User login
Three wild technologies about to change health care
When I was a child, I watched syndicated episodes of the original “Star Trek.” I was dazzled by the space travel, sure, but also the medical technology.
A handheld “tricorder” detected diseases, while an intramuscular injector (“hypospray”) could treat them. Sickbay “biobeds” came with real-time health monitors that looked futuristic at the time but seem primitive today.
Such visions inspired a lot of us kids to pursue science. Little did we know the real-life advances many of us would see in our lifetimes.
Artificial intelligence helping to spot disease, robots performing surgery, even video calls between doctor and patient – all these once sounded fantastical but now happen in clinical care.
Now, in the 23rd year of the 21st century, you might not believe wht we’ll be capable of next. Three especially wild examples are moving closer to clinical reality.
Human hibernation
Captain America, Han Solo, and “Star Trek” villain Khan – all were preserved at low temperatures and then revived, waking up alive and well months, decades, or centuries later. These are fictional examples, to be sure, but the science they’re rooted in is real.
(In one extreme case, a climber survived after almost 9 hours of efforts to revive him.)
Useful for a space traveler? Maybe not. But it’s potentially huge for someone with life-threatening injuries from a car accident or a gunshot wound.
That’s the thinking behind a breakthrough procedure that came after decades of research on pigs and dogs, now in a clinical trial. The idea: A person with massive blood loss whose heart has stopped is injected with an ice-cold fluid, cooling them from the inside, down to about 50° F.
Doctors already induce more modest hypothermia to protect the brain and other organs after cardiac arrest and during surgery on the aortic arch (the main artery carrying blood from the heart).
But this experimental procedure – called emergency preservation and resuscitation (EPR) – goes far beyond that, dramatically “decreasing the body’s need for oxygen and blood flow,” says Samuel Tisherman, MD, a trauma surgeon at the University of Maryland Medical Center and the trial’s lead researcher. This puts the patient in a state of suspended animation that “could buy time for surgeons to stop the bleeding and save more of these patients.”
The technique has been done on at least six patients, though none were reported to survive. The trial is expected to include 20 people by the time it wraps up in December, according to the listing on the U.S. clinical trials database. Though given the strict requirements for candidates (emergency trauma victims who are not likely to survive), one can’t exactly rely on a set schedule.
Still, the technology is promising. Someday we may even use it to keep patients in suspended animation for months or years, experts predict, helping astronauts through decades-long spaceflights, or stalling death in sick patients awaiting a cure.
Artificial womb
Another sci-fi classic: growing human babies outside the womb. Think the fetus fields from “The Matrix,” or the frozen embryos in “Alien: Covenant.”
In 1923, British biologist J.B.S. Haldane coined a term for that – ectogenesis. He predicted that 70% of pregnancies would take place, from fertilization to birth, in artificial wombs by 2074. That many seems unlikely, but the timeline is on track.
Developing an embryo outside the womb is already routine in in vitro fertilization. And technology enables preterm babies to survive through much of the second half of gestation. Normal human pregnancy is 40 weeks, and the youngest preterm baby ever to survive was 21 weeks and 1 day old, just a few days younger than a smattering of others who lived.
The biggest obstacle for babies younger than that is lung viability. Mechanical ventilation can damage the lungs and lead to a chronic (sometimes fatal) lung disease known as bronchopulmonary dysplasia. Avoiding this would mean figuring out a way to maintain fetal circulation – the intricate system that delivers oxygenated blood from the placenta to the fetus via the umbilical cord. Researchers at Children’s Hospital of Philadelphia have done this using a fetal lamb.
The key to their invention is a substitute placenta: an oxygenator connected to the lamb’s umbilical cord. Tubes inserted through the umbilical vein and arteries carry oxygenated blood from the “placenta” to the fetus, and deoxygenated blood back out. The lamb resides in an artificial, fluid-filled amniotic sac until its lungs and other organs are developed.
Fertility treatment could benefit, too. “An artificial womb may substitute in situations in which a gestational carrier – surrogate – is indicated,” says Paula Amato, MD, a professor of obstetrics and gynecology at Oregon Health and Science University, Portland. (Dr. Amato is not involved in the CHOP research.) For example: when the mother is missing a uterus or can’t carry a pregnancy safely.
No date is set for clinical trials yet. But according to the research, the main difference between human and lamb may come down to size. A lamb’s umbilical vessels are larger, so feeding in a tube is easier. With today’s advances in miniaturizing surgical methods, that seems like a challenge scientists can overcome.
Messenger RNA therapeutics
Back to “Star Trek.” The hypospray injector’s contents could cure just about any disease, even one newly discovered on a strange planet. That’s not unlike messenger RNA (mRNA) technology, a breakthrough that enabled scientists to quickly develop some of the first COVID-19 vaccines.
But vaccines are just the beginning of what this technology can do.
A whole field of immunotherapy is emerging that uses mRNA to deliver instructions to produce chimeric antigen receptor–modified immune cells (CAR-modified immune cells). These cells are engineered to target diseased cells and tissues, like cancer cells and harmful fibroblasts (scar tissue) that promote fibrosis in, for example, the heart and lungs.
The field is bursting with rodent research, and clinical trials have started for treating some advanced-stage malignancies.
Actual clinical use may be years away, but if all goes well, these medicines could help treat or even cure the core medical problems facing humanity. We’re talking cancer, heart disease, neurodegenerative disease – transforming one therapy into another by simply changing the mRNA’s “nucleotide sequence,” the blueprint containing instructions telling it what to do, and what disease to attack.
As this technology matures, we may start to feel as if we’re really on “Star Trek,” where Dr. Leonard “Bones” McCoy pulls out the same device to treat just about every disease or injury.
A version of this article first appeared on WebMD.com.
When I was a child, I watched syndicated episodes of the original “Star Trek.” I was dazzled by the space travel, sure, but also the medical technology.
A handheld “tricorder” detected diseases, while an intramuscular injector (“hypospray”) could treat them. Sickbay “biobeds” came with real-time health monitors that looked futuristic at the time but seem primitive today.
Such visions inspired a lot of us kids to pursue science. Little did we know the real-life advances many of us would see in our lifetimes.
Artificial intelligence helping to spot disease, robots performing surgery, even video calls between doctor and patient – all these once sounded fantastical but now happen in clinical care.
Now, in the 23rd year of the 21st century, you might not believe wht we’ll be capable of next. Three especially wild examples are moving closer to clinical reality.
Human hibernation
Captain America, Han Solo, and “Star Trek” villain Khan – all were preserved at low temperatures and then revived, waking up alive and well months, decades, or centuries later. These are fictional examples, to be sure, but the science they’re rooted in is real.
(In one extreme case, a climber survived after almost 9 hours of efforts to revive him.)
Useful for a space traveler? Maybe not. But it’s potentially huge for someone with life-threatening injuries from a car accident or a gunshot wound.
That’s the thinking behind a breakthrough procedure that came after decades of research on pigs and dogs, now in a clinical trial. The idea: A person with massive blood loss whose heart has stopped is injected with an ice-cold fluid, cooling them from the inside, down to about 50° F.
Doctors already induce more modest hypothermia to protect the brain and other organs after cardiac arrest and during surgery on the aortic arch (the main artery carrying blood from the heart).
But this experimental procedure – called emergency preservation and resuscitation (EPR) – goes far beyond that, dramatically “decreasing the body’s need for oxygen and blood flow,” says Samuel Tisherman, MD, a trauma surgeon at the University of Maryland Medical Center and the trial’s lead researcher. This puts the patient in a state of suspended animation that “could buy time for surgeons to stop the bleeding and save more of these patients.”
The technique has been done on at least six patients, though none were reported to survive. The trial is expected to include 20 people by the time it wraps up in December, according to the listing on the U.S. clinical trials database. Though given the strict requirements for candidates (emergency trauma victims who are not likely to survive), one can’t exactly rely on a set schedule.
Still, the technology is promising. Someday we may even use it to keep patients in suspended animation for months or years, experts predict, helping astronauts through decades-long spaceflights, or stalling death in sick patients awaiting a cure.
Artificial womb
Another sci-fi classic: growing human babies outside the womb. Think the fetus fields from “The Matrix,” or the frozen embryos in “Alien: Covenant.”
In 1923, British biologist J.B.S. Haldane coined a term for that – ectogenesis. He predicted that 70% of pregnancies would take place, from fertilization to birth, in artificial wombs by 2074. That many seems unlikely, but the timeline is on track.
Developing an embryo outside the womb is already routine in in vitro fertilization. And technology enables preterm babies to survive through much of the second half of gestation. Normal human pregnancy is 40 weeks, and the youngest preterm baby ever to survive was 21 weeks and 1 day old, just a few days younger than a smattering of others who lived.
The biggest obstacle for babies younger than that is lung viability. Mechanical ventilation can damage the lungs and lead to a chronic (sometimes fatal) lung disease known as bronchopulmonary dysplasia. Avoiding this would mean figuring out a way to maintain fetal circulation – the intricate system that delivers oxygenated blood from the placenta to the fetus via the umbilical cord. Researchers at Children’s Hospital of Philadelphia have done this using a fetal lamb.
The key to their invention is a substitute placenta: an oxygenator connected to the lamb’s umbilical cord. Tubes inserted through the umbilical vein and arteries carry oxygenated blood from the “placenta” to the fetus, and deoxygenated blood back out. The lamb resides in an artificial, fluid-filled amniotic sac until its lungs and other organs are developed.
Fertility treatment could benefit, too. “An artificial womb may substitute in situations in which a gestational carrier – surrogate – is indicated,” says Paula Amato, MD, a professor of obstetrics and gynecology at Oregon Health and Science University, Portland. (Dr. Amato is not involved in the CHOP research.) For example: when the mother is missing a uterus or can’t carry a pregnancy safely.
No date is set for clinical trials yet. But according to the research, the main difference between human and lamb may come down to size. A lamb’s umbilical vessels are larger, so feeding in a tube is easier. With today’s advances in miniaturizing surgical methods, that seems like a challenge scientists can overcome.
Messenger RNA therapeutics
Back to “Star Trek.” The hypospray injector’s contents could cure just about any disease, even one newly discovered on a strange planet. That’s not unlike messenger RNA (mRNA) technology, a breakthrough that enabled scientists to quickly develop some of the first COVID-19 vaccines.
But vaccines are just the beginning of what this technology can do.
A whole field of immunotherapy is emerging that uses mRNA to deliver instructions to produce chimeric antigen receptor–modified immune cells (CAR-modified immune cells). These cells are engineered to target diseased cells and tissues, like cancer cells and harmful fibroblasts (scar tissue) that promote fibrosis in, for example, the heart and lungs.
The field is bursting with rodent research, and clinical trials have started for treating some advanced-stage malignancies.
Actual clinical use may be years away, but if all goes well, these medicines could help treat or even cure the core medical problems facing humanity. We’re talking cancer, heart disease, neurodegenerative disease – transforming one therapy into another by simply changing the mRNA’s “nucleotide sequence,” the blueprint containing instructions telling it what to do, and what disease to attack.
As this technology matures, we may start to feel as if we’re really on “Star Trek,” where Dr. Leonard “Bones” McCoy pulls out the same device to treat just about every disease or injury.
A version of this article first appeared on WebMD.com.
When I was a child, I watched syndicated episodes of the original “Star Trek.” I was dazzled by the space travel, sure, but also the medical technology.
A handheld “tricorder” detected diseases, while an intramuscular injector (“hypospray”) could treat them. Sickbay “biobeds” came with real-time health monitors that looked futuristic at the time but seem primitive today.
Such visions inspired a lot of us kids to pursue science. Little did we know the real-life advances many of us would see in our lifetimes.
Artificial intelligence helping to spot disease, robots performing surgery, even video calls between doctor and patient – all these once sounded fantastical but now happen in clinical care.
Now, in the 23rd year of the 21st century, you might not believe wht we’ll be capable of next. Three especially wild examples are moving closer to clinical reality.
Human hibernation
Captain America, Han Solo, and “Star Trek” villain Khan – all were preserved at low temperatures and then revived, waking up alive and well months, decades, or centuries later. These are fictional examples, to be sure, but the science they’re rooted in is real.
(In one extreme case, a climber survived after almost 9 hours of efforts to revive him.)
Useful for a space traveler? Maybe not. But it’s potentially huge for someone with life-threatening injuries from a car accident or a gunshot wound.
That’s the thinking behind a breakthrough procedure that came after decades of research on pigs and dogs, now in a clinical trial. The idea: A person with massive blood loss whose heart has stopped is injected with an ice-cold fluid, cooling them from the inside, down to about 50° F.
Doctors already induce more modest hypothermia to protect the brain and other organs after cardiac arrest and during surgery on the aortic arch (the main artery carrying blood from the heart).
But this experimental procedure – called emergency preservation and resuscitation (EPR) – goes far beyond that, dramatically “decreasing the body’s need for oxygen and blood flow,” says Samuel Tisherman, MD, a trauma surgeon at the University of Maryland Medical Center and the trial’s lead researcher. This puts the patient in a state of suspended animation that “could buy time for surgeons to stop the bleeding and save more of these patients.”
The technique has been done on at least six patients, though none were reported to survive. The trial is expected to include 20 people by the time it wraps up in December, according to the listing on the U.S. clinical trials database. Though given the strict requirements for candidates (emergency trauma victims who are not likely to survive), one can’t exactly rely on a set schedule.
Still, the technology is promising. Someday we may even use it to keep patients in suspended animation for months or years, experts predict, helping astronauts through decades-long spaceflights, or stalling death in sick patients awaiting a cure.
Artificial womb
Another sci-fi classic: growing human babies outside the womb. Think the fetus fields from “The Matrix,” or the frozen embryos in “Alien: Covenant.”
In 1923, British biologist J.B.S. Haldane coined a term for that – ectogenesis. He predicted that 70% of pregnancies would take place, from fertilization to birth, in artificial wombs by 2074. That many seems unlikely, but the timeline is on track.
Developing an embryo outside the womb is already routine in in vitro fertilization. And technology enables preterm babies to survive through much of the second half of gestation. Normal human pregnancy is 40 weeks, and the youngest preterm baby ever to survive was 21 weeks and 1 day old, just a few days younger than a smattering of others who lived.
The biggest obstacle for babies younger than that is lung viability. Mechanical ventilation can damage the lungs and lead to a chronic (sometimes fatal) lung disease known as bronchopulmonary dysplasia. Avoiding this would mean figuring out a way to maintain fetal circulation – the intricate system that delivers oxygenated blood from the placenta to the fetus via the umbilical cord. Researchers at Children’s Hospital of Philadelphia have done this using a fetal lamb.
The key to their invention is a substitute placenta: an oxygenator connected to the lamb’s umbilical cord. Tubes inserted through the umbilical vein and arteries carry oxygenated blood from the “placenta” to the fetus, and deoxygenated blood back out. The lamb resides in an artificial, fluid-filled amniotic sac until its lungs and other organs are developed.
Fertility treatment could benefit, too. “An artificial womb may substitute in situations in which a gestational carrier – surrogate – is indicated,” says Paula Amato, MD, a professor of obstetrics and gynecology at Oregon Health and Science University, Portland. (Dr. Amato is not involved in the CHOP research.) For example: when the mother is missing a uterus or can’t carry a pregnancy safely.
No date is set for clinical trials yet. But according to the research, the main difference between human and lamb may come down to size. A lamb’s umbilical vessels are larger, so feeding in a tube is easier. With today’s advances in miniaturizing surgical methods, that seems like a challenge scientists can overcome.
Messenger RNA therapeutics
Back to “Star Trek.” The hypospray injector’s contents could cure just about any disease, even one newly discovered on a strange planet. That’s not unlike messenger RNA (mRNA) technology, a breakthrough that enabled scientists to quickly develop some of the first COVID-19 vaccines.
But vaccines are just the beginning of what this technology can do.
A whole field of immunotherapy is emerging that uses mRNA to deliver instructions to produce chimeric antigen receptor–modified immune cells (CAR-modified immune cells). These cells are engineered to target diseased cells and tissues, like cancer cells and harmful fibroblasts (scar tissue) that promote fibrosis in, for example, the heart and lungs.
The field is bursting with rodent research, and clinical trials have started for treating some advanced-stage malignancies.
Actual clinical use may be years away, but if all goes well, these medicines could help treat or even cure the core medical problems facing humanity. We’re talking cancer, heart disease, neurodegenerative disease – transforming one therapy into another by simply changing the mRNA’s “nucleotide sequence,” the blueprint containing instructions telling it what to do, and what disease to attack.
As this technology matures, we may start to feel as if we’re really on “Star Trek,” where Dr. Leonard “Bones” McCoy pulls out the same device to treat just about every disease or injury.
A version of this article first appeared on WebMD.com.
A new (old) drug joins the COVID fray, and guess what? It works
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
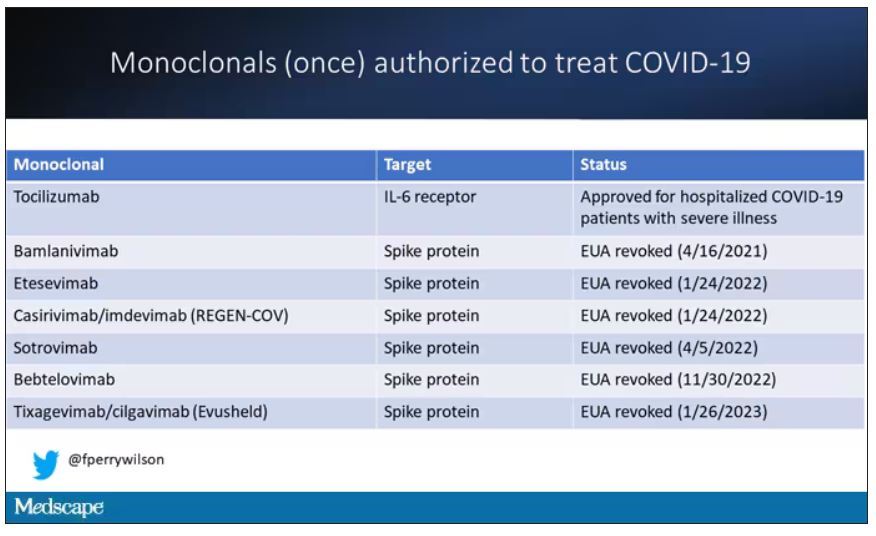
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.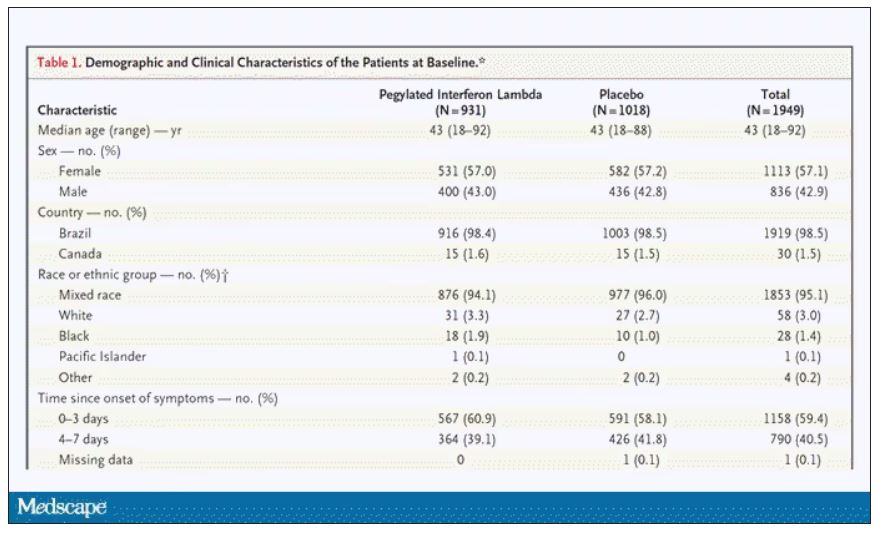
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.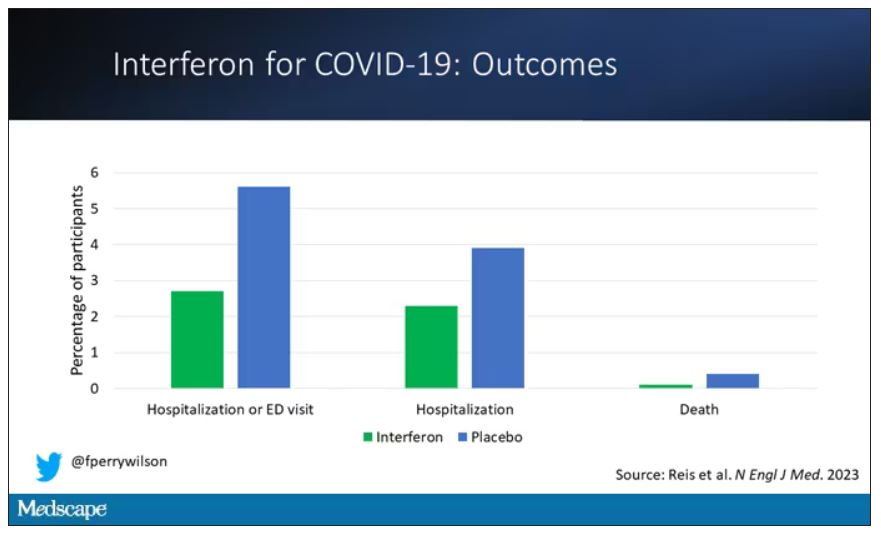
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.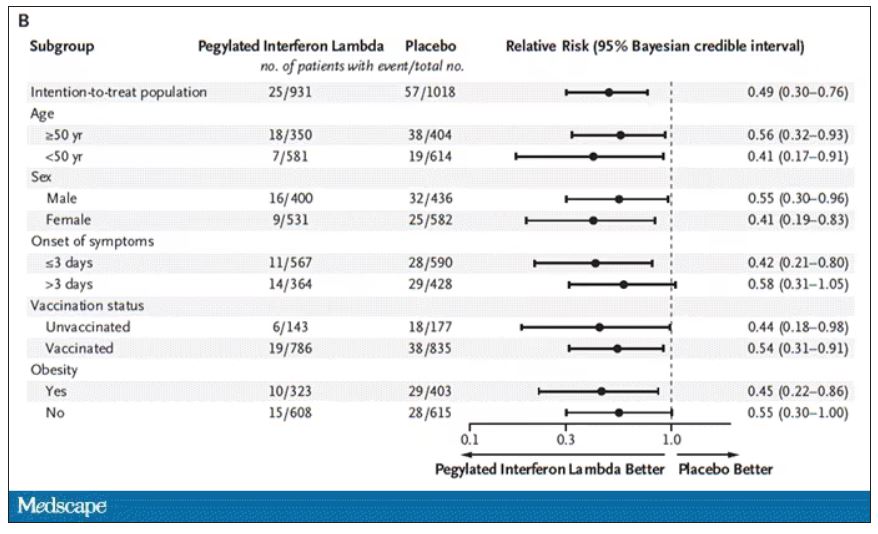
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.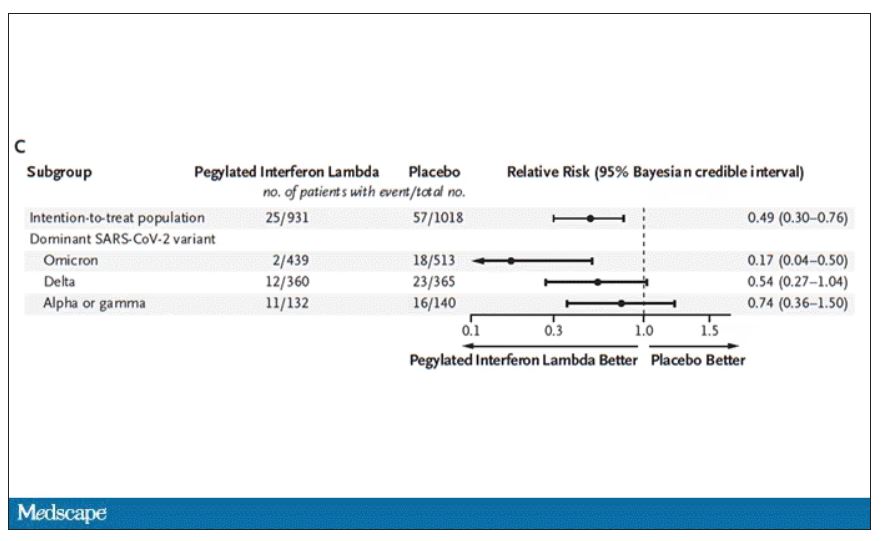
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.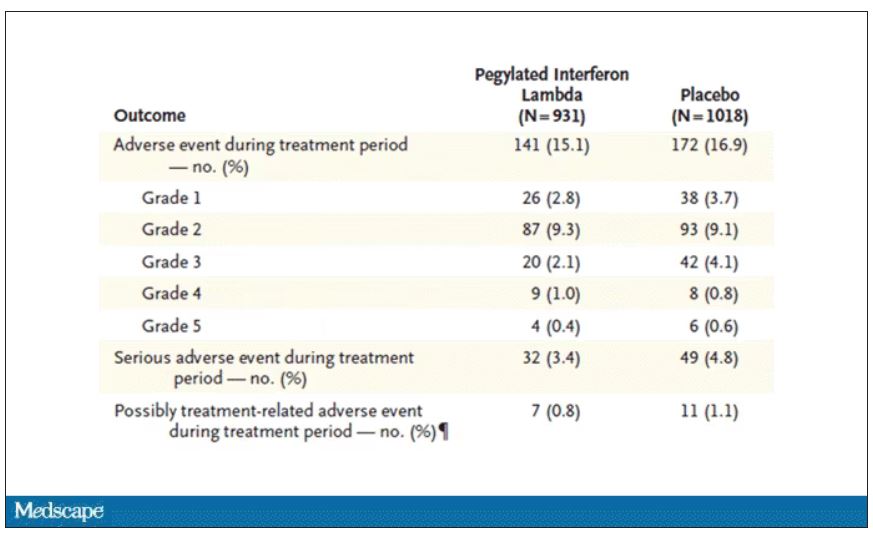
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
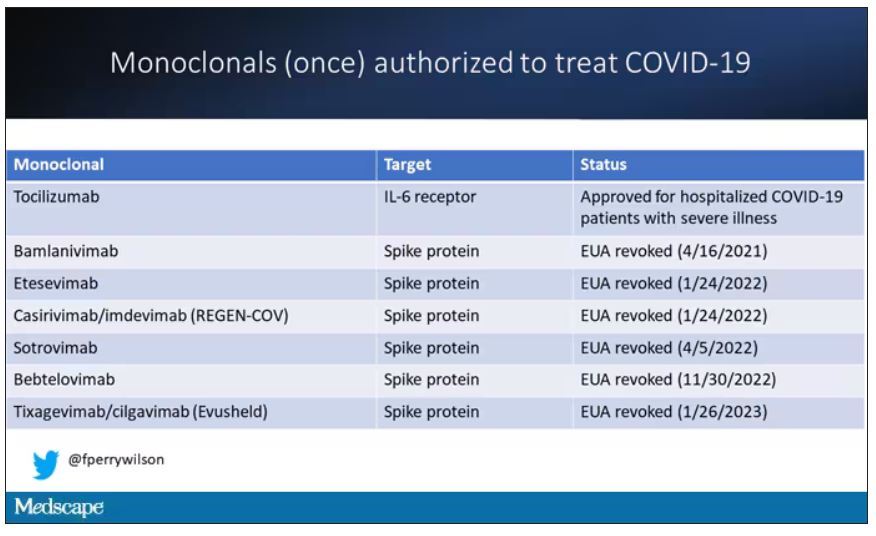
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.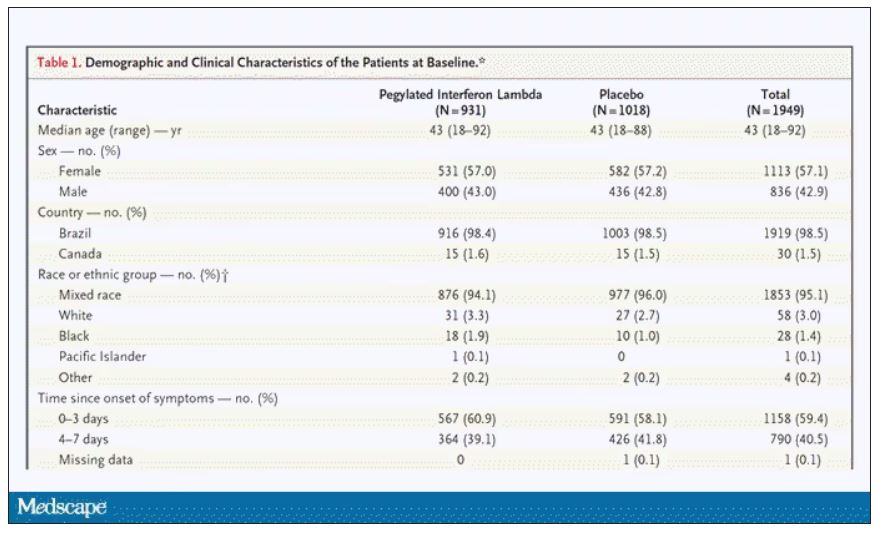
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.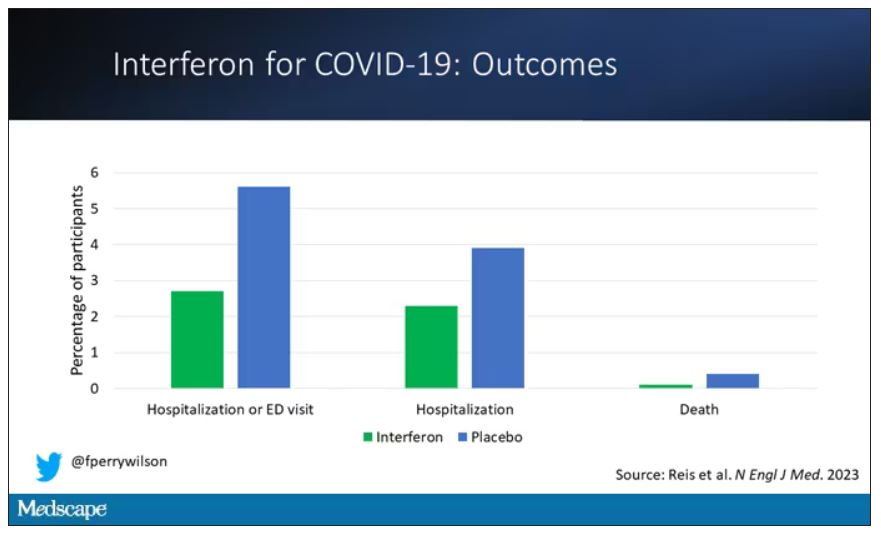
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.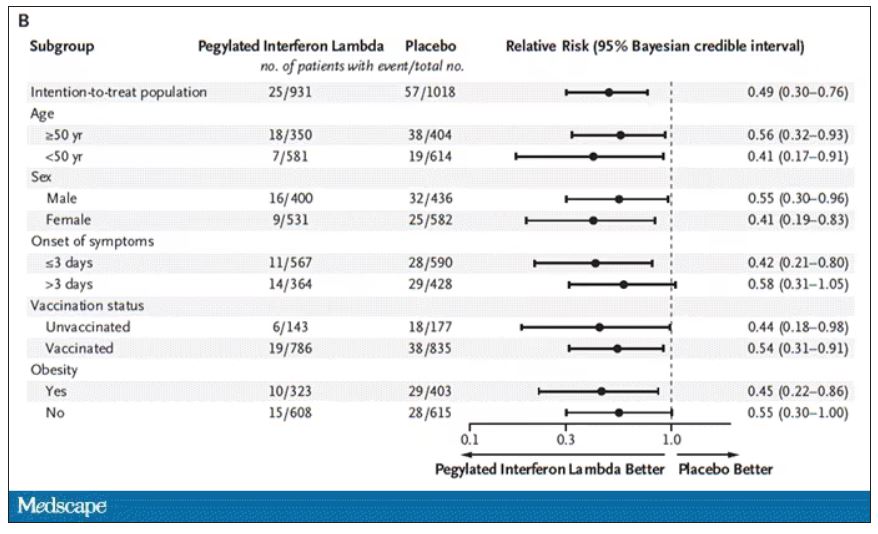
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.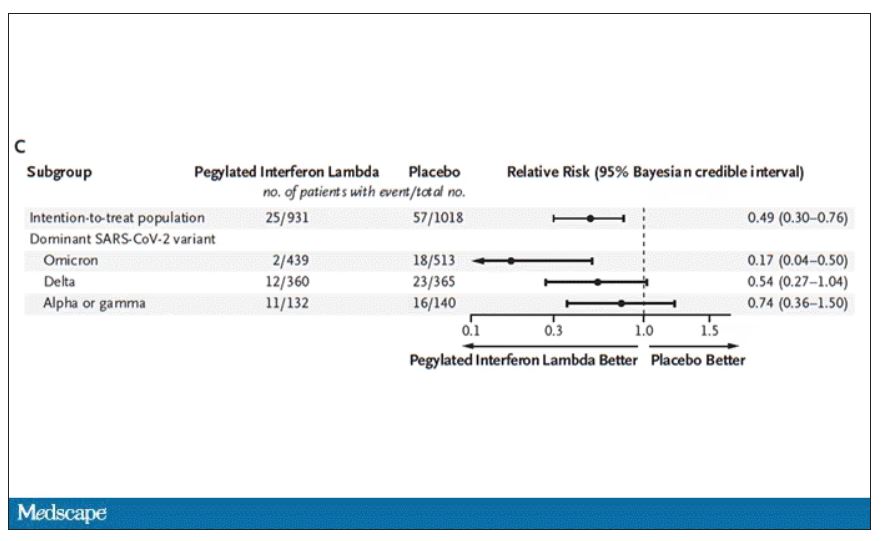
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.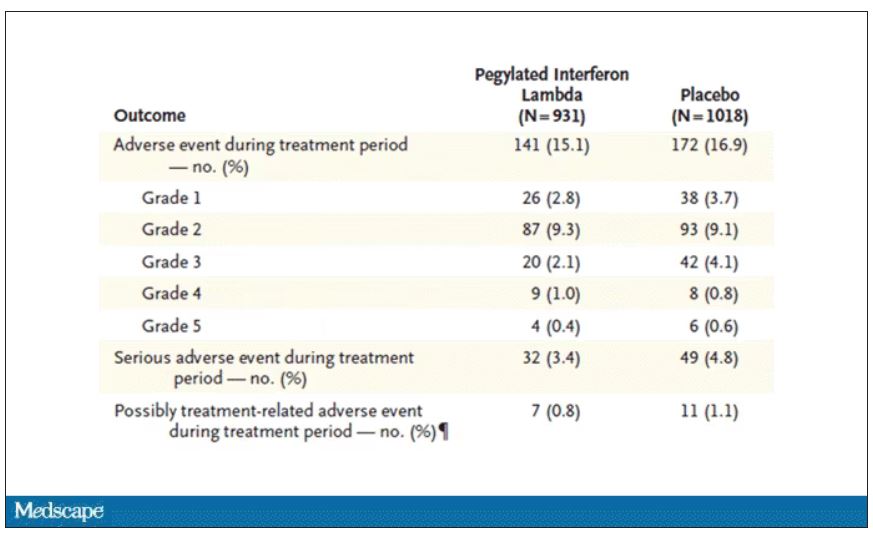
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
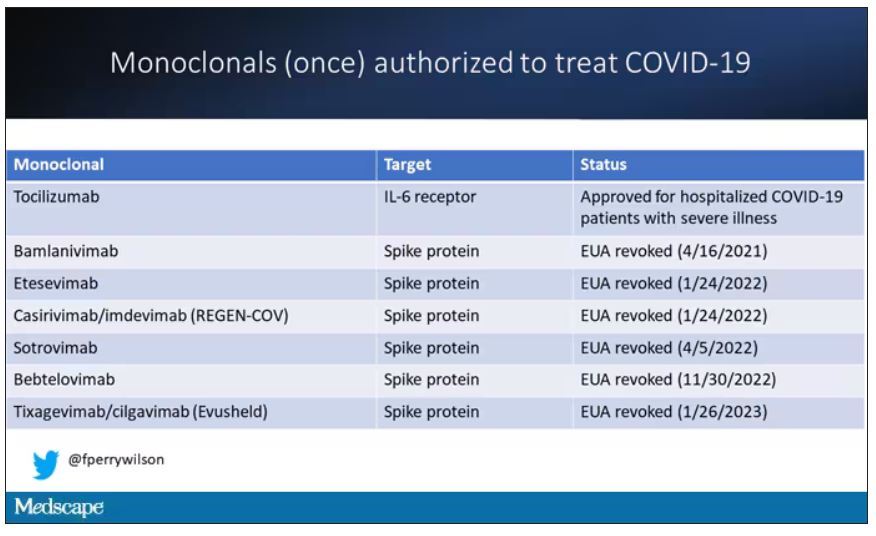
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.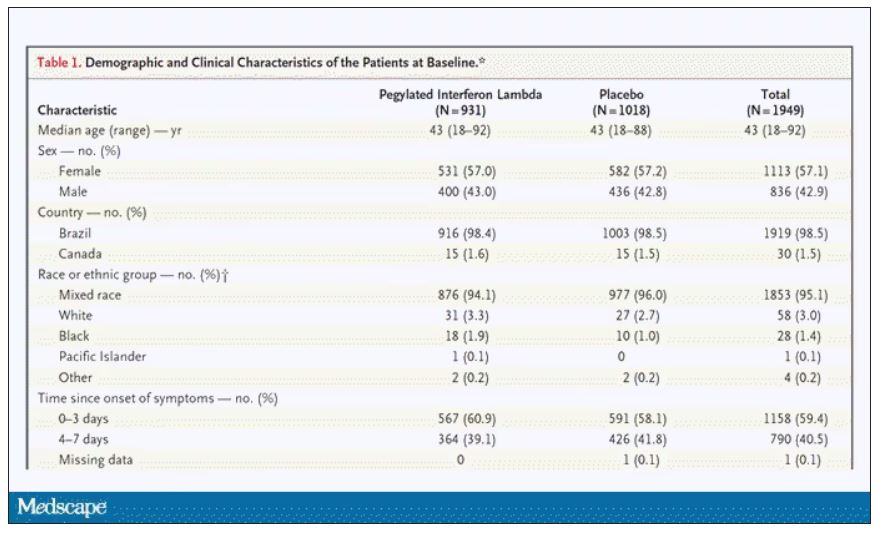
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.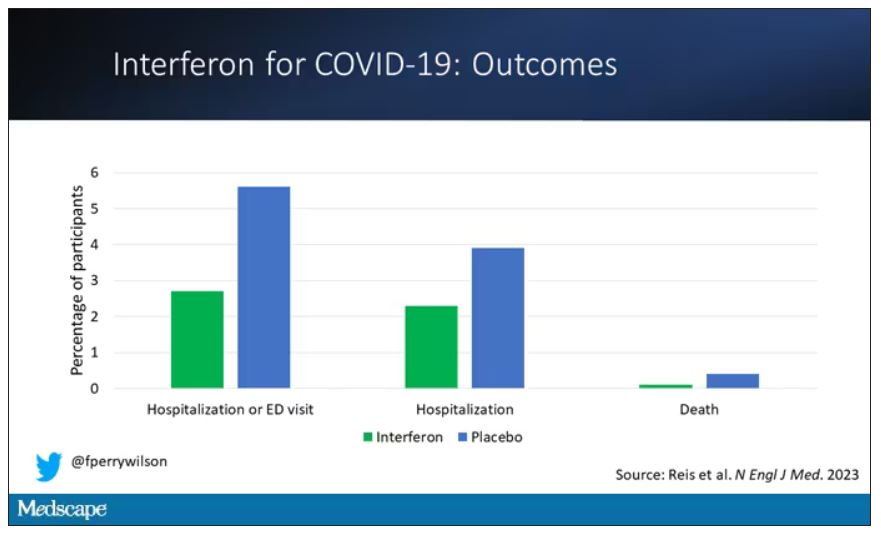
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.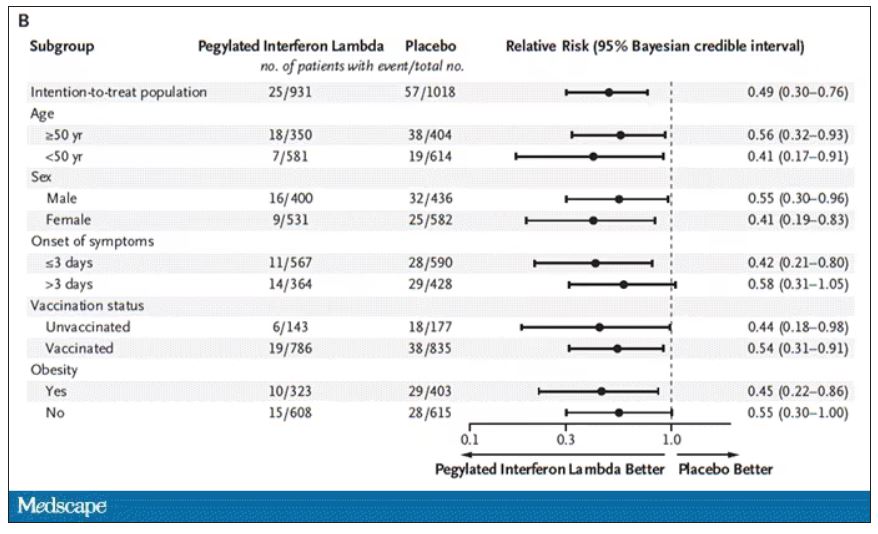
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.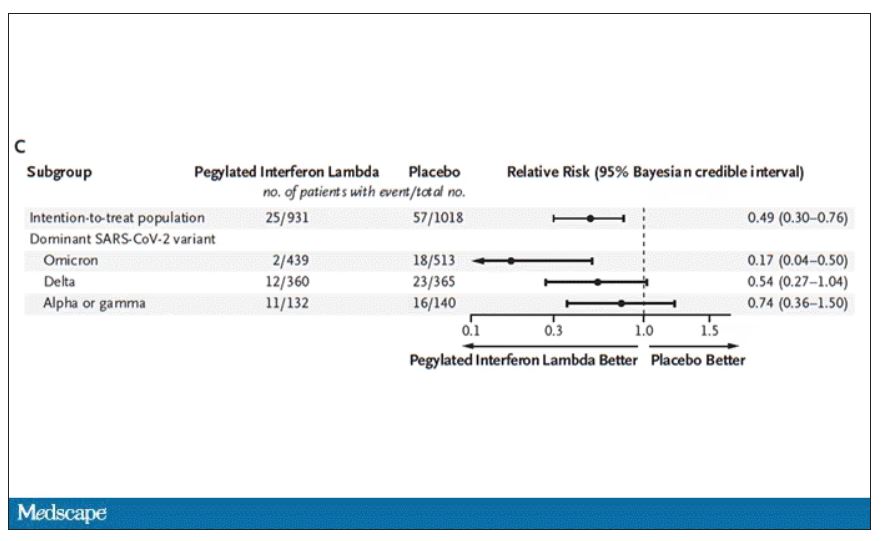
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.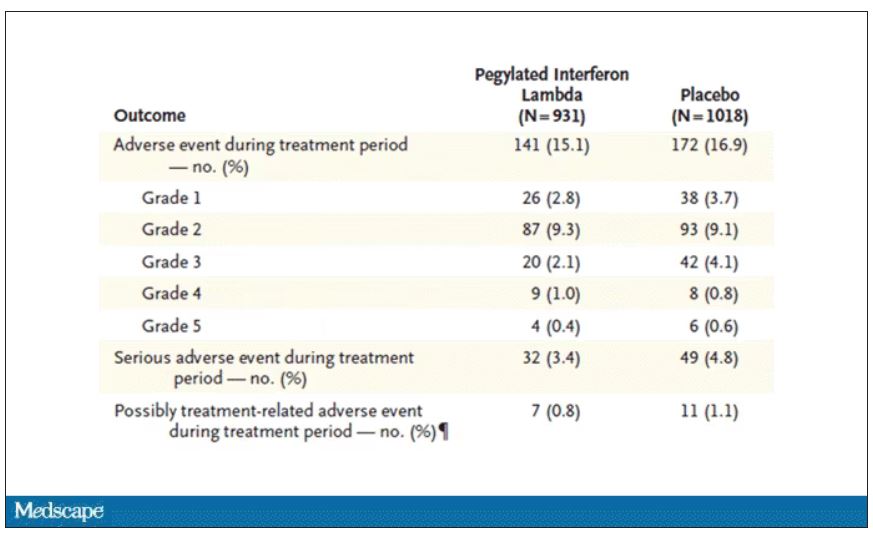
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Can pediatricians’ offices be urgent care centers again?
If you live in a suburban or semirural community you have seen at least one urgent care center open up in the last decade. They now number nearly 12,000 nationwide and are growing in number at a 7% rate. Urgent care center patient volume surged during the pandemic and an industry trade group reports it has risen 60% since 2019 (Meyerson N. Why urgent care centers are popping up everywhere. CNN Business. 2023 Jan 28).
According to a report on the CNN Business website, this growth is the result of “convenience, gaps in primary care, high costs of emergency room visits, and increased investment by health systems and equity groups.” Initially, these centers were generally staffed by physicians (70% in 2009) but as of 2022 this number has fallen to 16%. While there are conflicting data to support the claim that urgent care centers are overprescribing, it is pretty clear that their presence in a community encourages fragmented care and weakens established provider-patient relationships. One study has shown that although urgent care centers can prevent a costly emergency room visit ($1,649/visit) this advantage is offset by urgent care cost of more than $6,000.
In the same CNN report, Susan Kressly MD, chair of the AAP’s Private Payer Advocacy Advisory Committee, said: “There’s a need to keep up with society’s demand for quick turnaround, on-demand services that can’t be supported by underfunded primary care.”
Her observation suggests that there is an accelerating demand for timely primary care services. From my perch here in semirural Maine, I don’t see an increasing or unreasonable demand for timeliness by patients and families. Two decades ago, the practice I was in offered evening and weekend morning office hours and call-in times when patientsor parents could speak directly to a physician. These avenues of accessibility have disappeared community wide.
Back in the 1990s “the medical home” was all the buzz. We were encouraged to be the first and primary place to go for a broad range of preventive and responsive care. One-stop shopping at its best. Now it’s “knock, knock ... is anybody home?” Not if it’s getting dark, or it’s the weekend, or you have a minor injury. “Please call the urgent care center.”
I will admit that our dedicated call-in times were unusual and probably not sustainable for most practices. But, most practices back then would see children with acute illness and minor scrapes and trauma on a same-day basis. We dressed burns, splinted joints, and closed minor lacerations. What has changed to create the void that urgent care centers see as an opportunity to make money?
One explanation is the difficulty in finding folks (both providers and support people) who are willing to work a schedule that includes evenings and weekends. One study predicts that there will be a shortfall of 55,000 primary care physicians in the next decade, regardless of their work-life balance preferences. Sometimes it is a lack of creativity and foresight in creating flexible booking schedules that include ample time for patient- and parent-friendly same-day appointments. Minor injuries and skin problems can usually be managed quickly and effectively by an experienced clinician. Unquestionably, one of the big changes has been the shift in the patient mix leaning more toward time-consuming mental health complaints, which make it more difficult to leave open same-day slots. Restoring pediatricians’ offices to their former role as urgent care centers will require training not just more primary care physicians but also mental health consultants and providers.
First, we must decide that we want to become a real medical home that answers to a knock with a receptive response at almost any hour. By failing to accept the challenge of seeing our patients in a timely manner for their minor problems we will continue to fragment their care and threaten to make our relationship with them increasingly irrelevant.
It will mean rethinking how we schedule ourselves and our offices. It may require taking a hard look at how we spend our professional time. For example are annual checkups a must for every child at every age? Are all follow-up visits equally important? Would a phone call be just as effective? Most of all it will require adopting a mindset that we want to be complete physicians for our patients.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
If you live in a suburban or semirural community you have seen at least one urgent care center open up in the last decade. They now number nearly 12,000 nationwide and are growing in number at a 7% rate. Urgent care center patient volume surged during the pandemic and an industry trade group reports it has risen 60% since 2019 (Meyerson N. Why urgent care centers are popping up everywhere. CNN Business. 2023 Jan 28).
According to a report on the CNN Business website, this growth is the result of “convenience, gaps in primary care, high costs of emergency room visits, and increased investment by health systems and equity groups.” Initially, these centers were generally staffed by physicians (70% in 2009) but as of 2022 this number has fallen to 16%. While there are conflicting data to support the claim that urgent care centers are overprescribing, it is pretty clear that their presence in a community encourages fragmented care and weakens established provider-patient relationships. One study has shown that although urgent care centers can prevent a costly emergency room visit ($1,649/visit) this advantage is offset by urgent care cost of more than $6,000.
In the same CNN report, Susan Kressly MD, chair of the AAP’s Private Payer Advocacy Advisory Committee, said: “There’s a need to keep up with society’s demand for quick turnaround, on-demand services that can’t be supported by underfunded primary care.”
Her observation suggests that there is an accelerating demand for timely primary care services. From my perch here in semirural Maine, I don’t see an increasing or unreasonable demand for timeliness by patients and families. Two decades ago, the practice I was in offered evening and weekend morning office hours and call-in times when patientsor parents could speak directly to a physician. These avenues of accessibility have disappeared community wide.
Back in the 1990s “the medical home” was all the buzz. We were encouraged to be the first and primary place to go for a broad range of preventive and responsive care. One-stop shopping at its best. Now it’s “knock, knock ... is anybody home?” Not if it’s getting dark, or it’s the weekend, or you have a minor injury. “Please call the urgent care center.”
I will admit that our dedicated call-in times were unusual and probably not sustainable for most practices. But, most practices back then would see children with acute illness and minor scrapes and trauma on a same-day basis. We dressed burns, splinted joints, and closed minor lacerations. What has changed to create the void that urgent care centers see as an opportunity to make money?
One explanation is the difficulty in finding folks (both providers and support people) who are willing to work a schedule that includes evenings and weekends. One study predicts that there will be a shortfall of 55,000 primary care physicians in the next decade, regardless of their work-life balance preferences. Sometimes it is a lack of creativity and foresight in creating flexible booking schedules that include ample time for patient- and parent-friendly same-day appointments. Minor injuries and skin problems can usually be managed quickly and effectively by an experienced clinician. Unquestionably, one of the big changes has been the shift in the patient mix leaning more toward time-consuming mental health complaints, which make it more difficult to leave open same-day slots. Restoring pediatricians’ offices to their former role as urgent care centers will require training not just more primary care physicians but also mental health consultants and providers.
First, we must decide that we want to become a real medical home that answers to a knock with a receptive response at almost any hour. By failing to accept the challenge of seeing our patients in a timely manner for their minor problems we will continue to fragment their care and threaten to make our relationship with them increasingly irrelevant.
It will mean rethinking how we schedule ourselves and our offices. It may require taking a hard look at how we spend our professional time. For example are annual checkups a must for every child at every age? Are all follow-up visits equally important? Would a phone call be just as effective? Most of all it will require adopting a mindset that we want to be complete physicians for our patients.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
If you live in a suburban or semirural community you have seen at least one urgent care center open up in the last decade. They now number nearly 12,000 nationwide and are growing in number at a 7% rate. Urgent care center patient volume surged during the pandemic and an industry trade group reports it has risen 60% since 2019 (Meyerson N. Why urgent care centers are popping up everywhere. CNN Business. 2023 Jan 28).
According to a report on the CNN Business website, this growth is the result of “convenience, gaps in primary care, high costs of emergency room visits, and increased investment by health systems and equity groups.” Initially, these centers were generally staffed by physicians (70% in 2009) but as of 2022 this number has fallen to 16%. While there are conflicting data to support the claim that urgent care centers are overprescribing, it is pretty clear that their presence in a community encourages fragmented care and weakens established provider-patient relationships. One study has shown that although urgent care centers can prevent a costly emergency room visit ($1,649/visit) this advantage is offset by urgent care cost of more than $6,000.
In the same CNN report, Susan Kressly MD, chair of the AAP’s Private Payer Advocacy Advisory Committee, said: “There’s a need to keep up with society’s demand for quick turnaround, on-demand services that can’t be supported by underfunded primary care.”
Her observation suggests that there is an accelerating demand for timely primary care services. From my perch here in semirural Maine, I don’t see an increasing or unreasonable demand for timeliness by patients and families. Two decades ago, the practice I was in offered evening and weekend morning office hours and call-in times when patientsor parents could speak directly to a physician. These avenues of accessibility have disappeared community wide.
Back in the 1990s “the medical home” was all the buzz. We were encouraged to be the first and primary place to go for a broad range of preventive and responsive care. One-stop shopping at its best. Now it’s “knock, knock ... is anybody home?” Not if it’s getting dark, or it’s the weekend, or you have a minor injury. “Please call the urgent care center.”
I will admit that our dedicated call-in times were unusual and probably not sustainable for most practices. But, most practices back then would see children with acute illness and minor scrapes and trauma on a same-day basis. We dressed burns, splinted joints, and closed minor lacerations. What has changed to create the void that urgent care centers see as an opportunity to make money?
One explanation is the difficulty in finding folks (both providers and support people) who are willing to work a schedule that includes evenings and weekends. One study predicts that there will be a shortfall of 55,000 primary care physicians in the next decade, regardless of their work-life balance preferences. Sometimes it is a lack of creativity and foresight in creating flexible booking schedules that include ample time for patient- and parent-friendly same-day appointments. Minor injuries and skin problems can usually be managed quickly and effectively by an experienced clinician. Unquestionably, one of the big changes has been the shift in the patient mix leaning more toward time-consuming mental health complaints, which make it more difficult to leave open same-day slots. Restoring pediatricians’ offices to their former role as urgent care centers will require training not just more primary care physicians but also mental health consultants and providers.
First, we must decide that we want to become a real medical home that answers to a knock with a receptive response at almost any hour. By failing to accept the challenge of seeing our patients in a timely manner for their minor problems we will continue to fragment their care and threaten to make our relationship with them increasingly irrelevant.
It will mean rethinking how we schedule ourselves and our offices. It may require taking a hard look at how we spend our professional time. For example are annual checkups a must for every child at every age? Are all follow-up visits equally important? Would a phone call be just as effective? Most of all it will require adopting a mindset that we want to be complete physicians for our patients.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Little evidence to support lasers for ‘vaginal rejuvenation’
Laser devices licensed in Canada to treat genitourinary syndrome of menopause (GSM) are often marketed for vaginal rejuvenation with claims that they will tighten the vagina and improve sexual function, despite lack of evidence, a new commentary reveals.
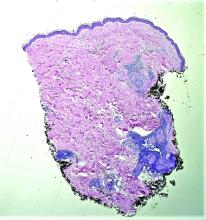
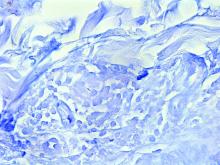
Vaginal lasers heat the vaginal epithelium and cause thermal necrosis. This intervention induces collagen remodeling and synthesis, neovascularization, and elastin formation and may result in improved vaginal elasticity and restoration of premenopausal epithelial function, according to coauthors Blayne Welk, MD, MSc, an associate professor of urologic surgery at Western University, London, Ont., and Erin Kelly, MD, a lecturer in obstetrics and gynecology at the University of Alberta, Edmonton.
Their patients’ questions and experiences with the laser devices prompted the commentary, they told this news organization.
“A large part of my practice involves addressing GSM and urinary incontinence,” said Dr. Kelly. “Many women present to the clinic having heard of vaginal laser procedures, having had vaginal laser procedures, or having been told they need vaginal laser procedures. My impression has been that these procedures are being marketed to women … without rigorous study.”
“Many women are reluctant to have mesh slings for stress incontinence due to some of the potential risks,” and they are looking for less invasive options, said Dr. Welk. Over the past few years, he has had increasing questions from patients about the use of lasers to improve this condition.
The commentary was published online in the Canadian Medical Association Journal.
Transparency needed
The first vaginal energy device was licensed by Health Canada in 2015 to treat GSM. That meant the device was deemed to have met basic safety, effectiveness, and quality criteria. But no controlled studies are required for regulatory approval of such devices, and after licensing, some providers rebranded the device indication from GSM to vaginal rejuvenation, said Dr. Kelly and Dr. Welk.
Vaginal laser therapies are offered throughout Canada, with at least one provider of vaginal rejuvenation procedures in the 10 most populous cities. Under the current system, the number of patients who pay for these procedures and the amount that they pay cannot be tracked. Nor can the number of vaginal laser systems active in Canada be tracked. Patients can refer themselves for the service, and providers’ publicly quoted costs (on websites, for example) are thousands of dollars for treatment.
The rebranding for vaginal rejuvenation “represents a difference between the licensing of a medical device by Health Canada and the way that these devices are used and marketed,” according to the commentary. “A procedure with limited high-quality evidence supporting its efficacy and a potential financial conflict of interest for providers may not be serving the best interests of people in Canada, even if the risk of adverse events is low.”
Updates to Canada’s medical devices action plan, including mandatory reporting of serious incidents and the ability to compel manufacturers to provide information on safety and effectiveness, “represent important progress,” according to Dr. Kelly and Dr. Welk. However, problems persist, including lack of a requirement for peer-reviewed, controlled studies.
Furthermore, women who undergo laser treatment for GSM, urinary incontinence, or vaginal rejuvenation may not receive a proper medical evaluation and standard treatments, the authors noted.
“I would like to see more transparency and public-facing information available on approved medical devices,” said Dr. Welk. “Health Canada has an online database of approved devices, but no information around the evidence submitted during the approval process is available, nor are the indications for the various devices.”
In addition, he said, many devices in the registry are listed by a serial number rather than the name that would be familiar to the public, “making it hard to match up information.”
Dr. Kelly added the “encouraging” news that the Canadian Society for Pelvic Medicine is working with Health Canada to “improve knowledge translation when it comes to transparency regarding medical devices.”
Medicine before marketing
“The commentary provides an accurate and evidence-based assessment of the use of vaginal laser treatments,” Jason Abbott, B Med (Hons), PhD, professor of gynecology at the University of New South Wales, Sydney, told this news organization. “The marketing of this device is a case of putting the cart before the horse. It is essential that strong, scientific, and reproducible studies be available on efficacy and safety before there is a direct-to-consumer marketing approach.”
Clinicians should advise patients when the treatment effect is likely to be minimal or risky, especially when there is a financial incentive to the clinician, he said. “Governments, regulators, and medical societies have a duty of care to the public to make sure that the medicine comes before the marketing. Otherwise, we are no better than snake oil sellers.
“Given the size of studies to date, the improvement in symptoms following treatment may be less than a few percent,” he noted. “That may be acceptable to some women. We don’t know.”
Dr. Abbott’s team is conducting research to define what women would want as a minimal level of improvement, the maximum cost, and the maximum risk from the laser procedure.
“In cancer … the benefit of a new treatment may only be a few percent for survival,” he said. “That may be completely acceptable for some or even many patients. What we cannot do, however, is extrapolate those same expectations to a treatment for a benign condition where quality of life is compromised.”
Echoing Dr. Kelly and Dr. Welk, Dr. Abbott said, “It is important that there be transparency in the clinical communication. Patients should be told that the best scientific studies that are judged based on their quality show there is no benefit to laser treatment for GSM or urinary incontinence.”
Although the medical risks may be low, he added, “financial risk also needs to be discussed. Patients should be encouraged to participate in clinical trials where there is no cost to them to gain the information first, before wholesale uptake of the treatment. … Should patients still wish to undergo the procedure once the risks and an honest account of the evidence is given to them, that of course is their choice.” Dr. Kelly, Dr. Welk, and Dr. Abbott had no commercial funding or relevant financial relationships to report.
A version of this article first appeared on Medscape.com.
Laser devices licensed in Canada to treat genitourinary syndrome of menopause (GSM) are often marketed for vaginal rejuvenation with claims that they will tighten the vagina and improve sexual function, despite lack of evidence, a new commentary reveals.
Vaginal lasers heat the vaginal epithelium and cause thermal necrosis. This intervention induces collagen remodeling and synthesis, neovascularization, and elastin formation and may result in improved vaginal elasticity and restoration of premenopausal epithelial function, according to coauthors Blayne Welk, MD, MSc, an associate professor of urologic surgery at Western University, London, Ont., and Erin Kelly, MD, a lecturer in obstetrics and gynecology at the University of Alberta, Edmonton.
Their patients’ questions and experiences with the laser devices prompted the commentary, they told this news organization.
“A large part of my practice involves addressing GSM and urinary incontinence,” said Dr. Kelly. “Many women present to the clinic having heard of vaginal laser procedures, having had vaginal laser procedures, or having been told they need vaginal laser procedures. My impression has been that these procedures are being marketed to women … without rigorous study.”
“Many women are reluctant to have mesh slings for stress incontinence due to some of the potential risks,” and they are looking for less invasive options, said Dr. Welk. Over the past few years, he has had increasing questions from patients about the use of lasers to improve this condition.
The commentary was published online in the Canadian Medical Association Journal.
Transparency needed
The first vaginal energy device was licensed by Health Canada in 2015 to treat GSM. That meant the device was deemed to have met basic safety, effectiveness, and quality criteria. But no controlled studies are required for regulatory approval of such devices, and after licensing, some providers rebranded the device indication from GSM to vaginal rejuvenation, said Dr. Kelly and Dr. Welk.
Vaginal laser therapies are offered throughout Canada, with at least one provider of vaginal rejuvenation procedures in the 10 most populous cities. Under the current system, the number of patients who pay for these procedures and the amount that they pay cannot be tracked. Nor can the number of vaginal laser systems active in Canada be tracked. Patients can refer themselves for the service, and providers’ publicly quoted costs (on websites, for example) are thousands of dollars for treatment.
The rebranding for vaginal rejuvenation “represents a difference between the licensing of a medical device by Health Canada and the way that these devices are used and marketed,” according to the commentary. “A procedure with limited high-quality evidence supporting its efficacy and a potential financial conflict of interest for providers may not be serving the best interests of people in Canada, even if the risk of adverse events is low.”
Updates to Canada’s medical devices action plan, including mandatory reporting of serious incidents and the ability to compel manufacturers to provide information on safety and effectiveness, “represent important progress,” according to Dr. Kelly and Dr. Welk. However, problems persist, including lack of a requirement for peer-reviewed, controlled studies.
Furthermore, women who undergo laser treatment for GSM, urinary incontinence, or vaginal rejuvenation may not receive a proper medical evaluation and standard treatments, the authors noted.
“I would like to see more transparency and public-facing information available on approved medical devices,” said Dr. Welk. “Health Canada has an online database of approved devices, but no information around the evidence submitted during the approval process is available, nor are the indications for the various devices.”
In addition, he said, many devices in the registry are listed by a serial number rather than the name that would be familiar to the public, “making it hard to match up information.”
Dr. Kelly added the “encouraging” news that the Canadian Society for Pelvic Medicine is working with Health Canada to “improve knowledge translation when it comes to transparency regarding medical devices.”
Medicine before marketing
“The commentary provides an accurate and evidence-based assessment of the use of vaginal laser treatments,” Jason Abbott, B Med (Hons), PhD, professor of gynecology at the University of New South Wales, Sydney, told this news organization. “The marketing of this device is a case of putting the cart before the horse. It is essential that strong, scientific, and reproducible studies be available on efficacy and safety before there is a direct-to-consumer marketing approach.”
Clinicians should advise patients when the treatment effect is likely to be minimal or risky, especially when there is a financial incentive to the clinician, he said. “Governments, regulators, and medical societies have a duty of care to the public to make sure that the medicine comes before the marketing. Otherwise, we are no better than snake oil sellers.
“Given the size of studies to date, the improvement in symptoms following treatment may be less than a few percent,” he noted. “That may be acceptable to some women. We don’t know.”
Dr. Abbott’s team is conducting research to define what women would want as a minimal level of improvement, the maximum cost, and the maximum risk from the laser procedure.
“In cancer … the benefit of a new treatment may only be a few percent for survival,” he said. “That may be completely acceptable for some or even many patients. What we cannot do, however, is extrapolate those same expectations to a treatment for a benign condition where quality of life is compromised.”
Echoing Dr. Kelly and Dr. Welk, Dr. Abbott said, “It is important that there be transparency in the clinical communication. Patients should be told that the best scientific studies that are judged based on their quality show there is no benefit to laser treatment for GSM or urinary incontinence.”
Although the medical risks may be low, he added, “financial risk also needs to be discussed. Patients should be encouraged to participate in clinical trials where there is no cost to them to gain the information first, before wholesale uptake of the treatment. … Should patients still wish to undergo the procedure once the risks and an honest account of the evidence is given to them, that of course is their choice.” Dr. Kelly, Dr. Welk, and Dr. Abbott had no commercial funding or relevant financial relationships to report.
A version of this article first appeared on Medscape.com.
Laser devices licensed in Canada to treat genitourinary syndrome of menopause (GSM) are often marketed for vaginal rejuvenation with claims that they will tighten the vagina and improve sexual function, despite lack of evidence, a new commentary reveals.
Vaginal lasers heat the vaginal epithelium and cause thermal necrosis. This intervention induces collagen remodeling and synthesis, neovascularization, and elastin formation and may result in improved vaginal elasticity and restoration of premenopausal epithelial function, according to coauthors Blayne Welk, MD, MSc, an associate professor of urologic surgery at Western University, London, Ont., and Erin Kelly, MD, a lecturer in obstetrics and gynecology at the University of Alberta, Edmonton.
Their patients’ questions and experiences with the laser devices prompted the commentary, they told this news organization.
“A large part of my practice involves addressing GSM and urinary incontinence,” said Dr. Kelly. “Many women present to the clinic having heard of vaginal laser procedures, having had vaginal laser procedures, or having been told they need vaginal laser procedures. My impression has been that these procedures are being marketed to women … without rigorous study.”
“Many women are reluctant to have mesh slings for stress incontinence due to some of the potential risks,” and they are looking for less invasive options, said Dr. Welk. Over the past few years, he has had increasing questions from patients about the use of lasers to improve this condition.
The commentary was published online in the Canadian Medical Association Journal.
Transparency needed
The first vaginal energy device was licensed by Health Canada in 2015 to treat GSM. That meant the device was deemed to have met basic safety, effectiveness, and quality criteria. But no controlled studies are required for regulatory approval of such devices, and after licensing, some providers rebranded the device indication from GSM to vaginal rejuvenation, said Dr. Kelly and Dr. Welk.
Vaginal laser therapies are offered throughout Canada, with at least one provider of vaginal rejuvenation procedures in the 10 most populous cities. Under the current system, the number of patients who pay for these procedures and the amount that they pay cannot be tracked. Nor can the number of vaginal laser systems active in Canada be tracked. Patients can refer themselves for the service, and providers’ publicly quoted costs (on websites, for example) are thousands of dollars for treatment.
The rebranding for vaginal rejuvenation “represents a difference between the licensing of a medical device by Health Canada and the way that these devices are used and marketed,” according to the commentary. “A procedure with limited high-quality evidence supporting its efficacy and a potential financial conflict of interest for providers may not be serving the best interests of people in Canada, even if the risk of adverse events is low.”
Updates to Canada’s medical devices action plan, including mandatory reporting of serious incidents and the ability to compel manufacturers to provide information on safety and effectiveness, “represent important progress,” according to Dr. Kelly and Dr. Welk. However, problems persist, including lack of a requirement for peer-reviewed, controlled studies.
Furthermore, women who undergo laser treatment for GSM, urinary incontinence, or vaginal rejuvenation may not receive a proper medical evaluation and standard treatments, the authors noted.
“I would like to see more transparency and public-facing information available on approved medical devices,” said Dr. Welk. “Health Canada has an online database of approved devices, but no information around the evidence submitted during the approval process is available, nor are the indications for the various devices.”
In addition, he said, many devices in the registry are listed by a serial number rather than the name that would be familiar to the public, “making it hard to match up information.”
Dr. Kelly added the “encouraging” news that the Canadian Society for Pelvic Medicine is working with Health Canada to “improve knowledge translation when it comes to transparency regarding medical devices.”
Medicine before marketing
“The commentary provides an accurate and evidence-based assessment of the use of vaginal laser treatments,” Jason Abbott, B Med (Hons), PhD, professor of gynecology at the University of New South Wales, Sydney, told this news organization. “The marketing of this device is a case of putting the cart before the horse. It is essential that strong, scientific, and reproducible studies be available on efficacy and safety before there is a direct-to-consumer marketing approach.”
Clinicians should advise patients when the treatment effect is likely to be minimal or risky, especially when there is a financial incentive to the clinician, he said. “Governments, regulators, and medical societies have a duty of care to the public to make sure that the medicine comes before the marketing. Otherwise, we are no better than snake oil sellers.
“Given the size of studies to date, the improvement in symptoms following treatment may be less than a few percent,” he noted. “That may be acceptable to some women. We don’t know.”
Dr. Abbott’s team is conducting research to define what women would want as a minimal level of improvement, the maximum cost, and the maximum risk from the laser procedure.
“In cancer … the benefit of a new treatment may only be a few percent for survival,” he said. “That may be completely acceptable for some or even many patients. What we cannot do, however, is extrapolate those same expectations to a treatment for a benign condition where quality of life is compromised.”
Echoing Dr. Kelly and Dr. Welk, Dr. Abbott said, “It is important that there be transparency in the clinical communication. Patients should be told that the best scientific studies that are judged based on their quality show there is no benefit to laser treatment for GSM or urinary incontinence.”
Although the medical risks may be low, he added, “financial risk also needs to be discussed. Patients should be encouraged to participate in clinical trials where there is no cost to them to gain the information first, before wholesale uptake of the treatment. … Should patients still wish to undergo the procedure once the risks and an honest account of the evidence is given to them, that of course is their choice.” Dr. Kelly, Dr. Welk, and Dr. Abbott had no commercial funding or relevant financial relationships to report.
A version of this article first appeared on Medscape.com.
Keto for life? Reasons to think twice
Is the ketogenic diet the only way to lose weight? Of course not! Keep track of calories in vs. calories out and almost anyone can lose weight. The problem is keeping it off. To understand that, we need to look at metabolic adaptation and the biology of obesity.
Our bodies have a “set point” that is epigenetically latched onto the environment the brain senses, just as the fetal environment responds to the maternal environment.
If food is plentiful, our hormones force us to eat until our bodies feel that there are enough fat stores to survive. Because of environmental influences such as highly processed food, preservatives, climate change, and regulation of temperature, our brains have decided that we need more adipose tissue than we did 50-100 years ago. It could be that an element in food has caused a dysfunction of the pathways that regulate our body weight, and most of us “defend” a higher body weight in this environment.
How to counteract that? Not easily. The ketogenic diet works temporarily just like any other diet where calorie intake is lower than usual. It seems to be agreeable to many people because they say they feel full after eating protein, fat, and perhaps some vegetables. Protein and fat are certainly more satiating than simple carbohydrates.
If strictly followed, a ketogenic diet will force the body to burn fat and go into ketosis. Without a source for glucose, the brain will burn ketones from fat stores. Owen and colleagues discovered this in 1969 when they did their now-famous studies of fasting in inpatients at Brigham and Women’s hospital, using IV amino acids to protect muscle mass.
Keto for life?
Is the ketogenic diet a healthy diet for the long term? That is a different question.
Of course not – we need high-fiber carbohydrate sources such as whole grains, fruits, and vegetables to keep the colon healthy and obtain the vitamins and minerals needed to make the Krebs cycle, or citric acid cycle, work at its best.
Why, then, are we promoting ketogenic diets for those with obesity and type 2 diabetes? Ketogenic or low-carbohydrate diets are easy to teach and can rapidly help patients lose weight and return their blood glucose, blood pressure, and other metabolic parameters to normal.
The patient will be instructed to avoid all highly processed foods. Studies have shown that highly processed foods, created to maximize flavor, “coerce” people to eat more calories than when presented with the same number of calories in unprocessed foods, a way to fool the brain.
Why are we fooling the brain?
We circumvent the natural satiety mechanisms that start with the gut. When we eat, our gastric fundus and intestinal stretch receptors start the process that informs the hypothalamus about food intake. Highly processed foods are usually devoid of fiber and volume, and pack in the calories in small volumes so that the stretch receptors are not activated until more calories are ingested. The study mentioned above developed two ad lib diets with the same number of calories, sugar, fat, and carbohydrate content – one ultraprocessed and the other unprocessed.
That explanation is just the tip of the iceberg, because a lot more than primitive stretch receptors is informing the brain. There are gut hormones that are secreted before and after meals, such as ghrelin, glucagon-like peptide 1 (GLP-1), glucose-dependent insulinotropic polypeptide (GIP), and cholecystokinin (CCK), among a slew of others. These peptide hormones are all secreted from gut cells into the blood or vagus nerve, or both, and alert the brain that there is or is not enough food to maintain body weight at its set point.
It’s a highly regulated and precise system that regulates body weight for survival of the species in this environment. However, the environment has changed over the past 100 years but our genetic makeup for survival of the fittest has not. The mechanism of action for defense of a higher body weight set point in this new environment has not been elucidated as yet. Most likely, there are many players or instigators involved, such as food-supply changes, sedentary lifestyle, ambient temperature, fetal programming, air quality, and global warming and climate change, to name a few.
The goal of obesity researchers is to investigate the underlying mechanisms of the increased prevalence of obesity over the past 100 years. The goal of obesity medicine specialists is to treat obesity in adults and children, and to prevent obesity as much as possible with lifestyle change and medications that have been shown to help “reverse” the metabolic adaptation to this environment. Our newest GLP-1/GIP receptor agonists have been shown in animal models to hit several pathways that lead to obesity. They are not just appetite suppressants. Yes, they do modulate appetite and satiety, but they also affect energy expenditure. The body’s normal reaction to a lack of calorie intake is to reduce resting energy expenditure until body weight increases back to “set point levels.” These agonists prevent that metabolic adaptation. That is why they are true agents that can treat obesity – the disease.
Back to the ketogenic diet. The ketogenic diet can fool the brain temporarily by using protein and fat to elicit satiety with less food intake in calories. After a while, however, gut hormones and other factors begin to counteract the weight loss with a reduction in resting energy and total energy expenditure, and other metabolic measures, to get the body back to a certain body weight set point.
The ketogenic diet also can help dieters avoid ultra- and highly processed foods. In the end, any type of diet that lowers caloric intake will work for weight loss, but it’s the maintenance of that weight loss that makes a long-term difference, and that involves closing the metabolic gap that the body generates to defend fat mass. Understanding this pathophysiology will allow obesity medicine specialists to assist patients with obesity to lose weight and keep it off.
Dr. Apovian is in the department of medicine, division of endocrinology, diabetes, and hypertension, and codirector, Center for Weight Management and Wellness, Harvard Medical School, Boston. She disclosed ties with Altimmune, Cowen and Company, Currax Pharmaceuticals, EPG Communication Holdings, Gelesis Srl, L-Nutra, NeuroBo Pharmaceuticals, National Institutes of Health, Patient-Centered Outcomes Research Institute, GI Dynamics, and Novo Nordisk. A version of this article first appeared on Medscape.com.
Is the ketogenic diet the only way to lose weight? Of course not! Keep track of calories in vs. calories out and almost anyone can lose weight. The problem is keeping it off. To understand that, we need to look at metabolic adaptation and the biology of obesity.
Our bodies have a “set point” that is epigenetically latched onto the environment the brain senses, just as the fetal environment responds to the maternal environment.
If food is plentiful, our hormones force us to eat until our bodies feel that there are enough fat stores to survive. Because of environmental influences such as highly processed food, preservatives, climate change, and regulation of temperature, our brains have decided that we need more adipose tissue than we did 50-100 years ago. It could be that an element in food has caused a dysfunction of the pathways that regulate our body weight, and most of us “defend” a higher body weight in this environment.
How to counteract that? Not easily. The ketogenic diet works temporarily just like any other diet where calorie intake is lower than usual. It seems to be agreeable to many people because they say they feel full after eating protein, fat, and perhaps some vegetables. Protein and fat are certainly more satiating than simple carbohydrates.
If strictly followed, a ketogenic diet will force the body to burn fat and go into ketosis. Without a source for glucose, the brain will burn ketones from fat stores. Owen and colleagues discovered this in 1969 when they did their now-famous studies of fasting in inpatients at Brigham and Women’s hospital, using IV amino acids to protect muscle mass.
Keto for life?
Is the ketogenic diet a healthy diet for the long term? That is a different question.
Of course not – we need high-fiber carbohydrate sources such as whole grains, fruits, and vegetables to keep the colon healthy and obtain the vitamins and minerals needed to make the Krebs cycle, or citric acid cycle, work at its best.
Why, then, are we promoting ketogenic diets for those with obesity and type 2 diabetes? Ketogenic or low-carbohydrate diets are easy to teach and can rapidly help patients lose weight and return their blood glucose, blood pressure, and other metabolic parameters to normal.
The patient will be instructed to avoid all highly processed foods. Studies have shown that highly processed foods, created to maximize flavor, “coerce” people to eat more calories than when presented with the same number of calories in unprocessed foods, a way to fool the brain.
Why are we fooling the brain?
We circumvent the natural satiety mechanisms that start with the gut. When we eat, our gastric fundus and intestinal stretch receptors start the process that informs the hypothalamus about food intake. Highly processed foods are usually devoid of fiber and volume, and pack in the calories in small volumes so that the stretch receptors are not activated until more calories are ingested. The study mentioned above developed two ad lib diets with the same number of calories, sugar, fat, and carbohydrate content – one ultraprocessed and the other unprocessed.
That explanation is just the tip of the iceberg, because a lot more than primitive stretch receptors is informing the brain. There are gut hormones that are secreted before and after meals, such as ghrelin, glucagon-like peptide 1 (GLP-1), glucose-dependent insulinotropic polypeptide (GIP), and cholecystokinin (CCK), among a slew of others. These peptide hormones are all secreted from gut cells into the blood or vagus nerve, or both, and alert the brain that there is or is not enough food to maintain body weight at its set point.
It’s a highly regulated and precise system that regulates body weight for survival of the species in this environment. However, the environment has changed over the past 100 years but our genetic makeup for survival of the fittest has not. The mechanism of action for defense of a higher body weight set point in this new environment has not been elucidated as yet. Most likely, there are many players or instigators involved, such as food-supply changes, sedentary lifestyle, ambient temperature, fetal programming, air quality, and global warming and climate change, to name a few.
The goal of obesity researchers is to investigate the underlying mechanisms of the increased prevalence of obesity over the past 100 years. The goal of obesity medicine specialists is to treat obesity in adults and children, and to prevent obesity as much as possible with lifestyle change and medications that have been shown to help “reverse” the metabolic adaptation to this environment. Our newest GLP-1/GIP receptor agonists have been shown in animal models to hit several pathways that lead to obesity. They are not just appetite suppressants. Yes, they do modulate appetite and satiety, but they also affect energy expenditure. The body’s normal reaction to a lack of calorie intake is to reduce resting energy expenditure until body weight increases back to “set point levels.” These agonists prevent that metabolic adaptation. That is why they are true agents that can treat obesity – the disease.
Back to the ketogenic diet. The ketogenic diet can fool the brain temporarily by using protein and fat to elicit satiety with less food intake in calories. After a while, however, gut hormones and other factors begin to counteract the weight loss with a reduction in resting energy and total energy expenditure, and other metabolic measures, to get the body back to a certain body weight set point.
The ketogenic diet also can help dieters avoid ultra- and highly processed foods. In the end, any type of diet that lowers caloric intake will work for weight loss, but it’s the maintenance of that weight loss that makes a long-term difference, and that involves closing the metabolic gap that the body generates to defend fat mass. Understanding this pathophysiology will allow obesity medicine specialists to assist patients with obesity to lose weight and keep it off.
Dr. Apovian is in the department of medicine, division of endocrinology, diabetes, and hypertension, and codirector, Center for Weight Management and Wellness, Harvard Medical School, Boston. She disclosed ties with Altimmune, Cowen and Company, Currax Pharmaceuticals, EPG Communication Holdings, Gelesis Srl, L-Nutra, NeuroBo Pharmaceuticals, National Institutes of Health, Patient-Centered Outcomes Research Institute, GI Dynamics, and Novo Nordisk. A version of this article first appeared on Medscape.com.
Is the ketogenic diet the only way to lose weight? Of course not! Keep track of calories in vs. calories out and almost anyone can lose weight. The problem is keeping it off. To understand that, we need to look at metabolic adaptation and the biology of obesity.
Our bodies have a “set point” that is epigenetically latched onto the environment the brain senses, just as the fetal environment responds to the maternal environment.
If food is plentiful, our hormones force us to eat until our bodies feel that there are enough fat stores to survive. Because of environmental influences such as highly processed food, preservatives, climate change, and regulation of temperature, our brains have decided that we need more adipose tissue than we did 50-100 years ago. It could be that an element in food has caused a dysfunction of the pathways that regulate our body weight, and most of us “defend” a higher body weight in this environment.
How to counteract that? Not easily. The ketogenic diet works temporarily just like any other diet where calorie intake is lower than usual. It seems to be agreeable to many people because they say they feel full after eating protein, fat, and perhaps some vegetables. Protein and fat are certainly more satiating than simple carbohydrates.
If strictly followed, a ketogenic diet will force the body to burn fat and go into ketosis. Without a source for glucose, the brain will burn ketones from fat stores. Owen and colleagues discovered this in 1969 when they did their now-famous studies of fasting in inpatients at Brigham and Women’s hospital, using IV amino acids to protect muscle mass.
Keto for life?
Is the ketogenic diet a healthy diet for the long term? That is a different question.
Of course not – we need high-fiber carbohydrate sources such as whole grains, fruits, and vegetables to keep the colon healthy and obtain the vitamins and minerals needed to make the Krebs cycle, or citric acid cycle, work at its best.
Why, then, are we promoting ketogenic diets for those with obesity and type 2 diabetes? Ketogenic or low-carbohydrate diets are easy to teach and can rapidly help patients lose weight and return their blood glucose, blood pressure, and other metabolic parameters to normal.
The patient will be instructed to avoid all highly processed foods. Studies have shown that highly processed foods, created to maximize flavor, “coerce” people to eat more calories than when presented with the same number of calories in unprocessed foods, a way to fool the brain.
Why are we fooling the brain?
We circumvent the natural satiety mechanisms that start with the gut. When we eat, our gastric fundus and intestinal stretch receptors start the process that informs the hypothalamus about food intake. Highly processed foods are usually devoid of fiber and volume, and pack in the calories in small volumes so that the stretch receptors are not activated until more calories are ingested. The study mentioned above developed two ad lib diets with the same number of calories, sugar, fat, and carbohydrate content – one ultraprocessed and the other unprocessed.
That explanation is just the tip of the iceberg, because a lot more than primitive stretch receptors is informing the brain. There are gut hormones that are secreted before and after meals, such as ghrelin, glucagon-like peptide 1 (GLP-1), glucose-dependent insulinotropic polypeptide (GIP), and cholecystokinin (CCK), among a slew of others. These peptide hormones are all secreted from gut cells into the blood or vagus nerve, or both, and alert the brain that there is or is not enough food to maintain body weight at its set point.
It’s a highly regulated and precise system that regulates body weight for survival of the species in this environment. However, the environment has changed over the past 100 years but our genetic makeup for survival of the fittest has not. The mechanism of action for defense of a higher body weight set point in this new environment has not been elucidated as yet. Most likely, there are many players or instigators involved, such as food-supply changes, sedentary lifestyle, ambient temperature, fetal programming, air quality, and global warming and climate change, to name a few.
The goal of obesity researchers is to investigate the underlying mechanisms of the increased prevalence of obesity over the past 100 years. The goal of obesity medicine specialists is to treat obesity in adults and children, and to prevent obesity as much as possible with lifestyle change and medications that have been shown to help “reverse” the metabolic adaptation to this environment. Our newest GLP-1/GIP receptor agonists have been shown in animal models to hit several pathways that lead to obesity. They are not just appetite suppressants. Yes, they do modulate appetite and satiety, but they also affect energy expenditure. The body’s normal reaction to a lack of calorie intake is to reduce resting energy expenditure until body weight increases back to “set point levels.” These agonists prevent that metabolic adaptation. That is why they are true agents that can treat obesity – the disease.
Back to the ketogenic diet. The ketogenic diet can fool the brain temporarily by using protein and fat to elicit satiety with less food intake in calories. After a while, however, gut hormones and other factors begin to counteract the weight loss with a reduction in resting energy and total energy expenditure, and other metabolic measures, to get the body back to a certain body weight set point.
The ketogenic diet also can help dieters avoid ultra- and highly processed foods. In the end, any type of diet that lowers caloric intake will work for weight loss, but it’s the maintenance of that weight loss that makes a long-term difference, and that involves closing the metabolic gap that the body generates to defend fat mass. Understanding this pathophysiology will allow obesity medicine specialists to assist patients with obesity to lose weight and keep it off.
Dr. Apovian is in the department of medicine, division of endocrinology, diabetes, and hypertension, and codirector, Center for Weight Management and Wellness, Harvard Medical School, Boston. She disclosed ties with Altimmune, Cowen and Company, Currax Pharmaceuticals, EPG Communication Holdings, Gelesis Srl, L-Nutra, NeuroBo Pharmaceuticals, National Institutes of Health, Patient-Centered Outcomes Research Institute, GI Dynamics, and Novo Nordisk. A version of this article first appeared on Medscape.com.
A White male presented with a 1½-year history of a progressive hypoesthetic annular, hyperpigmented plaque on the upper arm
Paucibacillary tuberculoid leprosy is characterized by few anesthetic hypo- or hyperpigmented lesions and can be accompanied by palpable peripheral nerve enlargements.
Tuberculoid leprosy presents histologically with epithelioid histiocytes with lymphocytes and Langhans giant cells. Neurotropic granulomas are also characteristic of tuberculoid leprosy. Fite staining allows for the identification of the acid-fast bacilli of M. leprae, which in some cases are quite few in number. The standard mycobacterium stain, Ziehl-Neelsen, is a good option for M. tuberculosis, but because of the relative weak mycolic acid coat of M. leprae, the Fite stain is more appropriate for identifying M. leprae.
Clinically, other than the presence of fewer than five hypoesthetic lesions that are either hypopigmented or erythematous, tuberculoid leprosy often presents with additional peripheral nerve involvement that manifests as numbness and tingling in hands and feet.1 This patient denied any tingling, weakness, or numbness, outside of the anesthetic lesion on his posterior upper arm.
The patient, born in the United States, had a remote history of military travel to Iraq, Kuwait, and the Philippines, but had not traveled internationally within the last 15 years, apart from a cruise to the Bahamas. He denied any known contact with individuals with similar lesions. He denied a history of contact with armadillos, but acknowledged that they are native to where he resides in central Florida, and that he had seen them in his yard.
Histopathological examination revealed an unremarkable epidermis with a superficial and deep perivascular, periadnexal, and perineural lymphohistiocytic infiltrate. Fite stain revealed rare rod-shaped organisms (Figure 2). These findings are consistent with a diagnosis of paucibacillary, tuberculoid leprosy.
The patient’s travel history to highly endemic areas (Middle East), as well as possible environmental contact with armadillos – including contact with soil that the armadillos occupied – could explain plausible modes of transmission. Following consultation with our infectious disease department and the National Hansen’s Disease Program, our patient began a planned course of therapy with 18 months of minocycline, rifampin, and moxifloxacin.
Human-to-human transmission of HD has been well documented; however, zoonotic transmission – specifically via the nine-banded armadillo (Dasypus novemcinctus) – serves as another suggested means of transmission, especially in the Southeastern United States.2-6 Travel to highly-endemic areas increases the risk of contracting HD, which may take up to 20 years following contact with the bacteria to manifest clinically.
While central Florida was previously thought to be a nonendemic area of disease, the incidence of the disease in this region has increased in recent years.7 Human-to-human transmission, which remains a concern with immigration from highly-endemic regions, occurs via long-term contact with nasal droplets of an infected person.8,9
Many patients in regions with very few cases of leprosy deny travel to other endemic regions and contact with infected people. Thus, zoonotic transmission remains a legitimate concern in the Southeastern United States – accounting, at least in part, for many of the non–human-transmitted cases of leprosy.2,10 We encourage clinicians to maintain a high level of clinical suspicion for leprosy when evaluating patients presenting with hypoesthetic cutaneous lesions and to obtain a travel history and to ask about armadillo exposure.
This case and the photos were submitted by Ms. Smith, from the University of South Florida, Tampa; Dr. Hatch and Dr. Sarriera-Lazaro, from the department of dermatology and cutaneous surgery, University of South Florida; and Dr. Turner and Dr. Beachkofsky, from the department of pathology and laboratory medicine at the James A. Haley Veterans’ Hospital, Tampa. Dr. Bilu Martin edited this case. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Leprosy (Hansen’s Disease), in: “Goldman’s Cecil Medicine,” 24th ed. (Philadelphia: W.B. Saunders, 2012: pp. 1950-4.
2. Sharma R et al. Emerg Infect Dis. 2015 Dec;21(12):2127-34.
3. Lane JE et al. J Am Acad Dermatol. 2006 Oct;55(4):714-6.
4. Clark BM et al. Am J Trop Med Hyg. 2008 Jun;78(6):962-7.
5. Bruce S et al. J Am Acad Dermatol. 2000 Aug;43(2 Pt 1):223-8.
6. Loughry WJ et al. J Wildl Dis. 2009 Jan;45(1):144-52.
7. FDo H. Florida charts: Hansen’s Disease (Leprosy). Health FDo. 2019. https://www.flhealthcharts.gov/ChartsReports/rdPage.aspx?rdReport=NonVitalIndNoGrpCounts.DataViewer&cid=174.
8. Maymone MBC et al. J Am Acad Dermatol. 2020 Jul;83(1):1-14.
9. Scollard DM et al. Clin Microbiol Rev. 2006 Apr;19(2):338-81.
10. Domozych R et al. JAAD Case Rep. 2016 May 12;2(3):189-92.
Paucibacillary tuberculoid leprosy is characterized by few anesthetic hypo- or hyperpigmented lesions and can be accompanied by palpable peripheral nerve enlargements.
Tuberculoid leprosy presents histologically with epithelioid histiocytes with lymphocytes and Langhans giant cells. Neurotropic granulomas are also characteristic of tuberculoid leprosy. Fite staining allows for the identification of the acid-fast bacilli of M. leprae, which in some cases are quite few in number. The standard mycobacterium stain, Ziehl-Neelsen, is a good option for M. tuberculosis, but because of the relative weak mycolic acid coat of M. leprae, the Fite stain is more appropriate for identifying M. leprae.
Clinically, other than the presence of fewer than five hypoesthetic lesions that are either hypopigmented or erythematous, tuberculoid leprosy often presents with additional peripheral nerve involvement that manifests as numbness and tingling in hands and feet.1 This patient denied any tingling, weakness, or numbness, outside of the anesthetic lesion on his posterior upper arm.
The patient, born in the United States, had a remote history of military travel to Iraq, Kuwait, and the Philippines, but had not traveled internationally within the last 15 years, apart from a cruise to the Bahamas. He denied any known contact with individuals with similar lesions. He denied a history of contact with armadillos, but acknowledged that they are native to where he resides in central Florida, and that he had seen them in his yard.
Histopathological examination revealed an unremarkable epidermis with a superficial and deep perivascular, periadnexal, and perineural lymphohistiocytic infiltrate. Fite stain revealed rare rod-shaped organisms (Figure 2). These findings are consistent with a diagnosis of paucibacillary, tuberculoid leprosy.
The patient’s travel history to highly endemic areas (Middle East), as well as possible environmental contact with armadillos – including contact with soil that the armadillos occupied – could explain plausible modes of transmission. Following consultation with our infectious disease department and the National Hansen’s Disease Program, our patient began a planned course of therapy with 18 months of minocycline, rifampin, and moxifloxacin.
Human-to-human transmission of HD has been well documented; however, zoonotic transmission – specifically via the nine-banded armadillo (Dasypus novemcinctus) – serves as another suggested means of transmission, especially in the Southeastern United States.2-6 Travel to highly-endemic areas increases the risk of contracting HD, which may take up to 20 years following contact with the bacteria to manifest clinically.
While central Florida was previously thought to be a nonendemic area of disease, the incidence of the disease in this region has increased in recent years.7 Human-to-human transmission, which remains a concern with immigration from highly-endemic regions, occurs via long-term contact with nasal droplets of an infected person.8,9
Many patients in regions with very few cases of leprosy deny travel to other endemic regions and contact with infected people. Thus, zoonotic transmission remains a legitimate concern in the Southeastern United States – accounting, at least in part, for many of the non–human-transmitted cases of leprosy.2,10 We encourage clinicians to maintain a high level of clinical suspicion for leprosy when evaluating patients presenting with hypoesthetic cutaneous lesions and to obtain a travel history and to ask about armadillo exposure.
This case and the photos were submitted by Ms. Smith, from the University of South Florida, Tampa; Dr. Hatch and Dr. Sarriera-Lazaro, from the department of dermatology and cutaneous surgery, University of South Florida; and Dr. Turner and Dr. Beachkofsky, from the department of pathology and laboratory medicine at the James A. Haley Veterans’ Hospital, Tampa. Dr. Bilu Martin edited this case. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Leprosy (Hansen’s Disease), in: “Goldman’s Cecil Medicine,” 24th ed. (Philadelphia: W.B. Saunders, 2012: pp. 1950-4.
2. Sharma R et al. Emerg Infect Dis. 2015 Dec;21(12):2127-34.
3. Lane JE et al. J Am Acad Dermatol. 2006 Oct;55(4):714-6.
4. Clark BM et al. Am J Trop Med Hyg. 2008 Jun;78(6):962-7.
5. Bruce S et al. J Am Acad Dermatol. 2000 Aug;43(2 Pt 1):223-8.
6. Loughry WJ et al. J Wildl Dis. 2009 Jan;45(1):144-52.
7. FDo H. Florida charts: Hansen’s Disease (Leprosy). Health FDo. 2019. https://www.flhealthcharts.gov/ChartsReports/rdPage.aspx?rdReport=NonVitalIndNoGrpCounts.DataViewer&cid=174.
8. Maymone MBC et al. J Am Acad Dermatol. 2020 Jul;83(1):1-14.
9. Scollard DM et al. Clin Microbiol Rev. 2006 Apr;19(2):338-81.
10. Domozych R et al. JAAD Case Rep. 2016 May 12;2(3):189-92.
Paucibacillary tuberculoid leprosy is characterized by few anesthetic hypo- or hyperpigmented lesions and can be accompanied by palpable peripheral nerve enlargements.
Tuberculoid leprosy presents histologically with epithelioid histiocytes with lymphocytes and Langhans giant cells. Neurotropic granulomas are also characteristic of tuberculoid leprosy. Fite staining allows for the identification of the acid-fast bacilli of M. leprae, which in some cases are quite few in number. The standard mycobacterium stain, Ziehl-Neelsen, is a good option for M. tuberculosis, but because of the relative weak mycolic acid coat of M. leprae, the Fite stain is more appropriate for identifying M. leprae.
Clinically, other than the presence of fewer than five hypoesthetic lesions that are either hypopigmented or erythematous, tuberculoid leprosy often presents with additional peripheral nerve involvement that manifests as numbness and tingling in hands and feet.1 This patient denied any tingling, weakness, or numbness, outside of the anesthetic lesion on his posterior upper arm.
The patient, born in the United States, had a remote history of military travel to Iraq, Kuwait, and the Philippines, but had not traveled internationally within the last 15 years, apart from a cruise to the Bahamas. He denied any known contact with individuals with similar lesions. He denied a history of contact with armadillos, but acknowledged that they are native to where he resides in central Florida, and that he had seen them in his yard.
Histopathological examination revealed an unremarkable epidermis with a superficial and deep perivascular, periadnexal, and perineural lymphohistiocytic infiltrate. Fite stain revealed rare rod-shaped organisms (Figure 2). These findings are consistent with a diagnosis of paucibacillary, tuberculoid leprosy.
The patient’s travel history to highly endemic areas (Middle East), as well as possible environmental contact with armadillos – including contact with soil that the armadillos occupied – could explain plausible modes of transmission. Following consultation with our infectious disease department and the National Hansen’s Disease Program, our patient began a planned course of therapy with 18 months of minocycline, rifampin, and moxifloxacin.
Human-to-human transmission of HD has been well documented; however, zoonotic transmission – specifically via the nine-banded armadillo (Dasypus novemcinctus) – serves as another suggested means of transmission, especially in the Southeastern United States.2-6 Travel to highly-endemic areas increases the risk of contracting HD, which may take up to 20 years following contact with the bacteria to manifest clinically.
While central Florida was previously thought to be a nonendemic area of disease, the incidence of the disease in this region has increased in recent years.7 Human-to-human transmission, which remains a concern with immigration from highly-endemic regions, occurs via long-term contact with nasal droplets of an infected person.8,9
Many patients in regions with very few cases of leprosy deny travel to other endemic regions and contact with infected people. Thus, zoonotic transmission remains a legitimate concern in the Southeastern United States – accounting, at least in part, for many of the non–human-transmitted cases of leprosy.2,10 We encourage clinicians to maintain a high level of clinical suspicion for leprosy when evaluating patients presenting with hypoesthetic cutaneous lesions and to obtain a travel history and to ask about armadillo exposure.
This case and the photos were submitted by Ms. Smith, from the University of South Florida, Tampa; Dr. Hatch and Dr. Sarriera-Lazaro, from the department of dermatology and cutaneous surgery, University of South Florida; and Dr. Turner and Dr. Beachkofsky, from the department of pathology and laboratory medicine at the James A. Haley Veterans’ Hospital, Tampa. Dr. Bilu Martin edited this case. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Leprosy (Hansen’s Disease), in: “Goldman’s Cecil Medicine,” 24th ed. (Philadelphia: W.B. Saunders, 2012: pp. 1950-4.
2. Sharma R et al. Emerg Infect Dis. 2015 Dec;21(12):2127-34.
3. Lane JE et al. J Am Acad Dermatol. 2006 Oct;55(4):714-6.
4. Clark BM et al. Am J Trop Med Hyg. 2008 Jun;78(6):962-7.
5. Bruce S et al. J Am Acad Dermatol. 2000 Aug;43(2 Pt 1):223-8.
6. Loughry WJ et al. J Wildl Dis. 2009 Jan;45(1):144-52.
7. FDo H. Florida charts: Hansen’s Disease (Leprosy). Health FDo. 2019. https://www.flhealthcharts.gov/ChartsReports/rdPage.aspx?rdReport=NonVitalIndNoGrpCounts.DataViewer&cid=174.
8. Maymone MBC et al. J Am Acad Dermatol. 2020 Jul;83(1):1-14.
9. Scollard DM et al. Clin Microbiol Rev. 2006 Apr;19(2):338-81.
10. Domozych R et al. JAAD Case Rep. 2016 May 12;2(3):189-92.
A 44-year-old White male presented with a 1½-year history of a progressive hypoesthetic annular, mildly hyperpigmented plaque on the left posterior upper arm.
He denied pruritus, pain, or systemic symptoms including weight loss, visual changes, cough, dyspnea, and abdominal pain. He also denied any paresthesia or weakness. On physical examination, there is a subtle, solitary 4-cm annular skin-colored thin plaque on the patient's left posterior upper arm (Figure 1).
Punch biopsy of the lesion was performed, and the histopathological findings are illustrated in Figure 2.
Advice on antibiotics for kids during shortages
Pharmacies are running out of the antibiotics used to treat serious infections in children. This leaves parents and doctors frustrated and scared.
After weeks of overcrowded waiting rooms, extended office hours, and countless telephone calls during the viral respiratory surge, pediatricians are now facing a new challenge: an ever-growing list of medication shortages, including many of the most commonly used antibiotics.
These shortages primarily affect liquid formulations, so children – and the pediatricians’ offices and pharmacies serving them – are disproportionately impacted. Though there are multiple factors contributing, antibiotic overuse for viral infections during the surge has undoubtedly catalyzed the current crisis. It can be scary for parents to watch a child miserable with fever, which is why parents and pediatricians look for a quick fix in antibiotics, but unnecessary prescriptions that contribute to ongoing shortages should be avoided. We, as practicing pediatricians, think that this is a moment for reflection on when and why we use antibiotics during viral season. Though antibiotic overuse may have led us into this shortage, better antibiotic stewardship may just lead us out of it.
Since amoxicillin was approved for medical use in 1974, it has been one of the most commonly prescribed antibiotics in children. It is particularly well-suited for use in children because it treats common pediatric infections such as ear infections, strep throat, and pneumonia. These factors, along with its low cost and bubblegum flavor, make it no surprise that amoxicillin was consistently one of the top 25 medications prescribed in the United States between 2013 and 2019, with over 25 million prescriptions annually.
Amoxicillin remains the best first-line treatment option for the most common bacterial respiratory tract infections in children. With liquid formulations scarce, pediatricians, parents, and pharmacists are getting creative with crushed tablets or sprinkling capsules when possible.
However, without liquid amoxicillin readily available in our pediatric arsenal, we have recently had to turn to antibiotics with higher costs and more side effects. These broad-spectrum antibiotics target a more extensive range of bacteria and are rarely necessary for common pediatric infections. Further, their use risks increasing the already dire problem of antibiotic resistance, which causes more than 35,000 deaths in the United States each year. And perhaps most importantly, broader spectrum antibiotics aren’t better than amoxicillin for the treatment of respiratory tract infections; they are sometimes worse.
The urge to turn to antibiotics as a potential cure for childhood illnesses is an understandable one for parents and clinicians alike. A common refrain in pediatrician offices is, “Isn’t there anything we can give them?” as parents look for respite in a long viral season. As viruses continue to surge, it is helpful to remember that children will get 8 to 10 viral infections per year, with most of those occurring in the fall and winter. When parents report that their child is always sick, they aren’t far off.
Most of these infections will be cured by a child’s own immune system rather than our medications. For example, in children older than 2 years, studies have demonstrated that waiting about 2 days to start antibiotics after an ear infection is diagnosed is just as effective as starting the antibiotics right away. As tempting as it is to ask for antibiotics early, that prescription may only worsen the situation if it is a virus. Instead, pediatricians can offer parents support in treating their children at home with humidifiers, pain/fever relievers when appropriate, honey in children over 12 months, and hydration.
This drug shortage is a pivotal moment for parents and clinicians to reconsider how and when we use antibiotics during viral season. Though antibiotics may be one of the greatest inventions of the 20th century, it is how we use them now that will determine our health in the century to come.
Dr. Lockwood is Associate Professor, department of pediatrics, University of Pennsylvania, Philadelphia. Dr. Same is Assistant Professor, department of clinical pediatrics, at the University of Pennsylvania. Neither reported any conflicts of interest.
A version of this article first appeared on Medscape.com.
Pharmacies are running out of the antibiotics used to treat serious infections in children. This leaves parents and doctors frustrated and scared.
After weeks of overcrowded waiting rooms, extended office hours, and countless telephone calls during the viral respiratory surge, pediatricians are now facing a new challenge: an ever-growing list of medication shortages, including many of the most commonly used antibiotics.
These shortages primarily affect liquid formulations, so children – and the pediatricians’ offices and pharmacies serving them – are disproportionately impacted. Though there are multiple factors contributing, antibiotic overuse for viral infections during the surge has undoubtedly catalyzed the current crisis. It can be scary for parents to watch a child miserable with fever, which is why parents and pediatricians look for a quick fix in antibiotics, but unnecessary prescriptions that contribute to ongoing shortages should be avoided. We, as practicing pediatricians, think that this is a moment for reflection on when and why we use antibiotics during viral season. Though antibiotic overuse may have led us into this shortage, better antibiotic stewardship may just lead us out of it.
Since amoxicillin was approved for medical use in 1974, it has been one of the most commonly prescribed antibiotics in children. It is particularly well-suited for use in children because it treats common pediatric infections such as ear infections, strep throat, and pneumonia. These factors, along with its low cost and bubblegum flavor, make it no surprise that amoxicillin was consistently one of the top 25 medications prescribed in the United States between 2013 and 2019, with over 25 million prescriptions annually.
Amoxicillin remains the best first-line treatment option for the most common bacterial respiratory tract infections in children. With liquid formulations scarce, pediatricians, parents, and pharmacists are getting creative with crushed tablets or sprinkling capsules when possible.
However, without liquid amoxicillin readily available in our pediatric arsenal, we have recently had to turn to antibiotics with higher costs and more side effects. These broad-spectrum antibiotics target a more extensive range of bacteria and are rarely necessary for common pediatric infections. Further, their use risks increasing the already dire problem of antibiotic resistance, which causes more than 35,000 deaths in the United States each year. And perhaps most importantly, broader spectrum antibiotics aren’t better than amoxicillin for the treatment of respiratory tract infections; they are sometimes worse.
The urge to turn to antibiotics as a potential cure for childhood illnesses is an understandable one for parents and clinicians alike. A common refrain in pediatrician offices is, “Isn’t there anything we can give them?” as parents look for respite in a long viral season. As viruses continue to surge, it is helpful to remember that children will get 8 to 10 viral infections per year, with most of those occurring in the fall and winter. When parents report that their child is always sick, they aren’t far off.
Most of these infections will be cured by a child’s own immune system rather than our medications. For example, in children older than 2 years, studies have demonstrated that waiting about 2 days to start antibiotics after an ear infection is diagnosed is just as effective as starting the antibiotics right away. As tempting as it is to ask for antibiotics early, that prescription may only worsen the situation if it is a virus. Instead, pediatricians can offer parents support in treating their children at home with humidifiers, pain/fever relievers when appropriate, honey in children over 12 months, and hydration.
This drug shortage is a pivotal moment for parents and clinicians to reconsider how and when we use antibiotics during viral season. Though antibiotics may be one of the greatest inventions of the 20th century, it is how we use them now that will determine our health in the century to come.
Dr. Lockwood is Associate Professor, department of pediatrics, University of Pennsylvania, Philadelphia. Dr. Same is Assistant Professor, department of clinical pediatrics, at the University of Pennsylvania. Neither reported any conflicts of interest.
A version of this article first appeared on Medscape.com.
Pharmacies are running out of the antibiotics used to treat serious infections in children. This leaves parents and doctors frustrated and scared.
After weeks of overcrowded waiting rooms, extended office hours, and countless telephone calls during the viral respiratory surge, pediatricians are now facing a new challenge: an ever-growing list of medication shortages, including many of the most commonly used antibiotics.
These shortages primarily affect liquid formulations, so children – and the pediatricians’ offices and pharmacies serving them – are disproportionately impacted. Though there are multiple factors contributing, antibiotic overuse for viral infections during the surge has undoubtedly catalyzed the current crisis. It can be scary for parents to watch a child miserable with fever, which is why parents and pediatricians look for a quick fix in antibiotics, but unnecessary prescriptions that contribute to ongoing shortages should be avoided. We, as practicing pediatricians, think that this is a moment for reflection on when and why we use antibiotics during viral season. Though antibiotic overuse may have led us into this shortage, better antibiotic stewardship may just lead us out of it.
Since amoxicillin was approved for medical use in 1974, it has been one of the most commonly prescribed antibiotics in children. It is particularly well-suited for use in children because it treats common pediatric infections such as ear infections, strep throat, and pneumonia. These factors, along with its low cost and bubblegum flavor, make it no surprise that amoxicillin was consistently one of the top 25 medications prescribed in the United States between 2013 and 2019, with over 25 million prescriptions annually.
Amoxicillin remains the best first-line treatment option for the most common bacterial respiratory tract infections in children. With liquid formulations scarce, pediatricians, parents, and pharmacists are getting creative with crushed tablets or sprinkling capsules when possible.
However, without liquid amoxicillin readily available in our pediatric arsenal, we have recently had to turn to antibiotics with higher costs and more side effects. These broad-spectrum antibiotics target a more extensive range of bacteria and are rarely necessary for common pediatric infections. Further, their use risks increasing the already dire problem of antibiotic resistance, which causes more than 35,000 deaths in the United States each year. And perhaps most importantly, broader spectrum antibiotics aren’t better than amoxicillin for the treatment of respiratory tract infections; they are sometimes worse.
The urge to turn to antibiotics as a potential cure for childhood illnesses is an understandable one for parents and clinicians alike. A common refrain in pediatrician offices is, “Isn’t there anything we can give them?” as parents look for respite in a long viral season. As viruses continue to surge, it is helpful to remember that children will get 8 to 10 viral infections per year, with most of those occurring in the fall and winter. When parents report that their child is always sick, they aren’t far off.
Most of these infections will be cured by a child’s own immune system rather than our medications. For example, in children older than 2 years, studies have demonstrated that waiting about 2 days to start antibiotics after an ear infection is diagnosed is just as effective as starting the antibiotics right away. As tempting as it is to ask for antibiotics early, that prescription may only worsen the situation if it is a virus. Instead, pediatricians can offer parents support in treating their children at home with humidifiers, pain/fever relievers when appropriate, honey in children over 12 months, and hydration.
This drug shortage is a pivotal moment for parents and clinicians to reconsider how and when we use antibiotics during viral season. Though antibiotics may be one of the greatest inventions of the 20th century, it is how we use them now that will determine our health in the century to come.
Dr. Lockwood is Associate Professor, department of pediatrics, University of Pennsylvania, Philadelphia. Dr. Same is Assistant Professor, department of clinical pediatrics, at the University of Pennsylvania. Neither reported any conflicts of interest.
A version of this article first appeared on Medscape.com.
Commenting on weight’s not rude. It’s dangerous.
It was the start of the fall semester of my sophomore year of college.
At my small women’s college, the previous semester’s gossip had been about our classmate, S*. She had gone from being very thin to noticeably gaining a lot of weight in a few months. The rumors were that S was pregnant and gave birth over summer break. As a busy biology premed major, this was my first time hearing the news. So when I saw her standing in the hallway, back to her previous weight, I was excited for her.
In true extravert fashion, I commented on the baby and her new size. But no sooner had the words left my mouth than I regretted them.
The hall grew awkwardly silent as S’s face flushed and she asked, “Excuse me?!” Instantly I knew that the rumors weren’t true.
Thankfully, at that moment, the classroom opened and we walked in. Whew! After class, S asked if we could talk. She explained that she had a thyroid tumor and struggled to adjust to the treatments, which caused her weight fluctuations. She had never been pregnant.
My awkward statement had been the first time anyone on campus had directly mentioned her weight, though she suspected that people were talking about her. We became fast friends after this rocky beginning. Although we lost touch after college, S taught me an invaluable lesson about making assumptions about people’s weight: Ask before you assume.
Now, years later, as an internist and obesity specialist, this lesson continues to be reinforced daily.
In daily life, comments about weight can be perceived as rude. In the clinical setting, however, assumptions about weight are a form of weight bias. Weight bias can lead to weight stigma and even be dangerous to health care.
Let’s discuss the insidious influence of weight bias in health care through two commonly used phrases and then look at a few solutions to address weight bias in health care individually and systematically.
Common weight bias assumptions
“Great job, you lost weight!” In checking your patient’s vital signs, you notice that this patient with obesity has a significant weight change. You congratulate them upon entering the room. Unfortunately, their weight loss was a result of minimal eating after losing a loved one. This isn’t healthy weight loss. One of the adverse effects of weight bias is that it infers that weight loss is always a good thing, especially in people with larger bodies. This is a dangerous presumption. Let’s remember that the body favors fat storage, hence why “unintentional weight loss” is a recognized medical condition prompting evaluation. We have to be careful not to celebrate weight loss “at all costs,” such as fad diets that haven’t been shown to improve health outcomes.
Furthermore, patients who lose weight quickly (more than 4-8 lb/month) require closer follow-up and evaluation for secondary causes of weight loss. Patients may lose weight at a faster rate with the new antiobesity medications, but clinicians still should ensure that age-appropriate health maintenance screening is done and be vigilant for secondary causes of weight changes.
“Have you tried losing weight yet?” Three times. That’s how many times Chanté Burkett went to her doctor about her painful, enlarging firm stomach. She was advised to continue working on weight loss, which she did diligently. But Ms. Burkett’s abdomen kept growing and her concerns were dismissed. A visit to urgent care and a CT scan revealed that Ms. Burkett’s excess abdominal “fat” was a 13-lb mucinous cystadenoma. Sadly, cases like hers aren’t rare, isolated events. Weight bias can cause anchoring on one diagnosis, preventing consideration of other diagnostic possibilities. Even worse, anchoring will lead to the wrong intervention, such as prescribing weight loss for presumed increased adiposity instead of ordering the appropriate testing.
It’s also essential to recognize that, even if someone does have the disease of obesity, weight loss isn’t the solution to every medical concern. Even if weight loss is helpful, other, more pressing treatments may still be necessary. Telling a person with obesity who has an acute complaint to “just lose weight” is comparable to telling a patient with coronary artery disease who presents with an 80% vessel occlusion and chest pain to follow a low-fat diet. In both cases, you need to address the acute concern appropriately, then focus on the chronic treatment.
Ways to reduce clinical weight bias
How do you reduce clinical weight bias?
Ask, don’t assume. The information from the scale is simply data. Instead of judging it positively or negatively and creating a story, ask the patient. An unbiased way to approach the conversation is to say, “Great to see you. You seem [positive adjective of choice]. How have you been?” Wait until the vitals section to objectively discuss weight unless the patient offers the discussion earlier or their chief complaint lists a weight-related concern.
Order necessary tests to evaluate weight. Weight is the vital sign that people wear externally, so we feel that we can readily interpret it without any further assessment. However, resist the urge to interpret scale data without context. Keeping an open mind helps prevent anchoring and missing critical clues in the clinical history.
Address weight changes effectively. Sometimes there is an indication to prescribe weight loss as part of the treatment plan. However, remember that weight loss isn’t simply “calories in vs. calories out.” Obesity is a complex medical disease that requires a multimodal treatment approach. As clinicians, we have access to the most powerful tools for weight loss. Unfortunately, weight bias contributes to limited prescribing of metabolic medications (“antiobesity medications” or AOMs). In addition, systemic weight bias prevents insurance coverage of AOMs. The Treat and Reduce Obesity Act has been introduced into Congress to help improve life-transforming access to AOMs.
Acknowledge your bias. Our experiences make us all susceptible to bias. The Harvard Weight Implicit Association Test is free and a helpful way to assess your level of weight bias. I take it annually to ensure that I remain objective in my practice.
Addressing weight bias needs to extend beyond the individual level.
Systemically, health care needs to address the following:
Language. Use people-centered language. For example, “People aren’t obese. They have obesity.”
Accessibility. Health care settings must be comfortable and accessible for people of all sizes. Furthermore, improvements to access the services that comprehensive obesity care requires, such as AOMs, bariatric procedures and bariatric surgery, mental health care, nutrition, fitness specialists, health coaches, and more, are needed.
Education. Medical students and trainees have to learn the newest obesity science and know how to treat obesity effectively. Acknowledge and address biased tools. Recent data have shown that some of our screening tools, such as body mass index, have inherent bias. It’s time to focus on using improved diagnostic tools and personalized treatments.
We are at a pivotal time in our scientific understanding of body weight regulation and the disease of obesity. Clinical weight bias is primarily rooted in flawed science influenced by biased cultural norms and other forms of discrimination, such as racial and gender bias. We must move past assumptions to give our patients the optimal individualized care they need. So next time you observe a weight change, instead of commenting on their weight, say, “Great to see you! How have you been?”
S*: Initial has been changed to protect privacy.
Dr. Gonsahn-Bollie is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating. Connect with her at www.embraceyouweightloss.com or on Instagram @embraceyoumd. Her bestselling book, “Embrace You: Your Guide to Transforming Weight Loss Misconceptions Into Lifelong Wellness”, was Healthline.com’s Best Overall Weight Loss Book of 2022 and one of Livestrong.com’s 8 Best Weight-Loss Books to Read in 2022. She has disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
It was the start of the fall semester of my sophomore year of college.
At my small women’s college, the previous semester’s gossip had been about our classmate, S*. She had gone from being very thin to noticeably gaining a lot of weight in a few months. The rumors were that S was pregnant and gave birth over summer break. As a busy biology premed major, this was my first time hearing the news. So when I saw her standing in the hallway, back to her previous weight, I was excited for her.
In true extravert fashion, I commented on the baby and her new size. But no sooner had the words left my mouth than I regretted them.
The hall grew awkwardly silent as S’s face flushed and she asked, “Excuse me?!” Instantly I knew that the rumors weren’t true.
Thankfully, at that moment, the classroom opened and we walked in. Whew! After class, S asked if we could talk. She explained that she had a thyroid tumor and struggled to adjust to the treatments, which caused her weight fluctuations. She had never been pregnant.
My awkward statement had been the first time anyone on campus had directly mentioned her weight, though she suspected that people were talking about her. We became fast friends after this rocky beginning. Although we lost touch after college, S taught me an invaluable lesson about making assumptions about people’s weight: Ask before you assume.
Now, years later, as an internist and obesity specialist, this lesson continues to be reinforced daily.
In daily life, comments about weight can be perceived as rude. In the clinical setting, however, assumptions about weight are a form of weight bias. Weight bias can lead to weight stigma and even be dangerous to health care.
Let’s discuss the insidious influence of weight bias in health care through two commonly used phrases and then look at a few solutions to address weight bias in health care individually and systematically.
Common weight bias assumptions
“Great job, you lost weight!” In checking your patient’s vital signs, you notice that this patient with obesity has a significant weight change. You congratulate them upon entering the room. Unfortunately, their weight loss was a result of minimal eating after losing a loved one. This isn’t healthy weight loss. One of the adverse effects of weight bias is that it infers that weight loss is always a good thing, especially in people with larger bodies. This is a dangerous presumption. Let’s remember that the body favors fat storage, hence why “unintentional weight loss” is a recognized medical condition prompting evaluation. We have to be careful not to celebrate weight loss “at all costs,” such as fad diets that haven’t been shown to improve health outcomes.
Furthermore, patients who lose weight quickly (more than 4-8 lb/month) require closer follow-up and evaluation for secondary causes of weight loss. Patients may lose weight at a faster rate with the new antiobesity medications, but clinicians still should ensure that age-appropriate health maintenance screening is done and be vigilant for secondary causes of weight changes.
“Have you tried losing weight yet?” Three times. That’s how many times Chanté Burkett went to her doctor about her painful, enlarging firm stomach. She was advised to continue working on weight loss, which she did diligently. But Ms. Burkett’s abdomen kept growing and her concerns were dismissed. A visit to urgent care and a CT scan revealed that Ms. Burkett’s excess abdominal “fat” was a 13-lb mucinous cystadenoma. Sadly, cases like hers aren’t rare, isolated events. Weight bias can cause anchoring on one diagnosis, preventing consideration of other diagnostic possibilities. Even worse, anchoring will lead to the wrong intervention, such as prescribing weight loss for presumed increased adiposity instead of ordering the appropriate testing.
It’s also essential to recognize that, even if someone does have the disease of obesity, weight loss isn’t the solution to every medical concern. Even if weight loss is helpful, other, more pressing treatments may still be necessary. Telling a person with obesity who has an acute complaint to “just lose weight” is comparable to telling a patient with coronary artery disease who presents with an 80% vessel occlusion and chest pain to follow a low-fat diet. In both cases, you need to address the acute concern appropriately, then focus on the chronic treatment.
Ways to reduce clinical weight bias
How do you reduce clinical weight bias?
Ask, don’t assume. The information from the scale is simply data. Instead of judging it positively or negatively and creating a story, ask the patient. An unbiased way to approach the conversation is to say, “Great to see you. You seem [positive adjective of choice]. How have you been?” Wait until the vitals section to objectively discuss weight unless the patient offers the discussion earlier or their chief complaint lists a weight-related concern.
Order necessary tests to evaluate weight. Weight is the vital sign that people wear externally, so we feel that we can readily interpret it without any further assessment. However, resist the urge to interpret scale data without context. Keeping an open mind helps prevent anchoring and missing critical clues in the clinical history.
Address weight changes effectively. Sometimes there is an indication to prescribe weight loss as part of the treatment plan. However, remember that weight loss isn’t simply “calories in vs. calories out.” Obesity is a complex medical disease that requires a multimodal treatment approach. As clinicians, we have access to the most powerful tools for weight loss. Unfortunately, weight bias contributes to limited prescribing of metabolic medications (“antiobesity medications” or AOMs). In addition, systemic weight bias prevents insurance coverage of AOMs. The Treat and Reduce Obesity Act has been introduced into Congress to help improve life-transforming access to AOMs.
Acknowledge your bias. Our experiences make us all susceptible to bias. The Harvard Weight Implicit Association Test is free and a helpful way to assess your level of weight bias. I take it annually to ensure that I remain objective in my practice.
Addressing weight bias needs to extend beyond the individual level.
Systemically, health care needs to address the following:
Language. Use people-centered language. For example, “People aren’t obese. They have obesity.”
Accessibility. Health care settings must be comfortable and accessible for people of all sizes. Furthermore, improvements to access the services that comprehensive obesity care requires, such as AOMs, bariatric procedures and bariatric surgery, mental health care, nutrition, fitness specialists, health coaches, and more, are needed.
Education. Medical students and trainees have to learn the newest obesity science and know how to treat obesity effectively. Acknowledge and address biased tools. Recent data have shown that some of our screening tools, such as body mass index, have inherent bias. It’s time to focus on using improved diagnostic tools and personalized treatments.
We are at a pivotal time in our scientific understanding of body weight regulation and the disease of obesity. Clinical weight bias is primarily rooted in flawed science influenced by biased cultural norms and other forms of discrimination, such as racial and gender bias. We must move past assumptions to give our patients the optimal individualized care they need. So next time you observe a weight change, instead of commenting on their weight, say, “Great to see you! How have you been?”
S*: Initial has been changed to protect privacy.
Dr. Gonsahn-Bollie is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating. Connect with her at www.embraceyouweightloss.com or on Instagram @embraceyoumd. Her bestselling book, “Embrace You: Your Guide to Transforming Weight Loss Misconceptions Into Lifelong Wellness”, was Healthline.com’s Best Overall Weight Loss Book of 2022 and one of Livestrong.com’s 8 Best Weight-Loss Books to Read in 2022. She has disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
It was the start of the fall semester of my sophomore year of college.
At my small women’s college, the previous semester’s gossip had been about our classmate, S*. She had gone from being very thin to noticeably gaining a lot of weight in a few months. The rumors were that S was pregnant and gave birth over summer break. As a busy biology premed major, this was my first time hearing the news. So when I saw her standing in the hallway, back to her previous weight, I was excited for her.
In true extravert fashion, I commented on the baby and her new size. But no sooner had the words left my mouth than I regretted them.
The hall grew awkwardly silent as S’s face flushed and she asked, “Excuse me?!” Instantly I knew that the rumors weren’t true.
Thankfully, at that moment, the classroom opened and we walked in. Whew! After class, S asked if we could talk. She explained that she had a thyroid tumor and struggled to adjust to the treatments, which caused her weight fluctuations. She had never been pregnant.
My awkward statement had been the first time anyone on campus had directly mentioned her weight, though she suspected that people were talking about her. We became fast friends after this rocky beginning. Although we lost touch after college, S taught me an invaluable lesson about making assumptions about people’s weight: Ask before you assume.
Now, years later, as an internist and obesity specialist, this lesson continues to be reinforced daily.
In daily life, comments about weight can be perceived as rude. In the clinical setting, however, assumptions about weight are a form of weight bias. Weight bias can lead to weight stigma and even be dangerous to health care.
Let’s discuss the insidious influence of weight bias in health care through two commonly used phrases and then look at a few solutions to address weight bias in health care individually and systematically.
Common weight bias assumptions
“Great job, you lost weight!” In checking your patient’s vital signs, you notice that this patient with obesity has a significant weight change. You congratulate them upon entering the room. Unfortunately, their weight loss was a result of minimal eating after losing a loved one. This isn’t healthy weight loss. One of the adverse effects of weight bias is that it infers that weight loss is always a good thing, especially in people with larger bodies. This is a dangerous presumption. Let’s remember that the body favors fat storage, hence why “unintentional weight loss” is a recognized medical condition prompting evaluation. We have to be careful not to celebrate weight loss “at all costs,” such as fad diets that haven’t been shown to improve health outcomes.
Furthermore, patients who lose weight quickly (more than 4-8 lb/month) require closer follow-up and evaluation for secondary causes of weight loss. Patients may lose weight at a faster rate with the new antiobesity medications, but clinicians still should ensure that age-appropriate health maintenance screening is done and be vigilant for secondary causes of weight changes.
“Have you tried losing weight yet?” Three times. That’s how many times Chanté Burkett went to her doctor about her painful, enlarging firm stomach. She was advised to continue working on weight loss, which she did diligently. But Ms. Burkett’s abdomen kept growing and her concerns were dismissed. A visit to urgent care and a CT scan revealed that Ms. Burkett’s excess abdominal “fat” was a 13-lb mucinous cystadenoma. Sadly, cases like hers aren’t rare, isolated events. Weight bias can cause anchoring on one diagnosis, preventing consideration of other diagnostic possibilities. Even worse, anchoring will lead to the wrong intervention, such as prescribing weight loss for presumed increased adiposity instead of ordering the appropriate testing.
It’s also essential to recognize that, even if someone does have the disease of obesity, weight loss isn’t the solution to every medical concern. Even if weight loss is helpful, other, more pressing treatments may still be necessary. Telling a person with obesity who has an acute complaint to “just lose weight” is comparable to telling a patient with coronary artery disease who presents with an 80% vessel occlusion and chest pain to follow a low-fat diet. In both cases, you need to address the acute concern appropriately, then focus on the chronic treatment.
Ways to reduce clinical weight bias
How do you reduce clinical weight bias?
Ask, don’t assume. The information from the scale is simply data. Instead of judging it positively or negatively and creating a story, ask the patient. An unbiased way to approach the conversation is to say, “Great to see you. You seem [positive adjective of choice]. How have you been?” Wait until the vitals section to objectively discuss weight unless the patient offers the discussion earlier or their chief complaint lists a weight-related concern.
Order necessary tests to evaluate weight. Weight is the vital sign that people wear externally, so we feel that we can readily interpret it without any further assessment. However, resist the urge to interpret scale data without context. Keeping an open mind helps prevent anchoring and missing critical clues in the clinical history.
Address weight changes effectively. Sometimes there is an indication to prescribe weight loss as part of the treatment plan. However, remember that weight loss isn’t simply “calories in vs. calories out.” Obesity is a complex medical disease that requires a multimodal treatment approach. As clinicians, we have access to the most powerful tools for weight loss. Unfortunately, weight bias contributes to limited prescribing of metabolic medications (“antiobesity medications” or AOMs). In addition, systemic weight bias prevents insurance coverage of AOMs. The Treat and Reduce Obesity Act has been introduced into Congress to help improve life-transforming access to AOMs.
Acknowledge your bias. Our experiences make us all susceptible to bias. The Harvard Weight Implicit Association Test is free and a helpful way to assess your level of weight bias. I take it annually to ensure that I remain objective in my practice.
Addressing weight bias needs to extend beyond the individual level.
Systemically, health care needs to address the following:
Language. Use people-centered language. For example, “People aren’t obese. They have obesity.”
Accessibility. Health care settings must be comfortable and accessible for people of all sizes. Furthermore, improvements to access the services that comprehensive obesity care requires, such as AOMs, bariatric procedures and bariatric surgery, mental health care, nutrition, fitness specialists, health coaches, and more, are needed.
Education. Medical students and trainees have to learn the newest obesity science and know how to treat obesity effectively. Acknowledge and address biased tools. Recent data have shown that some of our screening tools, such as body mass index, have inherent bias. It’s time to focus on using improved diagnostic tools and personalized treatments.
We are at a pivotal time in our scientific understanding of body weight regulation and the disease of obesity. Clinical weight bias is primarily rooted in flawed science influenced by biased cultural norms and other forms of discrimination, such as racial and gender bias. We must move past assumptions to give our patients the optimal individualized care they need. So next time you observe a weight change, instead of commenting on their weight, say, “Great to see you! How have you been?”
S*: Initial has been changed to protect privacy.
Dr. Gonsahn-Bollie is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating. Connect with her at www.embraceyouweightloss.com or on Instagram @embraceyoumd. Her bestselling book, “Embrace You: Your Guide to Transforming Weight Loss Misconceptions Into Lifelong Wellness”, was Healthline.com’s Best Overall Weight Loss Book of 2022 and one of Livestrong.com’s 8 Best Weight-Loss Books to Read in 2022. She has disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
The challenge of incidentally detected interstitial lung abnormalities
Clinicians working within the U.S. health care system order CTs; it’s just what we do, and we do it a lot. This isn’t necessarily bad, but an inevitable byproduct is the pandemic of incidental findings. One underrecognized but frequent “incidentaloma” on CT is an interstitial lung abnormality (ILA). The Fleischner Society defines an ILA as honeycombing, traction bronchiectasis, parenchymal distortions, and reticular abnormalities that take up more than 5% of a particular lung zone in a patient without a clinical diagnosis of interstitial lung disease (ILD). In essence, ILAs are both a radiographic and a clinical diagnosis.
ILAs are common. With the advent of lung cancer screening and advances in CT technology, we’re now inundated with detailed images of lung parenchyma in older smokers who are at high risk for respiratory disease. The resulting opportunity for early identification of disease is as exciting as the risk for overdiagnosis, excessive testing, and unnecessary treatment is frightening. Early diagnosis remains critical for preventing irreversible respiratory disease. But as with any disease process, when we attempt to detect pathology before it has become apparent, the line between benign change and true abnormality is blurred.
Such is the challenge with ILAs. Past studies have shown an association between ILAs and morbidity and mortality, but considerable uncertainty persists over what the ILAs represent and how they should be managed. A recent study published in the American Journal of Respiratory and Critical Care Medicine provides some clarity. The authors used data from the COPDGene cohort to correlate ILAs with lung testing, and functional and respiratory outcomes. As with other studies, they found that approximately 10% of the COPDGene patients that they examined had ILAs on CT and half of those met their criteria for “suspected ILD.” Suspected ILD was defined radiographically (definite fibrosis) and on lung function testing (abnormal forced vital capacity [FVC] or diffusing capacity of the lungs for carbon monoxide [DLCO]). The patients with suspected ILD had worse clinical outcomes; being a Black individual, pack-years of smoking, and GOLD stage on spirometry were independently associated with suspected ILD.
This type of study is urgently needed. Given their high prevalence, we’re in dire need of a valid model for risk stratifying ILAs. The authors of this study have moved us closer, but we’ve still got a long way to go. The study has significant limitations. First, although patients with previous documentation of ILD were excluded from COPDGene, no formal, multidisciplinary assessment was performed; therefore, some of the patients labeled as having ILA probably had diagnosable ILD. Their possible inclusion would falsely increase the prevalence of clinically important ILAs and exaggerate the relationship between ILAs and clinical outcomes.
The rhetorical gymnastics performed throughout the paper are necessary yet problematic. “Suspected ILD” is not a recognized diagnosis and the definition is therefore arbitrary. To the extent that “suspected ILD” requires an abnormality on spirometry or DLCO, one could argue it’s the lung function changes and not the radiographic findings that are driving the differences. In fact, “suspected ILD” was defined by lung function more often than radiographic criteria (16% had definite fibrosis on CT, 57% had an abnormal FVC, and 67% had an abnormal DLCO). Patients with ILAs without suspected ILD had outcomes that weren’t statistically different from those with no ILAs at all, implying that the lung testing and not the ILA is the better discriminator. Regardless, this leads us back to where we started before this paper was published: ILAs require lung function testing and referral to a pulmonologist for proper risk stratification. An accompanying editorial highlights these and other limitations.
One particular problem that isn’t addressed by the authors or the editorial is their findings on race. The authors concluded that Black persons with ILAs are more likely to have “suspected ILD.” However, their definition suffers from an insidious form of incorporation bias generated by the way they handled their DLCO reference values. The Global Lung Function Initiative equations they used were derived exclusively from White persons. In accordance with the recent American Thoracic Society/European Respiratory Society (ATS/ERS) statement on lung testing, the authors did not apply a fixed correction factor to adjust for race. Without such an adjustment, Black persons would be biased toward having lower percent predicted values for DLCO. In short, self-identified Black individuals would be more likely to have a predicted DLCO of less than 70% and to therefore meet criteria for “suspected ILD.” The resulting effects on biologic plausibility, causal inference, and the strength of the relationship between “suspected ILD” and clinical outcomes will vary by whether the association between race and lung function is considered a product of inherent biologic variability or a result of external (socioeconomic and environmental) effects.
In summary, ILAs remain a challenge for radiologists, primary care providers, pulmonologists, and anyone else who orders a CT of the lungs. Despite its limitations, I believe the recently published paper pushes us forward conceptually. Perhaps its most important contribution is showing that 50% of ILAs are clinically insignificant by definition. This offers further reassurance that a subset of ILAs can be dismissed. Now, all we need is an easy, cost-effective, and efficient way to identify this subset.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He covers a wide range of topics in pulmonary, critical care, and sleep medicine. He disclosed ties to Metapharm Inc., CHEST College, and WebMD. A version of this article originally appeared on Medscape.com.
Clinicians working within the U.S. health care system order CTs; it’s just what we do, and we do it a lot. This isn’t necessarily bad, but an inevitable byproduct is the pandemic of incidental findings. One underrecognized but frequent “incidentaloma” on CT is an interstitial lung abnormality (ILA). The Fleischner Society defines an ILA as honeycombing, traction bronchiectasis, parenchymal distortions, and reticular abnormalities that take up more than 5% of a particular lung zone in a patient without a clinical diagnosis of interstitial lung disease (ILD). In essence, ILAs are both a radiographic and a clinical diagnosis.
ILAs are common. With the advent of lung cancer screening and advances in CT technology, we’re now inundated with detailed images of lung parenchyma in older smokers who are at high risk for respiratory disease. The resulting opportunity for early identification of disease is as exciting as the risk for overdiagnosis, excessive testing, and unnecessary treatment is frightening. Early diagnosis remains critical for preventing irreversible respiratory disease. But as with any disease process, when we attempt to detect pathology before it has become apparent, the line between benign change and true abnormality is blurred.
Such is the challenge with ILAs. Past studies have shown an association between ILAs and morbidity and mortality, but considerable uncertainty persists over what the ILAs represent and how they should be managed. A recent study published in the American Journal of Respiratory and Critical Care Medicine provides some clarity. The authors used data from the COPDGene cohort to correlate ILAs with lung testing, and functional and respiratory outcomes. As with other studies, they found that approximately 10% of the COPDGene patients that they examined had ILAs on CT and half of those met their criteria for “suspected ILD.” Suspected ILD was defined radiographically (definite fibrosis) and on lung function testing (abnormal forced vital capacity [FVC] or diffusing capacity of the lungs for carbon monoxide [DLCO]). The patients with suspected ILD had worse clinical outcomes; being a Black individual, pack-years of smoking, and GOLD stage on spirometry were independently associated with suspected ILD.
This type of study is urgently needed. Given their high prevalence, we’re in dire need of a valid model for risk stratifying ILAs. The authors of this study have moved us closer, but we’ve still got a long way to go. The study has significant limitations. First, although patients with previous documentation of ILD were excluded from COPDGene, no formal, multidisciplinary assessment was performed; therefore, some of the patients labeled as having ILA probably had diagnosable ILD. Their possible inclusion would falsely increase the prevalence of clinically important ILAs and exaggerate the relationship between ILAs and clinical outcomes.
The rhetorical gymnastics performed throughout the paper are necessary yet problematic. “Suspected ILD” is not a recognized diagnosis and the definition is therefore arbitrary. To the extent that “suspected ILD” requires an abnormality on spirometry or DLCO, one could argue it’s the lung function changes and not the radiographic findings that are driving the differences. In fact, “suspected ILD” was defined by lung function more often than radiographic criteria (16% had definite fibrosis on CT, 57% had an abnormal FVC, and 67% had an abnormal DLCO). Patients with ILAs without suspected ILD had outcomes that weren’t statistically different from those with no ILAs at all, implying that the lung testing and not the ILA is the better discriminator. Regardless, this leads us back to where we started before this paper was published: ILAs require lung function testing and referral to a pulmonologist for proper risk stratification. An accompanying editorial highlights these and other limitations.
One particular problem that isn’t addressed by the authors or the editorial is their findings on race. The authors concluded that Black persons with ILAs are more likely to have “suspected ILD.” However, their definition suffers from an insidious form of incorporation bias generated by the way they handled their DLCO reference values. The Global Lung Function Initiative equations they used were derived exclusively from White persons. In accordance with the recent American Thoracic Society/European Respiratory Society (ATS/ERS) statement on lung testing, the authors did not apply a fixed correction factor to adjust for race. Without such an adjustment, Black persons would be biased toward having lower percent predicted values for DLCO. In short, self-identified Black individuals would be more likely to have a predicted DLCO of less than 70% and to therefore meet criteria for “suspected ILD.” The resulting effects on biologic plausibility, causal inference, and the strength of the relationship between “suspected ILD” and clinical outcomes will vary by whether the association between race and lung function is considered a product of inherent biologic variability or a result of external (socioeconomic and environmental) effects.
In summary, ILAs remain a challenge for radiologists, primary care providers, pulmonologists, and anyone else who orders a CT of the lungs. Despite its limitations, I believe the recently published paper pushes us forward conceptually. Perhaps its most important contribution is showing that 50% of ILAs are clinically insignificant by definition. This offers further reassurance that a subset of ILAs can be dismissed. Now, all we need is an easy, cost-effective, and efficient way to identify this subset.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He covers a wide range of topics in pulmonary, critical care, and sleep medicine. He disclosed ties to Metapharm Inc., CHEST College, and WebMD. A version of this article originally appeared on Medscape.com.
Clinicians working within the U.S. health care system order CTs; it’s just what we do, and we do it a lot. This isn’t necessarily bad, but an inevitable byproduct is the pandemic of incidental findings. One underrecognized but frequent “incidentaloma” on CT is an interstitial lung abnormality (ILA). The Fleischner Society defines an ILA as honeycombing, traction bronchiectasis, parenchymal distortions, and reticular abnormalities that take up more than 5% of a particular lung zone in a patient without a clinical diagnosis of interstitial lung disease (ILD). In essence, ILAs are both a radiographic and a clinical diagnosis.
ILAs are common. With the advent of lung cancer screening and advances in CT technology, we’re now inundated with detailed images of lung parenchyma in older smokers who are at high risk for respiratory disease. The resulting opportunity for early identification of disease is as exciting as the risk for overdiagnosis, excessive testing, and unnecessary treatment is frightening. Early diagnosis remains critical for preventing irreversible respiratory disease. But as with any disease process, when we attempt to detect pathology before it has become apparent, the line between benign change and true abnormality is blurred.
Such is the challenge with ILAs. Past studies have shown an association between ILAs and morbidity and mortality, but considerable uncertainty persists over what the ILAs represent and how they should be managed. A recent study published in the American Journal of Respiratory and Critical Care Medicine provides some clarity. The authors used data from the COPDGene cohort to correlate ILAs with lung testing, and functional and respiratory outcomes. As with other studies, they found that approximately 10% of the COPDGene patients that they examined had ILAs on CT and half of those met their criteria for “suspected ILD.” Suspected ILD was defined radiographically (definite fibrosis) and on lung function testing (abnormal forced vital capacity [FVC] or diffusing capacity of the lungs for carbon monoxide [DLCO]). The patients with suspected ILD had worse clinical outcomes; being a Black individual, pack-years of smoking, and GOLD stage on spirometry were independently associated with suspected ILD.
This type of study is urgently needed. Given their high prevalence, we’re in dire need of a valid model for risk stratifying ILAs. The authors of this study have moved us closer, but we’ve still got a long way to go. The study has significant limitations. First, although patients with previous documentation of ILD were excluded from COPDGene, no formal, multidisciplinary assessment was performed; therefore, some of the patients labeled as having ILA probably had diagnosable ILD. Their possible inclusion would falsely increase the prevalence of clinically important ILAs and exaggerate the relationship between ILAs and clinical outcomes.
The rhetorical gymnastics performed throughout the paper are necessary yet problematic. “Suspected ILD” is not a recognized diagnosis and the definition is therefore arbitrary. To the extent that “suspected ILD” requires an abnormality on spirometry or DLCO, one could argue it’s the lung function changes and not the radiographic findings that are driving the differences. In fact, “suspected ILD” was defined by lung function more often than radiographic criteria (16% had definite fibrosis on CT, 57% had an abnormal FVC, and 67% had an abnormal DLCO). Patients with ILAs without suspected ILD had outcomes that weren’t statistically different from those with no ILAs at all, implying that the lung testing and not the ILA is the better discriminator. Regardless, this leads us back to where we started before this paper was published: ILAs require lung function testing and referral to a pulmonologist for proper risk stratification. An accompanying editorial highlights these and other limitations.
One particular problem that isn’t addressed by the authors or the editorial is their findings on race. The authors concluded that Black persons with ILAs are more likely to have “suspected ILD.” However, their definition suffers from an insidious form of incorporation bias generated by the way they handled their DLCO reference values. The Global Lung Function Initiative equations they used were derived exclusively from White persons. In accordance with the recent American Thoracic Society/European Respiratory Society (ATS/ERS) statement on lung testing, the authors did not apply a fixed correction factor to adjust for race. Without such an adjustment, Black persons would be biased toward having lower percent predicted values for DLCO. In short, self-identified Black individuals would be more likely to have a predicted DLCO of less than 70% and to therefore meet criteria for “suspected ILD.” The resulting effects on biologic plausibility, causal inference, and the strength of the relationship between “suspected ILD” and clinical outcomes will vary by whether the association between race and lung function is considered a product of inherent biologic variability or a result of external (socioeconomic and environmental) effects.
In summary, ILAs remain a challenge for radiologists, primary care providers, pulmonologists, and anyone else who orders a CT of the lungs. Despite its limitations, I believe the recently published paper pushes us forward conceptually. Perhaps its most important contribution is showing that 50% of ILAs are clinically insignificant by definition. This offers further reassurance that a subset of ILAs can be dismissed. Now, all we need is an easy, cost-effective, and efficient way to identify this subset.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He covers a wide range of topics in pulmonary, critical care, and sleep medicine. He disclosed ties to Metapharm Inc., CHEST College, and WebMD. A version of this article originally appeared on Medscape.com.
‘Ozempic face’: Accepting wrinkles for improved health
This transcript has been edited for clarity.
Last week, a number of patients emailed me regarding their concerns about this phenomenon known as Ozempic face. I went on to read about what this meant. I live in Los Angeles, where most people appear to be on semaglutide (Ozempic). It’s the phenomenon where people lose weight relatively rapidly, making their faces thin out. Then what happens, apparently, is they look older because their face is more wrinkled and baggier. They might have to have further plastic surgery. I say that with slight sarcasm because of where I live.
I want to talk about what I think about this, living here where there’s a great pressure to prescribe semaglutide off label, and what I think about it for my patients with diabetes.
Historically, we haven’t had much in terms of effective medication for treating obesity, and frankly, now we do. We now have agents that are effective, that have relatively few side effects, and that have become part of what’s out there. People now want to use these agents, semaglutide, and there’s been a great need for these agents.
The problem, however, is twofold. One, as we all know, is that it has basically caused a shortage of medication for treating our patients who actually have type 2 diabetes and really need these medications to manage their disease. Then we have people who want these medications who can’t pay for them. Insurance doesn’t cover obesity medications, which is problematic and actually quite frustrating for people who, I think, really would benefit from using these medications.
What I tell people, frankly, is that until I have enough supply for my patients with type 2 diabetes, who need these agents to control their blood sugars, I want to keep this class of drugs available to them. I also hope we’re able to expand it more and more with improving insurance coverage – and that’s a big if, if you ask me – both for people who have prediabetes and for patients who are overweight and obese, because I think it’s really hard for people to lose weight.
It’s frustrating, and for many people, being overweight and obese causes all sorts of other health issues, not only diabetes. I believe that these drugs are both safe and effective and should be more available. I do think we need to be careful in terms of who we prescribe them to, at least at the moment. Hopefully, we’ll be able to expand their use.
Anything that can encourage our population to lose weight and maintain that weight loss is very important. We need to couple weight loss medications with lifestyle interventions. I think people can out-eat any medication; therefore, it’s very important to encourage our patients to eat better, to exercise more, and to do all the other things they need to do to reduce their risks for other comorbidities.
I am incredibly happy to have these newer agents on the market. I tell my patients – at least those who have diabetes – that they have to accept looking a little bit too thin for the benefits that we can see in using these medications.
Thank you.
Dr. Peters is professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts, and three books, on diabetes, and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations. She has ties with Abbott Diabetes Care, AstraZeneca Becton Dickinson, Boehringer Ingelheim Pharmaceuticals, Dexcom, Eli Lilly, Lexicon Pharmaceuticals, Livongo, MannKind Corporation, Medscape, Merck, Novo Nordisk, Omada Health, OptumHealth, Sanofi, and Zafgen. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Last week, a number of patients emailed me regarding their concerns about this phenomenon known as Ozempic face. I went on to read about what this meant. I live in Los Angeles, where most people appear to be on semaglutide (Ozempic). It’s the phenomenon where people lose weight relatively rapidly, making their faces thin out. Then what happens, apparently, is they look older because their face is more wrinkled and baggier. They might have to have further plastic surgery. I say that with slight sarcasm because of where I live.
I want to talk about what I think about this, living here where there’s a great pressure to prescribe semaglutide off label, and what I think about it for my patients with diabetes.
Historically, we haven’t had much in terms of effective medication for treating obesity, and frankly, now we do. We now have agents that are effective, that have relatively few side effects, and that have become part of what’s out there. People now want to use these agents, semaglutide, and there’s been a great need for these agents.
The problem, however, is twofold. One, as we all know, is that it has basically caused a shortage of medication for treating our patients who actually have type 2 diabetes and really need these medications to manage their disease. Then we have people who want these medications who can’t pay for them. Insurance doesn’t cover obesity medications, which is problematic and actually quite frustrating for people who, I think, really would benefit from using these medications.
What I tell people, frankly, is that until I have enough supply for my patients with type 2 diabetes, who need these agents to control their blood sugars, I want to keep this class of drugs available to them. I also hope we’re able to expand it more and more with improving insurance coverage – and that’s a big if, if you ask me – both for people who have prediabetes and for patients who are overweight and obese, because I think it’s really hard for people to lose weight.
It’s frustrating, and for many people, being overweight and obese causes all sorts of other health issues, not only diabetes. I believe that these drugs are both safe and effective and should be more available. I do think we need to be careful in terms of who we prescribe them to, at least at the moment. Hopefully, we’ll be able to expand their use.
Anything that can encourage our population to lose weight and maintain that weight loss is very important. We need to couple weight loss medications with lifestyle interventions. I think people can out-eat any medication; therefore, it’s very important to encourage our patients to eat better, to exercise more, and to do all the other things they need to do to reduce their risks for other comorbidities.
I am incredibly happy to have these newer agents on the market. I tell my patients – at least those who have diabetes – that they have to accept looking a little bit too thin for the benefits that we can see in using these medications.
Thank you.
Dr. Peters is professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts, and three books, on diabetes, and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations. She has ties with Abbott Diabetes Care, AstraZeneca Becton Dickinson, Boehringer Ingelheim Pharmaceuticals, Dexcom, Eli Lilly, Lexicon Pharmaceuticals, Livongo, MannKind Corporation, Medscape, Merck, Novo Nordisk, Omada Health, OptumHealth, Sanofi, and Zafgen. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Last week, a number of patients emailed me regarding their concerns about this phenomenon known as Ozempic face. I went on to read about what this meant. I live in Los Angeles, where most people appear to be on semaglutide (Ozempic). It’s the phenomenon where people lose weight relatively rapidly, making their faces thin out. Then what happens, apparently, is they look older because their face is more wrinkled and baggier. They might have to have further plastic surgery. I say that with slight sarcasm because of where I live.
I want to talk about what I think about this, living here where there’s a great pressure to prescribe semaglutide off label, and what I think about it for my patients with diabetes.
Historically, we haven’t had much in terms of effective medication for treating obesity, and frankly, now we do. We now have agents that are effective, that have relatively few side effects, and that have become part of what’s out there. People now want to use these agents, semaglutide, and there’s been a great need for these agents.
The problem, however, is twofold. One, as we all know, is that it has basically caused a shortage of medication for treating our patients who actually have type 2 diabetes and really need these medications to manage their disease. Then we have people who want these medications who can’t pay for them. Insurance doesn’t cover obesity medications, which is problematic and actually quite frustrating for people who, I think, really would benefit from using these medications.
What I tell people, frankly, is that until I have enough supply for my patients with type 2 diabetes, who need these agents to control their blood sugars, I want to keep this class of drugs available to them. I also hope we’re able to expand it more and more with improving insurance coverage – and that’s a big if, if you ask me – both for people who have prediabetes and for patients who are overweight and obese, because I think it’s really hard for people to lose weight.
It’s frustrating, and for many people, being overweight and obese causes all sorts of other health issues, not only diabetes. I believe that these drugs are both safe and effective and should be more available. I do think we need to be careful in terms of who we prescribe them to, at least at the moment. Hopefully, we’ll be able to expand their use.
Anything that can encourage our population to lose weight and maintain that weight loss is very important. We need to couple weight loss medications with lifestyle interventions. I think people can out-eat any medication; therefore, it’s very important to encourage our patients to eat better, to exercise more, and to do all the other things they need to do to reduce their risks for other comorbidities.
I am incredibly happy to have these newer agents on the market. I tell my patients – at least those who have diabetes – that they have to accept looking a little bit too thin for the benefits that we can see in using these medications.
Thank you.
Dr. Peters is professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts, and three books, on diabetes, and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations. She has ties with Abbott Diabetes Care, AstraZeneca Becton Dickinson, Boehringer Ingelheim Pharmaceuticals, Dexcom, Eli Lilly, Lexicon Pharmaceuticals, Livongo, MannKind Corporation, Medscape, Merck, Novo Nordisk, Omada Health, OptumHealth, Sanofi, and Zafgen. A version of this article originally appeared on Medscape.com.