User login
More weight loss linked with more benefit in STEP-HFpEF
AMSTERDAM – , including symptoms and physical limitations, exercise capacity, and inflammation, new analyses from the trial show.
At the annual congress of the European Society of Cardiology where he presented these new findings, Mikhail N. Kosiborod, MD, also posited that weight loss produced by weekly subcutaneous injections of 2.4 mg semaglutide (Wegovy) for 52 weeks in the study does not fully explain the multiple mechanisms that may be involved in producing this intervention’s effects in the STEP-HFpEF trial.
His report earlier at the congress and in a simultaneously published report of the trial’s primary outcomes established a role for medically induced weight loss in managing patients with obesity-phenotype HFpEF in a total of 529 randomized individuals with HFpEF and obesity but without diabetes.
The new analyses showed that for one of the two primary endpoints – the change from baseline in patients’ assessment on the Kansas City Cardiomyopathy Questionnaire Clinical Summary Score (KCCQ), the placebo-adjusted average change was a 16.1-point improvement in the 51 people with a 5%-10% weight loss during the 1-year study, and a 21.6-point improvement in the 58 who had at least a 20% weight loss, a between-group average 5.5 point difference that represents a clinically meaningful incremental improvement in this validated metric of symptoms and functional limitations.
Similar weight-related differences in benefit also occurred for the secondary outcomes of changes from baseline in 6-minute walk distance and in levels of C-reactive protein (CRP), a measure of systemic inflammation.
In an adjusted regression model, every 10% drop from baseline body weight was significantly linked with a 6.4-point improvement in KCCQ score, a 14.4 meter improvement in 6-minute walk distance, and a 28% relative reduction from baseline in CRP, reported Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
These new, prespecified analyses also showed that people with obesity and HFpEF responded roughly the same to semaglutide treatment compared with placebo-treated controls regardless of their starting body mass index, including people with class 1 (30-34 kg/m2), class 2 (35-39 kg/m2), and class 3 (≥ 40 kg/m2) obesity.
Simultaneously with Dr. Kosiborod’s report at the congress, these findings appeared in a report posted online in Nature Medicine.
Not every benefit was fully mediated by weight loss
These analyses “do not tell us how much of the benefit was mediated by weight loss, but the data do say that the more weight a person lost, the more benefit they got,” Dr. Kosiborod explained in an interview. “That is not the same as saying that everything is mediated by weight. It doesn’t say that nothing beyond weight loss matters.”
He and his associates are planning a mediation analysis of data from STEP-HFpEF that will more directly address this issue.
“It’s likely that people who lost more weight with semaglutide also had greater benefits from other effects of semaglutide at the same time. Weight loss is a good surrogate marker” for the range of effects that a person receives from treatment with semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, Dr. Kosiborod said.
“GLP-1 receptor agonists may have direct effects on atherosclerosis, as well as other effects that are uncoupled from weight loss,” such as proven anti-inflammatory effects, he added.
Another exploratory effect from semaglutide treatment in the study and reported by Dr. Kosiborod was a significant reduction in serum levels of N-terminal pro brain natriuretic peptide, an association never previously seen with weight loss in people with heart failure.
“The outcomes we’ve already seen in STEP-HFpEF were largely symptomatic, which are extraordinarily important, but there may be a completely different relationship between weight and clinical events,” said John E. Deanfield, PhD, a professor of cardiology at University College Hospital, London, who was not involved in the study.
Dr. Deanfield noted that important prognostic markers such as cholesterol levels and blood pressure reductions are usually not temporally related to weight loss. “The idea that [the benefits seen in STEP-HFpEF] are purely from weight loss is something we need to be careful about,” he said.
“My gut feeling is that at least 75% of the effect [in STEP-HFpEF} was due to weight loss,” said Naveed Sattar, PhD, professor of metabolic medicine at the University of Glasgow, who was not associated with the research.
STEP-HFpEF was funded by Novo Nordisk, the company that markets semaglutide (Wegovy). Dr. Kosiborod has been a consultant and adviser to, and has received honoraria from, Novo Nordisk. He has been a consultant to numerous other companies, received research grants from AstraZeneca, Boehringer Ingelheim, and Pfizer, honoraria from AstraZeneca, and is a stockholder in Artera Health and Saghmos Therapeutics. Dr. Deanfield has been a consultant to Novo Nordisk as well as to Aegerion, Amgen, Bayer, Boehringer Ingelheim, Merck, Novartis, Pfizer, Sanofi, and Takeda, and has received research funding from Aegerion, Colgate, MSD, Pfizer, and Roche. Dr. Sattar has been a consultant to Novo Nordisk as well as to Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Lilly, Novartis, Pfizer, and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
AMSTERDAM – , including symptoms and physical limitations, exercise capacity, and inflammation, new analyses from the trial show.
At the annual congress of the European Society of Cardiology where he presented these new findings, Mikhail N. Kosiborod, MD, also posited that weight loss produced by weekly subcutaneous injections of 2.4 mg semaglutide (Wegovy) for 52 weeks in the study does not fully explain the multiple mechanisms that may be involved in producing this intervention’s effects in the STEP-HFpEF trial.
His report earlier at the congress and in a simultaneously published report of the trial’s primary outcomes established a role for medically induced weight loss in managing patients with obesity-phenotype HFpEF in a total of 529 randomized individuals with HFpEF and obesity but without diabetes.
The new analyses showed that for one of the two primary endpoints – the change from baseline in patients’ assessment on the Kansas City Cardiomyopathy Questionnaire Clinical Summary Score (KCCQ), the placebo-adjusted average change was a 16.1-point improvement in the 51 people with a 5%-10% weight loss during the 1-year study, and a 21.6-point improvement in the 58 who had at least a 20% weight loss, a between-group average 5.5 point difference that represents a clinically meaningful incremental improvement in this validated metric of symptoms and functional limitations.
Similar weight-related differences in benefit also occurred for the secondary outcomes of changes from baseline in 6-minute walk distance and in levels of C-reactive protein (CRP), a measure of systemic inflammation.
In an adjusted regression model, every 10% drop from baseline body weight was significantly linked with a 6.4-point improvement in KCCQ score, a 14.4 meter improvement in 6-minute walk distance, and a 28% relative reduction from baseline in CRP, reported Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
These new, prespecified analyses also showed that people with obesity and HFpEF responded roughly the same to semaglutide treatment compared with placebo-treated controls regardless of their starting body mass index, including people with class 1 (30-34 kg/m2), class 2 (35-39 kg/m2), and class 3 (≥ 40 kg/m2) obesity.
Simultaneously with Dr. Kosiborod’s report at the congress, these findings appeared in a report posted online in Nature Medicine.
Not every benefit was fully mediated by weight loss
These analyses “do not tell us how much of the benefit was mediated by weight loss, but the data do say that the more weight a person lost, the more benefit they got,” Dr. Kosiborod explained in an interview. “That is not the same as saying that everything is mediated by weight. It doesn’t say that nothing beyond weight loss matters.”
He and his associates are planning a mediation analysis of data from STEP-HFpEF that will more directly address this issue.
“It’s likely that people who lost more weight with semaglutide also had greater benefits from other effects of semaglutide at the same time. Weight loss is a good surrogate marker” for the range of effects that a person receives from treatment with semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, Dr. Kosiborod said.
“GLP-1 receptor agonists may have direct effects on atherosclerosis, as well as other effects that are uncoupled from weight loss,” such as proven anti-inflammatory effects, he added.
Another exploratory effect from semaglutide treatment in the study and reported by Dr. Kosiborod was a significant reduction in serum levels of N-terminal pro brain natriuretic peptide, an association never previously seen with weight loss in people with heart failure.
“The outcomes we’ve already seen in STEP-HFpEF were largely symptomatic, which are extraordinarily important, but there may be a completely different relationship between weight and clinical events,” said John E. Deanfield, PhD, a professor of cardiology at University College Hospital, London, who was not involved in the study.
Dr. Deanfield noted that important prognostic markers such as cholesterol levels and blood pressure reductions are usually not temporally related to weight loss. “The idea that [the benefits seen in STEP-HFpEF] are purely from weight loss is something we need to be careful about,” he said.
“My gut feeling is that at least 75% of the effect [in STEP-HFpEF} was due to weight loss,” said Naveed Sattar, PhD, professor of metabolic medicine at the University of Glasgow, who was not associated with the research.
STEP-HFpEF was funded by Novo Nordisk, the company that markets semaglutide (Wegovy). Dr. Kosiborod has been a consultant and adviser to, and has received honoraria from, Novo Nordisk. He has been a consultant to numerous other companies, received research grants from AstraZeneca, Boehringer Ingelheim, and Pfizer, honoraria from AstraZeneca, and is a stockholder in Artera Health and Saghmos Therapeutics. Dr. Deanfield has been a consultant to Novo Nordisk as well as to Aegerion, Amgen, Bayer, Boehringer Ingelheim, Merck, Novartis, Pfizer, Sanofi, and Takeda, and has received research funding from Aegerion, Colgate, MSD, Pfizer, and Roche. Dr. Sattar has been a consultant to Novo Nordisk as well as to Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Lilly, Novartis, Pfizer, and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
AMSTERDAM – , including symptoms and physical limitations, exercise capacity, and inflammation, new analyses from the trial show.
At the annual congress of the European Society of Cardiology where he presented these new findings, Mikhail N. Kosiborod, MD, also posited that weight loss produced by weekly subcutaneous injections of 2.4 mg semaglutide (Wegovy) for 52 weeks in the study does not fully explain the multiple mechanisms that may be involved in producing this intervention’s effects in the STEP-HFpEF trial.
His report earlier at the congress and in a simultaneously published report of the trial’s primary outcomes established a role for medically induced weight loss in managing patients with obesity-phenotype HFpEF in a total of 529 randomized individuals with HFpEF and obesity but without diabetes.
The new analyses showed that for one of the two primary endpoints – the change from baseline in patients’ assessment on the Kansas City Cardiomyopathy Questionnaire Clinical Summary Score (KCCQ), the placebo-adjusted average change was a 16.1-point improvement in the 51 people with a 5%-10% weight loss during the 1-year study, and a 21.6-point improvement in the 58 who had at least a 20% weight loss, a between-group average 5.5 point difference that represents a clinically meaningful incremental improvement in this validated metric of symptoms and functional limitations.
Similar weight-related differences in benefit also occurred for the secondary outcomes of changes from baseline in 6-minute walk distance and in levels of C-reactive protein (CRP), a measure of systemic inflammation.
In an adjusted regression model, every 10% drop from baseline body weight was significantly linked with a 6.4-point improvement in KCCQ score, a 14.4 meter improvement in 6-minute walk distance, and a 28% relative reduction from baseline in CRP, reported Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
These new, prespecified analyses also showed that people with obesity and HFpEF responded roughly the same to semaglutide treatment compared with placebo-treated controls regardless of their starting body mass index, including people with class 1 (30-34 kg/m2), class 2 (35-39 kg/m2), and class 3 (≥ 40 kg/m2) obesity.
Simultaneously with Dr. Kosiborod’s report at the congress, these findings appeared in a report posted online in Nature Medicine.
Not every benefit was fully mediated by weight loss
These analyses “do not tell us how much of the benefit was mediated by weight loss, but the data do say that the more weight a person lost, the more benefit they got,” Dr. Kosiborod explained in an interview. “That is not the same as saying that everything is mediated by weight. It doesn’t say that nothing beyond weight loss matters.”
He and his associates are planning a mediation analysis of data from STEP-HFpEF that will more directly address this issue.
“It’s likely that people who lost more weight with semaglutide also had greater benefits from other effects of semaglutide at the same time. Weight loss is a good surrogate marker” for the range of effects that a person receives from treatment with semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, Dr. Kosiborod said.
“GLP-1 receptor agonists may have direct effects on atherosclerosis, as well as other effects that are uncoupled from weight loss,” such as proven anti-inflammatory effects, he added.
Another exploratory effect from semaglutide treatment in the study and reported by Dr. Kosiborod was a significant reduction in serum levels of N-terminal pro brain natriuretic peptide, an association never previously seen with weight loss in people with heart failure.
“The outcomes we’ve already seen in STEP-HFpEF were largely symptomatic, which are extraordinarily important, but there may be a completely different relationship between weight and clinical events,” said John E. Deanfield, PhD, a professor of cardiology at University College Hospital, London, who was not involved in the study.
Dr. Deanfield noted that important prognostic markers such as cholesterol levels and blood pressure reductions are usually not temporally related to weight loss. “The idea that [the benefits seen in STEP-HFpEF] are purely from weight loss is something we need to be careful about,” he said.
“My gut feeling is that at least 75% of the effect [in STEP-HFpEF} was due to weight loss,” said Naveed Sattar, PhD, professor of metabolic medicine at the University of Glasgow, who was not associated with the research.
STEP-HFpEF was funded by Novo Nordisk, the company that markets semaglutide (Wegovy). Dr. Kosiborod has been a consultant and adviser to, and has received honoraria from, Novo Nordisk. He has been a consultant to numerous other companies, received research grants from AstraZeneca, Boehringer Ingelheim, and Pfizer, honoraria from AstraZeneca, and is a stockholder in Artera Health and Saghmos Therapeutics. Dr. Deanfield has been a consultant to Novo Nordisk as well as to Aegerion, Amgen, Bayer, Boehringer Ingelheim, Merck, Novartis, Pfizer, Sanofi, and Takeda, and has received research funding from Aegerion, Colgate, MSD, Pfizer, and Roche. Dr. Sattar has been a consultant to Novo Nordisk as well as to Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Lilly, Novartis, Pfizer, and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
AT THE ESC CONGRESS 2023
Both too much and not enough sleep raises T2D risk
TOPLINE:
suggests an analysis of a Dutch study.
METHODOLOGY:
- Data on 5,561 participants aged 40–75 years from The Maastricht Study who completed the baseline survey between November 2010 and January 2018 and had full data available were included.
- Sleep duration was assessed as the in-bed time in minutes, using a median of 7 nights’ data from an activPAL3 (PAL Technologies) accelerometer, which is worn on the thigh.
- Glucose metabolism was determined via an oral glucose tolerance test and categorized as prediabetes or type 2 diabetes in line with World Health Organization diagnostic criteria.
- The association between sleep duration and type 2 diabetes was assessed on multivariate logistic regression analysis, taking into account a range of potential confounding factors.
TAKEAWAY:
- The mean age of the participants was 60.1 years, and there was an even split between men and women. In all, 832 had prediabetes and 1,341 type 2 diabetes, and the mean sleep duration was 8.3 hours.
- The results indicated there was a U-shaped relationship between sleep duration and type 2 diabetes, so that both long and short sleep durations increased the risk.
- In the fully adjusted model, a sleep duration of 5 hours was associated with an odds ratio for type 2 diabetes versus 8 hours sleep of 2.9. For a sleep duration of 12 hours, the odds ratio was 1.8.
- The association between sleep duration and diabetes was not significant.
IN PRACTICE:
The results “support the idea that sleep duration could be a relevant risk factor for type 2 diabetes independent of lifestyle risk factors, including diet, physical activity, smoking behavior, and alcohol consumption,” wrote the authors.
“These findings underpin the importance of promoting healthy sleep habits to avoid sleep deprivation,” they added.
STUDY DETAILS:
The research was led by Jeroen D. Albers, MSc, department of social medicine, Maastricht (the Netherlands) University, and published in Sleep Health. It is an analysis of The Maastricht Study.
LIMITATIONS:
The study is limited by its cross-sectional nature, particularly because there are “plausible causal paths between sleep duration and type 2 in both directions,” the authors note. The accelerometer used in the study also cannot reliably distinguish between waking and sleeping time in bed, with the potential for misclassification. Daytime naps were also not included, and long-term changes sleep patterns were not measured. In addition, it was not possible to control for some potential confounding factors.
DISCLOSURES:
The Maastricht Study was supported by the European Regional Development Fund via OP-Zuid, the Province of Limburg, the Dutch Ministry of Economic Affairs, Stichting De Weijerhorst, the Pearl String Initiative Diabetes, the School for Cardiovascular Diseases, the School for Public Health and Primary Care, the School for Nutrition and Translational Research in Metabolism, Stichting Annadal, Health Foundation Limburg, and unrestricted grants from Janssen-Cilag, Novo Nordisk, and Sanofi Aventis Netherlands. One author declares a relationship with Novo Nordisk outside the submitted work. No other relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
TOPLINE:
suggests an analysis of a Dutch study.
METHODOLOGY:
- Data on 5,561 participants aged 40–75 years from The Maastricht Study who completed the baseline survey between November 2010 and January 2018 and had full data available were included.
- Sleep duration was assessed as the in-bed time in minutes, using a median of 7 nights’ data from an activPAL3 (PAL Technologies) accelerometer, which is worn on the thigh.
- Glucose metabolism was determined via an oral glucose tolerance test and categorized as prediabetes or type 2 diabetes in line with World Health Organization diagnostic criteria.
- The association between sleep duration and type 2 diabetes was assessed on multivariate logistic regression analysis, taking into account a range of potential confounding factors.
TAKEAWAY:
- The mean age of the participants was 60.1 years, and there was an even split between men and women. In all, 832 had prediabetes and 1,341 type 2 diabetes, and the mean sleep duration was 8.3 hours.
- The results indicated there was a U-shaped relationship between sleep duration and type 2 diabetes, so that both long and short sleep durations increased the risk.
- In the fully adjusted model, a sleep duration of 5 hours was associated with an odds ratio for type 2 diabetes versus 8 hours sleep of 2.9. For a sleep duration of 12 hours, the odds ratio was 1.8.
- The association between sleep duration and diabetes was not significant.
IN PRACTICE:
The results “support the idea that sleep duration could be a relevant risk factor for type 2 diabetes independent of lifestyle risk factors, including diet, physical activity, smoking behavior, and alcohol consumption,” wrote the authors.
“These findings underpin the importance of promoting healthy sleep habits to avoid sleep deprivation,” they added.
STUDY DETAILS:
The research was led by Jeroen D. Albers, MSc, department of social medicine, Maastricht (the Netherlands) University, and published in Sleep Health. It is an analysis of The Maastricht Study.
LIMITATIONS:
The study is limited by its cross-sectional nature, particularly because there are “plausible causal paths between sleep duration and type 2 in both directions,” the authors note. The accelerometer used in the study also cannot reliably distinguish between waking and sleeping time in bed, with the potential for misclassification. Daytime naps were also not included, and long-term changes sleep patterns were not measured. In addition, it was not possible to control for some potential confounding factors.
DISCLOSURES:
The Maastricht Study was supported by the European Regional Development Fund via OP-Zuid, the Province of Limburg, the Dutch Ministry of Economic Affairs, Stichting De Weijerhorst, the Pearl String Initiative Diabetes, the School for Cardiovascular Diseases, the School for Public Health and Primary Care, the School for Nutrition and Translational Research in Metabolism, Stichting Annadal, Health Foundation Limburg, and unrestricted grants from Janssen-Cilag, Novo Nordisk, and Sanofi Aventis Netherlands. One author declares a relationship with Novo Nordisk outside the submitted work. No other relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
TOPLINE:
suggests an analysis of a Dutch study.
METHODOLOGY:
- Data on 5,561 participants aged 40–75 years from The Maastricht Study who completed the baseline survey between November 2010 and January 2018 and had full data available were included.
- Sleep duration was assessed as the in-bed time in minutes, using a median of 7 nights’ data from an activPAL3 (PAL Technologies) accelerometer, which is worn on the thigh.
- Glucose metabolism was determined via an oral glucose tolerance test and categorized as prediabetes or type 2 diabetes in line with World Health Organization diagnostic criteria.
- The association between sleep duration and type 2 diabetes was assessed on multivariate logistic regression analysis, taking into account a range of potential confounding factors.
TAKEAWAY:
- The mean age of the participants was 60.1 years, and there was an even split between men and women. In all, 832 had prediabetes and 1,341 type 2 diabetes, and the mean sleep duration was 8.3 hours.
- The results indicated there was a U-shaped relationship between sleep duration and type 2 diabetes, so that both long and short sleep durations increased the risk.
- In the fully adjusted model, a sleep duration of 5 hours was associated with an odds ratio for type 2 diabetes versus 8 hours sleep of 2.9. For a sleep duration of 12 hours, the odds ratio was 1.8.
- The association between sleep duration and diabetes was not significant.
IN PRACTICE:
The results “support the idea that sleep duration could be a relevant risk factor for type 2 diabetes independent of lifestyle risk factors, including diet, physical activity, smoking behavior, and alcohol consumption,” wrote the authors.
“These findings underpin the importance of promoting healthy sleep habits to avoid sleep deprivation,” they added.
STUDY DETAILS:
The research was led by Jeroen D. Albers, MSc, department of social medicine, Maastricht (the Netherlands) University, and published in Sleep Health. It is an analysis of The Maastricht Study.
LIMITATIONS:
The study is limited by its cross-sectional nature, particularly because there are “plausible causal paths between sleep duration and type 2 in both directions,” the authors note. The accelerometer used in the study also cannot reliably distinguish between waking and sleeping time in bed, with the potential for misclassification. Daytime naps were also not included, and long-term changes sleep patterns were not measured. In addition, it was not possible to control for some potential confounding factors.
DISCLOSURES:
The Maastricht Study was supported by the European Regional Development Fund via OP-Zuid, the Province of Limburg, the Dutch Ministry of Economic Affairs, Stichting De Weijerhorst, the Pearl String Initiative Diabetes, the School for Cardiovascular Diseases, the School for Public Health and Primary Care, the School for Nutrition and Translational Research in Metabolism, Stichting Annadal, Health Foundation Limburg, and unrestricted grants from Janssen-Cilag, Novo Nordisk, and Sanofi Aventis Netherlands. One author declares a relationship with Novo Nordisk outside the submitted work. No other relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
FROM SLEEP HEALTH
Severe COVID may cause long-term cellular changes: Study
The small study, published in Cell and funded by the National Institutes of Health, details how immune cells were analyzed through blood samples collected from 38 patients recovering from severe COVID and other critical illnesses, and from 19 healthy people. Researchers from Weill Cornell Medicine, New York, and The Jackson Laboratory for Genomic Medicine, Farmington, Conn., found through isolating hematopoietic stem cells that people recovering from severe bouts of COVID had changes to their DNA that were passed down to offspring cells.
The research team, led by Steven Josefowicz, PhD, of Weill Cornell’s pathology department, and Duygu Ucar, PhD, associate professor at The Jackson Laboratory for Genomic Medicine, discovered that this chain reaction of stem cell changes caused a boost in the production of monocytes. The authors found that, due to the innate cellular changes from a severe case of COVID, patients in recovery ended up producing a larger amount of inflammatory cytokines, rather than monocytes – distinct from samples collected from healthy patients and those recovering from other critical illnesses.
These changes to patients’ epigenetic landscapes were observed even a year after the initial COVID-19 infection. While the small participant pool meant that the research team could not establish a direct line between these innate changes and any ensuing health outcomes, the research provides us with clues as to why patients continue to struggle with inflammation and long COVID symptoms well after they recover.
While the authors reiterate the study’s limitations and hesitate to make any clear-cut associations between the results and long-term health outcomes, Wolfgang Leitner, PhD, from the NIH’s National Institute of Allergy and Infectious Diseases, predicts that long COVID can, at least in part, be explained by the changes in innate immune responses.
“Ideally, the authors would have had cells from each patient before they got infected, as a comparator, to see what the epigenetic landscape was before COVID changed it,” said Dr. Leitner. “Clear links between the severity of COVID and genetics were discovered already early in the pandemic and this paper should prompt follow-up studies that link mutations in immune genes with the epigenetic changes described here.”
Dr. Leitner said he had some initial predictions about the long-term impact of COVID-19, but he had not anticipated some of what the study’s findings now show.
“Unlike in the case of, for example, influenza, where the lungs go into ‘repair mode’ after the infection has been resolved – which leaves people susceptible to secondary infections for up to several months – this study shows that after severe COVID, the immune system remains in ‘emergency mode’ and in a heightened state of inflammation,” said Dr. Leitner.
“That further aggravates the problem the initial strong inflammation causes: even higher risk of autoimmune disease, but also, cancer.”
Commenting on the findings, Eric Topol, MD, editor-in-chief of Medscape Medical News, said the study presents “evidence that a key line of immune cells are essentially irrevocably, epigenetically altered and activated.
“You do not want to have this [COVID],” he added.
The study also highlights the researchers’ novel approach to isolating hematopoietic stem cells, found largely in bone marrow. This type of research has been limited in the past because of how costly and invasive it can be to analyze cells in bone marrow. But, by isolating and enriching hematopoietic stem cells, the team can decipher the full cellular diversity of the cells’ bone marrow counterparts.
“This revelation opened the doors to study, at single-cell resolution, how stem cells are affected upon infection and vaccination with a simple blood draw,” representatives from the Jackson lab said in a press release.
A version of this article appeared on Medscape.com.
The small study, published in Cell and funded by the National Institutes of Health, details how immune cells were analyzed through blood samples collected from 38 patients recovering from severe COVID and other critical illnesses, and from 19 healthy people. Researchers from Weill Cornell Medicine, New York, and The Jackson Laboratory for Genomic Medicine, Farmington, Conn., found through isolating hematopoietic stem cells that people recovering from severe bouts of COVID had changes to their DNA that were passed down to offspring cells.
The research team, led by Steven Josefowicz, PhD, of Weill Cornell’s pathology department, and Duygu Ucar, PhD, associate professor at The Jackson Laboratory for Genomic Medicine, discovered that this chain reaction of stem cell changes caused a boost in the production of monocytes. The authors found that, due to the innate cellular changes from a severe case of COVID, patients in recovery ended up producing a larger amount of inflammatory cytokines, rather than monocytes – distinct from samples collected from healthy patients and those recovering from other critical illnesses.
These changes to patients’ epigenetic landscapes were observed even a year after the initial COVID-19 infection. While the small participant pool meant that the research team could not establish a direct line between these innate changes and any ensuing health outcomes, the research provides us with clues as to why patients continue to struggle with inflammation and long COVID symptoms well after they recover.
While the authors reiterate the study’s limitations and hesitate to make any clear-cut associations between the results and long-term health outcomes, Wolfgang Leitner, PhD, from the NIH’s National Institute of Allergy and Infectious Diseases, predicts that long COVID can, at least in part, be explained by the changes in innate immune responses.
“Ideally, the authors would have had cells from each patient before they got infected, as a comparator, to see what the epigenetic landscape was before COVID changed it,” said Dr. Leitner. “Clear links between the severity of COVID and genetics were discovered already early in the pandemic and this paper should prompt follow-up studies that link mutations in immune genes with the epigenetic changes described here.”
Dr. Leitner said he had some initial predictions about the long-term impact of COVID-19, but he had not anticipated some of what the study’s findings now show.
“Unlike in the case of, for example, influenza, where the lungs go into ‘repair mode’ after the infection has been resolved – which leaves people susceptible to secondary infections for up to several months – this study shows that after severe COVID, the immune system remains in ‘emergency mode’ and in a heightened state of inflammation,” said Dr. Leitner.
“That further aggravates the problem the initial strong inflammation causes: even higher risk of autoimmune disease, but also, cancer.”
Commenting on the findings, Eric Topol, MD, editor-in-chief of Medscape Medical News, said the study presents “evidence that a key line of immune cells are essentially irrevocably, epigenetically altered and activated.
“You do not want to have this [COVID],” he added.
The study also highlights the researchers’ novel approach to isolating hematopoietic stem cells, found largely in bone marrow. This type of research has been limited in the past because of how costly and invasive it can be to analyze cells in bone marrow. But, by isolating and enriching hematopoietic stem cells, the team can decipher the full cellular diversity of the cells’ bone marrow counterparts.
“This revelation opened the doors to study, at single-cell resolution, how stem cells are affected upon infection and vaccination with a simple blood draw,” representatives from the Jackson lab said in a press release.
A version of this article appeared on Medscape.com.
The small study, published in Cell and funded by the National Institutes of Health, details how immune cells were analyzed through blood samples collected from 38 patients recovering from severe COVID and other critical illnesses, and from 19 healthy people. Researchers from Weill Cornell Medicine, New York, and The Jackson Laboratory for Genomic Medicine, Farmington, Conn., found through isolating hematopoietic stem cells that people recovering from severe bouts of COVID had changes to their DNA that were passed down to offspring cells.
The research team, led by Steven Josefowicz, PhD, of Weill Cornell’s pathology department, and Duygu Ucar, PhD, associate professor at The Jackson Laboratory for Genomic Medicine, discovered that this chain reaction of stem cell changes caused a boost in the production of monocytes. The authors found that, due to the innate cellular changes from a severe case of COVID, patients in recovery ended up producing a larger amount of inflammatory cytokines, rather than monocytes – distinct from samples collected from healthy patients and those recovering from other critical illnesses.
These changes to patients’ epigenetic landscapes were observed even a year after the initial COVID-19 infection. While the small participant pool meant that the research team could not establish a direct line between these innate changes and any ensuing health outcomes, the research provides us with clues as to why patients continue to struggle with inflammation and long COVID symptoms well after they recover.
While the authors reiterate the study’s limitations and hesitate to make any clear-cut associations between the results and long-term health outcomes, Wolfgang Leitner, PhD, from the NIH’s National Institute of Allergy and Infectious Diseases, predicts that long COVID can, at least in part, be explained by the changes in innate immune responses.
“Ideally, the authors would have had cells from each patient before they got infected, as a comparator, to see what the epigenetic landscape was before COVID changed it,” said Dr. Leitner. “Clear links between the severity of COVID and genetics were discovered already early in the pandemic and this paper should prompt follow-up studies that link mutations in immune genes with the epigenetic changes described here.”
Dr. Leitner said he had some initial predictions about the long-term impact of COVID-19, but he had not anticipated some of what the study’s findings now show.
“Unlike in the case of, for example, influenza, where the lungs go into ‘repair mode’ after the infection has been resolved – which leaves people susceptible to secondary infections for up to several months – this study shows that after severe COVID, the immune system remains in ‘emergency mode’ and in a heightened state of inflammation,” said Dr. Leitner.
“That further aggravates the problem the initial strong inflammation causes: even higher risk of autoimmune disease, but also, cancer.”
Commenting on the findings, Eric Topol, MD, editor-in-chief of Medscape Medical News, said the study presents “evidence that a key line of immune cells are essentially irrevocably, epigenetically altered and activated.
“You do not want to have this [COVID],” he added.
The study also highlights the researchers’ novel approach to isolating hematopoietic stem cells, found largely in bone marrow. This type of research has been limited in the past because of how costly and invasive it can be to analyze cells in bone marrow. But, by isolating and enriching hematopoietic stem cells, the team can decipher the full cellular diversity of the cells’ bone marrow counterparts.
“This revelation opened the doors to study, at single-cell resolution, how stem cells are affected upon infection and vaccination with a simple blood draw,” representatives from the Jackson lab said in a press release.
A version of this article appeared on Medscape.com.
FROM CELL
Cruel summer for medical students and Taylor Swift fans
Most medical students won’t see Taylor Swift perform her hit song “Cruel Summer,” but they will spend thousands of dollars on ERAS as they prepare for the 2024 residency match. Medical students applying for residency tend to be as stressed out as Swifties trying to score concert tickets. Aside from the expenses of residency applications, students also face an increasingly complex application process: a match algorithm many of them do not understand and major changes to the application process that most learn about right before the application cycle begins.
I have gone through two matches myself, one for internal medicine and one for neurology, and I have also guided students through the process for almost a decade as a dean of student affairs at a medical school. Every summer, the application process is filled with numerous changes, often with little, if any, warning for the students. One year, for example, a specialty required additional essays tailored to each program. Though this requirement may have helped programs discern which students are most enthusiastic about their programs, it also disadvantaged students working on busier rotations, strapped for time to write as many as 70 additional essays in a matter of weeks.
Other recent changes have included “signaling” programs, selecting preferred regions, and preinterview recordings for some specialties. In 2023, students cannot include more than 10 activities on their ERAS application. I have spoken to students at numerous medical schools concerned about the difficulty of selecting 10 activities out of dozens of meaningful pursuits throughout their journeys; this challenge is particularly acute for students who had other careers before entering medical school.
The stress continues to mount even after residency applications have been submitted. Students often feel tied to their phones because offers for residency interviews roll in day and night by email, and if they wait more than a few hours to respond, they’re often moved to a waiting list for their preferred interview date. One year, while we were rounding on patients, a student stepped away to schedule an interview; while doing so, he missed out on managing a patient who developed a neurologic emergency. Thankfully, many but not all specialties have put rules in place to allow students more time to think through interview offers. Having more time to think, even if it’s just 48 hours, may decrease stress, limit the negative impacts on medical education, and promote informed decisions during interview season.
To be sure, most changes are being made in an effort to improve the experience of the students and programs. But as with anything, the result has been a mix of good and bad. The transition to virtual interviews allowed students to apply more broadly to programs without worrying about travel costs. The move also benefits students with disabilities who face accessibility and other challenges with traveling. However, virtual interviews came with several downsides, including but not limited to an increased number of applications submitted (recall that this was also a benefit), interview hoarding, and challenges of connecting personally via virtual platform. Despite the virtual format, applicants increasingly are doing in-person second looks, which some worry may give those applicants an additional advantage over applicants who do not have the time or financial resources to travel for a second look. Despite these shortcomings, it is important that virtual interviews remain an option for those applicants who need it.
Another change, which has been extensively debated in medical education in recent years, was the switch to pass/fail on the USMLE Step 1 exam. Though this move decreased the stress students experienced in the first 2 years of medical school, it has resulted in a new challenge as many residency programs put more emphasis on USMLE Step 2. Many medical students feel they do not have a good gauge of their competitiveness until a few weeks before they submit their application, particularly those applicants attending medical schools that do not provide them with information regarding their class standing until right before they submit their applications.
By the time Swift’s Eras Tour ends in the summer of 2024, medical students will already have matched and started their residency programs. At the same time, a new batch of students will be entering the next year’s match. Though the number of anticipated changes may not reach the level of seismic activity caused by the Swifties at her Seattle concert, many medical students fear that the changes may be just like tectonic plates shifting the match process away from its original purpose: to provide an orderly and fair mechanism for matching the preferences of applicants for U.S. residency positions with the preferences of residency program directors.
Dr. Etienne is with WMCHealth Good Samaritan Hospital, New York, and New York Medical College. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Most medical students won’t see Taylor Swift perform her hit song “Cruel Summer,” but they will spend thousands of dollars on ERAS as they prepare for the 2024 residency match. Medical students applying for residency tend to be as stressed out as Swifties trying to score concert tickets. Aside from the expenses of residency applications, students also face an increasingly complex application process: a match algorithm many of them do not understand and major changes to the application process that most learn about right before the application cycle begins.
I have gone through two matches myself, one for internal medicine and one for neurology, and I have also guided students through the process for almost a decade as a dean of student affairs at a medical school. Every summer, the application process is filled with numerous changes, often with little, if any, warning for the students. One year, for example, a specialty required additional essays tailored to each program. Though this requirement may have helped programs discern which students are most enthusiastic about their programs, it also disadvantaged students working on busier rotations, strapped for time to write as many as 70 additional essays in a matter of weeks.
Other recent changes have included “signaling” programs, selecting preferred regions, and preinterview recordings for some specialties. In 2023, students cannot include more than 10 activities on their ERAS application. I have spoken to students at numerous medical schools concerned about the difficulty of selecting 10 activities out of dozens of meaningful pursuits throughout their journeys; this challenge is particularly acute for students who had other careers before entering medical school.
The stress continues to mount even after residency applications have been submitted. Students often feel tied to their phones because offers for residency interviews roll in day and night by email, and if they wait more than a few hours to respond, they’re often moved to a waiting list for their preferred interview date. One year, while we were rounding on patients, a student stepped away to schedule an interview; while doing so, he missed out on managing a patient who developed a neurologic emergency. Thankfully, many but not all specialties have put rules in place to allow students more time to think through interview offers. Having more time to think, even if it’s just 48 hours, may decrease stress, limit the negative impacts on medical education, and promote informed decisions during interview season.
To be sure, most changes are being made in an effort to improve the experience of the students and programs. But as with anything, the result has been a mix of good and bad. The transition to virtual interviews allowed students to apply more broadly to programs without worrying about travel costs. The move also benefits students with disabilities who face accessibility and other challenges with traveling. However, virtual interviews came with several downsides, including but not limited to an increased number of applications submitted (recall that this was also a benefit), interview hoarding, and challenges of connecting personally via virtual platform. Despite the virtual format, applicants increasingly are doing in-person second looks, which some worry may give those applicants an additional advantage over applicants who do not have the time or financial resources to travel for a second look. Despite these shortcomings, it is important that virtual interviews remain an option for those applicants who need it.
Another change, which has been extensively debated in medical education in recent years, was the switch to pass/fail on the USMLE Step 1 exam. Though this move decreased the stress students experienced in the first 2 years of medical school, it has resulted in a new challenge as many residency programs put more emphasis on USMLE Step 2. Many medical students feel they do not have a good gauge of their competitiveness until a few weeks before they submit their application, particularly those applicants attending medical schools that do not provide them with information regarding their class standing until right before they submit their applications.
By the time Swift’s Eras Tour ends in the summer of 2024, medical students will already have matched and started their residency programs. At the same time, a new batch of students will be entering the next year’s match. Though the number of anticipated changes may not reach the level of seismic activity caused by the Swifties at her Seattle concert, many medical students fear that the changes may be just like tectonic plates shifting the match process away from its original purpose: to provide an orderly and fair mechanism for matching the preferences of applicants for U.S. residency positions with the preferences of residency program directors.
Dr. Etienne is with WMCHealth Good Samaritan Hospital, New York, and New York Medical College. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Most medical students won’t see Taylor Swift perform her hit song “Cruel Summer,” but they will spend thousands of dollars on ERAS as they prepare for the 2024 residency match. Medical students applying for residency tend to be as stressed out as Swifties trying to score concert tickets. Aside from the expenses of residency applications, students also face an increasingly complex application process: a match algorithm many of them do not understand and major changes to the application process that most learn about right before the application cycle begins.
I have gone through two matches myself, one for internal medicine and one for neurology, and I have also guided students through the process for almost a decade as a dean of student affairs at a medical school. Every summer, the application process is filled with numerous changes, often with little, if any, warning for the students. One year, for example, a specialty required additional essays tailored to each program. Though this requirement may have helped programs discern which students are most enthusiastic about their programs, it also disadvantaged students working on busier rotations, strapped for time to write as many as 70 additional essays in a matter of weeks.
Other recent changes have included “signaling” programs, selecting preferred regions, and preinterview recordings for some specialties. In 2023, students cannot include more than 10 activities on their ERAS application. I have spoken to students at numerous medical schools concerned about the difficulty of selecting 10 activities out of dozens of meaningful pursuits throughout their journeys; this challenge is particularly acute for students who had other careers before entering medical school.
The stress continues to mount even after residency applications have been submitted. Students often feel tied to their phones because offers for residency interviews roll in day and night by email, and if they wait more than a few hours to respond, they’re often moved to a waiting list for their preferred interview date. One year, while we were rounding on patients, a student stepped away to schedule an interview; while doing so, he missed out on managing a patient who developed a neurologic emergency. Thankfully, many but not all specialties have put rules in place to allow students more time to think through interview offers. Having more time to think, even if it’s just 48 hours, may decrease stress, limit the negative impacts on medical education, and promote informed decisions during interview season.
To be sure, most changes are being made in an effort to improve the experience of the students and programs. But as with anything, the result has been a mix of good and bad. The transition to virtual interviews allowed students to apply more broadly to programs without worrying about travel costs. The move also benefits students with disabilities who face accessibility and other challenges with traveling. However, virtual interviews came with several downsides, including but not limited to an increased number of applications submitted (recall that this was also a benefit), interview hoarding, and challenges of connecting personally via virtual platform. Despite the virtual format, applicants increasingly are doing in-person second looks, which some worry may give those applicants an additional advantage over applicants who do not have the time or financial resources to travel for a second look. Despite these shortcomings, it is important that virtual interviews remain an option for those applicants who need it.
Another change, which has been extensively debated in medical education in recent years, was the switch to pass/fail on the USMLE Step 1 exam. Though this move decreased the stress students experienced in the first 2 years of medical school, it has resulted in a new challenge as many residency programs put more emphasis on USMLE Step 2. Many medical students feel they do not have a good gauge of their competitiveness until a few weeks before they submit their application, particularly those applicants attending medical schools that do not provide them with information regarding their class standing until right before they submit their applications.
By the time Swift’s Eras Tour ends in the summer of 2024, medical students will already have matched and started their residency programs. At the same time, a new batch of students will be entering the next year’s match. Though the number of anticipated changes may not reach the level of seismic activity caused by the Swifties at her Seattle concert, many medical students fear that the changes may be just like tectonic plates shifting the match process away from its original purpose: to provide an orderly and fair mechanism for matching the preferences of applicants for U.S. residency positions with the preferences of residency program directors.
Dr. Etienne is with WMCHealth Good Samaritan Hospital, New York, and New York Medical College. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
It’s not an assembly line
A lot of businesses benefit from being in private equity funds.
Health care isn’t one of them, and a recent report found that
This really shouldn’t surprise anyone. Such funds may offer glittering phrases like “improved technology” and “greater efficiency” but the bottom line is that they’re run by – and for – the shareholders. The majority of them aren’t going to be medical people or realize that you can’t run a medical practice like it’s a clothing retailer or electronic car manufacturer.
I’m not saying medicine isn’t a business – it is. I depend on my little practice to support three families, so keeping it in the black is important. But it also needs to run well to do that. Measures to increase revenue, like cutting my staff down (there are only two of them) or overbooking patients would seriously impact me effectively doing my part, which is playing doctor.
You can predict pretty accurately how long it will take to put a motor and bumper assembly on a specific model of car, but you can’t do that in medicine because people aren’t standardized. Even if you control variables such as same sex, age, and diagnosis, personalities vary widely, as do treatment decisions, questions they’ll have, and the “oh, another thing” factor.
That doesn’t happen at a bottling plant.
In the business model of health care, you’re hoping revenue will pay overhead and a reasonable salary for everyone. But when you add a private equity firm in, the shareholders also expect to be paid. Which means either revenue has to go up significantly, or costs have to be cut (layoffs, short staffing, reduced benefits, etc.), or a combination of both.
Regardless of which option is chosen, it isn’t good for the medical staff or the patients. Increasing the number of people seen in a given amount of time per doctor may be good for the shareholders, but it’s not good for the doctor or the person being cared for. Think of Lucy and Ethyl at the chocolate factory.
Even in an auto factory, if you speed up the rate of cars going through the assembly line, sooner or later mistakes will be made. Humans can’t keep up, and even robots will make errors if things aren’t aligned correctly, or are a few seconds ahead or behind the program. This is why they (hopefully) have quality control, to try and catch those things before they’re on the road.
Of course, cars are more easily fixable. When the mistake is found you repair or replace the part. You can’t do that as easily in people, and when serious mistakes happen it’s the doctor who’s held at fault – not the shareholders who pressured him or her to see patients faster and with less support.
Unfortunately, this is the way the current trend is going. The more people who are involved in the practice of medicine, in person or behind the scenes, the smaller each slice of the pie gets.
That’s not good for the patient, who’s the person at the center of it all and the reason why we’re here.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A lot of businesses benefit from being in private equity funds.
Health care isn’t one of them, and a recent report found that
This really shouldn’t surprise anyone. Such funds may offer glittering phrases like “improved technology” and “greater efficiency” but the bottom line is that they’re run by – and for – the shareholders. The majority of them aren’t going to be medical people or realize that you can’t run a medical practice like it’s a clothing retailer or electronic car manufacturer.
I’m not saying medicine isn’t a business – it is. I depend on my little practice to support three families, so keeping it in the black is important. But it also needs to run well to do that. Measures to increase revenue, like cutting my staff down (there are only two of them) or overbooking patients would seriously impact me effectively doing my part, which is playing doctor.
You can predict pretty accurately how long it will take to put a motor and bumper assembly on a specific model of car, but you can’t do that in medicine because people aren’t standardized. Even if you control variables such as same sex, age, and diagnosis, personalities vary widely, as do treatment decisions, questions they’ll have, and the “oh, another thing” factor.
That doesn’t happen at a bottling plant.
In the business model of health care, you’re hoping revenue will pay overhead and a reasonable salary for everyone. But when you add a private equity firm in, the shareholders also expect to be paid. Which means either revenue has to go up significantly, or costs have to be cut (layoffs, short staffing, reduced benefits, etc.), or a combination of both.
Regardless of which option is chosen, it isn’t good for the medical staff or the patients. Increasing the number of people seen in a given amount of time per doctor may be good for the shareholders, but it’s not good for the doctor or the person being cared for. Think of Lucy and Ethyl at the chocolate factory.
Even in an auto factory, if you speed up the rate of cars going through the assembly line, sooner or later mistakes will be made. Humans can’t keep up, and even robots will make errors if things aren’t aligned correctly, or are a few seconds ahead or behind the program. This is why they (hopefully) have quality control, to try and catch those things before they’re on the road.
Of course, cars are more easily fixable. When the mistake is found you repair or replace the part. You can’t do that as easily in people, and when serious mistakes happen it’s the doctor who’s held at fault – not the shareholders who pressured him or her to see patients faster and with less support.
Unfortunately, this is the way the current trend is going. The more people who are involved in the practice of medicine, in person or behind the scenes, the smaller each slice of the pie gets.
That’s not good for the patient, who’s the person at the center of it all and the reason why we’re here.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A lot of businesses benefit from being in private equity funds.
Health care isn’t one of them, and a recent report found that
This really shouldn’t surprise anyone. Such funds may offer glittering phrases like “improved technology” and “greater efficiency” but the bottom line is that they’re run by – and for – the shareholders. The majority of them aren’t going to be medical people or realize that you can’t run a medical practice like it’s a clothing retailer or electronic car manufacturer.
I’m not saying medicine isn’t a business – it is. I depend on my little practice to support three families, so keeping it in the black is important. But it also needs to run well to do that. Measures to increase revenue, like cutting my staff down (there are only two of them) or overbooking patients would seriously impact me effectively doing my part, which is playing doctor.
You can predict pretty accurately how long it will take to put a motor and bumper assembly on a specific model of car, but you can’t do that in medicine because people aren’t standardized. Even if you control variables such as same sex, age, and diagnosis, personalities vary widely, as do treatment decisions, questions they’ll have, and the “oh, another thing” factor.
That doesn’t happen at a bottling plant.
In the business model of health care, you’re hoping revenue will pay overhead and a reasonable salary for everyone. But when you add a private equity firm in, the shareholders also expect to be paid. Which means either revenue has to go up significantly, or costs have to be cut (layoffs, short staffing, reduced benefits, etc.), or a combination of both.
Regardless of which option is chosen, it isn’t good for the medical staff or the patients. Increasing the number of people seen in a given amount of time per doctor may be good for the shareholders, but it’s not good for the doctor or the person being cared for. Think of Lucy and Ethyl at the chocolate factory.
Even in an auto factory, if you speed up the rate of cars going through the assembly line, sooner or later mistakes will be made. Humans can’t keep up, and even robots will make errors if things aren’t aligned correctly, or are a few seconds ahead or behind the program. This is why they (hopefully) have quality control, to try and catch those things before they’re on the road.
Of course, cars are more easily fixable. When the mistake is found you repair or replace the part. You can’t do that as easily in people, and when serious mistakes happen it’s the doctor who’s held at fault – not the shareholders who pressured him or her to see patients faster and with less support.
Unfortunately, this is the way the current trend is going. The more people who are involved in the practice of medicine, in person or behind the scenes, the smaller each slice of the pie gets.
That’s not good for the patient, who’s the person at the center of it all and the reason why we’re here.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Inner lip erosions

The patient was having a flare of pemphigus vulgaris (PV), a rare and sometimes life-threatening acquired autoimmune blistering disease that affects the skin and/or mucosa. Ashkenazi Jewish patients and patients from Mediterranean and Middle Eastern countries are more likely to be affected.
In PV, acquired autoantibodies target the desmosomes that connect epithelial cells together, weakening the intercellular adhesion. It can affect skin, mucosa, or both. Patients present with fragile bullae or ulcers. The connections between the cells are often so damaged that rubbing on the skin creates a new blister called “Nikolsky sign.” In the mouth, bullae erode rapidly. Look for disease affecting the ocular conjunctiva or sclera, as well. PV can also occasionally affect the nasopharynx and esophagus, usually manifesting as hemoptysis, dysphagia, and nosebleeds with ulcer seen on endoscopy or otolaryngoscopy.
Although PV is often severe (and can warrant hospitalization when significant body surface area is involved), some patients may have few active lesions and can be managed safely as outpatients.
The diagnosis requires 2 biopsies and serum for indirect immunofluorescence. One biopsy (either by punch or shave to the upper dermis) is taken from the edge of a bulla or ulcer. Another biopsy (by punch or shave) is taken from nearby normal-looking skin or mucosa for testing the direct immunofluorescence pattern. In the mucosa, a punch biopsy may be left open or closed with absorbable sutures. A serum sample is taken for indirect immunofluorescence to differentiate pemphigus vulgaris from other forms of pemphigus.1
PV is treated by suppressing the immune system. Focal disease may be treated with super-potent topical steroids, including clobetasol 0.05% ointment. Even in the mouth, topical clobetasol 0.05% may be used off-label twice daily until control is achieved. When topical treatment is used in the mouth, advise patients to apply the clobetasol ointment to a piece of gauze and place the gauze (ointment side down) over affected areas for 20 to 30 minutes twice daily.
Patients with widespread or severe disease should be hospitalized. In severe cases, supportive wound care is provided, and treatment is aimed at immunosuppression. Systemic options include high-dose prednisone 0.5 to 1 mg/kg daily until clear, a steroid-sparing immunosuppressant such as mycophenolate mofetil up to 1000 mg bid, or rituximab in 1 of several regimens.
Three years prior to this patient’s visit, she had been successfully treated for PV with a course of rituximab. To treat the current flare, she was started on prednisone 60 mg/d. In addition, the plan was for her to complete 2 infusions of 1000 mg rituximab 2 weeks apart.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.
1. Didona, D, Schmidt, MF, Maglie, R, et al. Pemphigus and pemphigoids: clinical presentation, diagnosis and therapy. J Dtsch Dermatol Ges. 2023;1-20. doi: 10.1111/ddg.15174

The patient was having a flare of pemphigus vulgaris (PV), a rare and sometimes life-threatening acquired autoimmune blistering disease that affects the skin and/or mucosa. Ashkenazi Jewish patients and patients from Mediterranean and Middle Eastern countries are more likely to be affected.
In PV, acquired autoantibodies target the desmosomes that connect epithelial cells together, weakening the intercellular adhesion. It can affect skin, mucosa, or both. Patients present with fragile bullae or ulcers. The connections between the cells are often so damaged that rubbing on the skin creates a new blister called “Nikolsky sign.” In the mouth, bullae erode rapidly. Look for disease affecting the ocular conjunctiva or sclera, as well. PV can also occasionally affect the nasopharynx and esophagus, usually manifesting as hemoptysis, dysphagia, and nosebleeds with ulcer seen on endoscopy or otolaryngoscopy.
Although PV is often severe (and can warrant hospitalization when significant body surface area is involved), some patients may have few active lesions and can be managed safely as outpatients.
The diagnosis requires 2 biopsies and serum for indirect immunofluorescence. One biopsy (either by punch or shave to the upper dermis) is taken from the edge of a bulla or ulcer. Another biopsy (by punch or shave) is taken from nearby normal-looking skin or mucosa for testing the direct immunofluorescence pattern. In the mucosa, a punch biopsy may be left open or closed with absorbable sutures. A serum sample is taken for indirect immunofluorescence to differentiate pemphigus vulgaris from other forms of pemphigus.1
PV is treated by suppressing the immune system. Focal disease may be treated with super-potent topical steroids, including clobetasol 0.05% ointment. Even in the mouth, topical clobetasol 0.05% may be used off-label twice daily until control is achieved. When topical treatment is used in the mouth, advise patients to apply the clobetasol ointment to a piece of gauze and place the gauze (ointment side down) over affected areas for 20 to 30 minutes twice daily.
Patients with widespread or severe disease should be hospitalized. In severe cases, supportive wound care is provided, and treatment is aimed at immunosuppression. Systemic options include high-dose prednisone 0.5 to 1 mg/kg daily until clear, a steroid-sparing immunosuppressant such as mycophenolate mofetil up to 1000 mg bid, or rituximab in 1 of several regimens.
Three years prior to this patient’s visit, she had been successfully treated for PV with a course of rituximab. To treat the current flare, she was started on prednisone 60 mg/d. In addition, the plan was for her to complete 2 infusions of 1000 mg rituximab 2 weeks apart.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.

The patient was having a flare of pemphigus vulgaris (PV), a rare and sometimes life-threatening acquired autoimmune blistering disease that affects the skin and/or mucosa. Ashkenazi Jewish patients and patients from Mediterranean and Middle Eastern countries are more likely to be affected.
In PV, acquired autoantibodies target the desmosomes that connect epithelial cells together, weakening the intercellular adhesion. It can affect skin, mucosa, or both. Patients present with fragile bullae or ulcers. The connections between the cells are often so damaged that rubbing on the skin creates a new blister called “Nikolsky sign.” In the mouth, bullae erode rapidly. Look for disease affecting the ocular conjunctiva or sclera, as well. PV can also occasionally affect the nasopharynx and esophagus, usually manifesting as hemoptysis, dysphagia, and nosebleeds with ulcer seen on endoscopy or otolaryngoscopy.
Although PV is often severe (and can warrant hospitalization when significant body surface area is involved), some patients may have few active lesions and can be managed safely as outpatients.
The diagnosis requires 2 biopsies and serum for indirect immunofluorescence. One biopsy (either by punch or shave to the upper dermis) is taken from the edge of a bulla or ulcer. Another biopsy (by punch or shave) is taken from nearby normal-looking skin or mucosa for testing the direct immunofluorescence pattern. In the mucosa, a punch biopsy may be left open or closed with absorbable sutures. A serum sample is taken for indirect immunofluorescence to differentiate pemphigus vulgaris from other forms of pemphigus.1
PV is treated by suppressing the immune system. Focal disease may be treated with super-potent topical steroids, including clobetasol 0.05% ointment. Even in the mouth, topical clobetasol 0.05% may be used off-label twice daily until control is achieved. When topical treatment is used in the mouth, advise patients to apply the clobetasol ointment to a piece of gauze and place the gauze (ointment side down) over affected areas for 20 to 30 minutes twice daily.
Patients with widespread or severe disease should be hospitalized. In severe cases, supportive wound care is provided, and treatment is aimed at immunosuppression. Systemic options include high-dose prednisone 0.5 to 1 mg/kg daily until clear, a steroid-sparing immunosuppressant such as mycophenolate mofetil up to 1000 mg bid, or rituximab in 1 of several regimens.
Three years prior to this patient’s visit, she had been successfully treated for PV with a course of rituximab. To treat the current flare, she was started on prednisone 60 mg/d. In addition, the plan was for her to complete 2 infusions of 1000 mg rituximab 2 weeks apart.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.
1. Didona, D, Schmidt, MF, Maglie, R, et al. Pemphigus and pemphigoids: clinical presentation, diagnosis and therapy. J Dtsch Dermatol Ges. 2023;1-20. doi: 10.1111/ddg.15174
1. Didona, D, Schmidt, MF, Maglie, R, et al. Pemphigus and pemphigoids: clinical presentation, diagnosis and therapy. J Dtsch Dermatol Ges. 2023;1-20. doi: 10.1111/ddg.15174
IV iron shows only modest benefit in HF: HEART-FID
AMSTERDAM – , but the study failed to meet the specified more rigorous definition of significance (P = .01) on the primary hierarchical composite of death, hospitalizations for heart failure, or 6-minute walk distance.
The trial, which investigated intravenous ferric carboxymaltose treatment vs. placebo, also showed no statistical difference in the main secondary endpoint: time to cardiovascular death or first heart failure hospitalization.
It was hoped that HEART-FID, the largest study to date to look at intravenous iron supplementation in heart failure, would confirm benefits suggested in previous smaller studies, but its modest results seem to have, if anything, caused more uncertainly on whether supplementing iron is actually worthwhile.
The HEART-FID trial was presented at the annual congress of the European Society of Cardiology and simultaneously published online in the New England Journal of Medicine.
Another presentation at the ESC Congress reported a pooled meta-analysis of all the intravenous iron supplementation studies, including HEART-FID. This showed a significant reduction in one coprimary endpoint (cardiovascular hospitalization/CV death) but not in the other (heart failure hospitalization/CV death), which is the more traditional and well-recognized endpoint in heart failure trials.
The meta-analysis was also published online in the European Heart Journal.
HEART-FID lead investigator, Robert J. Mentz, MD, Duke University, Durham, N.C., said the totality of the evidence showed clinical benefits of intravenous iron supplementation with intravenous ferric carboxymaltose.
“I worry that people will focus on a P value rather than the actual clinical benefits seen across all the studies,” Dr. Mentz said in an interview. “Technically, this study was neutral in respect to the primary endpoint, but when we look at all the evidence with respect to ferric carboxymaltose, including this new pooled analysis, this does support clinical benefits.”
Comoderator of the ESC Hotline session at which the trial was presented, John McMurray, MD, University of Glasgow (Scotland), thought the trial had “muddied the waters a bit” on the issue of iron supplementation in heart failure.
“I would say we are in a less clear position on iron supplementation now than we were a few months ago. Those clinicians who have believed that checking iron levels and supplementing iron in those who are low is the right thing to do may now be wondering about that,” he told this news organization.
Dr. McMurray noted that initial impressions of the data from both HEART-FID and the meta-analysis suggested some benefit of intravenous iron on CV death/heart failure hospitalization in the first year, but on longer term follow-up, that benefit was less evident.
“We need to look further into why there is that discrepancy,” he said. “This could be a statistical phenomenon or could be something to do with the frequency of redosing over the longer term.”
He explained that several previous studies of intravenous iron supplementation in heart failure have reported apparent convincing benefits on quality of life and functional capacity, but there has been some uncertainty on this because of the difficulty in producing a placebo for intravenous iron.
“So, it would have been great to have some additional confirmation of these benefits and on harder endpoints,” he said, “but even in HEART-FID, there was only a small nonsignificant benefit in walking distance.”
HEART-FID
The HEART-FID trial randomly assigned 3,065 ambulatory patients with heart failure, a left ventricular ejection fraction of 40% or less, and iron deficiency to intravenous ferric carboxymaltose or placebo, given every 6 months as needed on the basis of iron indexes and hemoglobin levels, in addition to standard therapy for heart failure.
The primary outcome was a hierarchical composite of death within 12 months after randomization, hospitalizations for heart failure within 12 months after randomization, or change from baseline to 6 months in the 6-minute walk distance. The significance level was set at .01.
Results showed that death by month 12 occurred in 8.6% of the ferric carboxymaltose group and 10.3% of the placebo group; a total of 297 and 332 hospitalizations for heart failure, respectively, occurred by month 12; and the mean change from baseline to 6 months in the 6-minute walk distance was 8 meters in the ferric carboxymaltose group and 4 meters with placebo. The P value for the primary composite was .02.
The trial also used another method (unmatched win ratio) to analyze the hierarchical composite outcome in the ferric carboxymaltose group as compared with the placebo group that gave a result of 1.10 (99% confidence interval, 0.99-1.23).
During the follow-up period, CV death or hospitalization for heart failure (the main secondary outcome) occurred in 31.0% of the ferric carboxymaltose group and in 32.2% of the placebo group (hazard ratio, 0.93; 96% CI, 0.81-1.06).
Repeated dosing of ferric carboxymaltose appeared to be safe, with an acceptable adverse-event profile in most patients. The number of patients with serious adverse events occurring during the treatment period was similar in the two groups (27.0% in the ferric carboxymaltose group and 26.2% in the placebo group).
‘It’s hard to argue that we are not disappointed’
Designated discussant of the HEART-FID study at the ESC HOTLINE session, Scott Solomon, MD, Brigham and Women’s Hospital, Boston, described HEART-FID as “an extremely important and well-conducted trial.”
He noted that iron deficiency is extremely common in patients with heart failure, affecting at least about a third of patients, and is associated with reduced New York Heart Association class and reduced survival. Previous smaller studies have suggested benefit but have narrowly missed their primary endpoints. HEART-FID was a larger and sufficiently well-powered trial to test the hypothesis that iron supplementation can improve harder clinical endpoints.
Dr. Solomon said that the primary endpoint could be difficult to interpret, with a hierarchical composite, and a win ratio. “But I think it’s fair to say that the results are modest at best,” he added.
“When we look at the traditional cardiovascular death/heart failure hospitalization endpoint, one of the hard endpoints that we care about most in heart failure, it’s hard to argue that we are not disappointed,” he commented.
Referring to the P value of .01 threshold set for significance, which is based on new U.S. Food and Drug Administration regulatory standards, Dr. Solomon noted, “If they had used a standard P = .05 threshold, then they would be able to claim that this trial had met its primary endpoint. But, nevertheless, whatever threshold for significance we look at, the benefit was clearly modest.”
“As with all trials that show modest results, it will be useful to look at subgroups that are most likely to respond to the greatest extent to this therapy, and I look forward to learning more on this from further analyses,” Dr. Solomon concluded.
In an accompanying editorial in the New England Journal of Medicine, Pieter Martens, MD, and Wilfried Mullens, MD, PhD, Ziekenhuis Oost-Limburg, Genk, Belgium, and Hasselt (Belgium) University, point out that analyses from previous trials have suggested that intravenous iron did not have a treatment effect in patients with a transferrin saturation of more than 20%.
They note that, in the ferric carboxymaltose group in the HEART-FID trial, the mean transferrin saturation was 23.9% at baseline, higher than in previous studies.
Future analyses should assess the importance of the transferrin saturation value at baseline, which “could help redefine the definition of iron deficiency in patients with heart failure and, we hope, help clinicians determine which patients might benefit from intravenous iron supplementation,” they write.
Meta-analysis of trials
The meta-analysis of intravenous iron supplementation trials in heart failure was presented by Piotr Ponikowski, MD, Medical University Wroclaw (Poland).
The analysis pooled individual patient data from three double-blind, placebo-controlled trials – CONFIRM-HF 2, AFFIRM-AHF 3, and HEART-FID – giving a total of 4,475 patients, with 2,241 receiving ferric carboxymaltose and 2,234 receiving placebo.
The two prespecified composite primary endpoints were CV hospitalizations/CV death and heart failure hospitalizations/CV death.
These showed similar 13%-14% relative risk reductions with ferric carboxymaltose, but only the former was statistically significant.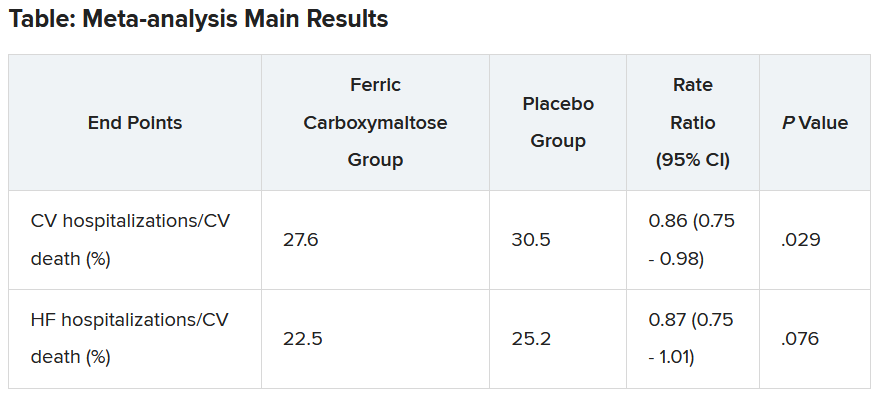
Similar results were seen when a fourth trial – IRONMAN (an open-label trial) – was included. In this case, the heart failure hospitalization/CV death endpoint was also nonsignificantly reduced with ferric carboxymaltose (rate ratio, 0.82; 95% CI, 0.58-1.07).
Subgroup analysis suggested that patients with higher transferrin saturation levels appeared to have a lack of treatment effect, whereas those with lower transferrin saturation (< 15%) showed significant treatment benefits.
A higher 6-month cumulative dose of ferric carboxymaltose – likely the result of redosing – may be associated with a slightly greater treatment effect after 6 months, Dr. Ponikowski reported.
He concluded: “These data support the use of intravenous ferric carboxymaltose to treat iron deficiency among patients with heart failure with reduced/mildly reduced LVEF [left ventricular ejection fraction] to reduce the risk of future hospitalization.”
“Our findings support additional research to challenge the current definition of iron deficiency in heart failure as an indication for IV iron therapy and to identify eligibility criteria for optimal redosing strategy,” Dr. Ponikowski added.
Discussant of the meta-analysis presentation at the ESC Hotline session, Pardeep Jhund, MD, University of Glasgow, suggested that the endpoint of most interest would be heart failure hospitalization/CV death in the analysis that included the IRONMAN trial, “which unfortunately did not meet statistical significance.”
In answer to the question “Where does this leave clinicians when treating patients?”Dr. Jhund said, “After yet another meta-analysis, I think the role of IV iron in reducing morbidity and mortality outcomes in heart failure remains questionable.”
“While the absence of evidence is not evidence of absence, the wide confidence intervals of the treatment effect on heart failure hospitalization/CV death leaves a lot of room for doubt about the efficacy of IV iron for reducing HF hospitalizations,” he concluded.
The HEART-FID trial was funded by American Regent, a Daiichi Sankyo Group company. Dr. Mentz reports receiving research support from American Regent and honoraria from American Regent, Vifor, and Pharmacosmos. Dr. Ponikowski reports consultancy fees/honoraria from Vifor Pharma, Boehringer Ingelheim, AstraZeneca, Servier, Novartis, Bayer, MSD, Pfizer, Moderna, Sanofi, and Radcliffe Group.
A version of this article first appeared on Medscape.com.
AMSTERDAM – , but the study failed to meet the specified more rigorous definition of significance (P = .01) on the primary hierarchical composite of death, hospitalizations for heart failure, or 6-minute walk distance.
The trial, which investigated intravenous ferric carboxymaltose treatment vs. placebo, also showed no statistical difference in the main secondary endpoint: time to cardiovascular death or first heart failure hospitalization.
It was hoped that HEART-FID, the largest study to date to look at intravenous iron supplementation in heart failure, would confirm benefits suggested in previous smaller studies, but its modest results seem to have, if anything, caused more uncertainly on whether supplementing iron is actually worthwhile.
The HEART-FID trial was presented at the annual congress of the European Society of Cardiology and simultaneously published online in the New England Journal of Medicine.
Another presentation at the ESC Congress reported a pooled meta-analysis of all the intravenous iron supplementation studies, including HEART-FID. This showed a significant reduction in one coprimary endpoint (cardiovascular hospitalization/CV death) but not in the other (heart failure hospitalization/CV death), which is the more traditional and well-recognized endpoint in heart failure trials.
The meta-analysis was also published online in the European Heart Journal.
HEART-FID lead investigator, Robert J. Mentz, MD, Duke University, Durham, N.C., said the totality of the evidence showed clinical benefits of intravenous iron supplementation with intravenous ferric carboxymaltose.
“I worry that people will focus on a P value rather than the actual clinical benefits seen across all the studies,” Dr. Mentz said in an interview. “Technically, this study was neutral in respect to the primary endpoint, but when we look at all the evidence with respect to ferric carboxymaltose, including this new pooled analysis, this does support clinical benefits.”
Comoderator of the ESC Hotline session at which the trial was presented, John McMurray, MD, University of Glasgow (Scotland), thought the trial had “muddied the waters a bit” on the issue of iron supplementation in heart failure.
“I would say we are in a less clear position on iron supplementation now than we were a few months ago. Those clinicians who have believed that checking iron levels and supplementing iron in those who are low is the right thing to do may now be wondering about that,” he told this news organization.
Dr. McMurray noted that initial impressions of the data from both HEART-FID and the meta-analysis suggested some benefit of intravenous iron on CV death/heart failure hospitalization in the first year, but on longer term follow-up, that benefit was less evident.
“We need to look further into why there is that discrepancy,” he said. “This could be a statistical phenomenon or could be something to do with the frequency of redosing over the longer term.”
He explained that several previous studies of intravenous iron supplementation in heart failure have reported apparent convincing benefits on quality of life and functional capacity, but there has been some uncertainty on this because of the difficulty in producing a placebo for intravenous iron.
“So, it would have been great to have some additional confirmation of these benefits and on harder endpoints,” he said, “but even in HEART-FID, there was only a small nonsignificant benefit in walking distance.”
HEART-FID
The HEART-FID trial randomly assigned 3,065 ambulatory patients with heart failure, a left ventricular ejection fraction of 40% or less, and iron deficiency to intravenous ferric carboxymaltose or placebo, given every 6 months as needed on the basis of iron indexes and hemoglobin levels, in addition to standard therapy for heart failure.
The primary outcome was a hierarchical composite of death within 12 months after randomization, hospitalizations for heart failure within 12 months after randomization, or change from baseline to 6 months in the 6-minute walk distance. The significance level was set at .01.
Results showed that death by month 12 occurred in 8.6% of the ferric carboxymaltose group and 10.3% of the placebo group; a total of 297 and 332 hospitalizations for heart failure, respectively, occurred by month 12; and the mean change from baseline to 6 months in the 6-minute walk distance was 8 meters in the ferric carboxymaltose group and 4 meters with placebo. The P value for the primary composite was .02.
The trial also used another method (unmatched win ratio) to analyze the hierarchical composite outcome in the ferric carboxymaltose group as compared with the placebo group that gave a result of 1.10 (99% confidence interval, 0.99-1.23).
During the follow-up period, CV death or hospitalization for heart failure (the main secondary outcome) occurred in 31.0% of the ferric carboxymaltose group and in 32.2% of the placebo group (hazard ratio, 0.93; 96% CI, 0.81-1.06).
Repeated dosing of ferric carboxymaltose appeared to be safe, with an acceptable adverse-event profile in most patients. The number of patients with serious adverse events occurring during the treatment period was similar in the two groups (27.0% in the ferric carboxymaltose group and 26.2% in the placebo group).
‘It’s hard to argue that we are not disappointed’
Designated discussant of the HEART-FID study at the ESC HOTLINE session, Scott Solomon, MD, Brigham and Women’s Hospital, Boston, described HEART-FID as “an extremely important and well-conducted trial.”
He noted that iron deficiency is extremely common in patients with heart failure, affecting at least about a third of patients, and is associated with reduced New York Heart Association class and reduced survival. Previous smaller studies have suggested benefit but have narrowly missed their primary endpoints. HEART-FID was a larger and sufficiently well-powered trial to test the hypothesis that iron supplementation can improve harder clinical endpoints.
Dr. Solomon said that the primary endpoint could be difficult to interpret, with a hierarchical composite, and a win ratio. “But I think it’s fair to say that the results are modest at best,” he added.
“When we look at the traditional cardiovascular death/heart failure hospitalization endpoint, one of the hard endpoints that we care about most in heart failure, it’s hard to argue that we are not disappointed,” he commented.
Referring to the P value of .01 threshold set for significance, which is based on new U.S. Food and Drug Administration regulatory standards, Dr. Solomon noted, “If they had used a standard P = .05 threshold, then they would be able to claim that this trial had met its primary endpoint. But, nevertheless, whatever threshold for significance we look at, the benefit was clearly modest.”
“As with all trials that show modest results, it will be useful to look at subgroups that are most likely to respond to the greatest extent to this therapy, and I look forward to learning more on this from further analyses,” Dr. Solomon concluded.
In an accompanying editorial in the New England Journal of Medicine, Pieter Martens, MD, and Wilfried Mullens, MD, PhD, Ziekenhuis Oost-Limburg, Genk, Belgium, and Hasselt (Belgium) University, point out that analyses from previous trials have suggested that intravenous iron did not have a treatment effect in patients with a transferrin saturation of more than 20%.
They note that, in the ferric carboxymaltose group in the HEART-FID trial, the mean transferrin saturation was 23.9% at baseline, higher than in previous studies.
Future analyses should assess the importance of the transferrin saturation value at baseline, which “could help redefine the definition of iron deficiency in patients with heart failure and, we hope, help clinicians determine which patients might benefit from intravenous iron supplementation,” they write.
Meta-analysis of trials
The meta-analysis of intravenous iron supplementation trials in heart failure was presented by Piotr Ponikowski, MD, Medical University Wroclaw (Poland).
The analysis pooled individual patient data from three double-blind, placebo-controlled trials – CONFIRM-HF 2, AFFIRM-AHF 3, and HEART-FID – giving a total of 4,475 patients, with 2,241 receiving ferric carboxymaltose and 2,234 receiving placebo.
The two prespecified composite primary endpoints were CV hospitalizations/CV death and heart failure hospitalizations/CV death.
These showed similar 13%-14% relative risk reductions with ferric carboxymaltose, but only the former was statistically significant.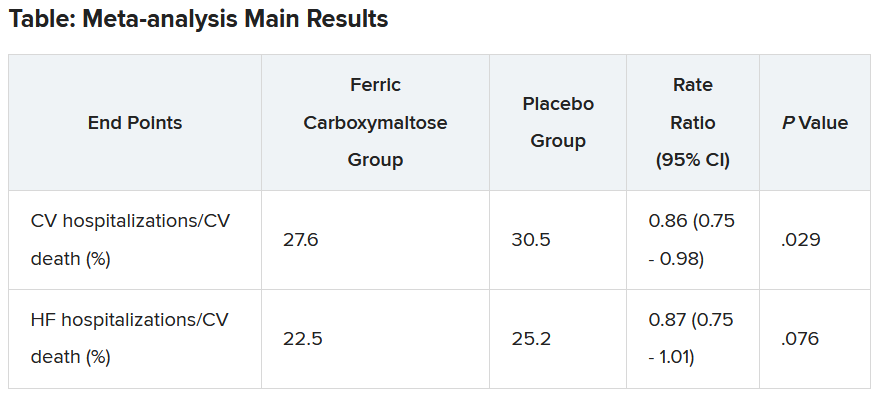
Similar results were seen when a fourth trial – IRONMAN (an open-label trial) – was included. In this case, the heart failure hospitalization/CV death endpoint was also nonsignificantly reduced with ferric carboxymaltose (rate ratio, 0.82; 95% CI, 0.58-1.07).
Subgroup analysis suggested that patients with higher transferrin saturation levels appeared to have a lack of treatment effect, whereas those with lower transferrin saturation (< 15%) showed significant treatment benefits.
A higher 6-month cumulative dose of ferric carboxymaltose – likely the result of redosing – may be associated with a slightly greater treatment effect after 6 months, Dr. Ponikowski reported.
He concluded: “These data support the use of intravenous ferric carboxymaltose to treat iron deficiency among patients with heart failure with reduced/mildly reduced LVEF [left ventricular ejection fraction] to reduce the risk of future hospitalization.”
“Our findings support additional research to challenge the current definition of iron deficiency in heart failure as an indication for IV iron therapy and to identify eligibility criteria for optimal redosing strategy,” Dr. Ponikowski added.
Discussant of the meta-analysis presentation at the ESC Hotline session, Pardeep Jhund, MD, University of Glasgow, suggested that the endpoint of most interest would be heart failure hospitalization/CV death in the analysis that included the IRONMAN trial, “which unfortunately did not meet statistical significance.”
In answer to the question “Where does this leave clinicians when treating patients?”Dr. Jhund said, “After yet another meta-analysis, I think the role of IV iron in reducing morbidity and mortality outcomes in heart failure remains questionable.”
“While the absence of evidence is not evidence of absence, the wide confidence intervals of the treatment effect on heart failure hospitalization/CV death leaves a lot of room for doubt about the efficacy of IV iron for reducing HF hospitalizations,” he concluded.
The HEART-FID trial was funded by American Regent, a Daiichi Sankyo Group company. Dr. Mentz reports receiving research support from American Regent and honoraria from American Regent, Vifor, and Pharmacosmos. Dr. Ponikowski reports consultancy fees/honoraria from Vifor Pharma, Boehringer Ingelheim, AstraZeneca, Servier, Novartis, Bayer, MSD, Pfizer, Moderna, Sanofi, and Radcliffe Group.
A version of this article first appeared on Medscape.com.
AMSTERDAM – , but the study failed to meet the specified more rigorous definition of significance (P = .01) on the primary hierarchical composite of death, hospitalizations for heart failure, or 6-minute walk distance.
The trial, which investigated intravenous ferric carboxymaltose treatment vs. placebo, also showed no statistical difference in the main secondary endpoint: time to cardiovascular death or first heart failure hospitalization.
It was hoped that HEART-FID, the largest study to date to look at intravenous iron supplementation in heart failure, would confirm benefits suggested in previous smaller studies, but its modest results seem to have, if anything, caused more uncertainly on whether supplementing iron is actually worthwhile.
The HEART-FID trial was presented at the annual congress of the European Society of Cardiology and simultaneously published online in the New England Journal of Medicine.
Another presentation at the ESC Congress reported a pooled meta-analysis of all the intravenous iron supplementation studies, including HEART-FID. This showed a significant reduction in one coprimary endpoint (cardiovascular hospitalization/CV death) but not in the other (heart failure hospitalization/CV death), which is the more traditional and well-recognized endpoint in heart failure trials.
The meta-analysis was also published online in the European Heart Journal.
HEART-FID lead investigator, Robert J. Mentz, MD, Duke University, Durham, N.C., said the totality of the evidence showed clinical benefits of intravenous iron supplementation with intravenous ferric carboxymaltose.
“I worry that people will focus on a P value rather than the actual clinical benefits seen across all the studies,” Dr. Mentz said in an interview. “Technically, this study was neutral in respect to the primary endpoint, but when we look at all the evidence with respect to ferric carboxymaltose, including this new pooled analysis, this does support clinical benefits.”
Comoderator of the ESC Hotline session at which the trial was presented, John McMurray, MD, University of Glasgow (Scotland), thought the trial had “muddied the waters a bit” on the issue of iron supplementation in heart failure.
“I would say we are in a less clear position on iron supplementation now than we were a few months ago. Those clinicians who have believed that checking iron levels and supplementing iron in those who are low is the right thing to do may now be wondering about that,” he told this news organization.
Dr. McMurray noted that initial impressions of the data from both HEART-FID and the meta-analysis suggested some benefit of intravenous iron on CV death/heart failure hospitalization in the first year, but on longer term follow-up, that benefit was less evident.
“We need to look further into why there is that discrepancy,” he said. “This could be a statistical phenomenon or could be something to do with the frequency of redosing over the longer term.”
He explained that several previous studies of intravenous iron supplementation in heart failure have reported apparent convincing benefits on quality of life and functional capacity, but there has been some uncertainty on this because of the difficulty in producing a placebo for intravenous iron.
“So, it would have been great to have some additional confirmation of these benefits and on harder endpoints,” he said, “but even in HEART-FID, there was only a small nonsignificant benefit in walking distance.”
HEART-FID
The HEART-FID trial randomly assigned 3,065 ambulatory patients with heart failure, a left ventricular ejection fraction of 40% or less, and iron deficiency to intravenous ferric carboxymaltose or placebo, given every 6 months as needed on the basis of iron indexes and hemoglobin levels, in addition to standard therapy for heart failure.
The primary outcome was a hierarchical composite of death within 12 months after randomization, hospitalizations for heart failure within 12 months after randomization, or change from baseline to 6 months in the 6-minute walk distance. The significance level was set at .01.
Results showed that death by month 12 occurred in 8.6% of the ferric carboxymaltose group and 10.3% of the placebo group; a total of 297 and 332 hospitalizations for heart failure, respectively, occurred by month 12; and the mean change from baseline to 6 months in the 6-minute walk distance was 8 meters in the ferric carboxymaltose group and 4 meters with placebo. The P value for the primary composite was .02.
The trial also used another method (unmatched win ratio) to analyze the hierarchical composite outcome in the ferric carboxymaltose group as compared with the placebo group that gave a result of 1.10 (99% confidence interval, 0.99-1.23).
During the follow-up period, CV death or hospitalization for heart failure (the main secondary outcome) occurred in 31.0% of the ferric carboxymaltose group and in 32.2% of the placebo group (hazard ratio, 0.93; 96% CI, 0.81-1.06).
Repeated dosing of ferric carboxymaltose appeared to be safe, with an acceptable adverse-event profile in most patients. The number of patients with serious adverse events occurring during the treatment period was similar in the two groups (27.0% in the ferric carboxymaltose group and 26.2% in the placebo group).
‘It’s hard to argue that we are not disappointed’
Designated discussant of the HEART-FID study at the ESC HOTLINE session, Scott Solomon, MD, Brigham and Women’s Hospital, Boston, described HEART-FID as “an extremely important and well-conducted trial.”
He noted that iron deficiency is extremely common in patients with heart failure, affecting at least about a third of patients, and is associated with reduced New York Heart Association class and reduced survival. Previous smaller studies have suggested benefit but have narrowly missed their primary endpoints. HEART-FID was a larger and sufficiently well-powered trial to test the hypothesis that iron supplementation can improve harder clinical endpoints.
Dr. Solomon said that the primary endpoint could be difficult to interpret, with a hierarchical composite, and a win ratio. “But I think it’s fair to say that the results are modest at best,” he added.
“When we look at the traditional cardiovascular death/heart failure hospitalization endpoint, one of the hard endpoints that we care about most in heart failure, it’s hard to argue that we are not disappointed,” he commented.
Referring to the P value of .01 threshold set for significance, which is based on new U.S. Food and Drug Administration regulatory standards, Dr. Solomon noted, “If they had used a standard P = .05 threshold, then they would be able to claim that this trial had met its primary endpoint. But, nevertheless, whatever threshold for significance we look at, the benefit was clearly modest.”
“As with all trials that show modest results, it will be useful to look at subgroups that are most likely to respond to the greatest extent to this therapy, and I look forward to learning more on this from further analyses,” Dr. Solomon concluded.
In an accompanying editorial in the New England Journal of Medicine, Pieter Martens, MD, and Wilfried Mullens, MD, PhD, Ziekenhuis Oost-Limburg, Genk, Belgium, and Hasselt (Belgium) University, point out that analyses from previous trials have suggested that intravenous iron did not have a treatment effect in patients with a transferrin saturation of more than 20%.
They note that, in the ferric carboxymaltose group in the HEART-FID trial, the mean transferrin saturation was 23.9% at baseline, higher than in previous studies.
Future analyses should assess the importance of the transferrin saturation value at baseline, which “could help redefine the definition of iron deficiency in patients with heart failure and, we hope, help clinicians determine which patients might benefit from intravenous iron supplementation,” they write.
Meta-analysis of trials
The meta-analysis of intravenous iron supplementation trials in heart failure was presented by Piotr Ponikowski, MD, Medical University Wroclaw (Poland).
The analysis pooled individual patient data from three double-blind, placebo-controlled trials – CONFIRM-HF 2, AFFIRM-AHF 3, and HEART-FID – giving a total of 4,475 patients, with 2,241 receiving ferric carboxymaltose and 2,234 receiving placebo.
The two prespecified composite primary endpoints were CV hospitalizations/CV death and heart failure hospitalizations/CV death.
These showed similar 13%-14% relative risk reductions with ferric carboxymaltose, but only the former was statistically significant.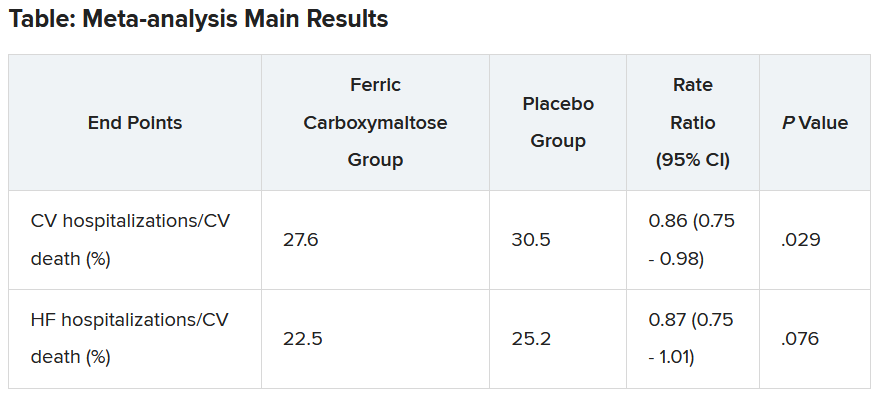
Similar results were seen when a fourth trial – IRONMAN (an open-label trial) – was included. In this case, the heart failure hospitalization/CV death endpoint was also nonsignificantly reduced with ferric carboxymaltose (rate ratio, 0.82; 95% CI, 0.58-1.07).
Subgroup analysis suggested that patients with higher transferrin saturation levels appeared to have a lack of treatment effect, whereas those with lower transferrin saturation (< 15%) showed significant treatment benefits.
A higher 6-month cumulative dose of ferric carboxymaltose – likely the result of redosing – may be associated with a slightly greater treatment effect after 6 months, Dr. Ponikowski reported.
He concluded: “These data support the use of intravenous ferric carboxymaltose to treat iron deficiency among patients with heart failure with reduced/mildly reduced LVEF [left ventricular ejection fraction] to reduce the risk of future hospitalization.”
“Our findings support additional research to challenge the current definition of iron deficiency in heart failure as an indication for IV iron therapy and to identify eligibility criteria for optimal redosing strategy,” Dr. Ponikowski added.
Discussant of the meta-analysis presentation at the ESC Hotline session, Pardeep Jhund, MD, University of Glasgow, suggested that the endpoint of most interest would be heart failure hospitalization/CV death in the analysis that included the IRONMAN trial, “which unfortunately did not meet statistical significance.”
In answer to the question “Where does this leave clinicians when treating patients?”Dr. Jhund said, “After yet another meta-analysis, I think the role of IV iron in reducing morbidity and mortality outcomes in heart failure remains questionable.”
“While the absence of evidence is not evidence of absence, the wide confidence intervals of the treatment effect on heart failure hospitalization/CV death leaves a lot of room for doubt about the efficacy of IV iron for reducing HF hospitalizations,” he concluded.
The HEART-FID trial was funded by American Regent, a Daiichi Sankyo Group company. Dr. Mentz reports receiving research support from American Regent and honoraria from American Regent, Vifor, and Pharmacosmos. Dr. Ponikowski reports consultancy fees/honoraria from Vifor Pharma, Boehringer Ingelheim, AstraZeneca, Servier, Novartis, Bayer, MSD, Pfizer, Moderna, Sanofi, and Radcliffe Group.
A version of this article first appeared on Medscape.com.
AT THE ESC CONGRESS 2023
Traditional Chinese medicine improves outcomes in HFrEF
When added to guideline-directed therapies for heart failure with reduced ejection fraction (HFrEF), a traditional Chinese medicine called qiliqiangxin reduced the composite endpoint of cardiovascular death and heart failure hospitalization by more than 20%, results of a large placebo-controlled trial show.
reported Xinli Li, MD, PhD, First Affiliated Hospital, Nanjing Medical University, China.
Qiliqiangxin, a commonly used therapy in China for cardiovascular disease, is not a single chemical entity but a treatment composed of 11 plant-based substances that together are associated with diuretic effects, vasodilation, and “cardiotonic” activity, Dr. Li said. He also cited studies showing an upregulation effect on peroxisome proliferator-activated receptor gamma coactivator 1-beta (PGC1-beta).
The results were presented at the annual congress of the European Society of Cardiology.
Hard endpoints pursued in rigorous design
There have been numerous studies of qiliqiangxin for cardiovascular diseases, including a double-blind study that associated this agent with a greater than 30% reduction in the surrogate endpoint of N-terminal pro–B-type natriuretic peptide (NT-proBNP).
In the newly completed multicenter trial, called QUEST, the goal was to determine whether this therapy could reduce hard endpoints relative to placebo in a rigorously conducted trial enrolling patients receiving an optimized triple-therapy heart failure regimen.
Few patients in the study received a sodium glucose cotransporter-2 (SGLT-2 inhibitor), which was not a standard at the time the study was designed but is now part of the quadruple guideline-directed medical therapy in most European and North American guidelines.
In this trial, 3,119 patients were randomly assigned at 133 centers in China to take four capsules of qiliqiangxin or placebo three times per day. At a median follow-up of 18.3 months, outcomes were evaluable in nearly all 1,561 patients randomly assigned to the experimental therapy and 1,555 patients randomly assigned to placebo.
The key inclusion criteria were a left ventricular ejection fraction of 40% or less and a serum NT-proBNP level of at least 450 pg/mL. Patients in New York Heart Association class IV heart failure were excluded.
At enrollment, more than 80% of patients in both arms were receiving a renin-angiotensin system (RAS) inhibitor (angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or angiotensin receptor neprilysin inhibitor), more than 80% were receiving a mineralocorticoid receptor antagonist, and more than 85% were receiving a beta-blocker.
Death and hospitalization reduced 22%
By hazard ratio, the primary composite endpoint of CV death and heart failure hospitalization was reduced by 22% relative to placebo (HR, 0.78; P < .001). When evaluated separately, the relative reductions in these respective endpoints were 17% (HR, 0.83; P = .045) and 24% (HR, 0.76; P = .002).
The risk reduction was robust (HR, 0.76; P < .001) in patients with an ischemic cause but nonsignificant in those without (HR, 0.92; P = .575). A significant benefit was sustained in patients receiving an angiotensin receptor neprilysin inhibitor (HR, 0.84; P = .041), as well as those who did not receive this class of drug (HR, 0.77; P = .012).
However, the benefit of qiliqiangxin among patients receiving all components of guideline-directed triple therapy (RAS inhibitor, beta-blocker, and mineralocorticoid antagonist) was only a trend (HR, 0.86; P = .079).
All-cause mortality, a secondary endpoint, was lower among patients randomly assigned to qiliqiangxin than to those assigned to placebo, but this difference fell just short of statistical significance (14.21% vs. 16.85%; P = .058).
Qiliqiangxin was well tolerated. The proportion of patients with a serious adverse event was numerically lower with qiliqiangxin than with placebo (17.43% vs. 19.74%), whereas discontinuations associated with an adverse event were numerically higher in the qiliqiangxin group (1.03% vs. 0.58%), albeit still very low in both study arms.
Overlap of drug benefits suspected
Given the safety of this drug and its highly significant reduction in a composite endpoint used in other major HFrEF trials, the ESC-invited discussant, Carolyn S.P. Lam, MBBS, PhD, National Heart Centre, Singapore, called the outcome “remarkable” and a validation for “the millions of people” who are already taking qiliqiangxin in China and other Asian countries.
Using the DAPA-HF trial as a point of reference, Dr. Lam noted that relative reduction in the composite endpoint of cardiovascular death for the SGLT-2 inhibitor dapagliflozin relative to placebo on top of triple guideline-directed medical therapy was lower (17% vs. 24%), but there were significant reductions in each of the components, as well as a nonsignificant signal of a mortality benefit.
However, Dr. Lam pointed out that there does seem to be more of an overlap for the benefits of qiliqiangxin than dapagliflozin relative to other components of triple therapy based on the lower rate of benefit when patients were optimized on triple therapy.
“The subgroup analysis [of this study] is very important,” Dr. Lam said. Qiliqiangxin may be best in patients who cannot take one or more of the components of triple therapy, she suggested, even though she called for further studies to test this theory. She also cautioned that the pill burden of four capsules taken three times per day might be onerous for some patients.
Of the many questions still to be answered, Dr. Lam noted that the low rate of enrollment for patients (< 10%) taking SGLT-2 inhibitors makes the contribution of qiliqiangxin unclear among those receiving the current standard of quadruple guideline-directed medical therapy.
She also suggested that it will be important to dissect the relative contribution of the different active ingredients of qiliqiangxin.
“This is not a purified compound that we are used to in Western medicine,” Dr. Lam said. While she praised the study as “scientifically rigorous” and indicated that the results support a clinical benefit from qiliqiangxin, she thinks an exploration of the mechanism or mechanisms of benefit is a next step in understanding where this therapy fits in HFrEF management.
Dr. Li reports financial relationships with AstraZeneca, Bayer, Novartis, Roche, and Yiling. Dr. Lam reports financial relationships with more than 25 pharmaceutical or device manufacturers, many of which produce therapies for heart failure, as well as with Medscape/WebMD Global LLC. The study was supported by the Chinese National Key Research and Development Project and Yiling Pharmaceuticals.
A version of this article appeared on Medscape.com.
When added to guideline-directed therapies for heart failure with reduced ejection fraction (HFrEF), a traditional Chinese medicine called qiliqiangxin reduced the composite endpoint of cardiovascular death and heart failure hospitalization by more than 20%, results of a large placebo-controlled trial show.
reported Xinli Li, MD, PhD, First Affiliated Hospital, Nanjing Medical University, China.
Qiliqiangxin, a commonly used therapy in China for cardiovascular disease, is not a single chemical entity but a treatment composed of 11 plant-based substances that together are associated with diuretic effects, vasodilation, and “cardiotonic” activity, Dr. Li said. He also cited studies showing an upregulation effect on peroxisome proliferator-activated receptor gamma coactivator 1-beta (PGC1-beta).
The results were presented at the annual congress of the European Society of Cardiology.
Hard endpoints pursued in rigorous design
There have been numerous studies of qiliqiangxin for cardiovascular diseases, including a double-blind study that associated this agent with a greater than 30% reduction in the surrogate endpoint of N-terminal pro–B-type natriuretic peptide (NT-proBNP).
In the newly completed multicenter trial, called QUEST, the goal was to determine whether this therapy could reduce hard endpoints relative to placebo in a rigorously conducted trial enrolling patients receiving an optimized triple-therapy heart failure regimen.
Few patients in the study received a sodium glucose cotransporter-2 (SGLT-2 inhibitor), which was not a standard at the time the study was designed but is now part of the quadruple guideline-directed medical therapy in most European and North American guidelines.
In this trial, 3,119 patients were randomly assigned at 133 centers in China to take four capsules of qiliqiangxin or placebo three times per day. At a median follow-up of 18.3 months, outcomes were evaluable in nearly all 1,561 patients randomly assigned to the experimental therapy and 1,555 patients randomly assigned to placebo.
The key inclusion criteria were a left ventricular ejection fraction of 40% or less and a serum NT-proBNP level of at least 450 pg/mL. Patients in New York Heart Association class IV heart failure were excluded.
At enrollment, more than 80% of patients in both arms were receiving a renin-angiotensin system (RAS) inhibitor (angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or angiotensin receptor neprilysin inhibitor), more than 80% were receiving a mineralocorticoid receptor antagonist, and more than 85% were receiving a beta-blocker.
Death and hospitalization reduced 22%
By hazard ratio, the primary composite endpoint of CV death and heart failure hospitalization was reduced by 22% relative to placebo (HR, 0.78; P < .001). When evaluated separately, the relative reductions in these respective endpoints were 17% (HR, 0.83; P = .045) and 24% (HR, 0.76; P = .002).
The risk reduction was robust (HR, 0.76; P < .001) in patients with an ischemic cause but nonsignificant in those without (HR, 0.92; P = .575). A significant benefit was sustained in patients receiving an angiotensin receptor neprilysin inhibitor (HR, 0.84; P = .041), as well as those who did not receive this class of drug (HR, 0.77; P = .012).
However, the benefit of qiliqiangxin among patients receiving all components of guideline-directed triple therapy (RAS inhibitor, beta-blocker, and mineralocorticoid antagonist) was only a trend (HR, 0.86; P = .079).
All-cause mortality, a secondary endpoint, was lower among patients randomly assigned to qiliqiangxin than to those assigned to placebo, but this difference fell just short of statistical significance (14.21% vs. 16.85%; P = .058).
Qiliqiangxin was well tolerated. The proportion of patients with a serious adverse event was numerically lower with qiliqiangxin than with placebo (17.43% vs. 19.74%), whereas discontinuations associated with an adverse event were numerically higher in the qiliqiangxin group (1.03% vs. 0.58%), albeit still very low in both study arms.
Overlap of drug benefits suspected
Given the safety of this drug and its highly significant reduction in a composite endpoint used in other major HFrEF trials, the ESC-invited discussant, Carolyn S.P. Lam, MBBS, PhD, National Heart Centre, Singapore, called the outcome “remarkable” and a validation for “the millions of people” who are already taking qiliqiangxin in China and other Asian countries.
Using the DAPA-HF trial as a point of reference, Dr. Lam noted that relative reduction in the composite endpoint of cardiovascular death for the SGLT-2 inhibitor dapagliflozin relative to placebo on top of triple guideline-directed medical therapy was lower (17% vs. 24%), but there were significant reductions in each of the components, as well as a nonsignificant signal of a mortality benefit.
However, Dr. Lam pointed out that there does seem to be more of an overlap for the benefits of qiliqiangxin than dapagliflozin relative to other components of triple therapy based on the lower rate of benefit when patients were optimized on triple therapy.
“The subgroup analysis [of this study] is very important,” Dr. Lam said. Qiliqiangxin may be best in patients who cannot take one or more of the components of triple therapy, she suggested, even though she called for further studies to test this theory. She also cautioned that the pill burden of four capsules taken three times per day might be onerous for some patients.
Of the many questions still to be answered, Dr. Lam noted that the low rate of enrollment for patients (< 10%) taking SGLT-2 inhibitors makes the contribution of qiliqiangxin unclear among those receiving the current standard of quadruple guideline-directed medical therapy.
She also suggested that it will be important to dissect the relative contribution of the different active ingredients of qiliqiangxin.
“This is not a purified compound that we are used to in Western medicine,” Dr. Lam said. While she praised the study as “scientifically rigorous” and indicated that the results support a clinical benefit from qiliqiangxin, she thinks an exploration of the mechanism or mechanisms of benefit is a next step in understanding where this therapy fits in HFrEF management.
Dr. Li reports financial relationships with AstraZeneca, Bayer, Novartis, Roche, and Yiling. Dr. Lam reports financial relationships with more than 25 pharmaceutical or device manufacturers, many of which produce therapies for heart failure, as well as with Medscape/WebMD Global LLC. The study was supported by the Chinese National Key Research and Development Project and Yiling Pharmaceuticals.
A version of this article appeared on Medscape.com.
When added to guideline-directed therapies for heart failure with reduced ejection fraction (HFrEF), a traditional Chinese medicine called qiliqiangxin reduced the composite endpoint of cardiovascular death and heart failure hospitalization by more than 20%, results of a large placebo-controlled trial show.
reported Xinli Li, MD, PhD, First Affiliated Hospital, Nanjing Medical University, China.
Qiliqiangxin, a commonly used therapy in China for cardiovascular disease, is not a single chemical entity but a treatment composed of 11 plant-based substances that together are associated with diuretic effects, vasodilation, and “cardiotonic” activity, Dr. Li said. He also cited studies showing an upregulation effect on peroxisome proliferator-activated receptor gamma coactivator 1-beta (PGC1-beta).
The results were presented at the annual congress of the European Society of Cardiology.
Hard endpoints pursued in rigorous design
There have been numerous studies of qiliqiangxin for cardiovascular diseases, including a double-blind study that associated this agent with a greater than 30% reduction in the surrogate endpoint of N-terminal pro–B-type natriuretic peptide (NT-proBNP).
In the newly completed multicenter trial, called QUEST, the goal was to determine whether this therapy could reduce hard endpoints relative to placebo in a rigorously conducted trial enrolling patients receiving an optimized triple-therapy heart failure regimen.
Few patients in the study received a sodium glucose cotransporter-2 (SGLT-2 inhibitor), which was not a standard at the time the study was designed but is now part of the quadruple guideline-directed medical therapy in most European and North American guidelines.
In this trial, 3,119 patients were randomly assigned at 133 centers in China to take four capsules of qiliqiangxin or placebo three times per day. At a median follow-up of 18.3 months, outcomes were evaluable in nearly all 1,561 patients randomly assigned to the experimental therapy and 1,555 patients randomly assigned to placebo.
The key inclusion criteria were a left ventricular ejection fraction of 40% or less and a serum NT-proBNP level of at least 450 pg/mL. Patients in New York Heart Association class IV heart failure were excluded.
At enrollment, more than 80% of patients in both arms were receiving a renin-angiotensin system (RAS) inhibitor (angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or angiotensin receptor neprilysin inhibitor), more than 80% were receiving a mineralocorticoid receptor antagonist, and more than 85% were receiving a beta-blocker.
Death and hospitalization reduced 22%
By hazard ratio, the primary composite endpoint of CV death and heart failure hospitalization was reduced by 22% relative to placebo (HR, 0.78; P < .001). When evaluated separately, the relative reductions in these respective endpoints were 17% (HR, 0.83; P = .045) and 24% (HR, 0.76; P = .002).
The risk reduction was robust (HR, 0.76; P < .001) in patients with an ischemic cause but nonsignificant in those without (HR, 0.92; P = .575). A significant benefit was sustained in patients receiving an angiotensin receptor neprilysin inhibitor (HR, 0.84; P = .041), as well as those who did not receive this class of drug (HR, 0.77; P = .012).
However, the benefit of qiliqiangxin among patients receiving all components of guideline-directed triple therapy (RAS inhibitor, beta-blocker, and mineralocorticoid antagonist) was only a trend (HR, 0.86; P = .079).
All-cause mortality, a secondary endpoint, was lower among patients randomly assigned to qiliqiangxin than to those assigned to placebo, but this difference fell just short of statistical significance (14.21% vs. 16.85%; P = .058).
Qiliqiangxin was well tolerated. The proportion of patients with a serious adverse event was numerically lower with qiliqiangxin than with placebo (17.43% vs. 19.74%), whereas discontinuations associated with an adverse event were numerically higher in the qiliqiangxin group (1.03% vs. 0.58%), albeit still very low in both study arms.
Overlap of drug benefits suspected
Given the safety of this drug and its highly significant reduction in a composite endpoint used in other major HFrEF trials, the ESC-invited discussant, Carolyn S.P. Lam, MBBS, PhD, National Heart Centre, Singapore, called the outcome “remarkable” and a validation for “the millions of people” who are already taking qiliqiangxin in China and other Asian countries.
Using the DAPA-HF trial as a point of reference, Dr. Lam noted that relative reduction in the composite endpoint of cardiovascular death for the SGLT-2 inhibitor dapagliflozin relative to placebo on top of triple guideline-directed medical therapy was lower (17% vs. 24%), but there were significant reductions in each of the components, as well as a nonsignificant signal of a mortality benefit.
However, Dr. Lam pointed out that there does seem to be more of an overlap for the benefits of qiliqiangxin than dapagliflozin relative to other components of triple therapy based on the lower rate of benefit when patients were optimized on triple therapy.
“The subgroup analysis [of this study] is very important,” Dr. Lam said. Qiliqiangxin may be best in patients who cannot take one or more of the components of triple therapy, she suggested, even though she called for further studies to test this theory. She also cautioned that the pill burden of four capsules taken three times per day might be onerous for some patients.
Of the many questions still to be answered, Dr. Lam noted that the low rate of enrollment for patients (< 10%) taking SGLT-2 inhibitors makes the contribution of qiliqiangxin unclear among those receiving the current standard of quadruple guideline-directed medical therapy.
She also suggested that it will be important to dissect the relative contribution of the different active ingredients of qiliqiangxin.
“This is not a purified compound that we are used to in Western medicine,” Dr. Lam said. While she praised the study as “scientifically rigorous” and indicated that the results support a clinical benefit from qiliqiangxin, she thinks an exploration of the mechanism or mechanisms of benefit is a next step in understanding where this therapy fits in HFrEF management.
Dr. Li reports financial relationships with AstraZeneca, Bayer, Novartis, Roche, and Yiling. Dr. Lam reports financial relationships with more than 25 pharmaceutical or device manufacturers, many of which produce therapies for heart failure, as well as with Medscape/WebMD Global LLC. The study was supported by the Chinese National Key Research and Development Project and Yiling Pharmaceuticals.
A version of this article appeared on Medscape.com.
FROM ESC CONGRESS 2023
Use of mental health services soared during pandemic
By the end of August 2022, overall use of mental health services was almost 40% higher than before the COVID-19 pandemic, while spending increased by 54%, according to a new study by researchers at the RAND Corporation.
During the early phase of the pandemic, from mid-March to mid-December 2020, before the vaccine was available, in-person visits decreased by 40%, while telehealth visits increased by 1,000%, reported Jonathan H. Cantor, PhD, and colleagues at RAND, and at Castlight Health, a benefit coordination provider, in a paper published online in JAMA Health Forum.
Between December 2020 and August 2022, telehealth visits stayed stable, but in-person visits creeped back up, eventually reaching 80% of prepandemic levels. However, “total utilization was higher than before the pandemic,” Dr. Cantor, a policy researcher at RAND, told this news organization.
“It could be that it’s easier for individuals to receive care via telehealth, but it could also just be that there’s a greater demand or need since the pandemic,” said Dr. Cantor. “We’ll just need more research to actually unpack what’s going on,” he said.
Initial per capita spending increased by about a third and was up overall by more than half. But it’s not clear how much of that is due to utilization or to price of services, said Dr. Cantor. Spending for telehealth services remained stable in the post-vaccine period, while spending on in-person visits returned to prepandemic levels.
Dr. Cantor and his colleagues were not able to determine whether utilization was by new or existing patients, but he said that would be good data to have. “It would be really important to know whether or not folks are initiating care because telehealth is making it easier,” he said.
The authors analyzed about 1.5 million claims for anxiety disorders, major depressive disorder, bipolar disorder, schizophrenia, and posttraumatic stress disorder, out of claims submitted by 7 million commercially insured adults whose self-insured employers used the Castlight benefit.
Dr. Cantor noted that this is just a small subset of the U.S. population. He said he’d like to have data from Medicare and Medicaid to fully assess the impact of the COVID-19 pandemic on mental health and of telehealth visits.
“This is a still-burgeoning field,” he said about telehealth. “We’re still trying to get a handle on how things are operating, given that there’s been so much change so rapidly.”
Meanwhile, 152 major employers responding to a large national survey this summer said that they’ve been grappling with how COVID-19 has affected workers. The employers include 72 Fortune 100 companies and provide health coverage for more than 60 million workers, retirees, and their families.
Seventy-seven percent said they are currently seeing an increase in depression, anxiety, and substance use disorders as a result of the pandemic, according to the Business Group on Health’s survey. That’s up from 44% in 2022.
Going forward, employers will focus on increasing access to mental health services, the survey reported.
“Our survey found that in 2024 and for the near future, employers will be acutely focused on addressing employees’ mental health needs while ensuring access and lowering cost barriers,” Ellen Kelsay, president and CEO of Business Group on Health, said in a statement.
The study was supported by grants from the National Institute of Mental Health and the National Institute on Aging. Coauthor Dena Bravata, MD, a Castlight employee, reported receiving personal fees from Castlight Health during the conduct of the study. Coauthor Christopher M. Whaley, a RAND employee, reported receiving personal fees from Castlight Health outside the submitted work.
A version of this article appeared on Medscape.com.
By the end of August 2022, overall use of mental health services was almost 40% higher than before the COVID-19 pandemic, while spending increased by 54%, according to a new study by researchers at the RAND Corporation.
During the early phase of the pandemic, from mid-March to mid-December 2020, before the vaccine was available, in-person visits decreased by 40%, while telehealth visits increased by 1,000%, reported Jonathan H. Cantor, PhD, and colleagues at RAND, and at Castlight Health, a benefit coordination provider, in a paper published online in JAMA Health Forum.
Between December 2020 and August 2022, telehealth visits stayed stable, but in-person visits creeped back up, eventually reaching 80% of prepandemic levels. However, “total utilization was higher than before the pandemic,” Dr. Cantor, a policy researcher at RAND, told this news organization.
“It could be that it’s easier for individuals to receive care via telehealth, but it could also just be that there’s a greater demand or need since the pandemic,” said Dr. Cantor. “We’ll just need more research to actually unpack what’s going on,” he said.
Initial per capita spending increased by about a third and was up overall by more than half. But it’s not clear how much of that is due to utilization or to price of services, said Dr. Cantor. Spending for telehealth services remained stable in the post-vaccine period, while spending on in-person visits returned to prepandemic levels.
Dr. Cantor and his colleagues were not able to determine whether utilization was by new or existing patients, but he said that would be good data to have. “It would be really important to know whether or not folks are initiating care because telehealth is making it easier,” he said.
The authors analyzed about 1.5 million claims for anxiety disorders, major depressive disorder, bipolar disorder, schizophrenia, and posttraumatic stress disorder, out of claims submitted by 7 million commercially insured adults whose self-insured employers used the Castlight benefit.
Dr. Cantor noted that this is just a small subset of the U.S. population. He said he’d like to have data from Medicare and Medicaid to fully assess the impact of the COVID-19 pandemic on mental health and of telehealth visits.
“This is a still-burgeoning field,” he said about telehealth. “We’re still trying to get a handle on how things are operating, given that there’s been so much change so rapidly.”
Meanwhile, 152 major employers responding to a large national survey this summer said that they’ve been grappling with how COVID-19 has affected workers. The employers include 72 Fortune 100 companies and provide health coverage for more than 60 million workers, retirees, and their families.
Seventy-seven percent said they are currently seeing an increase in depression, anxiety, and substance use disorders as a result of the pandemic, according to the Business Group on Health’s survey. That’s up from 44% in 2022.
Going forward, employers will focus on increasing access to mental health services, the survey reported.
“Our survey found that in 2024 and for the near future, employers will be acutely focused on addressing employees’ mental health needs while ensuring access and lowering cost barriers,” Ellen Kelsay, president and CEO of Business Group on Health, said in a statement.
The study was supported by grants from the National Institute of Mental Health and the National Institute on Aging. Coauthor Dena Bravata, MD, a Castlight employee, reported receiving personal fees from Castlight Health during the conduct of the study. Coauthor Christopher M. Whaley, a RAND employee, reported receiving personal fees from Castlight Health outside the submitted work.
A version of this article appeared on Medscape.com.
By the end of August 2022, overall use of mental health services was almost 40% higher than before the COVID-19 pandemic, while spending increased by 54%, according to a new study by researchers at the RAND Corporation.
During the early phase of the pandemic, from mid-March to mid-December 2020, before the vaccine was available, in-person visits decreased by 40%, while telehealth visits increased by 1,000%, reported Jonathan H. Cantor, PhD, and colleagues at RAND, and at Castlight Health, a benefit coordination provider, in a paper published online in JAMA Health Forum.
Between December 2020 and August 2022, telehealth visits stayed stable, but in-person visits creeped back up, eventually reaching 80% of prepandemic levels. However, “total utilization was higher than before the pandemic,” Dr. Cantor, a policy researcher at RAND, told this news organization.
“It could be that it’s easier for individuals to receive care via telehealth, but it could also just be that there’s a greater demand or need since the pandemic,” said Dr. Cantor. “We’ll just need more research to actually unpack what’s going on,” he said.
Initial per capita spending increased by about a third and was up overall by more than half. But it’s not clear how much of that is due to utilization or to price of services, said Dr. Cantor. Spending for telehealth services remained stable in the post-vaccine period, while spending on in-person visits returned to prepandemic levels.
Dr. Cantor and his colleagues were not able to determine whether utilization was by new or existing patients, but he said that would be good data to have. “It would be really important to know whether or not folks are initiating care because telehealth is making it easier,” he said.
The authors analyzed about 1.5 million claims for anxiety disorders, major depressive disorder, bipolar disorder, schizophrenia, and posttraumatic stress disorder, out of claims submitted by 7 million commercially insured adults whose self-insured employers used the Castlight benefit.
Dr. Cantor noted that this is just a small subset of the U.S. population. He said he’d like to have data from Medicare and Medicaid to fully assess the impact of the COVID-19 pandemic on mental health and of telehealth visits.
“This is a still-burgeoning field,” he said about telehealth. “We’re still trying to get a handle on how things are operating, given that there’s been so much change so rapidly.”
Meanwhile, 152 major employers responding to a large national survey this summer said that they’ve been grappling with how COVID-19 has affected workers. The employers include 72 Fortune 100 companies and provide health coverage for more than 60 million workers, retirees, and their families.
Seventy-seven percent said they are currently seeing an increase in depression, anxiety, and substance use disorders as a result of the pandemic, according to the Business Group on Health’s survey. That’s up from 44% in 2022.
Going forward, employers will focus on increasing access to mental health services, the survey reported.
“Our survey found that in 2024 and for the near future, employers will be acutely focused on addressing employees’ mental health needs while ensuring access and lowering cost barriers,” Ellen Kelsay, president and CEO of Business Group on Health, said in a statement.
The study was supported by grants from the National Institute of Mental Health and the National Institute on Aging. Coauthor Dena Bravata, MD, a Castlight employee, reported receiving personal fees from Castlight Health during the conduct of the study. Coauthor Christopher M. Whaley, a RAND employee, reported receiving personal fees from Castlight Health outside the submitted work.
A version of this article appeared on Medscape.com.
Rheumatology trials seem vulnerable to unblinding: Report
Until more is known about the potential for unblinding, clinicians need to keep in mind that patients and physicians could often guess accurately who was getting placebo or active drug, first author Cody Bruggemeyer, MD, a resident at the Medical College of Wisconsin, Milwaukee, said in an interview.
“It’s important that rheumatologists be aware of this potential issue and use their clinical reasoning and their ability to critically assess papers to evaluate the study design” of research on treatments, he said in an interview.
Dr. Bruggemeyer and coauthors at the Medical College of Wisconsin presented their assessment of the potential for unblinding in a Viewpoint article in The Lancet Rheumatology.
A sample of pivotal clinical trials
The authors selected a sample of pivotal studies of 14 commonly prescribed drugs for rheumatic conditions for which double-blind randomized controlled trials (RCTs) that compared the active ingredient with a placebo were available.
The 14 trials involved treatments classified as disease-modifying antirheumatic drugs (DMARDs), some of which were likely to produce side effects that placebos would not mimic, such as injection site and infusion reactions and difference in readings in lab reports, the authors wrote.
In their analysis, Dr. Bruggemeyer and colleagues evaluated discrepancies in the rates of adverse events reported between active drugs and placebos and classified the 14 studies as follows:
- High unblinding risk: Nine studies had a high estimated risk of unblinding, including trials of adalimumab with citrate (Humira), anakinra (Kineret), anifrolumab (Saphnelo), apremilast (Otezla), ixekizumab (Taltz), leflunomide (Arava), methotrexate, risankizumab (Skyrizi) and tofacitinib (Xeljanz).
- Moderate unblinding risk: Three studies had a moderate estimated risk of unblinding, including trials of azathioprine (Imuran), mycophenolate mofetil and tocilizumab (Actemra).
- Low unblinding risk: Two studies had a low estimated risk of unblinding. These involved tests of belimumab (Benlysta) and rituximab (Rituxan).
Many of the effectiveness measurements of treatments used in rheumatology depend on patients’ reports of relief of pain and other disease symptoms. For example, the widely used American College of Rheumatology 20% response for rheumatoid arthritis includes components that rely on patient and physician assessment of disease activity.
Unblinding risk to clinical trial validity
CTs are the highest level of evidence to establish efficacy, because the study design aims to mask whether the experimental treatment is a drug or placebo. In cases where patients and physicians are more likely to correctly detect use of an active drug, there can be biases that skew results toward reports of symptom improvement. Other patients’ views of their treatment may be distorted by accurate guesses that they have been given placebo, Dr. Bruggemeyer and coauthors wrote.
“The degree of these effects cannot be predicted, but they tend to erroneously inflate the perceived benefit of novel interventions,” they wrote.
The consequences of this unblinding may be minimal in cases where there’s a clear difference between the placebo and active drug, they said. As an example, they cited trials of interleukin-23 inhibitors for psoriasis, where skin clearance as measured by the Psoriatic Area and Severity Index 75 differed by more than 50% in absolute terms between the treatment and placebo groups.
But in other cases, there needs to be more attention paid to the potential role of unblinding, they wrote.
“Studies where effect sizes were small, contradictory, or dependent on subgroup analyses might be especially problematic, but commentary rarely reflects this issue or acknowledges the potential influence of unblinding,” they wrote.
In the paper, they call for more analysis of previous trials to look for unreported assessments of unblinding, while also asking that researchers consider surveying participants in future trials to evaluate the degree to which unblinding occurs.
“Advocacy from professional societies and the U.S. Food and Drug Administration itself might be necessary, but in the interim, rheumatologists should assume unblinding has occurred to some degree in most trials,” they wrote.
Unblinding measure needs validation
In an interview, Roy M. Fleischmann, MD, co–medical director of the Metroplex Clinical Research Center in Dallas, raised some objections to the paper. The paper addresses an interesting question about unblinding, but there should have been more work done, such as finding “a measure that is validated that can say whether you’ve been unblinded or not.”
He added that he was surprised the paper on unblinding in rheumatology trials was published in its current form.
“I would have sent it for a major rewrite” if asked to review this paper before publication, said Dr. Fleischmann, who as a reviewer for Lancet Rheumatology. “I would have said: ‘Okay, 90% of this paper is okay, but your gist is not correct.’ It should be: ‘Is this a problem?’ ”
Dr. Fleischmann said he would have recommended a different perspective to the paper. “That is, this could occur. Should we be looking at this, and how would we look at this?”
In the paper, the authors acknowledge their approach has not been validated, “but it highlights the potential effect of idiosyncratic adverse events,” they wrote.
There’s less funding in general for meta-research than for studies involving treatments, so researchers look for approaches that can be handled without requiring significant funding, and much of the research on the quality of research is conducted like this analysis of rheumatology trials, Michael Putman, MD, the corresponding author and is a rheumatologist and an assistant professor at the Medical College of Wisconsin, said in an interview.
“You’re mostly doing on a shoestring budget with yourself and trainees,” he said. Dr. Putman is an associate editor at the journal Rheumatology and also involved in meta-research, or efforts to understand how studies and trials answer questions about how medical treatments work.
In an Aug. 16 tweet, Dr. Putman said this issue of unintentional unblinding with rheumatology trials was something he’d “been ruminating about for awhile; took two all star trainees to push it over the top!”
One of the barriers to funding of meta-research is a tendency for major funding for medical studies to be focused on specific diseases or targets. With meta-research, it may be more difficult to explain how a specific project will advance efforts to treat or prevent a certain disease, Dr. Putman said.
“It’s a little more esoteric and maybe not quite as clear how these projects will move things forward,” Dr. Putman said.
In addition, the nature of meta-research is to question and often be critical of work that’s already been published, adding another hurdle in attempts to secure funding, he said.
Dr. Putman is supported by a Rheumatology Research Foundation Scientist Development Grant, receives research funding related to clinical trials by AbbVie and AstraZeneca, and consulting fees from Novartis. The other authors declared no competing interests.
Until more is known about the potential for unblinding, clinicians need to keep in mind that patients and physicians could often guess accurately who was getting placebo or active drug, first author Cody Bruggemeyer, MD, a resident at the Medical College of Wisconsin, Milwaukee, said in an interview.
“It’s important that rheumatologists be aware of this potential issue and use their clinical reasoning and their ability to critically assess papers to evaluate the study design” of research on treatments, he said in an interview.
Dr. Bruggemeyer and coauthors at the Medical College of Wisconsin presented their assessment of the potential for unblinding in a Viewpoint article in The Lancet Rheumatology.
A sample of pivotal clinical trials
The authors selected a sample of pivotal studies of 14 commonly prescribed drugs for rheumatic conditions for which double-blind randomized controlled trials (RCTs) that compared the active ingredient with a placebo were available.
The 14 trials involved treatments classified as disease-modifying antirheumatic drugs (DMARDs), some of which were likely to produce side effects that placebos would not mimic, such as injection site and infusion reactions and difference in readings in lab reports, the authors wrote.
In their analysis, Dr. Bruggemeyer and colleagues evaluated discrepancies in the rates of adverse events reported between active drugs and placebos and classified the 14 studies as follows:
- High unblinding risk: Nine studies had a high estimated risk of unblinding, including trials of adalimumab with citrate (Humira), anakinra (Kineret), anifrolumab (Saphnelo), apremilast (Otezla), ixekizumab (Taltz), leflunomide (Arava), methotrexate, risankizumab (Skyrizi) and tofacitinib (Xeljanz).
- Moderate unblinding risk: Three studies had a moderate estimated risk of unblinding, including trials of azathioprine (Imuran), mycophenolate mofetil and tocilizumab (Actemra).
- Low unblinding risk: Two studies had a low estimated risk of unblinding. These involved tests of belimumab (Benlysta) and rituximab (Rituxan).
Many of the effectiveness measurements of treatments used in rheumatology depend on patients’ reports of relief of pain and other disease symptoms. For example, the widely used American College of Rheumatology 20% response for rheumatoid arthritis includes components that rely on patient and physician assessment of disease activity.
Unblinding risk to clinical trial validity
CTs are the highest level of evidence to establish efficacy, because the study design aims to mask whether the experimental treatment is a drug or placebo. In cases where patients and physicians are more likely to correctly detect use of an active drug, there can be biases that skew results toward reports of symptom improvement. Other patients’ views of their treatment may be distorted by accurate guesses that they have been given placebo, Dr. Bruggemeyer and coauthors wrote.
“The degree of these effects cannot be predicted, but they tend to erroneously inflate the perceived benefit of novel interventions,” they wrote.
The consequences of this unblinding may be minimal in cases where there’s a clear difference between the placebo and active drug, they said. As an example, they cited trials of interleukin-23 inhibitors for psoriasis, where skin clearance as measured by the Psoriatic Area and Severity Index 75 differed by more than 50% in absolute terms between the treatment and placebo groups.
But in other cases, there needs to be more attention paid to the potential role of unblinding, they wrote.
“Studies where effect sizes were small, contradictory, or dependent on subgroup analyses might be especially problematic, but commentary rarely reflects this issue or acknowledges the potential influence of unblinding,” they wrote.
In the paper, they call for more analysis of previous trials to look for unreported assessments of unblinding, while also asking that researchers consider surveying participants in future trials to evaluate the degree to which unblinding occurs.
“Advocacy from professional societies and the U.S. Food and Drug Administration itself might be necessary, but in the interim, rheumatologists should assume unblinding has occurred to some degree in most trials,” they wrote.
Unblinding measure needs validation
In an interview, Roy M. Fleischmann, MD, co–medical director of the Metroplex Clinical Research Center in Dallas, raised some objections to the paper. The paper addresses an interesting question about unblinding, but there should have been more work done, such as finding “a measure that is validated that can say whether you’ve been unblinded or not.”
He added that he was surprised the paper on unblinding in rheumatology trials was published in its current form.
“I would have sent it for a major rewrite” if asked to review this paper before publication, said Dr. Fleischmann, who as a reviewer for Lancet Rheumatology. “I would have said: ‘Okay, 90% of this paper is okay, but your gist is not correct.’ It should be: ‘Is this a problem?’ ”
Dr. Fleischmann said he would have recommended a different perspective to the paper. “That is, this could occur. Should we be looking at this, and how would we look at this?”
In the paper, the authors acknowledge their approach has not been validated, “but it highlights the potential effect of idiosyncratic adverse events,” they wrote.
There’s less funding in general for meta-research than for studies involving treatments, so researchers look for approaches that can be handled without requiring significant funding, and much of the research on the quality of research is conducted like this analysis of rheumatology trials, Michael Putman, MD, the corresponding author and is a rheumatologist and an assistant professor at the Medical College of Wisconsin, said in an interview.
“You’re mostly doing on a shoestring budget with yourself and trainees,” he said. Dr. Putman is an associate editor at the journal Rheumatology and also involved in meta-research, or efforts to understand how studies and trials answer questions about how medical treatments work.
In an Aug. 16 tweet, Dr. Putman said this issue of unintentional unblinding with rheumatology trials was something he’d “been ruminating about for awhile; took two all star trainees to push it over the top!”
One of the barriers to funding of meta-research is a tendency for major funding for medical studies to be focused on specific diseases or targets. With meta-research, it may be more difficult to explain how a specific project will advance efforts to treat or prevent a certain disease, Dr. Putman said.
“It’s a little more esoteric and maybe not quite as clear how these projects will move things forward,” Dr. Putman said.
In addition, the nature of meta-research is to question and often be critical of work that’s already been published, adding another hurdle in attempts to secure funding, he said.
Dr. Putman is supported by a Rheumatology Research Foundation Scientist Development Grant, receives research funding related to clinical trials by AbbVie and AstraZeneca, and consulting fees from Novartis. The other authors declared no competing interests.
Until more is known about the potential for unblinding, clinicians need to keep in mind that patients and physicians could often guess accurately who was getting placebo or active drug, first author Cody Bruggemeyer, MD, a resident at the Medical College of Wisconsin, Milwaukee, said in an interview.
“It’s important that rheumatologists be aware of this potential issue and use their clinical reasoning and their ability to critically assess papers to evaluate the study design” of research on treatments, he said in an interview.
Dr. Bruggemeyer and coauthors at the Medical College of Wisconsin presented their assessment of the potential for unblinding in a Viewpoint article in The Lancet Rheumatology.
A sample of pivotal clinical trials
The authors selected a sample of pivotal studies of 14 commonly prescribed drugs for rheumatic conditions for which double-blind randomized controlled trials (RCTs) that compared the active ingredient with a placebo were available.
The 14 trials involved treatments classified as disease-modifying antirheumatic drugs (DMARDs), some of which were likely to produce side effects that placebos would not mimic, such as injection site and infusion reactions and difference in readings in lab reports, the authors wrote.
In their analysis, Dr. Bruggemeyer and colleagues evaluated discrepancies in the rates of adverse events reported between active drugs and placebos and classified the 14 studies as follows:
- High unblinding risk: Nine studies had a high estimated risk of unblinding, including trials of adalimumab with citrate (Humira), anakinra (Kineret), anifrolumab (Saphnelo), apremilast (Otezla), ixekizumab (Taltz), leflunomide (Arava), methotrexate, risankizumab (Skyrizi) and tofacitinib (Xeljanz).
- Moderate unblinding risk: Three studies had a moderate estimated risk of unblinding, including trials of azathioprine (Imuran), mycophenolate mofetil and tocilizumab (Actemra).
- Low unblinding risk: Two studies had a low estimated risk of unblinding. These involved tests of belimumab (Benlysta) and rituximab (Rituxan).
Many of the effectiveness measurements of treatments used in rheumatology depend on patients’ reports of relief of pain and other disease symptoms. For example, the widely used American College of Rheumatology 20% response for rheumatoid arthritis includes components that rely on patient and physician assessment of disease activity.
Unblinding risk to clinical trial validity
CTs are the highest level of evidence to establish efficacy, because the study design aims to mask whether the experimental treatment is a drug or placebo. In cases where patients and physicians are more likely to correctly detect use of an active drug, there can be biases that skew results toward reports of symptom improvement. Other patients’ views of their treatment may be distorted by accurate guesses that they have been given placebo, Dr. Bruggemeyer and coauthors wrote.
“The degree of these effects cannot be predicted, but they tend to erroneously inflate the perceived benefit of novel interventions,” they wrote.
The consequences of this unblinding may be minimal in cases where there’s a clear difference between the placebo and active drug, they said. As an example, they cited trials of interleukin-23 inhibitors for psoriasis, where skin clearance as measured by the Psoriatic Area and Severity Index 75 differed by more than 50% in absolute terms between the treatment and placebo groups.
But in other cases, there needs to be more attention paid to the potential role of unblinding, they wrote.
“Studies where effect sizes were small, contradictory, or dependent on subgroup analyses might be especially problematic, but commentary rarely reflects this issue or acknowledges the potential influence of unblinding,” they wrote.
In the paper, they call for more analysis of previous trials to look for unreported assessments of unblinding, while also asking that researchers consider surveying participants in future trials to evaluate the degree to which unblinding occurs.
“Advocacy from professional societies and the U.S. Food and Drug Administration itself might be necessary, but in the interim, rheumatologists should assume unblinding has occurred to some degree in most trials,” they wrote.
Unblinding measure needs validation
In an interview, Roy M. Fleischmann, MD, co–medical director of the Metroplex Clinical Research Center in Dallas, raised some objections to the paper. The paper addresses an interesting question about unblinding, but there should have been more work done, such as finding “a measure that is validated that can say whether you’ve been unblinded or not.”
He added that he was surprised the paper on unblinding in rheumatology trials was published in its current form.
“I would have sent it for a major rewrite” if asked to review this paper before publication, said Dr. Fleischmann, who as a reviewer for Lancet Rheumatology. “I would have said: ‘Okay, 90% of this paper is okay, but your gist is not correct.’ It should be: ‘Is this a problem?’ ”
Dr. Fleischmann said he would have recommended a different perspective to the paper. “That is, this could occur. Should we be looking at this, and how would we look at this?”
In the paper, the authors acknowledge their approach has not been validated, “but it highlights the potential effect of idiosyncratic adverse events,” they wrote.
There’s less funding in general for meta-research than for studies involving treatments, so researchers look for approaches that can be handled without requiring significant funding, and much of the research on the quality of research is conducted like this analysis of rheumatology trials, Michael Putman, MD, the corresponding author and is a rheumatologist and an assistant professor at the Medical College of Wisconsin, said in an interview.
“You’re mostly doing on a shoestring budget with yourself and trainees,” he said. Dr. Putman is an associate editor at the journal Rheumatology and also involved in meta-research, or efforts to understand how studies and trials answer questions about how medical treatments work.
In an Aug. 16 tweet, Dr. Putman said this issue of unintentional unblinding with rheumatology trials was something he’d “been ruminating about for awhile; took two all star trainees to push it over the top!”
One of the barriers to funding of meta-research is a tendency for major funding for medical studies to be focused on specific diseases or targets. With meta-research, it may be more difficult to explain how a specific project will advance efforts to treat or prevent a certain disease, Dr. Putman said.
“It’s a little more esoteric and maybe not quite as clear how these projects will move things forward,” Dr. Putman said.
In addition, the nature of meta-research is to question and often be critical of work that’s already been published, adding another hurdle in attempts to secure funding, he said.
Dr. Putman is supported by a Rheumatology Research Foundation Scientist Development Grant, receives research funding related to clinical trials by AbbVie and AstraZeneca, and consulting fees from Novartis. The other authors declared no competing interests.
FROM THE LANCET RHEUMATOLOGY






