User login
Diastolic heart failure and TOPCAT
The TOPCAT study, reported at the recent American Heart Association meeting in Dallas, examined the murky world of our understanding of heart failure occurring in patients with preserved left ventricular ejection fraction.
That seeming paradox has been the subject of physiologic and therapeutic controversy for some time. The realization that at least half of the patients admitted to the hospital with heart failure have normal or even supernormal left ventricular ejection fraction (HFpEF) has raised the therapeutic importance of this clinical entity. Of even more importance is the fact that patients with HFpEF exhibit morbidity and mortality similar to those heart failure patients with reduced left ventricular ejection fraction (HFrEF).
In an epidemiologic study in Olmsted County, Minnesota (N. Engl. J. Med. 2006;355:251-9), the 1-year mortality was 29% for HFpEF and 32% for HFrEF. Patients with HFpEF were more likely to be female (65.7% vs. 34.6%) and to have hypertension and atrial fibrillation than were those with HFrEF (62.7% vs. 48% and 41.3% vs. 28.5%, respectively).
Although we have significantly impacted mortality in patients who have HFrEF with the use of cardiac resynchronization therapy, implantable cardiac defibrillators, and medical therapy with beta-blockers and renin angiotensin inhibitors, we have failed to modify clinical outcomes in patients with HFpEF.
This has not been for a lack of trying. Several randomized clinical trials have been conducted with all of the drugs currently being used for HFrEF without any definitive results. An important problem in treating this population has been the heterogeneity of patients and multiple comorbidities, including chronic renal and pulmonary disease, acute hypertension, and atrial fibrillation that patients with HFpEF experience with the acute event. In addition, many of these patients are already receiving a multiplicity of concurrent therapies that have been approved for HFrEF for management.
Our understanding of the pathophysiology of HFpEF also remains cloudy. Both left and right ventricular hypertrophy with concomitant decrease in ventricular diastolic relaxation is the common observed echocardiographic abnormality. We have not as yet developed therapy for the treatment of diastolic dysfunction. Aldosterone antagonists, previously shown to be beneficial in patients with HFrEF, have emerged as likely candidates to improve HFpEF. Small clinical studies have shown improvement in diastolic function in elderly patients with hypertension and chronic renal disease. Consequently, the National Heart, Lung, and Blood Institute embarked on the TOPCAT study in 2006.
TOPCAT randomized 3,345 symptomatic heart failure patients who had a heart failure hospitalization in the previous year and with evidence of fluid retention, a left ventricular ejection fraction of more than 45%, controlled systolic blood pressure of less than 140 mm Hg, and elevated brain natriuretic peptide to treatment with placebo or spironolactone at 25 or 50 mg daily. A history of hypertension was present in 91%, coronary artery disease in 57%, atrial fibrillation in 35%, chronic renal disease in 35%, and diabetes in 32%. Patients included in the study had a mean LVEF of 56%; two thirds were in New York Heart Association class II and one third were in NYHA class III.
Over 80% of patients were receiving an ACE inhibitor or angiotensin receptor blocker, beta-blockers, and a diuretic. The mean dose of spironolactone was 25 mg. There was no significant difference in the primary outcome of cardiovascular death, nonfatal hospitalization or resuscitated cardiac arrest in the placebo and treated groups (20.4% and 18.6%, respectively). There was a significant decrease in heart failure hospitalization in the placebo compared to spironolactone patients (14.2% vs. 12.0%; P = .042). Both hyperkalemia greater than 5.5 mmol/L and an increase in serum creatinine were observed in the treated patients.
The striking observation in this trial, as it has been in previous trials, is the disparity between the epidemiologic mortality and the randomized controlled trial experience: 29% annual mortality in Olmsted County, compared with the 10.2% three-year mortality in TOPCAT. It appears that we are studying two separate diseases. And we are. After all the exclusion criteria included in the design of TOPCAT, we are unable to encapsulate the population at risk in this complex heart failure syndrome.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The TOPCAT study, reported at the recent American Heart Association meeting in Dallas, examined the murky world of our understanding of heart failure occurring in patients with preserved left ventricular ejection fraction.
That seeming paradox has been the subject of physiologic and therapeutic controversy for some time. The realization that at least half of the patients admitted to the hospital with heart failure have normal or even supernormal left ventricular ejection fraction (HFpEF) has raised the therapeutic importance of this clinical entity. Of even more importance is the fact that patients with HFpEF exhibit morbidity and mortality similar to those heart failure patients with reduced left ventricular ejection fraction (HFrEF).
In an epidemiologic study in Olmsted County, Minnesota (N. Engl. J. Med. 2006;355:251-9), the 1-year mortality was 29% for HFpEF and 32% for HFrEF. Patients with HFpEF were more likely to be female (65.7% vs. 34.6%) and to have hypertension and atrial fibrillation than were those with HFrEF (62.7% vs. 48% and 41.3% vs. 28.5%, respectively).
Although we have significantly impacted mortality in patients who have HFrEF with the use of cardiac resynchronization therapy, implantable cardiac defibrillators, and medical therapy with beta-blockers and renin angiotensin inhibitors, we have failed to modify clinical outcomes in patients with HFpEF.
This has not been for a lack of trying. Several randomized clinical trials have been conducted with all of the drugs currently being used for HFrEF without any definitive results. An important problem in treating this population has been the heterogeneity of patients and multiple comorbidities, including chronic renal and pulmonary disease, acute hypertension, and atrial fibrillation that patients with HFpEF experience with the acute event. In addition, many of these patients are already receiving a multiplicity of concurrent therapies that have been approved for HFrEF for management.
Our understanding of the pathophysiology of HFpEF also remains cloudy. Both left and right ventricular hypertrophy with concomitant decrease in ventricular diastolic relaxation is the common observed echocardiographic abnormality. We have not as yet developed therapy for the treatment of diastolic dysfunction. Aldosterone antagonists, previously shown to be beneficial in patients with HFrEF, have emerged as likely candidates to improve HFpEF. Small clinical studies have shown improvement in diastolic function in elderly patients with hypertension and chronic renal disease. Consequently, the National Heart, Lung, and Blood Institute embarked on the TOPCAT study in 2006.
TOPCAT randomized 3,345 symptomatic heart failure patients who had a heart failure hospitalization in the previous year and with evidence of fluid retention, a left ventricular ejection fraction of more than 45%, controlled systolic blood pressure of less than 140 mm Hg, and elevated brain natriuretic peptide to treatment with placebo or spironolactone at 25 or 50 mg daily. A history of hypertension was present in 91%, coronary artery disease in 57%, atrial fibrillation in 35%, chronic renal disease in 35%, and diabetes in 32%. Patients included in the study had a mean LVEF of 56%; two thirds were in New York Heart Association class II and one third were in NYHA class III.
Over 80% of patients were receiving an ACE inhibitor or angiotensin receptor blocker, beta-blockers, and a diuretic. The mean dose of spironolactone was 25 mg. There was no significant difference in the primary outcome of cardiovascular death, nonfatal hospitalization or resuscitated cardiac arrest in the placebo and treated groups (20.4% and 18.6%, respectively). There was a significant decrease in heart failure hospitalization in the placebo compared to spironolactone patients (14.2% vs. 12.0%; P = .042). Both hyperkalemia greater than 5.5 mmol/L and an increase in serum creatinine were observed in the treated patients.
The striking observation in this trial, as it has been in previous trials, is the disparity between the epidemiologic mortality and the randomized controlled trial experience: 29% annual mortality in Olmsted County, compared with the 10.2% three-year mortality in TOPCAT. It appears that we are studying two separate diseases. And we are. After all the exclusion criteria included in the design of TOPCAT, we are unable to encapsulate the population at risk in this complex heart failure syndrome.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The TOPCAT study, reported at the recent American Heart Association meeting in Dallas, examined the murky world of our understanding of heart failure occurring in patients with preserved left ventricular ejection fraction.
That seeming paradox has been the subject of physiologic and therapeutic controversy for some time. The realization that at least half of the patients admitted to the hospital with heart failure have normal or even supernormal left ventricular ejection fraction (HFpEF) has raised the therapeutic importance of this clinical entity. Of even more importance is the fact that patients with HFpEF exhibit morbidity and mortality similar to those heart failure patients with reduced left ventricular ejection fraction (HFrEF).
In an epidemiologic study in Olmsted County, Minnesota (N. Engl. J. Med. 2006;355:251-9), the 1-year mortality was 29% for HFpEF and 32% for HFrEF. Patients with HFpEF were more likely to be female (65.7% vs. 34.6%) and to have hypertension and atrial fibrillation than were those with HFrEF (62.7% vs. 48% and 41.3% vs. 28.5%, respectively).
Although we have significantly impacted mortality in patients who have HFrEF with the use of cardiac resynchronization therapy, implantable cardiac defibrillators, and medical therapy with beta-blockers and renin angiotensin inhibitors, we have failed to modify clinical outcomes in patients with HFpEF.
This has not been for a lack of trying. Several randomized clinical trials have been conducted with all of the drugs currently being used for HFrEF without any definitive results. An important problem in treating this population has been the heterogeneity of patients and multiple comorbidities, including chronic renal and pulmonary disease, acute hypertension, and atrial fibrillation that patients with HFpEF experience with the acute event. In addition, many of these patients are already receiving a multiplicity of concurrent therapies that have been approved for HFrEF for management.
Our understanding of the pathophysiology of HFpEF also remains cloudy. Both left and right ventricular hypertrophy with concomitant decrease in ventricular diastolic relaxation is the common observed echocardiographic abnormality. We have not as yet developed therapy for the treatment of diastolic dysfunction. Aldosterone antagonists, previously shown to be beneficial in patients with HFrEF, have emerged as likely candidates to improve HFpEF. Small clinical studies have shown improvement in diastolic function in elderly patients with hypertension and chronic renal disease. Consequently, the National Heart, Lung, and Blood Institute embarked on the TOPCAT study in 2006.
TOPCAT randomized 3,345 symptomatic heart failure patients who had a heart failure hospitalization in the previous year and with evidence of fluid retention, a left ventricular ejection fraction of more than 45%, controlled systolic blood pressure of less than 140 mm Hg, and elevated brain natriuretic peptide to treatment with placebo or spironolactone at 25 or 50 mg daily. A history of hypertension was present in 91%, coronary artery disease in 57%, atrial fibrillation in 35%, chronic renal disease in 35%, and diabetes in 32%. Patients included in the study had a mean LVEF of 56%; two thirds were in New York Heart Association class II and one third were in NYHA class III.
Over 80% of patients were receiving an ACE inhibitor or angiotensin receptor blocker, beta-blockers, and a diuretic. The mean dose of spironolactone was 25 mg. There was no significant difference in the primary outcome of cardiovascular death, nonfatal hospitalization or resuscitated cardiac arrest in the placebo and treated groups (20.4% and 18.6%, respectively). There was a significant decrease in heart failure hospitalization in the placebo compared to spironolactone patients (14.2% vs. 12.0%; P = .042). Both hyperkalemia greater than 5.5 mmol/L and an increase in serum creatinine were observed in the treated patients.
The striking observation in this trial, as it has been in previous trials, is the disparity between the epidemiologic mortality and the randomized controlled trial experience: 29% annual mortality in Olmsted County, compared with the 10.2% three-year mortality in TOPCAT. It appears that we are studying two separate diseases. And we are. After all the exclusion criteria included in the design of TOPCAT, we are unable to encapsulate the population at risk in this complex heart failure syndrome.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
UCSF Hospitalist Mini‐College
I hear and I forget, I see and I remember, I do and I understand.
Confucius
Hospital medicine, first described in 1996,[1] is the fastest growing specialty in United States medical history, now with approximately 40,000 practitioners.[2] Although hospitalists undoubtedly learned many of their key clinical skills during residency training, there is no hospitalist‐specific residency training pathway and a limited number of largely research‐oriented fellowships.[3] Furthermore, hospitalists are often asked to care for surgical patients, those with acute neurologic disorders, and patients in intensive care units, while also contributing to quality improvement and patient safety initiatives.[4] This suggests that the vast majority of hospitalists have not had specific training in many key competencies for the field.[5]
Continuing medical education (CME) has traditionally been the mechanism to maintain, develop, or increase the knowledge, skills, and professional performance of physicians.[6] Most CME activities, including those for hospitalists, are staged as live events in hotel conference rooms or as local events in a similarly passive learning environment (eg, grand rounds and medical staff meetings). Online programs, audiotapes, and expanding electronic media provide increasing and alternate methods for hospitalists to obtain their required CME. All of these activities passively deliver content to a group of diverse and experienced learners. They fail to take advantage of adult learning principles and may have little direct impact on professional practice.[7, 8] Traditional CME is often derided as a barrier to innovative educational methods for these reasons, as adults learn best through active participation, when the information is relevant and practically applied.[9, 10]
To provide practicing hospitalists with necessary continuing education, we designed the University of California, San Francisco (UCSF) Hospitalist Mini‐College (UHMC). This 3‐day course brings adult learners to the bedside for small‐group and active learning focused on content areas relevant to today's hospitalists. We describe the development, content, outcomes, and lessons learned from UHMC's first 5 years.
METHODS
Program Development
We aimed to develop a program that focused on curricular topics that would be highly valued by practicing hospitalists delivered in an active learning small‐group environment. We first conducted an informal needs assessment of community‐based hospitalists to better understand their roles and determine their perceptions of gaps in hospitalist training compared to current requirements for practice. We then reviewed available CME events targeting hospitalists and compared these curricula to the gaps discovered from the needs assessment. We also reviewed the Society of Hospital Medicine's core competencies to further identify gaps in scope of practice.[4] Finally, we reviewed the literature to identify CME curricular innovations in the clinical setting and found no published reports.
Program Setting, Participants, and Faculty
The UHMC course was developed and offered first in 2008 as a precourse to the UCSF Management of the Hospitalized Medicine course, a traditional CME offering that occurs annually in a hotel setting.[11] The UHMC takes place on the campus of UCSF Medical Center, a 600‐bed academic medical center in San Francisco. Registered participants were required to complete limited credentialing paperwork, which allowed them to directly observe clinical care and interact with hospitalized patients. Participants were not involved in any clinical decision making for the patients they met or examined. The course was limited to a maximum of 33 participants annually to optimize active participation, small‐group bedside activities, and a personalized learning experience. UCSF faculty selected to teach in the UHMC were chosen based on exemplary clinical and teaching skills. They collaborated with course directors in the development of their session‐specific goals and curriculum.
Program Description
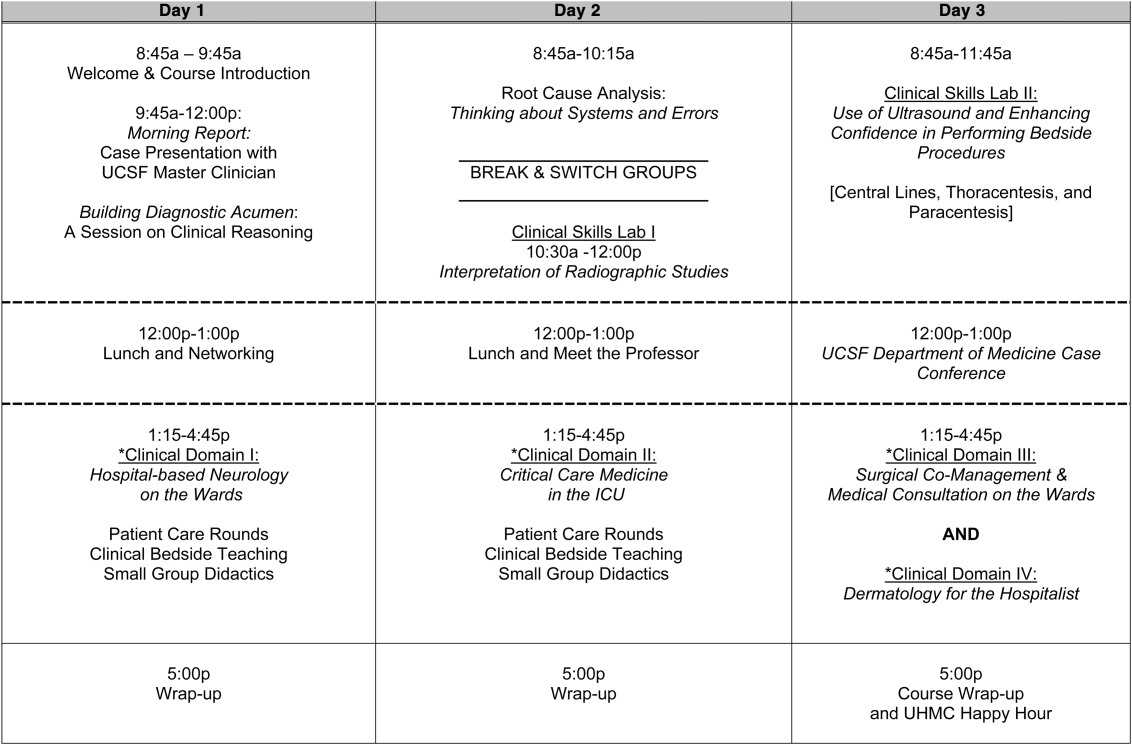
Figure 1 is a representative calendar view of the 3‐day UHMC course. The curricular topics were selected based on the findings from our needs assessment, our ability to deliver that curriculum using our small‐group active learning framework, and to minimize overlap with content of the larger course. Course curriculum was refined annually based on participant feedback and course director observations.
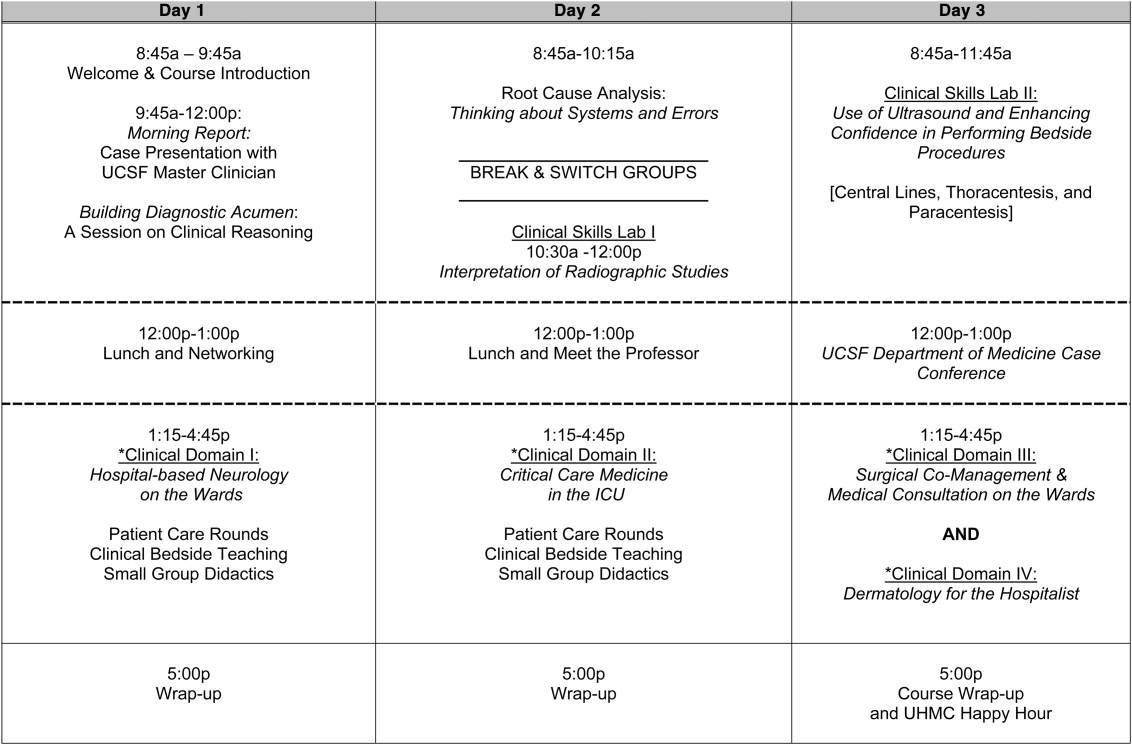
The program was built on a structure of 4 clinical domains and 2 clinical skills labs. The clinical domains included: (1) Hospital‐Based Neurology, (2) Critical Care Medicine in the Intensive Care Unit, (3) Surgical Comanagement and Medical Consultation, and (4) Hospital‐Based Dermatology. Participants were divided into 3 groups of 10 participants each and rotated through each domain in the afternoons. The clinical skills labs included: (1) Interpretation of Radiographic Studies and (2) Use of Ultrasound and Enhancing Confidence in Performing Bedside Procedures. We also developed specific sessions to teach about patient safety and to allow course attendees to participate in traditional academic learning vehicles (eg, a Morning Report and Morbidity and Mortality case conference). Below, we describe each session's format and content.
Clinical Domains
Hospital‐Based Neurology
Attendees participated in both bedside evaluation and case‐based discussions of common neurologic conditions seen in the hospital. In small groups of 5, participants were assigned patients to examine on the neurology ward. After their evaluations, they reported their findings to fellow participants and the faculty, setting the foundation for discussion of clinical management, review of neuroimaging, and exploration of current evidence to inform the patient's diagnosis and management. Participants and faculty then returned to the bedside to hone neurologic examination skills and complete the learning process. Given the unpredictability of what conditions would be represented on the ward in a given day, review of commonly seen conditions was always a focus, such as stroke, seizures, delirium, and neurologic examination pearls.
Critical Care
Attendees participated in case‐based discussions of common clinical conditions with similar review of current evidence, relevant imaging, and bedside exam pearls for the intubated patient. For this domain, attendees also participated in an advanced simulation tutorial in ventilator management, which was then applied at the bedside of intubated patients. Specific topics covered include sepsis, decompensated chronic obstructive lung disease, vasopressor selection, novel therapies in critically ill patients, and use of clinical pathways and protocols for improved quality of care.
Surgical Comanagement and Medical Consultation
Attendees participated in case‐based discussions applying current evidence to perioperative controversies and the care of the surgical patient. They also discussed the expanding role of the hospitalist in nonmedical patients.
Hospital‐Based Dermatology
Attendees participated in bedside evaluation of acute skin eruptions based on available patients admitted to the hospital. They discussed the approach to skin eruptions, key diagnoses, and when dermatologists should be consulted for their expertise. Specific topics included drug reactions, the red leg, life‐threating conditions (eg, Stevens‐Johnson syndrome), and dermatologic examination pearls. This domain was added in 2010.
Clinical Skills Labs
Radiology
In groups of 15, attendees reviewed common radiographs that hospitalists frequently order or evaluate (eg, chest x‐rays; kidney, ureter, and bladder; placement of endotracheal or feeding tube). They also reviewed the most relevant and not‐to‐miss findings on other commonly ordered studies such as abdominal or brain computerized tomography scans.
Hospital Procedures With Bedside Ultrasound
Attendees participated in a half‐day session to gain experience with the following procedures: paracentesis, lumbar puncture, thoracentesis, and central lines. They participated in an initial overview of procedural safety followed by hands‐on application sessions, in which they rotated through clinical workstations in groups of 5. At each work station, they were provided an opportunity to practice techniques, including the safe use of ultrasound on both live (standardized patients) and simulation models.
Other Sessions
Building Diagnostic Acumen and Clinical Reasoning
The opening session of the UHMC reintroduces attendees to the traditional academic morning report format, in which a case is presented and participants are asked to assess the information, develop differential diagnoses, discuss management options, and consider their own clinical reasoning skills. This provides frameworks for diagnostic reasoning, highlights common cognitive errors, and teaches attendees how to develop expertise in their own diagnostic thinking. The session also sets the stage and expectation for active learning and participation in the UHMC.
Root Cause Analysis and Systems Thinking
As the only nonclinical session in the UHMC, this session introduces participants to systems thinking and patient safety. Attendees participate in a root cause analysis role play surrounding a serious medical error and discuss the implications, their reflections, and then propose solutions through interactive table discussions. The session also emphasizes the key role hospitalists should play in improving patient safety.
Clinical Case Conference
Attendees participated in the weekly UCSF Department of Medicine Morbidity and Mortality conference. This is a traditional case conference that brings together learners, expert discussants, and an interesting or challenging case. This allows attendees to synthesize much of the course learning through active participation in the case discussion. Rather than creating a new conference for the participants, we brought the participants to the existing conference as part of their UHMC immersion experience.
Meet the Professor
Attendees participated in an informal discussion with a national leader (R.M.W.) in hospital medicine. This allowed for an interactive exchange of ideas and an understanding of the field overall.
Online Search Strategies
This interactive computer lab session allowed participants to explore the ever‐expanding number of online resources to answer clinical queries. This session was replaced in 2010 with the dermatology clinical domain based on participant feedback.
Program Evaluation
Participants completed a pre‐UHMC survey that provided demographic information and attributes about themselves, their clinical practice, and experience. Participants also completed course evaluations consistent with Accreditation Council for Continuing Medical Education standards following the program. The questions asked for each activity were rated on a 1‐to‐5 scale (1=poor, 5=excellent) and also included open‐ended questions to assess overall experiences.
RESULTS
Participant Demographics
During the first 5 years of the UHMC, 152 participants enrolled and completed the program; 91% completed the pre‐UHMC survey and 89% completed the postcourse evaluation. Table 1 describes the self‐reported participant demographics, including years in practice, number of hospitalist jobs, overall job satisfaction, and time spent doing clinical work. Overall, 68% of all participants had been self‐described hospitalists for 4 years, with 62% holding only 1 hospitalist job during that time; 77% reported being pretty or very satisfied with their jobs, and 72% reported clinical care as the attribute they love most in their job. Table 2 highlights the type of work attendees participate in within their clinical practice. More than half manage patients with neurologic disorders and care for critically ill patients, whereas virtually all perform preoperative medical evaluations and medical consultation
| Question | Response Options | 2008 (n=4) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average (n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| How long have you been a hospitalist? | 2 years | 52% | 35% | 37% | 30% | 25% | 36% |
| 24 years | 26% | 39% | 30% | 30% | 38% | 32% | |
| 510 years | 11% | 17% | 15% | 26% | 29% | 20% | |
| >10 years | 11% | 9% | 18% | 14% | 8% | 12% | |
| How many hospitalist jobs have you had? | 1 | 63% | 61% | 62% | 62% | 58% | 62% |
| 2 to 3 | 37% | 35% | 23% | 35% | 29% | 32% | |
| >3 | 0% | 4% | 15% | 1% | 13% | 5% | |
| How satisfied are you with your current position? | Not satisfied | 1% | 4% | 4% | 4% | 0% | 4% |
| Somewhat satisfied | 11% | 13% | 39% | 17% | 17% | 19% | |
| Pretty satisfied | 59% | 52% | 35% | 57% | 38% | 48% | |
| Very satisfied | 26% | 30% | 23% | 22% | 46% | 29% | |
| What do you love most about your job? | Clinical care | 85% | 61% | 65% | 84% | 67% | 72% |
| Teaching | 1% | 17% | 12% | 1% | 4% | 7% | |
| QI or safety work | 0% | 4% | 0% | 1% | 8% | 3% | |
| Other (not specified) | 14% | 18% | 23% | 14% | 21% | 18% | |
| What percent of your time is spent doing clinical care? | 100% | 39% | 36% | 52% | 46% | 58% | 46% |
| 75%100% | 58% | 50% | 37% | 42% | 33% | 44% | |
| 5075% | 0% | 9% | 11% | 12% | 4% | 7% | |
| 25%50% | 4% | 5% | 0% | 0% | 5% | 3% | |
| 25% | 0% | 0% | 0% | 0% | 0% | 0% | |
| Question | Response Options | 2008 (n=24) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average(n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| Do you primarily manage patients with neurologic disorders in your hospital? | Yes | 62% | 50% | 62% | 62% | 63% | 60% |
| Do you primarily manage critically ill ICU patients in your hospital? | Yes and without an intensivist | 19% | 23% | 19% | 27% | 21% | 22% |
| Yes but with an intensivist | 54% | 50% | 44% | 42% | 67% | 51% | |
| No | 27% | 27% | 37% | 31% | 13% | 27% | |
| Do you perform preoperative medical evaluations and medical consultation? | Yes | 96% | 91% | 96% | 96% | 92% | 94% |
| Which of the following describes your role in the care of surgical patients? | Traditional medical consultant | 33% | 28% | 28% | 30% | 24% | 29% |
| Comanagement (shared responsibility with surgeon) | 33% | 34% | 42% | 39% | 35% | 37% | |
| Attending of record with surgeon acting as consultant | 26% | 24% | 26% | 30% | 35% | 28% | |
| Do you have bedside ultrasound available in your daily practice? | Yes | 38% | 32% | 52% | 34% | 38% | 39% |
Participant Experience
Overall, participants rated the quality of the UHMC course highly (4.65; 15 scale). The neurology clinical domain (4.83) and clinical reasoning session (4.72) were the highest‐rated sessions. Compared to all UCSF CME course offerings between January 2010 and September 2012, the UHMC rated higher than the cumulative overall rating from those 227 courses (4.65 vs 4.44). For UCSF CME courses offered in 2011 and 2012, 78% of participants (n=11,447) reported a high or definite likelihood to change practice. For UHMC participants during the same time period (n=57), 98% reported a similar likelihood to change practice. Table 3 provides selected participant comments from their postcourse evaluations.
|
| Great pearls, broad ranging discussion of many controversial and common topics, and I loved the teaching format. |
| I thought the conception of the teaching model was really effectivehands‐on exams in small groups, each demonstrating a different part of the neurologic exam, followed by presentation and discussion, and ending in bedside rounds with the teaching faculty. |
| Excellent review of key topicswide variety of useful and practical points. Very high application value. |
| Great course. I'd take it again and again. It was a superb opportunity to review technique, equipment, and clinical decision making. |
| Overall outstanding course! Very informative and fun. Format was great. |
| Forward and clinically relevant. Like the bedside teaching and how they did it.The small size of the course and the close attention paid by the faculty teaching the course combined with the opportunity to see and examine patients in the hospital was outstanding. |
DISCUSSION
We developed an innovative CME program that brought participants to an academic health center for a participatory, hands‐on, and small‐group experience. They learned about topics relevant to today's hospitalists, rated the experience very highly, and reported a nearly unanimous likelihood to change their practice. Reflecting on our program's first 5 years, there were several lessons learned that may guide others committed to providing a similar CME experience.
First, hospital medicine is a dynamic field. Conducting a needs assessment to match clinical topics to what attendees required in their own practice was critical. Iterative changes from year to year reflected formal participant feedback as well as informal conversations with the teaching faculty. For instance, attendees were not only interested in the clinical topics but often wanted to see examples of clinical pathways, order sets, and other systems in place to improve care for patients with common conditions. Our participant presurvey also helped identify and reinforce the curricular topics that teaching faculty focused on each year. Being responsive to the changing needs of hospitalists and the environment is a crucial part of providing a relevant CME experience.
We also used an innovative approach to teaching, founded in adult and effective CME learning principles. CME activities are geared toward adult physicians, and studies of their effectiveness recommend that sessions should be interactive and utilize multiple modalities of learning.[12] When attendees actively participate and are provided an opportunity to practice skills, it may have a positive effect on patient outcomes.[13] All UHMC faculty were required to couple presentations of the latest evidence for clinical topics with small‐group and hands‐on learning modalities. This also required that we utilize a teaching faculty known for both their clinical expertise and teaching recognition. Together, the learning modalities and the teaching faculty likely accounted for the highly rated course experience and likelihood to change practice.
Finally, our course brought participants to an academic medical center and into the mix of clinical care as opposed to the more traditional hotel venue. This was necessary to deliver the curriculum as described, but also had the unexpected benefit of energizing the participants. Many had not been in a teaching setting since their residency training, and bringing them back into this milieu motivated them to learn and share their inspiration. As there are no published studies of CME experiences in the clinical environment, this observation is noteworthy and deserves to be explored and evaluated further.
What are the limitations of our approach to bringing CME to the bedside? First, the economics of an intensive 3‐day course with a maximum of 33 attendees are far different than those of a large hotel‐based offering. There are no exhibitors or outside contributions. The cost of the course to participants is $2500 (discounted if attending the larger course as well), which is 2 to 3 times higher than most traditional CME courses of the same length. Although the cost is high, the course has sold out each year with a waiting list. Part of the cost is also faculty time. The time, preparation, and need to teach on the fly to meet the differing participant educational needs is fundamentally different than delivering a single lecture in a hotel conference room. Not surprisingly, our faculty enjoy this teaching opportunity and find it equally unique and valuable; no faculty have dropped out of teaching the course, and many describe it as 1 of the teaching highlights of the year. Scalability of the UHMC is challenging for these reasons, but our model could be replicated in other teaching institutions, even as a local offering for their own providers.
In summary, we developed a hospital‐based, highly interactive, small‐group CME course that emphasizes case‐based teaching. The course has sold out each year, and evaluations suggest that it is highly valued and is meeting curricular goals better than more traditional CME courses. We hope our course description and success may motivate others to consider moving beyond the traditional CME for hospitalists and explore further innovations. With the field growing and changing at a rapid pace, innovative CME experiences will be necessary to assure that hospitalists continue to provide exemplary and safe care to their patients.
Acknowledgements
The authors thank Kapo Tam for her program management of the UHMC, and Katherine Li and Zachary Martin for their invaluable administrative support and coordination. The authors are also indebted to faculty colleagues for their time and roles in teaching within the program. They include Gupreet Dhaliwal, Andy Josephson, Vanja Douglas, Michelle Milic, Brian Daniels, Quinny Cheng, Lindy Fox, Diane Sliwka, Ralph Wang, and Thomas Urbania.
Disclosure: Nothing to report.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;337(7):514–517.
- Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Membership2/HospitalFocusedPractice/Hospital_Focused_Pra.htm. Accessed October 1, 2013.
- , , , . Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1–e7.
- Society of Hospital Medicine. Core competencies in hospital medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 1, 2013.
- , . The expanding role of hospitalists in the United States. Swiss Med Wkly. 2006;136(37‐38);591–596.
- Accreditation Council for Continuing Medical Education. CME content: definition and examples Available at: http://www.accme.org/requirements/accreditation‐requirements‐cme‐providers/policies‐and‐definitions/cme‐content‐definition‐and‐examples. Accessed October 1, 2013.
- , , , . Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–705.
- , . Continuing medical education and the physician as a learner: guide to the evidence. JAMA. 2002;288(9):1057–1060.
- , , , , . Barriers to innovation in continuing medical eduation. J Contin Educ Health Prof. 2008;28(3):148–156.
- . Adult learning theory for the 21st century. In: Merriam S. Thrid Update on Adult Learning Theory: New Directions for Adult and Continuing Education. San Francisco, CA: Jossey‐Bass; 2008:93–98.
- .UCSF management of the hospitalized patient CME course. Available at: http://www.ucsfcme.com/2014/MDM14P01/info.html. Accessed October 1, 2013.
- Continuing medical education effect on practice performance: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);42S–48S.
- Continuing medical education effect on clinical outcomes: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);49S–55S.
I hear and I forget, I see and I remember, I do and I understand.
Confucius
Hospital medicine, first described in 1996,[1] is the fastest growing specialty in United States medical history, now with approximately 40,000 practitioners.[2] Although hospitalists undoubtedly learned many of their key clinical skills during residency training, there is no hospitalist‐specific residency training pathway and a limited number of largely research‐oriented fellowships.[3] Furthermore, hospitalists are often asked to care for surgical patients, those with acute neurologic disorders, and patients in intensive care units, while also contributing to quality improvement and patient safety initiatives.[4] This suggests that the vast majority of hospitalists have not had specific training in many key competencies for the field.[5]
Continuing medical education (CME) has traditionally been the mechanism to maintain, develop, or increase the knowledge, skills, and professional performance of physicians.[6] Most CME activities, including those for hospitalists, are staged as live events in hotel conference rooms or as local events in a similarly passive learning environment (eg, grand rounds and medical staff meetings). Online programs, audiotapes, and expanding electronic media provide increasing and alternate methods for hospitalists to obtain their required CME. All of these activities passively deliver content to a group of diverse and experienced learners. They fail to take advantage of adult learning principles and may have little direct impact on professional practice.[7, 8] Traditional CME is often derided as a barrier to innovative educational methods for these reasons, as adults learn best through active participation, when the information is relevant and practically applied.[9, 10]
To provide practicing hospitalists with necessary continuing education, we designed the University of California, San Francisco (UCSF) Hospitalist Mini‐College (UHMC). This 3‐day course brings adult learners to the bedside for small‐group and active learning focused on content areas relevant to today's hospitalists. We describe the development, content, outcomes, and lessons learned from UHMC's first 5 years.
METHODS
Program Development
We aimed to develop a program that focused on curricular topics that would be highly valued by practicing hospitalists delivered in an active learning small‐group environment. We first conducted an informal needs assessment of community‐based hospitalists to better understand their roles and determine their perceptions of gaps in hospitalist training compared to current requirements for practice. We then reviewed available CME events targeting hospitalists and compared these curricula to the gaps discovered from the needs assessment. We also reviewed the Society of Hospital Medicine's core competencies to further identify gaps in scope of practice.[4] Finally, we reviewed the literature to identify CME curricular innovations in the clinical setting and found no published reports.
Program Setting, Participants, and Faculty
The UHMC course was developed and offered first in 2008 as a precourse to the UCSF Management of the Hospitalized Medicine course, a traditional CME offering that occurs annually in a hotel setting.[11] The UHMC takes place on the campus of UCSF Medical Center, a 600‐bed academic medical center in San Francisco. Registered participants were required to complete limited credentialing paperwork, which allowed them to directly observe clinical care and interact with hospitalized patients. Participants were not involved in any clinical decision making for the patients they met or examined. The course was limited to a maximum of 33 participants annually to optimize active participation, small‐group bedside activities, and a personalized learning experience. UCSF faculty selected to teach in the UHMC were chosen based on exemplary clinical and teaching skills. They collaborated with course directors in the development of their session‐specific goals and curriculum.
Program Description
Figure 1 is a representative calendar view of the 3‐day UHMC course. The curricular topics were selected based on the findings from our needs assessment, our ability to deliver that curriculum using our small‐group active learning framework, and to minimize overlap with content of the larger course. Course curriculum was refined annually based on participant feedback and course director observations.
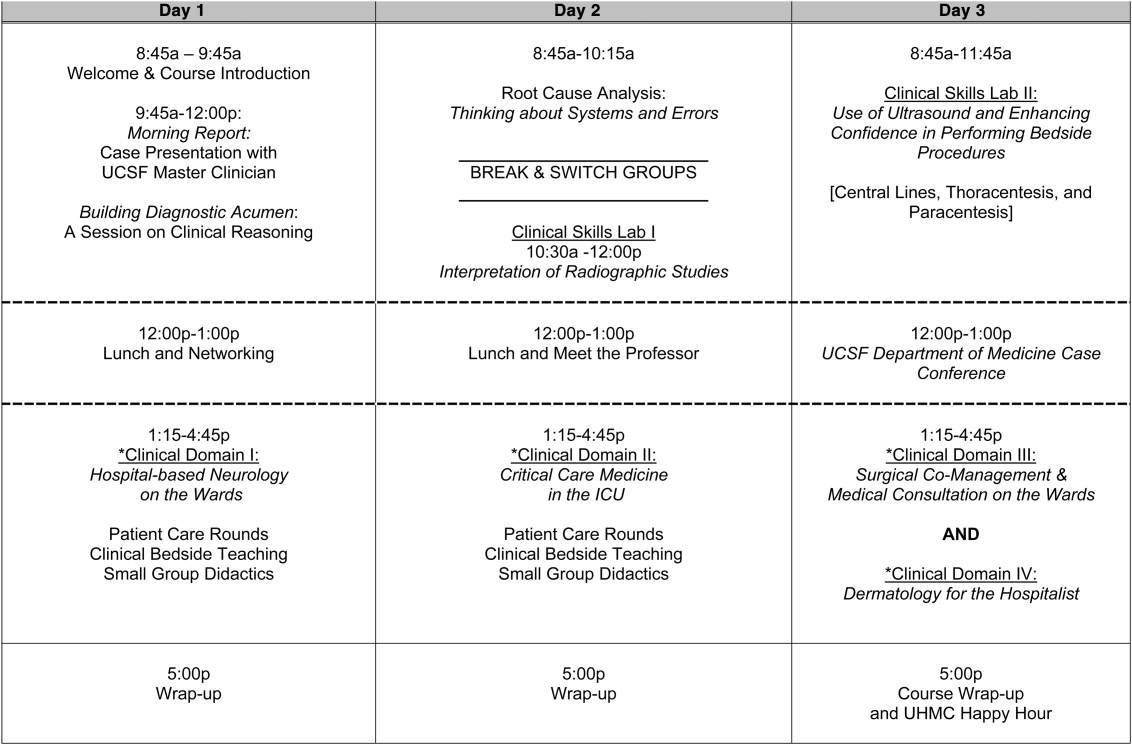
The program was built on a structure of 4 clinical domains and 2 clinical skills labs. The clinical domains included: (1) Hospital‐Based Neurology, (2) Critical Care Medicine in the Intensive Care Unit, (3) Surgical Comanagement and Medical Consultation, and (4) Hospital‐Based Dermatology. Participants were divided into 3 groups of 10 participants each and rotated through each domain in the afternoons. The clinical skills labs included: (1) Interpretation of Radiographic Studies and (2) Use of Ultrasound and Enhancing Confidence in Performing Bedside Procedures. We also developed specific sessions to teach about patient safety and to allow course attendees to participate in traditional academic learning vehicles (eg, a Morning Report and Morbidity and Mortality case conference). Below, we describe each session's format and content.
Clinical Domains
Hospital‐Based Neurology
Attendees participated in both bedside evaluation and case‐based discussions of common neurologic conditions seen in the hospital. In small groups of 5, participants were assigned patients to examine on the neurology ward. After their evaluations, they reported their findings to fellow participants and the faculty, setting the foundation for discussion of clinical management, review of neuroimaging, and exploration of current evidence to inform the patient's diagnosis and management. Participants and faculty then returned to the bedside to hone neurologic examination skills and complete the learning process. Given the unpredictability of what conditions would be represented on the ward in a given day, review of commonly seen conditions was always a focus, such as stroke, seizures, delirium, and neurologic examination pearls.
Critical Care
Attendees participated in case‐based discussions of common clinical conditions with similar review of current evidence, relevant imaging, and bedside exam pearls for the intubated patient. For this domain, attendees also participated in an advanced simulation tutorial in ventilator management, which was then applied at the bedside of intubated patients. Specific topics covered include sepsis, decompensated chronic obstructive lung disease, vasopressor selection, novel therapies in critically ill patients, and use of clinical pathways and protocols for improved quality of care.
Surgical Comanagement and Medical Consultation
Attendees participated in case‐based discussions applying current evidence to perioperative controversies and the care of the surgical patient. They also discussed the expanding role of the hospitalist in nonmedical patients.
Hospital‐Based Dermatology
Attendees participated in bedside evaluation of acute skin eruptions based on available patients admitted to the hospital. They discussed the approach to skin eruptions, key diagnoses, and when dermatologists should be consulted for their expertise. Specific topics included drug reactions, the red leg, life‐threating conditions (eg, Stevens‐Johnson syndrome), and dermatologic examination pearls. This domain was added in 2010.
Clinical Skills Labs
Radiology
In groups of 15, attendees reviewed common radiographs that hospitalists frequently order or evaluate (eg, chest x‐rays; kidney, ureter, and bladder; placement of endotracheal or feeding tube). They also reviewed the most relevant and not‐to‐miss findings on other commonly ordered studies such as abdominal or brain computerized tomography scans.
Hospital Procedures With Bedside Ultrasound
Attendees participated in a half‐day session to gain experience with the following procedures: paracentesis, lumbar puncture, thoracentesis, and central lines. They participated in an initial overview of procedural safety followed by hands‐on application sessions, in which they rotated through clinical workstations in groups of 5. At each work station, they were provided an opportunity to practice techniques, including the safe use of ultrasound on both live (standardized patients) and simulation models.
Other Sessions
Building Diagnostic Acumen and Clinical Reasoning
The opening session of the UHMC reintroduces attendees to the traditional academic morning report format, in which a case is presented and participants are asked to assess the information, develop differential diagnoses, discuss management options, and consider their own clinical reasoning skills. This provides frameworks for diagnostic reasoning, highlights common cognitive errors, and teaches attendees how to develop expertise in their own diagnostic thinking. The session also sets the stage and expectation for active learning and participation in the UHMC.
Root Cause Analysis and Systems Thinking
As the only nonclinical session in the UHMC, this session introduces participants to systems thinking and patient safety. Attendees participate in a root cause analysis role play surrounding a serious medical error and discuss the implications, their reflections, and then propose solutions through interactive table discussions. The session also emphasizes the key role hospitalists should play in improving patient safety.
Clinical Case Conference
Attendees participated in the weekly UCSF Department of Medicine Morbidity and Mortality conference. This is a traditional case conference that brings together learners, expert discussants, and an interesting or challenging case. This allows attendees to synthesize much of the course learning through active participation in the case discussion. Rather than creating a new conference for the participants, we brought the participants to the existing conference as part of their UHMC immersion experience.
Meet the Professor
Attendees participated in an informal discussion with a national leader (R.M.W.) in hospital medicine. This allowed for an interactive exchange of ideas and an understanding of the field overall.
Online Search Strategies
This interactive computer lab session allowed participants to explore the ever‐expanding number of online resources to answer clinical queries. This session was replaced in 2010 with the dermatology clinical domain based on participant feedback.
Program Evaluation
Participants completed a pre‐UHMC survey that provided demographic information and attributes about themselves, their clinical practice, and experience. Participants also completed course evaluations consistent with Accreditation Council for Continuing Medical Education standards following the program. The questions asked for each activity were rated on a 1‐to‐5 scale (1=poor, 5=excellent) and also included open‐ended questions to assess overall experiences.
RESULTS
Participant Demographics
During the first 5 years of the UHMC, 152 participants enrolled and completed the program; 91% completed the pre‐UHMC survey and 89% completed the postcourse evaluation. Table 1 describes the self‐reported participant demographics, including years in practice, number of hospitalist jobs, overall job satisfaction, and time spent doing clinical work. Overall, 68% of all participants had been self‐described hospitalists for 4 years, with 62% holding only 1 hospitalist job during that time; 77% reported being pretty or very satisfied with their jobs, and 72% reported clinical care as the attribute they love most in their job. Table 2 highlights the type of work attendees participate in within their clinical practice. More than half manage patients with neurologic disorders and care for critically ill patients, whereas virtually all perform preoperative medical evaluations and medical consultation
| Question | Response Options | 2008 (n=4) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average (n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| How long have you been a hospitalist? | 2 years | 52% | 35% | 37% | 30% | 25% | 36% |
| 24 years | 26% | 39% | 30% | 30% | 38% | 32% | |
| 510 years | 11% | 17% | 15% | 26% | 29% | 20% | |
| >10 years | 11% | 9% | 18% | 14% | 8% | 12% | |
| How many hospitalist jobs have you had? | 1 | 63% | 61% | 62% | 62% | 58% | 62% |
| 2 to 3 | 37% | 35% | 23% | 35% | 29% | 32% | |
| >3 | 0% | 4% | 15% | 1% | 13% | 5% | |
| How satisfied are you with your current position? | Not satisfied | 1% | 4% | 4% | 4% | 0% | 4% |
| Somewhat satisfied | 11% | 13% | 39% | 17% | 17% | 19% | |
| Pretty satisfied | 59% | 52% | 35% | 57% | 38% | 48% | |
| Very satisfied | 26% | 30% | 23% | 22% | 46% | 29% | |
| What do you love most about your job? | Clinical care | 85% | 61% | 65% | 84% | 67% | 72% |
| Teaching | 1% | 17% | 12% | 1% | 4% | 7% | |
| QI or safety work | 0% | 4% | 0% | 1% | 8% | 3% | |
| Other (not specified) | 14% | 18% | 23% | 14% | 21% | 18% | |
| What percent of your time is spent doing clinical care? | 100% | 39% | 36% | 52% | 46% | 58% | 46% |
| 75%100% | 58% | 50% | 37% | 42% | 33% | 44% | |
| 5075% | 0% | 9% | 11% | 12% | 4% | 7% | |
| 25%50% | 4% | 5% | 0% | 0% | 5% | 3% | |
| 25% | 0% | 0% | 0% | 0% | 0% | 0% | |
| Question | Response Options | 2008 (n=24) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average(n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| Do you primarily manage patients with neurologic disorders in your hospital? | Yes | 62% | 50% | 62% | 62% | 63% | 60% |
| Do you primarily manage critically ill ICU patients in your hospital? | Yes and without an intensivist | 19% | 23% | 19% | 27% | 21% | 22% |
| Yes but with an intensivist | 54% | 50% | 44% | 42% | 67% | 51% | |
| No | 27% | 27% | 37% | 31% | 13% | 27% | |
| Do you perform preoperative medical evaluations and medical consultation? | Yes | 96% | 91% | 96% | 96% | 92% | 94% |
| Which of the following describes your role in the care of surgical patients? | Traditional medical consultant | 33% | 28% | 28% | 30% | 24% | 29% |
| Comanagement (shared responsibility with surgeon) | 33% | 34% | 42% | 39% | 35% | 37% | |
| Attending of record with surgeon acting as consultant | 26% | 24% | 26% | 30% | 35% | 28% | |
| Do you have bedside ultrasound available in your daily practice? | Yes | 38% | 32% | 52% | 34% | 38% | 39% |
Participant Experience
Overall, participants rated the quality of the UHMC course highly (4.65; 15 scale). The neurology clinical domain (4.83) and clinical reasoning session (4.72) were the highest‐rated sessions. Compared to all UCSF CME course offerings between January 2010 and September 2012, the UHMC rated higher than the cumulative overall rating from those 227 courses (4.65 vs 4.44). For UCSF CME courses offered in 2011 and 2012, 78% of participants (n=11,447) reported a high or definite likelihood to change practice. For UHMC participants during the same time period (n=57), 98% reported a similar likelihood to change practice. Table 3 provides selected participant comments from their postcourse evaluations.
|
| Great pearls, broad ranging discussion of many controversial and common topics, and I loved the teaching format. |
| I thought the conception of the teaching model was really effectivehands‐on exams in small groups, each demonstrating a different part of the neurologic exam, followed by presentation and discussion, and ending in bedside rounds with the teaching faculty. |
| Excellent review of key topicswide variety of useful and practical points. Very high application value. |
| Great course. I'd take it again and again. It was a superb opportunity to review technique, equipment, and clinical decision making. |
| Overall outstanding course! Very informative and fun. Format was great. |
| Forward and clinically relevant. Like the bedside teaching and how they did it.The small size of the course and the close attention paid by the faculty teaching the course combined with the opportunity to see and examine patients in the hospital was outstanding. |
DISCUSSION
We developed an innovative CME program that brought participants to an academic health center for a participatory, hands‐on, and small‐group experience. They learned about topics relevant to today's hospitalists, rated the experience very highly, and reported a nearly unanimous likelihood to change their practice. Reflecting on our program's first 5 years, there were several lessons learned that may guide others committed to providing a similar CME experience.
First, hospital medicine is a dynamic field. Conducting a needs assessment to match clinical topics to what attendees required in their own practice was critical. Iterative changes from year to year reflected formal participant feedback as well as informal conversations with the teaching faculty. For instance, attendees were not only interested in the clinical topics but often wanted to see examples of clinical pathways, order sets, and other systems in place to improve care for patients with common conditions. Our participant presurvey also helped identify and reinforce the curricular topics that teaching faculty focused on each year. Being responsive to the changing needs of hospitalists and the environment is a crucial part of providing a relevant CME experience.
We also used an innovative approach to teaching, founded in adult and effective CME learning principles. CME activities are geared toward adult physicians, and studies of their effectiveness recommend that sessions should be interactive and utilize multiple modalities of learning.[12] When attendees actively participate and are provided an opportunity to practice skills, it may have a positive effect on patient outcomes.[13] All UHMC faculty were required to couple presentations of the latest evidence for clinical topics with small‐group and hands‐on learning modalities. This also required that we utilize a teaching faculty known for both their clinical expertise and teaching recognition. Together, the learning modalities and the teaching faculty likely accounted for the highly rated course experience and likelihood to change practice.
Finally, our course brought participants to an academic medical center and into the mix of clinical care as opposed to the more traditional hotel venue. This was necessary to deliver the curriculum as described, but also had the unexpected benefit of energizing the participants. Many had not been in a teaching setting since their residency training, and bringing them back into this milieu motivated them to learn and share their inspiration. As there are no published studies of CME experiences in the clinical environment, this observation is noteworthy and deserves to be explored and evaluated further.
What are the limitations of our approach to bringing CME to the bedside? First, the economics of an intensive 3‐day course with a maximum of 33 attendees are far different than those of a large hotel‐based offering. There are no exhibitors or outside contributions. The cost of the course to participants is $2500 (discounted if attending the larger course as well), which is 2 to 3 times higher than most traditional CME courses of the same length. Although the cost is high, the course has sold out each year with a waiting list. Part of the cost is also faculty time. The time, preparation, and need to teach on the fly to meet the differing participant educational needs is fundamentally different than delivering a single lecture in a hotel conference room. Not surprisingly, our faculty enjoy this teaching opportunity and find it equally unique and valuable; no faculty have dropped out of teaching the course, and many describe it as 1 of the teaching highlights of the year. Scalability of the UHMC is challenging for these reasons, but our model could be replicated in other teaching institutions, even as a local offering for their own providers.
In summary, we developed a hospital‐based, highly interactive, small‐group CME course that emphasizes case‐based teaching. The course has sold out each year, and evaluations suggest that it is highly valued and is meeting curricular goals better than more traditional CME courses. We hope our course description and success may motivate others to consider moving beyond the traditional CME for hospitalists and explore further innovations. With the field growing and changing at a rapid pace, innovative CME experiences will be necessary to assure that hospitalists continue to provide exemplary and safe care to their patients.
Acknowledgements
The authors thank Kapo Tam for her program management of the UHMC, and Katherine Li and Zachary Martin for their invaluable administrative support and coordination. The authors are also indebted to faculty colleagues for their time and roles in teaching within the program. They include Gupreet Dhaliwal, Andy Josephson, Vanja Douglas, Michelle Milic, Brian Daniels, Quinny Cheng, Lindy Fox, Diane Sliwka, Ralph Wang, and Thomas Urbania.
Disclosure: Nothing to report.
I hear and I forget, I see and I remember, I do and I understand.
Confucius
Hospital medicine, first described in 1996,[1] is the fastest growing specialty in United States medical history, now with approximately 40,000 practitioners.[2] Although hospitalists undoubtedly learned many of their key clinical skills during residency training, there is no hospitalist‐specific residency training pathway and a limited number of largely research‐oriented fellowships.[3] Furthermore, hospitalists are often asked to care for surgical patients, those with acute neurologic disorders, and patients in intensive care units, while also contributing to quality improvement and patient safety initiatives.[4] This suggests that the vast majority of hospitalists have not had specific training in many key competencies for the field.[5]
Continuing medical education (CME) has traditionally been the mechanism to maintain, develop, or increase the knowledge, skills, and professional performance of physicians.[6] Most CME activities, including those for hospitalists, are staged as live events in hotel conference rooms or as local events in a similarly passive learning environment (eg, grand rounds and medical staff meetings). Online programs, audiotapes, and expanding electronic media provide increasing and alternate methods for hospitalists to obtain their required CME. All of these activities passively deliver content to a group of diverse and experienced learners. They fail to take advantage of adult learning principles and may have little direct impact on professional practice.[7, 8] Traditional CME is often derided as a barrier to innovative educational methods for these reasons, as adults learn best through active participation, when the information is relevant and practically applied.[9, 10]
To provide practicing hospitalists with necessary continuing education, we designed the University of California, San Francisco (UCSF) Hospitalist Mini‐College (UHMC). This 3‐day course brings adult learners to the bedside for small‐group and active learning focused on content areas relevant to today's hospitalists. We describe the development, content, outcomes, and lessons learned from UHMC's first 5 years.
METHODS
Program Development
We aimed to develop a program that focused on curricular topics that would be highly valued by practicing hospitalists delivered in an active learning small‐group environment. We first conducted an informal needs assessment of community‐based hospitalists to better understand their roles and determine their perceptions of gaps in hospitalist training compared to current requirements for practice. We then reviewed available CME events targeting hospitalists and compared these curricula to the gaps discovered from the needs assessment. We also reviewed the Society of Hospital Medicine's core competencies to further identify gaps in scope of practice.[4] Finally, we reviewed the literature to identify CME curricular innovations in the clinical setting and found no published reports.
Program Setting, Participants, and Faculty
The UHMC course was developed and offered first in 2008 as a precourse to the UCSF Management of the Hospitalized Medicine course, a traditional CME offering that occurs annually in a hotel setting.[11] The UHMC takes place on the campus of UCSF Medical Center, a 600‐bed academic medical center in San Francisco. Registered participants were required to complete limited credentialing paperwork, which allowed them to directly observe clinical care and interact with hospitalized patients. Participants were not involved in any clinical decision making for the patients they met or examined. The course was limited to a maximum of 33 participants annually to optimize active participation, small‐group bedside activities, and a personalized learning experience. UCSF faculty selected to teach in the UHMC were chosen based on exemplary clinical and teaching skills. They collaborated with course directors in the development of their session‐specific goals and curriculum.
Program Description
Figure 1 is a representative calendar view of the 3‐day UHMC course. The curricular topics were selected based on the findings from our needs assessment, our ability to deliver that curriculum using our small‐group active learning framework, and to minimize overlap with content of the larger course. Course curriculum was refined annually based on participant feedback and course director observations.
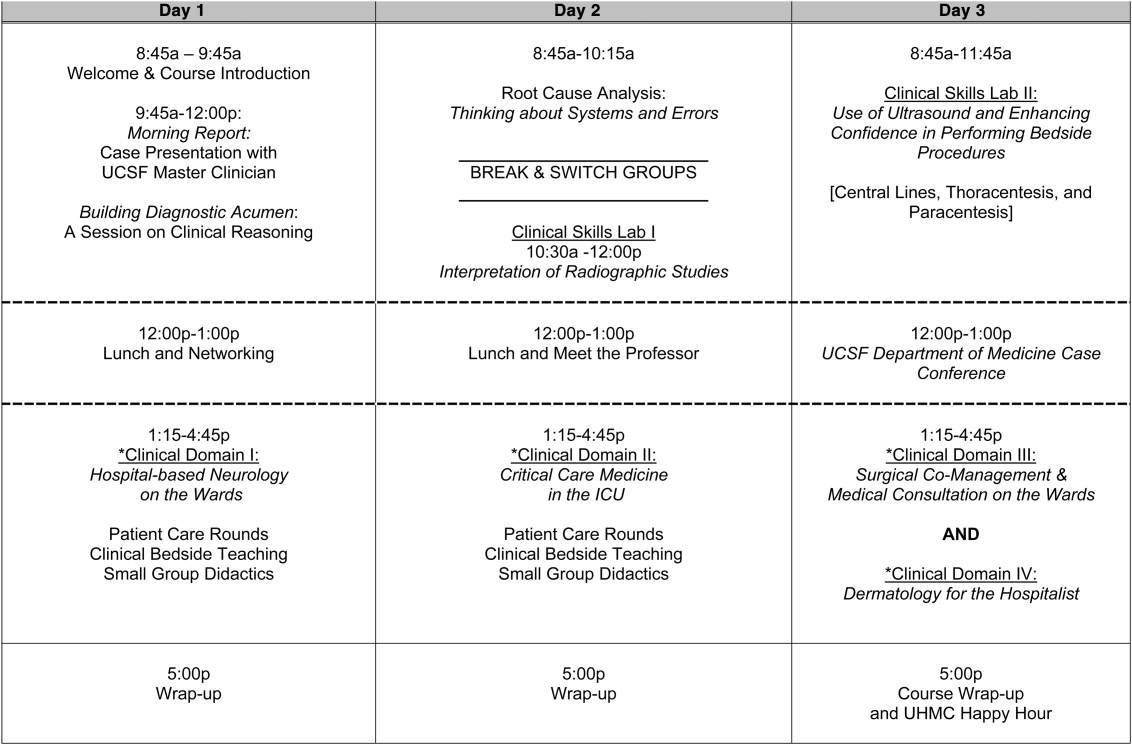
The program was built on a structure of 4 clinical domains and 2 clinical skills labs. The clinical domains included: (1) Hospital‐Based Neurology, (2) Critical Care Medicine in the Intensive Care Unit, (3) Surgical Comanagement and Medical Consultation, and (4) Hospital‐Based Dermatology. Participants were divided into 3 groups of 10 participants each and rotated through each domain in the afternoons. The clinical skills labs included: (1) Interpretation of Radiographic Studies and (2) Use of Ultrasound and Enhancing Confidence in Performing Bedside Procedures. We also developed specific sessions to teach about patient safety and to allow course attendees to participate in traditional academic learning vehicles (eg, a Morning Report and Morbidity and Mortality case conference). Below, we describe each session's format and content.
Clinical Domains
Hospital‐Based Neurology
Attendees participated in both bedside evaluation and case‐based discussions of common neurologic conditions seen in the hospital. In small groups of 5, participants were assigned patients to examine on the neurology ward. After their evaluations, they reported their findings to fellow participants and the faculty, setting the foundation for discussion of clinical management, review of neuroimaging, and exploration of current evidence to inform the patient's diagnosis and management. Participants and faculty then returned to the bedside to hone neurologic examination skills and complete the learning process. Given the unpredictability of what conditions would be represented on the ward in a given day, review of commonly seen conditions was always a focus, such as stroke, seizures, delirium, and neurologic examination pearls.
Critical Care
Attendees participated in case‐based discussions of common clinical conditions with similar review of current evidence, relevant imaging, and bedside exam pearls for the intubated patient. For this domain, attendees also participated in an advanced simulation tutorial in ventilator management, which was then applied at the bedside of intubated patients. Specific topics covered include sepsis, decompensated chronic obstructive lung disease, vasopressor selection, novel therapies in critically ill patients, and use of clinical pathways and protocols for improved quality of care.
Surgical Comanagement and Medical Consultation
Attendees participated in case‐based discussions applying current evidence to perioperative controversies and the care of the surgical patient. They also discussed the expanding role of the hospitalist in nonmedical patients.
Hospital‐Based Dermatology
Attendees participated in bedside evaluation of acute skin eruptions based on available patients admitted to the hospital. They discussed the approach to skin eruptions, key diagnoses, and when dermatologists should be consulted for their expertise. Specific topics included drug reactions, the red leg, life‐threating conditions (eg, Stevens‐Johnson syndrome), and dermatologic examination pearls. This domain was added in 2010.
Clinical Skills Labs
Radiology
In groups of 15, attendees reviewed common radiographs that hospitalists frequently order or evaluate (eg, chest x‐rays; kidney, ureter, and bladder; placement of endotracheal or feeding tube). They also reviewed the most relevant and not‐to‐miss findings on other commonly ordered studies such as abdominal or brain computerized tomography scans.
Hospital Procedures With Bedside Ultrasound
Attendees participated in a half‐day session to gain experience with the following procedures: paracentesis, lumbar puncture, thoracentesis, and central lines. They participated in an initial overview of procedural safety followed by hands‐on application sessions, in which they rotated through clinical workstations in groups of 5. At each work station, they were provided an opportunity to practice techniques, including the safe use of ultrasound on both live (standardized patients) and simulation models.
Other Sessions
Building Diagnostic Acumen and Clinical Reasoning
The opening session of the UHMC reintroduces attendees to the traditional academic morning report format, in which a case is presented and participants are asked to assess the information, develop differential diagnoses, discuss management options, and consider their own clinical reasoning skills. This provides frameworks for diagnostic reasoning, highlights common cognitive errors, and teaches attendees how to develop expertise in their own diagnostic thinking. The session also sets the stage and expectation for active learning and participation in the UHMC.
Root Cause Analysis and Systems Thinking
As the only nonclinical session in the UHMC, this session introduces participants to systems thinking and patient safety. Attendees participate in a root cause analysis role play surrounding a serious medical error and discuss the implications, their reflections, and then propose solutions through interactive table discussions. The session also emphasizes the key role hospitalists should play in improving patient safety.
Clinical Case Conference
Attendees participated in the weekly UCSF Department of Medicine Morbidity and Mortality conference. This is a traditional case conference that brings together learners, expert discussants, and an interesting or challenging case. This allows attendees to synthesize much of the course learning through active participation in the case discussion. Rather than creating a new conference for the participants, we brought the participants to the existing conference as part of their UHMC immersion experience.
Meet the Professor
Attendees participated in an informal discussion with a national leader (R.M.W.) in hospital medicine. This allowed for an interactive exchange of ideas and an understanding of the field overall.
Online Search Strategies
This interactive computer lab session allowed participants to explore the ever‐expanding number of online resources to answer clinical queries. This session was replaced in 2010 with the dermatology clinical domain based on participant feedback.
Program Evaluation
Participants completed a pre‐UHMC survey that provided demographic information and attributes about themselves, their clinical practice, and experience. Participants also completed course evaluations consistent with Accreditation Council for Continuing Medical Education standards following the program. The questions asked for each activity were rated on a 1‐to‐5 scale (1=poor, 5=excellent) and also included open‐ended questions to assess overall experiences.
RESULTS
Participant Demographics
During the first 5 years of the UHMC, 152 participants enrolled and completed the program; 91% completed the pre‐UHMC survey and 89% completed the postcourse evaluation. Table 1 describes the self‐reported participant demographics, including years in practice, number of hospitalist jobs, overall job satisfaction, and time spent doing clinical work. Overall, 68% of all participants had been self‐described hospitalists for 4 years, with 62% holding only 1 hospitalist job during that time; 77% reported being pretty or very satisfied with their jobs, and 72% reported clinical care as the attribute they love most in their job. Table 2 highlights the type of work attendees participate in within their clinical practice. More than half manage patients with neurologic disorders and care for critically ill patients, whereas virtually all perform preoperative medical evaluations and medical consultation
| Question | Response Options | 2008 (n=4) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average (n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| How long have you been a hospitalist? | 2 years | 52% | 35% | 37% | 30% | 25% | 36% |
| 24 years | 26% | 39% | 30% | 30% | 38% | 32% | |
| 510 years | 11% | 17% | 15% | 26% | 29% | 20% | |
| >10 years | 11% | 9% | 18% | 14% | 8% | 12% | |
| How many hospitalist jobs have you had? | 1 | 63% | 61% | 62% | 62% | 58% | 62% |
| 2 to 3 | 37% | 35% | 23% | 35% | 29% | 32% | |
| >3 | 0% | 4% | 15% | 1% | 13% | 5% | |
| How satisfied are you with your current position? | Not satisfied | 1% | 4% | 4% | 4% | 0% | 4% |
| Somewhat satisfied | 11% | 13% | 39% | 17% | 17% | 19% | |
| Pretty satisfied | 59% | 52% | 35% | 57% | 38% | 48% | |
| Very satisfied | 26% | 30% | 23% | 22% | 46% | 29% | |
| What do you love most about your job? | Clinical care | 85% | 61% | 65% | 84% | 67% | 72% |
| Teaching | 1% | 17% | 12% | 1% | 4% | 7% | |
| QI or safety work | 0% | 4% | 0% | 1% | 8% | 3% | |
| Other (not specified) | 14% | 18% | 23% | 14% | 21% | 18% | |
| What percent of your time is spent doing clinical care? | 100% | 39% | 36% | 52% | 46% | 58% | 46% |
| 75%100% | 58% | 50% | 37% | 42% | 33% | 44% | |
| 5075% | 0% | 9% | 11% | 12% | 4% | 7% | |
| 25%50% | 4% | 5% | 0% | 0% | 5% | 3% | |
| 25% | 0% | 0% | 0% | 0% | 0% | 0% | |
| Question | Response Options | 2008 (n=24) | 2009 (n=26) | 2010 (n=29) | 2011 (n=31) | 2012 (n=28) | Average(n=138) |
|---|---|---|---|---|---|---|---|
| |||||||
| Do you primarily manage patients with neurologic disorders in your hospital? | Yes | 62% | 50% | 62% | 62% | 63% | 60% |
| Do you primarily manage critically ill ICU patients in your hospital? | Yes and without an intensivist | 19% | 23% | 19% | 27% | 21% | 22% |
| Yes but with an intensivist | 54% | 50% | 44% | 42% | 67% | 51% | |
| No | 27% | 27% | 37% | 31% | 13% | 27% | |
| Do you perform preoperative medical evaluations and medical consultation? | Yes | 96% | 91% | 96% | 96% | 92% | 94% |
| Which of the following describes your role in the care of surgical patients? | Traditional medical consultant | 33% | 28% | 28% | 30% | 24% | 29% |
| Comanagement (shared responsibility with surgeon) | 33% | 34% | 42% | 39% | 35% | 37% | |
| Attending of record with surgeon acting as consultant | 26% | 24% | 26% | 30% | 35% | 28% | |
| Do you have bedside ultrasound available in your daily practice? | Yes | 38% | 32% | 52% | 34% | 38% | 39% |
Participant Experience
Overall, participants rated the quality of the UHMC course highly (4.65; 15 scale). The neurology clinical domain (4.83) and clinical reasoning session (4.72) were the highest‐rated sessions. Compared to all UCSF CME course offerings between January 2010 and September 2012, the UHMC rated higher than the cumulative overall rating from those 227 courses (4.65 vs 4.44). For UCSF CME courses offered in 2011 and 2012, 78% of participants (n=11,447) reported a high or definite likelihood to change practice. For UHMC participants during the same time period (n=57), 98% reported a similar likelihood to change practice. Table 3 provides selected participant comments from their postcourse evaluations.
|
| Great pearls, broad ranging discussion of many controversial and common topics, and I loved the teaching format. |
| I thought the conception of the teaching model was really effectivehands‐on exams in small groups, each demonstrating a different part of the neurologic exam, followed by presentation and discussion, and ending in bedside rounds with the teaching faculty. |
| Excellent review of key topicswide variety of useful and practical points. Very high application value. |
| Great course. I'd take it again and again. It was a superb opportunity to review technique, equipment, and clinical decision making. |
| Overall outstanding course! Very informative and fun. Format was great. |
| Forward and clinically relevant. Like the bedside teaching and how they did it.The small size of the course and the close attention paid by the faculty teaching the course combined with the opportunity to see and examine patients in the hospital was outstanding. |
DISCUSSION
We developed an innovative CME program that brought participants to an academic health center for a participatory, hands‐on, and small‐group experience. They learned about topics relevant to today's hospitalists, rated the experience very highly, and reported a nearly unanimous likelihood to change their practice. Reflecting on our program's first 5 years, there were several lessons learned that may guide others committed to providing a similar CME experience.
First, hospital medicine is a dynamic field. Conducting a needs assessment to match clinical topics to what attendees required in their own practice was critical. Iterative changes from year to year reflected formal participant feedback as well as informal conversations with the teaching faculty. For instance, attendees were not only interested in the clinical topics but often wanted to see examples of clinical pathways, order sets, and other systems in place to improve care for patients with common conditions. Our participant presurvey also helped identify and reinforce the curricular topics that teaching faculty focused on each year. Being responsive to the changing needs of hospitalists and the environment is a crucial part of providing a relevant CME experience.
We also used an innovative approach to teaching, founded in adult and effective CME learning principles. CME activities are geared toward adult physicians, and studies of their effectiveness recommend that sessions should be interactive and utilize multiple modalities of learning.[12] When attendees actively participate and are provided an opportunity to practice skills, it may have a positive effect on patient outcomes.[13] All UHMC faculty were required to couple presentations of the latest evidence for clinical topics with small‐group and hands‐on learning modalities. This also required that we utilize a teaching faculty known for both their clinical expertise and teaching recognition. Together, the learning modalities and the teaching faculty likely accounted for the highly rated course experience and likelihood to change practice.
Finally, our course brought participants to an academic medical center and into the mix of clinical care as opposed to the more traditional hotel venue. This was necessary to deliver the curriculum as described, but also had the unexpected benefit of energizing the participants. Many had not been in a teaching setting since their residency training, and bringing them back into this milieu motivated them to learn and share their inspiration. As there are no published studies of CME experiences in the clinical environment, this observation is noteworthy and deserves to be explored and evaluated further.
What are the limitations of our approach to bringing CME to the bedside? First, the economics of an intensive 3‐day course with a maximum of 33 attendees are far different than those of a large hotel‐based offering. There are no exhibitors or outside contributions. The cost of the course to participants is $2500 (discounted if attending the larger course as well), which is 2 to 3 times higher than most traditional CME courses of the same length. Although the cost is high, the course has sold out each year with a waiting list. Part of the cost is also faculty time. The time, preparation, and need to teach on the fly to meet the differing participant educational needs is fundamentally different than delivering a single lecture in a hotel conference room. Not surprisingly, our faculty enjoy this teaching opportunity and find it equally unique and valuable; no faculty have dropped out of teaching the course, and many describe it as 1 of the teaching highlights of the year. Scalability of the UHMC is challenging for these reasons, but our model could be replicated in other teaching institutions, even as a local offering for their own providers.
In summary, we developed a hospital‐based, highly interactive, small‐group CME course that emphasizes case‐based teaching. The course has sold out each year, and evaluations suggest that it is highly valued and is meeting curricular goals better than more traditional CME courses. We hope our course description and success may motivate others to consider moving beyond the traditional CME for hospitalists and explore further innovations. With the field growing and changing at a rapid pace, innovative CME experiences will be necessary to assure that hospitalists continue to provide exemplary and safe care to their patients.
Acknowledgements
The authors thank Kapo Tam for her program management of the UHMC, and Katherine Li and Zachary Martin for their invaluable administrative support and coordination. The authors are also indebted to faculty colleagues for their time and roles in teaching within the program. They include Gupreet Dhaliwal, Andy Josephson, Vanja Douglas, Michelle Milic, Brian Daniels, Quinny Cheng, Lindy Fox, Diane Sliwka, Ralph Wang, and Thomas Urbania.
Disclosure: Nothing to report.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;337(7):514–517.
- Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Membership2/HospitalFocusedPractice/Hospital_Focused_Pra.htm. Accessed October 1, 2013.
- , , , . Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1–e7.
- Society of Hospital Medicine. Core competencies in hospital medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 1, 2013.
- , . The expanding role of hospitalists in the United States. Swiss Med Wkly. 2006;136(37‐38);591–596.
- Accreditation Council for Continuing Medical Education. CME content: definition and examples Available at: http://www.accme.org/requirements/accreditation‐requirements‐cme‐providers/policies‐and‐definitions/cme‐content‐definition‐and‐examples. Accessed October 1, 2013.
- , , , . Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–705.
- , . Continuing medical education and the physician as a learner: guide to the evidence. JAMA. 2002;288(9):1057–1060.
- , , , , . Barriers to innovation in continuing medical eduation. J Contin Educ Health Prof. 2008;28(3):148–156.
- . Adult learning theory for the 21st century. In: Merriam S. Thrid Update on Adult Learning Theory: New Directions for Adult and Continuing Education. San Francisco, CA: Jossey‐Bass; 2008:93–98.
- .UCSF management of the hospitalized patient CME course. Available at: http://www.ucsfcme.com/2014/MDM14P01/info.html. Accessed October 1, 2013.
- Continuing medical education effect on practice performance: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);42S–48S.
- Continuing medical education effect on clinical outcomes: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);49S–55S.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;337(7):514–517.
- Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Membership2/HospitalFocusedPractice/Hospital_Focused_Pra.htm. Accessed October 1, 2013.
- , , , . Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1–e7.
- Society of Hospital Medicine. Core competencies in hospital medicine. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Education/CoreCurriculum/Core_Competencies.htm. Accessed October 1, 2013.
- , . The expanding role of hospitalists in the United States. Swiss Med Wkly. 2006;136(37‐38);591–596.
- Accreditation Council for Continuing Medical Education. CME content: definition and examples Available at: http://www.accme.org/requirements/accreditation‐requirements‐cme‐providers/policies‐and‐definitions/cme‐content‐definition‐and‐examples. Accessed October 1, 2013.
- , , , . Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–705.
- , . Continuing medical education and the physician as a learner: guide to the evidence. JAMA. 2002;288(9):1057–1060.
- , , , , . Barriers to innovation in continuing medical eduation. J Contin Educ Health Prof. 2008;28(3):148–156.
- . Adult learning theory for the 21st century. In: Merriam S. Thrid Update on Adult Learning Theory: New Directions for Adult and Continuing Education. San Francisco, CA: Jossey‐Bass; 2008:93–98.
- .UCSF management of the hospitalized patient CME course. Available at: http://www.ucsfcme.com/2014/MDM14P01/info.html. Accessed October 1, 2013.
- Continuing medical education effect on practice performance: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);42S–48S.
- Continuing medical education effect on clinical outcomes: effectiveness of continuing medical education: American College or Chest Physicians evidence‐based educational guidelines. Chest. 2009;135(3 suppl);49S–55S.
VTE Risk Spikes for Pregnant Patients Admitted to Hospitals Pre-Delivery
A British study that bills itself as the first to assess the impact of pre-delivery hospital admission on the incidence of VTE in pregnant women should serve as a clarion call to hospitalists, says a hospital physician and OB/GYN specialist.
Rob Olson, MD, FACOG, founding president of the Society of OB/GYN Hospitalists, says the report confirms empirically what most agree anecdotally: pregnant patients are at increased risk for VTE upon admission to the hospital, and those at highest risk should receive prophylaxis.
Published earlier this month in the British Medical Journal, the open-access report [PDF] found that hospital admissions during pregnancy were associated with a 17-fold increase in the risk of VTE. The risk remained sixfold higher for pregnant women 28 days after discharge, the report noted.
"This really quantifies it in a way I haven't seen before," says Dr. Olson, who practices in Bellingham, Wash. He says internal-medicine hospitalists should keep VTE prophylaxis front-of-mind for pregnant inpatients who during their hospital stay will likely experience a significant amount of bed rest. In those cases, he urges hospitalists to consult an obstetrician or an OB/GYN hospitalist, and consider use of compression devices or low-dose heparin.
"The more we understand the magnitude of the risks, the more we can mitigate against it," Dr. Olson adds. "The problem that you’re dealing with is something that doesn’t happen very often. Internists may see a bunch of pregnant patients and not have any problems. We want every pregnant admission to be a safe admission."
Visit our website for more information on OB/GYN hospitalists.
A British study that bills itself as the first to assess the impact of pre-delivery hospital admission on the incidence of VTE in pregnant women should serve as a clarion call to hospitalists, says a hospital physician and OB/GYN specialist.
Rob Olson, MD, FACOG, founding president of the Society of OB/GYN Hospitalists, says the report confirms empirically what most agree anecdotally: pregnant patients are at increased risk for VTE upon admission to the hospital, and those at highest risk should receive prophylaxis.
Published earlier this month in the British Medical Journal, the open-access report [PDF] found that hospital admissions during pregnancy were associated with a 17-fold increase in the risk of VTE. The risk remained sixfold higher for pregnant women 28 days after discharge, the report noted.
"This really quantifies it in a way I haven't seen before," says Dr. Olson, who practices in Bellingham, Wash. He says internal-medicine hospitalists should keep VTE prophylaxis front-of-mind for pregnant inpatients who during their hospital stay will likely experience a significant amount of bed rest. In those cases, he urges hospitalists to consult an obstetrician or an OB/GYN hospitalist, and consider use of compression devices or low-dose heparin.
"The more we understand the magnitude of the risks, the more we can mitigate against it," Dr. Olson adds. "The problem that you’re dealing with is something that doesn’t happen very often. Internists may see a bunch of pregnant patients and not have any problems. We want every pregnant admission to be a safe admission."
Visit our website for more information on OB/GYN hospitalists.
A British study that bills itself as the first to assess the impact of pre-delivery hospital admission on the incidence of VTE in pregnant women should serve as a clarion call to hospitalists, says a hospital physician and OB/GYN specialist.
Rob Olson, MD, FACOG, founding president of the Society of OB/GYN Hospitalists, says the report confirms empirically what most agree anecdotally: pregnant patients are at increased risk for VTE upon admission to the hospital, and those at highest risk should receive prophylaxis.
Published earlier this month in the British Medical Journal, the open-access report [PDF] found that hospital admissions during pregnancy were associated with a 17-fold increase in the risk of VTE. The risk remained sixfold higher for pregnant women 28 days after discharge, the report noted.
"This really quantifies it in a way I haven't seen before," says Dr. Olson, who practices in Bellingham, Wash. He says internal-medicine hospitalists should keep VTE prophylaxis front-of-mind for pregnant inpatients who during their hospital stay will likely experience a significant amount of bed rest. In those cases, he urges hospitalists to consult an obstetrician or an OB/GYN hospitalist, and consider use of compression devices or low-dose heparin.
"The more we understand the magnitude of the risks, the more we can mitigate against it," Dr. Olson adds. "The problem that you’re dealing with is something that doesn’t happen very often. Internists may see a bunch of pregnant patients and not have any problems. We want every pregnant admission to be a safe admission."
Visit our website for more information on OB/GYN hospitalists.
Readmission Penalties for COPD Diagnoses Slated for 2014
Next October, when COPD is added to the list of diagnoses for which hospital readmissions penalties are calculated, hospitalists will need to pay closer attention to comorbidities, home environments, socio-economic status, and other factors that can contribute to COPD readmissions.
This was a central theme at a recent conference on COPD and hospital readmissions sponsored by the COPD Foundation in Washington, D.C. The meeting brought together pulmonologists, policy makers, healthcare quality-improvement experts, and representatives from four national, patient-care transitions programs: the Care Transitions Program of the University of Colorado School of Medicine in Denver; Project RED (Re-Engineered Discharge) at Boston University Medical Center; the Transitional Care Model of the University of Pennsylvania in Philadelphia; and SHM's Project BOOST.
"This summit reinforces what has already been said, that there needs to be a comprehensive approach to COPD patients, not just managing the disease," said one of the conference’s key speakers, Mark Williams, MD, MHM, professor and chief of the division of hospital medicine at Northwestern University Feinberg School of Medicine in Chicago and principal investigator of Project BOOST. "Similar to heart failure, there needs to be support for the patient at home."
COPD is the third-leading cause of death in the U.S., with an estimated 15 million diagnosed patients and many more undiagnosed. One-fifth of hospitalized COPD patients are readmitted within 30 days, according to data from the Agency for Healthcare Research and Quality [PDF]. Many simultaneously present with heart disease, pneumonia, diabetes, or other comorbidities, and 62% of hospitalized COPD patients are readmitted for a condition other than COPD, says Brian Carlin, MD, senior staff physician at Allegheny General Hospital in Pittsburgh, Pa.
Preventing readmissions underscores the need for a patient-centered approach, says conference co-chair Jerry Krishnan, MD, PhD, professor of medicine and public health associate vice president for population health sciences at the University of Illinois Hospital and Health System in Chicago. "There's a tremendous amount of interest among physicians about the quality of care and health outcomes for these patients and conflicting evidence about what actually works," Dr. Krishnan says. "What works in one setting is unlikely to work in another setting."
Other physicians at the conference discussed ways hospitalists could help reduce COPD-related readmissions. Guidelines for non-pharmacologic interventions emphasize access to smoking cessation programs, immunizations for influenza, and pulmonary rehabilitation, says Byron Thomashow, MD, clinical professor of medicine at Columbia University Medical Center in New York City. "I also encourage all of my patients to exercise," he says.
Visit our website for more information on patient care and COPD.
Next October, when COPD is added to the list of diagnoses for which hospital readmissions penalties are calculated, hospitalists will need to pay closer attention to comorbidities, home environments, socio-economic status, and other factors that can contribute to COPD readmissions.
This was a central theme at a recent conference on COPD and hospital readmissions sponsored by the COPD Foundation in Washington, D.C. The meeting brought together pulmonologists, policy makers, healthcare quality-improvement experts, and representatives from four national, patient-care transitions programs: the Care Transitions Program of the University of Colorado School of Medicine in Denver; Project RED (Re-Engineered Discharge) at Boston University Medical Center; the Transitional Care Model of the University of Pennsylvania in Philadelphia; and SHM's Project BOOST.
"This summit reinforces what has already been said, that there needs to be a comprehensive approach to COPD patients, not just managing the disease," said one of the conference’s key speakers, Mark Williams, MD, MHM, professor and chief of the division of hospital medicine at Northwestern University Feinberg School of Medicine in Chicago and principal investigator of Project BOOST. "Similar to heart failure, there needs to be support for the patient at home."
COPD is the third-leading cause of death in the U.S., with an estimated 15 million diagnosed patients and many more undiagnosed. One-fifth of hospitalized COPD patients are readmitted within 30 days, according to data from the Agency for Healthcare Research and Quality [PDF]. Many simultaneously present with heart disease, pneumonia, diabetes, or other comorbidities, and 62% of hospitalized COPD patients are readmitted for a condition other than COPD, says Brian Carlin, MD, senior staff physician at Allegheny General Hospital in Pittsburgh, Pa.
Preventing readmissions underscores the need for a patient-centered approach, says conference co-chair Jerry Krishnan, MD, PhD, professor of medicine and public health associate vice president for population health sciences at the University of Illinois Hospital and Health System in Chicago. "There's a tremendous amount of interest among physicians about the quality of care and health outcomes for these patients and conflicting evidence about what actually works," Dr. Krishnan says. "What works in one setting is unlikely to work in another setting."
Other physicians at the conference discussed ways hospitalists could help reduce COPD-related readmissions. Guidelines for non-pharmacologic interventions emphasize access to smoking cessation programs, immunizations for influenza, and pulmonary rehabilitation, says Byron Thomashow, MD, clinical professor of medicine at Columbia University Medical Center in New York City. "I also encourage all of my patients to exercise," he says.
Visit our website for more information on patient care and COPD.
Next October, when COPD is added to the list of diagnoses for which hospital readmissions penalties are calculated, hospitalists will need to pay closer attention to comorbidities, home environments, socio-economic status, and other factors that can contribute to COPD readmissions.
This was a central theme at a recent conference on COPD and hospital readmissions sponsored by the COPD Foundation in Washington, D.C. The meeting brought together pulmonologists, policy makers, healthcare quality-improvement experts, and representatives from four national, patient-care transitions programs: the Care Transitions Program of the University of Colorado School of Medicine in Denver; Project RED (Re-Engineered Discharge) at Boston University Medical Center; the Transitional Care Model of the University of Pennsylvania in Philadelphia; and SHM's Project BOOST.
"This summit reinforces what has already been said, that there needs to be a comprehensive approach to COPD patients, not just managing the disease," said one of the conference’s key speakers, Mark Williams, MD, MHM, professor and chief of the division of hospital medicine at Northwestern University Feinberg School of Medicine in Chicago and principal investigator of Project BOOST. "Similar to heart failure, there needs to be support for the patient at home."
COPD is the third-leading cause of death in the U.S., with an estimated 15 million diagnosed patients and many more undiagnosed. One-fifth of hospitalized COPD patients are readmitted within 30 days, according to data from the Agency for Healthcare Research and Quality [PDF]. Many simultaneously present with heart disease, pneumonia, diabetes, or other comorbidities, and 62% of hospitalized COPD patients are readmitted for a condition other than COPD, says Brian Carlin, MD, senior staff physician at Allegheny General Hospital in Pittsburgh, Pa.
Preventing readmissions underscores the need for a patient-centered approach, says conference co-chair Jerry Krishnan, MD, PhD, professor of medicine and public health associate vice president for population health sciences at the University of Illinois Hospital and Health System in Chicago. "There's a tremendous amount of interest among physicians about the quality of care and health outcomes for these patients and conflicting evidence about what actually works," Dr. Krishnan says. "What works in one setting is unlikely to work in another setting."
Other physicians at the conference discussed ways hospitalists could help reduce COPD-related readmissions. Guidelines for non-pharmacologic interventions emphasize access to smoking cessation programs, immunizations for influenza, and pulmonary rehabilitation, says Byron Thomashow, MD, clinical professor of medicine at Columbia University Medical Center in New York City. "I also encourage all of my patients to exercise," he says.
Visit our website for more information on patient care and COPD.
Urolithiasis in a Patient With HIV Receiving Atazanavir
HIV Research Has Women to Thank; What the Affordable Care Act Means for the IHS; Making It Easier to Get the Right Health Care; Job Training for Veterans With Disabilities
Recognizing Posttraumatic Stress Disorder
Center for Health Equity Research and Promotion
Gout cases jump sevenfold in half-century
SAN DIEGO – The number of Americans with gout has climbed sevenfold during the last 50 years, according to Dr. Eswar Krishnan.
The population burden of illness imposed by gout has risen both in men and women across all age groups, but most strikingly so in men older than 65 years, said Dr. Krishnan, director of clinical epidemiology in the division of immunology and rheumatology at Stanford (Calif.) University.
He turned to National Health and Nutrition Examination Survey (NHANES) data to gain a more precise picture of U.S. trends in gout prevalence over time than has previously been available. He accomplished this by comparing age- and sex-specific rates from the 1959-1962 and the 2009-2010 editions of the long-running Centers for Disease Control and Prevention–sponsored surveys.
The unadjusted population-based prevalence of self-reported gout jumped from 6 cases per 1,000 during 1959-1962 to 26 per 1,000 in 2009-2010. The estimated number of gout cases climbed from 1.1 million in 1960 to 8.1 million in 2010. Yet the proportion of gout patients who were women remained steady at 31% over time.
The mean age of Americans with gout rose over the half-century from 54 to 61 years among men and from 55 to 65 years among women, he reported at the annual meeting of the American College of Rheumatology.
Statistical analysis indicated that the increase in gout cases among women during the last 50 years could be accounted for entirely by the much-discussed societal growth in abdominal obesity. In contrast, the explanation for the increased prevalence of gout in men was multifactorial. The bulk of the increase was associated with an increased life span and the graying of America, coupled with higher rates of hypertension, diabetes, and abdominal obesity.
However, an immeasurable portion of the increase in gout during the past half-century is probably due to increased awareness of the disease among the U.S. population, Dr. Krishnan added.
NHANES is sponsored by the Centers for Disease Control and Prevention. Dr. Krishnan reported having received research grants from Takeda, which markets gout medication.
SAN DIEGO – The number of Americans with gout has climbed sevenfold during the last 50 years, according to Dr. Eswar Krishnan.
The population burden of illness imposed by gout has risen both in men and women across all age groups, but most strikingly so in men older than 65 years, said Dr. Krishnan, director of clinical epidemiology in the division of immunology and rheumatology at Stanford (Calif.) University.
He turned to National Health and Nutrition Examination Survey (NHANES) data to gain a more precise picture of U.S. trends in gout prevalence over time than has previously been available. He accomplished this by comparing age- and sex-specific rates from the 1959-1962 and the 2009-2010 editions of the long-running Centers for Disease Control and Prevention–sponsored surveys.
The unadjusted population-based prevalence of self-reported gout jumped from 6 cases per 1,000 during 1959-1962 to 26 per 1,000 in 2009-2010. The estimated number of gout cases climbed from 1.1 million in 1960 to 8.1 million in 2010. Yet the proportion of gout patients who were women remained steady at 31% over time.
The mean age of Americans with gout rose over the half-century from 54 to 61 years among men and from 55 to 65 years among women, he reported at the annual meeting of the American College of Rheumatology.
Statistical analysis indicated that the increase in gout cases among women during the last 50 years could be accounted for entirely by the much-discussed societal growth in abdominal obesity. In contrast, the explanation for the increased prevalence of gout in men was multifactorial. The bulk of the increase was associated with an increased life span and the graying of America, coupled with higher rates of hypertension, diabetes, and abdominal obesity.
However, an immeasurable portion of the increase in gout during the past half-century is probably due to increased awareness of the disease among the U.S. population, Dr. Krishnan added.
NHANES is sponsored by the Centers for Disease Control and Prevention. Dr. Krishnan reported having received research grants from Takeda, which markets gout medication.
SAN DIEGO – The number of Americans with gout has climbed sevenfold during the last 50 years, according to Dr. Eswar Krishnan.
The population burden of illness imposed by gout has risen both in men and women across all age groups, but most strikingly so in men older than 65 years, said Dr. Krishnan, director of clinical epidemiology in the division of immunology and rheumatology at Stanford (Calif.) University.
He turned to National Health and Nutrition Examination Survey (NHANES) data to gain a more precise picture of U.S. trends in gout prevalence over time than has previously been available. He accomplished this by comparing age- and sex-specific rates from the 1959-1962 and the 2009-2010 editions of the long-running Centers for Disease Control and Prevention–sponsored surveys.
The unadjusted population-based prevalence of self-reported gout jumped from 6 cases per 1,000 during 1959-1962 to 26 per 1,000 in 2009-2010. The estimated number of gout cases climbed from 1.1 million in 1960 to 8.1 million in 2010. Yet the proportion of gout patients who were women remained steady at 31% over time.
The mean age of Americans with gout rose over the half-century from 54 to 61 years among men and from 55 to 65 years among women, he reported at the annual meeting of the American College of Rheumatology.
Statistical analysis indicated that the increase in gout cases among women during the last 50 years could be accounted for entirely by the much-discussed societal growth in abdominal obesity. In contrast, the explanation for the increased prevalence of gout in men was multifactorial. The bulk of the increase was associated with an increased life span and the graying of America, coupled with higher rates of hypertension, diabetes, and abdominal obesity.
However, an immeasurable portion of the increase in gout during the past half-century is probably due to increased awareness of the disease among the U.S. population, Dr. Krishnan added.
NHANES is sponsored by the Centers for Disease Control and Prevention. Dr. Krishnan reported having received research grants from Takeda, which markets gout medication.
AT THE ACR ANNUAL MEETING
Major finding: The estimated number of Americans with gout in the United States increased more than sevenfold from 1.1 million in 1960 to 8.1 million in 2010.
Data source: The National Health and Nutrition Examination Survey is a program of periodic, large, government-funded, national cross-sectional surveys involving a representative sample of the U.S. population.
Disclosures: The National Health and Nutrition Examination Survey is sponsored by the Centers for Disease Control and Prevention. The presenter reported receiving research grants from Takeda, which markets gout medication.
What is UnitedHealthcare doing?
A month ago, all five physicians in our practice received notice that we would no longer be covered under UnitedHealthcare Medicare Advantage plans. No reason was given, nor had we been given any kind of advanced notice that this was even a possibility. This was based on our business tax ID number, by the way, not on any individual doctor’s credentials. Very quickly it became evident that this was part of a 20%-30% reduction in their physician panels in multiple states, including Rhode Island, Connecticut, New York, New Jersey, Florida, Indiana, and Ohio.
What hasn’t been so easy to figure out is why. The insurance giant has not been forthcoming about the decision. In an advertisement in the Providence Journal, they cited "severe funding reductions for Medicare Advantage Plans."
Medicare Advantage Plans are Medicare plans that are administered by private insurance companies. They contract with the government to administer Medicare, and patients also pay a premium, making it profitable for insurers. These plans, however, are more expensive for the federal government, and in an effort to curtail the burgeoning cost of health care, "companies that don’t use 80% to 85% of revenues on care are forced to issue rebates to members for the difference," according to financial services company The Motley Fool.
In addition, there have been proposed rate cuts to Medicare Advantage Plans, in part to offset the cost of expanding Medicaid as the Affordable Care Act mandates. The Associated Press reported that UnitedHealthcare stock did not perform as expected in the third quarter of 2013. UnitedHealthcare blamed this on the rate cuts that the federal government imposed on Medicare.
So perhaps the Medicare Advantage Plans are not as profitable for the company as they once were, as the aforementioned advertisement in the Providence Journal implied. That does not explain the reduction of 20%-30% of their providers, though.
In a statement to the Hartford Courant, Dennis O’Brien, regional president of UnitedHealthcare Networks, had this to say: "We are assessing our network in Connecticut to help us provide higher quality and more affordable health care coverage for Medicare beneficiaries."
That explains nothing at all. It implies that the physicians they removed from their roster were of inferior quality and were costing them more money. And yet they have not given any explanation for what these "higher quality and more affordable" standards are. Furthermore, if quality and cost were the real issue, why would we be appropriate for UnitedHealthcare commercial patients but not for Medicare patients?
There has been a lot of speculation about why UnitedHealthcare is doing this, but until the company is more forthcoming, or is forced to account for its behavior (by subscribers or by politicians), we won’t really know.
In the meantime, the company’s unilateral decision will leave thousands of patients across states with interrupted medical care. It will take time for these patients to find new doctors, establish care, and build rapport.
If there is anything that’s become clearer to me from this debacle, it is this: We doctors hold ourselves accountable to our patients, but UnitedHealthcare, and maybe other private insurers as well, is accountable only to its shareholders.
In the debate over universal health care, health care is repeatedly referred to as a commodity that is malleable according to market forces. But this is a false equivalence, is it not? Chief Justice John Roberts’ preference for broccoli may be subject to supply and demand, but your right to health care should not be. That narrative needs to be reframed if people’s health and well-being are ever to trump the investors’ bottom line.
Dr. Chan practices rheumatology in Pawtucket, R.I.
A month ago, all five physicians in our practice received notice that we would no longer be covered under UnitedHealthcare Medicare Advantage plans. No reason was given, nor had we been given any kind of advanced notice that this was even a possibility. This was based on our business tax ID number, by the way, not on any individual doctor’s credentials. Very quickly it became evident that this was part of a 20%-30% reduction in their physician panels in multiple states, including Rhode Island, Connecticut, New York, New Jersey, Florida, Indiana, and Ohio.
What hasn’t been so easy to figure out is why. The insurance giant has not been forthcoming about the decision. In an advertisement in the Providence Journal, they cited "severe funding reductions for Medicare Advantage Plans."
Medicare Advantage Plans are Medicare plans that are administered by private insurance companies. They contract with the government to administer Medicare, and patients also pay a premium, making it profitable for insurers. These plans, however, are more expensive for the federal government, and in an effort to curtail the burgeoning cost of health care, "companies that don’t use 80% to 85% of revenues on care are forced to issue rebates to members for the difference," according to financial services company The Motley Fool.
In addition, there have been proposed rate cuts to Medicare Advantage Plans, in part to offset the cost of expanding Medicaid as the Affordable Care Act mandates. The Associated Press reported that UnitedHealthcare stock did not perform as expected in the third quarter of 2013. UnitedHealthcare blamed this on the rate cuts that the federal government imposed on Medicare.
So perhaps the Medicare Advantage Plans are not as profitable for the company as they once were, as the aforementioned advertisement in the Providence Journal implied. That does not explain the reduction of 20%-30% of their providers, though.
In a statement to the Hartford Courant, Dennis O’Brien, regional president of UnitedHealthcare Networks, had this to say: "We are assessing our network in Connecticut to help us provide higher quality and more affordable health care coverage for Medicare beneficiaries."
That explains nothing at all. It implies that the physicians they removed from their roster were of inferior quality and were costing them more money. And yet they have not given any explanation for what these "higher quality and more affordable" standards are. Furthermore, if quality and cost were the real issue, why would we be appropriate for UnitedHealthcare commercial patients but not for Medicare patients?
There has been a lot of speculation about why UnitedHealthcare is doing this, but until the company is more forthcoming, or is forced to account for its behavior (by subscribers or by politicians), we won’t really know.
In the meantime, the company’s unilateral decision will leave thousands of patients across states with interrupted medical care. It will take time for these patients to find new doctors, establish care, and build rapport.
If there is anything that’s become clearer to me from this debacle, it is this: We doctors hold ourselves accountable to our patients, but UnitedHealthcare, and maybe other private insurers as well, is accountable only to its shareholders.
In the debate over universal health care, health care is repeatedly referred to as a commodity that is malleable according to market forces. But this is a false equivalence, is it not? Chief Justice John Roberts’ preference for broccoli may be subject to supply and demand, but your right to health care should not be. That narrative needs to be reframed if people’s health and well-being are ever to trump the investors’ bottom line.
Dr. Chan practices rheumatology in Pawtucket, R.I.
A month ago, all five physicians in our practice received notice that we would no longer be covered under UnitedHealthcare Medicare Advantage plans. No reason was given, nor had we been given any kind of advanced notice that this was even a possibility. This was based on our business tax ID number, by the way, not on any individual doctor’s credentials. Very quickly it became evident that this was part of a 20%-30% reduction in their physician panels in multiple states, including Rhode Island, Connecticut, New York, New Jersey, Florida, Indiana, and Ohio.
What hasn’t been so easy to figure out is why. The insurance giant has not been forthcoming about the decision. In an advertisement in the Providence Journal, they cited "severe funding reductions for Medicare Advantage Plans."
Medicare Advantage Plans are Medicare plans that are administered by private insurance companies. They contract with the government to administer Medicare, and patients also pay a premium, making it profitable for insurers. These plans, however, are more expensive for the federal government, and in an effort to curtail the burgeoning cost of health care, "companies that don’t use 80% to 85% of revenues on care are forced to issue rebates to members for the difference," according to financial services company The Motley Fool.
In addition, there have been proposed rate cuts to Medicare Advantage Plans, in part to offset the cost of expanding Medicaid as the Affordable Care Act mandates. The Associated Press reported that UnitedHealthcare stock did not perform as expected in the third quarter of 2013. UnitedHealthcare blamed this on the rate cuts that the federal government imposed on Medicare.
So perhaps the Medicare Advantage Plans are not as profitable for the company as they once were, as the aforementioned advertisement in the Providence Journal implied. That does not explain the reduction of 20%-30% of their providers, though.
In a statement to the Hartford Courant, Dennis O’Brien, regional president of UnitedHealthcare Networks, had this to say: "We are assessing our network in Connecticut to help us provide higher quality and more affordable health care coverage for Medicare beneficiaries."
That explains nothing at all. It implies that the physicians they removed from their roster were of inferior quality and were costing them more money. And yet they have not given any explanation for what these "higher quality and more affordable" standards are. Furthermore, if quality and cost were the real issue, why would we be appropriate for UnitedHealthcare commercial patients but not for Medicare patients?
There has been a lot of speculation about why UnitedHealthcare is doing this, but until the company is more forthcoming, or is forced to account for its behavior (by subscribers or by politicians), we won’t really know.
In the meantime, the company’s unilateral decision will leave thousands of patients across states with interrupted medical care. It will take time for these patients to find new doctors, establish care, and build rapport.
If there is anything that’s become clearer to me from this debacle, it is this: We doctors hold ourselves accountable to our patients, but UnitedHealthcare, and maybe other private insurers as well, is accountable only to its shareholders.
In the debate over universal health care, health care is repeatedly referred to as a commodity that is malleable according to market forces. But this is a false equivalence, is it not? Chief Justice John Roberts’ preference for broccoli may be subject to supply and demand, but your right to health care should not be. That narrative needs to be reframed if people’s health and well-being are ever to trump the investors’ bottom line.
Dr. Chan practices rheumatology in Pawtucket, R.I.