User login
Mindfulness-based CBT an ‘important’ option for moderate depression
The findings suggest that “offering practitioner-supported MBCT-SH as an intervention for mild to moderate depression would improve outcomes and save money compared with practitioner-supported CBT-SH,” noted the investigators, led by Clara Strauss, PhD, DClinPsy, with the University of Sussex School of Psychology in England.
Practitioner-supported CBT-SH is recommended in U.K. national treatment guidelines for mild to moderate depression. However, some patients’ conditions don’t respond, and dropout rates are high.
The Low-Intensity Guided Help Through Mindfulness (LIGHTMind) trial tested practitioner-supported MBCT-SH as an alternative.
The findings have “important implications” for the more than 100,000 people currently offered CBT-SH for depression in the Improving Access to Psychological Therapies (IAPT) program each year and in publicly funded services elsewhere, the researchers noted.
If translated into routine practice, “this would see many more people recovering from depression while costing health services less money,” they added.
The study was published online in JAMA Psychiatry .
Practice changing?
The trial included 410 adults (mean age, 32 years; 62% women) with mild to moderate depression who were recruited from 10 publicly funded psychological therapy services in England as part of the IAPT program.
Participants were given one of two established self-help workbooks – The Mindful Way Workbook: An 8-Week Program to Free Yourself from Depression and Emotional Distress, written by the pioneers of MBCT, or Overcoming Depression and Low Mood, 3rd Edition: A Five Areas Approach, which is a CBT-SH program widely used in IAPT.
Use of the self-help books was supported by six structured phone or in-person sessions with a trained psychological well-being practitioner.
The primary outcome was depression symptom severity at 16 weeks, which was determined on the basis of Patient Health Questionnaire 9 (PHQ-9) score.
At 16 weeks following randomization, MBCT-SH led to significantly greater reductions in depression symptom severity compared with CBT-SH (mean PHQ-9 score, 7.2 vs. 8.6; between-group difference, 1.5 points; P = .009; d = −0.36).
MBCT-SH also had superior effects on anxiety symptom severity at 16 weeks.
At the 42-week follow-up, between-group effects on depression and anxiety symptom severity remained in the hypothesized direction but were nonsignificant.
This could be due in part by the greater postintervention psychological therapy accessed by participants in the CBT-SH group, the investigators noted.
Practitioner-supported MBCT-SH was more cost-effective than supported CBT-SH.
On average, the CBT-SH intervention cost health services £526 ($631) more per participant than the MBCT-SH intervention over the 42-week follow-up. The probability of MBCT-SH being cost-effective compared with CBT-SH exceeded 95%, the researchers noted.
Useful model for the United States
Commenting for this news organization, Zindel Segal, PhD, professor of psychology, University of Toronto, Scarborough, cautioned against making too much of the differences between the groups, because CBT-SH “trended positive and had a pretty healthy effect size, it just never reached significance.
“I wouldn’t say mindfulness drastically outperformed cognitive therapy. But cognitive therapy is a robust treatment in its own right, and so doing a little bit better is significant,” Dr. Segal said.
He also noted that, appropriately, the trial enrolled adults who were experiencing moderate depression and were not acutely ill. “That’s one of the rationales for self-help compared to providing patients with a more resource-intensive group treatment.
“If you look at the needs of people with moderate depression, what you find is that for cognitive therapy to work, negative thoughts and feelings need to be pervasive in order to make use of the techniques,” Dr. Segal explained.
“With mindfulness, you don’t need any to have constant negative thoughts or feelings. Anything that arises in your experience serves as grist for mill in terms of concentration and focus,” Dr. Segal said.
He also noted that mindfulness-based intervention is “more optimized” for people who are experiencing some measure of recovery or remission.
“It’s well suited for that, as it trends towards the wellness spectrum. But for people who might have greater levels of acuity or severity, cognitive-behavioral therapy might be indicated,” said Dr. Segal.
He also said the U.K. study findings are relevant to U.S. patients with depression.
“While it’s not disseminated in the same way through any kind of national program, the self-help books that are used are widely available, and the support that people were offered, either in person, telephone, or email, could be easily delivered. This would be a very useful model,” Dr. Segal said.
The LIGHTMind trial was funded by the National Institute for Health and Care Research and the Brighton and Sussex Clinical Trials Unit. Dr. Strauss has received grants from Headspace, is research lead for Sussex Mindfulness Centre, and has been chief investigator on National Institute for Health and Care Research. Dr. Segal is one of the authors of the MBCT-SH workbooks used in the study.
A version of this article first appeared on Medscape.com.
The findings suggest that “offering practitioner-supported MBCT-SH as an intervention for mild to moderate depression would improve outcomes and save money compared with practitioner-supported CBT-SH,” noted the investigators, led by Clara Strauss, PhD, DClinPsy, with the University of Sussex School of Psychology in England.
Practitioner-supported CBT-SH is recommended in U.K. national treatment guidelines for mild to moderate depression. However, some patients’ conditions don’t respond, and dropout rates are high.
The Low-Intensity Guided Help Through Mindfulness (LIGHTMind) trial tested practitioner-supported MBCT-SH as an alternative.
The findings have “important implications” for the more than 100,000 people currently offered CBT-SH for depression in the Improving Access to Psychological Therapies (IAPT) program each year and in publicly funded services elsewhere, the researchers noted.
If translated into routine practice, “this would see many more people recovering from depression while costing health services less money,” they added.
The study was published online in JAMA Psychiatry .
Practice changing?
The trial included 410 adults (mean age, 32 years; 62% women) with mild to moderate depression who were recruited from 10 publicly funded psychological therapy services in England as part of the IAPT program.
Participants were given one of two established self-help workbooks – The Mindful Way Workbook: An 8-Week Program to Free Yourself from Depression and Emotional Distress, written by the pioneers of MBCT, or Overcoming Depression and Low Mood, 3rd Edition: A Five Areas Approach, which is a CBT-SH program widely used in IAPT.
Use of the self-help books was supported by six structured phone or in-person sessions with a trained psychological well-being practitioner.
The primary outcome was depression symptom severity at 16 weeks, which was determined on the basis of Patient Health Questionnaire 9 (PHQ-9) score.
At 16 weeks following randomization, MBCT-SH led to significantly greater reductions in depression symptom severity compared with CBT-SH (mean PHQ-9 score, 7.2 vs. 8.6; between-group difference, 1.5 points; P = .009; d = −0.36).
MBCT-SH also had superior effects on anxiety symptom severity at 16 weeks.
At the 42-week follow-up, between-group effects on depression and anxiety symptom severity remained in the hypothesized direction but were nonsignificant.
This could be due in part by the greater postintervention psychological therapy accessed by participants in the CBT-SH group, the investigators noted.
Practitioner-supported MBCT-SH was more cost-effective than supported CBT-SH.
On average, the CBT-SH intervention cost health services £526 ($631) more per participant than the MBCT-SH intervention over the 42-week follow-up. The probability of MBCT-SH being cost-effective compared with CBT-SH exceeded 95%, the researchers noted.
Useful model for the United States
Commenting for this news organization, Zindel Segal, PhD, professor of psychology, University of Toronto, Scarborough, cautioned against making too much of the differences between the groups, because CBT-SH “trended positive and had a pretty healthy effect size, it just never reached significance.
“I wouldn’t say mindfulness drastically outperformed cognitive therapy. But cognitive therapy is a robust treatment in its own right, and so doing a little bit better is significant,” Dr. Segal said.
He also noted that, appropriately, the trial enrolled adults who were experiencing moderate depression and were not acutely ill. “That’s one of the rationales for self-help compared to providing patients with a more resource-intensive group treatment.
“If you look at the needs of people with moderate depression, what you find is that for cognitive therapy to work, negative thoughts and feelings need to be pervasive in order to make use of the techniques,” Dr. Segal explained.
“With mindfulness, you don’t need any to have constant negative thoughts or feelings. Anything that arises in your experience serves as grist for mill in terms of concentration and focus,” Dr. Segal said.
He also noted that mindfulness-based intervention is “more optimized” for people who are experiencing some measure of recovery or remission.
“It’s well suited for that, as it trends towards the wellness spectrum. But for people who might have greater levels of acuity or severity, cognitive-behavioral therapy might be indicated,” said Dr. Segal.
He also said the U.K. study findings are relevant to U.S. patients with depression.
“While it’s not disseminated in the same way through any kind of national program, the self-help books that are used are widely available, and the support that people were offered, either in person, telephone, or email, could be easily delivered. This would be a very useful model,” Dr. Segal said.
The LIGHTMind trial was funded by the National Institute for Health and Care Research and the Brighton and Sussex Clinical Trials Unit. Dr. Strauss has received grants from Headspace, is research lead for Sussex Mindfulness Centre, and has been chief investigator on National Institute for Health and Care Research. Dr. Segal is one of the authors of the MBCT-SH workbooks used in the study.
A version of this article first appeared on Medscape.com.
The findings suggest that “offering practitioner-supported MBCT-SH as an intervention for mild to moderate depression would improve outcomes and save money compared with practitioner-supported CBT-SH,” noted the investigators, led by Clara Strauss, PhD, DClinPsy, with the University of Sussex School of Psychology in England.
Practitioner-supported CBT-SH is recommended in U.K. national treatment guidelines for mild to moderate depression. However, some patients’ conditions don’t respond, and dropout rates are high.
The Low-Intensity Guided Help Through Mindfulness (LIGHTMind) trial tested practitioner-supported MBCT-SH as an alternative.
The findings have “important implications” for the more than 100,000 people currently offered CBT-SH for depression in the Improving Access to Psychological Therapies (IAPT) program each year and in publicly funded services elsewhere, the researchers noted.
If translated into routine practice, “this would see many more people recovering from depression while costing health services less money,” they added.
The study was published online in JAMA Psychiatry .
Practice changing?
The trial included 410 adults (mean age, 32 years; 62% women) with mild to moderate depression who were recruited from 10 publicly funded psychological therapy services in England as part of the IAPT program.
Participants were given one of two established self-help workbooks – The Mindful Way Workbook: An 8-Week Program to Free Yourself from Depression and Emotional Distress, written by the pioneers of MBCT, or Overcoming Depression and Low Mood, 3rd Edition: A Five Areas Approach, which is a CBT-SH program widely used in IAPT.
Use of the self-help books was supported by six structured phone or in-person sessions with a trained psychological well-being practitioner.
The primary outcome was depression symptom severity at 16 weeks, which was determined on the basis of Patient Health Questionnaire 9 (PHQ-9) score.
At 16 weeks following randomization, MBCT-SH led to significantly greater reductions in depression symptom severity compared with CBT-SH (mean PHQ-9 score, 7.2 vs. 8.6; between-group difference, 1.5 points; P = .009; d = −0.36).
MBCT-SH also had superior effects on anxiety symptom severity at 16 weeks.
At the 42-week follow-up, between-group effects on depression and anxiety symptom severity remained in the hypothesized direction but were nonsignificant.
This could be due in part by the greater postintervention psychological therapy accessed by participants in the CBT-SH group, the investigators noted.
Practitioner-supported MBCT-SH was more cost-effective than supported CBT-SH.
On average, the CBT-SH intervention cost health services £526 ($631) more per participant than the MBCT-SH intervention over the 42-week follow-up. The probability of MBCT-SH being cost-effective compared with CBT-SH exceeded 95%, the researchers noted.
Useful model for the United States
Commenting for this news organization, Zindel Segal, PhD, professor of psychology, University of Toronto, Scarborough, cautioned against making too much of the differences between the groups, because CBT-SH “trended positive and had a pretty healthy effect size, it just never reached significance.
“I wouldn’t say mindfulness drastically outperformed cognitive therapy. But cognitive therapy is a robust treatment in its own right, and so doing a little bit better is significant,” Dr. Segal said.
He also noted that, appropriately, the trial enrolled adults who were experiencing moderate depression and were not acutely ill. “That’s one of the rationales for self-help compared to providing patients with a more resource-intensive group treatment.
“If you look at the needs of people with moderate depression, what you find is that for cognitive therapy to work, negative thoughts and feelings need to be pervasive in order to make use of the techniques,” Dr. Segal explained.
“With mindfulness, you don’t need any to have constant negative thoughts or feelings. Anything that arises in your experience serves as grist for mill in terms of concentration and focus,” Dr. Segal said.
He also noted that mindfulness-based intervention is “more optimized” for people who are experiencing some measure of recovery or remission.
“It’s well suited for that, as it trends towards the wellness spectrum. But for people who might have greater levels of acuity or severity, cognitive-behavioral therapy might be indicated,” said Dr. Segal.
He also said the U.K. study findings are relevant to U.S. patients with depression.
“While it’s not disseminated in the same way through any kind of national program, the self-help books that are used are widely available, and the support that people were offered, either in person, telephone, or email, could be easily delivered. This would be a very useful model,” Dr. Segal said.
The LIGHTMind trial was funded by the National Institute for Health and Care Research and the Brighton and Sussex Clinical Trials Unit. Dr. Strauss has received grants from Headspace, is research lead for Sussex Mindfulness Centre, and has been chief investigator on National Institute for Health and Care Research. Dr. Segal is one of the authors of the MBCT-SH workbooks used in the study.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Doctor’s checklist for treating long COVID patients
Lisa McCorkell had a mild bout of COVID-19 in March 2020. Young and healthy, she assumed that she would bounce back quickly. But when her fatigue, shortness of breath, and brain fog persisted, she realized that she most likely had long COVID.
“Back then, we as patients basically coined the term,” she said. While her first primary care provider was sympathetic, they were unsure how to treat her. After her insurance changed, she ended up with a second primary care provider who didn’t take her symptoms seriously. “They dismissed my complaints and told me they were all in my head. I didn’t seek care for a while after that.”
Ms. McCorkell’s symptoms improved after her first COVID vaccine in the spring of 2021. She also finally found a new primary care doctor she could trust. But as one of the founders of the Patient-Led Research Collaborative, a group of researchers who study long COVID, she said many doctors still don’t know the hallmark symptoms of the condition or how to treat it.
“There’s still a lack of education on what long COVID is, and the symptoms associated with it,” she said. “Many of the symptoms that occur in long COVID are symptoms of other chronic conditions, such as chronic fatigue syndrome, that are often dismissed. And even if providers believe patients and send them for a workup, many of the routine blood and imaging tests come back normal.”
The term “long COVID” emerged in May 2020. And though the condition was recognized within a few months of the start of the pandemic, doctors weren’t sure how to screen or treat it.
While knowledge has developed since then, primary care doctors are still in a tough spot. They’re often the first providers that patients turn to when they have symptoms of long COVID.
“There’s no clear algorithm to pick up long COVID – there are no definite blood tests or biomarkers, or specific things to look for on a physical exam,” said Lawrence Purpura, MD, an infectious disease specialist and director of the long COVID clinic at Columbia University Medical Center, New York. “It’s a complicated disease that can impact every organ system of the body.”
Even so, emerging research has identified a checklist of sorts that doctors should consider when a patient seeks care for what appears to be long COVID. Among them: the key systems and organs impacted by the disease, the most common symptoms, useful therapeutic options for symptom management that have been found to help people with long COVID, and the best healthy lifestyle choices that doctors can recommend to help their patients
Here’s a closer look at each of these aspects, based on research and interviews with experts, patients, and doctors.
Key systems, organs impacted
About 10% of people who are infected with COVID-19 go on to have long COVID, according to a recent study that Ms. McCorkell helped coauthor. But more than 3 years into the pandemic, much about the condition is still a mystery.
COVID is a unique virus because it can spread far and wide in a patient’s body. A December 2022 study, published in Nature, autopsied 44 people who died of COVID and found that the virus could spread throughout the body and persist, in one case as long as 230 days after symptoms started.
“We know that there are dozens of symptoms across multiple organ systems,” said Ms. McCorkell. “That makes it harder for a primary care physician to connect the dots and associate it with COVID.”
A paper published in Nature Medicine proposed one way to help guide diagnosis. It divided symptoms into four groups:
- Cardiac and renal issues such as heart palpitations, chest pain, and kidney damage
- Sleep and anxiety problems like insomnia, waking up in the middle of the night, and anxiety
- In the musculoskeletal and nervous systems: musculoskeletal pain, osteoarthritis, and problems with mental skills
- In the digestive and respiratory systems: trouble breathing, asthma, stomach pain, nausea, and vomiting
There were also specific patterns in these groups. People in the first group were more likely to be older, male, have other conditions and to have been infected during the first wave of the COVID pandemic. People in the second group were over 60% female, and were more likely to have had previous allergies or asthma. The third group was also about 60% female, and many of them already had autoimmune conditions such as rheumatoid arthritis. Members of the fourth group – also 60% female – were the least likely of all the groups to have another condition.
This research is helpful, because it gives doctors a better sense of what conditions might make a patient more likely to get long COVID, as well as specific symptoms to look out for, said Steven Flanagan, MD, a physical medicine and rehabilitation specialist at New York University Langone Medical Center who also specializes in treating patients with long COVID.
But the “challenge there, though, for health care providers is that not everyone will fall neatly into one of these categories,” he stressed.
Checklist of symptoms
Although long COVID can be confusing, doctors say there are several symptoms that appear consistently that primary care providers should look out for, that could flag long COVID.
Postexertional malaise (PEM). This is different from simply feeling tired. “This term is often conflated with fatigue, but it’s very different,” said David Putrino, PhD, director of rehabilitation innovation at the Mount Sinai Health System in New York, who says that he sees it in about 90% of patients who come to his long COVID clinic.
PEM is the worsening of symptoms after physical or mental exertion. This usually occurs a day or 2 after the activity, but it can last for days, and sometimes weeks.
“It’s very different from fatigue, which is just a generalized tiredness, and exercise intolerance, where someone complains of not being able to do their usual workout on the treadmill,” he noted. “People with PEM are able to push through and do what they need to do, and then are hit with symptoms anywhere from 12 to 72 hours later.”
Dysautonomia. This is an umbrella term used to describe a dysfunction of the autonomic nervous system, which regulates bodily functions that you can’t control, like your blood pressure, heart rate, and breathing. This can cause symptoms such as heart palpitations, along with orthostatic intolerance, which means you can’t stand up for long without feeling faint or dizzy.
“In my practice, about 80% of patients meet criteria for dysautonomia,” said Dr. Putrino. Other research has found that it’s present in about two-thirds of long COVID patients.
One relatively easy way primary care providers can diagnose dysautonomia is to do the tilt table test. This helps check for postural orthostatic tachycardia syndrome (POTS), one of the most common forms of dysautonomia. During this exam, the patient lies flat on a table. As the head of the table is raised to an almost upright position, their heart rate and blood pressure are measured. Signs of POTS include an abnormal heart rate when you’re upright, as well as a worsening of symptoms.
Exercise intolerance. A review published in the journal JAMA Network Open analyzed 38 studies on long COVID and exercise and found that patients with the condition had a much harder time doing physical activity. Exercise capacity was reduced to levels that would be expected about a decade later in life, according to study authors.
“This is especially important because it can’t be explained just by deconditioning,” said Dr. Purpura. “Sometimes these patients are encouraged to ramp up exercise as a way to help with symptoms, but in these cases, encouraging them to push through can cause postexertional malaise, which sets patients back and delays recovery.”
While long COVID can cause dozens of symptoms, a paper Ms. McCorkell coauthored zeroed in on some of the most common ones: chest pain, heart palpitations, coughing, shortness of breath, belly pain, nausea, problems with mental skills, fatigue, disordered sleep, memory loss, ringing in the ears (tinnitus), erectile dysfunction, irregular menstruation, and worsened premenstrual syndrome.
While most primary care providers are familiar with some of these long COVID symptoms, they may not be aware of others.
“COVID itself seems to cause hormonal changes that can lead to erection and menstrual cycle problems,” explained Dr. Putrino. “But these may not be picked up in a visit if the patient is complaining of other signs of long COVID.”
It’s not just what symptoms are, but when they began to occur, he added. “Usually, these symptoms either start with the initial COVID infection, or begin sometime within 3 months after the acute COVID infection. That’s why it’s important for people with COVID to take notice of anything unusual that crops up within a month or 2 after getting sick.”
Can you prevent long COVID?
You can’t, but one of the best ways to reduce your risk is to get vaccinated. Getting at least one dose of a COVID vaccine before you test positive for COVID lowers your risk of long COVID by about 35% according to a study published in Antimicrobial Stewardship & Healthcare Epidemiology. Unvaccinated people who recovered from COVID, and then got a vaccine, lowered their own long COVID risk by 27%.
In addition, a study published in JAMA Internal Medicine found that women who were infected with COVID were less likely to go on to get long COVID and/or have less debilitating symptoms if they had a healthy lifestyle, which included the following: a healthy weight (a body mass index between 18.5 and 24.7 kg/m2), never-smoker, moderate alcohol consumption, a high-quality diet, 7-9 hours of sleep a night, and at least 150 minutes per week of physical activity
But Ms. McCorkell noted that she herself had a healthy preinfection lifestyle but got long COVID anyway, suggesting these approaches don’t work for everyone.
“I think one reason my symptoms weren’t addressed by primary care physicians for so long is because they looked at me and saw that I was young and healthy, so they dismissed my reports as being all in my head,” she explained. “But we know now anyone can get long COVID, regardless of age, health status, or disease severity. That’s why it’s so important that primary care physicians be able to recognize symptoms.”
A version of this article first appeared on WebMD.com.
Lisa McCorkell had a mild bout of COVID-19 in March 2020. Young and healthy, she assumed that she would bounce back quickly. But when her fatigue, shortness of breath, and brain fog persisted, she realized that she most likely had long COVID.
“Back then, we as patients basically coined the term,” she said. While her first primary care provider was sympathetic, they were unsure how to treat her. After her insurance changed, she ended up with a second primary care provider who didn’t take her symptoms seriously. “They dismissed my complaints and told me they were all in my head. I didn’t seek care for a while after that.”
Ms. McCorkell’s symptoms improved after her first COVID vaccine in the spring of 2021. She also finally found a new primary care doctor she could trust. But as one of the founders of the Patient-Led Research Collaborative, a group of researchers who study long COVID, she said many doctors still don’t know the hallmark symptoms of the condition or how to treat it.
“There’s still a lack of education on what long COVID is, and the symptoms associated with it,” she said. “Many of the symptoms that occur in long COVID are symptoms of other chronic conditions, such as chronic fatigue syndrome, that are often dismissed. And even if providers believe patients and send them for a workup, many of the routine blood and imaging tests come back normal.”
The term “long COVID” emerged in May 2020. And though the condition was recognized within a few months of the start of the pandemic, doctors weren’t sure how to screen or treat it.
While knowledge has developed since then, primary care doctors are still in a tough spot. They’re often the first providers that patients turn to when they have symptoms of long COVID.
“There’s no clear algorithm to pick up long COVID – there are no definite blood tests or biomarkers, or specific things to look for on a physical exam,” said Lawrence Purpura, MD, an infectious disease specialist and director of the long COVID clinic at Columbia University Medical Center, New York. “It’s a complicated disease that can impact every organ system of the body.”
Even so, emerging research has identified a checklist of sorts that doctors should consider when a patient seeks care for what appears to be long COVID. Among them: the key systems and organs impacted by the disease, the most common symptoms, useful therapeutic options for symptom management that have been found to help people with long COVID, and the best healthy lifestyle choices that doctors can recommend to help their patients
Here’s a closer look at each of these aspects, based on research and interviews with experts, patients, and doctors.
Key systems, organs impacted
About 10% of people who are infected with COVID-19 go on to have long COVID, according to a recent study that Ms. McCorkell helped coauthor. But more than 3 years into the pandemic, much about the condition is still a mystery.
COVID is a unique virus because it can spread far and wide in a patient’s body. A December 2022 study, published in Nature, autopsied 44 people who died of COVID and found that the virus could spread throughout the body and persist, in one case as long as 230 days after symptoms started.
“We know that there are dozens of symptoms across multiple organ systems,” said Ms. McCorkell. “That makes it harder for a primary care physician to connect the dots and associate it with COVID.”
A paper published in Nature Medicine proposed one way to help guide diagnosis. It divided symptoms into four groups:
- Cardiac and renal issues such as heart palpitations, chest pain, and kidney damage
- Sleep and anxiety problems like insomnia, waking up in the middle of the night, and anxiety
- In the musculoskeletal and nervous systems: musculoskeletal pain, osteoarthritis, and problems with mental skills
- In the digestive and respiratory systems: trouble breathing, asthma, stomach pain, nausea, and vomiting
There were also specific patterns in these groups. People in the first group were more likely to be older, male, have other conditions and to have been infected during the first wave of the COVID pandemic. People in the second group were over 60% female, and were more likely to have had previous allergies or asthma. The third group was also about 60% female, and many of them already had autoimmune conditions such as rheumatoid arthritis. Members of the fourth group – also 60% female – were the least likely of all the groups to have another condition.
This research is helpful, because it gives doctors a better sense of what conditions might make a patient more likely to get long COVID, as well as specific symptoms to look out for, said Steven Flanagan, MD, a physical medicine and rehabilitation specialist at New York University Langone Medical Center who also specializes in treating patients with long COVID.
But the “challenge there, though, for health care providers is that not everyone will fall neatly into one of these categories,” he stressed.
Checklist of symptoms
Although long COVID can be confusing, doctors say there are several symptoms that appear consistently that primary care providers should look out for, that could flag long COVID.
Postexertional malaise (PEM). This is different from simply feeling tired. “This term is often conflated with fatigue, but it’s very different,” said David Putrino, PhD, director of rehabilitation innovation at the Mount Sinai Health System in New York, who says that he sees it in about 90% of patients who come to his long COVID clinic.
PEM is the worsening of symptoms after physical or mental exertion. This usually occurs a day or 2 after the activity, but it can last for days, and sometimes weeks.
“It’s very different from fatigue, which is just a generalized tiredness, and exercise intolerance, where someone complains of not being able to do their usual workout on the treadmill,” he noted. “People with PEM are able to push through and do what they need to do, and then are hit with symptoms anywhere from 12 to 72 hours later.”
Dysautonomia. This is an umbrella term used to describe a dysfunction of the autonomic nervous system, which regulates bodily functions that you can’t control, like your blood pressure, heart rate, and breathing. This can cause symptoms such as heart palpitations, along with orthostatic intolerance, which means you can’t stand up for long without feeling faint or dizzy.
“In my practice, about 80% of patients meet criteria for dysautonomia,” said Dr. Putrino. Other research has found that it’s present in about two-thirds of long COVID patients.
One relatively easy way primary care providers can diagnose dysautonomia is to do the tilt table test. This helps check for postural orthostatic tachycardia syndrome (POTS), one of the most common forms of dysautonomia. During this exam, the patient lies flat on a table. As the head of the table is raised to an almost upright position, their heart rate and blood pressure are measured. Signs of POTS include an abnormal heart rate when you’re upright, as well as a worsening of symptoms.
Exercise intolerance. A review published in the journal JAMA Network Open analyzed 38 studies on long COVID and exercise and found that patients with the condition had a much harder time doing physical activity. Exercise capacity was reduced to levels that would be expected about a decade later in life, according to study authors.
“This is especially important because it can’t be explained just by deconditioning,” said Dr. Purpura. “Sometimes these patients are encouraged to ramp up exercise as a way to help with symptoms, but in these cases, encouraging them to push through can cause postexertional malaise, which sets patients back and delays recovery.”
While long COVID can cause dozens of symptoms, a paper Ms. McCorkell coauthored zeroed in on some of the most common ones: chest pain, heart palpitations, coughing, shortness of breath, belly pain, nausea, problems with mental skills, fatigue, disordered sleep, memory loss, ringing in the ears (tinnitus), erectile dysfunction, irregular menstruation, and worsened premenstrual syndrome.
While most primary care providers are familiar with some of these long COVID symptoms, they may not be aware of others.
“COVID itself seems to cause hormonal changes that can lead to erection and menstrual cycle problems,” explained Dr. Putrino. “But these may not be picked up in a visit if the patient is complaining of other signs of long COVID.”
It’s not just what symptoms are, but when they began to occur, he added. “Usually, these symptoms either start with the initial COVID infection, or begin sometime within 3 months after the acute COVID infection. That’s why it’s important for people with COVID to take notice of anything unusual that crops up within a month or 2 after getting sick.”
Can you prevent long COVID?
You can’t, but one of the best ways to reduce your risk is to get vaccinated. Getting at least one dose of a COVID vaccine before you test positive for COVID lowers your risk of long COVID by about 35% according to a study published in Antimicrobial Stewardship & Healthcare Epidemiology. Unvaccinated people who recovered from COVID, and then got a vaccine, lowered their own long COVID risk by 27%.
In addition, a study published in JAMA Internal Medicine found that women who were infected with COVID were less likely to go on to get long COVID and/or have less debilitating symptoms if they had a healthy lifestyle, which included the following: a healthy weight (a body mass index between 18.5 and 24.7 kg/m2), never-smoker, moderate alcohol consumption, a high-quality diet, 7-9 hours of sleep a night, and at least 150 minutes per week of physical activity
But Ms. McCorkell noted that she herself had a healthy preinfection lifestyle but got long COVID anyway, suggesting these approaches don’t work for everyone.
“I think one reason my symptoms weren’t addressed by primary care physicians for so long is because they looked at me and saw that I was young and healthy, so they dismissed my reports as being all in my head,” she explained. “But we know now anyone can get long COVID, regardless of age, health status, or disease severity. That’s why it’s so important that primary care physicians be able to recognize symptoms.”
A version of this article first appeared on WebMD.com.
Lisa McCorkell had a mild bout of COVID-19 in March 2020. Young and healthy, she assumed that she would bounce back quickly. But when her fatigue, shortness of breath, and brain fog persisted, she realized that she most likely had long COVID.
“Back then, we as patients basically coined the term,” she said. While her first primary care provider was sympathetic, they were unsure how to treat her. After her insurance changed, she ended up with a second primary care provider who didn’t take her symptoms seriously. “They dismissed my complaints and told me they were all in my head. I didn’t seek care for a while after that.”
Ms. McCorkell’s symptoms improved after her first COVID vaccine in the spring of 2021. She also finally found a new primary care doctor she could trust. But as one of the founders of the Patient-Led Research Collaborative, a group of researchers who study long COVID, she said many doctors still don’t know the hallmark symptoms of the condition or how to treat it.
“There’s still a lack of education on what long COVID is, and the symptoms associated with it,” she said. “Many of the symptoms that occur in long COVID are symptoms of other chronic conditions, such as chronic fatigue syndrome, that are often dismissed. And even if providers believe patients and send them for a workup, many of the routine blood and imaging tests come back normal.”
The term “long COVID” emerged in May 2020. And though the condition was recognized within a few months of the start of the pandemic, doctors weren’t sure how to screen or treat it.
While knowledge has developed since then, primary care doctors are still in a tough spot. They’re often the first providers that patients turn to when they have symptoms of long COVID.
“There’s no clear algorithm to pick up long COVID – there are no definite blood tests or biomarkers, or specific things to look for on a physical exam,” said Lawrence Purpura, MD, an infectious disease specialist and director of the long COVID clinic at Columbia University Medical Center, New York. “It’s a complicated disease that can impact every organ system of the body.”
Even so, emerging research has identified a checklist of sorts that doctors should consider when a patient seeks care for what appears to be long COVID. Among them: the key systems and organs impacted by the disease, the most common symptoms, useful therapeutic options for symptom management that have been found to help people with long COVID, and the best healthy lifestyle choices that doctors can recommend to help their patients
Here’s a closer look at each of these aspects, based on research and interviews with experts, patients, and doctors.
Key systems, organs impacted
About 10% of people who are infected with COVID-19 go on to have long COVID, according to a recent study that Ms. McCorkell helped coauthor. But more than 3 years into the pandemic, much about the condition is still a mystery.
COVID is a unique virus because it can spread far and wide in a patient’s body. A December 2022 study, published in Nature, autopsied 44 people who died of COVID and found that the virus could spread throughout the body and persist, in one case as long as 230 days after symptoms started.
“We know that there are dozens of symptoms across multiple organ systems,” said Ms. McCorkell. “That makes it harder for a primary care physician to connect the dots and associate it with COVID.”
A paper published in Nature Medicine proposed one way to help guide diagnosis. It divided symptoms into four groups:
- Cardiac and renal issues such as heart palpitations, chest pain, and kidney damage
- Sleep and anxiety problems like insomnia, waking up in the middle of the night, and anxiety
- In the musculoskeletal and nervous systems: musculoskeletal pain, osteoarthritis, and problems with mental skills
- In the digestive and respiratory systems: trouble breathing, asthma, stomach pain, nausea, and vomiting
There were also specific patterns in these groups. People in the first group were more likely to be older, male, have other conditions and to have been infected during the first wave of the COVID pandemic. People in the second group were over 60% female, and were more likely to have had previous allergies or asthma. The third group was also about 60% female, and many of them already had autoimmune conditions such as rheumatoid arthritis. Members of the fourth group – also 60% female – were the least likely of all the groups to have another condition.
This research is helpful, because it gives doctors a better sense of what conditions might make a patient more likely to get long COVID, as well as specific symptoms to look out for, said Steven Flanagan, MD, a physical medicine and rehabilitation specialist at New York University Langone Medical Center who also specializes in treating patients with long COVID.
But the “challenge there, though, for health care providers is that not everyone will fall neatly into one of these categories,” he stressed.
Checklist of symptoms
Although long COVID can be confusing, doctors say there are several symptoms that appear consistently that primary care providers should look out for, that could flag long COVID.
Postexertional malaise (PEM). This is different from simply feeling tired. “This term is often conflated with fatigue, but it’s very different,” said David Putrino, PhD, director of rehabilitation innovation at the Mount Sinai Health System in New York, who says that he sees it in about 90% of patients who come to his long COVID clinic.
PEM is the worsening of symptoms after physical or mental exertion. This usually occurs a day or 2 after the activity, but it can last for days, and sometimes weeks.
“It’s very different from fatigue, which is just a generalized tiredness, and exercise intolerance, where someone complains of not being able to do their usual workout on the treadmill,” he noted. “People with PEM are able to push through and do what they need to do, and then are hit with symptoms anywhere from 12 to 72 hours later.”
Dysautonomia. This is an umbrella term used to describe a dysfunction of the autonomic nervous system, which regulates bodily functions that you can’t control, like your blood pressure, heart rate, and breathing. This can cause symptoms such as heart palpitations, along with orthostatic intolerance, which means you can’t stand up for long without feeling faint or dizzy.
“In my practice, about 80% of patients meet criteria for dysautonomia,” said Dr. Putrino. Other research has found that it’s present in about two-thirds of long COVID patients.
One relatively easy way primary care providers can diagnose dysautonomia is to do the tilt table test. This helps check for postural orthostatic tachycardia syndrome (POTS), one of the most common forms of dysautonomia. During this exam, the patient lies flat on a table. As the head of the table is raised to an almost upright position, their heart rate and blood pressure are measured. Signs of POTS include an abnormal heart rate when you’re upright, as well as a worsening of symptoms.
Exercise intolerance. A review published in the journal JAMA Network Open analyzed 38 studies on long COVID and exercise and found that patients with the condition had a much harder time doing physical activity. Exercise capacity was reduced to levels that would be expected about a decade later in life, according to study authors.
“This is especially important because it can’t be explained just by deconditioning,” said Dr. Purpura. “Sometimes these patients are encouraged to ramp up exercise as a way to help with symptoms, but in these cases, encouraging them to push through can cause postexertional malaise, which sets patients back and delays recovery.”
While long COVID can cause dozens of symptoms, a paper Ms. McCorkell coauthored zeroed in on some of the most common ones: chest pain, heart palpitations, coughing, shortness of breath, belly pain, nausea, problems with mental skills, fatigue, disordered sleep, memory loss, ringing in the ears (tinnitus), erectile dysfunction, irregular menstruation, and worsened premenstrual syndrome.
While most primary care providers are familiar with some of these long COVID symptoms, they may not be aware of others.
“COVID itself seems to cause hormonal changes that can lead to erection and menstrual cycle problems,” explained Dr. Putrino. “But these may not be picked up in a visit if the patient is complaining of other signs of long COVID.”
It’s not just what symptoms are, but when they began to occur, he added. “Usually, these symptoms either start with the initial COVID infection, or begin sometime within 3 months after the acute COVID infection. That’s why it’s important for people with COVID to take notice of anything unusual that crops up within a month or 2 after getting sick.”
Can you prevent long COVID?
You can’t, but one of the best ways to reduce your risk is to get vaccinated. Getting at least one dose of a COVID vaccine before you test positive for COVID lowers your risk of long COVID by about 35% according to a study published in Antimicrobial Stewardship & Healthcare Epidemiology. Unvaccinated people who recovered from COVID, and then got a vaccine, lowered their own long COVID risk by 27%.
In addition, a study published in JAMA Internal Medicine found that women who were infected with COVID were less likely to go on to get long COVID and/or have less debilitating symptoms if they had a healthy lifestyle, which included the following: a healthy weight (a body mass index between 18.5 and 24.7 kg/m2), never-smoker, moderate alcohol consumption, a high-quality diet, 7-9 hours of sleep a night, and at least 150 minutes per week of physical activity
But Ms. McCorkell noted that she herself had a healthy preinfection lifestyle but got long COVID anyway, suggesting these approaches don’t work for everyone.
“I think one reason my symptoms weren’t addressed by primary care physicians for so long is because they looked at me and saw that I was young and healthy, so they dismissed my reports as being all in my head,” she explained. “But we know now anyone can get long COVID, regardless of age, health status, or disease severity. That’s why it’s so important that primary care physicians be able to recognize symptoms.”
A version of this article first appeared on WebMD.com.
Too high: Can you ID pot-induced psychosis?
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
Clozapine may curb schizophrenia’s ‘most dreaded outcome’
Investigators reviewed over 53,000 autopsy records, including over 600 from individuals whose autopsies revealed the presence of the antipsychotics clozapine or olanzapine, and found that those who took clozapine were significantly less likely to have died by suicide, compared with their counterparts who were taking olanzapine.
“Clozapine is an important and effective antisuicide medicine and should be strongly considered for treatment-resistant psychotic disorders, especially when the patient may be at risk for suicide,” study investigator Paul Nestadt, MD, associate professor, department of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, told this news organization.
The study was published online in The Journal of Clinical Psychiatry.
Underutilized medication
Clozapine is the only medication indicated for treatment-resistant schizophrenia and is considered “the most efficacious antipsychotic,” the investigators note. Unfortunately, it has “long been underutilized” for several reasons, including prescriber hesitancy and concerns about side effects.
The authors note that its mechanism of action and the basis for superior efficacy are “still poorly understood” but “may extend beyond neurotransmitter receptor binding.”
Importantly, it may have a beneficial impact on domains other than positive symptoms of schizophrenia, including suicidality. Several studies have shown that it’s beneficial in this regard, but it is “unclear whether the unique antisuicidal properties of clozapine are related to better symptom control ... or to the closer monitoring and follow-up mandated for clozapine use,” they note.
A previous trial, the International Suicide Prevention Trial (InterSePT), demonstrated that clozapine is associated with a greater reduction in suicidality, and the findings “led to an FDA indication for clozapine in reducing the risk of recurrent suicidal behavior.”
However, the authors note, “in the severely ill populations in these studies, it is difficult to be certain about patients’ adherence to prescribed clozapine.”
“Other studies, such as InterSePT, have shown some evidence of clozapine working to reduce suicide-related outcomes, such as attempts or suicidal ideation, but few have been sufficiently powered to measure an effect on actual suicide deaths,” said Dr. Nestadt.
“As a suicidologist, I feel it is very important that we understand what treatments and interventions can actually prevent suicide deaths, as most suicides are not associated with past attempts or ideation, with suicide decedents usually looking very different from characteristic nonfatal attempters, from a clinical or epidemiological standpoint,” he added.
“If we could show that clozapine actually decreases the likelihood of suicide deaths in our patients, it gives us more reason to choose it over less effective neuroleptics in our clinics – especially for patients at high risk of suicide,” he said.
For the study, the researchers reviewed 19-year state-wide autopsy records of Maryland’s Office of the Chief Medical Examiner, which “performs uniquely comprehensive death investigations.” Data included in these investigations are full toxicologic panels with postmortem blood levels of antipsychotics.
The researchers compared decedents who tested positive for clozapine and decedents who tested positive for olanzapine. They evaluated demographics, clinical features, and manner-of-death outcomes.
‘Untapped resource’
Of 53,133 decedents, olanzapine or clozapine was detected in the blood of 621 persons (n = 571 and n = 50, respectively).
There were no significant differences in age, sex, race, or urban residence between the decedents who were treated with olanzapine and those who received clozapine.
The odds of a death by suicide in those treated with clozapine were less than half of the odds among decedents who had been treated with olanzapine (odds ratio, 0.47; 95% confidence interval, 0.26-0.84; P = .011).
In sensitivity analyses, the investigators reanalyzed the data to compare clozapine with other antipsychotics, including chlorpromazine, thioridazine, quetiapine, and olanzapine, and the results were similar. The odds of suicide (compared with accident) in those taking clozapine were much lower than in those taking any other tested antipsychotics individually or in combination (OR, 0.42; 95% CI, 0.24-0.73; P = .002).
Dr. Nestadt outlined several hypotheses regarding the mechanism of clozapine’s antisuicidal properties.
“Most theories stem from the differences in its receptor affinity, compared [with] the other neuroleptics,” he said. “In addition to the more typical dopaminergic blockade seen in neuroleptics, clozapine enhances serotonin release and greatly increases peripheral norepinephrine.”
This has been shown to “grant clozapine a greater antidepressant effect than other neuroleptics while also potentially decreasing aggression and impulsivity, which are both strongly associated with suicide risk,” he said.
Clozapine may also “work to reduce the inflammation-triggered activation of the kynurenine pathway, which otherwise contributes to serotonin depletion,” he added.
He noted that some studies have shown that as many as 1 in 10 patients with schizophrenia die by suicide, “so addressing this risk is paramount,” and that clozapine can play an important role in this.
The authors note that the findings “also highlight the utility of state-wide autopsy records, an untapped resource for investigating the potential protective effect of psychiatric medications on suicide at a population level.
“Importantly, we can be certain that this was not an issue of nonadherence to treatment in either group, which is a common issue in the use of these drugs because, instead of prescription records or self-report, we used actual measurements of drug presence in decedents’ blood at death,” said Dr. Nestadt.
‘Strongly suggestive’ data
Commenting on the study, Maria Oquendo, MD, PhD, Ruth Meltzer Professor and chair of psychiatry, Perelman School of Medicine, University of Pennsylvania, Philadelphia, said most work on antisuicidal psychopharmacologic approaches “focuses on suicidal ideation or suicide attempts, due to the rarity of suicide death, even in high-risk populations.”
“Showing that clozapine may decrease risk for the most dreaded outcome of schizophrenia – suicide – is critically important,” said Dr. Oquendo, past president of the American Psychiatric Association.
Nevertheless, some questions remain, said Dr. Oquendo, who was not involved with the study. “Comparison of suicides to only accidental deaths has limitations. Many individuals who die due to accidents, like many suicides, are not similar to the general population,” she added.
However, she acknowledged, the data are strongly suggestive that clozapine protects against suicide.
“While not definitive, ideally these findings will stimulate changes in prescribing practices which may be lifesaving both literally – in terms of preventing suicides – and figuratively, given the drug’s effect on symptoms that impact quality of life and functioning,” said Dr. Oquendo.
The study received no funding or support. Dr. Nestadt is supported by the American Foundation for Suicide prevention and the National Institute on Drug Abuse. The other authors’ disclosures are listed in the original article. Dr. Oquendo receives royalties from the Research Foundation for Mental Hygiene for the commercial use of the Columbia Suicide Severity Rating Scale. She serves as an advisor to Alkermes, Mind Medicine, Sage Therapeutics, St. George’s University, and Fundacion Jimenez Diaz. Her family owns stock in Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
Investigators reviewed over 53,000 autopsy records, including over 600 from individuals whose autopsies revealed the presence of the antipsychotics clozapine or olanzapine, and found that those who took clozapine were significantly less likely to have died by suicide, compared with their counterparts who were taking olanzapine.
“Clozapine is an important and effective antisuicide medicine and should be strongly considered for treatment-resistant psychotic disorders, especially when the patient may be at risk for suicide,” study investigator Paul Nestadt, MD, associate professor, department of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, told this news organization.
The study was published online in The Journal of Clinical Psychiatry.
Underutilized medication
Clozapine is the only medication indicated for treatment-resistant schizophrenia and is considered “the most efficacious antipsychotic,” the investigators note. Unfortunately, it has “long been underutilized” for several reasons, including prescriber hesitancy and concerns about side effects.
The authors note that its mechanism of action and the basis for superior efficacy are “still poorly understood” but “may extend beyond neurotransmitter receptor binding.”
Importantly, it may have a beneficial impact on domains other than positive symptoms of schizophrenia, including suicidality. Several studies have shown that it’s beneficial in this regard, but it is “unclear whether the unique antisuicidal properties of clozapine are related to better symptom control ... or to the closer monitoring and follow-up mandated for clozapine use,” they note.
A previous trial, the International Suicide Prevention Trial (InterSePT), demonstrated that clozapine is associated with a greater reduction in suicidality, and the findings “led to an FDA indication for clozapine in reducing the risk of recurrent suicidal behavior.”
However, the authors note, “in the severely ill populations in these studies, it is difficult to be certain about patients’ adherence to prescribed clozapine.”
“Other studies, such as InterSePT, have shown some evidence of clozapine working to reduce suicide-related outcomes, such as attempts or suicidal ideation, but few have been sufficiently powered to measure an effect on actual suicide deaths,” said Dr. Nestadt.
“As a suicidologist, I feel it is very important that we understand what treatments and interventions can actually prevent suicide deaths, as most suicides are not associated with past attempts or ideation, with suicide decedents usually looking very different from characteristic nonfatal attempters, from a clinical or epidemiological standpoint,” he added.
“If we could show that clozapine actually decreases the likelihood of suicide deaths in our patients, it gives us more reason to choose it over less effective neuroleptics in our clinics – especially for patients at high risk of suicide,” he said.
For the study, the researchers reviewed 19-year state-wide autopsy records of Maryland’s Office of the Chief Medical Examiner, which “performs uniquely comprehensive death investigations.” Data included in these investigations are full toxicologic panels with postmortem blood levels of antipsychotics.
The researchers compared decedents who tested positive for clozapine and decedents who tested positive for olanzapine. They evaluated demographics, clinical features, and manner-of-death outcomes.
‘Untapped resource’
Of 53,133 decedents, olanzapine or clozapine was detected in the blood of 621 persons (n = 571 and n = 50, respectively).
There were no significant differences in age, sex, race, or urban residence between the decedents who were treated with olanzapine and those who received clozapine.
The odds of a death by suicide in those treated with clozapine were less than half of the odds among decedents who had been treated with olanzapine (odds ratio, 0.47; 95% confidence interval, 0.26-0.84; P = .011).
In sensitivity analyses, the investigators reanalyzed the data to compare clozapine with other antipsychotics, including chlorpromazine, thioridazine, quetiapine, and olanzapine, and the results were similar. The odds of suicide (compared with accident) in those taking clozapine were much lower than in those taking any other tested antipsychotics individually or in combination (OR, 0.42; 95% CI, 0.24-0.73; P = .002).
Dr. Nestadt outlined several hypotheses regarding the mechanism of clozapine’s antisuicidal properties.
“Most theories stem from the differences in its receptor affinity, compared [with] the other neuroleptics,” he said. “In addition to the more typical dopaminergic blockade seen in neuroleptics, clozapine enhances serotonin release and greatly increases peripheral norepinephrine.”
This has been shown to “grant clozapine a greater antidepressant effect than other neuroleptics while also potentially decreasing aggression and impulsivity, which are both strongly associated with suicide risk,” he said.
Clozapine may also “work to reduce the inflammation-triggered activation of the kynurenine pathway, which otherwise contributes to serotonin depletion,” he added.
He noted that some studies have shown that as many as 1 in 10 patients with schizophrenia die by suicide, “so addressing this risk is paramount,” and that clozapine can play an important role in this.
The authors note that the findings “also highlight the utility of state-wide autopsy records, an untapped resource for investigating the potential protective effect of psychiatric medications on suicide at a population level.
“Importantly, we can be certain that this was not an issue of nonadherence to treatment in either group, which is a common issue in the use of these drugs because, instead of prescription records or self-report, we used actual measurements of drug presence in decedents’ blood at death,” said Dr. Nestadt.
‘Strongly suggestive’ data
Commenting on the study, Maria Oquendo, MD, PhD, Ruth Meltzer Professor and chair of psychiatry, Perelman School of Medicine, University of Pennsylvania, Philadelphia, said most work on antisuicidal psychopharmacologic approaches “focuses on suicidal ideation or suicide attempts, due to the rarity of suicide death, even in high-risk populations.”
“Showing that clozapine may decrease risk for the most dreaded outcome of schizophrenia – suicide – is critically important,” said Dr. Oquendo, past president of the American Psychiatric Association.
Nevertheless, some questions remain, said Dr. Oquendo, who was not involved with the study. “Comparison of suicides to only accidental deaths has limitations. Many individuals who die due to accidents, like many suicides, are not similar to the general population,” she added.
However, she acknowledged, the data are strongly suggestive that clozapine protects against suicide.
“While not definitive, ideally these findings will stimulate changes in prescribing practices which may be lifesaving both literally – in terms of preventing suicides – and figuratively, given the drug’s effect on symptoms that impact quality of life and functioning,” said Dr. Oquendo.
The study received no funding or support. Dr. Nestadt is supported by the American Foundation for Suicide prevention and the National Institute on Drug Abuse. The other authors’ disclosures are listed in the original article. Dr. Oquendo receives royalties from the Research Foundation for Mental Hygiene for the commercial use of the Columbia Suicide Severity Rating Scale. She serves as an advisor to Alkermes, Mind Medicine, Sage Therapeutics, St. George’s University, and Fundacion Jimenez Diaz. Her family owns stock in Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
Investigators reviewed over 53,000 autopsy records, including over 600 from individuals whose autopsies revealed the presence of the antipsychotics clozapine or olanzapine, and found that those who took clozapine were significantly less likely to have died by suicide, compared with their counterparts who were taking olanzapine.
“Clozapine is an important and effective antisuicide medicine and should be strongly considered for treatment-resistant psychotic disorders, especially when the patient may be at risk for suicide,” study investigator Paul Nestadt, MD, associate professor, department of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, told this news organization.
The study was published online in The Journal of Clinical Psychiatry.
Underutilized medication
Clozapine is the only medication indicated for treatment-resistant schizophrenia and is considered “the most efficacious antipsychotic,” the investigators note. Unfortunately, it has “long been underutilized” for several reasons, including prescriber hesitancy and concerns about side effects.
The authors note that its mechanism of action and the basis for superior efficacy are “still poorly understood” but “may extend beyond neurotransmitter receptor binding.”
Importantly, it may have a beneficial impact on domains other than positive symptoms of schizophrenia, including suicidality. Several studies have shown that it’s beneficial in this regard, but it is “unclear whether the unique antisuicidal properties of clozapine are related to better symptom control ... or to the closer monitoring and follow-up mandated for clozapine use,” they note.
A previous trial, the International Suicide Prevention Trial (InterSePT), demonstrated that clozapine is associated with a greater reduction in suicidality, and the findings “led to an FDA indication for clozapine in reducing the risk of recurrent suicidal behavior.”
However, the authors note, “in the severely ill populations in these studies, it is difficult to be certain about patients’ adherence to prescribed clozapine.”
“Other studies, such as InterSePT, have shown some evidence of clozapine working to reduce suicide-related outcomes, such as attempts or suicidal ideation, but few have been sufficiently powered to measure an effect on actual suicide deaths,” said Dr. Nestadt.
“As a suicidologist, I feel it is very important that we understand what treatments and interventions can actually prevent suicide deaths, as most suicides are not associated with past attempts or ideation, with suicide decedents usually looking very different from characteristic nonfatal attempters, from a clinical or epidemiological standpoint,” he added.
“If we could show that clozapine actually decreases the likelihood of suicide deaths in our patients, it gives us more reason to choose it over less effective neuroleptics in our clinics – especially for patients at high risk of suicide,” he said.
For the study, the researchers reviewed 19-year state-wide autopsy records of Maryland’s Office of the Chief Medical Examiner, which “performs uniquely comprehensive death investigations.” Data included in these investigations are full toxicologic panels with postmortem blood levels of antipsychotics.
The researchers compared decedents who tested positive for clozapine and decedents who tested positive for olanzapine. They evaluated demographics, clinical features, and manner-of-death outcomes.
‘Untapped resource’
Of 53,133 decedents, olanzapine or clozapine was detected in the blood of 621 persons (n = 571 and n = 50, respectively).
There were no significant differences in age, sex, race, or urban residence between the decedents who were treated with olanzapine and those who received clozapine.
The odds of a death by suicide in those treated with clozapine were less than half of the odds among decedents who had been treated with olanzapine (odds ratio, 0.47; 95% confidence interval, 0.26-0.84; P = .011).
In sensitivity analyses, the investigators reanalyzed the data to compare clozapine with other antipsychotics, including chlorpromazine, thioridazine, quetiapine, and olanzapine, and the results were similar. The odds of suicide (compared with accident) in those taking clozapine were much lower than in those taking any other tested antipsychotics individually or in combination (OR, 0.42; 95% CI, 0.24-0.73; P = .002).
Dr. Nestadt outlined several hypotheses regarding the mechanism of clozapine’s antisuicidal properties.
“Most theories stem from the differences in its receptor affinity, compared [with] the other neuroleptics,” he said. “In addition to the more typical dopaminergic blockade seen in neuroleptics, clozapine enhances serotonin release and greatly increases peripheral norepinephrine.”
This has been shown to “grant clozapine a greater antidepressant effect than other neuroleptics while also potentially decreasing aggression and impulsivity, which are both strongly associated with suicide risk,” he said.
Clozapine may also “work to reduce the inflammation-triggered activation of the kynurenine pathway, which otherwise contributes to serotonin depletion,” he added.
He noted that some studies have shown that as many as 1 in 10 patients with schizophrenia die by suicide, “so addressing this risk is paramount,” and that clozapine can play an important role in this.
The authors note that the findings “also highlight the utility of state-wide autopsy records, an untapped resource for investigating the potential protective effect of psychiatric medications on suicide at a population level.
“Importantly, we can be certain that this was not an issue of nonadherence to treatment in either group, which is a common issue in the use of these drugs because, instead of prescription records or self-report, we used actual measurements of drug presence in decedents’ blood at death,” said Dr. Nestadt.
‘Strongly suggestive’ data
Commenting on the study, Maria Oquendo, MD, PhD, Ruth Meltzer Professor and chair of psychiatry, Perelman School of Medicine, University of Pennsylvania, Philadelphia, said most work on antisuicidal psychopharmacologic approaches “focuses on suicidal ideation or suicide attempts, due to the rarity of suicide death, even in high-risk populations.”
“Showing that clozapine may decrease risk for the most dreaded outcome of schizophrenia – suicide – is critically important,” said Dr. Oquendo, past president of the American Psychiatric Association.
Nevertheless, some questions remain, said Dr. Oquendo, who was not involved with the study. “Comparison of suicides to only accidental deaths has limitations. Many individuals who die due to accidents, like many suicides, are not similar to the general population,” she added.
However, she acknowledged, the data are strongly suggestive that clozapine protects against suicide.
“While not definitive, ideally these findings will stimulate changes in prescribing practices which may be lifesaving both literally – in terms of preventing suicides – and figuratively, given the drug’s effect on symptoms that impact quality of life and functioning,” said Dr. Oquendo.
The study received no funding or support. Dr. Nestadt is supported by the American Foundation for Suicide prevention and the National Institute on Drug Abuse. The other authors’ disclosures are listed in the original article. Dr. Oquendo receives royalties from the Research Foundation for Mental Hygiene for the commercial use of the Columbia Suicide Severity Rating Scale. She serves as an advisor to Alkermes, Mind Medicine, Sage Therapeutics, St. George’s University, and Fundacion Jimenez Diaz. Her family owns stock in Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
Low-dose olanzapine improves appetite in chemotherapy patients
Anorexia is a problem in approximately 50% of newly-diagnosed cancer patients, and can compromise survival, wrote study author Lakshmi Sandhya, MD, of Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India, and colleagues. In particular, patients with lung and gastrointestinal tract cancers are prone to anorexia during chemotherapy, they said. Olanzapine is a demonstrated appetite stimulant and has been used in cancer patients as a short-term antiemetic, but its use for long-term appetite stimulation has not been well-studied, they said.
In the study, published in the Journal of Clinical Oncology, the researchers randomized 124 adults aged 18 years and older to a 2.5 grams of olanzapine or placebo for 12 weeks. The participants had untreated, locally advanced, or metastatic gastric, hepatopancreaticobiliary (HPB), or lung cancers.
The median age of the participants was 55 years. The primary outcome was a weight gain greater than 5% and improved appetite based on the visual analog scale (VAS) and questionnaires. A change in nutritional status, quality of life (QOL), and chemotherapy toxicity, were secondary endpoints.
After 12 weeks, complete data were available for 58 patients in the olanzapine group and 54 in the placebo group. Of these, 60% of the olanzapine group and 9% of the placebo group met the primary endpoint of a weight gain greater than 5%. The proportion of patients with improved appetite based on VAS scores and questionnaire scores was significantly higher in olanzapine patients vs. placebo patients (43% vs. 13% and 22% vs. 4%, respectively).
In addition, 52% of the olanzapine group vs. 18% of the placebo group achieved more than 75% intake of recommended daily calories.
Most of the reported toxicities were not hematological and similar between the groups (85% for olanzapine vs. 88% for placebo). The proportion of patients with toxicities of grade 3 or higher was lower in the olanzapine group vs. the placebo group (12% vs. 37%, P = .002). Patients in the olanzapine group also reported significantly improved quality of life from baseline compared to the placebo patients.
The findings were limited by several factors including the heterogeneous cancers and treatment regimens, the lack of data on weight beyond 12 weeks, the relatively small study population, and the subjective nature of anorexia measurements, the researchers noted.
However, the results suggest that low-dose olanzapine is an effective and well-tolerated add-on intervention for the subset of patients at risk for anorexia at the start of chemotherapy, they said.
“Future studies could look at various cancers in a multicentric setting and long-term endpoints such as patient survival,” they concluded.
The study drug and placebo were funded by an intramural grant from Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER). The researchers had no financial conflicts to disclose.
Anorexia is a problem in approximately 50% of newly-diagnosed cancer patients, and can compromise survival, wrote study author Lakshmi Sandhya, MD, of Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India, and colleagues. In particular, patients with lung and gastrointestinal tract cancers are prone to anorexia during chemotherapy, they said. Olanzapine is a demonstrated appetite stimulant and has been used in cancer patients as a short-term antiemetic, but its use for long-term appetite stimulation has not been well-studied, they said.
In the study, published in the Journal of Clinical Oncology, the researchers randomized 124 adults aged 18 years and older to a 2.5 grams of olanzapine or placebo for 12 weeks. The participants had untreated, locally advanced, or metastatic gastric, hepatopancreaticobiliary (HPB), or lung cancers.
The median age of the participants was 55 years. The primary outcome was a weight gain greater than 5% and improved appetite based on the visual analog scale (VAS) and questionnaires. A change in nutritional status, quality of life (QOL), and chemotherapy toxicity, were secondary endpoints.
After 12 weeks, complete data were available for 58 patients in the olanzapine group and 54 in the placebo group. Of these, 60% of the olanzapine group and 9% of the placebo group met the primary endpoint of a weight gain greater than 5%. The proportion of patients with improved appetite based on VAS scores and questionnaire scores was significantly higher in olanzapine patients vs. placebo patients (43% vs. 13% and 22% vs. 4%, respectively).
In addition, 52% of the olanzapine group vs. 18% of the placebo group achieved more than 75% intake of recommended daily calories.
Most of the reported toxicities were not hematological and similar between the groups (85% for olanzapine vs. 88% for placebo). The proportion of patients with toxicities of grade 3 or higher was lower in the olanzapine group vs. the placebo group (12% vs. 37%, P = .002). Patients in the olanzapine group also reported significantly improved quality of life from baseline compared to the placebo patients.
The findings were limited by several factors including the heterogeneous cancers and treatment regimens, the lack of data on weight beyond 12 weeks, the relatively small study population, and the subjective nature of anorexia measurements, the researchers noted.
However, the results suggest that low-dose olanzapine is an effective and well-tolerated add-on intervention for the subset of patients at risk for anorexia at the start of chemotherapy, they said.
“Future studies could look at various cancers in a multicentric setting and long-term endpoints such as patient survival,” they concluded.
The study drug and placebo were funded by an intramural grant from Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER). The researchers had no financial conflicts to disclose.
Anorexia is a problem in approximately 50% of newly-diagnosed cancer patients, and can compromise survival, wrote study author Lakshmi Sandhya, MD, of Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India, and colleagues. In particular, patients with lung and gastrointestinal tract cancers are prone to anorexia during chemotherapy, they said. Olanzapine is a demonstrated appetite stimulant and has been used in cancer patients as a short-term antiemetic, but its use for long-term appetite stimulation has not been well-studied, they said.
In the study, published in the Journal of Clinical Oncology, the researchers randomized 124 adults aged 18 years and older to a 2.5 grams of olanzapine or placebo for 12 weeks. The participants had untreated, locally advanced, or metastatic gastric, hepatopancreaticobiliary (HPB), or lung cancers.
The median age of the participants was 55 years. The primary outcome was a weight gain greater than 5% and improved appetite based on the visual analog scale (VAS) and questionnaires. A change in nutritional status, quality of life (QOL), and chemotherapy toxicity, were secondary endpoints.
After 12 weeks, complete data were available for 58 patients in the olanzapine group and 54 in the placebo group. Of these, 60% of the olanzapine group and 9% of the placebo group met the primary endpoint of a weight gain greater than 5%. The proportion of patients with improved appetite based on VAS scores and questionnaire scores was significantly higher in olanzapine patients vs. placebo patients (43% vs. 13% and 22% vs. 4%, respectively).
In addition, 52% of the olanzapine group vs. 18% of the placebo group achieved more than 75% intake of recommended daily calories.
Most of the reported toxicities were not hematological and similar between the groups (85% for olanzapine vs. 88% for placebo). The proportion of patients with toxicities of grade 3 or higher was lower in the olanzapine group vs. the placebo group (12% vs. 37%, P = .002). Patients in the olanzapine group also reported significantly improved quality of life from baseline compared to the placebo patients.
The findings were limited by several factors including the heterogeneous cancers and treatment regimens, the lack of data on weight beyond 12 weeks, the relatively small study population, and the subjective nature of anorexia measurements, the researchers noted.
However, the results suggest that low-dose olanzapine is an effective and well-tolerated add-on intervention for the subset of patients at risk for anorexia at the start of chemotherapy, they said.
“Future studies could look at various cancers in a multicentric setting and long-term endpoints such as patient survival,” they concluded.
The study drug and placebo were funded by an intramural grant from Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER). The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Parkinson’s disease: What’s trauma got to do with it?
This transcript has been edited for clarity.
Kathrin LaFaver, MD: Hello. I’m happy to talk today to Dr. Indu Subramanian, clinical professor at University of California, Los Angeles, and director of the Parkinson’s Disease Research, Education and Clinical Center in Los Angeles. I am a neurologist in Saratoga Springs, New York, and we will be talking today about Indu’s new paper on childhood trauma and Parkinson’s disease. Welcome and thanks for taking the time.
Indu Subramanian, MD: Thank you so much for letting us highlight this important topic.
Dr. LaFaver: There are many papers published every month on Parkinson’s disease, but this topic stands out because it’s not a thing that has been commonly looked at. What gave you the idea to study this?
Neurology behind other specialties
Dr. Subramanian: Kathrin, you and I have been looking at things that can inform us about our patients – the person who’s standing in front of us when they come in and we’re giving them this diagnosis. I think that so much of what we’ve done [in the past] is a cookie cutter approach to giving everybody the standard treatment. [We’ve been assuming that] It doesn’t matter if they’re a man or woman. It doesn’t matter if they’re a veteran. It doesn’t matter if they may be from a minoritized population.
We’ve also been interested in approaches that are outside the box, right? We have this integrative medicine and lifestyle medicine background. I’ve been going to those meetings and really been struck by the mounting evidence on the importance of things like early adverse childhood events (ACEs), what zip code you live in, what your pollution index is, and how these things can affect people through their life and their health.
I think that it is high time neurologists pay attention to this. There’s been mounting evidence throughout many disease states, various types of cancers, and mental health. Cardiology is much more advanced, but we haven’t had much data in neurology. In fact, when we went to write this paper, there were just one or two papers that were looking at multiple sclerosis or general neurologic issues, but really nothing in Parkinson’s disease.
We know that Parkinson’s disease is not only a motor disease that affects mental health, but that it also affects nonmotor issues. Childhood adversity may affect how people progress or how quickly they may get a disease, and we were interested in how it may manifest in a disease like Parkinson’s disease.
That was the framework going to meetings. As we wrote this paper and were in various editing stages, there was a beautiful paper that came out by Nadine Burke Harris and team that really was a call to action for neurologists and caring about trauma.
Dr. LaFaver: I couldn’t agree more. It’s really an underrecognized issue. With my own background, being very interested in functional movement disorders, psychosomatic disorders, and so on, it becomes much more evident how common a trauma background is, not only for people we were traditionally asking about.
Why don’t you summarize your findings for us?
Adverse childhood events
Dr. Subramanian: This is a web-based survey, so obviously, these are patient self-reports of their disease. We have a large cohort of people that we’ve been following over 7 years. I’m looking at modifiable variables and what really impacts Parkinson’s disease. Some of our previous papers have looked at diet, exercise, and loneliness. This is the same cohort.
We ended up putting the ACEs questionnaire, which is 10 questions looking at whether you were exposed to certain things in your household below the age of 18. This is a relatively standard questionnaire that’s administered one time, and you get a score out of 10. This is something that has been pushed, at least in the state of California, as something that we should be checking more in all people coming in.
We introduced the survey, and we didn’t force everyone to take it. Unfortunately, there was 20% or so of our patients who chose not to answer these questions. One has to ask, who are those people that didn’t answer the questions? Are they the ones that may have had trauma and these questions were triggering? It was a gap. We didn’t add extra questions to explore why people didn’t answer those questions.
We have to also put this in context. We have a patient population that’s largely quite affluent, who are able to access web-based surveys through their computer, and largely Caucasian; there are not many minoritized populations in our cohort. We want to do better with that. We actually were able to gather a decent number of women. We represent women quite well in our survey. I think that’s because of this online approach and some of the things that we’re studying.
In our survey, we broke it down into people who had no ACEs, one to three ACEs, or four or more ACEs. This is a standard way to break down ACEs so that we’re able to categorize what to do with these patient populations.
What we saw – and it’s preliminary evidence – is that people who had higher ACE scores seemed to have more symptom severity when we controlled for things like years since diagnosis, age, and gender. They also seem to have a worse quality of life. There was some indication that there were more nonmotor issues in those populations, as you might expect, such as anxiety, depression, and things that presumably ACEs can affect separately.
There are some confounders, but I think we really want to use this as the first piece of evidence to hopefully pave the way for caring about trauma in Parkinson’s disease moving forward.
Dr. LaFaver: Thank you so much for that summary. You already mentioned the main methodology you used.
What is the next step for you? How do you see these findings informing our clinical care? Do you have suggestions for all of the neurologists listening in this regard?
PD not yet considered ACE-related
Dr. Subramanian: Dr. Burke Harris was the former surgeon general in California. She’s a woman of color and a brilliant speaker, and she had worked in inner cities, I think in San Francisco, with pediatric populations, seeing these effects of adversity in that time frame.
You see this population at risk, and then you’re following this cohort, which we knew from the Kaiser cohort determines earlier morbidity and mortality across a number of disease states. We’re seeing things like more heart attacks, more diabetes, and all kinds of things in these populations. This is not new news; we just have not been focusing on this.
In her paper, this call to action, they had talked about some ACE-related conditions that currently do not include Parkinson’s disease. There are three ACE-related neurologic conditions that people should be aware of. One is in the headache/pain universe. Another is in the stroke universe, and that’s understandable, given cardiovascular risk factors . Then the third is in this dementia risk category. I think Parkinson’s disease, as we know, can be associated with dementia. A large percentage of our patients get dementia, but we don’t have Parkinson’s disease called out in this framework.
What people are talking about is if you have no ACEs or are in this middle category of one to three ACEs and you don’t have an ACE-related diagnosis – which Parkinson’s disease is not currently – we just give some basic counseling about the importance of lifestyle. I think we would love to see that anyway. They’re talking about things like exercise, diet, sleep, social connection, getting out in nature, things like that, so just general counseling on the importance of that.
Then if you’re in this higher-risk category, and so with these ACE-related neurologic conditions, including dementia, headache, and stroke, if you had this middle range of one to three ACEs, they’re getting additional resources. Some of them may be referred for social work help or mental health support and things like that.
I’d really love to see that happening in Parkinson’s disease, because I think we have so many needs in our population. I’m always hoping to advocate for more mental health needs that are scarce and resources in the social support realm because I believe that social connection and social support is a huge buffer for this trauma.
ACEs are just one type of trauma. I take care of veterans in the Veterans [Affairs Department]. We have some information now coming out about posttraumatic stress disorder, predisposing to certain things in Parkinson’s disease, possibly head injury, and things like that. I think we have populations at risk that we can hopefully screen at intake, and I’m really pushing for that.
Maybe it’s not the neurologist that does this intake. It might be someone else on the team that can spend some time doing these questionnaires and understand if your patient has a high ACE score. Unless you ask, many patients don’t necessarily come forward to talk about this. I really am pushing for trying to screen and trying to advocate for more research in this area so that we can classify Parkinson’s disease as an ACE-related condition and thus give more resources from the mental health world, and also the social support world, to our patients.
Dr. LaFaver: Thank you. There are many important points, and I think it’s a very important thing to recognize that it may not be only trauma in childhood but also throughout life, as you said, and might really influence nonmotor symptoms of Parkinson’s disease in particular, including anxiety and pain, which are often difficult to treat.
I think there’s much more to do in research, advocacy, and education. We’re going to educate patients about this, and also educate other neurologists and providers. I think you mentioned that trauma-informed care is getting its spotlight in primary care and other specialties. I think we have catching up to do in neurology, and I think this is a really important work toward that goal.
Thank you so much for your work and for taking the time to share your thoughts. I hope to talk to you again soon.
Dr. Subramanian: Thank you so much, Kathrin.
Dr. LaFaver has disclosed no relevant financial relationships. Dr. Subramanian disclosed ties with Acorda Therapeutics.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Kathrin LaFaver, MD: Hello. I’m happy to talk today to Dr. Indu Subramanian, clinical professor at University of California, Los Angeles, and director of the Parkinson’s Disease Research, Education and Clinical Center in Los Angeles. I am a neurologist in Saratoga Springs, New York, and we will be talking today about Indu’s new paper on childhood trauma and Parkinson’s disease. Welcome and thanks for taking the time.
Indu Subramanian, MD: Thank you so much for letting us highlight this important topic.
Dr. LaFaver: There are many papers published every month on Parkinson’s disease, but this topic stands out because it’s not a thing that has been commonly looked at. What gave you the idea to study this?
Neurology behind other specialties
Dr. Subramanian: Kathrin, you and I have been looking at things that can inform us about our patients – the person who’s standing in front of us when they come in and we’re giving them this diagnosis. I think that so much of what we’ve done [in the past] is a cookie cutter approach to giving everybody the standard treatment. [We’ve been assuming that] It doesn’t matter if they’re a man or woman. It doesn’t matter if they’re a veteran. It doesn’t matter if they may be from a minoritized population.
We’ve also been interested in approaches that are outside the box, right? We have this integrative medicine and lifestyle medicine background. I’ve been going to those meetings and really been struck by the mounting evidence on the importance of things like early adverse childhood events (ACEs), what zip code you live in, what your pollution index is, and how these things can affect people through their life and their health.
I think that it is high time neurologists pay attention to this. There’s been mounting evidence throughout many disease states, various types of cancers, and mental health. Cardiology is much more advanced, but we haven’t had much data in neurology. In fact, when we went to write this paper, there were just one or two papers that were looking at multiple sclerosis or general neurologic issues, but really nothing in Parkinson’s disease.
We know that Parkinson’s disease is not only a motor disease that affects mental health, but that it also affects nonmotor issues. Childhood adversity may affect how people progress or how quickly they may get a disease, and we were interested in how it may manifest in a disease like Parkinson’s disease.
That was the framework going to meetings. As we wrote this paper and were in various editing stages, there was a beautiful paper that came out by Nadine Burke Harris and team that really was a call to action for neurologists and caring about trauma.
Dr. LaFaver: I couldn’t agree more. It’s really an underrecognized issue. With my own background, being very interested in functional movement disorders, psychosomatic disorders, and so on, it becomes much more evident how common a trauma background is, not only for people we were traditionally asking about.
Why don’t you summarize your findings for us?
Adverse childhood events
Dr. Subramanian: This is a web-based survey, so obviously, these are patient self-reports of their disease. We have a large cohort of people that we’ve been following over 7 years. I’m looking at modifiable variables and what really impacts Parkinson’s disease. Some of our previous papers have looked at diet, exercise, and loneliness. This is the same cohort.
We ended up putting the ACEs questionnaire, which is 10 questions looking at whether you were exposed to certain things in your household below the age of 18. This is a relatively standard questionnaire that’s administered one time, and you get a score out of 10. This is something that has been pushed, at least in the state of California, as something that we should be checking more in all people coming in.
We introduced the survey, and we didn’t force everyone to take it. Unfortunately, there was 20% or so of our patients who chose not to answer these questions. One has to ask, who are those people that didn’t answer the questions? Are they the ones that may have had trauma and these questions were triggering? It was a gap. We didn’t add extra questions to explore why people didn’t answer those questions.
We have to also put this in context. We have a patient population that’s largely quite affluent, who are able to access web-based surveys through their computer, and largely Caucasian; there are not many minoritized populations in our cohort. We want to do better with that. We actually were able to gather a decent number of women. We represent women quite well in our survey. I think that’s because of this online approach and some of the things that we’re studying.
In our survey, we broke it down into people who had no ACEs, one to three ACEs, or four or more ACEs. This is a standard way to break down ACEs so that we’re able to categorize what to do with these patient populations.
What we saw – and it’s preliminary evidence – is that people who had higher ACE scores seemed to have more symptom severity when we controlled for things like years since diagnosis, age, and gender. They also seem to have a worse quality of life. There was some indication that there were more nonmotor issues in those populations, as you might expect, such as anxiety, depression, and things that presumably ACEs can affect separately.
There are some confounders, but I think we really want to use this as the first piece of evidence to hopefully pave the way for caring about trauma in Parkinson’s disease moving forward.
Dr. LaFaver: Thank you so much for that summary. You already mentioned the main methodology you used.
What is the next step for you? How do you see these findings informing our clinical care? Do you have suggestions for all of the neurologists listening in this regard?
PD not yet considered ACE-related
Dr. Subramanian: Dr. Burke Harris was the former surgeon general in California. She’s a woman of color and a brilliant speaker, and she had worked in inner cities, I think in San Francisco, with pediatric populations, seeing these effects of adversity in that time frame.
You see this population at risk, and then you’re following this cohort, which we knew from the Kaiser cohort determines earlier morbidity and mortality across a number of disease states. We’re seeing things like more heart attacks, more diabetes, and all kinds of things in these populations. This is not new news; we just have not been focusing on this.
In her paper, this call to action, they had talked about some ACE-related conditions that currently do not include Parkinson’s disease. There are three ACE-related neurologic conditions that people should be aware of. One is in the headache/pain universe. Another is in the stroke universe, and that’s understandable, given cardiovascular risk factors . Then the third is in this dementia risk category. I think Parkinson’s disease, as we know, can be associated with dementia. A large percentage of our patients get dementia, but we don’t have Parkinson’s disease called out in this framework.
What people are talking about is if you have no ACEs or are in this middle category of one to three ACEs and you don’t have an ACE-related diagnosis – which Parkinson’s disease is not currently – we just give some basic counseling about the importance of lifestyle. I think we would love to see that anyway. They’re talking about things like exercise, diet, sleep, social connection, getting out in nature, things like that, so just general counseling on the importance of that.
Then if you’re in this higher-risk category, and so with these ACE-related neurologic conditions, including dementia, headache, and stroke, if you had this middle range of one to three ACEs, they’re getting additional resources. Some of them may be referred for social work help or mental health support and things like that.
I’d really love to see that happening in Parkinson’s disease, because I think we have so many needs in our population. I’m always hoping to advocate for more mental health needs that are scarce and resources in the social support realm because I believe that social connection and social support is a huge buffer for this trauma.
ACEs are just one type of trauma. I take care of veterans in the Veterans [Affairs Department]. We have some information now coming out about posttraumatic stress disorder, predisposing to certain things in Parkinson’s disease, possibly head injury, and things like that. I think we have populations at risk that we can hopefully screen at intake, and I’m really pushing for that.
Maybe it’s not the neurologist that does this intake. It might be someone else on the team that can spend some time doing these questionnaires and understand if your patient has a high ACE score. Unless you ask, many patients don’t necessarily come forward to talk about this. I really am pushing for trying to screen and trying to advocate for more research in this area so that we can classify Parkinson’s disease as an ACE-related condition and thus give more resources from the mental health world, and also the social support world, to our patients.
Dr. LaFaver: Thank you. There are many important points, and I think it’s a very important thing to recognize that it may not be only trauma in childhood but also throughout life, as you said, and might really influence nonmotor symptoms of Parkinson’s disease in particular, including anxiety and pain, which are often difficult to treat.
I think there’s much more to do in research, advocacy, and education. We’re going to educate patients about this, and also educate other neurologists and providers. I think you mentioned that trauma-informed care is getting its spotlight in primary care and other specialties. I think we have catching up to do in neurology, and I think this is a really important work toward that goal.
Thank you so much for your work and for taking the time to share your thoughts. I hope to talk to you again soon.
Dr. Subramanian: Thank you so much, Kathrin.
Dr. LaFaver has disclosed no relevant financial relationships. Dr. Subramanian disclosed ties with Acorda Therapeutics.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Kathrin LaFaver, MD: Hello. I’m happy to talk today to Dr. Indu Subramanian, clinical professor at University of California, Los Angeles, and director of the Parkinson’s Disease Research, Education and Clinical Center in Los Angeles. I am a neurologist in Saratoga Springs, New York, and we will be talking today about Indu’s new paper on childhood trauma and Parkinson’s disease. Welcome and thanks for taking the time.
Indu Subramanian, MD: Thank you so much for letting us highlight this important topic.
Dr. LaFaver: There are many papers published every month on Parkinson’s disease, but this topic stands out because it’s not a thing that has been commonly looked at. What gave you the idea to study this?
Neurology behind other specialties
Dr. Subramanian: Kathrin, you and I have been looking at things that can inform us about our patients – the person who’s standing in front of us when they come in and we’re giving them this diagnosis. I think that so much of what we’ve done [in the past] is a cookie cutter approach to giving everybody the standard treatment. [We’ve been assuming that] It doesn’t matter if they’re a man or woman. It doesn’t matter if they’re a veteran. It doesn’t matter if they may be from a minoritized population.
We’ve also been interested in approaches that are outside the box, right? We have this integrative medicine and lifestyle medicine background. I’ve been going to those meetings and really been struck by the mounting evidence on the importance of things like early adverse childhood events (ACEs), what zip code you live in, what your pollution index is, and how these things can affect people through their life and their health.
I think that it is high time neurologists pay attention to this. There’s been mounting evidence throughout many disease states, various types of cancers, and mental health. Cardiology is much more advanced, but we haven’t had much data in neurology. In fact, when we went to write this paper, there were just one or two papers that were looking at multiple sclerosis or general neurologic issues, but really nothing in Parkinson’s disease.
We know that Parkinson’s disease is not only a motor disease that affects mental health, but that it also affects nonmotor issues. Childhood adversity may affect how people progress or how quickly they may get a disease, and we were interested in how it may manifest in a disease like Parkinson’s disease.
That was the framework going to meetings. As we wrote this paper and were in various editing stages, there was a beautiful paper that came out by Nadine Burke Harris and team that really was a call to action for neurologists and caring about trauma.
Dr. LaFaver: I couldn’t agree more. It’s really an underrecognized issue. With my own background, being very interested in functional movement disorders, psychosomatic disorders, and so on, it becomes much more evident how common a trauma background is, not only for people we were traditionally asking about.
Why don’t you summarize your findings for us?
Adverse childhood events
Dr. Subramanian: This is a web-based survey, so obviously, these are patient self-reports of their disease. We have a large cohort of people that we’ve been following over 7 years. I’m looking at modifiable variables and what really impacts Parkinson’s disease. Some of our previous papers have looked at diet, exercise, and loneliness. This is the same cohort.
We ended up putting the ACEs questionnaire, which is 10 questions looking at whether you were exposed to certain things in your household below the age of 18. This is a relatively standard questionnaire that’s administered one time, and you get a score out of 10. This is something that has been pushed, at least in the state of California, as something that we should be checking more in all people coming in.
We introduced the survey, and we didn’t force everyone to take it. Unfortunately, there was 20% or so of our patients who chose not to answer these questions. One has to ask, who are those people that didn’t answer the questions? Are they the ones that may have had trauma and these questions were triggering? It was a gap. We didn’t add extra questions to explore why people didn’t answer those questions.
We have to also put this in context. We have a patient population that’s largely quite affluent, who are able to access web-based surveys through their computer, and largely Caucasian; there are not many minoritized populations in our cohort. We want to do better with that. We actually were able to gather a decent number of women. We represent women quite well in our survey. I think that’s because of this online approach and some of the things that we’re studying.
In our survey, we broke it down into people who had no ACEs, one to three ACEs, or four or more ACEs. This is a standard way to break down ACEs so that we’re able to categorize what to do with these patient populations.
What we saw – and it’s preliminary evidence – is that people who had higher ACE scores seemed to have more symptom severity when we controlled for things like years since diagnosis, age, and gender. They also seem to have a worse quality of life. There was some indication that there were more nonmotor issues in those populations, as you might expect, such as anxiety, depression, and things that presumably ACEs can affect separately.
There are some confounders, but I think we really want to use this as the first piece of evidence to hopefully pave the way for caring about trauma in Parkinson’s disease moving forward.
Dr. LaFaver: Thank you so much for that summary. You already mentioned the main methodology you used.
What is the next step for you? How do you see these findings informing our clinical care? Do you have suggestions for all of the neurologists listening in this regard?
PD not yet considered ACE-related
Dr. Subramanian: Dr. Burke Harris was the former surgeon general in California. She’s a woman of color and a brilliant speaker, and she had worked in inner cities, I think in San Francisco, with pediatric populations, seeing these effects of adversity in that time frame.
You see this population at risk, and then you’re following this cohort, which we knew from the Kaiser cohort determines earlier morbidity and mortality across a number of disease states. We’re seeing things like more heart attacks, more diabetes, and all kinds of things in these populations. This is not new news; we just have not been focusing on this.
In her paper, this call to action, they had talked about some ACE-related conditions that currently do not include Parkinson’s disease. There are three ACE-related neurologic conditions that people should be aware of. One is in the headache/pain universe. Another is in the stroke universe, and that’s understandable, given cardiovascular risk factors . Then the third is in this dementia risk category. I think Parkinson’s disease, as we know, can be associated with dementia. A large percentage of our patients get dementia, but we don’t have Parkinson’s disease called out in this framework.
What people are talking about is if you have no ACEs or are in this middle category of one to three ACEs and you don’t have an ACE-related diagnosis – which Parkinson’s disease is not currently – we just give some basic counseling about the importance of lifestyle. I think we would love to see that anyway. They’re talking about things like exercise, diet, sleep, social connection, getting out in nature, things like that, so just general counseling on the importance of that.
Then if you’re in this higher-risk category, and so with these ACE-related neurologic conditions, including dementia, headache, and stroke, if you had this middle range of one to three ACEs, they’re getting additional resources. Some of them may be referred for social work help or mental health support and things like that.
I’d really love to see that happening in Parkinson’s disease, because I think we have so many needs in our population. I’m always hoping to advocate for more mental health needs that are scarce and resources in the social support realm because I believe that social connection and social support is a huge buffer for this trauma.
ACEs are just one type of trauma. I take care of veterans in the Veterans [Affairs Department]. We have some information now coming out about posttraumatic stress disorder, predisposing to certain things in Parkinson’s disease, possibly head injury, and things like that. I think we have populations at risk that we can hopefully screen at intake, and I’m really pushing for that.
Maybe it’s not the neurologist that does this intake. It might be someone else on the team that can spend some time doing these questionnaires and understand if your patient has a high ACE score. Unless you ask, many patients don’t necessarily come forward to talk about this. I really am pushing for trying to screen and trying to advocate for more research in this area so that we can classify Parkinson’s disease as an ACE-related condition and thus give more resources from the mental health world, and also the social support world, to our patients.
Dr. LaFaver: Thank you. There are many important points, and I think it’s a very important thing to recognize that it may not be only trauma in childhood but also throughout life, as you said, and might really influence nonmotor symptoms of Parkinson’s disease in particular, including anxiety and pain, which are often difficult to treat.
I think there’s much more to do in research, advocacy, and education. We’re going to educate patients about this, and also educate other neurologists and providers. I think you mentioned that trauma-informed care is getting its spotlight in primary care and other specialties. I think we have catching up to do in neurology, and I think this is a really important work toward that goal.
Thank you so much for your work and for taking the time to share your thoughts. I hope to talk to you again soon.
Dr. Subramanian: Thank you so much, Kathrin.
Dr. LaFaver has disclosed no relevant financial relationships. Dr. Subramanian disclosed ties with Acorda Therapeutics.
A version of this article originally appeared on Medscape.com.
Pretransfer visits with pediatric and adult rheumatologists smooth adolescent transition
NEW ORLEANS – Implementing a pediatric transition program in which a patient meets with both their pediatric and soon-to-be adult rheumatologist during a visit before formal transition resulted in less time setting up the first adult visit, according to research presented at the Pediatric Rheumatology Symposium.
The presentation was one of two that focused on ways to improve the transition from pediatric to adult care for rheumatology patients. The other, a poster from researchers at Baylor College of Medicine, Houston, took the first steps toward learning what factors can help predict a successful transition.
“This period of transitioning from pediatric to adult care, both rheumatology specific and otherwise, is a high-risk time,” John M. Bridges, MD, a fourth-year pediatric rheumatology fellow at the University of Alabama at Birmingham, told attendees. “There are changes in insurance coverage, employment, geographic mobility, and shifting responsibilities between parents and children in the setting of a still-developing frontal lobe that contribute to the risk of this period. Risks include disease flare, and then organ damage, as well as issues with decreasing medication and therapy, adherence, unscheduled care utilization, and increasing loss to follow-up.”
Dr. Bridges developed a structured transition program called the Bridge to Adult Care from Childhood for Young Adults with Rheumatic Disease (BACC YARD) aimed at improving the pediatric transition period. The analysis he presented focused specifically on reducing loss to follow-up by introducing a pretransfer visit with both rheumatologists. The patient first meets with their pediatric rheumatologist.
During that visit, the adult rheumatologist attends and discusses the patient’s history and current therapy with the pediatric rheumatologist before entering the patient’s room and having “a brief introductory conversation, a sort of verbal handoff and handshake, in front of the patient,” Dr. Bridges explained. “Then I assume responsibility for this patient and their next visit is to see me, both proverbially and literally down the street at the adulthood rheumatology clinic, where this patient becomes a part of my continuity cohort.”
Bridges entered patients from this BACC YARD cohort into an observational registry that included their dual provider pretransfer visit and a posttransfer visit, occurring between July 2020 and May 2022. He compared these patients with a historical control cohort of 45 patients from March 2018 to March 2020, who had at least two pediatric rheumatology visits prior to their transfer to adult care and no documentation of outside rheumatology visits during the study period. Specifically, he examined at the requested and actual interval between patients’ final pediatric rheumatology visit and their first adult rheumatology visit.
The intervention cohort included 86 patients, mostly female (73%), with a median age of 20. About two-thirds were White (65%) and one-third (34%) were Black. One patient was Asian, and 7% were Hispanic. Just over half the patients had juvenile idiopathic arthritis (58%), and 30% had lupus and related connective tissue diseases. The other patients had vasculitis, uveitis, inflammatory myopathy, relapsing polychondritis, morphea, or syndrome of undifferentiated recurrent fever.
A total of 8% of these patients had previously been lost to follow-up at Children’s of Alabama before they re-established rheumatology care at UAB, and 3.5% came from a pediatric rheumatologist from somewhere other than Children’s of Alabama but established adult care at UAB through the BACC YARD program. Among the remaining patients, 65% (n = 56) had both a dual provider pretransfer visit and a posttransfer visit.
The BACC YARD patients requested their next rheumatology visit (the first adult one) a median 119 days after their last pediatric visit, and the actual time until that visit was a median 141 days (P < .05). By comparison, the 45 patients in the historical control group had a median 261 days between their last pediatric visit and their first adult visit (P < .001). The median days between visits was shorter for those with JIA (129 days) and lupus (119 days) than for patients with other conditions (149 days).
Bridges acknowledged that the study was limited by the small size of the cohort and potential contextual factors related to individual patients’ circumstances.
“We’re continuing to make iterative changes to this process to try to continue to improve the transition and its outcomes in this cohort,” Dr. Bridges said.
Aimee Hersh, MD, an associate professor of pediatric rheumatology and division chief of pediatric rheumatology at the University of Utah and Primary Children’s Hospital, both in Salt Lake City, attended the presentation and noted that the University of Utah has a very similar transfer program.
“I think one of the challenges of that model, and our model, is that you have to have a very specific type of physician who is both [medical-pediatrics] trained and has a specific interest in transition,” Dr. Hersh said in an interview. She noted that the adult rheumatologist at her institution didn’t train in pediatric rheumatology but did complete a meds-peds residency. “So if you can find an adult rheumatologist who can do something similar, can see older adolescent patients and serve as that transition bridge, then I think it is feasible.”
For practices that don’t have the resources for this kind of program, Dr. Hersh recommended the Got Transition program, which provides transition guidance that can be applied to any adolescent population with chronic illness.
The other study, led by Kristiana Nasto, BS, a third-year medical student at Baylor College of Medicine, reported on the findings from one aspect of a program also developed to improve the transition from pediatric to adult care for rheumatology patients. It included periodic self-reported evaluation using the validated Adolescent Assessment of Preparation for Transition (ADAPT) survey. As the first step to better understanding the factors that can predict successful transition, the researchers surveyed returning patients with any rheumatologic diagnosis, aged 14 years and older, between July 2021 and November 2022.
Since the survey was automated through the electronic medical record, patients and their caregivers could respond during in-person or virtual visit check-in. The researchers calculated three composite scores out of 100 for self-management, prescription management, and transfer planning, using responses from the ADAPT survey. Among 462 patients who returned 670 surveys, 87% provided surveys that could be scored for at least one composite score. Most respondents were female (75%), White (69%), non-Hispanic (64%), English speaking (90%), and aged 14-17 years (83%).
The overall average score for self-management from 401 respondents was 35. For prescription management, the average score was 59 from 288 respondents, and the average transfer planning score was 17 from 367 respondents. Self-management and transfer planning scores both improved with age (P = .0001). Self-management scores rose from an average of 20 at age 14 to an average of 64 at age 18 and older. Transfer planning scores increased from an average of 1 at age 14 to an average of 49 at age 18 and older. Prescription management scores remained high across all ages, from an average of 59 at age 14 to an average score of 66 at age 18 and older (P = .044). Although the scores did not statistically vary by age or race, Hispanic patients did score higher in self-management with an average of 44.5, compared with 31 among other patients (P = .0001).
Only 21% of patients completed two surveys, and 8.4% completed all three surveys. The average time between the first and second surveys was 4 months, during which there was no statistically significant change in self-management or prescription management scores, but transfer planning scores did increase from 14 to 21 (P = .008) among the 90 patients who completed those surveys.
The researchers concluded from their analysis that “participation in the transition pathway can rapidly improve transfer planning scores, [but] opportunities remain to improve readiness in all domains.” The researchers are in the process of developing Spanish-language surveys.
No external funding was noted for either study. Dr. Bridges, Dr. Hersh, and Ms. Nasto reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Implementing a pediatric transition program in which a patient meets with both their pediatric and soon-to-be adult rheumatologist during a visit before formal transition resulted in less time setting up the first adult visit, according to research presented at the Pediatric Rheumatology Symposium.
The presentation was one of two that focused on ways to improve the transition from pediatric to adult care for rheumatology patients. The other, a poster from researchers at Baylor College of Medicine, Houston, took the first steps toward learning what factors can help predict a successful transition.
“This period of transitioning from pediatric to adult care, both rheumatology specific and otherwise, is a high-risk time,” John M. Bridges, MD, a fourth-year pediatric rheumatology fellow at the University of Alabama at Birmingham, told attendees. “There are changes in insurance coverage, employment, geographic mobility, and shifting responsibilities between parents and children in the setting of a still-developing frontal lobe that contribute to the risk of this period. Risks include disease flare, and then organ damage, as well as issues with decreasing medication and therapy, adherence, unscheduled care utilization, and increasing loss to follow-up.”
Dr. Bridges developed a structured transition program called the Bridge to Adult Care from Childhood for Young Adults with Rheumatic Disease (BACC YARD) aimed at improving the pediatric transition period. The analysis he presented focused specifically on reducing loss to follow-up by introducing a pretransfer visit with both rheumatologists. The patient first meets with their pediatric rheumatologist.
During that visit, the adult rheumatologist attends and discusses the patient’s history and current therapy with the pediatric rheumatologist before entering the patient’s room and having “a brief introductory conversation, a sort of verbal handoff and handshake, in front of the patient,” Dr. Bridges explained. “Then I assume responsibility for this patient and their next visit is to see me, both proverbially and literally down the street at the adulthood rheumatology clinic, where this patient becomes a part of my continuity cohort.”
Bridges entered patients from this BACC YARD cohort into an observational registry that included their dual provider pretransfer visit and a posttransfer visit, occurring between July 2020 and May 2022. He compared these patients with a historical control cohort of 45 patients from March 2018 to March 2020, who had at least two pediatric rheumatology visits prior to their transfer to adult care and no documentation of outside rheumatology visits during the study period. Specifically, he examined at the requested and actual interval between patients’ final pediatric rheumatology visit and their first adult rheumatology visit.
The intervention cohort included 86 patients, mostly female (73%), with a median age of 20. About two-thirds were White (65%) and one-third (34%) were Black. One patient was Asian, and 7% were Hispanic. Just over half the patients had juvenile idiopathic arthritis (58%), and 30% had lupus and related connective tissue diseases. The other patients had vasculitis, uveitis, inflammatory myopathy, relapsing polychondritis, morphea, or syndrome of undifferentiated recurrent fever.
A total of 8% of these patients had previously been lost to follow-up at Children’s of Alabama before they re-established rheumatology care at UAB, and 3.5% came from a pediatric rheumatologist from somewhere other than Children’s of Alabama but established adult care at UAB through the BACC YARD program. Among the remaining patients, 65% (n = 56) had both a dual provider pretransfer visit and a posttransfer visit.
The BACC YARD patients requested their next rheumatology visit (the first adult one) a median 119 days after their last pediatric visit, and the actual time until that visit was a median 141 days (P < .05). By comparison, the 45 patients in the historical control group had a median 261 days between their last pediatric visit and their first adult visit (P < .001). The median days between visits was shorter for those with JIA (129 days) and lupus (119 days) than for patients with other conditions (149 days).
Bridges acknowledged that the study was limited by the small size of the cohort and potential contextual factors related to individual patients’ circumstances.
“We’re continuing to make iterative changes to this process to try to continue to improve the transition and its outcomes in this cohort,” Dr. Bridges said.
Aimee Hersh, MD, an associate professor of pediatric rheumatology and division chief of pediatric rheumatology at the University of Utah and Primary Children’s Hospital, both in Salt Lake City, attended the presentation and noted that the University of Utah has a very similar transfer program.
“I think one of the challenges of that model, and our model, is that you have to have a very specific type of physician who is both [medical-pediatrics] trained and has a specific interest in transition,” Dr. Hersh said in an interview. She noted that the adult rheumatologist at her institution didn’t train in pediatric rheumatology but did complete a meds-peds residency. “So if you can find an adult rheumatologist who can do something similar, can see older adolescent patients and serve as that transition bridge, then I think it is feasible.”
For practices that don’t have the resources for this kind of program, Dr. Hersh recommended the Got Transition program, which provides transition guidance that can be applied to any adolescent population with chronic illness.
The other study, led by Kristiana Nasto, BS, a third-year medical student at Baylor College of Medicine, reported on the findings from one aspect of a program also developed to improve the transition from pediatric to adult care for rheumatology patients. It included periodic self-reported evaluation using the validated Adolescent Assessment of Preparation for Transition (ADAPT) survey. As the first step to better understanding the factors that can predict successful transition, the researchers surveyed returning patients with any rheumatologic diagnosis, aged 14 years and older, between July 2021 and November 2022.
Since the survey was automated through the electronic medical record, patients and their caregivers could respond during in-person or virtual visit check-in. The researchers calculated three composite scores out of 100 for self-management, prescription management, and transfer planning, using responses from the ADAPT survey. Among 462 patients who returned 670 surveys, 87% provided surveys that could be scored for at least one composite score. Most respondents were female (75%), White (69%), non-Hispanic (64%), English speaking (90%), and aged 14-17 years (83%).
The overall average score for self-management from 401 respondents was 35. For prescription management, the average score was 59 from 288 respondents, and the average transfer planning score was 17 from 367 respondents. Self-management and transfer planning scores both improved with age (P = .0001). Self-management scores rose from an average of 20 at age 14 to an average of 64 at age 18 and older. Transfer planning scores increased from an average of 1 at age 14 to an average of 49 at age 18 and older. Prescription management scores remained high across all ages, from an average of 59 at age 14 to an average score of 66 at age 18 and older (P = .044). Although the scores did not statistically vary by age or race, Hispanic patients did score higher in self-management with an average of 44.5, compared with 31 among other patients (P = .0001).
Only 21% of patients completed two surveys, and 8.4% completed all three surveys. The average time between the first and second surveys was 4 months, during which there was no statistically significant change in self-management or prescription management scores, but transfer planning scores did increase from 14 to 21 (P = .008) among the 90 patients who completed those surveys.
The researchers concluded from their analysis that “participation in the transition pathway can rapidly improve transfer planning scores, [but] opportunities remain to improve readiness in all domains.” The researchers are in the process of developing Spanish-language surveys.
No external funding was noted for either study. Dr. Bridges, Dr. Hersh, and Ms. Nasto reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Implementing a pediatric transition program in which a patient meets with both their pediatric and soon-to-be adult rheumatologist during a visit before formal transition resulted in less time setting up the first adult visit, according to research presented at the Pediatric Rheumatology Symposium.
The presentation was one of two that focused on ways to improve the transition from pediatric to adult care for rheumatology patients. The other, a poster from researchers at Baylor College of Medicine, Houston, took the first steps toward learning what factors can help predict a successful transition.
“This period of transitioning from pediatric to adult care, both rheumatology specific and otherwise, is a high-risk time,” John M. Bridges, MD, a fourth-year pediatric rheumatology fellow at the University of Alabama at Birmingham, told attendees. “There are changes in insurance coverage, employment, geographic mobility, and shifting responsibilities between parents and children in the setting of a still-developing frontal lobe that contribute to the risk of this period. Risks include disease flare, and then organ damage, as well as issues with decreasing medication and therapy, adherence, unscheduled care utilization, and increasing loss to follow-up.”
Dr. Bridges developed a structured transition program called the Bridge to Adult Care from Childhood for Young Adults with Rheumatic Disease (BACC YARD) aimed at improving the pediatric transition period. The analysis he presented focused specifically on reducing loss to follow-up by introducing a pretransfer visit with both rheumatologists. The patient first meets with their pediatric rheumatologist.
During that visit, the adult rheumatologist attends and discusses the patient’s history and current therapy with the pediatric rheumatologist before entering the patient’s room and having “a brief introductory conversation, a sort of verbal handoff and handshake, in front of the patient,” Dr. Bridges explained. “Then I assume responsibility for this patient and their next visit is to see me, both proverbially and literally down the street at the adulthood rheumatology clinic, where this patient becomes a part of my continuity cohort.”
Bridges entered patients from this BACC YARD cohort into an observational registry that included their dual provider pretransfer visit and a posttransfer visit, occurring between July 2020 and May 2022. He compared these patients with a historical control cohort of 45 patients from March 2018 to March 2020, who had at least two pediatric rheumatology visits prior to their transfer to adult care and no documentation of outside rheumatology visits during the study period. Specifically, he examined at the requested and actual interval between patients’ final pediatric rheumatology visit and their first adult rheumatology visit.
The intervention cohort included 86 patients, mostly female (73%), with a median age of 20. About two-thirds were White (65%) and one-third (34%) were Black. One patient was Asian, and 7% were Hispanic. Just over half the patients had juvenile idiopathic arthritis (58%), and 30% had lupus and related connective tissue diseases. The other patients had vasculitis, uveitis, inflammatory myopathy, relapsing polychondritis, morphea, or syndrome of undifferentiated recurrent fever.
A total of 8% of these patients had previously been lost to follow-up at Children’s of Alabama before they re-established rheumatology care at UAB, and 3.5% came from a pediatric rheumatologist from somewhere other than Children’s of Alabama but established adult care at UAB through the BACC YARD program. Among the remaining patients, 65% (n = 56) had both a dual provider pretransfer visit and a posttransfer visit.
The BACC YARD patients requested their next rheumatology visit (the first adult one) a median 119 days after their last pediatric visit, and the actual time until that visit was a median 141 days (P < .05). By comparison, the 45 patients in the historical control group had a median 261 days between their last pediatric visit and their first adult visit (P < .001). The median days between visits was shorter for those with JIA (129 days) and lupus (119 days) than for patients with other conditions (149 days).
Bridges acknowledged that the study was limited by the small size of the cohort and potential contextual factors related to individual patients’ circumstances.
“We’re continuing to make iterative changes to this process to try to continue to improve the transition and its outcomes in this cohort,” Dr. Bridges said.
Aimee Hersh, MD, an associate professor of pediatric rheumatology and division chief of pediatric rheumatology at the University of Utah and Primary Children’s Hospital, both in Salt Lake City, attended the presentation and noted that the University of Utah has a very similar transfer program.
“I think one of the challenges of that model, and our model, is that you have to have a very specific type of physician who is both [medical-pediatrics] trained and has a specific interest in transition,” Dr. Hersh said in an interview. She noted that the adult rheumatologist at her institution didn’t train in pediatric rheumatology but did complete a meds-peds residency. “So if you can find an adult rheumatologist who can do something similar, can see older adolescent patients and serve as that transition bridge, then I think it is feasible.”
For practices that don’t have the resources for this kind of program, Dr. Hersh recommended the Got Transition program, which provides transition guidance that can be applied to any adolescent population with chronic illness.
The other study, led by Kristiana Nasto, BS, a third-year medical student at Baylor College of Medicine, reported on the findings from one aspect of a program also developed to improve the transition from pediatric to adult care for rheumatology patients. It included periodic self-reported evaluation using the validated Adolescent Assessment of Preparation for Transition (ADAPT) survey. As the first step to better understanding the factors that can predict successful transition, the researchers surveyed returning patients with any rheumatologic diagnosis, aged 14 years and older, between July 2021 and November 2022.
Since the survey was automated through the electronic medical record, patients and their caregivers could respond during in-person or virtual visit check-in. The researchers calculated three composite scores out of 100 for self-management, prescription management, and transfer planning, using responses from the ADAPT survey. Among 462 patients who returned 670 surveys, 87% provided surveys that could be scored for at least one composite score. Most respondents were female (75%), White (69%), non-Hispanic (64%), English speaking (90%), and aged 14-17 years (83%).
The overall average score for self-management from 401 respondents was 35. For prescription management, the average score was 59 from 288 respondents, and the average transfer planning score was 17 from 367 respondents. Self-management and transfer planning scores both improved with age (P = .0001). Self-management scores rose from an average of 20 at age 14 to an average of 64 at age 18 and older. Transfer planning scores increased from an average of 1 at age 14 to an average of 49 at age 18 and older. Prescription management scores remained high across all ages, from an average of 59 at age 14 to an average score of 66 at age 18 and older (P = .044). Although the scores did not statistically vary by age or race, Hispanic patients did score higher in self-management with an average of 44.5, compared with 31 among other patients (P = .0001).
Only 21% of patients completed two surveys, and 8.4% completed all three surveys. The average time between the first and second surveys was 4 months, during which there was no statistically significant change in self-management or prescription management scores, but transfer planning scores did increase from 14 to 21 (P = .008) among the 90 patients who completed those surveys.
The researchers concluded from their analysis that “participation in the transition pathway can rapidly improve transfer planning scores, [but] opportunities remain to improve readiness in all domains.” The researchers are in the process of developing Spanish-language surveys.
No external funding was noted for either study. Dr. Bridges, Dr. Hersh, and Ms. Nasto reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT PRSYM 2023
MRD: Powerful metric for CLL research
“MRD measurement is now a key feature of CLL clinical trials reporting. It can change CLL care by enabling approval of medication use in the wider (nontrial) patient population based on MRD data, without having to wait (ever-increasing) times for conventional trial outcomes, such as progression-free survival [PFS],” said study author Tahla Munir MD, of the department of hematology, at the Leeds (England) Teaching Hospitals of the National Health Service Trust.
“It also has potential to direct our treatment duration and follow-up strategies based on MRD results taken during or at the end of treatment, and to direct new treatment strategies, such as intermittent (as opposed to fixed-duration or continuous) treatment,” Dr. Munir said in an interview.
The review study defined MRD according to the detectable proportion of residual CLL cells. (Current international consensus for undetectable is U-MRD4 1 leukemic cell in 10,000 leukocytes.) The advantages and disadvantages of different MRD assays were analyzed. Multiparameter flow cytometry, an older technology, proved less sensitive to newer tests. It is reliable measuring to a sensitivity of U-MRD4 and more widely available than next-generation real-time quantitative polymerase chain reaction tests (NG-PCR).
“NG-PCR has the most potential for use in laboratory practice. It doesn’t require patient-specific primers and can detect around 1 CLL cell in 1x106 leukocytes. The biggest challenge is laboratory sequencing and bioinformatic capacity,” said lead study author Amelia Fisher, clinical research fellow at the division of cancer studies and pathology, University of Leeds.
“Multiple wells are required to gather adequate data to match the sensitivity of NGS. As this technology improves to match NGS sensitivity using fewer wells, once primers (bespoke to each patient) are designed it will provide a simple to use, rapid and easily reportable MRD tool, that could be scaled up in the event of MRD testing becoming routine practice,” explained Dr. Fisher.
The study also demonstrated how MRD can offer more in-depth insights into the success of treatments versus PFS. In the MURANO clinical trial, which compared venetoclax-rituximab treatment with standard chemoimmunotherapy (SC) to treat relapsed or refractory CLL, the PFS and overall survival (OS) remained significantly prolonged in the VR group at 5 years after therapy.
Analysis of MRD levels in the VR arm demonstrated that those with U-MRD4 had superior OS, with survival at 5 years of 95.3%, compared with those with higher rates of MRD (72.9%). A slower rate of MRD doubling time in the VR-treated patients, compared with the SC-treated patients, also buttressed the notion of moving from SC to VR treatment for the general CLL patient population.
Researchers cautioned that “a lot of the data is very recent, and therefore we do not have conventional trial outcomes, e.g., PFS and OS for all the studies. Some of the data we have is over a relatively short time period.”
An independent expert not associated with the study, Alessandra Ferrajoli, MD, associate medical director of the department of leukemia at the University of Texas MD Anderson Cancer Center, Houston, expressed agreement with the study’s main findings.
“It is very likely that MRD assessment will be incorporated as a standard measurement of treatment efficacy in patients with CLL in the near future. The technologies have evolved to high levels of sensitivity, and the methods are being successfully harmonized and standardized,” she said.
Neither the study authors nor Dr. Ferrajoli reported conflicts of interest.
“MRD measurement is now a key feature of CLL clinical trials reporting. It can change CLL care by enabling approval of medication use in the wider (nontrial) patient population based on MRD data, without having to wait (ever-increasing) times for conventional trial outcomes, such as progression-free survival [PFS],” said study author Tahla Munir MD, of the department of hematology, at the Leeds (England) Teaching Hospitals of the National Health Service Trust.
“It also has potential to direct our treatment duration and follow-up strategies based on MRD results taken during or at the end of treatment, and to direct new treatment strategies, such as intermittent (as opposed to fixed-duration or continuous) treatment,” Dr. Munir said in an interview.
The review study defined MRD according to the detectable proportion of residual CLL cells. (Current international consensus for undetectable is U-MRD4 1 leukemic cell in 10,000 leukocytes.) The advantages and disadvantages of different MRD assays were analyzed. Multiparameter flow cytometry, an older technology, proved less sensitive to newer tests. It is reliable measuring to a sensitivity of U-MRD4 and more widely available than next-generation real-time quantitative polymerase chain reaction tests (NG-PCR).
“NG-PCR has the most potential for use in laboratory practice. It doesn’t require patient-specific primers and can detect around 1 CLL cell in 1x106 leukocytes. The biggest challenge is laboratory sequencing and bioinformatic capacity,” said lead study author Amelia Fisher, clinical research fellow at the division of cancer studies and pathology, University of Leeds.
“Multiple wells are required to gather adequate data to match the sensitivity of NGS. As this technology improves to match NGS sensitivity using fewer wells, once primers (bespoke to each patient) are designed it will provide a simple to use, rapid and easily reportable MRD tool, that could be scaled up in the event of MRD testing becoming routine practice,” explained Dr. Fisher.
The study also demonstrated how MRD can offer more in-depth insights into the success of treatments versus PFS. In the MURANO clinical trial, which compared venetoclax-rituximab treatment with standard chemoimmunotherapy (SC) to treat relapsed or refractory CLL, the PFS and overall survival (OS) remained significantly prolonged in the VR group at 5 years after therapy.
Analysis of MRD levels in the VR arm demonstrated that those with U-MRD4 had superior OS, with survival at 5 years of 95.3%, compared with those with higher rates of MRD (72.9%). A slower rate of MRD doubling time in the VR-treated patients, compared with the SC-treated patients, also buttressed the notion of moving from SC to VR treatment for the general CLL patient population.
Researchers cautioned that “a lot of the data is very recent, and therefore we do not have conventional trial outcomes, e.g., PFS and OS for all the studies. Some of the data we have is over a relatively short time period.”
An independent expert not associated with the study, Alessandra Ferrajoli, MD, associate medical director of the department of leukemia at the University of Texas MD Anderson Cancer Center, Houston, expressed agreement with the study’s main findings.
“It is very likely that MRD assessment will be incorporated as a standard measurement of treatment efficacy in patients with CLL in the near future. The technologies have evolved to high levels of sensitivity, and the methods are being successfully harmonized and standardized,” she said.
Neither the study authors nor Dr. Ferrajoli reported conflicts of interest.
“MRD measurement is now a key feature of CLL clinical trials reporting. It can change CLL care by enabling approval of medication use in the wider (nontrial) patient population based on MRD data, without having to wait (ever-increasing) times for conventional trial outcomes, such as progression-free survival [PFS],” said study author Tahla Munir MD, of the department of hematology, at the Leeds (England) Teaching Hospitals of the National Health Service Trust.
“It also has potential to direct our treatment duration and follow-up strategies based on MRD results taken during or at the end of treatment, and to direct new treatment strategies, such as intermittent (as opposed to fixed-duration or continuous) treatment,” Dr. Munir said in an interview.
The review study defined MRD according to the detectable proportion of residual CLL cells. (Current international consensus for undetectable is U-MRD4 1 leukemic cell in 10,000 leukocytes.) The advantages and disadvantages of different MRD assays were analyzed. Multiparameter flow cytometry, an older technology, proved less sensitive to newer tests. It is reliable measuring to a sensitivity of U-MRD4 and more widely available than next-generation real-time quantitative polymerase chain reaction tests (NG-PCR).
“NG-PCR has the most potential for use in laboratory practice. It doesn’t require patient-specific primers and can detect around 1 CLL cell in 1x106 leukocytes. The biggest challenge is laboratory sequencing and bioinformatic capacity,” said lead study author Amelia Fisher, clinical research fellow at the division of cancer studies and pathology, University of Leeds.
“Multiple wells are required to gather adequate data to match the sensitivity of NGS. As this technology improves to match NGS sensitivity using fewer wells, once primers (bespoke to each patient) are designed it will provide a simple to use, rapid and easily reportable MRD tool, that could be scaled up in the event of MRD testing becoming routine practice,” explained Dr. Fisher.
The study also demonstrated how MRD can offer more in-depth insights into the success of treatments versus PFS. In the MURANO clinical trial, which compared venetoclax-rituximab treatment with standard chemoimmunotherapy (SC) to treat relapsed or refractory CLL, the PFS and overall survival (OS) remained significantly prolonged in the VR group at 5 years after therapy.
Analysis of MRD levels in the VR arm demonstrated that those with U-MRD4 had superior OS, with survival at 5 years of 95.3%, compared with those with higher rates of MRD (72.9%). A slower rate of MRD doubling time in the VR-treated patients, compared with the SC-treated patients, also buttressed the notion of moving from SC to VR treatment for the general CLL patient population.
Researchers cautioned that “a lot of the data is very recent, and therefore we do not have conventional trial outcomes, e.g., PFS and OS for all the studies. Some of the data we have is over a relatively short time period.”
An independent expert not associated with the study, Alessandra Ferrajoli, MD, associate medical director of the department of leukemia at the University of Texas MD Anderson Cancer Center, Houston, expressed agreement with the study’s main findings.
“It is very likely that MRD assessment will be incorporated as a standard measurement of treatment efficacy in patients with CLL in the near future. The technologies have evolved to high levels of sensitivity, and the methods are being successfully harmonized and standardized,” she said.
Neither the study authors nor Dr. Ferrajoli reported conflicts of interest.
FROM FRONTIERS IN ONCOLOGY
Cervical screening often stops at 65, but should it?
“Did you love your wife?” asks a character in “Rose,” a book by Martin Cruz Smith.
“No, but she became a fact through perseverance,” the man replied.
Medicine also has such relationships, it seems – tentative ideas that turned into fact simply by existing long enough.
Age 65 as the cutoff for cervical screening may be one such example. It has existed for 27 years with limited science to back it up. That may soon change with the launch of a $3.3 million study that is being funded by the National Institutes of Health (NIH). The study is intended to provide a more solid foundation for the benefits and harms of cervical screening for women older than 65.
It’s an important issue: 20% of all cervical cancer cases are found in women who are older than 65. Most of these patients have late-stage disease, which can be fatal. In the United States, 35% of cervical cancer deaths occur after age 65. But women in this age group are usually no longer screened for cervical cancer.
Back in 1996, the U.S. Preventive Services Task Force recommended that for women at average risk with adequate prior screening, cervical screening should stop at the age of 65. This recommendation has been carried forward year after year and has been incorporated into several other guidelines.
For example, current guidelines from the American Cancer Society, the American College of Obstetricians and Gynecologists, and the USPSTF recommend that cervical screening stop at aged 65 for patients with adequate prior screening.
“Adequate screening” is defined as three consecutive normal Pap tests or two consecutive negative human papillomavirus tests or two consecutive negative co-tests within the prior 10 years, with the most recent screening within 5 years and with no precancerous lesions in the past 25 years.
This all sounds reasonable; however, for most women, medical records aren’t up to the task of providing a clean bill of cervical health over many decades.
Explained Sarah Feldman, MD, an associate professor in obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston: “You know, when a patient says to me at 65, ‘Should I continue screening?’ I say, ‘Do you have all your results?’ And they’ll say, ‘Well, I remember I had a sort of abnormal pap 15 years ago,’ and I say, ‘All right; well, who knows what that was?’ So I’ll continue screening.”
According to George Sawaya, MD, professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Francisco, up to 60% of women do not meet the criteria to end screening at age 65. This means that each year in the United States, approximately 1.7 million women turn 65 and should, in theory, continue to undergo screening for cervical cancer.
Unfortunately, the evidence base for the harms and benefits of cervical screening after age 65 is almost nonexistent – at least by the current standards of evidence-based medicine.
“We need to be clear that we don’t really know the appropriateness of the screening after 65,” said Dr. Sawaya, “which is ironic, because cervical cancer screening is probably the most commonly implemented cancer screening test in the country because it starts so early and ends so late and it’s applied so frequently.”
Dr. Feldman agrees that the age 65 cutoff is “somewhat arbitrary.” She said, “Why don’t they want to consider it continuing past 65? I don’t really understand, I have to be honest with you.”
So what’s the scientific evidence backing up the 27-year-old recommendation?
In 2018, the USPSTF’s cervical-screening guidelines concluded “with moderate certainty that the benefits of screening in women older than 65 years who have had adequate prior screening and are not otherwise at high risk for cervical cancer do not outweigh the potential harms.”
This recommendation was based on a new decision model commissioned by the USPSTF. The model was needed because, as noted by the guidelines’ authors, “None of the screening trials enrolled women older than 65 years, so direct evidence on when to stop screening is not available.”
In 2020, the ACS carried out a fresh literature review and published its own recommendations. The ACS concluded that “the evidence for the effectiveness of screening beyond age 65 is limited, based solely on observational and modeling studies.”
As a result, the ACS assigned a “qualified recommendation” to the age-65 moratorium (defined as “less certainty about the balance of benefits and harms or about patients’ values and preferences”).
Most recently, the 2021 Updated Cervical Cancer Screening Guidelines, published by the American College of Obstetricians and Gynecologists, endorsed the recommendations of the USPSTF.
Dr. Sawaya said, “The whole issue about screening over 65 is complicated from a lot of perspectives. We don’t know a lot about the safety. We don’t really know a lot about patients’ perceptions of it. But we do know that there has to be an upper age limit after which screening is just simply imprudent.”
Dr. Sawaya acknowledges that there exists a “heck-why-not” attitude toward cervical screening after 65 among some physicians, given that the tests are quick and cheap and could save a life, but he sounds a note of caution.
“It’s like when we used to use old cameras: the film was cheap, but the developing was really expensive,” Dr. Sawaya said. “So it’s not necessarily about the tests being cheap, it’s about the cascade of events [that follow].”
Follow-up for cervical cancer can be more hazardous for a postmenopausal patient than for a younger woman, explained Dr. Sawaya, because the transformation zone of the cervix may be difficult to see on colposcopy. Instead of a straightforward 5-minute procedure in the doctor’s office, the older patient may need the operating room simply to provide the first biopsy.
In addition, treatments such as cone biopsy, loop excision, or ablation are also more worrying for older women, said Dr. Sawaya, “So you start thinking about the risks of anesthesia, you start thinking about the risks of bleeding and infection, etc. And these have not been well described in older people.”
To add to the uncertainty about the merits and risks of hunting out cervical cancer in older women, a lot has changed in women’s health since 1996.
Explained Dr. Sawaya, “This stake was put in the ground in 1996, ... but since that time, life expectancy has gained 5 years. So a logical person would say, ‘Oh, well, let’s just say it should be 70 now, right?’ [But] can we even use old studies to inform the current cohort of women who are entering this 65-year-and-older age group?”
To answer all these questions, a 5-year, $3.3 million study funded by the NIH through the National Cancer Institute is now underway.
The project, named Comparative Effectiveness Research to Validate and Improve Cervical Cancer Screening (CERVICCS 2), will be led by Dr. Sawaya and Michael Silverberg, PhD, associate director of the Behavioral Health, Aging and Infectious Diseases Section of Kaiser Permanente Northern California’s Division of Research.
It’s not possible to conduct a true randomized controlled trial in this field of medicine for ethical reasons, so CERVICCS 2 will emulate a randomized study by following the fate of approximately 280,000 women older than 65 who were long-term members of two large health systems during 2005-2022. – both before and after the crucial age 65 cutoff.
The California study will also look at the downsides of diagnostic procedures and surgical interventions that follow a positive screening result after the age of 65 and the personal experiences of the women involved.
Dr. Sawaya and Dr. Silverberg’s team will use software that emulates a clinical trial by utilizing observational data to compare the benefits and risks of screening continuation or screening cessation after age 65.
In effect, after 27 years of loyalty to a recommendation supported by low-quality evidence, medicine will finally have a reliable answer to the question, Should we continue to look for cervical cancer in women over 65?
Dr. Sawaya concluded: “There’s very few things that are packaged away and thought to be just the truth. And this is why we always have to be vigilant. ... And that’s what keeps science so interesting and exciting.”
Dr. Sawaya has disclosed no relevant financial relationships. Dr. Feldman writes for UpToDate and receives several NIH grants.
A version of this article first appeared on Medscape.com.
“Did you love your wife?” asks a character in “Rose,” a book by Martin Cruz Smith.
“No, but she became a fact through perseverance,” the man replied.
Medicine also has such relationships, it seems – tentative ideas that turned into fact simply by existing long enough.
Age 65 as the cutoff for cervical screening may be one such example. It has existed for 27 years with limited science to back it up. That may soon change with the launch of a $3.3 million study that is being funded by the National Institutes of Health (NIH). The study is intended to provide a more solid foundation for the benefits and harms of cervical screening for women older than 65.
It’s an important issue: 20% of all cervical cancer cases are found in women who are older than 65. Most of these patients have late-stage disease, which can be fatal. In the United States, 35% of cervical cancer deaths occur after age 65. But women in this age group are usually no longer screened for cervical cancer.
Back in 1996, the U.S. Preventive Services Task Force recommended that for women at average risk with adequate prior screening, cervical screening should stop at the age of 65. This recommendation has been carried forward year after year and has been incorporated into several other guidelines.
For example, current guidelines from the American Cancer Society, the American College of Obstetricians and Gynecologists, and the USPSTF recommend that cervical screening stop at aged 65 for patients with adequate prior screening.
“Adequate screening” is defined as three consecutive normal Pap tests or two consecutive negative human papillomavirus tests or two consecutive negative co-tests within the prior 10 years, with the most recent screening within 5 years and with no precancerous lesions in the past 25 years.
This all sounds reasonable; however, for most women, medical records aren’t up to the task of providing a clean bill of cervical health over many decades.
Explained Sarah Feldman, MD, an associate professor in obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston: “You know, when a patient says to me at 65, ‘Should I continue screening?’ I say, ‘Do you have all your results?’ And they’ll say, ‘Well, I remember I had a sort of abnormal pap 15 years ago,’ and I say, ‘All right; well, who knows what that was?’ So I’ll continue screening.”
According to George Sawaya, MD, professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Francisco, up to 60% of women do not meet the criteria to end screening at age 65. This means that each year in the United States, approximately 1.7 million women turn 65 and should, in theory, continue to undergo screening for cervical cancer.
Unfortunately, the evidence base for the harms and benefits of cervical screening after age 65 is almost nonexistent – at least by the current standards of evidence-based medicine.
“We need to be clear that we don’t really know the appropriateness of the screening after 65,” said Dr. Sawaya, “which is ironic, because cervical cancer screening is probably the most commonly implemented cancer screening test in the country because it starts so early and ends so late and it’s applied so frequently.”
Dr. Feldman agrees that the age 65 cutoff is “somewhat arbitrary.” She said, “Why don’t they want to consider it continuing past 65? I don’t really understand, I have to be honest with you.”
So what’s the scientific evidence backing up the 27-year-old recommendation?
In 2018, the USPSTF’s cervical-screening guidelines concluded “with moderate certainty that the benefits of screening in women older than 65 years who have had adequate prior screening and are not otherwise at high risk for cervical cancer do not outweigh the potential harms.”
This recommendation was based on a new decision model commissioned by the USPSTF. The model was needed because, as noted by the guidelines’ authors, “None of the screening trials enrolled women older than 65 years, so direct evidence on when to stop screening is not available.”
In 2020, the ACS carried out a fresh literature review and published its own recommendations. The ACS concluded that “the evidence for the effectiveness of screening beyond age 65 is limited, based solely on observational and modeling studies.”
As a result, the ACS assigned a “qualified recommendation” to the age-65 moratorium (defined as “less certainty about the balance of benefits and harms or about patients’ values and preferences”).
Most recently, the 2021 Updated Cervical Cancer Screening Guidelines, published by the American College of Obstetricians and Gynecologists, endorsed the recommendations of the USPSTF.
Dr. Sawaya said, “The whole issue about screening over 65 is complicated from a lot of perspectives. We don’t know a lot about the safety. We don’t really know a lot about patients’ perceptions of it. But we do know that there has to be an upper age limit after which screening is just simply imprudent.”
Dr. Sawaya acknowledges that there exists a “heck-why-not” attitude toward cervical screening after 65 among some physicians, given that the tests are quick and cheap and could save a life, but he sounds a note of caution.
“It’s like when we used to use old cameras: the film was cheap, but the developing was really expensive,” Dr. Sawaya said. “So it’s not necessarily about the tests being cheap, it’s about the cascade of events [that follow].”
Follow-up for cervical cancer can be more hazardous for a postmenopausal patient than for a younger woman, explained Dr. Sawaya, because the transformation zone of the cervix may be difficult to see on colposcopy. Instead of a straightforward 5-minute procedure in the doctor’s office, the older patient may need the operating room simply to provide the first biopsy.
In addition, treatments such as cone biopsy, loop excision, or ablation are also more worrying for older women, said Dr. Sawaya, “So you start thinking about the risks of anesthesia, you start thinking about the risks of bleeding and infection, etc. And these have not been well described in older people.”
To add to the uncertainty about the merits and risks of hunting out cervical cancer in older women, a lot has changed in women’s health since 1996.
Explained Dr. Sawaya, “This stake was put in the ground in 1996, ... but since that time, life expectancy has gained 5 years. So a logical person would say, ‘Oh, well, let’s just say it should be 70 now, right?’ [But] can we even use old studies to inform the current cohort of women who are entering this 65-year-and-older age group?”
To answer all these questions, a 5-year, $3.3 million study funded by the NIH through the National Cancer Institute is now underway.
The project, named Comparative Effectiveness Research to Validate and Improve Cervical Cancer Screening (CERVICCS 2), will be led by Dr. Sawaya and Michael Silverberg, PhD, associate director of the Behavioral Health, Aging and Infectious Diseases Section of Kaiser Permanente Northern California’s Division of Research.
It’s not possible to conduct a true randomized controlled trial in this field of medicine for ethical reasons, so CERVICCS 2 will emulate a randomized study by following the fate of approximately 280,000 women older than 65 who were long-term members of two large health systems during 2005-2022. – both before and after the crucial age 65 cutoff.
The California study will also look at the downsides of diagnostic procedures and surgical interventions that follow a positive screening result after the age of 65 and the personal experiences of the women involved.
Dr. Sawaya and Dr. Silverberg’s team will use software that emulates a clinical trial by utilizing observational data to compare the benefits and risks of screening continuation or screening cessation after age 65.
In effect, after 27 years of loyalty to a recommendation supported by low-quality evidence, medicine will finally have a reliable answer to the question, Should we continue to look for cervical cancer in women over 65?
Dr. Sawaya concluded: “There’s very few things that are packaged away and thought to be just the truth. And this is why we always have to be vigilant. ... And that’s what keeps science so interesting and exciting.”
Dr. Sawaya has disclosed no relevant financial relationships. Dr. Feldman writes for UpToDate and receives several NIH grants.
A version of this article first appeared on Medscape.com.
“Did you love your wife?” asks a character in “Rose,” a book by Martin Cruz Smith.
“No, but she became a fact through perseverance,” the man replied.
Medicine also has such relationships, it seems – tentative ideas that turned into fact simply by existing long enough.
Age 65 as the cutoff for cervical screening may be one such example. It has existed for 27 years with limited science to back it up. That may soon change with the launch of a $3.3 million study that is being funded by the National Institutes of Health (NIH). The study is intended to provide a more solid foundation for the benefits and harms of cervical screening for women older than 65.
It’s an important issue: 20% of all cervical cancer cases are found in women who are older than 65. Most of these patients have late-stage disease, which can be fatal. In the United States, 35% of cervical cancer deaths occur after age 65. But women in this age group are usually no longer screened for cervical cancer.
Back in 1996, the U.S. Preventive Services Task Force recommended that for women at average risk with adequate prior screening, cervical screening should stop at the age of 65. This recommendation has been carried forward year after year and has been incorporated into several other guidelines.
For example, current guidelines from the American Cancer Society, the American College of Obstetricians and Gynecologists, and the USPSTF recommend that cervical screening stop at aged 65 for patients with adequate prior screening.
“Adequate screening” is defined as three consecutive normal Pap tests or two consecutive negative human papillomavirus tests or two consecutive negative co-tests within the prior 10 years, with the most recent screening within 5 years and with no precancerous lesions in the past 25 years.
This all sounds reasonable; however, for most women, medical records aren’t up to the task of providing a clean bill of cervical health over many decades.
Explained Sarah Feldman, MD, an associate professor in obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston: “You know, when a patient says to me at 65, ‘Should I continue screening?’ I say, ‘Do you have all your results?’ And they’ll say, ‘Well, I remember I had a sort of abnormal pap 15 years ago,’ and I say, ‘All right; well, who knows what that was?’ So I’ll continue screening.”
According to George Sawaya, MD, professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Francisco, up to 60% of women do not meet the criteria to end screening at age 65. This means that each year in the United States, approximately 1.7 million women turn 65 and should, in theory, continue to undergo screening for cervical cancer.
Unfortunately, the evidence base for the harms and benefits of cervical screening after age 65 is almost nonexistent – at least by the current standards of evidence-based medicine.
“We need to be clear that we don’t really know the appropriateness of the screening after 65,” said Dr. Sawaya, “which is ironic, because cervical cancer screening is probably the most commonly implemented cancer screening test in the country because it starts so early and ends so late and it’s applied so frequently.”
Dr. Feldman agrees that the age 65 cutoff is “somewhat arbitrary.” She said, “Why don’t they want to consider it continuing past 65? I don’t really understand, I have to be honest with you.”
So what’s the scientific evidence backing up the 27-year-old recommendation?
In 2018, the USPSTF’s cervical-screening guidelines concluded “with moderate certainty that the benefits of screening in women older than 65 years who have had adequate prior screening and are not otherwise at high risk for cervical cancer do not outweigh the potential harms.”
This recommendation was based on a new decision model commissioned by the USPSTF. The model was needed because, as noted by the guidelines’ authors, “None of the screening trials enrolled women older than 65 years, so direct evidence on when to stop screening is not available.”
In 2020, the ACS carried out a fresh literature review and published its own recommendations. The ACS concluded that “the evidence for the effectiveness of screening beyond age 65 is limited, based solely on observational and modeling studies.”
As a result, the ACS assigned a “qualified recommendation” to the age-65 moratorium (defined as “less certainty about the balance of benefits and harms or about patients’ values and preferences”).
Most recently, the 2021 Updated Cervical Cancer Screening Guidelines, published by the American College of Obstetricians and Gynecologists, endorsed the recommendations of the USPSTF.
Dr. Sawaya said, “The whole issue about screening over 65 is complicated from a lot of perspectives. We don’t know a lot about the safety. We don’t really know a lot about patients’ perceptions of it. But we do know that there has to be an upper age limit after which screening is just simply imprudent.”
Dr. Sawaya acknowledges that there exists a “heck-why-not” attitude toward cervical screening after 65 among some physicians, given that the tests are quick and cheap and could save a life, but he sounds a note of caution.
“It’s like when we used to use old cameras: the film was cheap, but the developing was really expensive,” Dr. Sawaya said. “So it’s not necessarily about the tests being cheap, it’s about the cascade of events [that follow].”
Follow-up for cervical cancer can be more hazardous for a postmenopausal patient than for a younger woman, explained Dr. Sawaya, because the transformation zone of the cervix may be difficult to see on colposcopy. Instead of a straightforward 5-minute procedure in the doctor’s office, the older patient may need the operating room simply to provide the first biopsy.
In addition, treatments such as cone biopsy, loop excision, or ablation are also more worrying for older women, said Dr. Sawaya, “So you start thinking about the risks of anesthesia, you start thinking about the risks of bleeding and infection, etc. And these have not been well described in older people.”
To add to the uncertainty about the merits and risks of hunting out cervical cancer in older women, a lot has changed in women’s health since 1996.
Explained Dr. Sawaya, “This stake was put in the ground in 1996, ... but since that time, life expectancy has gained 5 years. So a logical person would say, ‘Oh, well, let’s just say it should be 70 now, right?’ [But] can we even use old studies to inform the current cohort of women who are entering this 65-year-and-older age group?”
To answer all these questions, a 5-year, $3.3 million study funded by the NIH through the National Cancer Institute is now underway.
The project, named Comparative Effectiveness Research to Validate and Improve Cervical Cancer Screening (CERVICCS 2), will be led by Dr. Sawaya and Michael Silverberg, PhD, associate director of the Behavioral Health, Aging and Infectious Diseases Section of Kaiser Permanente Northern California’s Division of Research.
It’s not possible to conduct a true randomized controlled trial in this field of medicine for ethical reasons, so CERVICCS 2 will emulate a randomized study by following the fate of approximately 280,000 women older than 65 who were long-term members of two large health systems during 2005-2022. – both before and after the crucial age 65 cutoff.
The California study will also look at the downsides of diagnostic procedures and surgical interventions that follow a positive screening result after the age of 65 and the personal experiences of the women involved.
Dr. Sawaya and Dr. Silverberg’s team will use software that emulates a clinical trial by utilizing observational data to compare the benefits and risks of screening continuation or screening cessation after age 65.
In effect, after 27 years of loyalty to a recommendation supported by low-quality evidence, medicine will finally have a reliable answer to the question, Should we continue to look for cervical cancer in women over 65?
Dr. Sawaya concluded: “There’s very few things that are packaged away and thought to be just the truth. And this is why we always have to be vigilant. ... And that’s what keeps science so interesting and exciting.”
Dr. Sawaya has disclosed no relevant financial relationships. Dr. Feldman writes for UpToDate and receives several NIH grants.
A version of this article first appeared on Medscape.com.
Magnesium-rich diet linked to lower dementia risk
Investigators studied more than 6,000 cognitively healthy individuals, aged 40-73, and found that those who consumed more than 550 mg of magnesium daily had a brain age approximately 1 year younger by age 55 years, compared with a person who consumed a normal magnesium intake (~360 mg per day).
“This research highlights the potential benefits of a diet high in magnesium and the role it plays in promoting good brain health,” lead author Khawlah Alateeq, a PhD candidate in neuroscience at Australian National University’s National Centre for Epidemiology and Population Health, said in an interview.
Clinicians “can use [the findings] to counsel patients on the benefits of increasing magnesium intake through a healthy diet and monitoring magnesium levels to prevent deficiencies,” she stated.
The study was published online in the European Journal of Nutrition.
Promising target
The researchers were motivated to conduct the study because of “the growing concern over the increasing prevalence of dementia,” Ms. Alateeq said.
“Since there is no cure for dementia, and the development of pharmacological treatment for dementia has been unsuccessful over the last 30 years, prevention has been suggested as an effective approach to address the issue,” she added.
Nutrition, Ms. Alateeq said, is a “modifiable risk factor that can influence brain health and is highly amenable to scalable and cost-effective interventions.” It represents “a promising target” for risk reduction at a population level.
Previous research shows individuals with lower magnesium levels are at higher risk for AD, while those with higher dietary magnesium intake may be at lower risk of progressing from normal aging to cognitive impairment.
Most previous studies, however, included participants older than age 60 years, and it’s “unclear when the neuroprotective effects of dietary magnesium become detectable,” the researchers note.
Moreover, dietary patterns change and fluctuate, potentially leading to changes in magnesium intake over time. These changes may have as much impact as absolute magnesium at any point in time.
In light of the “current lack of understanding of when and to what extent dietary magnesium exerts its protective effects on the brain,” the researchers examined the association between magnesium trajectories over time, brain matter, and white matter lesions.
They also examined the association between magnesium and several different blood pressure measures (mean arterial pressure, systolic blood pressure, diastolic blood pressure, and pulse pressure).
Since cardiovascular health, neurodegeneration, and brain shrinkage patterns differ between men and women, the researchers stratified their analyses by sex.
Brain volume differences
The researchers analyzed the dietary magnesium intake of 6,001 individuals (mean age, 55.3 years) selected from the UK Biobank – a prospective cohort study of participants aged 37-73 at baseline, who were assessed between 2005 and 2023.
For the current study, only participants with baseline DBP and SBP measurements and structural MRI scans were included. Participants were also required to be free of neurologic disorders and to have an available record of dietary magnesium intake.
Covariates included age, sex, education, health conditions, smoking status, body mass index, amount of physical activity, smoking status, and alcohol intake.
Over a 16-month period, participants completed an online questionnaire five times. Their responses were used to calculate daily magnesium intake. Foods of particular interest included leafy green vegetables, legumes, nuts, seeds, and whole grains, all of which are magnesium rich.
They used latent class analysis (LCA) to “identify mutually exclusive subgroup (classes) of magnesium intake trajectory separately for men and women.”
Men had a slightly higher prevalence of BP medication and diabetes, compared with women, and postmenopausal women had a higher prevalence of BP medication and diabetes, compared with premenopausal women.
Compared with lower baseline magnesium intake, higher baseline dietary intake of magnesium was associated with larger brain volumes in several regions in both men and women.
The latent class analysis identified three classes of magnesium intake:
In women in particular, the “high-decreasing” trajectory was significantly associated with larger brain volumes, compared with the “normal-stable” trajectory, while the “low-increasing” trajectory was associated with smaller brain volumes.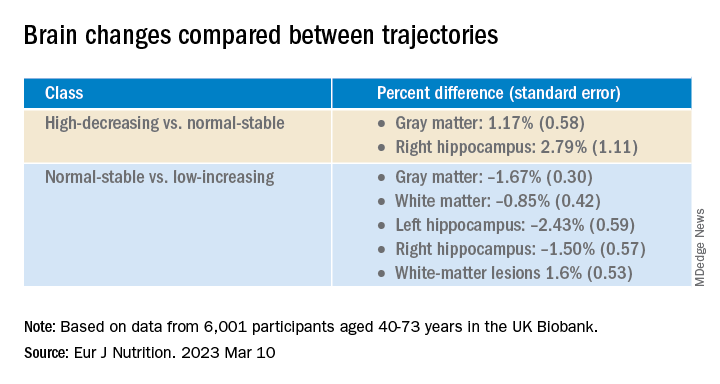
Even an increase of 1 mg of magnesium per day (above 350 mg/day) made a difference in brain volume, especially in women. The changes associated with every 1-mg increase are found in the table below: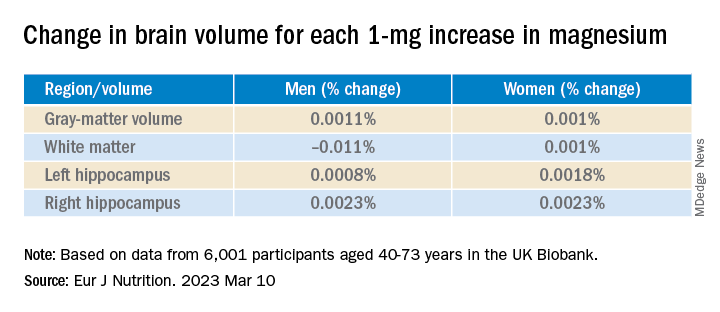
Associations between magnesium and BP measures were “mostly nonsignificant,” the researchers say, and the neuroprotective effect of higher magnesium intake in the high-decreasing trajectory was greater in postmenopausal versus premenopausal women.
“Our models indicate that compared to somebody with a normal magnesium intake (~350 mg per day), somebody in the top quartile of magnesium intake (≥ 550 mg per day) would be predicted to have a ~0.20% larger GM and ~0.46% larger RHC,” the authors summarize.
“In a population with an average age of 55 years, this effect corresponds to ~1 year of typical aging,” they note. “In other words, if this effect is generalizable to other populations, a 41% increase in magnesium intake may lead to significantly better brain health.”
Although the exact mechanisms underlying magnesium’s protective effects are “not yet clearly understood, there’s considerable evidence that magnesium levels are related to better cardiovascular health. Magnesium supplementation has been found to decrease blood pressure – and high blood pressure is a well-established risk factor for dementia,” said Ms. Alateeq.
Association, not causation
Yuko Hara, PhD, director of Aging and Prevention, Alzheimer’s Drug Discovery Foundation, noted that the study is observational and therefore shows an association, not causation.
“People eating a high-magnesium diet may also be eating a brain-healthy diet and getting high levels of nutrients/minerals other than magnesium alone,” suggested Dr. Hara, who was not involved with the study.
She noted that many foods are good sources of magnesium, including spinach, almonds, cashews, legumes, yogurt, brown rice, and avocados.
“Eating a brain-healthy diet (for example, the Mediterranean diet) is one of the Seven Steps to Protect Your Cognitive Vitality that ADDF’s Cognitive Vitality promotes,” she said.
Open Access funding was enabled and organized by the Council of Australian University Librarians and its Member Institutions. Ms. Alateeq, her co-authors, and Dr. Hara declare no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Investigators studied more than 6,000 cognitively healthy individuals, aged 40-73, and found that those who consumed more than 550 mg of magnesium daily had a brain age approximately 1 year younger by age 55 years, compared with a person who consumed a normal magnesium intake (~360 mg per day).
“This research highlights the potential benefits of a diet high in magnesium and the role it plays in promoting good brain health,” lead author Khawlah Alateeq, a PhD candidate in neuroscience at Australian National University’s National Centre for Epidemiology and Population Health, said in an interview.
Clinicians “can use [the findings] to counsel patients on the benefits of increasing magnesium intake through a healthy diet and monitoring magnesium levels to prevent deficiencies,” she stated.
The study was published online in the European Journal of Nutrition.
Promising target
The researchers were motivated to conduct the study because of “the growing concern over the increasing prevalence of dementia,” Ms. Alateeq said.
“Since there is no cure for dementia, and the development of pharmacological treatment for dementia has been unsuccessful over the last 30 years, prevention has been suggested as an effective approach to address the issue,” she added.
Nutrition, Ms. Alateeq said, is a “modifiable risk factor that can influence brain health and is highly amenable to scalable and cost-effective interventions.” It represents “a promising target” for risk reduction at a population level.
Previous research shows individuals with lower magnesium levels are at higher risk for AD, while those with higher dietary magnesium intake may be at lower risk of progressing from normal aging to cognitive impairment.
Most previous studies, however, included participants older than age 60 years, and it’s “unclear when the neuroprotective effects of dietary magnesium become detectable,” the researchers note.
Moreover, dietary patterns change and fluctuate, potentially leading to changes in magnesium intake over time. These changes may have as much impact as absolute magnesium at any point in time.
In light of the “current lack of understanding of when and to what extent dietary magnesium exerts its protective effects on the brain,” the researchers examined the association between magnesium trajectories over time, brain matter, and white matter lesions.
They also examined the association between magnesium and several different blood pressure measures (mean arterial pressure, systolic blood pressure, diastolic blood pressure, and pulse pressure).
Since cardiovascular health, neurodegeneration, and brain shrinkage patterns differ between men and women, the researchers stratified their analyses by sex.
Brain volume differences
The researchers analyzed the dietary magnesium intake of 6,001 individuals (mean age, 55.3 years) selected from the UK Biobank – a prospective cohort study of participants aged 37-73 at baseline, who were assessed between 2005 and 2023.
For the current study, only participants with baseline DBP and SBP measurements and structural MRI scans were included. Participants were also required to be free of neurologic disorders and to have an available record of dietary magnesium intake.
Covariates included age, sex, education, health conditions, smoking status, body mass index, amount of physical activity, smoking status, and alcohol intake.
Over a 16-month period, participants completed an online questionnaire five times. Their responses were used to calculate daily magnesium intake. Foods of particular interest included leafy green vegetables, legumes, nuts, seeds, and whole grains, all of which are magnesium rich.
They used latent class analysis (LCA) to “identify mutually exclusive subgroup (classes) of magnesium intake trajectory separately for men and women.”
Men had a slightly higher prevalence of BP medication and diabetes, compared with women, and postmenopausal women had a higher prevalence of BP medication and diabetes, compared with premenopausal women.
Compared with lower baseline magnesium intake, higher baseline dietary intake of magnesium was associated with larger brain volumes in several regions in both men and women.
The latent class analysis identified three classes of magnesium intake:
In women in particular, the “high-decreasing” trajectory was significantly associated with larger brain volumes, compared with the “normal-stable” trajectory, while the “low-increasing” trajectory was associated with smaller brain volumes.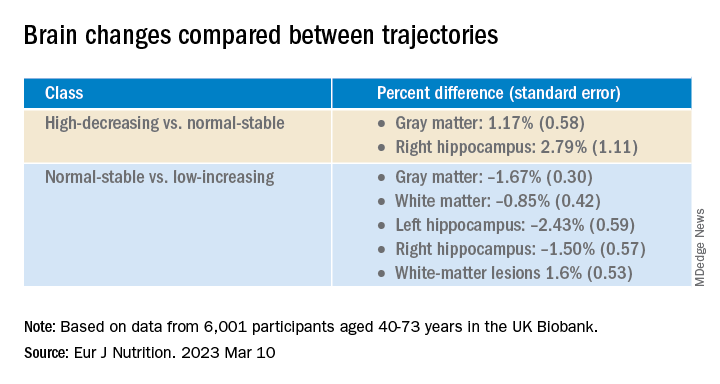
Even an increase of 1 mg of magnesium per day (above 350 mg/day) made a difference in brain volume, especially in women. The changes associated with every 1-mg increase are found in the table below: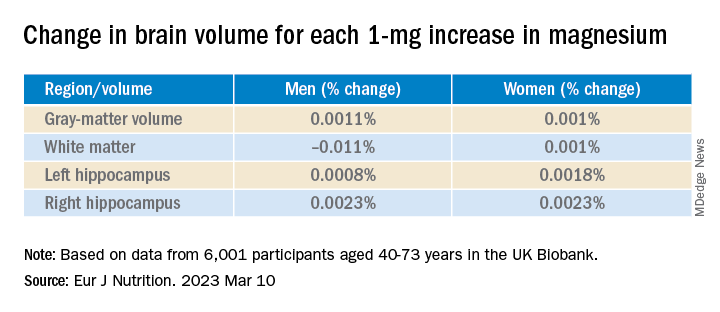
Associations between magnesium and BP measures were “mostly nonsignificant,” the researchers say, and the neuroprotective effect of higher magnesium intake in the high-decreasing trajectory was greater in postmenopausal versus premenopausal women.
“Our models indicate that compared to somebody with a normal magnesium intake (~350 mg per day), somebody in the top quartile of magnesium intake (≥ 550 mg per day) would be predicted to have a ~0.20% larger GM and ~0.46% larger RHC,” the authors summarize.
“In a population with an average age of 55 years, this effect corresponds to ~1 year of typical aging,” they note. “In other words, if this effect is generalizable to other populations, a 41% increase in magnesium intake may lead to significantly better brain health.”
Although the exact mechanisms underlying magnesium’s protective effects are “not yet clearly understood, there’s considerable evidence that magnesium levels are related to better cardiovascular health. Magnesium supplementation has been found to decrease blood pressure – and high blood pressure is a well-established risk factor for dementia,” said Ms. Alateeq.
Association, not causation
Yuko Hara, PhD, director of Aging and Prevention, Alzheimer’s Drug Discovery Foundation, noted that the study is observational and therefore shows an association, not causation.
“People eating a high-magnesium diet may also be eating a brain-healthy diet and getting high levels of nutrients/minerals other than magnesium alone,” suggested Dr. Hara, who was not involved with the study.
She noted that many foods are good sources of magnesium, including spinach, almonds, cashews, legumes, yogurt, brown rice, and avocados.
“Eating a brain-healthy diet (for example, the Mediterranean diet) is one of the Seven Steps to Protect Your Cognitive Vitality that ADDF’s Cognitive Vitality promotes,” she said.
Open Access funding was enabled and organized by the Council of Australian University Librarians and its Member Institutions. Ms. Alateeq, her co-authors, and Dr. Hara declare no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Investigators studied more than 6,000 cognitively healthy individuals, aged 40-73, and found that those who consumed more than 550 mg of magnesium daily had a brain age approximately 1 year younger by age 55 years, compared with a person who consumed a normal magnesium intake (~360 mg per day).
“This research highlights the potential benefits of a diet high in magnesium and the role it plays in promoting good brain health,” lead author Khawlah Alateeq, a PhD candidate in neuroscience at Australian National University’s National Centre for Epidemiology and Population Health, said in an interview.
Clinicians “can use [the findings] to counsel patients on the benefits of increasing magnesium intake through a healthy diet and monitoring magnesium levels to prevent deficiencies,” she stated.
The study was published online in the European Journal of Nutrition.
Promising target
The researchers were motivated to conduct the study because of “the growing concern over the increasing prevalence of dementia,” Ms. Alateeq said.
“Since there is no cure for dementia, and the development of pharmacological treatment for dementia has been unsuccessful over the last 30 years, prevention has been suggested as an effective approach to address the issue,” she added.
Nutrition, Ms. Alateeq said, is a “modifiable risk factor that can influence brain health and is highly amenable to scalable and cost-effective interventions.” It represents “a promising target” for risk reduction at a population level.
Previous research shows individuals with lower magnesium levels are at higher risk for AD, while those with higher dietary magnesium intake may be at lower risk of progressing from normal aging to cognitive impairment.
Most previous studies, however, included participants older than age 60 years, and it’s “unclear when the neuroprotective effects of dietary magnesium become detectable,” the researchers note.
Moreover, dietary patterns change and fluctuate, potentially leading to changes in magnesium intake over time. These changes may have as much impact as absolute magnesium at any point in time.
In light of the “current lack of understanding of when and to what extent dietary magnesium exerts its protective effects on the brain,” the researchers examined the association between magnesium trajectories over time, brain matter, and white matter lesions.
They also examined the association between magnesium and several different blood pressure measures (mean arterial pressure, systolic blood pressure, diastolic blood pressure, and pulse pressure).
Since cardiovascular health, neurodegeneration, and brain shrinkage patterns differ between men and women, the researchers stratified their analyses by sex.
Brain volume differences
The researchers analyzed the dietary magnesium intake of 6,001 individuals (mean age, 55.3 years) selected from the UK Biobank – a prospective cohort study of participants aged 37-73 at baseline, who were assessed between 2005 and 2023.
For the current study, only participants with baseline DBP and SBP measurements and structural MRI scans were included. Participants were also required to be free of neurologic disorders and to have an available record of dietary magnesium intake.
Covariates included age, sex, education, health conditions, smoking status, body mass index, amount of physical activity, smoking status, and alcohol intake.
Over a 16-month period, participants completed an online questionnaire five times. Their responses were used to calculate daily magnesium intake. Foods of particular interest included leafy green vegetables, legumes, nuts, seeds, and whole grains, all of which are magnesium rich.
They used latent class analysis (LCA) to “identify mutually exclusive subgroup (classes) of magnesium intake trajectory separately for men and women.”
Men had a slightly higher prevalence of BP medication and diabetes, compared with women, and postmenopausal women had a higher prevalence of BP medication and diabetes, compared with premenopausal women.
Compared with lower baseline magnesium intake, higher baseline dietary intake of magnesium was associated with larger brain volumes in several regions in both men and women.
The latent class analysis identified three classes of magnesium intake:
In women in particular, the “high-decreasing” trajectory was significantly associated with larger brain volumes, compared with the “normal-stable” trajectory, while the “low-increasing” trajectory was associated with smaller brain volumes.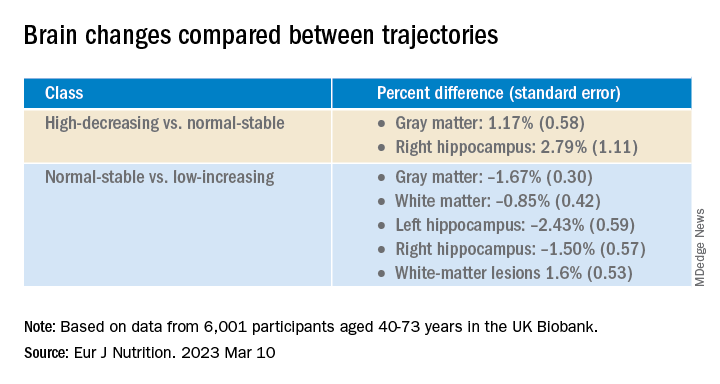
Even an increase of 1 mg of magnesium per day (above 350 mg/day) made a difference in brain volume, especially in women. The changes associated with every 1-mg increase are found in the table below: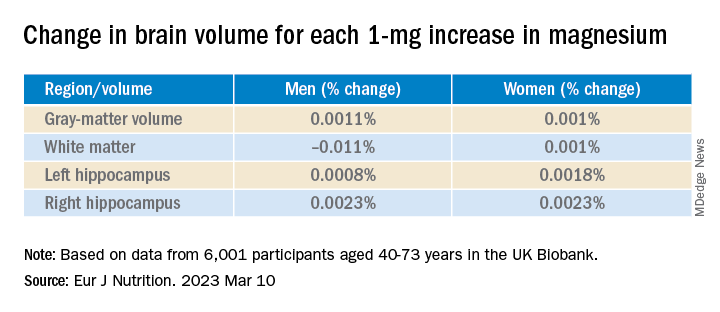
Associations between magnesium and BP measures were “mostly nonsignificant,” the researchers say, and the neuroprotective effect of higher magnesium intake in the high-decreasing trajectory was greater in postmenopausal versus premenopausal women.
“Our models indicate that compared to somebody with a normal magnesium intake (~350 mg per day), somebody in the top quartile of magnesium intake (≥ 550 mg per day) would be predicted to have a ~0.20% larger GM and ~0.46% larger RHC,” the authors summarize.
“In a population with an average age of 55 years, this effect corresponds to ~1 year of typical aging,” they note. “In other words, if this effect is generalizable to other populations, a 41% increase in magnesium intake may lead to significantly better brain health.”
Although the exact mechanisms underlying magnesium’s protective effects are “not yet clearly understood, there’s considerable evidence that magnesium levels are related to better cardiovascular health. Magnesium supplementation has been found to decrease blood pressure – and high blood pressure is a well-established risk factor for dementia,” said Ms. Alateeq.
Association, not causation
Yuko Hara, PhD, director of Aging and Prevention, Alzheimer’s Drug Discovery Foundation, noted that the study is observational and therefore shows an association, not causation.
“People eating a high-magnesium diet may also be eating a brain-healthy diet and getting high levels of nutrients/minerals other than magnesium alone,” suggested Dr. Hara, who was not involved with the study.
She noted that many foods are good sources of magnesium, including spinach, almonds, cashews, legumes, yogurt, brown rice, and avocados.
“Eating a brain-healthy diet (for example, the Mediterranean diet) is one of the Seven Steps to Protect Your Cognitive Vitality that ADDF’s Cognitive Vitality promotes,” she said.
Open Access funding was enabled and organized by the Council of Australian University Librarians and its Member Institutions. Ms. Alateeq, her co-authors, and Dr. Hara declare no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM EUROPEAN JOURNAL OF NUTRITION