User login
For HPV-negative women, longer screening intervals are effective
It may be safe to extend cervical cancer screening intervals beyond 5 years, at least for women who are not infected with human papillomavirus.
The rate of cervical cancers was the same among HPV-negative women, whether they had gone through two or three rounds of 5-year exams using both HPV testing and cervical cytology, a large Dutch study has found. This suggests a longer period between screenings wouldn’t significantly increase the risk of letting new cancers go unnoticed, Maaike G Dijkstra, MD, and associates reported (BMJ. 2016;355:i4924. doi: 10.1136/bmj.i4924).
The picture, however, is very different for women with an HPV infection, the researchers noted. These women were 12 times more likely to develop cervical cancer and up to 29 times more likely to have a cervical intraepithelial neoplasia of at least grade 3 (CIN3+), compared with women who were HPV negative.
The findings bring a measure of reassurance to the Dutch population, the researchers wrote. The Netherlands intends to lengthen its cervical cancer screening interval to 10 years for HPV-negative women aged 40 years or older.
“HPV-negative women have a very low risk of CIN3+ in the long term, indicating that extension of the current screening interval in the Netherlands to 10 years seems justifiable,” wrote Dr. Dijkstra of the VU University Medical Centre, Amsterdam, and her colleagues. “For HPV positive, triage negative women, the long term risk of CIN3+ was too high to support an extension of the screening interval beyond 5 years.”
The study assessed the 14-year risks of cervical cancer and CIN3+ in 43,339 women aged 29 years and older. As per national guidelines, all women underwent cervical cancer screening every 5 years, resulting in three rounds. They were randomized to receive HPV and cytology testing or cytology only.
Among HPV-negative women in the double-screening group, the cumulative cervical cancer incidence was 0.03% after round two and 0.09% after round three – not a statistically significant difference.
After round three, cervical cancer incidence among HPV-negative women with negative cytology (double negative) was similar to that among cytology-negative women from the control group after round two.
In the cytology-only group, the rates among negative women were 0.09% after round two of screening and 0.19% after round three.
“This indicated that a negative HPV test provides longer reassurance against cervical cancer than negative cytology,” the researchers noted.
HPV-positive women, however, faced much higher risks, regardless of the screening protocol. Even with negative cytology, they were 12 times more likely to have a cancer by round three than HPV-negative women. The risk of CIN3+ was up to 29 times higher. Even HPV-positive women with negative cytology, negative HPV 16/18 genotyping, and negative repeat cytology faced a 10-fold increased risk of CIN+3, the researchers reported.
Dr. Dijkstra reported having no financial disclosures. Several of the coauthors disclosed financial relationships with various pharmaceutical companies.
[email protected]
On Twitter @Alz_Gal
The ultimate goal of cervical cancer screening is to minimize unnecessary procedures while maximizing identification of preinvasive disease. The recent article by Dr. Dijkstra and her associates provides 14-year follow-up for a national population-based cervical screening randomized trial.
The authors, who focused their analysis on patients older than age 40, describe how HPV results allow for a more targeted intervention triage than cytology alone. The study is impressive in its large patient cohort and extremely low detection rate of cervical cancer among HPV-negative patients in the intervention group. Their main argument stems from identifying an equivalent risk for CIN3+ between patients who were negative for HPV at 10 years and those with negative cytology at 5 years.
In the United States, current guidelines endorse cotesting for patients in this age group, with a negative cotest requiring repeat testing at 5 years. Changes to the screening protocol in the United States are often met with skepticism and slow uptake. This study certainly shows strong data to support HPV testing as the preferred option, but when does the time gap between screenings become too large, particularly for women whose only health care evaluation is through the gynecologist? Patients often think that not needing yearly Pap test equates to no need for routine examinations. We may be missing out on the opportunity to not only grow the patient-physician relationship, but also impact other aspects of the patients’ general health.
This article may not change practice, but it does add considerable weight to the growing literature on primary HPV screening, especially in an older population.
Ritu Salani, MD, is associate professor of gynecologic oncology at Ohio State University in Columbus. Robert T. Neff, MD, is a second-year fellow in gynecologic oncology at the university. They reported having no relevant financial disclosures.
The ultimate goal of cervical cancer screening is to minimize unnecessary procedures while maximizing identification of preinvasive disease. The recent article by Dr. Dijkstra and her associates provides 14-year follow-up for a national population-based cervical screening randomized trial.
The authors, who focused their analysis on patients older than age 40, describe how HPV results allow for a more targeted intervention triage than cytology alone. The study is impressive in its large patient cohort and extremely low detection rate of cervical cancer among HPV-negative patients in the intervention group. Their main argument stems from identifying an equivalent risk for CIN3+ between patients who were negative for HPV at 10 years and those with negative cytology at 5 years.
In the United States, current guidelines endorse cotesting for patients in this age group, with a negative cotest requiring repeat testing at 5 years. Changes to the screening protocol in the United States are often met with skepticism and slow uptake. This study certainly shows strong data to support HPV testing as the preferred option, but when does the time gap between screenings become too large, particularly for women whose only health care evaluation is through the gynecologist? Patients often think that not needing yearly Pap test equates to no need for routine examinations. We may be missing out on the opportunity to not only grow the patient-physician relationship, but also impact other aspects of the patients’ general health.
This article may not change practice, but it does add considerable weight to the growing literature on primary HPV screening, especially in an older population.
Ritu Salani, MD, is associate professor of gynecologic oncology at Ohio State University in Columbus. Robert T. Neff, MD, is a second-year fellow in gynecologic oncology at the university. They reported having no relevant financial disclosures.
The ultimate goal of cervical cancer screening is to minimize unnecessary procedures while maximizing identification of preinvasive disease. The recent article by Dr. Dijkstra and her associates provides 14-year follow-up for a national population-based cervical screening randomized trial.
The authors, who focused their analysis on patients older than age 40, describe how HPV results allow for a more targeted intervention triage than cytology alone. The study is impressive in its large patient cohort and extremely low detection rate of cervical cancer among HPV-negative patients in the intervention group. Their main argument stems from identifying an equivalent risk for CIN3+ between patients who were negative for HPV at 10 years and those with negative cytology at 5 years.
In the United States, current guidelines endorse cotesting for patients in this age group, with a negative cotest requiring repeat testing at 5 years. Changes to the screening protocol in the United States are often met with skepticism and slow uptake. This study certainly shows strong data to support HPV testing as the preferred option, but when does the time gap between screenings become too large, particularly for women whose only health care evaluation is through the gynecologist? Patients often think that not needing yearly Pap test equates to no need for routine examinations. We may be missing out on the opportunity to not only grow the patient-physician relationship, but also impact other aspects of the patients’ general health.
This article may not change practice, but it does add considerable weight to the growing literature on primary HPV screening, especially in an older population.
Ritu Salani, MD, is associate professor of gynecologic oncology at Ohio State University in Columbus. Robert T. Neff, MD, is a second-year fellow in gynecologic oncology at the university. They reported having no relevant financial disclosures.
It may be safe to extend cervical cancer screening intervals beyond 5 years, at least for women who are not infected with human papillomavirus.
The rate of cervical cancers was the same among HPV-negative women, whether they had gone through two or three rounds of 5-year exams using both HPV testing and cervical cytology, a large Dutch study has found. This suggests a longer period between screenings wouldn’t significantly increase the risk of letting new cancers go unnoticed, Maaike G Dijkstra, MD, and associates reported (BMJ. 2016;355:i4924. doi: 10.1136/bmj.i4924).
The picture, however, is very different for women with an HPV infection, the researchers noted. These women were 12 times more likely to develop cervical cancer and up to 29 times more likely to have a cervical intraepithelial neoplasia of at least grade 3 (CIN3+), compared with women who were HPV negative.
The findings bring a measure of reassurance to the Dutch population, the researchers wrote. The Netherlands intends to lengthen its cervical cancer screening interval to 10 years for HPV-negative women aged 40 years or older.
“HPV-negative women have a very low risk of CIN3+ in the long term, indicating that extension of the current screening interval in the Netherlands to 10 years seems justifiable,” wrote Dr. Dijkstra of the VU University Medical Centre, Amsterdam, and her colleagues. “For HPV positive, triage negative women, the long term risk of CIN3+ was too high to support an extension of the screening interval beyond 5 years.”
The study assessed the 14-year risks of cervical cancer and CIN3+ in 43,339 women aged 29 years and older. As per national guidelines, all women underwent cervical cancer screening every 5 years, resulting in three rounds. They were randomized to receive HPV and cytology testing or cytology only.
Among HPV-negative women in the double-screening group, the cumulative cervical cancer incidence was 0.03% after round two and 0.09% after round three – not a statistically significant difference.
After round three, cervical cancer incidence among HPV-negative women with negative cytology (double negative) was similar to that among cytology-negative women from the control group after round two.
In the cytology-only group, the rates among negative women were 0.09% after round two of screening and 0.19% after round three.
“This indicated that a negative HPV test provides longer reassurance against cervical cancer than negative cytology,” the researchers noted.
HPV-positive women, however, faced much higher risks, regardless of the screening protocol. Even with negative cytology, they were 12 times more likely to have a cancer by round three than HPV-negative women. The risk of CIN3+ was up to 29 times higher. Even HPV-positive women with negative cytology, negative HPV 16/18 genotyping, and negative repeat cytology faced a 10-fold increased risk of CIN+3, the researchers reported.
Dr. Dijkstra reported having no financial disclosures. Several of the coauthors disclosed financial relationships with various pharmaceutical companies.
[email protected]
On Twitter @Alz_Gal
It may be safe to extend cervical cancer screening intervals beyond 5 years, at least for women who are not infected with human papillomavirus.
The rate of cervical cancers was the same among HPV-negative women, whether they had gone through two or three rounds of 5-year exams using both HPV testing and cervical cytology, a large Dutch study has found. This suggests a longer period between screenings wouldn’t significantly increase the risk of letting new cancers go unnoticed, Maaike G Dijkstra, MD, and associates reported (BMJ. 2016;355:i4924. doi: 10.1136/bmj.i4924).
The picture, however, is very different for women with an HPV infection, the researchers noted. These women were 12 times more likely to develop cervical cancer and up to 29 times more likely to have a cervical intraepithelial neoplasia of at least grade 3 (CIN3+), compared with women who were HPV negative.
The findings bring a measure of reassurance to the Dutch population, the researchers wrote. The Netherlands intends to lengthen its cervical cancer screening interval to 10 years for HPV-negative women aged 40 years or older.
“HPV-negative women have a very low risk of CIN3+ in the long term, indicating that extension of the current screening interval in the Netherlands to 10 years seems justifiable,” wrote Dr. Dijkstra of the VU University Medical Centre, Amsterdam, and her colleagues. “For HPV positive, triage negative women, the long term risk of CIN3+ was too high to support an extension of the screening interval beyond 5 years.”
The study assessed the 14-year risks of cervical cancer and CIN3+ in 43,339 women aged 29 years and older. As per national guidelines, all women underwent cervical cancer screening every 5 years, resulting in three rounds. They were randomized to receive HPV and cytology testing or cytology only.
Among HPV-negative women in the double-screening group, the cumulative cervical cancer incidence was 0.03% after round two and 0.09% after round three – not a statistically significant difference.
After round three, cervical cancer incidence among HPV-negative women with negative cytology (double negative) was similar to that among cytology-negative women from the control group after round two.
In the cytology-only group, the rates among negative women were 0.09% after round two of screening and 0.19% after round three.
“This indicated that a negative HPV test provides longer reassurance against cervical cancer than negative cytology,” the researchers noted.
HPV-positive women, however, faced much higher risks, regardless of the screening protocol. Even with negative cytology, they were 12 times more likely to have a cancer by round three than HPV-negative women. The risk of CIN3+ was up to 29 times higher. Even HPV-positive women with negative cytology, negative HPV 16/18 genotyping, and negative repeat cytology faced a 10-fold increased risk of CIN+3, the researchers reported.
Dr. Dijkstra reported having no financial disclosures. Several of the coauthors disclosed financial relationships with various pharmaceutical companies.
[email protected]
On Twitter @Alz_Gal
FROM BMJ
Key clinical point:
Major finding: The cumulative cervical cancer incidence was 0.03% after round two and 0.09% after round three – not a statistically significant difference.
Data source: The 14-year study randomized more than 43,000 women to either the double-method screen or just to cervical cytology.
Disclosures: Dr. Dijkstra reported having no financial disclosures. Several of the coauthors disclosed financial relationships with various pharmaceutical companies.
Rivaroxaban linked to more bleeding compared with dabigatran in elderly patients with nonvalvular AF
Rivaroxaban is associated with significantly more intra- and extracranial bleeding than is dabigatran in older patients who have nonvalvular atrial fibrillation, according to a report published online Oct. 3 in JAMA Internal Medicine.
This is the principal finding of a retrospective cohort study – the only study to directly compare the two oral non–vitamin-K-antagonists – that involved more than 118,000 patients who initiated anticoagulation treatment during a 2.5-year period. The Centers for Medicare & Medicaid Services and the Food and Drug Administration jointly conducted the study.
During the study period, rivaroxaban was used 2-3 times more often than was dabigatran in AF patients in the United States, “perhaps partly because of prescriber misperceptions about bleeding risks with dabigatran, arising from FDA receipt of a large number of postmarketing case reports following its approval. Ironically, we [now find] substantially higher bleeding risks with use of rivaroxaban than dabigatran,” said David J. Graham, MD, of the Office of Surveillance and Epidemiology, Center for Drug Evaluation and Research, FDA, Silver Spring, Md., and his associates.
The researchers assessed Medicare beneficiaries who initiated standard oral doses of rivaroxaban (66,651 patients) or dabigatran (52,240 patients) and were followed for a mean of 110 days.
The primary outcome measure – a composite of thromboembolic stroke, intracranial hemorrhage, major extracranial bleeding events including GI bleeding, and mortality – occurred in significantly more patients taking rivaroxaban than in those taking dabigatran. When the individual components of this composite outcome were considered, rivaroxaban was associated with significant increases in intracranial hemorrhage (HR, 1.65), major extracranial bleeding (HR, 1.48), and major GI bleeding (HR, 1.40); a nonsignificant decrease in thromboembolic stroke (HR, 0.81); and a nonsignificant increase in mortality (HR, 1.15).
In a further analysis of the data, rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment. In addition, rivaroxaban was associated with a significantly increased risk of death in two subgroups of patients: those aged 75 and older and those whose CHADS-2 scores indicated higher bleeding risk, Dr. Graham and his associates said (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.5954).
Of note, “the net increase in intracranial hemorrhage, the outcome with the highest case fatality rate, exceeded the net reduction in thromboembolic stroke” with rivaroxaban treatment, they added.
This “milestone” study offers real-world data for a large number of older patients with multiple comorbidities who constitute the rising tide of the AF population.
The findings should lead physicians to prescribe dabigatran over rivaroxaban in most patients with AF. Even though this was a retrospective cohort study, there are no prospective randomized trials directly comparing the two non–vitamin-K oral anticoagulants, and the few indirect comparisons derived from clinical trial data are very limited.
Anna L. Parks, MD, is at the University of California, San Francisco. Rita F. Redberg, M.D., is the editor of JAMA Internal Medicine and professor of cardiology at UCSF. Dr. Parks and Dr. Redberg made these remarks in an Editor’s Note accompanying Dr. Graham’s report (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.6429).
This “milestone” study offers real-world data for a large number of older patients with multiple comorbidities who constitute the rising tide of the AF population.
The findings should lead physicians to prescribe dabigatran over rivaroxaban in most patients with AF. Even though this was a retrospective cohort study, there are no prospective randomized trials directly comparing the two non–vitamin-K oral anticoagulants, and the few indirect comparisons derived from clinical trial data are very limited.
Anna L. Parks, MD, is at the University of California, San Francisco. Rita F. Redberg, M.D., is the editor of JAMA Internal Medicine and professor of cardiology at UCSF. Dr. Parks and Dr. Redberg made these remarks in an Editor’s Note accompanying Dr. Graham’s report (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.6429).
This “milestone” study offers real-world data for a large number of older patients with multiple comorbidities who constitute the rising tide of the AF population.
The findings should lead physicians to prescribe dabigatran over rivaroxaban in most patients with AF. Even though this was a retrospective cohort study, there are no prospective randomized trials directly comparing the two non–vitamin-K oral anticoagulants, and the few indirect comparisons derived from clinical trial data are very limited.
Anna L. Parks, MD, is at the University of California, San Francisco. Rita F. Redberg, M.D., is the editor of JAMA Internal Medicine and professor of cardiology at UCSF. Dr. Parks and Dr. Redberg made these remarks in an Editor’s Note accompanying Dr. Graham’s report (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.6429).
Rivaroxaban is associated with significantly more intra- and extracranial bleeding than is dabigatran in older patients who have nonvalvular atrial fibrillation, according to a report published online Oct. 3 in JAMA Internal Medicine.
This is the principal finding of a retrospective cohort study – the only study to directly compare the two oral non–vitamin-K-antagonists – that involved more than 118,000 patients who initiated anticoagulation treatment during a 2.5-year period. The Centers for Medicare & Medicaid Services and the Food and Drug Administration jointly conducted the study.
During the study period, rivaroxaban was used 2-3 times more often than was dabigatran in AF patients in the United States, “perhaps partly because of prescriber misperceptions about bleeding risks with dabigatran, arising from FDA receipt of a large number of postmarketing case reports following its approval. Ironically, we [now find] substantially higher bleeding risks with use of rivaroxaban than dabigatran,” said David J. Graham, MD, of the Office of Surveillance and Epidemiology, Center for Drug Evaluation and Research, FDA, Silver Spring, Md., and his associates.
The researchers assessed Medicare beneficiaries who initiated standard oral doses of rivaroxaban (66,651 patients) or dabigatran (52,240 patients) and were followed for a mean of 110 days.
The primary outcome measure – a composite of thromboembolic stroke, intracranial hemorrhage, major extracranial bleeding events including GI bleeding, and mortality – occurred in significantly more patients taking rivaroxaban than in those taking dabigatran. When the individual components of this composite outcome were considered, rivaroxaban was associated with significant increases in intracranial hemorrhage (HR, 1.65), major extracranial bleeding (HR, 1.48), and major GI bleeding (HR, 1.40); a nonsignificant decrease in thromboembolic stroke (HR, 0.81); and a nonsignificant increase in mortality (HR, 1.15).
In a further analysis of the data, rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment. In addition, rivaroxaban was associated with a significantly increased risk of death in two subgroups of patients: those aged 75 and older and those whose CHADS-2 scores indicated higher bleeding risk, Dr. Graham and his associates said (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.5954).
Of note, “the net increase in intracranial hemorrhage, the outcome with the highest case fatality rate, exceeded the net reduction in thromboembolic stroke” with rivaroxaban treatment, they added.
Rivaroxaban is associated with significantly more intra- and extracranial bleeding than is dabigatran in older patients who have nonvalvular atrial fibrillation, according to a report published online Oct. 3 in JAMA Internal Medicine.
This is the principal finding of a retrospective cohort study – the only study to directly compare the two oral non–vitamin-K-antagonists – that involved more than 118,000 patients who initiated anticoagulation treatment during a 2.5-year period. The Centers for Medicare & Medicaid Services and the Food and Drug Administration jointly conducted the study.
During the study period, rivaroxaban was used 2-3 times more often than was dabigatran in AF patients in the United States, “perhaps partly because of prescriber misperceptions about bleeding risks with dabigatran, arising from FDA receipt of a large number of postmarketing case reports following its approval. Ironically, we [now find] substantially higher bleeding risks with use of rivaroxaban than dabigatran,” said David J. Graham, MD, of the Office of Surveillance and Epidemiology, Center for Drug Evaluation and Research, FDA, Silver Spring, Md., and his associates.
The researchers assessed Medicare beneficiaries who initiated standard oral doses of rivaroxaban (66,651 patients) or dabigatran (52,240 patients) and were followed for a mean of 110 days.
The primary outcome measure – a composite of thromboembolic stroke, intracranial hemorrhage, major extracranial bleeding events including GI bleeding, and mortality – occurred in significantly more patients taking rivaroxaban than in those taking dabigatran. When the individual components of this composite outcome were considered, rivaroxaban was associated with significant increases in intracranial hemorrhage (HR, 1.65), major extracranial bleeding (HR, 1.48), and major GI bleeding (HR, 1.40); a nonsignificant decrease in thromboembolic stroke (HR, 0.81); and a nonsignificant increase in mortality (HR, 1.15).
In a further analysis of the data, rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment. In addition, rivaroxaban was associated with a significantly increased risk of death in two subgroups of patients: those aged 75 and older and those whose CHADS-2 scores indicated higher bleeding risk, Dr. Graham and his associates said (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.5954).
Of note, “the net increase in intracranial hemorrhage, the outcome with the highest case fatality rate, exceeded the net reduction in thromboembolic stroke” with rivaroxaban treatment, they added.
Key clinical point: Rivaroxaban is associated with significantly more intra- and extracranial bleeding than dabigatran in patients aged 75 and older with nonvalvular atrial fibrillation.
Major finding: Rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment.
Data source: A retrospective cohort study of 118,891 patients aged 65 and older who initiated anticoagulation therapy for AF during a 2.5-year period.
Disclosures: This study was conducted by employees or contractors of the Centers for Medicare & Medicaid Services and the Food and Drug Administration. Dr. Graham and his associates reported having no relevant financial disclosures.
COPD patient characteristics predict response to maintenance drug
Azithromycin maintenance therapy may be best reserved for patients with mild to moderate chronic obstructive pulmonary disease (COPD) and few symptoms, according to an analysis from the COLUMBUS randomized controlled trial. The study, reported on in Family Practice News, also revealed that patients with a high serum eosinophil level… http://www.familypracticenews.com/specialty-focus/pulmonary-sleep-medicine/single-article-page/copd-patient-characteristics-predict-response-to-maintenance-drug/f29efaba9a4874ed9b754fb87b77b663.html.
Azithromycin maintenance therapy may be best reserved for patients with mild to moderate chronic obstructive pulmonary disease (COPD) and few symptoms, according to an analysis from the COLUMBUS randomized controlled trial. The study, reported on in Family Practice News, also revealed that patients with a high serum eosinophil level… http://www.familypracticenews.com/specialty-focus/pulmonary-sleep-medicine/single-article-page/copd-patient-characteristics-predict-response-to-maintenance-drug/f29efaba9a4874ed9b754fb87b77b663.html.
Azithromycin maintenance therapy may be best reserved for patients with mild to moderate chronic obstructive pulmonary disease (COPD) and few symptoms, according to an analysis from the COLUMBUS randomized controlled trial. The study, reported on in Family Practice News, also revealed that patients with a high serum eosinophil level… http://www.familypracticenews.com/specialty-focus/pulmonary-sleep-medicine/single-article-page/copd-patient-characteristics-predict-response-to-maintenance-drug/f29efaba9a4874ed9b754fb87b77b663.html.
VIDEO: New oral anticoagulants cut intracranial bleeds in real-world atrial fib patients
During the first year on anticoagulant treatment, patients who received a new oral anticoagulant (NOAC) had an ischemic stroke rate similar to that of patients who received the traditional oral anticoagulant, warfarin. But they also had a significantly reduced rate of intracranial hemorrhage, according to Laila Stærk, MD, who reported on the findings at the annual congress of the European Society of Cardiology. The study included 43,299 Danish patients, of which 42% received warfarin, 29% received dabigatran, 16% received apixaban, and 13% received rivaroxaban. More on the results of this study are available in this article and video from Cardiology News: http://www.ecardiologynews.com/specialty-focus/arrhythmias-electrophysiology/single-article-page/video-noacs-cut-intracranial-bleeds-in-real-world-atrial-fib-patients/2c213686c34e2f2e9fb58000ff2cad80.html.
During the first year on anticoagulant treatment, patients who received a new oral anticoagulant (NOAC) had an ischemic stroke rate similar to that of patients who received the traditional oral anticoagulant, warfarin. But they also had a significantly reduced rate of intracranial hemorrhage, according to Laila Stærk, MD, who reported on the findings at the annual congress of the European Society of Cardiology. The study included 43,299 Danish patients, of which 42% received warfarin, 29% received dabigatran, 16% received apixaban, and 13% received rivaroxaban. More on the results of this study are available in this article and video from Cardiology News: http://www.ecardiologynews.com/specialty-focus/arrhythmias-electrophysiology/single-article-page/video-noacs-cut-intracranial-bleeds-in-real-world-atrial-fib-patients/2c213686c34e2f2e9fb58000ff2cad80.html.
During the first year on anticoagulant treatment, patients who received a new oral anticoagulant (NOAC) had an ischemic stroke rate similar to that of patients who received the traditional oral anticoagulant, warfarin. But they also had a significantly reduced rate of intracranial hemorrhage, according to Laila Stærk, MD, who reported on the findings at the annual congress of the European Society of Cardiology. The study included 43,299 Danish patients, of which 42% received warfarin, 29% received dabigatran, 16% received apixaban, and 13% received rivaroxaban. More on the results of this study are available in this article and video from Cardiology News: http://www.ecardiologynews.com/specialty-focus/arrhythmias-electrophysiology/single-article-page/video-noacs-cut-intracranial-bleeds-in-real-world-atrial-fib-patients/2c213686c34e2f2e9fb58000ff2cad80.html.
Malignant Transformation of an Aneurysmal Bone Cyst to Fibroblastic Osteosarcoma
Aneurysmal bone cysts (ABC) are expansile, hemorrhagic, non-neoplastic lesions that can be locally destructive1 and that can arise either de novo or secondary to another benign or malignant lesion.2 Although primary and secondary ABCs typically are benign, there are cases of malignant degeneration of primary ABCs, though the transformation arises almost exclusively in the context of prior radiation exposure.3-5 Malignant change without history of irradiation is rare; only 6 such cases have been reported.5-10 In 4 of these cases, the transformation was to osteosarcoma.5,8-10
Here we report on an ABC that degenerated into a fibroblastic osteosarcoma—the fifth such case in the medical literature. In addition to reviewing the earlier cases, we describe the radiologic and histologic underpinnings of this diagnosis and the insight that they provide into the pathogenesis of this rare process. Although the prevailing view is that ABCs are benign, it is important to know these lesions have the potential to undergo malignant transformation, even in the absence of prior radiation exposure. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A healthy and previously asymptomatic 37-year-old man presented with thigh pain after a minor fall onto a couch. Radiographs showed a diaphyseal femoral pathologic fracture adjacent to a small but benign-appearing cystic lesion (Figures 1A, 1B).
Two years later, the patient had a bicycle accident and, after 2 weeks of significantly increased thigh swelling, presented to the emergency department at the referring institution. Radiographs showed a lytic lesion in the femoral diaphysis that was highly suspicious for malignancy (Figures 3A, 3B).
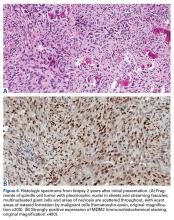
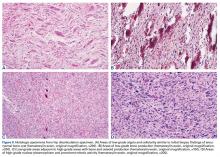
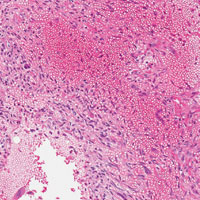
The initial biopsy specimens were evaluated at our institution and interpreted as being consistent with an ABC, with negative immunohistochemical staining for MDM2 (Figures 5A, 5B).
The patient underwent a 3-month course of neoadjuvant chemotherapy with cisplatin and doxorubicin. Interval-staging contrast-enhanced chest, abdomen, and pelvis computed tomography (CT) showed no evidence of metastatic disease. Preoperative MRI showed a significantly larger heterogeneous mass, now with neurovascular involvement, which precluded limb salvage.
Discussion
Aneurysmal bone cysts are expansile, hemorrhagic, locally destructive lesions that generally develop within the first 3 decades of life. Ever since they were first described by Jaffe and Lichtenstein11 in 1942, the most widely accepted theory of their pathogenesis has been that they begin as a benign reactive vascular process.12 However, more recent molecular studies by Oliveira and colleagues13 and Panoutsakopoulos and colleagues14 have demonstrated a clonal neoplastic basis for primary ABCs related to cytogenetic upregulation of oncogenes USP6 and CDH11 after translocation of 17p13 and 16q22.
Given the clonal nature of these lesions, it is surprising that malignant transformation is so rare. Until now, there have been only 4 reports of an ABC undergoing malignant degeneration to osteosarcoma without prior radiation exposure.
In this article, we have presented a fifth case of a primary ABC degenerating into an osteosarcoma, which in this instance was the fibroblastic subtype. This diagnosis was strongly supported by radiologic and pathologic evidence. From a radiologic perspective, imaging at initial presentation showed absolutely no suspicious features, and the same was true when follow-up radiographs were obtained, 1 month later. Although 1 month is short for a follow-up, the complete lack of radiographic changes would be highly unusual if in fact there had been a coexisting, undetected lesion as aggressive as the one that ultimately developed. Furthermore, imaging at second presentation, almost 2 years later, showed an extremely rapid evolution of findings over 1 month. Extrapolating back in time, we think this time course indicates the malignancy developed not long before its aggressive features were detected.
Genetic evidence suggests that most conventional high-grade osteosarcomas arise de novo from a mesenchymal precursor driven by multiple genetic aberrations. Less often, low-grade osteosarcomas progress to high-grade osteosarcomas. Amplification of 12q13-15 with resulting overexpression of MDM2 and CDK4 proteins is found in low-grade osteosarcomas and persists in examples that progress to higher-grade forms.15 Not only did review of our patient’s initial biopsy sample reveal no evidence of malignant features or abnormal mitotic activity, but the complete absence of MDM2 suggests not even a low-grade osteosarcoma was present at the time. By contrast, the second incisional biopsy specimen, 2 years later, showed markedly different histology and pronounced expression of MDM2 throughout the specimen. This finding suggests the histologically high-grade osteosarcoma did not arise de novo but rather secondarily from a low-grade osteosarcoma that had arisen from an ABC. Results of the final heterogeneous histology of the very large mass, which contained benign ABC areas indistinguishable from the initial biopsy sample, as well as areas of high-grade osteosarcoma, further support a multistep process of de-differentiation. Together, these findings are compelling evidence of malignant transformation of a primary ABC.
We acknowledge that the initial surgery performed at the outside hospital might have properly included frozen-section analysis of the biopsy material and that sampling error may have occurred during the index procedure—possibilities in the absence of complete lesional resection. In this case, however, the radiographic findings and the dominant histologic immunophenotype from medullary canal bone were both consistent with ABC and not osteosarcoma, lending support to malignant degeneration.
We have presented a fifth case of primary ABC degenerating into an osteosarcoma, now with immunohistochemical evidence supporting traditional radiologic and histologic evidence. Despite the rarity of the diagnosis, this case yields considerable insight into the pathogenetic mechanisms underlying malignant degeneration. Despite the widely held view that ABCs are benign, physicians caring for these patients must be aware that malignant transformation can occur.
Am J Orthop. 2016;45(6):E367-E372. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Donaldson WF. Aneurysmal bone cyst. J Bone Joint Surg Am. 1962;44:25-40.
2. Biesecker JL, Marcove RC, Huvos AG, Miké V. Aneurysmal bone cysts. A clinicopathologic study of 66 cases. Cancer. 1970;26(3):615-625.
3. Aho HJ, Aho AJ, Einola S. Aneurysmal bone cyst, a study of ultrastructure and malignant transformation. Virchows Arch A Pathol Anat Histol. 1982;395(2):169-179.
4. Tillman BP, Dahlin DC, Lipscomb PR, Stewart JR. Aneurysmal bone cyst: an analysis of ninety-five cases. Mayo Clin Proc. 1968;43(7):478-495.
5. Kyriakos M, Hardy D. Malignant transformation of aneurysmal bone cyst, with an analysis of the literature. Cancer. 1991;68(8):1770-1780.
6. Mei J, Gao YS, Wang SQ, Cai XS. Malignant transformation of aneurysmal bone cysts: a case report. Chin Med J (Engl). 2009;122(1):110-112.
7. Anract P, de Pinieux G, Jeanrot C, Babinet A, Forest M, Tomeno B. Malignant fibrous histiocytoma at the site of a previously treated aneurysmal bone cyst: a case report. J Bone Joint Surg Am. 2002;84(1):106-111.
8. Hsu CC, Wang JW, Huang CH, Chen WJ. Osteosarcoma at the site of a previously treated aneurysmal bone cyst. A case report. J Bone Joint Surg Am. 2005;87(2):395-398.
9. Wuisman P, Roessner A, Blasius S, Grünert J, Vestering T, Winkelmann W. High malignant surface osteosarcoma arising at the site of a previously treated aneurysmal bone cyst. J Cancer Res Clin Oncol. 1993;119(7):375-378.
10. Brindley GW, Greene JF Jr, Frankel LS. Case reports: malignant transformation of aneurysmal bone cysts. Clin Orthop Relat Res. 2005;(438):282-287.
11. Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst: with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg. 1942;44:1004-1025.
12. Mirra JM. Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. Philadelphia, PA: Lea & Febiger; 1989.
13. Oliveira AM, Chou MM, Perez-Atayde AR, Rosenberg AE. Aneurysmal bone cyst: a neoplasm driven by upregulation of the USP6 oncogene. J Clin Oncol. 2006;24(1):e1.
14. Panoutsakopoulos G, Pandis N, Kyriazoglou I, Gustafson P, Mertens F, Mandahl N. Recurrent t(16;17)(q22;p13) in aneurysmal bone cysts. Genes Chromosomes Cancer. 1999;26(3):265-266.
15. Dujardin F, Binh MB, Bouvier C, et al. MDM2 and CDK4 immunohistochemistry is a valuable tool in the differential diagnosis of low-grade osteosarcomas and other primary fibro-osseous lesions of the bone. Mod Pathol. 2001;24(5):624-637.
Aneurysmal bone cysts (ABC) are expansile, hemorrhagic, non-neoplastic lesions that can be locally destructive1 and that can arise either de novo or secondary to another benign or malignant lesion.2 Although primary and secondary ABCs typically are benign, there are cases of malignant degeneration of primary ABCs, though the transformation arises almost exclusively in the context of prior radiation exposure.3-5 Malignant change without history of irradiation is rare; only 6 such cases have been reported.5-10 In 4 of these cases, the transformation was to osteosarcoma.5,8-10
Here we report on an ABC that degenerated into a fibroblastic osteosarcoma—the fifth such case in the medical literature. In addition to reviewing the earlier cases, we describe the radiologic and histologic underpinnings of this diagnosis and the insight that they provide into the pathogenesis of this rare process. Although the prevailing view is that ABCs are benign, it is important to know these lesions have the potential to undergo malignant transformation, even in the absence of prior radiation exposure. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A healthy and previously asymptomatic 37-year-old man presented with thigh pain after a minor fall onto a couch. Radiographs showed a diaphyseal femoral pathologic fracture adjacent to a small but benign-appearing cystic lesion (Figures 1A, 1B).
Two years later, the patient had a bicycle accident and, after 2 weeks of significantly increased thigh swelling, presented to the emergency department at the referring institution. Radiographs showed a lytic lesion in the femoral diaphysis that was highly suspicious for malignancy (Figures 3A, 3B).
The initial biopsy specimens were evaluated at our institution and interpreted as being consistent with an ABC, with negative immunohistochemical staining for MDM2 (Figures 5A, 5B).
The patient underwent a 3-month course of neoadjuvant chemotherapy with cisplatin and doxorubicin. Interval-staging contrast-enhanced chest, abdomen, and pelvis computed tomography (CT) showed no evidence of metastatic disease. Preoperative MRI showed a significantly larger heterogeneous mass, now with neurovascular involvement, which precluded limb salvage.
Discussion
Aneurysmal bone cysts are expansile, hemorrhagic, locally destructive lesions that generally develop within the first 3 decades of life. Ever since they were first described by Jaffe and Lichtenstein11 in 1942, the most widely accepted theory of their pathogenesis has been that they begin as a benign reactive vascular process.12 However, more recent molecular studies by Oliveira and colleagues13 and Panoutsakopoulos and colleagues14 have demonstrated a clonal neoplastic basis for primary ABCs related to cytogenetic upregulation of oncogenes USP6 and CDH11 after translocation of 17p13 and 16q22.
Given the clonal nature of these lesions, it is surprising that malignant transformation is so rare. Until now, there have been only 4 reports of an ABC undergoing malignant degeneration to osteosarcoma without prior radiation exposure.
In this article, we have presented a fifth case of a primary ABC degenerating into an osteosarcoma, which in this instance was the fibroblastic subtype. This diagnosis was strongly supported by radiologic and pathologic evidence. From a radiologic perspective, imaging at initial presentation showed absolutely no suspicious features, and the same was true when follow-up radiographs were obtained, 1 month later. Although 1 month is short for a follow-up, the complete lack of radiographic changes would be highly unusual if in fact there had been a coexisting, undetected lesion as aggressive as the one that ultimately developed. Furthermore, imaging at second presentation, almost 2 years later, showed an extremely rapid evolution of findings over 1 month. Extrapolating back in time, we think this time course indicates the malignancy developed not long before its aggressive features were detected.
Genetic evidence suggests that most conventional high-grade osteosarcomas arise de novo from a mesenchymal precursor driven by multiple genetic aberrations. Less often, low-grade osteosarcomas progress to high-grade osteosarcomas. Amplification of 12q13-15 with resulting overexpression of MDM2 and CDK4 proteins is found in low-grade osteosarcomas and persists in examples that progress to higher-grade forms.15 Not only did review of our patient’s initial biopsy sample reveal no evidence of malignant features or abnormal mitotic activity, but the complete absence of MDM2 suggests not even a low-grade osteosarcoma was present at the time. By contrast, the second incisional biopsy specimen, 2 years later, showed markedly different histology and pronounced expression of MDM2 throughout the specimen. This finding suggests the histologically high-grade osteosarcoma did not arise de novo but rather secondarily from a low-grade osteosarcoma that had arisen from an ABC. Results of the final heterogeneous histology of the very large mass, which contained benign ABC areas indistinguishable from the initial biopsy sample, as well as areas of high-grade osteosarcoma, further support a multistep process of de-differentiation. Together, these findings are compelling evidence of malignant transformation of a primary ABC.
We acknowledge that the initial surgery performed at the outside hospital might have properly included frozen-section analysis of the biopsy material and that sampling error may have occurred during the index procedure—possibilities in the absence of complete lesional resection. In this case, however, the radiographic findings and the dominant histologic immunophenotype from medullary canal bone were both consistent with ABC and not osteosarcoma, lending support to malignant degeneration.
We have presented a fifth case of primary ABC degenerating into an osteosarcoma, now with immunohistochemical evidence supporting traditional radiologic and histologic evidence. Despite the rarity of the diagnosis, this case yields considerable insight into the pathogenetic mechanisms underlying malignant degeneration. Despite the widely held view that ABCs are benign, physicians caring for these patients must be aware that malignant transformation can occur.
Am J Orthop. 2016;45(6):E367-E372. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
Aneurysmal bone cysts (ABC) are expansile, hemorrhagic, non-neoplastic lesions that can be locally destructive1 and that can arise either de novo or secondary to another benign or malignant lesion.2 Although primary and secondary ABCs typically are benign, there are cases of malignant degeneration of primary ABCs, though the transformation arises almost exclusively in the context of prior radiation exposure.3-5 Malignant change without history of irradiation is rare; only 6 such cases have been reported.5-10 In 4 of these cases, the transformation was to osteosarcoma.5,8-10
Here we report on an ABC that degenerated into a fibroblastic osteosarcoma—the fifth such case in the medical literature. In addition to reviewing the earlier cases, we describe the radiologic and histologic underpinnings of this diagnosis and the insight that they provide into the pathogenesis of this rare process. Although the prevailing view is that ABCs are benign, it is important to know these lesions have the potential to undergo malignant transformation, even in the absence of prior radiation exposure. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A healthy and previously asymptomatic 37-year-old man presented with thigh pain after a minor fall onto a couch. Radiographs showed a diaphyseal femoral pathologic fracture adjacent to a small but benign-appearing cystic lesion (Figures 1A, 1B).
Two years later, the patient had a bicycle accident and, after 2 weeks of significantly increased thigh swelling, presented to the emergency department at the referring institution. Radiographs showed a lytic lesion in the femoral diaphysis that was highly suspicious for malignancy (Figures 3A, 3B).
The initial biopsy specimens were evaluated at our institution and interpreted as being consistent with an ABC, with negative immunohistochemical staining for MDM2 (Figures 5A, 5B).
The patient underwent a 3-month course of neoadjuvant chemotherapy with cisplatin and doxorubicin. Interval-staging contrast-enhanced chest, abdomen, and pelvis computed tomography (CT) showed no evidence of metastatic disease. Preoperative MRI showed a significantly larger heterogeneous mass, now with neurovascular involvement, which precluded limb salvage.
Discussion
Aneurysmal bone cysts are expansile, hemorrhagic, locally destructive lesions that generally develop within the first 3 decades of life. Ever since they were first described by Jaffe and Lichtenstein11 in 1942, the most widely accepted theory of their pathogenesis has been that they begin as a benign reactive vascular process.12 However, more recent molecular studies by Oliveira and colleagues13 and Panoutsakopoulos and colleagues14 have demonstrated a clonal neoplastic basis for primary ABCs related to cytogenetic upregulation of oncogenes USP6 and CDH11 after translocation of 17p13 and 16q22.
Given the clonal nature of these lesions, it is surprising that malignant transformation is so rare. Until now, there have been only 4 reports of an ABC undergoing malignant degeneration to osteosarcoma without prior radiation exposure.
In this article, we have presented a fifth case of a primary ABC degenerating into an osteosarcoma, which in this instance was the fibroblastic subtype. This diagnosis was strongly supported by radiologic and pathologic evidence. From a radiologic perspective, imaging at initial presentation showed absolutely no suspicious features, and the same was true when follow-up radiographs were obtained, 1 month later. Although 1 month is short for a follow-up, the complete lack of radiographic changes would be highly unusual if in fact there had been a coexisting, undetected lesion as aggressive as the one that ultimately developed. Furthermore, imaging at second presentation, almost 2 years later, showed an extremely rapid evolution of findings over 1 month. Extrapolating back in time, we think this time course indicates the malignancy developed not long before its aggressive features were detected.
Genetic evidence suggests that most conventional high-grade osteosarcomas arise de novo from a mesenchymal precursor driven by multiple genetic aberrations. Less often, low-grade osteosarcomas progress to high-grade osteosarcomas. Amplification of 12q13-15 with resulting overexpression of MDM2 and CDK4 proteins is found in low-grade osteosarcomas and persists in examples that progress to higher-grade forms.15 Not only did review of our patient’s initial biopsy sample reveal no evidence of malignant features or abnormal mitotic activity, but the complete absence of MDM2 suggests not even a low-grade osteosarcoma was present at the time. By contrast, the second incisional biopsy specimen, 2 years later, showed markedly different histology and pronounced expression of MDM2 throughout the specimen. This finding suggests the histologically high-grade osteosarcoma did not arise de novo but rather secondarily from a low-grade osteosarcoma that had arisen from an ABC. Results of the final heterogeneous histology of the very large mass, which contained benign ABC areas indistinguishable from the initial biopsy sample, as well as areas of high-grade osteosarcoma, further support a multistep process of de-differentiation. Together, these findings are compelling evidence of malignant transformation of a primary ABC.
We acknowledge that the initial surgery performed at the outside hospital might have properly included frozen-section analysis of the biopsy material and that sampling error may have occurred during the index procedure—possibilities in the absence of complete lesional resection. In this case, however, the radiographic findings and the dominant histologic immunophenotype from medullary canal bone were both consistent with ABC and not osteosarcoma, lending support to malignant degeneration.
We have presented a fifth case of primary ABC degenerating into an osteosarcoma, now with immunohistochemical evidence supporting traditional radiologic and histologic evidence. Despite the rarity of the diagnosis, this case yields considerable insight into the pathogenetic mechanisms underlying malignant degeneration. Despite the widely held view that ABCs are benign, physicians caring for these patients must be aware that malignant transformation can occur.
Am J Orthop. 2016;45(6):E367-E372. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Donaldson WF. Aneurysmal bone cyst. J Bone Joint Surg Am. 1962;44:25-40.
2. Biesecker JL, Marcove RC, Huvos AG, Miké V. Aneurysmal bone cysts. A clinicopathologic study of 66 cases. Cancer. 1970;26(3):615-625.
3. Aho HJ, Aho AJ, Einola S. Aneurysmal bone cyst, a study of ultrastructure and malignant transformation. Virchows Arch A Pathol Anat Histol. 1982;395(2):169-179.
4. Tillman BP, Dahlin DC, Lipscomb PR, Stewart JR. Aneurysmal bone cyst: an analysis of ninety-five cases. Mayo Clin Proc. 1968;43(7):478-495.
5. Kyriakos M, Hardy D. Malignant transformation of aneurysmal bone cyst, with an analysis of the literature. Cancer. 1991;68(8):1770-1780.
6. Mei J, Gao YS, Wang SQ, Cai XS. Malignant transformation of aneurysmal bone cysts: a case report. Chin Med J (Engl). 2009;122(1):110-112.
7. Anract P, de Pinieux G, Jeanrot C, Babinet A, Forest M, Tomeno B. Malignant fibrous histiocytoma at the site of a previously treated aneurysmal bone cyst: a case report. J Bone Joint Surg Am. 2002;84(1):106-111.
8. Hsu CC, Wang JW, Huang CH, Chen WJ. Osteosarcoma at the site of a previously treated aneurysmal bone cyst. A case report. J Bone Joint Surg Am. 2005;87(2):395-398.
9. Wuisman P, Roessner A, Blasius S, Grünert J, Vestering T, Winkelmann W. High malignant surface osteosarcoma arising at the site of a previously treated aneurysmal bone cyst. J Cancer Res Clin Oncol. 1993;119(7):375-378.
10. Brindley GW, Greene JF Jr, Frankel LS. Case reports: malignant transformation of aneurysmal bone cysts. Clin Orthop Relat Res. 2005;(438):282-287.
11. Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst: with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg. 1942;44:1004-1025.
12. Mirra JM. Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. Philadelphia, PA: Lea & Febiger; 1989.
13. Oliveira AM, Chou MM, Perez-Atayde AR, Rosenberg AE. Aneurysmal bone cyst: a neoplasm driven by upregulation of the USP6 oncogene. J Clin Oncol. 2006;24(1):e1.
14. Panoutsakopoulos G, Pandis N, Kyriazoglou I, Gustafson P, Mertens F, Mandahl N. Recurrent t(16;17)(q22;p13) in aneurysmal bone cysts. Genes Chromosomes Cancer. 1999;26(3):265-266.
15. Dujardin F, Binh MB, Bouvier C, et al. MDM2 and CDK4 immunohistochemistry is a valuable tool in the differential diagnosis of low-grade osteosarcomas and other primary fibro-osseous lesions of the bone. Mod Pathol. 2001;24(5):624-637.
1. Donaldson WF. Aneurysmal bone cyst. J Bone Joint Surg Am. 1962;44:25-40.
2. Biesecker JL, Marcove RC, Huvos AG, Miké V. Aneurysmal bone cysts. A clinicopathologic study of 66 cases. Cancer. 1970;26(3):615-625.
3. Aho HJ, Aho AJ, Einola S. Aneurysmal bone cyst, a study of ultrastructure and malignant transformation. Virchows Arch A Pathol Anat Histol. 1982;395(2):169-179.
4. Tillman BP, Dahlin DC, Lipscomb PR, Stewart JR. Aneurysmal bone cyst: an analysis of ninety-five cases. Mayo Clin Proc. 1968;43(7):478-495.
5. Kyriakos M, Hardy D. Malignant transformation of aneurysmal bone cyst, with an analysis of the literature. Cancer. 1991;68(8):1770-1780.
6. Mei J, Gao YS, Wang SQ, Cai XS. Malignant transformation of aneurysmal bone cysts: a case report. Chin Med J (Engl). 2009;122(1):110-112.
7. Anract P, de Pinieux G, Jeanrot C, Babinet A, Forest M, Tomeno B. Malignant fibrous histiocytoma at the site of a previously treated aneurysmal bone cyst: a case report. J Bone Joint Surg Am. 2002;84(1):106-111.
8. Hsu CC, Wang JW, Huang CH, Chen WJ. Osteosarcoma at the site of a previously treated aneurysmal bone cyst. A case report. J Bone Joint Surg Am. 2005;87(2):395-398.
9. Wuisman P, Roessner A, Blasius S, Grünert J, Vestering T, Winkelmann W. High malignant surface osteosarcoma arising at the site of a previously treated aneurysmal bone cyst. J Cancer Res Clin Oncol. 1993;119(7):375-378.
10. Brindley GW, Greene JF Jr, Frankel LS. Case reports: malignant transformation of aneurysmal bone cysts. Clin Orthop Relat Res. 2005;(438):282-287.
11. Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst: with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg. 1942;44:1004-1025.
12. Mirra JM. Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. Philadelphia, PA: Lea & Febiger; 1989.
13. Oliveira AM, Chou MM, Perez-Atayde AR, Rosenberg AE. Aneurysmal bone cyst: a neoplasm driven by upregulation of the USP6 oncogene. J Clin Oncol. 2006;24(1):e1.
14. Panoutsakopoulos G, Pandis N, Kyriazoglou I, Gustafson P, Mertens F, Mandahl N. Recurrent t(16;17)(q22;p13) in aneurysmal bone cysts. Genes Chromosomes Cancer. 1999;26(3):265-266.
15. Dujardin F, Binh MB, Bouvier C, et al. MDM2 and CDK4 immunohistochemistry is a valuable tool in the differential diagnosis of low-grade osteosarcomas and other primary fibro-osseous lesions of the bone. Mod Pathol. 2001;24(5):624-637.
Cerebral protection in TAVI reduces ischemic brain lesions
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Key clinical point: In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions.
Major finding: At 2 days, the number of new brain lesions was markedly lower in the filter group than in the control group (8 vs. 16), as was the lesion volume (466 mm vs. 800 mm).
Data source: A prospective single-center randomized clinical trial involving 100 patients undergoing TAVI for severe aortic stenosis.
Disclosures: This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Debunking Psoriasis Myths: Does UVB Phototherapy Cause Skin Cancer?
Myth: UVB phototherapy causes skin cancer
Phototherapy is a common treatment modality for psoriasis patients that can be used in the physician’s office or psoriasis clinic or at home. Options include UVB phototherapy (broadband and narrowband), which slows the growth of affected skin cells; psoralen plus UVA (PUVA), which slows excessive skin cell growth; and excimer laser therapy, which targets select areas of the skin affected by mild to moderate psoriasis and is particularly useful for scalp psoriasis. Each of these therapies may be combined with other topical and/or systemic psoriasis treatments. The effects of UV light on the skin and the connection to skin cancer is widely known. Therefore, patient education on the risk for skin cancer with phototherapy is essential.
Evidence suggests that UVB phototherapy remains a safe treatment modality. In a 2005 analysis of prospective and retrospective studies on skin cancer risk from UVB phototherapy, 11 studies (10 concerning psoriasis patients) were reviewed and the researchers concluded that all studies eventually showed no increased skin cancer risk with UVB phototherapy. One of the PUVA cohort studies examined genital skin cancers and found an increased rate of genital tumors associated with UVB phototherapy.
Another analysis to define the long-term carcinogenic risk for narrowband UVB treatment found that there was no association between narrowband UVB exposure alone (without PUVA) and any skin cancer. For patients treated with narrowband UVB and PUVA, there was a small increase in basal cell carcinomas.
Dermatologists should monitor psoriasis patients for self-administered treatment with tanning beds. Based on a questionnaire sent to approximately 14,000 subscribers of National Psoriasis Foundation emails, 62% of 617 tanners started tanning to treat psoriasis; they were more likely to have received medical phototherapy and had more severe psoriasis. Approximately 30% of these patients indicated that they used tanning as a self-treatment for psoriasis because of the inconvenience and cost of UV light treatment in a physician’s office as well as treatment failure of other therapies prescribed by the physician. “Our results imply that tanning bed usage among psoriasis sufferers is widespread and linked with tanning addiction,” reported Felton et al. “Practitioners should be particularly vigilant to the possibility of tanning bed usage in at-risk patients.” These patients may be at increased risk for skin cancer. Problematic tanning behaviors may be seen in younger female patients diagnosed with psoriasis at an early age as well as patients with severe psoriasis who were previously prescribed phototherapy treatment.
Expert Commentary on next page
Expert Commentary
UVB phototherapy is an effective therapy that does not increase the risk of nonmelanoma skin cancers (NMSCs), according to the 2 analyses mentioned above. When I discuss the risks and benefits of UVB phototherapy with psoriasis patients, I do say that there is a theoretical increased risk for NMSC but that the 2005 study mentioned above does not indicate an increased risk. However, UVB phototherapy and cyclosporine should not be combined, as this combination does increase the risk for NMSC.
Psoralen plus UVA definitely will increase the risk for NMSC, particularly squamous cell carcinoma. However, in this age of the biologics, PUVA use has fallen out of favor, partly due to the increased risk for NMSC, and many patients will not encounter dermatology practices that still use PUVA.
—Jashin J. Wu, MD (Los Angeles, California)
Felton S, Adinoff B, Jeon-Slaughter H, et al. The significant health threat from tanning bed use as a self-treatment for psoriasis. J Am Acad Dermatol. 2016;74:1015-1017.
Hearn RM, Kerr AC, Rahim KF, et al. Incidence of skin cancers in 3867 patients treated with narrow-band ultraviolet B phototherapy. Br J Dermatol. 2008;159:931-935.
Lee E, Koo J, Berger T. UVB phototherapy and skin cancer risk: a review of the literature. Int J Dermatol. 2005;44:355-360.
Phototherapy. National Psoriasis Foundation website. https://www.psoriasis.org/about-psoriasis/treatments/phototherapy . Accessed October 4, 2016.
Myth: UVB phototherapy causes skin cancer
Phototherapy is a common treatment modality for psoriasis patients that can be used in the physician’s office or psoriasis clinic or at home. Options include UVB phototherapy (broadband and narrowband), which slows the growth of affected skin cells; psoralen plus UVA (PUVA), which slows excessive skin cell growth; and excimer laser therapy, which targets select areas of the skin affected by mild to moderate psoriasis and is particularly useful for scalp psoriasis. Each of these therapies may be combined with other topical and/or systemic psoriasis treatments. The effects of UV light on the skin and the connection to skin cancer is widely known. Therefore, patient education on the risk for skin cancer with phototherapy is essential.
Evidence suggests that UVB phototherapy remains a safe treatment modality. In a 2005 analysis of prospective and retrospective studies on skin cancer risk from UVB phototherapy, 11 studies (10 concerning psoriasis patients) were reviewed and the researchers concluded that all studies eventually showed no increased skin cancer risk with UVB phototherapy. One of the PUVA cohort studies examined genital skin cancers and found an increased rate of genital tumors associated with UVB phototherapy.
Another analysis to define the long-term carcinogenic risk for narrowband UVB treatment found that there was no association between narrowband UVB exposure alone (without PUVA) and any skin cancer. For patients treated with narrowband UVB and PUVA, there was a small increase in basal cell carcinomas.
Dermatologists should monitor psoriasis patients for self-administered treatment with tanning beds. Based on a questionnaire sent to approximately 14,000 subscribers of National Psoriasis Foundation emails, 62% of 617 tanners started tanning to treat psoriasis; they were more likely to have received medical phototherapy and had more severe psoriasis. Approximately 30% of these patients indicated that they used tanning as a self-treatment for psoriasis because of the inconvenience and cost of UV light treatment in a physician’s office as well as treatment failure of other therapies prescribed by the physician. “Our results imply that tanning bed usage among psoriasis sufferers is widespread and linked with tanning addiction,” reported Felton et al. “Practitioners should be particularly vigilant to the possibility of tanning bed usage in at-risk patients.” These patients may be at increased risk for skin cancer. Problematic tanning behaviors may be seen in younger female patients diagnosed with psoriasis at an early age as well as patients with severe psoriasis who were previously prescribed phototherapy treatment.
Expert Commentary on next page
Expert Commentary
UVB phototherapy is an effective therapy that does not increase the risk of nonmelanoma skin cancers (NMSCs), according to the 2 analyses mentioned above. When I discuss the risks and benefits of UVB phototherapy with psoriasis patients, I do say that there is a theoretical increased risk for NMSC but that the 2005 study mentioned above does not indicate an increased risk. However, UVB phototherapy and cyclosporine should not be combined, as this combination does increase the risk for NMSC.
Psoralen plus UVA definitely will increase the risk for NMSC, particularly squamous cell carcinoma. However, in this age of the biologics, PUVA use has fallen out of favor, partly due to the increased risk for NMSC, and many patients will not encounter dermatology practices that still use PUVA.
—Jashin J. Wu, MD (Los Angeles, California)
Myth: UVB phototherapy causes skin cancer
Phototherapy is a common treatment modality for psoriasis patients that can be used in the physician’s office or psoriasis clinic or at home. Options include UVB phototherapy (broadband and narrowband), which slows the growth of affected skin cells; psoralen plus UVA (PUVA), which slows excessive skin cell growth; and excimer laser therapy, which targets select areas of the skin affected by mild to moderate psoriasis and is particularly useful for scalp psoriasis. Each of these therapies may be combined with other topical and/or systemic psoriasis treatments. The effects of UV light on the skin and the connection to skin cancer is widely known. Therefore, patient education on the risk for skin cancer with phototherapy is essential.
Evidence suggests that UVB phototherapy remains a safe treatment modality. In a 2005 analysis of prospective and retrospective studies on skin cancer risk from UVB phototherapy, 11 studies (10 concerning psoriasis patients) were reviewed and the researchers concluded that all studies eventually showed no increased skin cancer risk with UVB phototherapy. One of the PUVA cohort studies examined genital skin cancers and found an increased rate of genital tumors associated with UVB phototherapy.
Another analysis to define the long-term carcinogenic risk for narrowband UVB treatment found that there was no association between narrowband UVB exposure alone (without PUVA) and any skin cancer. For patients treated with narrowband UVB and PUVA, there was a small increase in basal cell carcinomas.
Dermatologists should monitor psoriasis patients for self-administered treatment with tanning beds. Based on a questionnaire sent to approximately 14,000 subscribers of National Psoriasis Foundation emails, 62% of 617 tanners started tanning to treat psoriasis; they were more likely to have received medical phototherapy and had more severe psoriasis. Approximately 30% of these patients indicated that they used tanning as a self-treatment for psoriasis because of the inconvenience and cost of UV light treatment in a physician’s office as well as treatment failure of other therapies prescribed by the physician. “Our results imply that tanning bed usage among psoriasis sufferers is widespread and linked with tanning addiction,” reported Felton et al. “Practitioners should be particularly vigilant to the possibility of tanning bed usage in at-risk patients.” These patients may be at increased risk for skin cancer. Problematic tanning behaviors may be seen in younger female patients diagnosed with psoriasis at an early age as well as patients with severe psoriasis who were previously prescribed phototherapy treatment.
Expert Commentary on next page
Expert Commentary
UVB phototherapy is an effective therapy that does not increase the risk of nonmelanoma skin cancers (NMSCs), according to the 2 analyses mentioned above. When I discuss the risks and benefits of UVB phototherapy with psoriasis patients, I do say that there is a theoretical increased risk for NMSC but that the 2005 study mentioned above does not indicate an increased risk. However, UVB phototherapy and cyclosporine should not be combined, as this combination does increase the risk for NMSC.
Psoralen plus UVA definitely will increase the risk for NMSC, particularly squamous cell carcinoma. However, in this age of the biologics, PUVA use has fallen out of favor, partly due to the increased risk for NMSC, and many patients will not encounter dermatology practices that still use PUVA.
—Jashin J. Wu, MD (Los Angeles, California)
Felton S, Adinoff B, Jeon-Slaughter H, et al. The significant health threat from tanning bed use as a self-treatment for psoriasis. J Am Acad Dermatol. 2016;74:1015-1017.
Hearn RM, Kerr AC, Rahim KF, et al. Incidence of skin cancers in 3867 patients treated with narrow-band ultraviolet B phototherapy. Br J Dermatol. 2008;159:931-935.
Lee E, Koo J, Berger T. UVB phototherapy and skin cancer risk: a review of the literature. Int J Dermatol. 2005;44:355-360.
Phototherapy. National Psoriasis Foundation website. https://www.psoriasis.org/about-psoriasis/treatments/phototherapy . Accessed October 4, 2016.
Felton S, Adinoff B, Jeon-Slaughter H, et al. The significant health threat from tanning bed use as a self-treatment for psoriasis. J Am Acad Dermatol. 2016;74:1015-1017.
Hearn RM, Kerr AC, Rahim KF, et al. Incidence of skin cancers in 3867 patients treated with narrow-band ultraviolet B phototherapy. Br J Dermatol. 2008;159:931-935.
Lee E, Koo J, Berger T. UVB phototherapy and skin cancer risk: a review of the literature. Int J Dermatol. 2005;44:355-360.
Phototherapy. National Psoriasis Foundation website. https://www.psoriasis.org/about-psoriasis/treatments/phototherapy . Accessed October 4, 2016.
Fast-Track EVAR protocol shown safe, effective, and cheaper
LAS VEGAS – A ‘fast-track” stenting method for endovascular abdominal aortic aneurysm repair (EVAR) enabled patients to be treated safely and effectively without general anesthetic or ICU admission, and with next-day discharge, Zvonimir Krajcer, MD, said at the 2016 Vascular Interventional Advances meeting.
Dr. Krajcer discussed the final results of the Prospective LIFE Registry, which followed 250 patients treated with the Ovation Abdominal Stent Graft platform, who had suitable femoral arteries to allow the use of the Perclose ProGlide Suture-Mediated Closure (SMC) System.
For the Fast-Track patients, vascular access, stent graft delivery, and deployment were successful. The Fast-Track EVAR protocol was successfully completed in 216 (87%) of the patients. In comparing the Fast-Track cohort (n = 216) to the non–Fast-Track cohort (n = 34), procedure time was found to be 84 vs. 110 minutes, the use of general anesthesia was 0% vs. 18%, and the need for ICU stay was 0% vs. 32%. Hospital stay for the two groups was 1.2 vs. 1.9 days, respectively.
Quality of life score improvement from baseline to 30 days as assessed via the EQ-5D questionnaire, was significantly greater in the Fast-Track patients, compared with the EVAR controls, said Dr. Krajcer, an interventional cardiologist at Texas Heart Institute and St. Luke’s Hospital, Houston, and a clinical professor of medicine at Baylor College of Medicine.
To determine adverse events, patients were followed through 1 month after treatment. The researchers found no device- or procedure-related major adverse events, abdominal aortic aneurysm (AAA) ruptures, surgical conversions, or AAA-related secondary interventions. One patient in the fast-track group died from acute respiratory failure. Overall, for the Fast-Track and control groups, the freedom from type I/III endoleak was 99% and 100%, respectively.
Dr. Krajcer reported that the 30-day hospital readmission rate in the LIFE study was 1.6%, compared to 8% reported for EVAR from the American College of Surgeons National Surgical Quality Improvement Program.
The economic analysis was performed comparing the Fast-Track patients to a control group, which consisted of a database of 8,306 patients treated with elective infrarenal EVAR at 3,750 U.S. hospitals based on inpatient discharge between 2012 and 2015. The researchers calculated costs related to access, anesthesia, ICU stay, and hospital stay.
The Fast-Track protocol showed $21,000 in perioperative cost savings relative to standard EVAR, largely driven by differences in hospital stay costs, according to Dr. Krajcer.
“Fast-track EVAR using the Ovation Prime stent graft is safe and feasible and lowers perioperative costs,” said Dr. Krajcer. “Our results warrant the establishment of a Fast-Track EVAR protocol in experienced EVAR centers,” he concluded.
Dr. Krajcer had nothing to disclose.
LAS VEGAS – A ‘fast-track” stenting method for endovascular abdominal aortic aneurysm repair (EVAR) enabled patients to be treated safely and effectively without general anesthetic or ICU admission, and with next-day discharge, Zvonimir Krajcer, MD, said at the 2016 Vascular Interventional Advances meeting.
Dr. Krajcer discussed the final results of the Prospective LIFE Registry, which followed 250 patients treated with the Ovation Abdominal Stent Graft platform, who had suitable femoral arteries to allow the use of the Perclose ProGlide Suture-Mediated Closure (SMC) System.
For the Fast-Track patients, vascular access, stent graft delivery, and deployment were successful. The Fast-Track EVAR protocol was successfully completed in 216 (87%) of the patients. In comparing the Fast-Track cohort (n = 216) to the non–Fast-Track cohort (n = 34), procedure time was found to be 84 vs. 110 minutes, the use of general anesthesia was 0% vs. 18%, and the need for ICU stay was 0% vs. 32%. Hospital stay for the two groups was 1.2 vs. 1.9 days, respectively.
Quality of life score improvement from baseline to 30 days as assessed via the EQ-5D questionnaire, was significantly greater in the Fast-Track patients, compared with the EVAR controls, said Dr. Krajcer, an interventional cardiologist at Texas Heart Institute and St. Luke’s Hospital, Houston, and a clinical professor of medicine at Baylor College of Medicine.
To determine adverse events, patients were followed through 1 month after treatment. The researchers found no device- or procedure-related major adverse events, abdominal aortic aneurysm (AAA) ruptures, surgical conversions, or AAA-related secondary interventions. One patient in the fast-track group died from acute respiratory failure. Overall, for the Fast-Track and control groups, the freedom from type I/III endoleak was 99% and 100%, respectively.
Dr. Krajcer reported that the 30-day hospital readmission rate in the LIFE study was 1.6%, compared to 8% reported for EVAR from the American College of Surgeons National Surgical Quality Improvement Program.
The economic analysis was performed comparing the Fast-Track patients to a control group, which consisted of a database of 8,306 patients treated with elective infrarenal EVAR at 3,750 U.S. hospitals based on inpatient discharge between 2012 and 2015. The researchers calculated costs related to access, anesthesia, ICU stay, and hospital stay.
The Fast-Track protocol showed $21,000 in perioperative cost savings relative to standard EVAR, largely driven by differences in hospital stay costs, according to Dr. Krajcer.
“Fast-track EVAR using the Ovation Prime stent graft is safe and feasible and lowers perioperative costs,” said Dr. Krajcer. “Our results warrant the establishment of a Fast-Track EVAR protocol in experienced EVAR centers,” he concluded.
Dr. Krajcer had nothing to disclose.
LAS VEGAS – A ‘fast-track” stenting method for endovascular abdominal aortic aneurysm repair (EVAR) enabled patients to be treated safely and effectively without general anesthetic or ICU admission, and with next-day discharge, Zvonimir Krajcer, MD, said at the 2016 Vascular Interventional Advances meeting.
Dr. Krajcer discussed the final results of the Prospective LIFE Registry, which followed 250 patients treated with the Ovation Abdominal Stent Graft platform, who had suitable femoral arteries to allow the use of the Perclose ProGlide Suture-Mediated Closure (SMC) System.
For the Fast-Track patients, vascular access, stent graft delivery, and deployment were successful. The Fast-Track EVAR protocol was successfully completed in 216 (87%) of the patients. In comparing the Fast-Track cohort (n = 216) to the non–Fast-Track cohort (n = 34), procedure time was found to be 84 vs. 110 minutes, the use of general anesthesia was 0% vs. 18%, and the need for ICU stay was 0% vs. 32%. Hospital stay for the two groups was 1.2 vs. 1.9 days, respectively.
Quality of life score improvement from baseline to 30 days as assessed via the EQ-5D questionnaire, was significantly greater in the Fast-Track patients, compared with the EVAR controls, said Dr. Krajcer, an interventional cardiologist at Texas Heart Institute and St. Luke’s Hospital, Houston, and a clinical professor of medicine at Baylor College of Medicine.
To determine adverse events, patients were followed through 1 month after treatment. The researchers found no device- or procedure-related major adverse events, abdominal aortic aneurysm (AAA) ruptures, surgical conversions, or AAA-related secondary interventions. One patient in the fast-track group died from acute respiratory failure. Overall, for the Fast-Track and control groups, the freedom from type I/III endoleak was 99% and 100%, respectively.
Dr. Krajcer reported that the 30-day hospital readmission rate in the LIFE study was 1.6%, compared to 8% reported for EVAR from the American College of Surgeons National Surgical Quality Improvement Program.
The economic analysis was performed comparing the Fast-Track patients to a control group, which consisted of a database of 8,306 patients treated with elective infrarenal EVAR at 3,750 U.S. hospitals based on inpatient discharge between 2012 and 2015. The researchers calculated costs related to access, anesthesia, ICU stay, and hospital stay.
The Fast-Track protocol showed $21,000 in perioperative cost savings relative to standard EVAR, largely driven by differences in hospital stay costs, according to Dr. Krajcer.
“Fast-track EVAR using the Ovation Prime stent graft is safe and feasible and lowers perioperative costs,” said Dr. Krajcer. “Our results warrant the establishment of a Fast-Track EVAR protocol in experienced EVAR centers,” he concluded.
Dr. Krajcer had nothing to disclose.
AT VIVA16
Key clinical point:
Major finding: Quality of life score improvement from baseline to 30 days was significantly greater in the Fast-Track patients, compared with the EVAR controls.
Data source: The researchers assessed 250 patients in the Prospective LIFE Registry and compared results to more than 8,000 patients in an EVAR database as controls.
Disclosures: Dr. Krajcer had nothing to disclose.
Sarcopenia an effective measure of frailty in elderly patients
WAIKOLOA, HAWAII – Sarcopenia is an independent predictor of 1-year mortality in elderly patients undergoing emergency abdominal surgery, results from a single-center study demonstrated.
“Setting expectations about operative outcomes is an important part of the preoperative counseling process, Erika L. Rangel, MD, FACS, said at the annual meeting of the American Association for the Surgery of Trauma. In a previous study that she and her associates conducted at Brigham and Women’s Hospital, Boston, the risk for mortality was found to continue long after hospital discharge in older patients who undergo emergency surgery: 16% at 30 days, 22% at 3 months, 28% at 6 months, and 32% 1 year after surgery (J Trauma and Acute Care Surg. 2015 Sep;79[3]:349-58).
Traditionally, surgeons use subjective opinion or basic scoring systems such as the American Society of Anesthesiologists (ASA) classification to stratify risk for surgery in elderly patients. “However, the ASA score can be subjective, and there’s inconsistency between evaluators,” Dr. Rangel said. “The Charlson Comorbidity [Index] rates a patient based on the presence or absence of 19 comorbidities, but it doesn’t tell the surgeon anything about the patient’s functional status.” Frailty is a good measure of an elderly patient’s physiologic reserve to withstand an operation, she continued, but is difficult to measure in the acute care setting. One solution is to measure sarcopenia, which predicts postoperative complications, disability, and mortality in elderly elective surgery patients. “The problem is that very few studies have looked at the impact of sarcopenia in the emergency surgery populations, and the ones that exist only look at short-term outcomes, which don’t completely capture the mortality risk,” she said.
In an effort to better understand how sarcopenia affects long-term outcomes after emergency surgery in the elderly, the researchers retrospectively reviewed patients aged 70 years or older who underwent urgent or emergent abdominal surgery at Brigham and Women’s between 2006 and 2011. Patients were stratified by operative severity using the POSSUM (Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity) score. Operations considered major included any laparotomy, open cholecystectomy, and bowel resection, while those considered moderate were laparoscopic cholecystectomy, appendectomy, and hernia repairs without bowel compromise. To measure sarcopenia, the researchers used preoperative CT images to calculate the average bilateral psoas muscle cross-sectional area at the L3 level, normalized for height. Primary outcome was 1-year mortality. Secondary outcomes were mortality at 30 days, 90 days, and 180 days.
Dr. Rangel reported results from 297 patients that were evaluated: 222 with no sarcopenia and 75 with sarcopenia. Their mean age was 78 years, 57% were female, and 84% were white. Compared with nonsarcopenic patients, sarcopenic patients did not differ in terms of age, sex, or race. Comorbidities were high in both groups, with 75% of patients having an ASA score of 3 or greater and 31% having a Charlson score of 4 or greater. More than 40% had some sort of underlying malignancy, yet there were no significant differences between the two groups in terms of ASA scores, Charlson scores, or the prevalence of malignancy.
Compared with nonsarcopenic patients, sarcopenic patients had longer hospital length of stay (14 vs. 11 days, respectively; P = .012), were more likely to require ICU care (67% vs. 50%; P = .012), and had higher in-hospital mortality (27% vs. 9%; P less than .01). In addition, sarcopenic patients had higher hazard ratios of mortality, compared with their nonsarcopenic counterparts, at 30 days (hazard ratio, 3.5; P = .01), 90 days (HR, 3.5; P less than .001), 180 days (HR, 2.6; P = .001), and at 1 year (HR, 2.5; P = .001).
“The measurement of sarcopenia is a practical tool that can be used at the bedside,” Dr. Rangel concluded. “It just takes 3 or 4 minutes using a single axial slice of a preoperative CT scan. Since it uses CT imaging that’s obtained for initial diagnostic purposes, it incurs no additional cost. The identification of sarcopenia has immediate applications for care of the geriatric patient. It should trigger the surgeon to set realistic goals of care and frame expectations about survival [and] should prompt processes of care that improve patient outcomes. High-risk patients might benefit from geriatric consultation or specialized geriatric pathways, early palliative care evaluation, and advance care planning.” She reported having no financial disclosures.
WAIKOLOA, HAWAII – Sarcopenia is an independent predictor of 1-year mortality in elderly patients undergoing emergency abdominal surgery, results from a single-center study demonstrated.
“Setting expectations about operative outcomes is an important part of the preoperative counseling process, Erika L. Rangel, MD, FACS, said at the annual meeting of the American Association for the Surgery of Trauma. In a previous study that she and her associates conducted at Brigham and Women’s Hospital, Boston, the risk for mortality was found to continue long after hospital discharge in older patients who undergo emergency surgery: 16% at 30 days, 22% at 3 months, 28% at 6 months, and 32% 1 year after surgery (J Trauma and Acute Care Surg. 2015 Sep;79[3]:349-58).
Traditionally, surgeons use subjective opinion or basic scoring systems such as the American Society of Anesthesiologists (ASA) classification to stratify risk for surgery in elderly patients. “However, the ASA score can be subjective, and there’s inconsistency between evaluators,” Dr. Rangel said. “The Charlson Comorbidity [Index] rates a patient based on the presence or absence of 19 comorbidities, but it doesn’t tell the surgeon anything about the patient’s functional status.” Frailty is a good measure of an elderly patient’s physiologic reserve to withstand an operation, she continued, but is difficult to measure in the acute care setting. One solution is to measure sarcopenia, which predicts postoperative complications, disability, and mortality in elderly elective surgery patients. “The problem is that very few studies have looked at the impact of sarcopenia in the emergency surgery populations, and the ones that exist only look at short-term outcomes, which don’t completely capture the mortality risk,” she said.
In an effort to better understand how sarcopenia affects long-term outcomes after emergency surgery in the elderly, the researchers retrospectively reviewed patients aged 70 years or older who underwent urgent or emergent abdominal surgery at Brigham and Women’s between 2006 and 2011. Patients were stratified by operative severity using the POSSUM (Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity) score. Operations considered major included any laparotomy, open cholecystectomy, and bowel resection, while those considered moderate were laparoscopic cholecystectomy, appendectomy, and hernia repairs without bowel compromise. To measure sarcopenia, the researchers used preoperative CT images to calculate the average bilateral psoas muscle cross-sectional area at the L3 level, normalized for height. Primary outcome was 1-year mortality. Secondary outcomes were mortality at 30 days, 90 days, and 180 days.
Dr. Rangel reported results from 297 patients that were evaluated: 222 with no sarcopenia and 75 with sarcopenia. Their mean age was 78 years, 57% were female, and 84% were white. Compared with nonsarcopenic patients, sarcopenic patients did not differ in terms of age, sex, or race. Comorbidities were high in both groups, with 75% of patients having an ASA score of 3 or greater and 31% having a Charlson score of 4 or greater. More than 40% had some sort of underlying malignancy, yet there were no significant differences between the two groups in terms of ASA scores, Charlson scores, or the prevalence of malignancy.
Compared with nonsarcopenic patients, sarcopenic patients had longer hospital length of stay (14 vs. 11 days, respectively; P = .012), were more likely to require ICU care (67% vs. 50%; P = .012), and had higher in-hospital mortality (27% vs. 9%; P less than .01). In addition, sarcopenic patients had higher hazard ratios of mortality, compared with their nonsarcopenic counterparts, at 30 days (hazard ratio, 3.5; P = .01), 90 days (HR, 3.5; P less than .001), 180 days (HR, 2.6; P = .001), and at 1 year (HR, 2.5; P = .001).
“The measurement of sarcopenia is a practical tool that can be used at the bedside,” Dr. Rangel concluded. “It just takes 3 or 4 minutes using a single axial slice of a preoperative CT scan. Since it uses CT imaging that’s obtained for initial diagnostic purposes, it incurs no additional cost. The identification of sarcopenia has immediate applications for care of the geriatric patient. It should trigger the surgeon to set realistic goals of care and frame expectations about survival [and] should prompt processes of care that improve patient outcomes. High-risk patients might benefit from geriatric consultation or specialized geriatric pathways, early palliative care evaluation, and advance care planning.” She reported having no financial disclosures.
WAIKOLOA, HAWAII – Sarcopenia is an independent predictor of 1-year mortality in elderly patients undergoing emergency abdominal surgery, results from a single-center study demonstrated.
“Setting expectations about operative outcomes is an important part of the preoperative counseling process, Erika L. Rangel, MD, FACS, said at the annual meeting of the American Association for the Surgery of Trauma. In a previous study that she and her associates conducted at Brigham and Women’s Hospital, Boston, the risk for mortality was found to continue long after hospital discharge in older patients who undergo emergency surgery: 16% at 30 days, 22% at 3 months, 28% at 6 months, and 32% 1 year after surgery (J Trauma and Acute Care Surg. 2015 Sep;79[3]:349-58).
Traditionally, surgeons use subjective opinion or basic scoring systems such as the American Society of Anesthesiologists (ASA) classification to stratify risk for surgery in elderly patients. “However, the ASA score can be subjective, and there’s inconsistency between evaluators,” Dr. Rangel said. “The Charlson Comorbidity [Index] rates a patient based on the presence or absence of 19 comorbidities, but it doesn’t tell the surgeon anything about the patient’s functional status.” Frailty is a good measure of an elderly patient’s physiologic reserve to withstand an operation, she continued, but is difficult to measure in the acute care setting. One solution is to measure sarcopenia, which predicts postoperative complications, disability, and mortality in elderly elective surgery patients. “The problem is that very few studies have looked at the impact of sarcopenia in the emergency surgery populations, and the ones that exist only look at short-term outcomes, which don’t completely capture the mortality risk,” she said.
In an effort to better understand how sarcopenia affects long-term outcomes after emergency surgery in the elderly, the researchers retrospectively reviewed patients aged 70 years or older who underwent urgent or emergent abdominal surgery at Brigham and Women’s between 2006 and 2011. Patients were stratified by operative severity using the POSSUM (Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity) score. Operations considered major included any laparotomy, open cholecystectomy, and bowel resection, while those considered moderate were laparoscopic cholecystectomy, appendectomy, and hernia repairs without bowel compromise. To measure sarcopenia, the researchers used preoperative CT images to calculate the average bilateral psoas muscle cross-sectional area at the L3 level, normalized for height. Primary outcome was 1-year mortality. Secondary outcomes were mortality at 30 days, 90 days, and 180 days.
Dr. Rangel reported results from 297 patients that were evaluated: 222 with no sarcopenia and 75 with sarcopenia. Their mean age was 78 years, 57% were female, and 84% were white. Compared with nonsarcopenic patients, sarcopenic patients did not differ in terms of age, sex, or race. Comorbidities were high in both groups, with 75% of patients having an ASA score of 3 or greater and 31% having a Charlson score of 4 or greater. More than 40% had some sort of underlying malignancy, yet there were no significant differences between the two groups in terms of ASA scores, Charlson scores, or the prevalence of malignancy.
Compared with nonsarcopenic patients, sarcopenic patients had longer hospital length of stay (14 vs. 11 days, respectively; P = .012), were more likely to require ICU care (67% vs. 50%; P = .012), and had higher in-hospital mortality (27% vs. 9%; P less than .01). In addition, sarcopenic patients had higher hazard ratios of mortality, compared with their nonsarcopenic counterparts, at 30 days (hazard ratio, 3.5; P = .01), 90 days (HR, 3.5; P less than .001), 180 days (HR, 2.6; P = .001), and at 1 year (HR, 2.5; P = .001).
“The measurement of sarcopenia is a practical tool that can be used at the bedside,” Dr. Rangel concluded. “It just takes 3 or 4 minutes using a single axial slice of a preoperative CT scan. Since it uses CT imaging that’s obtained for initial diagnostic purposes, it incurs no additional cost. The identification of sarcopenia has immediate applications for care of the geriatric patient. It should trigger the surgeon to set realistic goals of care and frame expectations about survival [and] should prompt processes of care that improve patient outcomes. High-risk patients might benefit from geriatric consultation or specialized geriatric pathways, early palliative care evaluation, and advance care planning.” She reported having no financial disclosures.
Key clinical point:
Major finding: Sarcopenic patients had higher hazard ratios of mortality, compared with their nonsarcopenic counterparts, at 30 days (HR, 3.5), 90 days (HR, 3.5), 180 days (HR, 2.6), and at 1 year (HR, 2.5).
Data source: A retrospective review of 297 patients aged 70 years or older who underwent urgent or emergent abdominal surgery at Brigham and Women’s between 2006 and 2011.
Disclosures: Dr. Rangel reported having no financial disclosures.
3D MRI Shows Advantages Over 2D Brachytherapy
Three-dimensional imaging techniques are changing the scope and precision of planning radiotherapy for cervical cancer. Researchers from Jiaotong University in China who compared planning using 3D magnetic resonance imaging and conventional 2D point A–based intracavitary brachytherapy (BT), say 3D imaging exhibits definite advantages “in a complex way.”
Conventional 2D planning (using a fixed reference point) can overestimate tumor dosages and underestimate the dosages for other organs at risk (OARs), such as rectum and bladder, the researchers say. By contrast in this study, they found that, in general, 3D MRI-based planning helped create accurate estimates for increased dose coverage in big tumors, eccentric tumors, and tumors invading adjacent tissues.
Related: Simultaneous Integrated Boost in Lieu of Vaginal Brachytherapy Boost in Endometrial Cancer
In the study, 79 patients with cervical cancer were treated first with CT-based external beam radiation therapy, then with high-dose rate BT (all patients underwent both 2D and 3D planning for HDR-BT). The researchers compared dose-volume histogram (DVH) parameters for gross tumor volume, high-risk clinical target volume, intermediate-risk clinical target volume, and OARs. Cervical cancer was confirmed by histologic examination on biopsy. Twenty patients had big tumors, and 59 had small tumors.
The researchers say their findings indicate that 3D MRI image-guided BT planning generally show advantages in the treatment of cervical cancer with the exception of cervical cancer that feature small tumors.
For small tumors, DVH parameters did not differ significantly between 2D and 3D BT planning. In big tumors, however, almost all DVH parameters were significantly higher in 3D planning compared with 2D planning. Doses to OARs were also higher.
Related: Early Cancer Detection Helps Underserved Women
The researchers found a “diverse” response of small vs big tumors. In the eccentric cervical tumors, 3D BT planning led to more required dosage and reduced doses to the OARs compared with 2D BT planning. In cervical tumors invading adjacent tissues, 3D planning generally increased the tumor dose coverage but diversely affected the doses to OARs compared with 2D planning.
Only in big tumors, the researchers conclude, does 3D BT planning show obvious advantage.
Source:
Ren J, Yuan W, Wang R, et al. PLoS One. 2016;11(9):e0161932.
doi: 10.1371/journal.pone.0161932.
Three-dimensional imaging techniques are changing the scope and precision of planning radiotherapy for cervical cancer. Researchers from Jiaotong University in China who compared planning using 3D magnetic resonance imaging and conventional 2D point A–based intracavitary brachytherapy (BT), say 3D imaging exhibits definite advantages “in a complex way.”
Conventional 2D planning (using a fixed reference point) can overestimate tumor dosages and underestimate the dosages for other organs at risk (OARs), such as rectum and bladder, the researchers say. By contrast in this study, they found that, in general, 3D MRI-based planning helped create accurate estimates for increased dose coverage in big tumors, eccentric tumors, and tumors invading adjacent tissues.
Related: Simultaneous Integrated Boost in Lieu of Vaginal Brachytherapy Boost in Endometrial Cancer
In the study, 79 patients with cervical cancer were treated first with CT-based external beam radiation therapy, then with high-dose rate BT (all patients underwent both 2D and 3D planning for HDR-BT). The researchers compared dose-volume histogram (DVH) parameters for gross tumor volume, high-risk clinical target volume, intermediate-risk clinical target volume, and OARs. Cervical cancer was confirmed by histologic examination on biopsy. Twenty patients had big tumors, and 59 had small tumors.
The researchers say their findings indicate that 3D MRI image-guided BT planning generally show advantages in the treatment of cervical cancer with the exception of cervical cancer that feature small tumors.
For small tumors, DVH parameters did not differ significantly between 2D and 3D BT planning. In big tumors, however, almost all DVH parameters were significantly higher in 3D planning compared with 2D planning. Doses to OARs were also higher.
Related: Early Cancer Detection Helps Underserved Women
The researchers found a “diverse” response of small vs big tumors. In the eccentric cervical tumors, 3D BT planning led to more required dosage and reduced doses to the OARs compared with 2D BT planning. In cervical tumors invading adjacent tissues, 3D planning generally increased the tumor dose coverage but diversely affected the doses to OARs compared with 2D planning.
Only in big tumors, the researchers conclude, does 3D BT planning show obvious advantage.
Source:
Ren J, Yuan W, Wang R, et al. PLoS One. 2016;11(9):e0161932.
doi: 10.1371/journal.pone.0161932.
Three-dimensional imaging techniques are changing the scope and precision of planning radiotherapy for cervical cancer. Researchers from Jiaotong University in China who compared planning using 3D magnetic resonance imaging and conventional 2D point A–based intracavitary brachytherapy (BT), say 3D imaging exhibits definite advantages “in a complex way.”
Conventional 2D planning (using a fixed reference point) can overestimate tumor dosages and underestimate the dosages for other organs at risk (OARs), such as rectum and bladder, the researchers say. By contrast in this study, they found that, in general, 3D MRI-based planning helped create accurate estimates for increased dose coverage in big tumors, eccentric tumors, and tumors invading adjacent tissues.
Related: Simultaneous Integrated Boost in Lieu of Vaginal Brachytherapy Boost in Endometrial Cancer
In the study, 79 patients with cervical cancer were treated first with CT-based external beam radiation therapy, then with high-dose rate BT (all patients underwent both 2D and 3D planning for HDR-BT). The researchers compared dose-volume histogram (DVH) parameters for gross tumor volume, high-risk clinical target volume, intermediate-risk clinical target volume, and OARs. Cervical cancer was confirmed by histologic examination on biopsy. Twenty patients had big tumors, and 59 had small tumors.
The researchers say their findings indicate that 3D MRI image-guided BT planning generally show advantages in the treatment of cervical cancer with the exception of cervical cancer that feature small tumors.
For small tumors, DVH parameters did not differ significantly between 2D and 3D BT planning. In big tumors, however, almost all DVH parameters were significantly higher in 3D planning compared with 2D planning. Doses to OARs were also higher.
Related: Early Cancer Detection Helps Underserved Women
The researchers found a “diverse” response of small vs big tumors. In the eccentric cervical tumors, 3D BT planning led to more required dosage and reduced doses to the OARs compared with 2D BT planning. In cervical tumors invading adjacent tissues, 3D planning generally increased the tumor dose coverage but diversely affected the doses to OARs compared with 2D planning.
Only in big tumors, the researchers conclude, does 3D BT planning show obvious advantage.
Source:
Ren J, Yuan W, Wang R, et al. PLoS One. 2016;11(9):e0161932.
doi: 10.1371/journal.pone.0161932.