on inpatient medicine reams: A prospective mixed-methods descriptive study. J Hosp Med. 2018;13:399-402. PubMed
2. Chi J, Verghese A. Clinical education and the electronic health record: the flipped patient. JAMA. 2010;312(22):2331-2332. DOI: 10.1001/jama.2014.12820. PubMed
2. Verghese A. Culture shock—patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. DOI: 10.1056/NEJMp0807461 PubMed
3. Czernik Z, Lin CT. A piece of my mind. Time at the bedside (Computing). JAMA. 2016;315(22):2399-2400. DOI: 10.1001/jama.2016.1722 PubMed
5. Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548-551. DOI: 10.1056/NEJMp068013 PubMed
6. Mehrotra A, Prochazka A. Improving value in health care--against the annual physical. N Engl J Med. 2015;373(16):1485-1487. DOI: 10.1056/NEJMp1507485 PubMed
7. Kugler J. Price and the evolution of the physical examination. JAMA Cardiol. 2018. DOI: 10.1001/jamacardio.2018.0002. [Epub ahead of print] PubMed
©2018 Society of Hospital Medicine
Faculty Development for Hospitalists: A Call to Arms
Over the past two decades, the field of hospital medicine has gone from relative obscurity to a viable career pathway for approximately 50,000 physicians in this country.1 A subset of hospitalists pursue careers in academic medicine, which is a pathway that traditionally includes education and scholarship in addition to patient care. While the academic career pathway is well paved in many clinical specialties, it is still relatively underdeveloped for academic hospitalists, and thus what defines career success for this group is even less clear.
In this issue of the Journal of Hospital Medicine, Cumbler et al. performed a qualitative analysis to explore how early career academic hospitalists self-define and perceive their career success.2 Drawing on interviews with 17 early-career hospitalists at 3 academic medical centers, the authors created a theoretical framework organized around a traditional conceptual model of career success that is divided into intrinsic and extrinsic motivating factors. They found that early-career academic hospitalists, (clinician-educators in first 2-5 years), defined their career success almost exclusively around factors intrinsic to their day-to-day job. These factors included such things as excitement about their daily work, developing proficiency in the delivery of high-quality clinical care, and passion for doing work that is meaningful to them. In addition to these immediate job satisfiers, many hospitalists emphasized long-term career success factors such as becoming an expert in a particular domain of hospital medicine and gaining respect and recognition within their local or national environment. Surprisingly, compensation and career advancement through promotion, two traditional external career success factors, were not uniformly valued.
These findings come at a critical time for our field in which early-career faculty outnumber mid- and late-career faculty by an order of magnitude. Indeed, how to develop, promote, sustain, and retain young hospitalists is a topic on the minds of most hospital medicine group directors. Putting aside the impact of hospitalist turnover on productivity, patient care outcomes, and morale within an individual hospital medicine group, we agree with the authors that understanding and cultivating career success for academic hospitalists is imperative for the future of our field. For this reason, we launched a formal faculty development program at Penn this year, which focuses on supporting the growth of hospitalists in their first two years on faculty. The findings of this study provide interesting new perspectives and encourage us to continue our focus on early-career academic hospitalists. We laud the previous efforts in this area and hope that the paper by Cumbler et al. encourages and inspires other programs to start or accelerate their hospitalist faculty development efforts.3-5
However, some findings from this study are somewhat perplexing or even a bit discouraging for those who are invested in faculty development in academia. For example, the authors raise the possibility that there may be a disconnect in the minds of early-career hospitalists as it pertains to their thoughts on career success. On the one hand, the hospitalists interviewed in this study are happy doing their clinical work and cite this as a primary driver of their career success. On the other hand, they equate career success with things such as developing expertise within a particular domain of hospital medicine, acquiring leadership roles, collaborating academically with other specialties or professions, or developing new innovations. Presumably this is part of the reason that they selected a job in an academic setting as opposed to a community setting. However, in order to achieve these goals, one must devote time and effort to purposefully developing them. Therefore, identifying and developing mentors who can assist early-career hospitalists with identifying, articulating, and developing strategies to achieve both their short- and long-term career goals is critical. One mentor–mentee conversation may reveal that an individual hospitalist values being an excellent clinician and has little interest in developing a niche within hospital medicine; another may reveal a lack of awareness of available professional development resources; still another may uncover a lack of realism regarding the time or skills it takes to achieve a particular career goal. These realities highlight an imperative for our field to develop robust and sustainable mentorship programs for not only early-career hospitalists but also some mid-career hospitalists whose careers may not yet be fully developed. Indeed, one of the biggest challenges that have emerged in our experience with a faculty development program at Penn is creating meaningful mentorship and career development advice for mid-career hospitalists (late assistant or early associate professors who are typically 5-10 years into their careers).
We found it interesting that the hospitalists interviewed did not mention three of the four pillars of career satisfaction outlined in the white paper on Hospitalist Career Satisfaction from the Society for Hospital Medicine: workload schedule, autonomy control, and community/environment.6 Perhaps this is because hospitalists, like many other professionals, recognize that feeling satisfied in one’s career is not the same as feeling successful. Satisfaction in one’s career refers to the foundational needs that one requires in order to feel content, whereas success is more often equated with achievement, even if that achievement is simply the acquisition of one’s goals for themselves. The reality is that given the constant growth and change within teaching hospitals, and therefore academic hospital medicine groups, tending to the satisfiers for hospitalists (eg, schedule and workload) often takes a front seat to assisting faculty in achieving their individual career potential. We assert that despite the inherent difficulty, academic hospital medicine group leaders need to focus their attention on both the satisfaction and career success of their early-career faculty.
Finally, this paper raises many interesting questions
In conclusion, the findings of Cumbler et al. should promote unrest among leaders of academic hospital medicine groups and their departments of medicine. While it is inspiring to see so many early-career hospitalists focused on their daily happiness at work, we are unsure about whether they have the knowledge, tools, and guidance to achieve their self-professed academic goals, which many equate with career success. Given the continued growth of the hospital medicine workforce, we view this important new work as a national call to arms for the purposeful development of academic hospitalist faculty development programs.
Disclosures
Dr. Myers and Dr. Greysen have nothing to disclose.
1. Wachter RM, Goldman L. Zero to 50,000-The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. PubMed
2. Cumbler E, Yirdaw E, Kneeland P, et al. What is career success for academic hospitalists? A qualitative analysis of early-career faculty perspectives. J Hosp Med. 2018;13(5):372-377. doi: 10.12788/jhm.2924. Published online first January 31, 2018. PubMed
3. Nagarur A, O’Neill RM, Lawton D, Greenwald JL. Supporting faculty development in hospital medicine: design and implementation of a personalized structured mentoring program. J Hosp Med. 2018;13(2):96-99. PubMed
4. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. PubMed
5. Howell E, Kravet S, Kisuule F, Wright SM. An innovative approach to supporting hospitalist physicians towards academic success. J Hosp Med. 2008;3(4):314-318. PubMed
6. Society of Hospital Medicine Career Satisfaction Taskforce: A Challenge for a new Specialty. A White paper on hospitalist career satisfaction. http://dev.hospitalmedicine.org/Web/Media_Center/shm_white_papers.aspx . Accessed February 9, 2018.
Over the past two decades, the field of hospital medicine has gone from relative obscurity to a viable career pathway for approximately 50,000 physicians in this country.1 A subset of hospitalists pursue careers in academic medicine, which is a pathway that traditionally includes education and scholarship in addition to patient care. While the academic career pathway is well paved in many clinical specialties, it is still relatively underdeveloped for academic hospitalists, and thus what defines career success for this group is even less clear.
In this issue of the Journal of Hospital Medicine, Cumbler et al. performed a qualitative analysis to explore how early career academic hospitalists self-define and perceive their career success.2 Drawing on interviews with 17 early-career hospitalists at 3 academic medical centers, the authors created a theoretical framework organized around a traditional conceptual model of career success that is divided into intrinsic and extrinsic motivating factors. They found that early-career academic hospitalists, (clinician-educators in first 2-5 years), defined their career success almost exclusively around factors intrinsic to their day-to-day job. These factors included such things as excitement about their daily work, developing proficiency in the delivery of high-quality clinical care, and passion for doing work that is meaningful to them. In addition to these immediate job satisfiers, many hospitalists emphasized long-term career success factors such as becoming an expert in a particular domain of hospital medicine and gaining respect and recognition within their local or national environment. Surprisingly, compensation and career advancement through promotion, two traditional external career success factors, were not uniformly valued.
These findings come at a critical time for our field in which early-career faculty outnumber mid- and late-career faculty by an order of magnitude. Indeed, how to develop, promote, sustain, and retain young hospitalists is a topic on the minds of most hospital medicine group directors. Putting aside the impact of hospitalist turnover on productivity, patient care outcomes, and morale within an individual hospital medicine group, we agree with the authors that understanding and cultivating career success for academic hospitalists is imperative for the future of our field. For this reason, we launched a formal faculty development program at Penn this year, which focuses on supporting the growth of hospitalists in their first two years on faculty. The findings of this study provide interesting new perspectives and encourage us to continue our focus on early-career academic hospitalists. We laud the previous efforts in this area and hope that the paper by Cumbler et al. encourages and inspires other programs to start or accelerate their hospitalist faculty development efforts.3-5
However, some findings from this study are somewhat perplexing or even a bit discouraging for those who are invested in faculty development in academia. For example, the authors raise the possibility that there may be a disconnect in the minds of early-career hospitalists as it pertains to their thoughts on career success. On the one hand, the hospitalists interviewed in this study are happy doing their clinical work and cite this as a primary driver of their career success. On the other hand, they equate career success with things such as developing expertise within a particular domain of hospital medicine, acquiring leadership roles, collaborating academically with other specialties or professions, or developing new innovations. Presumably this is part of the reason that they selected a job in an academic setting as opposed to a community setting. However, in order to achieve these goals, one must devote time and effort to purposefully developing them. Therefore, identifying and developing mentors who can assist early-career hospitalists with identifying, articulating, and developing strategies to achieve both their short- and long-term career goals is critical. One mentor–mentee conversation may reveal that an individual hospitalist values being an excellent clinician and has little interest in developing a niche within hospital medicine; another may reveal a lack of awareness of available professional development resources; still another may uncover a lack of realism regarding the time or skills it takes to achieve a particular career goal. These realities highlight an imperative for our field to develop robust and sustainable mentorship programs for not only early-career hospitalists but also some mid-career hospitalists whose careers may not yet be fully developed. Indeed, one of the biggest challenges that have emerged in our experience with a faculty development program at Penn is creating meaningful mentorship and career development advice for mid-career hospitalists (late assistant or early associate professors who are typically 5-10 years into their careers).
We found it interesting that the hospitalists interviewed did not mention three of the four pillars of career satisfaction outlined in the white paper on Hospitalist Career Satisfaction from the Society for Hospital Medicine: workload schedule, autonomy control, and community/environment.6 Perhaps this is because hospitalists, like many other professionals, recognize that feeling satisfied in one’s career is not the same as feeling successful. Satisfaction in one’s career refers to the foundational needs that one requires in order to feel content, whereas success is more often equated with achievement, even if that achievement is simply the acquisition of one’s goals for themselves. The reality is that given the constant growth and change within teaching hospitals, and therefore academic hospital medicine groups, tending to the satisfiers for hospitalists (eg, schedule and workload) often takes a front seat to assisting faculty in achieving their individual career potential. We assert that despite the inherent difficulty, academic hospital medicine group leaders need to focus their attention on both the satisfaction and career success of their early-career faculty.
Finally, this paper raises many interesting questions
In conclusion, the findings of Cumbler et al. should promote unrest among leaders of academic hospital medicine groups and their departments of medicine. While it is inspiring to see so many early-career hospitalists focused on their daily happiness at work, we are unsure about whether they have the knowledge, tools, and guidance to achieve their self-professed academic goals, which many equate with career success. Given the continued growth of the hospital medicine workforce, we view this important new work as a national call to arms for the purposeful development of academic hospitalist faculty development programs.
Disclosures
Dr. Myers and Dr. Greysen have nothing to disclose.
Over the past two decades, the field of hospital medicine has gone from relative obscurity to a viable career pathway for approximately 50,000 physicians in this country.1 A subset of hospitalists pursue careers in academic medicine, which is a pathway that traditionally includes education and scholarship in addition to patient care. While the academic career pathway is well paved in many clinical specialties, it is still relatively underdeveloped for academic hospitalists, and thus what defines career success for this group is even less clear.
In this issue of the Journal of Hospital Medicine, Cumbler et al. performed a qualitative analysis to explore how early career academic hospitalists self-define and perceive their career success.2 Drawing on interviews with 17 early-career hospitalists at 3 academic medical centers, the authors created a theoretical framework organized around a traditional conceptual model of career success that is divided into intrinsic and extrinsic motivating factors. They found that early-career academic hospitalists, (clinician-educators in first 2-5 years), defined their career success almost exclusively around factors intrinsic to their day-to-day job. These factors included such things as excitement about their daily work, developing proficiency in the delivery of high-quality clinical care, and passion for doing work that is meaningful to them. In addition to these immediate job satisfiers, many hospitalists emphasized long-term career success factors such as becoming an expert in a particular domain of hospital medicine and gaining respect and recognition within their local or national environment. Surprisingly, compensation and career advancement through promotion, two traditional external career success factors, were not uniformly valued.
These findings come at a critical time for our field in which early-career faculty outnumber mid- and late-career faculty by an order of magnitude. Indeed, how to develop, promote, sustain, and retain young hospitalists is a topic on the minds of most hospital medicine group directors. Putting aside the impact of hospitalist turnover on productivity, patient care outcomes, and morale within an individual hospital medicine group, we agree with the authors that understanding and cultivating career success for academic hospitalists is imperative for the future of our field. For this reason, we launched a formal faculty development program at Penn this year, which focuses on supporting the growth of hospitalists in their first two years on faculty. The findings of this study provide interesting new perspectives and encourage us to continue our focus on early-career academic hospitalists. We laud the previous efforts in this area and hope that the paper by Cumbler et al. encourages and inspires other programs to start or accelerate their hospitalist faculty development efforts.3-5
However, some findings from this study are somewhat perplexing or even a bit discouraging for those who are invested in faculty development in academia. For example, the authors raise the possibility that there may be a disconnect in the minds of early-career hospitalists as it pertains to their thoughts on career success. On the one hand, the hospitalists interviewed in this study are happy doing their clinical work and cite this as a primary driver of their career success. On the other hand, they equate career success with things such as developing expertise within a particular domain of hospital medicine, acquiring leadership roles, collaborating academically with other specialties or professions, or developing new innovations. Presumably this is part of the reason that they selected a job in an academic setting as opposed to a community setting. However, in order to achieve these goals, one must devote time and effort to purposefully developing them. Therefore, identifying and developing mentors who can assist early-career hospitalists with identifying, articulating, and developing strategies to achieve both their short- and long-term career goals is critical. One mentor–mentee conversation may reveal that an individual hospitalist values being an excellent clinician and has little interest in developing a niche within hospital medicine; another may reveal a lack of awareness of available professional development resources; still another may uncover a lack of realism regarding the time or skills it takes to achieve a particular career goal. These realities highlight an imperative for our field to develop robust and sustainable mentorship programs for not only early-career hospitalists but also some mid-career hospitalists whose careers may not yet be fully developed. Indeed, one of the biggest challenges that have emerged in our experience with a faculty development program at Penn is creating meaningful mentorship and career development advice for mid-career hospitalists (late assistant or early associate professors who are typically 5-10 years into their careers).
We found it interesting that the hospitalists interviewed did not mention three of the four pillars of career satisfaction outlined in the white paper on Hospitalist Career Satisfaction from the Society for Hospital Medicine: workload schedule, autonomy control, and community/environment.6 Perhaps this is because hospitalists, like many other professionals, recognize that feeling satisfied in one’s career is not the same as feeling successful. Satisfaction in one’s career refers to the foundational needs that one requires in order to feel content, whereas success is more often equated with achievement, even if that achievement is simply the acquisition of one’s goals for themselves. The reality is that given the constant growth and change within teaching hospitals, and therefore academic hospital medicine groups, tending to the satisfiers for hospitalists (eg, schedule and workload) often takes a front seat to assisting faculty in achieving their individual career potential. We assert that despite the inherent difficulty, academic hospital medicine group leaders need to focus their attention on both the satisfaction and career success of their early-career faculty.
Finally, this paper raises many interesting questions
In conclusion, the findings of Cumbler et al. should promote unrest among leaders of academic hospital medicine groups and their departments of medicine. While it is inspiring to see so many early-career hospitalists focused on their daily happiness at work, we are unsure about whether they have the knowledge, tools, and guidance to achieve their self-professed academic goals, which many equate with career success. Given the continued growth of the hospital medicine workforce, we view this important new work as a national call to arms for the purposeful development of academic hospitalist faculty development programs.
Disclosures
Dr. Myers and Dr. Greysen have nothing to disclose.
1. Wachter RM, Goldman L. Zero to 50,000-The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. PubMed
2. Cumbler E, Yirdaw E, Kneeland P, et al. What is career success for academic hospitalists? A qualitative analysis of early-career faculty perspectives. J Hosp Med. 2018;13(5):372-377. doi: 10.12788/jhm.2924. Published online first January 31, 2018. PubMed
3. Nagarur A, O’Neill RM, Lawton D, Greenwald JL. Supporting faculty development in hospital medicine: design and implementation of a personalized structured mentoring program. J Hosp Med. 2018;13(2):96-99. PubMed
4. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. PubMed
5. Howell E, Kravet S, Kisuule F, Wright SM. An innovative approach to supporting hospitalist physicians towards academic success. J Hosp Med. 2008;3(4):314-318. PubMed
6. Society of Hospital Medicine Career Satisfaction Taskforce: A Challenge for a new Specialty. A White paper on hospitalist career satisfaction. http://dev.hospitalmedicine.org/Web/Media_Center/shm_white_papers.aspx . Accessed February 9, 2018.
1. Wachter RM, Goldman L. Zero to 50,000-The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. PubMed
2. Cumbler E, Yirdaw E, Kneeland P, et al. What is career success for academic hospitalists? A qualitative analysis of early-career faculty perspectives. J Hosp Med. 2018;13(5):372-377. doi: 10.12788/jhm.2924. Published online first January 31, 2018. PubMed
3. Nagarur A, O’Neill RM, Lawton D, Greenwald JL. Supporting faculty development in hospital medicine: design and implementation of a personalized structured mentoring program. J Hosp Med. 2018;13(2):96-99. PubMed
4. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. PubMed
5. Howell E, Kravet S, Kisuule F, Wright SM. An innovative approach to supporting hospitalist physicians towards academic success. J Hosp Med. 2008;3(4):314-318. PubMed
6. Society of Hospital Medicine Career Satisfaction Taskforce: A Challenge for a new Specialty. A White paper on hospitalist career satisfaction. http://dev.hospitalmedicine.org/Web/Media_Center/shm_white_papers.aspx . Accessed February 9, 2018.
©2018 Society of Hospital Medicine