User login
Tackling a Delicate Subject With Heart Failure Patients
New and Noteworthy Information—January
Patients with multiple sclerosis (MS) disease activity have a higher rate of thinning of the ganglion cell/inner plexiform (GCIP) layer of the eye, researchers reported in the January 1 Neurology. Annual rates of GCIP thinning may be highest among patients with new gadolinium-enhancing lesions, new T2 lesions, and disease duration of less than five years. The investigators performed spectral-domain optical coherence tomography scans every six months on 164 patients with MS and 59 healthy controls. The mean follow-up time was 21.1 months. Annual GCIP thinning occurred 42% faster in patients with relapses, 54% faster in patients with new gadolinium-enhanced lesions, and 36% faster in patients with new T2 lesions.
Vaccination with a monovalent AS03 adjuvanted pandemic A/H1N1 2009 influenza vaccine does not appear to be associated with an increased risk of epileptic seizures, according to research published in the December 28, 2012, BMJ. Researchers studied 373,398 people with and without epilepsy who had received the vaccine. The primary end point was admission to a hospital or outpatient hospital care with epileptic seizures. The investigators found no increased risk of seizures in patients with epilepsy and a nonsignificantly decreased risk of seizures in persons without epilepsy during the initial seven-day risk period. During the subsequent 23-day risk period, people without epilepsy had a nonsignificantly increased risk of seizures, but patients with epilepsy had no increase in risk of seizures.
Variations in some genes associated with risk for psychiatric disorders may be observed as differences in brain structure in neonates, according to a study published in the January 2 online Cerebral Cortex. Investigators performed automated region-of-interest volumetry and tensor-based morphometry on 272 newborns who had had high-resolution MRI scans. The group found that estrogen receptor alpha (rs9340799) predicted intracranial volume. Polymorphisms in estrogen receptor alpha (rs9340799), as well as in disrupted-in-schizophrenia 1 (DISC1, rs821616), catechol-O-methyltransferase (COMT), neuregulin 1, apolipoprotein E, and brain-derived neurotrophic factor, were significantly associated with local variation in gray matter volume. “The results highlight the importance of prenatal brain development in mediating psychiatric risk,” noted the authors.
Four months after mild traumatic brain injury (TBI), white matter abnormalities may persist in children, even if cognitive symptoms have resolved, according to research published in the December 12, 2012, Journal of Neuroscience. The magnitude and duration of these abnormalities also appear to be greater in children with mild TBI than in adults with mild TBI. Researchers performed fractional anisotropy, axial diffusivity, and radial diffusivity on 15 children with semiacute mild TBI and 15 matched controls. Post-TBI cognitive dysfunction was observed in the domains of attention and processing speed. Increased anisotropy identified patients with pediatric mild TBI with 90% accuracy but was not associated with neuropsychologic deficits. Anisotropic diffusion may provide an objective biomarker of pediatric mild TBI.
The FDA has approved Eliquis (apixaban) for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation. In a phase III clinical trial, Eliquis, an oral anticoagulant, reduced the risk of stroke or systemic embolism by 21%, compared with warfarin. The drug primarily reduced the risk of hemorrhagic stroke and ischemic stroke that converted to hemorrhagic stroke, and it also decreased the risks of major bleeding and all-cause mortality, compared with warfarin. Eliquis inhibits Factor Xa, a blood-clotting protein, thus decreasing thrombin generation and blood clots. The recommended dose is 5 mg twice daily. For patients age 80 or older and those who weigh 60 kg or less, the recommended dose is 2.5 mg twice daily. Eliquis is manufactured by Bristol-Myers Squibb (New York City) and comarketed with Pfizer (New York City).
Intermittent fasting, together with a ketogenic diet, may reduce seizures in children with epilepsy to a greater extent than the ketogenic diet alone, investigators reported in the November 30, 2012, online Epilepsy Research. The researchers placed six children with an incomplete response to a ketogenic diet on an intermittent fasting regimen. The children, ages 2 to 7, fasted on alternate days. Four children had transient improvement in seizure control, but they also had hunger-related adverse reactions. Three patients adhered to the combined intermittent fasting and ketogenic diet regimen for two months. The ketogenic diet and intermittent fasting may not share the same anticonvulsant mechanisms, noted the authors.
The available evidence does not support the use of cannabis extract to treat multiple sclerosis (MS), according to a review published in the December 2012 Drug and Therapeutics Bulletin. Researchers concluded that the trial data for nabiximols, a mouth spray for patients with MS containing dronabinol and cannabidiol, were limited. In the trials, which were the basis for the drug’s approval, symptoms decreased in a slightly higher number of patients taking nabiximols, compared with patients taking placebo. The drug was used for relatively short periods (ie, six weeks to four months) in many of these studies, however, and no study compared nabiximols with another active ingredient. One properly designed trial with a sufficient number of patients showed no difference in symptom relief between participants who took nabiximols and those who did not.
Baseline depression was associated with mild cognitive impairment (MCI) and dementia in individuals 65 or older, researchers reported in the December 31, 2012, Archives of Neurology. Depression may coincide with cognitive impairment, but may not precede it, the study authors noted. The investigators studied 2,160 community-dwelling Medicare recipients in New York City. The team defined depression as a score of 4 or more on the Center for Epidemiological Studies Depression scale. MCI, dementia, and progression from MCI to dementia were the study’s main outcome measures. Baseline depression was associated with an increased risk of incident dementia, but not with incident MCI. Participants with MCI and comorbid depression at baseline had a higher risk of progression to dementia, but not Alzheimer’s disease.
Consumption of fructose resulted in a smaller increase in systemic glucose, insulin, and glucagon-like polypeptide 1 levels than consumption of glucose, according to research published in the January 2 JAMA. Glucose ingestion was associated with a significantly greater reduction in hypothalamic cerebral blood flow than fructose ingestion. Researchers performed MRIs of 20 healthy adults at baseline and after ingestion of a glucose or fructose drink. The blinded study had a random-order crossover design. Compared with baseline, glucose ingestion increased functional connectivity between the hypothalamus and the thalamus and striatum. Fructose increased connectivity between the hypothalamus and thalamus, but not the striatum. Fructose reduced regional cerebral blood flow in the thalamus, hippocampus, posterior cingulate cortex, fusiform, and visual cortex.
Research published in the January 7 online Epilepsia provides evidence for a shared genetic susceptibility to epilespsy and migraine with aura. Compared with migraine without aura, the prevalence of migraine with aura was significantly increased among patients with epilepsy who have two or more first-degree relatives with epilepsy. Investigators studied the prevalence of a history of migraine in 730 participants in the Epilepsy Phenome/Genome Project. Eligible participants were 12 or older, had nonacquired focal epilepsy or generalized epilepsy, and had one or more relative epilepsy of unknown cause. The researchers collected information on migraine with and without aura using an instrument validated for individuals 12 and older. The team also interviewed participants about the history of seizure disorders in nonenrolled family members.
Higher exposure to benomyl is associated with an increased risk for Parkinson’s disease, according to an epidemiologic study published in the December 24, 2012, online Proceedings of the National Academy of Sciences. In primary mesencephalic neurons, benomyl exposure inhibits aldehyde dehydrogenase (ALDH) and alters dopamine homeostasis. Investigators tested the effects of benomyl in cell cultures and confirmed that the chemical damaged or destroyed dopaminergic neurons. The researchers also found that benomyl caused the loss of dopaminergic neurons in zebrafish. The ALDH model for Parkinson’s disease etiology may help explain the selective vulnerability of dopaminergic neurons and describe the mechanism through which environmental toxicants contribute to Parkinson’s disease pathogenesis, the authors theorized.
Patients with a history of traumatic brain injury (TBI) and loss of consciousness may have an increased risk for future TBI and loss of consciousness, according to a study published in the November 21, 2012, online Journal of Neurology, Neurosurgery, and Psychiatry. Researchers are conducting an ongoing study of 4,225 nondemented adults age 65 and older. Participants are seen every two years, and 14% have reported a lifetime history of TBI and loss of consciousness. Individuals reporting a first injury before age 25 had an adjusted hazard ratio of 2.54 for TBI and loss of consciousness, compared with a hazard ratio of 3.79 for adults with first injury after age 55.
—Erik Greb
Patients with multiple sclerosis (MS) disease activity have a higher rate of thinning of the ganglion cell/inner plexiform (GCIP) layer of the eye, researchers reported in the January 1 Neurology. Annual rates of GCIP thinning may be highest among patients with new gadolinium-enhancing lesions, new T2 lesions, and disease duration of less than five years. The investigators performed spectral-domain optical coherence tomography scans every six months on 164 patients with MS and 59 healthy controls. The mean follow-up time was 21.1 months. Annual GCIP thinning occurred 42% faster in patients with relapses, 54% faster in patients with new gadolinium-enhanced lesions, and 36% faster in patients with new T2 lesions.
Vaccination with a monovalent AS03 adjuvanted pandemic A/H1N1 2009 influenza vaccine does not appear to be associated with an increased risk of epileptic seizures, according to research published in the December 28, 2012, BMJ. Researchers studied 373,398 people with and without epilepsy who had received the vaccine. The primary end point was admission to a hospital or outpatient hospital care with epileptic seizures. The investigators found no increased risk of seizures in patients with epilepsy and a nonsignificantly decreased risk of seizures in persons without epilepsy during the initial seven-day risk period. During the subsequent 23-day risk period, people without epilepsy had a nonsignificantly increased risk of seizures, but patients with epilepsy had no increase in risk of seizures.
Variations in some genes associated with risk for psychiatric disorders may be observed as differences in brain structure in neonates, according to a study published in the January 2 online Cerebral Cortex. Investigators performed automated region-of-interest volumetry and tensor-based morphometry on 272 newborns who had had high-resolution MRI scans. The group found that estrogen receptor alpha (rs9340799) predicted intracranial volume. Polymorphisms in estrogen receptor alpha (rs9340799), as well as in disrupted-in-schizophrenia 1 (DISC1, rs821616), catechol-O-methyltransferase (COMT), neuregulin 1, apolipoprotein E, and brain-derived neurotrophic factor, were significantly associated with local variation in gray matter volume. “The results highlight the importance of prenatal brain development in mediating psychiatric risk,” noted the authors.
Four months after mild traumatic brain injury (TBI), white matter abnormalities may persist in children, even if cognitive symptoms have resolved, according to research published in the December 12, 2012, Journal of Neuroscience. The magnitude and duration of these abnormalities also appear to be greater in children with mild TBI than in adults with mild TBI. Researchers performed fractional anisotropy, axial diffusivity, and radial diffusivity on 15 children with semiacute mild TBI and 15 matched controls. Post-TBI cognitive dysfunction was observed in the domains of attention and processing speed. Increased anisotropy identified patients with pediatric mild TBI with 90% accuracy but was not associated with neuropsychologic deficits. Anisotropic diffusion may provide an objective biomarker of pediatric mild TBI.
The FDA has approved Eliquis (apixaban) for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation. In a phase III clinical trial, Eliquis, an oral anticoagulant, reduced the risk of stroke or systemic embolism by 21%, compared with warfarin. The drug primarily reduced the risk of hemorrhagic stroke and ischemic stroke that converted to hemorrhagic stroke, and it also decreased the risks of major bleeding and all-cause mortality, compared with warfarin. Eliquis inhibits Factor Xa, a blood-clotting protein, thus decreasing thrombin generation and blood clots. The recommended dose is 5 mg twice daily. For patients age 80 or older and those who weigh 60 kg or less, the recommended dose is 2.5 mg twice daily. Eliquis is manufactured by Bristol-Myers Squibb (New York City) and comarketed with Pfizer (New York City).
Intermittent fasting, together with a ketogenic diet, may reduce seizures in children with epilepsy to a greater extent than the ketogenic diet alone, investigators reported in the November 30, 2012, online Epilepsy Research. The researchers placed six children with an incomplete response to a ketogenic diet on an intermittent fasting regimen. The children, ages 2 to 7, fasted on alternate days. Four children had transient improvement in seizure control, but they also had hunger-related adverse reactions. Three patients adhered to the combined intermittent fasting and ketogenic diet regimen for two months. The ketogenic diet and intermittent fasting may not share the same anticonvulsant mechanisms, noted the authors.
The available evidence does not support the use of cannabis extract to treat multiple sclerosis (MS), according to a review published in the December 2012 Drug and Therapeutics Bulletin. Researchers concluded that the trial data for nabiximols, a mouth spray for patients with MS containing dronabinol and cannabidiol, were limited. In the trials, which were the basis for the drug’s approval, symptoms decreased in a slightly higher number of patients taking nabiximols, compared with patients taking placebo. The drug was used for relatively short periods (ie, six weeks to four months) in many of these studies, however, and no study compared nabiximols with another active ingredient. One properly designed trial with a sufficient number of patients showed no difference in symptom relief between participants who took nabiximols and those who did not.
Baseline depression was associated with mild cognitive impairment (MCI) and dementia in individuals 65 or older, researchers reported in the December 31, 2012, Archives of Neurology. Depression may coincide with cognitive impairment, but may not precede it, the study authors noted. The investigators studied 2,160 community-dwelling Medicare recipients in New York City. The team defined depression as a score of 4 or more on the Center for Epidemiological Studies Depression scale. MCI, dementia, and progression from MCI to dementia were the study’s main outcome measures. Baseline depression was associated with an increased risk of incident dementia, but not with incident MCI. Participants with MCI and comorbid depression at baseline had a higher risk of progression to dementia, but not Alzheimer’s disease.
Consumption of fructose resulted in a smaller increase in systemic glucose, insulin, and glucagon-like polypeptide 1 levels than consumption of glucose, according to research published in the January 2 JAMA. Glucose ingestion was associated with a significantly greater reduction in hypothalamic cerebral blood flow than fructose ingestion. Researchers performed MRIs of 20 healthy adults at baseline and after ingestion of a glucose or fructose drink. The blinded study had a random-order crossover design. Compared with baseline, glucose ingestion increased functional connectivity between the hypothalamus and the thalamus and striatum. Fructose increased connectivity between the hypothalamus and thalamus, but not the striatum. Fructose reduced regional cerebral blood flow in the thalamus, hippocampus, posterior cingulate cortex, fusiform, and visual cortex.
Research published in the January 7 online Epilepsia provides evidence for a shared genetic susceptibility to epilespsy and migraine with aura. Compared with migraine without aura, the prevalence of migraine with aura was significantly increased among patients with epilepsy who have two or more first-degree relatives with epilepsy. Investigators studied the prevalence of a history of migraine in 730 participants in the Epilepsy Phenome/Genome Project. Eligible participants were 12 or older, had nonacquired focal epilepsy or generalized epilepsy, and had one or more relative epilepsy of unknown cause. The researchers collected information on migraine with and without aura using an instrument validated for individuals 12 and older. The team also interviewed participants about the history of seizure disorders in nonenrolled family members.
Higher exposure to benomyl is associated with an increased risk for Parkinson’s disease, according to an epidemiologic study published in the December 24, 2012, online Proceedings of the National Academy of Sciences. In primary mesencephalic neurons, benomyl exposure inhibits aldehyde dehydrogenase (ALDH) and alters dopamine homeostasis. Investigators tested the effects of benomyl in cell cultures and confirmed that the chemical damaged or destroyed dopaminergic neurons. The researchers also found that benomyl caused the loss of dopaminergic neurons in zebrafish. The ALDH model for Parkinson’s disease etiology may help explain the selective vulnerability of dopaminergic neurons and describe the mechanism through which environmental toxicants contribute to Parkinson’s disease pathogenesis, the authors theorized.
Patients with a history of traumatic brain injury (TBI) and loss of consciousness may have an increased risk for future TBI and loss of consciousness, according to a study published in the November 21, 2012, online Journal of Neurology, Neurosurgery, and Psychiatry. Researchers are conducting an ongoing study of 4,225 nondemented adults age 65 and older. Participants are seen every two years, and 14% have reported a lifetime history of TBI and loss of consciousness. Individuals reporting a first injury before age 25 had an adjusted hazard ratio of 2.54 for TBI and loss of consciousness, compared with a hazard ratio of 3.79 for adults with first injury after age 55.
—Erik Greb
Patients with multiple sclerosis (MS) disease activity have a higher rate of thinning of the ganglion cell/inner plexiform (GCIP) layer of the eye, researchers reported in the January 1 Neurology. Annual rates of GCIP thinning may be highest among patients with new gadolinium-enhancing lesions, new T2 lesions, and disease duration of less than five years. The investigators performed spectral-domain optical coherence tomography scans every six months on 164 patients with MS and 59 healthy controls. The mean follow-up time was 21.1 months. Annual GCIP thinning occurred 42% faster in patients with relapses, 54% faster in patients with new gadolinium-enhanced lesions, and 36% faster in patients with new T2 lesions.
Vaccination with a monovalent AS03 adjuvanted pandemic A/H1N1 2009 influenza vaccine does not appear to be associated with an increased risk of epileptic seizures, according to research published in the December 28, 2012, BMJ. Researchers studied 373,398 people with and without epilepsy who had received the vaccine. The primary end point was admission to a hospital or outpatient hospital care with epileptic seizures. The investigators found no increased risk of seizures in patients with epilepsy and a nonsignificantly decreased risk of seizures in persons without epilepsy during the initial seven-day risk period. During the subsequent 23-day risk period, people without epilepsy had a nonsignificantly increased risk of seizures, but patients with epilepsy had no increase in risk of seizures.
Variations in some genes associated with risk for psychiatric disorders may be observed as differences in brain structure in neonates, according to a study published in the January 2 online Cerebral Cortex. Investigators performed automated region-of-interest volumetry and tensor-based morphometry on 272 newborns who had had high-resolution MRI scans. The group found that estrogen receptor alpha (rs9340799) predicted intracranial volume. Polymorphisms in estrogen receptor alpha (rs9340799), as well as in disrupted-in-schizophrenia 1 (DISC1, rs821616), catechol-O-methyltransferase (COMT), neuregulin 1, apolipoprotein E, and brain-derived neurotrophic factor, were significantly associated with local variation in gray matter volume. “The results highlight the importance of prenatal brain development in mediating psychiatric risk,” noted the authors.
Four months after mild traumatic brain injury (TBI), white matter abnormalities may persist in children, even if cognitive symptoms have resolved, according to research published in the December 12, 2012, Journal of Neuroscience. The magnitude and duration of these abnormalities also appear to be greater in children with mild TBI than in adults with mild TBI. Researchers performed fractional anisotropy, axial diffusivity, and radial diffusivity on 15 children with semiacute mild TBI and 15 matched controls. Post-TBI cognitive dysfunction was observed in the domains of attention and processing speed. Increased anisotropy identified patients with pediatric mild TBI with 90% accuracy but was not associated with neuropsychologic deficits. Anisotropic diffusion may provide an objective biomarker of pediatric mild TBI.
The FDA has approved Eliquis (apixaban) for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation. In a phase III clinical trial, Eliquis, an oral anticoagulant, reduced the risk of stroke or systemic embolism by 21%, compared with warfarin. The drug primarily reduced the risk of hemorrhagic stroke and ischemic stroke that converted to hemorrhagic stroke, and it also decreased the risks of major bleeding and all-cause mortality, compared with warfarin. Eliquis inhibits Factor Xa, a blood-clotting protein, thus decreasing thrombin generation and blood clots. The recommended dose is 5 mg twice daily. For patients age 80 or older and those who weigh 60 kg or less, the recommended dose is 2.5 mg twice daily. Eliquis is manufactured by Bristol-Myers Squibb (New York City) and comarketed with Pfizer (New York City).
Intermittent fasting, together with a ketogenic diet, may reduce seizures in children with epilepsy to a greater extent than the ketogenic diet alone, investigators reported in the November 30, 2012, online Epilepsy Research. The researchers placed six children with an incomplete response to a ketogenic diet on an intermittent fasting regimen. The children, ages 2 to 7, fasted on alternate days. Four children had transient improvement in seizure control, but they also had hunger-related adverse reactions. Three patients adhered to the combined intermittent fasting and ketogenic diet regimen for two months. The ketogenic diet and intermittent fasting may not share the same anticonvulsant mechanisms, noted the authors.
The available evidence does not support the use of cannabis extract to treat multiple sclerosis (MS), according to a review published in the December 2012 Drug and Therapeutics Bulletin. Researchers concluded that the trial data for nabiximols, a mouth spray for patients with MS containing dronabinol and cannabidiol, were limited. In the trials, which were the basis for the drug’s approval, symptoms decreased in a slightly higher number of patients taking nabiximols, compared with patients taking placebo. The drug was used for relatively short periods (ie, six weeks to four months) in many of these studies, however, and no study compared nabiximols with another active ingredient. One properly designed trial with a sufficient number of patients showed no difference in symptom relief between participants who took nabiximols and those who did not.
Baseline depression was associated with mild cognitive impairment (MCI) and dementia in individuals 65 or older, researchers reported in the December 31, 2012, Archives of Neurology. Depression may coincide with cognitive impairment, but may not precede it, the study authors noted. The investigators studied 2,160 community-dwelling Medicare recipients in New York City. The team defined depression as a score of 4 or more on the Center for Epidemiological Studies Depression scale. MCI, dementia, and progression from MCI to dementia were the study’s main outcome measures. Baseline depression was associated with an increased risk of incident dementia, but not with incident MCI. Participants with MCI and comorbid depression at baseline had a higher risk of progression to dementia, but not Alzheimer’s disease.
Consumption of fructose resulted in a smaller increase in systemic glucose, insulin, and glucagon-like polypeptide 1 levels than consumption of glucose, according to research published in the January 2 JAMA. Glucose ingestion was associated with a significantly greater reduction in hypothalamic cerebral blood flow than fructose ingestion. Researchers performed MRIs of 20 healthy adults at baseline and after ingestion of a glucose or fructose drink. The blinded study had a random-order crossover design. Compared with baseline, glucose ingestion increased functional connectivity between the hypothalamus and the thalamus and striatum. Fructose increased connectivity between the hypothalamus and thalamus, but not the striatum. Fructose reduced regional cerebral blood flow in the thalamus, hippocampus, posterior cingulate cortex, fusiform, and visual cortex.
Research published in the January 7 online Epilepsia provides evidence for a shared genetic susceptibility to epilespsy and migraine with aura. Compared with migraine without aura, the prevalence of migraine with aura was significantly increased among patients with epilepsy who have two or more first-degree relatives with epilepsy. Investigators studied the prevalence of a history of migraine in 730 participants in the Epilepsy Phenome/Genome Project. Eligible participants were 12 or older, had nonacquired focal epilepsy or generalized epilepsy, and had one or more relative epilepsy of unknown cause. The researchers collected information on migraine with and without aura using an instrument validated for individuals 12 and older. The team also interviewed participants about the history of seizure disorders in nonenrolled family members.
Higher exposure to benomyl is associated with an increased risk for Parkinson’s disease, according to an epidemiologic study published in the December 24, 2012, online Proceedings of the National Academy of Sciences. In primary mesencephalic neurons, benomyl exposure inhibits aldehyde dehydrogenase (ALDH) and alters dopamine homeostasis. Investigators tested the effects of benomyl in cell cultures and confirmed that the chemical damaged or destroyed dopaminergic neurons. The researchers also found that benomyl caused the loss of dopaminergic neurons in zebrafish. The ALDH model for Parkinson’s disease etiology may help explain the selective vulnerability of dopaminergic neurons and describe the mechanism through which environmental toxicants contribute to Parkinson’s disease pathogenesis, the authors theorized.
Patients with a history of traumatic brain injury (TBI) and loss of consciousness may have an increased risk for future TBI and loss of consciousness, according to a study published in the November 21, 2012, online Journal of Neurology, Neurosurgery, and Psychiatry. Researchers are conducting an ongoing study of 4,225 nondemented adults age 65 and older. Participants are seen every two years, and 14% have reported a lifetime history of TBI and loss of consciousness. Individuals reporting a first injury before age 25 had an adjusted hazard ratio of 2.54 for TBI and loss of consciousness, compared with a hazard ratio of 3.79 for adults with first injury after age 55.
—Erik Greb
Man, 56, With Wrist Pain After a Fall
A white man, age 56, presented to his primary care clinician with wrist pain and swelling. Two days earlier, he had fallen from a step stool and landed on his right wrist. He treated the pain by resting, elevating his arm, applying ice, and taking ibuprofen 800 mg tid. He said he had lost strength in his hand and arm and was experiencing numbness and tingling in his right hand and fingers.
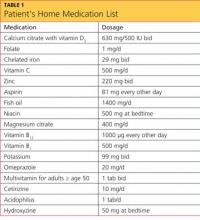
The patient’s medical history included hypertension, type 2 diabetes mellitus, morbid obesity, obstructive sleep apnea, asthma, carpel tunnel syndrome, and peripheral neuropathy. His surgical history was significant for duodenal switch gastric bypass surgery, performed eight years earlier, and his weight at the time of presentation was 200 lb; before his gastric bypass, he weighed 385 lb. Since the surgery, his hypertension, diabetes, asthma, and sleep apnea had all resolved. Table 1 shows a list of medications he was taking at the time of presentation.
The patient, a registered nurse, had been married for 30 years and had one child. He had quit smoking 15 years earlier, with a 43–pack-year smoking history. He reported social drinking but denied any recreational drug use. He was unaware of having any allergies to food or medication.
His vital signs on presentation were blood pressure, 110/75 mm Hg; heart rate, 53 beats/min; respiration, 18 breaths/min; O2 saturation, 97% on room air; and temperature, 97.5°F.
Physical exam revealed that the patient’s right wrist was ecchymotic and swollen with +1 pitting edema. The skin was warm and dry to the touch. Decreased range of motion was noted in the right wrist, compared with the left. Pain with point tenderness was noted at the right lateral wrist. Pulses were +3 with capillary refill of less than 3 seconds. The rest of the exam was unremarkable.
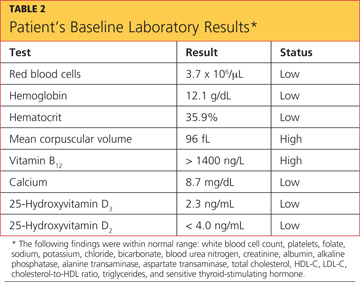
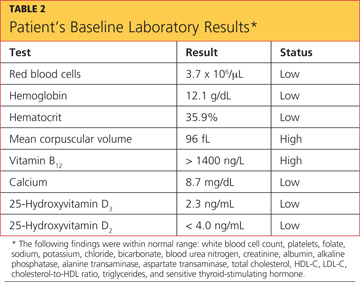
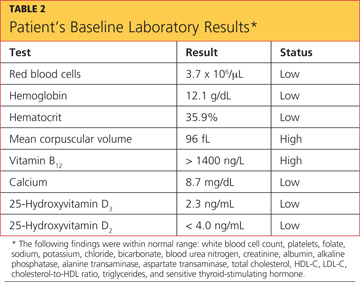
The differential diagnosis included fracture secondary to the fall, osteoporosis, osteopenia, osteomalacia, Paget’s disease, tumor, infection, and sprain or strain of the wrist. A wrist x-ray was ordered, as were the following baseline labs: complete blood count with differential (CBC), vitamin B12 and folate levels, blood chemistry, lipid profile, liver profile, total vitamin D, and sensitive thyroid-stimulating hormone. Test results are shown in Table 2.
X-ray of the wrist showed fracture only, making it possible to rule out Paget’s disease (ie, no patchy white areas noted in the bone) and tumor (no masses seen) as the immediate cause of fracture. Normal body temperature and normal white blood cell count eliminated the possibility of infection.
Because the patient was only 56 and had a history of bariatric surgery, further testing was pursued to investigate a cause for the weakened bone. Bone mineral density (BMD) testing revealed the following results:
• The lumbar spine in frontal projection measured 0.968 g/cm2 with a T-score of –2.2 and a Z-score of –2.2.
• Total BMD of the left hip was 0.863 g/cm2 with a T-score of –1.7 and a Z-score of –1.4.
• Total BMD of the left femoral neck was 0.863 g/cm2 with a T-score of 1.7 and a Z-score of –1.1.
These findings suggested osteopenia1,2 (not osteoporosis) in all sites, with a 12% decrease of BMD in the spine (suggesting increased risk for spinal fracture) and a 16.3% decrease of BMD in the hip since the patient’s most recent bone scan five years earlier (radiologist’s report). Other abnormal findings were elevated parathyroid hormone (PTH) serum, 95.7 pg/mL (reference range, 10 to 65 pg/mL); low total calcium serum, 8.7 mg/dL (reference range, 8.9 to 10.2 mg/dL), and low 25-hydroxyvitamin D total, 12.3 ng/mL (reference range, 25 to 80 ng/mL).
A 2010 clinical practice guideline from the Endocrine Society3 specifies that after malabsorptive surgery, vitamin D and calcium supplementation should be adjusted by a qualified medical professional, based on serum markers and measures of bone density. An endocrinologist who was consulted at the patient’s initial visit prescribed the following medications: vitamin D2, 50,000 U/wk PO; combined calcium citrate (vitamin D3) 500 IU with calcium 630 mg, 1 tab bid; and calcitriol 0.5 μg bid.
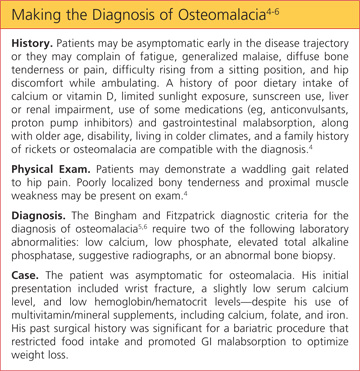
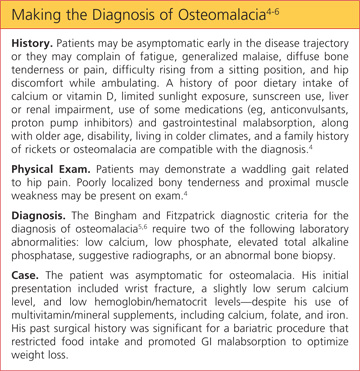
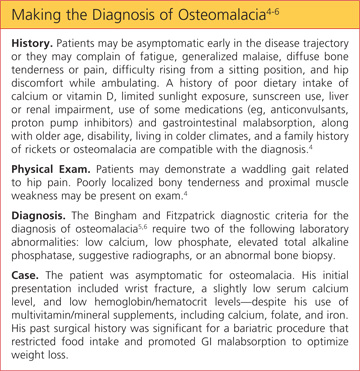
The patient’s final diagnosis was osteomalacia secondary to gastric bypass surgery. (See “Making the Diagnosis of Osteomalacia.”4-6)
DISCUSSION
According to 2008 data from the World Health Organization (WHO),7 1.4 billion persons older than 20 worldwide were overweight, and 200 million men and 300 million women were considered obese—meaning that one in every 10 adults worldwide is overweight or obese. In 2010, the WHO reports, 40 million children younger than 5 worldwide were considered overweight.7 Health care providers need to be prepared to care for the increasing number of patients who will undergo bariatric surgeries to treat obesity and its related comorbidities.8
Postoperative follow-up for the malabsorption deficiencies related to bariatric procedures should be performed every six months, including obtaining levels of alkaline phosphatase and others previously discussed. In addition, the Endocrine Society guideline3 recommends measuring levels of vitamin B12, albumin, pre-albumin, iron, and ferritin, and obtaining a CBC, a liver profile, glucose reading, creatinine measurement, and a metabolic profile at one month and two months after surgery, then every six months until two years after surgery, then annually if findings are stable.
Furthermore, the Endocrine Society3 recommends obtaining zinc levels every six months for the first year, then annually. An annual vitamin A level is optional.9 Yearly bone density testing is recommended until the patient’s BMD is deemed stable.3
Additionally, Koch and Finelli10 recommend performing the following labs postoperatively: hemoglobin A1C every three months; copper, magnesium, whole blood thiamine, vitamin B12, and a 24-hour urinary calcium every six months for the first three years, then once a year if findings remain stable.
Use of alcohol should be discouraged among patients who have undergone bariatric surgery, as its use alters micronutrient requirements and metabolism. Alcohol consumption may also contribute to dumping syndrome (ie, rapid gastric emptying).11
Any patient with a history of malabsorptive bypass surgery who complains of neurologic, visual, or skin disorders, anemia, or edema may require a further workup to rule out other absorptive deficiencies. These include vitamins A, E, and B12, zinc, folate, thiamine, niacin, selenium, and ferritin.10
Osteomalacia
Metabolic bone diseases can result from genetics, dietary factors, medication use, surgery, or hormonal irregularities. They alter the normal biochemical reactions in bone structure.
The three most common forms of metabolic bone disease are osteoporosis, osteopenia, and osteomalacia. The WHO diagnostic classifications and associated T-scores for bone mineral density1,2 indicate a T-score above –1.0 as normal. A score between –1.0 and –2.5 is indicative of osteopenia, and a score below –2.5 indicates osteoporosis. A T-score below –2.5 in the patient with a history of fragility fracture indicates severe osteoporosis.1,2
In osteomalacia, bone volume remains unchanged, but mineralization of osteoid in the mature compact and spongy bone is either delayed or inadequate. The remolding cycle continues unchanged in the formation of osteoid, but mineral calcification and deposition do not occur.3-5
Osteomalacia is normally considered a rare disorder, but it may become more common as increasing numbers of patients undergo gastric bypass operations.12,13 Primary care practitioners should monitor for this condition in such patients before serious bone loss or other problems develop.9,13,14
Vitamin D deficiency (see “Vitamin D Metabolism,”4,15-19 below), whether or not the result of gastric bypass surgery, is a major risk factor for osteomalacia. Disorders of the small bowel, the hepatobiliary system, and the pancreas are all common causes of vitamin D deficiency. Liver disease interferes with the metabolism of vitamin D. Diseases of the pancreas may cause a deficiency of bile salts, which are vital for the intestinal absorption of vitamin D.17

Restriction and Malabsorption
The case patient had undergone a gastric bypass (duodenal switch), in which a large portion of the stomach is removed and a large part of the small bowel rerouted—with both parts of the procedure causing malabsorption.11 It is in the small bowel that absorption of vitamin D and calcium takes place.
The duodenal switch gastric bypass surgery causes both restriction and malabsorption. Though similar to a biliopancreatic diversion, the duodenal switch preserves the distal stomach and the pylorus20 by way of a sleeve gastrectomy that is performed to reduce the gastric reservoir; the common channel length after revision is 100 cm, not 50 cm (as in conventional biliopancreatic diversion).13 The sleeve gastrectomy involves removal of parietal cells, reducing production of hydrochloric acid (which is necessary to break down food), and hindering the absorption of certain nutrients, including the fat-soluble vitamins, vitamin B12, and iron.12 Patients who take H2-blockers or proton pump inhibitors experience an additional decrease in the production and availability of HCl and may have an increased risk for fracture.14,20,21
In addition to its biliopancreatic diversion component, the duodenal switch diverts a large portion of the small bowel, with food restricted from moving through it. Vitamin D and protein are normally absorbed at the jejunum and ileum, but only when bile salts are present; after a duodenal switch, bile and pancreatic enzymes are not introduced into the small intestines until 75 to 100 cm before they reach the large intestine. Thus, absorption of vitamin D, protein, calcium, and other nutrients is impaired.20,22
Since phosphorus and magnesium are also absorbed at the sites of the duodenum and jejunum, malabsorption of these nutrients may occur in a patient who has undergone a duodenal switch. Although vitamin B12 is absorbed at the site of the distal ileum, it also requires gastric acid to free it from the food. Zinc absorption, which normally occurs at the site of the jejunum, may be impaired after duodenal switch surgery, and calcium supplementation, though essential, may further reduce zinc absorption.9 Iron absorption requires HCl, facilitated by the presence of vitamin C. Use of H2-blockers and proton pump inhibitors may impair iron metabolism, resulting in anemia.20
In a randomized controlled trial, Aasheim et al23 compared the effects of Roux-en-Y gastric bypass with those of duodenal switch gastric bypass on patients’ vitamin metabolism. The researchers concluded that patients who undergo a duodenal switch are at greater risk for vitamin A and D deficiencies in the first year after surgery; and for thiamine deficiency in the months following surgery as a result of malabsorption, compared with patients who undergo Roux-en-Y gastric bypass.20,23
Patient Management
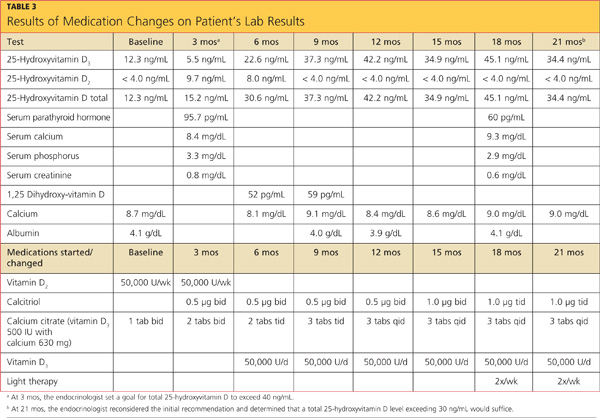
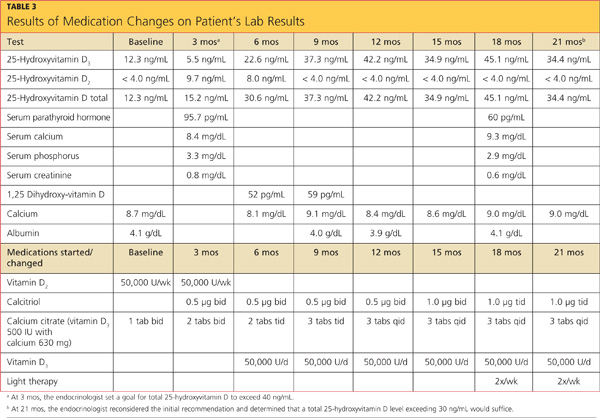
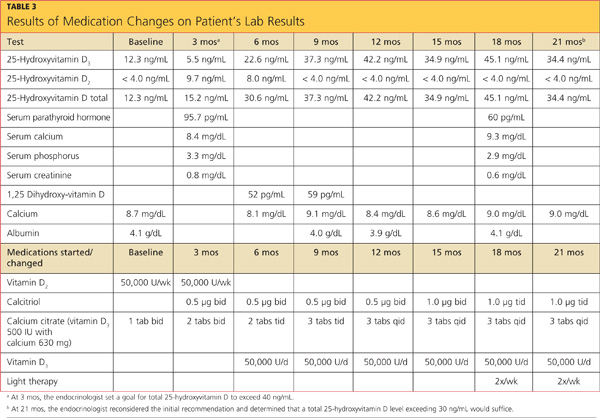
The case patient’s care necessitated consultations with endocrinology, dermatology, and gastroenterology (GI). Table 3 (below) shows the laboratory findings and the medication changes prompted by the patient’s physical exam and lab results. Table 4 lists the findings from other lab studies ordered throughout the patient’s course of treatment.
The endocrinologist was consulted at the first sign of osteopenia, and a workup was soon initiated, followed by treatment. GI was consulted six months after the beginning of treatment, when the patient began to complain of reflux while sleeping and frequent diarrhea throughout the day.
Results of esophagogastroduodenoscopy with biopsy ruled out celiac disease and mucosal ulceration, but a small hiatal hernia that was detected (< 3 cm) was determined to be an aggravating factor for the patient’s reflux. The patient was instructed in lifestyle modifications for hiatal hernia, including the need to remain upright one to two hours after eating before going to sleep to prevent aspiration. The patient was instructed to avoid taking iron and calcium within two hours of each other and to limit his alcohol intake. He was also educated in precautions against falls.
Dermatology was consulted nine months into treatment so that light therapy could be initiated, allowing the patient to take advantage of the body’s natural pathway to manufacture vitamin D3.
CONCLUSION
For post–bariatric surgery patients, primary care practitioners are in a position to coordinate care recommendations from multiple specialists, including those in nutrition, to determine the best course of action.
This case illustrates complications of bariatric surgery (malabsorption of key vitamins and minerals, wrist fracture, osteopenia, osteomalacia) that require diagnosis and treatment. The specialists and the primary care practitioner, along with the patient, had to weigh the risks and benefits of continued proton pump inhibitor use, as such medications can increase the risk for fracture. They also addressed the patient’s anemia and remained attentive to his preventive health care needs.
REFERENCES
1. Brusin JH. Update on bone densitometry. Radiol Technol. 2009;81(2):153BD-170BD.
2. Wilson CR. Essentials of bone densitometry for the medical physicist. Presented at: The American Association of Physicists in Medicine 2003 Annual Meeting; July 22-26, 2003; San Diego, CA.
3. Heber D, Greenway FL, Kaplan LM. et al. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(11):4825-4843.
4. Osteomalacia: step-by-step diagnostic approach (2011). http://bestpractice.bmj.com/best-practice/monograph/517/diagnosis/step-by-step.html. Accessed December 18, 2012.
5. Gifre L, Peris P, Monegal A, et al. Osteomalacia revisited : a report on 28 cases. Clin Rheumatol. 2011;30(5):639-645.
6. Bingham CT, Fitzpatrick LA. Noninvasive testing in the diagnosis of osteomalacia. Am J Med. 1993;95(5):519-523.
7. World Health Organization. Obesity and overweight (May 2012). Fact Sheet No 311. www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed December 18, 2012.
8. Tanner BD, Allen JW. Complications of bariatric surgery: implications for the covering physician. Am Surg. 2009;75(2):103-112.
9. Soleymani T, Tejavanija S, Morgan S. Obesity, bariatric surgery, and bone. Curr Opin Rheumatol. 2011;23(4):396-405.
10. Koch TR, Finelli FC. Postoperative metabolic and nutritional complications of bariatric surgery. Gastroenterol Clin North Am. 2010;39(1):109-124.
11. Manchester S, Roye GD. Bariatric surgery: an overview for dietetics professionals. Nutr Today. 2011;46(6):264-275.
12. Bal BS, Finelli FC, Shope TR, Koch TR. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8(9):544-546.
13. Iannelli A, Schneck AS, Dahman M, et al. Two-step laparoscopic duodenal switch for superobesity: a feasibility study. Surg Endosc. 2009;23(10):2385-2389.
14. Lalmohamed A, de Vries F, Bazelier MT, et al. Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ. 2012;345:e5085.
15. Holrick MF. Vitamin D: important for prevention of osteoporosis, cardiovascular heart disease, type 1 diabetes, autoimmune diseases, and some cancers. South Med J. 2005;98 (10):1024-1027.
16. Kalro BN. Vitamin D and the skeleton. Alt Ther Womens Health. 2009;2(4):25-32.
17. Crowther-Radulewicz CL, McCance KL. Alterations of musculoskeletal function. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1568-1617.
18. Huether SE. Structure and function of the renal and urologic systems. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1344-1364.
19. Bhan A, Rao AD, Rao DS. Osteomalacia as a result of vitamin D deficiency. Endocrinol Metab Clin North Am. 2010;39(2):321-331.
20. Decker GA, Swain JM, Crowell MD. Gastrointestinal and nutritional complications after bariatric surgery. Am J Gastroenterol. 2007;102(11):2571-2580.
21. Targownik LE, Lix LM, Metge C, et al. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008;179(4):319-326.
22. Ybarra J, Sánchez-Hernández J, Pérez A. Hypovitaminosis D and morbid obesity. Nurs Clin North Am. 2007;42(1):19-27.
23. Aasheim ET, Björkman S, Søvik TT, et al. Vitamin status after bariatric surgery: a randomized study of gastric bypass and duodenal switch. Am J Clin Nutr. 2009;90(1):15-22.
A white man, age 56, presented to his primary care clinician with wrist pain and swelling. Two days earlier, he had fallen from a step stool and landed on his right wrist. He treated the pain by resting, elevating his arm, applying ice, and taking ibuprofen 800 mg tid. He said he had lost strength in his hand and arm and was experiencing numbness and tingling in his right hand and fingers.
The patient’s medical history included hypertension, type 2 diabetes mellitus, morbid obesity, obstructive sleep apnea, asthma, carpel tunnel syndrome, and peripheral neuropathy. His surgical history was significant for duodenal switch gastric bypass surgery, performed eight years earlier, and his weight at the time of presentation was 200 lb; before his gastric bypass, he weighed 385 lb. Since the surgery, his hypertension, diabetes, asthma, and sleep apnea had all resolved. Table 1 shows a list of medications he was taking at the time of presentation.
The patient, a registered nurse, had been married for 30 years and had one child. He had quit smoking 15 years earlier, with a 43–pack-year smoking history. He reported social drinking but denied any recreational drug use. He was unaware of having any allergies to food or medication.
His vital signs on presentation were blood pressure, 110/75 mm Hg; heart rate, 53 beats/min; respiration, 18 breaths/min; O2 saturation, 97% on room air; and temperature, 97.5°F.
Physical exam revealed that the patient’s right wrist was ecchymotic and swollen with +1 pitting edema. The skin was warm and dry to the touch. Decreased range of motion was noted in the right wrist, compared with the left. Pain with point tenderness was noted at the right lateral wrist. Pulses were +3 with capillary refill of less than 3 seconds. The rest of the exam was unremarkable.
The differential diagnosis included fracture secondary to the fall, osteoporosis, osteopenia, osteomalacia, Paget’s disease, tumor, infection, and sprain or strain of the wrist. A wrist x-ray was ordered, as were the following baseline labs: complete blood count with differential (CBC), vitamin B12 and folate levels, blood chemistry, lipid profile, liver profile, total vitamin D, and sensitive thyroid-stimulating hormone. Test results are shown in Table 2.
X-ray of the wrist showed fracture only, making it possible to rule out Paget’s disease (ie, no patchy white areas noted in the bone) and tumor (no masses seen) as the immediate cause of fracture. Normal body temperature and normal white blood cell count eliminated the possibility of infection.
Because the patient was only 56 and had a history of bariatric surgery, further testing was pursued to investigate a cause for the weakened bone. Bone mineral density (BMD) testing revealed the following results:
• The lumbar spine in frontal projection measured 0.968 g/cm2 with a T-score of –2.2 and a Z-score of –2.2.
• Total BMD of the left hip was 0.863 g/cm2 with a T-score of –1.7 and a Z-score of –1.4.
• Total BMD of the left femoral neck was 0.863 g/cm2 with a T-score of 1.7 and a Z-score of –1.1.
These findings suggested osteopenia1,2 (not osteoporosis) in all sites, with a 12% decrease of BMD in the spine (suggesting increased risk for spinal fracture) and a 16.3% decrease of BMD in the hip since the patient’s most recent bone scan five years earlier (radiologist’s report). Other abnormal findings were elevated parathyroid hormone (PTH) serum, 95.7 pg/mL (reference range, 10 to 65 pg/mL); low total calcium serum, 8.7 mg/dL (reference range, 8.9 to 10.2 mg/dL), and low 25-hydroxyvitamin D total, 12.3 ng/mL (reference range, 25 to 80 ng/mL).
A 2010 clinical practice guideline from the Endocrine Society3 specifies that after malabsorptive surgery, vitamin D and calcium supplementation should be adjusted by a qualified medical professional, based on serum markers and measures of bone density. An endocrinologist who was consulted at the patient’s initial visit prescribed the following medications: vitamin D2, 50,000 U/wk PO; combined calcium citrate (vitamin D3) 500 IU with calcium 630 mg, 1 tab bid; and calcitriol 0.5 μg bid.
The patient’s final diagnosis was osteomalacia secondary to gastric bypass surgery. (See “Making the Diagnosis of Osteomalacia.”4-6)
DISCUSSION
According to 2008 data from the World Health Organization (WHO),7 1.4 billion persons older than 20 worldwide were overweight, and 200 million men and 300 million women were considered obese—meaning that one in every 10 adults worldwide is overweight or obese. In 2010, the WHO reports, 40 million children younger than 5 worldwide were considered overweight.7 Health care providers need to be prepared to care for the increasing number of patients who will undergo bariatric surgeries to treat obesity and its related comorbidities.8
Postoperative follow-up for the malabsorption deficiencies related to bariatric procedures should be performed every six months, including obtaining levels of alkaline phosphatase and others previously discussed. In addition, the Endocrine Society guideline3 recommends measuring levels of vitamin B12, albumin, pre-albumin, iron, and ferritin, and obtaining a CBC, a liver profile, glucose reading, creatinine measurement, and a metabolic profile at one month and two months after surgery, then every six months until two years after surgery, then annually if findings are stable.
Furthermore, the Endocrine Society3 recommends obtaining zinc levels every six months for the first year, then annually. An annual vitamin A level is optional.9 Yearly bone density testing is recommended until the patient’s BMD is deemed stable.3
Additionally, Koch and Finelli10 recommend performing the following labs postoperatively: hemoglobin A1C every three months; copper, magnesium, whole blood thiamine, vitamin B12, and a 24-hour urinary calcium every six months for the first three years, then once a year if findings remain stable.
Use of alcohol should be discouraged among patients who have undergone bariatric surgery, as its use alters micronutrient requirements and metabolism. Alcohol consumption may also contribute to dumping syndrome (ie, rapid gastric emptying).11
Any patient with a history of malabsorptive bypass surgery who complains of neurologic, visual, or skin disorders, anemia, or edema may require a further workup to rule out other absorptive deficiencies. These include vitamins A, E, and B12, zinc, folate, thiamine, niacin, selenium, and ferritin.10
Osteomalacia
Metabolic bone diseases can result from genetics, dietary factors, medication use, surgery, or hormonal irregularities. They alter the normal biochemical reactions in bone structure.
The three most common forms of metabolic bone disease are osteoporosis, osteopenia, and osteomalacia. The WHO diagnostic classifications and associated T-scores for bone mineral density1,2 indicate a T-score above –1.0 as normal. A score between –1.0 and –2.5 is indicative of osteopenia, and a score below –2.5 indicates osteoporosis. A T-score below –2.5 in the patient with a history of fragility fracture indicates severe osteoporosis.1,2
In osteomalacia, bone volume remains unchanged, but mineralization of osteoid in the mature compact and spongy bone is either delayed or inadequate. The remolding cycle continues unchanged in the formation of osteoid, but mineral calcification and deposition do not occur.3-5
Osteomalacia is normally considered a rare disorder, but it may become more common as increasing numbers of patients undergo gastric bypass operations.12,13 Primary care practitioners should monitor for this condition in such patients before serious bone loss or other problems develop.9,13,14
Vitamin D deficiency (see “Vitamin D Metabolism,”4,15-19 below), whether or not the result of gastric bypass surgery, is a major risk factor for osteomalacia. Disorders of the small bowel, the hepatobiliary system, and the pancreas are all common causes of vitamin D deficiency. Liver disease interferes with the metabolism of vitamin D. Diseases of the pancreas may cause a deficiency of bile salts, which are vital for the intestinal absorption of vitamin D.17

Restriction and Malabsorption
The case patient had undergone a gastric bypass (duodenal switch), in which a large portion of the stomach is removed and a large part of the small bowel rerouted—with both parts of the procedure causing malabsorption.11 It is in the small bowel that absorption of vitamin D and calcium takes place.
The duodenal switch gastric bypass surgery causes both restriction and malabsorption. Though similar to a biliopancreatic diversion, the duodenal switch preserves the distal stomach and the pylorus20 by way of a sleeve gastrectomy that is performed to reduce the gastric reservoir; the common channel length after revision is 100 cm, not 50 cm (as in conventional biliopancreatic diversion).13 The sleeve gastrectomy involves removal of parietal cells, reducing production of hydrochloric acid (which is necessary to break down food), and hindering the absorption of certain nutrients, including the fat-soluble vitamins, vitamin B12, and iron.12 Patients who take H2-blockers or proton pump inhibitors experience an additional decrease in the production and availability of HCl and may have an increased risk for fracture.14,20,21
In addition to its biliopancreatic diversion component, the duodenal switch diverts a large portion of the small bowel, with food restricted from moving through it. Vitamin D and protein are normally absorbed at the jejunum and ileum, but only when bile salts are present; after a duodenal switch, bile and pancreatic enzymes are not introduced into the small intestines until 75 to 100 cm before they reach the large intestine. Thus, absorption of vitamin D, protein, calcium, and other nutrients is impaired.20,22
Since phosphorus and magnesium are also absorbed at the sites of the duodenum and jejunum, malabsorption of these nutrients may occur in a patient who has undergone a duodenal switch. Although vitamin B12 is absorbed at the site of the distal ileum, it also requires gastric acid to free it from the food. Zinc absorption, which normally occurs at the site of the jejunum, may be impaired after duodenal switch surgery, and calcium supplementation, though essential, may further reduce zinc absorption.9 Iron absorption requires HCl, facilitated by the presence of vitamin C. Use of H2-blockers and proton pump inhibitors may impair iron metabolism, resulting in anemia.20
In a randomized controlled trial, Aasheim et al23 compared the effects of Roux-en-Y gastric bypass with those of duodenal switch gastric bypass on patients’ vitamin metabolism. The researchers concluded that patients who undergo a duodenal switch are at greater risk for vitamin A and D deficiencies in the first year after surgery; and for thiamine deficiency in the months following surgery as a result of malabsorption, compared with patients who undergo Roux-en-Y gastric bypass.20,23
Patient Management
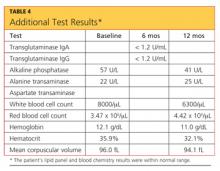
The case patient’s care necessitated consultations with endocrinology, dermatology, and gastroenterology (GI). Table 3 (below) shows the laboratory findings and the medication changes prompted by the patient’s physical exam and lab results. Table 4 lists the findings from other lab studies ordered throughout the patient’s course of treatment.
The endocrinologist was consulted at the first sign of osteopenia, and a workup was soon initiated, followed by treatment. GI was consulted six months after the beginning of treatment, when the patient began to complain of reflux while sleeping and frequent diarrhea throughout the day.
Results of esophagogastroduodenoscopy with biopsy ruled out celiac disease and mucosal ulceration, but a small hiatal hernia that was detected (< 3 cm) was determined to be an aggravating factor for the patient’s reflux. The patient was instructed in lifestyle modifications for hiatal hernia, including the need to remain upright one to two hours after eating before going to sleep to prevent aspiration. The patient was instructed to avoid taking iron and calcium within two hours of each other and to limit his alcohol intake. He was also educated in precautions against falls.
Dermatology was consulted nine months into treatment so that light therapy could be initiated, allowing the patient to take advantage of the body’s natural pathway to manufacture vitamin D3.
CONCLUSION
For post–bariatric surgery patients, primary care practitioners are in a position to coordinate care recommendations from multiple specialists, including those in nutrition, to determine the best course of action.
This case illustrates complications of bariatric surgery (malabsorption of key vitamins and minerals, wrist fracture, osteopenia, osteomalacia) that require diagnosis and treatment. The specialists and the primary care practitioner, along with the patient, had to weigh the risks and benefits of continued proton pump inhibitor use, as such medications can increase the risk for fracture. They also addressed the patient’s anemia and remained attentive to his preventive health care needs.
REFERENCES
1. Brusin JH. Update on bone densitometry. Radiol Technol. 2009;81(2):153BD-170BD.
2. Wilson CR. Essentials of bone densitometry for the medical physicist. Presented at: The American Association of Physicists in Medicine 2003 Annual Meeting; July 22-26, 2003; San Diego, CA.
3. Heber D, Greenway FL, Kaplan LM. et al. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(11):4825-4843.
4. Osteomalacia: step-by-step diagnostic approach (2011). http://bestpractice.bmj.com/best-practice/monograph/517/diagnosis/step-by-step.html. Accessed December 18, 2012.
5. Gifre L, Peris P, Monegal A, et al. Osteomalacia revisited : a report on 28 cases. Clin Rheumatol. 2011;30(5):639-645.
6. Bingham CT, Fitzpatrick LA. Noninvasive testing in the diagnosis of osteomalacia. Am J Med. 1993;95(5):519-523.
7. World Health Organization. Obesity and overweight (May 2012). Fact Sheet No 311. www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed December 18, 2012.
8. Tanner BD, Allen JW. Complications of bariatric surgery: implications for the covering physician. Am Surg. 2009;75(2):103-112.
9. Soleymani T, Tejavanija S, Morgan S. Obesity, bariatric surgery, and bone. Curr Opin Rheumatol. 2011;23(4):396-405.
10. Koch TR, Finelli FC. Postoperative metabolic and nutritional complications of bariatric surgery. Gastroenterol Clin North Am. 2010;39(1):109-124.
11. Manchester S, Roye GD. Bariatric surgery: an overview for dietetics professionals. Nutr Today. 2011;46(6):264-275.
12. Bal BS, Finelli FC, Shope TR, Koch TR. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8(9):544-546.
13. Iannelli A, Schneck AS, Dahman M, et al. Two-step laparoscopic duodenal switch for superobesity: a feasibility study. Surg Endosc. 2009;23(10):2385-2389.
14. Lalmohamed A, de Vries F, Bazelier MT, et al. Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ. 2012;345:e5085.
15. Holrick MF. Vitamin D: important for prevention of osteoporosis, cardiovascular heart disease, type 1 diabetes, autoimmune diseases, and some cancers. South Med J. 2005;98 (10):1024-1027.
16. Kalro BN. Vitamin D and the skeleton. Alt Ther Womens Health. 2009;2(4):25-32.
17. Crowther-Radulewicz CL, McCance KL. Alterations of musculoskeletal function. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1568-1617.
18. Huether SE. Structure and function of the renal and urologic systems. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1344-1364.
19. Bhan A, Rao AD, Rao DS. Osteomalacia as a result of vitamin D deficiency. Endocrinol Metab Clin North Am. 2010;39(2):321-331.
20. Decker GA, Swain JM, Crowell MD. Gastrointestinal and nutritional complications after bariatric surgery. Am J Gastroenterol. 2007;102(11):2571-2580.
21. Targownik LE, Lix LM, Metge C, et al. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008;179(4):319-326.
22. Ybarra J, Sánchez-Hernández J, Pérez A. Hypovitaminosis D and morbid obesity. Nurs Clin North Am. 2007;42(1):19-27.
23. Aasheim ET, Björkman S, Søvik TT, et al. Vitamin status after bariatric surgery: a randomized study of gastric bypass and duodenal switch. Am J Clin Nutr. 2009;90(1):15-22.
A white man, age 56, presented to his primary care clinician with wrist pain and swelling. Two days earlier, he had fallen from a step stool and landed on his right wrist. He treated the pain by resting, elevating his arm, applying ice, and taking ibuprofen 800 mg tid. He said he had lost strength in his hand and arm and was experiencing numbness and tingling in his right hand and fingers.
The patient’s medical history included hypertension, type 2 diabetes mellitus, morbid obesity, obstructive sleep apnea, asthma, carpel tunnel syndrome, and peripheral neuropathy. His surgical history was significant for duodenal switch gastric bypass surgery, performed eight years earlier, and his weight at the time of presentation was 200 lb; before his gastric bypass, he weighed 385 lb. Since the surgery, his hypertension, diabetes, asthma, and sleep apnea had all resolved. Table 1 shows a list of medications he was taking at the time of presentation.
The patient, a registered nurse, had been married for 30 years and had one child. He had quit smoking 15 years earlier, with a 43–pack-year smoking history. He reported social drinking but denied any recreational drug use. He was unaware of having any allergies to food or medication.
His vital signs on presentation were blood pressure, 110/75 mm Hg; heart rate, 53 beats/min; respiration, 18 breaths/min; O2 saturation, 97% on room air; and temperature, 97.5°F.
Physical exam revealed that the patient’s right wrist was ecchymotic and swollen with +1 pitting edema. The skin was warm and dry to the touch. Decreased range of motion was noted in the right wrist, compared with the left. Pain with point tenderness was noted at the right lateral wrist. Pulses were +3 with capillary refill of less than 3 seconds. The rest of the exam was unremarkable.
The differential diagnosis included fracture secondary to the fall, osteoporosis, osteopenia, osteomalacia, Paget’s disease, tumor, infection, and sprain or strain of the wrist. A wrist x-ray was ordered, as were the following baseline labs: complete blood count with differential (CBC), vitamin B12 and folate levels, blood chemistry, lipid profile, liver profile, total vitamin D, and sensitive thyroid-stimulating hormone. Test results are shown in Table 2.
X-ray of the wrist showed fracture only, making it possible to rule out Paget’s disease (ie, no patchy white areas noted in the bone) and tumor (no masses seen) as the immediate cause of fracture. Normal body temperature and normal white blood cell count eliminated the possibility of infection.
Because the patient was only 56 and had a history of bariatric surgery, further testing was pursued to investigate a cause for the weakened bone. Bone mineral density (BMD) testing revealed the following results:
• The lumbar spine in frontal projection measured 0.968 g/cm2 with a T-score of –2.2 and a Z-score of –2.2.
• Total BMD of the left hip was 0.863 g/cm2 with a T-score of –1.7 and a Z-score of –1.4.
• Total BMD of the left femoral neck was 0.863 g/cm2 with a T-score of 1.7 and a Z-score of –1.1.
These findings suggested osteopenia1,2 (not osteoporosis) in all sites, with a 12% decrease of BMD in the spine (suggesting increased risk for spinal fracture) and a 16.3% decrease of BMD in the hip since the patient’s most recent bone scan five years earlier (radiologist’s report). Other abnormal findings were elevated parathyroid hormone (PTH) serum, 95.7 pg/mL (reference range, 10 to 65 pg/mL); low total calcium serum, 8.7 mg/dL (reference range, 8.9 to 10.2 mg/dL), and low 25-hydroxyvitamin D total, 12.3 ng/mL (reference range, 25 to 80 ng/mL).
A 2010 clinical practice guideline from the Endocrine Society3 specifies that after malabsorptive surgery, vitamin D and calcium supplementation should be adjusted by a qualified medical professional, based on serum markers and measures of bone density. An endocrinologist who was consulted at the patient’s initial visit prescribed the following medications: vitamin D2, 50,000 U/wk PO; combined calcium citrate (vitamin D3) 500 IU with calcium 630 mg, 1 tab bid; and calcitriol 0.5 μg bid.
The patient’s final diagnosis was osteomalacia secondary to gastric bypass surgery. (See “Making the Diagnosis of Osteomalacia.”4-6)
DISCUSSION
According to 2008 data from the World Health Organization (WHO),7 1.4 billion persons older than 20 worldwide were overweight, and 200 million men and 300 million women were considered obese—meaning that one in every 10 adults worldwide is overweight or obese. In 2010, the WHO reports, 40 million children younger than 5 worldwide were considered overweight.7 Health care providers need to be prepared to care for the increasing number of patients who will undergo bariatric surgeries to treat obesity and its related comorbidities.8
Postoperative follow-up for the malabsorption deficiencies related to bariatric procedures should be performed every six months, including obtaining levels of alkaline phosphatase and others previously discussed. In addition, the Endocrine Society guideline3 recommends measuring levels of vitamin B12, albumin, pre-albumin, iron, and ferritin, and obtaining a CBC, a liver profile, glucose reading, creatinine measurement, and a metabolic profile at one month and two months after surgery, then every six months until two years after surgery, then annually if findings are stable.
Furthermore, the Endocrine Society3 recommends obtaining zinc levels every six months for the first year, then annually. An annual vitamin A level is optional.9 Yearly bone density testing is recommended until the patient’s BMD is deemed stable.3
Additionally, Koch and Finelli10 recommend performing the following labs postoperatively: hemoglobin A1C every three months; copper, magnesium, whole blood thiamine, vitamin B12, and a 24-hour urinary calcium every six months for the first three years, then once a year if findings remain stable.
Use of alcohol should be discouraged among patients who have undergone bariatric surgery, as its use alters micronutrient requirements and metabolism. Alcohol consumption may also contribute to dumping syndrome (ie, rapid gastric emptying).11
Any patient with a history of malabsorptive bypass surgery who complains of neurologic, visual, or skin disorders, anemia, or edema may require a further workup to rule out other absorptive deficiencies. These include vitamins A, E, and B12, zinc, folate, thiamine, niacin, selenium, and ferritin.10
Osteomalacia
Metabolic bone diseases can result from genetics, dietary factors, medication use, surgery, or hormonal irregularities. They alter the normal biochemical reactions in bone structure.
The three most common forms of metabolic bone disease are osteoporosis, osteopenia, and osteomalacia. The WHO diagnostic classifications and associated T-scores for bone mineral density1,2 indicate a T-score above –1.0 as normal. A score between –1.0 and –2.5 is indicative of osteopenia, and a score below –2.5 indicates osteoporosis. A T-score below –2.5 in the patient with a history of fragility fracture indicates severe osteoporosis.1,2
In osteomalacia, bone volume remains unchanged, but mineralization of osteoid in the mature compact and spongy bone is either delayed or inadequate. The remolding cycle continues unchanged in the formation of osteoid, but mineral calcification and deposition do not occur.3-5
Osteomalacia is normally considered a rare disorder, but it may become more common as increasing numbers of patients undergo gastric bypass operations.12,13 Primary care practitioners should monitor for this condition in such patients before serious bone loss or other problems develop.9,13,14
Vitamin D deficiency (see “Vitamin D Metabolism,”4,15-19 below), whether or not the result of gastric bypass surgery, is a major risk factor for osteomalacia. Disorders of the small bowel, the hepatobiliary system, and the pancreas are all common causes of vitamin D deficiency. Liver disease interferes with the metabolism of vitamin D. Diseases of the pancreas may cause a deficiency of bile salts, which are vital for the intestinal absorption of vitamin D.17

Restriction and Malabsorption
The case patient had undergone a gastric bypass (duodenal switch), in which a large portion of the stomach is removed and a large part of the small bowel rerouted—with both parts of the procedure causing malabsorption.11 It is in the small bowel that absorption of vitamin D and calcium takes place.
The duodenal switch gastric bypass surgery causes both restriction and malabsorption. Though similar to a biliopancreatic diversion, the duodenal switch preserves the distal stomach and the pylorus20 by way of a sleeve gastrectomy that is performed to reduce the gastric reservoir; the common channel length after revision is 100 cm, not 50 cm (as in conventional biliopancreatic diversion).13 The sleeve gastrectomy involves removal of parietal cells, reducing production of hydrochloric acid (which is necessary to break down food), and hindering the absorption of certain nutrients, including the fat-soluble vitamins, vitamin B12, and iron.12 Patients who take H2-blockers or proton pump inhibitors experience an additional decrease in the production and availability of HCl and may have an increased risk for fracture.14,20,21
In addition to its biliopancreatic diversion component, the duodenal switch diverts a large portion of the small bowel, with food restricted from moving through it. Vitamin D and protein are normally absorbed at the jejunum and ileum, but only when bile salts are present; after a duodenal switch, bile and pancreatic enzymes are not introduced into the small intestines until 75 to 100 cm before they reach the large intestine. Thus, absorption of vitamin D, protein, calcium, and other nutrients is impaired.20,22
Since phosphorus and magnesium are also absorbed at the sites of the duodenum and jejunum, malabsorption of these nutrients may occur in a patient who has undergone a duodenal switch. Although vitamin B12 is absorbed at the site of the distal ileum, it also requires gastric acid to free it from the food. Zinc absorption, which normally occurs at the site of the jejunum, may be impaired after duodenal switch surgery, and calcium supplementation, though essential, may further reduce zinc absorption.9 Iron absorption requires HCl, facilitated by the presence of vitamin C. Use of H2-blockers and proton pump inhibitors may impair iron metabolism, resulting in anemia.20
In a randomized controlled trial, Aasheim et al23 compared the effects of Roux-en-Y gastric bypass with those of duodenal switch gastric bypass on patients’ vitamin metabolism. The researchers concluded that patients who undergo a duodenal switch are at greater risk for vitamin A and D deficiencies in the first year after surgery; and for thiamine deficiency in the months following surgery as a result of malabsorption, compared with patients who undergo Roux-en-Y gastric bypass.20,23
Patient Management
The case patient’s care necessitated consultations with endocrinology, dermatology, and gastroenterology (GI). Table 3 (below) shows the laboratory findings and the medication changes prompted by the patient’s physical exam and lab results. Table 4 lists the findings from other lab studies ordered throughout the patient’s course of treatment.
The endocrinologist was consulted at the first sign of osteopenia, and a workup was soon initiated, followed by treatment. GI was consulted six months after the beginning of treatment, when the patient began to complain of reflux while sleeping and frequent diarrhea throughout the day.
Results of esophagogastroduodenoscopy with biopsy ruled out celiac disease and mucosal ulceration, but a small hiatal hernia that was detected (< 3 cm) was determined to be an aggravating factor for the patient’s reflux. The patient was instructed in lifestyle modifications for hiatal hernia, including the need to remain upright one to two hours after eating before going to sleep to prevent aspiration. The patient was instructed to avoid taking iron and calcium within two hours of each other and to limit his alcohol intake. He was also educated in precautions against falls.
Dermatology was consulted nine months into treatment so that light therapy could be initiated, allowing the patient to take advantage of the body’s natural pathway to manufacture vitamin D3.
CONCLUSION
For post–bariatric surgery patients, primary care practitioners are in a position to coordinate care recommendations from multiple specialists, including those in nutrition, to determine the best course of action.
This case illustrates complications of bariatric surgery (malabsorption of key vitamins and minerals, wrist fracture, osteopenia, osteomalacia) that require diagnosis and treatment. The specialists and the primary care practitioner, along with the patient, had to weigh the risks and benefits of continued proton pump inhibitor use, as such medications can increase the risk for fracture. They also addressed the patient’s anemia and remained attentive to his preventive health care needs.
REFERENCES
1. Brusin JH. Update on bone densitometry. Radiol Technol. 2009;81(2):153BD-170BD.
2. Wilson CR. Essentials of bone densitometry for the medical physicist. Presented at: The American Association of Physicists in Medicine 2003 Annual Meeting; July 22-26, 2003; San Diego, CA.
3. Heber D, Greenway FL, Kaplan LM. et al. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(11):4825-4843.
4. Osteomalacia: step-by-step diagnostic approach (2011). http://bestpractice.bmj.com/best-practice/monograph/517/diagnosis/step-by-step.html. Accessed December 18, 2012.
5. Gifre L, Peris P, Monegal A, et al. Osteomalacia revisited : a report on 28 cases. Clin Rheumatol. 2011;30(5):639-645.
6. Bingham CT, Fitzpatrick LA. Noninvasive testing in the diagnosis of osteomalacia. Am J Med. 1993;95(5):519-523.
7. World Health Organization. Obesity and overweight (May 2012). Fact Sheet No 311. www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed December 18, 2012.
8. Tanner BD, Allen JW. Complications of bariatric surgery: implications for the covering physician. Am Surg. 2009;75(2):103-112.
9. Soleymani T, Tejavanija S, Morgan S. Obesity, bariatric surgery, and bone. Curr Opin Rheumatol. 2011;23(4):396-405.
10. Koch TR, Finelli FC. Postoperative metabolic and nutritional complications of bariatric surgery. Gastroenterol Clin North Am. 2010;39(1):109-124.
11. Manchester S, Roye GD. Bariatric surgery: an overview for dietetics professionals. Nutr Today. 2011;46(6):264-275.
12. Bal BS, Finelli FC, Shope TR, Koch TR. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8(9):544-546.
13. Iannelli A, Schneck AS, Dahman M, et al. Two-step laparoscopic duodenal switch for superobesity: a feasibility study. Surg Endosc. 2009;23(10):2385-2389.
14. Lalmohamed A, de Vries F, Bazelier MT, et al. Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ. 2012;345:e5085.
15. Holrick MF. Vitamin D: important for prevention of osteoporosis, cardiovascular heart disease, type 1 diabetes, autoimmune diseases, and some cancers. South Med J. 2005;98 (10):1024-1027.
16. Kalro BN. Vitamin D and the skeleton. Alt Ther Womens Health. 2009;2(4):25-32.
17. Crowther-Radulewicz CL, McCance KL. Alterations of musculoskeletal function. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1568-1617.
18. Huether SE. Structure and function of the renal and urologic systems. In: McCance KL, Huether SE, Brashers VL, Rote NS, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 6th ed. Maryland Heights, MO: Mosby Elsevier; 2010:1344-1364.
19. Bhan A, Rao AD, Rao DS. Osteomalacia as a result of vitamin D deficiency. Endocrinol Metab Clin North Am. 2010;39(2):321-331.
20. Decker GA, Swain JM, Crowell MD. Gastrointestinal and nutritional complications after bariatric surgery. Am J Gastroenterol. 2007;102(11):2571-2580.
21. Targownik LE, Lix LM, Metge C, et al. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008;179(4):319-326.
22. Ybarra J, Sánchez-Hernández J, Pérez A. Hypovitaminosis D and morbid obesity. Nurs Clin North Am. 2007;42(1):19-27.
23. Aasheim ET, Björkman S, Søvik TT, et al. Vitamin status after bariatric surgery: a randomized study of gastric bypass and duodenal switch. Am J Clin Nutr. 2009;90(1):15-22.
Underlying Factors Influence Insulin's Effect
Q: Help! How do you proceed if, after you’ve continually increased a patient’s insulin dose, his/her blood glucose levels do not improve?
This is a common scenario in diabetes management. Here are nine things to consider when a patient’s situation just doesn’t make sense clinically:
1. Noncompliance with the prescribed dose. This is the most common scenario. Ask the patient, “How many injections do you miss in a typical week?” Assure that he or she is actually taking the currently prescribed amount of insulin before you further increase the dose.
2. Inaccurate insulin dosing. This problem can be due to impaired vision, poor technique, dexterity issues, or dementia. Ask the patient to demonstrate for you how he/she draws up and takes the insulin at home. You might just be surprised at what you see, even in patients who have been giving themselves insulin for years. Consider prescribing an insulin pen or having a family member or significant other dose the insulin if the patient is no longer reliable to accurately dose it for him- or herself.
3. “Bad insulin.” What this actually means is loss of potency. This can be caused by improper storage, exposure to heat or cold, or use of an insulin delivery device (ie, vial or pen) past the 28- to 45-day period recommended, depending on the type of insulin. Replace the vial or pen and re-assess for improvement in diabetes control.
4. Lipohypertrophy of injection sites due to overuse. Palpate and visually inspect injection sites to look for firm or hypertrophied tissue. Advise the patient to avoid these areas for future injection, as absorption from these sites can be poor and unpredictable.
5. Dietary issues. The patient may be increasing his/her food intake along with the increased insulin doses. One clue that should raise suspicion for this occurrence is rapidly increasing body weight. Consider referring the patient to a dietitian for nutrition counseling.
6. New medication. Sometimes a new treatment is added to a patient’s regimen by another provider, and the medication might have an adverse effect on blood glucose control. Common examples include steroids (typically a cortisone injection) or methylprednisolone dose-packs taken during an asthma flare.
7. Occult infection. Urinary tract infections, pneumonia, and the like can impact blood glucose control. Consider ordering a urinalysis and complete blood count if infection seems a likely cause.
8. Major life stressors. Inquire as to what is happening in the patient’s life that might impact his/her body’s response to insulin. They might be in the middle of a divorce or other family crisis or experiencing severe stress at work.
9. Technique and equipment issues. Inaccurate glucose monitoring technique or use of expired strips can lead to “false high” readings. Also, patients with a continuous glucose monitor may record false high results when they are taking acetaminophen. If this is the case, increasing the insulin dose will often result in hypoglycemia.
It may be helpful to keep this clinical checklist handy and add to it any other issues that you come across when the clinical picture doesn’t make sense. You may also want to consider referral to a diabetes educator; patients will often confide what is really going on to an educator in a longer visit, rather than in the typically shorter visits with their health care provider.
SUGGESTED READING
Sadler C, Einhorn D. Tailoring insulin regimens for type 2 diabetes mellitus. JAAPA. 1998;11(4):55-71.
Q: Help! How do you proceed if, after you’ve continually increased a patient’s insulin dose, his/her blood glucose levels do not improve?
This is a common scenario in diabetes management. Here are nine things to consider when a patient’s situation just doesn’t make sense clinically:
1. Noncompliance with the prescribed dose. This is the most common scenario. Ask the patient, “How many injections do you miss in a typical week?” Assure that he or she is actually taking the currently prescribed amount of insulin before you further increase the dose.
2. Inaccurate insulin dosing. This problem can be due to impaired vision, poor technique, dexterity issues, or dementia. Ask the patient to demonstrate for you how he/she draws up and takes the insulin at home. You might just be surprised at what you see, even in patients who have been giving themselves insulin for years. Consider prescribing an insulin pen or having a family member or significant other dose the insulin if the patient is no longer reliable to accurately dose it for him- or herself.
3. “Bad insulin.” What this actually means is loss of potency. This can be caused by improper storage, exposure to heat or cold, or use of an insulin delivery device (ie, vial or pen) past the 28- to 45-day period recommended, depending on the type of insulin. Replace the vial or pen and re-assess for improvement in diabetes control.
4. Lipohypertrophy of injection sites due to overuse. Palpate and visually inspect injection sites to look for firm or hypertrophied tissue. Advise the patient to avoid these areas for future injection, as absorption from these sites can be poor and unpredictable.
5. Dietary issues. The patient may be increasing his/her food intake along with the increased insulin doses. One clue that should raise suspicion for this occurrence is rapidly increasing body weight. Consider referring the patient to a dietitian for nutrition counseling.
6. New medication. Sometimes a new treatment is added to a patient’s regimen by another provider, and the medication might have an adverse effect on blood glucose control. Common examples include steroids (typically a cortisone injection) or methylprednisolone dose-packs taken during an asthma flare.
7. Occult infection. Urinary tract infections, pneumonia, and the like can impact blood glucose control. Consider ordering a urinalysis and complete blood count if infection seems a likely cause.
8. Major life stressors. Inquire as to what is happening in the patient’s life that might impact his/her body’s response to insulin. They might be in the middle of a divorce or other family crisis or experiencing severe stress at work.
9. Technique and equipment issues. Inaccurate glucose monitoring technique or use of expired strips can lead to “false high” readings. Also, patients with a continuous glucose monitor may record false high results when they are taking acetaminophen. If this is the case, increasing the insulin dose will often result in hypoglycemia.
It may be helpful to keep this clinical checklist handy and add to it any other issues that you come across when the clinical picture doesn’t make sense. You may also want to consider referral to a diabetes educator; patients will often confide what is really going on to an educator in a longer visit, rather than in the typically shorter visits with their health care provider.
SUGGESTED READING
Sadler C, Einhorn D. Tailoring insulin regimens for type 2 diabetes mellitus. JAAPA. 1998;11(4):55-71.
Q: Help! How do you proceed if, after you’ve continually increased a patient’s insulin dose, his/her blood glucose levels do not improve?
This is a common scenario in diabetes management. Here are nine things to consider when a patient’s situation just doesn’t make sense clinically:
1. Noncompliance with the prescribed dose. This is the most common scenario. Ask the patient, “How many injections do you miss in a typical week?” Assure that he or she is actually taking the currently prescribed amount of insulin before you further increase the dose.
2. Inaccurate insulin dosing. This problem can be due to impaired vision, poor technique, dexterity issues, or dementia. Ask the patient to demonstrate for you how he/she draws up and takes the insulin at home. You might just be surprised at what you see, even in patients who have been giving themselves insulin for years. Consider prescribing an insulin pen or having a family member or significant other dose the insulin if the patient is no longer reliable to accurately dose it for him- or herself.
3. “Bad insulin.” What this actually means is loss of potency. This can be caused by improper storage, exposure to heat or cold, or use of an insulin delivery device (ie, vial or pen) past the 28- to 45-day period recommended, depending on the type of insulin. Replace the vial or pen and re-assess for improvement in diabetes control.
4. Lipohypertrophy of injection sites due to overuse. Palpate and visually inspect injection sites to look for firm or hypertrophied tissue. Advise the patient to avoid these areas for future injection, as absorption from these sites can be poor and unpredictable.
5. Dietary issues. The patient may be increasing his/her food intake along with the increased insulin doses. One clue that should raise suspicion for this occurrence is rapidly increasing body weight. Consider referring the patient to a dietitian for nutrition counseling.
6. New medication. Sometimes a new treatment is added to a patient’s regimen by another provider, and the medication might have an adverse effect on blood glucose control. Common examples include steroids (typically a cortisone injection) or methylprednisolone dose-packs taken during an asthma flare.
7. Occult infection. Urinary tract infections, pneumonia, and the like can impact blood glucose control. Consider ordering a urinalysis and complete blood count if infection seems a likely cause.
8. Major life stressors. Inquire as to what is happening in the patient’s life that might impact his/her body’s response to insulin. They might be in the middle of a divorce or other family crisis or experiencing severe stress at work.
9. Technique and equipment issues. Inaccurate glucose monitoring technique or use of expired strips can lead to “false high” readings. Also, patients with a continuous glucose monitor may record false high results when they are taking acetaminophen. If this is the case, increasing the insulin dose will often result in hypoglycemia.
It may be helpful to keep this clinical checklist handy and add to it any other issues that you come across when the clinical picture doesn’t make sense. You may also want to consider referral to a diabetes educator; patients will often confide what is really going on to an educator in a longer visit, rather than in the typically shorter visits with their health care provider.
SUGGESTED READING
Sadler C, Einhorn D. Tailoring insulin regimens for type 2 diabetes mellitus. JAAPA. 1998;11(4):55-71.
New-Generation Radiofrequency Technology
Angiotensin-Converting Enzyme Inhibitor-Induced Angioedema
Cutis Tricolor
Circumscribed Acral Hypokeratosis
Paranoid, agitated, and manipulative
CASE: Agitation
Mrs. M, age 39, presents to the emergency department (ED) with altered mental status. She is escorted by her husband and the police. She has a history of severe alcohol dependence, bipolar disorder (BD), anxiety, borderline personality disorder (BPD), hypothyroidism, and bulimia, and had gastric bypass surgery 4 years ago. Her husband called 911 when he could no longer manage Mrs. M’s agitated state. The police found her to be extremely paranoid, restless, and disoriented. Her husband reports that she shouted “the world is going to end” before she escaped naked into her neighborhood streets.
On several occasions Mrs. M had been admitted to the same hospital for alcohol withdrawal and dependence with subsequent liver failure, leading to jaundice, coagulopathy, and ascites. During these hospitalizations, she exhibited poor behavioral tendencies, unhealthy psychological defenses, and chronic maladaptive coping and defense mechanisms congruent with her BPD diagnosis. Specifically, she engaged in splitting of hospital staff, ranging from extreme flattery to overt devaluation and hostility. Other defense mechanisms included denial, distortion, acting out, and passive-aggressive behavior. During these admissions, Mrs. M often displayed deficits in recall and attention on Mini-Mental State Examination (MMSE), but these deficits were associated with concurrent alcohol use and improved rapidly during her stay.
In her current presentation, Mrs. M’s mental status change is more pronounced and atypical compared with earlier admissions. Her outpatient medication regimen includes lamotrigine, 100 mg/d, levothyroxine, 88 mcg/d, venlafaxine extended release (XR), 75 mg/d, clonazepam, 3 mg/d, docusate as needed for constipation, and a daily multivitamin.
The authors’ observations
Delirium is a disturbance of consciousness manifested by a reduced clarity of awareness (impairment in attention) and change in cognition (impairment in orientation, memory, and language).1,2 The disturbance develops over a short time and tends to fluctuate during the day. Delirium is a direct physiological consequence of a general medical condition, substance use (intoxication or withdrawal), or both (Table).3
Delirium generally is a reversible mental disorder but can progress to irreversible brain damage. Prompt and accurate diagnosis of delirium is essential,4 although the condition often is underdiagnosed or misdiagnosed because of lack of recognition.
Table
DSM-IV-TR diagnostic criteria for delirium
|
| Source: Reference 3 |
Patients who have convoluted histories, such as Mrs. M, are common and difficult to manage and treat. These patients become substantially more complex when they are admitted to inpatient medical or surgical services. The need to clarify between delirium (primarily medical) and depression (primarily psychiatric) becomes paramount when administering treatment and evaluating decision-making capacity.5 In Mrs. M’s case, internal medicine, neurology, and psychiatry teams each had a different approach to altered mental status. Each team’s different terminology, assessment, and objectives further complicated an already challenging case.6
EVALUATION: Confounding results
The ED physicians offer a working diagnosis of acute mental status change, administer IV lorazepam, 4 mg, and order restraints for Mrs. M’s severe agitation. Her initial vital signs reveal slightly elevated blood pressure (140/90 mm Hg) and tachycardia (115 beats per minute). Internal medicine clinicians note that Mrs. M is not in acute distress, although she refuses to speak and has a small amount of dried blood on her lips, presumably from a struggle with the police before coming to the hospital, but this is not certain. Her abdomen is not tender; she has normal bowel sounds, and no asterixis is noted on neurologic exam. Physical exam is otherwise normal. A noncontrast head CT scan shows no acute process. Initial lab values show elevations in ammonia (277 μg/dL) and γ-glutamyl transpeptidase (68 U/L). Thyroid-stimulating hormone is 1.45 mlU/L, prothrombin time is 19.5 s, partial thromboplastin time is 40.3 s, and international normalized ratio is 1.67. The internal medicine team admits Mrs. M to the intensive care unit (ICU) for further management of her mental status change with alcohol withdrawal or hepatic encephalopathy as the most likely etiologies.
Mrs. M’s husband says that his wife has not consumed alcohol in the last 4 months in preparation for a possible liver transplant; however, past interactions with Mrs. M’s family suggest they are unreliable. The Clinical Institute Withdrawal Assessment (CIWA) protocol is implemented in case her symptoms are caused by alcohol withdrawal. Her vital signs are stable and IV lorazepam, 4 mg, is administered once for agitation. Mrs. M’s husband also reports that 1 month ago his wife underwent a transjugular intrahepatic portosystemic shunt (TIPS) procedure for portal hypertension. Outpatient psychotropics (lamotrigine, 100 mg/d, and venlafaxine XR, 75 mg/d) are restarted because withdrawal from these drugs may exacerbate her symptoms. In the ICU Mrs. M experiences a tonic-clonic seizure with fecal incontinence and bitten tongue, which results in a consultation from neurology and the psychiatry consultation-liaison service.
Psychiatry recommends withholding psychotropics, stopping CIWA, and using vital sign parameters along with objective signs of diaphoresis and tremors as indicators of alcohol withdrawal for lorazepam administration. Mrs. M receives IV haloperidol, 1 mg, once during her second day in the hospital for severe agitation, but this medication is discontinued because of concern about lowering her seizure threshold.7 After treatment with lactulose, her ammonia levels trend down to 33 μg/dL, but her altered mental state persists with significant deficits in attention and orientation.
The neurology service performs an EEG that shows no slow-wave, triphasic waves, or epileptiform activity, which likely would be present in delirium or seizures. See Figure 1 for an example of triphasic waves on an EEG and Figure 2 for Mrs. M's EEG results. Subsequent lumbar puncture, MRI, and a second EEG are unremarkable. By the fifth hospital day, Mrs. M is calm and her paranoia has subsided, but she still is confused and disoriented. Psychiatry orders a third EEG while she is in this confused state; it shows no pathologic process. Based on these examinations, neurology posits that Mrs. M is not encephalopathic.
Figure 1: Representative sample of triphasic waves
This EEG tracing is from a 54-year-old woman who underwent prolonged abdominal surgery for lysis of adhesions during which she suffered an intraoperative left subinsular stroke followed by nonconvulsive status epilepticus. The tracing demonstrates typical morphology with the positive sharp transient preceded and followed by smaller amplitude negative deflections. Symmetric, frontal predominance of findings seen is this tracing is common
Figure 2: Mrs. M’s EEG results
This is a representative tracing of Mrs. M’s 3 EEGs revealing an 8.5 to 9 Hz dominant alpha rhythm. There is superimposed frontally dominant beta fast activity, which is consistent with known administration of benzodiazepines
The authors’ observations
Mrs. M had repeated admissions for alcohol dependence and subsequent liver failure. Her recent hospitalization was complicated by a TIPS procedure done 1 month ago. The incidence of hepatic encephalopathy in patients undergoing TIPS is >30%, especially in the first month post-procedure, which raised suspicion that hepatic encephalopathy played a significant role in Mrs. M’s delirium.8
Because of frequent hospitalization, Mrs. M was well known to the internal medicine, neurology, and psychiatry teams, and each used different terms to describe her mental state. Internal medicine used the phrase “acute mental status change,” which covers a broad differential. Neurology used “encephalopathy,” which also is a general term. Psychiatry used “delirium,” which has narrower and more specific diagnostic criteria. Engel et al9 described the delirious patient as having “cerebral insufficiency” with universally abnormal EEG. Regardless of terminology, based on Mrs. M’s acute confusion, one would expect an abnormal EEG, but repeat EEGs were unremarkable.
Interpreting EEG
EEG is one of the few tools available for measuring acute changes in cerebral function, and an EEG slowing remains a hallmark in encephalopathic processes.10,11 Initially, the 3 specialties agreed that Mrs. M’s presentation likely was caused by underlying medical issues or substances (alcohol or others). EEG can help recognize delirium, and, in some cases, elucidate the underlying cause.10,12 It was surprising that Mrs. M’s EEGs were normal despite a clinical presentation of delirium. Because of the normal EEG findings, neurology leaned toward a primary psychiatric (“functional”) etiology as the cause of her delirium vs a general medical condition or alcohol withdrawal (“organic”).
A literature search in regards to sensitivity of EEG in delirium revealed conflicting statements and data. A standard textbook in neurology and psychiatry states that “a normal EEG virtually excludes a toxic-metabolic encephalopathy.”13 The American Psychiatric Association’s (APA) practice guidelines for delirium states: “The presence of EEG abnormalities has fairly good sensitivities for delirium (in one study, the sensitivity was found to be 75%), but the absence does not rule out the diagnosis; thus the EEG is no substitute for careful clinical observation.”6
At the beginning of Mrs. M’s care, in discussion with the neurology and internal medicine teams, we argued that Mrs. M was experiencing delirium despite her initial normal EEG. We did not expect that 2 subsequent EEGs would be normal, especially because the teams witnessed the final EEG being performed while Mrs. M was clinically evaluated and observed to be in a state of delirium.
OUTCOME: Cause still unknown
By the 6th day of hospitalization, Mrs. M’s vitals are normal and she remains hemodynamically stable. Differential diagnosis remains wide and unclear. The psychiatry team feels she could have atypical catatonia due to an underlying mood disorder. One hour after a trial of IV lorazepam, 1 mg, Mrs. M is more lucid and fully oriented, with MMSE of 28/30 (recall was 1/3), indicating normal cognition. During the exam, a psychiatry resident notes Mrs. M winks and feigns a yawn at the medical students and nurses in the room, displaying her boredom with the interview and simplicity of the mental status exam questions. Later that evening, Mrs. M exhibits bizarre sexual gestures toward male hospital staff, including licking a male nursing staff member’s hand.
Although Mrs. M’s initial confusion resolved, the severity of her comorbid psychiatric history warrants inpatient psychiatric hospitalization. She agrees to transfer to the psychiatric ward after she confesses anxiety regarding death, intense demoralization, and guilt related to her condition and her relationship with her 12-year-old daughter. She tearfully reports that she discontinued her psychotropic medications shortly after stopping alcohol 4 months ago. Shortly before her transfer, psychiatry is called back to the medicine floor because of Mrs. M’s disruptive behavior.
The team finds Mrs. M in her hospital gown, pursuing her husband in the hallway as he is leaving, yelling profanities and blaming him for her horrible experience in the hospital. Based on her demeanor, the team determines that she is back to her baseline mental state despite her mood disorder, and that her upcoming inpatient psychiatric stay likely would be too short to address her comorbid personality disorder. The next day she signs out of the hospital against medical advice.
The authors’ observations
We never clearly identified the specific etiology responsible for Mrs. M’s delirium. We assume at the initial presentation she had toxic-metabolic encephalopathy that rapidly resolved with lactulose treatment and lowering her ammonia. She then had a single tonic-clonic seizure, perhaps related to stopping and then restarting her psychotropics. Her subsequent confusion, bizarre sexual behavior, and demeanor on her final hospital days were more indicative of her psychiatric diagnoses. We now suspect that Mrs. M’s delirium was briefer than presumed and she returned to her baseline borderline personality, resulting in some factitious staging of delirium to confuse her 3 treating teams (a psychoanalyst may say this was a form of projective identification).
We felt that if Mrs. M truly was delirious due to metabolic or hepatic dysfunction or alcohol withdrawal, she would have had abnormal EEG findings. We discovered that the notion of “75% sensitivity” of EEG abnormalities cited in the APA guidelines comes from studies that include patients with “psychogenic” and “organic” delirium. Acute manias and agitated psychoses were termed “psychogenic delirium” and acute confusion due to medical conditions or substance issues was termed “organic delirium.”9,12,14-16
This poses a circular reasoning in the diagnostic criteria and clinical approach to delirium. The fallacy is that, according to DSM-IV-TR, delirium is supposed to be the result of a direct physiological consequence of a general medical condition or substance use (criterion D), and cannot be due to psychosis (eg, schizophrenia) or mania (eg, BD). We question the presumptive 75% sensitivity of EEG abnormalities in patients with delirium because it is possible that when some of these studies were conducted the definition of delirium was not solidified or fully understood. We suspect the sensitivity would be much higher if the correct definition of delirium according to DSM-IV-TR is used in future studies. To improve interdisciplinary communication and future research, it would be constructive if all disciplines could agree on a single term, with the same diagnostic criteria, when evaluating a patient with acute confusion.
Related Resources
- Meagher D. Delirium: the role of psychiatry. Advances in Psychiatric Treatment. 2001;7:433-442.
- Casey DA, DeFazio JV Jr, Vansickle K, et al. Delirium. Quick recognition, careful evaluation, and appropriate treatment. Postgrad Med. 1996;100(1):121-4, 128, 133-134.
Drug Brand Names
- Clonazepam • Klonopin
- Docusate • Surfak
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Levothyroxine • Levoxyl, Synthtoid
- Venlafaxine XR • Effexor XR
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. Government. The authors are employees of the U.S. Government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the U.S. Government.” Title 17 U.S.C. 101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
1. Katz IR, Mossey J, Sussman N, et al. Bedside clinical and electrophysiological assessment: assessment of change in vulnerable patients. Int Psychogeriatr. 1991;3(2):289-300.
2. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
3. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
4. McPhee SJ, Papadakis M, Rabow MW. CURRENT medical diagnosis and treatment. New York NY: McGraw Hill Medical; 2012.
5. Brody B. Who has capacity? N Engl J Med. 2009;361(3):232-233.
6. Practice guideline for the treatment of patients with delirium. American Psychiatric Association. Am J Psychiatry. 1999;156(5 suppl):1-20.
7. Fricchione GL, Nejad SH, Esses JA, et al. Postoperative delirium. Am J Psychiatry. 2008;165(7):803-812.
8. Sanyal AJ, Freedman AM, Shiffman ML, et al. Portosystemic encephalopathy after transjugular intrahepatic portosystemic shunt: results of a prospective controlled study. Hepatology. 1994;20(1 pt 1):46-55.
9. Engel GL, Romano J. Delirium a syndrome of cerebral insufficiency. 1959. J Neuropsychiatry Clin Neurosci. 2004;16(4):526-538.
10. Pro JD, Wells CE. The use of the electroencephalogram in the diagnosis of delirium. Dis Nerv Syst. 1977;38(10):804-808.
11. Sidhu KS, Balon R, Ajluni V, et al. Standard EEG and the difficult-to-assess mental status. Ann Clin Psychiatry. 2009;21(2):103-108.
12. Brenner RP. Utility of EEG in delirium: past views and current practice. Int Psychogeriatr. 1991;3(2):211-229.
13. Kaufman DM. Clinical neurology for psychiatrists. 5th ed. Philadelphia PA: Saunders; 2001: 230-232.
14. Bond TC. Recognition of acute delirious mania. Arch Gen Psychiatry. 1980;37(5):553-554.
15. Krauthammer C, Klerman GL. Secondary mania: manic syndromes associated with antecedent physical illness or drugs. Arch Gen Psychiatry. 1978;35(11):1333-1339.
16. Larson EW, Richelson E. Organic causes of mania. Mayo Clin Proc. 1988;63(9):906-912.
CASE: Agitation
Mrs. M, age 39, presents to the emergency department (ED) with altered mental status. She is escorted by her husband and the police. She has a history of severe alcohol dependence, bipolar disorder (BD), anxiety, borderline personality disorder (BPD), hypothyroidism, and bulimia, and had gastric bypass surgery 4 years ago. Her husband called 911 when he could no longer manage Mrs. M’s agitated state. The police found her to be extremely paranoid, restless, and disoriented. Her husband reports that she shouted “the world is going to end” before she escaped naked into her neighborhood streets.
On several occasions Mrs. M had been admitted to the same hospital for alcohol withdrawal and dependence with subsequent liver failure, leading to jaundice, coagulopathy, and ascites. During these hospitalizations, she exhibited poor behavioral tendencies, unhealthy psychological defenses, and chronic maladaptive coping and defense mechanisms congruent with her BPD diagnosis. Specifically, she engaged in splitting of hospital staff, ranging from extreme flattery to overt devaluation and hostility. Other defense mechanisms included denial, distortion, acting out, and passive-aggressive behavior. During these admissions, Mrs. M often displayed deficits in recall and attention on Mini-Mental State Examination (MMSE), but these deficits were associated with concurrent alcohol use and improved rapidly during her stay.
In her current presentation, Mrs. M’s mental status change is more pronounced and atypical compared with earlier admissions. Her outpatient medication regimen includes lamotrigine, 100 mg/d, levothyroxine, 88 mcg/d, venlafaxine extended release (XR), 75 mg/d, clonazepam, 3 mg/d, docusate as needed for constipation, and a daily multivitamin.
The authors’ observations
Delirium is a disturbance of consciousness manifested by a reduced clarity of awareness (impairment in attention) and change in cognition (impairment in orientation, memory, and language).1,2 The disturbance develops over a short time and tends to fluctuate during the day. Delirium is a direct physiological consequence of a general medical condition, substance use (intoxication or withdrawal), or both (Table).3
Delirium generally is a reversible mental disorder but can progress to irreversible brain damage. Prompt and accurate diagnosis of delirium is essential,4 although the condition often is underdiagnosed or misdiagnosed because of lack of recognition.
Table
DSM-IV-TR diagnostic criteria for delirium
|
| Source: Reference 3 |
Patients who have convoluted histories, such as Mrs. M, are common and difficult to manage and treat. These patients become substantially more complex when they are admitted to inpatient medical or surgical services. The need to clarify between delirium (primarily medical) and depression (primarily psychiatric) becomes paramount when administering treatment and evaluating decision-making capacity.5 In Mrs. M’s case, internal medicine, neurology, and psychiatry teams each had a different approach to altered mental status. Each team’s different terminology, assessment, and objectives further complicated an already challenging case.6
EVALUATION: Confounding results
The ED physicians offer a working diagnosis of acute mental status change, administer IV lorazepam, 4 mg, and order restraints for Mrs. M’s severe agitation. Her initial vital signs reveal slightly elevated blood pressure (140/90 mm Hg) and tachycardia (115 beats per minute). Internal medicine clinicians note that Mrs. M is not in acute distress, although she refuses to speak and has a small amount of dried blood on her lips, presumably from a struggle with the police before coming to the hospital, but this is not certain. Her abdomen is not tender; she has normal bowel sounds, and no asterixis is noted on neurologic exam. Physical exam is otherwise normal. A noncontrast head CT scan shows no acute process. Initial lab values show elevations in ammonia (277 μg/dL) and γ-glutamyl transpeptidase (68 U/L). Thyroid-stimulating hormone is 1.45 mlU/L, prothrombin time is 19.5 s, partial thromboplastin time is 40.3 s, and international normalized ratio is 1.67. The internal medicine team admits Mrs. M to the intensive care unit (ICU) for further management of her mental status change with alcohol withdrawal or hepatic encephalopathy as the most likely etiologies.
Mrs. M’s husband says that his wife has not consumed alcohol in the last 4 months in preparation for a possible liver transplant; however, past interactions with Mrs. M’s family suggest they are unreliable. The Clinical Institute Withdrawal Assessment (CIWA) protocol is implemented in case her symptoms are caused by alcohol withdrawal. Her vital signs are stable and IV lorazepam, 4 mg, is administered once for agitation. Mrs. M’s husband also reports that 1 month ago his wife underwent a transjugular intrahepatic portosystemic shunt (TIPS) procedure for portal hypertension. Outpatient psychotropics (lamotrigine, 100 mg/d, and venlafaxine XR, 75 mg/d) are restarted because withdrawal from these drugs may exacerbate her symptoms. In the ICU Mrs. M experiences a tonic-clonic seizure with fecal incontinence and bitten tongue, which results in a consultation from neurology and the psychiatry consultation-liaison service.
Psychiatry recommends withholding psychotropics, stopping CIWA, and using vital sign parameters along with objective signs of diaphoresis and tremors as indicators of alcohol withdrawal for lorazepam administration. Mrs. M receives IV haloperidol, 1 mg, once during her second day in the hospital for severe agitation, but this medication is discontinued because of concern about lowering her seizure threshold.7 After treatment with lactulose, her ammonia levels trend down to 33 μg/dL, but her altered mental state persists with significant deficits in attention and orientation.
The neurology service performs an EEG that shows no slow-wave, triphasic waves, or epileptiform activity, which likely would be present in delirium or seizures. See Figure 1 for an example of triphasic waves on an EEG and Figure 2 for Mrs. M's EEG results. Subsequent lumbar puncture, MRI, and a second EEG are unremarkable. By the fifth hospital day, Mrs. M is calm and her paranoia has subsided, but she still is confused and disoriented. Psychiatry orders a third EEG while she is in this confused state; it shows no pathologic process. Based on these examinations, neurology posits that Mrs. M is not encephalopathic.
Figure 1: Representative sample of triphasic waves
This EEG tracing is from a 54-year-old woman who underwent prolonged abdominal surgery for lysis of adhesions during which she suffered an intraoperative left subinsular stroke followed by nonconvulsive status epilepticus. The tracing demonstrates typical morphology with the positive sharp transient preceded and followed by smaller amplitude negative deflections. Symmetric, frontal predominance of findings seen is this tracing is common
Figure 2: Mrs. M’s EEG results
This is a representative tracing of Mrs. M’s 3 EEGs revealing an 8.5 to 9 Hz dominant alpha rhythm. There is superimposed frontally dominant beta fast activity, which is consistent with known administration of benzodiazepines
The authors’ observations
Mrs. M had repeated admissions for alcohol dependence and subsequent liver failure. Her recent hospitalization was complicated by a TIPS procedure done 1 month ago. The incidence of hepatic encephalopathy in patients undergoing TIPS is >30%, especially in the first month post-procedure, which raised suspicion that hepatic encephalopathy played a significant role in Mrs. M’s delirium.8
Because of frequent hospitalization, Mrs. M was well known to the internal medicine, neurology, and psychiatry teams, and each used different terms to describe her mental state. Internal medicine used the phrase “acute mental status change,” which covers a broad differential. Neurology used “encephalopathy,” which also is a general term. Psychiatry used “delirium,” which has narrower and more specific diagnostic criteria. Engel et al9 described the delirious patient as having “cerebral insufficiency” with universally abnormal EEG. Regardless of terminology, based on Mrs. M’s acute confusion, one would expect an abnormal EEG, but repeat EEGs were unremarkable.
Interpreting EEG
EEG is one of the few tools available for measuring acute changes in cerebral function, and an EEG slowing remains a hallmark in encephalopathic processes.10,11 Initially, the 3 specialties agreed that Mrs. M’s presentation likely was caused by underlying medical issues or substances (alcohol or others). EEG can help recognize delirium, and, in some cases, elucidate the underlying cause.10,12 It was surprising that Mrs. M’s EEGs were normal despite a clinical presentation of delirium. Because of the normal EEG findings, neurology leaned toward a primary psychiatric (“functional”) etiology as the cause of her delirium vs a general medical condition or alcohol withdrawal (“organic”).
A literature search in regards to sensitivity of EEG in delirium revealed conflicting statements and data. A standard textbook in neurology and psychiatry states that “a normal EEG virtually excludes a toxic-metabolic encephalopathy.”13 The American Psychiatric Association’s (APA) practice guidelines for delirium states: “The presence of EEG abnormalities has fairly good sensitivities for delirium (in one study, the sensitivity was found to be 75%), but the absence does not rule out the diagnosis; thus the EEG is no substitute for careful clinical observation.”6
At the beginning of Mrs. M’s care, in discussion with the neurology and internal medicine teams, we argued that Mrs. M was experiencing delirium despite her initial normal EEG. We did not expect that 2 subsequent EEGs would be normal, especially because the teams witnessed the final EEG being performed while Mrs. M was clinically evaluated and observed to be in a state of delirium.
OUTCOME: Cause still unknown
By the 6th day of hospitalization, Mrs. M’s vitals are normal and she remains hemodynamically stable. Differential diagnosis remains wide and unclear. The psychiatry team feels she could have atypical catatonia due to an underlying mood disorder. One hour after a trial of IV lorazepam, 1 mg, Mrs. M is more lucid and fully oriented, with MMSE of 28/30 (recall was 1/3), indicating normal cognition. During the exam, a psychiatry resident notes Mrs. M winks and feigns a yawn at the medical students and nurses in the room, displaying her boredom with the interview and simplicity of the mental status exam questions. Later that evening, Mrs. M exhibits bizarre sexual gestures toward male hospital staff, including licking a male nursing staff member’s hand.
Although Mrs. M’s initial confusion resolved, the severity of her comorbid psychiatric history warrants inpatient psychiatric hospitalization. She agrees to transfer to the psychiatric ward after she confesses anxiety regarding death, intense demoralization, and guilt related to her condition and her relationship with her 12-year-old daughter. She tearfully reports that she discontinued her psychotropic medications shortly after stopping alcohol 4 months ago. Shortly before her transfer, psychiatry is called back to the medicine floor because of Mrs. M’s disruptive behavior.
The team finds Mrs. M in her hospital gown, pursuing her husband in the hallway as he is leaving, yelling profanities and blaming him for her horrible experience in the hospital. Based on her demeanor, the team determines that she is back to her baseline mental state despite her mood disorder, and that her upcoming inpatient psychiatric stay likely would be too short to address her comorbid personality disorder. The next day she signs out of the hospital against medical advice.
The authors’ observations
We never clearly identified the specific etiology responsible for Mrs. M’s delirium. We assume at the initial presentation she had toxic-metabolic encephalopathy that rapidly resolved with lactulose treatment and lowering her ammonia. She then had a single tonic-clonic seizure, perhaps related to stopping and then restarting her psychotropics. Her subsequent confusion, bizarre sexual behavior, and demeanor on her final hospital days were more indicative of her psychiatric diagnoses. We now suspect that Mrs. M’s delirium was briefer than presumed and she returned to her baseline borderline personality, resulting in some factitious staging of delirium to confuse her 3 treating teams (a psychoanalyst may say this was a form of projective identification).
We felt that if Mrs. M truly was delirious due to metabolic or hepatic dysfunction or alcohol withdrawal, she would have had abnormal EEG findings. We discovered that the notion of “75% sensitivity” of EEG abnormalities cited in the APA guidelines comes from studies that include patients with “psychogenic” and “organic” delirium. Acute manias and agitated psychoses were termed “psychogenic delirium” and acute confusion due to medical conditions or substance issues was termed “organic delirium.”9,12,14-16
This poses a circular reasoning in the diagnostic criteria and clinical approach to delirium. The fallacy is that, according to DSM-IV-TR, delirium is supposed to be the result of a direct physiological consequence of a general medical condition or substance use (criterion D), and cannot be due to psychosis (eg, schizophrenia) or mania (eg, BD). We question the presumptive 75% sensitivity of EEG abnormalities in patients with delirium because it is possible that when some of these studies were conducted the definition of delirium was not solidified or fully understood. We suspect the sensitivity would be much higher if the correct definition of delirium according to DSM-IV-TR is used in future studies. To improve interdisciplinary communication and future research, it would be constructive if all disciplines could agree on a single term, with the same diagnostic criteria, when evaluating a patient with acute confusion.
Related Resources
- Meagher D. Delirium: the role of psychiatry. Advances in Psychiatric Treatment. 2001;7:433-442.
- Casey DA, DeFazio JV Jr, Vansickle K, et al. Delirium. Quick recognition, careful evaluation, and appropriate treatment. Postgrad Med. 1996;100(1):121-4, 128, 133-134.
Drug Brand Names
- Clonazepam • Klonopin
- Docusate • Surfak
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Levothyroxine • Levoxyl, Synthtoid
- Venlafaxine XR • Effexor XR
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. Government. The authors are employees of the U.S. Government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the U.S. Government.” Title 17 U.S.C. 101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
CASE: Agitation
Mrs. M, age 39, presents to the emergency department (ED) with altered mental status. She is escorted by her husband and the police. She has a history of severe alcohol dependence, bipolar disorder (BD), anxiety, borderline personality disorder (BPD), hypothyroidism, and bulimia, and had gastric bypass surgery 4 years ago. Her husband called 911 when he could no longer manage Mrs. M’s agitated state. The police found her to be extremely paranoid, restless, and disoriented. Her husband reports that she shouted “the world is going to end” before she escaped naked into her neighborhood streets.
On several occasions Mrs. M had been admitted to the same hospital for alcohol withdrawal and dependence with subsequent liver failure, leading to jaundice, coagulopathy, and ascites. During these hospitalizations, she exhibited poor behavioral tendencies, unhealthy psychological defenses, and chronic maladaptive coping and defense mechanisms congruent with her BPD diagnosis. Specifically, she engaged in splitting of hospital staff, ranging from extreme flattery to overt devaluation and hostility. Other defense mechanisms included denial, distortion, acting out, and passive-aggressive behavior. During these admissions, Mrs. M often displayed deficits in recall and attention on Mini-Mental State Examination (MMSE), but these deficits were associated with concurrent alcohol use and improved rapidly during her stay.
In her current presentation, Mrs. M’s mental status change is more pronounced and atypical compared with earlier admissions. Her outpatient medication regimen includes lamotrigine, 100 mg/d, levothyroxine, 88 mcg/d, venlafaxine extended release (XR), 75 mg/d, clonazepam, 3 mg/d, docusate as needed for constipation, and a daily multivitamin.
The authors’ observations
Delirium is a disturbance of consciousness manifested by a reduced clarity of awareness (impairment in attention) and change in cognition (impairment in orientation, memory, and language).1,2 The disturbance develops over a short time and tends to fluctuate during the day. Delirium is a direct physiological consequence of a general medical condition, substance use (intoxication or withdrawal), or both (Table).3
Delirium generally is a reversible mental disorder but can progress to irreversible brain damage. Prompt and accurate diagnosis of delirium is essential,4 although the condition often is underdiagnosed or misdiagnosed because of lack of recognition.
Table
DSM-IV-TR diagnostic criteria for delirium
|
| Source: Reference 3 |
Patients who have convoluted histories, such as Mrs. M, are common and difficult to manage and treat. These patients become substantially more complex when they are admitted to inpatient medical or surgical services. The need to clarify between delirium (primarily medical) and depression (primarily psychiatric) becomes paramount when administering treatment and evaluating decision-making capacity.5 In Mrs. M’s case, internal medicine, neurology, and psychiatry teams each had a different approach to altered mental status. Each team’s different terminology, assessment, and objectives further complicated an already challenging case.6
EVALUATION: Confounding results
The ED physicians offer a working diagnosis of acute mental status change, administer IV lorazepam, 4 mg, and order restraints for Mrs. M’s severe agitation. Her initial vital signs reveal slightly elevated blood pressure (140/90 mm Hg) and tachycardia (115 beats per minute). Internal medicine clinicians note that Mrs. M is not in acute distress, although she refuses to speak and has a small amount of dried blood on her lips, presumably from a struggle with the police before coming to the hospital, but this is not certain. Her abdomen is not tender; she has normal bowel sounds, and no asterixis is noted on neurologic exam. Physical exam is otherwise normal. A noncontrast head CT scan shows no acute process. Initial lab values show elevations in ammonia (277 μg/dL) and γ-glutamyl transpeptidase (68 U/L). Thyroid-stimulating hormone is 1.45 mlU/L, prothrombin time is 19.5 s, partial thromboplastin time is 40.3 s, and international normalized ratio is 1.67. The internal medicine team admits Mrs. M to the intensive care unit (ICU) for further management of her mental status change with alcohol withdrawal or hepatic encephalopathy as the most likely etiologies.
Mrs. M’s husband says that his wife has not consumed alcohol in the last 4 months in preparation for a possible liver transplant; however, past interactions with Mrs. M’s family suggest they are unreliable. The Clinical Institute Withdrawal Assessment (CIWA) protocol is implemented in case her symptoms are caused by alcohol withdrawal. Her vital signs are stable and IV lorazepam, 4 mg, is administered once for agitation. Mrs. M’s husband also reports that 1 month ago his wife underwent a transjugular intrahepatic portosystemic shunt (TIPS) procedure for portal hypertension. Outpatient psychotropics (lamotrigine, 100 mg/d, and venlafaxine XR, 75 mg/d) are restarted because withdrawal from these drugs may exacerbate her symptoms. In the ICU Mrs. M experiences a tonic-clonic seizure with fecal incontinence and bitten tongue, which results in a consultation from neurology and the psychiatry consultation-liaison service.
Psychiatry recommends withholding psychotropics, stopping CIWA, and using vital sign parameters along with objective signs of diaphoresis and tremors as indicators of alcohol withdrawal for lorazepam administration. Mrs. M receives IV haloperidol, 1 mg, once during her second day in the hospital for severe agitation, but this medication is discontinued because of concern about lowering her seizure threshold.7 After treatment with lactulose, her ammonia levels trend down to 33 μg/dL, but her altered mental state persists with significant deficits in attention and orientation.
The neurology service performs an EEG that shows no slow-wave, triphasic waves, or epileptiform activity, which likely would be present in delirium or seizures. See Figure 1 for an example of triphasic waves on an EEG and Figure 2 for Mrs. M's EEG results. Subsequent lumbar puncture, MRI, and a second EEG are unremarkable. By the fifth hospital day, Mrs. M is calm and her paranoia has subsided, but she still is confused and disoriented. Psychiatry orders a third EEG while she is in this confused state; it shows no pathologic process. Based on these examinations, neurology posits that Mrs. M is not encephalopathic.
Figure 1: Representative sample of triphasic waves
This EEG tracing is from a 54-year-old woman who underwent prolonged abdominal surgery for lysis of adhesions during which she suffered an intraoperative left subinsular stroke followed by nonconvulsive status epilepticus. The tracing demonstrates typical morphology with the positive sharp transient preceded and followed by smaller amplitude negative deflections. Symmetric, frontal predominance of findings seen is this tracing is common
Figure 2: Mrs. M’s EEG results
This is a representative tracing of Mrs. M’s 3 EEGs revealing an 8.5 to 9 Hz dominant alpha rhythm. There is superimposed frontally dominant beta fast activity, which is consistent with known administration of benzodiazepines
The authors’ observations
Mrs. M had repeated admissions for alcohol dependence and subsequent liver failure. Her recent hospitalization was complicated by a TIPS procedure done 1 month ago. The incidence of hepatic encephalopathy in patients undergoing TIPS is >30%, especially in the first month post-procedure, which raised suspicion that hepatic encephalopathy played a significant role in Mrs. M’s delirium.8
Because of frequent hospitalization, Mrs. M was well known to the internal medicine, neurology, and psychiatry teams, and each used different terms to describe her mental state. Internal medicine used the phrase “acute mental status change,” which covers a broad differential. Neurology used “encephalopathy,” which also is a general term. Psychiatry used “delirium,” which has narrower and more specific diagnostic criteria. Engel et al9 described the delirious patient as having “cerebral insufficiency” with universally abnormal EEG. Regardless of terminology, based on Mrs. M’s acute confusion, one would expect an abnormal EEG, but repeat EEGs were unremarkable.
Interpreting EEG
EEG is one of the few tools available for measuring acute changes in cerebral function, and an EEG slowing remains a hallmark in encephalopathic processes.10,11 Initially, the 3 specialties agreed that Mrs. M’s presentation likely was caused by underlying medical issues or substances (alcohol or others). EEG can help recognize delirium, and, in some cases, elucidate the underlying cause.10,12 It was surprising that Mrs. M’s EEGs were normal despite a clinical presentation of delirium. Because of the normal EEG findings, neurology leaned toward a primary psychiatric (“functional”) etiology as the cause of her delirium vs a general medical condition or alcohol withdrawal (“organic”).
A literature search in regards to sensitivity of EEG in delirium revealed conflicting statements and data. A standard textbook in neurology and psychiatry states that “a normal EEG virtually excludes a toxic-metabolic encephalopathy.”13 The American Psychiatric Association’s (APA) practice guidelines for delirium states: “The presence of EEG abnormalities has fairly good sensitivities for delirium (in one study, the sensitivity was found to be 75%), but the absence does not rule out the diagnosis; thus the EEG is no substitute for careful clinical observation.”6
At the beginning of Mrs. M’s care, in discussion with the neurology and internal medicine teams, we argued that Mrs. M was experiencing delirium despite her initial normal EEG. We did not expect that 2 subsequent EEGs would be normal, especially because the teams witnessed the final EEG being performed while Mrs. M was clinically evaluated and observed to be in a state of delirium.
OUTCOME: Cause still unknown
By the 6th day of hospitalization, Mrs. M’s vitals are normal and she remains hemodynamically stable. Differential diagnosis remains wide and unclear. The psychiatry team feels she could have atypical catatonia due to an underlying mood disorder. One hour after a trial of IV lorazepam, 1 mg, Mrs. M is more lucid and fully oriented, with MMSE of 28/30 (recall was 1/3), indicating normal cognition. During the exam, a psychiatry resident notes Mrs. M winks and feigns a yawn at the medical students and nurses in the room, displaying her boredom with the interview and simplicity of the mental status exam questions. Later that evening, Mrs. M exhibits bizarre sexual gestures toward male hospital staff, including licking a male nursing staff member’s hand.
Although Mrs. M’s initial confusion resolved, the severity of her comorbid psychiatric history warrants inpatient psychiatric hospitalization. She agrees to transfer to the psychiatric ward after she confesses anxiety regarding death, intense demoralization, and guilt related to her condition and her relationship with her 12-year-old daughter. She tearfully reports that she discontinued her psychotropic medications shortly after stopping alcohol 4 months ago. Shortly before her transfer, psychiatry is called back to the medicine floor because of Mrs. M’s disruptive behavior.
The team finds Mrs. M in her hospital gown, pursuing her husband in the hallway as he is leaving, yelling profanities and blaming him for her horrible experience in the hospital. Based on her demeanor, the team determines that she is back to her baseline mental state despite her mood disorder, and that her upcoming inpatient psychiatric stay likely would be too short to address her comorbid personality disorder. The next day she signs out of the hospital against medical advice.
The authors’ observations
We never clearly identified the specific etiology responsible for Mrs. M’s delirium. We assume at the initial presentation she had toxic-metabolic encephalopathy that rapidly resolved with lactulose treatment and lowering her ammonia. She then had a single tonic-clonic seizure, perhaps related to stopping and then restarting her psychotropics. Her subsequent confusion, bizarre sexual behavior, and demeanor on her final hospital days were more indicative of her psychiatric diagnoses. We now suspect that Mrs. M’s delirium was briefer than presumed and she returned to her baseline borderline personality, resulting in some factitious staging of delirium to confuse her 3 treating teams (a psychoanalyst may say this was a form of projective identification).
We felt that if Mrs. M truly was delirious due to metabolic or hepatic dysfunction or alcohol withdrawal, she would have had abnormal EEG findings. We discovered that the notion of “75% sensitivity” of EEG abnormalities cited in the APA guidelines comes from studies that include patients with “psychogenic” and “organic” delirium. Acute manias and agitated psychoses were termed “psychogenic delirium” and acute confusion due to medical conditions or substance issues was termed “organic delirium.”9,12,14-16
This poses a circular reasoning in the diagnostic criteria and clinical approach to delirium. The fallacy is that, according to DSM-IV-TR, delirium is supposed to be the result of a direct physiological consequence of a general medical condition or substance use (criterion D), and cannot be due to psychosis (eg, schizophrenia) or mania (eg, BD). We question the presumptive 75% sensitivity of EEG abnormalities in patients with delirium because it is possible that when some of these studies were conducted the definition of delirium was not solidified or fully understood. We suspect the sensitivity would be much higher if the correct definition of delirium according to DSM-IV-TR is used in future studies. To improve interdisciplinary communication and future research, it would be constructive if all disciplines could agree on a single term, with the same diagnostic criteria, when evaluating a patient with acute confusion.
Related Resources
- Meagher D. Delirium: the role of psychiatry. Advances in Psychiatric Treatment. 2001;7:433-442.
- Casey DA, DeFazio JV Jr, Vansickle K, et al. Delirium. Quick recognition, careful evaluation, and appropriate treatment. Postgrad Med. 1996;100(1):121-4, 128, 133-134.
Drug Brand Names
- Clonazepam • Klonopin
- Docusate • Surfak
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lorazepam • Ativan
- Levothyroxine • Levoxyl, Synthtoid
- Venlafaxine XR • Effexor XR
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgment
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. Government. The authors are employees of the U.S. Government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the U.S. Government.” Title 17 U.S.C. 101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
1. Katz IR, Mossey J, Sussman N, et al. Bedside clinical and electrophysiological assessment: assessment of change in vulnerable patients. Int Psychogeriatr. 1991;3(2):289-300.
2. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
3. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
4. McPhee SJ, Papadakis M, Rabow MW. CURRENT medical diagnosis and treatment. New York NY: McGraw Hill Medical; 2012.
5. Brody B. Who has capacity? N Engl J Med. 2009;361(3):232-233.
6. Practice guideline for the treatment of patients with delirium. American Psychiatric Association. Am J Psychiatry. 1999;156(5 suppl):1-20.
7. Fricchione GL, Nejad SH, Esses JA, et al. Postoperative delirium. Am J Psychiatry. 2008;165(7):803-812.
8. Sanyal AJ, Freedman AM, Shiffman ML, et al. Portosystemic encephalopathy after transjugular intrahepatic portosystemic shunt: results of a prospective controlled study. Hepatology. 1994;20(1 pt 1):46-55.
9. Engel GL, Romano J. Delirium a syndrome of cerebral insufficiency. 1959. J Neuropsychiatry Clin Neurosci. 2004;16(4):526-538.
10. Pro JD, Wells CE. The use of the electroencephalogram in the diagnosis of delirium. Dis Nerv Syst. 1977;38(10):804-808.
11. Sidhu KS, Balon R, Ajluni V, et al. Standard EEG and the difficult-to-assess mental status. Ann Clin Psychiatry. 2009;21(2):103-108.
12. Brenner RP. Utility of EEG in delirium: past views and current practice. Int Psychogeriatr. 1991;3(2):211-229.
13. Kaufman DM. Clinical neurology for psychiatrists. 5th ed. Philadelphia PA: Saunders; 2001: 230-232.
14. Bond TC. Recognition of acute delirious mania. Arch Gen Psychiatry. 1980;37(5):553-554.
15. Krauthammer C, Klerman GL. Secondary mania: manic syndromes associated with antecedent physical illness or drugs. Arch Gen Psychiatry. 1978;35(11):1333-1339.
16. Larson EW, Richelson E. Organic causes of mania. Mayo Clin Proc. 1988;63(9):906-912.
1. Katz IR, Mossey J, Sussman N, et al. Bedside clinical and electrophysiological assessment: assessment of change in vulnerable patients. Int Psychogeriatr. 1991;3(2):289-300.
2. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
3. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
4. McPhee SJ, Papadakis M, Rabow MW. CURRENT medical diagnosis and treatment. New York NY: McGraw Hill Medical; 2012.
5. Brody B. Who has capacity? N Engl J Med. 2009;361(3):232-233.
6. Practice guideline for the treatment of patients with delirium. American Psychiatric Association. Am J Psychiatry. 1999;156(5 suppl):1-20.
7. Fricchione GL, Nejad SH, Esses JA, et al. Postoperative delirium. Am J Psychiatry. 2008;165(7):803-812.
8. Sanyal AJ, Freedman AM, Shiffman ML, et al. Portosystemic encephalopathy after transjugular intrahepatic portosystemic shunt: results of a prospective controlled study. Hepatology. 1994;20(1 pt 1):46-55.
9. Engel GL, Romano J. Delirium a syndrome of cerebral insufficiency. 1959. J Neuropsychiatry Clin Neurosci. 2004;16(4):526-538.
10. Pro JD, Wells CE. The use of the electroencephalogram in the diagnosis of delirium. Dis Nerv Syst. 1977;38(10):804-808.
11. Sidhu KS, Balon R, Ajluni V, et al. Standard EEG and the difficult-to-assess mental status. Ann Clin Psychiatry. 2009;21(2):103-108.
12. Brenner RP. Utility of EEG in delirium: past views and current practice. Int Psychogeriatr. 1991;3(2):211-229.
13. Kaufman DM. Clinical neurology for psychiatrists. 5th ed. Philadelphia PA: Saunders; 2001: 230-232.
14. Bond TC. Recognition of acute delirious mania. Arch Gen Psychiatry. 1980;37(5):553-554.
15. Krauthammer C, Klerman GL. Secondary mania: manic syndromes associated with antecedent physical illness or drugs. Arch Gen Psychiatry. 1978;35(11):1333-1339.
16. Larson EW, Richelson E. Organic causes of mania. Mayo Clin Proc. 1988;63(9):906-912.
One twin has cerebral palsy; $103M verdict … and more
AFTER PREMATURE RUPTURE OF MEMBRANES at 25 weeks’ gestation, a woman went to the emergency department (ED) and was later released. Eight days later, she returned to the ED with abdominal pain; a soporific drug was administered. After several hours, it was determined that she was in labor. Twins were delivered vaginally. One child has cerebral palsy and requires assistance in daily activities, although her cognitive function is intact.
PARENTS’ CLAIM The mother should not have been released after premature rupture of her membranes. The nurses and ObGyns failed to timely recognize that the mother was in labor, and failed to prevent premature delivery. Proper recognition of contractions would have allowed for administration of a tocolytic to delay delivery. That drug had been effectively administered during the first two trimesters of the pregnancy. A cesarean delivery should have been performed.
DEFENDANTS’ DEFENSE There was no negligence. The hospital argued that fetal heart-rate monitors did not suggest contractions.
VERDICT A $103 million New York verdict was returned against the hospital; a defense verdict was returned for the physicians.
Perforated uterus and severed iliac artery after D&C
A GYNECOLOGIC SURGEON performed a dilation and curettage (D&C) on a 47-year-old woman. During surgery, the patient suffered a perforated uterus and a severed iliac artery, resulting in a myocardial infarction.
PATIENT’S CLAIM The surgeon failed to dilate the cervix appropriately to assess the cervical and endometrial cavity length, and then failed to use proper instrumentation in the uterus. He did not assess uterine shape before the D&C. The patient suffered cognitive and emotional injuries, and will require additional surgery.
PHYSICIAN’S DEFENSE The patient’s anatomy is abnormal. A perforation is a known complication of a D&C.
VERDICT A $350,000 Wisconsin settlement was reached.
Failure to monitor a high-risk patient
A WOMAN WITH A HEART CONDITION who routinely took a beta-blocker plus migraine medication also had lupus. Her pregnancy was therefore at high risk for developing intrauterine growth restriction. Her US Navy ObGyn was advised by a maternal-fetal medicine (MFM) specialist to monitor the pregnancy closely with frequent ultrasonography and other tests that were never performed.
The baby was born by emergency cesarean delivery at 36 weeks’ gestation. The child suffered severe hypoxia and a brain hemorrhage just before delivery, which caused serious, permanent physical and neurologic injuries. He needs 24-hour care, is confined to a wheelchair, and requires a feeding tube.
PATIENT’S CLAIM The ObGyn failed to monitor the mother for fetal growth restriction as recommended by the MFM specialist.
DEFENDANTS’ DEFENSE There was no negligence; the mother was treated properly.
VERDICT After a $28 million Virginia verdict was awarded, the parties continued to dispute whether the judgment would be paid under California law (where the child was born) or Virginia law (where the case was filed). Prior to a rehearing, a $25 million settlement was reached.
Uterine cancer went undiagnosed
A WOMAN IN HER 50s saw her gynecologist in March 2004 to report vaginal staining. She did not return to the physician’s office until January 2005, when she reported daily vaginal bleeding. Ultrasonography showed a 4-cm mass in the endometrial cavity, consistent with a large polyp. A hysteroscopy and biopsy revealed that the woman had uterine cancer. She underwent a hysterectomy and radiation therapy, but the cancer metastasized to her lungs and she died in October 2006.
ESTATE’S CLAIM The gynecologist failed to diagnose uterine cancer in a timely manner.
PHYSICIAN’S DEFENSE The patient’s cancer was aggressive; an earlier diagnosis would not have changed the outcome.
VERDICT A $820,000 Massachusetts settlement was reached.
WHEN A 51-YEAR-OLD WOMAN NOTICED A BULGE in her vagina, she consulted her gynecologist. He determined the cause to be a cystocele and rectocele, and recommended a tension-free vaginal tape–obturator (TVT-O) procedure with anterior and posterior colporrhaphy.
The patient awoke from surgery in severe pain and was told that she had lost a lot of blood. Two weeks later, the physician explained that the stitches, not yet absorbed, were causing an abrasion, and that more vaginal tissue had been removed than planned.
Two more weeks passed, and the patient used a mirror to look at her vagina but could not see the opening. The TVT-O tape had created a ridge of tissue in the anterior vagina, causing severe stenosis. Vaginal dilators were required to expand the vagina. Entrapment of the dorsal clitoral nerve by the TVT-O tape was also discovered. The patient continues to experience dyspareunia and groin pain.
PATIENT’S CLAIM The gynecologist failed to tell her that, 2 months before surgery, the FDA had issued a public health warning about complications associated with transvaginal placement of surgical mesh during prolapse and urinary incontinence repair. Nor was she informed that the defendant had just completed training in TVT-O surgery, was not fully credentialed, and was proctored during the procedure.
PHYSICIAN’S DEFENSE The case was settled before the trial concluded.
VERDICT A $390,000 Virginia settlement was reached.
Lumpectomy, though no mass palpated
A 52-YEAR-OLD WOMAN FOUND A LUMP in her left breast. Her internist ordered mammography, which identified a 2-cm oval, asymmetrical density in the upper inner quadrant of the left breast. The radiologist recommended ultrasonography (US).
The patient consulted a surgical oncologist, who performed fine-needle aspiration. Pathology identified “clusters of malignant cells consistent with carcinoma,” and suggested a confirmatory biopsy. The oncologist recommended lumpectomy and sentinel node biopsy.
On the day of surgery, the patient could not locate the mass. The oncologist testified that he had palpated it. During surgery, gross examination did not show a mass or tumor. Frozen sections of sentinel nodes did not reveal evidence of cancer.
The patient suffered postsurgical seromas and lymphedema. The lymphedema has partially resolved, but causes pain in her left arm and breast.
PATIENT’S CLAIM The surgical oncologist should have performed US before surgery. It was negligent to continue with surgery when there were negative intraoperative findings for cancer or a mass.
PHYSICIAN’S DEFENSE Proper care was provided.
VERDICT A $950,000 Illinois verdict was returned.
Genetic testing fails to identify cystic fibrosis in one twin
AFTER HAVING ONE CHILD with cystic fibrosis (CF), parents underwent genetic testing. Embryos were prepared for in vitro fertilization (IVF) and sent to a genetic-testing laboratory. The lab reported that the embryos were negative for CF. Two embryos were implanted, and the mother gave birth to twins, one of which has CF.
PARENTS’ CLAIM Multiple errors by the genetic-testing laboratory led to an incorrect report on the embryos. The parents claimed wrongful birth.
DEFENDANTS’ DEFENSE The testing laboratory and physician owner argued that amniocentesis should have been performed during the pregnancy to rule out CF.
VERDICT The trial judge denied the use of the amniocentesis defense because an abortion would have been the only option available, and abortion is against the public policy of Tennessee. The court entered summary judgment on liability for the parents.
A $13 million verdict was returned, including $7 million to the parents for emotional distress.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
AFTER PREMATURE RUPTURE OF MEMBRANES at 25 weeks’ gestation, a woman went to the emergency department (ED) and was later released. Eight days later, she returned to the ED with abdominal pain; a soporific drug was administered. After several hours, it was determined that she was in labor. Twins were delivered vaginally. One child has cerebral palsy and requires assistance in daily activities, although her cognitive function is intact.
PARENTS’ CLAIM The mother should not have been released after premature rupture of her membranes. The nurses and ObGyns failed to timely recognize that the mother was in labor, and failed to prevent premature delivery. Proper recognition of contractions would have allowed for administration of a tocolytic to delay delivery. That drug had been effectively administered during the first two trimesters of the pregnancy. A cesarean delivery should have been performed.
DEFENDANTS’ DEFENSE There was no negligence. The hospital argued that fetal heart-rate monitors did not suggest contractions.
VERDICT A $103 million New York verdict was returned against the hospital; a defense verdict was returned for the physicians.
Perforated uterus and severed iliac artery after D&C
A GYNECOLOGIC SURGEON performed a dilation and curettage (D&C) on a 47-year-old woman. During surgery, the patient suffered a perforated uterus and a severed iliac artery, resulting in a myocardial infarction.
PATIENT’S CLAIM The surgeon failed to dilate the cervix appropriately to assess the cervical and endometrial cavity length, and then failed to use proper instrumentation in the uterus. He did not assess uterine shape before the D&C. The patient suffered cognitive and emotional injuries, and will require additional surgery.
PHYSICIAN’S DEFENSE The patient’s anatomy is abnormal. A perforation is a known complication of a D&C.
VERDICT A $350,000 Wisconsin settlement was reached.
Failure to monitor a high-risk patient
A WOMAN WITH A HEART CONDITION who routinely took a beta-blocker plus migraine medication also had lupus. Her pregnancy was therefore at high risk for developing intrauterine growth restriction. Her US Navy ObGyn was advised by a maternal-fetal medicine (MFM) specialist to monitor the pregnancy closely with frequent ultrasonography and other tests that were never performed.
The baby was born by emergency cesarean delivery at 36 weeks’ gestation. The child suffered severe hypoxia and a brain hemorrhage just before delivery, which caused serious, permanent physical and neurologic injuries. He needs 24-hour care, is confined to a wheelchair, and requires a feeding tube.
PATIENT’S CLAIM The ObGyn failed to monitor the mother for fetal growth restriction as recommended by the MFM specialist.
DEFENDANTS’ DEFENSE There was no negligence; the mother was treated properly.
VERDICT After a $28 million Virginia verdict was awarded, the parties continued to dispute whether the judgment would be paid under California law (where the child was born) or Virginia law (where the case was filed). Prior to a rehearing, a $25 million settlement was reached.
Uterine cancer went undiagnosed
A WOMAN IN HER 50s saw her gynecologist in March 2004 to report vaginal staining. She did not return to the physician’s office until January 2005, when she reported daily vaginal bleeding. Ultrasonography showed a 4-cm mass in the endometrial cavity, consistent with a large polyp. A hysteroscopy and biopsy revealed that the woman had uterine cancer. She underwent a hysterectomy and radiation therapy, but the cancer metastasized to her lungs and she died in October 2006.
ESTATE’S CLAIM The gynecologist failed to diagnose uterine cancer in a timely manner.
PHYSICIAN’S DEFENSE The patient’s cancer was aggressive; an earlier diagnosis would not have changed the outcome.
VERDICT A $820,000 Massachusetts settlement was reached.
WHEN A 51-YEAR-OLD WOMAN NOTICED A BULGE in her vagina, she consulted her gynecologist. He determined the cause to be a cystocele and rectocele, and recommended a tension-free vaginal tape–obturator (TVT-O) procedure with anterior and posterior colporrhaphy.
The patient awoke from surgery in severe pain and was told that she had lost a lot of blood. Two weeks later, the physician explained that the stitches, not yet absorbed, were causing an abrasion, and that more vaginal tissue had been removed than planned.
Two more weeks passed, and the patient used a mirror to look at her vagina but could not see the opening. The TVT-O tape had created a ridge of tissue in the anterior vagina, causing severe stenosis. Vaginal dilators were required to expand the vagina. Entrapment of the dorsal clitoral nerve by the TVT-O tape was also discovered. The patient continues to experience dyspareunia and groin pain.
PATIENT’S CLAIM The gynecologist failed to tell her that, 2 months before surgery, the FDA had issued a public health warning about complications associated with transvaginal placement of surgical mesh during prolapse and urinary incontinence repair. Nor was she informed that the defendant had just completed training in TVT-O surgery, was not fully credentialed, and was proctored during the procedure.
PHYSICIAN’S DEFENSE The case was settled before the trial concluded.
VERDICT A $390,000 Virginia settlement was reached.
Lumpectomy, though no mass palpated
A 52-YEAR-OLD WOMAN FOUND A LUMP in her left breast. Her internist ordered mammography, which identified a 2-cm oval, asymmetrical density in the upper inner quadrant of the left breast. The radiologist recommended ultrasonography (US).
The patient consulted a surgical oncologist, who performed fine-needle aspiration. Pathology identified “clusters of malignant cells consistent with carcinoma,” and suggested a confirmatory biopsy. The oncologist recommended lumpectomy and sentinel node biopsy.
On the day of surgery, the patient could not locate the mass. The oncologist testified that he had palpated it. During surgery, gross examination did not show a mass or tumor. Frozen sections of sentinel nodes did not reveal evidence of cancer.
The patient suffered postsurgical seromas and lymphedema. The lymphedema has partially resolved, but causes pain in her left arm and breast.
PATIENT’S CLAIM The surgical oncologist should have performed US before surgery. It was negligent to continue with surgery when there were negative intraoperative findings for cancer or a mass.
PHYSICIAN’S DEFENSE Proper care was provided.
VERDICT A $950,000 Illinois verdict was returned.
Genetic testing fails to identify cystic fibrosis in one twin
AFTER HAVING ONE CHILD with cystic fibrosis (CF), parents underwent genetic testing. Embryos were prepared for in vitro fertilization (IVF) and sent to a genetic-testing laboratory. The lab reported that the embryos were negative for CF. Two embryos were implanted, and the mother gave birth to twins, one of which has CF.
PARENTS’ CLAIM Multiple errors by the genetic-testing laboratory led to an incorrect report on the embryos. The parents claimed wrongful birth.
DEFENDANTS’ DEFENSE The testing laboratory and physician owner argued that amniocentesis should have been performed during the pregnancy to rule out CF.
VERDICT The trial judge denied the use of the amniocentesis defense because an abortion would have been the only option available, and abortion is against the public policy of Tennessee. The court entered summary judgment on liability for the parents.
A $13 million verdict was returned, including $7 million to the parents for emotional distress.
AFTER PREMATURE RUPTURE OF MEMBRANES at 25 weeks’ gestation, a woman went to the emergency department (ED) and was later released. Eight days later, she returned to the ED with abdominal pain; a soporific drug was administered. After several hours, it was determined that she was in labor. Twins were delivered vaginally. One child has cerebral palsy and requires assistance in daily activities, although her cognitive function is intact.
PARENTS’ CLAIM The mother should not have been released after premature rupture of her membranes. The nurses and ObGyns failed to timely recognize that the mother was in labor, and failed to prevent premature delivery. Proper recognition of contractions would have allowed for administration of a tocolytic to delay delivery. That drug had been effectively administered during the first two trimesters of the pregnancy. A cesarean delivery should have been performed.
DEFENDANTS’ DEFENSE There was no negligence. The hospital argued that fetal heart-rate monitors did not suggest contractions.
VERDICT A $103 million New York verdict was returned against the hospital; a defense verdict was returned for the physicians.
Perforated uterus and severed iliac artery after D&C
A GYNECOLOGIC SURGEON performed a dilation and curettage (D&C) on a 47-year-old woman. During surgery, the patient suffered a perforated uterus and a severed iliac artery, resulting in a myocardial infarction.
PATIENT’S CLAIM The surgeon failed to dilate the cervix appropriately to assess the cervical and endometrial cavity length, and then failed to use proper instrumentation in the uterus. He did not assess uterine shape before the D&C. The patient suffered cognitive and emotional injuries, and will require additional surgery.
PHYSICIAN’S DEFENSE The patient’s anatomy is abnormal. A perforation is a known complication of a D&C.
VERDICT A $350,000 Wisconsin settlement was reached.
Failure to monitor a high-risk patient
A WOMAN WITH A HEART CONDITION who routinely took a beta-blocker plus migraine medication also had lupus. Her pregnancy was therefore at high risk for developing intrauterine growth restriction. Her US Navy ObGyn was advised by a maternal-fetal medicine (MFM) specialist to monitor the pregnancy closely with frequent ultrasonography and other tests that were never performed.
The baby was born by emergency cesarean delivery at 36 weeks’ gestation. The child suffered severe hypoxia and a brain hemorrhage just before delivery, which caused serious, permanent physical and neurologic injuries. He needs 24-hour care, is confined to a wheelchair, and requires a feeding tube.
PATIENT’S CLAIM The ObGyn failed to monitor the mother for fetal growth restriction as recommended by the MFM specialist.
DEFENDANTS’ DEFENSE There was no negligence; the mother was treated properly.
VERDICT After a $28 million Virginia verdict was awarded, the parties continued to dispute whether the judgment would be paid under California law (where the child was born) or Virginia law (where the case was filed). Prior to a rehearing, a $25 million settlement was reached.
Uterine cancer went undiagnosed
A WOMAN IN HER 50s saw her gynecologist in March 2004 to report vaginal staining. She did not return to the physician’s office until January 2005, when she reported daily vaginal bleeding. Ultrasonography showed a 4-cm mass in the endometrial cavity, consistent with a large polyp. A hysteroscopy and biopsy revealed that the woman had uterine cancer. She underwent a hysterectomy and radiation therapy, but the cancer metastasized to her lungs and she died in October 2006.
ESTATE’S CLAIM The gynecologist failed to diagnose uterine cancer in a timely manner.
PHYSICIAN’S DEFENSE The patient’s cancer was aggressive; an earlier diagnosis would not have changed the outcome.
VERDICT A $820,000 Massachusetts settlement was reached.
WHEN A 51-YEAR-OLD WOMAN NOTICED A BULGE in her vagina, she consulted her gynecologist. He determined the cause to be a cystocele and rectocele, and recommended a tension-free vaginal tape–obturator (TVT-O) procedure with anterior and posterior colporrhaphy.
The patient awoke from surgery in severe pain and was told that she had lost a lot of blood. Two weeks later, the physician explained that the stitches, not yet absorbed, were causing an abrasion, and that more vaginal tissue had been removed than planned.
Two more weeks passed, and the patient used a mirror to look at her vagina but could not see the opening. The TVT-O tape had created a ridge of tissue in the anterior vagina, causing severe stenosis. Vaginal dilators were required to expand the vagina. Entrapment of the dorsal clitoral nerve by the TVT-O tape was also discovered. The patient continues to experience dyspareunia and groin pain.
PATIENT’S CLAIM The gynecologist failed to tell her that, 2 months before surgery, the FDA had issued a public health warning about complications associated with transvaginal placement of surgical mesh during prolapse and urinary incontinence repair. Nor was she informed that the defendant had just completed training in TVT-O surgery, was not fully credentialed, and was proctored during the procedure.
PHYSICIAN’S DEFENSE The case was settled before the trial concluded.
VERDICT A $390,000 Virginia settlement was reached.
Lumpectomy, though no mass palpated
A 52-YEAR-OLD WOMAN FOUND A LUMP in her left breast. Her internist ordered mammography, which identified a 2-cm oval, asymmetrical density in the upper inner quadrant of the left breast. The radiologist recommended ultrasonography (US).
The patient consulted a surgical oncologist, who performed fine-needle aspiration. Pathology identified “clusters of malignant cells consistent with carcinoma,” and suggested a confirmatory biopsy. The oncologist recommended lumpectomy and sentinel node biopsy.
On the day of surgery, the patient could not locate the mass. The oncologist testified that he had palpated it. During surgery, gross examination did not show a mass or tumor. Frozen sections of sentinel nodes did not reveal evidence of cancer.
The patient suffered postsurgical seromas and lymphedema. The lymphedema has partially resolved, but causes pain in her left arm and breast.
PATIENT’S CLAIM The surgical oncologist should have performed US before surgery. It was negligent to continue with surgery when there were negative intraoperative findings for cancer or a mass.
PHYSICIAN’S DEFENSE Proper care was provided.
VERDICT A $950,000 Illinois verdict was returned.
Genetic testing fails to identify cystic fibrosis in one twin
AFTER HAVING ONE CHILD with cystic fibrosis (CF), parents underwent genetic testing. Embryos were prepared for in vitro fertilization (IVF) and sent to a genetic-testing laboratory. The lab reported that the embryos were negative for CF. Two embryos were implanted, and the mother gave birth to twins, one of which has CF.
PARENTS’ CLAIM Multiple errors by the genetic-testing laboratory led to an incorrect report on the embryos. The parents claimed wrongful birth.
DEFENDANTS’ DEFENSE The testing laboratory and physician owner argued that amniocentesis should have been performed during the pregnancy to rule out CF.
VERDICT The trial judge denied the use of the amniocentesis defense because an abortion would have been the only option available, and abortion is against the public policy of Tennessee. The court entered summary judgment on liability for the parents.
A $13 million verdict was returned, including $7 million to the parents for emotional distress.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.