User login
Too high: Can you ID pot-induced psychosis?
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
Pretransfer visits with pediatric and adult rheumatologists smooth adolescent transition
NEW ORLEANS – Implementing a pediatric transition program in which a patient meets with both their pediatric and soon-to-be adult rheumatologist during a visit before formal transition resulted in less time setting up the first adult visit, according to research presented at the Pediatric Rheumatology Symposium.
The presentation was one of two that focused on ways to improve the transition from pediatric to adult care for rheumatology patients. The other, a poster from researchers at Baylor College of Medicine, Houston, took the first steps toward learning what factors can help predict a successful transition.
“This period of transitioning from pediatric to adult care, both rheumatology specific and otherwise, is a high-risk time,” John M. Bridges, MD, a fourth-year pediatric rheumatology fellow at the University of Alabama at Birmingham, told attendees. “There are changes in insurance coverage, employment, geographic mobility, and shifting responsibilities between parents and children in the setting of a still-developing frontal lobe that contribute to the risk of this period. Risks include disease flare, and then organ damage, as well as issues with decreasing medication and therapy, adherence, unscheduled care utilization, and increasing loss to follow-up.”
Dr. Bridges developed a structured transition program called the Bridge to Adult Care from Childhood for Young Adults with Rheumatic Disease (BACC YARD) aimed at improving the pediatric transition period. The analysis he presented focused specifically on reducing loss to follow-up by introducing a pretransfer visit with both rheumatologists. The patient first meets with their pediatric rheumatologist.
During that visit, the adult rheumatologist attends and discusses the patient’s history and current therapy with the pediatric rheumatologist before entering the patient’s room and having “a brief introductory conversation, a sort of verbal handoff and handshake, in front of the patient,” Dr. Bridges explained. “Then I assume responsibility for this patient and their next visit is to see me, both proverbially and literally down the street at the adulthood rheumatology clinic, where this patient becomes a part of my continuity cohort.”
Bridges entered patients from this BACC YARD cohort into an observational registry that included their dual provider pretransfer visit and a posttransfer visit, occurring between July 2020 and May 2022. He compared these patients with a historical control cohort of 45 patients from March 2018 to March 2020, who had at least two pediatric rheumatology visits prior to their transfer to adult care and no documentation of outside rheumatology visits during the study period. Specifically, he examined at the requested and actual interval between patients’ final pediatric rheumatology visit and their first adult rheumatology visit.
The intervention cohort included 86 patients, mostly female (73%), with a median age of 20. About two-thirds were White (65%) and one-third (34%) were Black. One patient was Asian, and 7% were Hispanic. Just over half the patients had juvenile idiopathic arthritis (58%), and 30% had lupus and related connective tissue diseases. The other patients had vasculitis, uveitis, inflammatory myopathy, relapsing polychondritis, morphea, or syndrome of undifferentiated recurrent fever.
A total of 8% of these patients had previously been lost to follow-up at Children’s of Alabama before they re-established rheumatology care at UAB, and 3.5% came from a pediatric rheumatologist from somewhere other than Children’s of Alabama but established adult care at UAB through the BACC YARD program. Among the remaining patients, 65% (n = 56) had both a dual provider pretransfer visit and a posttransfer visit.
The BACC YARD patients requested their next rheumatology visit (the first adult one) a median 119 days after their last pediatric visit, and the actual time until that visit was a median 141 days (P < .05). By comparison, the 45 patients in the historical control group had a median 261 days between their last pediatric visit and their first adult visit (P < .001). The median days between visits was shorter for those with JIA (129 days) and lupus (119 days) than for patients with other conditions (149 days).
Bridges acknowledged that the study was limited by the small size of the cohort and potential contextual factors related to individual patients’ circumstances.
“We’re continuing to make iterative changes to this process to try to continue to improve the transition and its outcomes in this cohort,” Dr. Bridges said.
Aimee Hersh, MD, an associate professor of pediatric rheumatology and division chief of pediatric rheumatology at the University of Utah and Primary Children’s Hospital, both in Salt Lake City, attended the presentation and noted that the University of Utah has a very similar transfer program.
“I think one of the challenges of that model, and our model, is that you have to have a very specific type of physician who is both [medical-pediatrics] trained and has a specific interest in transition,” Dr. Hersh said in an interview. She noted that the adult rheumatologist at her institution didn’t train in pediatric rheumatology but did complete a meds-peds residency. “So if you can find an adult rheumatologist who can do something similar, can see older adolescent patients and serve as that transition bridge, then I think it is feasible.”
For practices that don’t have the resources for this kind of program, Dr. Hersh recommended the Got Transition program, which provides transition guidance that can be applied to any adolescent population with chronic illness.
The other study, led by Kristiana Nasto, BS, a third-year medical student at Baylor College of Medicine, reported on the findings from one aspect of a program also developed to improve the transition from pediatric to adult care for rheumatology patients. It included periodic self-reported evaluation using the validated Adolescent Assessment of Preparation for Transition (ADAPT) survey. As the first step to better understanding the factors that can predict successful transition, the researchers surveyed returning patients with any rheumatologic diagnosis, aged 14 years and older, between July 2021 and November 2022.
Since the survey was automated through the electronic medical record, patients and their caregivers could respond during in-person or virtual visit check-in. The researchers calculated three composite scores out of 100 for self-management, prescription management, and transfer planning, using responses from the ADAPT survey. Among 462 patients who returned 670 surveys, 87% provided surveys that could be scored for at least one composite score. Most respondents were female (75%), White (69%), non-Hispanic (64%), English speaking (90%), and aged 14-17 years (83%).
The overall average score for self-management from 401 respondents was 35. For prescription management, the average score was 59 from 288 respondents, and the average transfer planning score was 17 from 367 respondents. Self-management and transfer planning scores both improved with age (P = .0001). Self-management scores rose from an average of 20 at age 14 to an average of 64 at age 18 and older. Transfer planning scores increased from an average of 1 at age 14 to an average of 49 at age 18 and older. Prescription management scores remained high across all ages, from an average of 59 at age 14 to an average score of 66 at age 18 and older (P = .044). Although the scores did not statistically vary by age or race, Hispanic patients did score higher in self-management with an average of 44.5, compared with 31 among other patients (P = .0001).
Only 21% of patients completed two surveys, and 8.4% completed all three surveys. The average time between the first and second surveys was 4 months, during which there was no statistically significant change in self-management or prescription management scores, but transfer planning scores did increase from 14 to 21 (P = .008) among the 90 patients who completed those surveys.
The researchers concluded from their analysis that “participation in the transition pathway can rapidly improve transfer planning scores, [but] opportunities remain to improve readiness in all domains.” The researchers are in the process of developing Spanish-language surveys.
No external funding was noted for either study. Dr. Bridges, Dr. Hersh, and Ms. Nasto reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Implementing a pediatric transition program in which a patient meets with both their pediatric and soon-to-be adult rheumatologist during a visit before formal transition resulted in less time setting up the first adult visit, according to research presented at the Pediatric Rheumatology Symposium.
The presentation was one of two that focused on ways to improve the transition from pediatric to adult care for rheumatology patients. The other, a poster from researchers at Baylor College of Medicine, Houston, took the first steps toward learning what factors can help predict a successful transition.
“This period of transitioning from pediatric to adult care, both rheumatology specific and otherwise, is a high-risk time,” John M. Bridges, MD, a fourth-year pediatric rheumatology fellow at the University of Alabama at Birmingham, told attendees. “There are changes in insurance coverage, employment, geographic mobility, and shifting responsibilities between parents and children in the setting of a still-developing frontal lobe that contribute to the risk of this period. Risks include disease flare, and then organ damage, as well as issues with decreasing medication and therapy, adherence, unscheduled care utilization, and increasing loss to follow-up.”
Dr. Bridges developed a structured transition program called the Bridge to Adult Care from Childhood for Young Adults with Rheumatic Disease (BACC YARD) aimed at improving the pediatric transition period. The analysis he presented focused specifically on reducing loss to follow-up by introducing a pretransfer visit with both rheumatologists. The patient first meets with their pediatric rheumatologist.
During that visit, the adult rheumatologist attends and discusses the patient’s history and current therapy with the pediatric rheumatologist before entering the patient’s room and having “a brief introductory conversation, a sort of verbal handoff and handshake, in front of the patient,” Dr. Bridges explained. “Then I assume responsibility for this patient and their next visit is to see me, both proverbially and literally down the street at the adulthood rheumatology clinic, where this patient becomes a part of my continuity cohort.”
Bridges entered patients from this BACC YARD cohort into an observational registry that included their dual provider pretransfer visit and a posttransfer visit, occurring between July 2020 and May 2022. He compared these patients with a historical control cohort of 45 patients from March 2018 to March 2020, who had at least two pediatric rheumatology visits prior to their transfer to adult care and no documentation of outside rheumatology visits during the study period. Specifically, he examined at the requested and actual interval between patients’ final pediatric rheumatology visit and their first adult rheumatology visit.
The intervention cohort included 86 patients, mostly female (73%), with a median age of 20. About two-thirds were White (65%) and one-third (34%) were Black. One patient was Asian, and 7% were Hispanic. Just over half the patients had juvenile idiopathic arthritis (58%), and 30% had lupus and related connective tissue diseases. The other patients had vasculitis, uveitis, inflammatory myopathy, relapsing polychondritis, morphea, or syndrome of undifferentiated recurrent fever.
A total of 8% of these patients had previously been lost to follow-up at Children’s of Alabama before they re-established rheumatology care at UAB, and 3.5% came from a pediatric rheumatologist from somewhere other than Children’s of Alabama but established adult care at UAB through the BACC YARD program. Among the remaining patients, 65% (n = 56) had both a dual provider pretransfer visit and a posttransfer visit.
The BACC YARD patients requested their next rheumatology visit (the first adult one) a median 119 days after their last pediatric visit, and the actual time until that visit was a median 141 days (P < .05). By comparison, the 45 patients in the historical control group had a median 261 days between their last pediatric visit and their first adult visit (P < .001). The median days between visits was shorter for those with JIA (129 days) and lupus (119 days) than for patients with other conditions (149 days).
Bridges acknowledged that the study was limited by the small size of the cohort and potential contextual factors related to individual patients’ circumstances.
“We’re continuing to make iterative changes to this process to try to continue to improve the transition and its outcomes in this cohort,” Dr. Bridges said.
Aimee Hersh, MD, an associate professor of pediatric rheumatology and division chief of pediatric rheumatology at the University of Utah and Primary Children’s Hospital, both in Salt Lake City, attended the presentation and noted that the University of Utah has a very similar transfer program.
“I think one of the challenges of that model, and our model, is that you have to have a very specific type of physician who is both [medical-pediatrics] trained and has a specific interest in transition,” Dr. Hersh said in an interview. She noted that the adult rheumatologist at her institution didn’t train in pediatric rheumatology but did complete a meds-peds residency. “So if you can find an adult rheumatologist who can do something similar, can see older adolescent patients and serve as that transition bridge, then I think it is feasible.”
For practices that don’t have the resources for this kind of program, Dr. Hersh recommended the Got Transition program, which provides transition guidance that can be applied to any adolescent population with chronic illness.
The other study, led by Kristiana Nasto, BS, a third-year medical student at Baylor College of Medicine, reported on the findings from one aspect of a program also developed to improve the transition from pediatric to adult care for rheumatology patients. It included periodic self-reported evaluation using the validated Adolescent Assessment of Preparation for Transition (ADAPT) survey. As the first step to better understanding the factors that can predict successful transition, the researchers surveyed returning patients with any rheumatologic diagnosis, aged 14 years and older, between July 2021 and November 2022.
Since the survey was automated through the electronic medical record, patients and their caregivers could respond during in-person or virtual visit check-in. The researchers calculated three composite scores out of 100 for self-management, prescription management, and transfer planning, using responses from the ADAPT survey. Among 462 patients who returned 670 surveys, 87% provided surveys that could be scored for at least one composite score. Most respondents were female (75%), White (69%), non-Hispanic (64%), English speaking (90%), and aged 14-17 years (83%).
The overall average score for self-management from 401 respondents was 35. For prescription management, the average score was 59 from 288 respondents, and the average transfer planning score was 17 from 367 respondents. Self-management and transfer planning scores both improved with age (P = .0001). Self-management scores rose from an average of 20 at age 14 to an average of 64 at age 18 and older. Transfer planning scores increased from an average of 1 at age 14 to an average of 49 at age 18 and older. Prescription management scores remained high across all ages, from an average of 59 at age 14 to an average score of 66 at age 18 and older (P = .044). Although the scores did not statistically vary by age or race, Hispanic patients did score higher in self-management with an average of 44.5, compared with 31 among other patients (P = .0001).
Only 21% of patients completed two surveys, and 8.4% completed all three surveys. The average time between the first and second surveys was 4 months, during which there was no statistically significant change in self-management or prescription management scores, but transfer planning scores did increase from 14 to 21 (P = .008) among the 90 patients who completed those surveys.
The researchers concluded from their analysis that “participation in the transition pathway can rapidly improve transfer planning scores, [but] opportunities remain to improve readiness in all domains.” The researchers are in the process of developing Spanish-language surveys.
No external funding was noted for either study. Dr. Bridges, Dr. Hersh, and Ms. Nasto reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Implementing a pediatric transition program in which a patient meets with both their pediatric and soon-to-be adult rheumatologist during a visit before formal transition resulted in less time setting up the first adult visit, according to research presented at the Pediatric Rheumatology Symposium.
The presentation was one of two that focused on ways to improve the transition from pediatric to adult care for rheumatology patients. The other, a poster from researchers at Baylor College of Medicine, Houston, took the first steps toward learning what factors can help predict a successful transition.
“This period of transitioning from pediatric to adult care, both rheumatology specific and otherwise, is a high-risk time,” John M. Bridges, MD, a fourth-year pediatric rheumatology fellow at the University of Alabama at Birmingham, told attendees. “There are changes in insurance coverage, employment, geographic mobility, and shifting responsibilities between parents and children in the setting of a still-developing frontal lobe that contribute to the risk of this period. Risks include disease flare, and then organ damage, as well as issues with decreasing medication and therapy, adherence, unscheduled care utilization, and increasing loss to follow-up.”
Dr. Bridges developed a structured transition program called the Bridge to Adult Care from Childhood for Young Adults with Rheumatic Disease (BACC YARD) aimed at improving the pediatric transition period. The analysis he presented focused specifically on reducing loss to follow-up by introducing a pretransfer visit with both rheumatologists. The patient first meets with their pediatric rheumatologist.
During that visit, the adult rheumatologist attends and discusses the patient’s history and current therapy with the pediatric rheumatologist before entering the patient’s room and having “a brief introductory conversation, a sort of verbal handoff and handshake, in front of the patient,” Dr. Bridges explained. “Then I assume responsibility for this patient and their next visit is to see me, both proverbially and literally down the street at the adulthood rheumatology clinic, where this patient becomes a part of my continuity cohort.”
Bridges entered patients from this BACC YARD cohort into an observational registry that included their dual provider pretransfer visit and a posttransfer visit, occurring between July 2020 and May 2022. He compared these patients with a historical control cohort of 45 patients from March 2018 to March 2020, who had at least two pediatric rheumatology visits prior to their transfer to adult care and no documentation of outside rheumatology visits during the study period. Specifically, he examined at the requested and actual interval between patients’ final pediatric rheumatology visit and their first adult rheumatology visit.
The intervention cohort included 86 patients, mostly female (73%), with a median age of 20. About two-thirds were White (65%) and one-third (34%) were Black. One patient was Asian, and 7% were Hispanic. Just over half the patients had juvenile idiopathic arthritis (58%), and 30% had lupus and related connective tissue diseases. The other patients had vasculitis, uveitis, inflammatory myopathy, relapsing polychondritis, morphea, or syndrome of undifferentiated recurrent fever.
A total of 8% of these patients had previously been lost to follow-up at Children’s of Alabama before they re-established rheumatology care at UAB, and 3.5% came from a pediatric rheumatologist from somewhere other than Children’s of Alabama but established adult care at UAB through the BACC YARD program. Among the remaining patients, 65% (n = 56) had both a dual provider pretransfer visit and a posttransfer visit.
The BACC YARD patients requested their next rheumatology visit (the first adult one) a median 119 days after their last pediatric visit, and the actual time until that visit was a median 141 days (P < .05). By comparison, the 45 patients in the historical control group had a median 261 days between their last pediatric visit and their first adult visit (P < .001). The median days between visits was shorter for those with JIA (129 days) and lupus (119 days) than for patients with other conditions (149 days).
Bridges acknowledged that the study was limited by the small size of the cohort and potential contextual factors related to individual patients’ circumstances.
“We’re continuing to make iterative changes to this process to try to continue to improve the transition and its outcomes in this cohort,” Dr. Bridges said.
Aimee Hersh, MD, an associate professor of pediatric rheumatology and division chief of pediatric rheumatology at the University of Utah and Primary Children’s Hospital, both in Salt Lake City, attended the presentation and noted that the University of Utah has a very similar transfer program.
“I think one of the challenges of that model, and our model, is that you have to have a very specific type of physician who is both [medical-pediatrics] trained and has a specific interest in transition,” Dr. Hersh said in an interview. She noted that the adult rheumatologist at her institution didn’t train in pediatric rheumatology but did complete a meds-peds residency. “So if you can find an adult rheumatologist who can do something similar, can see older adolescent patients and serve as that transition bridge, then I think it is feasible.”
For practices that don’t have the resources for this kind of program, Dr. Hersh recommended the Got Transition program, which provides transition guidance that can be applied to any adolescent population with chronic illness.
The other study, led by Kristiana Nasto, BS, a third-year medical student at Baylor College of Medicine, reported on the findings from one aspect of a program also developed to improve the transition from pediatric to adult care for rheumatology patients. It included periodic self-reported evaluation using the validated Adolescent Assessment of Preparation for Transition (ADAPT) survey. As the first step to better understanding the factors that can predict successful transition, the researchers surveyed returning patients with any rheumatologic diagnosis, aged 14 years and older, between July 2021 and November 2022.
Since the survey was automated through the electronic medical record, patients and their caregivers could respond during in-person or virtual visit check-in. The researchers calculated three composite scores out of 100 for self-management, prescription management, and transfer planning, using responses from the ADAPT survey. Among 462 patients who returned 670 surveys, 87% provided surveys that could be scored for at least one composite score. Most respondents were female (75%), White (69%), non-Hispanic (64%), English speaking (90%), and aged 14-17 years (83%).
The overall average score for self-management from 401 respondents was 35. For prescription management, the average score was 59 from 288 respondents, and the average transfer planning score was 17 from 367 respondents. Self-management and transfer planning scores both improved with age (P = .0001). Self-management scores rose from an average of 20 at age 14 to an average of 64 at age 18 and older. Transfer planning scores increased from an average of 1 at age 14 to an average of 49 at age 18 and older. Prescription management scores remained high across all ages, from an average of 59 at age 14 to an average score of 66 at age 18 and older (P = .044). Although the scores did not statistically vary by age or race, Hispanic patients did score higher in self-management with an average of 44.5, compared with 31 among other patients (P = .0001).
Only 21% of patients completed two surveys, and 8.4% completed all three surveys. The average time between the first and second surveys was 4 months, during which there was no statistically significant change in self-management or prescription management scores, but transfer planning scores did increase from 14 to 21 (P = .008) among the 90 patients who completed those surveys.
The researchers concluded from their analysis that “participation in the transition pathway can rapidly improve transfer planning scores, [but] opportunities remain to improve readiness in all domains.” The researchers are in the process of developing Spanish-language surveys.
No external funding was noted for either study. Dr. Bridges, Dr. Hersh, and Ms. Nasto reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT PRSYM 2023
Autism: Is it in the water?
This transcript has been edited for clarity.
Few diseases have stymied explanation like autism spectrum disorder (ASD). We know that the prevalence has been increasing dramatically, but we aren’t quite sure whether that is because of more screening and awareness or more fundamental changes. We know that much of the risk appears to be genetic, but there may be 1,000 genes involved in the syndrome. We know that certain environmental exposures, like pollution, might increase the risk – perhaps on a susceptible genetic background – but we’re not really sure which exposures are most harmful.
So, the search continues, across all domains of inquiry from cell culture to large epidemiologic analyses. And this week, a new player enters the field, and, as they say, it’s something in the water.
We’re talking about this paper, by Zeyan Liew and colleagues, appearing in JAMA Pediatrics.
Using the incredibly robust health data infrastructure in Denmark, the researchers were able to identify 8,842 children born between 2000 and 2013 with ASD and matched each one to five control kids of the same sex and age without autism.
They then mapped the location the mothers of these kids lived while they were pregnant – down to 5 meters resolution, actually – to groundwater lithium levels.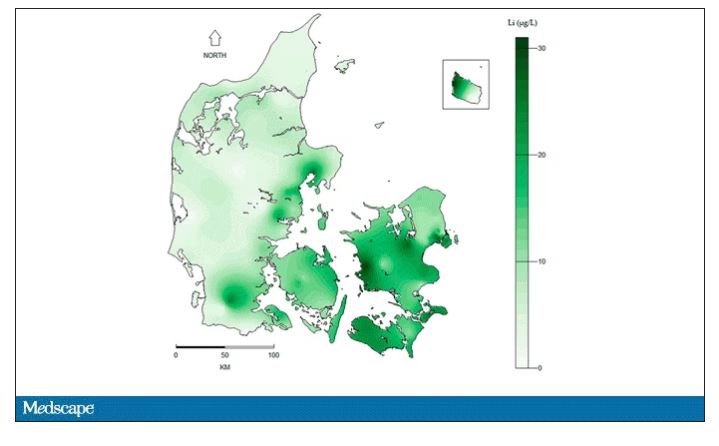
Once that was done, the analysis was straightforward. Would moms who were pregnant in areas with higher groundwater lithium levels be more likely to have kids with ASD?
The results show a rather steady and consistent association between higher lithium levels in groundwater and the prevalence of ASD in children.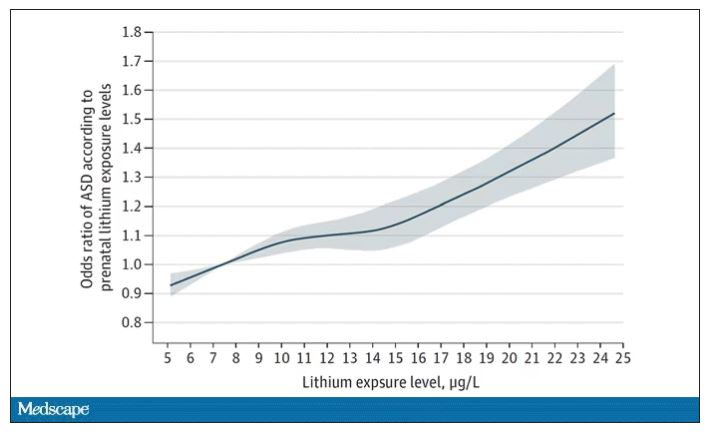
We’re not talking huge numbers, but moms who lived in the areas of the highest quartile of lithium were about 46% more likely to have a child with ASD. That’s a relative risk, of course – this would be like an increase from 1 in 100 kids to 1.5 in 100 kids. But still, it’s intriguing.
But the case is far from closed here.
Groundwater concentration of lithium and the amount of lithium a pregnant mother ingests are not the same thing. It does turn out that virtually all drinking water in Denmark comes from groundwater sources – but not all lithium comes from drinking water. There are plenty of dietary sources of lithium as well. And, of course, there is medical lithium, but we’ll get to that in a second.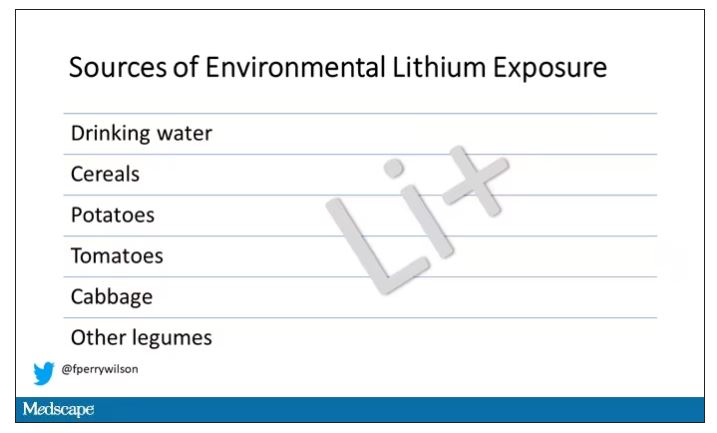
First, let’s talk about those lithium measurements. They were taken in 2013 – after all these kids were born. The authors acknowledge this limitation but show a high correlation between measured levels in 2013 and earlier measured levels from prior studies, suggesting that lithium levels in a given area are quite constant over time. That’s great – but if lithium levels are constant over time, this study does nothing to shed light on why autism diagnoses seem to be increasing.
Let’s put some numbers to the lithium concentrations the authors examined. The average was about 12 mcg/L.
As a reminder, a standard therapeutic dose of lithium used for bipolar disorder is like 600 mg. That means you’d need to drink more than 2,500 of those 5-gallon jugs that sit on your water cooler, per day, to approximate the dose you’d get from a lithium tablet. Of course, small doses can still cause toxicity – but I wanted to put this in perspective.
Also, we have some data on pregnant women who take medical lithium. An analysis of nine studies showed that first-trimester lithium use may be associated with congenital malformations – particularly some specific heart malformations – and some birth complications. But three of four separate studies looking at longer-term neurodevelopmental outcomes did not find any effect on development, attainment of milestones, or IQ. One study of 15 kids exposed to medical lithium in utero did note minor neurologic dysfunction in one child and a low verbal IQ in another – but that’s a very small study.
Of course, lithium levels vary around the world as well. The U.S. Geological Survey examined lithium content in groundwater in the United States, as you can see here.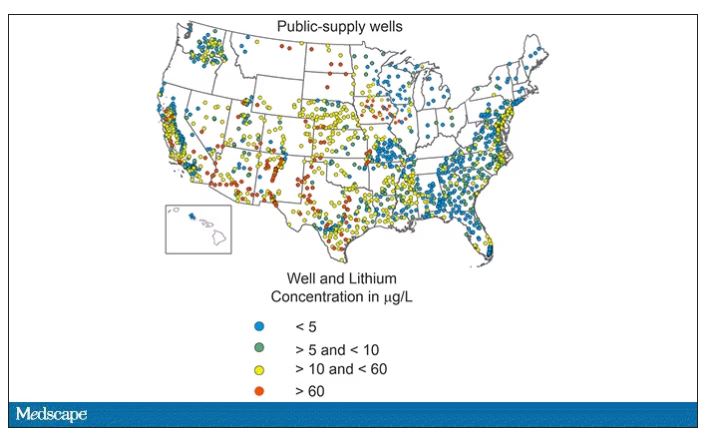
Our numbers are pretty similar to Denmark’s – in the 0-60 range. But an area in the Argentine Andes has levels as high as 1,600 mcg/L. A study of 194 babies from that area found higher lithium exposure was associated with lower fetal size, but I haven’t seen follow-up on neurodevelopmental outcomes.
The point is that there is a lot of variability here. It would be really interesting to map groundwater lithium levels to autism rates around the world. As a teaser, I will point out that, if you look at worldwide autism rates, you may be able to convince yourself that they are higher in more arid climates, and arid climates tend to have more groundwater lithium. But I’m really reaching here. More work needs to be done.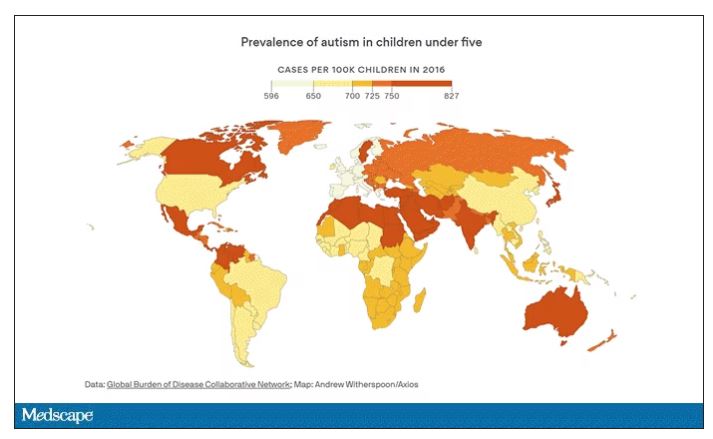
And I hope it is done quickly. Lithium is in the midst of becoming a very important commodity thanks to the shift to electric vehicles. While we can hope that recycling will claim most of those batteries at the end of their life, some will escape reclamation and potentially put more lithium into the drinking water. I’d like to know how risky that is before it happens.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. He has disclosed no relevant financial relationships. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and his new book, “How Medicine Works and When It Doesn’t”, is available now.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Few diseases have stymied explanation like autism spectrum disorder (ASD). We know that the prevalence has been increasing dramatically, but we aren’t quite sure whether that is because of more screening and awareness or more fundamental changes. We know that much of the risk appears to be genetic, but there may be 1,000 genes involved in the syndrome. We know that certain environmental exposures, like pollution, might increase the risk – perhaps on a susceptible genetic background – but we’re not really sure which exposures are most harmful.
So, the search continues, across all domains of inquiry from cell culture to large epidemiologic analyses. And this week, a new player enters the field, and, as they say, it’s something in the water.
We’re talking about this paper, by Zeyan Liew and colleagues, appearing in JAMA Pediatrics.
Using the incredibly robust health data infrastructure in Denmark, the researchers were able to identify 8,842 children born between 2000 and 2013 with ASD and matched each one to five control kids of the same sex and age without autism.
They then mapped the location the mothers of these kids lived while they were pregnant – down to 5 meters resolution, actually – to groundwater lithium levels.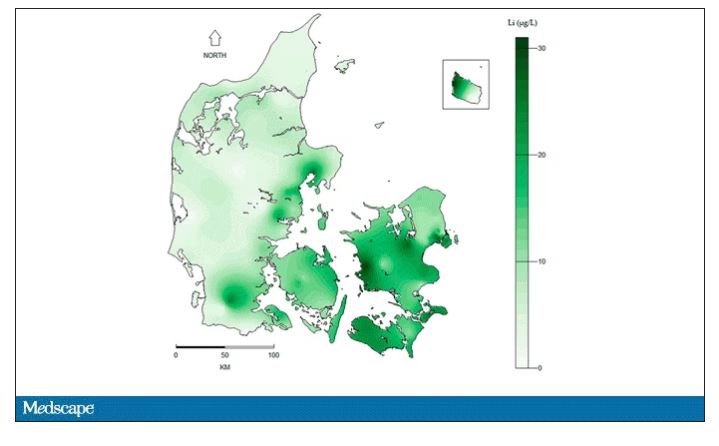
Once that was done, the analysis was straightforward. Would moms who were pregnant in areas with higher groundwater lithium levels be more likely to have kids with ASD?
The results show a rather steady and consistent association between higher lithium levels in groundwater and the prevalence of ASD in children.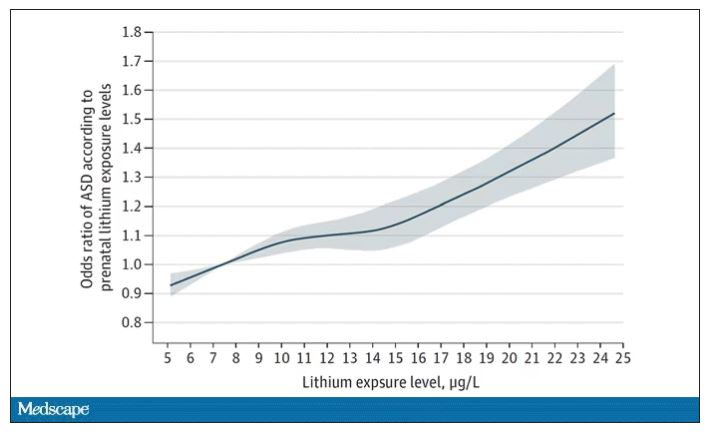
We’re not talking huge numbers, but moms who lived in the areas of the highest quartile of lithium were about 46% more likely to have a child with ASD. That’s a relative risk, of course – this would be like an increase from 1 in 100 kids to 1.5 in 100 kids. But still, it’s intriguing.
But the case is far from closed here.
Groundwater concentration of lithium and the amount of lithium a pregnant mother ingests are not the same thing. It does turn out that virtually all drinking water in Denmark comes from groundwater sources – but not all lithium comes from drinking water. There are plenty of dietary sources of lithium as well. And, of course, there is medical lithium, but we’ll get to that in a second.
First, let’s talk about those lithium measurements. They were taken in 2013 – after all these kids were born. The authors acknowledge this limitation but show a high correlation between measured levels in 2013 and earlier measured levels from prior studies, suggesting that lithium levels in a given area are quite constant over time. That’s great – but if lithium levels are constant over time, this study does nothing to shed light on why autism diagnoses seem to be increasing.
Let’s put some numbers to the lithium concentrations the authors examined. The average was about 12 mcg/L.
As a reminder, a standard therapeutic dose of lithium used for bipolar disorder is like 600 mg. That means you’d need to drink more than 2,500 of those 5-gallon jugs that sit on your water cooler, per day, to approximate the dose you’d get from a lithium tablet. Of course, small doses can still cause toxicity – but I wanted to put this in perspective.
Also, we have some data on pregnant women who take medical lithium. An analysis of nine studies showed that first-trimester lithium use may be associated with congenital malformations – particularly some specific heart malformations – and some birth complications. But three of four separate studies looking at longer-term neurodevelopmental outcomes did not find any effect on development, attainment of milestones, or IQ. One study of 15 kids exposed to medical lithium in utero did note minor neurologic dysfunction in one child and a low verbal IQ in another – but that’s a very small study.
Of course, lithium levels vary around the world as well. The U.S. Geological Survey examined lithium content in groundwater in the United States, as you can see here.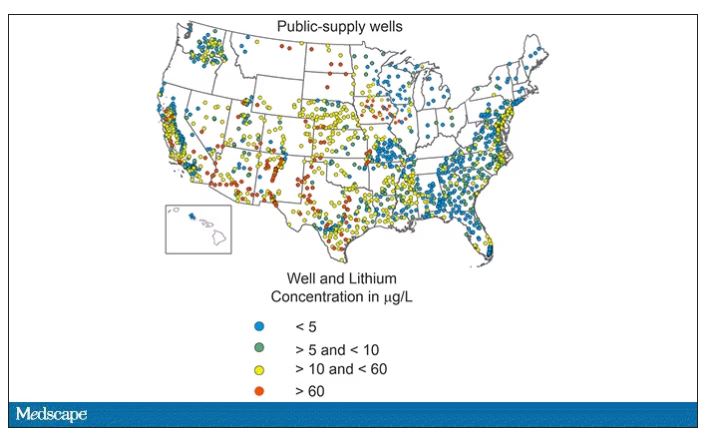
Our numbers are pretty similar to Denmark’s – in the 0-60 range. But an area in the Argentine Andes has levels as high as 1,600 mcg/L. A study of 194 babies from that area found higher lithium exposure was associated with lower fetal size, but I haven’t seen follow-up on neurodevelopmental outcomes.
The point is that there is a lot of variability here. It would be really interesting to map groundwater lithium levels to autism rates around the world. As a teaser, I will point out that, if you look at worldwide autism rates, you may be able to convince yourself that they are higher in more arid climates, and arid climates tend to have more groundwater lithium. But I’m really reaching here. More work needs to be done.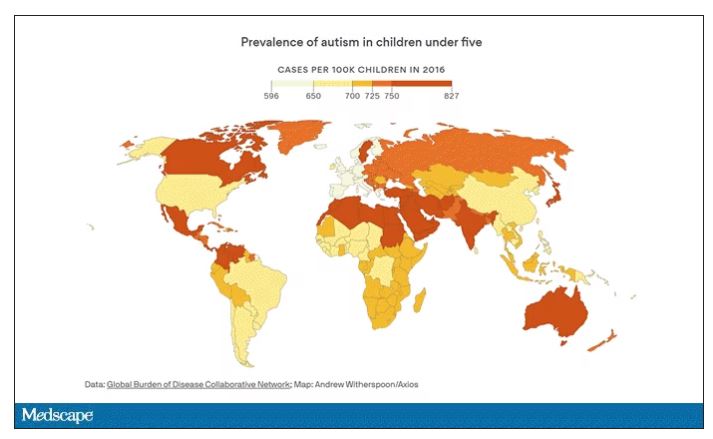
And I hope it is done quickly. Lithium is in the midst of becoming a very important commodity thanks to the shift to electric vehicles. While we can hope that recycling will claim most of those batteries at the end of their life, some will escape reclamation and potentially put more lithium into the drinking water. I’d like to know how risky that is before it happens.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. He has disclosed no relevant financial relationships. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and his new book, “How Medicine Works and When It Doesn’t”, is available now.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Few diseases have stymied explanation like autism spectrum disorder (ASD). We know that the prevalence has been increasing dramatically, but we aren’t quite sure whether that is because of more screening and awareness or more fundamental changes. We know that much of the risk appears to be genetic, but there may be 1,000 genes involved in the syndrome. We know that certain environmental exposures, like pollution, might increase the risk – perhaps on a susceptible genetic background – but we’re not really sure which exposures are most harmful.
So, the search continues, across all domains of inquiry from cell culture to large epidemiologic analyses. And this week, a new player enters the field, and, as they say, it’s something in the water.
We’re talking about this paper, by Zeyan Liew and colleagues, appearing in JAMA Pediatrics.
Using the incredibly robust health data infrastructure in Denmark, the researchers were able to identify 8,842 children born between 2000 and 2013 with ASD and matched each one to five control kids of the same sex and age without autism.
They then mapped the location the mothers of these kids lived while they were pregnant – down to 5 meters resolution, actually – to groundwater lithium levels.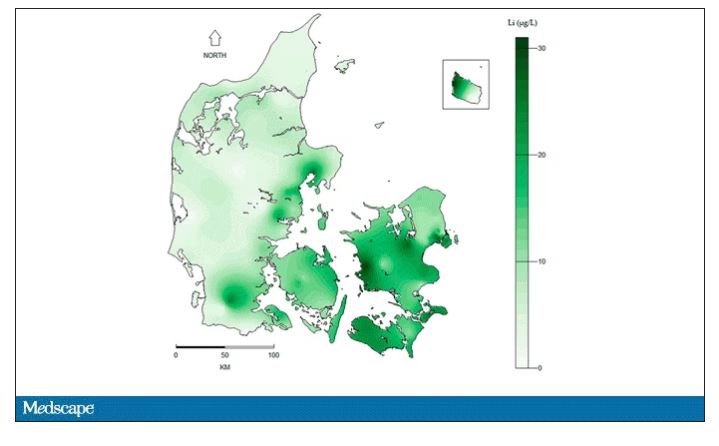
Once that was done, the analysis was straightforward. Would moms who were pregnant in areas with higher groundwater lithium levels be more likely to have kids with ASD?
The results show a rather steady and consistent association between higher lithium levels in groundwater and the prevalence of ASD in children.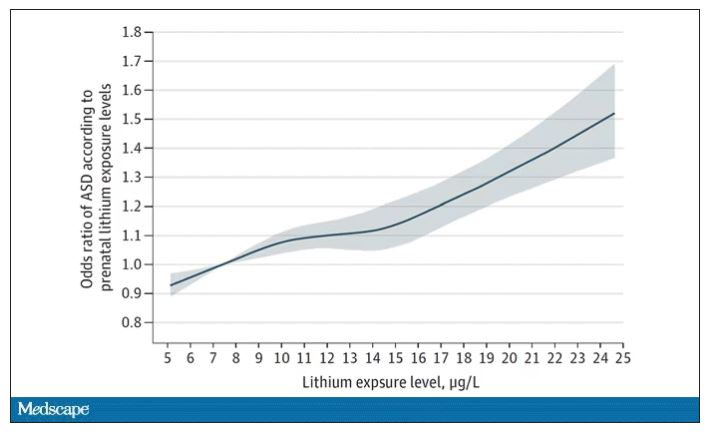
We’re not talking huge numbers, but moms who lived in the areas of the highest quartile of lithium were about 46% more likely to have a child with ASD. That’s a relative risk, of course – this would be like an increase from 1 in 100 kids to 1.5 in 100 kids. But still, it’s intriguing.
But the case is far from closed here.
Groundwater concentration of lithium and the amount of lithium a pregnant mother ingests are not the same thing. It does turn out that virtually all drinking water in Denmark comes from groundwater sources – but not all lithium comes from drinking water. There are plenty of dietary sources of lithium as well. And, of course, there is medical lithium, but we’ll get to that in a second.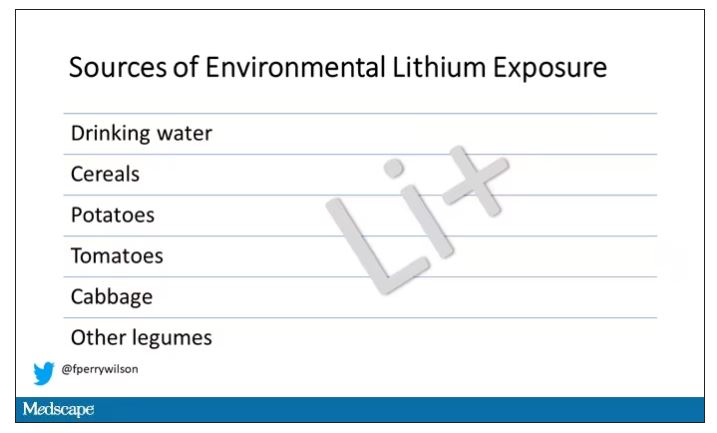
First, let’s talk about those lithium measurements. They were taken in 2013 – after all these kids were born. The authors acknowledge this limitation but show a high correlation between measured levels in 2013 and earlier measured levels from prior studies, suggesting that lithium levels in a given area are quite constant over time. That’s great – but if lithium levels are constant over time, this study does nothing to shed light on why autism diagnoses seem to be increasing.
Let’s put some numbers to the lithium concentrations the authors examined. The average was about 12 mcg/L.
As a reminder, a standard therapeutic dose of lithium used for bipolar disorder is like 600 mg. That means you’d need to drink more than 2,500 of those 5-gallon jugs that sit on your water cooler, per day, to approximate the dose you’d get from a lithium tablet. Of course, small doses can still cause toxicity – but I wanted to put this in perspective.
Also, we have some data on pregnant women who take medical lithium. An analysis of nine studies showed that first-trimester lithium use may be associated with congenital malformations – particularly some specific heart malformations – and some birth complications. But three of four separate studies looking at longer-term neurodevelopmental outcomes did not find any effect on development, attainment of milestones, or IQ. One study of 15 kids exposed to medical lithium in utero did note minor neurologic dysfunction in one child and a low verbal IQ in another – but that’s a very small study.
Of course, lithium levels vary around the world as well. The U.S. Geological Survey examined lithium content in groundwater in the United States, as you can see here.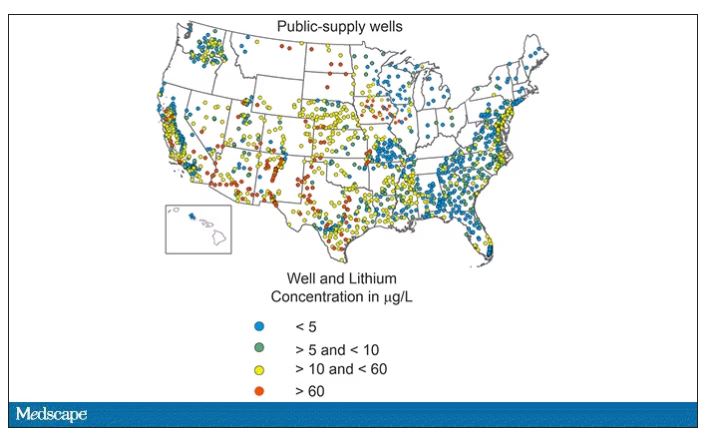
Our numbers are pretty similar to Denmark’s – in the 0-60 range. But an area in the Argentine Andes has levels as high as 1,600 mcg/L. A study of 194 babies from that area found higher lithium exposure was associated with lower fetal size, but I haven’t seen follow-up on neurodevelopmental outcomes.
The point is that there is a lot of variability here. It would be really interesting to map groundwater lithium levels to autism rates around the world. As a teaser, I will point out that, if you look at worldwide autism rates, you may be able to convince yourself that they are higher in more arid climates, and arid climates tend to have more groundwater lithium. But I’m really reaching here. More work needs to be done.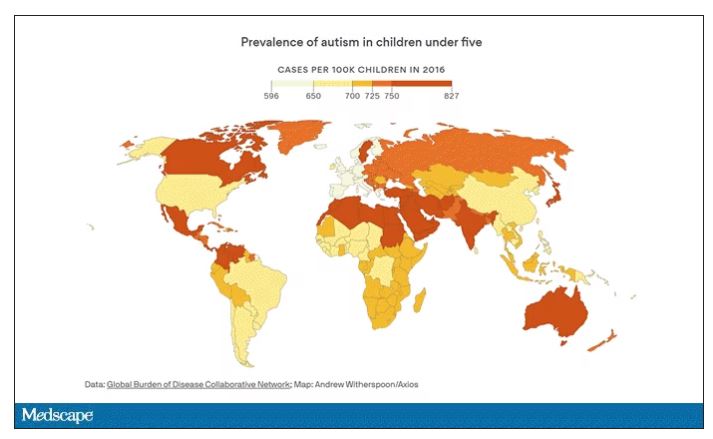
And I hope it is done quickly. Lithium is in the midst of becoming a very important commodity thanks to the shift to electric vehicles. While we can hope that recycling will claim most of those batteries at the end of their life, some will escape reclamation and potentially put more lithium into the drinking water. I’d like to know how risky that is before it happens.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. He has disclosed no relevant financial relationships. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and his new book, “How Medicine Works and When It Doesn’t”, is available now.
A version of this article originally appeared on Medscape.com.
Children ate more fruits and vegetables during longer meals: Study
Adding 10 minutes to family mealtimes increased children’s consumption of fruits and vegetables by approximately one portion, based on data from 50 parent-child dyads.
Family meals are known to affect children’s food choices and preferences and can be an effective setting for improving children’s nutrition, wrote Mattea Dallacker, PhD, of the University of Mannheim, Germany, and colleagues.
However, the effect of extending meal duration on increasing fruit and vegetable intake in particular has not been examined, they said.
In a study published in JAMA Network Open, the researchers provided two free evening meals to 50 parent-child dyads under each of two different conditions. The control condition was defined by the families as a regular family mealtime duration (an average meal was 20.83 minutes), while the intervention was an average meal time 10 minutes (50%) longer. The age of the parents ranged from 22 to 55 years, with a mean of 43 years; 72% of the parent participants were mothers. The children’s ages ranged from 6 to 11 years, with a mean of 8 years, with approximately equal numbers of boys and girls.
The study was conducted in a family meal laboratory setting in Berlin, and groups were randomized to the longer or shorter meal setting first. The primary outcome was the total number of pieces of fruit and vegetables eaten by the child as part of each of the two meals.
Both meals were the “typical German evening meal of sliced bread, cold cuts of cheese and meat, and bite-sized pieces of fruits and vegetables,” followed by a dessert course of chocolate pudding or fruit yogurt and cookies, the researchers wrote. Beverages were water and one sugar-sweetened beverage; the specific foods and beverages were based on the child’s preferences, reported in an online preassessment, and the foods were consistent for the longer and shorter meals. All participants were asked not to eat for 2 hours prior to arriving for their meals at the laboratory.
During longer meals, children ate an average of seven additional bite-sized pieces of fruits and vegetables, which translates to approximately a full portion (defined as 100 g, such as a medium apple), the researchers wrote. The difference was significant compared with the shorter meals for fruits (P = .01) and vegetables (P < .001).
A piece of fruit was approximately 10 grams (6-10 g for grapes and tangerine segments; 10-14 g for cherry tomatoes; and 9-11 g for apple, banana, carrot, or cucumber). Other foods served with the meals included cheese, meats, butter, and sweet spreads.
Children also ate more slowly (defined as fewer bites per minute) during the longer meals, and they reported significantly greater satiety after the longer meals (P < .001 for both). The consumption of bread and cold cuts was similar for the two meal settings.
“Higher intake of fruits and vegetables during longer meals cannot be explained by longer exposure to food alone; otherwise, an increased intake of bread and cold cuts would have occurred,” the researchers wrote in their discussion. “One possible explanation is that the fruits and vegetables were cut into bite-sized pieces, making them convenient to eat.”
Further analysis showed that during the longer meals, more fruits and vegetables were consumed overall, but more vegetables were eaten from the start of the meal, while the additional fruit was eaten during the additional time at the end.
The findings were limited by several factors, primarily use of a laboratory setting that does not generalize to natural eating environments, the researchers noted. Other potential limitations included the effect of a video cameras on desirable behaviors and the limited ethnic and socioeconomic diversity of the study population, they said. The results were strengthened by the within-dyad study design that allowed for control of factors such as video observation, but more research is needed with more diverse groups and across longer time frames, the researchers said.
However, the results suggest that adding 10 minutes to a family mealtime can yield significant improvements in children’s diets, they said. They suggested strategies including playing music chosen by the child/children and setting rules that everyone must remain at the table for a certain length of time, with fruits and vegetables available on the table.
“If the effects of this simple, inexpensive, and low-threshold intervention prove stable over time, it could contribute to addressing a major public health problem,” the researchers concluded.
Findings intriguing, more data needed
The current study is important because food and vegetable intake in the majority of children falls below the recommended daily allowance, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
The key take-home message for clinicians is the continued need to stress the importance of family meals, said Dr. Kinsella. “Many children continue to be overbooked with activities, and it may be rare for many families to sit down together for a meal for any length of time.”
Don’t discount the potential effect of a longer school lunch on children’s fruit and vegetable consumption as well, she added. “Advocating for longer lunch time is important, as many kids report not being able to finish their lunch at school.”
The current study was limited by being conducted in a lab setting, which may have influenced children’s desire for different foods, “also they had fewer distractions, and were being offered favorite foods,” said Dr. Kinsella.
Looking ahead, “it would be interesting to see if this result carried over to nonpreferred fruits and veggies and made any difference for picky eaters,” she said.
The study received no outside funding. The open-access publication of the study (but not the study itself) was supported by the Max Planck Institute for Human Development Library Open Access Fund. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Adding 10 minutes to family mealtimes increased children’s consumption of fruits and vegetables by approximately one portion, based on data from 50 parent-child dyads.
Family meals are known to affect children’s food choices and preferences and can be an effective setting for improving children’s nutrition, wrote Mattea Dallacker, PhD, of the University of Mannheim, Germany, and colleagues.
However, the effect of extending meal duration on increasing fruit and vegetable intake in particular has not been examined, they said.
In a study published in JAMA Network Open, the researchers provided two free evening meals to 50 parent-child dyads under each of two different conditions. The control condition was defined by the families as a regular family mealtime duration (an average meal was 20.83 minutes), while the intervention was an average meal time 10 minutes (50%) longer. The age of the parents ranged from 22 to 55 years, with a mean of 43 years; 72% of the parent participants were mothers. The children’s ages ranged from 6 to 11 years, with a mean of 8 years, with approximately equal numbers of boys and girls.
The study was conducted in a family meal laboratory setting in Berlin, and groups were randomized to the longer or shorter meal setting first. The primary outcome was the total number of pieces of fruit and vegetables eaten by the child as part of each of the two meals.
Both meals were the “typical German evening meal of sliced bread, cold cuts of cheese and meat, and bite-sized pieces of fruits and vegetables,” followed by a dessert course of chocolate pudding or fruit yogurt and cookies, the researchers wrote. Beverages were water and one sugar-sweetened beverage; the specific foods and beverages were based on the child’s preferences, reported in an online preassessment, and the foods were consistent for the longer and shorter meals. All participants were asked not to eat for 2 hours prior to arriving for their meals at the laboratory.
During longer meals, children ate an average of seven additional bite-sized pieces of fruits and vegetables, which translates to approximately a full portion (defined as 100 g, such as a medium apple), the researchers wrote. The difference was significant compared with the shorter meals for fruits (P = .01) and vegetables (P < .001).
A piece of fruit was approximately 10 grams (6-10 g for grapes and tangerine segments; 10-14 g for cherry tomatoes; and 9-11 g for apple, banana, carrot, or cucumber). Other foods served with the meals included cheese, meats, butter, and sweet spreads.
Children also ate more slowly (defined as fewer bites per minute) during the longer meals, and they reported significantly greater satiety after the longer meals (P < .001 for both). The consumption of bread and cold cuts was similar for the two meal settings.
“Higher intake of fruits and vegetables during longer meals cannot be explained by longer exposure to food alone; otherwise, an increased intake of bread and cold cuts would have occurred,” the researchers wrote in their discussion. “One possible explanation is that the fruits and vegetables were cut into bite-sized pieces, making them convenient to eat.”
Further analysis showed that during the longer meals, more fruits and vegetables were consumed overall, but more vegetables were eaten from the start of the meal, while the additional fruit was eaten during the additional time at the end.
The findings were limited by several factors, primarily use of a laboratory setting that does not generalize to natural eating environments, the researchers noted. Other potential limitations included the effect of a video cameras on desirable behaviors and the limited ethnic and socioeconomic diversity of the study population, they said. The results were strengthened by the within-dyad study design that allowed for control of factors such as video observation, but more research is needed with more diverse groups and across longer time frames, the researchers said.
However, the results suggest that adding 10 minutes to a family mealtime can yield significant improvements in children’s diets, they said. They suggested strategies including playing music chosen by the child/children and setting rules that everyone must remain at the table for a certain length of time, with fruits and vegetables available on the table.
“If the effects of this simple, inexpensive, and low-threshold intervention prove stable over time, it could contribute to addressing a major public health problem,” the researchers concluded.
Findings intriguing, more data needed
The current study is important because food and vegetable intake in the majority of children falls below the recommended daily allowance, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
The key take-home message for clinicians is the continued need to stress the importance of family meals, said Dr. Kinsella. “Many children continue to be overbooked with activities, and it may be rare for many families to sit down together for a meal for any length of time.”
Don’t discount the potential effect of a longer school lunch on children’s fruit and vegetable consumption as well, she added. “Advocating for longer lunch time is important, as many kids report not being able to finish their lunch at school.”
The current study was limited by being conducted in a lab setting, which may have influenced children’s desire for different foods, “also they had fewer distractions, and were being offered favorite foods,” said Dr. Kinsella.
Looking ahead, “it would be interesting to see if this result carried over to nonpreferred fruits and veggies and made any difference for picky eaters,” she said.
The study received no outside funding. The open-access publication of the study (but not the study itself) was supported by the Max Planck Institute for Human Development Library Open Access Fund. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Adding 10 minutes to family mealtimes increased children’s consumption of fruits and vegetables by approximately one portion, based on data from 50 parent-child dyads.
Family meals are known to affect children’s food choices and preferences and can be an effective setting for improving children’s nutrition, wrote Mattea Dallacker, PhD, of the University of Mannheim, Germany, and colleagues.
However, the effect of extending meal duration on increasing fruit and vegetable intake in particular has not been examined, they said.
In a study published in JAMA Network Open, the researchers provided two free evening meals to 50 parent-child dyads under each of two different conditions. The control condition was defined by the families as a regular family mealtime duration (an average meal was 20.83 minutes), while the intervention was an average meal time 10 minutes (50%) longer. The age of the parents ranged from 22 to 55 years, with a mean of 43 years; 72% of the parent participants were mothers. The children’s ages ranged from 6 to 11 years, with a mean of 8 years, with approximately equal numbers of boys and girls.
The study was conducted in a family meal laboratory setting in Berlin, and groups were randomized to the longer or shorter meal setting first. The primary outcome was the total number of pieces of fruit and vegetables eaten by the child as part of each of the two meals.
Both meals were the “typical German evening meal of sliced bread, cold cuts of cheese and meat, and bite-sized pieces of fruits and vegetables,” followed by a dessert course of chocolate pudding or fruit yogurt and cookies, the researchers wrote. Beverages were water and one sugar-sweetened beverage; the specific foods and beverages were based on the child’s preferences, reported in an online preassessment, and the foods were consistent for the longer and shorter meals. All participants were asked not to eat for 2 hours prior to arriving for their meals at the laboratory.
During longer meals, children ate an average of seven additional bite-sized pieces of fruits and vegetables, which translates to approximately a full portion (defined as 100 g, such as a medium apple), the researchers wrote. The difference was significant compared with the shorter meals for fruits (P = .01) and vegetables (P < .001).
A piece of fruit was approximately 10 grams (6-10 g for grapes and tangerine segments; 10-14 g for cherry tomatoes; and 9-11 g for apple, banana, carrot, or cucumber). Other foods served with the meals included cheese, meats, butter, and sweet spreads.
Children also ate more slowly (defined as fewer bites per minute) during the longer meals, and they reported significantly greater satiety after the longer meals (P < .001 for both). The consumption of bread and cold cuts was similar for the two meal settings.
“Higher intake of fruits and vegetables during longer meals cannot be explained by longer exposure to food alone; otherwise, an increased intake of bread and cold cuts would have occurred,” the researchers wrote in their discussion. “One possible explanation is that the fruits and vegetables were cut into bite-sized pieces, making them convenient to eat.”
Further analysis showed that during the longer meals, more fruits and vegetables were consumed overall, but more vegetables were eaten from the start of the meal, while the additional fruit was eaten during the additional time at the end.
The findings were limited by several factors, primarily use of a laboratory setting that does not generalize to natural eating environments, the researchers noted. Other potential limitations included the effect of a video cameras on desirable behaviors and the limited ethnic and socioeconomic diversity of the study population, they said. The results were strengthened by the within-dyad study design that allowed for control of factors such as video observation, but more research is needed with more diverse groups and across longer time frames, the researchers said.
However, the results suggest that adding 10 minutes to a family mealtime can yield significant improvements in children’s diets, they said. They suggested strategies including playing music chosen by the child/children and setting rules that everyone must remain at the table for a certain length of time, with fruits and vegetables available on the table.
“If the effects of this simple, inexpensive, and low-threshold intervention prove stable over time, it could contribute to addressing a major public health problem,” the researchers concluded.
Findings intriguing, more data needed
The current study is important because food and vegetable intake in the majority of children falls below the recommended daily allowance, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
The key take-home message for clinicians is the continued need to stress the importance of family meals, said Dr. Kinsella. “Many children continue to be overbooked with activities, and it may be rare for many families to sit down together for a meal for any length of time.”
Don’t discount the potential effect of a longer school lunch on children’s fruit and vegetable consumption as well, she added. “Advocating for longer lunch time is important, as many kids report not being able to finish their lunch at school.”
The current study was limited by being conducted in a lab setting, which may have influenced children’s desire for different foods, “also they had fewer distractions, and were being offered favorite foods,” said Dr. Kinsella.
Looking ahead, “it would be interesting to see if this result carried over to nonpreferred fruits and veggies and made any difference for picky eaters,” she said.
The study received no outside funding. The open-access publication of the study (but not the study itself) was supported by the Max Planck Institute for Human Development Library Open Access Fund. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM JAMA NETWORK OPEN
Likely cause of mysterious hepatitis outbreak in children identified
Coinfection with AAV2 and a human adenovirus (HAdV), in particular, appears to leave some children more vulnerable to this acute hepatitis of unknown origin, researchers reported in three studies published online in Nature. Coinfection with Epstein-Barr virus (EBV), herpes, and enterovirus also were found. Adeno-associated viruses are not considered pathogenic on their own and require a “helper” virus for productive infection.
“I am quite confident that we have identified the key viruses involved because we used a comprehensive metagenomic sequencing approach to look for potential infections from any virus or non-viral pathogen,” Charles Chiu, MD, PhD, senior author and professor of laboratory medicine and medicine/infectious diseases at the University of California, San Francisco, said in an interview.
Dr. Chiu and colleagues propose that lockdowns and social isolation during the COVID-19 pandemic left more children susceptible. A major aspect of immunity in childhood is the adaptive immune response – both cell-mediated and humoral – shaped in part by exposure to viruses and other pathogens early in life, Dr. Chiu said.
“Due to COVID-19, a large population of children did not experience this, so it is possible once restrictions were lifted, they were suddenly exposed over a short period of time to multiple viruses that, in a poorly trained immune system, would have increased their risk of developing severe disease,” he said.
This theory has been popular, especially because cases of unexplained acute hepatitis peaked during the height of the COVID-19 pandemic when isolation was common, William F. Balistreri, MD, who was not affiliated with the study, told this news organization. Dr. Balistreri is professor of pediatrics and director emeritus of the Pediatric Liver Care Center at Cincinnati Children’s Hospital Medical Center.
Identifying the culprits
Determining what factors might be involved was the main aim of the etiology study by Dr. Chiu and colleagues published online in Nature.
The journal simultaneously published a genomic study confirming the presence of AAV2 and other suspected viruses and a genomic and laboratory study further corroborating the results.
More than 1,000 children worldwide had been diagnosed with unexplained acute pediatric hepatitis as of August 2022. In the United States, there have been 358 cases, including 22 in which the child required a liver transplant and 13 in which the child died.
This new form of hepatitis, first detected in October 2021, does not fit into existing classifications of types A through E, so some researchers refer to the condition as acute non–A-E hepatitis of unknown etiology.
The investigators started with an important clue based on previous research: the role adenovirus might play. Dr. Chiu and colleagues assessed 27 blood, stool, and other samples from 16 affected children who each previously tested positive for adenoviruses. The researchers included cases of the condition identified up until May 22, 2022. The median age was 3 years, and approximately half were boys.
They compared viruses present in these children with those in 113 controls without the mysterious hepatitis. The control group consisted of 15 children who were hospitalized with a nonhepatitis inflammatory condition, 27 with a noninflammatory condition, 30 with acute hepatitis of known origin, 12 with acute gastroenteritis and an HAdV-positive stool sample, and 11 with acute gastroenteritis and an HAdV-negative stool sample, as well as 18 blood donors. The median age was 7 years.
The researchers assessed samples using multiple technologies, including metagenomic sequencing, tiling multiplex polymerase chain reaction (PCR) amplicon sequencing, metagenomic sequencing with probe capture viral enrichment, and virus-specific PCR. Many of these advanced techniques were not even available 5-10 years ago, Dr. Chiu said.
Key findings
Blood samples were available for 14 of the 16 children with acute hepatitis of unknown origin. Among this study group, AAV2 was found in 13 (93%). No other adeno-associated viruses were found. HAdV was detected in all 14 children: HAdV-41 in 11 children and HAdV-40, HAdV-2, and an untypeable strain in one child each. This finding was not intuitive because HAdVs are not commonly associated with hepatitis, according to the study.
AAV2 was much less common in the control group. For example, it was found in none of the children with hepatitis of known origin and in only four children (3.5%) with acute gastroenteritis and HAdV-positive stool. Of note, neither AAV2 nor HAdV-41 was detected among the 30 pediatric controls with acute hepatitis of defined etiology nor 42 of the hospitalized children without hepatitis, the researchers wrote.
In the search for other viruses in the study group, metagenomic sequencing detected EBV, also known as human herpesvirus (HHV)–4, in two children, cytomegalovirus (CMV) in one child, and HAdV type C in one child.
Analysis of whole blood revealed enterovirus A71 in one patient. HAdV type C also was detected in one child on the basis of a nasopharyngeal swab, and picobirnavirus was found in a stool sample from another patient.
Researchers conducted virus-specific PCR tests on both patient groups to identify additional viruses that may be associated with the unexplained acute hepatitis. EBV/HHV-4 was detected in 11 children (79%) in the study group vs. in 1 child (0.88%) in the control group. HHV-6 was detected in seven children (50%) in the study group, compared with one case in the control group. CMV was not detected in any of the children in the study group versus vs. two children (1.8%) in the control group.
“Although we found significant differences in the relative proportions of EBV and HHV-6 in cases compared to controls, we do not believe that these viruses are the primary cause of acute severe hepatitis,” the researchers wrote. The viral load of the two herpes viruses were very low, so the positive results could represent integrated proviral DNA rather than bona fide low-level herpesvirus. In addition, herpesvirus can be reactivated by an inflammatory condition.
“Nevertheless, it is striking that among the 16 cases (in the study group), dual, triple, or quadruple infections with AAV2, adenovirus, and one or both herpesviruses were detected in whole blood from at least 12 cases (75%),” the researchers wrote.
Management of suspected hepatitis
The study’s key messages for parents and health care providers “are awareness and reassurance,” Dr. Balistreri said in an interview.
Vigilance also is warranted if a child develops prodromal symptoms including respiratory and/or gastrointestinal signs such as nausea, vomiting, diarrhea, and abdomen pain, he said. If jaundice or scleral icterus is noted, then hepatitis should be suspected.
Some patients need hospitalization and quickly recover. In very rare instances, the inflammation may progress to liver failure and transplantation, Dr. Balistreri said.
“Reassurance is based on the good news that most children with acute hepatitis get better. If a case arises, it is good practice to keep the child well hydrated, offer a normal diet, and avoid medications that may be cleared by the liver,” Dr. Balistreri added.
“Of course, COVID-19 vaccination is strongly suggested,” he said.
Some existing treatments could help against unexplained acute hepatitis, Dr. Chiu said. “The findings suggest that antiviral therapy might be effective in these cases.”
Cidofovir can be effective against adenovirus, according to a report in The Lancet . Similarly, ganciclovir or valganciclovir may have activity against EBV/HHV-4 or HHV-6, Dr. Chiu said. “However, antiviral therapy is not available for AAV2.”
The three studies published in Nature “offer compelling evidence, from disparate centers, of a linkage of outbreak cases to infection by AAV2,” Dr. Balistreri said. The studies also suggest that liver injury was related to abnormal immune responses. This is an important clinical distinction, indicating a potential therapeutic approach to future cases – immunosuppression rather than anti-adenoviral agents, he said.
“We await further studies of this important concept,” Dr. Balistreri said.
Many unanswered questions remain about the condition’s etiology, he added. Is there a synergy or shared susceptibility related to SARS-CoV-2? Is the COVID-19 virus helping to trigger these infections, or does it increase the risk once infected? Also, are other epigenetic factors or viruses involved?
Moving forward
The next steps in the research could go beyond identifying presence of these different viruses and determining which one(s) are contributing the most to the acute pediatric hepatitis, Dr. Chiu said.
The researchers also would like to test early results from the United Kingdom that identified a potential association of acute severe hepatitis with the presence of human leukocyte antigen genotype DRB1*04:01, he added.
They also might investigate other unintended potential clinical consequences of the COVID-19 pandemic, including long COVID and resurgence of infections from other viruses, such as respiratory syncytial virus, influenza, and enterovirus D68.
The study was supported by the Centers for Disease Control and Prevention, the National Institutes of Health, the Department of Homeland Security, and other grants. Dr. Chiu is a founder of Delve Bio and on the scientific advisory board for Delve Bio, Mammoth Biosciences, BiomeSense, and Poppy Health. Dr. Balistreri had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Coinfection with AAV2 and a human adenovirus (HAdV), in particular, appears to leave some children more vulnerable to this acute hepatitis of unknown origin, researchers reported in three studies published online in Nature. Coinfection with Epstein-Barr virus (EBV), herpes, and enterovirus also were found. Adeno-associated viruses are not considered pathogenic on their own and require a “helper” virus for productive infection.
“I am quite confident that we have identified the key viruses involved because we used a comprehensive metagenomic sequencing approach to look for potential infections from any virus or non-viral pathogen,” Charles Chiu, MD, PhD, senior author and professor of laboratory medicine and medicine/infectious diseases at the University of California, San Francisco, said in an interview.
Dr. Chiu and colleagues propose that lockdowns and social isolation during the COVID-19 pandemic left more children susceptible. A major aspect of immunity in childhood is the adaptive immune response – both cell-mediated and humoral – shaped in part by exposure to viruses and other pathogens early in life, Dr. Chiu said.
“Due to COVID-19, a large population of children did not experience this, so it is possible once restrictions were lifted, they were suddenly exposed over a short period of time to multiple viruses that, in a poorly trained immune system, would have increased their risk of developing severe disease,” he said.
This theory has been popular, especially because cases of unexplained acute hepatitis peaked during the height of the COVID-19 pandemic when isolation was common, William F. Balistreri, MD, who was not affiliated with the study, told this news organization. Dr. Balistreri is professor of pediatrics and director emeritus of the Pediatric Liver Care Center at Cincinnati Children’s Hospital Medical Center.
Identifying the culprits
Determining what factors might be involved was the main aim of the etiology study by Dr. Chiu and colleagues published online in Nature.
The journal simultaneously published a genomic study confirming the presence of AAV2 and other suspected viruses and a genomic and laboratory study further corroborating the results.
More than 1,000 children worldwide had been diagnosed with unexplained acute pediatric hepatitis as of August 2022. In the United States, there have been 358 cases, including 22 in which the child required a liver transplant and 13 in which the child died.
This new form of hepatitis, first detected in October 2021, does not fit into existing classifications of types A through E, so some researchers refer to the condition as acute non–A-E hepatitis of unknown etiology.
The investigators started with an important clue based on previous research: the role adenovirus might play. Dr. Chiu and colleagues assessed 27 blood, stool, and other samples from 16 affected children who each previously tested positive for adenoviruses. The researchers included cases of the condition identified up until May 22, 2022. The median age was 3 years, and approximately half were boys.
They compared viruses present in these children with those in 113 controls without the mysterious hepatitis. The control group consisted of 15 children who were hospitalized with a nonhepatitis inflammatory condition, 27 with a noninflammatory condition, 30 with acute hepatitis of known origin, 12 with acute gastroenteritis and an HAdV-positive stool sample, and 11 with acute gastroenteritis and an HAdV-negative stool sample, as well as 18 blood donors. The median age was 7 years.
The researchers assessed samples using multiple technologies, including metagenomic sequencing, tiling multiplex polymerase chain reaction (PCR) amplicon sequencing, metagenomic sequencing with probe capture viral enrichment, and virus-specific PCR. Many of these advanced techniques were not even available 5-10 years ago, Dr. Chiu said.
Key findings
Blood samples were available for 14 of the 16 children with acute hepatitis of unknown origin. Among this study group, AAV2 was found in 13 (93%). No other adeno-associated viruses were found. HAdV was detected in all 14 children: HAdV-41 in 11 children and HAdV-40, HAdV-2, and an untypeable strain in one child each. This finding was not intuitive because HAdVs are not commonly associated with hepatitis, according to the study.
AAV2 was much less common in the control group. For example, it was found in none of the children with hepatitis of known origin and in only four children (3.5%) with acute gastroenteritis and HAdV-positive stool. Of note, neither AAV2 nor HAdV-41 was detected among the 30 pediatric controls with acute hepatitis of defined etiology nor 42 of the hospitalized children without hepatitis, the researchers wrote.
In the search for other viruses in the study group, metagenomic sequencing detected EBV, also known as human herpesvirus (HHV)–4, in two children, cytomegalovirus (CMV) in one child, and HAdV type C in one child.
Analysis of whole blood revealed enterovirus A71 in one patient. HAdV type C also was detected in one child on the basis of a nasopharyngeal swab, and picobirnavirus was found in a stool sample from another patient.
Researchers conducted virus-specific PCR tests on both patient groups to identify additional viruses that may be associated with the unexplained acute hepatitis. EBV/HHV-4 was detected in 11 children (79%) in the study group vs. in 1 child (0.88%) in the control group. HHV-6 was detected in seven children (50%) in the study group, compared with one case in the control group. CMV was not detected in any of the children in the study group versus vs. two children (1.8%) in the control group.
“Although we found significant differences in the relative proportions of EBV and HHV-6 in cases compared to controls, we do not believe that these viruses are the primary cause of acute severe hepatitis,” the researchers wrote. The viral load of the two herpes viruses were very low, so the positive results could represent integrated proviral DNA rather than bona fide low-level herpesvirus. In addition, herpesvirus can be reactivated by an inflammatory condition.
“Nevertheless, it is striking that among the 16 cases (in the study group), dual, triple, or quadruple infections with AAV2, adenovirus, and one or both herpesviruses were detected in whole blood from at least 12 cases (75%),” the researchers wrote.
Management of suspected hepatitis
The study’s key messages for parents and health care providers “are awareness and reassurance,” Dr. Balistreri said in an interview.
Vigilance also is warranted if a child develops prodromal symptoms including respiratory and/or gastrointestinal signs such as nausea, vomiting, diarrhea, and abdomen pain, he said. If jaundice or scleral icterus is noted, then hepatitis should be suspected.
Some patients need hospitalization and quickly recover. In very rare instances, the inflammation may progress to liver failure and transplantation, Dr. Balistreri said.
“Reassurance is based on the good news that most children with acute hepatitis get better. If a case arises, it is good practice to keep the child well hydrated, offer a normal diet, and avoid medications that may be cleared by the liver,” Dr. Balistreri added.
“Of course, COVID-19 vaccination is strongly suggested,” he said.
Some existing treatments could help against unexplained acute hepatitis, Dr. Chiu said. “The findings suggest that antiviral therapy might be effective in these cases.”
Cidofovir can be effective against adenovirus, according to a report in The Lancet . Similarly, ganciclovir or valganciclovir may have activity against EBV/HHV-4 or HHV-6, Dr. Chiu said. “However, antiviral therapy is not available for AAV2.”
The three studies published in Nature “offer compelling evidence, from disparate centers, of a linkage of outbreak cases to infection by AAV2,” Dr. Balistreri said. The studies also suggest that liver injury was related to abnormal immune responses. This is an important clinical distinction, indicating a potential therapeutic approach to future cases – immunosuppression rather than anti-adenoviral agents, he said.
“We await further studies of this important concept,” Dr. Balistreri said.
Many unanswered questions remain about the condition’s etiology, he added. Is there a synergy or shared susceptibility related to SARS-CoV-2? Is the COVID-19 virus helping to trigger these infections, or does it increase the risk once infected? Also, are other epigenetic factors or viruses involved?
Moving forward
The next steps in the research could go beyond identifying presence of these different viruses and determining which one(s) are contributing the most to the acute pediatric hepatitis, Dr. Chiu said.
The researchers also would like to test early results from the United Kingdom that identified a potential association of acute severe hepatitis with the presence of human leukocyte antigen genotype DRB1*04:01, he added.
They also might investigate other unintended potential clinical consequences of the COVID-19 pandemic, including long COVID and resurgence of infections from other viruses, such as respiratory syncytial virus, influenza, and enterovirus D68.
The study was supported by the Centers for Disease Control and Prevention, the National Institutes of Health, the Department of Homeland Security, and other grants. Dr. Chiu is a founder of Delve Bio and on the scientific advisory board for Delve Bio, Mammoth Biosciences, BiomeSense, and Poppy Health. Dr. Balistreri had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Coinfection with AAV2 and a human adenovirus (HAdV), in particular, appears to leave some children more vulnerable to this acute hepatitis of unknown origin, researchers reported in three studies published online in Nature. Coinfection with Epstein-Barr virus (EBV), herpes, and enterovirus also were found. Adeno-associated viruses are not considered pathogenic on their own and require a “helper” virus for productive infection.
“I am quite confident that we have identified the key viruses involved because we used a comprehensive metagenomic sequencing approach to look for potential infections from any virus or non-viral pathogen,” Charles Chiu, MD, PhD, senior author and professor of laboratory medicine and medicine/infectious diseases at the University of California, San Francisco, said in an interview.
Dr. Chiu and colleagues propose that lockdowns and social isolation during the COVID-19 pandemic left more children susceptible. A major aspect of immunity in childhood is the adaptive immune response – both cell-mediated and humoral – shaped in part by exposure to viruses and other pathogens early in life, Dr. Chiu said.
“Due to COVID-19, a large population of children did not experience this, so it is possible once restrictions were lifted, they were suddenly exposed over a short period of time to multiple viruses that, in a poorly trained immune system, would have increased their risk of developing severe disease,” he said.
This theory has been popular, especially because cases of unexplained acute hepatitis peaked during the height of the COVID-19 pandemic when isolation was common, William F. Balistreri, MD, who was not affiliated with the study, told this news organization. Dr. Balistreri is professor of pediatrics and director emeritus of the Pediatric Liver Care Center at Cincinnati Children’s Hospital Medical Center.
Identifying the culprits
Determining what factors might be involved was the main aim of the etiology study by Dr. Chiu and colleagues published online in Nature.
The journal simultaneously published a genomic study confirming the presence of AAV2 and other suspected viruses and a genomic and laboratory study further corroborating the results.
More than 1,000 children worldwide had been diagnosed with unexplained acute pediatric hepatitis as of August 2022. In the United States, there have been 358 cases, including 22 in which the child required a liver transplant and 13 in which the child died.
This new form of hepatitis, first detected in October 2021, does not fit into existing classifications of types A through E, so some researchers refer to the condition as acute non–A-E hepatitis of unknown etiology.
The investigators started with an important clue based on previous research: the role adenovirus might play. Dr. Chiu and colleagues assessed 27 blood, stool, and other samples from 16 affected children who each previously tested positive for adenoviruses. The researchers included cases of the condition identified up until May 22, 2022. The median age was 3 years, and approximately half were boys.
They compared viruses present in these children with those in 113 controls without the mysterious hepatitis. The control group consisted of 15 children who were hospitalized with a nonhepatitis inflammatory condition, 27 with a noninflammatory condition, 30 with acute hepatitis of known origin, 12 with acute gastroenteritis and an HAdV-positive stool sample, and 11 with acute gastroenteritis and an HAdV-negative stool sample, as well as 18 blood donors. The median age was 7 years.
The researchers assessed samples using multiple technologies, including metagenomic sequencing, tiling multiplex polymerase chain reaction (PCR) amplicon sequencing, metagenomic sequencing with probe capture viral enrichment, and virus-specific PCR. Many of these advanced techniques were not even available 5-10 years ago, Dr. Chiu said.
Key findings
Blood samples were available for 14 of the 16 children with acute hepatitis of unknown origin. Among this study group, AAV2 was found in 13 (93%). No other adeno-associated viruses were found. HAdV was detected in all 14 children: HAdV-41 in 11 children and HAdV-40, HAdV-2, and an untypeable strain in one child each. This finding was not intuitive because HAdVs are not commonly associated with hepatitis, according to the study.
AAV2 was much less common in the control group. For example, it was found in none of the children with hepatitis of known origin and in only four children (3.5%) with acute gastroenteritis and HAdV-positive stool. Of note, neither AAV2 nor HAdV-41 was detected among the 30 pediatric controls with acute hepatitis of defined etiology nor 42 of the hospitalized children without hepatitis, the researchers wrote.
In the search for other viruses in the study group, metagenomic sequencing detected EBV, also known as human herpesvirus (HHV)–4, in two children, cytomegalovirus (CMV) in one child, and HAdV type C in one child.
Analysis of whole blood revealed enterovirus A71 in one patient. HAdV type C also was detected in one child on the basis of a nasopharyngeal swab, and picobirnavirus was found in a stool sample from another patient.
Researchers conducted virus-specific PCR tests on both patient groups to identify additional viruses that may be associated with the unexplained acute hepatitis. EBV/HHV-4 was detected in 11 children (79%) in the study group vs. in 1 child (0.88%) in the control group. HHV-6 was detected in seven children (50%) in the study group, compared with one case in the control group. CMV was not detected in any of the children in the study group versus vs. two children (1.8%) in the control group.
“Although we found significant differences in the relative proportions of EBV and HHV-6 in cases compared to controls, we do not believe that these viruses are the primary cause of acute severe hepatitis,” the researchers wrote. The viral load of the two herpes viruses were very low, so the positive results could represent integrated proviral DNA rather than bona fide low-level herpesvirus. In addition, herpesvirus can be reactivated by an inflammatory condition.
“Nevertheless, it is striking that among the 16 cases (in the study group), dual, triple, or quadruple infections with AAV2, adenovirus, and one or both herpesviruses were detected in whole blood from at least 12 cases (75%),” the researchers wrote.
Management of suspected hepatitis
The study’s key messages for parents and health care providers “are awareness and reassurance,” Dr. Balistreri said in an interview.
Vigilance also is warranted if a child develops prodromal symptoms including respiratory and/or gastrointestinal signs such as nausea, vomiting, diarrhea, and abdomen pain, he said. If jaundice or scleral icterus is noted, then hepatitis should be suspected.
Some patients need hospitalization and quickly recover. In very rare instances, the inflammation may progress to liver failure and transplantation, Dr. Balistreri said.
“Reassurance is based on the good news that most children with acute hepatitis get better. If a case arises, it is good practice to keep the child well hydrated, offer a normal diet, and avoid medications that may be cleared by the liver,” Dr. Balistreri added.
“Of course, COVID-19 vaccination is strongly suggested,” he said.
Some existing treatments could help against unexplained acute hepatitis, Dr. Chiu said. “The findings suggest that antiviral therapy might be effective in these cases.”
Cidofovir can be effective against adenovirus, according to a report in The Lancet . Similarly, ganciclovir or valganciclovir may have activity against EBV/HHV-4 or HHV-6, Dr. Chiu said. “However, antiviral therapy is not available for AAV2.”
The three studies published in Nature “offer compelling evidence, from disparate centers, of a linkage of outbreak cases to infection by AAV2,” Dr. Balistreri said. The studies also suggest that liver injury was related to abnormal immune responses. This is an important clinical distinction, indicating a potential therapeutic approach to future cases – immunosuppression rather than anti-adenoviral agents, he said.
“We await further studies of this important concept,” Dr. Balistreri said.
Many unanswered questions remain about the condition’s etiology, he added. Is there a synergy or shared susceptibility related to SARS-CoV-2? Is the COVID-19 virus helping to trigger these infections, or does it increase the risk once infected? Also, are other epigenetic factors or viruses involved?
Moving forward
The next steps in the research could go beyond identifying presence of these different viruses and determining which one(s) are contributing the most to the acute pediatric hepatitis, Dr. Chiu said.
The researchers also would like to test early results from the United Kingdom that identified a potential association of acute severe hepatitis with the presence of human leukocyte antigen genotype DRB1*04:01, he added.
They also might investigate other unintended potential clinical consequences of the COVID-19 pandemic, including long COVID and resurgence of infections from other viruses, such as respiratory syncytial virus, influenza, and enterovirus D68.
The study was supported by the Centers for Disease Control and Prevention, the National Institutes of Health, the Department of Homeland Security, and other grants. Dr. Chiu is a founder of Delve Bio and on the scientific advisory board for Delve Bio, Mammoth Biosciences, BiomeSense, and Poppy Health. Dr. Balistreri had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM NATURE
Is vaping a gateway to cigarettes for kids?
Vaping may not be a gateway to long-term cigarette use for adolescents, a new study published in JAMA Network Open suggests.
Many studies have found that youth who vape are more likely to take up cigarette smoking, but whether that new habit lasts for a month or a lifetime has been unclear.
The percentage of adolescents who move on to smoking after starting to vape remains low, and those who do start smoking are unlikely to continue doing so for a long time, the new research shows.
“If they simply experiment with smoking but do not continue, their risks of smoking-related adverse health outcomes are low,” said Ruoyan Sun, PhD, assistant professor with the department of health policy and organization at the University of Alabama at Birmingham and the study’s lead author. “But if they do become regular or established smokers, then the risks can be substantial.”
Dr. Sun and her colleagues analyzed data from several waves of the longitudinal Population Assessment of Tobacco and Health study. Participants included 8,671 children and adolescents aged 12-17 years. Among teens who had ever vaped, 6% began smoking cigarettes and continued to smoke in the subsequent 3 years, the researchers found (95% confidence interval, 4.5%-8.0%), compared with 1.1% among teens who never vaped (95% CI, 0.8%-1.3%).
“The real concern is whether vaping is inducing significant numbers of young people to become confirmed smokers,” said Dr. Sun. “The answer is that it does not.”
Previous studies using PATH data have suggested that adolescents who use e-cigarettes are up to 3.5 times more likely than nonusers to start smoking tobacco cigarettes and that they may continue to use both products.
But in the new study, despite the low overall number of cigarette smokers, those in the group who used e-cigarettes were 81% more likely to continue smoking tobacco cigarettes after 3 years, compared with those who did not use e-cigarettes, researchers found (95% CI, 1.03-3.18).
Rachel Boykan, MD, clinical professor of pediatrics and attending physician at Stony Brook (N.Y.) Children’s Hospital, said that despite the findings, the overall messaging to patients remains the same: Vaping is linked to smoking.
“There is still a risk of initiation smoking among e-cigarette users – that is the take-home message,” Dr. Boykan, who was not affiliated with the study, said. “No risk of smoking initiation is acceptable. And of course, as we are learning, there are significant health risks with e-cigarette use alone.”
Among the entire group of teens, approximately 4% of the adolescents began smoking cigarettes; only 2.5% continued to smoke in the subsequent 3 years, the researchers found.
“Based on our odds ratio result, e-cigarette users are more likely to report continued cigarette smoking,” said Dr. Sun. “However, the risk differences were not significant.”
The low numbers of teens who continued to smoke also suggests that adolescents are more likely to quit than become long-term smokers.
Nicotine dependence may adversely affect the ability of adolescents to learn, remember, and maintain attention. Early research has suggested that long-term e-cigarette smokers may be at increased risk of developing some of the same conditions as tobacco smokers, such as chronic lung disease.
Brian Jenssen, MD, a pediatrician at Children’s Hospital of Philadelphia and assistant professor in the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, said that the analysis is limited in part because it does not include changes in smoking and vaping trends since the pandemic started, “which seems to have increased the risk of smoking and vaping use.”
Data from the 2022 National Youth Tobacco survey found that although the rate of middle school and high school students who begin to use e-cigarettes has steadily decreased during the past two decades, those who vape report using the devices more frequently.
Subsequent use of cigarettes is also only one measure of risk from vapes.
“The goal isn’t just about cigarettes,” said Dr. Jenssen, who was not affiliated with the new study. “The goal is about helping children live tobacco- and nicotine-free lives, and there seems to be an increasing intensity of use, which is causing its own health risks.”
The current study findings do not change how clinicians should counsel their patients, and they should continue to advise teens to abstain from vaping, he added.
Dr. Sun said it’s common for youth to experiment with multiple tobacco products.
“Clinicians should continue to monitor youth tobacco-use behaviors but with their concern being focused on youthful patients who sustain smoking instead of just trying cigarettes,” she said.
Some of the study authors received support from the National Cancer Institute of the National Institutes of Health and the U.S. Food and Drug Administration’s Center for Tobacco Products.
A version of this article first appeared on Medscape.com.
Vaping may not be a gateway to long-term cigarette use for adolescents, a new study published in JAMA Network Open suggests.
Many studies have found that youth who vape are more likely to take up cigarette smoking, but whether that new habit lasts for a month or a lifetime has been unclear.
The percentage of adolescents who move on to smoking after starting to vape remains low, and those who do start smoking are unlikely to continue doing so for a long time, the new research shows.
“If they simply experiment with smoking but do not continue, their risks of smoking-related adverse health outcomes are low,” said Ruoyan Sun, PhD, assistant professor with the department of health policy and organization at the University of Alabama at Birmingham and the study’s lead author. “But if they do become regular or established smokers, then the risks can be substantial.”
Dr. Sun and her colleagues analyzed data from several waves of the longitudinal Population Assessment of Tobacco and Health study. Participants included 8,671 children and adolescents aged 12-17 years. Among teens who had ever vaped, 6% began smoking cigarettes and continued to smoke in the subsequent 3 years, the researchers found (95% confidence interval, 4.5%-8.0%), compared with 1.1% among teens who never vaped (95% CI, 0.8%-1.3%).
“The real concern is whether vaping is inducing significant numbers of young people to become confirmed smokers,” said Dr. Sun. “The answer is that it does not.”
Previous studies using PATH data have suggested that adolescents who use e-cigarettes are up to 3.5 times more likely than nonusers to start smoking tobacco cigarettes and that they may continue to use both products.
But in the new study, despite the low overall number of cigarette smokers, those in the group who used e-cigarettes were 81% more likely to continue smoking tobacco cigarettes after 3 years, compared with those who did not use e-cigarettes, researchers found (95% CI, 1.03-3.18).
Rachel Boykan, MD, clinical professor of pediatrics and attending physician at Stony Brook (N.Y.) Children’s Hospital, said that despite the findings, the overall messaging to patients remains the same: Vaping is linked to smoking.
“There is still a risk of initiation smoking among e-cigarette users – that is the take-home message,” Dr. Boykan, who was not affiliated with the study, said. “No risk of smoking initiation is acceptable. And of course, as we are learning, there are significant health risks with e-cigarette use alone.”
Among the entire group of teens, approximately 4% of the adolescents began smoking cigarettes; only 2.5% continued to smoke in the subsequent 3 years, the researchers found.
“Based on our odds ratio result, e-cigarette users are more likely to report continued cigarette smoking,” said Dr. Sun. “However, the risk differences were not significant.”
The low numbers of teens who continued to smoke also suggests that adolescents are more likely to quit than become long-term smokers.
Nicotine dependence may adversely affect the ability of adolescents to learn, remember, and maintain attention. Early research has suggested that long-term e-cigarette smokers may be at increased risk of developing some of the same conditions as tobacco smokers, such as chronic lung disease.
Brian Jenssen, MD, a pediatrician at Children’s Hospital of Philadelphia and assistant professor in the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, said that the analysis is limited in part because it does not include changes in smoking and vaping trends since the pandemic started, “which seems to have increased the risk of smoking and vaping use.”
Data from the 2022 National Youth Tobacco survey found that although the rate of middle school and high school students who begin to use e-cigarettes has steadily decreased during the past two decades, those who vape report using the devices more frequently.
Subsequent use of cigarettes is also only one measure of risk from vapes.
“The goal isn’t just about cigarettes,” said Dr. Jenssen, who was not affiliated with the new study. “The goal is about helping children live tobacco- and nicotine-free lives, and there seems to be an increasing intensity of use, which is causing its own health risks.”
The current study findings do not change how clinicians should counsel their patients, and they should continue to advise teens to abstain from vaping, he added.
Dr. Sun said it’s common for youth to experiment with multiple tobacco products.
“Clinicians should continue to monitor youth tobacco-use behaviors but with their concern being focused on youthful patients who sustain smoking instead of just trying cigarettes,” she said.
Some of the study authors received support from the National Cancer Institute of the National Institutes of Health and the U.S. Food and Drug Administration’s Center for Tobacco Products.
A version of this article first appeared on Medscape.com.
Vaping may not be a gateway to long-term cigarette use for adolescents, a new study published in JAMA Network Open suggests.
Many studies have found that youth who vape are more likely to take up cigarette smoking, but whether that new habit lasts for a month or a lifetime has been unclear.
The percentage of adolescents who move on to smoking after starting to vape remains low, and those who do start smoking are unlikely to continue doing so for a long time, the new research shows.
“If they simply experiment with smoking but do not continue, their risks of smoking-related adverse health outcomes are low,” said Ruoyan Sun, PhD, assistant professor with the department of health policy and organization at the University of Alabama at Birmingham and the study’s lead author. “But if they do become regular or established smokers, then the risks can be substantial.”
Dr. Sun and her colleagues analyzed data from several waves of the longitudinal Population Assessment of Tobacco and Health study. Participants included 8,671 children and adolescents aged 12-17 years. Among teens who had ever vaped, 6% began smoking cigarettes and continued to smoke in the subsequent 3 years, the researchers found (95% confidence interval, 4.5%-8.0%), compared with 1.1% among teens who never vaped (95% CI, 0.8%-1.3%).
“The real concern is whether vaping is inducing significant numbers of young people to become confirmed smokers,” said Dr. Sun. “The answer is that it does not.”
Previous studies using PATH data have suggested that adolescents who use e-cigarettes are up to 3.5 times more likely than nonusers to start smoking tobacco cigarettes and that they may continue to use both products.
But in the new study, despite the low overall number of cigarette smokers, those in the group who used e-cigarettes were 81% more likely to continue smoking tobacco cigarettes after 3 years, compared with those who did not use e-cigarettes, researchers found (95% CI, 1.03-3.18).
Rachel Boykan, MD, clinical professor of pediatrics and attending physician at Stony Brook (N.Y.) Children’s Hospital, said that despite the findings, the overall messaging to patients remains the same: Vaping is linked to smoking.
“There is still a risk of initiation smoking among e-cigarette users – that is the take-home message,” Dr. Boykan, who was not affiliated with the study, said. “No risk of smoking initiation is acceptable. And of course, as we are learning, there are significant health risks with e-cigarette use alone.”
Among the entire group of teens, approximately 4% of the adolescents began smoking cigarettes; only 2.5% continued to smoke in the subsequent 3 years, the researchers found.
“Based on our odds ratio result, e-cigarette users are more likely to report continued cigarette smoking,” said Dr. Sun. “However, the risk differences were not significant.”
The low numbers of teens who continued to smoke also suggests that adolescents are more likely to quit than become long-term smokers.
Nicotine dependence may adversely affect the ability of adolescents to learn, remember, and maintain attention. Early research has suggested that long-term e-cigarette smokers may be at increased risk of developing some of the same conditions as tobacco smokers, such as chronic lung disease.
Brian Jenssen, MD, a pediatrician at Children’s Hospital of Philadelphia and assistant professor in the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, said that the analysis is limited in part because it does not include changes in smoking and vaping trends since the pandemic started, “which seems to have increased the risk of smoking and vaping use.”
Data from the 2022 National Youth Tobacco survey found that although the rate of middle school and high school students who begin to use e-cigarettes has steadily decreased during the past two decades, those who vape report using the devices more frequently.
Subsequent use of cigarettes is also only one measure of risk from vapes.
“The goal isn’t just about cigarettes,” said Dr. Jenssen, who was not affiliated with the new study. “The goal is about helping children live tobacco- and nicotine-free lives, and there seems to be an increasing intensity of use, which is causing its own health risks.”
The current study findings do not change how clinicians should counsel their patients, and they should continue to advise teens to abstain from vaping, he added.
Dr. Sun said it’s common for youth to experiment with multiple tobacco products.
“Clinicians should continue to monitor youth tobacco-use behaviors but with their concern being focused on youthful patients who sustain smoking instead of just trying cigarettes,” she said.
Some of the study authors received support from the National Cancer Institute of the National Institutes of Health and the U.S. Food and Drug Administration’s Center for Tobacco Products.
A version of this article first appeared on Medscape.com.
New AHA statement on pediatric primary hypertension issued
the American Heart Association said in a new scientific statement.
“Children can have secondary hypertension that is caused by an underlying condition such as chronic kidney disease, endocrine disorders, cardiac anomalies, and some syndromes. However, primary hypertension is now recognized as the most common type of hypertension in childhood,” Bonita Falkner, MD, chair of the writing group and emeritus professor of medicine and pediatrics, Thomas Jefferson University, Philadelphia, said in an interview.
And hypertensive children are “highly likely” to become hypertensive adults and to have measurable target organ injury, particularly left ventricular hypertrophy and vascular stiffening, the writing group noted.
The AHA statement on primary pediatric hypertension was published online in Hypertension.
Primary or essential hypertension occurs in up to 5% of children and adolescents in the United States and other countries.
The American Academy of Pediatrics (AAP), European Society of Hypertension and Hypertension Canada all define hypertension as repeated BP readings at or above the 95th percentile for children, but the thresholds differ by age.
The AAP adopts 130/80 mm Hg starting at age 13 years; the European Society of Hypertension adopts 140/90 mm Hg starting at age 16 years; and Hypertension Canada adopts 120/80 mm Hg for those aged 6-11 years and 130/85 mm Hg for those aged 12-17 years.
Adolescents entering adulthood with a BP < 120/80 mm Hg is an optimal goal, the writing group advised.
They recommend that health care professionals be trained on evidence-based methods to obtain accurate and reliable BP values with either auscultatory or oscillometric methods.
When the initial BP measurement is abnormal, repeat measurement by auscultation is recommended, within the same visit if possible, and then within weeks if the screening BP is hypertensive, or months if the screening BP is elevated.
Because BP levels are variable, even within a single visit, “best practice” is to obtain up to three BP measurements and to record the average of the latter two measurements unless the first measurement is normal, the writing group said. Further confirmation of diagnosis of hypertension can be obtained with 24-hour ambulatory BP monitoring (ABPM).
“Primary hypertension in youth is difficult to recognize in asymptomatic, otherwise healthy youth. There is now evidence that children and adolescents with primary hypertension may also have cardiac and vascular injury due to the hypertension,” Dr. Falkner told this news organization.
“If not identified and treated, the condition can progress to hypertension in young adulthood with heightened risk of premature cardiovascular events,” Dr. Falkner said.
The writing group said “primordial prevention” is an important public health goal because a population with lower BP will have fewer comorbidities related to hypertension and CVD.
Modifiable risk factors for primary hypertension in childhood include obesity, physical inactivity and poor diet/nutrition, disturbed sleep patterns, and environmental stress.
A healthy lifestyle in childhood – including eating healthy food, encouraging physical activity that leads to improved physical fitness and healthy sleep, and avoiding the development of obesity – may help mitigate the risk of hypertension in childhood, the writing group noted.
Looking ahead, they said efforts to improve recognition and diagnosis of high BP in children, as well as clinical trials to evaluate medical treatment and recommend public health initiatives, are all vital to combat rising rates of primary hypertension in children.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Council on Hypertension, the Council on Lifelong Congenital Heart Disease and Heart Health in the Young, the Council on Kidney in Cardiovascular Disease, the Council on Lifestyle and Cardiometabolic Health, and the Council on Cardiovascular and Stroke Nursing.
A version of this article first appeared on Medscape.com.
the American Heart Association said in a new scientific statement.
“Children can have secondary hypertension that is caused by an underlying condition such as chronic kidney disease, endocrine disorders, cardiac anomalies, and some syndromes. However, primary hypertension is now recognized as the most common type of hypertension in childhood,” Bonita Falkner, MD, chair of the writing group and emeritus professor of medicine and pediatrics, Thomas Jefferson University, Philadelphia, said in an interview.
And hypertensive children are “highly likely” to become hypertensive adults and to have measurable target organ injury, particularly left ventricular hypertrophy and vascular stiffening, the writing group noted.
The AHA statement on primary pediatric hypertension was published online in Hypertension.
Primary or essential hypertension occurs in up to 5% of children and adolescents in the United States and other countries.
The American Academy of Pediatrics (AAP), European Society of Hypertension and Hypertension Canada all define hypertension as repeated BP readings at or above the 95th percentile for children, but the thresholds differ by age.
The AAP adopts 130/80 mm Hg starting at age 13 years; the European Society of Hypertension adopts 140/90 mm Hg starting at age 16 years; and Hypertension Canada adopts 120/80 mm Hg for those aged 6-11 years and 130/85 mm Hg for those aged 12-17 years.
Adolescents entering adulthood with a BP < 120/80 mm Hg is an optimal goal, the writing group advised.
They recommend that health care professionals be trained on evidence-based methods to obtain accurate and reliable BP values with either auscultatory or oscillometric methods.
When the initial BP measurement is abnormal, repeat measurement by auscultation is recommended, within the same visit if possible, and then within weeks if the screening BP is hypertensive, or months if the screening BP is elevated.
Because BP levels are variable, even within a single visit, “best practice” is to obtain up to three BP measurements and to record the average of the latter two measurements unless the first measurement is normal, the writing group said. Further confirmation of diagnosis of hypertension can be obtained with 24-hour ambulatory BP monitoring (ABPM).
“Primary hypertension in youth is difficult to recognize in asymptomatic, otherwise healthy youth. There is now evidence that children and adolescents with primary hypertension may also have cardiac and vascular injury due to the hypertension,” Dr. Falkner told this news organization.
“If not identified and treated, the condition can progress to hypertension in young adulthood with heightened risk of premature cardiovascular events,” Dr. Falkner said.
The writing group said “primordial prevention” is an important public health goal because a population with lower BP will have fewer comorbidities related to hypertension and CVD.
Modifiable risk factors for primary hypertension in childhood include obesity, physical inactivity and poor diet/nutrition, disturbed sleep patterns, and environmental stress.
A healthy lifestyle in childhood – including eating healthy food, encouraging physical activity that leads to improved physical fitness and healthy sleep, and avoiding the development of obesity – may help mitigate the risk of hypertension in childhood, the writing group noted.
Looking ahead, they said efforts to improve recognition and diagnosis of high BP in children, as well as clinical trials to evaluate medical treatment and recommend public health initiatives, are all vital to combat rising rates of primary hypertension in children.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Council on Hypertension, the Council on Lifelong Congenital Heart Disease and Heart Health in the Young, the Council on Kidney in Cardiovascular Disease, the Council on Lifestyle and Cardiometabolic Health, and the Council on Cardiovascular and Stroke Nursing.
A version of this article first appeared on Medscape.com.
the American Heart Association said in a new scientific statement.
“Children can have secondary hypertension that is caused by an underlying condition such as chronic kidney disease, endocrine disorders, cardiac anomalies, and some syndromes. However, primary hypertension is now recognized as the most common type of hypertension in childhood,” Bonita Falkner, MD, chair of the writing group and emeritus professor of medicine and pediatrics, Thomas Jefferson University, Philadelphia, said in an interview.
And hypertensive children are “highly likely” to become hypertensive adults and to have measurable target organ injury, particularly left ventricular hypertrophy and vascular stiffening, the writing group noted.
The AHA statement on primary pediatric hypertension was published online in Hypertension.
Primary or essential hypertension occurs in up to 5% of children and adolescents in the United States and other countries.
The American Academy of Pediatrics (AAP), European Society of Hypertension and Hypertension Canada all define hypertension as repeated BP readings at or above the 95th percentile for children, but the thresholds differ by age.
The AAP adopts 130/80 mm Hg starting at age 13 years; the European Society of Hypertension adopts 140/90 mm Hg starting at age 16 years; and Hypertension Canada adopts 120/80 mm Hg for those aged 6-11 years and 130/85 mm Hg for those aged 12-17 years.
Adolescents entering adulthood with a BP < 120/80 mm Hg is an optimal goal, the writing group advised.
They recommend that health care professionals be trained on evidence-based methods to obtain accurate and reliable BP values with either auscultatory or oscillometric methods.
When the initial BP measurement is abnormal, repeat measurement by auscultation is recommended, within the same visit if possible, and then within weeks if the screening BP is hypertensive, or months if the screening BP is elevated.
Because BP levels are variable, even within a single visit, “best practice” is to obtain up to three BP measurements and to record the average of the latter two measurements unless the first measurement is normal, the writing group said. Further confirmation of diagnosis of hypertension can be obtained with 24-hour ambulatory BP monitoring (ABPM).
“Primary hypertension in youth is difficult to recognize in asymptomatic, otherwise healthy youth. There is now evidence that children and adolescents with primary hypertension may also have cardiac and vascular injury due to the hypertension,” Dr. Falkner told this news organization.
“If not identified and treated, the condition can progress to hypertension in young adulthood with heightened risk of premature cardiovascular events,” Dr. Falkner said.
The writing group said “primordial prevention” is an important public health goal because a population with lower BP will have fewer comorbidities related to hypertension and CVD.
Modifiable risk factors for primary hypertension in childhood include obesity, physical inactivity and poor diet/nutrition, disturbed sleep patterns, and environmental stress.
A healthy lifestyle in childhood – including eating healthy food, encouraging physical activity that leads to improved physical fitness and healthy sleep, and avoiding the development of obesity – may help mitigate the risk of hypertension in childhood, the writing group noted.
Looking ahead, they said efforts to improve recognition and diagnosis of high BP in children, as well as clinical trials to evaluate medical treatment and recommend public health initiatives, are all vital to combat rising rates of primary hypertension in children.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Council on Hypertension, the Council on Lifelong Congenital Heart Disease and Heart Health in the Young, the Council on Kidney in Cardiovascular Disease, the Council on Lifestyle and Cardiometabolic Health, and the Council on Cardiovascular and Stroke Nursing.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION
Childhood lupus severity linked to social determinants of health
NEW ORLEANS – The sociodemographic characteristics of Black and Hispanic children with systemic lupus erythematosus (SLE) appear to play a strong role in influencing the severity of disease in these patients, according to two studies presented at the Pediatric Rheumatology Symposium.
One study showed an association between multiple determinants of health and disease severity among children seen in a large Texas city, and a separate descriptive cross-sectional cohort study of predominantly Black children at two centers in Mississippi and Alabama reinforced the finding of greater severity of disease and social hardships among this racial group.
The findings from both studies supplement existing evidence that the prevalence of childhood-onset SLE is greater among Black and Hispanic children.
“Several demographic and social determinants of health parameters influenced disease severity at levels that reached statistical significance, including insurance status, race/ethnicity, referral source, PCP [primary care provider] availability, primary language, and transportation needs,” Emily Beil, MD, a pediatric rheumatologist at Texas Children’s Hospital in Houston, told attendees at the conference, which was sponsored by the American College of Rheumatology. Her team’s goal, she said, was to “better understand our patient population and social disparities that contribute to disease severity.”
Dr. Beil and her colleagues conducted a retrospective review of 136 children who had been diagnosed with childhood-onset SLE between January 2018 and May 2022 at Texas Children’s Hospital. Only children who were younger than 18 years at the time of diagnosis at Texas Children’s were included. The analysis considered demographics, clinical characteristics, insurance status, social work consultation, access to a primary care provider, transportation needs, primary language, and other parameters related to social determinants of health.
The average age of the patients was 13 years, and most were girls (82%). Just over half were Hispanic (53%), and just over a quarter were Black (26%). Half had Medicaid or participated in the Children’s Health Insurance Program (CHIP), and 1 in 10 were uninsured (10%). Half the diagnoses were made during an inpatient admission; 36% were made on the floor, and 14% were made in the intensive care unit (ICU).
The average Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score was 12.5, and 48.5% of patients had severe disease, indicated by a score of at least 12. Only two in three children were documented as having a primary care physician (66%), and 32% preferred a language other than English. Most of the children (80%) had a social work consult.
Black and biracial children had higher SLEDAI scores at presentation. Non-Hispanic White children were less likely to have a social work consult, compared with other racial/ethnic groups (P = .01 for both). Central nervous system involvement was most prevalent among Black patients (P = .004). Cyclophosphamide was used most often for Black and biracial patients.
Uninsured patients were most likely to be diagnosed on an inpatient floor. The highest proportion of ICU admissions was among patients insured by Medicaid (P = .034). Average SLEDAI scores were highest among uninsured patients, followed by Medicaid patients. More than half of the patients who did not have insurance lacked access to a regular primary care provider, compared with 12% of Medicaid patients and 7% of privately insured patients (P = .001). All the uninsured patients had transportation needs, which was a significantly higher rate than among those with Medicaid (13%) or private insurance (15%) (P = .001). The highest percentage of social work consults was among patients who were insured by Medicaid or were without insurance (P = .001).
Salient demographics and clinical features
In the second presentation, Anita Dhanrajani, MD, assistant professor of pediatrics at the University of Mississippi Medical Center in Jackson, began by noting that Alabama and Mississippi are ranked in the top 10 states for the highest poverty rate: Mississippi is No. 1, and Alabama is No. 7. Further, 40% of children in Mississippi and 29% of children in Alabama are of African American ancestry, she said.
“So, we know that this population that we’re dealing with has several high-risk factors that can lead them to have poor outcomes, and yet, we haven’t really ever characterized their clinical features or their social demographic features,” Dr. Dhanrajani told attendees. “My hope is that with this very miniscule first step, we’re able to move towards solutions to decrease health care disparities in this population.”
She presented findings regarding the first of three aims in the study, which was to describe the baseline clinical, demographic, and socioeconomic profiles of childhood lupus patients at the two centers. The two other aims were to examine genetic factors potentially linked to poor outcomes in the cohort and to assess the mental health status of the population.
The study relied on a retrospective chart review for the 17 patients at the University of Mississippi Medical Center and on Childhood Arthritis and Rheumatology Research Alliance registry data for the 19 patients at the University of Alabama at Birmingham. Most of the patients (86%) were female, Black (78%), and insured by Medicaid (64%). The average age at diagnosis was 13 years. Most (83%) also lived in a ZIP code that met the criteria for a medium-high or high Social Vulnerability Index. The children had to travel an average 75 miles to see a rheumatologist, compared with the national average of 43 miles.
At diagnosis, their average Systemic Lupus International Collaborating Clinics (SLICC) score was 8.8, their average American College of Rheumatology score was 5.2, and their average SLEDAI score was 12.1 – the latter was substantially higher than the average 3.1 score in a multiethnic Canadian cohort (the 1000 Canadian Faces of Lupus Study) with 10% Black children (P < .00001). The SLEDAI score dropped to 6.8 at 6 months and to 4 at 1 year. Nearly half (47%) had a SLICC Damage Index (SDI) greater than 0, and one-third had an SDI of 2 or greater, compared with 16% and 7%, respectively, reported in other recent studies (P < .0001 for both).
“These disparities are very difficult to investigate in terms of causal relationships and [are] likely to be very modifiable,” Coziana Ciurtin, MD, PhD, associate professor of rheumatology at University College London, told this news organization. “I think the socioeconomic status, the level of education, poverty, [type of] medical insurance, and probably genetic variants are all underpinning the presentation, damage, or disease activity being very high, and also organ involvement,” such as the greater CNS involvement seen in non-White patients.
Being mindful of these risk profiles can help doctors in asking about patients’ support at home and their families’ education, beliefs, and cultural practices, Dr. Ciurtin added. “Helping them to engage and be involved in decision-making is probably the most important” aspect of learning this information about families, she said.
Collecting this information should not be the sole responsibility of the physician, added Eve Smith, PhD, MBCHB, an academic clinical lecturer at the University of Liverpool, England, who attended the presentations. Dr. Smith noted a discussion in a work group during the previous day of the conference concerning questionnaires for screening patients regarding the need for social services and for identifying areas in which patients and their families were having difficulties.
“Obviously, if you’re going to do that, you have to have access to someone who can actually help to deal with that. Some hospitals have patient navigators that can help, for example, with a food security issue to highlight resources within the community, so it’s not all on the doctor,” Dr. Smith said. “To really make a difference in this area, it can’t just be down to the doctor. There needs to be social care, there needs to be community-based interventions and things to do about it. Doctors can help identify these patients, or maybe somebody in the [medical] team can help with that, but there needs to be an intervention. Otherwise, you’re left with this problem without a solution that you can’t do anything about.”
The researchers did not note any external funding for either study. Dr. Beil, Dr. Dhanrajani, Dr. Smith, and Dr. Ciurtin reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
NEW ORLEANS – The sociodemographic characteristics of Black and Hispanic children with systemic lupus erythematosus (SLE) appear to play a strong role in influencing the severity of disease in these patients, according to two studies presented at the Pediatric Rheumatology Symposium.
One study showed an association between multiple determinants of health and disease severity among children seen in a large Texas city, and a separate descriptive cross-sectional cohort study of predominantly Black children at two centers in Mississippi and Alabama reinforced the finding of greater severity of disease and social hardships among this racial group.
The findings from both studies supplement existing evidence that the prevalence of childhood-onset SLE is greater among Black and Hispanic children.
“Several demographic and social determinants of health parameters influenced disease severity at levels that reached statistical significance, including insurance status, race/ethnicity, referral source, PCP [primary care provider] availability, primary language, and transportation needs,” Emily Beil, MD, a pediatric rheumatologist at Texas Children’s Hospital in Houston, told attendees at the conference, which was sponsored by the American College of Rheumatology. Her team’s goal, she said, was to “better understand our patient population and social disparities that contribute to disease severity.”
Dr. Beil and her colleagues conducted a retrospective review of 136 children who had been diagnosed with childhood-onset SLE between January 2018 and May 2022 at Texas Children’s Hospital. Only children who were younger than 18 years at the time of diagnosis at Texas Children’s were included. The analysis considered demographics, clinical characteristics, insurance status, social work consultation, access to a primary care provider, transportation needs, primary language, and other parameters related to social determinants of health.
The average age of the patients was 13 years, and most were girls (82%). Just over half were Hispanic (53%), and just over a quarter were Black (26%). Half had Medicaid or participated in the Children’s Health Insurance Program (CHIP), and 1 in 10 were uninsured (10%). Half the diagnoses were made during an inpatient admission; 36% were made on the floor, and 14% were made in the intensive care unit (ICU).
The average Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score was 12.5, and 48.5% of patients had severe disease, indicated by a score of at least 12. Only two in three children were documented as having a primary care physician (66%), and 32% preferred a language other than English. Most of the children (80%) had a social work consult.
Black and biracial children had higher SLEDAI scores at presentation. Non-Hispanic White children were less likely to have a social work consult, compared with other racial/ethnic groups (P = .01 for both). Central nervous system involvement was most prevalent among Black patients (P = .004). Cyclophosphamide was used most often for Black and biracial patients.
Uninsured patients were most likely to be diagnosed on an inpatient floor. The highest proportion of ICU admissions was among patients insured by Medicaid (P = .034). Average SLEDAI scores were highest among uninsured patients, followed by Medicaid patients. More than half of the patients who did not have insurance lacked access to a regular primary care provider, compared with 12% of Medicaid patients and 7% of privately insured patients (P = .001). All the uninsured patients had transportation needs, which was a significantly higher rate than among those with Medicaid (13%) or private insurance (15%) (P = .001). The highest percentage of social work consults was among patients who were insured by Medicaid or were without insurance (P = .001).
Salient demographics and clinical features
In the second presentation, Anita Dhanrajani, MD, assistant professor of pediatrics at the University of Mississippi Medical Center in Jackson, began by noting that Alabama and Mississippi are ranked in the top 10 states for the highest poverty rate: Mississippi is No. 1, and Alabama is No. 7. Further, 40% of children in Mississippi and 29% of children in Alabama are of African American ancestry, she said.
“So, we know that this population that we’re dealing with has several high-risk factors that can lead them to have poor outcomes, and yet, we haven’t really ever characterized their clinical features or their social demographic features,” Dr. Dhanrajani told attendees. “My hope is that with this very miniscule first step, we’re able to move towards solutions to decrease health care disparities in this population.”
She presented findings regarding the first of three aims in the study, which was to describe the baseline clinical, demographic, and socioeconomic profiles of childhood lupus patients at the two centers. The two other aims were to examine genetic factors potentially linked to poor outcomes in the cohort and to assess the mental health status of the population.
The study relied on a retrospective chart review for the 17 patients at the University of Mississippi Medical Center and on Childhood Arthritis and Rheumatology Research Alliance registry data for the 19 patients at the University of Alabama at Birmingham. Most of the patients (86%) were female, Black (78%), and insured by Medicaid (64%). The average age at diagnosis was 13 years. Most (83%) also lived in a ZIP code that met the criteria for a medium-high or high Social Vulnerability Index. The children had to travel an average 75 miles to see a rheumatologist, compared with the national average of 43 miles.
At diagnosis, their average Systemic Lupus International Collaborating Clinics (SLICC) score was 8.8, their average American College of Rheumatology score was 5.2, and their average SLEDAI score was 12.1 – the latter was substantially higher than the average 3.1 score in a multiethnic Canadian cohort (the 1000 Canadian Faces of Lupus Study) with 10% Black children (P < .00001). The SLEDAI score dropped to 6.8 at 6 months and to 4 at 1 year. Nearly half (47%) had a SLICC Damage Index (SDI) greater than 0, and one-third had an SDI of 2 or greater, compared with 16% and 7%, respectively, reported in other recent studies (P < .0001 for both).
“These disparities are very difficult to investigate in terms of causal relationships and [are] likely to be very modifiable,” Coziana Ciurtin, MD, PhD, associate professor of rheumatology at University College London, told this news organization. “I think the socioeconomic status, the level of education, poverty, [type of] medical insurance, and probably genetic variants are all underpinning the presentation, damage, or disease activity being very high, and also organ involvement,” such as the greater CNS involvement seen in non-White patients.
Being mindful of these risk profiles can help doctors in asking about patients’ support at home and their families’ education, beliefs, and cultural practices, Dr. Ciurtin added. “Helping them to engage and be involved in decision-making is probably the most important” aspect of learning this information about families, she said.
Collecting this information should not be the sole responsibility of the physician, added Eve Smith, PhD, MBCHB, an academic clinical lecturer at the University of Liverpool, England, who attended the presentations. Dr. Smith noted a discussion in a work group during the previous day of the conference concerning questionnaires for screening patients regarding the need for social services and for identifying areas in which patients and their families were having difficulties.
“Obviously, if you’re going to do that, you have to have access to someone who can actually help to deal with that. Some hospitals have patient navigators that can help, for example, with a food security issue to highlight resources within the community, so it’s not all on the doctor,” Dr. Smith said. “To really make a difference in this area, it can’t just be down to the doctor. There needs to be social care, there needs to be community-based interventions and things to do about it. Doctors can help identify these patients, or maybe somebody in the [medical] team can help with that, but there needs to be an intervention. Otherwise, you’re left with this problem without a solution that you can’t do anything about.”
The researchers did not note any external funding for either study. Dr. Beil, Dr. Dhanrajani, Dr. Smith, and Dr. Ciurtin reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
NEW ORLEANS – The sociodemographic characteristics of Black and Hispanic children with systemic lupus erythematosus (SLE) appear to play a strong role in influencing the severity of disease in these patients, according to two studies presented at the Pediatric Rheumatology Symposium.
One study showed an association between multiple determinants of health and disease severity among children seen in a large Texas city, and a separate descriptive cross-sectional cohort study of predominantly Black children at two centers in Mississippi and Alabama reinforced the finding of greater severity of disease and social hardships among this racial group.
The findings from both studies supplement existing evidence that the prevalence of childhood-onset SLE is greater among Black and Hispanic children.
“Several demographic and social determinants of health parameters influenced disease severity at levels that reached statistical significance, including insurance status, race/ethnicity, referral source, PCP [primary care provider] availability, primary language, and transportation needs,” Emily Beil, MD, a pediatric rheumatologist at Texas Children’s Hospital in Houston, told attendees at the conference, which was sponsored by the American College of Rheumatology. Her team’s goal, she said, was to “better understand our patient population and social disparities that contribute to disease severity.”
Dr. Beil and her colleagues conducted a retrospective review of 136 children who had been diagnosed with childhood-onset SLE between January 2018 and May 2022 at Texas Children’s Hospital. Only children who were younger than 18 years at the time of diagnosis at Texas Children’s were included. The analysis considered demographics, clinical characteristics, insurance status, social work consultation, access to a primary care provider, transportation needs, primary language, and other parameters related to social determinants of health.
The average age of the patients was 13 years, and most were girls (82%). Just over half were Hispanic (53%), and just over a quarter were Black (26%). Half had Medicaid or participated in the Children’s Health Insurance Program (CHIP), and 1 in 10 were uninsured (10%). Half the diagnoses were made during an inpatient admission; 36% were made on the floor, and 14% were made in the intensive care unit (ICU).
The average Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score was 12.5, and 48.5% of patients had severe disease, indicated by a score of at least 12. Only two in three children were documented as having a primary care physician (66%), and 32% preferred a language other than English. Most of the children (80%) had a social work consult.
Black and biracial children had higher SLEDAI scores at presentation. Non-Hispanic White children were less likely to have a social work consult, compared with other racial/ethnic groups (P = .01 for both). Central nervous system involvement was most prevalent among Black patients (P = .004). Cyclophosphamide was used most often for Black and biracial patients.
Uninsured patients were most likely to be diagnosed on an inpatient floor. The highest proportion of ICU admissions was among patients insured by Medicaid (P = .034). Average SLEDAI scores were highest among uninsured patients, followed by Medicaid patients. More than half of the patients who did not have insurance lacked access to a regular primary care provider, compared with 12% of Medicaid patients and 7% of privately insured patients (P = .001). All the uninsured patients had transportation needs, which was a significantly higher rate than among those with Medicaid (13%) or private insurance (15%) (P = .001). The highest percentage of social work consults was among patients who were insured by Medicaid or were without insurance (P = .001).
Salient demographics and clinical features
In the second presentation, Anita Dhanrajani, MD, assistant professor of pediatrics at the University of Mississippi Medical Center in Jackson, began by noting that Alabama and Mississippi are ranked in the top 10 states for the highest poverty rate: Mississippi is No. 1, and Alabama is No. 7. Further, 40% of children in Mississippi and 29% of children in Alabama are of African American ancestry, she said.
“So, we know that this population that we’re dealing with has several high-risk factors that can lead them to have poor outcomes, and yet, we haven’t really ever characterized their clinical features or their social demographic features,” Dr. Dhanrajani told attendees. “My hope is that with this very miniscule first step, we’re able to move towards solutions to decrease health care disparities in this population.”
She presented findings regarding the first of three aims in the study, which was to describe the baseline clinical, demographic, and socioeconomic profiles of childhood lupus patients at the two centers. The two other aims were to examine genetic factors potentially linked to poor outcomes in the cohort and to assess the mental health status of the population.
The study relied on a retrospective chart review for the 17 patients at the University of Mississippi Medical Center and on Childhood Arthritis and Rheumatology Research Alliance registry data for the 19 patients at the University of Alabama at Birmingham. Most of the patients (86%) were female, Black (78%), and insured by Medicaid (64%). The average age at diagnosis was 13 years. Most (83%) also lived in a ZIP code that met the criteria for a medium-high or high Social Vulnerability Index. The children had to travel an average 75 miles to see a rheumatologist, compared with the national average of 43 miles.
At diagnosis, their average Systemic Lupus International Collaborating Clinics (SLICC) score was 8.8, their average American College of Rheumatology score was 5.2, and their average SLEDAI score was 12.1 – the latter was substantially higher than the average 3.1 score in a multiethnic Canadian cohort (the 1000 Canadian Faces of Lupus Study) with 10% Black children (P < .00001). The SLEDAI score dropped to 6.8 at 6 months and to 4 at 1 year. Nearly half (47%) had a SLICC Damage Index (SDI) greater than 0, and one-third had an SDI of 2 or greater, compared with 16% and 7%, respectively, reported in other recent studies (P < .0001 for both).
“These disparities are very difficult to investigate in terms of causal relationships and [are] likely to be very modifiable,” Coziana Ciurtin, MD, PhD, associate professor of rheumatology at University College London, told this news organization. “I think the socioeconomic status, the level of education, poverty, [type of] medical insurance, and probably genetic variants are all underpinning the presentation, damage, or disease activity being very high, and also organ involvement,” such as the greater CNS involvement seen in non-White patients.
Being mindful of these risk profiles can help doctors in asking about patients’ support at home and their families’ education, beliefs, and cultural practices, Dr. Ciurtin added. “Helping them to engage and be involved in decision-making is probably the most important” aspect of learning this information about families, she said.
Collecting this information should not be the sole responsibility of the physician, added Eve Smith, PhD, MBCHB, an academic clinical lecturer at the University of Liverpool, England, who attended the presentations. Dr. Smith noted a discussion in a work group during the previous day of the conference concerning questionnaires for screening patients regarding the need for social services and for identifying areas in which patients and their families were having difficulties.
“Obviously, if you’re going to do that, you have to have access to someone who can actually help to deal with that. Some hospitals have patient navigators that can help, for example, with a food security issue to highlight resources within the community, so it’s not all on the doctor,” Dr. Smith said. “To really make a difference in this area, it can’t just be down to the doctor. There needs to be social care, there needs to be community-based interventions and things to do about it. Doctors can help identify these patients, or maybe somebody in the [medical] team can help with that, but there needs to be an intervention. Otherwise, you’re left with this problem without a solution that you can’t do anything about.”
The researchers did not note any external funding for either study. Dr. Beil, Dr. Dhanrajani, Dr. Smith, and Dr. Ciurtin reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT PRSYM 2023
Little change in rheumatology faculty coverage in pediatric residency programs in nearly 20 years
NEW ORLEANS – More than one-third of pediatric residency programs do not have a pediatric rheumatologist on faculty, a situation that has changed little since 2004, according to a poster presented at the Pediatric Rheumatology Symposium 2023 conference.
“This shortage has significant downstream effects,” according to author Miriah Gillispie-Taylor, MD, an assistant professor of pediatric rheumatology at Baylor College of Medicine and Texas Children’s Hospital in Houston. Without adequate education, it’s unreasonable to expect that a pediatrician will recognize the great diversity of presentations among rheumatic diseases, for example. “Without recognition, patients are not referred in a timely manner, and earlier identification and treatment of rheumatic diseases leads to improved outcomes,” Dr. Gillispie-Taylor said.
Currently, eight U.S. states do not have a board-certified pediatric rheumatologist, including Alaska. Dr. Gillispie-Taylor cited a 2006 study that found that one-third of medical schools (33%) and 40% of U.S. pediatric residency programs did not have an on-site pediatric rheumatologist in 2004.
As the long-standing workforce shortage in pediatric rheumatology continues, Dr. Gillispie-Taylor and her colleagues investigated whether increasing awareness of this problem has influenced the number of United States and Puerto Rico residency training programs with pediatric rheumatology faculty from 2004 to present.
The researchers identified 212 pediatric residency programs accredited by the Accreditation Council for Graduate Medical Education for 2022-2023 and reviewed their program website to see which ones had affiliated pediatric rheumatology faculty. After determining the faculty from the website for 85% of the programs, the researchers emailed the other programs to find out whether a pediatric rheumatologist was on faculty, filling out another 6% of the programs. Most of the remaining uncategorized programs (7%) were categorized at a meeting of the Childhood Arthritis and Rheumatology Research Alliance medical education workgroup. Only 2% of programs could not be ultimately categorized.
The region with the greatest proportion of pediatric residency programs that had a pediatric rheumatologist was the Southeast, where 95% (36 of 38 programs) of programs had one on faculty. The Southwest, comprising Texas, Oklahoma, New Mexico, and Arizona, had the lowest proportion: 43% (9 of 21 programs). For the other regions, 69% of the West/Pacific Northwest (18 of 26), 62% of the Midwest (28 of 45), and 61% of the Northeast (39 of 64) programs had a pediatric rheumatologist on faculty. Three of Puerto Rico’s four programs had one as well.
Overall, 63% of programs had a pediatric rheumatologist on faculty, and 36% did not; the state of three programs was unknown.
The large proportion of programs without a pediatric rheumatologist “limits exposure to rheumatologic conditions and learning opportunities during residency and contribute to declining fellow match rates,” the authors concluded. They noted that only 62.8% of pediatric rheumatology fellowship positions were filled in 2022, down slightly from the 69.2% filled in 2021, according to report data from the National Matching Resident Program.
The researchers acknowledged that their results could be skewed if website information was outdated for any programs, and it’s difficult to determine which programs might lack resources on the basis of only publicly available information. Though programs without pediatric rheumatologists might benefit from visiting professorships, it can be difficult to identify which ones, they added.
The authors recommend two next steps: one, establishing areas of essential knowledge in pediatric rheumatology to enable the creation of learning objectives so programs can focus their educational efforts; and two, continuing efforts to understand residents’ motivation to pursue fellowships in pediatric rheumatology for the purpose of improving recruitment.
Two medical students at Dr. Gillispie-Taylor’s institution spoke with this news organization about their thoughts on the findings and how they were approaching their own career goals in medicine in light of these findings.
Kyla Fergason, a second-year medical student at Baylor College of Medicine, said that she thinks she wants to pursue pediatrics or meds-peds. Though she’s not sure whether she specifically wants to pursue pediatric rheumatology, she is very interested in the area and said that she has learned much from the Pediatric Rheumatology Symposium conference. She found the dearth of pediatric rheumatology faculty at residency programs worrisome, particularly in states like Alaska and Hawaii because they aren’t contiguous with the rest of the United States. Only three pediatric rheumatologists are practicing in Hawaii.
“It’s really concerning that sometimes there is not any rheumatologist there to see the patient,” Ms. Fergason told this news organization. “These are diseases that affect people chronically throughout their entire lives, so it’s definitely concerning to think that, at a time when they could be helped and there could be interventions made, none are made because there’s just no one available.”
Kristiana Nasto, a third-year medical student at Baylor College of Medicine, is similarly interested in pediatrics but leaning more toward meds-peds and has an interest in rheumatology as well. She was surprised at how many programs had no pediatric rheumatologist on faculty because Baylor has a robust program.
“I was not aware of the fact that other states or other parts of Texas do not have the luxury of the great rheumatologists that we have at Baylor College of Medicine,” Ms. Nasto said. “That can definitely impact care for many patients because some of these rheumatologic diseases are so unique and challenging to treat that they require specialized care, so it makes me a bit sad that this is the case.”
Dr. Gillispie-Taylor has received an educational grant from Pfizer. Ms. Fergason and Ms. Nasto had no disclosures. No external funding was noted for the study.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – More than one-third of pediatric residency programs do not have a pediatric rheumatologist on faculty, a situation that has changed little since 2004, according to a poster presented at the Pediatric Rheumatology Symposium 2023 conference.
“This shortage has significant downstream effects,” according to author Miriah Gillispie-Taylor, MD, an assistant professor of pediatric rheumatology at Baylor College of Medicine and Texas Children’s Hospital in Houston. Without adequate education, it’s unreasonable to expect that a pediatrician will recognize the great diversity of presentations among rheumatic diseases, for example. “Without recognition, patients are not referred in a timely manner, and earlier identification and treatment of rheumatic diseases leads to improved outcomes,” Dr. Gillispie-Taylor said.
Currently, eight U.S. states do not have a board-certified pediatric rheumatologist, including Alaska. Dr. Gillispie-Taylor cited a 2006 study that found that one-third of medical schools (33%) and 40% of U.S. pediatric residency programs did not have an on-site pediatric rheumatologist in 2004.
As the long-standing workforce shortage in pediatric rheumatology continues, Dr. Gillispie-Taylor and her colleagues investigated whether increasing awareness of this problem has influenced the number of United States and Puerto Rico residency training programs with pediatric rheumatology faculty from 2004 to present.
The researchers identified 212 pediatric residency programs accredited by the Accreditation Council for Graduate Medical Education for 2022-2023 and reviewed their program website to see which ones had affiliated pediatric rheumatology faculty. After determining the faculty from the website for 85% of the programs, the researchers emailed the other programs to find out whether a pediatric rheumatologist was on faculty, filling out another 6% of the programs. Most of the remaining uncategorized programs (7%) were categorized at a meeting of the Childhood Arthritis and Rheumatology Research Alliance medical education workgroup. Only 2% of programs could not be ultimately categorized.
The region with the greatest proportion of pediatric residency programs that had a pediatric rheumatologist was the Southeast, where 95% (36 of 38 programs) of programs had one on faculty. The Southwest, comprising Texas, Oklahoma, New Mexico, and Arizona, had the lowest proportion: 43% (9 of 21 programs). For the other regions, 69% of the West/Pacific Northwest (18 of 26), 62% of the Midwest (28 of 45), and 61% of the Northeast (39 of 64) programs had a pediatric rheumatologist on faculty. Three of Puerto Rico’s four programs had one as well.
Overall, 63% of programs had a pediatric rheumatologist on faculty, and 36% did not; the state of three programs was unknown.
The large proportion of programs without a pediatric rheumatologist “limits exposure to rheumatologic conditions and learning opportunities during residency and contribute to declining fellow match rates,” the authors concluded. They noted that only 62.8% of pediatric rheumatology fellowship positions were filled in 2022, down slightly from the 69.2% filled in 2021, according to report data from the National Matching Resident Program.
The researchers acknowledged that their results could be skewed if website information was outdated for any programs, and it’s difficult to determine which programs might lack resources on the basis of only publicly available information. Though programs without pediatric rheumatologists might benefit from visiting professorships, it can be difficult to identify which ones, they added.
The authors recommend two next steps: one, establishing areas of essential knowledge in pediatric rheumatology to enable the creation of learning objectives so programs can focus their educational efforts; and two, continuing efforts to understand residents’ motivation to pursue fellowships in pediatric rheumatology for the purpose of improving recruitment.
Two medical students at Dr. Gillispie-Taylor’s institution spoke with this news organization about their thoughts on the findings and how they were approaching their own career goals in medicine in light of these findings.
Kyla Fergason, a second-year medical student at Baylor College of Medicine, said that she thinks she wants to pursue pediatrics or meds-peds. Though she’s not sure whether she specifically wants to pursue pediatric rheumatology, she is very interested in the area and said that she has learned much from the Pediatric Rheumatology Symposium conference. She found the dearth of pediatric rheumatology faculty at residency programs worrisome, particularly in states like Alaska and Hawaii because they aren’t contiguous with the rest of the United States. Only three pediatric rheumatologists are practicing in Hawaii.
“It’s really concerning that sometimes there is not any rheumatologist there to see the patient,” Ms. Fergason told this news organization. “These are diseases that affect people chronically throughout their entire lives, so it’s definitely concerning to think that, at a time when they could be helped and there could be interventions made, none are made because there’s just no one available.”
Kristiana Nasto, a third-year medical student at Baylor College of Medicine, is similarly interested in pediatrics but leaning more toward meds-peds and has an interest in rheumatology as well. She was surprised at how many programs had no pediatric rheumatologist on faculty because Baylor has a robust program.
“I was not aware of the fact that other states or other parts of Texas do not have the luxury of the great rheumatologists that we have at Baylor College of Medicine,” Ms. Nasto said. “That can definitely impact care for many patients because some of these rheumatologic diseases are so unique and challenging to treat that they require specialized care, so it makes me a bit sad that this is the case.”
Dr. Gillispie-Taylor has received an educational grant from Pfizer. Ms. Fergason and Ms. Nasto had no disclosures. No external funding was noted for the study.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – More than one-third of pediatric residency programs do not have a pediatric rheumatologist on faculty, a situation that has changed little since 2004, according to a poster presented at the Pediatric Rheumatology Symposium 2023 conference.
“This shortage has significant downstream effects,” according to author Miriah Gillispie-Taylor, MD, an assistant professor of pediatric rheumatology at Baylor College of Medicine and Texas Children’s Hospital in Houston. Without adequate education, it’s unreasonable to expect that a pediatrician will recognize the great diversity of presentations among rheumatic diseases, for example. “Without recognition, patients are not referred in a timely manner, and earlier identification and treatment of rheumatic diseases leads to improved outcomes,” Dr. Gillispie-Taylor said.
Currently, eight U.S. states do not have a board-certified pediatric rheumatologist, including Alaska. Dr. Gillispie-Taylor cited a 2006 study that found that one-third of medical schools (33%) and 40% of U.S. pediatric residency programs did not have an on-site pediatric rheumatologist in 2004.
As the long-standing workforce shortage in pediatric rheumatology continues, Dr. Gillispie-Taylor and her colleagues investigated whether increasing awareness of this problem has influenced the number of United States and Puerto Rico residency training programs with pediatric rheumatology faculty from 2004 to present.
The researchers identified 212 pediatric residency programs accredited by the Accreditation Council for Graduate Medical Education for 2022-2023 and reviewed their program website to see which ones had affiliated pediatric rheumatology faculty. After determining the faculty from the website for 85% of the programs, the researchers emailed the other programs to find out whether a pediatric rheumatologist was on faculty, filling out another 6% of the programs. Most of the remaining uncategorized programs (7%) were categorized at a meeting of the Childhood Arthritis and Rheumatology Research Alliance medical education workgroup. Only 2% of programs could not be ultimately categorized.
The region with the greatest proportion of pediatric residency programs that had a pediatric rheumatologist was the Southeast, where 95% (36 of 38 programs) of programs had one on faculty. The Southwest, comprising Texas, Oklahoma, New Mexico, and Arizona, had the lowest proportion: 43% (9 of 21 programs). For the other regions, 69% of the West/Pacific Northwest (18 of 26), 62% of the Midwest (28 of 45), and 61% of the Northeast (39 of 64) programs had a pediatric rheumatologist on faculty. Three of Puerto Rico’s four programs had one as well.
Overall, 63% of programs had a pediatric rheumatologist on faculty, and 36% did not; the state of three programs was unknown.
The large proportion of programs without a pediatric rheumatologist “limits exposure to rheumatologic conditions and learning opportunities during residency and contribute to declining fellow match rates,” the authors concluded. They noted that only 62.8% of pediatric rheumatology fellowship positions were filled in 2022, down slightly from the 69.2% filled in 2021, according to report data from the National Matching Resident Program.
The researchers acknowledged that their results could be skewed if website information was outdated for any programs, and it’s difficult to determine which programs might lack resources on the basis of only publicly available information. Though programs without pediatric rheumatologists might benefit from visiting professorships, it can be difficult to identify which ones, they added.
The authors recommend two next steps: one, establishing areas of essential knowledge in pediatric rheumatology to enable the creation of learning objectives so programs can focus their educational efforts; and two, continuing efforts to understand residents’ motivation to pursue fellowships in pediatric rheumatology for the purpose of improving recruitment.
Two medical students at Dr. Gillispie-Taylor’s institution spoke with this news organization about their thoughts on the findings and how they were approaching their own career goals in medicine in light of these findings.
Kyla Fergason, a second-year medical student at Baylor College of Medicine, said that she thinks she wants to pursue pediatrics or meds-peds. Though she’s not sure whether she specifically wants to pursue pediatric rheumatology, she is very interested in the area and said that she has learned much from the Pediatric Rheumatology Symposium conference. She found the dearth of pediatric rheumatology faculty at residency programs worrisome, particularly in states like Alaska and Hawaii because they aren’t contiguous with the rest of the United States. Only three pediatric rheumatologists are practicing in Hawaii.
“It’s really concerning that sometimes there is not any rheumatologist there to see the patient,” Ms. Fergason told this news organization. “These are diseases that affect people chronically throughout their entire lives, so it’s definitely concerning to think that, at a time when they could be helped and there could be interventions made, none are made because there’s just no one available.”
Kristiana Nasto, a third-year medical student at Baylor College of Medicine, is similarly interested in pediatrics but leaning more toward meds-peds and has an interest in rheumatology as well. She was surprised at how many programs had no pediatric rheumatologist on faculty because Baylor has a robust program.
“I was not aware of the fact that other states or other parts of Texas do not have the luxury of the great rheumatologists that we have at Baylor College of Medicine,” Ms. Nasto said. “That can definitely impact care for many patients because some of these rheumatologic diseases are so unique and challenging to treat that they require specialized care, so it makes me a bit sad that this is the case.”
Dr. Gillispie-Taylor has received an educational grant from Pfizer. Ms. Fergason and Ms. Nasto had no disclosures. No external funding was noted for the study.
A version of this article first appeared on Medscape.com.
AT PRSYM 2023
Clonidine: Off-label uses in pediatric patients
Clonidine is a centrally acting alpha-2 agonist originally developed for treating hypertension. It is believed to work by stimulating alpha-2 receptors in various areas of the brain. It is nonselective, binding alpha-2A, -2B, and -2C receptors, and mediates inattentiveness, hyperactivity, impulsivity, sedation, and hypotension.1 Clonidine is available as immediate-release (IR), extended-release, and patch formulations, with typical doses ranging from 0.1 to 0.4 mg/d. The most common adverse effects are anticholinergic, such as sedation, dry mouth, and constipation. Since clonidine is effective at lowering blood pressure, the main safety concern is the possibility of rebound hypertension if abruptly stopped, which necessitates a short taper period.1
In child and adolescent psychiatry, the only FDA-approved use of clonidine is for treating attention-deficit/hyperactivity disorder (ADHD). Yet this medication has been increasingly used off-label for several common psychiatric ailments in pediatric patients. In this article, we discuss potential uses of clonidine in child and adolescent psychiatry; except for ADHD, all uses we describe are off-label.
ADHD. Clonidine is effective both as a monotherapy and as an adjunctive therapy to stimulants for pediatric ADHD. When used alone, clonidine is better suited for patients who have hyperactivity as their primary concern, whereas stimulants may be better suited for patients with inattentive subtypes. It also can help reduce sleep disturbances associated with the use of stimulants, especially insomnia.1
Tics/Tourette syndrome. Clonidine is a first-line treatment for tics in Tourette syndrome, demonstrating high efficacy with limited or no adverse effects. Furthermore, ADHD is the most common comorbid condition in patients with dystonic tics, which makes clonidine useful for simultaneously treating both conditions.2
Insomnia. Currently, there are no FDA-approved medications for treating sleep disorders in children and adolescents. However, clonidine is among the most used medications for childhood sleep difficulties, second only to antihistamines. The IR formulation is often preferred for this indication due to increased sedation.3
Posttraumatic stress disorder (PTSD). Research has shown clonidine can help reduce hyperarousal symptoms, address sleep difficulties, and reduce PTSD trauma nightmares, anxiety, and irritability.4
Substance detoxification. Clonidine successfully suppresses opiate withdrawal signs and symptoms by reducing sympathetic overactivity. It can help with alcohol withdrawal and smoking cessation.2
Antipsychotic-induced akathisia. Controlled trials have shown that clonidine significantly reduces akathisia associated with the use of antipsychotics.2
Sialorrhea. Due to its anticholinergic effects, clonidine can effectively reduce antipsychotic-induced hypersalivation.2
Behavioral disturbances. Due to its sedative and anti-impulsive properties, clonidine can be used to address broadly defined behavioral issues, including anxiety-related behaviors, aggression, and agitation, although there is a lack of proven efficacy.1,2,4
1. Stahl SM, Grady MM, Muntner N. Stahl’s Essential Psychopharmacology: Prescriber’s Guide: Children and Adolescents. Cambridge University Press; 2019.
2. Naguy A. Clonidine use in psychiatry: panacea or panache. Pharmacology. 2016;98(1-2):87-92. doi:10.1159/000446441
3. Jang YJ, Choi H, Han TS, et al. Effectiveness of clonidine in child and adolescent sleep disorders. Psychiatry Investig. 2022;19(9):738-747. doi:10.30773/pi.2022.0117
4. Bajor LA, Balsara C, Osser DN. An evidence-based approach to psychopharmacology for posttraumatic stress disorder (PTSD) - 2022 update. Psychiatry Res. 2022;317:114840. doi:10.1016/j.psychres.2022.114840
Clonidine is a centrally acting alpha-2 agonist originally developed for treating hypertension. It is believed to work by stimulating alpha-2 receptors in various areas of the brain. It is nonselective, binding alpha-2A, -2B, and -2C receptors, and mediates inattentiveness, hyperactivity, impulsivity, sedation, and hypotension.1 Clonidine is available as immediate-release (IR), extended-release, and patch formulations, with typical doses ranging from 0.1 to 0.4 mg/d. The most common adverse effects are anticholinergic, such as sedation, dry mouth, and constipation. Since clonidine is effective at lowering blood pressure, the main safety concern is the possibility of rebound hypertension if abruptly stopped, which necessitates a short taper period.1
In child and adolescent psychiatry, the only FDA-approved use of clonidine is for treating attention-deficit/hyperactivity disorder (ADHD). Yet this medication has been increasingly used off-label for several common psychiatric ailments in pediatric patients. In this article, we discuss potential uses of clonidine in child and adolescent psychiatry; except for ADHD, all uses we describe are off-label.
ADHD. Clonidine is effective both as a monotherapy and as an adjunctive therapy to stimulants for pediatric ADHD. When used alone, clonidine is better suited for patients who have hyperactivity as their primary concern, whereas stimulants may be better suited for patients with inattentive subtypes. It also can help reduce sleep disturbances associated with the use of stimulants, especially insomnia.1
Tics/Tourette syndrome. Clonidine is a first-line treatment for tics in Tourette syndrome, demonstrating high efficacy with limited or no adverse effects. Furthermore, ADHD is the most common comorbid condition in patients with dystonic tics, which makes clonidine useful for simultaneously treating both conditions.2
Insomnia. Currently, there are no FDA-approved medications for treating sleep disorders in children and adolescents. However, clonidine is among the most used medications for childhood sleep difficulties, second only to antihistamines. The IR formulation is often preferred for this indication due to increased sedation.3
Posttraumatic stress disorder (PTSD). Research has shown clonidine can help reduce hyperarousal symptoms, address sleep difficulties, and reduce PTSD trauma nightmares, anxiety, and irritability.4
Substance detoxification. Clonidine successfully suppresses opiate withdrawal signs and symptoms by reducing sympathetic overactivity. It can help with alcohol withdrawal and smoking cessation.2
Antipsychotic-induced akathisia. Controlled trials have shown that clonidine significantly reduces akathisia associated with the use of antipsychotics.2
Sialorrhea. Due to its anticholinergic effects, clonidine can effectively reduce antipsychotic-induced hypersalivation.2
Behavioral disturbances. Due to its sedative and anti-impulsive properties, clonidine can be used to address broadly defined behavioral issues, including anxiety-related behaviors, aggression, and agitation, although there is a lack of proven efficacy.1,2,4
Clonidine is a centrally acting alpha-2 agonist originally developed for treating hypertension. It is believed to work by stimulating alpha-2 receptors in various areas of the brain. It is nonselective, binding alpha-2A, -2B, and -2C receptors, and mediates inattentiveness, hyperactivity, impulsivity, sedation, and hypotension.1 Clonidine is available as immediate-release (IR), extended-release, and patch formulations, with typical doses ranging from 0.1 to 0.4 mg/d. The most common adverse effects are anticholinergic, such as sedation, dry mouth, and constipation. Since clonidine is effective at lowering blood pressure, the main safety concern is the possibility of rebound hypertension if abruptly stopped, which necessitates a short taper period.1
In child and adolescent psychiatry, the only FDA-approved use of clonidine is for treating attention-deficit/hyperactivity disorder (ADHD). Yet this medication has been increasingly used off-label for several common psychiatric ailments in pediatric patients. In this article, we discuss potential uses of clonidine in child and adolescent psychiatry; except for ADHD, all uses we describe are off-label.
ADHD. Clonidine is effective both as a monotherapy and as an adjunctive therapy to stimulants for pediatric ADHD. When used alone, clonidine is better suited for patients who have hyperactivity as their primary concern, whereas stimulants may be better suited for patients with inattentive subtypes. It also can help reduce sleep disturbances associated with the use of stimulants, especially insomnia.1
Tics/Tourette syndrome. Clonidine is a first-line treatment for tics in Tourette syndrome, demonstrating high efficacy with limited or no adverse effects. Furthermore, ADHD is the most common comorbid condition in patients with dystonic tics, which makes clonidine useful for simultaneously treating both conditions.2
Insomnia. Currently, there are no FDA-approved medications for treating sleep disorders in children and adolescents. However, clonidine is among the most used medications for childhood sleep difficulties, second only to antihistamines. The IR formulation is often preferred for this indication due to increased sedation.3
Posttraumatic stress disorder (PTSD). Research has shown clonidine can help reduce hyperarousal symptoms, address sleep difficulties, and reduce PTSD trauma nightmares, anxiety, and irritability.4
Substance detoxification. Clonidine successfully suppresses opiate withdrawal signs and symptoms by reducing sympathetic overactivity. It can help with alcohol withdrawal and smoking cessation.2
Antipsychotic-induced akathisia. Controlled trials have shown that clonidine significantly reduces akathisia associated with the use of antipsychotics.2
Sialorrhea. Due to its anticholinergic effects, clonidine can effectively reduce antipsychotic-induced hypersalivation.2
Behavioral disturbances. Due to its sedative and anti-impulsive properties, clonidine can be used to address broadly defined behavioral issues, including anxiety-related behaviors, aggression, and agitation, although there is a lack of proven efficacy.1,2,4
1. Stahl SM, Grady MM, Muntner N. Stahl’s Essential Psychopharmacology: Prescriber’s Guide: Children and Adolescents. Cambridge University Press; 2019.
2. Naguy A. Clonidine use in psychiatry: panacea or panache. Pharmacology. 2016;98(1-2):87-92. doi:10.1159/000446441
3. Jang YJ, Choi H, Han TS, et al. Effectiveness of clonidine in child and adolescent sleep disorders. Psychiatry Investig. 2022;19(9):738-747. doi:10.30773/pi.2022.0117
4. Bajor LA, Balsara C, Osser DN. An evidence-based approach to psychopharmacology for posttraumatic stress disorder (PTSD) - 2022 update. Psychiatry Res. 2022;317:114840. doi:10.1016/j.psychres.2022.114840
1. Stahl SM, Grady MM, Muntner N. Stahl’s Essential Psychopharmacology: Prescriber’s Guide: Children and Adolescents. Cambridge University Press; 2019.
2. Naguy A. Clonidine use in psychiatry: panacea or panache. Pharmacology. 2016;98(1-2):87-92. doi:10.1159/000446441
3. Jang YJ, Choi H, Han TS, et al. Effectiveness of clonidine in child and adolescent sleep disorders. Psychiatry Investig. 2022;19(9):738-747. doi:10.30773/pi.2022.0117
4. Bajor LA, Balsara C, Osser DN. An evidence-based approach to psychopharmacology for posttraumatic stress disorder (PTSD) - 2022 update. Psychiatry Res. 2022;317:114840. doi:10.1016/j.psychres.2022.114840


