User login
Study Points to Risk Factors for Lymphoma
Certain lifestyle, dietary, environmental, serologic, and genetic factors may raise the risk of non-Hodgkin lymphoma (NHL), according to researchers who reviewed 40 years of follow-up data from the Nurses’ Health Study (NHS).
Related: Exercise Lowers Risk of Some Cancers
The researchers, from Brigham and Women’s Hospital, Harvard, and Boston University, all in Massachusetts, aimed to highlight the NHS’s contributions to epidemiologic knowledge of endometrial, ovarian, pancreatic, and hematologic cancers. They focused on findings that identified novel risk factors or markers of early detection or helped clarify discrepant literature.
Because the researchers say severe immune compromise is the “strongest, best-established risk factor” for NHL, they studied factors that might lead to subclinical immune dysregulation, such as diet, body mass index (BMI), and supplement use. They found several risk factors and biomarkers for NHL and more than 35 distinct tumors in that category, including chronic lymphocytic leukemia. Trans fats and red meat, for instance, doubled the risk of NHL. The researchers also found a higher risk for women who reported long-term multivitamin use. However, they found no risk associated with diet or sugar-sweetened soda or aspartame or with dietary intake of vitamin D.
Related: IBD and the Risk of Oral Cancer
Greater adiposity during childhood and adolescence was significantly associated with NHL. The researchers also observed a 19% increased risk of all NHL per 5 kg/m2 increase in BMI in young adulthood. Interestingly, taller women also had a higher risk of NHL.
The researchers conducted one of the first prospective studies to evaluate a putative inverse association of NHL risk with exposure to ambient ultraviolet radiation. They found, “contrary to expectation,” a 10% to 20% increased risk of NHL among women with the highest (vs lowest) ultraviolet-B exposure at baseline and birth, 15 years, and 30 years.
In investigating biomarkers, the researchers noted a “suggestive increase” in chronic lymphocytic leukemia risk associated with an Epstein-Barr virus antibody profile indicative of poor host immune control of the virus.
Related: Sexual Orientation and Cancer Risk
The researchers have established several working groups to study cancers, such as NHL and multiple myeloma. They also are collecting archival tissue specimens for NHL, multiple myeloma, and Hodgkin lymphoma, for better evaluation of factors related to the unique molecular subsets of hematologic tumors.
Source:
Birmann BM, Barnard ME, Bertrand KA, et al. Am J Public Health. 2016;106(9):1608-1615.
doi: 10.2105/AJPH.2016.303337.
Certain lifestyle, dietary, environmental, serologic, and genetic factors may raise the risk of non-Hodgkin lymphoma (NHL), according to researchers who reviewed 40 years of follow-up data from the Nurses’ Health Study (NHS).
Related: Exercise Lowers Risk of Some Cancers
The researchers, from Brigham and Women’s Hospital, Harvard, and Boston University, all in Massachusetts, aimed to highlight the NHS’s contributions to epidemiologic knowledge of endometrial, ovarian, pancreatic, and hematologic cancers. They focused on findings that identified novel risk factors or markers of early detection or helped clarify discrepant literature.
Because the researchers say severe immune compromise is the “strongest, best-established risk factor” for NHL, they studied factors that might lead to subclinical immune dysregulation, such as diet, body mass index (BMI), and supplement use. They found several risk factors and biomarkers for NHL and more than 35 distinct tumors in that category, including chronic lymphocytic leukemia. Trans fats and red meat, for instance, doubled the risk of NHL. The researchers also found a higher risk for women who reported long-term multivitamin use. However, they found no risk associated with diet or sugar-sweetened soda or aspartame or with dietary intake of vitamin D.
Related: IBD and the Risk of Oral Cancer
Greater adiposity during childhood and adolescence was significantly associated with NHL. The researchers also observed a 19% increased risk of all NHL per 5 kg/m2 increase in BMI in young adulthood. Interestingly, taller women also had a higher risk of NHL.
The researchers conducted one of the first prospective studies to evaluate a putative inverse association of NHL risk with exposure to ambient ultraviolet radiation. They found, “contrary to expectation,” a 10% to 20% increased risk of NHL among women with the highest (vs lowest) ultraviolet-B exposure at baseline and birth, 15 years, and 30 years.
In investigating biomarkers, the researchers noted a “suggestive increase” in chronic lymphocytic leukemia risk associated with an Epstein-Barr virus antibody profile indicative of poor host immune control of the virus.
Related: Sexual Orientation and Cancer Risk
The researchers have established several working groups to study cancers, such as NHL and multiple myeloma. They also are collecting archival tissue specimens for NHL, multiple myeloma, and Hodgkin lymphoma, for better evaluation of factors related to the unique molecular subsets of hematologic tumors.
Source:
Birmann BM, Barnard ME, Bertrand KA, et al. Am J Public Health. 2016;106(9):1608-1615.
doi: 10.2105/AJPH.2016.303337.
Certain lifestyle, dietary, environmental, serologic, and genetic factors may raise the risk of non-Hodgkin lymphoma (NHL), according to researchers who reviewed 40 years of follow-up data from the Nurses’ Health Study (NHS).
Related: Exercise Lowers Risk of Some Cancers
The researchers, from Brigham and Women’s Hospital, Harvard, and Boston University, all in Massachusetts, aimed to highlight the NHS’s contributions to epidemiologic knowledge of endometrial, ovarian, pancreatic, and hematologic cancers. They focused on findings that identified novel risk factors or markers of early detection or helped clarify discrepant literature.
Because the researchers say severe immune compromise is the “strongest, best-established risk factor” for NHL, they studied factors that might lead to subclinical immune dysregulation, such as diet, body mass index (BMI), and supplement use. They found several risk factors and biomarkers for NHL and more than 35 distinct tumors in that category, including chronic lymphocytic leukemia. Trans fats and red meat, for instance, doubled the risk of NHL. The researchers also found a higher risk for women who reported long-term multivitamin use. However, they found no risk associated with diet or sugar-sweetened soda or aspartame or with dietary intake of vitamin D.
Related: IBD and the Risk of Oral Cancer
Greater adiposity during childhood and adolescence was significantly associated with NHL. The researchers also observed a 19% increased risk of all NHL per 5 kg/m2 increase in BMI in young adulthood. Interestingly, taller women also had a higher risk of NHL.
The researchers conducted one of the first prospective studies to evaluate a putative inverse association of NHL risk with exposure to ambient ultraviolet radiation. They found, “contrary to expectation,” a 10% to 20% increased risk of NHL among women with the highest (vs lowest) ultraviolet-B exposure at baseline and birth, 15 years, and 30 years.
In investigating biomarkers, the researchers noted a “suggestive increase” in chronic lymphocytic leukemia risk associated with an Epstein-Barr virus antibody profile indicative of poor host immune control of the virus.
Related: Sexual Orientation and Cancer Risk
The researchers have established several working groups to study cancers, such as NHL and multiple myeloma. They also are collecting archival tissue specimens for NHL, multiple myeloma, and Hodgkin lymphoma, for better evaluation of factors related to the unique molecular subsets of hematologic tumors.
Source:
Birmann BM, Barnard ME, Bertrand KA, et al. Am J Public Health. 2016;106(9):1608-1615.
doi: 10.2105/AJPH.2016.303337.
Solving the VA Physician Shortage Problem: The Right Thing to Do
In this presidential election cycle, health care issues are at the forefront of political discussions. In particular, presidential candidate Donald Trump has spotlighted the issue of caring for veterans by offering a 10-point plan.1 Mr. Trump insists that his plan would ensure that veterans have convenient access to the best quality care and “decrease wait time, improve health care outcomes, and facilitate a seamless transition from service to civilian life.”2
Whether one agrees with Mr. Trump’s policy proposals or not, one thing is clear: We need to provide better care for our veterans.3 Even the Veterans Choice Program, enacted 2 years ago, has shown signs of substantial difficulties.4 The improvement of veteran care likely requires a multifaceted approach. There are many factors that can, and do, hinder the optimal delivery of care, but the shortages of nurses, pharmacists, nurse practitioners, physician assistants, and other health care providers is one of the most important.5
The shortage of physicians, which is the focus of this editorial, is especially acute.5 The Office of Inspector General (OIG) determined that a shortage of medical officers (defined as health care providers with an MD or DO degree) was the top issue affecting veteran care and the nurse shortage was second.5 However, the study did not break down the physician shortage by clinical specialty. According to other reports, the VA’s specialty physician shortage seems to vary. While some VA medical centers (VAMCs) had a shortage of primary care physicians (PCPs), others had a greater need for specialists.6,7
Enhancing communication regarding the importance of veteran care, improving the VA physician recruitment process, and reducing the compensation disparity between VA physicians and non-VA physicians may help reduce the VA physician shortage indicated by OIG. Still the best way to resolve the VA physician shortage is unclear.
I propose that instituting a service requirement for graduating residents is possibly a more effective way to solve the VA physician shortage. I will delineate my argument in 3 simple points: fairness, feasibility, and altruism.
Fairness
The VAMCs have been the backbone of resident physician training and therefore deserve to be served by the graduating residents they help to train. Historically, VAMCs often have been affiliated with nearby medical schools to provide veterans with state-of-the-art health care. In turn, VAMCs provide some of the best training opportunities for resident physicians and medical students. Drs. Magnuson and DeBakey conceived the idea of a “marriage” between a VAMC and a medical school following World War II.8 With few exceptions, the best residency programs have at least 1 VAMC affiliation. According to the 2016 ranking of the best medical schools in the U.S. by U.S. News and World Report, 13 of the top 15 medical schools have a VAMC affiliate.9 Currently, the VA has formal affiliation agreements with 135 of 141 medical schools.8
Each year, VAMCs provide practical experience to medical students, resident physicians, and other health care trainees. In 2013, more than 20,000 medical students, 41,000 resident physicians, and 300 fellowship physicians received part or all of their training at VAMCs. Overall, about 70% of all U.S. physicians received their training at VA facilities.
Moreover, VAMCs provide not only the training facility and opportunity, but also substantial financial support to train residents: They currently fund more than 10,000 full-time equivalent positions for residents, about one-third of all resident positions in the U.S.8 While other federal government funding for residency training programs has flat-lined, the VA is the only federal government agency that has received increased funding recently.8 Most of the remaining federal funding for residency programs is provided through Medicare.
Given that the federal government (and the VA in particular) has provided so much support for resident physician training, it is perhaps fair that we ask our graduated residents to help solve the VA physician shortage. In addition, VA could consider tying in this service with a student loan reduction program, which would make this arrangement not only ethically compelling, but also financially practical.
Feasibility
Currently about 30,000 resident physicians graduate from 4,756 programs in the U.S. yearly.10 It has been estimated there is a shortage of 1,400 VA physicians in the U.S. The VA needs < 5% of graduating resident physicians to serve in VAMCs for 1 year in order to completely and certainly solve the physician shortage problem.
To be sure, the optimum resolution would be for the VA to recruit permanent physicians who build long-term, trusting relationships with patients and continuity of care. However, with the current situation in which permanent positions are left unfilled, a short-term program may be better than the status quo. In addition, having experienced the VA working environment, some of these newly graduated physicians serving short-term at the VA may decide later to make the VA a permanent home.
How do we then carry out this requirement? First, we could ask for volunteers once the VA determines the exact number of physicians needed in a given year. If resident physicians volunteers cannot meet VA’s needs, the remaining slots can be filled using a lottery.
Logistically, a lottery can be achieved in the following way. The process needs to be started 3 years before graduation due to residents’ need for advanced career planning. For the 3-year residency program, the lottery would be held at the beginning of the first year of residency. For the 5-year residency program, the lottery would be held at the beginning of third year of residency. All residency programs would be required to report the names of residents and residents who volunteer for 1 year VA service after residency to a central government depository, which would run a random, computerized process to generate names of the residents for the obligation. Residents would learn the lottery results no later than the end of that training year, so residents would have 2 years to plan for their careers, either for a permanent job or additional fellowship training, according to the lottery outcomes. Obviously, federal legislation would be needed to fund and establish the rightful authority to enforce the arrangement.
Altruism
Whether a person is a Republican, Democrat, or independent, we all sincerely appreciate the sacrifice that veterans provide to protect our nation through the ages. Regardless if one agrees with the objective of a particular war or not, our veterans served at the command of the presidents from both major parties. Veterans simply serve their country with their lives on the line. Since World War I, 116,516 World War I, 405,399 World War II, 54,246 Korean War, 90,220 Vietnam War, and 4,424 Operation Iraq Freedom U.S. soldiers and military personnel have died for our country during active duty.11,12 In addition, many more veterans experienced permanent injuries and illness while protecting our country and our freedom.11,12 Is it too much to ask our graduated residents, albeit a tiny percentage, to share some of the burden to care for our national heroes for just 1 year? I certainly do not think so.
One possible way to raise national awareness of the need for veteran health care is to make this issue a national service obligation, much like that of military service. We could promote the concept in a slogan, such as “The soldiers’ obligation: Serve the nation in the front lines; the nation’s obligation: Provides care when soldiers return home.” Volunteerism is the preferred method of military recruitment. However, if voluntary enlistment does not fulfill the military need, drafting may be the next necessity. The same logical argument can be used to promote the solution for the VA physician shortage.
Although I’ve focused on the solution for physicians, the same process can be expanded for the shortage of nurses, nurse practitioners, physician assistants, and other health care providers. That way, the VA patient would receive even better care.
I’ve served as a part-time VA physician for 25 consecutive years, and I have gladly provided care for our veterans and would be delighted to welcome our graduating residents in joining me and other dedicated VA physicians in this noble effort. As one Chicago VAMC banner beautifully depicted, “Honored to serve … those who served” (Figure), this is, indeed, the right thing to do.
1. Snyder C. Donald Trump vows to take on ‘corrupt’ Veterans Affairs. Fox News. October 31, 2016. http://www.foxnews.com/politics/2015/10/31/donald-trump-vows-to-take-on-corrupt-veterans-affairs.html. Accessed August 30, 2016.
2. Veterans administration reforms that will make America great again. https://assets.donaldjtrump.com/veterans-administration-reforms.pdf. Accessed August 29, 2016.
3. Galvan A. Problems remain at Phoenix VA hospital after scandal. The Washington Times. April 9, 2015. http://www.washingtontimes.com/news/2015/apr/9/problems-remain-at-phoenix-va-hospital-after-scand. Accessed August 30, 2016.
4. Walsh S. How congress and the VA left many veterans without a ‘choice’ [transcript]. Morning Edition. National Public Radio. http://www.npr.org/2016/05/17/478215589/how-congress-and-the-va-left-many-veterans-without-a-choice. Published May 17, 2016. Accessed August 29, 2016.
5. VA Office of Inspector General. OIG determination of veterans health administration’s occupational staffing shortages. http://www.va.gov/oig/pubs/VAOIG-15-00430-103.pdf. Accessed August 30, 2016.
6. Oppel RA Jr, Goodnough A. Doctor shortage is cited in delays at VA hospitals. The New York Times. http://www.nytimes.com/2014/05/30/us/doctor-shortages-cited-in-va-hospital-waits.html. Published May 29, 2014. Accessed August 30, 2016.
7. Grover A, Prescott JE, Shick M. AAMC presentation to the Department of Veterans Affairs Commission on Care. https://commissiononcare.sites.usa.gov/files/2016/01/20151116-09-AAMC_Presentation_to_Commission_on_Care-111715.pdf. Published November 17, 2015. Accessed August 30, 2016.
8. McDonald RA. Viewpoint: VA’s affiliations with medical schools are good for veterans and all Americans. https://www.aamc.org/newsroom/reporter/april2015/429704/viewpoint.html. Published April 2015. Accessed August 30, 2016.
9. U.S. News and World Report. Best medical schools: Research. http://grad-schools.usnews.rankingsandreviews.com/best-graduate-schools/top-medical-schools/research-rankings. Accessed August 30, 2016.
10. The Match. 2015 residency match largest on record with more than 41,000 applicants vying for over 30,000 residency positions in 4,756 programs [press release]. http://www.nrmp.org/press-release-2015-residency-match-largest-on-record-with-more-than-41000-applicants-vying-for-over-30000-residency-positions-in-4756-programs. Accessed August 30, 2016.
11. Department of Veterans Affairs, Office of Public Affairs. America’s wars. http://www.va.gov/opa/publications/factsheets/fs_americas_wars.pdf. Accessed August 30, 2016.
12. U.S. Department of Defense. Casualty status. http://www.defense.gov/casualty.pdf. Accessed August 30, 2016.
In this presidential election cycle, health care issues are at the forefront of political discussions. In particular, presidential candidate Donald Trump has spotlighted the issue of caring for veterans by offering a 10-point plan.1 Mr. Trump insists that his plan would ensure that veterans have convenient access to the best quality care and “decrease wait time, improve health care outcomes, and facilitate a seamless transition from service to civilian life.”2
Whether one agrees with Mr. Trump’s policy proposals or not, one thing is clear: We need to provide better care for our veterans.3 Even the Veterans Choice Program, enacted 2 years ago, has shown signs of substantial difficulties.4 The improvement of veteran care likely requires a multifaceted approach. There are many factors that can, and do, hinder the optimal delivery of care, but the shortages of nurses, pharmacists, nurse practitioners, physician assistants, and other health care providers is one of the most important.5
The shortage of physicians, which is the focus of this editorial, is especially acute.5 The Office of Inspector General (OIG) determined that a shortage of medical officers (defined as health care providers with an MD or DO degree) was the top issue affecting veteran care and the nurse shortage was second.5 However, the study did not break down the physician shortage by clinical specialty. According to other reports, the VA’s specialty physician shortage seems to vary. While some VA medical centers (VAMCs) had a shortage of primary care physicians (PCPs), others had a greater need for specialists.6,7
Enhancing communication regarding the importance of veteran care, improving the VA physician recruitment process, and reducing the compensation disparity between VA physicians and non-VA physicians may help reduce the VA physician shortage indicated by OIG. Still the best way to resolve the VA physician shortage is unclear.
I propose that instituting a service requirement for graduating residents is possibly a more effective way to solve the VA physician shortage. I will delineate my argument in 3 simple points: fairness, feasibility, and altruism.
Fairness
The VAMCs have been the backbone of resident physician training and therefore deserve to be served by the graduating residents they help to train. Historically, VAMCs often have been affiliated with nearby medical schools to provide veterans with state-of-the-art health care. In turn, VAMCs provide some of the best training opportunities for resident physicians and medical students. Drs. Magnuson and DeBakey conceived the idea of a “marriage” between a VAMC and a medical school following World War II.8 With few exceptions, the best residency programs have at least 1 VAMC affiliation. According to the 2016 ranking of the best medical schools in the U.S. by U.S. News and World Report, 13 of the top 15 medical schools have a VAMC affiliate.9 Currently, the VA has formal affiliation agreements with 135 of 141 medical schools.8
Each year, VAMCs provide practical experience to medical students, resident physicians, and other health care trainees. In 2013, more than 20,000 medical students, 41,000 resident physicians, and 300 fellowship physicians received part or all of their training at VAMCs. Overall, about 70% of all U.S. physicians received their training at VA facilities.
Moreover, VAMCs provide not only the training facility and opportunity, but also substantial financial support to train residents: They currently fund more than 10,000 full-time equivalent positions for residents, about one-third of all resident positions in the U.S.8 While other federal government funding for residency training programs has flat-lined, the VA is the only federal government agency that has received increased funding recently.8 Most of the remaining federal funding for residency programs is provided through Medicare.
Given that the federal government (and the VA in particular) has provided so much support for resident physician training, it is perhaps fair that we ask our graduated residents to help solve the VA physician shortage. In addition, VA could consider tying in this service with a student loan reduction program, which would make this arrangement not only ethically compelling, but also financially practical.
Feasibility
Currently about 30,000 resident physicians graduate from 4,756 programs in the U.S. yearly.10 It has been estimated there is a shortage of 1,400 VA physicians in the U.S. The VA needs < 5% of graduating resident physicians to serve in VAMCs for 1 year in order to completely and certainly solve the physician shortage problem.
To be sure, the optimum resolution would be for the VA to recruit permanent physicians who build long-term, trusting relationships with patients and continuity of care. However, with the current situation in which permanent positions are left unfilled, a short-term program may be better than the status quo. In addition, having experienced the VA working environment, some of these newly graduated physicians serving short-term at the VA may decide later to make the VA a permanent home.
How do we then carry out this requirement? First, we could ask for volunteers once the VA determines the exact number of physicians needed in a given year. If resident physicians volunteers cannot meet VA’s needs, the remaining slots can be filled using a lottery.
Logistically, a lottery can be achieved in the following way. The process needs to be started 3 years before graduation due to residents’ need for advanced career planning. For the 3-year residency program, the lottery would be held at the beginning of the first year of residency. For the 5-year residency program, the lottery would be held at the beginning of third year of residency. All residency programs would be required to report the names of residents and residents who volunteer for 1 year VA service after residency to a central government depository, which would run a random, computerized process to generate names of the residents for the obligation. Residents would learn the lottery results no later than the end of that training year, so residents would have 2 years to plan for their careers, either for a permanent job or additional fellowship training, according to the lottery outcomes. Obviously, federal legislation would be needed to fund and establish the rightful authority to enforce the arrangement.
Altruism
Whether a person is a Republican, Democrat, or independent, we all sincerely appreciate the sacrifice that veterans provide to protect our nation through the ages. Regardless if one agrees with the objective of a particular war or not, our veterans served at the command of the presidents from both major parties. Veterans simply serve their country with their lives on the line. Since World War I, 116,516 World War I, 405,399 World War II, 54,246 Korean War, 90,220 Vietnam War, and 4,424 Operation Iraq Freedom U.S. soldiers and military personnel have died for our country during active duty.11,12 In addition, many more veterans experienced permanent injuries and illness while protecting our country and our freedom.11,12 Is it too much to ask our graduated residents, albeit a tiny percentage, to share some of the burden to care for our national heroes for just 1 year? I certainly do not think so.
One possible way to raise national awareness of the need for veteran health care is to make this issue a national service obligation, much like that of military service. We could promote the concept in a slogan, such as “The soldiers’ obligation: Serve the nation in the front lines; the nation’s obligation: Provides care when soldiers return home.” Volunteerism is the preferred method of military recruitment. However, if voluntary enlistment does not fulfill the military need, drafting may be the next necessity. The same logical argument can be used to promote the solution for the VA physician shortage.
Although I’ve focused on the solution for physicians, the same process can be expanded for the shortage of nurses, nurse practitioners, physician assistants, and other health care providers. That way, the VA patient would receive even better care.
I’ve served as a part-time VA physician for 25 consecutive years, and I have gladly provided care for our veterans and would be delighted to welcome our graduating residents in joining me and other dedicated VA physicians in this noble effort. As one Chicago VAMC banner beautifully depicted, “Honored to serve … those who served” (Figure), this is, indeed, the right thing to do.
In this presidential election cycle, health care issues are at the forefront of political discussions. In particular, presidential candidate Donald Trump has spotlighted the issue of caring for veterans by offering a 10-point plan.1 Mr. Trump insists that his plan would ensure that veterans have convenient access to the best quality care and “decrease wait time, improve health care outcomes, and facilitate a seamless transition from service to civilian life.”2
Whether one agrees with Mr. Trump’s policy proposals or not, one thing is clear: We need to provide better care for our veterans.3 Even the Veterans Choice Program, enacted 2 years ago, has shown signs of substantial difficulties.4 The improvement of veteran care likely requires a multifaceted approach. There are many factors that can, and do, hinder the optimal delivery of care, but the shortages of nurses, pharmacists, nurse practitioners, physician assistants, and other health care providers is one of the most important.5
The shortage of physicians, which is the focus of this editorial, is especially acute.5 The Office of Inspector General (OIG) determined that a shortage of medical officers (defined as health care providers with an MD or DO degree) was the top issue affecting veteran care and the nurse shortage was second.5 However, the study did not break down the physician shortage by clinical specialty. According to other reports, the VA’s specialty physician shortage seems to vary. While some VA medical centers (VAMCs) had a shortage of primary care physicians (PCPs), others had a greater need for specialists.6,7
Enhancing communication regarding the importance of veteran care, improving the VA physician recruitment process, and reducing the compensation disparity between VA physicians and non-VA physicians may help reduce the VA physician shortage indicated by OIG. Still the best way to resolve the VA physician shortage is unclear.
I propose that instituting a service requirement for graduating residents is possibly a more effective way to solve the VA physician shortage. I will delineate my argument in 3 simple points: fairness, feasibility, and altruism.
Fairness
The VAMCs have been the backbone of resident physician training and therefore deserve to be served by the graduating residents they help to train. Historically, VAMCs often have been affiliated with nearby medical schools to provide veterans with state-of-the-art health care. In turn, VAMCs provide some of the best training opportunities for resident physicians and medical students. Drs. Magnuson and DeBakey conceived the idea of a “marriage” between a VAMC and a medical school following World War II.8 With few exceptions, the best residency programs have at least 1 VAMC affiliation. According to the 2016 ranking of the best medical schools in the U.S. by U.S. News and World Report, 13 of the top 15 medical schools have a VAMC affiliate.9 Currently, the VA has formal affiliation agreements with 135 of 141 medical schools.8
Each year, VAMCs provide practical experience to medical students, resident physicians, and other health care trainees. In 2013, more than 20,000 medical students, 41,000 resident physicians, and 300 fellowship physicians received part or all of their training at VAMCs. Overall, about 70% of all U.S. physicians received their training at VA facilities.
Moreover, VAMCs provide not only the training facility and opportunity, but also substantial financial support to train residents: They currently fund more than 10,000 full-time equivalent positions for residents, about one-third of all resident positions in the U.S.8 While other federal government funding for residency training programs has flat-lined, the VA is the only federal government agency that has received increased funding recently.8 Most of the remaining federal funding for residency programs is provided through Medicare.
Given that the federal government (and the VA in particular) has provided so much support for resident physician training, it is perhaps fair that we ask our graduated residents to help solve the VA physician shortage. In addition, VA could consider tying in this service with a student loan reduction program, which would make this arrangement not only ethically compelling, but also financially practical.
Feasibility
Currently about 30,000 resident physicians graduate from 4,756 programs in the U.S. yearly.10 It has been estimated there is a shortage of 1,400 VA physicians in the U.S. The VA needs < 5% of graduating resident physicians to serve in VAMCs for 1 year in order to completely and certainly solve the physician shortage problem.
To be sure, the optimum resolution would be for the VA to recruit permanent physicians who build long-term, trusting relationships with patients and continuity of care. However, with the current situation in which permanent positions are left unfilled, a short-term program may be better than the status quo. In addition, having experienced the VA working environment, some of these newly graduated physicians serving short-term at the VA may decide later to make the VA a permanent home.
How do we then carry out this requirement? First, we could ask for volunteers once the VA determines the exact number of physicians needed in a given year. If resident physicians volunteers cannot meet VA’s needs, the remaining slots can be filled using a lottery.
Logistically, a lottery can be achieved in the following way. The process needs to be started 3 years before graduation due to residents’ need for advanced career planning. For the 3-year residency program, the lottery would be held at the beginning of the first year of residency. For the 5-year residency program, the lottery would be held at the beginning of third year of residency. All residency programs would be required to report the names of residents and residents who volunteer for 1 year VA service after residency to a central government depository, which would run a random, computerized process to generate names of the residents for the obligation. Residents would learn the lottery results no later than the end of that training year, so residents would have 2 years to plan for their careers, either for a permanent job or additional fellowship training, according to the lottery outcomes. Obviously, federal legislation would be needed to fund and establish the rightful authority to enforce the arrangement.
Altruism
Whether a person is a Republican, Democrat, or independent, we all sincerely appreciate the sacrifice that veterans provide to protect our nation through the ages. Regardless if one agrees with the objective of a particular war or not, our veterans served at the command of the presidents from both major parties. Veterans simply serve their country with their lives on the line. Since World War I, 116,516 World War I, 405,399 World War II, 54,246 Korean War, 90,220 Vietnam War, and 4,424 Operation Iraq Freedom U.S. soldiers and military personnel have died for our country during active duty.11,12 In addition, many more veterans experienced permanent injuries and illness while protecting our country and our freedom.11,12 Is it too much to ask our graduated residents, albeit a tiny percentage, to share some of the burden to care for our national heroes for just 1 year? I certainly do not think so.
One possible way to raise national awareness of the need for veteran health care is to make this issue a national service obligation, much like that of military service. We could promote the concept in a slogan, such as “The soldiers’ obligation: Serve the nation in the front lines; the nation’s obligation: Provides care when soldiers return home.” Volunteerism is the preferred method of military recruitment. However, if voluntary enlistment does not fulfill the military need, drafting may be the next necessity. The same logical argument can be used to promote the solution for the VA physician shortage.
Although I’ve focused on the solution for physicians, the same process can be expanded for the shortage of nurses, nurse practitioners, physician assistants, and other health care providers. That way, the VA patient would receive even better care.
I’ve served as a part-time VA physician for 25 consecutive years, and I have gladly provided care for our veterans and would be delighted to welcome our graduating residents in joining me and other dedicated VA physicians in this noble effort. As one Chicago VAMC banner beautifully depicted, “Honored to serve … those who served” (Figure), this is, indeed, the right thing to do.
1. Snyder C. Donald Trump vows to take on ‘corrupt’ Veterans Affairs. Fox News. October 31, 2016. http://www.foxnews.com/politics/2015/10/31/donald-trump-vows-to-take-on-corrupt-veterans-affairs.html. Accessed August 30, 2016.
2. Veterans administration reforms that will make America great again. https://assets.donaldjtrump.com/veterans-administration-reforms.pdf. Accessed August 29, 2016.
3. Galvan A. Problems remain at Phoenix VA hospital after scandal. The Washington Times. April 9, 2015. http://www.washingtontimes.com/news/2015/apr/9/problems-remain-at-phoenix-va-hospital-after-scand. Accessed August 30, 2016.
4. Walsh S. How congress and the VA left many veterans without a ‘choice’ [transcript]. Morning Edition. National Public Radio. http://www.npr.org/2016/05/17/478215589/how-congress-and-the-va-left-many-veterans-without-a-choice. Published May 17, 2016. Accessed August 29, 2016.
5. VA Office of Inspector General. OIG determination of veterans health administration’s occupational staffing shortages. http://www.va.gov/oig/pubs/VAOIG-15-00430-103.pdf. Accessed August 30, 2016.
6. Oppel RA Jr, Goodnough A. Doctor shortage is cited in delays at VA hospitals. The New York Times. http://www.nytimes.com/2014/05/30/us/doctor-shortages-cited-in-va-hospital-waits.html. Published May 29, 2014. Accessed August 30, 2016.
7. Grover A, Prescott JE, Shick M. AAMC presentation to the Department of Veterans Affairs Commission on Care. https://commissiononcare.sites.usa.gov/files/2016/01/20151116-09-AAMC_Presentation_to_Commission_on_Care-111715.pdf. Published November 17, 2015. Accessed August 30, 2016.
8. McDonald RA. Viewpoint: VA’s affiliations with medical schools are good for veterans and all Americans. https://www.aamc.org/newsroom/reporter/april2015/429704/viewpoint.html. Published April 2015. Accessed August 30, 2016.
9. U.S. News and World Report. Best medical schools: Research. http://grad-schools.usnews.rankingsandreviews.com/best-graduate-schools/top-medical-schools/research-rankings. Accessed August 30, 2016.
10. The Match. 2015 residency match largest on record with more than 41,000 applicants vying for over 30,000 residency positions in 4,756 programs [press release]. http://www.nrmp.org/press-release-2015-residency-match-largest-on-record-with-more-than-41000-applicants-vying-for-over-30000-residency-positions-in-4756-programs. Accessed August 30, 2016.
11. Department of Veterans Affairs, Office of Public Affairs. America’s wars. http://www.va.gov/opa/publications/factsheets/fs_americas_wars.pdf. Accessed August 30, 2016.
12. U.S. Department of Defense. Casualty status. http://www.defense.gov/casualty.pdf. Accessed August 30, 2016.
1. Snyder C. Donald Trump vows to take on ‘corrupt’ Veterans Affairs. Fox News. October 31, 2016. http://www.foxnews.com/politics/2015/10/31/donald-trump-vows-to-take-on-corrupt-veterans-affairs.html. Accessed August 30, 2016.
2. Veterans administration reforms that will make America great again. https://assets.donaldjtrump.com/veterans-administration-reforms.pdf. Accessed August 29, 2016.
3. Galvan A. Problems remain at Phoenix VA hospital after scandal. The Washington Times. April 9, 2015. http://www.washingtontimes.com/news/2015/apr/9/problems-remain-at-phoenix-va-hospital-after-scand. Accessed August 30, 2016.
4. Walsh S. How congress and the VA left many veterans without a ‘choice’ [transcript]. Morning Edition. National Public Radio. http://www.npr.org/2016/05/17/478215589/how-congress-and-the-va-left-many-veterans-without-a-choice. Published May 17, 2016. Accessed August 29, 2016.
5. VA Office of Inspector General. OIG determination of veterans health administration’s occupational staffing shortages. http://www.va.gov/oig/pubs/VAOIG-15-00430-103.pdf. Accessed August 30, 2016.
6. Oppel RA Jr, Goodnough A. Doctor shortage is cited in delays at VA hospitals. The New York Times. http://www.nytimes.com/2014/05/30/us/doctor-shortages-cited-in-va-hospital-waits.html. Published May 29, 2014. Accessed August 30, 2016.
7. Grover A, Prescott JE, Shick M. AAMC presentation to the Department of Veterans Affairs Commission on Care. https://commissiononcare.sites.usa.gov/files/2016/01/20151116-09-AAMC_Presentation_to_Commission_on_Care-111715.pdf. Published November 17, 2015. Accessed August 30, 2016.
8. McDonald RA. Viewpoint: VA’s affiliations with medical schools are good for veterans and all Americans. https://www.aamc.org/newsroom/reporter/april2015/429704/viewpoint.html. Published April 2015. Accessed August 30, 2016.
9. U.S. News and World Report. Best medical schools: Research. http://grad-schools.usnews.rankingsandreviews.com/best-graduate-schools/top-medical-schools/research-rankings. Accessed August 30, 2016.
10. The Match. 2015 residency match largest on record with more than 41,000 applicants vying for over 30,000 residency positions in 4,756 programs [press release]. http://www.nrmp.org/press-release-2015-residency-match-largest-on-record-with-more-than-41000-applicants-vying-for-over-30000-residency-positions-in-4756-programs. Accessed August 30, 2016.
11. Department of Veterans Affairs, Office of Public Affairs. America’s wars. http://www.va.gov/opa/publications/factsheets/fs_americas_wars.pdf. Accessed August 30, 2016.
12. U.S. Department of Defense. Casualty status. http://www.defense.gov/casualty.pdf. Accessed August 30, 2016.
How to Better Connect with Patients
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
View a chart outlining key communication tactics
What I Say and Do
Before entering a patient’s room, I take a “mindful moment,” a brief mindfulness practice to boost empathy. This is a quick, simple, and effective way for me to rehab my empathy muscle.
Why I Do It
From empathy comes our desire to care about another human being, to connect with them, and to understand and be understood.
Many of the colleagues I talk to about patient experience echo the same sentiment: They feel powerless to change someone else’s experience, which is bundled with the immovable variables of their own perceptions and contexts.
While I believe there is truth to that, we can certainly change our experience, and that is what matters to patients. As my mentor and coach Anya Sophia Mann reminded me recently, “We are not responsible for the patient experience. We are responsible for our own experience, which we then bring to our patients. Your heart connection to your own empathic center is beautifully contagious and will spread to those around you throughout your day.”
How I Do It
We may think that empathy is an innate talent, but the literature supports that it is a skill like any other that can be taught, practiced, and deliberately and consciously turned up and down like the brightness on your smartphone.
A heartfelt patient experience starts with the feeling of connection to our own heart. But we can’t think our way into a feeling. If I let my head lead the way, I shield my heart from participating in true communication with the patient. We are both left without connection, without a sense of purpose, without fulfillment—empty and tired.
For the antidote, I choose to create an experience for my body to feel rather than an idea for my head to think about. Ironically, mindfulness starts not with the mind but with the body and, more precisely, with the breath.
Before entering the patient’s room, usually as I’m rubbing the hand sanitizer between my fingers, I take a deep breath that expands my belly instead of my chest, then I exhale, leaving plenty of time for the complete out breath. Next, I make the choice to be curious about the sensations in my body: “What have I carried with me from my interaction with the previous patient (or the nurse or the driver in front of me during my commute)? Does my jaw feel tight? Where do I feel stuck? Where exactly does that lump in my throat begin and end?”
The instruction here is just to notice without judgment. From that place of noticing, I have done a quick erasing of my emotional whiteboard to create space where I can respond rather than react to what is most important to my patient. I invite you to try these steps and notice what shifts happen for you and your patients. You won’t know it until you try it—and feel it—for yourself.
- Pause long enough to feel the ground supporting you under both feet.
- Take a deep, cleansing belly breath. Exhale fully without added effort.
- Notice, without judgment, the sensations in your body.
- Feel the space created by the melting and releasing of those feelings.
- Bring that feeling of space with you as you begin the conversation with the patient.
Michael Donlin, ACNP-BC, FHM, is an inpatient nurse practitioner for the Department of Medicine, VA Boston Healthcare System.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
View a chart outlining key communication tactics
What I Say and Do
Before entering a patient’s room, I take a “mindful moment,” a brief mindfulness practice to boost empathy. This is a quick, simple, and effective way for me to rehab my empathy muscle.
Why I Do It
From empathy comes our desire to care about another human being, to connect with them, and to understand and be understood.
Many of the colleagues I talk to about patient experience echo the same sentiment: They feel powerless to change someone else’s experience, which is bundled with the immovable variables of their own perceptions and contexts.
While I believe there is truth to that, we can certainly change our experience, and that is what matters to patients. As my mentor and coach Anya Sophia Mann reminded me recently, “We are not responsible for the patient experience. We are responsible for our own experience, which we then bring to our patients. Your heart connection to your own empathic center is beautifully contagious and will spread to those around you throughout your day.”
How I Do It
We may think that empathy is an innate talent, but the literature supports that it is a skill like any other that can be taught, practiced, and deliberately and consciously turned up and down like the brightness on your smartphone.
A heartfelt patient experience starts with the feeling of connection to our own heart. But we can’t think our way into a feeling. If I let my head lead the way, I shield my heart from participating in true communication with the patient. We are both left without connection, without a sense of purpose, without fulfillment—empty and tired.
For the antidote, I choose to create an experience for my body to feel rather than an idea for my head to think about. Ironically, mindfulness starts not with the mind but with the body and, more precisely, with the breath.
Before entering the patient’s room, usually as I’m rubbing the hand sanitizer between my fingers, I take a deep breath that expands my belly instead of my chest, then I exhale, leaving plenty of time for the complete out breath. Next, I make the choice to be curious about the sensations in my body: “What have I carried with me from my interaction with the previous patient (or the nurse or the driver in front of me during my commute)? Does my jaw feel tight? Where do I feel stuck? Where exactly does that lump in my throat begin and end?”
The instruction here is just to notice without judgment. From that place of noticing, I have done a quick erasing of my emotional whiteboard to create space where I can respond rather than react to what is most important to my patient. I invite you to try these steps and notice what shifts happen for you and your patients. You won’t know it until you try it—and feel it—for yourself.
- Pause long enough to feel the ground supporting you under both feet.
- Take a deep, cleansing belly breath. Exhale fully without added effort.
- Notice, without judgment, the sensations in your body.
- Feel the space created by the melting and releasing of those feelings.
- Bring that feeling of space with you as you begin the conversation with the patient.
Michael Donlin, ACNP-BC, FHM, is an inpatient nurse practitioner for the Department of Medicine, VA Boston Healthcare System.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
View a chart outlining key communication tactics
What I Say and Do
Before entering a patient’s room, I take a “mindful moment,” a brief mindfulness practice to boost empathy. This is a quick, simple, and effective way for me to rehab my empathy muscle.
Why I Do It
From empathy comes our desire to care about another human being, to connect with them, and to understand and be understood.
Many of the colleagues I talk to about patient experience echo the same sentiment: They feel powerless to change someone else’s experience, which is bundled with the immovable variables of their own perceptions and contexts.
While I believe there is truth to that, we can certainly change our experience, and that is what matters to patients. As my mentor and coach Anya Sophia Mann reminded me recently, “We are not responsible for the patient experience. We are responsible for our own experience, which we then bring to our patients. Your heart connection to your own empathic center is beautifully contagious and will spread to those around you throughout your day.”
How I Do It
We may think that empathy is an innate talent, but the literature supports that it is a skill like any other that can be taught, practiced, and deliberately and consciously turned up and down like the brightness on your smartphone.
A heartfelt patient experience starts with the feeling of connection to our own heart. But we can’t think our way into a feeling. If I let my head lead the way, I shield my heart from participating in true communication with the patient. We are both left without connection, without a sense of purpose, without fulfillment—empty and tired.
For the antidote, I choose to create an experience for my body to feel rather than an idea for my head to think about. Ironically, mindfulness starts not with the mind but with the body and, more precisely, with the breath.
Before entering the patient’s room, usually as I’m rubbing the hand sanitizer between my fingers, I take a deep breath that expands my belly instead of my chest, then I exhale, leaving plenty of time for the complete out breath. Next, I make the choice to be curious about the sensations in my body: “What have I carried with me from my interaction with the previous patient (or the nurse or the driver in front of me during my commute)? Does my jaw feel tight? Where do I feel stuck? Where exactly does that lump in my throat begin and end?”
The instruction here is just to notice without judgment. From that place of noticing, I have done a quick erasing of my emotional whiteboard to create space where I can respond rather than react to what is most important to my patient. I invite you to try these steps and notice what shifts happen for you and your patients. You won’t know it until you try it—and feel it—for yourself.
- Pause long enough to feel the ground supporting you under both feet.
- Take a deep, cleansing belly breath. Exhale fully without added effort.
- Notice, without judgment, the sensations in your body.
- Feel the space created by the melting and releasing of those feelings.
- Bring that feeling of space with you as you begin the conversation with the patient.
Michael Donlin, ACNP-BC, FHM, is an inpatient nurse practitioner for the Department of Medicine, VA Boston Healthcare System.
Vitamin D affects HSPC production, team says
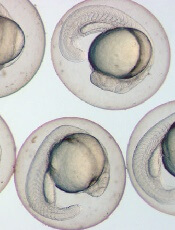
Photo by Ian Johnston
The availability of vitamin D during embryonic development can affect hematopoietic stem and progenitor cells (HSPCs), according to research published in Cell Reports.
Experiments with zebrafish embryos suggested that vitamin D acts directly on HSPCs to increase proliferation.
Similarly, in HSPCs from human umbilical cords, treatment with vitamin D enhanced hematopoietic colony numbers.
Researchers therefore theorized that vitamin D supplementation might be useful for HSPC expansion prior to transplant.
“We clearly showed that not getting enough vitamin D can alter how blood stem cells are formed,” said study author Trista North, PhD, of Beth Israel Deaconess Medical Center in Boston, Massachusetts.
“Vitamin D was having a direct response on the blood stem cells, and it changed what those cells did in terms of multiplying and staying alive.”
The researchers found, in both human and zebrafish tissue, that 1,25(OH)D3 (active vitamin D3) had an impact on HSPC production and function.
Investigation into the mechanism revealed that CXCL8-CXCR1/2 signaling functions downstream of 1,25(OH)D3-mediated vitamin D receptor stimulation to directly regulate HSPC production and expansion.
“What was surprising was that vitamin D is having an impact so early,” Dr North said. “We really only thought about vitamin D in terms of bone development and maintenance, but we clearly show that, whether they were zebrafish or human blood stem cells, they can respond directly to the nutrient.”
One caveat is the researchers did face difficulty testing the response in mice, as the animals don’t have the same vitamin D inflammatory targets observed in zebrafish and humans.
Additionally, the team didn’t know the vitamin D levels in the umbilical cord blood samples they tested, which may have influenced the outcome of their analysis.
As a next step, Dr North and her colleagues hope to test cord blood samples for which they know the vitamin D status to see if umbilical cords with healthy levels respond better or worse to stimulation than cords from vitamin-D-deficient donors. ![]()
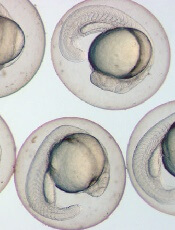
Photo by Ian Johnston
The availability of vitamin D during embryonic development can affect hematopoietic stem and progenitor cells (HSPCs), according to research published in Cell Reports.
Experiments with zebrafish embryos suggested that vitamin D acts directly on HSPCs to increase proliferation.
Similarly, in HSPCs from human umbilical cords, treatment with vitamin D enhanced hematopoietic colony numbers.
Researchers therefore theorized that vitamin D supplementation might be useful for HSPC expansion prior to transplant.
“We clearly showed that not getting enough vitamin D can alter how blood stem cells are formed,” said study author Trista North, PhD, of Beth Israel Deaconess Medical Center in Boston, Massachusetts.
“Vitamin D was having a direct response on the blood stem cells, and it changed what those cells did in terms of multiplying and staying alive.”
The researchers found, in both human and zebrafish tissue, that 1,25(OH)D3 (active vitamin D3) had an impact on HSPC production and function.
Investigation into the mechanism revealed that CXCL8-CXCR1/2 signaling functions downstream of 1,25(OH)D3-mediated vitamin D receptor stimulation to directly regulate HSPC production and expansion.
“What was surprising was that vitamin D is having an impact so early,” Dr North said. “We really only thought about vitamin D in terms of bone development and maintenance, but we clearly show that, whether they were zebrafish or human blood stem cells, they can respond directly to the nutrient.”
One caveat is the researchers did face difficulty testing the response in mice, as the animals don’t have the same vitamin D inflammatory targets observed in zebrafish and humans.
Additionally, the team didn’t know the vitamin D levels in the umbilical cord blood samples they tested, which may have influenced the outcome of their analysis.
As a next step, Dr North and her colleagues hope to test cord blood samples for which they know the vitamin D status to see if umbilical cords with healthy levels respond better or worse to stimulation than cords from vitamin-D-deficient donors. ![]()
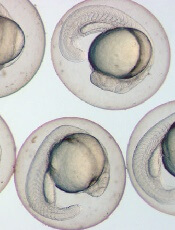
Photo by Ian Johnston
The availability of vitamin D during embryonic development can affect hematopoietic stem and progenitor cells (HSPCs), according to research published in Cell Reports.
Experiments with zebrafish embryos suggested that vitamin D acts directly on HSPCs to increase proliferation.
Similarly, in HSPCs from human umbilical cords, treatment with vitamin D enhanced hematopoietic colony numbers.
Researchers therefore theorized that vitamin D supplementation might be useful for HSPC expansion prior to transplant.
“We clearly showed that not getting enough vitamin D can alter how blood stem cells are formed,” said study author Trista North, PhD, of Beth Israel Deaconess Medical Center in Boston, Massachusetts.
“Vitamin D was having a direct response on the blood stem cells, and it changed what those cells did in terms of multiplying and staying alive.”
The researchers found, in both human and zebrafish tissue, that 1,25(OH)D3 (active vitamin D3) had an impact on HSPC production and function.
Investigation into the mechanism revealed that CXCL8-CXCR1/2 signaling functions downstream of 1,25(OH)D3-mediated vitamin D receptor stimulation to directly regulate HSPC production and expansion.
“What was surprising was that vitamin D is having an impact so early,” Dr North said. “We really only thought about vitamin D in terms of bone development and maintenance, but we clearly show that, whether they were zebrafish or human blood stem cells, they can respond directly to the nutrient.”
One caveat is the researchers did face difficulty testing the response in mice, as the animals don’t have the same vitamin D inflammatory targets observed in zebrafish and humans.
Additionally, the team didn’t know the vitamin D levels in the umbilical cord blood samples they tested, which may have influenced the outcome of their analysis.
As a next step, Dr North and her colleagues hope to test cord blood samples for which they know the vitamin D status to see if umbilical cords with healthy levels respond better or worse to stimulation than cords from vitamin-D-deficient donors. ![]()
Lifestyle may impact life expectancy in mild SCD

alongside a normal one
Image by Betty Pace
A case series published in Blood indicates that some patients with mildly symptomatic sickle cell disease (SCD) can live long lives if they
comply with treatment recommendations and lead a healthy lifestyle.
The paper includes details on 4 women with milder forms of SCD who survived beyond age 80.
“For those with mild forms of SCD, these women show that lifestyle modifications may improve disease outcomes,” said author Samir K. Ballas, MD, of Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia, Pennsylvania.
Three of the women described in this case series were treated at the Sickle Cell Center of Thomas Jefferson University, and 1 was treated in Brazil’s Instituto de Hematologia Arthur de Siqueira Cavalcanti in Rio de Janeiro.
The women had different ancestries—2 African-American, 1 Italian-American, and 1 African-Brazilian—and different diagnoses—2 with hemoglobin SC disease and 2 with sickle cell anemia. But all 4 women had what Dr Ballas called “desirable” disease states.
“These women never had a stroke, never had recurrent acute chest syndrome, had a relatively high fetal hemoglobin count, and had infrequent painful crises,” Dr Ballas said. “Patients like this usually—but not always—experience relatively mild SCD, and they live longer with better quality of life.”
In addition, all of the women took steps to maintain and improve their health and had long-term family support. Dr Ballas said these factors likely contributed to the women’s long lives and high quality of life.
“All of the women were non-smokers who consumed little to no alcohol and maintained a normal body mass index,” he said. “This was coupled with a strong compliance to their treatment regimens and excellent family support at home.”
Family support was defined as having a spouse or child who provided attentive, ongoing care. And all of the women had at least 1 such caregiver.
Treatment compliance was based on observations by healthcare providers, including study authors. According to these observations, all of the women showed “excellent” adherence when it came to medication intake, appointments, and referrals.
As the women had relatively mild disease states, none of them were qualified to receive treatment with hydroxyurea. Instead, they received hydration, vaccination (including annual flu shots), and blood transfusion and analgesics as needed.
Even with their mild disease states and healthy lifestyles, these women did not live crisis-free lives. Each experienced disease-related complications necessitating medical attention.
The women had 0 to 3 vaso-occlusive crises per year. Two women required frequent transfusions (and had iron overload), and 2 required occasional transfusions. One woman had 2 episodes of acute chest syndrome, and the second episode led to her death.
Ultimately, 3 of the women died. One died of acute chest syndrome and septicemia at age 82, and another died of cardiac complications at age 86. For a third woman, the cause of death, at age 82, was unknown. The fourth woman remains alive at age 82.
As the median life expectancy of women with SCD in the US is 47, Dr Ballas and his colleagues said these 4 women may “provide a blueprint of how to live a long life despite having a serious medical condition like SCD.”
“I would often come out to the waiting room and find these ladies talking with other SCD patients, and I could tell that they gave others hope, that just because they have SCD does not mean that they are doomed to die by their 40s . . . ,” Dr Ballas said. “[I]f they take care of themselves and live closely with those who can help keep them well, that there is hope for them to lead long, full lives.” ![]()

alongside a normal one
Image by Betty Pace
A case series published in Blood indicates that some patients with mildly symptomatic sickle cell disease (SCD) can live long lives if they
comply with treatment recommendations and lead a healthy lifestyle.
The paper includes details on 4 women with milder forms of SCD who survived beyond age 80.
“For those with mild forms of SCD, these women show that lifestyle modifications may improve disease outcomes,” said author Samir K. Ballas, MD, of Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia, Pennsylvania.
Three of the women described in this case series were treated at the Sickle Cell Center of Thomas Jefferson University, and 1 was treated in Brazil’s Instituto de Hematologia Arthur de Siqueira Cavalcanti in Rio de Janeiro.
The women had different ancestries—2 African-American, 1 Italian-American, and 1 African-Brazilian—and different diagnoses—2 with hemoglobin SC disease and 2 with sickle cell anemia. But all 4 women had what Dr Ballas called “desirable” disease states.
“These women never had a stroke, never had recurrent acute chest syndrome, had a relatively high fetal hemoglobin count, and had infrequent painful crises,” Dr Ballas said. “Patients like this usually—but not always—experience relatively mild SCD, and they live longer with better quality of life.”
In addition, all of the women took steps to maintain and improve their health and had long-term family support. Dr Ballas said these factors likely contributed to the women’s long lives and high quality of life.
“All of the women were non-smokers who consumed little to no alcohol and maintained a normal body mass index,” he said. “This was coupled with a strong compliance to their treatment regimens and excellent family support at home.”
Family support was defined as having a spouse or child who provided attentive, ongoing care. And all of the women had at least 1 such caregiver.
Treatment compliance was based on observations by healthcare providers, including study authors. According to these observations, all of the women showed “excellent” adherence when it came to medication intake, appointments, and referrals.
As the women had relatively mild disease states, none of them were qualified to receive treatment with hydroxyurea. Instead, they received hydration, vaccination (including annual flu shots), and blood transfusion and analgesics as needed.
Even with their mild disease states and healthy lifestyles, these women did not live crisis-free lives. Each experienced disease-related complications necessitating medical attention.
The women had 0 to 3 vaso-occlusive crises per year. Two women required frequent transfusions (and had iron overload), and 2 required occasional transfusions. One woman had 2 episodes of acute chest syndrome, and the second episode led to her death.
Ultimately, 3 of the women died. One died of acute chest syndrome and septicemia at age 82, and another died of cardiac complications at age 86. For a third woman, the cause of death, at age 82, was unknown. The fourth woman remains alive at age 82.
As the median life expectancy of women with SCD in the US is 47, Dr Ballas and his colleagues said these 4 women may “provide a blueprint of how to live a long life despite having a serious medical condition like SCD.”
“I would often come out to the waiting room and find these ladies talking with other SCD patients, and I could tell that they gave others hope, that just because they have SCD does not mean that they are doomed to die by their 40s . . . ,” Dr Ballas said. “[I]f they take care of themselves and live closely with those who can help keep them well, that there is hope for them to lead long, full lives.” ![]()

alongside a normal one
Image by Betty Pace
A case series published in Blood indicates that some patients with mildly symptomatic sickle cell disease (SCD) can live long lives if they
comply with treatment recommendations and lead a healthy lifestyle.
The paper includes details on 4 women with milder forms of SCD who survived beyond age 80.
“For those with mild forms of SCD, these women show that lifestyle modifications may improve disease outcomes,” said author Samir K. Ballas, MD, of Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia, Pennsylvania.
Three of the women described in this case series were treated at the Sickle Cell Center of Thomas Jefferson University, and 1 was treated in Brazil’s Instituto de Hematologia Arthur de Siqueira Cavalcanti in Rio de Janeiro.
The women had different ancestries—2 African-American, 1 Italian-American, and 1 African-Brazilian—and different diagnoses—2 with hemoglobin SC disease and 2 with sickle cell anemia. But all 4 women had what Dr Ballas called “desirable” disease states.
“These women never had a stroke, never had recurrent acute chest syndrome, had a relatively high fetal hemoglobin count, and had infrequent painful crises,” Dr Ballas said. “Patients like this usually—but not always—experience relatively mild SCD, and they live longer with better quality of life.”
In addition, all of the women took steps to maintain and improve their health and had long-term family support. Dr Ballas said these factors likely contributed to the women’s long lives and high quality of life.
“All of the women were non-smokers who consumed little to no alcohol and maintained a normal body mass index,” he said. “This was coupled with a strong compliance to their treatment regimens and excellent family support at home.”
Family support was defined as having a spouse or child who provided attentive, ongoing care. And all of the women had at least 1 such caregiver.
Treatment compliance was based on observations by healthcare providers, including study authors. According to these observations, all of the women showed “excellent” adherence when it came to medication intake, appointments, and referrals.
As the women had relatively mild disease states, none of them were qualified to receive treatment with hydroxyurea. Instead, they received hydration, vaccination (including annual flu shots), and blood transfusion and analgesics as needed.
Even with their mild disease states and healthy lifestyles, these women did not live crisis-free lives. Each experienced disease-related complications necessitating medical attention.
The women had 0 to 3 vaso-occlusive crises per year. Two women required frequent transfusions (and had iron overload), and 2 required occasional transfusions. One woman had 2 episodes of acute chest syndrome, and the second episode led to her death.
Ultimately, 3 of the women died. One died of acute chest syndrome and septicemia at age 82, and another died of cardiac complications at age 86. For a third woman, the cause of death, at age 82, was unknown. The fourth woman remains alive at age 82.
As the median life expectancy of women with SCD in the US is 47, Dr Ballas and his colleagues said these 4 women may “provide a blueprint of how to live a long life despite having a serious medical condition like SCD.”
“I would often come out to the waiting room and find these ladies talking with other SCD patients, and I could tell that they gave others hope, that just because they have SCD does not mean that they are doomed to die by their 40s . . . ,” Dr Ballas said. “[I]f they take care of themselves and live closely with those who can help keep them well, that there is hope for them to lead long, full lives.” ![]()
Factor IX therapy approved in Australia

The Australian Therapeutic Goods Administration has approved albutrepenonacog alfa (Idelvion) to treat hemophilia B patients of all ages.
Albutrepenonacog alfa is a fusion protein linking recombinant coagulation factor IX with recombinant albumin.
The product is now approved in Australia for use as routine prophylaxis to prevent and reduce the frequency of bleeding, for on-demand control of bleeding, and for perioperative management of
bleeding.
Albutrepenonacog alfa has also been approved in Canada, the European Union, Japan, Switzerland, and the US.
Albutrepenonacog alfa is being developed by CSL Behring.
The company says albutrepenonacog alfa is the first and only Australian-registered factor IX therapy that delivers high-level protection from bleeding with up to 14-day dosing for appropriate patients.
According to CSL Behring, albutrepenonacog alfa can deliver high-level protection by maintaining factor IX activity levels at an average of 20% in patients treated prophylactically every 7 days and an average of 12% in patients treated prophylactically every 14 days.
“The Australian Haemophilia Centre Directors’ Organisation (AHCDO) views the development of effective long-acting clotting factor concentrates as a major step forward in the management of our patients with hemophilia,” said Simon McRae, MMBS, consultant hematologist and chairman of AHCDO.
“The ability to maintain clotting factor levels above a level that prevent the vast majority of bleeding events with less frequent infusions has the potential to improve long-term outcomes in individuals with hemophilia.”
Phase 3 trial
The Therapeutic Goods Administration approved albutrepenonacog alfa based on results of the PROLONG-9FP clinical development program. PROLONG-9FP includes phase 1, 2, and 3 studies evaluating the safety and efficacy of albutrepenonacog alfa in adults and children (ages 1 to 61) with hemophilia B.
Data from the phase 3 study were published in Blood. The study included 63 previously treated male patients with severe hemophilia B. They had a mean age of 33 (range, 12 to 61).
The patients were divided into 2 groups. Group 1 (n=40) received routine prophylaxis with albutrepenonacog alfa once every 7 days for 26 weeks, followed by a 7-, 10-, or 14-day prophylaxis regimen for a mean of 50, 38, or 51 weeks, respectively.
Group 2 received on-demand treatment with albutrepenonacog alfa for bleeding episodes for 26 weeks (n=23) and then switched to a 7-day prophylaxis regimen for a mean of 45 weeks (n=19).
The median annualized bleeding rate (ABR) was 2.0 in the prophylaxis arm (group 1) and 23.5 in the on-demand treatment arm (group 2). The median spontaneous ABRs were 0.0 and 17.0, respectively.
For patients in group 2, there was a significant reduction in median ABRs when patients switched from on-demand treatment to prophylaxis—19.22 and 1.58, respectively (P<0.0001). And there was a significant reduction in median spontaneous ABRs—15.43 and 0.00, respectively (P<0.0001).
Overall, 98.6% of bleeding episodes were treated successfully, including 93.6% that were treated with a single injection of albutrepenonacog alfa.
None of the patients developed inhibitors or experienced thromboembolic events, anaphylaxis, or life-threatening adverse events (AEs).
There were 347 treatment-emergent AEs reported in 54 (85.7%) patients. The most common were nasopharyngitis (25.4%), headache (23.8%), arthralgia (4.3%), and influenza (11.1%).
Eleven mild/moderate AEs in 5 patients (7.9%) were considered possibly related to albutrepenonacog alfa. Two patients discontinued treatment due to AEs—1 with hypersensitivity and 1 with headache.
“I have seen first-hand the benefits Idelvion has had on children with hemophilia B,” said PROLONG-9FP investigator Julie Curtin, MBBS, PhD, of The Children’s Hospital at Westmead in New South Wales.
“Idelvion has enabled children on regular treatment with factor IX to reduce the frequency of infusions without increasing their risk of bleeding. For a child to only need an injection every 1-2 weeks is a good step forward in the management of hemophilia B, which I welcome, and I am sure my patients will welcome this improvement too.” ![]()

The Australian Therapeutic Goods Administration has approved albutrepenonacog alfa (Idelvion) to treat hemophilia B patients of all ages.
Albutrepenonacog alfa is a fusion protein linking recombinant coagulation factor IX with recombinant albumin.
The product is now approved in Australia for use as routine prophylaxis to prevent and reduce the frequency of bleeding, for on-demand control of bleeding, and for perioperative management of
bleeding.
Albutrepenonacog alfa has also been approved in Canada, the European Union, Japan, Switzerland, and the US.
Albutrepenonacog alfa is being developed by CSL Behring.
The company says albutrepenonacog alfa is the first and only Australian-registered factor IX therapy that delivers high-level protection from bleeding with up to 14-day dosing for appropriate patients.
According to CSL Behring, albutrepenonacog alfa can deliver high-level protection by maintaining factor IX activity levels at an average of 20% in patients treated prophylactically every 7 days and an average of 12% in patients treated prophylactically every 14 days.
“The Australian Haemophilia Centre Directors’ Organisation (AHCDO) views the development of effective long-acting clotting factor concentrates as a major step forward in the management of our patients with hemophilia,” said Simon McRae, MMBS, consultant hematologist and chairman of AHCDO.
“The ability to maintain clotting factor levels above a level that prevent the vast majority of bleeding events with less frequent infusions has the potential to improve long-term outcomes in individuals with hemophilia.”
Phase 3 trial
The Therapeutic Goods Administration approved albutrepenonacog alfa based on results of the PROLONG-9FP clinical development program. PROLONG-9FP includes phase 1, 2, and 3 studies evaluating the safety and efficacy of albutrepenonacog alfa in adults and children (ages 1 to 61) with hemophilia B.
Data from the phase 3 study were published in Blood. The study included 63 previously treated male patients with severe hemophilia B. They had a mean age of 33 (range, 12 to 61).
The patients were divided into 2 groups. Group 1 (n=40) received routine prophylaxis with albutrepenonacog alfa once every 7 days for 26 weeks, followed by a 7-, 10-, or 14-day prophylaxis regimen for a mean of 50, 38, or 51 weeks, respectively.
Group 2 received on-demand treatment with albutrepenonacog alfa for bleeding episodes for 26 weeks (n=23) and then switched to a 7-day prophylaxis regimen for a mean of 45 weeks (n=19).
The median annualized bleeding rate (ABR) was 2.0 in the prophylaxis arm (group 1) and 23.5 in the on-demand treatment arm (group 2). The median spontaneous ABRs were 0.0 and 17.0, respectively.
For patients in group 2, there was a significant reduction in median ABRs when patients switched from on-demand treatment to prophylaxis—19.22 and 1.58, respectively (P<0.0001). And there was a significant reduction in median spontaneous ABRs—15.43 and 0.00, respectively (P<0.0001).
Overall, 98.6% of bleeding episodes were treated successfully, including 93.6% that were treated with a single injection of albutrepenonacog alfa.
None of the patients developed inhibitors or experienced thromboembolic events, anaphylaxis, or life-threatening adverse events (AEs).
There were 347 treatment-emergent AEs reported in 54 (85.7%) patients. The most common were nasopharyngitis (25.4%), headache (23.8%), arthralgia (4.3%), and influenza (11.1%).
Eleven mild/moderate AEs in 5 patients (7.9%) were considered possibly related to albutrepenonacog alfa. Two patients discontinued treatment due to AEs—1 with hypersensitivity and 1 with headache.
“I have seen first-hand the benefits Idelvion has had on children with hemophilia B,” said PROLONG-9FP investigator Julie Curtin, MBBS, PhD, of The Children’s Hospital at Westmead in New South Wales.
“Idelvion has enabled children on regular treatment with factor IX to reduce the frequency of infusions without increasing their risk of bleeding. For a child to only need an injection every 1-2 weeks is a good step forward in the management of hemophilia B, which I welcome, and I am sure my patients will welcome this improvement too.” ![]()

The Australian Therapeutic Goods Administration has approved albutrepenonacog alfa (Idelvion) to treat hemophilia B patients of all ages.
Albutrepenonacog alfa is a fusion protein linking recombinant coagulation factor IX with recombinant albumin.
The product is now approved in Australia for use as routine prophylaxis to prevent and reduce the frequency of bleeding, for on-demand control of bleeding, and for perioperative management of
bleeding.
Albutrepenonacog alfa has also been approved in Canada, the European Union, Japan, Switzerland, and the US.
Albutrepenonacog alfa is being developed by CSL Behring.
The company says albutrepenonacog alfa is the first and only Australian-registered factor IX therapy that delivers high-level protection from bleeding with up to 14-day dosing for appropriate patients.
According to CSL Behring, albutrepenonacog alfa can deliver high-level protection by maintaining factor IX activity levels at an average of 20% in patients treated prophylactically every 7 days and an average of 12% in patients treated prophylactically every 14 days.
“The Australian Haemophilia Centre Directors’ Organisation (AHCDO) views the development of effective long-acting clotting factor concentrates as a major step forward in the management of our patients with hemophilia,” said Simon McRae, MMBS, consultant hematologist and chairman of AHCDO.
“The ability to maintain clotting factor levels above a level that prevent the vast majority of bleeding events with less frequent infusions has the potential to improve long-term outcomes in individuals with hemophilia.”
Phase 3 trial
The Therapeutic Goods Administration approved albutrepenonacog alfa based on results of the PROLONG-9FP clinical development program. PROLONG-9FP includes phase 1, 2, and 3 studies evaluating the safety and efficacy of albutrepenonacog alfa in adults and children (ages 1 to 61) with hemophilia B.
Data from the phase 3 study were published in Blood. The study included 63 previously treated male patients with severe hemophilia B. They had a mean age of 33 (range, 12 to 61).
The patients were divided into 2 groups. Group 1 (n=40) received routine prophylaxis with albutrepenonacog alfa once every 7 days for 26 weeks, followed by a 7-, 10-, or 14-day prophylaxis regimen for a mean of 50, 38, or 51 weeks, respectively.
Group 2 received on-demand treatment with albutrepenonacog alfa for bleeding episodes for 26 weeks (n=23) and then switched to a 7-day prophylaxis regimen for a mean of 45 weeks (n=19).
The median annualized bleeding rate (ABR) was 2.0 in the prophylaxis arm (group 1) and 23.5 in the on-demand treatment arm (group 2). The median spontaneous ABRs were 0.0 and 17.0, respectively.
For patients in group 2, there was a significant reduction in median ABRs when patients switched from on-demand treatment to prophylaxis—19.22 and 1.58, respectively (P<0.0001). And there was a significant reduction in median spontaneous ABRs—15.43 and 0.00, respectively (P<0.0001).
Overall, 98.6% of bleeding episodes were treated successfully, including 93.6% that were treated with a single injection of albutrepenonacog alfa.
None of the patients developed inhibitors or experienced thromboembolic events, anaphylaxis, or life-threatening adverse events (AEs).
There were 347 treatment-emergent AEs reported in 54 (85.7%) patients. The most common were nasopharyngitis (25.4%), headache (23.8%), arthralgia (4.3%), and influenza (11.1%).
Eleven mild/moderate AEs in 5 patients (7.9%) were considered possibly related to albutrepenonacog alfa. Two patients discontinued treatment due to AEs—1 with hypersensitivity and 1 with headache.
“I have seen first-hand the benefits Idelvion has had on children with hemophilia B,” said PROLONG-9FP investigator Julie Curtin, MBBS, PhD, of The Children’s Hospital at Westmead in New South Wales.
“Idelvion has enabled children on regular treatment with factor IX to reduce the frequency of infusions without increasing their risk of bleeding. For a child to only need an injection every 1-2 weeks is a good step forward in the management of hemophilia B, which I welcome, and I am sure my patients will welcome this improvement too.” ![]()
Inflammation may predict transformation to AML

Inflammatory signaling in mesenchymal niche cells can be used to predict the transformation from pre-leukemic syndrome to acute myeloid leukemia (AML), according to preclinical research published in Cell Stem Cell.
“This discovery sheds new light on the long-standing association between inflammation and cancer,” said study author Marc Raaijmakers, MD, PhD, of the Erasmus MC Cancer Institute in Rotterdam, Netherlands.
“The elucidation of the molecular mechanism underlying this concept opens the prospect of improved diagnosis of patients at increased risk for the development of leukemia and the potential of future, niche-targeted therapy to delay or prevent the development of leukemia.”
In a previous study, Dr Raaijmakers and his colleagues discovered that mutations in mesenchymal progenitor cells can induce myelodysplasia in mice and promote the development of AML.
With the current study, the researchers wanted to build upon those findings by identifying the underlying mechanisms and determining their relevance to human disease.
So the team performed massive parallel RNA sequencing of mesenchymal cells in mice with Shwachman-Diamond syndrome and bone marrow samples from patients with Shwachman-Diamond syndrome, Diamond-Blackfan anemia, and myelodysplastic syndromes (MDS).
The researchers found that mesenchymal cells in these pre-leukemic disorders are under stress. The stress leads to the release of inflammatory molecules called S100A8 and S100A9, which cause mitochondrial and DNA damage in hematopoietic stem and progenitor cells.
The team also found that activation of this inflammatory pathway in mesenchymal cells predicted the development of AML and clinical outcomes in patients with MDS.
Leukemic evolution occurred in 29.4% (5/17) of MDS patients whose mesenchymal cells overexpressed S100A8/9 and 14.2% (4/28) of MDS patients without S100A8/9 overexpression.
The time to leukemic evolution and the length of progression-free survival were both significantly shorter in niche S100A8/9+ patients than niche S100A8/9- patients.
The average time to leukemic evolution was 3.4 months and 18.5 months, respectively (P=0.03). And the median progression-free survival was 11.5 months and 53 months, respectively (P=0.03)
The researchers believe these findings, if confirmed in subsequent studies, could lead to the development of tests to identify patients with pre-leukemic syndromes who have a high risk of developing AML.
“These high-risk patients could be treated more aggressively at an earlier stage, thereby preventing or slowing down disease progression,” Dr Raaijmakers said. “Moreover, the findings suggest that new drugs targeting the inflammatory pathway should be tested in future preclinical studies.” ![]()

Inflammatory signaling in mesenchymal niche cells can be used to predict the transformation from pre-leukemic syndrome to acute myeloid leukemia (AML), according to preclinical research published in Cell Stem Cell.
“This discovery sheds new light on the long-standing association between inflammation and cancer,” said study author Marc Raaijmakers, MD, PhD, of the Erasmus MC Cancer Institute in Rotterdam, Netherlands.
“The elucidation of the molecular mechanism underlying this concept opens the prospect of improved diagnosis of patients at increased risk for the development of leukemia and the potential of future, niche-targeted therapy to delay or prevent the development of leukemia.”
In a previous study, Dr Raaijmakers and his colleagues discovered that mutations in mesenchymal progenitor cells can induce myelodysplasia in mice and promote the development of AML.
With the current study, the researchers wanted to build upon those findings by identifying the underlying mechanisms and determining their relevance to human disease.
So the team performed massive parallel RNA sequencing of mesenchymal cells in mice with Shwachman-Diamond syndrome and bone marrow samples from patients with Shwachman-Diamond syndrome, Diamond-Blackfan anemia, and myelodysplastic syndromes (MDS).
The researchers found that mesenchymal cells in these pre-leukemic disorders are under stress. The stress leads to the release of inflammatory molecules called S100A8 and S100A9, which cause mitochondrial and DNA damage in hematopoietic stem and progenitor cells.
The team also found that activation of this inflammatory pathway in mesenchymal cells predicted the development of AML and clinical outcomes in patients with MDS.
Leukemic evolution occurred in 29.4% (5/17) of MDS patients whose mesenchymal cells overexpressed S100A8/9 and 14.2% (4/28) of MDS patients without S100A8/9 overexpression.
The time to leukemic evolution and the length of progression-free survival were both significantly shorter in niche S100A8/9+ patients than niche S100A8/9- patients.
The average time to leukemic evolution was 3.4 months and 18.5 months, respectively (P=0.03). And the median progression-free survival was 11.5 months and 53 months, respectively (P=0.03)
The researchers believe these findings, if confirmed in subsequent studies, could lead to the development of tests to identify patients with pre-leukemic syndromes who have a high risk of developing AML.
“These high-risk patients could be treated more aggressively at an earlier stage, thereby preventing or slowing down disease progression,” Dr Raaijmakers said. “Moreover, the findings suggest that new drugs targeting the inflammatory pathway should be tested in future preclinical studies.” ![]()

Inflammatory signaling in mesenchymal niche cells can be used to predict the transformation from pre-leukemic syndrome to acute myeloid leukemia (AML), according to preclinical research published in Cell Stem Cell.
“This discovery sheds new light on the long-standing association between inflammation and cancer,” said study author Marc Raaijmakers, MD, PhD, of the Erasmus MC Cancer Institute in Rotterdam, Netherlands.
“The elucidation of the molecular mechanism underlying this concept opens the prospect of improved diagnosis of patients at increased risk for the development of leukemia and the potential of future, niche-targeted therapy to delay or prevent the development of leukemia.”
In a previous study, Dr Raaijmakers and his colleagues discovered that mutations in mesenchymal progenitor cells can induce myelodysplasia in mice and promote the development of AML.
With the current study, the researchers wanted to build upon those findings by identifying the underlying mechanisms and determining their relevance to human disease.
So the team performed massive parallel RNA sequencing of mesenchymal cells in mice with Shwachman-Diamond syndrome and bone marrow samples from patients with Shwachman-Diamond syndrome, Diamond-Blackfan anemia, and myelodysplastic syndromes (MDS).
The researchers found that mesenchymal cells in these pre-leukemic disorders are under stress. The stress leads to the release of inflammatory molecules called S100A8 and S100A9, which cause mitochondrial and DNA damage in hematopoietic stem and progenitor cells.
The team also found that activation of this inflammatory pathway in mesenchymal cells predicted the development of AML and clinical outcomes in patients with MDS.
Leukemic evolution occurred in 29.4% (5/17) of MDS patients whose mesenchymal cells overexpressed S100A8/9 and 14.2% (4/28) of MDS patients without S100A8/9 overexpression.
The time to leukemic evolution and the length of progression-free survival were both significantly shorter in niche S100A8/9+ patients than niche S100A8/9- patients.
The average time to leukemic evolution was 3.4 months and 18.5 months, respectively (P=0.03). And the median progression-free survival was 11.5 months and 53 months, respectively (P=0.03)
The researchers believe these findings, if confirmed in subsequent studies, could lead to the development of tests to identify patients with pre-leukemic syndromes who have a high risk of developing AML.
“These high-risk patients could be treated more aggressively at an earlier stage, thereby preventing or slowing down disease progression,” Dr Raaijmakers said. “Moreover, the findings suggest that new drugs targeting the inflammatory pathway should be tested in future preclinical studies.” ![]()
His Head Is In the Game–His Heart, Not So Much
ANSWER
The correct interpretation includes normal sinus rhythm with a new anterior myocardial infarction (MI) and inferolateral injury.
Criteria for an anterior MI include Q waves in leads V2 to V6 and hyperacute ST-T wave changes. V1 is usually spared.
Inferolateral injury is evidenced by the presence of Q waves and absence of R waves in leads III and aVF.
The patient’s cardiac catheterization revealed left anterior descending and circumflex artery disease.
ANSWER
The correct interpretation includes normal sinus rhythm with a new anterior myocardial infarction (MI) and inferolateral injury.
Criteria for an anterior MI include Q waves in leads V2 to V6 and hyperacute ST-T wave changes. V1 is usually spared.
Inferolateral injury is evidenced by the presence of Q waves and absence of R waves in leads III and aVF.
The patient’s cardiac catheterization revealed left anterior descending and circumflex artery disease.
ANSWER
The correct interpretation includes normal sinus rhythm with a new anterior myocardial infarction (MI) and inferolateral injury.
Criteria for an anterior MI include Q waves in leads V2 to V6 and hyperacute ST-T wave changes. V1 is usually spared.
Inferolateral injury is evidenced by the presence of Q waves and absence of R waves in leads III and aVF.
The patient’s cardiac catheterization revealed left anterior descending and circumflex artery disease.
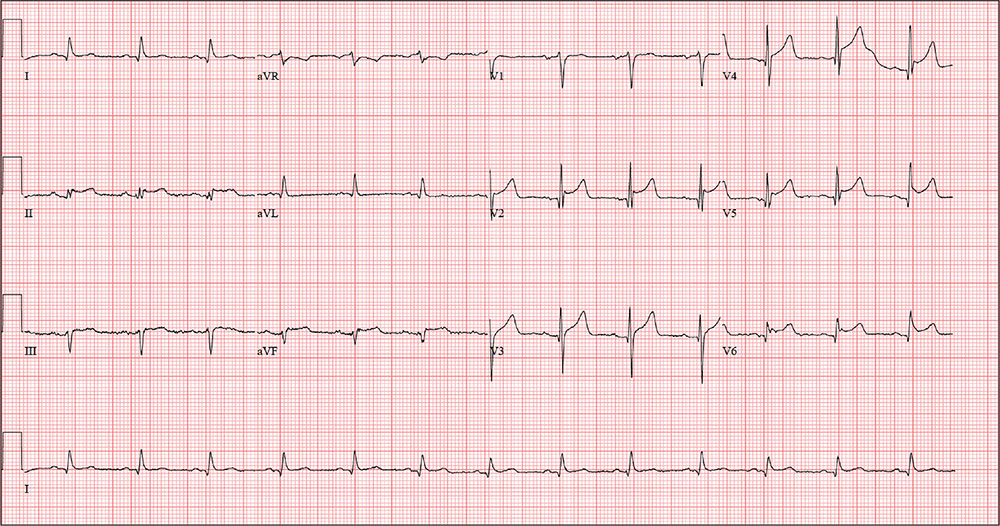
While playing in a company racquetball tournament, a 47-year-old man suddenly collapses. He is unresponsive, without a pulse, and his coworkers immediately initiate CPR. A single shock from an on-site AED successfully resuscitates him from ventricular fibrillation. Paramedics arrive within 12 minutes, by which time the patient is conscious and responsive to commands.
During transportation to the emergency department, however, he develops ventricular tachycardia and loses consciousness; a single shock cardioverts him to normal sinus rhythm. An ECG is ordered and the cardiac catheterization team mobilized.
While waiting, you contact the patient’s wife by telephone. She tells you that her husband has been complaining of chest discomfort for the past week and woke up two nights ago with what he described as “indigestion.” She says she suggested he see a clinician, and he agreed to do so—but not until after the tournament.
His medical history is remarkable only for chronic gastroesophageal reflux disease (GERD), for which he takes chewable antacids on a daily basis. He has no prior cardiac or pulmonary history. There is no surgical history apart from a tonsillectomy in childhood.
The patient is the Chief Operating Officer at a local manufacturing facility. He is married and has three children. His parents and grandparents are alive and in good health, aside from some arthritis in the older generation.
The review of systems, obtained from his wife, is noncontributory. She says he is in excellent health—he jogs, rides mountain bikes, and enjoys racquetball. Her husband attributed his recent chest discomfort to GERD; when she asked if it could be cardiac related, he adamantly denied the possibility, as he was in “excellent health” with “good genes.”
Vital signs include a blood pressure of 118/56 mm Hg; pulse, 80 beats/min; respiratory rate, 18 breaths/min-1; and O2 saturation, 100% on 2 L oxygen. He is afebrile.
Physical exam reveals a thin, otherwise healthy male who appears anxious and apprehensive. He denies ongoing chest pain but states that his chest wall is sore beneath the defibrillator pads. A focal exam reveals normal lung sounds and a regular rate and rhythm with no murmurs, gallops, or rubs. The abdomen is soft and nontender. All peripheral pulses are strong and equal bilaterally, and there are no focal neurologic signs.
The ECG taken at admission shows a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc interval, 370/426 ms; P axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation of the ECG?
Registry, multisite care, bundled vaccines improve HPV vaccination rate among teens
Bundling vaccines, coordinating multisite medical access, and overseeing vaccination status through an internally developed immunization registry has consistently led to Denver Health’s reporting higher-than-average HPV vaccination rates among adolescents, according to investigators.
Despite the Advisory Committee on Immunization Practice’s 2006 recommendation for routine adolescent human papillomavirus (HPV) vaccination and the Healthy People goal of 80% vaccine coverage in adolescents by 2020, HPV vaccination rates have lagged behind those of other routinely administered adolescent vaccinations, such as meningococcal conjugate vaccine (MCV4) and Tdap, reported Anna-Lisa Farmar, MD, of Denver Health, and her associates (Pediatrics. 2016 Oct 5. doi: 10.1542/peds.2015-2653).
For their study, Dr. Farmar and her associates outlined the vaccination procedures and tactics used at Denver Health’s 8 health centers and 16 school-based health centers and examined vaccine registry data for 11,463 patients to understand why the health system has been successful and to learn how it can further improve.
The multipronged vaccination procedures and tactics employed at Denver Health are designed to overcome specific HPV vaccination barriers such as concern about the vaccine’s safety, parental belief that their children are not sexually active, lack of insurance coverage, lack of knowledge about HPV, and providers missing opportunities to administer the vaccine, as well as barriers affecting low-income patients: transportation issues, low access to care, and inability to take time off work.
“For all patients presenting for acute or preventative visits, there is a standard process for the medical assistants to follow that leads to vaccines being offered to the patient,” the authors wrote. This process begins with and is organized by VaxTrax, a Denver Health internally developed immunization registry that informs medical providers of a patient’s vaccination status.
Denver Health medical providers are encouraged to bundle common vaccines together, to not present vaccines as optional or required, and to review their individual vaccine coverage rates, which are distributed monthly. In addition, school-based health centers offer vaccination drives and adolescents can receive medical care at any of the Denver Health sites, thereby increasing the opportunities for providers and patients to interact.
“Avoiding missed opportunities for vaccination and providing a strong recommendation for the HPV vaccine were key procedures that likely contributed to high coverage rates,” Dr. Farmar and her associates wrote.
The researchers found that of the 11,463 patients included in analysis, the majority completing the HPV vaccination series were female, Hispanic, and low-income. “These results are consistent with previous research examining national and state trends,” they noted.
“To our knowledge, language has not been examined as a potential factor in HPV coverage rates. The practice of continuing to approach families who have refused HPV vaccination in the past addresses the patient groups with lower vaccine completion rates, such as English-speaking and higher-income families. These families may require recurring discussion over time with a primary provider to overcome barriers to vaccination,” the researchers wrote.
This study received no external funding, and the researchers had no relevant disclosures to report.
[email protected]
On Twitter @jessnicolecraig
Bundling vaccines, coordinating multisite medical access, and overseeing vaccination status through an internally developed immunization registry has consistently led to Denver Health’s reporting higher-than-average HPV vaccination rates among adolescents, according to investigators.
Despite the Advisory Committee on Immunization Practice’s 2006 recommendation for routine adolescent human papillomavirus (HPV) vaccination and the Healthy People goal of 80% vaccine coverage in adolescents by 2020, HPV vaccination rates have lagged behind those of other routinely administered adolescent vaccinations, such as meningococcal conjugate vaccine (MCV4) and Tdap, reported Anna-Lisa Farmar, MD, of Denver Health, and her associates (Pediatrics. 2016 Oct 5. doi: 10.1542/peds.2015-2653).
For their study, Dr. Farmar and her associates outlined the vaccination procedures and tactics used at Denver Health’s 8 health centers and 16 school-based health centers and examined vaccine registry data for 11,463 patients to understand why the health system has been successful and to learn how it can further improve.
The multipronged vaccination procedures and tactics employed at Denver Health are designed to overcome specific HPV vaccination barriers such as concern about the vaccine’s safety, parental belief that their children are not sexually active, lack of insurance coverage, lack of knowledge about HPV, and providers missing opportunities to administer the vaccine, as well as barriers affecting low-income patients: transportation issues, low access to care, and inability to take time off work.
“For all patients presenting for acute or preventative visits, there is a standard process for the medical assistants to follow that leads to vaccines being offered to the patient,” the authors wrote. This process begins with and is organized by VaxTrax, a Denver Health internally developed immunization registry that informs medical providers of a patient’s vaccination status.
Denver Health medical providers are encouraged to bundle common vaccines together, to not present vaccines as optional or required, and to review their individual vaccine coverage rates, which are distributed monthly. In addition, school-based health centers offer vaccination drives and adolescents can receive medical care at any of the Denver Health sites, thereby increasing the opportunities for providers and patients to interact.
“Avoiding missed opportunities for vaccination and providing a strong recommendation for the HPV vaccine were key procedures that likely contributed to high coverage rates,” Dr. Farmar and her associates wrote.
The researchers found that of the 11,463 patients included in analysis, the majority completing the HPV vaccination series were female, Hispanic, and low-income. “These results are consistent with previous research examining national and state trends,” they noted.
“To our knowledge, language has not been examined as a potential factor in HPV coverage rates. The practice of continuing to approach families who have refused HPV vaccination in the past addresses the patient groups with lower vaccine completion rates, such as English-speaking and higher-income families. These families may require recurring discussion over time with a primary provider to overcome barriers to vaccination,” the researchers wrote.
This study received no external funding, and the researchers had no relevant disclosures to report.
[email protected]
On Twitter @jessnicolecraig
Bundling vaccines, coordinating multisite medical access, and overseeing vaccination status through an internally developed immunization registry has consistently led to Denver Health’s reporting higher-than-average HPV vaccination rates among adolescents, according to investigators.
Despite the Advisory Committee on Immunization Practice’s 2006 recommendation for routine adolescent human papillomavirus (HPV) vaccination and the Healthy People goal of 80% vaccine coverage in adolescents by 2020, HPV vaccination rates have lagged behind those of other routinely administered adolescent vaccinations, such as meningococcal conjugate vaccine (MCV4) and Tdap, reported Anna-Lisa Farmar, MD, of Denver Health, and her associates (Pediatrics. 2016 Oct 5. doi: 10.1542/peds.2015-2653).
For their study, Dr. Farmar and her associates outlined the vaccination procedures and tactics used at Denver Health’s 8 health centers and 16 school-based health centers and examined vaccine registry data for 11,463 patients to understand why the health system has been successful and to learn how it can further improve.
The multipronged vaccination procedures and tactics employed at Denver Health are designed to overcome specific HPV vaccination barriers such as concern about the vaccine’s safety, parental belief that their children are not sexually active, lack of insurance coverage, lack of knowledge about HPV, and providers missing opportunities to administer the vaccine, as well as barriers affecting low-income patients: transportation issues, low access to care, and inability to take time off work.
“For all patients presenting for acute or preventative visits, there is a standard process for the medical assistants to follow that leads to vaccines being offered to the patient,” the authors wrote. This process begins with and is organized by VaxTrax, a Denver Health internally developed immunization registry that informs medical providers of a patient’s vaccination status.
Denver Health medical providers are encouraged to bundle common vaccines together, to not present vaccines as optional or required, and to review their individual vaccine coverage rates, which are distributed monthly. In addition, school-based health centers offer vaccination drives and adolescents can receive medical care at any of the Denver Health sites, thereby increasing the opportunities for providers and patients to interact.
“Avoiding missed opportunities for vaccination and providing a strong recommendation for the HPV vaccine were key procedures that likely contributed to high coverage rates,” Dr. Farmar and her associates wrote.
The researchers found that of the 11,463 patients included in analysis, the majority completing the HPV vaccination series were female, Hispanic, and low-income. “These results are consistent with previous research examining national and state trends,” they noted.
“To our knowledge, language has not been examined as a potential factor in HPV coverage rates. The practice of continuing to approach families who have refused HPV vaccination in the past addresses the patient groups with lower vaccine completion rates, such as English-speaking and higher-income families. These families may require recurring discussion over time with a primary provider to overcome barriers to vaccination,” the researchers wrote.
This study received no external funding, and the researchers had no relevant disclosures to report.
[email protected]
On Twitter @jessnicolecraig
FROM PEDIATRICS
Key clinical point:
Major finding: In 2014, the national average of adolescents receiving three or more doses of the HPV vaccine was 40% for girls and 22% for boys. At Denver Health, those rates were 67% and 60%, respectively.
Data source: A retrospective study of 11,463 adolescent patients.
Disclosures: This study received no external funding, and the researchers had no relevant disclosures to report.
Laparoscopic hysterectomy best in morbidly obese uterine cancer patients
BOSTON – Total laparoscopic hysterectomy had fewer complications and a shorter length of stay among morbidly obese women with uterine cancer, compared with an abdominal approach, according to findings presented at the annual Minimally Invasive Surgery Week.
“We wanted to look at current trends and see if we’re doing more the abdominal route or adopting more minimally invasive surgery, but also find out what obesity has to do with it,” Emad Mikhail, MD, of the University of South Florida in Tampa, said in an interview. “Morbidly obese patients are a really vulnerable group of patients; they have a lot of medical comorbidities, and when they need surgery they have an increased risk of having poor perioperative outcomes because of their BMI [body mass index].”
More than half of the cases were total laparoscopic hysterectomy (1,025), a third were total abdominal hysterectomy (672), about 12% were laparoscopic assisted vaginal hysterectomy (248), and less than 3% were total vaginal hysterectomy (57).
Comparing total abdominal and total laparoscopic hysterectomy – the two most commonly performed type of hysterectomy in the study – median operative times were notably higher in total laparoscopic hysterectomy: 171 minutes versus 150 minutes (P less than .05). But the laparoscopic approach had a shorter length of stay, a lower rate of hospital readmissions, and fewer surgical complications.
Within the total laparoscopic hysterectomy cohort, length of stay averaged 1 day. Dr. Mikhail reported that this cohort also had 14 blood transfusions, 13 superficial surgical site infections, 5 deep incisional surgical site infections, and 41 readmissions within 30 days, all of which were significantly lower than in the total abdominal hysterectomy cohort (P less than .05).
Mean BMI was similar in the two groups, with 34.0 in the total abdominal hysterectomy cohort and 33.7 in the total laparoscopic hysterectomy cohort.
“As the BMI goes up, more [minimally invasive surgery] is adopted, which is a great finding,” Dr. Mikhail said. “It actually serves the purpose of vulnerable patients. Instead of having an increase in perioperative morbidity, they should benefit more from a [minimally invasive surgery] approach, which this study is showing.”
Next, Dr. Mikhail said he wants to tease out what types of procedures subspecialists are performing among morbidly obese patients with uterine cancer. This type of data collection would be easier, he added, if minimally invasive gynecologic surgeons had their own taxonomy code.
“Without a code, we cannot pull data and see if being a fellowship-trained, minimally invasive surgeon has a benefit for patients,” he said. “Are those surgeons offering more minimally invasive techniques for morbidly obese patients?”
Dr. Mikhail reported having no relevant financial disclosures. The meeting was held by the Society of Laparoendoscopic Surgeons.
BOSTON – Total laparoscopic hysterectomy had fewer complications and a shorter length of stay among morbidly obese women with uterine cancer, compared with an abdominal approach, according to findings presented at the annual Minimally Invasive Surgery Week.
“We wanted to look at current trends and see if we’re doing more the abdominal route or adopting more minimally invasive surgery, but also find out what obesity has to do with it,” Emad Mikhail, MD, of the University of South Florida in Tampa, said in an interview. “Morbidly obese patients are a really vulnerable group of patients; they have a lot of medical comorbidities, and when they need surgery they have an increased risk of having poor perioperative outcomes because of their BMI [body mass index].”
More than half of the cases were total laparoscopic hysterectomy (1,025), a third were total abdominal hysterectomy (672), about 12% were laparoscopic assisted vaginal hysterectomy (248), and less than 3% were total vaginal hysterectomy (57).
Comparing total abdominal and total laparoscopic hysterectomy – the two most commonly performed type of hysterectomy in the study – median operative times were notably higher in total laparoscopic hysterectomy: 171 minutes versus 150 minutes (P less than .05). But the laparoscopic approach had a shorter length of stay, a lower rate of hospital readmissions, and fewer surgical complications.
Within the total laparoscopic hysterectomy cohort, length of stay averaged 1 day. Dr. Mikhail reported that this cohort also had 14 blood transfusions, 13 superficial surgical site infections, 5 deep incisional surgical site infections, and 41 readmissions within 30 days, all of which were significantly lower than in the total abdominal hysterectomy cohort (P less than .05).
Mean BMI was similar in the two groups, with 34.0 in the total abdominal hysterectomy cohort and 33.7 in the total laparoscopic hysterectomy cohort.
“As the BMI goes up, more [minimally invasive surgery] is adopted, which is a great finding,” Dr. Mikhail said. “It actually serves the purpose of vulnerable patients. Instead of having an increase in perioperative morbidity, they should benefit more from a [minimally invasive surgery] approach, which this study is showing.”
Next, Dr. Mikhail said he wants to tease out what types of procedures subspecialists are performing among morbidly obese patients with uterine cancer. This type of data collection would be easier, he added, if minimally invasive gynecologic surgeons had their own taxonomy code.
“Without a code, we cannot pull data and see if being a fellowship-trained, minimally invasive surgeon has a benefit for patients,” he said. “Are those surgeons offering more minimally invasive techniques for morbidly obese patients?”
Dr. Mikhail reported having no relevant financial disclosures. The meeting was held by the Society of Laparoendoscopic Surgeons.
BOSTON – Total laparoscopic hysterectomy had fewer complications and a shorter length of stay among morbidly obese women with uterine cancer, compared with an abdominal approach, according to findings presented at the annual Minimally Invasive Surgery Week.
“We wanted to look at current trends and see if we’re doing more the abdominal route or adopting more minimally invasive surgery, but also find out what obesity has to do with it,” Emad Mikhail, MD, of the University of South Florida in Tampa, said in an interview. “Morbidly obese patients are a really vulnerable group of patients; they have a lot of medical comorbidities, and when they need surgery they have an increased risk of having poor perioperative outcomes because of their BMI [body mass index].”
More than half of the cases were total laparoscopic hysterectomy (1,025), a third were total abdominal hysterectomy (672), about 12% were laparoscopic assisted vaginal hysterectomy (248), and less than 3% were total vaginal hysterectomy (57).
Comparing total abdominal and total laparoscopic hysterectomy – the two most commonly performed type of hysterectomy in the study – median operative times were notably higher in total laparoscopic hysterectomy: 171 minutes versus 150 minutes (P less than .05). But the laparoscopic approach had a shorter length of stay, a lower rate of hospital readmissions, and fewer surgical complications.
Within the total laparoscopic hysterectomy cohort, length of stay averaged 1 day. Dr. Mikhail reported that this cohort also had 14 blood transfusions, 13 superficial surgical site infections, 5 deep incisional surgical site infections, and 41 readmissions within 30 days, all of which were significantly lower than in the total abdominal hysterectomy cohort (P less than .05).
Mean BMI was similar in the two groups, with 34.0 in the total abdominal hysterectomy cohort and 33.7 in the total laparoscopic hysterectomy cohort.
“As the BMI goes up, more [minimally invasive surgery] is adopted, which is a great finding,” Dr. Mikhail said. “It actually serves the purpose of vulnerable patients. Instead of having an increase in perioperative morbidity, they should benefit more from a [minimally invasive surgery] approach, which this study is showing.”
Next, Dr. Mikhail said he wants to tease out what types of procedures subspecialists are performing among morbidly obese patients with uterine cancer. This type of data collection would be easier, he added, if minimally invasive gynecologic surgeons had their own taxonomy code.
“Without a code, we cannot pull data and see if being a fellowship-trained, minimally invasive surgeon has a benefit for patients,” he said. “Are those surgeons offering more minimally invasive techniques for morbidly obese patients?”
Dr. Mikhail reported having no relevant financial disclosures. The meeting was held by the Society of Laparoendoscopic Surgeons.
Key clinical point:
Major finding: Total laparoscopic hysterectomy had shorter length of stay, fewer transfusions, fewer surgical site infections, and fewer readmissions, compared with total abdominal hysterectomy (P less than .05).
Data source: Retrospective review of data on 2,002 morbidly obese patients with uterine cancer in the ACS-NSQIP database.
Disclosures: Dr. Mikhail reported having no relevant financial disclosures.