User login
CDC finds cluster of newborns with late VKDB

Photo by Bertrand Devouard
The Centers for Disease Control and Prevention (CDC) has identified a
small group of newborns in Tennessee with late vitamin K deficiency
bleeding (VKDB).
The agency reported 4 cases of late VKDB, a
serious but preventable bleeding disorder that can cause intracranial
hemorrhage, neurological deficits, and death.
In each case, the newborn’s parents
declined a vitamin K injection at birth, mainly because they were
uninformed about the risk of late VKBD.
Preliminary findings of the CDC’s investigation, in collaboration with the Tennessee Department of Health, appear in the current issue of the Morbidity and Mortality Weekly Report.
“Not giving vitamin K at birth is an emerging trend that can have devastating outcomes for infants and their families,” said CDC Director Tom Frieden, MD. “Ensuring that every newborn receives a vitamin K injection at birth is critical to protect infants.”
Between February and September of this year, 4 cases of late VKDB were diagnosed at a hospital in Nashville, Tennessee.
Three of the infants experienced intracranial hemorrhage, and the fourth had gastrointestinal bleeding. None of the patients had received a vitamin K injection at birth.
Fortunately, all of the infants survived. The patient with gastrointestinal bleeding has made a full recovery. And the 3 infants with intracranial hemorrhage are being followed by neurologists.
One patient has an apparent gross motor deficit, but it seems the others do not. However, all of the patients are still less than 1 year of age, so the full impact of VKDB might only become apparent with time.
The infants’ parents said they declined vitamin K prophylaxis for a number of reasons, including concern about an increased risk of leukemia, the belief that the injection was unnecessary, and a desire to minimize the newborn’s exposure to “toxins.”
Concern about the increased risk of leukemia associated with vitamin K prophylaxis was initially generated by a report published in 1992, but the finding has not been replicated in subsequent studies.
In all cases, parents were uninformed or insufficiently informed about the risk of late VKDB. Most parents only learned about the possibility of late VKDB after their infants developed the condition.
These findings illustrate the importance of educating parents about vitamin K prophylaxis, said Lauren Marcewicz, MD, of the CDC’s National Center on Birth Defects and Developmental Disabilities.
A vitamin K injection at birth has been standard practice in the US since it was first recommended as prophylaxis for late VKDB by the American Academy of Pediatrics in 1961.
The late form of VKDB can develop in infants 2 weeks to 6 months of age who did not receive a vitamin K injection and do not have enough vitamin K-dependent proteins in their bodies to allow normal blood clotting. If untreated, this can cause intracranial hemorrhage, which may lead to neurological problems and can be fatal.
The risk for developing late VKDB has been estimated at 81 times greater among infants who do not receive a vitamin K injection at birth than in infants who do receive it.
The CDC said it is currently working with the Tennessee Department of Health to determine if other cases of late VKDB occurred in the state in recent years.
In addition, a case-control study is underway to assess whether any additional risk factors might contribute to the development of late VKDB in children who do not receive vitamin K prophylaxis. ![]()

Photo by Bertrand Devouard
The Centers for Disease Control and Prevention (CDC) has identified a
small group of newborns in Tennessee with late vitamin K deficiency
bleeding (VKDB).
The agency reported 4 cases of late VKDB, a
serious but preventable bleeding disorder that can cause intracranial
hemorrhage, neurological deficits, and death.
In each case, the newborn’s parents
declined a vitamin K injection at birth, mainly because they were
uninformed about the risk of late VKBD.
Preliminary findings of the CDC’s investigation, in collaboration with the Tennessee Department of Health, appear in the current issue of the Morbidity and Mortality Weekly Report.
“Not giving vitamin K at birth is an emerging trend that can have devastating outcomes for infants and their families,” said CDC Director Tom Frieden, MD. “Ensuring that every newborn receives a vitamin K injection at birth is critical to protect infants.”
Between February and September of this year, 4 cases of late VKDB were diagnosed at a hospital in Nashville, Tennessee.
Three of the infants experienced intracranial hemorrhage, and the fourth had gastrointestinal bleeding. None of the patients had received a vitamin K injection at birth.
Fortunately, all of the infants survived. The patient with gastrointestinal bleeding has made a full recovery. And the 3 infants with intracranial hemorrhage are being followed by neurologists.
One patient has an apparent gross motor deficit, but it seems the others do not. However, all of the patients are still less than 1 year of age, so the full impact of VKDB might only become apparent with time.
The infants’ parents said they declined vitamin K prophylaxis for a number of reasons, including concern about an increased risk of leukemia, the belief that the injection was unnecessary, and a desire to minimize the newborn’s exposure to “toxins.”
Concern about the increased risk of leukemia associated with vitamin K prophylaxis was initially generated by a report published in 1992, but the finding has not been replicated in subsequent studies.
In all cases, parents were uninformed or insufficiently informed about the risk of late VKDB. Most parents only learned about the possibility of late VKDB after their infants developed the condition.
These findings illustrate the importance of educating parents about vitamin K prophylaxis, said Lauren Marcewicz, MD, of the CDC’s National Center on Birth Defects and Developmental Disabilities.
A vitamin K injection at birth has been standard practice in the US since it was first recommended as prophylaxis for late VKDB by the American Academy of Pediatrics in 1961.
The late form of VKDB can develop in infants 2 weeks to 6 months of age who did not receive a vitamin K injection and do not have enough vitamin K-dependent proteins in their bodies to allow normal blood clotting. If untreated, this can cause intracranial hemorrhage, which may lead to neurological problems and can be fatal.
The risk for developing late VKDB has been estimated at 81 times greater among infants who do not receive a vitamin K injection at birth than in infants who do receive it.
The CDC said it is currently working with the Tennessee Department of Health to determine if other cases of late VKDB occurred in the state in recent years.
In addition, a case-control study is underway to assess whether any additional risk factors might contribute to the development of late VKDB in children who do not receive vitamin K prophylaxis. ![]()

Photo by Bertrand Devouard
The Centers for Disease Control and Prevention (CDC) has identified a
small group of newborns in Tennessee with late vitamin K deficiency
bleeding (VKDB).
The agency reported 4 cases of late VKDB, a
serious but preventable bleeding disorder that can cause intracranial
hemorrhage, neurological deficits, and death.
In each case, the newborn’s parents
declined a vitamin K injection at birth, mainly because they were
uninformed about the risk of late VKBD.
Preliminary findings of the CDC’s investigation, in collaboration with the Tennessee Department of Health, appear in the current issue of the Morbidity and Mortality Weekly Report.
“Not giving vitamin K at birth is an emerging trend that can have devastating outcomes for infants and their families,” said CDC Director Tom Frieden, MD. “Ensuring that every newborn receives a vitamin K injection at birth is critical to protect infants.”
Between February and September of this year, 4 cases of late VKDB were diagnosed at a hospital in Nashville, Tennessee.
Three of the infants experienced intracranial hemorrhage, and the fourth had gastrointestinal bleeding. None of the patients had received a vitamin K injection at birth.
Fortunately, all of the infants survived. The patient with gastrointestinal bleeding has made a full recovery. And the 3 infants with intracranial hemorrhage are being followed by neurologists.
One patient has an apparent gross motor deficit, but it seems the others do not. However, all of the patients are still less than 1 year of age, so the full impact of VKDB might only become apparent with time.
The infants’ parents said they declined vitamin K prophylaxis for a number of reasons, including concern about an increased risk of leukemia, the belief that the injection was unnecessary, and a desire to minimize the newborn’s exposure to “toxins.”
Concern about the increased risk of leukemia associated with vitamin K prophylaxis was initially generated by a report published in 1992, but the finding has not been replicated in subsequent studies.
In all cases, parents were uninformed or insufficiently informed about the risk of late VKDB. Most parents only learned about the possibility of late VKDB after their infants developed the condition.
These findings illustrate the importance of educating parents about vitamin K prophylaxis, said Lauren Marcewicz, MD, of the CDC’s National Center on Birth Defects and Developmental Disabilities.
A vitamin K injection at birth has been standard practice in the US since it was first recommended as prophylaxis for late VKDB by the American Academy of Pediatrics in 1961.
The late form of VKDB can develop in infants 2 weeks to 6 months of age who did not receive a vitamin K injection and do not have enough vitamin K-dependent proteins in their bodies to allow normal blood clotting. If untreated, this can cause intracranial hemorrhage, which may lead to neurological problems and can be fatal.
The risk for developing late VKDB has been estimated at 81 times greater among infants who do not receive a vitamin K injection at birth than in infants who do receive it.
The CDC said it is currently working with the Tennessee Department of Health to determine if other cases of late VKDB occurred in the state in recent years.
In addition, a case-control study is underway to assess whether any additional risk factors might contribute to the development of late VKDB in children who do not receive vitamin K prophylaxis. ![]()
Evaluating an Academic Hospitalist Service
Improving quality while reducing costs remains important for hospitals across the United States, including the approximately 150 hospitals that are part of the Veterans Affairs (VA) healthcare system.[1, 2] The field of hospital medicine has grown rapidly, leading to predictions that the majority of inpatient care in the United States eventually will be delivered by hospitalists.[3, 4] In 2010, 57% of US hospitals had hospitalists on staff, including 87% of hospitals with 200 beds,[5] and nearly 80% of VA hospitals.[6]
The demand for hospitalists within teaching hospitals has grown in part as a response to the mandate to reduce residency work hours.[7] Furthermore, previous research has found that hospitalist care is associated with modest reductions in length of stay (LOS) and weak but inconsistent differences in quality.[8] The educational effect of hospitalists has been far less examined. The limited number of studies published to date suggests that hospitalists may improve resident learning and house‐officer satisfaction in academic medical centers and community teaching hospitals[9, 10, 11] and provide positive experiences for medical students12,13; however, Wachter et al reported no significant changes in clinical outcomes or patient, faculty, and house‐staff satisfaction in a newly designed hospital medicine service in San Francisco.[14] Additionally, whether using hospitalists influences nurse‐physician communication[15] is unknown.
Recognizing the limited and sometimes conflicting evidence about the hospitalist model, we report the results of a 3‐year quasi‐experimental evaluation of the experience at our medical center with academic hospitalists. As part of a VA Systems Redesign Improvement Capability Grantknown as the Hospital Outcomes Program of Excellence (HOPE) Initiativewe created a hospitalist‐based medicine team focused on quality improvement, medical education, and patient outcomes.
METHODS
Setting and Design
The main hospital of the VA Ann Arbor Healthcare System, located in Ann Arbor, Michigan, operates 105 acute‐care beds and 40 extended‐care beds. At the time of this evaluation, the medicine service consisted of 4 internal medicine teamsGold, Silver, Burgundy, and Yelloweach of which was responsible for admitting patients on a rotating basis every fourth day, with limited numbers of admissions occurring between each team's primary admitting day. Each team is led by an attending physician, a board‐certified (or board‐eligible) general internist or subspecialist who is also a faculty member at the University of Michigan Medical School. Each team has a senior medical resident, 2 to 3 interns, and 3 to 5 medical students (mostly third‐year students). In total, there are approximately 50 senior medical residents, 60 interns, and 170 medical students who rotate through the medicine service each year. Traditional rounding involves the medical students and interns receiving sign‐out from the overnight team in the morning, then pre‐rounding on each patient by obtaining an interval history, performing an exam, and checking any test results. A tentative plan of care is formed with the senior medical resident, usually by discussing each patient very quickly in the team room. Attending rounds are then conducted, with the physician team visiting each patient one by one to review and plan all aspects of care in detail. When time allows, small segments of teaching may occur during these attending work rounds. This system had been in place for >20 years.
Resulting in part from a grant received from the VA Systems Redesign Central Office (ie, the HOPE Initiative), the Gold team was modified in July 2009 and an academic hospitalist (S.S.) was assigned to head this team. Specific hospitalists were selected by the Associate Chief of Medicine (S.S.) and the Chief of Medicine (R.H.M.) to serve as Gold team attendings on a regular basis. The other teams continued to be overseen by the Chief of Medicine, and the Gold team remained within the medicine service. Characteristics of the Gold and nonGold team attendings can be found in Table 1. The 3 other teams initially were noninterventional concurrent control groups. However, during the second year of the evaluation, the Silver team adopted some of the initiatives as a result of the preliminary findings observed on Gold. Specifically, in the second year of the evaluation, approximately 42% of attendings on the Silver team were from the Gold team. This increased in the third year to 67% of coverage by Gold team attendings on the Silver team. The evaluation of the Gold team ended in June 2012.
| Characteristic | Gold Team | Non‐Gold Teams |
|---|---|---|
| Total number of attendings | 14 | 57 |
| Sex, % | ||
| Male | 79 | 58 |
| Female | 21 | 42 |
| Median years postresidency (range) | 10 (130) | 7 (141) |
| Subspecialists, % | 14 | 40 |
| Median days on service per year (range) | 53 (574) | 30 (592) |
The clinical interventions implemented on the Gold team were quality‐improvement work and were therefore exempt from institutional review board review. Human subjects' approval was, however, received to conduct interviews as part of a qualitative assessment.
Clinical Interventions
Several interventions involving the clinical care delivered were introduced on the Gold team, with a focus on improving communication among healthcare workers (Table 2).
| Clinical Interventions | Educational Interventions |
|---|---|
| Modified structure of attending rounds | Modified structure of attending rounds |
| Circle of Concern rounds | Attending reading list |
| Clinical Care Coordinator | Nifty Fifty reading list for learners |
| Regular attending team meetings | Website to provide expectations to learners |
| Two‐month per year commitment by attendings |
Structure of Attending Rounds
The structure of morning rounds was modified on the Gold team. Similar to the traditional structure, medical students and interns on the Gold team receive sign‐out from the overnight team in the morning. However, interns and students may or may not conduct pre‐rounds on each patient. The majority of time between sign‐out and the arrival of the attending physician is spent on work rounds. The senior resident leads rounds with the interns and students, discussing each patient while focusing on overnight events and current symptoms, new physical‐examination findings, and laboratory and test data. The plan of care to be presented to the attending is then formulated with the senior resident. The attending physician then leads Circle of Concern rounds with an expanded team, including a charge nurse, a clinical pharmacist, and a nurse Clinical Care Coordinator. Attending rounds tend to use an E‐AP format: significant Events overnight are discussed, followed by an Assessment & Plan by problem for the top active problems. Using this model, the attendings are able to focus more on teaching and discussing the patient plan than in the traditional model (in which the learner presents the details of the subjective, objective, laboratory, and radiographic data, with limited time left for the assessment and plan for each problem).
Circle of Concern Rounds
Suzanne Gordon described the Circle of Concern in her book Nursing Against the Odds.[16] From her observations, she noted that physicians typically form a circle to discuss patient care during rounds. The circle expands when another physician joins the group; however, the circle does not similarly expand to include nurses when they approach the group. Instead, nurses typically remain on the periphery, listening silently or trying to communicate to physicians' backs.[16] Thus, to promote nurse‐physician communication, Circle of Concern rounds were formally introduced on the Gold team. Each morning, the charge nurse rounds with the team and is encouraged to bring up nursing concerns. The inpatient clinical pharmacist is also included 2 to 3 times per week to help provide education to residents and students and perform medication reconciliation.
Clinical Care Coordinator
The role of the nurse Clinical Care Coordinatoralso introduced on the Gold teamis to provide continuity of patient care, facilitate interdisciplinary communication, facilitate patient discharge, ensure appropriate appointments are scheduled, communicate with the ambulatory care service to ensure proper transition between inpatient and outpatient care, and help educate residents and students on VA procedures and resources.
Regular Gold Team Meetings
All Gold team attendings are expected to dedicate 2 months per year to inpatient service (divided into half‐month blocks), instead of the average 1 month per year for attendings on the other teams. The Gold team attendings, unlike the other teams, also attend bimonthly meetings to discuss strategies for running the team.
Educational Interventions
Given the high number of learners on the medicine service, we wanted to enhance the educational experience for our learners. We thus implemented various interventions, in addition to the change in the structure of rounds, as described below.
Reading List for Learners: The Nifty Fifty
Because reading about clinical medicine is an integral part of medical education, we make explicit our expectation that residents and students read something clinically relevant every day. To promote this, we have provided a Nifty Fifty reading list of key articles. The PDF of each article is provided, along with a brief summary highlighting key points.
Reading List for Gold Attendings and Support Staff
To promote a common understanding of leadership techniques, management books are provided to Gold attending physicians and other members of the team (eg, Care Coordinator, nurse researcher, systems redesign engineer). One book is discussed at each Gold team meeting (Table 3), with participants taking turns leading the discussion.
| Book Title | Author(s) |
|---|---|
| The One Minute Manager | Ken Blanchard and Spencer Johnson |
| Good to Great | Jim Collins |
| Good to Great and the Social Sectors | Jim Collins |
| The Checklist Manifesto: How to Get Things Right | Atul Gawande |
| The Five Dysfunctions of a Team: A Leadership Fable | Patrick Lencioni |
| Getting to Yes: Negotiating Agreement Without Giving In | Roger Fisher, William Ury, and Bruce Patton |
| The Effective Executive: The Definitive Guide to Getting the Right Things Done | Peter Drucker |
| A Sense of Urgency | John Kotter |
| The Power of Positive Deviance: How Unlikely Innovators Solve the World's Toughest Problems | Richard Pascale, Jerry Sternin, and Monique Sternin |
| On the Mend: Revolutionizing Healthcare to Save Lives and Transform the Industry | John Toussaint and Roger Gerard |
| Outliers: The Story of Success | Malcolm Gladwell |
| Nursing Against the Odds: How Health Care Cost Cutting, Media Stereotypes, and Medical Hubris Undermine Nurses and Patient Care | Suzanne Gordon |
| How the Mighty Fall and Why Some Companies Never Give In | Jim Collins |
| What the Best College Teachers Do | Ken Bain |
| The Creative Destruction of Medicine | Eric Topol |
| What Got You Here Won't Get You There: How Successful People Become Even More Successful! | Marshall Goldsmith |
Website
A HOPE Initiative website was created (
Qualitative Assessment
To evaluate our efforts, we conducted a thorough qualitative assessment during the third year of the program. A total of 35 semistructured qualitative interviews were conducted with patients and staff from all levels of the organization, including senior leadership. The qualitative assessment was led by research staff from the Center for Clinical Management Research, who were minimally involved in the redesign effort and could provide an unbiased view of the initiative. Field notes from the semistructured interviews were analyzed, with themes developed using a descriptive approach and through discussion by a multidisciplinary team, which included building team consensus on findings that were supported by clear evidence in the data.[17]
Quantitative Outcome Measures
Clinical Outcomes
To determine if our communication and educational interventions had an impact on patient care, we used hospital administrative data to evaluate admission rates, LOS, and readmission rates for all 4 of the medicine teams. Additional clinical measures were assessed as needed. For example, we monitored the impact of the clinical pharmacist during a 4‐week pilot study by asking the Clinical Care Coordinator to track the proportion of patient encounters (n=170) in which the clinical pharmacist changed management or provided education to team members. Additionally, 2 staff surveys were conducted. The first survey focused on healthcare‐worker communication and was given to inpatient nurses and physicians (including attendings, residents, and medical students) who were recently on an inpatient medical service rotation. The survey included questions from previously validated communication measures,[18, 19, 20] as well as study‐specific questions. The second survey evaluated the new role of the Clinical Care Coordinator (Appendix). Both physicians and nurses who interacted with the Gold team's Clinical Care Coordinator were asked to complete this survey.
Educational Outcomes
To assess the educational interventions, we used learner evaluations of attendings, by both residents and medical students, and standardized internal medicine National Board of Medical Examiners Subject Examination (or shelf) scores for third‐year medical students. A separate evaluation of medical student perceptions of the rounding structure introduced on the Gold team using survey design has already been published.[21]
Statistical Analyses
Data from all sources were analyzed using SAS 9.3 (SAS Institute, Inc., Cary, NC). Outliers for the LOS variable were removed from the analysis. Means and frequency distributions were examined for all variables. Student t tests and [2] tests of independence were used to compare data between groups. Multivariable linear regression models controlling for time (preintervention vs postintervention) were used to assess the effect of the HOPE Initiative on patient LOS and readmission rates. In all cases, 2‐tailed P values of 0.05 or less were considered statistically significant.
Role of the Funding Source
The VA Office of Systems Redesign provided funding but was not involved in the design or conduct of the study, data analysis, or preparation of the manuscript.
RESULTS
Clinical Outcomes
Patient Outcomes
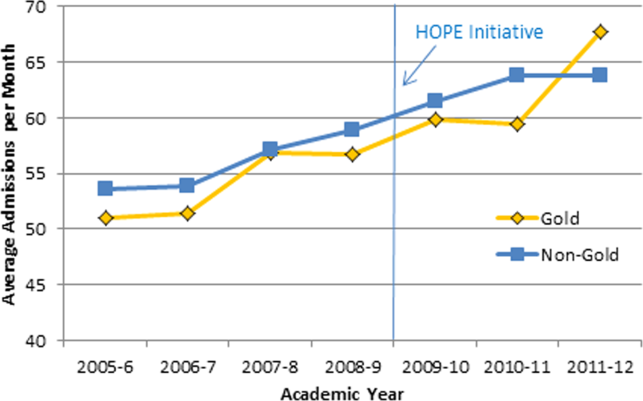
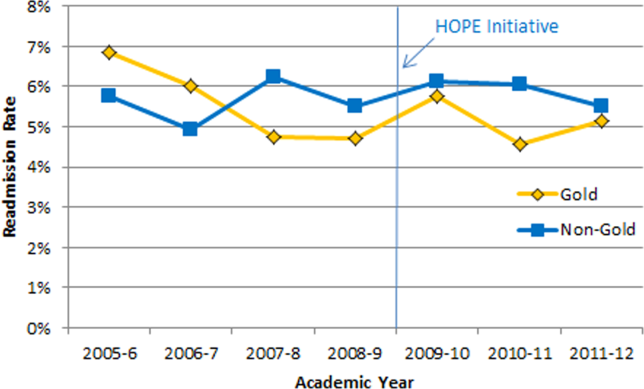
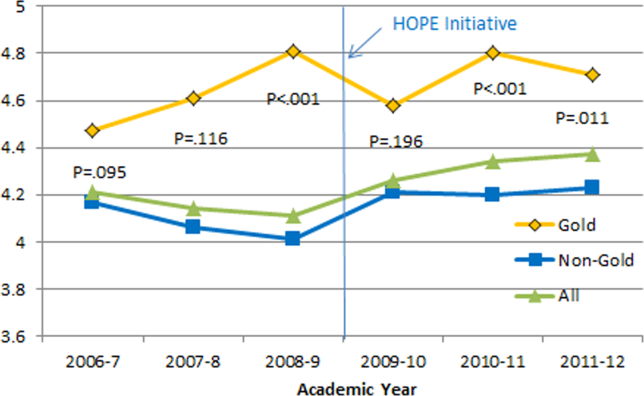
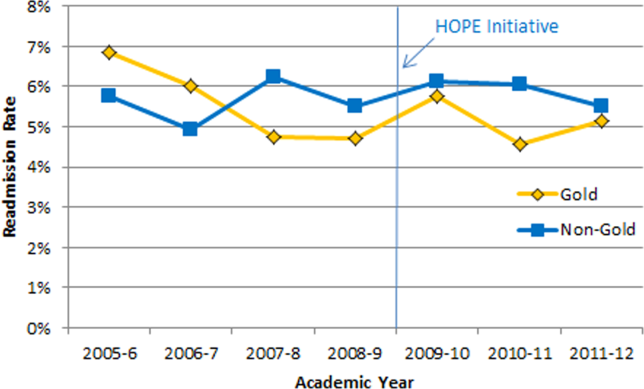
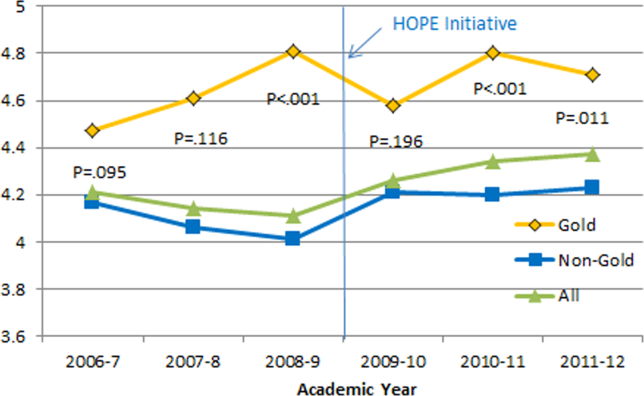
Our multivariable linear regression analysis, controlling for time, showed a significant reduction in LOS of approximately 0.3 days on all teams after the HOPE Initiative began (P=0.004). There were no significant differences between the Gold and non‐Gold teams in the multivariate models when controlling for time for any of the patient‐outcome measures. The number of admissions increased for all 4 medical teams (Figure 1), but, as shown in Figures 2 and 3, the readmission rates for all teams remained relatively stable over this same period of time.


Clinical Pharmacist on Gold Team Rounds
The inpatient clinical pharmacist changed the management plan for 22% of the patients seen on rounds. Contributions from the clinical pharmacist included adjusting the dosing of ordered medication and correcting medication reconciliation. Education and pharmaceutical information was provided to the team in another 6% of the 170 consecutive patient encounters evaluated.
Perception of Circle of Concern Rounds
Circle of Concern rounds were generally well‐received by both nurses and physicians. In a healthcare‐worker communication survey, completed by 38 physicians (62% response rate) and 48 nurses (54% response rate), the majority of both physicians (83%) and nurses (68%) felt Circle of Concern rounds improved communication.
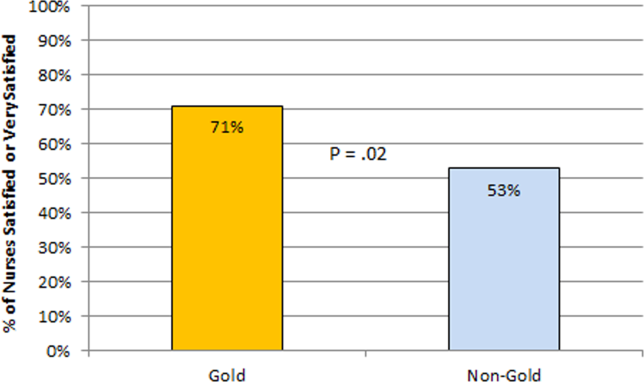
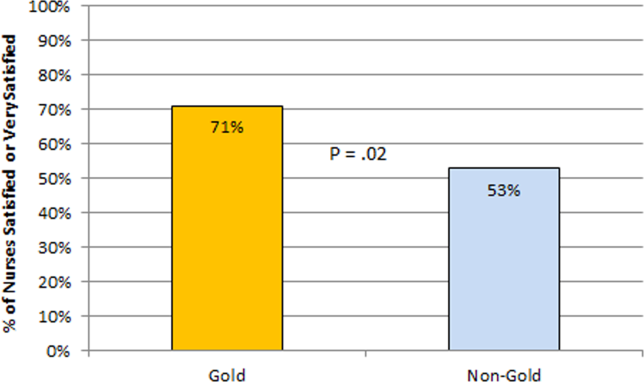
Nurse Perception of Communication
The healthcare‐worker communication survey asked inpatient nurses to rate communication between nurses and physicians on each of the 4 medicine teams. Significantly more nurses were satisfied with communication with the Gold team (71%) compared with the other 3 medicine teams (53%; P=0.02) (Figure 4).
Perception of the Clinical Care Coordinator
In total, 20 physicians (87% response rate) and 10 nurses (56% response rate) completed the Clinical Care Coordinator survey. The physician results were overwhelmingly positive: 100% were satisfied or very satisfied with the role; 100% felt each team should have a Clinical Care Coordinator; and 100% agreed or strongly agreed that the Clinical Care Coordinator ensures that appropriate follow‐up is arranged, provides continuity of care, assists with interdisciplinary communication, and helps facilitate discharge. The majority of nurses was also satisfied or very satisfied with the Clinical Care Coordinator role and felt each team should have one.
Educational Outcomes
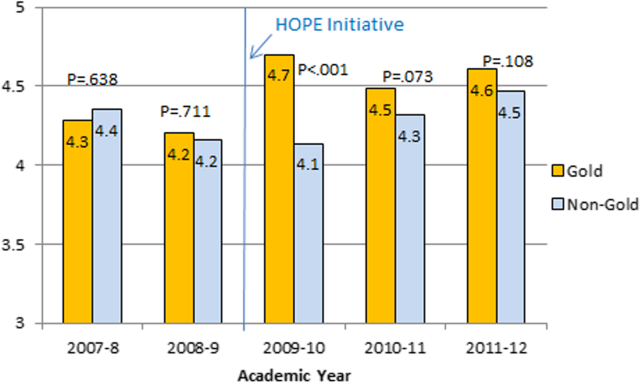
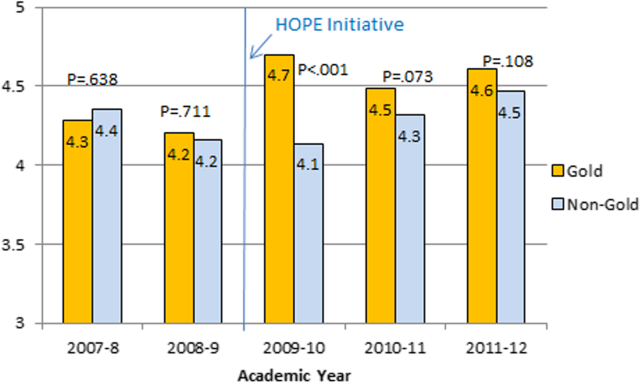
House Officer Evaluation of Attendings
Monthly evaluations of attending physicians by house officers (Figure 5) revealed that prior to the HOPE Initiative, little differences were observed between teams, as would be expected because attending assignment was largely random. After the intervention date of July 2009, however, significant differences were noted, with Gold team attendings receiving significantly higher teaching evaluations immediately after the introduction of the HOPE Initiative. Although ratings for Gold attendings remained more favorable, the difference was no longer statistically significant in the second and third year of the initiative, likely due to Gold attendings serving on other medicine teams, which contributed to an improvement in ratings of all attendings.
Medical Student Evaluation of Attendings
Monthly evaluations of attending physicians by third‐year medical students (Figure 6) revealed differences between the Gold attendings and all others, with the attendings that joined the Gold team in 2009 receiving higher teaching evaluations even before the HOPE Initiative started. However, this difference remained statistically significant in years 2 and 3 postinitiative, despite the addition of 4 new junior attendings.
Medical Student Medicine Shelf Scores
The national average on the shelf exam, which reflects learning after the internal medicine third‐year clerkship, has ranged from 75 to 78 for the past several years, with University of Michigan students averaging significantly higher scores prior to and after the HOPE Initiative. However, following the HOPE Initiative, third‐year medical students on the Gold team scored significantly higher on the shelf exam compared with their colleagues on the non‐Gold teams (84 vs 82; P=0.006). This difference in the shelf exam scores, although small, is statistically significant. It represents a measurable improvement in shelf scores in our system and demonstrates the potential educational benefit for the students. Over this same time period, scores on the United States Medical Licensing Exam, given to medical students at the beginning of their third year, remained stable (233 preHOPE Initiative; 234 postHOPE Initiative).
Qualitative Assessment
Qualitative data collected as part of our evaluation of the HOPE Initiative also suggested that nurse‐physician communication had improved since the start of the project. In particular, they reported positively on the Gold team in general, the Circle of Concern rounds, and the Clinical Care Coordinator (Table 4).
| Staff Type | Statement1 |
|---|---|
| |
| Nurse | [Gold is] above and beyond other [teams]. Other teams don't run as smoothly. |
| Nurse | There has been a difference in communication [on Gold]. You can tell the difference in how they communicate with staff. We know the Clinical Care Coordinator or charge nurse is rounding with that team, so there is more communication. |
| Nurse | The most important thing that has improved communication is the Circle of Concern rounds. |
| Physician | [The Gold Clinical Care Coordinator] expedites care, not only what to do but who to call. She can convey the urgency. On rounds she is able to break off, put in an order, place a call, talk to a patient. Things that we would do at 11 AM she gets to at 9 AM. A couple of hours may not seem like much, but sometimes it can make the difference between things happening that day instead of the next. |
| Physician | The Clinical Care Coordinator is completely indispensable. Major benefit to providing care to Veterans. |
| Physician | I like to think Gold has lifted all of the teams to a higher level. |
| Medical student | It may be due to personalities vs the Gold [team] itself, but there is more emphasis on best practices. Are we following guidelines even if it is not related to the primary reason for admission? |
| Medical student | Gold is very collegial and nurses/physicians know one another by name. Physicians request rather than order; this sets a good example to me on how to approach the nurses. |
| Chief resident | [Gold attendings] encourage senior residents to take charge and run the team, although the attending is there for back‐up and support. This provides great learning for the residents. Interns and medical students also are affected because they have to step up their game as well. |
DISCUSSION
Within academic medical centers, hospitalists are expected to care for patients, teach, and help improve the quality and efficiency of hospital‐based care.[7] The Department of Veterans Affairs runs the largest integrated healthcare system in the United States, with approximately 80% of VA hospitals having hospital medicine programs. Overall, one‐third of US residents perform part of their residency training at a VA hospital.[22, 23] Thus, the effects of a system‐wide change at a VA hospital may have implications throughout the country. We studied one such intervention. Our primary findings are that we were able to improve communication and learner education with minimal effects on patient outcomes. While overall LOS decreased slightly postintervention, after taking into account secular trends, readmission rates did not.
We are not the first to evaluate a hospital medicine team using a quasi‐experimental design. For example, Meltzer and colleagues evaluated a hospitalist program at the University of Chicago Medical Center and found that, by the second year of operation, hospitalist care was associated with significantly shorter LOS (0.49 days), reduced costs, and decreased mortality.[24] Auerbach also evaluated a newly created hospital medicine service, finding decreased LOS (0.61 days), lower costs, and lower risk of mortality by the second year of the program.[25]
Improving nurse‐physician communication is considered important for avoiding medical error,[26] yet there has been limited empirical study of methods to improve communication within the medical profession.[27] Based both on our surveys and qualitative interviews, healthcare‐worker communication appeared to improve on the Gold team during the study. A key component of this improvement is likely related to instituting Circle of Concern rounds, in which nurses joined the medical team during attending rounds. Such an intervention likely helped to address organizational silence[28] and enhance the psychological safety of the nursing staff, because the attending physician was proactive about soliciting the input of nurses during rounds.[29] Such leader inclusivenesswords and deeds exhibited by leaders that invite and appreciate others' contributionscan aid interdisciplinary teams in overcoming the negative effects of status differences, thereby promoting collaboration.[29] The inclusion of nurses on rounds is also relationship‐building, which Gotlib Conn and colleagues found was important to improved interprofessional communication and collaboration.[30] In the future, using a tool such as the Teamwork Effectiveness Assessment Module (TEAM) developed by the American Board of Internal Medicine[31] could provide further evaluation of the impact on interprofessional teamwork and communication.
The focus on learner education, though evaluated in prior studies, is also novel. One previous survey of medical students showed that engaging students in substantive discussions is associated with greater student satisfaction.[32] Another survey of medical students found that attendings who were enthusiastic about teaching, inspired confidence in knowledge and skills, provided useful feedback, and encouraged increased student responsibility were viewed as more effective teachers.[33] No previous study that we are aware of, however, has looked at actual educational outcomes, such as shelf scores. The National Board of Medical Examiners reports that the Medicine subject exam is scaled to have a mean of 70 and a standard deviation of 8.[34] Thus, a mean increase in score of 2 points is small, but not trivial. This shows improvement in a hard educational outcome. Additionally, 2 points, although small in the context of total score and standard deviation, may make a substantial difference to an individual student in terms of overall grade, and, thus, residency applications. Our finding that third‐year medical students on the Gold team performed significantly better than University of Michigan third‐year medical students on other teams is an intriguing finding that warrants confirmation. On the other hand, this finding is consistent with a previous report evaluating learner satisfaction in which Bodnar et al found improved ratings of quantity and quality of teaching on teams with a nontraditional structure (Gold team).[21] Moreover, despite relatively few studies, the reason underlying the educational benefit of hospitalists should surprise few. The hospitalist model ensures that learners are supervised by physicians who are experts in the care of hospitalized patients.[35] Hospitalists hired at teaching hospitals to work on services with learners are generally chosen because they possess superior educational skills.[7]
Our findings should be interpreted in the context of the following limitations. First, our study focused on a single academically affiliated VA hospital. As other VA hospitals are pursuing a similar approach (eg, the Houston and Detroit VA medical centers), replicating our results will be important. Second, the VA system, although the largest integrated healthcare system in the United States, has unique characteristicssuch as an integrated electronic health record and predominantly male patient populationthat may make generalizations to the larger US healthcare system challenging. Third, there was a slightly lower response rate among nurses on a few of the surveys to evaluate our efforts; however, this rate of response is standard at our facility. Finally, our evaluation lacks an empirical measure of healthcare‐worker communication, such as incident reports.
Despite these limitations, our results have important implications. Using both quantitative and qualitative assessment, we found that academic hospitalists have the ability to improve healthcare‐worker communication and enhance learner education without increasing LOS. These findings are directly applicable to VA medical centers and potentially applicable to other academic medical centers.
Acknowledgments
The authors thank Milisa Manojlovich, PhD, RN, Edward Kennedy, MS, and Andrew Hickner, MSI, for help with preparation of this manuscript.
Disclosures: This work was funded by a US Department of Veterans Affairs, Office of Systems Redesign Improvement Capability grant. The findings and conclusions in this report are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs. Dr. Saint reports receiving travel reimbursement for giving invited talks at the Society of Hospital Medicine's National Meeting, as well as serving on the advisory boards of Doximity and Jvion.
APPENDIX
Survey to Evaluate the Care Coordinator Position
| Yes | No | Not Sure | |
| Q1. Are you familiar with the role of the Care Coordinator on the Gold Service (Susan Lee)? | 1 | 2 | 3 |
Please indicate how much you agree or disagree with the statements below.
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | Don't Know | |
| Q2. The Care Coordinator ensures that appropriate primary care follow‐up and any other appropriate services are arranged. | 1 | 2 | 3 | 4 | 5 | 9 |
| Q3. The Care Coordinator provides continuity of patient care on the Gold Service. | 1 | 2 | 3 | 4 | 5 | 9 |
| Q4. The Care Coordinator helps educate House Officers and Medical Students on VA processes (e.g., CPRS). | 1 | 2 | 3 | 4 | 5 | 9 |
| Q5. The Care Coordinator assists with interdisciplinary communication between the medical team and other services (e.g., nursing, ambulatory care, pharmacy, social work) | 1 | 2 | 3 | 4 | 5 | 9 |
| Q6. The Care Coordinator helps facilitate patient discharge. | 1 | 2 | 3 | 4 | 5 | 9 |
| Q7. The Care Coordinator initiates communication with the ambulatory care teams to coordinate care. | 1 | 2 | 3 | 4 | 5 | 9 |
| Yes | No | |
| Q8. Are you a physician (attending or resident), or medical student who has been on more than one medical team at the VA (Gold, Silver, Burgundy, or Yellow)? | 1 | 2 |
If no, please skip to Q13
If yes, comparing your experience on the Gold Service (with the Care Coordinator) to your experience on any of the other services (Silver, Burgundy, or Yellow):
| Not at All | Very Little | Somewhat | To a Great Extent | |
| Q9. To what extent does the presence of a Care Coordinator affect patient care? | 1 | 2 | 3 | 4 |
| Q10. To what extent does the presence of a Care Coordinator improve patient flow? | 1 | 2 | 3 | 4 |
| Q11. To what extent does the presence of a Care Coordinator assist with education? | 1 | 2 | 3 | 4 |
| Q12. To what extent does the presence of a Care Coordinator contribute to attending rounds? | 1 | 2 | 3 | 4 |
| Yes | No | |
| Q13. Do you work [as a nurse] in ambulatory care? | 1 | 2 |
If no, please skip to Q17.
If yes, comparing your experience with the Gold Service (with the Care Coordinator) to the other services (Silver, Burgundy, or Yellow):
| Not at All | Very Little | Somewhat | To a Great Extent | |
| Q14. To what extent does the presence of a Care Coordinator improve coordination of care between inpatient and outpatient services? | 1 | 2 | 3 | 4 |
| Q15. To what extent does the presence of a Care Coordinator help identify high risk patients who require follow‐up? | 1 | 2 | 3 | 4 |
| Q16. To what extent does the presence of a Care Coordinator ensure follow‐up appointments are scheduled? | 1 | 2 | 3 | 4 |
| Yes | No | Not Sure | |
| Q17. Do you think each medical team should have a Care Coordinator? | 1 | 2 | 3 |
| Q18. Are there any additional tasks or duties you think would improve the effectiveness of the Care Coordinator? |
| Very Satisfied | Satisfied | Neutral | Dissatisfied | Very Dissatisfied | |
| Q19. Overall how satisfied are you with the role of the Care Coordinator on the Gold Service? | 1 | 2 | 3 | 4 | 5 |
| Q20. Do you have any other comments about the role of the Care Coordinator? |
| Q21. What is your position? |
| 1. Physician (attending or resident) or medical student |
| 2. Nurse (inpatient or ambulatory care) |
- Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, D.C.: National Academies Press; 2000.
- Institute of Medicine of the National Academies. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academies Press; 2001.
- , , , . Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102–1112.
- . Growth in care provided by hospitalists. N Engl J Med. 2009;360(26):2789–2791.
- American Hospital Association. AHA Annual Survey of Hospitals, 2010. Chicago, IL: Health Forum, LLC; 2010.
- , , , . Preventing hospital‐acquired infections: a national survey of practices reported by U.S. hospitals in 2005 and 2009. J Gen Intern Med. 2012;27(7):773–779.
- , . Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;19(4):392–393.
- , . Do hospitalist physicians improve the quality of inpatient care delivery? A systematic review of process, efficiency and outcome measures. BMC Med. 2011;9:58.
- , , , . Effect of hospitalist attending physicians on trainee educational experiences: a systematic review. J Hosp Med. 2009;4(8):490–498.
- , , , , , . Resident satisfaction on an academic hospitalist service: time to teach. Am J Med. 2002;112(7):597–601.
- , , , et al. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19(4):293–301.
- , . Third‐year medical students' evaluation of hospitalist and nonhospitalist faculty during the inpatient portion of their pediatrics clerkships. J Hosp Med. 2007;2(1):17–22.
- , , , . Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations. Acad Med. 2004;79(1):78–82.
- , , , , . Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279(19):1560–1565.
- . Nurse/physician communication through a sensemaking lens: shifting the paradigm to improve patient safety. Med Care. 2010;48(11):941–946.
- . Nursing Against the Odds: How Health Care Cost Cutting, Media Stereotypes, and Medical Hubris Undermine Nurses and Patient Care. Ithaca, NY: Cornell University Press; 2005.
- . Focus on research methods: whatever happened to qualitative description? Res Nurs Health. 2000;23:334–340.
- , , , , . Organizational assessment in intensive care units (ICUs): construct development, reliability, and validity of the ICU nurse‐physician questionnaire. Med Care. 1991;29(8):709–726.
- . Development of an instrument to measure collaboration and satisfaction about care decisions. J Adv Nurs. 1994;20(1):176–182.
- . Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–188.
- , , . Does the structure of inpatient rounds affect medical student education? Int J Med Educ. 2013;4:96–100.
- U.S. Department of Veterans Affairs, Office of Academic Affiliations. Medical and Dental Education Program. Available at: http://www.va. gov/oaa/GME_default.asp. Published 2012. Accessed May 08, 2013.
- , . Graduate medical education, 2011–2012. JAMA. 2012;308(21):2264–2279.
- , , , et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(11):866–874.
- , , , , , . Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859–865.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- , , . ‘It depends': medical residents' perspectives on working with nurses. Am J Nurs. 2009;109(7):34–44.
- , . Organizational silence: a barrier to change and development in a pluralistic world. Acad Manage Rev. 2000;25(4):706–725.
- , . Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organiz Behav. 2006;27:941–966.
- , , , , . Interprofessional communication with hospitalist and consultant physicians in general internal medicine: a qualitative study. BMC Health Serv Res. 2012;12:437.
- , , , , , . A new tool to give hospitalists feedback to improve interprofessional teamwork and advance patient care. Health Aff (Millwood). 2012;31(11):2485–2492.
- , , , , , . Impact of instructional practices on student satisfaction with attendings' teaching in the inpatient component of internal medicine clerkships. J Gen Intern Med. 2006;21(1):7–12.
- , . Medical students' perceptions of the elements of effective inpatient teaching by attending physicians and housestaff. J Gen Intern Med. 2005;20(7):635–639.
- National Board of Medical Examiners Subject Examination Program. Internal Medicine Advanced Clinical Examination, score interpretation guide. Available at: http://www.nbme.org/PDF/SampleScoreReports/Internal_Medicine_ACE_Score_Report.pdf. Published 2011. Accessed September 13, 2013.
- . The impact of hospitalists on medical education and the academic health system. Ann Intern Med. 1999;130(4 part 2):364–367.
Improving quality while reducing costs remains important for hospitals across the United States, including the approximately 150 hospitals that are part of the Veterans Affairs (VA) healthcare system.[1, 2] The field of hospital medicine has grown rapidly, leading to predictions that the majority of inpatient care in the United States eventually will be delivered by hospitalists.[3, 4] In 2010, 57% of US hospitals had hospitalists on staff, including 87% of hospitals with 200 beds,[5] and nearly 80% of VA hospitals.[6]
The demand for hospitalists within teaching hospitals has grown in part as a response to the mandate to reduce residency work hours.[7] Furthermore, previous research has found that hospitalist care is associated with modest reductions in length of stay (LOS) and weak but inconsistent differences in quality.[8] The educational effect of hospitalists has been far less examined. The limited number of studies published to date suggests that hospitalists may improve resident learning and house‐officer satisfaction in academic medical centers and community teaching hospitals[9, 10, 11] and provide positive experiences for medical students12,13; however, Wachter et al reported no significant changes in clinical outcomes or patient, faculty, and house‐staff satisfaction in a newly designed hospital medicine service in San Francisco.[14] Additionally, whether using hospitalists influences nurse‐physician communication[15] is unknown.
Recognizing the limited and sometimes conflicting evidence about the hospitalist model, we report the results of a 3‐year quasi‐experimental evaluation of the experience at our medical center with academic hospitalists. As part of a VA Systems Redesign Improvement Capability Grantknown as the Hospital Outcomes Program of Excellence (HOPE) Initiativewe created a hospitalist‐based medicine team focused on quality improvement, medical education, and patient outcomes.
METHODS
Setting and Design
The main hospital of the VA Ann Arbor Healthcare System, located in Ann Arbor, Michigan, operates 105 acute‐care beds and 40 extended‐care beds. At the time of this evaluation, the medicine service consisted of 4 internal medicine teamsGold, Silver, Burgundy, and Yelloweach of which was responsible for admitting patients on a rotating basis every fourth day, with limited numbers of admissions occurring between each team's primary admitting day. Each team is led by an attending physician, a board‐certified (or board‐eligible) general internist or subspecialist who is also a faculty member at the University of Michigan Medical School. Each team has a senior medical resident, 2 to 3 interns, and 3 to 5 medical students (mostly third‐year students). In total, there are approximately 50 senior medical residents, 60 interns, and 170 medical students who rotate through the medicine service each year. Traditional rounding involves the medical students and interns receiving sign‐out from the overnight team in the morning, then pre‐rounding on each patient by obtaining an interval history, performing an exam, and checking any test results. A tentative plan of care is formed with the senior medical resident, usually by discussing each patient very quickly in the team room. Attending rounds are then conducted, with the physician team visiting each patient one by one to review and plan all aspects of care in detail. When time allows, small segments of teaching may occur during these attending work rounds. This system had been in place for >20 years.
Resulting in part from a grant received from the VA Systems Redesign Central Office (ie, the HOPE Initiative), the Gold team was modified in July 2009 and an academic hospitalist (S.S.) was assigned to head this team. Specific hospitalists were selected by the Associate Chief of Medicine (S.S.) and the Chief of Medicine (R.H.M.) to serve as Gold team attendings on a regular basis. The other teams continued to be overseen by the Chief of Medicine, and the Gold team remained within the medicine service. Characteristics of the Gold and nonGold team attendings can be found in Table 1. The 3 other teams initially were noninterventional concurrent control groups. However, during the second year of the evaluation, the Silver team adopted some of the initiatives as a result of the preliminary findings observed on Gold. Specifically, in the second year of the evaluation, approximately 42% of attendings on the Silver team were from the Gold team. This increased in the third year to 67% of coverage by Gold team attendings on the Silver team. The evaluation of the Gold team ended in June 2012.
| Characteristic | Gold Team | Non‐Gold Teams |
|---|---|---|
| Total number of attendings | 14 | 57 |
| Sex, % | ||
| Male | 79 | 58 |
| Female | 21 | 42 |
| Median years postresidency (range) | 10 (130) | 7 (141) |
| Subspecialists, % | 14 | 40 |
| Median days on service per year (range) | 53 (574) | 30 (592) |
The clinical interventions implemented on the Gold team were quality‐improvement work and were therefore exempt from institutional review board review. Human subjects' approval was, however, received to conduct interviews as part of a qualitative assessment.
Clinical Interventions
Several interventions involving the clinical care delivered were introduced on the Gold team, with a focus on improving communication among healthcare workers (Table 2).
| Clinical Interventions | Educational Interventions |
|---|---|
| Modified structure of attending rounds | Modified structure of attending rounds |
| Circle of Concern rounds | Attending reading list |
| Clinical Care Coordinator | Nifty Fifty reading list for learners |
| Regular attending team meetings | Website to provide expectations to learners |
| Two‐month per year commitment by attendings |
Structure of Attending Rounds
The structure of morning rounds was modified on the Gold team. Similar to the traditional structure, medical students and interns on the Gold team receive sign‐out from the overnight team in the morning. However, interns and students may or may not conduct pre‐rounds on each patient. The majority of time between sign‐out and the arrival of the attending physician is spent on work rounds. The senior resident leads rounds with the interns and students, discussing each patient while focusing on overnight events and current symptoms, new physical‐examination findings, and laboratory and test data. The plan of care to be presented to the attending is then formulated with the senior resident. The attending physician then leads Circle of Concern rounds with an expanded team, including a charge nurse, a clinical pharmacist, and a nurse Clinical Care Coordinator. Attending rounds tend to use an E‐AP format: significant Events overnight are discussed, followed by an Assessment & Plan by problem for the top active problems. Using this model, the attendings are able to focus more on teaching and discussing the patient plan than in the traditional model (in which the learner presents the details of the subjective, objective, laboratory, and radiographic data, with limited time left for the assessment and plan for each problem).
Circle of Concern Rounds
Suzanne Gordon described the Circle of Concern in her book Nursing Against the Odds.[16] From her observations, she noted that physicians typically form a circle to discuss patient care during rounds. The circle expands when another physician joins the group; however, the circle does not similarly expand to include nurses when they approach the group. Instead, nurses typically remain on the periphery, listening silently or trying to communicate to physicians' backs.[16] Thus, to promote nurse‐physician communication, Circle of Concern rounds were formally introduced on the Gold team. Each morning, the charge nurse rounds with the team and is encouraged to bring up nursing concerns. The inpatient clinical pharmacist is also included 2 to 3 times per week to help provide education to residents and students and perform medication reconciliation.
Clinical Care Coordinator
The role of the nurse Clinical Care Coordinatoralso introduced on the Gold teamis to provide continuity of patient care, facilitate interdisciplinary communication, facilitate patient discharge, ensure appropriate appointments are scheduled, communicate with the ambulatory care service to ensure proper transition between inpatient and outpatient care, and help educate residents and students on VA procedures and resources.
Regular Gold Team Meetings
All Gold team attendings are expected to dedicate 2 months per year to inpatient service (divided into half‐month blocks), instead of the average 1 month per year for attendings on the other teams. The Gold team attendings, unlike the other teams, also attend bimonthly meetings to discuss strategies for running the team.
Educational Interventions
Given the high number of learners on the medicine service, we wanted to enhance the educational experience for our learners. We thus implemented various interventions, in addition to the change in the structure of rounds, as described below.
Reading List for Learners: The Nifty Fifty
Because reading about clinical medicine is an integral part of medical education, we make explicit our expectation that residents and students read something clinically relevant every day. To promote this, we have provided a Nifty Fifty reading list of key articles. The PDF of each article is provided, along with a brief summary highlighting key points.
Reading List for Gold Attendings and Support Staff
To promote a common understanding of leadership techniques, management books are provided to Gold attending physicians and other members of the team (eg, Care Coordinator, nurse researcher, systems redesign engineer). One book is discussed at each Gold team meeting (Table 3), with participants taking turns leading the discussion.
| Book Title | Author(s) |
|---|---|
| The One Minute Manager | Ken Blanchard and Spencer Johnson |
| Good to Great | Jim Collins |
| Good to Great and the Social Sectors | Jim Collins |
| The Checklist Manifesto: How to Get Things Right | Atul Gawande |
| The Five Dysfunctions of a Team: A Leadership Fable | Patrick Lencioni |
| Getting to Yes: Negotiating Agreement Without Giving In | Roger Fisher, William Ury, and Bruce Patton |
| The Effective Executive: The Definitive Guide to Getting the Right Things Done | Peter Drucker |
| A Sense of Urgency | John Kotter |
| The Power of Positive Deviance: How Unlikely Innovators Solve the World's Toughest Problems | Richard Pascale, Jerry Sternin, and Monique Sternin |
| On the Mend: Revolutionizing Healthcare to Save Lives and Transform the Industry | John Toussaint and Roger Gerard |
| Outliers: The Story of Success | Malcolm Gladwell |
| Nursing Against the Odds: How Health Care Cost Cutting, Media Stereotypes, and Medical Hubris Undermine Nurses and Patient Care | Suzanne Gordon |
| How the Mighty Fall and Why Some Companies Never Give In | Jim Collins |
| What the Best College Teachers Do | Ken Bain |
| The Creative Destruction of Medicine | Eric Topol |
| What Got You Here Won't Get You There: How Successful People Become Even More Successful! | Marshall Goldsmith |
Website
A HOPE Initiative website was created (
Qualitative Assessment
To evaluate our efforts, we conducted a thorough qualitative assessment during the third year of the program. A total of 35 semistructured qualitative interviews were conducted with patients and staff from all levels of the organization, including senior leadership. The qualitative assessment was led by research staff from the Center for Clinical Management Research, who were minimally involved in the redesign effort and could provide an unbiased view of the initiative. Field notes from the semistructured interviews were analyzed, with themes developed using a descriptive approach and through discussion by a multidisciplinary team, which included building team consensus on findings that were supported by clear evidence in the data.[17]
Quantitative Outcome Measures
Clinical Outcomes
To determine if our communication and educational interventions had an impact on patient care, we used hospital administrative data to evaluate admission rates, LOS, and readmission rates for all 4 of the medicine teams. Additional clinical measures were assessed as needed. For example, we monitored the impact of the clinical pharmacist during a 4‐week pilot study by asking the Clinical Care Coordinator to track the proportion of patient encounters (n=170) in which the clinical pharmacist changed management or provided education to team members. Additionally, 2 staff surveys were conducted. The first survey focused on healthcare‐worker communication and was given to inpatient nurses and physicians (including attendings, residents, and medical students) who were recently on an inpatient medical service rotation. The survey included questions from previously validated communication measures,[18, 19, 20] as well as study‐specific questions. The second survey evaluated the new role of the Clinical Care Coordinator (Appendix). Both physicians and nurses who interacted with the Gold team's Clinical Care Coordinator were asked to complete this survey.
Educational Outcomes
To assess the educational interventions, we used learner evaluations of attendings, by both residents and medical students, and standardized internal medicine National Board of Medical Examiners Subject Examination (or shelf) scores for third‐year medical students. A separate evaluation of medical student perceptions of the rounding structure introduced on the Gold team using survey design has already been published.[21]
Statistical Analyses
Data from all sources were analyzed using SAS 9.3 (SAS Institute, Inc., Cary, NC). Outliers for the LOS variable were removed from the analysis. Means and frequency distributions were examined for all variables. Student t tests and [2] tests of independence were used to compare data between groups. Multivariable linear regression models controlling for time (preintervention vs postintervention) were used to assess the effect of the HOPE Initiative on patient LOS and readmission rates. In all cases, 2‐tailed P values of 0.05 or less were considered statistically significant.
Role of the Funding Source
The VA Office of Systems Redesign provided funding but was not involved in the design or conduct of the study, data analysis, or preparation of the manuscript.
RESULTS
Clinical Outcomes
Patient Outcomes
Our multivariable linear regression analysis, controlling for time, showed a significant reduction in LOS of approximately 0.3 days on all teams after the HOPE Initiative began (P=0.004). There were no significant differences between the Gold and non‐Gold teams in the multivariate models when controlling for time for any of the patient‐outcome measures. The number of admissions increased for all 4 medical teams (Figure 1), but, as shown in Figures 2 and 3, the readmission rates for all teams remained relatively stable over this same period of time.


Clinical Pharmacist on Gold Team Rounds
The inpatient clinical pharmacist changed the management plan for 22% of the patients seen on rounds. Contributions from the clinical pharmacist included adjusting the dosing of ordered medication and correcting medication reconciliation. Education and pharmaceutical information was provided to the team in another 6% of the 170 consecutive patient encounters evaluated.
Perception of Circle of Concern Rounds
Circle of Concern rounds were generally well‐received by both nurses and physicians. In a healthcare‐worker communication survey, completed by 38 physicians (62% response rate) and 48 nurses (54% response rate), the majority of both physicians (83%) and nurses (68%) felt Circle of Concern rounds improved communication.
Nurse Perception of Communication
The healthcare‐worker communication survey asked inpatient nurses to rate communication between nurses and physicians on each of the 4 medicine teams. Significantly more nurses were satisfied with communication with the Gold team (71%) compared with the other 3 medicine teams (53%; P=0.02) (Figure 4).
Perception of the Clinical Care Coordinator
In total, 20 physicians (87% response rate) and 10 nurses (56% response rate) completed the Clinical Care Coordinator survey. The physician results were overwhelmingly positive: 100% were satisfied or very satisfied with the role; 100% felt each team should have a Clinical Care Coordinator; and 100% agreed or strongly agreed that the Clinical Care Coordinator ensures that appropriate follow‐up is arranged, provides continuity of care, assists with interdisciplinary communication, and helps facilitate discharge. The majority of nurses was also satisfied or very satisfied with the Clinical Care Coordinator role and felt each team should have one.
Educational Outcomes
House Officer Evaluation of Attendings
Monthly evaluations of attending physicians by house officers (Figure 5) revealed that prior to the HOPE Initiative, little differences were observed between teams, as would be expected because attending assignment was largely random. After the intervention date of July 2009, however, significant differences were noted, with Gold team attendings receiving significantly higher teaching evaluations immediately after the introduction of the HOPE Initiative. Although ratings for Gold attendings remained more favorable, the difference was no longer statistically significant in the second and third year of the initiative, likely due to Gold attendings serving on other medicine teams, which contributed to an improvement in ratings of all attendings.
Medical Student Evaluation of Attendings
Monthly evaluations of attending physicians by third‐year medical students (Figure 6) revealed differences between the Gold attendings and all others, with the attendings that joined the Gold team in 2009 receiving higher teaching evaluations even before the HOPE Initiative started. However, this difference remained statistically significant in years 2 and 3 postinitiative, despite the addition of 4 new junior attendings.
Medical Student Medicine Shelf Scores
The national average on the shelf exam, which reflects learning after the internal medicine third‐year clerkship, has ranged from 75 to 78 for the past several years, with University of Michigan students averaging significantly higher scores prior to and after the HOPE Initiative. However, following the HOPE Initiative, third‐year medical students on the Gold team scored significantly higher on the shelf exam compared with their colleagues on the non‐Gold teams (84 vs 82; P=0.006). This difference in the shelf exam scores, although small, is statistically significant. It represents a measurable improvement in shelf scores in our system and demonstrates the potential educational benefit for the students. Over this same time period, scores on the United States Medical Licensing Exam, given to medical students at the beginning of their third year, remained stable (233 preHOPE Initiative; 234 postHOPE Initiative).
Qualitative Assessment
Qualitative data collected as part of our evaluation of the HOPE Initiative also suggested that nurse‐physician communication had improved since the start of the project. In particular, they reported positively on the Gold team in general, the Circle of Concern rounds, and the Clinical Care Coordinator (Table 4).
| Staff Type | Statement1 |
|---|---|
| |
| Nurse | [Gold is] above and beyond other [teams]. Other teams don't run as smoothly. |
| Nurse | There has been a difference in communication [on Gold]. You can tell the difference in how they communicate with staff. We know the Clinical Care Coordinator or charge nurse is rounding with that team, so there is more communication. |
| Nurse | The most important thing that has improved communication is the Circle of Concern rounds. |
| Physician | [The Gold Clinical Care Coordinator] expedites care, not only what to do but who to call. She can convey the urgency. On rounds she is able to break off, put in an order, place a call, talk to a patient. Things that we would do at 11 AM she gets to at 9 AM. A couple of hours may not seem like much, but sometimes it can make the difference between things happening that day instead of the next. |
| Physician | The Clinical Care Coordinator is completely indispensable. Major benefit to providing care to Veterans. |
| Physician | I like to think Gold has lifted all of the teams to a higher level. |
| Medical student | It may be due to personalities vs the Gold [team] itself, but there is more emphasis on best practices. Are we following guidelines even if it is not related to the primary reason for admission? |
| Medical student | Gold is very collegial and nurses/physicians know one another by name. Physicians request rather than order; this sets a good example to me on how to approach the nurses. |
| Chief resident | [Gold attendings] encourage senior residents to take charge and run the team, although the attending is there for back‐up and support. This provides great learning for the residents. Interns and medical students also are affected because they have to step up their game as well. |
DISCUSSION
Within academic medical centers, hospitalists are expected to care for patients, teach, and help improve the quality and efficiency of hospital‐based care.[7] The Department of Veterans Affairs runs the largest integrated healthcare system in the United States, with approximately 80% of VA hospitals having hospital medicine programs. Overall, one‐third of US residents perform part of their residency training at a VA hospital.[22, 23] Thus, the effects of a system‐wide change at a VA hospital may have implications throughout the country. We studied one such intervention. Our primary findings are that we were able to improve communication and learner education with minimal effects on patient outcomes. While overall LOS decreased slightly postintervention, after taking into account secular trends, readmission rates did not.
We are not the first to evaluate a hospital medicine team using a quasi‐experimental design. For example, Meltzer and colleagues evaluated a hospitalist program at the University of Chicago Medical Center and found that, by the second year of operation, hospitalist care was associated with significantly shorter LOS (0.49 days), reduced costs, and decreased mortality.[24] Auerbach also evaluated a newly created hospital medicine service, finding decreased LOS (0.61 days), lower costs, and lower risk of mortality by the second year of the program.[25]
Improving nurse‐physician communication is considered important for avoiding medical error,[26] yet there has been limited empirical study of methods to improve communication within the medical profession.[27] Based both on our surveys and qualitative interviews, healthcare‐worker communication appeared to improve on the Gold team during the study. A key component of this improvement is likely related to instituting Circle of Concern rounds, in which nurses joined the medical team during attending rounds. Such an intervention likely helped to address organizational silence[28] and enhance the psychological safety of the nursing staff, because the attending physician was proactive about soliciting the input of nurses during rounds.[29] Such leader inclusivenesswords and deeds exhibited by leaders that invite and appreciate others' contributionscan aid interdisciplinary teams in overcoming the negative effects of status differences, thereby promoting collaboration.[29] The inclusion of nurses on rounds is also relationship‐building, which Gotlib Conn and colleagues found was important to improved interprofessional communication and collaboration.[30] In the future, using a tool such as the Teamwork Effectiveness Assessment Module (TEAM) developed by the American Board of Internal Medicine[31] could provide further evaluation of the impact on interprofessional teamwork and communication.
The focus on learner education, though evaluated in prior studies, is also novel. One previous survey of medical students showed that engaging students in substantive discussions is associated with greater student satisfaction.[32] Another survey of medical students found that attendings who were enthusiastic about teaching, inspired confidence in knowledge and skills, provided useful feedback, and encouraged increased student responsibility were viewed as more effective teachers.[33] No previous study that we are aware of, however, has looked at actual educational outcomes, such as shelf scores. The National Board of Medical Examiners reports that the Medicine subject exam is scaled to have a mean of 70 and a standard deviation of 8.[34] Thus, a mean increase in score of 2 points is small, but not trivial. This shows improvement in a hard educational outcome. Additionally, 2 points, although small in the context of total score and standard deviation, may make a substantial difference to an individual student in terms of overall grade, and, thus, residency applications. Our finding that third‐year medical students on the Gold team performed significantly better than University of Michigan third‐year medical students on other teams is an intriguing finding that warrants confirmation. On the other hand, this finding is consistent with a previous report evaluating learner satisfaction in which Bodnar et al found improved ratings of quantity and quality of teaching on teams with a nontraditional structure (Gold team).[21] Moreover, despite relatively few studies, the reason underlying the educational benefit of hospitalists should surprise few. The hospitalist model ensures that learners are supervised by physicians who are experts in the care of hospitalized patients.[35] Hospitalists hired at teaching hospitals to work on services with learners are generally chosen because they possess superior educational skills.[7]
Our findings should be interpreted in the context of the following limitations. First, our study focused on a single academically affiliated VA hospital. As other VA hospitals are pursuing a similar approach (eg, the Houston and Detroit VA medical centers), replicating our results will be important. Second, the VA system, although the largest integrated healthcare system in the United States, has unique characteristicssuch as an integrated electronic health record and predominantly male patient populationthat may make generalizations to the larger US healthcare system challenging. Third, there was a slightly lower response rate among nurses on a few of the surveys to evaluate our efforts; however, this rate of response is standard at our facility. Finally, our evaluation lacks an empirical measure of healthcare‐worker communication, such as incident reports.
Despite these limitations, our results have important implications. Using both quantitative and qualitative assessment, we found that academic hospitalists have the ability to improve healthcare‐worker communication and enhance learner education without increasing LOS. These findings are directly applicable to VA medical centers and potentially applicable to other academic medical centers.
Acknowledgments
The authors thank Milisa Manojlovich, PhD, RN, Edward Kennedy, MS, and Andrew Hickner, MSI, for help with preparation of this manuscript.
Disclosures: This work was funded by a US Department of Veterans Affairs, Office of Systems Redesign Improvement Capability grant. The findings and conclusions in this report are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs. Dr. Saint reports receiving travel reimbursement for giving invited talks at the Society of Hospital Medicine's National Meeting, as well as serving on the advisory boards of Doximity and Jvion.
APPENDIX
Survey to Evaluate the Care Coordinator Position
| Yes | No | Not Sure | |
| Q1. Are you familiar with the role of the Care Coordinator on the Gold Service (Susan Lee)? | 1 | 2 | 3 |
Please indicate how much you agree or disagree with the statements below.
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | Don't Know | |
| Q2. The Care Coordinator ensures that appropriate primary care follow‐up and any other appropriate services are arranged. | 1 | 2 | 3 | 4 | 5 | 9 |
| Q3. The Care Coordinator provides continuity of patient care on the Gold Service. | 1 | 2 | 3 | 4 | 5 | 9 |
| Q4. The Care Coordinator helps educate House Officers and Medical Students on VA processes (e.g., CPRS). | 1 | 2 | 3 | 4 | 5 | 9 |
| Q5. The Care Coordinator assists with interdisciplinary communication between the medical team and other services (e.g., nursing, ambulatory care, pharmacy, social work) | 1 | 2 | 3 | 4 | 5 | 9 |
| Q6. The Care Coordinator helps facilitate patient discharge. | 1 | 2 | 3 | 4 | 5 | 9 |
| Q7. The Care Coordinator initiates communication with the ambulatory care teams to coordinate care. | 1 | 2 | 3 | 4 | 5 | 9 |
| Yes | No | |
| Q8. Are you a physician (attending or resident), or medical student who has been on more than one medical team at the VA (Gold, Silver, Burgundy, or Yellow)? | 1 | 2 |
If no, please skip to Q13
If yes, comparing your experience on the Gold Service (with the Care Coordinator) to your experience on any of the other services (Silver, Burgundy, or Yellow):
| Not at All | Very Little | Somewhat | To a Great Extent | |
| Q9. To what extent does the presence of a Care Coordinator affect patient care? | 1 | 2 | 3 | 4 |
| Q10. To what extent does the presence of a Care Coordinator improve patient flow? | 1 | 2 | 3 | 4 |
| Q11. To what extent does the presence of a Care Coordinator assist with education? | 1 | 2 | 3 | 4 |
| Q12. To what extent does the presence of a Care Coordinator contribute to attending rounds? | 1 | 2 | 3 | 4 |
| Yes | No | |
| Q13. Do you work [as a nurse] in ambulatory care? | 1 | 2 |
If no, please skip to Q17.
If yes, comparing your experience with the Gold Service (with the Care Coordinator) to the other services (Silver, Burgundy, or Yellow):
| Not at All | Very Little | Somewhat | To a Great Extent | |
| Q14. To what extent does the presence of a Care Coordinator improve coordination of care between inpatient and outpatient services? | 1 | 2 | 3 | 4 |
| Q15. To what extent does the presence of a Care Coordinator help identify high risk patients who require follow‐up? | 1 | 2 | 3 | 4 |
| Q16. To what extent does the presence of a Care Coordinator ensure follow‐up appointments are scheduled? | 1 | 2 | 3 | 4 |
| Yes | No | Not Sure | |
| Q17. Do you think each medical team should have a Care Coordinator? | 1 | 2 | 3 |
| Q18. Are there any additional tasks or duties you think would improve the effectiveness of the Care Coordinator? |
| Very Satisfied | Satisfied | Neutral | Dissatisfied | Very Dissatisfied | |
| Q19. Overall how satisfied are you with the role of the Care Coordinator on the Gold Service? | 1 | 2 | 3 | 4 | 5 |
| Q20. Do you have any other comments about the role of the Care Coordinator? |
| Q21. What is your position? |
| 1. Physician (attending or resident) or medical student |
| 2. Nurse (inpatient or ambulatory care) |
Improving quality while reducing costs remains important for hospitals across the United States, including the approximately 150 hospitals that are part of the Veterans Affairs (VA) healthcare system.[1, 2] The field of hospital medicine has grown rapidly, leading to predictions that the majority of inpatient care in the United States eventually will be delivered by hospitalists.[3, 4] In 2010, 57% of US hospitals had hospitalists on staff, including 87% of hospitals with 200 beds,[5] and nearly 80% of VA hospitals.[6]
The demand for hospitalists within teaching hospitals has grown in part as a response to the mandate to reduce residency work hours.[7] Furthermore, previous research has found that hospitalist care is associated with modest reductions in length of stay (LOS) and weak but inconsistent differences in quality.[8] The educational effect of hospitalists has been far less examined. The limited number of studies published to date suggests that hospitalists may improve resident learning and house‐officer satisfaction in academic medical centers and community teaching hospitals[9, 10, 11] and provide positive experiences for medical students12,13; however, Wachter et al reported no significant changes in clinical outcomes or patient, faculty, and house‐staff satisfaction in a newly designed hospital medicine service in San Francisco.[14] Additionally, whether using hospitalists influences nurse‐physician communication[15] is unknown.
Recognizing the limited and sometimes conflicting evidence about the hospitalist model, we report the results of a 3‐year quasi‐experimental evaluation of the experience at our medical center with academic hospitalists. As part of a VA Systems Redesign Improvement Capability Grantknown as the Hospital Outcomes Program of Excellence (HOPE) Initiativewe created a hospitalist‐based medicine team focused on quality improvement, medical education, and patient outcomes.
METHODS
Setting and Design
The main hospital of the VA Ann Arbor Healthcare System, located in Ann Arbor, Michigan, operates 105 acute‐care beds and 40 extended‐care beds. At the time of this evaluation, the medicine service consisted of 4 internal medicine teamsGold, Silver, Burgundy, and Yelloweach of which was responsible for admitting patients on a rotating basis every fourth day, with limited numbers of admissions occurring between each team's primary admitting day. Each team is led by an attending physician, a board‐certified (or board‐eligible) general internist or subspecialist who is also a faculty member at the University of Michigan Medical School. Each team has a senior medical resident, 2 to 3 interns, and 3 to 5 medical students (mostly third‐year students). In total, there are approximately 50 senior medical residents, 60 interns, and 170 medical students who rotate through the medicine service each year. Traditional rounding involves the medical students and interns receiving sign‐out from the overnight team in the morning, then pre‐rounding on each patient by obtaining an interval history, performing an exam, and checking any test results. A tentative plan of care is formed with the senior medical resident, usually by discussing each patient very quickly in the team room. Attending rounds are then conducted, with the physician team visiting each patient one by one to review and plan all aspects of care in detail. When time allows, small segments of teaching may occur during these attending work rounds. This system had been in place for >20 years.
Resulting in part from a grant received from the VA Systems Redesign Central Office (ie, the HOPE Initiative), the Gold team was modified in July 2009 and an academic hospitalist (S.S.) was assigned to head this team. Specific hospitalists were selected by the Associate Chief of Medicine (S.S.) and the Chief of Medicine (R.H.M.) to serve as Gold team attendings on a regular basis. The other teams continued to be overseen by the Chief of Medicine, and the Gold team remained within the medicine service. Characteristics of the Gold and nonGold team attendings can be found in Table 1. The 3 other teams initially were noninterventional concurrent control groups. However, during the second year of the evaluation, the Silver team adopted some of the initiatives as a result of the preliminary findings observed on Gold. Specifically, in the second year of the evaluation, approximately 42% of attendings on the Silver team were from the Gold team. This increased in the third year to 67% of coverage by Gold team attendings on the Silver team. The evaluation of the Gold team ended in June 2012.
| Characteristic | Gold Team | Non‐Gold Teams |
|---|---|---|
| Total number of attendings | 14 | 57 |
| Sex, % | ||
| Male | 79 | 58 |
| Female | 21 | 42 |
| Median years postresidency (range) | 10 (130) | 7 (141) |
| Subspecialists, % | 14 | 40 |
| Median days on service per year (range) | 53 (574) | 30 (592) |
The clinical interventions implemented on the Gold team were quality‐improvement work and were therefore exempt from institutional review board review. Human subjects' approval was, however, received to conduct interviews as part of a qualitative assessment.
Clinical Interventions
Several interventions involving the clinical care delivered were introduced on the Gold team, with a focus on improving communication among healthcare workers (Table 2).
| Clinical Interventions | Educational Interventions |
|---|---|
| Modified structure of attending rounds | Modified structure of attending rounds |
| Circle of Concern rounds | Attending reading list |
| Clinical Care Coordinator | Nifty Fifty reading list for learners |
| Regular attending team meetings | Website to provide expectations to learners |
| Two‐month per year commitment by attendings |
Structure of Attending Rounds
The structure of morning rounds was modified on the Gold team. Similar to the traditional structure, medical students and interns on the Gold team receive sign‐out from the overnight team in the morning. However, interns and students may or may not conduct pre‐rounds on each patient. The majority of time between sign‐out and the arrival of the attending physician is spent on work rounds. The senior resident leads rounds with the interns and students, discussing each patient while focusing on overnight events and current symptoms, new physical‐examination findings, and laboratory and test data. The plan of care to be presented to the attending is then formulated with the senior resident. The attending physician then leads Circle of Concern rounds with an expanded team, including a charge nurse, a clinical pharmacist, and a nurse Clinical Care Coordinator. Attending rounds tend to use an E‐AP format: significant Events overnight are discussed, followed by an Assessment & Plan by problem for the top active problems. Using this model, the attendings are able to focus more on teaching and discussing the patient plan than in the traditional model (in which the learner presents the details of the subjective, objective, laboratory, and radiographic data, with limited time left for the assessment and plan for each problem).
Circle of Concern Rounds
Suzanne Gordon described the Circle of Concern in her book Nursing Against the Odds.[16] From her observations, she noted that physicians typically form a circle to discuss patient care during rounds. The circle expands when another physician joins the group; however, the circle does not similarly expand to include nurses when they approach the group. Instead, nurses typically remain on the periphery, listening silently or trying to communicate to physicians' backs.[16] Thus, to promote nurse‐physician communication, Circle of Concern rounds were formally introduced on the Gold team. Each morning, the charge nurse rounds with the team and is encouraged to bring up nursing concerns. The inpatient clinical pharmacist is also included 2 to 3 times per week to help provide education to residents and students and perform medication reconciliation.
Clinical Care Coordinator
The role of the nurse Clinical Care Coordinatoralso introduced on the Gold teamis to provide continuity of patient care, facilitate interdisciplinary communication, facilitate patient discharge, ensure appropriate appointments are scheduled, communicate with the ambulatory care service to ensure proper transition between inpatient and outpatient care, and help educate residents and students on VA procedures and resources.
Regular Gold Team Meetings
All Gold team attendings are expected to dedicate 2 months per year to inpatient service (divided into half‐month blocks), instead of the average 1 month per year for attendings on the other teams. The Gold team attendings, unlike the other teams, also attend bimonthly meetings to discuss strategies for running the team.
Educational Interventions
Given the high number of learners on the medicine service, we wanted to enhance the educational experience for our learners. We thus implemented various interventions, in addition to the change in the structure of rounds, as described below.
Reading List for Learners: The Nifty Fifty
Because reading about clinical medicine is an integral part of medical education, we make explicit our expectation that residents and students read something clinically relevant every day. To promote this, we have provided a Nifty Fifty reading list of key articles. The PDF of each article is provided, along with a brief summary highlighting key points.
Reading List for Gold Attendings and Support Staff
To promote a common understanding of leadership techniques, management books are provided to Gold attending physicians and other members of the team (eg, Care Coordinator, nurse researcher, systems redesign engineer). One book is discussed at each Gold team meeting (Table 3), with participants taking turns leading the discussion.
| Book Title | Author(s) |
|---|---|
| The One Minute Manager | Ken Blanchard and Spencer Johnson |
| Good to Great | Jim Collins |
| Good to Great and the Social Sectors | Jim Collins |
| The Checklist Manifesto: How to Get Things Right | Atul Gawande |
| The Five Dysfunctions of a Team: A Leadership Fable | Patrick Lencioni |
| Getting to Yes: Negotiating Agreement Without Giving In | Roger Fisher, William Ury, and Bruce Patton |
| The Effective Executive: The Definitive Guide to Getting the Right Things Done | Peter Drucker |
| A Sense of Urgency | John Kotter |
| The Power of Positive Deviance: How Unlikely Innovators Solve the World's Toughest Problems | Richard Pascale, Jerry Sternin, and Monique Sternin |
| On the Mend: Revolutionizing Healthcare to Save Lives and Transform the Industry | John Toussaint and Roger Gerard |
| Outliers: The Story of Success | Malcolm Gladwell |
| Nursing Against the Odds: How Health Care Cost Cutting, Media Stereotypes, and Medical Hubris Undermine Nurses and Patient Care | Suzanne Gordon |
| How the Mighty Fall and Why Some Companies Never Give In | Jim Collins |
| What the Best College Teachers Do | Ken Bain |
| The Creative Destruction of Medicine | Eric Topol |
| What Got You Here Won't Get You There: How Successful People Become Even More Successful! | Marshall Goldsmith |
Website
A HOPE Initiative website was created (
Qualitative Assessment
To evaluate our efforts, we conducted a thorough qualitative assessment during the third year of the program. A total of 35 semistructured qualitative interviews were conducted with patients and staff from all levels of the organization, including senior leadership. The qualitative assessment was led by research staff from the Center for Clinical Management Research, who were minimally involved in the redesign effort and could provide an unbiased view of the initiative. Field notes from the semistructured interviews were analyzed, with themes developed using a descriptive approach and through discussion by a multidisciplinary team, which included building team consensus on findings that were supported by clear evidence in the data.[17]
Quantitative Outcome Measures
Clinical Outcomes
To determine if our communication and educational interventions had an impact on patient care, we used hospital administrative data to evaluate admission rates, LOS, and readmission rates for all 4 of the medicine teams. Additional clinical measures were assessed as needed. For example, we monitored the impact of the clinical pharmacist during a 4‐week pilot study by asking the Clinical Care Coordinator to track the proportion of patient encounters (n=170) in which the clinical pharmacist changed management or provided education to team members. Additionally, 2 staff surveys were conducted. The first survey focused on healthcare‐worker communication and was given to inpatient nurses and physicians (including attendings, residents, and medical students) who were recently on an inpatient medical service rotation. The survey included questions from previously validated communication measures,[18, 19, 20] as well as study‐specific questions. The second survey evaluated the new role of the Clinical Care Coordinator (Appendix). Both physicians and nurses who interacted with the Gold team's Clinical Care Coordinator were asked to complete this survey.
Educational Outcomes
To assess the educational interventions, we used learner evaluations of attendings, by both residents and medical students, and standardized internal medicine National Board of Medical Examiners Subject Examination (or shelf) scores for third‐year medical students. A separate evaluation of medical student perceptions of the rounding structure introduced on the Gold team using survey design has already been published.[21]
Statistical Analyses
Data from all sources were analyzed using SAS 9.3 (SAS Institute, Inc., Cary, NC). Outliers for the LOS variable were removed from the analysis. Means and frequency distributions were examined for all variables. Student t tests and [2] tests of independence were used to compare data between groups. Multivariable linear regression models controlling for time (preintervention vs postintervention) were used to assess the effect of the HOPE Initiative on patient LOS and readmission rates. In all cases, 2‐tailed P values of 0.05 or less were considered statistically significant.
Role of the Funding Source
The VA Office of Systems Redesign provided funding but was not involved in the design or conduct of the study, data analysis, or preparation of the manuscript.
RESULTS
Clinical Outcomes
Patient Outcomes
Our multivariable linear regression analysis, controlling for time, showed a significant reduction in LOS of approximately 0.3 days on all teams after the HOPE Initiative began (P=0.004). There were no significant differences between the Gold and non‐Gold teams in the multivariate models when controlling for time for any of the patient‐outcome measures. The number of admissions increased for all 4 medical teams (Figure 1), but, as shown in Figures 2 and 3, the readmission rates for all teams remained relatively stable over this same period of time.

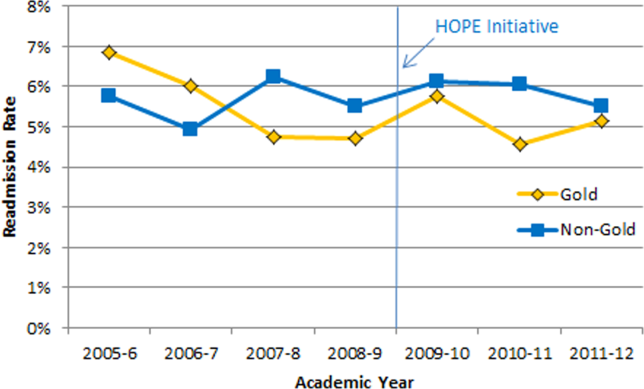

Clinical Pharmacist on Gold Team Rounds
The inpatient clinical pharmacist changed the management plan for 22% of the patients seen on rounds. Contributions from the clinical pharmacist included adjusting the dosing of ordered medication and correcting medication reconciliation. Education and pharmaceutical information was provided to the team in another 6% of the 170 consecutive patient encounters evaluated.
Perception of Circle of Concern Rounds
Circle of Concern rounds were generally well‐received by both nurses and physicians. In a healthcare‐worker communication survey, completed by 38 physicians (62% response rate) and 48 nurses (54% response rate), the majority of both physicians (83%) and nurses (68%) felt Circle of Concern rounds improved communication.
Nurse Perception of Communication
The healthcare‐worker communication survey asked inpatient nurses to rate communication between nurses and physicians on each of the 4 medicine teams. Significantly more nurses were satisfied with communication with the Gold team (71%) compared with the other 3 medicine teams (53%; P=0.02) (Figure 4).
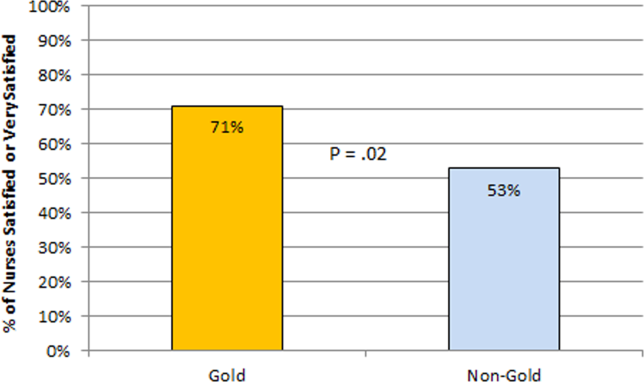
Perception of the Clinical Care Coordinator
In total, 20 physicians (87% response rate) and 10 nurses (56% response rate) completed the Clinical Care Coordinator survey. The physician results were overwhelmingly positive: 100% were satisfied or very satisfied with the role; 100% felt each team should have a Clinical Care Coordinator; and 100% agreed or strongly agreed that the Clinical Care Coordinator ensures that appropriate follow‐up is arranged, provides continuity of care, assists with interdisciplinary communication, and helps facilitate discharge. The majority of nurses was also satisfied or very satisfied with the Clinical Care Coordinator role and felt each team should have one.
Educational Outcomes
House Officer Evaluation of Attendings
Monthly evaluations of attending physicians by house officers (Figure 5) revealed that prior to the HOPE Initiative, little differences were observed between teams, as would be expected because attending assignment was largely random. After the intervention date of July 2009, however, significant differences were noted, with Gold team attendings receiving significantly higher teaching evaluations immediately after the introduction of the HOPE Initiative. Although ratings for Gold attendings remained more favorable, the difference was no longer statistically significant in the second and third year of the initiative, likely due to Gold attendings serving on other medicine teams, which contributed to an improvement in ratings of all attendings.
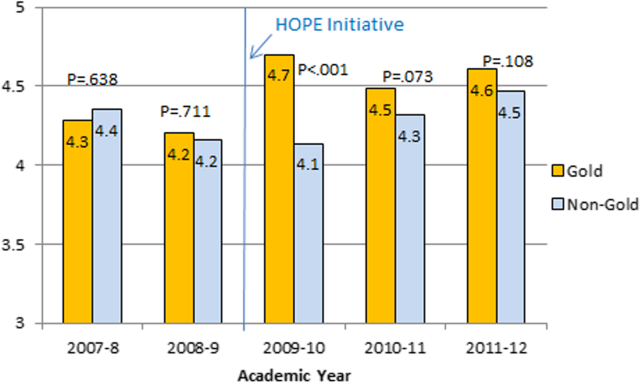
Medical Student Evaluation of Attendings
Monthly evaluations of attending physicians by third‐year medical students (Figure 6) revealed differences between the Gold attendings and all others, with the attendings that joined the Gold team in 2009 receiving higher teaching evaluations even before the HOPE Initiative started. However, this difference remained statistically significant in years 2 and 3 postinitiative, despite the addition of 4 new junior attendings.
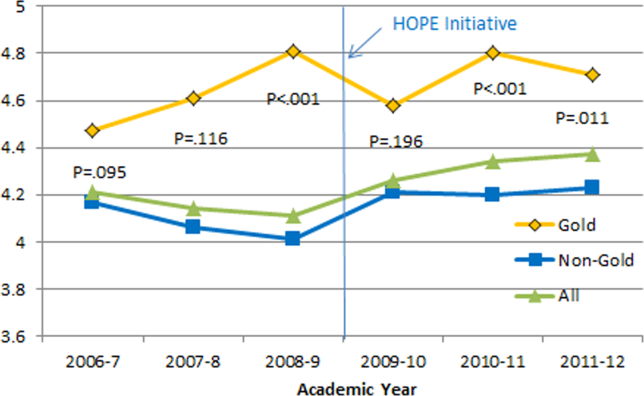
Medical Student Medicine Shelf Scores
The national average on the shelf exam, which reflects learning after the internal medicine third‐year clerkship, has ranged from 75 to 78 for the past several years, with University of Michigan students averaging significantly higher scores prior to and after the HOPE Initiative. However, following the HOPE Initiative, third‐year medical students on the Gold team scored significantly higher on the shelf exam compared with their colleagues on the non‐Gold teams (84 vs 82; P=0.006). This difference in the shelf exam scores, although small, is statistically significant. It represents a measurable improvement in shelf scores in our system and demonstrates the potential educational benefit for the students. Over this same time period, scores on the United States Medical Licensing Exam, given to medical students at the beginning of their third year, remained stable (233 preHOPE Initiative; 234 postHOPE Initiative).
Qualitative Assessment
Qualitative data collected as part of our evaluation of the HOPE Initiative also suggested that nurse‐physician communication had improved since the start of the project. In particular, they reported positively on the Gold team in general, the Circle of Concern rounds, and the Clinical Care Coordinator (Table 4).
| Staff Type | Statement1 |
|---|---|
| |
| Nurse | [Gold is] above and beyond other [teams]. Other teams don't run as smoothly. |
| Nurse | There has been a difference in communication [on Gold]. You can tell the difference in how they communicate with staff. We know the Clinical Care Coordinator or charge nurse is rounding with that team, so there is more communication. |
| Nurse | The most important thing that has improved communication is the Circle of Concern rounds. |
| Physician | [The Gold Clinical Care Coordinator] expedites care, not only what to do but who to call. She can convey the urgency. On rounds she is able to break off, put in an order, place a call, talk to a patient. Things that we would do at 11 AM she gets to at 9 AM. A couple of hours may not seem like much, but sometimes it can make the difference between things happening that day instead of the next. |
| Physician | The Clinical Care Coordinator is completely indispensable. Major benefit to providing care to Veterans. |
| Physician | I like to think Gold has lifted all of the teams to a higher level. |
| Medical student | It may be due to personalities vs the Gold [team] itself, but there is more emphasis on best practices. Are we following guidelines even if it is not related to the primary reason for admission? |
| Medical student | Gold is very collegial and nurses/physicians know one another by name. Physicians request rather than order; this sets a good example to me on how to approach the nurses. |
| Chief resident | [Gold attendings] encourage senior residents to take charge and run the team, although the attending is there for back‐up and support. This provides great learning for the residents. Interns and medical students also are affected because they have to step up their game as well. |
DISCUSSION
Within academic medical centers, hospitalists are expected to care for patients, teach, and help improve the quality and efficiency of hospital‐based care.[7] The Department of Veterans Affairs runs the largest integrated healthcare system in the United States, with approximately 80% of VA hospitals having hospital medicine programs. Overall, one‐third of US residents perform part of their residency training at a VA hospital.[22, 23] Thus, the effects of a system‐wide change at a VA hospital may have implications throughout the country. We studied one such intervention. Our primary findings are that we were able to improve communication and learner education with minimal effects on patient outcomes. While overall LOS decreased slightly postintervention, after taking into account secular trends, readmission rates did not.
We are not the first to evaluate a hospital medicine team using a quasi‐experimental design. For example, Meltzer and colleagues evaluated a hospitalist program at the University of Chicago Medical Center and found that, by the second year of operation, hospitalist care was associated with significantly shorter LOS (0.49 days), reduced costs, and decreased mortality.[24] Auerbach also evaluated a newly created hospital medicine service, finding decreased LOS (0.61 days), lower costs, and lower risk of mortality by the second year of the program.[25]
Improving nurse‐physician communication is considered important for avoiding medical error,[26] yet there has been limited empirical study of methods to improve communication within the medical profession.[27] Based both on our surveys and qualitative interviews, healthcare‐worker communication appeared to improve on the Gold team during the study. A key component of this improvement is likely related to instituting Circle of Concern rounds, in which nurses joined the medical team during attending rounds. Such an intervention likely helped to address organizational silence[28] and enhance the psychological safety of the nursing staff, because the attending physician was proactive about soliciting the input of nurses during rounds.[29] Such leader inclusivenesswords and deeds exhibited by leaders that invite and appreciate others' contributionscan aid interdisciplinary teams in overcoming the negative effects of status differences, thereby promoting collaboration.[29] The inclusion of nurses on rounds is also relationship‐building, which Gotlib Conn and colleagues found was important to improved interprofessional communication and collaboration.[30] In the future, using a tool such as the Teamwork Effectiveness Assessment Module (TEAM) developed by the American Board of Internal Medicine[31] could provide further evaluation of the impact on interprofessional teamwork and communication.
The focus on learner education, though evaluated in prior studies, is also novel. One previous survey of medical students showed that engaging students in substantive discussions is associated with greater student satisfaction.[32] Another survey of medical students found that attendings who were enthusiastic about teaching, inspired confidence in knowledge and skills, provided useful feedback, and encouraged increased student responsibility were viewed as more effective teachers.[33] No previous study that we are aware of, however, has looked at actual educational outcomes, such as shelf scores. The National Board of Medical Examiners reports that the Medicine subject exam is scaled to have a mean of 70 and a standard deviation of 8.[34] Thus, a mean increase in score of 2 points is small, but not trivial. This shows improvement in a hard educational outcome. Additionally, 2 points, although small in the context of total score and standard deviation, may make a substantial difference to an individual student in terms of overall grade, and, thus, residency applications. Our finding that third‐year medical students on the Gold team performed significantly better than University of Michigan third‐year medical students on other teams is an intriguing finding that warrants confirmation. On the other hand, this finding is consistent with a previous report evaluating learner satisfaction in which Bodnar et al found improved ratings of quantity and quality of teaching on teams with a nontraditional structure (Gold team).[21] Moreover, despite relatively few studies, the reason underlying the educational benefit of hospitalists should surprise few. The hospitalist model ensures that learners are supervised by physicians who are experts in the care of hospitalized patients.[35] Hospitalists hired at teaching hospitals to work on services with learners are generally chosen because they possess superior educational skills.[7]
Our findings should be interpreted in the context of the following limitations. First, our study focused on a single academically affiliated VA hospital. As other VA hospitals are pursuing a similar approach (eg, the Houston and Detroit VA medical centers), replicating our results will be important. Second, the VA system, although the largest integrated healthcare system in the United States, has unique characteristicssuch as an integrated electronic health record and predominantly male patient populationthat may make generalizations to the larger US healthcare system challenging. Third, there was a slightly lower response rate among nurses on a few of the surveys to evaluate our efforts; however, this rate of response is standard at our facility. Finally, our evaluation lacks an empirical measure of healthcare‐worker communication, such as incident reports.
Despite these limitations, our results have important implications. Using both quantitative and qualitative assessment, we found that academic hospitalists have the ability to improve healthcare‐worker communication and enhance learner education without increasing LOS. These findings are directly applicable to VA medical centers and potentially applicable to other academic medical centers.
Acknowledgments
The authors thank Milisa Manojlovich, PhD, RN, Edward Kennedy, MS, and Andrew Hickner, MSI, for help with preparation of this manuscript.
Disclosures: This work was funded by a US Department of Veterans Affairs, Office of Systems Redesign Improvement Capability grant. The findings and conclusions in this report are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs. Dr. Saint reports receiving travel reimbursement for giving invited talks at the Society of Hospital Medicine's National Meeting, as well as serving on the advisory boards of Doximity and Jvion.
APPENDIX
Survey to Evaluate the Care Coordinator Position
| Yes | No | Not Sure | |
| Q1. Are you familiar with the role of the Care Coordinator on the Gold Service (Susan Lee)? | 1 | 2 | 3 |
Please indicate how much you agree or disagree with the statements below.
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | Don't Know | |
| Q2. The Care Coordinator ensures that appropriate primary care follow‐up and any other appropriate services are arranged. | 1 | 2 | 3 | 4 | 5 | 9 |
| Q3. The Care Coordinator provides continuity of patient care on the Gold Service. | 1 | 2 | 3 | 4 | 5 | 9 |
| Q4. The Care Coordinator helps educate House Officers and Medical Students on VA processes (e.g., CPRS). | 1 | 2 | 3 | 4 | 5 | 9 |
| Q5. The Care Coordinator assists with interdisciplinary communication between the medical team and other services (e.g., nursing, ambulatory care, pharmacy, social work) | 1 | 2 | 3 | 4 | 5 | 9 |
| Q6. The Care Coordinator helps facilitate patient discharge. | 1 | 2 | 3 | 4 | 5 | 9 |
| Q7. The Care Coordinator initiates communication with the ambulatory care teams to coordinate care. | 1 | 2 | 3 | 4 | 5 | 9 |
| Yes | No | |
| Q8. Are you a physician (attending or resident), or medical student who has been on more than one medical team at the VA (Gold, Silver, Burgundy, or Yellow)? | 1 | 2 |
If no, please skip to Q13
If yes, comparing your experience on the Gold Service (with the Care Coordinator) to your experience on any of the other services (Silver, Burgundy, or Yellow):
| Not at All | Very Little | Somewhat | To a Great Extent | |
| Q9. To what extent does the presence of a Care Coordinator affect patient care? | 1 | 2 | 3 | 4 |
| Q10. To what extent does the presence of a Care Coordinator improve patient flow? | 1 | 2 | 3 | 4 |
| Q11. To what extent does the presence of a Care Coordinator assist with education? | 1 | 2 | 3 | 4 |
| Q12. To what extent does the presence of a Care Coordinator contribute to attending rounds? | 1 | 2 | 3 | 4 |
| Yes | No | |
| Q13. Do you work [as a nurse] in ambulatory care? | 1 | 2 |
If no, please skip to Q17.
If yes, comparing your experience with the Gold Service (with the Care Coordinator) to the other services (Silver, Burgundy, or Yellow):
| Not at All | Very Little | Somewhat | To a Great Extent | |
| Q14. To what extent does the presence of a Care Coordinator improve coordination of care between inpatient and outpatient services? | 1 | 2 | 3 | 4 |
| Q15. To what extent does the presence of a Care Coordinator help identify high risk patients who require follow‐up? | 1 | 2 | 3 | 4 |
| Q16. To what extent does the presence of a Care Coordinator ensure follow‐up appointments are scheduled? | 1 | 2 | 3 | 4 |
| Yes | No | Not Sure | |
| Q17. Do you think each medical team should have a Care Coordinator? | 1 | 2 | 3 |
| Q18. Are there any additional tasks or duties you think would improve the effectiveness of the Care Coordinator? |
| Very Satisfied | Satisfied | Neutral | Dissatisfied | Very Dissatisfied | |
| Q19. Overall how satisfied are you with the role of the Care Coordinator on the Gold Service? | 1 | 2 | 3 | 4 | 5 |
| Q20. Do you have any other comments about the role of the Care Coordinator? |
| Q21. What is your position? |
| 1. Physician (attending or resident) or medical student |
| 2. Nurse (inpatient or ambulatory care) |
- Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, D.C.: National Academies Press; 2000.
- Institute of Medicine of the National Academies. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academies Press; 2001.
- , , , . Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102–1112.
- . Growth in care provided by hospitalists. N Engl J Med. 2009;360(26):2789–2791.
- American Hospital Association. AHA Annual Survey of Hospitals, 2010. Chicago, IL: Health Forum, LLC; 2010.
- , , , . Preventing hospital‐acquired infections: a national survey of practices reported by U.S. hospitals in 2005 and 2009. J Gen Intern Med. 2012;27(7):773–779.
- , . Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;19(4):392–393.
- , . Do hospitalist physicians improve the quality of inpatient care delivery? A systematic review of process, efficiency and outcome measures. BMC Med. 2011;9:58.
- , , , . Effect of hospitalist attending physicians on trainee educational experiences: a systematic review. J Hosp Med. 2009;4(8):490–498.
- , , , , , . Resident satisfaction on an academic hospitalist service: time to teach. Am J Med. 2002;112(7):597–601.
- , , , et al. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19(4):293–301.
- , . Third‐year medical students' evaluation of hospitalist and nonhospitalist faculty during the inpatient portion of their pediatrics clerkships. J Hosp Med. 2007;2(1):17–22.
- , , , . Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations. Acad Med. 2004;79(1):78–82.
- , , , , . Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279(19):1560–1565.
- . Nurse/physician communication through a sensemaking lens: shifting the paradigm to improve patient safety. Med Care. 2010;48(11):941–946.
- . Nursing Against the Odds: How Health Care Cost Cutting, Media Stereotypes, and Medical Hubris Undermine Nurses and Patient Care. Ithaca, NY: Cornell University Press; 2005.
- . Focus on research methods: whatever happened to qualitative description? Res Nurs Health. 2000;23:334–340.
- , , , , . Organizational assessment in intensive care units (ICUs): construct development, reliability, and validity of the ICU nurse‐physician questionnaire. Med Care. 1991;29(8):709–726.
- . Development of an instrument to measure collaboration and satisfaction about care decisions. J Adv Nurs. 1994;20(1):176–182.
- . Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–188.
- , , . Does the structure of inpatient rounds affect medical student education? Int J Med Educ. 2013;4:96–100.
- U.S. Department of Veterans Affairs, Office of Academic Affiliations. Medical and Dental Education Program. Available at: http://www.va. gov/oaa/GME_default.asp. Published 2012. Accessed May 08, 2013.
- , . Graduate medical education, 2011–2012. JAMA. 2012;308(21):2264–2279.
- , , , et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(11):866–874.
- , , , , , . Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859–865.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- , , . ‘It depends': medical residents' perspectives on working with nurses. Am J Nurs. 2009;109(7):34–44.
- , . Organizational silence: a barrier to change and development in a pluralistic world. Acad Manage Rev. 2000;25(4):706–725.
- , . Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organiz Behav. 2006;27:941–966.
- , , , , . Interprofessional communication with hospitalist and consultant physicians in general internal medicine: a qualitative study. BMC Health Serv Res. 2012;12:437.
- , , , , , . A new tool to give hospitalists feedback to improve interprofessional teamwork and advance patient care. Health Aff (Millwood). 2012;31(11):2485–2492.
- , , , , , . Impact of instructional practices on student satisfaction with attendings' teaching in the inpatient component of internal medicine clerkships. J Gen Intern Med. 2006;21(1):7–12.
- , . Medical students' perceptions of the elements of effective inpatient teaching by attending physicians and housestaff. J Gen Intern Med. 2005;20(7):635–639.
- National Board of Medical Examiners Subject Examination Program. Internal Medicine Advanced Clinical Examination, score interpretation guide. Available at: http://www.nbme.org/PDF/SampleScoreReports/Internal_Medicine_ACE_Score_Report.pdf. Published 2011. Accessed September 13, 2013.
- . The impact of hospitalists on medical education and the academic health system. Ann Intern Med. 1999;130(4 part 2):364–367.
- Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, D.C.: National Academies Press; 2000.
- Institute of Medicine of the National Academies. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academies Press; 2001.
- , , , . Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102–1112.
- . Growth in care provided by hospitalists. N Engl J Med. 2009;360(26):2789–2791.
- American Hospital Association. AHA Annual Survey of Hospitals, 2010. Chicago, IL: Health Forum, LLC; 2010.
- , , , . Preventing hospital‐acquired infections: a national survey of practices reported by U.S. hospitals in 2005 and 2009. J Gen Intern Med. 2012;27(7):773–779.
- , . Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;19(4):392–393.
- , . Do hospitalist physicians improve the quality of inpatient care delivery? A systematic review of process, efficiency and outcome measures. BMC Med. 2011;9:58.
- , , , . Effect of hospitalist attending physicians on trainee educational experiences: a systematic review. J Hosp Med. 2009;4(8):490–498.
- , , , , , . Resident satisfaction on an academic hospitalist service: time to teach. Am J Med. 2002;112(7):597–601.
- , , , et al. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19(4):293–301.
- , . Third‐year medical students' evaluation of hospitalist and nonhospitalist faculty during the inpatient portion of their pediatrics clerkships. J Hosp Med. 2007;2(1):17–22.
- , , , . Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations. Acad Med. 2004;79(1):78–82.
- , , , , . Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279(19):1560–1565.
- . Nurse/physician communication through a sensemaking lens: shifting the paradigm to improve patient safety. Med Care. 2010;48(11):941–946.
- . Nursing Against the Odds: How Health Care Cost Cutting, Media Stereotypes, and Medical Hubris Undermine Nurses and Patient Care. Ithaca, NY: Cornell University Press; 2005.
- . Focus on research methods: whatever happened to qualitative description? Res Nurs Health. 2000;23:334–340.
- , , , , . Organizational assessment in intensive care units (ICUs): construct development, reliability, and validity of the ICU nurse‐physician questionnaire. Med Care. 1991;29(8):709–726.
- . Development of an instrument to measure collaboration and satisfaction about care decisions. J Adv Nurs. 1994;20(1):176–182.
- . Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–188.
- , , . Does the structure of inpatient rounds affect medical student education? Int J Med Educ. 2013;4:96–100.
- U.S. Department of Veterans Affairs, Office of Academic Affiliations. Medical and Dental Education Program. Available at: http://www.va. gov/oaa/GME_default.asp. Published 2012. Accessed May 08, 2013.
- , . Graduate medical education, 2011–2012. JAMA. 2012;308(21):2264–2279.
- , , , et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(11):866–874.
- , , , , , . Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859–865.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- , , . ‘It depends': medical residents' perspectives on working with nurses. Am J Nurs. 2009;109(7):34–44.
- , . Organizational silence: a barrier to change and development in a pluralistic world. Acad Manage Rev. 2000;25(4):706–725.
- , . Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organiz Behav. 2006;27:941–966.
- , , , , . Interprofessional communication with hospitalist and consultant physicians in general internal medicine: a qualitative study. BMC Health Serv Res. 2012;12:437.
- , , , , , . A new tool to give hospitalists feedback to improve interprofessional teamwork and advance patient care. Health Aff (Millwood). 2012;31(11):2485–2492.
- , , , , , . Impact of instructional practices on student satisfaction with attendings' teaching in the inpatient component of internal medicine clerkships. J Gen Intern Med. 2006;21(1):7–12.
- , . Medical students' perceptions of the elements of effective inpatient teaching by attending physicians and housestaff. J Gen Intern Med. 2005;20(7):635–639.
- National Board of Medical Examiners Subject Examination Program. Internal Medicine Advanced Clinical Examination, score interpretation guide. Available at: http://www.nbme.org/PDF/SampleScoreReports/Internal_Medicine_ACE_Score_Report.pdf. Published 2011. Accessed September 13, 2013.
- . The impact of hospitalists on medical education and the academic health system. Ann Intern Med. 1999;130(4 part 2):364–367.
© 2013 Society of The Authors. Journal of Hospital Medicine published by Wiley Periodicals, Inc. on behalf of Society of Hospital Medicine.
Pediatrics Preoperative Evaluation
Pediatric hospitalists are increasingly following their adult counterparts' lead in participating in comanagement programs with surgeons. In the 20112012 Society of Hospital Medicine survey of hospitalist practice models, 94% of adult hospitalists and 72% of pediatric hospitalists reported comanaging surgical patients.[1] Adult patients comanaged postoperatively have shown equivalent clinical outcomes with strong endorsement from nurses and surgeons in 1 study[2] and reduced morbidity, mortality, and length of stay in other studies.[3, 4]
One of the drivers of pediatric hospitalists comanaging surgical patients may be the increased complexity of hospitalized children.[5, 6, 7, 8] Two pediatric studies have assessed hospitalistsurgeon comanagement of medically complex children in the postoperative period. One study evaluating 14 patients undergoing spinal fusion surgery for neuromuscular scoliosis showed an association between pediatric hospitalist comanagement and a decreased length of stay, with decreased variability in postoperative length of stay.[9] A study of 207 medically complex children undergoing spinal fusion surgery for neuromuscular scoliosis suggested an association between comanagement and reduced laboratory studies and parenteral nutrition but an initial increase in costs.[10]
Pediatric hospitalist programs have also followed adult programs' lead in evaluating surgical patients preoperatively. Studies of preoperative medical evaluations for adult surgical patients have reported mixed results, with improved use of recommended medical therapies, length of stay, and mortality postoperatively in 1 study,[11] whereas other studies have reported longer lengths of stay and higher costs.[12, 13] One adult study described a protocol‐based approach in which hospitalists coordinated pulmonary and cardiac evaluations for high‐risk spine patients but did not report any outcomes.[14] A pediatric study from the Netherlands described a multidisciplinary team approach to these patients, including both preoperative and postoperative evaluation, but did not include a hospitalist or general pediatrician nor present data on outcomes.[15]
In 2009, we began a hospitalist preoperative evaluation program for patients with neuromuscular scoliosis in anticipation of spinal fusion surgery. This program was established by the hospital administration in response to 2 sentinel events. Hospitalists, who had already begun comanaging surgical patients postoperatively, were required to see patients with neuromuscular scoliosis preoperatively. Hospitalists were felt to be knowledgeable about postoperative complications of spinal fusion surgery and were thought to perhaps be able to prevent certain postoperative complications.
In the current study, we sought to evaluate certain outcomes associated with this preoperative program. We hypothesized that evaluations for more complex patients would be more likely to be associated with preoperative changes. We evaluated how frequently hospitalists make recommendations for changes in patients' medical regimens or request further diagnostic evaluations and if any clinical characteristics were associated with hospitalists making these recommendations.
METHODS
Setting/Program Structure
We conducted a retrospective chart review of all 214 patients with the diagnosis of neuromuscular scoliosis who were seen for a preoperative evaluation by a pediatric hospitalist at our institution from November 2009 through September 2012. Nemours/AI duPont Hospital for Children is a 200‐bed freestanding children's hospital with 11 pediatric orthopedic surgeons, 5 of whom perform spinal fusion surgery on patients with neuromuscular scoliosis. Our hospitalist group consists of 6 hospitalists, all of whom rotate on the medically complex comanagement service for 1 week at a time. The hospitalist who was assigned to the medically complex comanagement service for the week saw both postoperative patients and an average of 1 to 2 preoperative patients that week. All patients with neuromuscular scoliosis who were scheduled for spinal fusion surgery were seen preoperatively by a hospitalist. These patients included any with an underlying diagnosis of cerebral palsy, myopathy, skeletal dysplasia, or syndrome such as neurofibromatosis. Patients who were scheduled for spinal fusion surgery were referred to the hospitalists via the orthopedic scheduling department or perioperative services. These patients were typically seen in the general pediatrics outpatient area or in the outpatient orthopedics area of the hospital 1 to 2 months prior to surgery. The goal of the preoperative visit was to ensure patients were evaluated thoroughly before surgery. Hospitalists were given authority to delay or even cancel surgery, though in no case in this study was surgery cancelled. Hospitalists were responsible for following up on consultations and further studies obtained before surgery. Patients with a Cobb angle of more than 90 were by policy referred to pulmonology and cardiology for a preoperative evaluation. Further testing in those domains, such as pulmonary function testing or echocardiograms, was at the discretion of the appropriate specialist.
Study Procedure
After receiving approval from the hospital institutional review board, we performed a case series study. Three investigators (D.R., S.C., and D.P.) reviewed the preoperative visit note for each patient. We identified all patients who had spinal fusion surgery for neuromuscular scoliosis via International Classification of Diseases, 9th Revision (ICD‐9) codes, including that for neuromuscular scoliosis, and reviewed the patients' charts for preoperative visits. We used the preoperative note from the hospitalist as the definitive source for clinical information about the patient such as underlying diagnosis or etiology of the neuromuscular scoliosis. We used a structured data abstraction form to collect data regarding patient demographics, date of visit, time to surgery, type of surgery, number of standing daily (not as‐needed) preoperative prescription medications, and dependence on medical technology. We defined seizure disorder as present when a patient was taking standing prescription medication for seizures or had been recommended to take standing medication for seizures.
We recorded patient comorbidities related to the gastrointestinal, cardiac, and pulmonary systems. Prior to chart review, we agreed on standard definitions for significant problems in these arenas. We defined a significant problem as one in which a standing prescription medication was required, medical technology was required, or a subspecialist was consulted on a regular basis. To establish inter‐rater reliability using this definition, the 3 investigators independently reviewed an initial series of 5 charts. Inter‐rater reliability was established at 90%.
Main Outcome Measures
We recorded whether the hospitalist made any preoperative recommendations. Recommendations were categorized as: change in medication, changes in nutrition, laboratory or imaging studies, other diagnostic tests, or subspecialty referral. We defined a medication change as any change that involved a new prescription medication to be used on a standing basis, a change in dosing to a standing prescription medication, or the discontinuing of a standing prescription medication. We did not include changes in medications used on an as‐needed basis. We also recorded whether the hospitalist made any recommendations regarding further preoperative evaluation such as laboratory studies, imaging studies, other studies, or consultation with a subspecialist. We did not include laboratory studies that are routinely obtained preoperatively such as coagulation studies or blood count. We then recorded whether the hospitalist contacted a subspecialist or requested that an evaluation be done by that subspecialist prior to surgery.
Analysis
We used Stata 12 software (StataCorp, College Station, TX) to conduct all analyses. We used frequencies to describe categorical variables. Linear variables were not normally distributed and were therefore described using median and interquartile range. We calculated the simple, unadjusted odds ratio (OR) (95% confidence interval [CI]) of the hospitalist making a recommendation during the preoperative visit based on each variable. We defined statistical significance as a P value <0.05.
RESULTS
Overall, 214 patients were included in our study. Typical patients included those with cerebral palsy scheduled to undergo posterior spinal fusion surgery. Many had significant comorbidities, including seizures and gastrointestinal (GI) disease, and were dependent on medical technology.
Regarding hospitalist recommendations, overall 155 patients (72%) received at least 1 recommendation. Types of recommendations are listed in Table 1. The most common type of recommendation regarding the patient's current regimen was medication change (82 patients, 38%). Recommendations for changes in nutrition were made in 46 patients (21%). Subspecialist input was elicited in 76 patients (36%); a subspecialist appointment was suggested most commonly (36 patients, 17%), whereas a telephone consultation occurred in 15 patients (7%). Hospitalists also frequently requested further diagnostic evaluation, especially laboratory studies (41 patients, 19%). Imaging studies were requested less frequently (11 patients, 5.1%) as were other studies such as electrocardiograms and pulmonary function tests (6 patients, 2.8%, each). No patient received a preoperative hospitalist recommendation to cancel or postpone surgery.
| Type of Recommendation | n (%) |
|---|---|
| |
| Changes in regimen | |
| Medication change (start new, discontinue, change dose) | 82 (38%) |
| Nutrition modification | 46 (21%) |
| Further diagnostic evaluation | |
| Laboratory studies | 41 (19%) |
| Imaging studies | 11 (5%) |
| Pulmonary function tests | 6 (3%) |
| Electrocardiograms | 6 (3%) |
| Referral to or contacted subspecialist | 76 (36%) |
Certain patient characteristics were associated with a statistically significant increase in likelihood of a preoperative intervention by the pediatric hospitalist (Table 2). These included type of surgery (OR: 2.70, 95% CI: 1.22‐5.97 for posterior spinal fusion), number of preoperative prescription medications (OR: 1.19, 95% CI: 1.06‐1.34), and nonambulatory status (OR: 2.02, 95% CI: 1.09‐3.74). Underlying disease also showed a statistically significant association with recommendations being made; patients were more likely to receive recommendations if they had cerebral palsy (OR: 2.01, 95% CI: 1.03‐3.92), spina bifida (OR: 2.33, 95% CI: 1.90‐3.48), and neuropathy (all had recommendations). An underlying diagnosis of skeletal dysplasia was statistically significantly associated with a decreased rate of recommendations being made (OR: 0.29, 95% CI: 0.14‐0.61). Patients with seizures (OR: 2.68, 95% CI: 1.29‐5.57) or GI comorbidity were more likely to receive a preoperative recommendation made by the hospitalist (OR: 3.35, 95% CI: 1.74‐6.45), but patients with cardiac and pulmonary comorbidities were not.
| Characteristics | Number (%) or Median (IQR) | Recommendations? | ||
|---|---|---|---|---|
| Yes, n=155 | No, n=59 | Odds of Recommendation, OR (95% CI) | ||
| ||||
| Demographics | ||||
| Gender, female | 106 (50%) | 77 (60%) | 29 (49%) | 0.97 (0.53‐1.78) |
| Age, y | 13 (1016) | 13 (1016) | 12 (1016) | 1.05 (0.98‐1.12) |
| Year of visit | ||||
| 2009 | 41 (19%) | 32 (21%) | 9 (15%) | Ref |
| 2010 | 65 (30%) | 47 (30%) | 18 (30%) | 0.73 (0.29‐1.84) |
| 2011 | 64 (30%) | 43 (28%) | 21 (36%) | 0.58 (0.23‐1.42) |
| 2012 | 44 (21%) | 33 (21%) | 11 (19%) | 0.84 (0.31‐2.31) |
| Days from visit to surgery | 34 (1445) | 35 (1747) | 27 (841) | 1.02 (1.001.03) |
| Type of surgerya | ||||
| PSF | 184 (86%) | 139 (90%) | 45 (76%) | 2.70 (1.22‐5.97) |
| Growing rod | 9 (4.7%) | 6 (4%) | 3 (5%) | 0.75 (0.18‐3.11) |
| Cervical fusion | 17 (7.9%) | 9 6%) | 8 (13%) | 0.39 (0.14‐1.07) |
| Halo, then PSF | 4 (1.9%) | 1 (0.6%) | 3 (5%) | 0.12 (0.01‐1.19) |
| Underlying diseasea | ||||
| Cerebral palsy | 78 (36%) | 63 (41%) | 15 (25%) | 2.01 (1.03‐3.92) |
| Neuropathy | 4 (2%) | 4 (3%) | 0 (0%) | All had recommendations |
| Myopathy | 19 (9%) | 16 (10%) | 3 (5%) | 2.14 (0.60‐7.66) |
| Metabolic disorder | 6 (3%) | 4 (3%) | 2 (3%) | 0.75 (0.13‐4.23) |
| Skeletal dysplasia | 38 (18%) | 19 (12%) | 19 (32%) | 0.29 (0.14‐0.61) |
| Spina bifida | 7 (3%) | 6 (4%) | 1 (2%) | 2.33 (1.90‐3.48) |
| Genetic disorder (including osteogenesis imperfecta) | 40 (19%) | 28 (18%) | 12 (20%) | 0.86 (0.41‐1.84) |
| Other | 22 (10%) | 15 (10%) | 7 (12%) | 0.79 (0.31‐2.06) |
| Number of preoperative prescription medications | 2 (15) | 3 (15) | 1 (03) | 1.19 (1.06‐1.34) |
| Institutionalized | 9 (4.2%) | 6 (4%) | 3 (5%) | 0.75 (0.18‐3.11) |
| Nonambulatory | 114 (54%) | 90 (59%) | 24 (41%) | 2.02 (1.09‐3.74) |
| Dependence on technologya | ||||
| Feeding tube | 89 (41.6%) | 66 (43%) | 23 (39%) | 1.16 (0.63‐2.14) |
| Baclofen pump | 20 (9.3%) | 18 (12%) | 2 (3%) | 3.74 (0.84‐16.67) |
| Ventriculoperitoneal shunt | 24 (11.2%) | 18 (12%) | 6 (10%) | 1.16 (0.44‐3.08) |
| Vagal nerve stimulator/deep brain stimulator | 8 (3.7%) | 6 (4%) | 2 (3%) | 1.15 (0.22‐5.85) |
| Tracheostomy | 13 (6.1%) | 9 (6%) | 4 (7%) | 0.85 (0.25‐2.86) |
| Home mechanical ventilation (not BiPAP) | 6 (2.8%) | 5 (3%) | 1 (2%) | 1.93 (0.22‐16.90) |
| Home oxygen, BiPAP, or CPAP | 25 (11.7%) | 22 (14%) | 3 (5%) | 3.09 (0.89‐10.73) |
| Seizure disorder | 70 (33%) | 59 (38%) | 11 (19%) | 2.68 (1.29‐5.57) |
| Significant GI comorbidity | 102 (48%) | 86 (55%) | 16 (27%) | 3.35 (1.74‐6.45) |
| Significant cardiac comorbidity | 37 (17.3%) | 26 (17%) | 11 (19%) | 0.88 (0.40‐1.92) |
| Significant pulmonary comorbidity | 78 (36.4%) | 57 (37%) | 21 (36%) | 1.05 (0.56‐1.97) |
DISCUSSION
This is the first large study to examine the role of the pediatric hospitalist in preoperative evaluation of complex surgical patients. Our program developed as an evolution of a postoperative program that we have described previously.[10] The postoperative component of our comanagement program began in 2003, and the preoperative aspect was added in 2009. We believe that the preoperative component to our program contributed in some degree to the decrease in utilization of certain aspects of postoperative care over time such as parenteral nutrition. This change may have occurred because of improved bowel management perioperatively, for instance. Although the preoperative hospitalist evaluation program was instituted by our hospital administration, we felt a preoperative hospitalist evaluation represented a standardized, comprehensive way to evaluate patients before surgery. By 2009, the hospitalists at our hospital had already developed some expertise in managing patients after undergoing spinal fusion surgery.
The fact that hospitalists made recommendations for changes in medications, nutritional management, or diagnostic tests at such a high rate (72%) is interesting. We were not surprised by this finding based on anecdotal evidence because we feel that many of these patients may receive somewhat fragmented care because they often see multiple medical specialists. The high rate of interventions noted in our study may result from the fact that hospitalists who comanage these patients frequently after spinal fusion surgery were attempting to prevent postoperative complications that they see after this type of surgery. Many pediatric hospitalists have developed significant experience in caring for medically complex children and thus may feel more comfortable making preoperative recommendations than other general pediatricians.
We were not surprised to find that hospitalists made preoperative recommendations more frequently in children who had seizures, significant GI comorbidity, and who were nonambulatory. We also noted a statistically significant increased rate of recommendations when patients were on more preoperative medications. We believe that these variables suggest a population that is more medically complex. The importance of selecting medically complex patients for hospitalist comanagement has been noted previously.[16] Therefore, comanagement programs looking to maximize patient benefit for a preoperative hospitalist evaluation program might limit these visits to those who are most medically complex. We found a particularly low yield in evaluation of patients with skeletal dysplasia for example and may discontinue seeing these patients preoperatively.
We found the lack of statistically significant change in rate of hospitalist recommendations among patients with cardiac and pulmonary comorbidities interesting. Whether this was related to the mandatory preoperative pulmonology and cardiology visits is not certain. We hope to study the impact of these preoperative visits in the future as we continue to evaluate our perioperative program.
Several limitations of this study deserve note. This study was performed at 1 institution with 1 group of hospitalists and 1 group of orthopedic surgeons. Two of the study authors (D.R. and D.P.) were among the hospitalists involved with the clinical program. The study was retrospective and nonrandomized. We did not contact primary care physicians as a rule for further information about these patients. In this study, we did not specifically study the impact of hospitalist preoperative evaluations on postoperative outcomes, although the preoperative component represented an important aspect of the more systematic intervention described elsewhere.[10]
CONCLUSIONS
A preoperative program for pediatric hospitalists to see children in anticipation of spinal surgery for neuromuscular scoliosis leads to a high rate of recommendations for changes in medical management or diagnostic evaluation. Certain patient characteristics are more highly associated with hospitalists making these recommendations prior to surgery.
- 2012 State of Hospital Medicine Report, Society of Hospital Medicine. Further information available at: http://www.hospitalmedicine.org/survey.
- , , , et al.; Hospitalist‐Orthopedic Team Trial Investigators. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28–38.
- , , , et al. Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma. 2006;20(3):172–178, discussion 179–180.
- , , , et al. Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med. 2005;165(7):796–801.
- , , . Hospitalist care of the medically complex child. Pediatr Clin North Am. 2005;52(4):1165–1167.
- , , , et al. Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126(4):638–646.
- , , , et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655.
- , , , et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–538.
- , , , et al. Pediatric hospitalist comanagement of spinal fusion surgery patients. J Hosp Med. 2007;2:23–30.
- , , , et al. Outcomes and costs associated with hospitalist comanagement of medically complex children undergoing spinal fusion surgery. Hosp Pediatr. 2013;3(3):233–241.
- , , , et al. Perioperative processes and outcomes after implementation of a hospitalist‐run preoperative clinic. J Hosp Med. 2012 7:697–701.
- , , , , . Outcomes and processes of care related to preoperative medical consultation. Arch Intern Med. 2010;170(15):1365–1374.
- , , , et al. Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med. 2007;167(21):2338–2344.
- , , , et al. Standardizing care for high‐risk patients in spine surgery: the Northwestern High‐Risk Spine Protocol. Spine. 2010;35(25):2232–2238.
- , , , . Neuromuscular scoliosis: clinical evaluation pre‐ and postoperative. J Pediatr Orthop. 2000;9:217–220.
- . Just because you can, doesn't mean that you should: a call for the rational application of hospitalist comanagement. J Hosp Med. 2008:3:398–402.
Pediatric hospitalists are increasingly following their adult counterparts' lead in participating in comanagement programs with surgeons. In the 20112012 Society of Hospital Medicine survey of hospitalist practice models, 94% of adult hospitalists and 72% of pediatric hospitalists reported comanaging surgical patients.[1] Adult patients comanaged postoperatively have shown equivalent clinical outcomes with strong endorsement from nurses and surgeons in 1 study[2] and reduced morbidity, mortality, and length of stay in other studies.[3, 4]
One of the drivers of pediatric hospitalists comanaging surgical patients may be the increased complexity of hospitalized children.[5, 6, 7, 8] Two pediatric studies have assessed hospitalistsurgeon comanagement of medically complex children in the postoperative period. One study evaluating 14 patients undergoing spinal fusion surgery for neuromuscular scoliosis showed an association between pediatric hospitalist comanagement and a decreased length of stay, with decreased variability in postoperative length of stay.[9] A study of 207 medically complex children undergoing spinal fusion surgery for neuromuscular scoliosis suggested an association between comanagement and reduced laboratory studies and parenteral nutrition but an initial increase in costs.[10]
Pediatric hospitalist programs have also followed adult programs' lead in evaluating surgical patients preoperatively. Studies of preoperative medical evaluations for adult surgical patients have reported mixed results, with improved use of recommended medical therapies, length of stay, and mortality postoperatively in 1 study,[11] whereas other studies have reported longer lengths of stay and higher costs.[12, 13] One adult study described a protocol‐based approach in which hospitalists coordinated pulmonary and cardiac evaluations for high‐risk spine patients but did not report any outcomes.[14] A pediatric study from the Netherlands described a multidisciplinary team approach to these patients, including both preoperative and postoperative evaluation, but did not include a hospitalist or general pediatrician nor present data on outcomes.[15]
In 2009, we began a hospitalist preoperative evaluation program for patients with neuromuscular scoliosis in anticipation of spinal fusion surgery. This program was established by the hospital administration in response to 2 sentinel events. Hospitalists, who had already begun comanaging surgical patients postoperatively, were required to see patients with neuromuscular scoliosis preoperatively. Hospitalists were felt to be knowledgeable about postoperative complications of spinal fusion surgery and were thought to perhaps be able to prevent certain postoperative complications.
In the current study, we sought to evaluate certain outcomes associated with this preoperative program. We hypothesized that evaluations for more complex patients would be more likely to be associated with preoperative changes. We evaluated how frequently hospitalists make recommendations for changes in patients' medical regimens or request further diagnostic evaluations and if any clinical characteristics were associated with hospitalists making these recommendations.
METHODS
Setting/Program Structure
We conducted a retrospective chart review of all 214 patients with the diagnosis of neuromuscular scoliosis who were seen for a preoperative evaluation by a pediatric hospitalist at our institution from November 2009 through September 2012. Nemours/AI duPont Hospital for Children is a 200‐bed freestanding children's hospital with 11 pediatric orthopedic surgeons, 5 of whom perform spinal fusion surgery on patients with neuromuscular scoliosis. Our hospitalist group consists of 6 hospitalists, all of whom rotate on the medically complex comanagement service for 1 week at a time. The hospitalist who was assigned to the medically complex comanagement service for the week saw both postoperative patients and an average of 1 to 2 preoperative patients that week. All patients with neuromuscular scoliosis who were scheduled for spinal fusion surgery were seen preoperatively by a hospitalist. These patients included any with an underlying diagnosis of cerebral palsy, myopathy, skeletal dysplasia, or syndrome such as neurofibromatosis. Patients who were scheduled for spinal fusion surgery were referred to the hospitalists via the orthopedic scheduling department or perioperative services. These patients were typically seen in the general pediatrics outpatient area or in the outpatient orthopedics area of the hospital 1 to 2 months prior to surgery. The goal of the preoperative visit was to ensure patients were evaluated thoroughly before surgery. Hospitalists were given authority to delay or even cancel surgery, though in no case in this study was surgery cancelled. Hospitalists were responsible for following up on consultations and further studies obtained before surgery. Patients with a Cobb angle of more than 90 were by policy referred to pulmonology and cardiology for a preoperative evaluation. Further testing in those domains, such as pulmonary function testing or echocardiograms, was at the discretion of the appropriate specialist.
Study Procedure
After receiving approval from the hospital institutional review board, we performed a case series study. Three investigators (D.R., S.C., and D.P.) reviewed the preoperative visit note for each patient. We identified all patients who had spinal fusion surgery for neuromuscular scoliosis via International Classification of Diseases, 9th Revision (ICD‐9) codes, including that for neuromuscular scoliosis, and reviewed the patients' charts for preoperative visits. We used the preoperative note from the hospitalist as the definitive source for clinical information about the patient such as underlying diagnosis or etiology of the neuromuscular scoliosis. We used a structured data abstraction form to collect data regarding patient demographics, date of visit, time to surgery, type of surgery, number of standing daily (not as‐needed) preoperative prescription medications, and dependence on medical technology. We defined seizure disorder as present when a patient was taking standing prescription medication for seizures or had been recommended to take standing medication for seizures.
We recorded patient comorbidities related to the gastrointestinal, cardiac, and pulmonary systems. Prior to chart review, we agreed on standard definitions for significant problems in these arenas. We defined a significant problem as one in which a standing prescription medication was required, medical technology was required, or a subspecialist was consulted on a regular basis. To establish inter‐rater reliability using this definition, the 3 investigators independently reviewed an initial series of 5 charts. Inter‐rater reliability was established at 90%.
Main Outcome Measures
We recorded whether the hospitalist made any preoperative recommendations. Recommendations were categorized as: change in medication, changes in nutrition, laboratory or imaging studies, other diagnostic tests, or subspecialty referral. We defined a medication change as any change that involved a new prescription medication to be used on a standing basis, a change in dosing to a standing prescription medication, or the discontinuing of a standing prescription medication. We did not include changes in medications used on an as‐needed basis. We also recorded whether the hospitalist made any recommendations regarding further preoperative evaluation such as laboratory studies, imaging studies, other studies, or consultation with a subspecialist. We did not include laboratory studies that are routinely obtained preoperatively such as coagulation studies or blood count. We then recorded whether the hospitalist contacted a subspecialist or requested that an evaluation be done by that subspecialist prior to surgery.
Analysis
We used Stata 12 software (StataCorp, College Station, TX) to conduct all analyses. We used frequencies to describe categorical variables. Linear variables were not normally distributed and were therefore described using median and interquartile range. We calculated the simple, unadjusted odds ratio (OR) (95% confidence interval [CI]) of the hospitalist making a recommendation during the preoperative visit based on each variable. We defined statistical significance as a P value <0.05.
RESULTS
Overall, 214 patients were included in our study. Typical patients included those with cerebral palsy scheduled to undergo posterior spinal fusion surgery. Many had significant comorbidities, including seizures and gastrointestinal (GI) disease, and were dependent on medical technology.
Regarding hospitalist recommendations, overall 155 patients (72%) received at least 1 recommendation. Types of recommendations are listed in Table 1. The most common type of recommendation regarding the patient's current regimen was medication change (82 patients, 38%). Recommendations for changes in nutrition were made in 46 patients (21%). Subspecialist input was elicited in 76 patients (36%); a subspecialist appointment was suggested most commonly (36 patients, 17%), whereas a telephone consultation occurred in 15 patients (7%). Hospitalists also frequently requested further diagnostic evaluation, especially laboratory studies (41 patients, 19%). Imaging studies were requested less frequently (11 patients, 5.1%) as were other studies such as electrocardiograms and pulmonary function tests (6 patients, 2.8%, each). No patient received a preoperative hospitalist recommendation to cancel or postpone surgery.
| Type of Recommendation | n (%) |
|---|---|
| |
| Changes in regimen | |
| Medication change (start new, discontinue, change dose) | 82 (38%) |
| Nutrition modification | 46 (21%) |
| Further diagnostic evaluation | |
| Laboratory studies | 41 (19%) |
| Imaging studies | 11 (5%) |
| Pulmonary function tests | 6 (3%) |
| Electrocardiograms | 6 (3%) |
| Referral to or contacted subspecialist | 76 (36%) |
Certain patient characteristics were associated with a statistically significant increase in likelihood of a preoperative intervention by the pediatric hospitalist (Table 2). These included type of surgery (OR: 2.70, 95% CI: 1.22‐5.97 for posterior spinal fusion), number of preoperative prescription medications (OR: 1.19, 95% CI: 1.06‐1.34), and nonambulatory status (OR: 2.02, 95% CI: 1.09‐3.74). Underlying disease also showed a statistically significant association with recommendations being made; patients were more likely to receive recommendations if they had cerebral palsy (OR: 2.01, 95% CI: 1.03‐3.92), spina bifida (OR: 2.33, 95% CI: 1.90‐3.48), and neuropathy (all had recommendations). An underlying diagnosis of skeletal dysplasia was statistically significantly associated with a decreased rate of recommendations being made (OR: 0.29, 95% CI: 0.14‐0.61). Patients with seizures (OR: 2.68, 95% CI: 1.29‐5.57) or GI comorbidity were more likely to receive a preoperative recommendation made by the hospitalist (OR: 3.35, 95% CI: 1.74‐6.45), but patients with cardiac and pulmonary comorbidities were not.
| Characteristics | Number (%) or Median (IQR) | Recommendations? | ||
|---|---|---|---|---|
| Yes, n=155 | No, n=59 | Odds of Recommendation, OR (95% CI) | ||
| ||||
| Demographics | ||||
| Gender, female | 106 (50%) | 77 (60%) | 29 (49%) | 0.97 (0.53‐1.78) |
| Age, y | 13 (1016) | 13 (1016) | 12 (1016) | 1.05 (0.98‐1.12) |
| Year of visit | ||||
| 2009 | 41 (19%) | 32 (21%) | 9 (15%) | Ref |
| 2010 | 65 (30%) | 47 (30%) | 18 (30%) | 0.73 (0.29‐1.84) |
| 2011 | 64 (30%) | 43 (28%) | 21 (36%) | 0.58 (0.23‐1.42) |
| 2012 | 44 (21%) | 33 (21%) | 11 (19%) | 0.84 (0.31‐2.31) |
| Days from visit to surgery | 34 (1445) | 35 (1747) | 27 (841) | 1.02 (1.001.03) |
| Type of surgerya | ||||
| PSF | 184 (86%) | 139 (90%) | 45 (76%) | 2.70 (1.22‐5.97) |
| Growing rod | 9 (4.7%) | 6 (4%) | 3 (5%) | 0.75 (0.18‐3.11) |
| Cervical fusion | 17 (7.9%) | 9 6%) | 8 (13%) | 0.39 (0.14‐1.07) |
| Halo, then PSF | 4 (1.9%) | 1 (0.6%) | 3 (5%) | 0.12 (0.01‐1.19) |
| Underlying diseasea | ||||
| Cerebral palsy | 78 (36%) | 63 (41%) | 15 (25%) | 2.01 (1.03‐3.92) |
| Neuropathy | 4 (2%) | 4 (3%) | 0 (0%) | All had recommendations |
| Myopathy | 19 (9%) | 16 (10%) | 3 (5%) | 2.14 (0.60‐7.66) |
| Metabolic disorder | 6 (3%) | 4 (3%) | 2 (3%) | 0.75 (0.13‐4.23) |
| Skeletal dysplasia | 38 (18%) | 19 (12%) | 19 (32%) | 0.29 (0.14‐0.61) |
| Spina bifida | 7 (3%) | 6 (4%) | 1 (2%) | 2.33 (1.90‐3.48) |
| Genetic disorder (including osteogenesis imperfecta) | 40 (19%) | 28 (18%) | 12 (20%) | 0.86 (0.41‐1.84) |
| Other | 22 (10%) | 15 (10%) | 7 (12%) | 0.79 (0.31‐2.06) |
| Number of preoperative prescription medications | 2 (15) | 3 (15) | 1 (03) | 1.19 (1.06‐1.34) |
| Institutionalized | 9 (4.2%) | 6 (4%) | 3 (5%) | 0.75 (0.18‐3.11) |
| Nonambulatory | 114 (54%) | 90 (59%) | 24 (41%) | 2.02 (1.09‐3.74) |
| Dependence on technologya | ||||
| Feeding tube | 89 (41.6%) | 66 (43%) | 23 (39%) | 1.16 (0.63‐2.14) |
| Baclofen pump | 20 (9.3%) | 18 (12%) | 2 (3%) | 3.74 (0.84‐16.67) |
| Ventriculoperitoneal shunt | 24 (11.2%) | 18 (12%) | 6 (10%) | 1.16 (0.44‐3.08) |
| Vagal nerve stimulator/deep brain stimulator | 8 (3.7%) | 6 (4%) | 2 (3%) | 1.15 (0.22‐5.85) |
| Tracheostomy | 13 (6.1%) | 9 (6%) | 4 (7%) | 0.85 (0.25‐2.86) |
| Home mechanical ventilation (not BiPAP) | 6 (2.8%) | 5 (3%) | 1 (2%) | 1.93 (0.22‐16.90) |
| Home oxygen, BiPAP, or CPAP | 25 (11.7%) | 22 (14%) | 3 (5%) | 3.09 (0.89‐10.73) |
| Seizure disorder | 70 (33%) | 59 (38%) | 11 (19%) | 2.68 (1.29‐5.57) |
| Significant GI comorbidity | 102 (48%) | 86 (55%) | 16 (27%) | 3.35 (1.74‐6.45) |
| Significant cardiac comorbidity | 37 (17.3%) | 26 (17%) | 11 (19%) | 0.88 (0.40‐1.92) |
| Significant pulmonary comorbidity | 78 (36.4%) | 57 (37%) | 21 (36%) | 1.05 (0.56‐1.97) |
DISCUSSION
This is the first large study to examine the role of the pediatric hospitalist in preoperative evaluation of complex surgical patients. Our program developed as an evolution of a postoperative program that we have described previously.[10] The postoperative component of our comanagement program began in 2003, and the preoperative aspect was added in 2009. We believe that the preoperative component to our program contributed in some degree to the decrease in utilization of certain aspects of postoperative care over time such as parenteral nutrition. This change may have occurred because of improved bowel management perioperatively, for instance. Although the preoperative hospitalist evaluation program was instituted by our hospital administration, we felt a preoperative hospitalist evaluation represented a standardized, comprehensive way to evaluate patients before surgery. By 2009, the hospitalists at our hospital had already developed some expertise in managing patients after undergoing spinal fusion surgery.
The fact that hospitalists made recommendations for changes in medications, nutritional management, or diagnostic tests at such a high rate (72%) is interesting. We were not surprised by this finding based on anecdotal evidence because we feel that many of these patients may receive somewhat fragmented care because they often see multiple medical specialists. The high rate of interventions noted in our study may result from the fact that hospitalists who comanage these patients frequently after spinal fusion surgery were attempting to prevent postoperative complications that they see after this type of surgery. Many pediatric hospitalists have developed significant experience in caring for medically complex children and thus may feel more comfortable making preoperative recommendations than other general pediatricians.
We were not surprised to find that hospitalists made preoperative recommendations more frequently in children who had seizures, significant GI comorbidity, and who were nonambulatory. We also noted a statistically significant increased rate of recommendations when patients were on more preoperative medications. We believe that these variables suggest a population that is more medically complex. The importance of selecting medically complex patients for hospitalist comanagement has been noted previously.[16] Therefore, comanagement programs looking to maximize patient benefit for a preoperative hospitalist evaluation program might limit these visits to those who are most medically complex. We found a particularly low yield in evaluation of patients with skeletal dysplasia for example and may discontinue seeing these patients preoperatively.
We found the lack of statistically significant change in rate of hospitalist recommendations among patients with cardiac and pulmonary comorbidities interesting. Whether this was related to the mandatory preoperative pulmonology and cardiology visits is not certain. We hope to study the impact of these preoperative visits in the future as we continue to evaluate our perioperative program.
Several limitations of this study deserve note. This study was performed at 1 institution with 1 group of hospitalists and 1 group of orthopedic surgeons. Two of the study authors (D.R. and D.P.) were among the hospitalists involved with the clinical program. The study was retrospective and nonrandomized. We did not contact primary care physicians as a rule for further information about these patients. In this study, we did not specifically study the impact of hospitalist preoperative evaluations on postoperative outcomes, although the preoperative component represented an important aspect of the more systematic intervention described elsewhere.[10]
CONCLUSIONS
A preoperative program for pediatric hospitalists to see children in anticipation of spinal surgery for neuromuscular scoliosis leads to a high rate of recommendations for changes in medical management or diagnostic evaluation. Certain patient characteristics are more highly associated with hospitalists making these recommendations prior to surgery.
Pediatric hospitalists are increasingly following their adult counterparts' lead in participating in comanagement programs with surgeons. In the 20112012 Society of Hospital Medicine survey of hospitalist practice models, 94% of adult hospitalists and 72% of pediatric hospitalists reported comanaging surgical patients.[1] Adult patients comanaged postoperatively have shown equivalent clinical outcomes with strong endorsement from nurses and surgeons in 1 study[2] and reduced morbidity, mortality, and length of stay in other studies.[3, 4]
One of the drivers of pediatric hospitalists comanaging surgical patients may be the increased complexity of hospitalized children.[5, 6, 7, 8] Two pediatric studies have assessed hospitalistsurgeon comanagement of medically complex children in the postoperative period. One study evaluating 14 patients undergoing spinal fusion surgery for neuromuscular scoliosis showed an association between pediatric hospitalist comanagement and a decreased length of stay, with decreased variability in postoperative length of stay.[9] A study of 207 medically complex children undergoing spinal fusion surgery for neuromuscular scoliosis suggested an association between comanagement and reduced laboratory studies and parenteral nutrition but an initial increase in costs.[10]
Pediatric hospitalist programs have also followed adult programs' lead in evaluating surgical patients preoperatively. Studies of preoperative medical evaluations for adult surgical patients have reported mixed results, with improved use of recommended medical therapies, length of stay, and mortality postoperatively in 1 study,[11] whereas other studies have reported longer lengths of stay and higher costs.[12, 13] One adult study described a protocol‐based approach in which hospitalists coordinated pulmonary and cardiac evaluations for high‐risk spine patients but did not report any outcomes.[14] A pediatric study from the Netherlands described a multidisciplinary team approach to these patients, including both preoperative and postoperative evaluation, but did not include a hospitalist or general pediatrician nor present data on outcomes.[15]
In 2009, we began a hospitalist preoperative evaluation program for patients with neuromuscular scoliosis in anticipation of spinal fusion surgery. This program was established by the hospital administration in response to 2 sentinel events. Hospitalists, who had already begun comanaging surgical patients postoperatively, were required to see patients with neuromuscular scoliosis preoperatively. Hospitalists were felt to be knowledgeable about postoperative complications of spinal fusion surgery and were thought to perhaps be able to prevent certain postoperative complications.
In the current study, we sought to evaluate certain outcomes associated with this preoperative program. We hypothesized that evaluations for more complex patients would be more likely to be associated with preoperative changes. We evaluated how frequently hospitalists make recommendations for changes in patients' medical regimens or request further diagnostic evaluations and if any clinical characteristics were associated with hospitalists making these recommendations.
METHODS
Setting/Program Structure
We conducted a retrospective chart review of all 214 patients with the diagnosis of neuromuscular scoliosis who were seen for a preoperative evaluation by a pediatric hospitalist at our institution from November 2009 through September 2012. Nemours/AI duPont Hospital for Children is a 200‐bed freestanding children's hospital with 11 pediatric orthopedic surgeons, 5 of whom perform spinal fusion surgery on patients with neuromuscular scoliosis. Our hospitalist group consists of 6 hospitalists, all of whom rotate on the medically complex comanagement service for 1 week at a time. The hospitalist who was assigned to the medically complex comanagement service for the week saw both postoperative patients and an average of 1 to 2 preoperative patients that week. All patients with neuromuscular scoliosis who were scheduled for spinal fusion surgery were seen preoperatively by a hospitalist. These patients included any with an underlying diagnosis of cerebral palsy, myopathy, skeletal dysplasia, or syndrome such as neurofibromatosis. Patients who were scheduled for spinal fusion surgery were referred to the hospitalists via the orthopedic scheduling department or perioperative services. These patients were typically seen in the general pediatrics outpatient area or in the outpatient orthopedics area of the hospital 1 to 2 months prior to surgery. The goal of the preoperative visit was to ensure patients were evaluated thoroughly before surgery. Hospitalists were given authority to delay or even cancel surgery, though in no case in this study was surgery cancelled. Hospitalists were responsible for following up on consultations and further studies obtained before surgery. Patients with a Cobb angle of more than 90 were by policy referred to pulmonology and cardiology for a preoperative evaluation. Further testing in those domains, such as pulmonary function testing or echocardiograms, was at the discretion of the appropriate specialist.
Study Procedure
After receiving approval from the hospital institutional review board, we performed a case series study. Three investigators (D.R., S.C., and D.P.) reviewed the preoperative visit note for each patient. We identified all patients who had spinal fusion surgery for neuromuscular scoliosis via International Classification of Diseases, 9th Revision (ICD‐9) codes, including that for neuromuscular scoliosis, and reviewed the patients' charts for preoperative visits. We used the preoperative note from the hospitalist as the definitive source for clinical information about the patient such as underlying diagnosis or etiology of the neuromuscular scoliosis. We used a structured data abstraction form to collect data regarding patient demographics, date of visit, time to surgery, type of surgery, number of standing daily (not as‐needed) preoperative prescription medications, and dependence on medical technology. We defined seizure disorder as present when a patient was taking standing prescription medication for seizures or had been recommended to take standing medication for seizures.
We recorded patient comorbidities related to the gastrointestinal, cardiac, and pulmonary systems. Prior to chart review, we agreed on standard definitions for significant problems in these arenas. We defined a significant problem as one in which a standing prescription medication was required, medical technology was required, or a subspecialist was consulted on a regular basis. To establish inter‐rater reliability using this definition, the 3 investigators independently reviewed an initial series of 5 charts. Inter‐rater reliability was established at 90%.
Main Outcome Measures
We recorded whether the hospitalist made any preoperative recommendations. Recommendations were categorized as: change in medication, changes in nutrition, laboratory or imaging studies, other diagnostic tests, or subspecialty referral. We defined a medication change as any change that involved a new prescription medication to be used on a standing basis, a change in dosing to a standing prescription medication, or the discontinuing of a standing prescription medication. We did not include changes in medications used on an as‐needed basis. We also recorded whether the hospitalist made any recommendations regarding further preoperative evaluation such as laboratory studies, imaging studies, other studies, or consultation with a subspecialist. We did not include laboratory studies that are routinely obtained preoperatively such as coagulation studies or blood count. We then recorded whether the hospitalist contacted a subspecialist or requested that an evaluation be done by that subspecialist prior to surgery.
Analysis
We used Stata 12 software (StataCorp, College Station, TX) to conduct all analyses. We used frequencies to describe categorical variables. Linear variables were not normally distributed and were therefore described using median and interquartile range. We calculated the simple, unadjusted odds ratio (OR) (95% confidence interval [CI]) of the hospitalist making a recommendation during the preoperative visit based on each variable. We defined statistical significance as a P value <0.05.
RESULTS
Overall, 214 patients were included in our study. Typical patients included those with cerebral palsy scheduled to undergo posterior spinal fusion surgery. Many had significant comorbidities, including seizures and gastrointestinal (GI) disease, and were dependent on medical technology.
Regarding hospitalist recommendations, overall 155 patients (72%) received at least 1 recommendation. Types of recommendations are listed in Table 1. The most common type of recommendation regarding the patient's current regimen was medication change (82 patients, 38%). Recommendations for changes in nutrition were made in 46 patients (21%). Subspecialist input was elicited in 76 patients (36%); a subspecialist appointment was suggested most commonly (36 patients, 17%), whereas a telephone consultation occurred in 15 patients (7%). Hospitalists also frequently requested further diagnostic evaluation, especially laboratory studies (41 patients, 19%). Imaging studies were requested less frequently (11 patients, 5.1%) as were other studies such as electrocardiograms and pulmonary function tests (6 patients, 2.8%, each). No patient received a preoperative hospitalist recommendation to cancel or postpone surgery.
| Type of Recommendation | n (%) |
|---|---|
| |
| Changes in regimen | |
| Medication change (start new, discontinue, change dose) | 82 (38%) |
| Nutrition modification | 46 (21%) |
| Further diagnostic evaluation | |
| Laboratory studies | 41 (19%) |
| Imaging studies | 11 (5%) |
| Pulmonary function tests | 6 (3%) |
| Electrocardiograms | 6 (3%) |
| Referral to or contacted subspecialist | 76 (36%) |
Certain patient characteristics were associated with a statistically significant increase in likelihood of a preoperative intervention by the pediatric hospitalist (Table 2). These included type of surgery (OR: 2.70, 95% CI: 1.22‐5.97 for posterior spinal fusion), number of preoperative prescription medications (OR: 1.19, 95% CI: 1.06‐1.34), and nonambulatory status (OR: 2.02, 95% CI: 1.09‐3.74). Underlying disease also showed a statistically significant association with recommendations being made; patients were more likely to receive recommendations if they had cerebral palsy (OR: 2.01, 95% CI: 1.03‐3.92), spina bifida (OR: 2.33, 95% CI: 1.90‐3.48), and neuropathy (all had recommendations). An underlying diagnosis of skeletal dysplasia was statistically significantly associated with a decreased rate of recommendations being made (OR: 0.29, 95% CI: 0.14‐0.61). Patients with seizures (OR: 2.68, 95% CI: 1.29‐5.57) or GI comorbidity were more likely to receive a preoperative recommendation made by the hospitalist (OR: 3.35, 95% CI: 1.74‐6.45), but patients with cardiac and pulmonary comorbidities were not.
| Characteristics | Number (%) or Median (IQR) | Recommendations? | ||
|---|---|---|---|---|
| Yes, n=155 | No, n=59 | Odds of Recommendation, OR (95% CI) | ||
| ||||
| Demographics | ||||
| Gender, female | 106 (50%) | 77 (60%) | 29 (49%) | 0.97 (0.53‐1.78) |
| Age, y | 13 (1016) | 13 (1016) | 12 (1016) | 1.05 (0.98‐1.12) |
| Year of visit | ||||
| 2009 | 41 (19%) | 32 (21%) | 9 (15%) | Ref |
| 2010 | 65 (30%) | 47 (30%) | 18 (30%) | 0.73 (0.29‐1.84) |
| 2011 | 64 (30%) | 43 (28%) | 21 (36%) | 0.58 (0.23‐1.42) |
| 2012 | 44 (21%) | 33 (21%) | 11 (19%) | 0.84 (0.31‐2.31) |
| Days from visit to surgery | 34 (1445) | 35 (1747) | 27 (841) | 1.02 (1.001.03) |
| Type of surgerya | ||||
| PSF | 184 (86%) | 139 (90%) | 45 (76%) | 2.70 (1.22‐5.97) |
| Growing rod | 9 (4.7%) | 6 (4%) | 3 (5%) | 0.75 (0.18‐3.11) |
| Cervical fusion | 17 (7.9%) | 9 6%) | 8 (13%) | 0.39 (0.14‐1.07) |
| Halo, then PSF | 4 (1.9%) | 1 (0.6%) | 3 (5%) | 0.12 (0.01‐1.19) |
| Underlying diseasea | ||||
| Cerebral palsy | 78 (36%) | 63 (41%) | 15 (25%) | 2.01 (1.03‐3.92) |
| Neuropathy | 4 (2%) | 4 (3%) | 0 (0%) | All had recommendations |
| Myopathy | 19 (9%) | 16 (10%) | 3 (5%) | 2.14 (0.60‐7.66) |
| Metabolic disorder | 6 (3%) | 4 (3%) | 2 (3%) | 0.75 (0.13‐4.23) |
| Skeletal dysplasia | 38 (18%) | 19 (12%) | 19 (32%) | 0.29 (0.14‐0.61) |
| Spina bifida | 7 (3%) | 6 (4%) | 1 (2%) | 2.33 (1.90‐3.48) |
| Genetic disorder (including osteogenesis imperfecta) | 40 (19%) | 28 (18%) | 12 (20%) | 0.86 (0.41‐1.84) |
| Other | 22 (10%) | 15 (10%) | 7 (12%) | 0.79 (0.31‐2.06) |
| Number of preoperative prescription medications | 2 (15) | 3 (15) | 1 (03) | 1.19 (1.06‐1.34) |
| Institutionalized | 9 (4.2%) | 6 (4%) | 3 (5%) | 0.75 (0.18‐3.11) |
| Nonambulatory | 114 (54%) | 90 (59%) | 24 (41%) | 2.02 (1.09‐3.74) |
| Dependence on technologya | ||||
| Feeding tube | 89 (41.6%) | 66 (43%) | 23 (39%) | 1.16 (0.63‐2.14) |
| Baclofen pump | 20 (9.3%) | 18 (12%) | 2 (3%) | 3.74 (0.84‐16.67) |
| Ventriculoperitoneal shunt | 24 (11.2%) | 18 (12%) | 6 (10%) | 1.16 (0.44‐3.08) |
| Vagal nerve stimulator/deep brain stimulator | 8 (3.7%) | 6 (4%) | 2 (3%) | 1.15 (0.22‐5.85) |
| Tracheostomy | 13 (6.1%) | 9 (6%) | 4 (7%) | 0.85 (0.25‐2.86) |
| Home mechanical ventilation (not BiPAP) | 6 (2.8%) | 5 (3%) | 1 (2%) | 1.93 (0.22‐16.90) |
| Home oxygen, BiPAP, or CPAP | 25 (11.7%) | 22 (14%) | 3 (5%) | 3.09 (0.89‐10.73) |
| Seizure disorder | 70 (33%) | 59 (38%) | 11 (19%) | 2.68 (1.29‐5.57) |
| Significant GI comorbidity | 102 (48%) | 86 (55%) | 16 (27%) | 3.35 (1.74‐6.45) |
| Significant cardiac comorbidity | 37 (17.3%) | 26 (17%) | 11 (19%) | 0.88 (0.40‐1.92) |
| Significant pulmonary comorbidity | 78 (36.4%) | 57 (37%) | 21 (36%) | 1.05 (0.56‐1.97) |
DISCUSSION
This is the first large study to examine the role of the pediatric hospitalist in preoperative evaluation of complex surgical patients. Our program developed as an evolution of a postoperative program that we have described previously.[10] The postoperative component of our comanagement program began in 2003, and the preoperative aspect was added in 2009. We believe that the preoperative component to our program contributed in some degree to the decrease in utilization of certain aspects of postoperative care over time such as parenteral nutrition. This change may have occurred because of improved bowel management perioperatively, for instance. Although the preoperative hospitalist evaluation program was instituted by our hospital administration, we felt a preoperative hospitalist evaluation represented a standardized, comprehensive way to evaluate patients before surgery. By 2009, the hospitalists at our hospital had already developed some expertise in managing patients after undergoing spinal fusion surgery.
The fact that hospitalists made recommendations for changes in medications, nutritional management, or diagnostic tests at such a high rate (72%) is interesting. We were not surprised by this finding based on anecdotal evidence because we feel that many of these patients may receive somewhat fragmented care because they often see multiple medical specialists. The high rate of interventions noted in our study may result from the fact that hospitalists who comanage these patients frequently after spinal fusion surgery were attempting to prevent postoperative complications that they see after this type of surgery. Many pediatric hospitalists have developed significant experience in caring for medically complex children and thus may feel more comfortable making preoperative recommendations than other general pediatricians.
We were not surprised to find that hospitalists made preoperative recommendations more frequently in children who had seizures, significant GI comorbidity, and who were nonambulatory. We also noted a statistically significant increased rate of recommendations when patients were on more preoperative medications. We believe that these variables suggest a population that is more medically complex. The importance of selecting medically complex patients for hospitalist comanagement has been noted previously.[16] Therefore, comanagement programs looking to maximize patient benefit for a preoperative hospitalist evaluation program might limit these visits to those who are most medically complex. We found a particularly low yield in evaluation of patients with skeletal dysplasia for example and may discontinue seeing these patients preoperatively.
We found the lack of statistically significant change in rate of hospitalist recommendations among patients with cardiac and pulmonary comorbidities interesting. Whether this was related to the mandatory preoperative pulmonology and cardiology visits is not certain. We hope to study the impact of these preoperative visits in the future as we continue to evaluate our perioperative program.
Several limitations of this study deserve note. This study was performed at 1 institution with 1 group of hospitalists and 1 group of orthopedic surgeons. Two of the study authors (D.R. and D.P.) were among the hospitalists involved with the clinical program. The study was retrospective and nonrandomized. We did not contact primary care physicians as a rule for further information about these patients. In this study, we did not specifically study the impact of hospitalist preoperative evaluations on postoperative outcomes, although the preoperative component represented an important aspect of the more systematic intervention described elsewhere.[10]
CONCLUSIONS
A preoperative program for pediatric hospitalists to see children in anticipation of spinal surgery for neuromuscular scoliosis leads to a high rate of recommendations for changes in medical management or diagnostic evaluation. Certain patient characteristics are more highly associated with hospitalists making these recommendations prior to surgery.
- 2012 State of Hospital Medicine Report, Society of Hospital Medicine. Further information available at: http://www.hospitalmedicine.org/survey.
- , , , et al.; Hospitalist‐Orthopedic Team Trial Investigators. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28–38.
- , , , et al. Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma. 2006;20(3):172–178, discussion 179–180.
- , , , et al. Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med. 2005;165(7):796–801.
- , , . Hospitalist care of the medically complex child. Pediatr Clin North Am. 2005;52(4):1165–1167.
- , , , et al. Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126(4):638–646.
- , , , et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655.
- , , , et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–538.
- , , , et al. Pediatric hospitalist comanagement of spinal fusion surgery patients. J Hosp Med. 2007;2:23–30.
- , , , et al. Outcomes and costs associated with hospitalist comanagement of medically complex children undergoing spinal fusion surgery. Hosp Pediatr. 2013;3(3):233–241.
- , , , et al. Perioperative processes and outcomes after implementation of a hospitalist‐run preoperative clinic. J Hosp Med. 2012 7:697–701.
- , , , , . Outcomes and processes of care related to preoperative medical consultation. Arch Intern Med. 2010;170(15):1365–1374.
- , , , et al. Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med. 2007;167(21):2338–2344.
- , , , et al. Standardizing care for high‐risk patients in spine surgery: the Northwestern High‐Risk Spine Protocol. Spine. 2010;35(25):2232–2238.
- , , , . Neuromuscular scoliosis: clinical evaluation pre‐ and postoperative. J Pediatr Orthop. 2000;9:217–220.
- . Just because you can, doesn't mean that you should: a call for the rational application of hospitalist comanagement. J Hosp Med. 2008:3:398–402.
- 2012 State of Hospital Medicine Report, Society of Hospital Medicine. Further information available at: http://www.hospitalmedicine.org/survey.
- , , , et al.; Hospitalist‐Orthopedic Team Trial Investigators. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28–38.
- , , , et al. Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma. 2006;20(3):172–178, discussion 179–180.
- , , , et al. Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med. 2005;165(7):796–801.
- , , . Hospitalist care of the medically complex child. Pediatr Clin North Am. 2005;52(4):1165–1167.
- , , , et al. Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126(4):638–646.
- , , , et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655.
- , , , et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–538.
- , , , et al. Pediatric hospitalist comanagement of spinal fusion surgery patients. J Hosp Med. 2007;2:23–30.
- , , , et al. Outcomes and costs associated with hospitalist comanagement of medically complex children undergoing spinal fusion surgery. Hosp Pediatr. 2013;3(3):233–241.
- , , , et al. Perioperative processes and outcomes after implementation of a hospitalist‐run preoperative clinic. J Hosp Med. 2012 7:697–701.
- , , , , . Outcomes and processes of care related to preoperative medical consultation. Arch Intern Med. 2010;170(15):1365–1374.
- , , , et al. Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med. 2007;167(21):2338–2344.
- , , , et al. Standardizing care for high‐risk patients in spine surgery: the Northwestern High‐Risk Spine Protocol. Spine. 2010;35(25):2232–2238.
- , , , . Neuromuscular scoliosis: clinical evaluation pre‐ and postoperative. J Pediatr Orthop. 2000;9:217–220.
- . Just because you can, doesn't mean that you should: a call for the rational application of hospitalist comanagement. J Hosp Med. 2008:3:398–402.
© 2013 Society of Hospital Medicine
Face Sheet and Provider Identification
Acute illness requiring hospitalization can be overwhelming for children and their families who are coping with illness and the synthesis of information from a variety of healthcare providers.[1] Patient and family centeredness is endorsed by the Institute of Medicine and the American Academy of Pediatrics[2, 3] as central to quality healthcare. In academic institutions, the presence of medical students and residents adds to the number of providers families encounter. In July 2011, the Accreditation Council for Graduate Medical Education implemented new duty hour restrictions, limiting first year residents to a maximum of 16 hour shifts.[4] Consequently, caregivers and patients may be in contact with more healthcare providers; this fractured care may confuse patients and caregivers, and increase dissatisfaction with care.[5]
The primary objective of our study was to determine the effect of a face sheet tool on the percentage of medical team members correctly identified by caregivers. The secondary objective was to determine the effect of a face sheet tool on the evaluation and satisfaction rating of the medical team by caregivers. We hypothesized that caregivers who receive the face sheet tool will correctly identify a greater percentage of team members by name and role and have higher overall satisfaction with their hospital stay.
METHODS
We performed a prospective controlled study on 2 general pediatric units at Cincinnati Children's Hospital Medical Center (CCHMC). Patients on the intervention unit received the face sheet tool, whereas the concurrent control unit maintained usual procedures. Both units have 24 beds and care for general pediatric patients primarily covered by 4 resident teams and the hospital medicine faculty. Two paired resident teams composed of 2 senior residents, 3 to 4 interns, and 4 medical students primarily admit to each general pediatric unit. Team members rotate through day and night shifts. All employees and rotating students are required to wear the hospital issued identification badge that includes their names, photos, credentials, and role. The study was conducted from November 1, 2011 to November 30, 2011.
Included patients were admitted to the study units by the usual protocol at our hospital, in which nurse patient‐flow coordinators determine bed assignments. We excluded families whose children had an inpatient hospital stay of 12 hours and families who did not speak English. All patient families scheduled to be discharged later in the day on weekday mornings from the 2 study units were approached for study participation. Families were not compensated for their participation.
A face sheet tool, which is a sheet of paper with pictures and names of the intervention team attendings, senior residents, interns, and medical students as well as a description of team member roles, was distributed to patients and their caregivers. The face sheet tools were created using Microsoft Publisher (Microsoft Corp., Redmond, WA). Neither families nor providers were blinded to the intervention, and the residents assumed responsibility for introducing the face sheet tool to families.
For our primary outcome measure, the research coordinator asked participating caregivers to match provider photographs with names and roles by placing laminated pictures backed with Velcro tape in the appropriate position on a laminated poster sheet. Initially, we collected overall accuracy of identification by name and role. In the second week, we began collecting specific data on the attending physician.
The satisfaction survey consisted of the American Board of Internal Medicine (ABIM) patient satisfaction questionnaire, composed of 10, 5‐point Likert scale questions,[6, 7] and an overall rating of hospital question, On a scale from 1 to 10, with 1 being the worst possible hospital and 10 being the best possible hospital, what number would you rate this hospital? from the Hospital Consumer Assessment of Health Plans Survey.[8] Questions were asked aloud and families responded to the questions orally. A written list was also provided to families. We collected data on length of stay (LOS) at the time of outcome assessment as well as previous hospitalizations.
Data Analysis
Differences between the intervention and control groups for relationship of survey respondent to child, prior hospitalization, and LOS were evaluated using the Fisher exact, 2, and 2‐sample t test, respectively. Hospital LOS was log‐transformed prior to analysis. The effect of the face sheet tool was evaluated by analyzing the differences between the intervention and control groups in the proportion of correctly identified names and roles using the Wilcoxon rank sum test and using the Fisher exact test for attending identification. Skewed Likert scale satisfaction ratings and overall hospital ratings were dichotomized at the highest score possible and analyzed using the 2 test. An analysis adjusting for prior hospitalization and LOS was done using generalized linear models, with a Poisson link for the number of correctly identified names/roles and an offset for the number of names/roles given.
Our research was reviewed by the CCHMC institutional review board and deemed exempt.
RESULTS
A total of 96 families were approached for enrollment (50 in the intervention and 46 in the control). Of these, 86 families agreed to participate. Three families in the intervention group did not receive the face sheet tool and were excluded from analysis, leaving an analytic cohort of 83 (41 in intervention and 42 in control). Attending recognition by role was collected from 54 families (28 in intervention group and 26 in control group) and by name from 34 families (15 in intervention group and 19 in control group). Table 1 displays characteristics of each group. Among the 83 study participants, LOS at time of outcome assessment ranged from 0.4 to 12.0 days, and the number of medical team members that cared for these patients ranged from 3 to 14.
| Intervention, n=41 | Control, n=42 | P Valuea | |
|---|---|---|---|
| |||
| Relationship to patient | 0.67 | ||
| Mother | 33 (80%) | 35 (83%) | |
| Father | 5 (12%) | 6 (14%) | |
| Grandmother/legal guardian | 3 (7%) | 1 (2%) | |
| Prior hospitalization, yes | 12 (29%) | 24 (57%) | 0.01 |
| Length of stay (days) | 1.07 (0.861.34) | 1.32 (1.051.67) | 0.20 |
Families in the intervention group had a higher percentage of correctly identified members of the medical team by name and role as compared to the control group (Table 2). These findings remained significant after adjusting for LOS and prior hospitalization. In addition, in a subset of families with attending data available, more families accurately identified attending name and attending role in the intervention as compared to control group.
| Intervention | Control | P Valuea | |
|---|---|---|---|
| |||
| Medical team, proportion correctly identified: | N=41 | N=41 | |
| Medical team names | 25% (14, 58) | 11% (0, 25) | 0.01b |
| Medical team roles | 50% (37, 67) | 25% (12, 44) | 0.01b |
| Attending, correctly identified: | |||
| Attending's name | N=15 | N=19 | |
| 14 (93%), | 10 (53%), | 0.02c | |
| Attending's role | N=28 | N=26 | |
| 26 (93%) | 16 (62%) | 0.01 | |
| Patient satisfaction, best possible score for: | N=41 | N=42 | |
| Q1: Telling you everything, being truthful | 21 (51%) | 21 (50%) | 0.91 |
| Q2: Greeting you warmly, being friendly | 26 (63%) | 25 (60%) | 0.72 |
| Q3: Treating you like you're on the same level | 29 (71%) | 25 (60%) | 0.28 |
| Q4: Letting you tell your story, listening | 27 (66%) | 23 (55%) | 0.30 |
| Q5: Showing interest in you as a person | 26 (63%) | 23 (55%) | 0.42 |
| Q6: Warning your child during the physical exam | 21 (51%) | 21 (50%) | 0.91 |
| Q7: Discussing options, asking your opinion | 20 (49%) | 17 (40%) | 0.45 |
| Q8: Encouraging questions, answering clearly | 23 (56%) | 19 (45%) | 0.32 |
| Q9: Explaining what you need to know | 22 (54%) | 18 (43%) | 0.32 |
| Q10: Using words you can understand | 26 (63%) | 18 (43%) | 0.06 |
| Overall hospital rating | 27 (66%) | 26 (62%) | 0.71 |
No significant differences were noted between the groups when comparing all individual ABIM survey question scores or the overall hospital satisfaction rating (Table 2). Scores in both intervention and control groups were high in all categories.
DISCUSSION
Caregivers given the face sheet tool were better able to identify medical team members by name and role than caregivers in the control group. Previous studies have shown similar results.[9, 10] Families encountered a large number of providers (median of 8) during stays that were on average quite brief (median LOS of 23.6 hours). Despite the significant increase in caregivers' ability to identify providers, the effect was modest.
Our findings add to prior work on face sheet tools in pediatrics and internal medicine.[9, 10, 11] Our study occurred after the residency duty hour restrictions. We described the high number of providers that families encounter in this context. It is the first study to our knowledge to quantify the number of providers that families encounter after these changes and to report on how well families can identify these clinicians by name and role. Unlike other studies, satisfaction scores were not improved.[9] Potential reasons for this include: (1) caregiver knowledge of 2 to 4 key members of the team and not the whole team may be the primary driver of satisfaction, (2) caregiver activation or empowerment may be a more responsive measure than overall satisfaction, and (3) our satisfaction measures may have ceiling effects and/or be elevated in both groups by social desirability bias.
Our study highlights the need for further investigation of quality outcomes associated with residency work hour changes.[12, 13, 14] Specifically, exposure to large numbers of providers may hinder families from accurately identifying those entrusted with the care of their loved one. Of note, our research coordinator needed to present as many as 14 provider pictures to 1 family with a hospital stay of 24 hours. Large numbers of providers may create challenges in building rapport, ensuring effective communication and developing trust with families. We chose to evaluate identification of each team member by caregivers; our findings are suggestive of the need for alternative strategies. A more valuable intervention might target identification of key team members (eg, attending, primary intern, primary senior resident). A policy statement regarding transitions of care recommended the establishment of mechanisms to ensure patients and their families know who is responsible for their care.[15] Efforts toward achieving this goal are essential.
This study has several limitations. The study was completed at a single institution, and thus generalizability may be limited. Although the intervention and control units have similar characteristics, randomization did not occur at the patient level. The control group had significantly more patients who had greater than 1 admission compared to the intervention group. Patients enrolled in the study were from a weekday convenience sample; therefore, potential differences in results based on weekend admissions were unable to be assessed. The exclusion of nonEnglish‐speaking families could limit generalizability to this population. Social desirability bias may have elevated the scores in both groups. Providers tasked with the responsibility of introducing the face sheet tool to families did so in a nonstandardized way and may have interacted differently with families compared to the control team. Finally, our project's aim was focused on the effect of a face sheet tool on the identification and satisfaction rating of the medical team by caregivers. Truly family‐centered care would include efforts to improve families' knowledge of and satisfaction with all members of the healthcare team.
A photo‐based face sheet tool helped caregivers better identify their child's care providers by name and role in the hospital. Satisfaction scores were similar in both groups.
Acknowledgements
The authors thank the Pediatric Research in Inpatient Settings network, and specifically Drs. Karen Wilson and Samir Shah, for their assistance during a workshop at the Pediatric Hospital Medicine 2012 meeting in July 2012, during which a first draft of this manuscript was produced.
Disclosure: Nothing to report.
- , , , , . A child's admission to hospital: a qualitative study examining the experiences of parents. Intensive Care Med. 2005;31(9):1248–1254.
- Committee on Quality of Health Care in America. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
- Committee on Hospital Care and Institute for Patient‐ and Family‐Centered Care. Patient‐ and family‐centered care and the pediatrician's role. Pediatrics. 2012;129(2):394–404.
- , , . The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3.
- , , , . Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83(3):292–297.
- PSQ Project Co‐Investigators. Final Report on the Patient Satisfaction Questionnaire Project. Philadelphia, PA: American Board of Internal Medicine; 1989.
- , , , et al. Effect of multisource feedback on resident communication skills and professionalism: a randomized controlled trial. Arch Pediatr Adolesc Med. 2007;161(1):44–49.
- , , , , . Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev. 2010;67(1):27–37.
- , , , . PHACES (Photographs of Academic Clinicians and Their Educational Status): a tool to improve delivery of family‐centered care. Acad Pediatr. 2010;10(2):138–145.
- , , , et al. Improving inpatients' identification of their doctors: use of FACE cards. Jt Comm J Qual Patient Saf. 2009;35(12):613–619.
- , . “Don't call me ‘mom’: how parents want to be greeted by their pediatrician. Clin Pediatr. 2009;48(7):720–722.
- , , , , , . Better rested, but more stressed? Evidence of the effects of resident work hour restrictions. Acad Pediatr. 2012;12(4):335–343.
- , , , et al. Pediatric residents' perspectives on reducing work hours and lengthening residency: a national survey. Pediatrics. 2012;130(1):99–107.
- , , , . Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist. J Hosp Med. 2012;7(4):299–303.
- , , , et al. Transitions of Care Consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, and Society for Academic Emergency Medicine. J Hosp Med. 2009;4(6):364–370.
Acute illness requiring hospitalization can be overwhelming for children and their families who are coping with illness and the synthesis of information from a variety of healthcare providers.[1] Patient and family centeredness is endorsed by the Institute of Medicine and the American Academy of Pediatrics[2, 3] as central to quality healthcare. In academic institutions, the presence of medical students and residents adds to the number of providers families encounter. In July 2011, the Accreditation Council for Graduate Medical Education implemented new duty hour restrictions, limiting first year residents to a maximum of 16 hour shifts.[4] Consequently, caregivers and patients may be in contact with more healthcare providers; this fractured care may confuse patients and caregivers, and increase dissatisfaction with care.[5]
The primary objective of our study was to determine the effect of a face sheet tool on the percentage of medical team members correctly identified by caregivers. The secondary objective was to determine the effect of a face sheet tool on the evaluation and satisfaction rating of the medical team by caregivers. We hypothesized that caregivers who receive the face sheet tool will correctly identify a greater percentage of team members by name and role and have higher overall satisfaction with their hospital stay.
METHODS
We performed a prospective controlled study on 2 general pediatric units at Cincinnati Children's Hospital Medical Center (CCHMC). Patients on the intervention unit received the face sheet tool, whereas the concurrent control unit maintained usual procedures. Both units have 24 beds and care for general pediatric patients primarily covered by 4 resident teams and the hospital medicine faculty. Two paired resident teams composed of 2 senior residents, 3 to 4 interns, and 4 medical students primarily admit to each general pediatric unit. Team members rotate through day and night shifts. All employees and rotating students are required to wear the hospital issued identification badge that includes their names, photos, credentials, and role. The study was conducted from November 1, 2011 to November 30, 2011.
Included patients were admitted to the study units by the usual protocol at our hospital, in which nurse patient‐flow coordinators determine bed assignments. We excluded families whose children had an inpatient hospital stay of 12 hours and families who did not speak English. All patient families scheduled to be discharged later in the day on weekday mornings from the 2 study units were approached for study participation. Families were not compensated for their participation.
A face sheet tool, which is a sheet of paper with pictures and names of the intervention team attendings, senior residents, interns, and medical students as well as a description of team member roles, was distributed to patients and their caregivers. The face sheet tools were created using Microsoft Publisher (Microsoft Corp., Redmond, WA). Neither families nor providers were blinded to the intervention, and the residents assumed responsibility for introducing the face sheet tool to families.
For our primary outcome measure, the research coordinator asked participating caregivers to match provider photographs with names and roles by placing laminated pictures backed with Velcro tape in the appropriate position on a laminated poster sheet. Initially, we collected overall accuracy of identification by name and role. In the second week, we began collecting specific data on the attending physician.
The satisfaction survey consisted of the American Board of Internal Medicine (ABIM) patient satisfaction questionnaire, composed of 10, 5‐point Likert scale questions,[6, 7] and an overall rating of hospital question, On a scale from 1 to 10, with 1 being the worst possible hospital and 10 being the best possible hospital, what number would you rate this hospital? from the Hospital Consumer Assessment of Health Plans Survey.[8] Questions were asked aloud and families responded to the questions orally. A written list was also provided to families. We collected data on length of stay (LOS) at the time of outcome assessment as well as previous hospitalizations.
Data Analysis
Differences between the intervention and control groups for relationship of survey respondent to child, prior hospitalization, and LOS were evaluated using the Fisher exact, 2, and 2‐sample t test, respectively. Hospital LOS was log‐transformed prior to analysis. The effect of the face sheet tool was evaluated by analyzing the differences between the intervention and control groups in the proportion of correctly identified names and roles using the Wilcoxon rank sum test and using the Fisher exact test for attending identification. Skewed Likert scale satisfaction ratings and overall hospital ratings were dichotomized at the highest score possible and analyzed using the 2 test. An analysis adjusting for prior hospitalization and LOS was done using generalized linear models, with a Poisson link for the number of correctly identified names/roles and an offset for the number of names/roles given.
Our research was reviewed by the CCHMC institutional review board and deemed exempt.
RESULTS
A total of 96 families were approached for enrollment (50 in the intervention and 46 in the control). Of these, 86 families agreed to participate. Three families in the intervention group did not receive the face sheet tool and were excluded from analysis, leaving an analytic cohort of 83 (41 in intervention and 42 in control). Attending recognition by role was collected from 54 families (28 in intervention group and 26 in control group) and by name from 34 families (15 in intervention group and 19 in control group). Table 1 displays characteristics of each group. Among the 83 study participants, LOS at time of outcome assessment ranged from 0.4 to 12.0 days, and the number of medical team members that cared for these patients ranged from 3 to 14.
| Intervention, n=41 | Control, n=42 | P Valuea | |
|---|---|---|---|
| |||
| Relationship to patient | 0.67 | ||
| Mother | 33 (80%) | 35 (83%) | |
| Father | 5 (12%) | 6 (14%) | |
| Grandmother/legal guardian | 3 (7%) | 1 (2%) | |
| Prior hospitalization, yes | 12 (29%) | 24 (57%) | 0.01 |
| Length of stay (days) | 1.07 (0.861.34) | 1.32 (1.051.67) | 0.20 |
Families in the intervention group had a higher percentage of correctly identified members of the medical team by name and role as compared to the control group (Table 2). These findings remained significant after adjusting for LOS and prior hospitalization. In addition, in a subset of families with attending data available, more families accurately identified attending name and attending role in the intervention as compared to control group.
| Intervention | Control | P Valuea | |
|---|---|---|---|
| |||
| Medical team, proportion correctly identified: | N=41 | N=41 | |
| Medical team names | 25% (14, 58) | 11% (0, 25) | 0.01b |
| Medical team roles | 50% (37, 67) | 25% (12, 44) | 0.01b |
| Attending, correctly identified: | |||
| Attending's name | N=15 | N=19 | |
| 14 (93%), | 10 (53%), | 0.02c | |
| Attending's role | N=28 | N=26 | |
| 26 (93%) | 16 (62%) | 0.01 | |
| Patient satisfaction, best possible score for: | N=41 | N=42 | |
| Q1: Telling you everything, being truthful | 21 (51%) | 21 (50%) | 0.91 |
| Q2: Greeting you warmly, being friendly | 26 (63%) | 25 (60%) | 0.72 |
| Q3: Treating you like you're on the same level | 29 (71%) | 25 (60%) | 0.28 |
| Q4: Letting you tell your story, listening | 27 (66%) | 23 (55%) | 0.30 |
| Q5: Showing interest in you as a person | 26 (63%) | 23 (55%) | 0.42 |
| Q6: Warning your child during the physical exam | 21 (51%) | 21 (50%) | 0.91 |
| Q7: Discussing options, asking your opinion | 20 (49%) | 17 (40%) | 0.45 |
| Q8: Encouraging questions, answering clearly | 23 (56%) | 19 (45%) | 0.32 |
| Q9: Explaining what you need to know | 22 (54%) | 18 (43%) | 0.32 |
| Q10: Using words you can understand | 26 (63%) | 18 (43%) | 0.06 |
| Overall hospital rating | 27 (66%) | 26 (62%) | 0.71 |
No significant differences were noted between the groups when comparing all individual ABIM survey question scores or the overall hospital satisfaction rating (Table 2). Scores in both intervention and control groups were high in all categories.
DISCUSSION
Caregivers given the face sheet tool were better able to identify medical team members by name and role than caregivers in the control group. Previous studies have shown similar results.[9, 10] Families encountered a large number of providers (median of 8) during stays that were on average quite brief (median LOS of 23.6 hours). Despite the significant increase in caregivers' ability to identify providers, the effect was modest.
Our findings add to prior work on face sheet tools in pediatrics and internal medicine.[9, 10, 11] Our study occurred after the residency duty hour restrictions. We described the high number of providers that families encounter in this context. It is the first study to our knowledge to quantify the number of providers that families encounter after these changes and to report on how well families can identify these clinicians by name and role. Unlike other studies, satisfaction scores were not improved.[9] Potential reasons for this include: (1) caregiver knowledge of 2 to 4 key members of the team and not the whole team may be the primary driver of satisfaction, (2) caregiver activation or empowerment may be a more responsive measure than overall satisfaction, and (3) our satisfaction measures may have ceiling effects and/or be elevated in both groups by social desirability bias.
Our study highlights the need for further investigation of quality outcomes associated with residency work hour changes.[12, 13, 14] Specifically, exposure to large numbers of providers may hinder families from accurately identifying those entrusted with the care of their loved one. Of note, our research coordinator needed to present as many as 14 provider pictures to 1 family with a hospital stay of 24 hours. Large numbers of providers may create challenges in building rapport, ensuring effective communication and developing trust with families. We chose to evaluate identification of each team member by caregivers; our findings are suggestive of the need for alternative strategies. A more valuable intervention might target identification of key team members (eg, attending, primary intern, primary senior resident). A policy statement regarding transitions of care recommended the establishment of mechanisms to ensure patients and their families know who is responsible for their care.[15] Efforts toward achieving this goal are essential.
This study has several limitations. The study was completed at a single institution, and thus generalizability may be limited. Although the intervention and control units have similar characteristics, randomization did not occur at the patient level. The control group had significantly more patients who had greater than 1 admission compared to the intervention group. Patients enrolled in the study were from a weekday convenience sample; therefore, potential differences in results based on weekend admissions were unable to be assessed. The exclusion of nonEnglish‐speaking families could limit generalizability to this population. Social desirability bias may have elevated the scores in both groups. Providers tasked with the responsibility of introducing the face sheet tool to families did so in a nonstandardized way and may have interacted differently with families compared to the control team. Finally, our project's aim was focused on the effect of a face sheet tool on the identification and satisfaction rating of the medical team by caregivers. Truly family‐centered care would include efforts to improve families' knowledge of and satisfaction with all members of the healthcare team.
A photo‐based face sheet tool helped caregivers better identify their child's care providers by name and role in the hospital. Satisfaction scores were similar in both groups.
Acknowledgements
The authors thank the Pediatric Research in Inpatient Settings network, and specifically Drs. Karen Wilson and Samir Shah, for their assistance during a workshop at the Pediatric Hospital Medicine 2012 meeting in July 2012, during which a first draft of this manuscript was produced.
Disclosure: Nothing to report.
Acute illness requiring hospitalization can be overwhelming for children and their families who are coping with illness and the synthesis of information from a variety of healthcare providers.[1] Patient and family centeredness is endorsed by the Institute of Medicine and the American Academy of Pediatrics[2, 3] as central to quality healthcare. In academic institutions, the presence of medical students and residents adds to the number of providers families encounter. In July 2011, the Accreditation Council for Graduate Medical Education implemented new duty hour restrictions, limiting first year residents to a maximum of 16 hour shifts.[4] Consequently, caregivers and patients may be in contact with more healthcare providers; this fractured care may confuse patients and caregivers, and increase dissatisfaction with care.[5]
The primary objective of our study was to determine the effect of a face sheet tool on the percentage of medical team members correctly identified by caregivers. The secondary objective was to determine the effect of a face sheet tool on the evaluation and satisfaction rating of the medical team by caregivers. We hypothesized that caregivers who receive the face sheet tool will correctly identify a greater percentage of team members by name and role and have higher overall satisfaction with their hospital stay.
METHODS
We performed a prospective controlled study on 2 general pediatric units at Cincinnati Children's Hospital Medical Center (CCHMC). Patients on the intervention unit received the face sheet tool, whereas the concurrent control unit maintained usual procedures. Both units have 24 beds and care for general pediatric patients primarily covered by 4 resident teams and the hospital medicine faculty. Two paired resident teams composed of 2 senior residents, 3 to 4 interns, and 4 medical students primarily admit to each general pediatric unit. Team members rotate through day and night shifts. All employees and rotating students are required to wear the hospital issued identification badge that includes their names, photos, credentials, and role. The study was conducted from November 1, 2011 to November 30, 2011.
Included patients were admitted to the study units by the usual protocol at our hospital, in which nurse patient‐flow coordinators determine bed assignments. We excluded families whose children had an inpatient hospital stay of 12 hours and families who did not speak English. All patient families scheduled to be discharged later in the day on weekday mornings from the 2 study units were approached for study participation. Families were not compensated for their participation.
A face sheet tool, which is a sheet of paper with pictures and names of the intervention team attendings, senior residents, interns, and medical students as well as a description of team member roles, was distributed to patients and their caregivers. The face sheet tools were created using Microsoft Publisher (Microsoft Corp., Redmond, WA). Neither families nor providers were blinded to the intervention, and the residents assumed responsibility for introducing the face sheet tool to families.
For our primary outcome measure, the research coordinator asked participating caregivers to match provider photographs with names and roles by placing laminated pictures backed with Velcro tape in the appropriate position on a laminated poster sheet. Initially, we collected overall accuracy of identification by name and role. In the second week, we began collecting specific data on the attending physician.
The satisfaction survey consisted of the American Board of Internal Medicine (ABIM) patient satisfaction questionnaire, composed of 10, 5‐point Likert scale questions,[6, 7] and an overall rating of hospital question, On a scale from 1 to 10, with 1 being the worst possible hospital and 10 being the best possible hospital, what number would you rate this hospital? from the Hospital Consumer Assessment of Health Plans Survey.[8] Questions were asked aloud and families responded to the questions orally. A written list was also provided to families. We collected data on length of stay (LOS) at the time of outcome assessment as well as previous hospitalizations.
Data Analysis
Differences between the intervention and control groups for relationship of survey respondent to child, prior hospitalization, and LOS were evaluated using the Fisher exact, 2, and 2‐sample t test, respectively. Hospital LOS was log‐transformed prior to analysis. The effect of the face sheet tool was evaluated by analyzing the differences between the intervention and control groups in the proportion of correctly identified names and roles using the Wilcoxon rank sum test and using the Fisher exact test for attending identification. Skewed Likert scale satisfaction ratings and overall hospital ratings were dichotomized at the highest score possible and analyzed using the 2 test. An analysis adjusting for prior hospitalization and LOS was done using generalized linear models, with a Poisson link for the number of correctly identified names/roles and an offset for the number of names/roles given.
Our research was reviewed by the CCHMC institutional review board and deemed exempt.
RESULTS
A total of 96 families were approached for enrollment (50 in the intervention and 46 in the control). Of these, 86 families agreed to participate. Three families in the intervention group did not receive the face sheet tool and were excluded from analysis, leaving an analytic cohort of 83 (41 in intervention and 42 in control). Attending recognition by role was collected from 54 families (28 in intervention group and 26 in control group) and by name from 34 families (15 in intervention group and 19 in control group). Table 1 displays characteristics of each group. Among the 83 study participants, LOS at time of outcome assessment ranged from 0.4 to 12.0 days, and the number of medical team members that cared for these patients ranged from 3 to 14.
| Intervention, n=41 | Control, n=42 | P Valuea | |
|---|---|---|---|
| |||
| Relationship to patient | 0.67 | ||
| Mother | 33 (80%) | 35 (83%) | |
| Father | 5 (12%) | 6 (14%) | |
| Grandmother/legal guardian | 3 (7%) | 1 (2%) | |
| Prior hospitalization, yes | 12 (29%) | 24 (57%) | 0.01 |
| Length of stay (days) | 1.07 (0.861.34) | 1.32 (1.051.67) | 0.20 |
Families in the intervention group had a higher percentage of correctly identified members of the medical team by name and role as compared to the control group (Table 2). These findings remained significant after adjusting for LOS and prior hospitalization. In addition, in a subset of families with attending data available, more families accurately identified attending name and attending role in the intervention as compared to control group.
| Intervention | Control | P Valuea | |
|---|---|---|---|
| |||
| Medical team, proportion correctly identified: | N=41 | N=41 | |
| Medical team names | 25% (14, 58) | 11% (0, 25) | 0.01b |
| Medical team roles | 50% (37, 67) | 25% (12, 44) | 0.01b |
| Attending, correctly identified: | |||
| Attending's name | N=15 | N=19 | |
| 14 (93%), | 10 (53%), | 0.02c | |
| Attending's role | N=28 | N=26 | |
| 26 (93%) | 16 (62%) | 0.01 | |
| Patient satisfaction, best possible score for: | N=41 | N=42 | |
| Q1: Telling you everything, being truthful | 21 (51%) | 21 (50%) | 0.91 |
| Q2: Greeting you warmly, being friendly | 26 (63%) | 25 (60%) | 0.72 |
| Q3: Treating you like you're on the same level | 29 (71%) | 25 (60%) | 0.28 |
| Q4: Letting you tell your story, listening | 27 (66%) | 23 (55%) | 0.30 |
| Q5: Showing interest in you as a person | 26 (63%) | 23 (55%) | 0.42 |
| Q6: Warning your child during the physical exam | 21 (51%) | 21 (50%) | 0.91 |
| Q7: Discussing options, asking your opinion | 20 (49%) | 17 (40%) | 0.45 |
| Q8: Encouraging questions, answering clearly | 23 (56%) | 19 (45%) | 0.32 |
| Q9: Explaining what you need to know | 22 (54%) | 18 (43%) | 0.32 |
| Q10: Using words you can understand | 26 (63%) | 18 (43%) | 0.06 |
| Overall hospital rating | 27 (66%) | 26 (62%) | 0.71 |
No significant differences were noted between the groups when comparing all individual ABIM survey question scores or the overall hospital satisfaction rating (Table 2). Scores in both intervention and control groups were high in all categories.
DISCUSSION
Caregivers given the face sheet tool were better able to identify medical team members by name and role than caregivers in the control group. Previous studies have shown similar results.[9, 10] Families encountered a large number of providers (median of 8) during stays that were on average quite brief (median LOS of 23.6 hours). Despite the significant increase in caregivers' ability to identify providers, the effect was modest.
Our findings add to prior work on face sheet tools in pediatrics and internal medicine.[9, 10, 11] Our study occurred after the residency duty hour restrictions. We described the high number of providers that families encounter in this context. It is the first study to our knowledge to quantify the number of providers that families encounter after these changes and to report on how well families can identify these clinicians by name and role. Unlike other studies, satisfaction scores were not improved.[9] Potential reasons for this include: (1) caregiver knowledge of 2 to 4 key members of the team and not the whole team may be the primary driver of satisfaction, (2) caregiver activation or empowerment may be a more responsive measure than overall satisfaction, and (3) our satisfaction measures may have ceiling effects and/or be elevated in both groups by social desirability bias.
Our study highlights the need for further investigation of quality outcomes associated with residency work hour changes.[12, 13, 14] Specifically, exposure to large numbers of providers may hinder families from accurately identifying those entrusted with the care of their loved one. Of note, our research coordinator needed to present as many as 14 provider pictures to 1 family with a hospital stay of 24 hours. Large numbers of providers may create challenges in building rapport, ensuring effective communication and developing trust with families. We chose to evaluate identification of each team member by caregivers; our findings are suggestive of the need for alternative strategies. A more valuable intervention might target identification of key team members (eg, attending, primary intern, primary senior resident). A policy statement regarding transitions of care recommended the establishment of mechanisms to ensure patients and their families know who is responsible for their care.[15] Efforts toward achieving this goal are essential.
This study has several limitations. The study was completed at a single institution, and thus generalizability may be limited. Although the intervention and control units have similar characteristics, randomization did not occur at the patient level. The control group had significantly more patients who had greater than 1 admission compared to the intervention group. Patients enrolled in the study were from a weekday convenience sample; therefore, potential differences in results based on weekend admissions were unable to be assessed. The exclusion of nonEnglish‐speaking families could limit generalizability to this population. Social desirability bias may have elevated the scores in both groups. Providers tasked with the responsibility of introducing the face sheet tool to families did so in a nonstandardized way and may have interacted differently with families compared to the control team. Finally, our project's aim was focused on the effect of a face sheet tool on the identification and satisfaction rating of the medical team by caregivers. Truly family‐centered care would include efforts to improve families' knowledge of and satisfaction with all members of the healthcare team.
A photo‐based face sheet tool helped caregivers better identify their child's care providers by name and role in the hospital. Satisfaction scores were similar in both groups.
Acknowledgements
The authors thank the Pediatric Research in Inpatient Settings network, and specifically Drs. Karen Wilson and Samir Shah, for their assistance during a workshop at the Pediatric Hospital Medicine 2012 meeting in July 2012, during which a first draft of this manuscript was produced.
Disclosure: Nothing to report.
- , , , , . A child's admission to hospital: a qualitative study examining the experiences of parents. Intensive Care Med. 2005;31(9):1248–1254.
- Committee on Quality of Health Care in America. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
- Committee on Hospital Care and Institute for Patient‐ and Family‐Centered Care. Patient‐ and family‐centered care and the pediatrician's role. Pediatrics. 2012;129(2):394–404.
- , , . The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3.
- , , , . Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83(3):292–297.
- PSQ Project Co‐Investigators. Final Report on the Patient Satisfaction Questionnaire Project. Philadelphia, PA: American Board of Internal Medicine; 1989.
- , , , et al. Effect of multisource feedback on resident communication skills and professionalism: a randomized controlled trial. Arch Pediatr Adolesc Med. 2007;161(1):44–49.
- , , , , . Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev. 2010;67(1):27–37.
- , , , . PHACES (Photographs of Academic Clinicians and Their Educational Status): a tool to improve delivery of family‐centered care. Acad Pediatr. 2010;10(2):138–145.
- , , , et al. Improving inpatients' identification of their doctors: use of FACE cards. Jt Comm J Qual Patient Saf. 2009;35(12):613–619.
- , . “Don't call me ‘mom’: how parents want to be greeted by their pediatrician. Clin Pediatr. 2009;48(7):720–722.
- , , , , , . Better rested, but more stressed? Evidence of the effects of resident work hour restrictions. Acad Pediatr. 2012;12(4):335–343.
- , , , et al. Pediatric residents' perspectives on reducing work hours and lengthening residency: a national survey. Pediatrics. 2012;130(1):99–107.
- , , , . Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist. J Hosp Med. 2012;7(4):299–303.
- , , , et al. Transitions of Care Consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, and Society for Academic Emergency Medicine. J Hosp Med. 2009;4(6):364–370.
- , , , , . A child's admission to hospital: a qualitative study examining the experiences of parents. Intensive Care Med. 2005;31(9):1248–1254.
- Committee on Quality of Health Care in America. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
- Committee on Hospital Care and Institute for Patient‐ and Family‐Centered Care. Patient‐ and family‐centered care and the pediatrician's role. Pediatrics. 2012;129(2):394–404.
- , , . The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3.
- , , , . Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83(3):292–297.
- PSQ Project Co‐Investigators. Final Report on the Patient Satisfaction Questionnaire Project. Philadelphia, PA: American Board of Internal Medicine; 1989.
- , , , et al. Effect of multisource feedback on resident communication skills and professionalism: a randomized controlled trial. Arch Pediatr Adolesc Med. 2007;161(1):44–49.
- , , , , . Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev. 2010;67(1):27–37.
- , , , . PHACES (Photographs of Academic Clinicians and Their Educational Status): a tool to improve delivery of family‐centered care. Acad Pediatr. 2010;10(2):138–145.
- , , , et al. Improving inpatients' identification of their doctors: use of FACE cards. Jt Comm J Qual Patient Saf. 2009;35(12):613–619.
- , . “Don't call me ‘mom’: how parents want to be greeted by their pediatrician. Clin Pediatr. 2009;48(7):720–722.
- , , , , , . Better rested, but more stressed? Evidence of the effects of resident work hour restrictions. Acad Pediatr. 2012;12(4):335–343.
- , , , et al. Pediatric residents' perspectives on reducing work hours and lengthening residency: a national survey. Pediatrics. 2012;130(1):99–107.
- , , , . Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist. J Hosp Med. 2012;7(4):299–303.
- , , , et al. Transitions of Care Consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, and Society for Academic Emergency Medicine. J Hosp Med. 2009;4(6):364–370.
IVC Ultrasound Imaging Training
The use of hand‐carried ultrasound by nonspecialists is increasing. Of particular interest to hospitalists is bedside ultrasound assessment of the inferior vena cava (IVC), which more accurately estimates left atrial pressure than does assessment of jugular venous pressure by physical examination.[1] Invasively measured central venous pressure (CVP) also correlates closely with estimates from IVC imaging.[1, 2, 3, 4] Although quick, accurate bedside determination of CVP may have broad potential applications in hospital medicine,[5, 6, 7, 8] of particular interest to patients and their advocates is whether hospitalists are sufficiently skilled to perform this procedure. Lucas et al. found that 8 hospitalists trained to perform 6 cardiac assessments by hand‐carried ultrasound could identify an enlarged IVC with moderate accuracy (sensitivity 56%, specificity 86%).[9] To our knowledge, no other study has examined whether hospitalists can readily develop the skills to accurately assess the IVC by ultrasound. We therefore studied whether the skills needed to acquire and interpret IVC images by ultrasound could be acquired by hospitalists after a brief training program.
METHODS
Study Populations
Hospitalists and volunteer subjects both provided informed consent to participate in this study, which was approved by the Johns Hopkins University School of Medicine Institutional Review Board. Nonpregnant volunteer subjects at least 18 years of age who agreed to attend training sessions were solicited from the investigators' ambulatory clinic patient population (see Supporting Information, Appendix A, in the online version of this article) and were compensated for their time. Volunteer subjects were solicited to represent a range of cardiac pathology. Hospitalists were solicited from among 28 members of the Johns Hopkins Bayview Medical Center's Division of Hospital Medicine, a nationally renowned academic hospitalist program comprising tenure‐track faculty who dedicate at least 30% of their time to academic endeavors.
Image Acquisition and Interpretation
A pocket‐sized portable hand‐carried ultrasound device was used for all IVC images (Vscan; GE Healthcare, Milwaukee, WI). All IVC images were acquired using the conventional methods with a subcostal view while the patient is supine. Cine loops of the IVC with respiration were captured in the longitudinal axis. Diameters were obtained approximately and by convention, approximately 2 cm from the IVC and right atrial junction. The IVC minimum diameter was measured during a cine loop of a patient performing a nasal sniff. The IVC collapsibility was determined by the formula: IVC Collapsibility Index=(IVCmaxIVCmin/IVCmax), where IVCmax and IVCmin represent the maximum and minimum IVC diameters respectively.[2] The IVC maximum diameters and collapsibility measurements that were used to estimate CVP are shown in the Supporting Information, Appendix B, in the online version of this article.
Educational Intervention and Skills Performance Assessment
One to 2 days prior to the in‐person training session, hospitalists were provided a brief introductory online curriculum (see Supporting Information, Appendix B, in the online version of this article). Groups of 3 to 4 hospitalists then completed an in‐person training and testing session (7 hours total time), which consisted of a precourse survey, a didactic session, and up to 4 hours of practice time with 10 volunteer subjects supervised by an experienced board‐certified cardiologist (G.A.H.) and a research echocardiography technician (C.M.). The survey included details on medical training, years in practice, prior ultrasound experience, and confidence in obtaining and interpreting IVC images. Confidence was rated on a Likert scale from 1=strongly confident to 5=not confident (3=neutral).
Next, each hospitalist's skills were assessed on 5 volunteer subjects selected by the cardiologist to represent a range of IVC appearance and body mass index (BMI). After appropriately identifying the IVC, they were first asked to make a visual qualitative judgement whether the IVC collapsed more than 50% during rapid inspiration or a sniff maneuver. Then hospitalists measured IVC diameter in a longitudinal view and calculated IVC collapsibility. Performance was evaluated by an experienced cardiologist (G.A.H.), who directly observed each hospitalist acquire and interpret IVC images and judged them relative to his own hand‐carried ultrasound assessments on the same subjects performed just before the hospitalists' scans. For each volunteer imaged, hospitalists had to acquire a technically adequate image of the IVC and correctly measure the inspiratory and expiratory IVC diameters. Hospitalists then had to estimate CVP by interpreting IVC diameters and collapsibility in 10 previously acquired sets of IVC video and still images. First, the hospitalists performed visual IVC collapsibility assessments (IVC collapse more than 50%) of video clips showing IVC appearance at baseline and during a rapid inspiration or sniff, without any measurements provided. Then, using still images showing premeasured maximum and minimum IVC diameters, they estimated CVP based on calculating IVC collapsibility (see Supporting Information, Appendix B, in the online version of this article for correlation of CVP to IVC maximum diameter and collapsibility). At the end of initial training hospitalists were again surveyed on confidence and also rated level of agreement (Likert scale, 1=strongly agree to 5=strongly disagree) regarding their ability to adequately obtain and accurately interpret IVC images and measurements. The post‐training survey also reviewed the training curriculum and asked hospitalists to identify potential barriers to clinical use of IVC ultrasound.
Following initial training, hospitalists were provided with a hand‐carried ultrasound device and allowed to use the device for IVC imaging on their general medical inpatients; the hospitalists could access the research echocardiography technician (C.M.) for assistance if desired. The number of additional patients imaged and whether scans were assisted was recorded for the study. At least 6 weeks after initial training, the hospitalists' IVC image acquisition and interpretation skills were again assessed on 5 volunteer subjects. At the follow‐up assessment, 4 of the 5 volunteers were new volunteers compared to the hospitalists' initial skills testing.
Statistics
The mean and standard deviations were used to describe continuous variables and percentages to describe proportions, and survey responses were described using medians and the interquartile ranges (25th percentile, 75th percentile). Wilcoxon rank sum tests were used to measure the pre‐ and post‐training differences in the individual survey responses (Stata Statistical Software: Release 12; StataCorp, College Station, TX).
RESULTS
From among 18 hospitalist volunteers, the 10 board‐certified hospitalists who could attend 1 of the scheduled training sessions were enrolled and completed the study. Hospitalists' demographic information and performance are summarized in Table 1. Hospitalists completed the initial online curriculum in an average of 18.37 minutes. After the in‐person training session, 8 of 10 hospitalists acquired adequate IVC images on all 5 volunteer subjects. One hospitalist obtained adequate images in 4 of 5 patients. Another hospitalist only obtained adequate images in 3 of 5 patients; a hepatic vein and the abdominal aorta were erroneously measured instead of the IVC in 1 subject each. This hospitalist later performed supervised IVC imaging on 7 additional hospital inpatients and was the only hospitalist to request additional direct supervision by the research echocardiography technician. All hospitalists were able to accurately quantify the IVC collapsibility index and estimate the CVP from all 10 prerecorded cases showing still images and video clips of the IVC. Based on IVC images, 1 of the 5 volunteers used in testing each day had a very elevated CVP, and the other 4 had CVPs ranging from low to normal. The volunteer's average BMI was overweight at 27.4, with a range from 15.4 to 37.1.
| Hospitalist | Years in Practice | Previous Ultrasound Training (Hours)a | No. of Subjects Adequately Imaged and Correctly Interpreted After First Session (5 Maximum) | No. of Subjects Adequately Imaged and Correctly Interpreted at Follow‐up (5 Maximum) | After Study Completion Felt Training Was Adequate to Perform IVC Imagingb |
|---|---|---|---|---|---|
| |||||
| 1 | 5.5 | 10 | 5 | 5 | 4 |
| 2 | 0.8 | 0 | 5 | 5 | 5 |
| 3 | 1.8 | 4.5 | 3 | 4 | 2 |
| 4 | 1.8 | 0 | 5 | 5 | 5 |
| 5 | 10.5 | 6 | 5 | 5 | 5 |
| 6 | 1.7 | 1 | 5 | 5 | 5 |
| 7 | 0.6 | 0 | 5 | 5 | 5 |
| 8 | 2.6 | 0 | 4 | 5 | 4 |
| 9 | 1.7 | 0 | 5 | 5 | 5 |
| 10 | 5.5 | 10 | 5 | 5 | 5 |
At 7.40.7 weeks (range, 6.98.6 weeks) follow‐up, 9 of 10 hospitalists obtained adequate IVC images in all 5 volunteer subjects and interpreted them correctly for estimating CVP. The hospitalist who performed most poorly at the initial assessment acquired adequate images and interpreted them correctly in 4 of 5 patients at follow‐up. Overall, hospitalists' visual assessment of IVC collapsibility index agreed with the quantitative collapsibility index calculation in 180 of 198 (91%) of the interpretable encounters. By the time of the follow‐up assessment, hospitalists had performed IVC imaging on 3.93.0 additional hospital inpatients (range, 011 inpatients). Lack of time assigned to the clinical service was the main barrier limiting further IVC imaging during that interval. Hospitalists also identified time constraints and need for secure yet accessible device storage as other barriers.
None of the hospitalists had previous experience imaging the IVC, and prior to training they rated their average confidence to acquire an IVC image and interpret it by the hand‐carried ultrasound device at 3 (3, 4) and 3 (3, 4), respectively. After the initial training session, 9 of 10 hospitalists believed they had received adequate online and in‐person training and were confident in their ability to acquire and interpret IVC images. After all training sessions the hospitalists on average rated their confidence statistically significantly better for acquiring and interpreting IVC images at 2 (1, 2) (P=0.005) and 2 (1, 2) (P=0.004), respectively compared to baseline.
DISCUSSION
This study shows that after a relatively brief training intervention, hospitalists can develop and over a short term retain important skills in the acquisition and interpretation of IVC images to estimate CVP. Estimating CVP is key to the care of many patients, but cannot be done accurately by most physicians.[10] Although our study has a number of limitations, the ability to estimate CVP acquired after only a brief training intervention could have important effects on patient care. Given that a dilated IVC with reduced respiratory collapsibility was found to be a statistically significant predictor of 30‐day readmission for heart failure,11 key clinical outcomes to measure in future work include whether IVC ultrasound assessment can help guide diuresis, limit complications, and ultimately reduce rehospitalizations for heart failure, the most expensive diagnosis for Medicare.[12]
Because hand‐carried ultrasound is a point‐of‐care diagnostic tool, we also examined the ability of hospitalists to visually approximate the IVC collapsibility index. Hospitalists' qualitative performance (IVC collapsibility judged correctly 91% of the time without performing formal measurements) is consistent with studies involving emergency medicine physicians and suggests that CVP may be rapidly and accurately estimated in most instances.[13] There may be, however, value to formally measuring the IVC maximum diameter, because it may be inaccurately visually estimated due to changes in scale when the imaging depth is adjusted. Accurately measuring the IVC maximum diameter is important because a maximum diameter of more than 2.0 cm is evidence of an elevated right atrial pressure (82% sensitivity and 84% specificity for predicting right atrial pressure of 10 mm Hg or above) and an elevated pulmonary capillary wedge pressure (75% sensitivity and 83% specificity for pulmonary capillary wedge pressure of 15 mm Hg or more).[14]
Limitations
Our findings should be interpreted cautiously given the relatively small number of hospitalists and subjects used for hand‐carried ultrasound imaging. Although our direct observations of hospitalist performance in IVC imaging were based on objective measurements performed and interpreted accurately, we did not record the images, which would have allowed separate analyses of inter‐rater reliability measures. The majority of volunteer subjects were chronically ill, but they were nonetheless stable outpatients and may have been easier to position and image relative to acutely ill inpatients. Hospitalist self‐selected participation may introduce a bias favoring hospitalists interested in learning hand‐carried ultrasound skills; however, nearly half of the hospitalist group volunteered and enrollments in the study were based only on their availability for the previously scheduled study dates.
IMPLICATIONS FOR TRAINING
Our study, especially the assessment of the hospitalists' ability to retain their skills, adds to what is known about training hospitalists in hand‐carried ultrasound and may help inform deliberations among hospitalists as to whether to join other professional societies in defining specialty‐specific bedside ultrasound indications and training protocols.[9, 15] As individuals acquire new skills at variable rates, training cannot be defined by the number of procedures performed, but rather by the need to provide objective evidence of acquired procedural skills. Thus, going forward there is also a need to develop and validate tools for assessment of competence in IVC imaging skills.
Disclosures
This project was funded as an investigator‐sponsored research project by General Electric (GE) Medical Systems Ultrasound and Primary Care Diagnostics, LLC. The devices used in this training were supplied by GE. All authors had access to the data and contributed to the preparation of the manuscript. GE was not involved in the study design, analysis, or preparation of the manuscript. All authors received research support to perform this study from the funding source.
- , , , et al. A comparison by medicine residents of physical examination versus hand‐carried ultrasound for estimation of right atrial pressure. Am J Cardiol. 2007;99(11):1614–1616.
- , , . Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990;66:493–496.
- , , , et al. Reappraisal of the use of inferior vena cava for estimating right atrial pressure. J Am Soc Echocardiogr. 2007;20:857–861.
- , , , et al. Use of hand‐carried ultrasound, B‐type natriuretic peptide, and clinical assessment in identifying abnormal left ventricular filling pressures in patients referred for right heart catheterization. J Cardiac Fail. 2010;16:69–75.
- , , . Identification of congestive heart failure via respiratory variation of inferior vena cava diameter. Am J Emerg Med. 2009;27:71–75.
- , , , . Role of inferior vena cava diameter in assessment of volume status: a meta‐analysis. Am J Emerg Med. 2012;30(8):1414–1419.e1.
- , , , et al. Qualitative assessment of the inferior vena cava: useful tool for the evaluation of fluid status in critically ill patients. Am Surg. 2012;78(4):468–470.
- , , , et al. Inferior vena cava collapsibility to guide fluid removal in slow continuous ultrafiltration: a pilot study. Intensive Care Med 2010;36:692–696.
- , , , et al. Diagnostic accuracy of hospitalist‐performed hand‐carried ultrasound echocardiography after a brief training program. J Hosp Med. 2009;4(6):340–349.
- , , . Can the clinical examination diagnose left‐sided heart failure in adults? JAMA. 1997;277:1712–1719.
- , , , et al. Comparison of hand‐carried ultrasound assessment of the inferior vena cava and N‐terminal pro‐brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1:595–601.
- , , . Rehospitalizations among patients in the Medicare Fee‐for‐Service Program. N Engl J Med. 2009;360:1418–1428.
- , , , et al. The interrater reliability of inferior vena cava ultrasound by bedside clinician sonographers in emergency department patients. Acad Emerg Med. 2011;18:98–101.
- , , , et al. Usefulness of hand‐carried ultrasound to predict elevated left ventricular filling pressure. Am J Cardiol. 2009;103:246–247.
- , , , et al. Hospitalist performance of cardiac hand‐carried ultrasound after focused training. Am J Med. 2007;120(11):1000–1004.
The use of hand‐carried ultrasound by nonspecialists is increasing. Of particular interest to hospitalists is bedside ultrasound assessment of the inferior vena cava (IVC), which more accurately estimates left atrial pressure than does assessment of jugular venous pressure by physical examination.[1] Invasively measured central venous pressure (CVP) also correlates closely with estimates from IVC imaging.[1, 2, 3, 4] Although quick, accurate bedside determination of CVP may have broad potential applications in hospital medicine,[5, 6, 7, 8] of particular interest to patients and their advocates is whether hospitalists are sufficiently skilled to perform this procedure. Lucas et al. found that 8 hospitalists trained to perform 6 cardiac assessments by hand‐carried ultrasound could identify an enlarged IVC with moderate accuracy (sensitivity 56%, specificity 86%).[9] To our knowledge, no other study has examined whether hospitalists can readily develop the skills to accurately assess the IVC by ultrasound. We therefore studied whether the skills needed to acquire and interpret IVC images by ultrasound could be acquired by hospitalists after a brief training program.
METHODS
Study Populations
Hospitalists and volunteer subjects both provided informed consent to participate in this study, which was approved by the Johns Hopkins University School of Medicine Institutional Review Board. Nonpregnant volunteer subjects at least 18 years of age who agreed to attend training sessions were solicited from the investigators' ambulatory clinic patient population (see Supporting Information, Appendix A, in the online version of this article) and were compensated for their time. Volunteer subjects were solicited to represent a range of cardiac pathology. Hospitalists were solicited from among 28 members of the Johns Hopkins Bayview Medical Center's Division of Hospital Medicine, a nationally renowned academic hospitalist program comprising tenure‐track faculty who dedicate at least 30% of their time to academic endeavors.
Image Acquisition and Interpretation
A pocket‐sized portable hand‐carried ultrasound device was used for all IVC images (Vscan; GE Healthcare, Milwaukee, WI). All IVC images were acquired using the conventional methods with a subcostal view while the patient is supine. Cine loops of the IVC with respiration were captured in the longitudinal axis. Diameters were obtained approximately and by convention, approximately 2 cm from the IVC and right atrial junction. The IVC minimum diameter was measured during a cine loop of a patient performing a nasal sniff. The IVC collapsibility was determined by the formula: IVC Collapsibility Index=(IVCmaxIVCmin/IVCmax), where IVCmax and IVCmin represent the maximum and minimum IVC diameters respectively.[2] The IVC maximum diameters and collapsibility measurements that were used to estimate CVP are shown in the Supporting Information, Appendix B, in the online version of this article.
Educational Intervention and Skills Performance Assessment
One to 2 days prior to the in‐person training session, hospitalists were provided a brief introductory online curriculum (see Supporting Information, Appendix B, in the online version of this article). Groups of 3 to 4 hospitalists then completed an in‐person training and testing session (7 hours total time), which consisted of a precourse survey, a didactic session, and up to 4 hours of practice time with 10 volunteer subjects supervised by an experienced board‐certified cardiologist (G.A.H.) and a research echocardiography technician (C.M.). The survey included details on medical training, years in practice, prior ultrasound experience, and confidence in obtaining and interpreting IVC images. Confidence was rated on a Likert scale from 1=strongly confident to 5=not confident (3=neutral).
Next, each hospitalist's skills were assessed on 5 volunteer subjects selected by the cardiologist to represent a range of IVC appearance and body mass index (BMI). After appropriately identifying the IVC, they were first asked to make a visual qualitative judgement whether the IVC collapsed more than 50% during rapid inspiration or a sniff maneuver. Then hospitalists measured IVC diameter in a longitudinal view and calculated IVC collapsibility. Performance was evaluated by an experienced cardiologist (G.A.H.), who directly observed each hospitalist acquire and interpret IVC images and judged them relative to his own hand‐carried ultrasound assessments on the same subjects performed just before the hospitalists' scans. For each volunteer imaged, hospitalists had to acquire a technically adequate image of the IVC and correctly measure the inspiratory and expiratory IVC diameters. Hospitalists then had to estimate CVP by interpreting IVC diameters and collapsibility in 10 previously acquired sets of IVC video and still images. First, the hospitalists performed visual IVC collapsibility assessments (IVC collapse more than 50%) of video clips showing IVC appearance at baseline and during a rapid inspiration or sniff, without any measurements provided. Then, using still images showing premeasured maximum and minimum IVC diameters, they estimated CVP based on calculating IVC collapsibility (see Supporting Information, Appendix B, in the online version of this article for correlation of CVP to IVC maximum diameter and collapsibility). At the end of initial training hospitalists were again surveyed on confidence and also rated level of agreement (Likert scale, 1=strongly agree to 5=strongly disagree) regarding their ability to adequately obtain and accurately interpret IVC images and measurements. The post‐training survey also reviewed the training curriculum and asked hospitalists to identify potential barriers to clinical use of IVC ultrasound.
Following initial training, hospitalists were provided with a hand‐carried ultrasound device and allowed to use the device for IVC imaging on their general medical inpatients; the hospitalists could access the research echocardiography technician (C.M.) for assistance if desired. The number of additional patients imaged and whether scans were assisted was recorded for the study. At least 6 weeks after initial training, the hospitalists' IVC image acquisition and interpretation skills were again assessed on 5 volunteer subjects. At the follow‐up assessment, 4 of the 5 volunteers were new volunteers compared to the hospitalists' initial skills testing.
Statistics
The mean and standard deviations were used to describe continuous variables and percentages to describe proportions, and survey responses were described using medians and the interquartile ranges (25th percentile, 75th percentile). Wilcoxon rank sum tests were used to measure the pre‐ and post‐training differences in the individual survey responses (Stata Statistical Software: Release 12; StataCorp, College Station, TX).
RESULTS
From among 18 hospitalist volunteers, the 10 board‐certified hospitalists who could attend 1 of the scheduled training sessions were enrolled and completed the study. Hospitalists' demographic information and performance are summarized in Table 1. Hospitalists completed the initial online curriculum in an average of 18.37 minutes. After the in‐person training session, 8 of 10 hospitalists acquired adequate IVC images on all 5 volunteer subjects. One hospitalist obtained adequate images in 4 of 5 patients. Another hospitalist only obtained adequate images in 3 of 5 patients; a hepatic vein and the abdominal aorta were erroneously measured instead of the IVC in 1 subject each. This hospitalist later performed supervised IVC imaging on 7 additional hospital inpatients and was the only hospitalist to request additional direct supervision by the research echocardiography technician. All hospitalists were able to accurately quantify the IVC collapsibility index and estimate the CVP from all 10 prerecorded cases showing still images and video clips of the IVC. Based on IVC images, 1 of the 5 volunteers used in testing each day had a very elevated CVP, and the other 4 had CVPs ranging from low to normal. The volunteer's average BMI was overweight at 27.4, with a range from 15.4 to 37.1.
| Hospitalist | Years in Practice | Previous Ultrasound Training (Hours)a | No. of Subjects Adequately Imaged and Correctly Interpreted After First Session (5 Maximum) | No. of Subjects Adequately Imaged and Correctly Interpreted at Follow‐up (5 Maximum) | After Study Completion Felt Training Was Adequate to Perform IVC Imagingb |
|---|---|---|---|---|---|
| |||||
| 1 | 5.5 | 10 | 5 | 5 | 4 |
| 2 | 0.8 | 0 | 5 | 5 | 5 |
| 3 | 1.8 | 4.5 | 3 | 4 | 2 |
| 4 | 1.8 | 0 | 5 | 5 | 5 |
| 5 | 10.5 | 6 | 5 | 5 | 5 |
| 6 | 1.7 | 1 | 5 | 5 | 5 |
| 7 | 0.6 | 0 | 5 | 5 | 5 |
| 8 | 2.6 | 0 | 4 | 5 | 4 |
| 9 | 1.7 | 0 | 5 | 5 | 5 |
| 10 | 5.5 | 10 | 5 | 5 | 5 |
At 7.40.7 weeks (range, 6.98.6 weeks) follow‐up, 9 of 10 hospitalists obtained adequate IVC images in all 5 volunteer subjects and interpreted them correctly for estimating CVP. The hospitalist who performed most poorly at the initial assessment acquired adequate images and interpreted them correctly in 4 of 5 patients at follow‐up. Overall, hospitalists' visual assessment of IVC collapsibility index agreed with the quantitative collapsibility index calculation in 180 of 198 (91%) of the interpretable encounters. By the time of the follow‐up assessment, hospitalists had performed IVC imaging on 3.93.0 additional hospital inpatients (range, 011 inpatients). Lack of time assigned to the clinical service was the main barrier limiting further IVC imaging during that interval. Hospitalists also identified time constraints and need for secure yet accessible device storage as other barriers.
None of the hospitalists had previous experience imaging the IVC, and prior to training they rated their average confidence to acquire an IVC image and interpret it by the hand‐carried ultrasound device at 3 (3, 4) and 3 (3, 4), respectively. After the initial training session, 9 of 10 hospitalists believed they had received adequate online and in‐person training and were confident in their ability to acquire and interpret IVC images. After all training sessions the hospitalists on average rated their confidence statistically significantly better for acquiring and interpreting IVC images at 2 (1, 2) (P=0.005) and 2 (1, 2) (P=0.004), respectively compared to baseline.
DISCUSSION
This study shows that after a relatively brief training intervention, hospitalists can develop and over a short term retain important skills in the acquisition and interpretation of IVC images to estimate CVP. Estimating CVP is key to the care of many patients, but cannot be done accurately by most physicians.[10] Although our study has a number of limitations, the ability to estimate CVP acquired after only a brief training intervention could have important effects on patient care. Given that a dilated IVC with reduced respiratory collapsibility was found to be a statistically significant predictor of 30‐day readmission for heart failure,11 key clinical outcomes to measure in future work include whether IVC ultrasound assessment can help guide diuresis, limit complications, and ultimately reduce rehospitalizations for heart failure, the most expensive diagnosis for Medicare.[12]
Because hand‐carried ultrasound is a point‐of‐care diagnostic tool, we also examined the ability of hospitalists to visually approximate the IVC collapsibility index. Hospitalists' qualitative performance (IVC collapsibility judged correctly 91% of the time without performing formal measurements) is consistent with studies involving emergency medicine physicians and suggests that CVP may be rapidly and accurately estimated in most instances.[13] There may be, however, value to formally measuring the IVC maximum diameter, because it may be inaccurately visually estimated due to changes in scale when the imaging depth is adjusted. Accurately measuring the IVC maximum diameter is important because a maximum diameter of more than 2.0 cm is evidence of an elevated right atrial pressure (82% sensitivity and 84% specificity for predicting right atrial pressure of 10 mm Hg or above) and an elevated pulmonary capillary wedge pressure (75% sensitivity and 83% specificity for pulmonary capillary wedge pressure of 15 mm Hg or more).[14]
Limitations
Our findings should be interpreted cautiously given the relatively small number of hospitalists and subjects used for hand‐carried ultrasound imaging. Although our direct observations of hospitalist performance in IVC imaging were based on objective measurements performed and interpreted accurately, we did not record the images, which would have allowed separate analyses of inter‐rater reliability measures. The majority of volunteer subjects were chronically ill, but they were nonetheless stable outpatients and may have been easier to position and image relative to acutely ill inpatients. Hospitalist self‐selected participation may introduce a bias favoring hospitalists interested in learning hand‐carried ultrasound skills; however, nearly half of the hospitalist group volunteered and enrollments in the study were based only on their availability for the previously scheduled study dates.
IMPLICATIONS FOR TRAINING
Our study, especially the assessment of the hospitalists' ability to retain their skills, adds to what is known about training hospitalists in hand‐carried ultrasound and may help inform deliberations among hospitalists as to whether to join other professional societies in defining specialty‐specific bedside ultrasound indications and training protocols.[9, 15] As individuals acquire new skills at variable rates, training cannot be defined by the number of procedures performed, but rather by the need to provide objective evidence of acquired procedural skills. Thus, going forward there is also a need to develop and validate tools for assessment of competence in IVC imaging skills.
Disclosures
This project was funded as an investigator‐sponsored research project by General Electric (GE) Medical Systems Ultrasound and Primary Care Diagnostics, LLC. The devices used in this training were supplied by GE. All authors had access to the data and contributed to the preparation of the manuscript. GE was not involved in the study design, analysis, or preparation of the manuscript. All authors received research support to perform this study from the funding source.
The use of hand‐carried ultrasound by nonspecialists is increasing. Of particular interest to hospitalists is bedside ultrasound assessment of the inferior vena cava (IVC), which more accurately estimates left atrial pressure than does assessment of jugular venous pressure by physical examination.[1] Invasively measured central venous pressure (CVP) also correlates closely with estimates from IVC imaging.[1, 2, 3, 4] Although quick, accurate bedside determination of CVP may have broad potential applications in hospital medicine,[5, 6, 7, 8] of particular interest to patients and their advocates is whether hospitalists are sufficiently skilled to perform this procedure. Lucas et al. found that 8 hospitalists trained to perform 6 cardiac assessments by hand‐carried ultrasound could identify an enlarged IVC with moderate accuracy (sensitivity 56%, specificity 86%).[9] To our knowledge, no other study has examined whether hospitalists can readily develop the skills to accurately assess the IVC by ultrasound. We therefore studied whether the skills needed to acquire and interpret IVC images by ultrasound could be acquired by hospitalists after a brief training program.
METHODS
Study Populations
Hospitalists and volunteer subjects both provided informed consent to participate in this study, which was approved by the Johns Hopkins University School of Medicine Institutional Review Board. Nonpregnant volunteer subjects at least 18 years of age who agreed to attend training sessions were solicited from the investigators' ambulatory clinic patient population (see Supporting Information, Appendix A, in the online version of this article) and were compensated for their time. Volunteer subjects were solicited to represent a range of cardiac pathology. Hospitalists were solicited from among 28 members of the Johns Hopkins Bayview Medical Center's Division of Hospital Medicine, a nationally renowned academic hospitalist program comprising tenure‐track faculty who dedicate at least 30% of their time to academic endeavors.
Image Acquisition and Interpretation
A pocket‐sized portable hand‐carried ultrasound device was used for all IVC images (Vscan; GE Healthcare, Milwaukee, WI). All IVC images were acquired using the conventional methods with a subcostal view while the patient is supine. Cine loops of the IVC with respiration were captured in the longitudinal axis. Diameters were obtained approximately and by convention, approximately 2 cm from the IVC and right atrial junction. The IVC minimum diameter was measured during a cine loop of a patient performing a nasal sniff. The IVC collapsibility was determined by the formula: IVC Collapsibility Index=(IVCmaxIVCmin/IVCmax), where IVCmax and IVCmin represent the maximum and minimum IVC diameters respectively.[2] The IVC maximum diameters and collapsibility measurements that were used to estimate CVP are shown in the Supporting Information, Appendix B, in the online version of this article.
Educational Intervention and Skills Performance Assessment
One to 2 days prior to the in‐person training session, hospitalists were provided a brief introductory online curriculum (see Supporting Information, Appendix B, in the online version of this article). Groups of 3 to 4 hospitalists then completed an in‐person training and testing session (7 hours total time), which consisted of a precourse survey, a didactic session, and up to 4 hours of practice time with 10 volunteer subjects supervised by an experienced board‐certified cardiologist (G.A.H.) and a research echocardiography technician (C.M.). The survey included details on medical training, years in practice, prior ultrasound experience, and confidence in obtaining and interpreting IVC images. Confidence was rated on a Likert scale from 1=strongly confident to 5=not confident (3=neutral).
Next, each hospitalist's skills were assessed on 5 volunteer subjects selected by the cardiologist to represent a range of IVC appearance and body mass index (BMI). After appropriately identifying the IVC, they were first asked to make a visual qualitative judgement whether the IVC collapsed more than 50% during rapid inspiration or a sniff maneuver. Then hospitalists measured IVC diameter in a longitudinal view and calculated IVC collapsibility. Performance was evaluated by an experienced cardiologist (G.A.H.), who directly observed each hospitalist acquire and interpret IVC images and judged them relative to his own hand‐carried ultrasound assessments on the same subjects performed just before the hospitalists' scans. For each volunteer imaged, hospitalists had to acquire a technically adequate image of the IVC and correctly measure the inspiratory and expiratory IVC diameters. Hospitalists then had to estimate CVP by interpreting IVC diameters and collapsibility in 10 previously acquired sets of IVC video and still images. First, the hospitalists performed visual IVC collapsibility assessments (IVC collapse more than 50%) of video clips showing IVC appearance at baseline and during a rapid inspiration or sniff, without any measurements provided. Then, using still images showing premeasured maximum and minimum IVC diameters, they estimated CVP based on calculating IVC collapsibility (see Supporting Information, Appendix B, in the online version of this article for correlation of CVP to IVC maximum diameter and collapsibility). At the end of initial training hospitalists were again surveyed on confidence and also rated level of agreement (Likert scale, 1=strongly agree to 5=strongly disagree) regarding their ability to adequately obtain and accurately interpret IVC images and measurements. The post‐training survey also reviewed the training curriculum and asked hospitalists to identify potential barriers to clinical use of IVC ultrasound.
Following initial training, hospitalists were provided with a hand‐carried ultrasound device and allowed to use the device for IVC imaging on their general medical inpatients; the hospitalists could access the research echocardiography technician (C.M.) for assistance if desired. The number of additional patients imaged and whether scans were assisted was recorded for the study. At least 6 weeks after initial training, the hospitalists' IVC image acquisition and interpretation skills were again assessed on 5 volunteer subjects. At the follow‐up assessment, 4 of the 5 volunteers were new volunteers compared to the hospitalists' initial skills testing.
Statistics
The mean and standard deviations were used to describe continuous variables and percentages to describe proportions, and survey responses were described using medians and the interquartile ranges (25th percentile, 75th percentile). Wilcoxon rank sum tests were used to measure the pre‐ and post‐training differences in the individual survey responses (Stata Statistical Software: Release 12; StataCorp, College Station, TX).
RESULTS
From among 18 hospitalist volunteers, the 10 board‐certified hospitalists who could attend 1 of the scheduled training sessions were enrolled and completed the study. Hospitalists' demographic information and performance are summarized in Table 1. Hospitalists completed the initial online curriculum in an average of 18.37 minutes. After the in‐person training session, 8 of 10 hospitalists acquired adequate IVC images on all 5 volunteer subjects. One hospitalist obtained adequate images in 4 of 5 patients. Another hospitalist only obtained adequate images in 3 of 5 patients; a hepatic vein and the abdominal aorta were erroneously measured instead of the IVC in 1 subject each. This hospitalist later performed supervised IVC imaging on 7 additional hospital inpatients and was the only hospitalist to request additional direct supervision by the research echocardiography technician. All hospitalists were able to accurately quantify the IVC collapsibility index and estimate the CVP from all 10 prerecorded cases showing still images and video clips of the IVC. Based on IVC images, 1 of the 5 volunteers used in testing each day had a very elevated CVP, and the other 4 had CVPs ranging from low to normal. The volunteer's average BMI was overweight at 27.4, with a range from 15.4 to 37.1.
| Hospitalist | Years in Practice | Previous Ultrasound Training (Hours)a | No. of Subjects Adequately Imaged and Correctly Interpreted After First Session (5 Maximum) | No. of Subjects Adequately Imaged and Correctly Interpreted at Follow‐up (5 Maximum) | After Study Completion Felt Training Was Adequate to Perform IVC Imagingb |
|---|---|---|---|---|---|
| |||||
| 1 | 5.5 | 10 | 5 | 5 | 4 |
| 2 | 0.8 | 0 | 5 | 5 | 5 |
| 3 | 1.8 | 4.5 | 3 | 4 | 2 |
| 4 | 1.8 | 0 | 5 | 5 | 5 |
| 5 | 10.5 | 6 | 5 | 5 | 5 |
| 6 | 1.7 | 1 | 5 | 5 | 5 |
| 7 | 0.6 | 0 | 5 | 5 | 5 |
| 8 | 2.6 | 0 | 4 | 5 | 4 |
| 9 | 1.7 | 0 | 5 | 5 | 5 |
| 10 | 5.5 | 10 | 5 | 5 | 5 |
At 7.40.7 weeks (range, 6.98.6 weeks) follow‐up, 9 of 10 hospitalists obtained adequate IVC images in all 5 volunteer subjects and interpreted them correctly for estimating CVP. The hospitalist who performed most poorly at the initial assessment acquired adequate images and interpreted them correctly in 4 of 5 patients at follow‐up. Overall, hospitalists' visual assessment of IVC collapsibility index agreed with the quantitative collapsibility index calculation in 180 of 198 (91%) of the interpretable encounters. By the time of the follow‐up assessment, hospitalists had performed IVC imaging on 3.93.0 additional hospital inpatients (range, 011 inpatients). Lack of time assigned to the clinical service was the main barrier limiting further IVC imaging during that interval. Hospitalists also identified time constraints and need for secure yet accessible device storage as other barriers.
None of the hospitalists had previous experience imaging the IVC, and prior to training they rated their average confidence to acquire an IVC image and interpret it by the hand‐carried ultrasound device at 3 (3, 4) and 3 (3, 4), respectively. After the initial training session, 9 of 10 hospitalists believed they had received adequate online and in‐person training and were confident in their ability to acquire and interpret IVC images. After all training sessions the hospitalists on average rated their confidence statistically significantly better for acquiring and interpreting IVC images at 2 (1, 2) (P=0.005) and 2 (1, 2) (P=0.004), respectively compared to baseline.
DISCUSSION
This study shows that after a relatively brief training intervention, hospitalists can develop and over a short term retain important skills in the acquisition and interpretation of IVC images to estimate CVP. Estimating CVP is key to the care of many patients, but cannot be done accurately by most physicians.[10] Although our study has a number of limitations, the ability to estimate CVP acquired after only a brief training intervention could have important effects on patient care. Given that a dilated IVC with reduced respiratory collapsibility was found to be a statistically significant predictor of 30‐day readmission for heart failure,11 key clinical outcomes to measure in future work include whether IVC ultrasound assessment can help guide diuresis, limit complications, and ultimately reduce rehospitalizations for heart failure, the most expensive diagnosis for Medicare.[12]
Because hand‐carried ultrasound is a point‐of‐care diagnostic tool, we also examined the ability of hospitalists to visually approximate the IVC collapsibility index. Hospitalists' qualitative performance (IVC collapsibility judged correctly 91% of the time without performing formal measurements) is consistent with studies involving emergency medicine physicians and suggests that CVP may be rapidly and accurately estimated in most instances.[13] There may be, however, value to formally measuring the IVC maximum diameter, because it may be inaccurately visually estimated due to changes in scale when the imaging depth is adjusted. Accurately measuring the IVC maximum diameter is important because a maximum diameter of more than 2.0 cm is evidence of an elevated right atrial pressure (82% sensitivity and 84% specificity for predicting right atrial pressure of 10 mm Hg or above) and an elevated pulmonary capillary wedge pressure (75% sensitivity and 83% specificity for pulmonary capillary wedge pressure of 15 mm Hg or more).[14]
Limitations
Our findings should be interpreted cautiously given the relatively small number of hospitalists and subjects used for hand‐carried ultrasound imaging. Although our direct observations of hospitalist performance in IVC imaging were based on objective measurements performed and interpreted accurately, we did not record the images, which would have allowed separate analyses of inter‐rater reliability measures. The majority of volunteer subjects were chronically ill, but they were nonetheless stable outpatients and may have been easier to position and image relative to acutely ill inpatients. Hospitalist self‐selected participation may introduce a bias favoring hospitalists interested in learning hand‐carried ultrasound skills; however, nearly half of the hospitalist group volunteered and enrollments in the study were based only on their availability for the previously scheduled study dates.
IMPLICATIONS FOR TRAINING
Our study, especially the assessment of the hospitalists' ability to retain their skills, adds to what is known about training hospitalists in hand‐carried ultrasound and may help inform deliberations among hospitalists as to whether to join other professional societies in defining specialty‐specific bedside ultrasound indications and training protocols.[9, 15] As individuals acquire new skills at variable rates, training cannot be defined by the number of procedures performed, but rather by the need to provide objective evidence of acquired procedural skills. Thus, going forward there is also a need to develop and validate tools for assessment of competence in IVC imaging skills.
Disclosures
This project was funded as an investigator‐sponsored research project by General Electric (GE) Medical Systems Ultrasound and Primary Care Diagnostics, LLC. The devices used in this training were supplied by GE. All authors had access to the data and contributed to the preparation of the manuscript. GE was not involved in the study design, analysis, or preparation of the manuscript. All authors received research support to perform this study from the funding source.
- , , , et al. A comparison by medicine residents of physical examination versus hand‐carried ultrasound for estimation of right atrial pressure. Am J Cardiol. 2007;99(11):1614–1616.
- , , . Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990;66:493–496.
- , , , et al. Reappraisal of the use of inferior vena cava for estimating right atrial pressure. J Am Soc Echocardiogr. 2007;20:857–861.
- , , , et al. Use of hand‐carried ultrasound, B‐type natriuretic peptide, and clinical assessment in identifying abnormal left ventricular filling pressures in patients referred for right heart catheterization. J Cardiac Fail. 2010;16:69–75.
- , , . Identification of congestive heart failure via respiratory variation of inferior vena cava diameter. Am J Emerg Med. 2009;27:71–75.
- , , , . Role of inferior vena cava diameter in assessment of volume status: a meta‐analysis. Am J Emerg Med. 2012;30(8):1414–1419.e1.
- , , , et al. Qualitative assessment of the inferior vena cava: useful tool for the evaluation of fluid status in critically ill patients. Am Surg. 2012;78(4):468–470.
- , , , et al. Inferior vena cava collapsibility to guide fluid removal in slow continuous ultrafiltration: a pilot study. Intensive Care Med 2010;36:692–696.
- , , , et al. Diagnostic accuracy of hospitalist‐performed hand‐carried ultrasound echocardiography after a brief training program. J Hosp Med. 2009;4(6):340–349.
- , , . Can the clinical examination diagnose left‐sided heart failure in adults? JAMA. 1997;277:1712–1719.
- , , , et al. Comparison of hand‐carried ultrasound assessment of the inferior vena cava and N‐terminal pro‐brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1:595–601.
- , , . Rehospitalizations among patients in the Medicare Fee‐for‐Service Program. N Engl J Med. 2009;360:1418–1428.
- , , , et al. The interrater reliability of inferior vena cava ultrasound by bedside clinician sonographers in emergency department patients. Acad Emerg Med. 2011;18:98–101.
- , , , et al. Usefulness of hand‐carried ultrasound to predict elevated left ventricular filling pressure. Am J Cardiol. 2009;103:246–247.
- , , , et al. Hospitalist performance of cardiac hand‐carried ultrasound after focused training. Am J Med. 2007;120(11):1000–1004.
- , , , et al. A comparison by medicine residents of physical examination versus hand‐carried ultrasound for estimation of right atrial pressure. Am J Cardiol. 2007;99(11):1614–1616.
- , , . Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990;66:493–496.
- , , , et al. Reappraisal of the use of inferior vena cava for estimating right atrial pressure. J Am Soc Echocardiogr. 2007;20:857–861.
- , , , et al. Use of hand‐carried ultrasound, B‐type natriuretic peptide, and clinical assessment in identifying abnormal left ventricular filling pressures in patients referred for right heart catheterization. J Cardiac Fail. 2010;16:69–75.
- , , . Identification of congestive heart failure via respiratory variation of inferior vena cava diameter. Am J Emerg Med. 2009;27:71–75.
- , , , . Role of inferior vena cava diameter in assessment of volume status: a meta‐analysis. Am J Emerg Med. 2012;30(8):1414–1419.e1.
- , , , et al. Qualitative assessment of the inferior vena cava: useful tool for the evaluation of fluid status in critically ill patients. Am Surg. 2012;78(4):468–470.
- , , , et al. Inferior vena cava collapsibility to guide fluid removal in slow continuous ultrafiltration: a pilot study. Intensive Care Med 2010;36:692–696.
- , , , et al. Diagnostic accuracy of hospitalist‐performed hand‐carried ultrasound echocardiography after a brief training program. J Hosp Med. 2009;4(6):340–349.
- , , . Can the clinical examination diagnose left‐sided heart failure in adults? JAMA. 1997;277:1712–1719.
- , , , et al. Comparison of hand‐carried ultrasound assessment of the inferior vena cava and N‐terminal pro‐brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1:595–601.
- , , . Rehospitalizations among patients in the Medicare Fee‐for‐Service Program. N Engl J Med. 2009;360:1418–1428.
- , , , et al. The interrater reliability of inferior vena cava ultrasound by bedside clinician sonographers in emergency department patients. Acad Emerg Med. 2011;18:98–101.
- , , , et al. Usefulness of hand‐carried ultrasound to predict elevated left ventricular filling pressure. Am J Cardiol. 2009;103:246–247.
- , , , et al. Hospitalist performance of cardiac hand‐carried ultrasound after focused training. Am J Med. 2007;120(11):1000–1004.
Spectral gradient acoustic reflectometry aids diagnosis of acute otitis media and otitis media with effusion
Spectral gradient acoustic reflectometer (SGAR) is a technology to assist in the detection of middle ear fluid occurring in the context of diagnosing acute otitis media (AOM) and otitis media with effusion (OME). The technology involves sending a harmless, inaudible sonar-like sound wave from the emitter that goes through the tympanic membrane, hits the posterior wall of the middle ear space, and bounces back to the sound detector in the device. If there is only air in the middle ear space, the sound wave bounces back quickly, and you get a high reading. If the sound wave bounces back more slowly, there is middle ear effusion. The thicker the effusion, the more likely it is pus and an AOM or a chronic OME (depending on the clinical situation), causing the sound wave to bounce back more slowly and giving a low reading.
The specificity of a high reading is remarkable at around 95%, so a high reading is a big reassurance that middle ear effusion is absent. A lower reading suggests effusion and the lower it is, the greater the sensitivity. When I get an unexpected higher or lower reading, I go back and reexamine the patient.
I asked our nurses to compare the handheld tympanometer to the SGAR. They actually perform the testing, and I interpret it. The nurses said:
• The SGAR is easier to use because of how quickly a readout is obtained.
• If a child is crying or moving, they can still get a readout.
• You don’t have to change the tip of the SGAR for the size of the external ear canal.
• The SGAR is easier to read than the tympanometer.
• The SGAR is easier to interpret for the parents.
• You don’t have to get a seal with the ear canal with SGAR, as you do with a tympanometer.
• The SGAR uses a disposable tip.
I asked our office manager to look up our use of the SGAR and tympanometer during our everyday practice. We found that SGAR or tympanometry was used in 12% of patient encounters in which the diagnosis of AOM or OME was part of the chief complaint. The ratio of use was 3:1, favoring SGAR. The most frequent use was in 30% of patient encounters tied to the diagnosis of "otalgia" (388.70) because with that diagnosis, we are stating to parents and patients that there is no middle ear pathology seen on exam, and it is confirmed by a test using sonar waves with the SGAR device. Our nurse practitioners and physician assistants particularly find the use of the SGAR beneficial in helping to reassure the parents and patients that they have not missed an AOM or OME.
The billing code is the same for SGAR and tympanometry (92567), so the fee payment is the same for both tests. Our second most common use is in association with possible AOM (382.9) at 12% of visits. Third is OME (381.02) used in a follow-up visit to determine the presence and thickness of persisting effusion.
About one-quarter of children seen in our practice with a chief complaint of "earache" receive the diagnosis of otalgia, often confirmed by SGAR, and do not receive an antibiotic. Thus, they are offsetting the charge for the procedure by saving on the costs of antibiotics and the accumulation of excessive diagnoses of AOM and OME leading to ear tube surgeries and tonsillectomy/adenoidectomy. The diagnosis of AOM and OME requires a middle ear effusion to be accurate, and only SGAR measures detection of middle ear effusion. SGAR is a must own device for clinicians who exam ears. SGAR can help in conjunction with otoscopy for a difficult diagnosis of AOM. If I am having troubleremoving wax, or if the external ear canal is particularly curved, or if I’m on the fence or the parent seems to need further evidence of my diagnosis, I turn to the SGAR. If I can get a reading, then it can really help, and my nurses are successful in getting a reading about 90% of the time. The main issue is ear canal wax, because occlusion by wax of more than 50% of the external ear canal opening causes invalid readings.
We should prescribe antibiotics for AOM in my opinion, but not for otalgia and not if the diagnosis is uncertain. The SGAR device when properly used can help to reduce unnecessary use of antibiotics and their complications. In prior "ID Consult" columns, I have discussed improving the diagnostic accuracy of AOM and OME. Performing a good otoscopic exam with the best tools available and combining that exam with SGAR or tympanometry, in selected cases, is the best practice in my opinion, and what I do in my own practice.
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute, Rochester General Hospital, N.Y. He is also a pediatrician at Legacy Pediatrics in Rochester. E-mail him at [email protected]. Innovia Medical, the company that is bringing the SGAR EarCheck Pro back to market in 2014 after improvement and the addition of a USB port to allow the import of the data readout into the electronic medical record, asked Dr. Pichichero to assess the SGAR device.
Spectral gradient acoustic reflectometer (SGAR) is a technology to assist in the detection of middle ear fluid occurring in the context of diagnosing acute otitis media (AOM) and otitis media with effusion (OME). The technology involves sending a harmless, inaudible sonar-like sound wave from the emitter that goes through the tympanic membrane, hits the posterior wall of the middle ear space, and bounces back to the sound detector in the device. If there is only air in the middle ear space, the sound wave bounces back quickly, and you get a high reading. If the sound wave bounces back more slowly, there is middle ear effusion. The thicker the effusion, the more likely it is pus and an AOM or a chronic OME (depending on the clinical situation), causing the sound wave to bounce back more slowly and giving a low reading.
The specificity of a high reading is remarkable at around 95%, so a high reading is a big reassurance that middle ear effusion is absent. A lower reading suggests effusion and the lower it is, the greater the sensitivity. When I get an unexpected higher or lower reading, I go back and reexamine the patient.
I asked our nurses to compare the handheld tympanometer to the SGAR. They actually perform the testing, and I interpret it. The nurses said:
• The SGAR is easier to use because of how quickly a readout is obtained.
• If a child is crying or moving, they can still get a readout.
• You don’t have to change the tip of the SGAR for the size of the external ear canal.
• The SGAR is easier to read than the tympanometer.
• The SGAR is easier to interpret for the parents.
• You don’t have to get a seal with the ear canal with SGAR, as you do with a tympanometer.
• The SGAR uses a disposable tip.
I asked our office manager to look up our use of the SGAR and tympanometer during our everyday practice. We found that SGAR or tympanometry was used in 12% of patient encounters in which the diagnosis of AOM or OME was part of the chief complaint. The ratio of use was 3:1, favoring SGAR. The most frequent use was in 30% of patient encounters tied to the diagnosis of "otalgia" (388.70) because with that diagnosis, we are stating to parents and patients that there is no middle ear pathology seen on exam, and it is confirmed by a test using sonar waves with the SGAR device. Our nurse practitioners and physician assistants particularly find the use of the SGAR beneficial in helping to reassure the parents and patients that they have not missed an AOM or OME.
The billing code is the same for SGAR and tympanometry (92567), so the fee payment is the same for both tests. Our second most common use is in association with possible AOM (382.9) at 12% of visits. Third is OME (381.02) used in a follow-up visit to determine the presence and thickness of persisting effusion.
About one-quarter of children seen in our practice with a chief complaint of "earache" receive the diagnosis of otalgia, often confirmed by SGAR, and do not receive an antibiotic. Thus, they are offsetting the charge for the procedure by saving on the costs of antibiotics and the accumulation of excessive diagnoses of AOM and OME leading to ear tube surgeries and tonsillectomy/adenoidectomy. The diagnosis of AOM and OME requires a middle ear effusion to be accurate, and only SGAR measures detection of middle ear effusion. SGAR is a must own device for clinicians who exam ears. SGAR can help in conjunction with otoscopy for a difficult diagnosis of AOM. If I am having troubleremoving wax, or if the external ear canal is particularly curved, or if I’m on the fence or the parent seems to need further evidence of my diagnosis, I turn to the SGAR. If I can get a reading, then it can really help, and my nurses are successful in getting a reading about 90% of the time. The main issue is ear canal wax, because occlusion by wax of more than 50% of the external ear canal opening causes invalid readings.
We should prescribe antibiotics for AOM in my opinion, but not for otalgia and not if the diagnosis is uncertain. The SGAR device when properly used can help to reduce unnecessary use of antibiotics and their complications. In prior "ID Consult" columns, I have discussed improving the diagnostic accuracy of AOM and OME. Performing a good otoscopic exam with the best tools available and combining that exam with SGAR or tympanometry, in selected cases, is the best practice in my opinion, and what I do in my own practice.
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute, Rochester General Hospital, N.Y. He is also a pediatrician at Legacy Pediatrics in Rochester. E-mail him at [email protected]. Innovia Medical, the company that is bringing the SGAR EarCheck Pro back to market in 2014 after improvement and the addition of a USB port to allow the import of the data readout into the electronic medical record, asked Dr. Pichichero to assess the SGAR device.
Spectral gradient acoustic reflectometer (SGAR) is a technology to assist in the detection of middle ear fluid occurring in the context of diagnosing acute otitis media (AOM) and otitis media with effusion (OME). The technology involves sending a harmless, inaudible sonar-like sound wave from the emitter that goes through the tympanic membrane, hits the posterior wall of the middle ear space, and bounces back to the sound detector in the device. If there is only air in the middle ear space, the sound wave bounces back quickly, and you get a high reading. If the sound wave bounces back more slowly, there is middle ear effusion. The thicker the effusion, the more likely it is pus and an AOM or a chronic OME (depending on the clinical situation), causing the sound wave to bounce back more slowly and giving a low reading.
The specificity of a high reading is remarkable at around 95%, so a high reading is a big reassurance that middle ear effusion is absent. A lower reading suggests effusion and the lower it is, the greater the sensitivity. When I get an unexpected higher or lower reading, I go back and reexamine the patient.
I asked our nurses to compare the handheld tympanometer to the SGAR. They actually perform the testing, and I interpret it. The nurses said:
• The SGAR is easier to use because of how quickly a readout is obtained.
• If a child is crying or moving, they can still get a readout.
• You don’t have to change the tip of the SGAR for the size of the external ear canal.
• The SGAR is easier to read than the tympanometer.
• The SGAR is easier to interpret for the parents.
• You don’t have to get a seal with the ear canal with SGAR, as you do with a tympanometer.
• The SGAR uses a disposable tip.
I asked our office manager to look up our use of the SGAR and tympanometer during our everyday practice. We found that SGAR or tympanometry was used in 12% of patient encounters in which the diagnosis of AOM or OME was part of the chief complaint. The ratio of use was 3:1, favoring SGAR. The most frequent use was in 30% of patient encounters tied to the diagnosis of "otalgia" (388.70) because with that diagnosis, we are stating to parents and patients that there is no middle ear pathology seen on exam, and it is confirmed by a test using sonar waves with the SGAR device. Our nurse practitioners and physician assistants particularly find the use of the SGAR beneficial in helping to reassure the parents and patients that they have not missed an AOM or OME.
The billing code is the same for SGAR and tympanometry (92567), so the fee payment is the same for both tests. Our second most common use is in association with possible AOM (382.9) at 12% of visits. Third is OME (381.02) used in a follow-up visit to determine the presence and thickness of persisting effusion.
About one-quarter of children seen in our practice with a chief complaint of "earache" receive the diagnosis of otalgia, often confirmed by SGAR, and do not receive an antibiotic. Thus, they are offsetting the charge for the procedure by saving on the costs of antibiotics and the accumulation of excessive diagnoses of AOM and OME leading to ear tube surgeries and tonsillectomy/adenoidectomy. The diagnosis of AOM and OME requires a middle ear effusion to be accurate, and only SGAR measures detection of middle ear effusion. SGAR is a must own device for clinicians who exam ears. SGAR can help in conjunction with otoscopy for a difficult diagnosis of AOM. If I am having troubleremoving wax, or if the external ear canal is particularly curved, or if I’m on the fence or the parent seems to need further evidence of my diagnosis, I turn to the SGAR. If I can get a reading, then it can really help, and my nurses are successful in getting a reading about 90% of the time. The main issue is ear canal wax, because occlusion by wax of more than 50% of the external ear canal opening causes invalid readings.
We should prescribe antibiotics for AOM in my opinion, but not for otalgia and not if the diagnosis is uncertain. The SGAR device when properly used can help to reduce unnecessary use of antibiotics and their complications. In prior "ID Consult" columns, I have discussed improving the diagnostic accuracy of AOM and OME. Performing a good otoscopic exam with the best tools available and combining that exam with SGAR or tympanometry, in selected cases, is the best practice in my opinion, and what I do in my own practice.
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute, Rochester General Hospital, N.Y. He is also a pediatrician at Legacy Pediatrics in Rochester. E-mail him at [email protected]. Innovia Medical, the company that is bringing the SGAR EarCheck Pro back to market in 2014 after improvement and the addition of a USB port to allow the import of the data readout into the electronic medical record, asked Dr. Pichichero to assess the SGAR device.
Low serum uric acid levels protect against progressions of renal disease
SAN DIEGO – Patients who achieve a serum uric acid level of less than 6 mg/dL based on current gout management guidelines demonstrated a 37% reduction in progression of renal disease, a large retrospective study showed.
"There are numerous studies showing that people with renal disease can develop hyperuricemia," Dr. Gerald D. Levy said during a press briefing at the annual meeting of the American College of Rheumatology. "Some of them will also develop gout. There are a few small studies showing that in humans, you can reverse hyperuricemia with urate lowering therapy and make an impact in renal disease. We wanted to see if this is true."
Dr. Levy of the division of rheumatology in the department of internal medicine at Kaiser Permanente Medical Group, Downey, Calif., was the lead investigators in a study of 111,992 Kaiser Permanente Southern California patients with a serum uric acid (SUA) level of 7 mg/dL or greater from Jan. 1, 2002, to Dec. 31, 2010. Patients with at least 12 months of health plan membership, including drug benefit prior to the index date, were studied. All patients had at least one SUA and glomerular filtration rate (GFR) level measurement in the 6-month period prior to the index date and at least one SUA and one GFR in the follow-up period following the index date. Primary outcome events were at least a 30% worsening of renal function, initiation of dialysis, having a GFR of less than 15 mL/min, and undergoing a kidney transplant.
Patients with a new diagnosis of cancer were excluded from the analysis, as were those with HIV, glomerulonephritis, and/or organ transplant other than a kidney transplant.
Dr. Levy reported results from 16,186 patients who were divided into three groups: those who were never treated with urate-lowering therapy (ULT; 11,192); those who were treated with ULT less than 80% of the time from the index date to the end of follow-up period (3,902); and those who were treated with ULT 80% of the time or more from the index date to the end of the follow-up period (1,092). Of the three treatment groups, those who were treated with ULT 80% of the time or more during the study tended to be older and have more comorbid conditions, compared with the other two groups. They also began their ULT therapy earlier.
Among all patients combined, factors significantly associated with renal disease progression included having diabetes (hazard ratio, 1.96), hypertension (HR, 1.50), heart failure (HR, 1.39), previous hospitalizations (HR, 1.33), and being female (HR, 1.49) and older (HR, 1.03). The researchers found that time on ULT was not significantly associated with a reduction in renal disease progression outcome events (HR, 1.27, among those on ULT less than 80% of the time during the study vs. HR, 1.08, among those on ULT 80% of the time or more during the study). However, patients who achieved an SUA level below 6 mg/dL – a treatment goal in the 2012 ACR guidelines for management of gout – demonstrated a 37% reduction in renal disease progression (HR, 0.63; P less than .0001).
Dr. Levy acknowledged certain limitations of the study, including its retrospective design and the fact that patients with stage 4 and 5 chronic kidney disease were not included. "This is an important area, because if we can delay the worsening of renal disease in these folks, perhaps we’re abetting dialysis, which is growing by leaps and bounds in this country," he said. "Each dialysis patient now costs about $80,000 per year to take care of. If we could push that back even for a few years it would have a tremendous impact."
Dr. Levy had no relevant financial conflicts to disclose.
SAN DIEGO – Patients who achieve a serum uric acid level of less than 6 mg/dL based on current gout management guidelines demonstrated a 37% reduction in progression of renal disease, a large retrospective study showed.
"There are numerous studies showing that people with renal disease can develop hyperuricemia," Dr. Gerald D. Levy said during a press briefing at the annual meeting of the American College of Rheumatology. "Some of them will also develop gout. There are a few small studies showing that in humans, you can reverse hyperuricemia with urate lowering therapy and make an impact in renal disease. We wanted to see if this is true."
Dr. Levy of the division of rheumatology in the department of internal medicine at Kaiser Permanente Medical Group, Downey, Calif., was the lead investigators in a study of 111,992 Kaiser Permanente Southern California patients with a serum uric acid (SUA) level of 7 mg/dL or greater from Jan. 1, 2002, to Dec. 31, 2010. Patients with at least 12 months of health plan membership, including drug benefit prior to the index date, were studied. All patients had at least one SUA and glomerular filtration rate (GFR) level measurement in the 6-month period prior to the index date and at least one SUA and one GFR in the follow-up period following the index date. Primary outcome events were at least a 30% worsening of renal function, initiation of dialysis, having a GFR of less than 15 mL/min, and undergoing a kidney transplant.
Patients with a new diagnosis of cancer were excluded from the analysis, as were those with HIV, glomerulonephritis, and/or organ transplant other than a kidney transplant.
Dr. Levy reported results from 16,186 patients who were divided into three groups: those who were never treated with urate-lowering therapy (ULT; 11,192); those who were treated with ULT less than 80% of the time from the index date to the end of follow-up period (3,902); and those who were treated with ULT 80% of the time or more from the index date to the end of the follow-up period (1,092). Of the three treatment groups, those who were treated with ULT 80% of the time or more during the study tended to be older and have more comorbid conditions, compared with the other two groups. They also began their ULT therapy earlier.
Among all patients combined, factors significantly associated with renal disease progression included having diabetes (hazard ratio, 1.96), hypertension (HR, 1.50), heart failure (HR, 1.39), previous hospitalizations (HR, 1.33), and being female (HR, 1.49) and older (HR, 1.03). The researchers found that time on ULT was not significantly associated with a reduction in renal disease progression outcome events (HR, 1.27, among those on ULT less than 80% of the time during the study vs. HR, 1.08, among those on ULT 80% of the time or more during the study). However, patients who achieved an SUA level below 6 mg/dL – a treatment goal in the 2012 ACR guidelines for management of gout – demonstrated a 37% reduction in renal disease progression (HR, 0.63; P less than .0001).
Dr. Levy acknowledged certain limitations of the study, including its retrospective design and the fact that patients with stage 4 and 5 chronic kidney disease were not included. "This is an important area, because if we can delay the worsening of renal disease in these folks, perhaps we’re abetting dialysis, which is growing by leaps and bounds in this country," he said. "Each dialysis patient now costs about $80,000 per year to take care of. If we could push that back even for a few years it would have a tremendous impact."
Dr. Levy had no relevant financial conflicts to disclose.
SAN DIEGO – Patients who achieve a serum uric acid level of less than 6 mg/dL based on current gout management guidelines demonstrated a 37% reduction in progression of renal disease, a large retrospective study showed.
"There are numerous studies showing that people with renal disease can develop hyperuricemia," Dr. Gerald D. Levy said during a press briefing at the annual meeting of the American College of Rheumatology. "Some of them will also develop gout. There are a few small studies showing that in humans, you can reverse hyperuricemia with urate lowering therapy and make an impact in renal disease. We wanted to see if this is true."
Dr. Levy of the division of rheumatology in the department of internal medicine at Kaiser Permanente Medical Group, Downey, Calif., was the lead investigators in a study of 111,992 Kaiser Permanente Southern California patients with a serum uric acid (SUA) level of 7 mg/dL or greater from Jan. 1, 2002, to Dec. 31, 2010. Patients with at least 12 months of health plan membership, including drug benefit prior to the index date, were studied. All patients had at least one SUA and glomerular filtration rate (GFR) level measurement in the 6-month period prior to the index date and at least one SUA and one GFR in the follow-up period following the index date. Primary outcome events were at least a 30% worsening of renal function, initiation of dialysis, having a GFR of less than 15 mL/min, and undergoing a kidney transplant.
Patients with a new diagnosis of cancer were excluded from the analysis, as were those with HIV, glomerulonephritis, and/or organ transplant other than a kidney transplant.
Dr. Levy reported results from 16,186 patients who were divided into three groups: those who were never treated with urate-lowering therapy (ULT; 11,192); those who were treated with ULT less than 80% of the time from the index date to the end of follow-up period (3,902); and those who were treated with ULT 80% of the time or more from the index date to the end of the follow-up period (1,092). Of the three treatment groups, those who were treated with ULT 80% of the time or more during the study tended to be older and have more comorbid conditions, compared with the other two groups. They also began their ULT therapy earlier.
Among all patients combined, factors significantly associated with renal disease progression included having diabetes (hazard ratio, 1.96), hypertension (HR, 1.50), heart failure (HR, 1.39), previous hospitalizations (HR, 1.33), and being female (HR, 1.49) and older (HR, 1.03). The researchers found that time on ULT was not significantly associated with a reduction in renal disease progression outcome events (HR, 1.27, among those on ULT less than 80% of the time during the study vs. HR, 1.08, among those on ULT 80% of the time or more during the study). However, patients who achieved an SUA level below 6 mg/dL – a treatment goal in the 2012 ACR guidelines for management of gout – demonstrated a 37% reduction in renal disease progression (HR, 0.63; P less than .0001).
Dr. Levy acknowledged certain limitations of the study, including its retrospective design and the fact that patients with stage 4 and 5 chronic kidney disease were not included. "This is an important area, because if we can delay the worsening of renal disease in these folks, perhaps we’re abetting dialysis, which is growing by leaps and bounds in this country," he said. "Each dialysis patient now costs about $80,000 per year to take care of. If we could push that back even for a few years it would have a tremendous impact."
Dr. Levy had no relevant financial conflicts to disclose.
AT THE ACR ANNUAL MEETING
Major finding: Patients who achieved a serum uric acid level below 6 mg/dL – a treatment goal in the 2012 ACR guidelines for management of gout – demonstrated a 37% reduction in renal disease progression (HR, 0.63; P less than .0001).
Data source: A study of 16,186 patients who were divided into three groups: those who were never treated with urate-lowering therapy (ULT; 11,192), those who were treated with ULT less than 80% of the time from the index date to the end of follow-up period (3,902), and those who were treated with ULT 80% of the time or more from the index date to the end of the follow-up period (1,092).
Disclosures: Dr. Levy said that he had no relevant financial conflicts to disclose.
Factor can prevent bleeding in hemophilia A
Results of a phase 3 trial suggest a recombinant factor VIII Fc fusion protein (rFVIIIFc/efmoroctocog alfa, Eloctate/Elocta) can be used to prevent or reduce bleeding episodes in patients with severe hemophilia A.
Researchers found that prophylaxis with rFVIIIFc resulted in low annualized bleeding rates, and patients did not develop neutralizing antibodies.
Furthermore, the product was generally well-tolerated and had a prolonged half-life when compared with recombinant factor VIII.
Data from this study, called A-LONG, have been published in Blood.
Researchers tested rFVIIIFc in 165 male patients with severe hemophilia A who were 12 years of age and older.
Patients were divided into 3 treatment arms. Arm 1 received individualized prophylaxis, or 25 to 65 IU/kg every 3 to 5 days (n=118). Patients in arm 2 received a weekly prophylactic dose of 65 IU/kg (n=24). And patients in arm 3 received episodic treatment at doses of 10 to 50 IU/kg (n=23).
A total of 153 patients completed the study, and 757 bleeding episodes were treated with rFVIIIFc. Across the treatment arms, 87.3% of bleeding episodes were resolved with 1 injection of rFVIIIFc.
The annualized bleeding rate was significantly reduced with prophylaxis—by 92% for patients in arm 1 and 76% for those in arm 2—when compared with episodic treatment.
This was based on annualized bleeding rate estimates from a negative binomial regression model—2.91 for arm 1, 8.92 for arm 2, and 37.25 for arm 3.
The median annualized bleeding rates were 1.6 in arm 1, 3.6 in arm 2, and 33.6 in arm 3.
In arm 3, there were 9 patients who received rFVIIIFc to control bleeding during major surgery. In these cases, physicians rated the hemostatic response as “excellent” (n=8) or “good” (n=1).
There were no serious adverse events related to rFVIIIFc, and none of the patients developed neutralizing antibodies.
The most common adverse events (with an incidence of 5% or more) that occurred outside the perioperative period included nasopharyngitis, arthralgia, headache, and upper respiratory infection.
The researchers also compared the pharmacokinetics of rFVIIIFc and recombinant factor VIII. And they found the terminal half-life of rFVIIIFc was extended 1.5-fold compared to recombinant factor VIII—19.0 hours and 12.4 hours, respectively.
rFVIIIFc was developed using Fc fusion technology, which takes advantage of a naturally occurring pathway that delays the breakdown of IgG1 protein in the body by recycling it back into the bloodstream. This technology prolongs the time rFVIIIFc circulates in the body.
“There is an unmet medical need in the hemophilia community for longer intervals between prophylactic infusions while maintaining good control of bleeding episodes,” said study author Johnny Mahlangu, MD, director of the Haemophilia Comprehensive Care Centre at the University of the Witwatersrand and National Health Laboratory Service in Johannesburg, South Africa.
“A-LONG is the first clinical study to show that effective control over breakthrough bleeding may be achieved with once- or twice-weekly prophylactic infusions in people with severe hemophilia A.”
This study was funded by Biogen Idec, makers of rFVIIIFc. ![]()
Results of a phase 3 trial suggest a recombinant factor VIII Fc fusion protein (rFVIIIFc/efmoroctocog alfa, Eloctate/Elocta) can be used to prevent or reduce bleeding episodes in patients with severe hemophilia A.
Researchers found that prophylaxis with rFVIIIFc resulted in low annualized bleeding rates, and patients did not develop neutralizing antibodies.
Furthermore, the product was generally well-tolerated and had a prolonged half-life when compared with recombinant factor VIII.
Data from this study, called A-LONG, have been published in Blood.
Researchers tested rFVIIIFc in 165 male patients with severe hemophilia A who were 12 years of age and older.
Patients were divided into 3 treatment arms. Arm 1 received individualized prophylaxis, or 25 to 65 IU/kg every 3 to 5 days (n=118). Patients in arm 2 received a weekly prophylactic dose of 65 IU/kg (n=24). And patients in arm 3 received episodic treatment at doses of 10 to 50 IU/kg (n=23).
A total of 153 patients completed the study, and 757 bleeding episodes were treated with rFVIIIFc. Across the treatment arms, 87.3% of bleeding episodes were resolved with 1 injection of rFVIIIFc.
The annualized bleeding rate was significantly reduced with prophylaxis—by 92% for patients in arm 1 and 76% for those in arm 2—when compared with episodic treatment.
This was based on annualized bleeding rate estimates from a negative binomial regression model—2.91 for arm 1, 8.92 for arm 2, and 37.25 for arm 3.
The median annualized bleeding rates were 1.6 in arm 1, 3.6 in arm 2, and 33.6 in arm 3.
In arm 3, there were 9 patients who received rFVIIIFc to control bleeding during major surgery. In these cases, physicians rated the hemostatic response as “excellent” (n=8) or “good” (n=1).
There were no serious adverse events related to rFVIIIFc, and none of the patients developed neutralizing antibodies.
The most common adverse events (with an incidence of 5% or more) that occurred outside the perioperative period included nasopharyngitis, arthralgia, headache, and upper respiratory infection.
The researchers also compared the pharmacokinetics of rFVIIIFc and recombinant factor VIII. And they found the terminal half-life of rFVIIIFc was extended 1.5-fold compared to recombinant factor VIII—19.0 hours and 12.4 hours, respectively.
rFVIIIFc was developed using Fc fusion technology, which takes advantage of a naturally occurring pathway that delays the breakdown of IgG1 protein in the body by recycling it back into the bloodstream. This technology prolongs the time rFVIIIFc circulates in the body.
“There is an unmet medical need in the hemophilia community for longer intervals between prophylactic infusions while maintaining good control of bleeding episodes,” said study author Johnny Mahlangu, MD, director of the Haemophilia Comprehensive Care Centre at the University of the Witwatersrand and National Health Laboratory Service in Johannesburg, South Africa.
“A-LONG is the first clinical study to show that effective control over breakthrough bleeding may be achieved with once- or twice-weekly prophylactic infusions in people with severe hemophilia A.”
This study was funded by Biogen Idec, makers of rFVIIIFc. ![]()
Results of a phase 3 trial suggest a recombinant factor VIII Fc fusion protein (rFVIIIFc/efmoroctocog alfa, Eloctate/Elocta) can be used to prevent or reduce bleeding episodes in patients with severe hemophilia A.
Researchers found that prophylaxis with rFVIIIFc resulted in low annualized bleeding rates, and patients did not develop neutralizing antibodies.
Furthermore, the product was generally well-tolerated and had a prolonged half-life when compared with recombinant factor VIII.
Data from this study, called A-LONG, have been published in Blood.
Researchers tested rFVIIIFc in 165 male patients with severe hemophilia A who were 12 years of age and older.
Patients were divided into 3 treatment arms. Arm 1 received individualized prophylaxis, or 25 to 65 IU/kg every 3 to 5 days (n=118). Patients in arm 2 received a weekly prophylactic dose of 65 IU/kg (n=24). And patients in arm 3 received episodic treatment at doses of 10 to 50 IU/kg (n=23).
A total of 153 patients completed the study, and 757 bleeding episodes were treated with rFVIIIFc. Across the treatment arms, 87.3% of bleeding episodes were resolved with 1 injection of rFVIIIFc.
The annualized bleeding rate was significantly reduced with prophylaxis—by 92% for patients in arm 1 and 76% for those in arm 2—when compared with episodic treatment.
This was based on annualized bleeding rate estimates from a negative binomial regression model—2.91 for arm 1, 8.92 for arm 2, and 37.25 for arm 3.
The median annualized bleeding rates were 1.6 in arm 1, 3.6 in arm 2, and 33.6 in arm 3.
In arm 3, there were 9 patients who received rFVIIIFc to control bleeding during major surgery. In these cases, physicians rated the hemostatic response as “excellent” (n=8) or “good” (n=1).
There were no serious adverse events related to rFVIIIFc, and none of the patients developed neutralizing antibodies.
The most common adverse events (with an incidence of 5% or more) that occurred outside the perioperative period included nasopharyngitis, arthralgia, headache, and upper respiratory infection.
The researchers also compared the pharmacokinetics of rFVIIIFc and recombinant factor VIII. And they found the terminal half-life of rFVIIIFc was extended 1.5-fold compared to recombinant factor VIII—19.0 hours and 12.4 hours, respectively.
rFVIIIFc was developed using Fc fusion technology, which takes advantage of a naturally occurring pathway that delays the breakdown of IgG1 protein in the body by recycling it back into the bloodstream. This technology prolongs the time rFVIIIFc circulates in the body.
“There is an unmet medical need in the hemophilia community for longer intervals between prophylactic infusions while maintaining good control of bleeding episodes,” said study author Johnny Mahlangu, MD, director of the Haemophilia Comprehensive Care Centre at the University of the Witwatersrand and National Health Laboratory Service in Johannesburg, South Africa.
“A-LONG is the first clinical study to show that effective control over breakthrough bleeding may be achieved with once- or twice-weekly prophylactic infusions in people with severe hemophilia A.”
This study was funded by Biogen Idec, makers of rFVIIIFc. ![]()
FDA approves ibrutinib for previously treated MCL

The US Food and Drug Administration (FDA) has has granted accelerated approval for
ibrutinib (Imbruvica) to treat patients with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
Ibrutinib works by inhibiting the function of Bruton’s tyrosine kinase, a molecule that plays an important role in the survival of malignant B cells.
The drug showed promising results in the phase 2 PCYC-1104 trial, which was presented at ASH 2012 and published in NEJM in August.
The FDA granted ibrutinib breakthrough therapy designation because of these results and the life-threatening nature of MCL. Ibrutinib is the second drug with breakthrough therapy designation to receive FDA approval.
The FDA granted ibrutinib accelerated approval, rather than traditional approval, because the drug has not yet shown a clinical benefit. Accelerated approval of a drug is based
on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to
predict clinical benefit.
PCYC-1104 trial
The data published in NEJM included 111 patients who received ibrutinib at 560 mg daily in continuous, 28-day cycles until disease progression.
The
overall response rate was 68%, with a complete response rate of 21% and
a partial response rate of 47%. With an estimated median follow-up of
15.3 months, the estimated median response duration was 17.5 months.
The
estimated progression-free survival was 13.9 months, and the overall
survival was not reached. The estimated rate of overall survival was 58%
at 18 months.
Common nonhematologic adverse events included
diarrhea (50%), fatigue (41%), nausea (31%), peripheral edema (28%),
dyspnea (27%), constipation (25%), upper respiratory tract infection
(23%), vomiting (23%), and decreased appetite (21%). The most common
grade 3, 4, or 5 infection was pneumonia (6%).
Grade 3 and 4
hematologic adverse events included neutropenia (16%), thrombocytopenia
(11%), and anemia (10%). Grade 3 bleeding events occurred in 5 patients.
The “Warnings and Precautions” section of ibrutinib’s prescribing information notes that patients taking ibrutinib have experienced hemorrhage, fatal and non-fatal infections, myelosuppression, renal toxicity, second primary malignancies, and embryo-fetal toxicity.
For the full prescribing information, visit http://www.imbruvica.com/downloads/Prescribing_Information.pdf.
Ibrutinib is now commercially available. It is co-marketed by Pharmacyclics (based in Sunnyvale, California) and Janssen Biotech, Inc. (based in Raritan, New Jersey). ![]()

The US Food and Drug Administration (FDA) has has granted accelerated approval for
ibrutinib (Imbruvica) to treat patients with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
Ibrutinib works by inhibiting the function of Bruton’s tyrosine kinase, a molecule that plays an important role in the survival of malignant B cells.
The drug showed promising results in the phase 2 PCYC-1104 trial, which was presented at ASH 2012 and published in NEJM in August.
The FDA granted ibrutinib breakthrough therapy designation because of these results and the life-threatening nature of MCL. Ibrutinib is the second drug with breakthrough therapy designation to receive FDA approval.
The FDA granted ibrutinib accelerated approval, rather than traditional approval, because the drug has not yet shown a clinical benefit. Accelerated approval of a drug is based
on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to
predict clinical benefit.
PCYC-1104 trial
The data published in NEJM included 111 patients who received ibrutinib at 560 mg daily in continuous, 28-day cycles until disease progression.
The
overall response rate was 68%, with a complete response rate of 21% and
a partial response rate of 47%. With an estimated median follow-up of
15.3 months, the estimated median response duration was 17.5 months.
The
estimated progression-free survival was 13.9 months, and the overall
survival was not reached. The estimated rate of overall survival was 58%
at 18 months.
Common nonhematologic adverse events included
diarrhea (50%), fatigue (41%), nausea (31%), peripheral edema (28%),
dyspnea (27%), constipation (25%), upper respiratory tract infection
(23%), vomiting (23%), and decreased appetite (21%). The most common
grade 3, 4, or 5 infection was pneumonia (6%).
Grade 3 and 4
hematologic adverse events included neutropenia (16%), thrombocytopenia
(11%), and anemia (10%). Grade 3 bleeding events occurred in 5 patients.
The “Warnings and Precautions” section of ibrutinib’s prescribing information notes that patients taking ibrutinib have experienced hemorrhage, fatal and non-fatal infections, myelosuppression, renal toxicity, second primary malignancies, and embryo-fetal toxicity.
For the full prescribing information, visit http://www.imbruvica.com/downloads/Prescribing_Information.pdf.
Ibrutinib is now commercially available. It is co-marketed by Pharmacyclics (based in Sunnyvale, California) and Janssen Biotech, Inc. (based in Raritan, New Jersey). ![]()

The US Food and Drug Administration (FDA) has has granted accelerated approval for
ibrutinib (Imbruvica) to treat patients with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
Ibrutinib works by inhibiting the function of Bruton’s tyrosine kinase, a molecule that plays an important role in the survival of malignant B cells.
The drug showed promising results in the phase 2 PCYC-1104 trial, which was presented at ASH 2012 and published in NEJM in August.
The FDA granted ibrutinib breakthrough therapy designation because of these results and the life-threatening nature of MCL. Ibrutinib is the second drug with breakthrough therapy designation to receive FDA approval.
The FDA granted ibrutinib accelerated approval, rather than traditional approval, because the drug has not yet shown a clinical benefit. Accelerated approval of a drug is based
on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to
predict clinical benefit.
PCYC-1104 trial
The data published in NEJM included 111 patients who received ibrutinib at 560 mg daily in continuous, 28-day cycles until disease progression.
The
overall response rate was 68%, with a complete response rate of 21% and
a partial response rate of 47%. With an estimated median follow-up of
15.3 months, the estimated median response duration was 17.5 months.
The
estimated progression-free survival was 13.9 months, and the overall
survival was not reached. The estimated rate of overall survival was 58%
at 18 months.
Common nonhematologic adverse events included
diarrhea (50%), fatigue (41%), nausea (31%), peripheral edema (28%),
dyspnea (27%), constipation (25%), upper respiratory tract infection
(23%), vomiting (23%), and decreased appetite (21%). The most common
grade 3, 4, or 5 infection was pneumonia (6%).
Grade 3 and 4
hematologic adverse events included neutropenia (16%), thrombocytopenia
(11%), and anemia (10%). Grade 3 bleeding events occurred in 5 patients.
The “Warnings and Precautions” section of ibrutinib’s prescribing information notes that patients taking ibrutinib have experienced hemorrhage, fatal and non-fatal infections, myelosuppression, renal toxicity, second primary malignancies, and embryo-fetal toxicity.
For the full prescribing information, visit http://www.imbruvica.com/downloads/Prescribing_Information.pdf.
Ibrutinib is now commercially available. It is co-marketed by Pharmacyclics (based in Sunnyvale, California) and Janssen Biotech, Inc. (based in Raritan, New Jersey). ![]()
Ibrutinib approved for mantle cell lymphoma
Ibrutinib is now approved for the treatment of patients with mantle cell lymphoma who have received at least one prior therapy, the Food and Drug Administration announced Nov. 13.
The once-daily, oral therapy, marketed as Imbruvica, is the second drug to receive FDA approval under the breakthrough therapy designation established to speed the development and review of treatments for serious or life-threatening diseases.
"Imbruvica’s approval demonstrates the FDA’s commitment to making treatments available to patients with rare diseases," Dr. Richard Pazdur, director of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, said in a statement.
Mantle cell lymphoma is an orphan disease, with only about 2,900 new cases of MCL diagnosed each year. MCL comprises only about 6% of all non-Hodgkin’s lymphoma cases in the United States.
Ibrutinib’s approval comes a little more than 4 months after the new drug application was filed in June 2013 and is based on a phase II study reporting an investigator-assessed overall response rate of 66% at a daily dose of 560 mg ibrutinib in 111 patients with relapsed or refractory MCL after a median of three prior therapies. The median duration of response was 17.5 months. An improvement in survival and disease-related symptoms has not been established.
Ibrutinib works by blocking Bruton’s tyrosine kinase, a mediator of the B-cell receptor signaling pathway that has been shown in nonclinical studies to inhibit malignant B-cell survival.
The FDA also granted ibrutinib priority review and orphan-product designation, because the drug demonstrated "the potential to be a significant improvement in safety or effectiveness in the treatment of a serious condition and is intended to treat a rare disease," according to the FDA statement.
Ibrutinib is the third drug approved to treat MCL. In June 2013, the FDA approved the oral thalidomide analogue lenalidomide (Revlimid) for the treatment of MCL that had relapsed or progressed after two prior therapies including bortezomib (Velcade), a subcutaneous therapy that has been available for MCL since 2006.
"It is gratifying to see an early example of the new breakthrough therapy designation pathway meeting its intention – getting promising treatments to patients who are waiting for new options," Dr. Ellen V. Sigal, chairperson and founder of the Washington-based Friends of Cancer Research advocacy organization, said in a statement issued by Janssen Biotech, which is comarketing the drug with Pharmacyclics.
The two companies are expected to continue with phase III studies of ibrutinib and have also submitted the drug to the FDA for the treatment of previously treated chronic lymphocytic leukemia/small lymphocytic lymphoma.
In the pivotal MCL trial, the most common treatment-related adverse events with single-agent ibrutinib were mild or moderate diarrhea, fatigue, and nausea (N. Engl. J. Med. 2013;369:507-16). Grade 3 or higher hematologic events were neutropenia (16%), thrombocytopenia (11%), and anemia (10%).
Ibrutinib is now approved for the treatment of patients with mantle cell lymphoma who have received at least one prior therapy, the Food and Drug Administration announced Nov. 13.
The once-daily, oral therapy, marketed as Imbruvica, is the second drug to receive FDA approval under the breakthrough therapy designation established to speed the development and review of treatments for serious or life-threatening diseases.
"Imbruvica’s approval demonstrates the FDA’s commitment to making treatments available to patients with rare diseases," Dr. Richard Pazdur, director of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, said in a statement.
Mantle cell lymphoma is an orphan disease, with only about 2,900 new cases of MCL diagnosed each year. MCL comprises only about 6% of all non-Hodgkin’s lymphoma cases in the United States.
Ibrutinib’s approval comes a little more than 4 months after the new drug application was filed in June 2013 and is based on a phase II study reporting an investigator-assessed overall response rate of 66% at a daily dose of 560 mg ibrutinib in 111 patients with relapsed or refractory MCL after a median of three prior therapies. The median duration of response was 17.5 months. An improvement in survival and disease-related symptoms has not been established.
Ibrutinib works by blocking Bruton’s tyrosine kinase, a mediator of the B-cell receptor signaling pathway that has been shown in nonclinical studies to inhibit malignant B-cell survival.
The FDA also granted ibrutinib priority review and orphan-product designation, because the drug demonstrated "the potential to be a significant improvement in safety or effectiveness in the treatment of a serious condition and is intended to treat a rare disease," according to the FDA statement.
Ibrutinib is the third drug approved to treat MCL. In June 2013, the FDA approved the oral thalidomide analogue lenalidomide (Revlimid) for the treatment of MCL that had relapsed or progressed after two prior therapies including bortezomib (Velcade), a subcutaneous therapy that has been available for MCL since 2006.
"It is gratifying to see an early example of the new breakthrough therapy designation pathway meeting its intention – getting promising treatments to patients who are waiting for new options," Dr. Ellen V. Sigal, chairperson and founder of the Washington-based Friends of Cancer Research advocacy organization, said in a statement issued by Janssen Biotech, which is comarketing the drug with Pharmacyclics.
The two companies are expected to continue with phase III studies of ibrutinib and have also submitted the drug to the FDA for the treatment of previously treated chronic lymphocytic leukemia/small lymphocytic lymphoma.
In the pivotal MCL trial, the most common treatment-related adverse events with single-agent ibrutinib were mild or moderate diarrhea, fatigue, and nausea (N. Engl. J. Med. 2013;369:507-16). Grade 3 or higher hematologic events were neutropenia (16%), thrombocytopenia (11%), and anemia (10%).
Ibrutinib is now approved for the treatment of patients with mantle cell lymphoma who have received at least one prior therapy, the Food and Drug Administration announced Nov. 13.
The once-daily, oral therapy, marketed as Imbruvica, is the second drug to receive FDA approval under the breakthrough therapy designation established to speed the development and review of treatments for serious or life-threatening diseases.
"Imbruvica’s approval demonstrates the FDA’s commitment to making treatments available to patients with rare diseases," Dr. Richard Pazdur, director of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, said in a statement.
Mantle cell lymphoma is an orphan disease, with only about 2,900 new cases of MCL diagnosed each year. MCL comprises only about 6% of all non-Hodgkin’s lymphoma cases in the United States.
Ibrutinib’s approval comes a little more than 4 months after the new drug application was filed in June 2013 and is based on a phase II study reporting an investigator-assessed overall response rate of 66% at a daily dose of 560 mg ibrutinib in 111 patients with relapsed or refractory MCL after a median of three prior therapies. The median duration of response was 17.5 months. An improvement in survival and disease-related symptoms has not been established.
Ibrutinib works by blocking Bruton’s tyrosine kinase, a mediator of the B-cell receptor signaling pathway that has been shown in nonclinical studies to inhibit malignant B-cell survival.
The FDA also granted ibrutinib priority review and orphan-product designation, because the drug demonstrated "the potential to be a significant improvement in safety or effectiveness in the treatment of a serious condition and is intended to treat a rare disease," according to the FDA statement.
Ibrutinib is the third drug approved to treat MCL. In June 2013, the FDA approved the oral thalidomide analogue lenalidomide (Revlimid) for the treatment of MCL that had relapsed or progressed after two prior therapies including bortezomib (Velcade), a subcutaneous therapy that has been available for MCL since 2006.
"It is gratifying to see an early example of the new breakthrough therapy designation pathway meeting its intention – getting promising treatments to patients who are waiting for new options," Dr. Ellen V. Sigal, chairperson and founder of the Washington-based Friends of Cancer Research advocacy organization, said in a statement issued by Janssen Biotech, which is comarketing the drug with Pharmacyclics.
The two companies are expected to continue with phase III studies of ibrutinib and have also submitted the drug to the FDA for the treatment of previously treated chronic lymphocytic leukemia/small lymphocytic lymphoma.
In the pivotal MCL trial, the most common treatment-related adverse events with single-agent ibrutinib were mild or moderate diarrhea, fatigue, and nausea (N. Engl. J. Med. 2013;369:507-16). Grade 3 or higher hematologic events were neutropenia (16%), thrombocytopenia (11%), and anemia (10%).