User login
Apply now for the 2016 Claude H. Organ, Jr., MD, FACS, Traveling Fellowship
The American College of Surgeons (ACS) is now accepting applications for the 2016 Claude H. Organ, Jr., MD, FACS, Traveling Fellowship. The deadline for all application materials is June 1.
The family and friends of the late Dr. Organ established an endowment through the ACS Foundation to provide funding for this fellowship, which is awarded annually to an outstanding young surgeon from the Society of Black Academic Surgeons, the Association of Women Surgeons, or the Surgical Section of the National Medical Association. The fellowship, in the amount of $5,000, enables a U.S. or Canadian Fellow or Associate Fellow younger than age 45 who is a member of one of these societies to attend an educational meeting or participate in an extended visit to an institution of his or her choice, tailored to his or her research interests.
Past awardees have used their fellowships to develop their careers in creative ways. The most recent fellow, Kathie-Ann Joseph, MD, MPH, FACS, associate professor of surgery, New York University School of Medicine, and chief of surgery, Bellevue Hospital Center, New York, NY, is researching how health care systems work in a major metropolitan area, with a focus on the ways that large hospitals systems manage care for underserved women.
The full requirements for the Claude H. Organ, Jr., MD, FACS, Traveling Fellowship are posted at facs.org/member-services/scholarships/special/organ. The 2016 awardee will be informed of the College’s decision by August 2016. Questions and application materials should be submitted to the attention of Kate Early, ACS Scholarships Administrator, at [email protected].
The American College of Surgeons (ACS) is now accepting applications for the 2016 Claude H. Organ, Jr., MD, FACS, Traveling Fellowship. The deadline for all application materials is June 1.
The family and friends of the late Dr. Organ established an endowment through the ACS Foundation to provide funding for this fellowship, which is awarded annually to an outstanding young surgeon from the Society of Black Academic Surgeons, the Association of Women Surgeons, or the Surgical Section of the National Medical Association. The fellowship, in the amount of $5,000, enables a U.S. or Canadian Fellow or Associate Fellow younger than age 45 who is a member of one of these societies to attend an educational meeting or participate in an extended visit to an institution of his or her choice, tailored to his or her research interests.
Past awardees have used their fellowships to develop their careers in creative ways. The most recent fellow, Kathie-Ann Joseph, MD, MPH, FACS, associate professor of surgery, New York University School of Medicine, and chief of surgery, Bellevue Hospital Center, New York, NY, is researching how health care systems work in a major metropolitan area, with a focus on the ways that large hospitals systems manage care for underserved women.
The full requirements for the Claude H. Organ, Jr., MD, FACS, Traveling Fellowship are posted at facs.org/member-services/scholarships/special/organ. The 2016 awardee will be informed of the College’s decision by August 2016. Questions and application materials should be submitted to the attention of Kate Early, ACS Scholarships Administrator, at [email protected].
The American College of Surgeons (ACS) is now accepting applications for the 2016 Claude H. Organ, Jr., MD, FACS, Traveling Fellowship. The deadline for all application materials is June 1.
The family and friends of the late Dr. Organ established an endowment through the ACS Foundation to provide funding for this fellowship, which is awarded annually to an outstanding young surgeon from the Society of Black Academic Surgeons, the Association of Women Surgeons, or the Surgical Section of the National Medical Association. The fellowship, in the amount of $5,000, enables a U.S. or Canadian Fellow or Associate Fellow younger than age 45 who is a member of one of these societies to attend an educational meeting or participate in an extended visit to an institution of his or her choice, tailored to his or her research interests.
Past awardees have used their fellowships to develop their careers in creative ways. The most recent fellow, Kathie-Ann Joseph, MD, MPH, FACS, associate professor of surgery, New York University School of Medicine, and chief of surgery, Bellevue Hospital Center, New York, NY, is researching how health care systems work in a major metropolitan area, with a focus on the ways that large hospitals systems manage care for underserved women.
The full requirements for the Claude H. Organ, Jr., MD, FACS, Traveling Fellowship are posted at facs.org/member-services/scholarships/special/organ. The 2016 awardee will be informed of the College’s decision by August 2016. Questions and application materials should be submitted to the attention of Kate Early, ACS Scholarships Administrator, at [email protected].
Your online reputation
Have you ever run across a negative or even malicious comment about you or your practice on the web, in full view of the world? You’re certainly not alone.
Chances are it was on one of those doctor rating sites, whose supposedly “objective” evaluations are anything but fair or accurate; one curmudgeon, angry about something that usually has nothing to do with your clinical skills, can use his First Amendment–protected right to trash you unfairly, as thousands of satisfied patients remain silent.
What to do? You could hire one of the many companies in the rapidly burgeoning field of online reputation management; but that can cost hundreds to thousands of dollars per month for monitoring and intervention, and there are no guarantees of success.
A better solution is to generate your own search results – positive ones – that will overwhelm any negative comments that search engines might find. Start with the social networking sites. However you feel about networking, there’s no getting around the fact that personal pages on Facebook, LinkedIn, and Twitter rank very high on major search engines. (Some consultants say a favorable LinkedIn profile is particularly helpful because of that site’s reputation as a “professional” network.) Your community activities, charitable work, interesting hobbies – anything that casts you in a favorable light – need to be mentioned prominently in your network profiles.
You can also use Google’s profiling tool (https://plus.google.com/up/accounts/) to create a sterling bio, complete with links to URLs, photos, and anything else that shows you in the best possible light. And your Google profile will be at or near the top of any Google search.
Wikipedia articles also go to the top of most searches, so if you’re notable enough to merit mention in one – or to have one of your own – see that it is done, and updated regularly. You can’t do that yourself, however; Wikipedia’s conflict of interest rules forbid writing or editing content about yourself. Someone with a theoretically “neutral point of view” will have to do it.
If you don’t yet have a website, now would be a good time. As I’ve discussed many times, a professionally designed site will be far more attractive and polished than anything you could build yourself. Furthermore, an experienced designer will employ “search engine optimization” (SEO), meaning that content will be created in a way that is readily visible to search engine users.
Leave design and SEO to the pros, but don’t delegate the content itself; as captain of the ship you are responsible for all the facts and opinions on your site. And remember that once it’s online, it’s online forever; consider the ramifications of anything you post on any site (yours or others) before hitting the “send” button. “The most damaging item about you,” one consultant told me, “could well be something you posted yourself.” Just ask any of several prominent politicians who have famously sabotaged their own careers online.
That said, don’t be shy about creating content. Make your (noncontroversial) opinions known on Facebook and Twitter. If social networks are not your thing, add a blog to your web site and write about what you know, and what interests you. If you have expertise in a particular field, write about that.
Incidentally, if the URL for your web site is not your name, you should also register your name as a separate domain name – if only to be sure that a trickster, or someone with the same name and a bad reputation, doesn’t get it.
Set up an RSS news feed for yourself, so you’ll know immediately anytime your name pops up in news or gossip sites, or on blogs. If something untrue is posted about you, take action. Reputable news sites and blogs have their own reputations to protect, and so can usually be persuaded to correct anything that is demonstrably false. Try to get the error removed entirely, or corrected within the original article. An erratum on the last page of the next edition will be ignored, and will leave the false information online, intact.
Unfair comments on doctor rating sites are unlikely to be removed unless they are blatantly libelous; but there is nothing wrong with encouraging happy patients to write favorable reviews. Turnabout is fair play.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Have you ever run across a negative or even malicious comment about you or your practice on the web, in full view of the world? You’re certainly not alone.
Chances are it was on one of those doctor rating sites, whose supposedly “objective” evaluations are anything but fair or accurate; one curmudgeon, angry about something that usually has nothing to do with your clinical skills, can use his First Amendment–protected right to trash you unfairly, as thousands of satisfied patients remain silent.
What to do? You could hire one of the many companies in the rapidly burgeoning field of online reputation management; but that can cost hundreds to thousands of dollars per month for monitoring and intervention, and there are no guarantees of success.
A better solution is to generate your own search results – positive ones – that will overwhelm any negative comments that search engines might find. Start with the social networking sites. However you feel about networking, there’s no getting around the fact that personal pages on Facebook, LinkedIn, and Twitter rank very high on major search engines. (Some consultants say a favorable LinkedIn profile is particularly helpful because of that site’s reputation as a “professional” network.) Your community activities, charitable work, interesting hobbies – anything that casts you in a favorable light – need to be mentioned prominently in your network profiles.
You can also use Google’s profiling tool (https://plus.google.com/up/accounts/) to create a sterling bio, complete with links to URLs, photos, and anything else that shows you in the best possible light. And your Google profile will be at or near the top of any Google search.
Wikipedia articles also go to the top of most searches, so if you’re notable enough to merit mention in one – or to have one of your own – see that it is done, and updated regularly. You can’t do that yourself, however; Wikipedia’s conflict of interest rules forbid writing or editing content about yourself. Someone with a theoretically “neutral point of view” will have to do it.
If you don’t yet have a website, now would be a good time. As I’ve discussed many times, a professionally designed site will be far more attractive and polished than anything you could build yourself. Furthermore, an experienced designer will employ “search engine optimization” (SEO), meaning that content will be created in a way that is readily visible to search engine users.
Leave design and SEO to the pros, but don’t delegate the content itself; as captain of the ship you are responsible for all the facts and opinions on your site. And remember that once it’s online, it’s online forever; consider the ramifications of anything you post on any site (yours or others) before hitting the “send” button. “The most damaging item about you,” one consultant told me, “could well be something you posted yourself.” Just ask any of several prominent politicians who have famously sabotaged their own careers online.
That said, don’t be shy about creating content. Make your (noncontroversial) opinions known on Facebook and Twitter. If social networks are not your thing, add a blog to your web site and write about what you know, and what interests you. If you have expertise in a particular field, write about that.
Incidentally, if the URL for your web site is not your name, you should also register your name as a separate domain name – if only to be sure that a trickster, or someone with the same name and a bad reputation, doesn’t get it.
Set up an RSS news feed for yourself, so you’ll know immediately anytime your name pops up in news or gossip sites, or on blogs. If something untrue is posted about you, take action. Reputable news sites and blogs have their own reputations to protect, and so can usually be persuaded to correct anything that is demonstrably false. Try to get the error removed entirely, or corrected within the original article. An erratum on the last page of the next edition will be ignored, and will leave the false information online, intact.
Unfair comments on doctor rating sites are unlikely to be removed unless they are blatantly libelous; but there is nothing wrong with encouraging happy patients to write favorable reviews. Turnabout is fair play.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Have you ever run across a negative or even malicious comment about you or your practice on the web, in full view of the world? You’re certainly not alone.
Chances are it was on one of those doctor rating sites, whose supposedly “objective” evaluations are anything but fair or accurate; one curmudgeon, angry about something that usually has nothing to do with your clinical skills, can use his First Amendment–protected right to trash you unfairly, as thousands of satisfied patients remain silent.
What to do? You could hire one of the many companies in the rapidly burgeoning field of online reputation management; but that can cost hundreds to thousands of dollars per month for monitoring and intervention, and there are no guarantees of success.
A better solution is to generate your own search results – positive ones – that will overwhelm any negative comments that search engines might find. Start with the social networking sites. However you feel about networking, there’s no getting around the fact that personal pages on Facebook, LinkedIn, and Twitter rank very high on major search engines. (Some consultants say a favorable LinkedIn profile is particularly helpful because of that site’s reputation as a “professional” network.) Your community activities, charitable work, interesting hobbies – anything that casts you in a favorable light – need to be mentioned prominently in your network profiles.
You can also use Google’s profiling tool (https://plus.google.com/up/accounts/) to create a sterling bio, complete with links to URLs, photos, and anything else that shows you in the best possible light. And your Google profile will be at or near the top of any Google search.
Wikipedia articles also go to the top of most searches, so if you’re notable enough to merit mention in one – or to have one of your own – see that it is done, and updated regularly. You can’t do that yourself, however; Wikipedia’s conflict of interest rules forbid writing or editing content about yourself. Someone with a theoretically “neutral point of view” will have to do it.
If you don’t yet have a website, now would be a good time. As I’ve discussed many times, a professionally designed site will be far more attractive and polished than anything you could build yourself. Furthermore, an experienced designer will employ “search engine optimization” (SEO), meaning that content will be created in a way that is readily visible to search engine users.
Leave design and SEO to the pros, but don’t delegate the content itself; as captain of the ship you are responsible for all the facts and opinions on your site. And remember that once it’s online, it’s online forever; consider the ramifications of anything you post on any site (yours or others) before hitting the “send” button. “The most damaging item about you,” one consultant told me, “could well be something you posted yourself.” Just ask any of several prominent politicians who have famously sabotaged their own careers online.
That said, don’t be shy about creating content. Make your (noncontroversial) opinions known on Facebook and Twitter. If social networks are not your thing, add a blog to your web site and write about what you know, and what interests you. If you have expertise in a particular field, write about that.
Incidentally, if the URL for your web site is not your name, you should also register your name as a separate domain name – if only to be sure that a trickster, or someone with the same name and a bad reputation, doesn’t get it.
Set up an RSS news feed for yourself, so you’ll know immediately anytime your name pops up in news or gossip sites, or on blogs. If something untrue is posted about you, take action. Reputable news sites and blogs have their own reputations to protect, and so can usually be persuaded to correct anything that is demonstrably false. Try to get the error removed entirely, or corrected within the original article. An erratum on the last page of the next edition will be ignored, and will leave the false information online, intact.
Unfair comments on doctor rating sites are unlikely to be removed unless they are blatantly libelous; but there is nothing wrong with encouraging happy patients to write favorable reviews. Turnabout is fair play.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
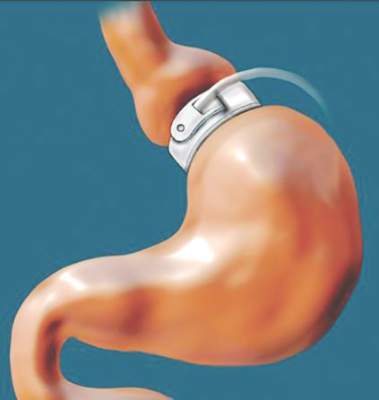
Earlier bariatric surgery may improve cardiovascular outcomes
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
AT ACC 16
Key clinical point: Morbidly obese patients who underwent bariatric surgery before age 45 years had a reduced risk of adverse cardiovascular outcomes vs. those aged 45 or older at the time of surgery, despite similar weight loss.
Major finding: Older vs. younger age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8).
Data source: A review of outcomes in 828 laparoscopic adjustable gastric banding patients.
Disclosures: The authors reported having no disclosures.
AAN updates botulinum toxin guidelines for most established uses
VANCOUVER – A new American Academy of Neurology practice guideline on the efficacy and safety evidence for botulinum toxin treatment of blepharospasm, cervical dystonia, spasticity, and headache has updated the last recommendations published in 2008, but leaves some relevant clinical concerns and off-label uses unaddressed.
The 2016 update, published April 18 in Neurology, adds new individual evidence for the use of the four branded formulations of the two commercially available botulinum toxin serotypes, A and B, for the aforementioned indications rather than lumping all recommendations for botulinum toxin together as in the 2008 guidelines. However, questions remain on the differences between the different products in clinical practice, especially since the formulations show little clinical difference in head-to-head comparisons for some of the indications, especially for the serotype A formulations.
In a press briefing on the new guidelines at the annual meeting of the American Academy of Neurology, guidelines coauthor Dr. Mark Hallett noted that nothing really surprised the experienced 14-member committee that put the guidelines together. “The reason that we chose these four different diseases is because we already had the sense that they were going to change in the particular ways that they did. We didn’t know exactly, of course, what was going to happen, but we had a sense that there were sufficient data that it was worth looking at them.”
For blepharospasm, the totality of evidence suggests that onabotulinumtoxinA (onaBoNT-A; Botox) and incobotulinumtoxinA (incoBoNT-A; Xeomin) injections should be considered and are probably safe and effective (level B recommendation), while abobotulinumtoxinA (aboBoNT-A; Dysport) may be considered (level C) and is possibly effective. The evidence shows that incoBoNT-A and onaBoNT-A have equivalent efficacy and aboBoNT-A and onaBoNT-A are possibly equivalent. There was not enough evidence to determine the efficacy of rimabotulinumtoxinB for blepharospasm (rimaBoNT-B; Myobloc).
The rigorousness of clinical trials in evaluating the efficacy and safety of botulinum toxin has evolved since the Food and Drug Administration approved onaBoNT-A and incoBoNT-A to treat blepharospasm, but no new trials have been conducted to give it a higher level of recommendation despite their well-known magnitude of benefit, said Dr. Hallett, chief of the National Institute of Neurological Disorders and Stroke medical neurology branch and its human motor control section.
New evidence added to the already well-established data on the effectiveness of botulinum toxin for cervical dystonia suggest that onaBoNT-A and incoBoNT-A are probably safe and effective and should be considered. In addition, aboBoNT-A and rimaBoNT-B have already proven effectiveness and safety and should be offered. The lack of class I studies for onaBoNT-A and incoBoNT-A led to the lower level of recommendation for them despite an extensive clinical history of their use in cervical dystonia, the guideline committee wrote (Neurology. 2016 Apr 18. doi: 10.1212/WNL.0000000000002560).
In adults with upper-limb spasticity, all three serotype A formulations – onaBoNT-A, aboBoNT-A, and incoBoNT-A – are effective and safe in reducing symptoms and improving passive limb function. All three achieved level A evidence to recommend that they should be offered. One comparative trial showed enough evidence to say that onaBoNT-A is probably superior to tizanidine for reducing upper-extremity tone and should be considered before it. RimaBoNT-B has level B evidence to advise that it should be considered and is probably safe and effective. None of the formulations have enough data to determine their efficacy on active limb function.
Fewer trials have examined the safety and effectiveness of botulinum toxin formulations for reducing lower leg spasticity in adults. The guidelines panel found enough evidence to recommend that aboBoNT-A and onaBoNT-A are safe and effective and should be offered (level A). There were no trials with high enough level of quality to determine whether incoBoNT-A or rimaBoNT-B were effective for lower-leg spasticity. None of the four agents had enough evidence to support their ability to improve active function associated with lower-limb spasticity.
At the press briefing, guidelines first author Dr. David M. Simpson expressed hope that a more refined methodology for evaluating spasticity might be achieved in future trials of botulinum toxin to detect the potentially subtle effects the agents may have on certain patients who are more likely to achieve benefits in active limb function. Currently, trials use a standardized set of outcomes to try to detect differences in patients with wide-ranging severity of symptoms and types of injury that led to spasticity. Dr. Simpson is professor of neurology at Mount Sinai in New York, as well as director of the neuromuscular diseases division and director of the clinical neurophysiology laboratories.
Positive results for onaBoNT-A in two pivotal trials in chronic migraine that were published since the last guidelines give the formulation the only FDA-approved indication for a botulinum toxin in chronic migraine and earned it a level A recommendation from the guidelines committee. However, in the trials it had a relatively small magnitude of efficacy in reducing the number of headache days by 15% versus placebo. The guidelines also advise not using onaBoNT-A in episodic migraine based on three negative trials. No high-quality trials have evaluated any formulation to change the overall 2008 guidelines’ advice that botulinum toxin is probably ineffective for treating chronic tension-type headaches.
Familiarity with appropriate dosing and side effects may allow clinicians to use the products off-label for indications in the guidelines for which clinical trials were not available, Dr. Richard L. Barbano of the movement disorders division at the University of Rochester noted in an editorial about the guidelines (Neurol Clin Pract. 2016 Apr 18. doi: 10.1212/CPJ.0000000000000244). “Off-label use is common in clinical practice. Little data exist to indicate that any of the different formulations, with attention to appropriate dosing and side effects, would not be effective in treating these other conditions. There are also a number of other neurologic conditions not discussed in the guideline in which botulinum toxin has shown efficacy, such as hemifacial spasm and other focal dystonias. Lack of sufficient high-level evidence to support a level A or B guideline recommendation does not negate their potential utility and likewise, there is little evidence to recommend one formulation over another.”
“In some circumstances where the drugs are relatively equivalent, some people prefer to stick with one so they get used to it more, and they can have more of a sense of what the dosing is, given that the doses may be different with the compounds and have different side effects,” Dr. Hallett said in an interview, noting that availability and price also might enter into a clinician’s decision on what to do.
Dr. Barbano also said that cost and value are becoming more important, and neurologists should consider when botulinum toxin therapy should be chosen among existing alternative treatment options, particularly for chronic migraine.
The guidelines are endorsed by the American Association of Neuromuscular & Electrodiagnostic Medicine and the American Society of Plastic Surgeons.
Dr. Hallett reported serving as chair of the Neurotoxin Institute Advisory Council and has received research grants from Allergan and Merz Pharmaceuticals. Dr. Simpson reported receiving research grants from and served as a consultant for Allergan, Ipsen, Merz Pharmaceuticals, and Acorda Therapeutics. Five other coauthors of the guidelines disclosed relationships with manufacturers of botulinum toxin formulations. Dr. Barbano reported serving on a scientific advisory board for Allergan and receiving research support from Allergan, Vaccinex, and Biotie.
VANCOUVER – A new American Academy of Neurology practice guideline on the efficacy and safety evidence for botulinum toxin treatment of blepharospasm, cervical dystonia, spasticity, and headache has updated the last recommendations published in 2008, but leaves some relevant clinical concerns and off-label uses unaddressed.
The 2016 update, published April 18 in Neurology, adds new individual evidence for the use of the four branded formulations of the two commercially available botulinum toxin serotypes, A and B, for the aforementioned indications rather than lumping all recommendations for botulinum toxin together as in the 2008 guidelines. However, questions remain on the differences between the different products in clinical practice, especially since the formulations show little clinical difference in head-to-head comparisons for some of the indications, especially for the serotype A formulations.
In a press briefing on the new guidelines at the annual meeting of the American Academy of Neurology, guidelines coauthor Dr. Mark Hallett noted that nothing really surprised the experienced 14-member committee that put the guidelines together. “The reason that we chose these four different diseases is because we already had the sense that they were going to change in the particular ways that they did. We didn’t know exactly, of course, what was going to happen, but we had a sense that there were sufficient data that it was worth looking at them.”
For blepharospasm, the totality of evidence suggests that onabotulinumtoxinA (onaBoNT-A; Botox) and incobotulinumtoxinA (incoBoNT-A; Xeomin) injections should be considered and are probably safe and effective (level B recommendation), while abobotulinumtoxinA (aboBoNT-A; Dysport) may be considered (level C) and is possibly effective. The evidence shows that incoBoNT-A and onaBoNT-A have equivalent efficacy and aboBoNT-A and onaBoNT-A are possibly equivalent. There was not enough evidence to determine the efficacy of rimabotulinumtoxinB for blepharospasm (rimaBoNT-B; Myobloc).
The rigorousness of clinical trials in evaluating the efficacy and safety of botulinum toxin has evolved since the Food and Drug Administration approved onaBoNT-A and incoBoNT-A to treat blepharospasm, but no new trials have been conducted to give it a higher level of recommendation despite their well-known magnitude of benefit, said Dr. Hallett, chief of the National Institute of Neurological Disorders and Stroke medical neurology branch and its human motor control section.
New evidence added to the already well-established data on the effectiveness of botulinum toxin for cervical dystonia suggest that onaBoNT-A and incoBoNT-A are probably safe and effective and should be considered. In addition, aboBoNT-A and rimaBoNT-B have already proven effectiveness and safety and should be offered. The lack of class I studies for onaBoNT-A and incoBoNT-A led to the lower level of recommendation for them despite an extensive clinical history of their use in cervical dystonia, the guideline committee wrote (Neurology. 2016 Apr 18. doi: 10.1212/WNL.0000000000002560).
In adults with upper-limb spasticity, all three serotype A formulations – onaBoNT-A, aboBoNT-A, and incoBoNT-A – are effective and safe in reducing symptoms and improving passive limb function. All three achieved level A evidence to recommend that they should be offered. One comparative trial showed enough evidence to say that onaBoNT-A is probably superior to tizanidine for reducing upper-extremity tone and should be considered before it. RimaBoNT-B has level B evidence to advise that it should be considered and is probably safe and effective. None of the formulations have enough data to determine their efficacy on active limb function.
Fewer trials have examined the safety and effectiveness of botulinum toxin formulations for reducing lower leg spasticity in adults. The guidelines panel found enough evidence to recommend that aboBoNT-A and onaBoNT-A are safe and effective and should be offered (level A). There were no trials with high enough level of quality to determine whether incoBoNT-A or rimaBoNT-B were effective for lower-leg spasticity. None of the four agents had enough evidence to support their ability to improve active function associated with lower-limb spasticity.
At the press briefing, guidelines first author Dr. David M. Simpson expressed hope that a more refined methodology for evaluating spasticity might be achieved in future trials of botulinum toxin to detect the potentially subtle effects the agents may have on certain patients who are more likely to achieve benefits in active limb function. Currently, trials use a standardized set of outcomes to try to detect differences in patients with wide-ranging severity of symptoms and types of injury that led to spasticity. Dr. Simpson is professor of neurology at Mount Sinai in New York, as well as director of the neuromuscular diseases division and director of the clinical neurophysiology laboratories.
Positive results for onaBoNT-A in two pivotal trials in chronic migraine that were published since the last guidelines give the formulation the only FDA-approved indication for a botulinum toxin in chronic migraine and earned it a level A recommendation from the guidelines committee. However, in the trials it had a relatively small magnitude of efficacy in reducing the number of headache days by 15% versus placebo. The guidelines also advise not using onaBoNT-A in episodic migraine based on three negative trials. No high-quality trials have evaluated any formulation to change the overall 2008 guidelines’ advice that botulinum toxin is probably ineffective for treating chronic tension-type headaches.
Familiarity with appropriate dosing and side effects may allow clinicians to use the products off-label for indications in the guidelines for which clinical trials were not available, Dr. Richard L. Barbano of the movement disorders division at the University of Rochester noted in an editorial about the guidelines (Neurol Clin Pract. 2016 Apr 18. doi: 10.1212/CPJ.0000000000000244). “Off-label use is common in clinical practice. Little data exist to indicate that any of the different formulations, with attention to appropriate dosing and side effects, would not be effective in treating these other conditions. There are also a number of other neurologic conditions not discussed in the guideline in which botulinum toxin has shown efficacy, such as hemifacial spasm and other focal dystonias. Lack of sufficient high-level evidence to support a level A or B guideline recommendation does not negate their potential utility and likewise, there is little evidence to recommend one formulation over another.”
“In some circumstances where the drugs are relatively equivalent, some people prefer to stick with one so they get used to it more, and they can have more of a sense of what the dosing is, given that the doses may be different with the compounds and have different side effects,” Dr. Hallett said in an interview, noting that availability and price also might enter into a clinician’s decision on what to do.
Dr. Barbano also said that cost and value are becoming more important, and neurologists should consider when botulinum toxin therapy should be chosen among existing alternative treatment options, particularly for chronic migraine.
The guidelines are endorsed by the American Association of Neuromuscular & Electrodiagnostic Medicine and the American Society of Plastic Surgeons.
Dr. Hallett reported serving as chair of the Neurotoxin Institute Advisory Council and has received research grants from Allergan and Merz Pharmaceuticals. Dr. Simpson reported receiving research grants from and served as a consultant for Allergan, Ipsen, Merz Pharmaceuticals, and Acorda Therapeutics. Five other coauthors of the guidelines disclosed relationships with manufacturers of botulinum toxin formulations. Dr. Barbano reported serving on a scientific advisory board for Allergan and receiving research support from Allergan, Vaccinex, and Biotie.
VANCOUVER – A new American Academy of Neurology practice guideline on the efficacy and safety evidence for botulinum toxin treatment of blepharospasm, cervical dystonia, spasticity, and headache has updated the last recommendations published in 2008, but leaves some relevant clinical concerns and off-label uses unaddressed.
The 2016 update, published April 18 in Neurology, adds new individual evidence for the use of the four branded formulations of the two commercially available botulinum toxin serotypes, A and B, for the aforementioned indications rather than lumping all recommendations for botulinum toxin together as in the 2008 guidelines. However, questions remain on the differences between the different products in clinical practice, especially since the formulations show little clinical difference in head-to-head comparisons for some of the indications, especially for the serotype A formulations.
In a press briefing on the new guidelines at the annual meeting of the American Academy of Neurology, guidelines coauthor Dr. Mark Hallett noted that nothing really surprised the experienced 14-member committee that put the guidelines together. “The reason that we chose these four different diseases is because we already had the sense that they were going to change in the particular ways that they did. We didn’t know exactly, of course, what was going to happen, but we had a sense that there were sufficient data that it was worth looking at them.”
For blepharospasm, the totality of evidence suggests that onabotulinumtoxinA (onaBoNT-A; Botox) and incobotulinumtoxinA (incoBoNT-A; Xeomin) injections should be considered and are probably safe and effective (level B recommendation), while abobotulinumtoxinA (aboBoNT-A; Dysport) may be considered (level C) and is possibly effective. The evidence shows that incoBoNT-A and onaBoNT-A have equivalent efficacy and aboBoNT-A and onaBoNT-A are possibly equivalent. There was not enough evidence to determine the efficacy of rimabotulinumtoxinB for blepharospasm (rimaBoNT-B; Myobloc).
The rigorousness of clinical trials in evaluating the efficacy and safety of botulinum toxin has evolved since the Food and Drug Administration approved onaBoNT-A and incoBoNT-A to treat blepharospasm, but no new trials have been conducted to give it a higher level of recommendation despite their well-known magnitude of benefit, said Dr. Hallett, chief of the National Institute of Neurological Disorders and Stroke medical neurology branch and its human motor control section.
New evidence added to the already well-established data on the effectiveness of botulinum toxin for cervical dystonia suggest that onaBoNT-A and incoBoNT-A are probably safe and effective and should be considered. In addition, aboBoNT-A and rimaBoNT-B have already proven effectiveness and safety and should be offered. The lack of class I studies for onaBoNT-A and incoBoNT-A led to the lower level of recommendation for them despite an extensive clinical history of their use in cervical dystonia, the guideline committee wrote (Neurology. 2016 Apr 18. doi: 10.1212/WNL.0000000000002560).
In adults with upper-limb spasticity, all three serotype A formulations – onaBoNT-A, aboBoNT-A, and incoBoNT-A – are effective and safe in reducing symptoms and improving passive limb function. All three achieved level A evidence to recommend that they should be offered. One comparative trial showed enough evidence to say that onaBoNT-A is probably superior to tizanidine for reducing upper-extremity tone and should be considered before it. RimaBoNT-B has level B evidence to advise that it should be considered and is probably safe and effective. None of the formulations have enough data to determine their efficacy on active limb function.
Fewer trials have examined the safety and effectiveness of botulinum toxin formulations for reducing lower leg spasticity in adults. The guidelines panel found enough evidence to recommend that aboBoNT-A and onaBoNT-A are safe and effective and should be offered (level A). There were no trials with high enough level of quality to determine whether incoBoNT-A or rimaBoNT-B were effective for lower-leg spasticity. None of the four agents had enough evidence to support their ability to improve active function associated with lower-limb spasticity.
At the press briefing, guidelines first author Dr. David M. Simpson expressed hope that a more refined methodology for evaluating spasticity might be achieved in future trials of botulinum toxin to detect the potentially subtle effects the agents may have on certain patients who are more likely to achieve benefits in active limb function. Currently, trials use a standardized set of outcomes to try to detect differences in patients with wide-ranging severity of symptoms and types of injury that led to spasticity. Dr. Simpson is professor of neurology at Mount Sinai in New York, as well as director of the neuromuscular diseases division and director of the clinical neurophysiology laboratories.
Positive results for onaBoNT-A in two pivotal trials in chronic migraine that were published since the last guidelines give the formulation the only FDA-approved indication for a botulinum toxin in chronic migraine and earned it a level A recommendation from the guidelines committee. However, in the trials it had a relatively small magnitude of efficacy in reducing the number of headache days by 15% versus placebo. The guidelines also advise not using onaBoNT-A in episodic migraine based on three negative trials. No high-quality trials have evaluated any formulation to change the overall 2008 guidelines’ advice that botulinum toxin is probably ineffective for treating chronic tension-type headaches.
Familiarity with appropriate dosing and side effects may allow clinicians to use the products off-label for indications in the guidelines for which clinical trials were not available, Dr. Richard L. Barbano of the movement disorders division at the University of Rochester noted in an editorial about the guidelines (Neurol Clin Pract. 2016 Apr 18. doi: 10.1212/CPJ.0000000000000244). “Off-label use is common in clinical practice. Little data exist to indicate that any of the different formulations, with attention to appropriate dosing and side effects, would not be effective in treating these other conditions. There are also a number of other neurologic conditions not discussed in the guideline in which botulinum toxin has shown efficacy, such as hemifacial spasm and other focal dystonias. Lack of sufficient high-level evidence to support a level A or B guideline recommendation does not negate their potential utility and likewise, there is little evidence to recommend one formulation over another.”
“In some circumstances where the drugs are relatively equivalent, some people prefer to stick with one so they get used to it more, and they can have more of a sense of what the dosing is, given that the doses may be different with the compounds and have different side effects,” Dr. Hallett said in an interview, noting that availability and price also might enter into a clinician’s decision on what to do.
Dr. Barbano also said that cost and value are becoming more important, and neurologists should consider when botulinum toxin therapy should be chosen among existing alternative treatment options, particularly for chronic migraine.
The guidelines are endorsed by the American Association of Neuromuscular & Electrodiagnostic Medicine and the American Society of Plastic Surgeons.
Dr. Hallett reported serving as chair of the Neurotoxin Institute Advisory Council and has received research grants from Allergan and Merz Pharmaceuticals. Dr. Simpson reported receiving research grants from and served as a consultant for Allergan, Ipsen, Merz Pharmaceuticals, and Acorda Therapeutics. Five other coauthors of the guidelines disclosed relationships with manufacturers of botulinum toxin formulations. Dr. Barbano reported serving on a scientific advisory board for Allergan and receiving research support from Allergan, Vaccinex, and Biotie.
AT THE AAN 2016 ANNUAL MEETING
Centers for Medicare & Medicaid Services (CMS) Eliminates Two-Midnight Rule's Inpatient Payment Cuts: Report
According to the report, CMS estimated the two-midnight policy would increase Medicare spending by ~$220 million due to expected increases in admissions. Hospitals also will see a one-time increase of 0.6% in fiscal 2017, making up for the 0.2% reduction to the rates the last three years.
According to the report, CMS estimated the two-midnight policy would increase Medicare spending by ~$220 million due to expected increases in admissions. Hospitals also will see a one-time increase of 0.6% in fiscal 2017, making up for the 0.2% reduction to the rates the last three years.
According to the report, CMS estimated the two-midnight policy would increase Medicare spending by ~$220 million due to expected increases in admissions. Hospitals also will see a one-time increase of 0.6% in fiscal 2017, making up for the 0.2% reduction to the rates the last three years.
Using the Common Sense Model in Daily Clinical Practice for Improving Medication Adherence
From Genoa-QoL Healthcare and the University of Michigan College of Pharmacy, Ann Arbor, MI.
Abstract
- Objective: To review the Common Sense Model, a framework that can be used for understanding patients’ behavior, including taking or not taking medications as prescribed.
- Methods: Descriptive report.
- Results: Medication adherence, a critical component of achieving good patient outcomes and reducing medical costs, is dependent upon patient illness beliefs. The Common Sense Model holds that these beliefs can be categorized as illness identity, cause, consequence, control, and timeline. Effective communication is necessary to understand the beliefs that patients hold and help them understand their condition. Good communication also can allay fears and other emotions that can be disruptive to achieving good outcomes.
- Conclusion: Clinicians should seek to understand their patients’ illness beliefs and collaborate with them to achieve desired health outcomes.
Clinical practice is based on scientific evidence, by which medical problems are diagnosed and treatment recommendations are made. However, the role of the patient may not be completely recognized as an integral part of the process of patient care. The impact of failing to adequately recognize the patient perspective is evident in medication nonadherence. Health psychology research can provide clinicians insight into patients’ perceptions and behavior. This paper reviews the Common Sense Model (CSM), a behavioral model that provides a framework that can be used in understanding patients’ behavior. In this paper I will discuss the model and how it can be a possible strategy for improving adherence.
Making the Case for CSM in Daily Practice
It can be difficult to realize that persons seeking medical attention would not take medications as prescribed by a physician. In fact, studies reveal that on average, 16.4% of prescribed medications will not be picked up from the pharmacy [1]. Of those patients who do pick up their medication, approximately 1 out of 4 will not take them as prescribed [2]. Such medication nonadherence leads to poor health outcomes and increased health care costs [3,4]. There are many reasons for medication nonadherence [5], and there is no single solution to improving medication adherence [6]. A Cochrane review of randomized controlled trials evaluating various interventions intended to enhance patient adherence to prescribed medications for medical conditions found them to have limited effectiveness. Interventions assessed included health and medication information, reminder calls, follow-up assessment of medication therapy, social support, and simplification of the treatment regimen [6]. In an exploratory study of patients with chronic health conditions, Kucukarslan et al found patients’ beliefs about their illness and their medication are integral to their health care decisions [7]. Their findings were consistent with the CSM, which is based on Leventhal’s theory of self-regulation.
Self-regulation theory states that rational people will make decisions to reduce their health threat. Patients’ perceptions of their selves and environments drives their behavior. So in the presence of a health threat, a person will seek to eliminate or reduce that threat. However, coping behavior is complex. A person may decide to follow the advice of his clinician, follow some other advice (from family, friends, advertising, etc.), or do nothing. The premise of self-regulation is that people will choose a common sense approach to their health threat [8]. Therefore, clinicians must understand their patients’ viewpoint of themselves and their health condition so they may help guide them toward healthy outcomes.
The Common Sense Model
The CSM is a framework for understanding patient behavior when faced with a health threat. It holds that patients form common sense representations of their illness using information from 5 domains [8]: (1) the identity of the illness (the label the patient gives to the condition and symptoms); (2) the cause of the illness; (3) the consequences of the illness (beliefs about how the illness will impact the patient’s well-being); (4) whether the illness can be controlled or cured; and (5) timeline (beliefs about how long the condition will last). A patient may either act to address the health threat or choose to ignore it. Patient emotions are proposed to have a role on patient behavior along with the 5 dimensions of illness perception.
Illness Identity
Illness identity is the label patients place on the health threat; it is most likely not the same as the signs and symptoms clinicians use. Therefore, the first misconnect between physician and patient may be in describing the illness. Chen et al studied illness identity as perceived by patients with hypertension [9,10]. Illness identity was defined as (1) hypertension-related symptoms, (2) symptoms experienced before and after their diagnosis; and (3) symptoms used to predict high blood pressure. Although hypertension is asymptomatic, patients do perceive symptoms such as headache associated with their hypertension. The researchers found those patients who identified more symptoms were more likely to believe that their symptoms caused the hypertension and were correspondingly less likely to use their medication. For them, when the headache subsides, so does the hypertension.
Physicians should find out how patients assess their health condition and provide them tools for evaluating their response to medication. In the case of hypertension, the physician could have the patient check their blood pressure with and without the headache to demonstrate that hypertension occurs even when the patient is not “symptomatic.” The point is to converse with the patient to learn how they view their condition. Clinicians should resist the “urge” to correct patients. Taking time to help patients better understand their condition is important. A misstep:
Patient: I can tell when my blood pressure is high. I get a pounding headache.
Doctor: High blood pressure is an asymptomatic condition. Your headaches are not caused by your high blood pressure.
Patients may choose to ignore the clinician if they feel strongly about how they define their illness. It is better to listen to the patient and offer steps to learn about their health condition. Here is a better response from the physician:
Doctor: You are telling me that you can tell when your blood pressure is high. So when your head aches your pressure is high, right?
Patient: Yes.
Doctor: Let me tell you more about high blood pressure. High blood pressure is also present without headaches...
Illness Causes
There are multiple causative factors patients may associate with their disease. Causes attributed to disease may be based on patient experiences, input from family and friends, and cultural factors. Causes may include emotional state, stress or worry, overwork, genetic predisposition, or environmental factors (eg, pollution). Jessop and Rutter found patients who perceive their condition as due to uncontrollable factors, such as chance, germs, or pollution, were less likely to take their medication [11]. Similar findings were published by Chen et al [9]. They found psychological factors, environmental risk factors (eg, smoking, diet), and even bad luck or chance associated with less likelihood of taking medications as prescribed. Clinicians should explore patients’ perceptions of causes of a condition. Patients strive to eliminate the perceived cause, thus eliminating the need to take medication. In some cultures, bad luck or chance drives patients’ decisions to not take medication, or they believe in fate and do not accept treatment. Whether they feel they can control their condition by eliminating the cause or have a fatalistic view that the cause of their condition is not within their control, the clinician must work with the patient to reduce the impact of misperceptions or significance of perceived causes.
Illness Consequence
Consequence associated with the health condition is an important factor in patient behavior [12]. Patients must understand the specific threats to their health if a condition is left untreated or uncontrolled. Patients’ view of illness consequence may be formed by their own perceived vulnerability or susceptibility and the perceived seriousness of the condition. For example, patients with hypertension should be informed about the impact of high blood pressure on their bodies and the consequence of disability from stroke, dependency on dialysis from kidney failure, or death. They may not consider themselves susceptible to illness since they “feel healthy” and may decide to delay treatment. Patients with conditions such as asthma or heart failure may believe they are cured when their symptoms abate and therefore believe they have no more need for medication. Such patients need education to understand that they are asymptomatic because they are well controlled with medication.
Illness Control
Patients may feel they can control their health condition by changing their behavior, changing their environment, and/or by taking prescribed medication. As discussed earlier, cause and control both work together to form patient beliefs and actions. Patients will take their medications as prescribed if they believe in the effectiveness of medication to control their condition [11,13–15]. Interestingly, Ross found those who felt they had more control over their illness were more likely not to take their medication as prescribed [12]. These persons are more likely to not want to become “dependent” on medication. Their feeling was that they can make changes in their lives and thereby improve their health condition.
Physicians should invite patients’ thoughts as to what should be done to improve their health condition, and collaborate with the patient on an action plan for change if change is expected to improve/control the health condition. Follow-up to assess the patient’s health status longitudinally is necessary.
In this exchange, the patient feels he can control his hypertension on his own:
Doctor: I recommend that you start taking medication to control your blood pressure. Uncontrolled high blood pressure can lead to many health problems.
Patient: I am not ready to start taking medication.
Doctor: What are your reasons?
Patient: I am under a lot of stress at work. Once I get control of this stress, my blood pressure will go down.
Doctor: Getting control of your stress at work is important. Let me tell you more about high blood pressure.
Patient: Okay.
Doctor: There is no one cause of your high blood pressure. Eliminating your work stress will most likely not reduce your blood pressure....
Timeline
Health conditions can be acute, chronic, or cyclical (ie, seasonal); however, patients may have different perceptions of the duration of their health condition. In Kucukarslan et al, some patients did not believe their hypertension was a lifelong condition because they felt they would be able to cure it [7]. For example, as illustrated above, patients may believe that stress causes their hypertension, and if the stress could be controlled, then their blood pressure would normalize. Conversely, Ross et al found that patients who viewed their hypertension as a long-term condition were more likely to believe their medications were necessary and thus more likely to take their medication as prescribed [12]. A lifelong or chronic health condition is a difficult concept for patients to accept, especially ones who may view themselves as too young to have the condition.
Emotions
After being informed about their health condition, patients may feel emotions that are not apparent to the practitioner. These may include worry, depression, anger, anxiety, or fear. Emotions may impact their decision to take medication [12,14]. Listening for patients’ responses to health information provided by the clinician and letting patients know they have been heard will help allay strong negative emotions [16]. Good communication builds trust between the clinician and patient.
Conclusion
Patients receive medical advice from clinicians that may be inconsistent with their beliefs and understanding of their health condition. Studies of medication nonadherence find many factors contribute to it and no one tool to improve medication adherence exists. However, the consequence of medication nonadherence are great and include include worsening condition, increased comorbid disease, and increased health care costs. Understanding patients’ beliefs about their health condition is an important step toward reducing medication nonadherence. The CSM provides a framework for clinicians to guide patients toward effective decision-making. Listening to the patient explain how they view their condition—how they define it, the causes, consequences, how to control it, and how long it will last or if it will progress—are important to the process of working with the patient manage their condition effectively. Clinicians’ reaction to these perceptions are important, and dismissing them may alienate patients. Effective communication is necessary to understand patients’ perspectives and to help them manage their health condition.
Corresponding author: Suzan N. Kucukarslan, PhD, RPh, [email protected].
Financial disclosures: None.
1. Gadkari AS, McHorney CA. Medication non-fulfillment rates and reasons: a narrative systematic review. Curr Med Res Opin 2010;26:683–785.
2. DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care 2004;42:200–9.
3. Ho PM, Rumsfeld JS, Masoudi FA, et al. The effect of medication non-adherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med 2006;166;1836–41.
4. Benjamin RM. Medication adherence: Helping patients take their medicines as directed. Pub Health Rep 2012;2–3.
5. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005;353:487–97.
6. Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev 2008;(2):CD000011.
7. Kucukarslan SN, Lewis NJW, Shimp LA, et al. Exploring patient experiences with prescription medicines to identify unmet patient needs: implications for research and practice. Res Social Adm Pharm 2012;8:321–332.
8. Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health, and behavior: a perceptual-cognitive approach. Psychol Health 1998;13:717–33.
9. Chen S-L, Tsai J-C, Chou K-R. Illness perceptions and adherence to therapeutic regimens among patients with hypertension: A structural model approach. Int J Nurs Stud 2011;48:235–45.
10. Chen S-L, Tsai J-C, Lee W-L. The impact of illness perception on adherence to therapeutic regimens of patients with hypertension in Taiwan. J Clin Nurs 2009;18:2234–44.
11. Jessop DC, Rutter DR. Adherence to asthma medication: the role of illness representations. Psychol Health 2003;18:595–612.
12. Ross S, Walker A, MacLeod M. Patient compliance in hypertension:role of illness perceptions and treatment beliefs. J Hum Hypertension 2004;18:607–13.
13 Searle A, Norman P. Thompson R. Vedhara K. A prospective examination of illness belies and coping in patients with type 2 diabetes. Br J Health Psychol 2007;12:621–38.
14. Zugelj U, Zuparnicic M, Komidar L, et al. Self-reported adherence behavior in adolescent hypertensive patients: the role of illness representation and personality. J Pediatr Psychol 2010;35:1049–60.
15. Horne R, Weinman J. Self-regulation and self-management in asthma: exploring the role of illness perception and treatment beliefs in explaining non-adherence to preventer medication. Psychol Health 2002;17:17–32.
16. Northouse LL, Northouse PG. Health communication: strategies for health professionals. Stamford: Prentice Hall; 1998.
From Genoa-QoL Healthcare and the University of Michigan College of Pharmacy, Ann Arbor, MI.
Abstract
- Objective: To review the Common Sense Model, a framework that can be used for understanding patients’ behavior, including taking or not taking medications as prescribed.
- Methods: Descriptive report.
- Results: Medication adherence, a critical component of achieving good patient outcomes and reducing medical costs, is dependent upon patient illness beliefs. The Common Sense Model holds that these beliefs can be categorized as illness identity, cause, consequence, control, and timeline. Effective communication is necessary to understand the beliefs that patients hold and help them understand their condition. Good communication also can allay fears and other emotions that can be disruptive to achieving good outcomes.
- Conclusion: Clinicians should seek to understand their patients’ illness beliefs and collaborate with them to achieve desired health outcomes.
Clinical practice is based on scientific evidence, by which medical problems are diagnosed and treatment recommendations are made. However, the role of the patient may not be completely recognized as an integral part of the process of patient care. The impact of failing to adequately recognize the patient perspective is evident in medication nonadherence. Health psychology research can provide clinicians insight into patients’ perceptions and behavior. This paper reviews the Common Sense Model (CSM), a behavioral model that provides a framework that can be used in understanding patients’ behavior. In this paper I will discuss the model and how it can be a possible strategy for improving adherence.
Making the Case for CSM in Daily Practice
It can be difficult to realize that persons seeking medical attention would not take medications as prescribed by a physician. In fact, studies reveal that on average, 16.4% of prescribed medications will not be picked up from the pharmacy [1]. Of those patients who do pick up their medication, approximately 1 out of 4 will not take them as prescribed [2]. Such medication nonadherence leads to poor health outcomes and increased health care costs [3,4]. There are many reasons for medication nonadherence [5], and there is no single solution to improving medication adherence [6]. A Cochrane review of randomized controlled trials evaluating various interventions intended to enhance patient adherence to prescribed medications for medical conditions found them to have limited effectiveness. Interventions assessed included health and medication information, reminder calls, follow-up assessment of medication therapy, social support, and simplification of the treatment regimen [6]. In an exploratory study of patients with chronic health conditions, Kucukarslan et al found patients’ beliefs about their illness and their medication are integral to their health care decisions [7]. Their findings were consistent with the CSM, which is based on Leventhal’s theory of self-regulation.
Self-regulation theory states that rational people will make decisions to reduce their health threat. Patients’ perceptions of their selves and environments drives their behavior. So in the presence of a health threat, a person will seek to eliminate or reduce that threat. However, coping behavior is complex. A person may decide to follow the advice of his clinician, follow some other advice (from family, friends, advertising, etc.), or do nothing. The premise of self-regulation is that people will choose a common sense approach to their health threat [8]. Therefore, clinicians must understand their patients’ viewpoint of themselves and their health condition so they may help guide them toward healthy outcomes.
The Common Sense Model
The CSM is a framework for understanding patient behavior when faced with a health threat. It holds that patients form common sense representations of their illness using information from 5 domains [8]: (1) the identity of the illness (the label the patient gives to the condition and symptoms); (2) the cause of the illness; (3) the consequences of the illness (beliefs about how the illness will impact the patient’s well-being); (4) whether the illness can be controlled or cured; and (5) timeline (beliefs about how long the condition will last). A patient may either act to address the health threat or choose to ignore it. Patient emotions are proposed to have a role on patient behavior along with the 5 dimensions of illness perception.
Illness Identity
Illness identity is the label patients place on the health threat; it is most likely not the same as the signs and symptoms clinicians use. Therefore, the first misconnect between physician and patient may be in describing the illness. Chen et al studied illness identity as perceived by patients with hypertension [9,10]. Illness identity was defined as (1) hypertension-related symptoms, (2) symptoms experienced before and after their diagnosis; and (3) symptoms used to predict high blood pressure. Although hypertension is asymptomatic, patients do perceive symptoms such as headache associated with their hypertension. The researchers found those patients who identified more symptoms were more likely to believe that their symptoms caused the hypertension and were correspondingly less likely to use their medication. For them, when the headache subsides, so does the hypertension.
Physicians should find out how patients assess their health condition and provide them tools for evaluating their response to medication. In the case of hypertension, the physician could have the patient check their blood pressure with and without the headache to demonstrate that hypertension occurs even when the patient is not “symptomatic.” The point is to converse with the patient to learn how they view their condition. Clinicians should resist the “urge” to correct patients. Taking time to help patients better understand their condition is important. A misstep:
Patient: I can tell when my blood pressure is high. I get a pounding headache.
Doctor: High blood pressure is an asymptomatic condition. Your headaches are not caused by your high blood pressure.
Patients may choose to ignore the clinician if they feel strongly about how they define their illness. It is better to listen to the patient and offer steps to learn about their health condition. Here is a better response from the physician:
Doctor: You are telling me that you can tell when your blood pressure is high. So when your head aches your pressure is high, right?
Patient: Yes.
Doctor: Let me tell you more about high blood pressure. High blood pressure is also present without headaches...
Illness Causes
There are multiple causative factors patients may associate with their disease. Causes attributed to disease may be based on patient experiences, input from family and friends, and cultural factors. Causes may include emotional state, stress or worry, overwork, genetic predisposition, or environmental factors (eg, pollution). Jessop and Rutter found patients who perceive their condition as due to uncontrollable factors, such as chance, germs, or pollution, were less likely to take their medication [11]. Similar findings were published by Chen et al [9]. They found psychological factors, environmental risk factors (eg, smoking, diet), and even bad luck or chance associated with less likelihood of taking medications as prescribed. Clinicians should explore patients’ perceptions of causes of a condition. Patients strive to eliminate the perceived cause, thus eliminating the need to take medication. In some cultures, bad luck or chance drives patients’ decisions to not take medication, or they believe in fate and do not accept treatment. Whether they feel they can control their condition by eliminating the cause or have a fatalistic view that the cause of their condition is not within their control, the clinician must work with the patient to reduce the impact of misperceptions or significance of perceived causes.
Illness Consequence
Consequence associated with the health condition is an important factor in patient behavior [12]. Patients must understand the specific threats to their health if a condition is left untreated or uncontrolled. Patients’ view of illness consequence may be formed by their own perceived vulnerability or susceptibility and the perceived seriousness of the condition. For example, patients with hypertension should be informed about the impact of high blood pressure on their bodies and the consequence of disability from stroke, dependency on dialysis from kidney failure, or death. They may not consider themselves susceptible to illness since they “feel healthy” and may decide to delay treatment. Patients with conditions such as asthma or heart failure may believe they are cured when their symptoms abate and therefore believe they have no more need for medication. Such patients need education to understand that they are asymptomatic because they are well controlled with medication.
Illness Control
Patients may feel they can control their health condition by changing their behavior, changing their environment, and/or by taking prescribed medication. As discussed earlier, cause and control both work together to form patient beliefs and actions. Patients will take their medications as prescribed if they believe in the effectiveness of medication to control their condition [11,13–15]. Interestingly, Ross found those who felt they had more control over their illness were more likely not to take their medication as prescribed [12]. These persons are more likely to not want to become “dependent” on medication. Their feeling was that they can make changes in their lives and thereby improve their health condition.
Physicians should invite patients’ thoughts as to what should be done to improve their health condition, and collaborate with the patient on an action plan for change if change is expected to improve/control the health condition. Follow-up to assess the patient’s health status longitudinally is necessary.
In this exchange, the patient feels he can control his hypertension on his own:
Doctor: I recommend that you start taking medication to control your blood pressure. Uncontrolled high blood pressure can lead to many health problems.
Patient: I am not ready to start taking medication.
Doctor: What are your reasons?
Patient: I am under a lot of stress at work. Once I get control of this stress, my blood pressure will go down.
Doctor: Getting control of your stress at work is important. Let me tell you more about high blood pressure.
Patient: Okay.
Doctor: There is no one cause of your high blood pressure. Eliminating your work stress will most likely not reduce your blood pressure....
Timeline
Health conditions can be acute, chronic, or cyclical (ie, seasonal); however, patients may have different perceptions of the duration of their health condition. In Kucukarslan et al, some patients did not believe their hypertension was a lifelong condition because they felt they would be able to cure it [7]. For example, as illustrated above, patients may believe that stress causes their hypertension, and if the stress could be controlled, then their blood pressure would normalize. Conversely, Ross et al found that patients who viewed their hypertension as a long-term condition were more likely to believe their medications were necessary and thus more likely to take their medication as prescribed [12]. A lifelong or chronic health condition is a difficult concept for patients to accept, especially ones who may view themselves as too young to have the condition.
Emotions
After being informed about their health condition, patients may feel emotions that are not apparent to the practitioner. These may include worry, depression, anger, anxiety, or fear. Emotions may impact their decision to take medication [12,14]. Listening for patients’ responses to health information provided by the clinician and letting patients know they have been heard will help allay strong negative emotions [16]. Good communication builds trust between the clinician and patient.
Conclusion
Patients receive medical advice from clinicians that may be inconsistent with their beliefs and understanding of their health condition. Studies of medication nonadherence find many factors contribute to it and no one tool to improve medication adherence exists. However, the consequence of medication nonadherence are great and include include worsening condition, increased comorbid disease, and increased health care costs. Understanding patients’ beliefs about their health condition is an important step toward reducing medication nonadherence. The CSM provides a framework for clinicians to guide patients toward effective decision-making. Listening to the patient explain how they view their condition—how they define it, the causes, consequences, how to control it, and how long it will last or if it will progress—are important to the process of working with the patient manage their condition effectively. Clinicians’ reaction to these perceptions are important, and dismissing them may alienate patients. Effective communication is necessary to understand patients’ perspectives and to help them manage their health condition.
Corresponding author: Suzan N. Kucukarslan, PhD, RPh, [email protected].
Financial disclosures: None.
From Genoa-QoL Healthcare and the University of Michigan College of Pharmacy, Ann Arbor, MI.
Abstract
- Objective: To review the Common Sense Model, a framework that can be used for understanding patients’ behavior, including taking or not taking medications as prescribed.
- Methods: Descriptive report.
- Results: Medication adherence, a critical component of achieving good patient outcomes and reducing medical costs, is dependent upon patient illness beliefs. The Common Sense Model holds that these beliefs can be categorized as illness identity, cause, consequence, control, and timeline. Effective communication is necessary to understand the beliefs that patients hold and help them understand their condition. Good communication also can allay fears and other emotions that can be disruptive to achieving good outcomes.
- Conclusion: Clinicians should seek to understand their patients’ illness beliefs and collaborate with them to achieve desired health outcomes.
Clinical practice is based on scientific evidence, by which medical problems are diagnosed and treatment recommendations are made. However, the role of the patient may not be completely recognized as an integral part of the process of patient care. The impact of failing to adequately recognize the patient perspective is evident in medication nonadherence. Health psychology research can provide clinicians insight into patients’ perceptions and behavior. This paper reviews the Common Sense Model (CSM), a behavioral model that provides a framework that can be used in understanding patients’ behavior. In this paper I will discuss the model and how it can be a possible strategy for improving adherence.
Making the Case for CSM in Daily Practice
It can be difficult to realize that persons seeking medical attention would not take medications as prescribed by a physician. In fact, studies reveal that on average, 16.4% of prescribed medications will not be picked up from the pharmacy [1]. Of those patients who do pick up their medication, approximately 1 out of 4 will not take them as prescribed [2]. Such medication nonadherence leads to poor health outcomes and increased health care costs [3,4]. There are many reasons for medication nonadherence [5], and there is no single solution to improving medication adherence [6]. A Cochrane review of randomized controlled trials evaluating various interventions intended to enhance patient adherence to prescribed medications for medical conditions found them to have limited effectiveness. Interventions assessed included health and medication information, reminder calls, follow-up assessment of medication therapy, social support, and simplification of the treatment regimen [6]. In an exploratory study of patients with chronic health conditions, Kucukarslan et al found patients’ beliefs about their illness and their medication are integral to their health care decisions [7]. Their findings were consistent with the CSM, which is based on Leventhal’s theory of self-regulation.
Self-regulation theory states that rational people will make decisions to reduce their health threat. Patients’ perceptions of their selves and environments drives their behavior. So in the presence of a health threat, a person will seek to eliminate or reduce that threat. However, coping behavior is complex. A person may decide to follow the advice of his clinician, follow some other advice (from family, friends, advertising, etc.), or do nothing. The premise of self-regulation is that people will choose a common sense approach to their health threat [8]. Therefore, clinicians must understand their patients’ viewpoint of themselves and their health condition so they may help guide them toward healthy outcomes.
The Common Sense Model
The CSM is a framework for understanding patient behavior when faced with a health threat. It holds that patients form common sense representations of their illness using information from 5 domains [8]: (1) the identity of the illness (the label the patient gives to the condition and symptoms); (2) the cause of the illness; (3) the consequences of the illness (beliefs about how the illness will impact the patient’s well-being); (4) whether the illness can be controlled or cured; and (5) timeline (beliefs about how long the condition will last). A patient may either act to address the health threat or choose to ignore it. Patient emotions are proposed to have a role on patient behavior along with the 5 dimensions of illness perception.
Illness Identity
Illness identity is the label patients place on the health threat; it is most likely not the same as the signs and symptoms clinicians use. Therefore, the first misconnect between physician and patient may be in describing the illness. Chen et al studied illness identity as perceived by patients with hypertension [9,10]. Illness identity was defined as (1) hypertension-related symptoms, (2) symptoms experienced before and after their diagnosis; and (3) symptoms used to predict high blood pressure. Although hypertension is asymptomatic, patients do perceive symptoms such as headache associated with their hypertension. The researchers found those patients who identified more symptoms were more likely to believe that their symptoms caused the hypertension and were correspondingly less likely to use their medication. For them, when the headache subsides, so does the hypertension.
Physicians should find out how patients assess their health condition and provide them tools for evaluating their response to medication. In the case of hypertension, the physician could have the patient check their blood pressure with and without the headache to demonstrate that hypertension occurs even when the patient is not “symptomatic.” The point is to converse with the patient to learn how they view their condition. Clinicians should resist the “urge” to correct patients. Taking time to help patients better understand their condition is important. A misstep:
Patient: I can tell when my blood pressure is high. I get a pounding headache.
Doctor: High blood pressure is an asymptomatic condition. Your headaches are not caused by your high blood pressure.
Patients may choose to ignore the clinician if they feel strongly about how they define their illness. It is better to listen to the patient and offer steps to learn about their health condition. Here is a better response from the physician:
Doctor: You are telling me that you can tell when your blood pressure is high. So when your head aches your pressure is high, right?
Patient: Yes.
Doctor: Let me tell you more about high blood pressure. High blood pressure is also present without headaches...
Illness Causes
There are multiple causative factors patients may associate with their disease. Causes attributed to disease may be based on patient experiences, input from family and friends, and cultural factors. Causes may include emotional state, stress or worry, overwork, genetic predisposition, or environmental factors (eg, pollution). Jessop and Rutter found patients who perceive their condition as due to uncontrollable factors, such as chance, germs, or pollution, were less likely to take their medication [11]. Similar findings were published by Chen et al [9]. They found psychological factors, environmental risk factors (eg, smoking, diet), and even bad luck or chance associated with less likelihood of taking medications as prescribed. Clinicians should explore patients’ perceptions of causes of a condition. Patients strive to eliminate the perceived cause, thus eliminating the need to take medication. In some cultures, bad luck or chance drives patients’ decisions to not take medication, or they believe in fate and do not accept treatment. Whether they feel they can control their condition by eliminating the cause or have a fatalistic view that the cause of their condition is not within their control, the clinician must work with the patient to reduce the impact of misperceptions or significance of perceived causes.
Illness Consequence
Consequence associated with the health condition is an important factor in patient behavior [12]. Patients must understand the specific threats to their health if a condition is left untreated or uncontrolled. Patients’ view of illness consequence may be formed by their own perceived vulnerability or susceptibility and the perceived seriousness of the condition. For example, patients with hypertension should be informed about the impact of high blood pressure on their bodies and the consequence of disability from stroke, dependency on dialysis from kidney failure, or death. They may not consider themselves susceptible to illness since they “feel healthy” and may decide to delay treatment. Patients with conditions such as asthma or heart failure may believe they are cured when their symptoms abate and therefore believe they have no more need for medication. Such patients need education to understand that they are asymptomatic because they are well controlled with medication.
Illness Control
Patients may feel they can control their health condition by changing their behavior, changing their environment, and/or by taking prescribed medication. As discussed earlier, cause and control both work together to form patient beliefs and actions. Patients will take their medications as prescribed if they believe in the effectiveness of medication to control their condition [11,13–15]. Interestingly, Ross found those who felt they had more control over their illness were more likely not to take their medication as prescribed [12]. These persons are more likely to not want to become “dependent” on medication. Their feeling was that they can make changes in their lives and thereby improve their health condition.
Physicians should invite patients’ thoughts as to what should be done to improve their health condition, and collaborate with the patient on an action plan for change if change is expected to improve/control the health condition. Follow-up to assess the patient’s health status longitudinally is necessary.
In this exchange, the patient feels he can control his hypertension on his own:
Doctor: I recommend that you start taking medication to control your blood pressure. Uncontrolled high blood pressure can lead to many health problems.
Patient: I am not ready to start taking medication.
Doctor: What are your reasons?
Patient: I am under a lot of stress at work. Once I get control of this stress, my blood pressure will go down.
Doctor: Getting control of your stress at work is important. Let me tell you more about high blood pressure.
Patient: Okay.
Doctor: There is no one cause of your high blood pressure. Eliminating your work stress will most likely not reduce your blood pressure....
Timeline
Health conditions can be acute, chronic, or cyclical (ie, seasonal); however, patients may have different perceptions of the duration of their health condition. In Kucukarslan et al, some patients did not believe their hypertension was a lifelong condition because they felt they would be able to cure it [7]. For example, as illustrated above, patients may believe that stress causes their hypertension, and if the stress could be controlled, then their blood pressure would normalize. Conversely, Ross et al found that patients who viewed their hypertension as a long-term condition were more likely to believe their medications were necessary and thus more likely to take their medication as prescribed [12]. A lifelong or chronic health condition is a difficult concept for patients to accept, especially ones who may view themselves as too young to have the condition.
Emotions
After being informed about their health condition, patients may feel emotions that are not apparent to the practitioner. These may include worry, depression, anger, anxiety, or fear. Emotions may impact their decision to take medication [12,14]. Listening for patients’ responses to health information provided by the clinician and letting patients know they have been heard will help allay strong negative emotions [16]. Good communication builds trust between the clinician and patient.
Conclusion
Patients receive medical advice from clinicians that may be inconsistent with their beliefs and understanding of their health condition. Studies of medication nonadherence find many factors contribute to it and no one tool to improve medication adherence exists. However, the consequence of medication nonadherence are great and include include worsening condition, increased comorbid disease, and increased health care costs. Understanding patients’ beliefs about their health condition is an important step toward reducing medication nonadherence. The CSM provides a framework for clinicians to guide patients toward effective decision-making. Listening to the patient explain how they view their condition—how they define it, the causes, consequences, how to control it, and how long it will last or if it will progress—are important to the process of working with the patient manage their condition effectively. Clinicians’ reaction to these perceptions are important, and dismissing them may alienate patients. Effective communication is necessary to understand patients’ perspectives and to help them manage their health condition.
Corresponding author: Suzan N. Kucukarslan, PhD, RPh, [email protected].
Financial disclosures: None.
1. Gadkari AS, McHorney CA. Medication non-fulfillment rates and reasons: a narrative systematic review. Curr Med Res Opin 2010;26:683–785.
2. DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care 2004;42:200–9.
3. Ho PM, Rumsfeld JS, Masoudi FA, et al. The effect of medication non-adherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med 2006;166;1836–41.
4. Benjamin RM. Medication adherence: Helping patients take their medicines as directed. Pub Health Rep 2012;2–3.
5. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005;353:487–97.
6. Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev 2008;(2):CD000011.
7. Kucukarslan SN, Lewis NJW, Shimp LA, et al. Exploring patient experiences with prescription medicines to identify unmet patient needs: implications for research and practice. Res Social Adm Pharm 2012;8:321–332.
8. Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health, and behavior: a perceptual-cognitive approach. Psychol Health 1998;13:717–33.
9. Chen S-L, Tsai J-C, Chou K-R. Illness perceptions and adherence to therapeutic regimens among patients with hypertension: A structural model approach. Int J Nurs Stud 2011;48:235–45.
10. Chen S-L, Tsai J-C, Lee W-L. The impact of illness perception on adherence to therapeutic regimens of patients with hypertension in Taiwan. J Clin Nurs 2009;18:2234–44.
11. Jessop DC, Rutter DR. Adherence to asthma medication: the role of illness representations. Psychol Health 2003;18:595–612.
12. Ross S, Walker A, MacLeod M. Patient compliance in hypertension:role of illness perceptions and treatment beliefs. J Hum Hypertension 2004;18:607–13.
13 Searle A, Norman P. Thompson R. Vedhara K. A prospective examination of illness belies and coping in patients with type 2 diabetes. Br J Health Psychol 2007;12:621–38.
14. Zugelj U, Zuparnicic M, Komidar L, et al. Self-reported adherence behavior in adolescent hypertensive patients: the role of illness representation and personality. J Pediatr Psychol 2010;35:1049–60.
15. Horne R, Weinman J. Self-regulation and self-management in asthma: exploring the role of illness perception and treatment beliefs in explaining non-adherence to preventer medication. Psychol Health 2002;17:17–32.
16. Northouse LL, Northouse PG. Health communication: strategies for health professionals. Stamford: Prentice Hall; 1998.
1. Gadkari AS, McHorney CA. Medication non-fulfillment rates and reasons: a narrative systematic review. Curr Med Res Opin 2010;26:683–785.
2. DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care 2004;42:200–9.
3. Ho PM, Rumsfeld JS, Masoudi FA, et al. The effect of medication non-adherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med 2006;166;1836–41.
4. Benjamin RM. Medication adherence: Helping patients take their medicines as directed. Pub Health Rep 2012;2–3.
5. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005;353:487–97.
6. Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev 2008;(2):CD000011.
7. Kucukarslan SN, Lewis NJW, Shimp LA, et al. Exploring patient experiences with prescription medicines to identify unmet patient needs: implications for research and practice. Res Social Adm Pharm 2012;8:321–332.
8. Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health, and behavior: a perceptual-cognitive approach. Psychol Health 1998;13:717–33.
9. Chen S-L, Tsai J-C, Chou K-R. Illness perceptions and adherence to therapeutic regimens among patients with hypertension: A structural model approach. Int J Nurs Stud 2011;48:235–45.
10. Chen S-L, Tsai J-C, Lee W-L. The impact of illness perception on adherence to therapeutic regimens of patients with hypertension in Taiwan. J Clin Nurs 2009;18:2234–44.
11. Jessop DC, Rutter DR. Adherence to asthma medication: the role of illness representations. Psychol Health 2003;18:595–612.
12. Ross S, Walker A, MacLeod M. Patient compliance in hypertension:role of illness perceptions and treatment beliefs. J Hum Hypertension 2004;18:607–13.
13 Searle A, Norman P. Thompson R. Vedhara K. A prospective examination of illness belies and coping in patients with type 2 diabetes. Br J Health Psychol 2007;12:621–38.
14. Zugelj U, Zuparnicic M, Komidar L, et al. Self-reported adherence behavior in adolescent hypertensive patients: the role of illness representation and personality. J Pediatr Psychol 2010;35:1049–60.
15. Horne R, Weinman J. Self-regulation and self-management in asthma: exploring the role of illness perception and treatment beliefs in explaining non-adherence to preventer medication. Psychol Health 2002;17:17–32.
16. Northouse LL, Northouse PG. Health communication: strategies for health professionals. Stamford: Prentice Hall; 1998.
Patients, Persistence, and Partnership: Creating and Sustaining Patient and Family Advisory Councils in a Hospital Setting
From the Center for Patients and Families (Dr. Fagan, Ms. Wong, Ms. Morrison, Ms. Carnie), and the Division of Women’s Health and Gender Biology (Dr. Lewis-O’Connor), Brigham and Women’s Hospital, Boston, MA.
Abstract
- Objective: To describe and illustrate the phases of creating, recruiting, launching, and sustaining a successful Patient and Family Advisory Council (PFAC) in a hospital setting.
- Method: Descriptive report.
- Results: There are 4 stages in creating and establishing a PFAC: council preparation, patient/family advisor recruitment, council launch, and sustaining an established council. Each stage poses challenges that need to be addressed in order to progress to the next stage. The ability for hospital leadership to authentically partner with patient and family advisors is key to maintaining and sustaining PFACs.
- Conclusion: The success of a PFAC is based on leadership support, advisors’ commitment to their PFAC, and the ability to sustain the council. PFACs can promote patient- and family-centered care and shift the model of care from a prescribed model to one that embraces partnerships with patients while advancing care delivery. As patient- and family-centered care advances, it is important that best practices and resources for building and sustaining PFACs are developed and made available to ensure all hospitals have access to this valuable resource.
Throughout the country, families, patients, and health care professionals are working together in new ways, including within patient and family advisory councils (PFACs). First established in the 1990s, PFACs became widespread after patient-centeredness was identified by the Institute of Medicine as one of the 6 aims of quality health care [1]. PFACs were created to institutionalize a partnership between hospital leadership, clinicians, patients, and families to improve care delivery. Through this partnership, PFACs facilitate the sharing of patient perspectives and input on hospital policies and programs; serve as a resource to providers; and promote relationships between staff, patients, and family members [2]. PFACs also play an important role in promoting patient- and family-centered care, ensuring that patient needs and values are at the center of the care delivery system.
The BWH Center for Patients and Families includes the executive director, a project manager, and a senior patient advisor, who together oversee the PFACs. The project manager provides logistical support and is available as concerns arise, working closely with the senior patient advisor to ensure patient/family advisors are acclimated to their role and all PFACs run smoothly. The senior patient advisor is a volunteer advisor and patient advocate with long term experience creating and sustaining PFACs and mentoring patient/family advisors. Her role as a mentor includes attending PFAC meetings to model skills and behaviors for other advisors and working with them to ensure they are comfortable in their PFAC. Her advocacy work includes listening to and helping to articulate lived patient/family experiences as compelling narratives, which can be shared with hospital leadership and used as exemplars to spur change. Together, the team recruits and trains patient/family advisors, support all phases of PFAC development, and represent the patient/family voice within the hospital.
In this article, we describe and illustrate the 4 stages of creating and sustaining a successful PFAC to provide guidance and lessons learned to organizations seeking to develop this valuable resource. These stages are: (1) council preparation, (2) patient/family advisor recruitment, (3) council launch, and (4) sustaining an established council.
Council Preparation
Preparation of the PFAC occurs once hospital or service line leadership has identified a need for and is committed to having a PFAC. Leadership contacts the executive director of the Center for Patients and Families to discuss the strategy and vision of the council. The executive director describes the attributes sought in an advisor and the core principles of patient- and family-centered care. This discussion includes recruitment methods, meeting logistics, and who will serve as council chair. The council chair should be in a leadership role and willing to champion the PFAC for their service line. The executive director discusses what is being planned with relevant clinicians and staff at a staff meeting in order to foster buy-in and involve them in the council recruitment process.
The BWH Center for Patients and Families has adapted Institute for Patient- and Family-Centered Care recommendations for PFAC logistics and structure [3]. Councils generally meet monthly for 90 minutes excluding August and December. As volunteers, our advisors receive no monetary compensation but receive complimentary parking and are often provided meals. Advisors are asked to commit to a 3-year term with the understanding that personal issues can arise and their commitment may change; after their term, they are welcome to continue. We recommend to leadership that PFACs be comprised of no more than 1 staff member to every 4 advisors. This ratio seeks to address any potential power imbalance and promotes a feeling of ownership of their council . The project manager works with leadership in creating council guidelines, including the council’s goals, expectations, and each member’s role.
Patient/Family Advisor Recruitment
We ask service line providers and staff to nominate patients and family members they believe would be suitable advisors. The attributes we look for in an advisor include their ability to: (1) share personal experiences in ways that professional and support staff can learn from, (2) see the big picture of a challenge or scenario and give advice using the lens of the patient or family member, (3) be interested in more than one agenda item, (4) speak to multiple operational topics, (5) listen to other points of view and be empathetic, (6) connect with other advisors and staff, and (7) have a good sense of humor. Candidates with both positive and negative experiences are sought so that we can learn and improve from their experience [2].
To find advisors with these attributes, we ask providers to review their schedule and think about who they look forward to seeing or connect with on a personal level. This method has proven successful at producing candidates that have the attributes we seek. It is vital that the patients we recruit are able to see past their own personal experiences to understand broader objectives and how they fit into the bigger picture, enabling them to participate in a variety of projects and committees. There are no educational or specific skill requirements to become an advisor; the only requirement is that candidates must have experience as a patient or caregiver (family member) of a patient at BWH.
Recommended patients receive a letter notifying them that they have been nominated to be an advisor on a PFAC by their treating clinician. The project manager contacts potential advisors to see if they are interested and provides a brief description of PFACs and the role of patient/family advisors. The project manager emphasizes the importance of patient/family input to the hospital, describing the opportunities patient/family advisors have to contribute their expertise as a patient or caregiver to decisions and projects that will positively affect future patient care. Examples of past successful PFAC projects are shared to give a sense of the importance of the advisor role within the hospital and the appreciation hospital leadership has for PFAC contributions. The project manager reiterates that their clinician nominated them to the council to encourage the candidate to feel that their voice deserves to be heard.
Interested candidates are interviewed by phone by the team. Each candidate is asked the same questions: (1) How long have you been a patient in the clinic or unit?; (2) Describe your experiences in this clinic/service; and (3) Describe what works well and what could be improved in your care. During the interview, we listen to their personal narrative and their perspective on their care, which allows us to assess whether they have the attributes of a successful patient/family advisor. Candidate’s narratives illustrate how they would share their concerns, contribute to solutions, and if they have the ability to see beyond their own personal agenda. We also listen carefully for themes of tolerance, operational insight, empathy, and problem-solving capabilities. Interviews take about 15–20 minutes, depending on how many follow-up questions we have for the candidate and if they have questions for us.
After the phone interview, the team determines whether the candidate would be an appropriate patient/family advisor. If there are any concerns and more information is needed, the project manager reaches out to the staff and contacts the candidate to invite them for an in-person interview. Of the interviewed candidates, about 75% to 80% are invited to join. Candidates who are not chosen are generally unable to clearly articulate issues they see within the hospital/clinic, may have personal relationships with the staff (ie, friends with the physician), or cannot see pass their own issues and are inflexible in their thinking. Those not chosen receive a note thanking them for their time and interest. The candidates chosen to be advisors are on boarded through BWH volunteer services and must attend a 3-hour BWH volunteer orientation, be HIPAA compliant, and be cleared by occupational health before receiving their advisor ID badge and beginning service.
Council Launch
Once the advisors have been recruited and oriented, the council enters the launching stage, which lasts from the council’s first meeting until the 1-year anniversary. The first meeting agenda is designed to introduce staff and advisors to each other. Advisors each share their health care narratives and the staff shares their motivations for participating in the council. The council chair reviews the purpose and goals of the council.
During the first year, the council gains experience working together as a team. Council projects are initially chosen by the council chair and should be reasonably simple to accomplish and meaningful to advisors so that advisors recognize that their feedback is being heard and acted on. Example projects include creating clearer directional sign-age, assessing recliners for patient rooms, and providing feedback on patient handouts to ensure patient friendliness.
As the council advances, projects can be initiated by the advisors. This process is facilitated when an advisor is added as council co-chair, which usually occurs at the end of the first year. Projects often arise from similar concerns shared by advisors during the recruitment interview process.
Sustaining an Established Council
A council is considered established when it enters its second year and has named a patient advisor as a co-chair. Established councils have undertaken projects such as improving the layout of the whiteboards in patient rooms and providing feedback to staff on how to manage challenging patients. In addition, established councils may be tapped when service lines without a PFAC seek to gather advisor feedback for a project. For example, one of our established councils has provided feedback on two patient safety research projects.
Councils are sustained by continually engaging advisors in projects that are of value to them, both in their department and hospital-wide. Advisors should be given the opportunity to prioritize and set new council goals. One of the overarching goals for all our PFACs is to improve communication between patients and staff. Councils at this stage often participate in grand rounds or attend staff meetings to share their narratives, enabling providers to understand their perspective. The council can also be engaged in grant-funded research initiatives. Having PFACs involved in various projects allows advisors to bring their narratives to a wider audience and be a part of change from numerous avenues within the hospital.
Patient and Family Advisory Councils in Practice
BWH has 16 PFACs in various stages of growth. To illustrate the variety in council structure and function, we describe 3 PFACs below. Each has unique composition and goals based on the needs of service line leadership.
Shapiro Cardiovascular PFAC
The Shapiro Cardiovascular Center, a LEED silver-certified building and with private patient rooms that welcome family members to stay with their loved ones [4], opened in 2008. The chief nursing officer felt the care provided in this new space should promote and embody PFCC. With the assistance of the Center for Patients and Families, the associate chief nursing officer was charged with creating the Shapiro Cardiovascular PFAC. Launched in May 2011, this PFAC provides input to improve the patient experience for inpatient and ambulatory care housed in the Shapiro Center.
The Shapiro PFAC originally consisted of medical/surgical cardiac and heart transplant patients; renal transplant recipients and donors later joined. Initially, this council worked on patient/visitor guidelines for the inpatient units. As the council became more experienced, advisors interviewed nursing director candidates for cardiac surgery ICU and organized two PFCC nursing grand rounds. These grand rounds featured a panel of Shapiro advisors sharing their perspective of their hospital care and reflections on their healing process. This council has also provided feedback on hospital-wide projects, such as the refinement of a nursing fall prevention tool and the development of patient-informed measures of a successful surgery. As advisors became more experienced, they were recruited by the executive director to be part of other committees and research projects.
The Shapiro PFAC is one of the oldest councils at BWH, consisting of 12 advisors and 3 staff members, with most of the inaugural advisors remaining. Because the council chair has changed twice since 2011, this council does not have a formal advisor co-chair but the council remains a cohesive team as they work in partnership with the newest chair. To sustain this PFAC, leadership has consistently engaged the council in operational projects. For example, the associate chief nursing officer has suggested advisors be part of unit-based councils composed of staff nurses and educators who work to improve patient care within their unit. Advisors have also been invited to participate in staff and nursing director meetings to share their narratives and allow staff to reflect on the care they provide patients.
LGBTQ PFAC
In the fall of 2014, BWH held an educational Lesbian, Gay, Bisexual, Transgender, and Queer (LGBTQ) patient experience forum prompted by a complaint from the wife of a maternity patient that the care they received was not patient/family-centered. During this panel discussion, 4 LGBTQ patients described their care at BWH, including what went well and what their providers could have done better. There was an acknowledgement by a majority of providers in the audience that they did not receive training on inclusive care for LGBTQ patients and their families. The providers identified the need to be educated on LGBTQ issues and care concerns, and their desire to work towards creating a warm and inclusive environment that better serves LGBTQ patients. This organic request for education was met with enthusiasm from the panel participants and led to a commitment to form an LGBTQ PFAC at BWH.
The LGBTQ PFAC is co-chaired by the executive director of the Center for Patients and Families and a LGBTQ patient advisor who receives his care at BWH. It was important for this council to be co-led by an advisor from the beginning to acknowledge and validate LGBTQ experiences of care which had previously been marginalized. Because LGBTQ patients interact with all service lines at BWH, it made sense that a central operational leader with significant experience listening and responding to the patient voice co-leads the group. This council is composed of LGBTQ patients, their caregivers/partners/spouses, BWH LGBTQ staff that also receive healthcare from BWH, and LGBTQ academic stakeholders who provide historical contextualization to inform change.
The LGBTQ PFAC began the preparation phase in April 2015 and launched as a hospital-wide council in October 2015. This launch was widely publicized so that all BWH employees would know this council was created to elevate LGBTQ patients and caregivers into the mainstream hospital consciousness. The goals for this year are to partner with the existing LGBTQ employee group to create a standardized LGBTQ provider directory, educate staff on the healthcare needs of the community, and promote educational awareness, compassionate understanding, and improved care for transgender patients. As this council matures into the established stage, new projects will be taken on in line with the needs seen by members.
Women’s Health Council
The Women’s Health Council is a unique PFAC established in 2012. The council serves a population of trauma survivors cared for by the Coordinated Approach to Recovery and Empowerment (C.A.R.E.) clinic at BWH, also founded in 2012. Patients who receive care in this clinic have experienced violence and trauma, including domestic and sexual violence, child maltreatment, and human trafficking. Due to previous experience leading a PFAC, the C.A.R.E. Director understood the importance of patient input and engaged patients as advisors while forming the clinic.
The C.A.R.E. clinic serves both men and women but the majority of survivors served are female; thus, the patient advisors on its PFAC are all female. To recruit advisors, clinicians, and social workers at the clinic refer potential candidates to the C.A.R.E. Director, who then interviews them. The criteria for advisors for this council include being a female survivor of violence and trauma, being physically and mentally able to serve, and able to participate in a way that does not re-traumatize them. There are currently 14 advisors on the council with a goal to grow to 30 advisors. Experience has shown that members become busy with family, school and careers and may need to step away for short periods of time; thus, the council seeks to continually recruit to ensure robust membership.
Instead of the usual monthly scheduled meetings, this council holds “meetings on demand.” Advisors are polled via email to find a time in the near future that works for the group. The PFAC generally uses a web conferencing platform for their meetings and has an in-person meeting once or twice a year. Also unlike other councils, this council does not require their advisors to share their personal narratives; it is up to each advisor to decide what to share.
This council has accomplished numerous goals since its inception, including its first task of giving the C.A.R.E. clinic its name. The council has provided feedback on the development of the C.A.R.E. brochure and website and serves as key informants in all aspects of policy and procedures for the C.A.R.E. clinic. Additionally, they have provided input on how to create a safe environment for patients and screen patients to identify a victim of violence or human trafficking [5]. This council has been sustained by the strong community fostered by the director and projects led by the advisors, as each advisor has a vested interest in ensuring the clinic provides a safe environment for patients seeking care. This year, the council is hoping to host experts from the Boston Health Commission to share best practices in providing services to victims of abuse and violence.
Lessons Learned
The BWH Center for Patients and Families has encountered challenges when creating and sustaining PFACs, such as recruiting advisors from diverse ethnic, cultural, and economic backgrounds. Currently, our advisor population is primarily comprised of Caucasian patient/family members from middle and upper economic backgrounds, though it has increasingly diversified as the program has grown. We believe the lack of representation from other backgrounds is due to scheduling difficulties, the lack of payment for advisors, visibility of the PFAC program, and, potentially, cultural norms that promote deference to medical expertise. We have worked to increase PFAC diversity by asking providers to specifically seek out and nominate patients that will broaden our reach as a council.
Retaining and recruiting advisors after the PFACs have launched can also present a challenge. Some advisors have had to resign due to job demands, relocation, health issues, or the need to take care of family. To resolve this issue, we have asked PFAC chairs to continuously actively recruit advisors. By doing so, the councils gain new perspectives and ensure there are adequate number of advisors should a vacancy occur.
Sustaining PFACs once they are established requires time, effort, and commitment of leadership, advisors, and dedicated staff resources. The council needs to be continuously engaged in meaningful projects and feel that their participation is impactful and creates change. It is important that clinical leadership stays actively involved and attends all PFAC meetings. If there is a change in leadership as we experienced on our Shapiro PFAC, it is critical that the interim chair participates and supports the goal of the council. Regardless, leadership must show sustained enthusiasm for PFAC engagement and achievement.
Employing technology can also help sustain councils. Although we prefer in-person meetings, the option to attend meetings through online or phone conferencing should be made available to support advisors who are unable to attend in person. At this time, only one of our councils uses web conferencing, while several of our councils offer an option to call in via a conference line. The conference line has been beneficial in helping us retain and engage advisors who travel a significant distance to attend meetings.
We recognize that BWH has many resources available due to its status as a large, academic medical center in an urban center. Nonetheless, PFACs can play a vital role in hospitals no matter the setting, location, or size as long as there is buy in from hospital leadership. Although BWH has 16 PFACs, it is not necessary to have this many councils. Having one PFAC may be sufficient for smaller hospitals; the ideal number of councils depends on the size and complexity of the institution. Hospitals without a dedicated department like the Center for Patients and Families can create PFACs by partnering with volunteer services, patient engagement, or quality and safety departments. Existing departments with the capability to train advisors and provide meeting resources to support patient/family recruitment and engagement should be harnessed whenever possible. It is, however, important to have a dedicated staff member to serve as a point person for the advisors should they have any questions or concerns. Technology, such as web conferencing described above, can facilitate attendance by patient/family advisors who have limited time or resources and will be valuable for hospitals in a rural setting. The stages we have described are critical to the success of creating and sustaining a PFAC regardless of where they are developed and can be adapted to fit the unique needs and environments of any healthcare setting.
Conclusion
BWH’s Center for Patients and Families has created 16 PFACs since 2008, which are in various stages of development. Our PFACs are successful for many reasons, including a rigorous recruitment and interview process, leadership support, advisors’ commitment to their PFAC, and making modifications made based on lessons learned, as illustrated by the 3 PFACs discussed. We are able to sustain our councils by continually engagingadvisors, having leadership partner with advisors, setting feasible goals, and recruiting new advisors for a fresh perspective. PFACs promote patient- and family-centered care and can shift the model of care from a prescribed model to one that embraces collaboration with patients while advancing care delivery. As patient- and family-centered care advances, it is important that best practices for building and sustaining PFACs are developed and made available to ensure all hospitals have access to this valuable resource.
Corresponding author: Celene Wong, MHA, Center for Patients and Families, Brigham and Women’s Hospital, 75 Francis St., Boston, MA 02115, [email protected].
Financial disclosures: None.
1. Institute of Medicine (US). Committee on Quality of Health Care in America. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. Accessed 6 Apr 2016 at www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf.
2. Institute for Patient- and Family-Centered Care. Institute for Patient- and Family-Centered Care creating patient and family advisory councils. Oct 2010. Accessed 10 Jan 2016 at www.ipfcc.org/advance/Advisory_Councils.pdf.
3. Institute for Patient- and Family-Centered Care. Institute for Patient- and Family-Centered Care core concepts. Dec 2010. Accessed 10 Jan 2016 at www.ipfcc.org/faq.html.
4. NBBJ. Caring to connect. 2016. Accessed 22 Feb 2016 at www.nbbj.com/work/brigham-and-womens-hospital-shapiro/.
5. Lewis-O’Connor A, Chadwick M. Engaging the voice of patients affected by gender-based violence: informing practice and policy. J Forensic Nurs 2015;11:240–9.
From the Center for Patients and Families (Dr. Fagan, Ms. Wong, Ms. Morrison, Ms. Carnie), and the Division of Women’s Health and Gender Biology (Dr. Lewis-O’Connor), Brigham and Women’s Hospital, Boston, MA.
Abstract
- Objective: To describe and illustrate the phases of creating, recruiting, launching, and sustaining a successful Patient and Family Advisory Council (PFAC) in a hospital setting.
- Method: Descriptive report.
- Results: There are 4 stages in creating and establishing a PFAC: council preparation, patient/family advisor recruitment, council launch, and sustaining an established council. Each stage poses challenges that need to be addressed in order to progress to the next stage. The ability for hospital leadership to authentically partner with patient and family advisors is key to maintaining and sustaining PFACs.
- Conclusion: The success of a PFAC is based on leadership support, advisors’ commitment to their PFAC, and the ability to sustain the council. PFACs can promote patient- and family-centered care and shift the model of care from a prescribed model to one that embraces partnerships with patients while advancing care delivery. As patient- and family-centered care advances, it is important that best practices and resources for building and sustaining PFACs are developed and made available to ensure all hospitals have access to this valuable resource.
Throughout the country, families, patients, and health care professionals are working together in new ways, including within patient and family advisory councils (PFACs). First established in the 1990s, PFACs became widespread after patient-centeredness was identified by the Institute of Medicine as one of the 6 aims of quality health care [1]. PFACs were created to institutionalize a partnership between hospital leadership, clinicians, patients, and families to improve care delivery. Through this partnership, PFACs facilitate the sharing of patient perspectives and input on hospital policies and programs; serve as a resource to providers; and promote relationships between staff, patients, and family members [2]. PFACs also play an important role in promoting patient- and family-centered care, ensuring that patient needs and values are at the center of the care delivery system.
The BWH Center for Patients and Families includes the executive director, a project manager, and a senior patient advisor, who together oversee the PFACs. The project manager provides logistical support and is available as concerns arise, working closely with the senior patient advisor to ensure patient/family advisors are acclimated to their role and all PFACs run smoothly. The senior patient advisor is a volunteer advisor and patient advocate with long term experience creating and sustaining PFACs and mentoring patient/family advisors. Her role as a mentor includes attending PFAC meetings to model skills and behaviors for other advisors and working with them to ensure they are comfortable in their PFAC. Her advocacy work includes listening to and helping to articulate lived patient/family experiences as compelling narratives, which can be shared with hospital leadership and used as exemplars to spur change. Together, the team recruits and trains patient/family advisors, support all phases of PFAC development, and represent the patient/family voice within the hospital.
In this article, we describe and illustrate the 4 stages of creating and sustaining a successful PFAC to provide guidance and lessons learned to organizations seeking to develop this valuable resource. These stages are: (1) council preparation, (2) patient/family advisor recruitment, (3) council launch, and (4) sustaining an established council.
Council Preparation
Preparation of the PFAC occurs once hospital or service line leadership has identified a need for and is committed to having a PFAC. Leadership contacts the executive director of the Center for Patients and Families to discuss the strategy and vision of the council. The executive director describes the attributes sought in an advisor and the core principles of patient- and family-centered care. This discussion includes recruitment methods, meeting logistics, and who will serve as council chair. The council chair should be in a leadership role and willing to champion the PFAC for their service line. The executive director discusses what is being planned with relevant clinicians and staff at a staff meeting in order to foster buy-in and involve them in the council recruitment process.
The BWH Center for Patients and Families has adapted Institute for Patient- and Family-Centered Care recommendations for PFAC logistics and structure [3]. Councils generally meet monthly for 90 minutes excluding August and December. As volunteers, our advisors receive no monetary compensation but receive complimentary parking and are often provided meals. Advisors are asked to commit to a 3-year term with the understanding that personal issues can arise and their commitment may change; after their term, they are welcome to continue. We recommend to leadership that PFACs be comprised of no more than 1 staff member to every 4 advisors. This ratio seeks to address any potential power imbalance and promotes a feeling of ownership of their council . The project manager works with leadership in creating council guidelines, including the council’s goals, expectations, and each member’s role.
Patient/Family Advisor Recruitment
We ask service line providers and staff to nominate patients and family members they believe would be suitable advisors. The attributes we look for in an advisor include their ability to: (1) share personal experiences in ways that professional and support staff can learn from, (2) see the big picture of a challenge or scenario and give advice using the lens of the patient or family member, (3) be interested in more than one agenda item, (4) speak to multiple operational topics, (5) listen to other points of view and be empathetic, (6) connect with other advisors and staff, and (7) have a good sense of humor. Candidates with both positive and negative experiences are sought so that we can learn and improve from their experience [2].
To find advisors with these attributes, we ask providers to review their schedule and think about who they look forward to seeing or connect with on a personal level. This method has proven successful at producing candidates that have the attributes we seek. It is vital that the patients we recruit are able to see past their own personal experiences to understand broader objectives and how they fit into the bigger picture, enabling them to participate in a variety of projects and committees. There are no educational or specific skill requirements to become an advisor; the only requirement is that candidates must have experience as a patient or caregiver (family member) of a patient at BWH.
Recommended patients receive a letter notifying them that they have been nominated to be an advisor on a PFAC by their treating clinician. The project manager contacts potential advisors to see if they are interested and provides a brief description of PFACs and the role of patient/family advisors. The project manager emphasizes the importance of patient/family input to the hospital, describing the opportunities patient/family advisors have to contribute their expertise as a patient or caregiver to decisions and projects that will positively affect future patient care. Examples of past successful PFAC projects are shared to give a sense of the importance of the advisor role within the hospital and the appreciation hospital leadership has for PFAC contributions. The project manager reiterates that their clinician nominated them to the council to encourage the candidate to feel that their voice deserves to be heard.
Interested candidates are interviewed by phone by the team. Each candidate is asked the same questions: (1) How long have you been a patient in the clinic or unit?; (2) Describe your experiences in this clinic/service; and (3) Describe what works well and what could be improved in your care. During the interview, we listen to their personal narrative and their perspective on their care, which allows us to assess whether they have the attributes of a successful patient/family advisor. Candidate’s narratives illustrate how they would share their concerns, contribute to solutions, and if they have the ability to see beyond their own personal agenda. We also listen carefully for themes of tolerance, operational insight, empathy, and problem-solving capabilities. Interviews take about 15–20 minutes, depending on how many follow-up questions we have for the candidate and if they have questions for us.
After the phone interview, the team determines whether the candidate would be an appropriate patient/family advisor. If there are any concerns and more information is needed, the project manager reaches out to the staff and contacts the candidate to invite them for an in-person interview. Of the interviewed candidates, about 75% to 80% are invited to join. Candidates who are not chosen are generally unable to clearly articulate issues they see within the hospital/clinic, may have personal relationships with the staff (ie, friends with the physician), or cannot see pass their own issues and are inflexible in their thinking. Those not chosen receive a note thanking them for their time and interest. The candidates chosen to be advisors are on boarded through BWH volunteer services and must attend a 3-hour BWH volunteer orientation, be HIPAA compliant, and be cleared by occupational health before receiving their advisor ID badge and beginning service.
Council Launch
Once the advisors have been recruited and oriented, the council enters the launching stage, which lasts from the council’s first meeting until the 1-year anniversary. The first meeting agenda is designed to introduce staff and advisors to each other. Advisors each share their health care narratives and the staff shares their motivations for participating in the council. The council chair reviews the purpose and goals of the council.
During the first year, the council gains experience working together as a team. Council projects are initially chosen by the council chair and should be reasonably simple to accomplish and meaningful to advisors so that advisors recognize that their feedback is being heard and acted on. Example projects include creating clearer directional sign-age, assessing recliners for patient rooms, and providing feedback on patient handouts to ensure patient friendliness.
As the council advances, projects can be initiated by the advisors. This process is facilitated when an advisor is added as council co-chair, which usually occurs at the end of the first year. Projects often arise from similar concerns shared by advisors during the recruitment interview process.
Sustaining an Established Council
A council is considered established when it enters its second year and has named a patient advisor as a co-chair. Established councils have undertaken projects such as improving the layout of the whiteboards in patient rooms and providing feedback to staff on how to manage challenging patients. In addition, established councils may be tapped when service lines without a PFAC seek to gather advisor feedback for a project. For example, one of our established councils has provided feedback on two patient safety research projects.
Councils are sustained by continually engaging advisors in projects that are of value to them, both in their department and hospital-wide. Advisors should be given the opportunity to prioritize and set new council goals. One of the overarching goals for all our PFACs is to improve communication between patients and staff. Councils at this stage often participate in grand rounds or attend staff meetings to share their narratives, enabling providers to understand their perspective. The council can also be engaged in grant-funded research initiatives. Having PFACs involved in various projects allows advisors to bring their narratives to a wider audience and be a part of change from numerous avenues within the hospital.
Patient and Family Advisory Councils in Practice
BWH has 16 PFACs in various stages of growth. To illustrate the variety in council structure and function, we describe 3 PFACs below. Each has unique composition and goals based on the needs of service line leadership.
Shapiro Cardiovascular PFAC
The Shapiro Cardiovascular Center, a LEED silver-certified building and with private patient rooms that welcome family members to stay with their loved ones [4], opened in 2008. The chief nursing officer felt the care provided in this new space should promote and embody PFCC. With the assistance of the Center for Patients and Families, the associate chief nursing officer was charged with creating the Shapiro Cardiovascular PFAC. Launched in May 2011, this PFAC provides input to improve the patient experience for inpatient and ambulatory care housed in the Shapiro Center.
The Shapiro PFAC originally consisted of medical/surgical cardiac and heart transplant patients; renal transplant recipients and donors later joined. Initially, this council worked on patient/visitor guidelines for the inpatient units. As the council became more experienced, advisors interviewed nursing director candidates for cardiac surgery ICU and organized two PFCC nursing grand rounds. These grand rounds featured a panel of Shapiro advisors sharing their perspective of their hospital care and reflections on their healing process. This council has also provided feedback on hospital-wide projects, such as the refinement of a nursing fall prevention tool and the development of patient-informed measures of a successful surgery. As advisors became more experienced, they were recruited by the executive director to be part of other committees and research projects.
The Shapiro PFAC is one of the oldest councils at BWH, consisting of 12 advisors and 3 staff members, with most of the inaugural advisors remaining. Because the council chair has changed twice since 2011, this council does not have a formal advisor co-chair but the council remains a cohesive team as they work in partnership with the newest chair. To sustain this PFAC, leadership has consistently engaged the council in operational projects. For example, the associate chief nursing officer has suggested advisors be part of unit-based councils composed of staff nurses and educators who work to improve patient care within their unit. Advisors have also been invited to participate in staff and nursing director meetings to share their narratives and allow staff to reflect on the care they provide patients.
LGBTQ PFAC
In the fall of 2014, BWH held an educational Lesbian, Gay, Bisexual, Transgender, and Queer (LGBTQ) patient experience forum prompted by a complaint from the wife of a maternity patient that the care they received was not patient/family-centered. During this panel discussion, 4 LGBTQ patients described their care at BWH, including what went well and what their providers could have done better. There was an acknowledgement by a majority of providers in the audience that they did not receive training on inclusive care for LGBTQ patients and their families. The providers identified the need to be educated on LGBTQ issues and care concerns, and their desire to work towards creating a warm and inclusive environment that better serves LGBTQ patients. This organic request for education was met with enthusiasm from the panel participants and led to a commitment to form an LGBTQ PFAC at BWH.
The LGBTQ PFAC is co-chaired by the executive director of the Center for Patients and Families and a LGBTQ patient advisor who receives his care at BWH. It was important for this council to be co-led by an advisor from the beginning to acknowledge and validate LGBTQ experiences of care which had previously been marginalized. Because LGBTQ patients interact with all service lines at BWH, it made sense that a central operational leader with significant experience listening and responding to the patient voice co-leads the group. This council is composed of LGBTQ patients, their caregivers/partners/spouses, BWH LGBTQ staff that also receive healthcare from BWH, and LGBTQ academic stakeholders who provide historical contextualization to inform change.
The LGBTQ PFAC began the preparation phase in April 2015 and launched as a hospital-wide council in October 2015. This launch was widely publicized so that all BWH employees would know this council was created to elevate LGBTQ patients and caregivers into the mainstream hospital consciousness. The goals for this year are to partner with the existing LGBTQ employee group to create a standardized LGBTQ provider directory, educate staff on the healthcare needs of the community, and promote educational awareness, compassionate understanding, and improved care for transgender patients. As this council matures into the established stage, new projects will be taken on in line with the needs seen by members.
Women’s Health Council
The Women’s Health Council is a unique PFAC established in 2012. The council serves a population of trauma survivors cared for by the Coordinated Approach to Recovery and Empowerment (C.A.R.E.) clinic at BWH, also founded in 2012. Patients who receive care in this clinic have experienced violence and trauma, including domestic and sexual violence, child maltreatment, and human trafficking. Due to previous experience leading a PFAC, the C.A.R.E. Director understood the importance of patient input and engaged patients as advisors while forming the clinic.
The C.A.R.E. clinic serves both men and women but the majority of survivors served are female; thus, the patient advisors on its PFAC are all female. To recruit advisors, clinicians, and social workers at the clinic refer potential candidates to the C.A.R.E. Director, who then interviews them. The criteria for advisors for this council include being a female survivor of violence and trauma, being physically and mentally able to serve, and able to participate in a way that does not re-traumatize them. There are currently 14 advisors on the council with a goal to grow to 30 advisors. Experience has shown that members become busy with family, school and careers and may need to step away for short periods of time; thus, the council seeks to continually recruit to ensure robust membership.
Instead of the usual monthly scheduled meetings, this council holds “meetings on demand.” Advisors are polled via email to find a time in the near future that works for the group. The PFAC generally uses a web conferencing platform for their meetings and has an in-person meeting once or twice a year. Also unlike other councils, this council does not require their advisors to share their personal narratives; it is up to each advisor to decide what to share.
This council has accomplished numerous goals since its inception, including its first task of giving the C.A.R.E. clinic its name. The council has provided feedback on the development of the C.A.R.E. brochure and website and serves as key informants in all aspects of policy and procedures for the C.A.R.E. clinic. Additionally, they have provided input on how to create a safe environment for patients and screen patients to identify a victim of violence or human trafficking [5]. This council has been sustained by the strong community fostered by the director and projects led by the advisors, as each advisor has a vested interest in ensuring the clinic provides a safe environment for patients seeking care. This year, the council is hoping to host experts from the Boston Health Commission to share best practices in providing services to victims of abuse and violence.
Lessons Learned
The BWH Center for Patients and Families has encountered challenges when creating and sustaining PFACs, such as recruiting advisors from diverse ethnic, cultural, and economic backgrounds. Currently, our advisor population is primarily comprised of Caucasian patient/family members from middle and upper economic backgrounds, though it has increasingly diversified as the program has grown. We believe the lack of representation from other backgrounds is due to scheduling difficulties, the lack of payment for advisors, visibility of the PFAC program, and, potentially, cultural norms that promote deference to medical expertise. We have worked to increase PFAC diversity by asking providers to specifically seek out and nominate patients that will broaden our reach as a council.
Retaining and recruiting advisors after the PFACs have launched can also present a challenge. Some advisors have had to resign due to job demands, relocation, health issues, or the need to take care of family. To resolve this issue, we have asked PFAC chairs to continuously actively recruit advisors. By doing so, the councils gain new perspectives and ensure there are adequate number of advisors should a vacancy occur.
Sustaining PFACs once they are established requires time, effort, and commitment of leadership, advisors, and dedicated staff resources. The council needs to be continuously engaged in meaningful projects and feel that their participation is impactful and creates change. It is important that clinical leadership stays actively involved and attends all PFAC meetings. If there is a change in leadership as we experienced on our Shapiro PFAC, it is critical that the interim chair participates and supports the goal of the council. Regardless, leadership must show sustained enthusiasm for PFAC engagement and achievement.
Employing technology can also help sustain councils. Although we prefer in-person meetings, the option to attend meetings through online or phone conferencing should be made available to support advisors who are unable to attend in person. At this time, only one of our councils uses web conferencing, while several of our councils offer an option to call in via a conference line. The conference line has been beneficial in helping us retain and engage advisors who travel a significant distance to attend meetings.
We recognize that BWH has many resources available due to its status as a large, academic medical center in an urban center. Nonetheless, PFACs can play a vital role in hospitals no matter the setting, location, or size as long as there is buy in from hospital leadership. Although BWH has 16 PFACs, it is not necessary to have this many councils. Having one PFAC may be sufficient for smaller hospitals; the ideal number of councils depends on the size and complexity of the institution. Hospitals without a dedicated department like the Center for Patients and Families can create PFACs by partnering with volunteer services, patient engagement, or quality and safety departments. Existing departments with the capability to train advisors and provide meeting resources to support patient/family recruitment and engagement should be harnessed whenever possible. It is, however, important to have a dedicated staff member to serve as a point person for the advisors should they have any questions or concerns. Technology, such as web conferencing described above, can facilitate attendance by patient/family advisors who have limited time or resources and will be valuable for hospitals in a rural setting. The stages we have described are critical to the success of creating and sustaining a PFAC regardless of where they are developed and can be adapted to fit the unique needs and environments of any healthcare setting.
Conclusion
BWH’s Center for Patients and Families has created 16 PFACs since 2008, which are in various stages of development. Our PFACs are successful for many reasons, including a rigorous recruitment and interview process, leadership support, advisors’ commitment to their PFAC, and making modifications made based on lessons learned, as illustrated by the 3 PFACs discussed. We are able to sustain our councils by continually engagingadvisors, having leadership partner with advisors, setting feasible goals, and recruiting new advisors for a fresh perspective. PFACs promote patient- and family-centered care and can shift the model of care from a prescribed model to one that embraces collaboration with patients while advancing care delivery. As patient- and family-centered care advances, it is important that best practices for building and sustaining PFACs are developed and made available to ensure all hospitals have access to this valuable resource.
Corresponding author: Celene Wong, MHA, Center for Patients and Families, Brigham and Women’s Hospital, 75 Francis St., Boston, MA 02115, [email protected].
Financial disclosures: None.
From the Center for Patients and Families (Dr. Fagan, Ms. Wong, Ms. Morrison, Ms. Carnie), and the Division of Women’s Health and Gender Biology (Dr. Lewis-O’Connor), Brigham and Women’s Hospital, Boston, MA.
Abstract
- Objective: To describe and illustrate the phases of creating, recruiting, launching, and sustaining a successful Patient and Family Advisory Council (PFAC) in a hospital setting.
- Method: Descriptive report.
- Results: There are 4 stages in creating and establishing a PFAC: council preparation, patient/family advisor recruitment, council launch, and sustaining an established council. Each stage poses challenges that need to be addressed in order to progress to the next stage. The ability for hospital leadership to authentically partner with patient and family advisors is key to maintaining and sustaining PFACs.
- Conclusion: The success of a PFAC is based on leadership support, advisors’ commitment to their PFAC, and the ability to sustain the council. PFACs can promote patient- and family-centered care and shift the model of care from a prescribed model to one that embraces partnerships with patients while advancing care delivery. As patient- and family-centered care advances, it is important that best practices and resources for building and sustaining PFACs are developed and made available to ensure all hospitals have access to this valuable resource.
Throughout the country, families, patients, and health care professionals are working together in new ways, including within patient and family advisory councils (PFACs). First established in the 1990s, PFACs became widespread after patient-centeredness was identified by the Institute of Medicine as one of the 6 aims of quality health care [1]. PFACs were created to institutionalize a partnership between hospital leadership, clinicians, patients, and families to improve care delivery. Through this partnership, PFACs facilitate the sharing of patient perspectives and input on hospital policies and programs; serve as a resource to providers; and promote relationships between staff, patients, and family members [2]. PFACs also play an important role in promoting patient- and family-centered care, ensuring that patient needs and values are at the center of the care delivery system.
The BWH Center for Patients and Families includes the executive director, a project manager, and a senior patient advisor, who together oversee the PFACs. The project manager provides logistical support and is available as concerns arise, working closely with the senior patient advisor to ensure patient/family advisors are acclimated to their role and all PFACs run smoothly. The senior patient advisor is a volunteer advisor and patient advocate with long term experience creating and sustaining PFACs and mentoring patient/family advisors. Her role as a mentor includes attending PFAC meetings to model skills and behaviors for other advisors and working with them to ensure they are comfortable in their PFAC. Her advocacy work includes listening to and helping to articulate lived patient/family experiences as compelling narratives, which can be shared with hospital leadership and used as exemplars to spur change. Together, the team recruits and trains patient/family advisors, support all phases of PFAC development, and represent the patient/family voice within the hospital.
In this article, we describe and illustrate the 4 stages of creating and sustaining a successful PFAC to provide guidance and lessons learned to organizations seeking to develop this valuable resource. These stages are: (1) council preparation, (2) patient/family advisor recruitment, (3) council launch, and (4) sustaining an established council.
Council Preparation
Preparation of the PFAC occurs once hospital or service line leadership has identified a need for and is committed to having a PFAC. Leadership contacts the executive director of the Center for Patients and Families to discuss the strategy and vision of the council. The executive director describes the attributes sought in an advisor and the core principles of patient- and family-centered care. This discussion includes recruitment methods, meeting logistics, and who will serve as council chair. The council chair should be in a leadership role and willing to champion the PFAC for their service line. The executive director discusses what is being planned with relevant clinicians and staff at a staff meeting in order to foster buy-in and involve them in the council recruitment process.
The BWH Center for Patients and Families has adapted Institute for Patient- and Family-Centered Care recommendations for PFAC logistics and structure [3]. Councils generally meet monthly for 90 minutes excluding August and December. As volunteers, our advisors receive no monetary compensation but receive complimentary parking and are often provided meals. Advisors are asked to commit to a 3-year term with the understanding that personal issues can arise and their commitment may change; after their term, they are welcome to continue. We recommend to leadership that PFACs be comprised of no more than 1 staff member to every 4 advisors. This ratio seeks to address any potential power imbalance and promotes a feeling of ownership of their council . The project manager works with leadership in creating council guidelines, including the council’s goals, expectations, and each member’s role.
Patient/Family Advisor Recruitment
We ask service line providers and staff to nominate patients and family members they believe would be suitable advisors. The attributes we look for in an advisor include their ability to: (1) share personal experiences in ways that professional and support staff can learn from, (2) see the big picture of a challenge or scenario and give advice using the lens of the patient or family member, (3) be interested in more than one agenda item, (4) speak to multiple operational topics, (5) listen to other points of view and be empathetic, (6) connect with other advisors and staff, and (7) have a good sense of humor. Candidates with both positive and negative experiences are sought so that we can learn and improve from their experience [2].
To find advisors with these attributes, we ask providers to review their schedule and think about who they look forward to seeing or connect with on a personal level. This method has proven successful at producing candidates that have the attributes we seek. It is vital that the patients we recruit are able to see past their own personal experiences to understand broader objectives and how they fit into the bigger picture, enabling them to participate in a variety of projects and committees. There are no educational or specific skill requirements to become an advisor; the only requirement is that candidates must have experience as a patient or caregiver (family member) of a patient at BWH.
Recommended patients receive a letter notifying them that they have been nominated to be an advisor on a PFAC by their treating clinician. The project manager contacts potential advisors to see if they are interested and provides a brief description of PFACs and the role of patient/family advisors. The project manager emphasizes the importance of patient/family input to the hospital, describing the opportunities patient/family advisors have to contribute their expertise as a patient or caregiver to decisions and projects that will positively affect future patient care. Examples of past successful PFAC projects are shared to give a sense of the importance of the advisor role within the hospital and the appreciation hospital leadership has for PFAC contributions. The project manager reiterates that their clinician nominated them to the council to encourage the candidate to feel that their voice deserves to be heard.
Interested candidates are interviewed by phone by the team. Each candidate is asked the same questions: (1) How long have you been a patient in the clinic or unit?; (2) Describe your experiences in this clinic/service; and (3) Describe what works well and what could be improved in your care. During the interview, we listen to their personal narrative and their perspective on their care, which allows us to assess whether they have the attributes of a successful patient/family advisor. Candidate’s narratives illustrate how they would share their concerns, contribute to solutions, and if they have the ability to see beyond their own personal agenda. We also listen carefully for themes of tolerance, operational insight, empathy, and problem-solving capabilities. Interviews take about 15–20 minutes, depending on how many follow-up questions we have for the candidate and if they have questions for us.
After the phone interview, the team determines whether the candidate would be an appropriate patient/family advisor. If there are any concerns and more information is needed, the project manager reaches out to the staff and contacts the candidate to invite them for an in-person interview. Of the interviewed candidates, about 75% to 80% are invited to join. Candidates who are not chosen are generally unable to clearly articulate issues they see within the hospital/clinic, may have personal relationships with the staff (ie, friends with the physician), or cannot see pass their own issues and are inflexible in their thinking. Those not chosen receive a note thanking them for their time and interest. The candidates chosen to be advisors are on boarded through BWH volunteer services and must attend a 3-hour BWH volunteer orientation, be HIPAA compliant, and be cleared by occupational health before receiving their advisor ID badge and beginning service.
Council Launch
Once the advisors have been recruited and oriented, the council enters the launching stage, which lasts from the council’s first meeting until the 1-year anniversary. The first meeting agenda is designed to introduce staff and advisors to each other. Advisors each share their health care narratives and the staff shares their motivations for participating in the council. The council chair reviews the purpose and goals of the council.
During the first year, the council gains experience working together as a team. Council projects are initially chosen by the council chair and should be reasonably simple to accomplish and meaningful to advisors so that advisors recognize that their feedback is being heard and acted on. Example projects include creating clearer directional sign-age, assessing recliners for patient rooms, and providing feedback on patient handouts to ensure patient friendliness.
As the council advances, projects can be initiated by the advisors. This process is facilitated when an advisor is added as council co-chair, which usually occurs at the end of the first year. Projects often arise from similar concerns shared by advisors during the recruitment interview process.
Sustaining an Established Council
A council is considered established when it enters its second year and has named a patient advisor as a co-chair. Established councils have undertaken projects such as improving the layout of the whiteboards in patient rooms and providing feedback to staff on how to manage challenging patients. In addition, established councils may be tapped when service lines without a PFAC seek to gather advisor feedback for a project. For example, one of our established councils has provided feedback on two patient safety research projects.
Councils are sustained by continually engaging advisors in projects that are of value to them, both in their department and hospital-wide. Advisors should be given the opportunity to prioritize and set new council goals. One of the overarching goals for all our PFACs is to improve communication between patients and staff. Councils at this stage often participate in grand rounds or attend staff meetings to share their narratives, enabling providers to understand their perspective. The council can also be engaged in grant-funded research initiatives. Having PFACs involved in various projects allows advisors to bring their narratives to a wider audience and be a part of change from numerous avenues within the hospital.
Patient and Family Advisory Councils in Practice
BWH has 16 PFACs in various stages of growth. To illustrate the variety in council structure and function, we describe 3 PFACs below. Each has unique composition and goals based on the needs of service line leadership.
Shapiro Cardiovascular PFAC
The Shapiro Cardiovascular Center, a LEED silver-certified building and with private patient rooms that welcome family members to stay with their loved ones [4], opened in 2008. The chief nursing officer felt the care provided in this new space should promote and embody PFCC. With the assistance of the Center for Patients and Families, the associate chief nursing officer was charged with creating the Shapiro Cardiovascular PFAC. Launched in May 2011, this PFAC provides input to improve the patient experience for inpatient and ambulatory care housed in the Shapiro Center.
The Shapiro PFAC originally consisted of medical/surgical cardiac and heart transplant patients; renal transplant recipients and donors later joined. Initially, this council worked on patient/visitor guidelines for the inpatient units. As the council became more experienced, advisors interviewed nursing director candidates for cardiac surgery ICU and organized two PFCC nursing grand rounds. These grand rounds featured a panel of Shapiro advisors sharing their perspective of their hospital care and reflections on their healing process. This council has also provided feedback on hospital-wide projects, such as the refinement of a nursing fall prevention tool and the development of patient-informed measures of a successful surgery. As advisors became more experienced, they were recruited by the executive director to be part of other committees and research projects.
The Shapiro PFAC is one of the oldest councils at BWH, consisting of 12 advisors and 3 staff members, with most of the inaugural advisors remaining. Because the council chair has changed twice since 2011, this council does not have a formal advisor co-chair but the council remains a cohesive team as they work in partnership with the newest chair. To sustain this PFAC, leadership has consistently engaged the council in operational projects. For example, the associate chief nursing officer has suggested advisors be part of unit-based councils composed of staff nurses and educators who work to improve patient care within their unit. Advisors have also been invited to participate in staff and nursing director meetings to share their narratives and allow staff to reflect on the care they provide patients.
LGBTQ PFAC
In the fall of 2014, BWH held an educational Lesbian, Gay, Bisexual, Transgender, and Queer (LGBTQ) patient experience forum prompted by a complaint from the wife of a maternity patient that the care they received was not patient/family-centered. During this panel discussion, 4 LGBTQ patients described their care at BWH, including what went well and what their providers could have done better. There was an acknowledgement by a majority of providers in the audience that they did not receive training on inclusive care for LGBTQ patients and their families. The providers identified the need to be educated on LGBTQ issues and care concerns, and their desire to work towards creating a warm and inclusive environment that better serves LGBTQ patients. This organic request for education was met with enthusiasm from the panel participants and led to a commitment to form an LGBTQ PFAC at BWH.
The LGBTQ PFAC is co-chaired by the executive director of the Center for Patients and Families and a LGBTQ patient advisor who receives his care at BWH. It was important for this council to be co-led by an advisor from the beginning to acknowledge and validate LGBTQ experiences of care which had previously been marginalized. Because LGBTQ patients interact with all service lines at BWH, it made sense that a central operational leader with significant experience listening and responding to the patient voice co-leads the group. This council is composed of LGBTQ patients, their caregivers/partners/spouses, BWH LGBTQ staff that also receive healthcare from BWH, and LGBTQ academic stakeholders who provide historical contextualization to inform change.
The LGBTQ PFAC began the preparation phase in April 2015 and launched as a hospital-wide council in October 2015. This launch was widely publicized so that all BWH employees would know this council was created to elevate LGBTQ patients and caregivers into the mainstream hospital consciousness. The goals for this year are to partner with the existing LGBTQ employee group to create a standardized LGBTQ provider directory, educate staff on the healthcare needs of the community, and promote educational awareness, compassionate understanding, and improved care for transgender patients. As this council matures into the established stage, new projects will be taken on in line with the needs seen by members.
Women’s Health Council
The Women’s Health Council is a unique PFAC established in 2012. The council serves a population of trauma survivors cared for by the Coordinated Approach to Recovery and Empowerment (C.A.R.E.) clinic at BWH, also founded in 2012. Patients who receive care in this clinic have experienced violence and trauma, including domestic and sexual violence, child maltreatment, and human trafficking. Due to previous experience leading a PFAC, the C.A.R.E. Director understood the importance of patient input and engaged patients as advisors while forming the clinic.
The C.A.R.E. clinic serves both men and women but the majority of survivors served are female; thus, the patient advisors on its PFAC are all female. To recruit advisors, clinicians, and social workers at the clinic refer potential candidates to the C.A.R.E. Director, who then interviews them. The criteria for advisors for this council include being a female survivor of violence and trauma, being physically and mentally able to serve, and able to participate in a way that does not re-traumatize them. There are currently 14 advisors on the council with a goal to grow to 30 advisors. Experience has shown that members become busy with family, school and careers and may need to step away for short periods of time; thus, the council seeks to continually recruit to ensure robust membership.
Instead of the usual monthly scheduled meetings, this council holds “meetings on demand.” Advisors are polled via email to find a time in the near future that works for the group. The PFAC generally uses a web conferencing platform for their meetings and has an in-person meeting once or twice a year. Also unlike other councils, this council does not require their advisors to share their personal narratives; it is up to each advisor to decide what to share.
This council has accomplished numerous goals since its inception, including its first task of giving the C.A.R.E. clinic its name. The council has provided feedback on the development of the C.A.R.E. brochure and website and serves as key informants in all aspects of policy and procedures for the C.A.R.E. clinic. Additionally, they have provided input on how to create a safe environment for patients and screen patients to identify a victim of violence or human trafficking [5]. This council has been sustained by the strong community fostered by the director and projects led by the advisors, as each advisor has a vested interest in ensuring the clinic provides a safe environment for patients seeking care. This year, the council is hoping to host experts from the Boston Health Commission to share best practices in providing services to victims of abuse and violence.
Lessons Learned
The BWH Center for Patients and Families has encountered challenges when creating and sustaining PFACs, such as recruiting advisors from diverse ethnic, cultural, and economic backgrounds. Currently, our advisor population is primarily comprised of Caucasian patient/family members from middle and upper economic backgrounds, though it has increasingly diversified as the program has grown. We believe the lack of representation from other backgrounds is due to scheduling difficulties, the lack of payment for advisors, visibility of the PFAC program, and, potentially, cultural norms that promote deference to medical expertise. We have worked to increase PFAC diversity by asking providers to specifically seek out and nominate patients that will broaden our reach as a council.
Retaining and recruiting advisors after the PFACs have launched can also present a challenge. Some advisors have had to resign due to job demands, relocation, health issues, or the need to take care of family. To resolve this issue, we have asked PFAC chairs to continuously actively recruit advisors. By doing so, the councils gain new perspectives and ensure there are adequate number of advisors should a vacancy occur.
Sustaining PFACs once they are established requires time, effort, and commitment of leadership, advisors, and dedicated staff resources. The council needs to be continuously engaged in meaningful projects and feel that their participation is impactful and creates change. It is important that clinical leadership stays actively involved and attends all PFAC meetings. If there is a change in leadership as we experienced on our Shapiro PFAC, it is critical that the interim chair participates and supports the goal of the council. Regardless, leadership must show sustained enthusiasm for PFAC engagement and achievement.
Employing technology can also help sustain councils. Although we prefer in-person meetings, the option to attend meetings through online or phone conferencing should be made available to support advisors who are unable to attend in person. At this time, only one of our councils uses web conferencing, while several of our councils offer an option to call in via a conference line. The conference line has been beneficial in helping us retain and engage advisors who travel a significant distance to attend meetings.
We recognize that BWH has many resources available due to its status as a large, academic medical center in an urban center. Nonetheless, PFACs can play a vital role in hospitals no matter the setting, location, or size as long as there is buy in from hospital leadership. Although BWH has 16 PFACs, it is not necessary to have this many councils. Having one PFAC may be sufficient for smaller hospitals; the ideal number of councils depends on the size and complexity of the institution. Hospitals without a dedicated department like the Center for Patients and Families can create PFACs by partnering with volunteer services, patient engagement, or quality and safety departments. Existing departments with the capability to train advisors and provide meeting resources to support patient/family recruitment and engagement should be harnessed whenever possible. It is, however, important to have a dedicated staff member to serve as a point person for the advisors should they have any questions or concerns. Technology, such as web conferencing described above, can facilitate attendance by patient/family advisors who have limited time or resources and will be valuable for hospitals in a rural setting. The stages we have described are critical to the success of creating and sustaining a PFAC regardless of where they are developed and can be adapted to fit the unique needs and environments of any healthcare setting.
Conclusion
BWH’s Center for Patients and Families has created 16 PFACs since 2008, which are in various stages of development. Our PFACs are successful for many reasons, including a rigorous recruitment and interview process, leadership support, advisors’ commitment to their PFAC, and making modifications made based on lessons learned, as illustrated by the 3 PFACs discussed. We are able to sustain our councils by continually engagingadvisors, having leadership partner with advisors, setting feasible goals, and recruiting new advisors for a fresh perspective. PFACs promote patient- and family-centered care and can shift the model of care from a prescribed model to one that embraces collaboration with patients while advancing care delivery. As patient- and family-centered care advances, it is important that best practices for building and sustaining PFACs are developed and made available to ensure all hospitals have access to this valuable resource.
Corresponding author: Celene Wong, MHA, Center for Patients and Families, Brigham and Women’s Hospital, 75 Francis St., Boston, MA 02115, [email protected].
Financial disclosures: None.
1. Institute of Medicine (US). Committee on Quality of Health Care in America. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. Accessed 6 Apr 2016 at www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf.
2. Institute for Patient- and Family-Centered Care. Institute for Patient- and Family-Centered Care creating patient and family advisory councils. Oct 2010. Accessed 10 Jan 2016 at www.ipfcc.org/advance/Advisory_Councils.pdf.
3. Institute for Patient- and Family-Centered Care. Institute for Patient- and Family-Centered Care core concepts. Dec 2010. Accessed 10 Jan 2016 at www.ipfcc.org/faq.html.
4. NBBJ. Caring to connect. 2016. Accessed 22 Feb 2016 at www.nbbj.com/work/brigham-and-womens-hospital-shapiro/.
5. Lewis-O’Connor A, Chadwick M. Engaging the voice of patients affected by gender-based violence: informing practice and policy. J Forensic Nurs 2015;11:240–9.
1. Institute of Medicine (US). Committee on Quality of Health Care in America. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. Accessed 6 Apr 2016 at www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf.
2. Institute for Patient- and Family-Centered Care. Institute for Patient- and Family-Centered Care creating patient and family advisory councils. Oct 2010. Accessed 10 Jan 2016 at www.ipfcc.org/advance/Advisory_Councils.pdf.
3. Institute for Patient- and Family-Centered Care. Institute for Patient- and Family-Centered Care core concepts. Dec 2010. Accessed 10 Jan 2016 at www.ipfcc.org/faq.html.
4. NBBJ. Caring to connect. 2016. Accessed 22 Feb 2016 at www.nbbj.com/work/brigham-and-womens-hospital-shapiro/.
5. Lewis-O’Connor A, Chadwick M. Engaging the voice of patients affected by gender-based violence: informing practice and policy. J Forensic Nurs 2015;11:240–9.
Pharmacists’ Involvement in Medication Management Along the Continuum of Care: Challenges, Lessons Learned, and Implications for Health Systems
From The Johns Hopkins Hospital, Baltimore, MD.
The project described was supported by grant # 1C1CMS331053-01-00 from the U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. The research presented was conducted by the awardee. Findings may or may not be consistent with or confirmed by the findings of the independent evaluation contractor.
Abstract
- Background: Medication management is becoming more complex, with new medications entering the market, drug prices increasing, and patients transferring into and out of the hospital. Transitions of care services are being implemented to prevent readmissions and increase patient satisfaction. Pharmacists play a key role by expanding clinical services provided to patients around medication management.
- Objective: To describe a pharmacy transitions of care model at a large academic teaching hospital and lessons learned during implementation.
- Methods: A pharmacy bundle of services was initially developed in a medical patient population and included medication reconciliation, patient education targeting high-risk medications, post-discharge follow-up phone calls, and bedside discharge prescription delivery. This bundle was expanded to other patient populations through the use of residency-trained pharmacists, pharmacy residents, pharmacy students, and certified pharmacy technicians.
- Results: Challenges were faced when implementing our transitions of care services, including expanding care coordination team coverage with existing resources, training pharmacy staff in new roles, determining the needs of patients cared for by teams we had not previously been integrated into, and creating our discharge prescription delivery program. During this process, we learned to rethink the role of pharmacists on our team, value the support within our institution to create change in order to improve patient care, and continuously evaluate this process.
- Conclusion: We are at an opportune time to expand the scope of the inpatient pharmacist to provide advanced medication-related services to patients. Residency training is creating individuals who will thrive in these new models.
Medication management around the acute care inpatient stay is a challenging but crucial task to ensure patient safety and desired clinical outcomes. The first step in successful medication management is to understand the patient’s medication regimen in the home environment. Patients may take medications differently than prescribed; skip medication doses intentionally to make a supply last longer; use over-the-counter medications, herbal supplements, or someone else’s medication based on the recommendation of family or friends; or discontinue medications based on side effects or media influence. Over the course of the inpatient stay, medication management involves adjusting doses based on changes in organ function, detecting side effects and potential drug interactions, and monitoring clinical outcomes to ensure appropriate drug therapy is being prescribed. As the patient approaches discharge, ensuring the patient understands the indications for his/her medications, has self-monitoring techniques to recognize efficacy or adverse effects, and has access to discharge medications is important. Lastly, long-term medication management includes patient access to pharmaceutical expertise over time. Pharmacists’ involvement in medication therapy management services and patient-centered medical homes is key to ensuring safe and effective medication use over time.
In 2009, the Johns Hopkins Health System Readmission Prevention Task Force developed strategies to reduce preventable readmissions and improve transitions of care. In 2011, a new multidisciplinary approach to patient care was implemented at the Johns Hopkins Hospital (JHH) to optimize care coordination and improve acute care management. Using this approach, care coordination teams composed of physicians, nurses, pharmacists, nurse case managers, social workers, physical/occupational therapists, nutritionists, and home care coordinators meet on a daily basis to discuss the inpatient and discharge care needs of patients in order to improve care transitions and reduce preventable readmissions. In 2012, JHH was awarded a 3-year innovation grant from the Centers for Medicaid & Medicare Services (CMS) that would assist with expansion of these care coordination teams to every unit of the hospital. Prior to implementation of the care coordination model at JHH in 2011, there were 3 pharmacists who consistently rounded on 3 inpatient medicine teams (one pharmacist also had operational responsibilities). Pharmacists were deemed by the task force to be key providers of medication management and, thus, essential members of the care coordination team. Due to an inability to hire a new pharmacist for every care coordination team, the department of pharmacy needed to determine how to provide consistent pharmacist coverage utilizing current resources. This report describes the challenges faced and lessons learned by our adult inpatient pharmacy division when implementing a pharmacy bundle of services to improve care transitions for an adult patient population.
Setting
JHH is an 1192-bed academic teaching hospital located in Baltimore, Maryland. At JHH, the department of pharmacy has 4 inpatient divisions that service the medication needs of different patient populations: medicine, critical care/surgery, oncology, and pediatrics. The adultinpatient pharmacy division covers medicine units in addition to obstetrics, neurology, and surgery units. It is responsible for 486 inpatient beds on 22 units and was the first division to provide the pharmacy bundle of services described below. Currently, 11 rounding and 5 operational pharmacists provide care coordination and order verification support, respectively, for the division during day shift.
Program Overview
Rounding pharmacists on care coordination teams address acute care medication issues and provide a bundle of services that includes targeted patient education, medication reconciliation, post-discharge follow-up phone calls, and discharge prescription planning. The full details of these services have been described [1]. Briefly, patients newly initiated on medications deemed ”high-risk” (eg, anticoagulation, insulin, metered dose inhalers, dual antiplatelets) receive education by a member of the pharmacy team (ie, pharmacist, pharmacy resident, or pharmacy student) prior to discharge. Those patients who receive education are offered a post-discharge follow-up phone call to assess for any questions or issues. Patients who accept this service are contacted 48 to 72 hours post-discharge. Specific patient populations (eg, patients with congestive heart failure, diabetes) are also targeted for completion of medication reconciliation. If patients are being discharged with prescriptions, they are offered our “Meds for Home” service. Patients who accept this service have their prescriptions filled at one of our outpatient pharmacies and delivered to the unit prior to discharge. Highly trained certified pharmacy technicians, called “Meds for Home” coordinators (MHCs; previously known as transitions pharmacist extenders), facilitate this process.
Challenges Faced
Care Coordination Team Coverage
One challenge to implementation of the pharmacy bundle of services was providing consistent team coverage with adequately trained pharmacists. It was not feasible to hire a pharmacist to cover each of the care coordination teams. To address gaps in coverage, we initially utilized postgraduate year 1 and 2 (PGY1 and 2) pharmacy residents on an internal medicine rotation to cover care coordination teams without a rounding pharmacist. However, this method proved unreliable as a pharmacy resident was not scheduled for an internal medicine rotation each month. In the beginning, our division had 3 rounding and 9 operational pharmacists during day shift. To provide sufficient clinical coverage while still adequately addressing order verification needs, a major restructuring of our pharmacy model was necessary. We increased the bed-to-pharmacist ratio for order verification, which allowed the number of operational pharmacists to decrease from 9 to 5. Those 4 remaining pharmacists were now available to serve as rounding pharmacists. Along with hiring 2 additional rounding pharmacists with funding from the CMS innovation grant, we were able to increase the number of care coordination teams consistently covered from 3 to 9.
Although we expanded pharmacist coverage of care coordination teams, time constraints prevented all patients who met criteria for patient education or medication reconciliation to have these services completed in a timely manner or at all by a pharmacist. Our rounding pharmacists’ responsibilities also included participation in high-level activities such as order set reviews for a new provider order entry system, ambulatory clinic time, stewardship activities, and quality improvement projects. In order to increase our scope, we utilized pharmacy technicians, students, and residents to assist with completing these tasks. All pharmacy students and residents on rotation within our division participated in a daily huddle Monday through Friday. Rounding pharmacists whose unit had patient education needs that could not be met by that pharmacist submitted requests by a set time. Those patient education tasks were then divided amongst the pharmacy learners at the huddle for completion. Prior to being allowed to independently counsel patients, pharmacy learners’ patient education skills were evaluated by preceptors. To facilitate timely completion of medication histories, technicians were hired. These medication history technicians are available Monday through Friday to complete medication histories for patients admitted to specific medicine units, ideally within 24 hours of admission. Rounding pharmacists are notified of completion of medication histories via our electronic medical record and reconcile that list with the patient’s inpatient medication list. Any clinically relevant discrepancies are communicated to providers. Pharmacy learners may also collect medication histories.
Training Rounding Pharmacists
Another challenge we faced was providing adequate training for operational pharmacists transitioning to a rounding position. Residency training is crucial in providing the level of skill necessary to identify complex drug therapy problems, adjust treatment regimens, and create plans where limited data exist to drive drug therapy recommendations [2,3]. Rotations during the final year of pharmacy school provide exposure to interacting with patients and providers. Completion of PGY1 residency training allows a pharmacist to practice as a generalist with a broad range of experiences provided during the year to identify medication-related problems. PGY2 residency training allows the pharmacist to spend a concentrated year in the chosen area of expertise and gain a deeper knowledge of medication use in a specific patient population or area of practice [2]. After 2 years of clinical residency training, pharmacists have the skills to interact with patients and multidisciplinary teams to optimize medication regimens, provide medication education, and measure the value they bring to the health care of patients.
Some of the operational pharmacists who were transitioning to the rounding pharmacist role had no training beyond pharmacy school or had only completed a PGY1 pharmacy residency. Initially, training for this new role lasted only a few days and consisted of orientation to the unit and observation of care coordination rounds. We learned that this brief amount of training was insufficient, even for those with PGY1 pharmacy residency training. In order to ensure that these rounding pharmacists could successfully provide the bundle of services and meet the high clinical demands of the inpatient service, we developed a comprehensive training program. Those interested in transitioning from an operational to a rounding pharmacist role must now complete a 6-week training program. The first 2 weeks consists of improving patient education and medication history skills. The remaining 4 weeks are spent honing clinical rounding skills. Rounding pharmacists-in-training also receive a formal review of their performance utilizing an evaluation form developed by the American Society of Health-System Pharmacists (ASHP) for pharmacy residents.
Establishing a Pharmacy Bundle and the Role of a Rounding Pharmacist on New Units
Some of the units implementing care coordination teams, such as neurology, did not previously have a pharmacist rounding on those units. Furthermore, these units had a high patient census (eg, 60 patients), which made it difficult for one pharmacist to clinically evaluate every patient. Multiple specialty teams also admitted patients to a single unit, which made it challenging for the pharmacist to develop strong working relationships with providers. As such, rounding pharmacists deployed to those units had difficulty establishing their role on the team, especially for those pharmacists without or with only 1 year of postgraduate training. To address this issue, a PGY2-trained pharmacist rounded on the unit to assess which areas/teams had the greatest need for a pharmacist. Completing this needs assessment on these units allowed for the rounding pharmacist to more effectively use his/her time. It also allowed for a smoother transition from operational to rounding pharmacist by removing the burden of establishing a brand new role and identifying necessary tasks to be completed throughout the day.
We also discovered on these new care coordination units that our patient criteria for education and medication reconciliation were not universal. We developed and initiated our pharmacy bundle of services in a medical patient population. As we expanded these services to other patient care areas, the targeted list of medications/conditions changed. For example, surgical patients had a greater need for education around opioid therapy and complex bowel regimens while neurology patients needed education regarding antiepileptic regimens. Similarly, patients requiring medication reconciliation also changed. Nurses were performing medication reconciliation for patients with elective surgeries and had a system that worked for that population. Therefore, we did not need to focus efforts for this population around medication reconciliation and could shift our focus more towards medication education.
Optimizing the Delivery of Discharge Prescriptions
The Meds for Home workflow has been updated multiple times since implementation. These changes resulted from early and frequent meetings with nurses, case managers, providers, and the pharmacy team. The Meds for Home service uses an outpatient pharmacy located within the hospital that has high prescription volumes at baseline to fill discharge prescriptions. Due to the volume of out-patient prescriptions and unexpected discharges, delays in prescription delivery occurred. To improve efficiency, a separate workflow and space were designated for filling Meds for Home prescriptions. Initially, MHCs were visiting floors to pick-up and deliver prescriptions at set times (ie, 10 am, 2 pm, and 5 pm). Instead of using set pick-up and delivery times, the Meds for Home service now uses a rolling 2-hour turnaround time during service hours. Additionally, providers, case managers, and units were educated to provide discharge prescriptions, especially those requiring prior authorization, as early as possible to expedite service. By identifying these issues early in the process, we were able to develop a different strategy that worked for the units, providers, and pharmacy.
Lessons Learned
The time of transition from one level of care to another is a vulnerable time for patients, as it is a time when medication-related problems often arise. In an elderly patient population, one study demonstrated that contributing factors for medication discrepancies following hospital discharge included unintended nonadherence and inadequate discharge instructions, and patients experiencing a medication discrepancy were at a significantly higher risk of readmission [4]. Hospital readmissions have also been linked to a lack of adequate follow-up in the outpatient setting [5]. Pharmacists should become more involved in preventing medication-related problems during the times of transition by performing activities such as medication reconciliation, patient education, and assessment of patient outcomes post-discharge [6,7]. Studies have demonstrated that pharmacists are able to reduce medication-related adverse events during and after hospitalization by completing these activities [8–10]. Residency-trained pharmacists are well-equipped to provide these services and are needed to create new processes and models to meet the ever changing demands of health care payers and accrediting bodies. ASHP recommends pharmacists entering into careers in health systems be at least PGY1-trained while the American College of Clinical Pharmacy (ACCP) envisions all pharmacists involved in direct patient care complete residency training [11,12]. Health systems will continue to be challenged with transforming pharmacy models to allow for this influx of highly trained individuals in a time of budget constraints. Below, we describe the lessons we learned while implementing our pharmacy bundle of services and think are essential for other institutions to consider when initiating their own services.
Rethink the Role of the Pharmacist
As health systems acquire smaller hospitals, the role of the pharmacist may need to be redefined and reinvented. The responsibilities of a pharmacist in a large academic hospital may be different than those of a pharmacist with the same skill set in a community hospital. However, despite the difference in practice setting, the same core pharmacy services around medication use can still be deployed. Participation in transitions of care activities is a relatively new concept for many pharmacists as residency training programs traditionally focused on caring for patients within a defined setting such as the intensive care unit or ambulatory care. The pharmacy profession should define the role of the clinical pharmacist in order to make the incorporation of transitions of care responsibilities into job expectations easier for all. The ACCP outlines this need and sets forth recommendations for clinical pharmacists’ responsibilities within the health care team to include assessing patients and medication regimens, developing and implementing medication-related therapy plans, and evaluating clinical outcomes [13]. Pharmacy leadership organizations, including ASHP and ACCP, offer resources providing the vision of pharmacy practice and expectations for which institutions should be reaching. Pharmacy departments should use these resources to complete gap analyses of current processes and those envisioned for the future to help guide efforts for change at their own institutions.
Obtain Support Within Your Institution
Gaining support from hospital leadership for advancing pharmacists’ involvement in patient care is instrumental. Without leadership support at both the institutional and department of pharmacy levels, pharmacists with advanced training may be hindered from practicing at the top of their license. Furthermore, support by leadership of pharmacy residency programs and experiential student learning sites at the institution is also important. Pharmacy residents and students became indispensable in our model and allowed us to expand our reach to more patients. We used residents to cover additional teams that were previously uncovered by a rounding pharmacist and, along with students, provide medication reconciliation, patient education, and follow-up phone calls to more patients. Requiring participation in the pharmacy bundle of services for rotations also allowed us to train these individuals about the value of transitions of care and see the challenges patients face in gaining access to medications. In a survey of academic medical center executives, pharmacy directors, and pharmacists at 8 institutions, residents were noted to add value to the institution through decreasing drug-related errors and drug costs, expansion of clinical services, and enhancing opportunities for research [14].
Support from other disciplines is also essential. Collaborating with other disciplines should occur prior to, during, and beyond implementation. We collaborated with providers, nurses, case managers, social workers and many other disciplines during all phases of the process. Being inclusive during the planning process allowed everyone to understand each other’s role and to provide input on how we could work together to best utilize everyone’s resources. This multidisciplinary approach to developing pharmacy services also allowed an opportunity to collaborate on research and evaluate our processes with other disciplines.
Tracking interventions will demonstrate the value of pharmacists, technicians, and other pharmacy team members participating in these advanced roles. This information will be useful when justifying the practice model to hospital leadership and for recruiting new pharmacists, residents, and technicians to the institution. Additionally, defining both outcome (eg, 30-day readmission rates, HCAHPS scores) and process (eg, number of patient education sessions performed, number of medication discrepancies reconciled) measures upfront is important in order for those involved to understand how their work will be assessed. These data will be useful in determining whether the intervention is making an impact early on and allow for restructuring of the process if not.
Create Depth in Your Team While Engaging Current Resources
We spent a significant amount of time planning the implementation of our pharmacy bundle of services, collaborating with other disciplines, and training our pharmacy team members. We hired highly trained and competent people into new positions and ensured every-one clearly understood their responsibilities. This was a critical step in order to ensure we were providing optimal care to our patients and integrating leaders into our team. We also utilized our current workforce to fill new clinical rounding pharmacist or technician roles. For those pharmacists who had not completed a residency, we required the pharmacists to complete a compact training program similar to that required of our residents [1]. This training ensured that important services were being performed adequately by each rounding pharmacist. Similarly, technicians transitioning from a primarily medication dispensing role to a MHC or medication history role received extensive training to assist with developing their new skill set.
Creating relationships with an outpatient pharmacy is essential to ensure patients are discharged from the hospital on medications they can afford long-term. We are fortunate to have 5 outpatient pharmacies on the JHH campus that are under the Johns Hopkins Health System umbrella, which made collaboration between the inpatient and outpatient teams seamless. However, many hospitals may not be directly affiliated with an outpatient pharmacy with which to collaborate or may contract with a retail chain pharmacy. In the latter case, inpatient and outpatient pharmacies must work together to define roles around transitions of care and how to best serve the patient in a collaborative manner. If no onsite outpatient pharmacy exists, dedicated resources should be acquired to serve as a liaison between the inpatient team and the outpatient pharmacy. These resources may work through issues such as formulary preferences, prior authorization requests, and connecting the patient to the medication either through bedside delivery or filling at the patient’s community pharmacy. Community pharmacies recognize the cost benefit they could gain through 340B pricing and specialty drug dispensing when working in collaboration with healthcare systems. However, health systems must be aware that collaborating with outpatient pharmacy partnerships will create further challenges as providers ensure patient preference for use of a particular pharmacy is honored and cost-sharing is incorporated into models.
Continuously Reevaluate Your Services
As implementation of our pharmacy bundle of services began, meeting early and often was essential to identify issues and adjust our workflow to resolve those issues quickly. When the inpatient component of the pharmacy bundle of services was first implemented, rounding pharmacists and pharmacy leadership initially met on a weekly basis to provide feedback on the practice model and develop resolutions for any issues. However, it is important to also include other disciplines in the evaluation process. For the Meds for Home program, pharmacy leadership not only met with MHCs but also with providers, nurses, case managers, and social workers for feedback on how to improve the service. Although the workflow of our pharmacy bundle of services are more established, evaluations still occur albeit less frequently.
Conclusion
Pharmacists’ involvement in transitions of care should become part of the daily responsibility. Health systems should understand how efforts to expand pharmacists’ interventions align with overall hospital goals. Many hospitals may already have programs in place to help with transitions of care. Pharmacists can help expand current efforts through increased visibility to physicians and patients as well as collaboration with outpatient pharmacies to ensure medications are effective and affordable for patients long-term.
Note: The project described was supported by grant no. 1C1CMS331053-01-00 from the U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. The research presented was conducted by the awardee. Findings may or may not be consistent with or confirmed by the findings of the independent evaluation contractor.
Corresponding author: Vi Gilmore, PharmD, BCPS, Clinical Pharmacy Specialist, Internal Medicine, The Johns Hopkins Hospital, 600 N. Wolfe Street, Carnegie 180, Baltimore, MD 21287, [email protected].
Financial disclosures: None.
1. Gilmore V, Efird L, Fu D, et al. Implementation of transitions-of-care services through acute care and outpatient pharmacy collaboration. Am J Health Syst Pharm 2015;72:737–44.
2. American College of Clinical Pharmacy, Burke JM, Miller WA, et al. Clinical pharmacist competencies. Pharmacotherapy 2008;28:806–15.
3. American Society of Health-System Pharmacists. ASHP accreditation standard for postgraduate year one (PGY1) pharmacy residency programs. Available at www.ashp.org/DocLibrary/Accreditation/Newly-approved-PGY1-Standard-September-2014.pdf.
4. Coleman EA, Smith JD, Raha D, Min S. Posthospital medication discrepancies: prevalence and contributing factors. Arch Intern Med 2005:165:1842–7.
5. Jackson C, Shahsahebi M, Wedlake T, DuBard C. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med 2015;13:115–22.
6. American College of Clinical Pharmacy, Hume AL, Kirwin J, et al. Improving care transitions: current practice and future opportunities for pharmacists. Pharmacotherapy 2012;32:e326–37.
7. Cobaugh DJ, Amin A, Bookwalter T, et al. ASHP-SHM joint statement on hospitalist-pharmacist collaboration. Am J Health Syst Pharm 2008;65:260–3.
8. Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med 2006;166:565–71.
9. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization. Ann Intern Med 2009;150:178–87.
10. Murphy EM, Oxencis CJ, Klauck JA, et al. Medication reconciliation at an academic medical center: implementation of a comprehensive program from admission to discharge. Am J Health Syst Pharm 2009;66:2126–31.
11. Myers CE. ASHP Health-System Pharmacy 2015 Initiative. Am J Health-Syst Pharm 2004;61:657.
12. Murphy JE, Nappi JM, Bosso JA, et al. ACCP position statement. American College of Clinical Pharmacy’s vision of the future: postgraduate pharmacy residency training as a prerequisite for direct patient care. Pharmacotherapy 2006;26:
722–33.
13. Harris IM, Phillips B, Boyce E, et al. Clinical pharmacy should adopt a consistent process of direct patient care. Pharmacotherapy 2014;34:e133–48.
14. Fuller PD, Smith KM, Hinman RK, et al. Value of pharmacy residency training: a survey of the academic medical center perspective. Am J Health Syst Pharm 2012;69:158–65.
From The Johns Hopkins Hospital, Baltimore, MD.
The project described was supported by grant # 1C1CMS331053-01-00 from the U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. The research presented was conducted by the awardee. Findings may or may not be consistent with or confirmed by the findings of the independent evaluation contractor.
Abstract
- Background: Medication management is becoming more complex, with new medications entering the market, drug prices increasing, and patients transferring into and out of the hospital. Transitions of care services are being implemented to prevent readmissions and increase patient satisfaction. Pharmacists play a key role by expanding clinical services provided to patients around medication management.
- Objective: To describe a pharmacy transitions of care model at a large academic teaching hospital and lessons learned during implementation.
- Methods: A pharmacy bundle of services was initially developed in a medical patient population and included medication reconciliation, patient education targeting high-risk medications, post-discharge follow-up phone calls, and bedside discharge prescription delivery. This bundle was expanded to other patient populations through the use of residency-trained pharmacists, pharmacy residents, pharmacy students, and certified pharmacy technicians.
- Results: Challenges were faced when implementing our transitions of care services, including expanding care coordination team coverage with existing resources, training pharmacy staff in new roles, determining the needs of patients cared for by teams we had not previously been integrated into, and creating our discharge prescription delivery program. During this process, we learned to rethink the role of pharmacists on our team, value the support within our institution to create change in order to improve patient care, and continuously evaluate this process.
- Conclusion: We are at an opportune time to expand the scope of the inpatient pharmacist to provide advanced medication-related services to patients. Residency training is creating individuals who will thrive in these new models.
Medication management around the acute care inpatient stay is a challenging but crucial task to ensure patient safety and desired clinical outcomes. The first step in successful medication management is to understand the patient’s medication regimen in the home environment. Patients may take medications differently than prescribed; skip medication doses intentionally to make a supply last longer; use over-the-counter medications, herbal supplements, or someone else’s medication based on the recommendation of family or friends; or discontinue medications based on side effects or media influence. Over the course of the inpatient stay, medication management involves adjusting doses based on changes in organ function, detecting side effects and potential drug interactions, and monitoring clinical outcomes to ensure appropriate drug therapy is being prescribed. As the patient approaches discharge, ensuring the patient understands the indications for his/her medications, has self-monitoring techniques to recognize efficacy or adverse effects, and has access to discharge medications is important. Lastly, long-term medication management includes patient access to pharmaceutical expertise over time. Pharmacists’ involvement in medication therapy management services and patient-centered medical homes is key to ensuring safe and effective medication use over time.
In 2009, the Johns Hopkins Health System Readmission Prevention Task Force developed strategies to reduce preventable readmissions and improve transitions of care. In 2011, a new multidisciplinary approach to patient care was implemented at the Johns Hopkins Hospital (JHH) to optimize care coordination and improve acute care management. Using this approach, care coordination teams composed of physicians, nurses, pharmacists, nurse case managers, social workers, physical/occupational therapists, nutritionists, and home care coordinators meet on a daily basis to discuss the inpatient and discharge care needs of patients in order to improve care transitions and reduce preventable readmissions. In 2012, JHH was awarded a 3-year innovation grant from the Centers for Medicaid & Medicare Services (CMS) that would assist with expansion of these care coordination teams to every unit of the hospital. Prior to implementation of the care coordination model at JHH in 2011, there were 3 pharmacists who consistently rounded on 3 inpatient medicine teams (one pharmacist also had operational responsibilities). Pharmacists were deemed by the task force to be key providers of medication management and, thus, essential members of the care coordination team. Due to an inability to hire a new pharmacist for every care coordination team, the department of pharmacy needed to determine how to provide consistent pharmacist coverage utilizing current resources. This report describes the challenges faced and lessons learned by our adult inpatient pharmacy division when implementing a pharmacy bundle of services to improve care transitions for an adult patient population.
Setting
JHH is an 1192-bed academic teaching hospital located in Baltimore, Maryland. At JHH, the department of pharmacy has 4 inpatient divisions that service the medication needs of different patient populations: medicine, critical care/surgery, oncology, and pediatrics. The adultinpatient pharmacy division covers medicine units in addition to obstetrics, neurology, and surgery units. It is responsible for 486 inpatient beds on 22 units and was the first division to provide the pharmacy bundle of services described below. Currently, 11 rounding and 5 operational pharmacists provide care coordination and order verification support, respectively, for the division during day shift.
Program Overview
Rounding pharmacists on care coordination teams address acute care medication issues and provide a bundle of services that includes targeted patient education, medication reconciliation, post-discharge follow-up phone calls, and discharge prescription planning. The full details of these services have been described [1]. Briefly, patients newly initiated on medications deemed ”high-risk” (eg, anticoagulation, insulin, metered dose inhalers, dual antiplatelets) receive education by a member of the pharmacy team (ie, pharmacist, pharmacy resident, or pharmacy student) prior to discharge. Those patients who receive education are offered a post-discharge follow-up phone call to assess for any questions or issues. Patients who accept this service are contacted 48 to 72 hours post-discharge. Specific patient populations (eg, patients with congestive heart failure, diabetes) are also targeted for completion of medication reconciliation. If patients are being discharged with prescriptions, they are offered our “Meds for Home” service. Patients who accept this service have their prescriptions filled at one of our outpatient pharmacies and delivered to the unit prior to discharge. Highly trained certified pharmacy technicians, called “Meds for Home” coordinators (MHCs; previously known as transitions pharmacist extenders), facilitate this process.
Challenges Faced
Care Coordination Team Coverage
One challenge to implementation of the pharmacy bundle of services was providing consistent team coverage with adequately trained pharmacists. It was not feasible to hire a pharmacist to cover each of the care coordination teams. To address gaps in coverage, we initially utilized postgraduate year 1 and 2 (PGY1 and 2) pharmacy residents on an internal medicine rotation to cover care coordination teams without a rounding pharmacist. However, this method proved unreliable as a pharmacy resident was not scheduled for an internal medicine rotation each month. In the beginning, our division had 3 rounding and 9 operational pharmacists during day shift. To provide sufficient clinical coverage while still adequately addressing order verification needs, a major restructuring of our pharmacy model was necessary. We increased the bed-to-pharmacist ratio for order verification, which allowed the number of operational pharmacists to decrease from 9 to 5. Those 4 remaining pharmacists were now available to serve as rounding pharmacists. Along with hiring 2 additional rounding pharmacists with funding from the CMS innovation grant, we were able to increase the number of care coordination teams consistently covered from 3 to 9.
Although we expanded pharmacist coverage of care coordination teams, time constraints prevented all patients who met criteria for patient education or medication reconciliation to have these services completed in a timely manner or at all by a pharmacist. Our rounding pharmacists’ responsibilities also included participation in high-level activities such as order set reviews for a new provider order entry system, ambulatory clinic time, stewardship activities, and quality improvement projects. In order to increase our scope, we utilized pharmacy technicians, students, and residents to assist with completing these tasks. All pharmacy students and residents on rotation within our division participated in a daily huddle Monday through Friday. Rounding pharmacists whose unit had patient education needs that could not be met by that pharmacist submitted requests by a set time. Those patient education tasks were then divided amongst the pharmacy learners at the huddle for completion. Prior to being allowed to independently counsel patients, pharmacy learners’ patient education skills were evaluated by preceptors. To facilitate timely completion of medication histories, technicians were hired. These medication history technicians are available Monday through Friday to complete medication histories for patients admitted to specific medicine units, ideally within 24 hours of admission. Rounding pharmacists are notified of completion of medication histories via our electronic medical record and reconcile that list with the patient’s inpatient medication list. Any clinically relevant discrepancies are communicated to providers. Pharmacy learners may also collect medication histories.
Training Rounding Pharmacists
Another challenge we faced was providing adequate training for operational pharmacists transitioning to a rounding position. Residency training is crucial in providing the level of skill necessary to identify complex drug therapy problems, adjust treatment regimens, and create plans where limited data exist to drive drug therapy recommendations [2,3]. Rotations during the final year of pharmacy school provide exposure to interacting with patients and providers. Completion of PGY1 residency training allows a pharmacist to practice as a generalist with a broad range of experiences provided during the year to identify medication-related problems. PGY2 residency training allows the pharmacist to spend a concentrated year in the chosen area of expertise and gain a deeper knowledge of medication use in a specific patient population or area of practice [2]. After 2 years of clinical residency training, pharmacists have the skills to interact with patients and multidisciplinary teams to optimize medication regimens, provide medication education, and measure the value they bring to the health care of patients.
Some of the operational pharmacists who were transitioning to the rounding pharmacist role had no training beyond pharmacy school or had only completed a PGY1 pharmacy residency. Initially, training for this new role lasted only a few days and consisted of orientation to the unit and observation of care coordination rounds. We learned that this brief amount of training was insufficient, even for those with PGY1 pharmacy residency training. In order to ensure that these rounding pharmacists could successfully provide the bundle of services and meet the high clinical demands of the inpatient service, we developed a comprehensive training program. Those interested in transitioning from an operational to a rounding pharmacist role must now complete a 6-week training program. The first 2 weeks consists of improving patient education and medication history skills. The remaining 4 weeks are spent honing clinical rounding skills. Rounding pharmacists-in-training also receive a formal review of their performance utilizing an evaluation form developed by the American Society of Health-System Pharmacists (ASHP) for pharmacy residents.
Establishing a Pharmacy Bundle and the Role of a Rounding Pharmacist on New Units
Some of the units implementing care coordination teams, such as neurology, did not previously have a pharmacist rounding on those units. Furthermore, these units had a high patient census (eg, 60 patients), which made it difficult for one pharmacist to clinically evaluate every patient. Multiple specialty teams also admitted patients to a single unit, which made it challenging for the pharmacist to develop strong working relationships with providers. As such, rounding pharmacists deployed to those units had difficulty establishing their role on the team, especially for those pharmacists without or with only 1 year of postgraduate training. To address this issue, a PGY2-trained pharmacist rounded on the unit to assess which areas/teams had the greatest need for a pharmacist. Completing this needs assessment on these units allowed for the rounding pharmacist to more effectively use his/her time. It also allowed for a smoother transition from operational to rounding pharmacist by removing the burden of establishing a brand new role and identifying necessary tasks to be completed throughout the day.
We also discovered on these new care coordination units that our patient criteria for education and medication reconciliation were not universal. We developed and initiated our pharmacy bundle of services in a medical patient population. As we expanded these services to other patient care areas, the targeted list of medications/conditions changed. For example, surgical patients had a greater need for education around opioid therapy and complex bowel regimens while neurology patients needed education regarding antiepileptic regimens. Similarly, patients requiring medication reconciliation also changed. Nurses were performing medication reconciliation for patients with elective surgeries and had a system that worked for that population. Therefore, we did not need to focus efforts for this population around medication reconciliation and could shift our focus more towards medication education.
Optimizing the Delivery of Discharge Prescriptions
The Meds for Home workflow has been updated multiple times since implementation. These changes resulted from early and frequent meetings with nurses, case managers, providers, and the pharmacy team. The Meds for Home service uses an outpatient pharmacy located within the hospital that has high prescription volumes at baseline to fill discharge prescriptions. Due to the volume of out-patient prescriptions and unexpected discharges, delays in prescription delivery occurred. To improve efficiency, a separate workflow and space were designated for filling Meds for Home prescriptions. Initially, MHCs were visiting floors to pick-up and deliver prescriptions at set times (ie, 10 am, 2 pm, and 5 pm). Instead of using set pick-up and delivery times, the Meds for Home service now uses a rolling 2-hour turnaround time during service hours. Additionally, providers, case managers, and units were educated to provide discharge prescriptions, especially those requiring prior authorization, as early as possible to expedite service. By identifying these issues early in the process, we were able to develop a different strategy that worked for the units, providers, and pharmacy.
Lessons Learned
The time of transition from one level of care to another is a vulnerable time for patients, as it is a time when medication-related problems often arise. In an elderly patient population, one study demonstrated that contributing factors for medication discrepancies following hospital discharge included unintended nonadherence and inadequate discharge instructions, and patients experiencing a medication discrepancy were at a significantly higher risk of readmission [4]. Hospital readmissions have also been linked to a lack of adequate follow-up in the outpatient setting [5]. Pharmacists should become more involved in preventing medication-related problems during the times of transition by performing activities such as medication reconciliation, patient education, and assessment of patient outcomes post-discharge [6,7]. Studies have demonstrated that pharmacists are able to reduce medication-related adverse events during and after hospitalization by completing these activities [8–10]. Residency-trained pharmacists are well-equipped to provide these services and are needed to create new processes and models to meet the ever changing demands of health care payers and accrediting bodies. ASHP recommends pharmacists entering into careers in health systems be at least PGY1-trained while the American College of Clinical Pharmacy (ACCP) envisions all pharmacists involved in direct patient care complete residency training [11,12]. Health systems will continue to be challenged with transforming pharmacy models to allow for this influx of highly trained individuals in a time of budget constraints. Below, we describe the lessons we learned while implementing our pharmacy bundle of services and think are essential for other institutions to consider when initiating their own services.
Rethink the Role of the Pharmacist
As health systems acquire smaller hospitals, the role of the pharmacist may need to be redefined and reinvented. The responsibilities of a pharmacist in a large academic hospital may be different than those of a pharmacist with the same skill set in a community hospital. However, despite the difference in practice setting, the same core pharmacy services around medication use can still be deployed. Participation in transitions of care activities is a relatively new concept for many pharmacists as residency training programs traditionally focused on caring for patients within a defined setting such as the intensive care unit or ambulatory care. The pharmacy profession should define the role of the clinical pharmacist in order to make the incorporation of transitions of care responsibilities into job expectations easier for all. The ACCP outlines this need and sets forth recommendations for clinical pharmacists’ responsibilities within the health care team to include assessing patients and medication regimens, developing and implementing medication-related therapy plans, and evaluating clinical outcomes [13]. Pharmacy leadership organizations, including ASHP and ACCP, offer resources providing the vision of pharmacy practice and expectations for which institutions should be reaching. Pharmacy departments should use these resources to complete gap analyses of current processes and those envisioned for the future to help guide efforts for change at their own institutions.
Obtain Support Within Your Institution
Gaining support from hospital leadership for advancing pharmacists’ involvement in patient care is instrumental. Without leadership support at both the institutional and department of pharmacy levels, pharmacists with advanced training may be hindered from practicing at the top of their license. Furthermore, support by leadership of pharmacy residency programs and experiential student learning sites at the institution is also important. Pharmacy residents and students became indispensable in our model and allowed us to expand our reach to more patients. We used residents to cover additional teams that were previously uncovered by a rounding pharmacist and, along with students, provide medication reconciliation, patient education, and follow-up phone calls to more patients. Requiring participation in the pharmacy bundle of services for rotations also allowed us to train these individuals about the value of transitions of care and see the challenges patients face in gaining access to medications. In a survey of academic medical center executives, pharmacy directors, and pharmacists at 8 institutions, residents were noted to add value to the institution through decreasing drug-related errors and drug costs, expansion of clinical services, and enhancing opportunities for research [14].
Support from other disciplines is also essential. Collaborating with other disciplines should occur prior to, during, and beyond implementation. We collaborated with providers, nurses, case managers, social workers and many other disciplines during all phases of the process. Being inclusive during the planning process allowed everyone to understand each other’s role and to provide input on how we could work together to best utilize everyone’s resources. This multidisciplinary approach to developing pharmacy services also allowed an opportunity to collaborate on research and evaluate our processes with other disciplines.
Tracking interventions will demonstrate the value of pharmacists, technicians, and other pharmacy team members participating in these advanced roles. This information will be useful when justifying the practice model to hospital leadership and for recruiting new pharmacists, residents, and technicians to the institution. Additionally, defining both outcome (eg, 30-day readmission rates, HCAHPS scores) and process (eg, number of patient education sessions performed, number of medication discrepancies reconciled) measures upfront is important in order for those involved to understand how their work will be assessed. These data will be useful in determining whether the intervention is making an impact early on and allow for restructuring of the process if not.
Create Depth in Your Team While Engaging Current Resources
We spent a significant amount of time planning the implementation of our pharmacy bundle of services, collaborating with other disciplines, and training our pharmacy team members. We hired highly trained and competent people into new positions and ensured every-one clearly understood their responsibilities. This was a critical step in order to ensure we were providing optimal care to our patients and integrating leaders into our team. We also utilized our current workforce to fill new clinical rounding pharmacist or technician roles. For those pharmacists who had not completed a residency, we required the pharmacists to complete a compact training program similar to that required of our residents [1]. This training ensured that important services were being performed adequately by each rounding pharmacist. Similarly, technicians transitioning from a primarily medication dispensing role to a MHC or medication history role received extensive training to assist with developing their new skill set.
Creating relationships with an outpatient pharmacy is essential to ensure patients are discharged from the hospital on medications they can afford long-term. We are fortunate to have 5 outpatient pharmacies on the JHH campus that are under the Johns Hopkins Health System umbrella, which made collaboration between the inpatient and outpatient teams seamless. However, many hospitals may not be directly affiliated with an outpatient pharmacy with which to collaborate or may contract with a retail chain pharmacy. In the latter case, inpatient and outpatient pharmacies must work together to define roles around transitions of care and how to best serve the patient in a collaborative manner. If no onsite outpatient pharmacy exists, dedicated resources should be acquired to serve as a liaison between the inpatient team and the outpatient pharmacy. These resources may work through issues such as formulary preferences, prior authorization requests, and connecting the patient to the medication either through bedside delivery or filling at the patient’s community pharmacy. Community pharmacies recognize the cost benefit they could gain through 340B pricing and specialty drug dispensing when working in collaboration with healthcare systems. However, health systems must be aware that collaborating with outpatient pharmacy partnerships will create further challenges as providers ensure patient preference for use of a particular pharmacy is honored and cost-sharing is incorporated into models.
Continuously Reevaluate Your Services
As implementation of our pharmacy bundle of services began, meeting early and often was essential to identify issues and adjust our workflow to resolve those issues quickly. When the inpatient component of the pharmacy bundle of services was first implemented, rounding pharmacists and pharmacy leadership initially met on a weekly basis to provide feedback on the practice model and develop resolutions for any issues. However, it is important to also include other disciplines in the evaluation process. For the Meds for Home program, pharmacy leadership not only met with MHCs but also with providers, nurses, case managers, and social workers for feedback on how to improve the service. Although the workflow of our pharmacy bundle of services are more established, evaluations still occur albeit less frequently.
Conclusion
Pharmacists’ involvement in transitions of care should become part of the daily responsibility. Health systems should understand how efforts to expand pharmacists’ interventions align with overall hospital goals. Many hospitals may already have programs in place to help with transitions of care. Pharmacists can help expand current efforts through increased visibility to physicians and patients as well as collaboration with outpatient pharmacies to ensure medications are effective and affordable for patients long-term.
Note: The project described was supported by grant no. 1C1CMS331053-01-00 from the U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. The research presented was conducted by the awardee. Findings may or may not be consistent with or confirmed by the findings of the independent evaluation contractor.
Corresponding author: Vi Gilmore, PharmD, BCPS, Clinical Pharmacy Specialist, Internal Medicine, The Johns Hopkins Hospital, 600 N. Wolfe Street, Carnegie 180, Baltimore, MD 21287, [email protected].
Financial disclosures: None.
From The Johns Hopkins Hospital, Baltimore, MD.
The project described was supported by grant # 1C1CMS331053-01-00 from the U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. The research presented was conducted by the awardee. Findings may or may not be consistent with or confirmed by the findings of the independent evaluation contractor.
Abstract
- Background: Medication management is becoming more complex, with new medications entering the market, drug prices increasing, and patients transferring into and out of the hospital. Transitions of care services are being implemented to prevent readmissions and increase patient satisfaction. Pharmacists play a key role by expanding clinical services provided to patients around medication management.
- Objective: To describe a pharmacy transitions of care model at a large academic teaching hospital and lessons learned during implementation.
- Methods: A pharmacy bundle of services was initially developed in a medical patient population and included medication reconciliation, patient education targeting high-risk medications, post-discharge follow-up phone calls, and bedside discharge prescription delivery. This bundle was expanded to other patient populations through the use of residency-trained pharmacists, pharmacy residents, pharmacy students, and certified pharmacy technicians.
- Results: Challenges were faced when implementing our transitions of care services, including expanding care coordination team coverage with existing resources, training pharmacy staff in new roles, determining the needs of patients cared for by teams we had not previously been integrated into, and creating our discharge prescription delivery program. During this process, we learned to rethink the role of pharmacists on our team, value the support within our institution to create change in order to improve patient care, and continuously evaluate this process.
- Conclusion: We are at an opportune time to expand the scope of the inpatient pharmacist to provide advanced medication-related services to patients. Residency training is creating individuals who will thrive in these new models.
Medication management around the acute care inpatient stay is a challenging but crucial task to ensure patient safety and desired clinical outcomes. The first step in successful medication management is to understand the patient’s medication regimen in the home environment. Patients may take medications differently than prescribed; skip medication doses intentionally to make a supply last longer; use over-the-counter medications, herbal supplements, or someone else’s medication based on the recommendation of family or friends; or discontinue medications based on side effects or media influence. Over the course of the inpatient stay, medication management involves adjusting doses based on changes in organ function, detecting side effects and potential drug interactions, and monitoring clinical outcomes to ensure appropriate drug therapy is being prescribed. As the patient approaches discharge, ensuring the patient understands the indications for his/her medications, has self-monitoring techniques to recognize efficacy or adverse effects, and has access to discharge medications is important. Lastly, long-term medication management includes patient access to pharmaceutical expertise over time. Pharmacists’ involvement in medication therapy management services and patient-centered medical homes is key to ensuring safe and effective medication use over time.
In 2009, the Johns Hopkins Health System Readmission Prevention Task Force developed strategies to reduce preventable readmissions and improve transitions of care. In 2011, a new multidisciplinary approach to patient care was implemented at the Johns Hopkins Hospital (JHH) to optimize care coordination and improve acute care management. Using this approach, care coordination teams composed of physicians, nurses, pharmacists, nurse case managers, social workers, physical/occupational therapists, nutritionists, and home care coordinators meet on a daily basis to discuss the inpatient and discharge care needs of patients in order to improve care transitions and reduce preventable readmissions. In 2012, JHH was awarded a 3-year innovation grant from the Centers for Medicaid & Medicare Services (CMS) that would assist with expansion of these care coordination teams to every unit of the hospital. Prior to implementation of the care coordination model at JHH in 2011, there were 3 pharmacists who consistently rounded on 3 inpatient medicine teams (one pharmacist also had operational responsibilities). Pharmacists were deemed by the task force to be key providers of medication management and, thus, essential members of the care coordination team. Due to an inability to hire a new pharmacist for every care coordination team, the department of pharmacy needed to determine how to provide consistent pharmacist coverage utilizing current resources. This report describes the challenges faced and lessons learned by our adult inpatient pharmacy division when implementing a pharmacy bundle of services to improve care transitions for an adult patient population.
Setting
JHH is an 1192-bed academic teaching hospital located in Baltimore, Maryland. At JHH, the department of pharmacy has 4 inpatient divisions that service the medication needs of different patient populations: medicine, critical care/surgery, oncology, and pediatrics. The adultinpatient pharmacy division covers medicine units in addition to obstetrics, neurology, and surgery units. It is responsible for 486 inpatient beds on 22 units and was the first division to provide the pharmacy bundle of services described below. Currently, 11 rounding and 5 operational pharmacists provide care coordination and order verification support, respectively, for the division during day shift.
Program Overview
Rounding pharmacists on care coordination teams address acute care medication issues and provide a bundle of services that includes targeted patient education, medication reconciliation, post-discharge follow-up phone calls, and discharge prescription planning. The full details of these services have been described [1]. Briefly, patients newly initiated on medications deemed ”high-risk” (eg, anticoagulation, insulin, metered dose inhalers, dual antiplatelets) receive education by a member of the pharmacy team (ie, pharmacist, pharmacy resident, or pharmacy student) prior to discharge. Those patients who receive education are offered a post-discharge follow-up phone call to assess for any questions or issues. Patients who accept this service are contacted 48 to 72 hours post-discharge. Specific patient populations (eg, patients with congestive heart failure, diabetes) are also targeted for completion of medication reconciliation. If patients are being discharged with prescriptions, they are offered our “Meds for Home” service. Patients who accept this service have their prescriptions filled at one of our outpatient pharmacies and delivered to the unit prior to discharge. Highly trained certified pharmacy technicians, called “Meds for Home” coordinators (MHCs; previously known as transitions pharmacist extenders), facilitate this process.
Challenges Faced
Care Coordination Team Coverage
One challenge to implementation of the pharmacy bundle of services was providing consistent team coverage with adequately trained pharmacists. It was not feasible to hire a pharmacist to cover each of the care coordination teams. To address gaps in coverage, we initially utilized postgraduate year 1 and 2 (PGY1 and 2) pharmacy residents on an internal medicine rotation to cover care coordination teams without a rounding pharmacist. However, this method proved unreliable as a pharmacy resident was not scheduled for an internal medicine rotation each month. In the beginning, our division had 3 rounding and 9 operational pharmacists during day shift. To provide sufficient clinical coverage while still adequately addressing order verification needs, a major restructuring of our pharmacy model was necessary. We increased the bed-to-pharmacist ratio for order verification, which allowed the number of operational pharmacists to decrease from 9 to 5. Those 4 remaining pharmacists were now available to serve as rounding pharmacists. Along with hiring 2 additional rounding pharmacists with funding from the CMS innovation grant, we were able to increase the number of care coordination teams consistently covered from 3 to 9.
Although we expanded pharmacist coverage of care coordination teams, time constraints prevented all patients who met criteria for patient education or medication reconciliation to have these services completed in a timely manner or at all by a pharmacist. Our rounding pharmacists’ responsibilities also included participation in high-level activities such as order set reviews for a new provider order entry system, ambulatory clinic time, stewardship activities, and quality improvement projects. In order to increase our scope, we utilized pharmacy technicians, students, and residents to assist with completing these tasks. All pharmacy students and residents on rotation within our division participated in a daily huddle Monday through Friday. Rounding pharmacists whose unit had patient education needs that could not be met by that pharmacist submitted requests by a set time. Those patient education tasks were then divided amongst the pharmacy learners at the huddle for completion. Prior to being allowed to independently counsel patients, pharmacy learners’ patient education skills were evaluated by preceptors. To facilitate timely completion of medication histories, technicians were hired. These medication history technicians are available Monday through Friday to complete medication histories for patients admitted to specific medicine units, ideally within 24 hours of admission. Rounding pharmacists are notified of completion of medication histories via our electronic medical record and reconcile that list with the patient’s inpatient medication list. Any clinically relevant discrepancies are communicated to providers. Pharmacy learners may also collect medication histories.
Training Rounding Pharmacists
Another challenge we faced was providing adequate training for operational pharmacists transitioning to a rounding position. Residency training is crucial in providing the level of skill necessary to identify complex drug therapy problems, adjust treatment regimens, and create plans where limited data exist to drive drug therapy recommendations [2,3]. Rotations during the final year of pharmacy school provide exposure to interacting with patients and providers. Completion of PGY1 residency training allows a pharmacist to practice as a generalist with a broad range of experiences provided during the year to identify medication-related problems. PGY2 residency training allows the pharmacist to spend a concentrated year in the chosen area of expertise and gain a deeper knowledge of medication use in a specific patient population or area of practice [2]. After 2 years of clinical residency training, pharmacists have the skills to interact with patients and multidisciplinary teams to optimize medication regimens, provide medication education, and measure the value they bring to the health care of patients.
Some of the operational pharmacists who were transitioning to the rounding pharmacist role had no training beyond pharmacy school or had only completed a PGY1 pharmacy residency. Initially, training for this new role lasted only a few days and consisted of orientation to the unit and observation of care coordination rounds. We learned that this brief amount of training was insufficient, even for those with PGY1 pharmacy residency training. In order to ensure that these rounding pharmacists could successfully provide the bundle of services and meet the high clinical demands of the inpatient service, we developed a comprehensive training program. Those interested in transitioning from an operational to a rounding pharmacist role must now complete a 6-week training program. The first 2 weeks consists of improving patient education and medication history skills. The remaining 4 weeks are spent honing clinical rounding skills. Rounding pharmacists-in-training also receive a formal review of their performance utilizing an evaluation form developed by the American Society of Health-System Pharmacists (ASHP) for pharmacy residents.
Establishing a Pharmacy Bundle and the Role of a Rounding Pharmacist on New Units
Some of the units implementing care coordination teams, such as neurology, did not previously have a pharmacist rounding on those units. Furthermore, these units had a high patient census (eg, 60 patients), which made it difficult for one pharmacist to clinically evaluate every patient. Multiple specialty teams also admitted patients to a single unit, which made it challenging for the pharmacist to develop strong working relationships with providers. As such, rounding pharmacists deployed to those units had difficulty establishing their role on the team, especially for those pharmacists without or with only 1 year of postgraduate training. To address this issue, a PGY2-trained pharmacist rounded on the unit to assess which areas/teams had the greatest need for a pharmacist. Completing this needs assessment on these units allowed for the rounding pharmacist to more effectively use his/her time. It also allowed for a smoother transition from operational to rounding pharmacist by removing the burden of establishing a brand new role and identifying necessary tasks to be completed throughout the day.
We also discovered on these new care coordination units that our patient criteria for education and medication reconciliation were not universal. We developed and initiated our pharmacy bundle of services in a medical patient population. As we expanded these services to other patient care areas, the targeted list of medications/conditions changed. For example, surgical patients had a greater need for education around opioid therapy and complex bowel regimens while neurology patients needed education regarding antiepileptic regimens. Similarly, patients requiring medication reconciliation also changed. Nurses were performing medication reconciliation for patients with elective surgeries and had a system that worked for that population. Therefore, we did not need to focus efforts for this population around medication reconciliation and could shift our focus more towards medication education.
Optimizing the Delivery of Discharge Prescriptions
The Meds for Home workflow has been updated multiple times since implementation. These changes resulted from early and frequent meetings with nurses, case managers, providers, and the pharmacy team. The Meds for Home service uses an outpatient pharmacy located within the hospital that has high prescription volumes at baseline to fill discharge prescriptions. Due to the volume of out-patient prescriptions and unexpected discharges, delays in prescription delivery occurred. To improve efficiency, a separate workflow and space were designated for filling Meds for Home prescriptions. Initially, MHCs were visiting floors to pick-up and deliver prescriptions at set times (ie, 10 am, 2 pm, and 5 pm). Instead of using set pick-up and delivery times, the Meds for Home service now uses a rolling 2-hour turnaround time during service hours. Additionally, providers, case managers, and units were educated to provide discharge prescriptions, especially those requiring prior authorization, as early as possible to expedite service. By identifying these issues early in the process, we were able to develop a different strategy that worked for the units, providers, and pharmacy.
Lessons Learned
The time of transition from one level of care to another is a vulnerable time for patients, as it is a time when medication-related problems often arise. In an elderly patient population, one study demonstrated that contributing factors for medication discrepancies following hospital discharge included unintended nonadherence and inadequate discharge instructions, and patients experiencing a medication discrepancy were at a significantly higher risk of readmission [4]. Hospital readmissions have also been linked to a lack of adequate follow-up in the outpatient setting [5]. Pharmacists should become more involved in preventing medication-related problems during the times of transition by performing activities such as medication reconciliation, patient education, and assessment of patient outcomes post-discharge [6,7]. Studies have demonstrated that pharmacists are able to reduce medication-related adverse events during and after hospitalization by completing these activities [8–10]. Residency-trained pharmacists are well-equipped to provide these services and are needed to create new processes and models to meet the ever changing demands of health care payers and accrediting bodies. ASHP recommends pharmacists entering into careers in health systems be at least PGY1-trained while the American College of Clinical Pharmacy (ACCP) envisions all pharmacists involved in direct patient care complete residency training [11,12]. Health systems will continue to be challenged with transforming pharmacy models to allow for this influx of highly trained individuals in a time of budget constraints. Below, we describe the lessons we learned while implementing our pharmacy bundle of services and think are essential for other institutions to consider when initiating their own services.
Rethink the Role of the Pharmacist
As health systems acquire smaller hospitals, the role of the pharmacist may need to be redefined and reinvented. The responsibilities of a pharmacist in a large academic hospital may be different than those of a pharmacist with the same skill set in a community hospital. However, despite the difference in practice setting, the same core pharmacy services around medication use can still be deployed. Participation in transitions of care activities is a relatively new concept for many pharmacists as residency training programs traditionally focused on caring for patients within a defined setting such as the intensive care unit or ambulatory care. The pharmacy profession should define the role of the clinical pharmacist in order to make the incorporation of transitions of care responsibilities into job expectations easier for all. The ACCP outlines this need and sets forth recommendations for clinical pharmacists’ responsibilities within the health care team to include assessing patients and medication regimens, developing and implementing medication-related therapy plans, and evaluating clinical outcomes [13]. Pharmacy leadership organizations, including ASHP and ACCP, offer resources providing the vision of pharmacy practice and expectations for which institutions should be reaching. Pharmacy departments should use these resources to complete gap analyses of current processes and those envisioned for the future to help guide efforts for change at their own institutions.
Obtain Support Within Your Institution
Gaining support from hospital leadership for advancing pharmacists’ involvement in patient care is instrumental. Without leadership support at both the institutional and department of pharmacy levels, pharmacists with advanced training may be hindered from practicing at the top of their license. Furthermore, support by leadership of pharmacy residency programs and experiential student learning sites at the institution is also important. Pharmacy residents and students became indispensable in our model and allowed us to expand our reach to more patients. We used residents to cover additional teams that were previously uncovered by a rounding pharmacist and, along with students, provide medication reconciliation, patient education, and follow-up phone calls to more patients. Requiring participation in the pharmacy bundle of services for rotations also allowed us to train these individuals about the value of transitions of care and see the challenges patients face in gaining access to medications. In a survey of academic medical center executives, pharmacy directors, and pharmacists at 8 institutions, residents were noted to add value to the institution through decreasing drug-related errors and drug costs, expansion of clinical services, and enhancing opportunities for research [14].
Support from other disciplines is also essential. Collaborating with other disciplines should occur prior to, during, and beyond implementation. We collaborated with providers, nurses, case managers, social workers and many other disciplines during all phases of the process. Being inclusive during the planning process allowed everyone to understand each other’s role and to provide input on how we could work together to best utilize everyone’s resources. This multidisciplinary approach to developing pharmacy services also allowed an opportunity to collaborate on research and evaluate our processes with other disciplines.
Tracking interventions will demonstrate the value of pharmacists, technicians, and other pharmacy team members participating in these advanced roles. This information will be useful when justifying the practice model to hospital leadership and for recruiting new pharmacists, residents, and technicians to the institution. Additionally, defining both outcome (eg, 30-day readmission rates, HCAHPS scores) and process (eg, number of patient education sessions performed, number of medication discrepancies reconciled) measures upfront is important in order for those involved to understand how their work will be assessed. These data will be useful in determining whether the intervention is making an impact early on and allow for restructuring of the process if not.
Create Depth in Your Team While Engaging Current Resources
We spent a significant amount of time planning the implementation of our pharmacy bundle of services, collaborating with other disciplines, and training our pharmacy team members. We hired highly trained and competent people into new positions and ensured every-one clearly understood their responsibilities. This was a critical step in order to ensure we were providing optimal care to our patients and integrating leaders into our team. We also utilized our current workforce to fill new clinical rounding pharmacist or technician roles. For those pharmacists who had not completed a residency, we required the pharmacists to complete a compact training program similar to that required of our residents [1]. This training ensured that important services were being performed adequately by each rounding pharmacist. Similarly, technicians transitioning from a primarily medication dispensing role to a MHC or medication history role received extensive training to assist with developing their new skill set.
Creating relationships with an outpatient pharmacy is essential to ensure patients are discharged from the hospital on medications they can afford long-term. We are fortunate to have 5 outpatient pharmacies on the JHH campus that are under the Johns Hopkins Health System umbrella, which made collaboration between the inpatient and outpatient teams seamless. However, many hospitals may not be directly affiliated with an outpatient pharmacy with which to collaborate or may contract with a retail chain pharmacy. In the latter case, inpatient and outpatient pharmacies must work together to define roles around transitions of care and how to best serve the patient in a collaborative manner. If no onsite outpatient pharmacy exists, dedicated resources should be acquired to serve as a liaison between the inpatient team and the outpatient pharmacy. These resources may work through issues such as formulary preferences, prior authorization requests, and connecting the patient to the medication either through bedside delivery or filling at the patient’s community pharmacy. Community pharmacies recognize the cost benefit they could gain through 340B pricing and specialty drug dispensing when working in collaboration with healthcare systems. However, health systems must be aware that collaborating with outpatient pharmacy partnerships will create further challenges as providers ensure patient preference for use of a particular pharmacy is honored and cost-sharing is incorporated into models.
Continuously Reevaluate Your Services
As implementation of our pharmacy bundle of services began, meeting early and often was essential to identify issues and adjust our workflow to resolve those issues quickly. When the inpatient component of the pharmacy bundle of services was first implemented, rounding pharmacists and pharmacy leadership initially met on a weekly basis to provide feedback on the practice model and develop resolutions for any issues. However, it is important to also include other disciplines in the evaluation process. For the Meds for Home program, pharmacy leadership not only met with MHCs but also with providers, nurses, case managers, and social workers for feedback on how to improve the service. Although the workflow of our pharmacy bundle of services are more established, evaluations still occur albeit less frequently.
Conclusion
Pharmacists’ involvement in transitions of care should become part of the daily responsibility. Health systems should understand how efforts to expand pharmacists’ interventions align with overall hospital goals. Many hospitals may already have programs in place to help with transitions of care. Pharmacists can help expand current efforts through increased visibility to physicians and patients as well as collaboration with outpatient pharmacies to ensure medications are effective and affordable for patients long-term.
Note: The project described was supported by grant no. 1C1CMS331053-01-00 from the U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. The research presented was conducted by the awardee. Findings may or may not be consistent with or confirmed by the findings of the independent evaluation contractor.
Corresponding author: Vi Gilmore, PharmD, BCPS, Clinical Pharmacy Specialist, Internal Medicine, The Johns Hopkins Hospital, 600 N. Wolfe Street, Carnegie 180, Baltimore, MD 21287, [email protected].
Financial disclosures: None.
1. Gilmore V, Efird L, Fu D, et al. Implementation of transitions-of-care services through acute care and outpatient pharmacy collaboration. Am J Health Syst Pharm 2015;72:737–44.
2. American College of Clinical Pharmacy, Burke JM, Miller WA, et al. Clinical pharmacist competencies. Pharmacotherapy 2008;28:806–15.
3. American Society of Health-System Pharmacists. ASHP accreditation standard for postgraduate year one (PGY1) pharmacy residency programs. Available at www.ashp.org/DocLibrary/Accreditation/Newly-approved-PGY1-Standard-September-2014.pdf.
4. Coleman EA, Smith JD, Raha D, Min S. Posthospital medication discrepancies: prevalence and contributing factors. Arch Intern Med 2005:165:1842–7.
5. Jackson C, Shahsahebi M, Wedlake T, DuBard C. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med 2015;13:115–22.
6. American College of Clinical Pharmacy, Hume AL, Kirwin J, et al. Improving care transitions: current practice and future opportunities for pharmacists. Pharmacotherapy 2012;32:e326–37.
7. Cobaugh DJ, Amin A, Bookwalter T, et al. ASHP-SHM joint statement on hospitalist-pharmacist collaboration. Am J Health Syst Pharm 2008;65:260–3.
8. Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med 2006;166:565–71.
9. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization. Ann Intern Med 2009;150:178–87.
10. Murphy EM, Oxencis CJ, Klauck JA, et al. Medication reconciliation at an academic medical center: implementation of a comprehensive program from admission to discharge. Am J Health Syst Pharm 2009;66:2126–31.
11. Myers CE. ASHP Health-System Pharmacy 2015 Initiative. Am J Health-Syst Pharm 2004;61:657.
12. Murphy JE, Nappi JM, Bosso JA, et al. ACCP position statement. American College of Clinical Pharmacy’s vision of the future: postgraduate pharmacy residency training as a prerequisite for direct patient care. Pharmacotherapy 2006;26:
722–33.
13. Harris IM, Phillips B, Boyce E, et al. Clinical pharmacy should adopt a consistent process of direct patient care. Pharmacotherapy 2014;34:e133–48.
14. Fuller PD, Smith KM, Hinman RK, et al. Value of pharmacy residency training: a survey of the academic medical center perspective. Am J Health Syst Pharm 2012;69:158–65.
1. Gilmore V, Efird L, Fu D, et al. Implementation of transitions-of-care services through acute care and outpatient pharmacy collaboration. Am J Health Syst Pharm 2015;72:737–44.
2. American College of Clinical Pharmacy, Burke JM, Miller WA, et al. Clinical pharmacist competencies. Pharmacotherapy 2008;28:806–15.
3. American Society of Health-System Pharmacists. ASHP accreditation standard for postgraduate year one (PGY1) pharmacy residency programs. Available at www.ashp.org/DocLibrary/Accreditation/Newly-approved-PGY1-Standard-September-2014.pdf.
4. Coleman EA, Smith JD, Raha D, Min S. Posthospital medication discrepancies: prevalence and contributing factors. Arch Intern Med 2005:165:1842–7.
5. Jackson C, Shahsahebi M, Wedlake T, DuBard C. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med 2015;13:115–22.
6. American College of Clinical Pharmacy, Hume AL, Kirwin J, et al. Improving care transitions: current practice and future opportunities for pharmacists. Pharmacotherapy 2012;32:e326–37.
7. Cobaugh DJ, Amin A, Bookwalter T, et al. ASHP-SHM joint statement on hospitalist-pharmacist collaboration. Am J Health Syst Pharm 2008;65:260–3.
8. Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med 2006;166:565–71.
9. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization. Ann Intern Med 2009;150:178–87.
10. Murphy EM, Oxencis CJ, Klauck JA, et al. Medication reconciliation at an academic medical center: implementation of a comprehensive program from admission to discharge. Am J Health Syst Pharm 2009;66:2126–31.
11. Myers CE. ASHP Health-System Pharmacy 2015 Initiative. Am J Health-Syst Pharm 2004;61:657.
12. Murphy JE, Nappi JM, Bosso JA, et al. ACCP position statement. American College of Clinical Pharmacy’s vision of the future: postgraduate pharmacy residency training as a prerequisite for direct patient care. Pharmacotherapy 2006;26:
722–33.
13. Harris IM, Phillips B, Boyce E, et al. Clinical pharmacy should adopt a consistent process of direct patient care. Pharmacotherapy 2014;34:e133–48.
14. Fuller PD, Smith KM, Hinman RK, et al. Value of pharmacy residency training: a survey of the academic medical center perspective. Am J Health Syst Pharm 2012;69:158–65.
Group Visits for Discussing Advance Care Planning
Study Overview
Objective. To describe the feasibility of a primary care–based group visit model focused on advance care planning.
Design. Qualitative study.
Setting and participants. Participants were patients attending the Senior Clinic, a patient-centered medical home at the University of Colorado Hospital in Aurora, CO. Patients had to be aged 65, English speakers, and receiving primary care at the Clinic. Participants could be referred by their primary care clinician, a partner or friend, or self-refer in response to flyers. Clinicians were not asked to prioritize patients with poor health status or known end-of-life needs.
Intervention. Groups of patients met for 2 sessions (1 month apart), each 2 hours in length, facilitated by a geriatrician and a social worker. About 1 hour was spent on discussion of advance care planning concepts, including sharing experiences and considering values. Other time in the session was for introductions/rapport building, individual goal setting, and optional completion or directives and/or individual clinical visits. Facilitators were supported by a Facilitator’s Communication Guide and used educational materials and handouts with the group.
Main outcome measures. Researchers used the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework to evaluate the project.
Main results. Patients were referred by 10 out of 11 clinicians. Of 80 patients approached, 32 participated in 5 group visit cohorts (40% participation rate) and 27 participated in both sessions (84% retention rate). Mean age was 79 years; 59% of participants were female and 72% white. Most evaluated the group visit as better than usual clinic visits for discussing advance care planning. Patients reported increases in detailed advance care planning conversations after participating (19% to 41%, P = 0.02). Patients were willing to share personal values and challenges related to advance care planning and they initiated discussions about a broad range of relevant topics.
Conclusion. A group visit to facilitate discussions about advance care planning and increase patient engagement is feasible. This model warrants further evaluation for effectiveness in improving advance care planning outcomes for patients, clinicians, and the system.
Commentary
An understanding of patients’ care goals is an essential element of high-quality care, allowing clinicians to align the care provided with what is most important to the patient [1]. Existing evidence does not support the commonly held belief that communication about end-of-life issues increases patient distress [1]. Early discussions about goals of care are associated with better quality of life, reduced use of nonbeneficial medical care near death, enhanced goal-consistent care, positive family outcomes, and reduced costs; however, significant barriers to having advance care planning discussions exist [2], including communication issues and lack of appropriate counseling by clinicians in primary care. Clinicians cite limited time and lack of clinic-based support as factors that impede discussions with patients about advance care planning.
New models are being developed in order to facilitate the process. Group medical visits have been recognized as a useful and effective strategy for approaching patients [1]. The current study describes what the authorssay is the first advance care planning group visit, which they named the “Conversation Group Medical Visit” (CGMV). Its aim is to engage patients in a discussion of key advance care planning concepts and support patient-initiated advance care planning actions, such as choosing surrogate decision makers, deciding on preferences during serious illness, discussing preferences with decision makers and health care providers, and documenting advance directives in the electronic health record [3].
As part of the group medical visits, participants receive an agenda, a personal copy of their EHR highlighting current advance care planning documentation, if any, and a blank medical durable power of attorney form. Facilitators use educational materials including videos from the PREPARE website (prepareforyourcare.org) that demonstrate a family’s conversation, advance directives, and various degrees of flexibility in the decision-making role. A Conversation Starter Kit is also used, which prompts individuals to think about their values and guides conversations about preferences.
Researcher used the RE-AIM framework [4] to evaluate the implementation of this group medical visit model. This framework looks at Reach (if older adults would participate in the medical group visits), Effectiveness (related to participant’s engagement in the conversations), the Adoption of the model by health providers (clinician referral patterns), Implementation (related to the attendance of patients at both clinical and group visits and aspects of planning discussed), and Maintenance (not assessed in this study).
There was a 40% participation rate. Reasons given for declining to participate were having participated in past advance care planning conversation or having an existing advance directive (30%), lack of interest (13%), illness (3.3%), lack of transportation (3.3%), and other/unknown (50%). Regarding effectiveness, the majority of patients rated the group visit as better than usual clinic visits for talking about advance care planning. Participants reported that they received useful information and felt comfortable talking about advance care planning in the group. In addition, participants reported finding it helpful to talk with others about advance care planning (92%). Participants also reported an overall increase (19% to 41%) in advance care planning conversations with family members after participating in the group visit (P =0.02). Participants said these conversations included enough details that they felt confident that their family members knew their wishes. Thus, enrollment in a CGMV led to improvements in conversation not only between patient and health care provider but also between family members.
Several themes were identified during discussions. Patients shared personal values and challenges related to advance care planning. Also, the facilitated discussions introduced key advance care planning concepts and encouraged patients to share related experiences, questions, successes, and challenges in regards to these topics. An interesting finding was that patients in groups of 4 or 5 seemed less engaged in the discussion than those in groups of 7 to 9 patients.
Applications for Clinical Practice
This novel strategy to faciliate discussions about advance care planning showed promising results and appears feasible, but further study is needed to evaluate the model. It may prove useful as a new model of advance care planning in primary care. Further longitudinal research is encouraged.
—Paloma Cesar de Sales, BS, RN, MS
1. Bernacki RE, Block SD; American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med 2014;174:1994–2003.
2. Lum HD, Sudore RL, Bekelman DB. Advance care planning in the elderly. Med Clin North Am 2015;99:391–403.
3. Fried TR, Bullock K, Iannone L, O’Leary JR. Understanding advance care planning as a process of health behavior change. J Am Geriatr Soc 2009;57:1547–55.
4. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322–7.
Study Overview
Objective. To describe the feasibility of a primary care–based group visit model focused on advance care planning.
Design. Qualitative study.
Setting and participants. Participants were patients attending the Senior Clinic, a patient-centered medical home at the University of Colorado Hospital in Aurora, CO. Patients had to be aged 65, English speakers, and receiving primary care at the Clinic. Participants could be referred by their primary care clinician, a partner or friend, or self-refer in response to flyers. Clinicians were not asked to prioritize patients with poor health status or known end-of-life needs.
Intervention. Groups of patients met for 2 sessions (1 month apart), each 2 hours in length, facilitated by a geriatrician and a social worker. About 1 hour was spent on discussion of advance care planning concepts, including sharing experiences and considering values. Other time in the session was for introductions/rapport building, individual goal setting, and optional completion or directives and/or individual clinical visits. Facilitators were supported by a Facilitator’s Communication Guide and used educational materials and handouts with the group.
Main outcome measures. Researchers used the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework to evaluate the project.
Main results. Patients were referred by 10 out of 11 clinicians. Of 80 patients approached, 32 participated in 5 group visit cohorts (40% participation rate) and 27 participated in both sessions (84% retention rate). Mean age was 79 years; 59% of participants were female and 72% white. Most evaluated the group visit as better than usual clinic visits for discussing advance care planning. Patients reported increases in detailed advance care planning conversations after participating (19% to 41%, P = 0.02). Patients were willing to share personal values and challenges related to advance care planning and they initiated discussions about a broad range of relevant topics.
Conclusion. A group visit to facilitate discussions about advance care planning and increase patient engagement is feasible. This model warrants further evaluation for effectiveness in improving advance care planning outcomes for patients, clinicians, and the system.
Commentary
An understanding of patients’ care goals is an essential element of high-quality care, allowing clinicians to align the care provided with what is most important to the patient [1]. Existing evidence does not support the commonly held belief that communication about end-of-life issues increases patient distress [1]. Early discussions about goals of care are associated with better quality of life, reduced use of nonbeneficial medical care near death, enhanced goal-consistent care, positive family outcomes, and reduced costs; however, significant barriers to having advance care planning discussions exist [2], including communication issues and lack of appropriate counseling by clinicians in primary care. Clinicians cite limited time and lack of clinic-based support as factors that impede discussions with patients about advance care planning.
New models are being developed in order to facilitate the process. Group medical visits have been recognized as a useful and effective strategy for approaching patients [1]. The current study describes what the authorssay is the first advance care planning group visit, which they named the “Conversation Group Medical Visit” (CGMV). Its aim is to engage patients in a discussion of key advance care planning concepts and support patient-initiated advance care planning actions, such as choosing surrogate decision makers, deciding on preferences during serious illness, discussing preferences with decision makers and health care providers, and documenting advance directives in the electronic health record [3].
As part of the group medical visits, participants receive an agenda, a personal copy of their EHR highlighting current advance care planning documentation, if any, and a blank medical durable power of attorney form. Facilitators use educational materials including videos from the PREPARE website (prepareforyourcare.org) that demonstrate a family’s conversation, advance directives, and various degrees of flexibility in the decision-making role. A Conversation Starter Kit is also used, which prompts individuals to think about their values and guides conversations about preferences.
Researcher used the RE-AIM framework [4] to evaluate the implementation of this group medical visit model. This framework looks at Reach (if older adults would participate in the medical group visits), Effectiveness (related to participant’s engagement in the conversations), the Adoption of the model by health providers (clinician referral patterns), Implementation (related to the attendance of patients at both clinical and group visits and aspects of planning discussed), and Maintenance (not assessed in this study).
There was a 40% participation rate. Reasons given for declining to participate were having participated in past advance care planning conversation or having an existing advance directive (30%), lack of interest (13%), illness (3.3%), lack of transportation (3.3%), and other/unknown (50%). Regarding effectiveness, the majority of patients rated the group visit as better than usual clinic visits for talking about advance care planning. Participants reported that they received useful information and felt comfortable talking about advance care planning in the group. In addition, participants reported finding it helpful to talk with others about advance care planning (92%). Participants also reported an overall increase (19% to 41%) in advance care planning conversations with family members after participating in the group visit (P =0.02). Participants said these conversations included enough details that they felt confident that their family members knew their wishes. Thus, enrollment in a CGMV led to improvements in conversation not only between patient and health care provider but also between family members.
Several themes were identified during discussions. Patients shared personal values and challenges related to advance care planning. Also, the facilitated discussions introduced key advance care planning concepts and encouraged patients to share related experiences, questions, successes, and challenges in regards to these topics. An interesting finding was that patients in groups of 4 or 5 seemed less engaged in the discussion than those in groups of 7 to 9 patients.
Applications for Clinical Practice
This novel strategy to faciliate discussions about advance care planning showed promising results and appears feasible, but further study is needed to evaluate the model. It may prove useful as a new model of advance care planning in primary care. Further longitudinal research is encouraged.
—Paloma Cesar de Sales, BS, RN, MS
Study Overview
Objective. To describe the feasibility of a primary care–based group visit model focused on advance care planning.
Design. Qualitative study.
Setting and participants. Participants were patients attending the Senior Clinic, a patient-centered medical home at the University of Colorado Hospital in Aurora, CO. Patients had to be aged 65, English speakers, and receiving primary care at the Clinic. Participants could be referred by their primary care clinician, a partner or friend, or self-refer in response to flyers. Clinicians were not asked to prioritize patients with poor health status or known end-of-life needs.
Intervention. Groups of patients met for 2 sessions (1 month apart), each 2 hours in length, facilitated by a geriatrician and a social worker. About 1 hour was spent on discussion of advance care planning concepts, including sharing experiences and considering values. Other time in the session was for introductions/rapport building, individual goal setting, and optional completion or directives and/or individual clinical visits. Facilitators were supported by a Facilitator’s Communication Guide and used educational materials and handouts with the group.
Main outcome measures. Researchers used the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework to evaluate the project.
Main results. Patients were referred by 10 out of 11 clinicians. Of 80 patients approached, 32 participated in 5 group visit cohorts (40% participation rate) and 27 participated in both sessions (84% retention rate). Mean age was 79 years; 59% of participants were female and 72% white. Most evaluated the group visit as better than usual clinic visits for discussing advance care planning. Patients reported increases in detailed advance care planning conversations after participating (19% to 41%, P = 0.02). Patients were willing to share personal values and challenges related to advance care planning and they initiated discussions about a broad range of relevant topics.
Conclusion. A group visit to facilitate discussions about advance care planning and increase patient engagement is feasible. This model warrants further evaluation for effectiveness in improving advance care planning outcomes for patients, clinicians, and the system.
Commentary
An understanding of patients’ care goals is an essential element of high-quality care, allowing clinicians to align the care provided with what is most important to the patient [1]. Existing evidence does not support the commonly held belief that communication about end-of-life issues increases patient distress [1]. Early discussions about goals of care are associated with better quality of life, reduced use of nonbeneficial medical care near death, enhanced goal-consistent care, positive family outcomes, and reduced costs; however, significant barriers to having advance care planning discussions exist [2], including communication issues and lack of appropriate counseling by clinicians in primary care. Clinicians cite limited time and lack of clinic-based support as factors that impede discussions with patients about advance care planning.
New models are being developed in order to facilitate the process. Group medical visits have been recognized as a useful and effective strategy for approaching patients [1]. The current study describes what the authorssay is the first advance care planning group visit, which they named the “Conversation Group Medical Visit” (CGMV). Its aim is to engage patients in a discussion of key advance care planning concepts and support patient-initiated advance care planning actions, such as choosing surrogate decision makers, deciding on preferences during serious illness, discussing preferences with decision makers and health care providers, and documenting advance directives in the electronic health record [3].
As part of the group medical visits, participants receive an agenda, a personal copy of their EHR highlighting current advance care planning documentation, if any, and a blank medical durable power of attorney form. Facilitators use educational materials including videos from the PREPARE website (prepareforyourcare.org) that demonstrate a family’s conversation, advance directives, and various degrees of flexibility in the decision-making role. A Conversation Starter Kit is also used, which prompts individuals to think about their values and guides conversations about preferences.
Researcher used the RE-AIM framework [4] to evaluate the implementation of this group medical visit model. This framework looks at Reach (if older adults would participate in the medical group visits), Effectiveness (related to participant’s engagement in the conversations), the Adoption of the model by health providers (clinician referral patterns), Implementation (related to the attendance of patients at both clinical and group visits and aspects of planning discussed), and Maintenance (not assessed in this study).
There was a 40% participation rate. Reasons given for declining to participate were having participated in past advance care planning conversation or having an existing advance directive (30%), lack of interest (13%), illness (3.3%), lack of transportation (3.3%), and other/unknown (50%). Regarding effectiveness, the majority of patients rated the group visit as better than usual clinic visits for talking about advance care planning. Participants reported that they received useful information and felt comfortable talking about advance care planning in the group. In addition, participants reported finding it helpful to talk with others about advance care planning (92%). Participants also reported an overall increase (19% to 41%) in advance care planning conversations with family members after participating in the group visit (P =0.02). Participants said these conversations included enough details that they felt confident that their family members knew their wishes. Thus, enrollment in a CGMV led to improvements in conversation not only between patient and health care provider but also between family members.
Several themes were identified during discussions. Patients shared personal values and challenges related to advance care planning. Also, the facilitated discussions introduced key advance care planning concepts and encouraged patients to share related experiences, questions, successes, and challenges in regards to these topics. An interesting finding was that patients in groups of 4 or 5 seemed less engaged in the discussion than those in groups of 7 to 9 patients.
Applications for Clinical Practice
This novel strategy to faciliate discussions about advance care planning showed promising results and appears feasible, but further study is needed to evaluate the model. It may prove useful as a new model of advance care planning in primary care. Further longitudinal research is encouraged.
—Paloma Cesar de Sales, BS, RN, MS
1. Bernacki RE, Block SD; American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med 2014;174:1994–2003.
2. Lum HD, Sudore RL, Bekelman DB. Advance care planning in the elderly. Med Clin North Am 2015;99:391–403.
3. Fried TR, Bullock K, Iannone L, O’Leary JR. Understanding advance care planning as a process of health behavior change. J Am Geriatr Soc 2009;57:1547–55.
4. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322–7.
1. Bernacki RE, Block SD; American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med 2014;174:1994–2003.
2. Lum HD, Sudore RL, Bekelman DB. Advance care planning in the elderly. Med Clin North Am 2015;99:391–403.
3. Fried TR, Bullock K, Iannone L, O’Leary JR. Understanding advance care planning as a process of health behavior change. J Am Geriatr Soc 2009;57:1547–55.
4. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322–7.
Acupuncture for Menopausal Vasomotor Symptoms
Study Overview
Objective. To examine the effects of acupuncture on vasomotor symptoms (VMS) and quality of life in perimenopausal and postmenopausal women.
Design. Pragmatic randomized controlled trial.
Setting and participants. Participants were perimenopausal and postmenopausal women aged 45 to 60 years who had 4 or more VMS episodes a day. Women were excluded if they had initiated or changed a dose of any VMS treatment in the 4 weeks prior to the study, initiated or changed the dose of an antidepressant in the prior 3 months, had received acupuncture in the prior 4 weeks, self-reported their health as poor or fair, or had a diagnosis of hemophilia. The study was conducted at the Wake Forest School of Medicine and the Chapel Hill Doctors Healthcare Center in North Carolina with women recruited from the community. Potential participants completed a 2-week hot flash diary to establish that they met the eligibility criteria of 4 or more hot flashes a day.
Intervention. Eligible participants were randomized to either the experimental group, who received up to 20 acupuncture treatments over a 6-month period, or a waitlist control group who received usual care for 6 months followed by the same 6 months of acupuncture treatment received by the experimental group. The researchers decided not to use sham acupuncture in the control group because outside of the experiment women would not receive sham acupuncture and because it has been shown to have an effect on menopausal symptoms in other studies.
Participants could receive up to 20 acupuncture treatments from 1 of the 4 study licensed acupuncturists over a period of 6 months. The acupuncturist assessed the participant and made a traditional Chinese medicine diagnosis to guide treatment at the initial and each subsequent visit. During treatment, acupuncture needles were inserted 0.5 to 3 cm through the skin to achieve a “de Qi” sensation, which is a sensation of heaviness, numbness, soreness, or distention at the insertion site. Acupuncturists were permitted to administer additional acupuncture-related treatments with the exception of the use of Chinese herbal remedies. Additionally, participants were permitted to start other treatments, and 11 women in the acupuncture group and 2 women in the control group started other behavioral treatments during the study.
Main outcome measures. The primary outcome measure was the frequency and severity of hot flashes and night sweats, measured using the Daily Diary of Hot Flashes (DDHF). Secondary measures were the following quality of life indicators: hot flash interference (the degree to which hot flashes interfered with specific daily activities), measured using the Hot Flash-related Daily Interference Scale; sleep quality, measured using the Pittsburgh Sleep Quality Index (PSQI) and the PROMIS Sleep Disturbance short form; menopause related symptoms other than VMS, measured using the Women’s Health Questionaire (WHQ); depression, measured using the short form of the Center for Epidemiologic Studies Depression scale (CESD-10); anxiety, measured using the General Anxiety Disorder (GAD-7) and the PROMIS Anxiety short form; perceived stress, measured using the Perceived Stress Scale (PSS); and health-related quality of life (HRQOL), measured using a global visual analog scale (VAS) and the Physical and Mental Health Component scores of the Medical Outcomes Study short form health survey (SF-36).
Main results. The final sample size was 209 women, with 170 randomized to the acupuncture group and 39 to the control group. There were no significant differences between the groups at baseline. The retention rate was 89% at 6 months and 84% at 12 months. At 6 months there was a 36.7% decrease VMS frequency in the acupuncture group compared to a 6.0% increase in the control group (P < 0.001). At 12 months the decrease in VMS frequency was 29.5% in the acupuncture group. The control group began acupuncture at 6 months and by 12 months the frequency of VMS in this group was 31.0% less than at baseline (P < 0.001). Overall, the maximal effect was achieved at week 7 with a median of 8 acupuncture treatments. Sensitivity analysis indicated that there were no differences in effect in those who started other behavioral treatments during this period. There were also significant improvements in scores on the hot flash interference scale (P < 0.001), fewer sleep problems on the sleep measures, and fewer symptoms on the WHQ for women in the acupuncture group and these effects were maintained at 12 months. In addition, similar results were found in the control group after they initiated acupuncture at 6 months.
Conclusion. Overall, acupuncture resulted in significant and sustained improvements in VMS and quality of life measures.
Commentary
More than half of women will experience frequent VMS beginning with the menopause transition [1] and lasting an average of 7.4 years [2]. The effect of VMS on women’s quality of life is considerable, including anxiety, stress, decreased energy, sleep disruption and interference with leisure, social, and work activities [3,4]. Estrogen therapy remains the most effective therapy for VMS; however, its use is contraindicated in many women and duration of use is limited [5]. Therefore, safe and effective alternate therapies are needed.
Acupuncture is a traditional Chinese medicine therapy that has gained popularity in recent years for therapeutic management of many conditions, including pain, nausea related to pregnancy or chemotherapy, anxiety, headache, and addiction. Evidence regarding effectiveness has been equivocal, with studies of its effectiveness in some conditions, such as nausea and dental pain, showing strong positive results while evidence for its use in other conditions is lacking or inconsistent [6]. There have been consistent positive findings in prior research of the use of acupuncture to reduce the severity and frequency of VMS, however, according to the authors of this study, little is known about the long-term effects or the effect on quality of life. Additionally, most studies use sham acupuncture in the control group, which would not be offered to women outside a study protocol and has been shown to have a physiological effect of its own. Therefore, the authors conducted a pragmatic randomized control trial; designing the intervention so that it more closely reflected what happens in a real world clinical setting, to examine the overall effects and effect on quality of life measures.
The results of this study were a significant positive effect of acupuncture on the frequency and severity of VMS in the acupuncture group that was sustained over 12 months and improvements on all quality of life measures. There was also a significant effect in the control group when they received the intervention after the initial 6-month period. As the authors note, it is unclear if improvements in the quality of life indicators were a direct effect of the acupuncture or secondary to the relief of the vasomotor symptoms. Its use in women who experience other menopause-related symptoms, such as mood disorders or sleep disruption, in the absence of VMS needs further study.
The authors compare their results with that of research on the use of selective serotonin reuptake inhibitors (SSRIs) for VMS, one of the more efficacious alternatives to hormone therapy. As they note, though the reduction was somewhat less than that found with SSRIs (for example 35% for acupuncture vs. 47% with escitalopram), the risk of adverse effects is much lower with acupuncture. The only reported adverse effects in this study were 2 women who reported pain during treatment and 1 who reported numbness while SSRIs are known to have significant adverse effects. In addition, the results in this study were sustained longer, until the final follow-up at 6 months, while women who used escitalopram relapsed three weeks after discontinuing the medication.
The use of a pragmatic design allows for more confidence that the findings will translate to the real world setting. The number and timing of acupuncture treatments were determined by each woman with the acupuncturist as would happen in the clinical setting. In addition, the initiation of other therapies during the treatment stage was allowed, with 11 women in the acupuncture group and 2 women in the treatment group starting other behavioral interventions during that time. Though this approach has a small chance of introducing confounding variables, sensitivity analysis indicated it did not. As such, this design results in a study that is an accurate reflection of the experience of women receiving acupuncture in the clinical setting and thus good external validity.
There were 2 limitations of note. Though retention was excellent, 89% and 84% for the acupuncture and control group respectively, it is unknown if the women who dropped out did so due to lack of improvement, in which case the actual reduction in VMS would have been less than reported. Additionally, the use of self-report (diaries) of VMS can be unreliable and biased.
Applications for Clinical Practice
The results of this study indicate that acupuncture offers women a safe and effective therapy for VMS. The optimal dose appears to be 8 treatments. Clinicians should consider it as a first-line treatment for women with moderate to severe VMS who have contraindications to hormone therapy and before prescribing SSRI therapy, which carries the potential for significant adverse effects.
—Karen Roush, PhD, RN
1. Gold EB, Colvin A, Avis N, Bromberger J, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women’s health across the nation. Am J Public Health 2006;96:1226–35.
2. Avis NE, Crawford SL, Greendale G, et al; Study of Women’s Health Across the Nation. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med 2015;175:531–9.
3. Williams RE, Levine KB, Kalilani L, et al. Menopause-specific questionnaire assessment in US population-based study shows negative impact on health-related quality of life. Maturitas 2009;62:153–9.
4. Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: a comprehensive review. Health Qual Life Outcomes 2005;3:47.
5. North American Menopause Society. Treatment of menopause-associated vasomotor symptoms: position statement of The North American Menopause Society. Menopause 2004;11:11–33.
6. Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med 2002;136:374–83.
Study Overview
Objective. To examine the effects of acupuncture on vasomotor symptoms (VMS) and quality of life in perimenopausal and postmenopausal women.
Design. Pragmatic randomized controlled trial.
Setting and participants. Participants were perimenopausal and postmenopausal women aged 45 to 60 years who had 4 or more VMS episodes a day. Women were excluded if they had initiated or changed a dose of any VMS treatment in the 4 weeks prior to the study, initiated or changed the dose of an antidepressant in the prior 3 months, had received acupuncture in the prior 4 weeks, self-reported their health as poor or fair, or had a diagnosis of hemophilia. The study was conducted at the Wake Forest School of Medicine and the Chapel Hill Doctors Healthcare Center in North Carolina with women recruited from the community. Potential participants completed a 2-week hot flash diary to establish that they met the eligibility criteria of 4 or more hot flashes a day.
Intervention. Eligible participants were randomized to either the experimental group, who received up to 20 acupuncture treatments over a 6-month period, or a waitlist control group who received usual care for 6 months followed by the same 6 months of acupuncture treatment received by the experimental group. The researchers decided not to use sham acupuncture in the control group because outside of the experiment women would not receive sham acupuncture and because it has been shown to have an effect on menopausal symptoms in other studies.
Participants could receive up to 20 acupuncture treatments from 1 of the 4 study licensed acupuncturists over a period of 6 months. The acupuncturist assessed the participant and made a traditional Chinese medicine diagnosis to guide treatment at the initial and each subsequent visit. During treatment, acupuncture needles were inserted 0.5 to 3 cm through the skin to achieve a “de Qi” sensation, which is a sensation of heaviness, numbness, soreness, or distention at the insertion site. Acupuncturists were permitted to administer additional acupuncture-related treatments with the exception of the use of Chinese herbal remedies. Additionally, participants were permitted to start other treatments, and 11 women in the acupuncture group and 2 women in the control group started other behavioral treatments during the study.
Main outcome measures. The primary outcome measure was the frequency and severity of hot flashes and night sweats, measured using the Daily Diary of Hot Flashes (DDHF). Secondary measures were the following quality of life indicators: hot flash interference (the degree to which hot flashes interfered with specific daily activities), measured using the Hot Flash-related Daily Interference Scale; sleep quality, measured using the Pittsburgh Sleep Quality Index (PSQI) and the PROMIS Sleep Disturbance short form; menopause related symptoms other than VMS, measured using the Women’s Health Questionaire (WHQ); depression, measured using the short form of the Center for Epidemiologic Studies Depression scale (CESD-10); anxiety, measured using the General Anxiety Disorder (GAD-7) and the PROMIS Anxiety short form; perceived stress, measured using the Perceived Stress Scale (PSS); and health-related quality of life (HRQOL), measured using a global visual analog scale (VAS) and the Physical and Mental Health Component scores of the Medical Outcomes Study short form health survey (SF-36).
Main results. The final sample size was 209 women, with 170 randomized to the acupuncture group and 39 to the control group. There were no significant differences between the groups at baseline. The retention rate was 89% at 6 months and 84% at 12 months. At 6 months there was a 36.7% decrease VMS frequency in the acupuncture group compared to a 6.0% increase in the control group (P < 0.001). At 12 months the decrease in VMS frequency was 29.5% in the acupuncture group. The control group began acupuncture at 6 months and by 12 months the frequency of VMS in this group was 31.0% less than at baseline (P < 0.001). Overall, the maximal effect was achieved at week 7 with a median of 8 acupuncture treatments. Sensitivity analysis indicated that there were no differences in effect in those who started other behavioral treatments during this period. There were also significant improvements in scores on the hot flash interference scale (P < 0.001), fewer sleep problems on the sleep measures, and fewer symptoms on the WHQ for women in the acupuncture group and these effects were maintained at 12 months. In addition, similar results were found in the control group after they initiated acupuncture at 6 months.
Conclusion. Overall, acupuncture resulted in significant and sustained improvements in VMS and quality of life measures.
Commentary
More than half of women will experience frequent VMS beginning with the menopause transition [1] and lasting an average of 7.4 years [2]. The effect of VMS on women’s quality of life is considerable, including anxiety, stress, decreased energy, sleep disruption and interference with leisure, social, and work activities [3,4]. Estrogen therapy remains the most effective therapy for VMS; however, its use is contraindicated in many women and duration of use is limited [5]. Therefore, safe and effective alternate therapies are needed.
Acupuncture is a traditional Chinese medicine therapy that has gained popularity in recent years for therapeutic management of many conditions, including pain, nausea related to pregnancy or chemotherapy, anxiety, headache, and addiction. Evidence regarding effectiveness has been equivocal, with studies of its effectiveness in some conditions, such as nausea and dental pain, showing strong positive results while evidence for its use in other conditions is lacking or inconsistent [6]. There have been consistent positive findings in prior research of the use of acupuncture to reduce the severity and frequency of VMS, however, according to the authors of this study, little is known about the long-term effects or the effect on quality of life. Additionally, most studies use sham acupuncture in the control group, which would not be offered to women outside a study protocol and has been shown to have a physiological effect of its own. Therefore, the authors conducted a pragmatic randomized control trial; designing the intervention so that it more closely reflected what happens in a real world clinical setting, to examine the overall effects and effect on quality of life measures.
The results of this study were a significant positive effect of acupuncture on the frequency and severity of VMS in the acupuncture group that was sustained over 12 months and improvements on all quality of life measures. There was also a significant effect in the control group when they received the intervention after the initial 6-month period. As the authors note, it is unclear if improvements in the quality of life indicators were a direct effect of the acupuncture or secondary to the relief of the vasomotor symptoms. Its use in women who experience other menopause-related symptoms, such as mood disorders or sleep disruption, in the absence of VMS needs further study.
The authors compare their results with that of research on the use of selective serotonin reuptake inhibitors (SSRIs) for VMS, one of the more efficacious alternatives to hormone therapy. As they note, though the reduction was somewhat less than that found with SSRIs (for example 35% for acupuncture vs. 47% with escitalopram), the risk of adverse effects is much lower with acupuncture. The only reported adverse effects in this study were 2 women who reported pain during treatment and 1 who reported numbness while SSRIs are known to have significant adverse effects. In addition, the results in this study were sustained longer, until the final follow-up at 6 months, while women who used escitalopram relapsed three weeks after discontinuing the medication.
The use of a pragmatic design allows for more confidence that the findings will translate to the real world setting. The number and timing of acupuncture treatments were determined by each woman with the acupuncturist as would happen in the clinical setting. In addition, the initiation of other therapies during the treatment stage was allowed, with 11 women in the acupuncture group and 2 women in the treatment group starting other behavioral interventions during that time. Though this approach has a small chance of introducing confounding variables, sensitivity analysis indicated it did not. As such, this design results in a study that is an accurate reflection of the experience of women receiving acupuncture in the clinical setting and thus good external validity.
There were 2 limitations of note. Though retention was excellent, 89% and 84% for the acupuncture and control group respectively, it is unknown if the women who dropped out did so due to lack of improvement, in which case the actual reduction in VMS would have been less than reported. Additionally, the use of self-report (diaries) of VMS can be unreliable and biased.
Applications for Clinical Practice
The results of this study indicate that acupuncture offers women a safe and effective therapy for VMS. The optimal dose appears to be 8 treatments. Clinicians should consider it as a first-line treatment for women with moderate to severe VMS who have contraindications to hormone therapy and before prescribing SSRI therapy, which carries the potential for significant adverse effects.
—Karen Roush, PhD, RN
Study Overview
Objective. To examine the effects of acupuncture on vasomotor symptoms (VMS) and quality of life in perimenopausal and postmenopausal women.
Design. Pragmatic randomized controlled trial.
Setting and participants. Participants were perimenopausal and postmenopausal women aged 45 to 60 years who had 4 or more VMS episodes a day. Women were excluded if they had initiated or changed a dose of any VMS treatment in the 4 weeks prior to the study, initiated or changed the dose of an antidepressant in the prior 3 months, had received acupuncture in the prior 4 weeks, self-reported their health as poor or fair, or had a diagnosis of hemophilia. The study was conducted at the Wake Forest School of Medicine and the Chapel Hill Doctors Healthcare Center in North Carolina with women recruited from the community. Potential participants completed a 2-week hot flash diary to establish that they met the eligibility criteria of 4 or more hot flashes a day.
Intervention. Eligible participants were randomized to either the experimental group, who received up to 20 acupuncture treatments over a 6-month period, or a waitlist control group who received usual care for 6 months followed by the same 6 months of acupuncture treatment received by the experimental group. The researchers decided not to use sham acupuncture in the control group because outside of the experiment women would not receive sham acupuncture and because it has been shown to have an effect on menopausal symptoms in other studies.
Participants could receive up to 20 acupuncture treatments from 1 of the 4 study licensed acupuncturists over a period of 6 months. The acupuncturist assessed the participant and made a traditional Chinese medicine diagnosis to guide treatment at the initial and each subsequent visit. During treatment, acupuncture needles were inserted 0.5 to 3 cm through the skin to achieve a “de Qi” sensation, which is a sensation of heaviness, numbness, soreness, or distention at the insertion site. Acupuncturists were permitted to administer additional acupuncture-related treatments with the exception of the use of Chinese herbal remedies. Additionally, participants were permitted to start other treatments, and 11 women in the acupuncture group and 2 women in the control group started other behavioral treatments during the study.
Main outcome measures. The primary outcome measure was the frequency and severity of hot flashes and night sweats, measured using the Daily Diary of Hot Flashes (DDHF). Secondary measures were the following quality of life indicators: hot flash interference (the degree to which hot flashes interfered with specific daily activities), measured using the Hot Flash-related Daily Interference Scale; sleep quality, measured using the Pittsburgh Sleep Quality Index (PSQI) and the PROMIS Sleep Disturbance short form; menopause related symptoms other than VMS, measured using the Women’s Health Questionaire (WHQ); depression, measured using the short form of the Center for Epidemiologic Studies Depression scale (CESD-10); anxiety, measured using the General Anxiety Disorder (GAD-7) and the PROMIS Anxiety short form; perceived stress, measured using the Perceived Stress Scale (PSS); and health-related quality of life (HRQOL), measured using a global visual analog scale (VAS) and the Physical and Mental Health Component scores of the Medical Outcomes Study short form health survey (SF-36).
Main results. The final sample size was 209 women, with 170 randomized to the acupuncture group and 39 to the control group. There were no significant differences between the groups at baseline. The retention rate was 89% at 6 months and 84% at 12 months. At 6 months there was a 36.7% decrease VMS frequency in the acupuncture group compared to a 6.0% increase in the control group (P < 0.001). At 12 months the decrease in VMS frequency was 29.5% in the acupuncture group. The control group began acupuncture at 6 months and by 12 months the frequency of VMS in this group was 31.0% less than at baseline (P < 0.001). Overall, the maximal effect was achieved at week 7 with a median of 8 acupuncture treatments. Sensitivity analysis indicated that there were no differences in effect in those who started other behavioral treatments during this period. There were also significant improvements in scores on the hot flash interference scale (P < 0.001), fewer sleep problems on the sleep measures, and fewer symptoms on the WHQ for women in the acupuncture group and these effects were maintained at 12 months. In addition, similar results were found in the control group after they initiated acupuncture at 6 months.
Conclusion. Overall, acupuncture resulted in significant and sustained improvements in VMS and quality of life measures.
Commentary
More than half of women will experience frequent VMS beginning with the menopause transition [1] and lasting an average of 7.4 years [2]. The effect of VMS on women’s quality of life is considerable, including anxiety, stress, decreased energy, sleep disruption and interference with leisure, social, and work activities [3,4]. Estrogen therapy remains the most effective therapy for VMS; however, its use is contraindicated in many women and duration of use is limited [5]. Therefore, safe and effective alternate therapies are needed.
Acupuncture is a traditional Chinese medicine therapy that has gained popularity in recent years for therapeutic management of many conditions, including pain, nausea related to pregnancy or chemotherapy, anxiety, headache, and addiction. Evidence regarding effectiveness has been equivocal, with studies of its effectiveness in some conditions, such as nausea and dental pain, showing strong positive results while evidence for its use in other conditions is lacking or inconsistent [6]. There have been consistent positive findings in prior research of the use of acupuncture to reduce the severity and frequency of VMS, however, according to the authors of this study, little is known about the long-term effects or the effect on quality of life. Additionally, most studies use sham acupuncture in the control group, which would not be offered to women outside a study protocol and has been shown to have a physiological effect of its own. Therefore, the authors conducted a pragmatic randomized control trial; designing the intervention so that it more closely reflected what happens in a real world clinical setting, to examine the overall effects and effect on quality of life measures.
The results of this study were a significant positive effect of acupuncture on the frequency and severity of VMS in the acupuncture group that was sustained over 12 months and improvements on all quality of life measures. There was also a significant effect in the control group when they received the intervention after the initial 6-month period. As the authors note, it is unclear if improvements in the quality of life indicators were a direct effect of the acupuncture or secondary to the relief of the vasomotor symptoms. Its use in women who experience other menopause-related symptoms, such as mood disorders or sleep disruption, in the absence of VMS needs further study.
The authors compare their results with that of research on the use of selective serotonin reuptake inhibitors (SSRIs) for VMS, one of the more efficacious alternatives to hormone therapy. As they note, though the reduction was somewhat less than that found with SSRIs (for example 35% for acupuncture vs. 47% with escitalopram), the risk of adverse effects is much lower with acupuncture. The only reported adverse effects in this study were 2 women who reported pain during treatment and 1 who reported numbness while SSRIs are known to have significant adverse effects. In addition, the results in this study were sustained longer, until the final follow-up at 6 months, while women who used escitalopram relapsed three weeks after discontinuing the medication.
The use of a pragmatic design allows for more confidence that the findings will translate to the real world setting. The number and timing of acupuncture treatments were determined by each woman with the acupuncturist as would happen in the clinical setting. In addition, the initiation of other therapies during the treatment stage was allowed, with 11 women in the acupuncture group and 2 women in the treatment group starting other behavioral interventions during that time. Though this approach has a small chance of introducing confounding variables, sensitivity analysis indicated it did not. As such, this design results in a study that is an accurate reflection of the experience of women receiving acupuncture in the clinical setting and thus good external validity.
There were 2 limitations of note. Though retention was excellent, 89% and 84% for the acupuncture and control group respectively, it is unknown if the women who dropped out did so due to lack of improvement, in which case the actual reduction in VMS would have been less than reported. Additionally, the use of self-report (diaries) of VMS can be unreliable and biased.
Applications for Clinical Practice
The results of this study indicate that acupuncture offers women a safe and effective therapy for VMS. The optimal dose appears to be 8 treatments. Clinicians should consider it as a first-line treatment for women with moderate to severe VMS who have contraindications to hormone therapy and before prescribing SSRI therapy, which carries the potential for significant adverse effects.
—Karen Roush, PhD, RN
1. Gold EB, Colvin A, Avis N, Bromberger J, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women’s health across the nation. Am J Public Health 2006;96:1226–35.
2. Avis NE, Crawford SL, Greendale G, et al; Study of Women’s Health Across the Nation. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med 2015;175:531–9.
3. Williams RE, Levine KB, Kalilani L, et al. Menopause-specific questionnaire assessment in US population-based study shows negative impact on health-related quality of life. Maturitas 2009;62:153–9.
4. Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: a comprehensive review. Health Qual Life Outcomes 2005;3:47.
5. North American Menopause Society. Treatment of menopause-associated vasomotor symptoms: position statement of The North American Menopause Society. Menopause 2004;11:11–33.
6. Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med 2002;136:374–83.
1. Gold EB, Colvin A, Avis N, Bromberger J, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women’s health across the nation. Am J Public Health 2006;96:1226–35.
2. Avis NE, Crawford SL, Greendale G, et al; Study of Women’s Health Across the Nation. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med 2015;175:531–9.
3. Williams RE, Levine KB, Kalilani L, et al. Menopause-specific questionnaire assessment in US population-based study shows negative impact on health-related quality of life. Maturitas 2009;62:153–9.
4. Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: a comprehensive review. Health Qual Life Outcomes 2005;3:47.
5. North American Menopause Society. Treatment of menopause-associated vasomotor symptoms: position statement of The North American Menopause Society. Menopause 2004;11:11–33.
6. Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med 2002;136:374–83.