User login
FDA panel leans toward more robust breast implant surveillance
SILVER SPRING, MD. – A mandatory, comprehensive approach to collecting adverse event data from breast implant recipients was favored during a March 25 hearing by a Food and Drug Administration advisory panel that oversees surgical devices.
This additional data could offer more complete information during the informed consent process for breast implants and potentially validate a new, autoimmune-like syndrome – breast implant illness (BII).
On the first day of a scheduled 2-day hearing, the advisory panel held no votes and took no formal actions. After a day of expert presentations and comments from more than 40 members of the public – mostly personal stories from affected patients and from plastic surgeons who place breast implants, panel members discussed a handful of questions from the FDA about relevant data to collect to better define the risks posed to breast implant recipients from breast-implant associated anaplastic large cell lymphoma (BIA-ALCL) and BII.
The advisory panel meeting took place as reports recently appeared documenting the scope of BIA-ALCL (Plast Reconstr Surg. 2019 March;143[3S]:65S-73S) and how to diagnose and manage BIA-ALCL (Aesthetic Surg J. 2019 March;39[S1}:S3-S13), and the existence of BII (Plast Reconstr Surg. 2019 March;143[3S]:74S-81S).
During the day’s two public comment periods, the panel heard from several women who gave brief accounts of developing and dealing with BIA-ALCL or BII.
“We think it’s important that all breast implant patients be aware of the risk for BIA-ALCL,” said Binita Ashar, MD, director of the FDAs Division of Surgical Devices. The FDA “is asking the panel what further steps need to be taken to understand the BIA-ALCL risk,” said Dr. Ashar as she opened the meeting of the General and Plastic Surgery Devices Panel of the Medical Devices Advisory Committee.
While the agency, as well as the plastic surgery community, have acknowledged the existence of BIA-ALCL since 2011, only recently have good data emerged on the scope of the complication. During the hearing, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, reported on his analysis of 457 unique cases of BIA-ALCL reported to the FDA since 2011. He found that the vast majority of cases had occurred in women who had received textured implants while a relatively small minority were linked with the placement of smooth implants.
Further scrutiny of the reported details of each case showed that none of the lymphomas were linked with a confirmed instance of “pure” smooth implant exposure. He also estimated the U.S. incidence of BIA-ALCL as roughly one case for every 20,000 implants. Complete, en bloc removal of the implant seems to be the most effective way to treat the cancer; most explanted patients have a good prognosis, he said.
Despite the apparent link between textured implants specifically and onset of BIA-ALCL, some panel members did not see a ban on textured implants as the answer.
Texturing the implant helps to stabilize the implant in position. Without texturing “we would need to use something else to stabilize the implant, or there would be a tsunami of reoperations,” said panel member Mary H. McGrath, MD, professor of surgery at the University of California, San Francisco. The main alternative to texturing for stabilizing implants is to wrap them in place using surgical mesh, but that approach may also cause problems.
“Instead of just taking textured implants off the market, we need to also look at their advantages. A critical issue is informed consent,” said panel member Marc E. Lippman, MD, a professor of medicine at Georgetown University, Washington. Banning smooth implants based on what’s known so far “would be an extraordinary over reaction,” he said during the first day’s session.
Current U.S. anecdotal experience suggests that a ban may not even be necessary because “plastic surgeons are more and more walking away from textured implants” because of the apparent link to BIA-ALCL, Dr. McGrath said.
BII has been a more recent and more controversial complication of breast implants. As recently as September 2018, Dr. Ashar said in a written statement that “the agency continues to believe that the weight of the currently available scientific evidence does not conclusively demonstrate an association between breast implants and connective tissue diseases,” the types of symptoms that characterize BII.
While the panel heard no new, conclusive evidence of a causal link between breast implants and the range of symptoms that some implant recipients report and is now collectively known as BII, several participants seemed convinced that the syndrome was real and needed better surveillance and study.
“It’s in the same family as chronic fatigue syndrome and fibromyalgia. It’s not a diagnosis, but a set of symptoms.” said Benjamin O. Anderson, MD, a surgical oncologist and professor of surgery at the University of Washington in Seattle and a panel member. “It’s a giant challenge. BII is a constellation of difficult symptoms. We need to think about how we ask patients, what are your symptoms?”
Frank R. Lewis Jr., MD, committee chair, said a more standardized measure of the most common BII symptoms is needed. “That may be exceedingly difficult, with as many as a hundred reported symptoms,” said Dr. Lewis, executive director, emeritus, of the American Board of Surgery in Philadelphia.
The hearing featured results from some of the most research projects aimed at fleshing out an understanding of BII.
Diana Zuckerman, PhD, president of the National Center for Health Research, reported data she and her associates collected in an online survey completed in late 2018 and early 2019 by 449 women who had approached the Center for help in getting health insurance coverage for medically-necessary explantation of their breast implants.
Their most common symptoms included joint, muscle or back pain, weakness or stiffness; fatigue; “brain fog;” and anxiety and depression. More than two-thirds of the respondents had a family history and 3% had a personal history of an autoimmune disease, and 61% said their symptoms improved after their implants were removed, Dr. Zuckerman reported during her presentation to the panel.
During the discussion, panel members seemed intent on expanding mandatory, routine surveillance to all breast implants placed in U.S. practice.
Andrea L. Pusic, MD, president of the Plastic Surgery Foundation, summarized the recent launch of the National Breast Implant Registry by the Foundation and its parent organization, the American Society of Plastic Surgeons. These organizations, and plastic surgeons in general, would be amenable to collecting the data the FDA deemed necessary to better track BIA-ALCL and BII, said Dr. Pusic, professor of surgery at Harvard Medical School and chief of plastic and reconstructive surgery at Brigham and Women’s Hospital in Boston.
“Plastic surgeons are willing to enter these data because we know they are important,” she told the FDA panel.
Dr. Ashar, Dr. Clemens, Dr. McGrath, Dr. Lippman, Dr. Anderson, Dr. Lewis, Dr. Zuckerman, and Dr. Pusic reported having no relevant commercial disclosures.
SILVER SPRING, MD. – A mandatory, comprehensive approach to collecting adverse event data from breast implant recipients was favored during a March 25 hearing by a Food and Drug Administration advisory panel that oversees surgical devices.
This additional data could offer more complete information during the informed consent process for breast implants and potentially validate a new, autoimmune-like syndrome – breast implant illness (BII).
On the first day of a scheduled 2-day hearing, the advisory panel held no votes and took no formal actions. After a day of expert presentations and comments from more than 40 members of the public – mostly personal stories from affected patients and from plastic surgeons who place breast implants, panel members discussed a handful of questions from the FDA about relevant data to collect to better define the risks posed to breast implant recipients from breast-implant associated anaplastic large cell lymphoma (BIA-ALCL) and BII.
The advisory panel meeting took place as reports recently appeared documenting the scope of BIA-ALCL (Plast Reconstr Surg. 2019 March;143[3S]:65S-73S) and how to diagnose and manage BIA-ALCL (Aesthetic Surg J. 2019 March;39[S1}:S3-S13), and the existence of BII (Plast Reconstr Surg. 2019 March;143[3S]:74S-81S).
During the day’s two public comment periods, the panel heard from several women who gave brief accounts of developing and dealing with BIA-ALCL or BII.
“We think it’s important that all breast implant patients be aware of the risk for BIA-ALCL,” said Binita Ashar, MD, director of the FDAs Division of Surgical Devices. The FDA “is asking the panel what further steps need to be taken to understand the BIA-ALCL risk,” said Dr. Ashar as she opened the meeting of the General and Plastic Surgery Devices Panel of the Medical Devices Advisory Committee.
While the agency, as well as the plastic surgery community, have acknowledged the existence of BIA-ALCL since 2011, only recently have good data emerged on the scope of the complication. During the hearing, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, reported on his analysis of 457 unique cases of BIA-ALCL reported to the FDA since 2011. He found that the vast majority of cases had occurred in women who had received textured implants while a relatively small minority were linked with the placement of smooth implants.
Further scrutiny of the reported details of each case showed that none of the lymphomas were linked with a confirmed instance of “pure” smooth implant exposure. He also estimated the U.S. incidence of BIA-ALCL as roughly one case for every 20,000 implants. Complete, en bloc removal of the implant seems to be the most effective way to treat the cancer; most explanted patients have a good prognosis, he said.
Despite the apparent link between textured implants specifically and onset of BIA-ALCL, some panel members did not see a ban on textured implants as the answer.
Texturing the implant helps to stabilize the implant in position. Without texturing “we would need to use something else to stabilize the implant, or there would be a tsunami of reoperations,” said panel member Mary H. McGrath, MD, professor of surgery at the University of California, San Francisco. The main alternative to texturing for stabilizing implants is to wrap them in place using surgical mesh, but that approach may also cause problems.
“Instead of just taking textured implants off the market, we need to also look at their advantages. A critical issue is informed consent,” said panel member Marc E. Lippman, MD, a professor of medicine at Georgetown University, Washington. Banning smooth implants based on what’s known so far “would be an extraordinary over reaction,” he said during the first day’s session.
Current U.S. anecdotal experience suggests that a ban may not even be necessary because “plastic surgeons are more and more walking away from textured implants” because of the apparent link to BIA-ALCL, Dr. McGrath said.
BII has been a more recent and more controversial complication of breast implants. As recently as September 2018, Dr. Ashar said in a written statement that “the agency continues to believe that the weight of the currently available scientific evidence does not conclusively demonstrate an association between breast implants and connective tissue diseases,” the types of symptoms that characterize BII.
While the panel heard no new, conclusive evidence of a causal link between breast implants and the range of symptoms that some implant recipients report and is now collectively known as BII, several participants seemed convinced that the syndrome was real and needed better surveillance and study.
“It’s in the same family as chronic fatigue syndrome and fibromyalgia. It’s not a diagnosis, but a set of symptoms.” said Benjamin O. Anderson, MD, a surgical oncologist and professor of surgery at the University of Washington in Seattle and a panel member. “It’s a giant challenge. BII is a constellation of difficult symptoms. We need to think about how we ask patients, what are your symptoms?”
Frank R. Lewis Jr., MD, committee chair, said a more standardized measure of the most common BII symptoms is needed. “That may be exceedingly difficult, with as many as a hundred reported symptoms,” said Dr. Lewis, executive director, emeritus, of the American Board of Surgery in Philadelphia.
The hearing featured results from some of the most research projects aimed at fleshing out an understanding of BII.
Diana Zuckerman, PhD, president of the National Center for Health Research, reported data she and her associates collected in an online survey completed in late 2018 and early 2019 by 449 women who had approached the Center for help in getting health insurance coverage for medically-necessary explantation of their breast implants.
Their most common symptoms included joint, muscle or back pain, weakness or stiffness; fatigue; “brain fog;” and anxiety and depression. More than two-thirds of the respondents had a family history and 3% had a personal history of an autoimmune disease, and 61% said their symptoms improved after their implants were removed, Dr. Zuckerman reported during her presentation to the panel.
During the discussion, panel members seemed intent on expanding mandatory, routine surveillance to all breast implants placed in U.S. practice.
Andrea L. Pusic, MD, president of the Plastic Surgery Foundation, summarized the recent launch of the National Breast Implant Registry by the Foundation and its parent organization, the American Society of Plastic Surgeons. These organizations, and plastic surgeons in general, would be amenable to collecting the data the FDA deemed necessary to better track BIA-ALCL and BII, said Dr. Pusic, professor of surgery at Harvard Medical School and chief of plastic and reconstructive surgery at Brigham and Women’s Hospital in Boston.
“Plastic surgeons are willing to enter these data because we know they are important,” she told the FDA panel.
Dr. Ashar, Dr. Clemens, Dr. McGrath, Dr. Lippman, Dr. Anderson, Dr. Lewis, Dr. Zuckerman, and Dr. Pusic reported having no relevant commercial disclosures.
SILVER SPRING, MD. – A mandatory, comprehensive approach to collecting adverse event data from breast implant recipients was favored during a March 25 hearing by a Food and Drug Administration advisory panel that oversees surgical devices.
This additional data could offer more complete information during the informed consent process for breast implants and potentially validate a new, autoimmune-like syndrome – breast implant illness (BII).
On the first day of a scheduled 2-day hearing, the advisory panel held no votes and took no formal actions. After a day of expert presentations and comments from more than 40 members of the public – mostly personal stories from affected patients and from plastic surgeons who place breast implants, panel members discussed a handful of questions from the FDA about relevant data to collect to better define the risks posed to breast implant recipients from breast-implant associated anaplastic large cell lymphoma (BIA-ALCL) and BII.
The advisory panel meeting took place as reports recently appeared documenting the scope of BIA-ALCL (Plast Reconstr Surg. 2019 March;143[3S]:65S-73S) and how to diagnose and manage BIA-ALCL (Aesthetic Surg J. 2019 March;39[S1}:S3-S13), and the existence of BII (Plast Reconstr Surg. 2019 March;143[3S]:74S-81S).
During the day’s two public comment periods, the panel heard from several women who gave brief accounts of developing and dealing with BIA-ALCL or BII.
“We think it’s important that all breast implant patients be aware of the risk for BIA-ALCL,” said Binita Ashar, MD, director of the FDAs Division of Surgical Devices. The FDA “is asking the panel what further steps need to be taken to understand the BIA-ALCL risk,” said Dr. Ashar as she opened the meeting of the General and Plastic Surgery Devices Panel of the Medical Devices Advisory Committee.
While the agency, as well as the plastic surgery community, have acknowledged the existence of BIA-ALCL since 2011, only recently have good data emerged on the scope of the complication. During the hearing, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, reported on his analysis of 457 unique cases of BIA-ALCL reported to the FDA since 2011. He found that the vast majority of cases had occurred in women who had received textured implants while a relatively small minority were linked with the placement of smooth implants.
Further scrutiny of the reported details of each case showed that none of the lymphomas were linked with a confirmed instance of “pure” smooth implant exposure. He also estimated the U.S. incidence of BIA-ALCL as roughly one case for every 20,000 implants. Complete, en bloc removal of the implant seems to be the most effective way to treat the cancer; most explanted patients have a good prognosis, he said.
Despite the apparent link between textured implants specifically and onset of BIA-ALCL, some panel members did not see a ban on textured implants as the answer.
Texturing the implant helps to stabilize the implant in position. Without texturing “we would need to use something else to stabilize the implant, or there would be a tsunami of reoperations,” said panel member Mary H. McGrath, MD, professor of surgery at the University of California, San Francisco. The main alternative to texturing for stabilizing implants is to wrap them in place using surgical mesh, but that approach may also cause problems.
“Instead of just taking textured implants off the market, we need to also look at their advantages. A critical issue is informed consent,” said panel member Marc E. Lippman, MD, a professor of medicine at Georgetown University, Washington. Banning smooth implants based on what’s known so far “would be an extraordinary over reaction,” he said during the first day’s session.
Current U.S. anecdotal experience suggests that a ban may not even be necessary because “plastic surgeons are more and more walking away from textured implants” because of the apparent link to BIA-ALCL, Dr. McGrath said.
BII has been a more recent and more controversial complication of breast implants. As recently as September 2018, Dr. Ashar said in a written statement that “the agency continues to believe that the weight of the currently available scientific evidence does not conclusively demonstrate an association between breast implants and connective tissue diseases,” the types of symptoms that characterize BII.
While the panel heard no new, conclusive evidence of a causal link between breast implants and the range of symptoms that some implant recipients report and is now collectively known as BII, several participants seemed convinced that the syndrome was real and needed better surveillance and study.
“It’s in the same family as chronic fatigue syndrome and fibromyalgia. It’s not a diagnosis, but a set of symptoms.” said Benjamin O. Anderson, MD, a surgical oncologist and professor of surgery at the University of Washington in Seattle and a panel member. “It’s a giant challenge. BII is a constellation of difficult symptoms. We need to think about how we ask patients, what are your symptoms?”
Frank R. Lewis Jr., MD, committee chair, said a more standardized measure of the most common BII symptoms is needed. “That may be exceedingly difficult, with as many as a hundred reported symptoms,” said Dr. Lewis, executive director, emeritus, of the American Board of Surgery in Philadelphia.
The hearing featured results from some of the most research projects aimed at fleshing out an understanding of BII.
Diana Zuckerman, PhD, president of the National Center for Health Research, reported data she and her associates collected in an online survey completed in late 2018 and early 2019 by 449 women who had approached the Center for help in getting health insurance coverage for medically-necessary explantation of their breast implants.
Their most common symptoms included joint, muscle or back pain, weakness or stiffness; fatigue; “brain fog;” and anxiety and depression. More than two-thirds of the respondents had a family history and 3% had a personal history of an autoimmune disease, and 61% said their symptoms improved after their implants were removed, Dr. Zuckerman reported during her presentation to the panel.
During the discussion, panel members seemed intent on expanding mandatory, routine surveillance to all breast implants placed in U.S. practice.
Andrea L. Pusic, MD, president of the Plastic Surgery Foundation, summarized the recent launch of the National Breast Implant Registry by the Foundation and its parent organization, the American Society of Plastic Surgeons. These organizations, and plastic surgeons in general, would be amenable to collecting the data the FDA deemed necessary to better track BIA-ALCL and BII, said Dr. Pusic, professor of surgery at Harvard Medical School and chief of plastic and reconstructive surgery at Brigham and Women’s Hospital in Boston.
“Plastic surgeons are willing to enter these data because we know they are important,” she told the FDA panel.
Dr. Ashar, Dr. Clemens, Dr. McGrath, Dr. Lippman, Dr. Anderson, Dr. Lewis, Dr. Zuckerman, and Dr. Pusic reported having no relevant commercial disclosures.
REPORTING FROM AN FDA ADVISORY COMMITTEE MEETING
Case report may link gluteal implants to lymphoma
Patients with textured silicone gluteal implants could be at risk of anaplastic large cell lymphoma, based on a possible case of ALCL in a patient diagnosed 1 year after implant placement.
The 49-year-old woman was initially diagnosed with anaplastic lymphoma kinase–negative ALCL via a lung mass and pleural fluid before bilateral gluteal ulceration occurred 1 month later, reported Orr Shauly of the University of Southern California in Los Angeles, and his colleagues.
Soft-tissue disease and fluid accumulation around the gluteal implants suggested that the lung mass had metastasized from primary neoplasia in the gluteal region. If ALCL did originate at the site of the gluteal implants, it would represent a first for silicone implant–associated ALCL, which has historically been associated exclusively with breast implants.
“As many as 200 cases of [breast implant-associated ALCL] have been described worldwide, with a majority in the context of cosmetic primary breast augmentation or cancer-related breast reconstruction with the use of a textured implant (57% of all cases),” the investigators wrote in Aesthetic Surgery Journal. “Recently however, it has been hypothesized that the relationship of ALCL with the placement of textured silicone implants may not [be] limited to the breast due to its multifactorial nature and association with texturization of the implant surface.”
During the initial work-up, a CT showed fluid collection and enhancement around the gluteal implants. Following ALCL diagnosis via lung mass biopsy and histopathology, the patient was transferred to a different facility for chemotherapy. When the patient presented 1 month later to the original facility with gluteal ulceration, the oncology team suspected infection; however, all cultures from fluid around the implants were negative.
Because of the possibility of false-negative tests, the patient was started on a regimen of acyclovir, vancomycin, metronidazole, and isavuconazole. Explantation was planned, but before this could occur, the patient deteriorated rapidly and died of respiratory and renal failure.
ALCL was not confirmed via cytology or histopathology in the gluteal region, and the patient’s family did not consent to autopsy, so a definitive diagnosis of gluteal implant–associated ALCL remained elusive.
“In this instance, it can only be concluded that the patient’s condition may have been associated with placement of textured silicone gluteal implants, but [we] still lack evidence of causation,” the investigators wrote. “It should also be noted that ALCL does not typically present with skin ulceration, and this may be a unique disease process in this patient or as a result of her bedridden state given the late stage of her disease. Furthermore, this presentation was uniquely aggressive and presented extremely quickly after placement of the gluteal implants. In most patients, ALCL develops and presents approximately 10 years after implantation.”
The investigators cautioned that “care should be taken to avoid sensationalizing all implant-associated ALCL.”
The authors reported having no conflicts of interest and the study did not receive funding.
SOURCE: Shauly O et al. Aesthet Surg J. 2019 Feb 15. doi: 10.1093/asj/sjz044.
Patients with textured silicone gluteal implants could be at risk of anaplastic large cell lymphoma, based on a possible case of ALCL in a patient diagnosed 1 year after implant placement.
The 49-year-old woman was initially diagnosed with anaplastic lymphoma kinase–negative ALCL via a lung mass and pleural fluid before bilateral gluteal ulceration occurred 1 month later, reported Orr Shauly of the University of Southern California in Los Angeles, and his colleagues.
Soft-tissue disease and fluid accumulation around the gluteal implants suggested that the lung mass had metastasized from primary neoplasia in the gluteal region. If ALCL did originate at the site of the gluteal implants, it would represent a first for silicone implant–associated ALCL, which has historically been associated exclusively with breast implants.
“As many as 200 cases of [breast implant-associated ALCL] have been described worldwide, with a majority in the context of cosmetic primary breast augmentation or cancer-related breast reconstruction with the use of a textured implant (57% of all cases),” the investigators wrote in Aesthetic Surgery Journal. “Recently however, it has been hypothesized that the relationship of ALCL with the placement of textured silicone implants may not [be] limited to the breast due to its multifactorial nature and association with texturization of the implant surface.”
During the initial work-up, a CT showed fluid collection and enhancement around the gluteal implants. Following ALCL diagnosis via lung mass biopsy and histopathology, the patient was transferred to a different facility for chemotherapy. When the patient presented 1 month later to the original facility with gluteal ulceration, the oncology team suspected infection; however, all cultures from fluid around the implants were negative.
Because of the possibility of false-negative tests, the patient was started on a regimen of acyclovir, vancomycin, metronidazole, and isavuconazole. Explantation was planned, but before this could occur, the patient deteriorated rapidly and died of respiratory and renal failure.
ALCL was not confirmed via cytology or histopathology in the gluteal region, and the patient’s family did not consent to autopsy, so a definitive diagnosis of gluteal implant–associated ALCL remained elusive.
“In this instance, it can only be concluded that the patient’s condition may have been associated with placement of textured silicone gluteal implants, but [we] still lack evidence of causation,” the investigators wrote. “It should also be noted that ALCL does not typically present with skin ulceration, and this may be a unique disease process in this patient or as a result of her bedridden state given the late stage of her disease. Furthermore, this presentation was uniquely aggressive and presented extremely quickly after placement of the gluteal implants. In most patients, ALCL develops and presents approximately 10 years after implantation.”
The investigators cautioned that “care should be taken to avoid sensationalizing all implant-associated ALCL.”
The authors reported having no conflicts of interest and the study did not receive funding.
SOURCE: Shauly O et al. Aesthet Surg J. 2019 Feb 15. doi: 10.1093/asj/sjz044.
Patients with textured silicone gluteal implants could be at risk of anaplastic large cell lymphoma, based on a possible case of ALCL in a patient diagnosed 1 year after implant placement.
The 49-year-old woman was initially diagnosed with anaplastic lymphoma kinase–negative ALCL via a lung mass and pleural fluid before bilateral gluteal ulceration occurred 1 month later, reported Orr Shauly of the University of Southern California in Los Angeles, and his colleagues.
Soft-tissue disease and fluid accumulation around the gluteal implants suggested that the lung mass had metastasized from primary neoplasia in the gluteal region. If ALCL did originate at the site of the gluteal implants, it would represent a first for silicone implant–associated ALCL, which has historically been associated exclusively with breast implants.
“As many as 200 cases of [breast implant-associated ALCL] have been described worldwide, with a majority in the context of cosmetic primary breast augmentation or cancer-related breast reconstruction with the use of a textured implant (57% of all cases),” the investigators wrote in Aesthetic Surgery Journal. “Recently however, it has been hypothesized that the relationship of ALCL with the placement of textured silicone implants may not [be] limited to the breast due to its multifactorial nature and association with texturization of the implant surface.”
During the initial work-up, a CT showed fluid collection and enhancement around the gluteal implants. Following ALCL diagnosis via lung mass biopsy and histopathology, the patient was transferred to a different facility for chemotherapy. When the patient presented 1 month later to the original facility with gluteal ulceration, the oncology team suspected infection; however, all cultures from fluid around the implants were negative.
Because of the possibility of false-negative tests, the patient was started on a regimen of acyclovir, vancomycin, metronidazole, and isavuconazole. Explantation was planned, but before this could occur, the patient deteriorated rapidly and died of respiratory and renal failure.
ALCL was not confirmed via cytology or histopathology in the gluteal region, and the patient’s family did not consent to autopsy, so a definitive diagnosis of gluteal implant–associated ALCL remained elusive.
“In this instance, it can only be concluded that the patient’s condition may have been associated with placement of textured silicone gluteal implants, but [we] still lack evidence of causation,” the investigators wrote. “It should also be noted that ALCL does not typically present with skin ulceration, and this may be a unique disease process in this patient or as a result of her bedridden state given the late stage of her disease. Furthermore, this presentation was uniquely aggressive and presented extremely quickly after placement of the gluteal implants. In most patients, ALCL develops and presents approximately 10 years after implantation.”
The investigators cautioned that “care should be taken to avoid sensationalizing all implant-associated ALCL.”
The authors reported having no conflicts of interest and the study did not receive funding.
SOURCE: Shauly O et al. Aesthet Surg J. 2019 Feb 15. doi: 10.1093/asj/sjz044.
FROM AESTHETIC SURGERY JOURNAL
How, and when, to use fat grafting for scars
BOSTON – according to Benjamin Levi, MD, director of the burn/wound and regenerative medicine laboratory at the University of Michigan, Ann Arbor.
Some corners of the Internet tout it as “some sort of magic stem cell surgery,” Dr. Levi said, but in reality, for scar surgeons, it’s just another useful tool in the armamentarium, one that excels at filling skin depressions due to underlying tissue loss, whether from burns, trauma, or surgery. Unlike hyaluronic acid and other options, fat grafts last; about half of injected adipocytes remain indefinitely. Fat grafting might also help soften scars, he said.
To get the most out of the procedure, of course, it has to be done correctly, so Dr. Levi took a few minutes at the annual clinical congress of the American College of Surgeons to share his tips on harvesting and spinning down fat grafts, injecting adipocytes, and other matters. Although the concepts of fat grafting are straightforward, the techniques are a bit tricky. Dr. Levi hoped his treatment pearls would help other physicians, especially those considering adding fat grafting to their practice.
BOSTON – according to Benjamin Levi, MD, director of the burn/wound and regenerative medicine laboratory at the University of Michigan, Ann Arbor.
Some corners of the Internet tout it as “some sort of magic stem cell surgery,” Dr. Levi said, but in reality, for scar surgeons, it’s just another useful tool in the armamentarium, one that excels at filling skin depressions due to underlying tissue loss, whether from burns, trauma, or surgery. Unlike hyaluronic acid and other options, fat grafts last; about half of injected adipocytes remain indefinitely. Fat grafting might also help soften scars, he said.
To get the most out of the procedure, of course, it has to be done correctly, so Dr. Levi took a few minutes at the annual clinical congress of the American College of Surgeons to share his tips on harvesting and spinning down fat grafts, injecting adipocytes, and other matters. Although the concepts of fat grafting are straightforward, the techniques are a bit tricky. Dr. Levi hoped his treatment pearls would help other physicians, especially those considering adding fat grafting to their practice.
BOSTON – according to Benjamin Levi, MD, director of the burn/wound and regenerative medicine laboratory at the University of Michigan, Ann Arbor.
Some corners of the Internet tout it as “some sort of magic stem cell surgery,” Dr. Levi said, but in reality, for scar surgeons, it’s just another useful tool in the armamentarium, one that excels at filling skin depressions due to underlying tissue loss, whether from burns, trauma, or surgery. Unlike hyaluronic acid and other options, fat grafts last; about half of injected adipocytes remain indefinitely. Fat grafting might also help soften scars, he said.
To get the most out of the procedure, of course, it has to be done correctly, so Dr. Levi took a few minutes at the annual clinical congress of the American College of Surgeons to share his tips on harvesting and spinning down fat grafts, injecting adipocytes, and other matters. Although the concepts of fat grafting are straightforward, the techniques are a bit tricky. Dr. Levi hoped his treatment pearls would help other physicians, especially those considering adding fat grafting to their practice.
EXPERT ANALYSIS FROM THE ACS CLINICAL CONGRESS
Is female genital cosmetic surgery going mainstream?
Experts describe the field of female genital cosmetic surgery as the “Wild West,” but the lack of regulation and consensus has not kept it from exploding in recent years.
More than 10,000 labiaplasties were performed in 2016, a 23% jump over the previous year, and the procedures are offered by more than 35% of all plastic surgeons, according to data from the American Society for Aesthetic Plastic Surgery. As another indicator of increasing attention to the appearance of female genitalia, a 2013 survey of U.S. women revealed that more than 80% performed some sort of pubic hair grooming (JAMA Dermatol. 2016;152[10]:1106-13).
Dr. Iglesia recounted being contacted by a National Gallery of Art staff member, who, when confronted with Gustave Courbet’s L’Origine du Monde, an 1866 below-the-waist portrait of a nude woman, asked, “Is this normal? Do women have this much hair?” Dr. Iglesia said she reassured the staff member that the woman in the portrait did indeed have a normal female Tanner stage IV or V escutcheon. However, she said, social media and other images in the popular press have essentially erased female pubic hair from the public eye, even in explicit imagery that involves female nudity.
“This is an ideal that men and women are seeing in social media, in pornography, and even in the lay press.” And now, she said, “We’re in a new era of sex surgeries, with these ‘nips and tucks’ below the belt.”
Labiaplasty
The combination of a newly-hairless genital region, together with portrayals of adult women with a “Barbie doll” appearance, may contribute to women feeling self-conscious about labia minora protruding beyond the labia majora. Dr. Iglesia, who is section director for female pelvic medicine and reconstructive surgery at MedStar Washington Hospital Center, Washington, D.C., said this is true even though the normal length of labia minora can range from 7 mm to 5 cm.
That’s where labiaplasty comes in. The procedure, which can be performed with conventional surgical techniques or with a laser, is sometimes done for functional reasons.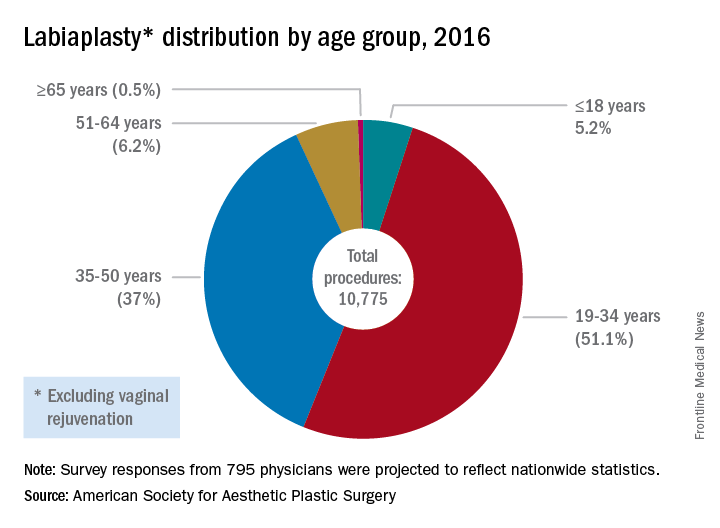
The waters are murkier when labiaplasty is performed for cosmetic reasons, to get that “Barbie doll” look, with some offices advertising the procedure as “designer lips,” Dr. Iglesia said.
In 2007, ACOG issued a committee opinion expressing concern about the lack of data and sometimes deceptive marketing practices surrounding a number of cosmetic vaginal surgeries (Obstet Gynecol 2007;110:737–8). The policy was reaffirmed in 2017.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/is-it-appropriate-to-perform-gynecologic-procedures-such-as-labiaplasty-for-cosmetic-reasons?iframe=1"}]Similarly, the Society of Obstetricians and Gynaecologists of Canada issued a 2013 statement about labiaplasty and other female genital cosmetic surgeries saying that “there is little evidence to support any of the female genital cosmetic surgeries in terms of improvement to sexual satisfaction or self-images. Physicians choosing to proceed with these cosmetic procedures should not promote these surgeries for the enhancement of sexual function and advertising of female genital cosmetic surgical procedures should be avoided.”
However, Mickey Karram, MD, who is director of the urogynecology program at Christ Hospital, Cincinnatti, said that informed consent is the key to dealing appropriately with these procedures.
“If a patient is physically bothered from a cosmetic standpoint that her labia are larger than she thinks they should be, and they are bothering her, is it appropriate or inappropriate to potentially discuss with her a labiaplasty?” Dr. Karram said at the ACOG meeting. For the patient who understands the risk and is also clear that the procedure is not medically necessary, he said he “feels strongly” that labiaplasty should be an option.
Fractional laser
The introduction of the fractional laser to gynecology is also adding to the debate about the appropriate integration of gynecologic procedures that may have nonmedical uses, such as vaginal “tightening.” Used primarily intravaginally, these devices have shallow penetration and are meant to stimulate collagen, proteoglycan, and hyaluronic acid synthesis with minimal tissue damage and downtime. One such device, the MonaLisa Touch, is marketed in the United States by Cynosure.
These energy sources hold great promise for the genitourinary syndrome of menopause (GSM) and other conditions, Dr. Karram said. “Many of these energy sources are being promoted for actual disease states, like vulvovaginal atrophy and lichen sclerosus,” he said.
Dr. Iglesia is not so sure: “This is not the fountain of youth.” She pointed out that the vasculature and innervation of the vagina and vulva are complex, with the outer one-eighth of the vagina being much more highly innervated. Laser treatment with a shallow penetration depth may not get at all of the issues that contribute to GSM.
“Is marketing ahead of the science? I would say yes,” she said. “There’s too much hype about this curing vaginal dryness and making your sex life better.”
Dr. Zahn also urged caution with the use of this technology. “The data are very limited, but, despite this, it’s become a very popular and highly-advertised approach. We need larger studies and more longitudinal data. This is especially true since one of the proposed ways this device works is by stimulating fibrosis. In every other body system, fibrosis stimulation may result in scarring. We have no idea if this is the case with this device. If it is, its application could result in worsening of bodily function, especially in regard to dyspareunia,” he said. “We clearly need more data.”
In 2016, ACOG issued a position statement about the fractional carbon dioxide and yttrium-aluminum-garnet laser systems that had received clearance from the Food and Drug Administration. The statement advised both ob.gyns. and patients that “this technology is, in fact, neither approved nor cleared by the FDA for the specific indication of treating vulvovaginal atrophy.”
Both Dr. Karram and Dr. Iglesia are investigators in an ongoing randomized, placebo- and sham-controlled trial comparing vaginal estrogen and laser therapy used both in conjunction and singly.
‘No-go’ procedures
Though Dr. Karram and Dr. Iglesia disagree on whether cosmetic labiaplasty is appropriate, they were in agreement that certain procedures are so untested, or have such potential risk with no proven benefit, that they should not be performed at all. The procedures on both physicians’ “no-go” lists included clitoral unhooding, G-spot amplification, “revirginification” in any form, vulval recontouring with autologous fat, and the so-called “O-shot,” injections of platelet-rich plasma that are touted as augmenting the sexual experience.
What’s to be done?
There is also agreement that a lack of common terminology is a significant problem. Step one, Dr. Karram said, is doing away with the term vaginal rejuvenation. “This is a terrible term. … There’s no real definition for this term.” He called for a multidisciplinary working group that would bring together gynecologists, plastic surgeons, and dermatologists to begin the work of terminology standardization.
From there, he proposed that the group develop a classification system that clarifies whether procedures are being done for cosmetic reasons, to enhance the sexual experience, or to address a specific disease state. Finally, he said, the group should recommend standardized outcome metrics that can be used to study the various interventions.
Dr. Zahn applauded this notion. “It’s a great point. I agree that multiple disciplines should be involved in examining outcomes, statistics, and criteria for evaluating procedures.”
And gynecologists should be leading this effort, Dr. Karram suggested. “Who knows this anatomy the best? We do.” He added, “If it’s going to be addressed, it should be addressed by us.”
But, Dr. Iglesia said she worries about vulnerable populations, such as adolescents and cancer survivors, who may undergo surgeries, for which the benefits may not outweigh the potential risks. For labiaplasty and laser resurfacing techniques, there have been a small number of studies on outcomes and patient satisfaction that have generally been conducted at single centers with no comparison arms and limited follow-up, she said.
“I also am concerned about pain, scarring, altered sensation, painful sex that could develop, wound complications, and what happens over time,” especially when these procedures may be performed on adolescents or women in their 20s or 30s who may later go on to have children, Dr. Iglesia said.
The question, she said, is not just whether gynecologists are better equipped than plastic surgeons or dermatologists to be performing female genital cosmetic surgery, “but should we be doing this at all?”
Dr. Zahn emphasized the need for evidence to guide decision making. “There has to be data that there is benefit and that the benefit outweighs the potential harm. There is no data on most cosmetic gynecologic procedures. If there are no data, they shouldn’t be done because we would not have the information necessary to appropriately counsel patients,” he said.
Dr. Karram has a financial relationship with Cynosure, which markets the MonaLisa Touch system in the United States. Dr. Iglesia reported that she had no relevant financial disclosures. Dr. Zahn is employed by ACOG.
[email protected]
On Twitter @karioakes
Experts describe the field of female genital cosmetic surgery as the “Wild West,” but the lack of regulation and consensus has not kept it from exploding in recent years.
More than 10,000 labiaplasties were performed in 2016, a 23% jump over the previous year, and the procedures are offered by more than 35% of all plastic surgeons, according to data from the American Society for Aesthetic Plastic Surgery. As another indicator of increasing attention to the appearance of female genitalia, a 2013 survey of U.S. women revealed that more than 80% performed some sort of pubic hair grooming (JAMA Dermatol. 2016;152[10]:1106-13).
Dr. Iglesia recounted being contacted by a National Gallery of Art staff member, who, when confronted with Gustave Courbet’s L’Origine du Monde, an 1866 below-the-waist portrait of a nude woman, asked, “Is this normal? Do women have this much hair?” Dr. Iglesia said she reassured the staff member that the woman in the portrait did indeed have a normal female Tanner stage IV or V escutcheon. However, she said, social media and other images in the popular press have essentially erased female pubic hair from the public eye, even in explicit imagery that involves female nudity.
“This is an ideal that men and women are seeing in social media, in pornography, and even in the lay press.” And now, she said, “We’re in a new era of sex surgeries, with these ‘nips and tucks’ below the belt.”
Labiaplasty
The combination of a newly-hairless genital region, together with portrayals of adult women with a “Barbie doll” appearance, may contribute to women feeling self-conscious about labia minora protruding beyond the labia majora. Dr. Iglesia, who is section director for female pelvic medicine and reconstructive surgery at MedStar Washington Hospital Center, Washington, D.C., said this is true even though the normal length of labia minora can range from 7 mm to 5 cm.
That’s where labiaplasty comes in. The procedure, which can be performed with conventional surgical techniques or with a laser, is sometimes done for functional reasons.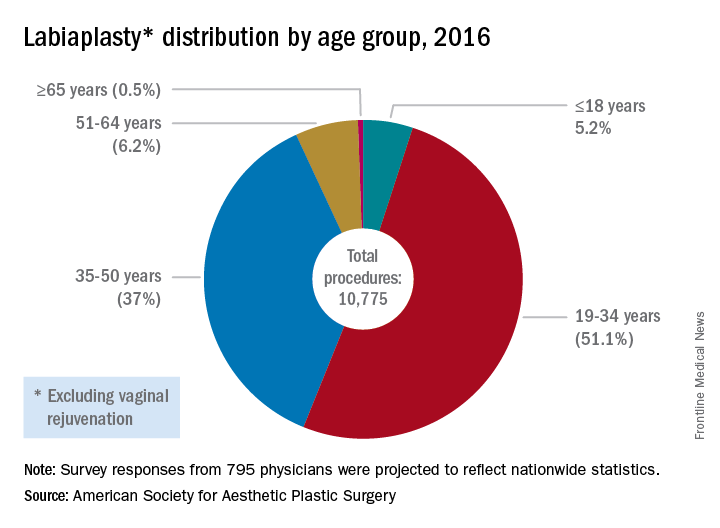
The waters are murkier when labiaplasty is performed for cosmetic reasons, to get that “Barbie doll” look, with some offices advertising the procedure as “designer lips,” Dr. Iglesia said.
In 2007, ACOG issued a committee opinion expressing concern about the lack of data and sometimes deceptive marketing practices surrounding a number of cosmetic vaginal surgeries (Obstet Gynecol 2007;110:737–8). The policy was reaffirmed in 2017.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/is-it-appropriate-to-perform-gynecologic-procedures-such-as-labiaplasty-for-cosmetic-reasons?iframe=1"}]Similarly, the Society of Obstetricians and Gynaecologists of Canada issued a 2013 statement about labiaplasty and other female genital cosmetic surgeries saying that “there is little evidence to support any of the female genital cosmetic surgeries in terms of improvement to sexual satisfaction or self-images. Physicians choosing to proceed with these cosmetic procedures should not promote these surgeries for the enhancement of sexual function and advertising of female genital cosmetic surgical procedures should be avoided.”
However, Mickey Karram, MD, who is director of the urogynecology program at Christ Hospital, Cincinnatti, said that informed consent is the key to dealing appropriately with these procedures.
“If a patient is physically bothered from a cosmetic standpoint that her labia are larger than she thinks they should be, and they are bothering her, is it appropriate or inappropriate to potentially discuss with her a labiaplasty?” Dr. Karram said at the ACOG meeting. For the patient who understands the risk and is also clear that the procedure is not medically necessary, he said he “feels strongly” that labiaplasty should be an option.
Fractional laser
The introduction of the fractional laser to gynecology is also adding to the debate about the appropriate integration of gynecologic procedures that may have nonmedical uses, such as vaginal “tightening.” Used primarily intravaginally, these devices have shallow penetration and are meant to stimulate collagen, proteoglycan, and hyaluronic acid synthesis with minimal tissue damage and downtime. One such device, the MonaLisa Touch, is marketed in the United States by Cynosure.
These energy sources hold great promise for the genitourinary syndrome of menopause (GSM) and other conditions, Dr. Karram said. “Many of these energy sources are being promoted for actual disease states, like vulvovaginal atrophy and lichen sclerosus,” he said.
Dr. Iglesia is not so sure: “This is not the fountain of youth.” She pointed out that the vasculature and innervation of the vagina and vulva are complex, with the outer one-eighth of the vagina being much more highly innervated. Laser treatment with a shallow penetration depth may not get at all of the issues that contribute to GSM.
“Is marketing ahead of the science? I would say yes,” she said. “There’s too much hype about this curing vaginal dryness and making your sex life better.”
Dr. Zahn also urged caution with the use of this technology. “The data are very limited, but, despite this, it’s become a very popular and highly-advertised approach. We need larger studies and more longitudinal data. This is especially true since one of the proposed ways this device works is by stimulating fibrosis. In every other body system, fibrosis stimulation may result in scarring. We have no idea if this is the case with this device. If it is, its application could result in worsening of bodily function, especially in regard to dyspareunia,” he said. “We clearly need more data.”
In 2016, ACOG issued a position statement about the fractional carbon dioxide and yttrium-aluminum-garnet laser systems that had received clearance from the Food and Drug Administration. The statement advised both ob.gyns. and patients that “this technology is, in fact, neither approved nor cleared by the FDA for the specific indication of treating vulvovaginal atrophy.”
Both Dr. Karram and Dr. Iglesia are investigators in an ongoing randomized, placebo- and sham-controlled trial comparing vaginal estrogen and laser therapy used both in conjunction and singly.
‘No-go’ procedures
Though Dr. Karram and Dr. Iglesia disagree on whether cosmetic labiaplasty is appropriate, they were in agreement that certain procedures are so untested, or have such potential risk with no proven benefit, that they should not be performed at all. The procedures on both physicians’ “no-go” lists included clitoral unhooding, G-spot amplification, “revirginification” in any form, vulval recontouring with autologous fat, and the so-called “O-shot,” injections of platelet-rich plasma that are touted as augmenting the sexual experience.
What’s to be done?
There is also agreement that a lack of common terminology is a significant problem. Step one, Dr. Karram said, is doing away with the term vaginal rejuvenation. “This is a terrible term. … There’s no real definition for this term.” He called for a multidisciplinary working group that would bring together gynecologists, plastic surgeons, and dermatologists to begin the work of terminology standardization.
From there, he proposed that the group develop a classification system that clarifies whether procedures are being done for cosmetic reasons, to enhance the sexual experience, or to address a specific disease state. Finally, he said, the group should recommend standardized outcome metrics that can be used to study the various interventions.
Dr. Zahn applauded this notion. “It’s a great point. I agree that multiple disciplines should be involved in examining outcomes, statistics, and criteria for evaluating procedures.”
And gynecologists should be leading this effort, Dr. Karram suggested. “Who knows this anatomy the best? We do.” He added, “If it’s going to be addressed, it should be addressed by us.”
But, Dr. Iglesia said she worries about vulnerable populations, such as adolescents and cancer survivors, who may undergo surgeries, for which the benefits may not outweigh the potential risks. For labiaplasty and laser resurfacing techniques, there have been a small number of studies on outcomes and patient satisfaction that have generally been conducted at single centers with no comparison arms and limited follow-up, she said.
“I also am concerned about pain, scarring, altered sensation, painful sex that could develop, wound complications, and what happens over time,” especially when these procedures may be performed on adolescents or women in their 20s or 30s who may later go on to have children, Dr. Iglesia said.
The question, she said, is not just whether gynecologists are better equipped than plastic surgeons or dermatologists to be performing female genital cosmetic surgery, “but should we be doing this at all?”
Dr. Zahn emphasized the need for evidence to guide decision making. “There has to be data that there is benefit and that the benefit outweighs the potential harm. There is no data on most cosmetic gynecologic procedures. If there are no data, they shouldn’t be done because we would not have the information necessary to appropriately counsel patients,” he said.
Dr. Karram has a financial relationship with Cynosure, which markets the MonaLisa Touch system in the United States. Dr. Iglesia reported that she had no relevant financial disclosures. Dr. Zahn is employed by ACOG.
[email protected]
On Twitter @karioakes
Experts describe the field of female genital cosmetic surgery as the “Wild West,” but the lack of regulation and consensus has not kept it from exploding in recent years.
More than 10,000 labiaplasties were performed in 2016, a 23% jump over the previous year, and the procedures are offered by more than 35% of all plastic surgeons, according to data from the American Society for Aesthetic Plastic Surgery. As another indicator of increasing attention to the appearance of female genitalia, a 2013 survey of U.S. women revealed that more than 80% performed some sort of pubic hair grooming (JAMA Dermatol. 2016;152[10]:1106-13).
Dr. Iglesia recounted being contacted by a National Gallery of Art staff member, who, when confronted with Gustave Courbet’s L’Origine du Monde, an 1866 below-the-waist portrait of a nude woman, asked, “Is this normal? Do women have this much hair?” Dr. Iglesia said she reassured the staff member that the woman in the portrait did indeed have a normal female Tanner stage IV or V escutcheon. However, she said, social media and other images in the popular press have essentially erased female pubic hair from the public eye, even in explicit imagery that involves female nudity.
“This is an ideal that men and women are seeing in social media, in pornography, and even in the lay press.” And now, she said, “We’re in a new era of sex surgeries, with these ‘nips and tucks’ below the belt.”
Labiaplasty
The combination of a newly-hairless genital region, together with portrayals of adult women with a “Barbie doll” appearance, may contribute to women feeling self-conscious about labia minora protruding beyond the labia majora. Dr. Iglesia, who is section director for female pelvic medicine and reconstructive surgery at MedStar Washington Hospital Center, Washington, D.C., said this is true even though the normal length of labia minora can range from 7 mm to 5 cm.
That’s where labiaplasty comes in. The procedure, which can be performed with conventional surgical techniques or with a laser, is sometimes done for functional reasons.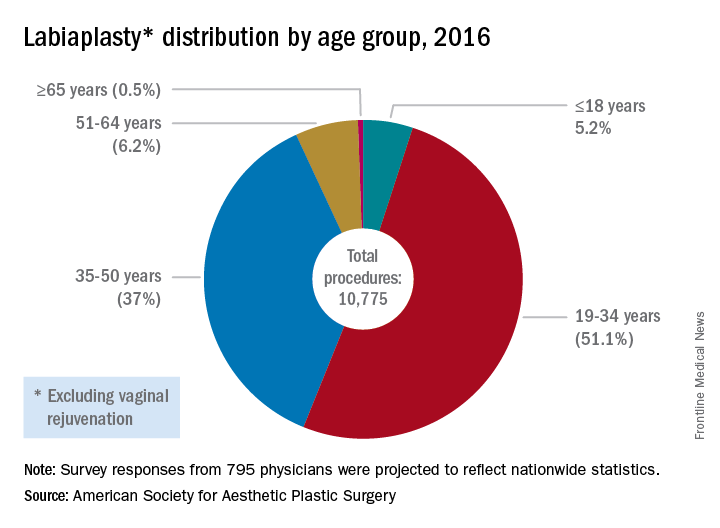
The waters are murkier when labiaplasty is performed for cosmetic reasons, to get that “Barbie doll” look, with some offices advertising the procedure as “designer lips,” Dr. Iglesia said.
In 2007, ACOG issued a committee opinion expressing concern about the lack of data and sometimes deceptive marketing practices surrounding a number of cosmetic vaginal surgeries (Obstet Gynecol 2007;110:737–8). The policy was reaffirmed in 2017.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/is-it-appropriate-to-perform-gynecologic-procedures-such-as-labiaplasty-for-cosmetic-reasons?iframe=1"}]Similarly, the Society of Obstetricians and Gynaecologists of Canada issued a 2013 statement about labiaplasty and other female genital cosmetic surgeries saying that “there is little evidence to support any of the female genital cosmetic surgeries in terms of improvement to sexual satisfaction or self-images. Physicians choosing to proceed with these cosmetic procedures should not promote these surgeries for the enhancement of sexual function and advertising of female genital cosmetic surgical procedures should be avoided.”
However, Mickey Karram, MD, who is director of the urogynecology program at Christ Hospital, Cincinnatti, said that informed consent is the key to dealing appropriately with these procedures.
“If a patient is physically bothered from a cosmetic standpoint that her labia are larger than she thinks they should be, and they are bothering her, is it appropriate or inappropriate to potentially discuss with her a labiaplasty?” Dr. Karram said at the ACOG meeting. For the patient who understands the risk and is also clear that the procedure is not medically necessary, he said he “feels strongly” that labiaplasty should be an option.
Fractional laser
The introduction of the fractional laser to gynecology is also adding to the debate about the appropriate integration of gynecologic procedures that may have nonmedical uses, such as vaginal “tightening.” Used primarily intravaginally, these devices have shallow penetration and are meant to stimulate collagen, proteoglycan, and hyaluronic acid synthesis with minimal tissue damage and downtime. One such device, the MonaLisa Touch, is marketed in the United States by Cynosure.
These energy sources hold great promise for the genitourinary syndrome of menopause (GSM) and other conditions, Dr. Karram said. “Many of these energy sources are being promoted for actual disease states, like vulvovaginal atrophy and lichen sclerosus,” he said.
Dr. Iglesia is not so sure: “This is not the fountain of youth.” She pointed out that the vasculature and innervation of the vagina and vulva are complex, with the outer one-eighth of the vagina being much more highly innervated. Laser treatment with a shallow penetration depth may not get at all of the issues that contribute to GSM.
“Is marketing ahead of the science? I would say yes,” she said. “There’s too much hype about this curing vaginal dryness and making your sex life better.”
Dr. Zahn also urged caution with the use of this technology. “The data are very limited, but, despite this, it’s become a very popular and highly-advertised approach. We need larger studies and more longitudinal data. This is especially true since one of the proposed ways this device works is by stimulating fibrosis. In every other body system, fibrosis stimulation may result in scarring. We have no idea if this is the case with this device. If it is, its application could result in worsening of bodily function, especially in regard to dyspareunia,” he said. “We clearly need more data.”
In 2016, ACOG issued a position statement about the fractional carbon dioxide and yttrium-aluminum-garnet laser systems that had received clearance from the Food and Drug Administration. The statement advised both ob.gyns. and patients that “this technology is, in fact, neither approved nor cleared by the FDA for the specific indication of treating vulvovaginal atrophy.”
Both Dr. Karram and Dr. Iglesia are investigators in an ongoing randomized, placebo- and sham-controlled trial comparing vaginal estrogen and laser therapy used both in conjunction and singly.
‘No-go’ procedures
Though Dr. Karram and Dr. Iglesia disagree on whether cosmetic labiaplasty is appropriate, they were in agreement that certain procedures are so untested, or have such potential risk with no proven benefit, that they should not be performed at all. The procedures on both physicians’ “no-go” lists included clitoral unhooding, G-spot amplification, “revirginification” in any form, vulval recontouring with autologous fat, and the so-called “O-shot,” injections of platelet-rich plasma that are touted as augmenting the sexual experience.
What’s to be done?
There is also agreement that a lack of common terminology is a significant problem. Step one, Dr. Karram said, is doing away with the term vaginal rejuvenation. “This is a terrible term. … There’s no real definition for this term.” He called for a multidisciplinary working group that would bring together gynecologists, plastic surgeons, and dermatologists to begin the work of terminology standardization.
From there, he proposed that the group develop a classification system that clarifies whether procedures are being done for cosmetic reasons, to enhance the sexual experience, or to address a specific disease state. Finally, he said, the group should recommend standardized outcome metrics that can be used to study the various interventions.
Dr. Zahn applauded this notion. “It’s a great point. I agree that multiple disciplines should be involved in examining outcomes, statistics, and criteria for evaluating procedures.”
And gynecologists should be leading this effort, Dr. Karram suggested. “Who knows this anatomy the best? We do.” He added, “If it’s going to be addressed, it should be addressed by us.”
But, Dr. Iglesia said she worries about vulnerable populations, such as adolescents and cancer survivors, who may undergo surgeries, for which the benefits may not outweigh the potential risks. For labiaplasty and laser resurfacing techniques, there have been a small number of studies on outcomes and patient satisfaction that have generally been conducted at single centers with no comparison arms and limited follow-up, she said.
“I also am concerned about pain, scarring, altered sensation, painful sex that could develop, wound complications, and what happens over time,” especially when these procedures may be performed on adolescents or women in their 20s or 30s who may later go on to have children, Dr. Iglesia said.
The question, she said, is not just whether gynecologists are better equipped than plastic surgeons or dermatologists to be performing female genital cosmetic surgery, “but should we be doing this at all?”
Dr. Zahn emphasized the need for evidence to guide decision making. “There has to be data that there is benefit and that the benefit outweighs the potential harm. There is no data on most cosmetic gynecologic procedures. If there are no data, they shouldn’t be done because we would not have the information necessary to appropriately counsel patients,” he said.
Dr. Karram has a financial relationship with Cynosure, which markets the MonaLisa Touch system in the United States. Dr. Iglesia reported that she had no relevant financial disclosures. Dr. Zahn is employed by ACOG.
[email protected]
On Twitter @karioakes
Resection reduces inflammatory breast cancer lesion recurrence
LAS VEGAS – In patients with nonmetastatic inflammatory breast cancer (IBC), aggressive surgical resection can reduce local/regional recurrence rates to levels comparable to those seen in patients with noninflammatory breast cancer.
The key to the improved outcome is the presence of a plastic surgeon who can help close a tricky incision. “We have a multidisciplinary team that allows us to call upon the plastic surgeons if we can’t control the incision, and they help us with a flap closure,” said Kelly Rosso, MD, a breast surgical oncology fellow at the MD Anderson Cancer Center, Houston, who presented the study results at the annual meeting of the American Society of Breast Surgeons.
To see if their surgical interventions were producing better outcomes, the team analyzed data from 114 patients with nonmetastatic inflammatory breast cancer who had received trimodality therapy (neoadjuvant chemotherapy, surgery, and radiation therapy) from 2007 to 2015.
The median patient age was 52 years, and the median follow-up period was 3.6 years. In total, 55% of patients had N2 IBC, and 45% had N3 disease.
Nearly all (113 of 114) patients had negative surgical margins. A total of 29 patients died during the follow-up period, and the 5-year survival rate was 69%. The odds of a local/regional recurrence over 2 years was 3% (95% confidence interval, 1%-10%). The 2-year odds of recurrence or distant metastasis was 23% (95% CI, 16%-32%).
Dr. Lucci said that he suspects that many surgeons avoid resection of inflammatory breast cancer lesions under the assumption that the disease is metastatic in nature and fear that an attempt at local control would put the patient through unnecessary surgery with little benefit.
The new study challenges that belief. “I think this is a changing paradigm. We have to consider that those patients need to be thought of as still resectable and think about getting rid of that local disease, at the very least to improve their quality of life and hopefully to improve their overall outcome,” Dr. Lucci said.
The results should be readily achievable in other centers, he added. “If they have a plastic surgeon who’s willing to help them, they can resect to negative margins just as well [as in noninflammatory patients]. And, if they have a radiation therapist who’s dedicated to doing a more aggressive course, they can achieve the same results.”
Dr. Rosso and Dr. Lucci reported having no financial disclosures.
LAS VEGAS – In patients with nonmetastatic inflammatory breast cancer (IBC), aggressive surgical resection can reduce local/regional recurrence rates to levels comparable to those seen in patients with noninflammatory breast cancer.
The key to the improved outcome is the presence of a plastic surgeon who can help close a tricky incision. “We have a multidisciplinary team that allows us to call upon the plastic surgeons if we can’t control the incision, and they help us with a flap closure,” said Kelly Rosso, MD, a breast surgical oncology fellow at the MD Anderson Cancer Center, Houston, who presented the study results at the annual meeting of the American Society of Breast Surgeons.
To see if their surgical interventions were producing better outcomes, the team analyzed data from 114 patients with nonmetastatic inflammatory breast cancer who had received trimodality therapy (neoadjuvant chemotherapy, surgery, and radiation therapy) from 2007 to 2015.
The median patient age was 52 years, and the median follow-up period was 3.6 years. In total, 55% of patients had N2 IBC, and 45% had N3 disease.
Nearly all (113 of 114) patients had negative surgical margins. A total of 29 patients died during the follow-up period, and the 5-year survival rate was 69%. The odds of a local/regional recurrence over 2 years was 3% (95% confidence interval, 1%-10%). The 2-year odds of recurrence or distant metastasis was 23% (95% CI, 16%-32%).
Dr. Lucci said that he suspects that many surgeons avoid resection of inflammatory breast cancer lesions under the assumption that the disease is metastatic in nature and fear that an attempt at local control would put the patient through unnecessary surgery with little benefit.
The new study challenges that belief. “I think this is a changing paradigm. We have to consider that those patients need to be thought of as still resectable and think about getting rid of that local disease, at the very least to improve their quality of life and hopefully to improve their overall outcome,” Dr. Lucci said.
The results should be readily achievable in other centers, he added. “If they have a plastic surgeon who’s willing to help them, they can resect to negative margins just as well [as in noninflammatory patients]. And, if they have a radiation therapist who’s dedicated to doing a more aggressive course, they can achieve the same results.”
Dr. Rosso and Dr. Lucci reported having no financial disclosures.
LAS VEGAS – In patients with nonmetastatic inflammatory breast cancer (IBC), aggressive surgical resection can reduce local/regional recurrence rates to levels comparable to those seen in patients with noninflammatory breast cancer.
The key to the improved outcome is the presence of a plastic surgeon who can help close a tricky incision. “We have a multidisciplinary team that allows us to call upon the plastic surgeons if we can’t control the incision, and they help us with a flap closure,” said Kelly Rosso, MD, a breast surgical oncology fellow at the MD Anderson Cancer Center, Houston, who presented the study results at the annual meeting of the American Society of Breast Surgeons.
To see if their surgical interventions were producing better outcomes, the team analyzed data from 114 patients with nonmetastatic inflammatory breast cancer who had received trimodality therapy (neoadjuvant chemotherapy, surgery, and radiation therapy) from 2007 to 2015.
The median patient age was 52 years, and the median follow-up period was 3.6 years. In total, 55% of patients had N2 IBC, and 45% had N3 disease.
Nearly all (113 of 114) patients had negative surgical margins. A total of 29 patients died during the follow-up period, and the 5-year survival rate was 69%. The odds of a local/regional recurrence over 2 years was 3% (95% confidence interval, 1%-10%). The 2-year odds of recurrence or distant metastasis was 23% (95% CI, 16%-32%).
Dr. Lucci said that he suspects that many surgeons avoid resection of inflammatory breast cancer lesions under the assumption that the disease is metastatic in nature and fear that an attempt at local control would put the patient through unnecessary surgery with little benefit.
The new study challenges that belief. “I think this is a changing paradigm. We have to consider that those patients need to be thought of as still resectable and think about getting rid of that local disease, at the very least to improve their quality of life and hopefully to improve their overall outcome,” Dr. Lucci said.
The results should be readily achievable in other centers, he added. “If they have a plastic surgeon who’s willing to help them, they can resect to negative margins just as well [as in noninflammatory patients]. And, if they have a radiation therapist who’s dedicated to doing a more aggressive course, they can achieve the same results.”
Dr. Rosso and Dr. Lucci reported having no financial disclosures.
At ASBS 2017
Key clinical point:
Major finding: The odds of a local/regional recurrence over 2 years were 3%.
Data source: A retrospective analysis of 114 patients.
Disclosures: Dr. Rosso and Dr. Lucci reported having no financial disclosures.
Most people who undergo gender reassignment surgery appreciate the results
ORLANDO – Gender reassignment surgery is the most extreme step for those transgender individuals who wish to complete the transformation to the opposite sex. While many transgender people do not opt to take this step, it may be an option for people who still have gender dysphoria after a thorough diagnostic work-up by a mental health professional, hormonal treatment, and having lived in the desired gender role as a “real-life test.”
Dr. Stan Monstrey, of Ghent University Hospital, Belgium, is an experienced gender reassignment surgeon and reported at the annual meeting of the American Academy of Clinical Endocrinology that between 1995 and 2005, he saw about 20-30 new patients a year. But now, he said, “We operate on a weekly basis between a minimum of three and sometimes six or seven transsexuals, so ... in our practice, probably between 90% and 95% are still going the whole way, still want what was called initially binary surgery.”
Transwomen: Male to female
The transformation procedure for male to female begins with feminizing aesthetic procedures, such as reducing the Adam’s apple (laryngeal prominence of the thyroid cartilage) and chin, frontal boss of the forehead, and possibly other facial work such as rhinoplasty. “Sometimes minor changes can have a huge effect on the face of the patient,” Dr. Monstrey said. “This is becoming, in our opinion, increasingly important for transwomen.”
Then, in about 75% of cases, Dr. Monstrey performs at least two surgeries under the same anesthesia – breast augmentation and perineal transformation. He said even after years of hormone therapy, most such patients have only a limited amount of breast tissue but want more prominent breasts. Implants can be placed behind or in front of the pectoralis muscle via inframammary, transaxillary, or occasionally periareolar approaches. Results are immediate, and complications are rare.
Another technique, which has become very popular over the past 5-10 years, is lipofilling to fill defects and depressions in the breasts. Stem cells contained in the fat may help soften scars. But when faced with a patient who had a BRCA1 mutation, the surgeons would not use lipofilling, fearing the potential for breast cancer, and would use prostheses instead (J Sex Med. 2014 Oct;11:2496-9). Still, questions remain about even using hormone treatments in such a patient.
Dr. Monstrey mentioned that in Belgium, breast augmentation for transwomen is considered reconstructive surgery and is always reimbursed whereas it is considered aesthetic surgery and never reimbursed for non-transwomen who want larger breasts. (For transmen, breast amputation is similarly reimbursed.)
The second operation is genital transformation. Basically, the interior of the penis is removed and the skin is invaginated to form a vagina of 8-18.5 cm and a scrotal flap, along with castration and removal of the penile bulb erectile tissue (corpus spongiosum) posteriorly. It is important to protect the rectal wall, which is not very strong. The foreskin becomes the new clitoral hood and inner side of the labia minora, and the clitoris is formed by reducing and transposing the penile glans. If the patient had a small penis and not enough tissue for the reconstruction, skin flaps from various other sites can be used.
Among more than 1,200 patients, 92% could achieve orgasm. Rectovaginal fistulas occurred in 4 patients, 19 needed repositioning of the urethra, 21 needed an operation to lengthen the vagina, and 95 needed aesthetic correction of the vulva. Dr. Monstrey said many patients have asked him when they should tell their new boyfriends about their transformation, meaning that the surgery was quite convincing even with penetrative sex.
If the first operation does not work, another technique is to use an isolated piece of colon or sigmoid bowel, which has been performed completely laparoscopically by a very skilled gastroenterologic surgeon at the hospital in Ghent.
Speaking to a roomful of endocrinologists, Dr. Monstrey told them, “I’ll be the first one to agree with you that indeed puberty blockers are a very good thing. However, we as surgeons are not so enthusiastic about them because … it is impossible to create a normal vagina” because of a lack of available tissue from the underdeveloped penis.
Transmen: Female to male
“Transmen react much better to hormonal therapy than do transwomen,” he said. “If they hide their breasts they really look like men. The disadvantage is that the surgical treatment is much more complex.” The most important operation for them is subcutaneous mastectomy and male contouring. A small, semiareolar incision leaves almost no scar. Most patients still require excision of redundant skin of the breasts.
Phalloplasty is a complex operation aimed at giving the patient an aesthetic phallus, a normal scrotum, the ability to void while standing, and to perform sexual intercourse, all while protecting erogenous sensation, with minimal morbidity and mortality. Dr. Monstrey reported that he has performed 600-700 phalloplasties.
The most common technique has been to use a free vascularized flap from another bodily site with the artery, vein, and nerves to reconnect at the phalloplasty site. Because the skin is very thin on the inner forearm, it is often used and allows forming an inner tube for the urethra and an outer tube for the penis. The surgery may have to be done in three or four stages for the best results. From pictures that Dr. Monstrey showed, it was obvious that the constructed penises were not absolutely natural in appearance, but he said most patients were “rather happy” with them, despite many of these patients being quite demanding. A scrotum is constructed from transposition of the labia minora.
Unfortunately, voiding while standing is often a problem, with 197 out of 562 patients (35%) having a fistula and urine leakage, but this issue frequently corrects itself. “More difficult to treat are the strictures with stenosis, which can be a problem voiding,” he said (occurring in 78/562). Other complications were 5 complete and 43 partial flap failures, 4 cases of compression syndrome, 58 cases of delayed wound healing, and 15 cases of transient ischemia. Flap failures occurred mainly in smokers, “so we don’t operate on smokers anymore,” he said.
One year after the constructive surgery, a penile prosthesis is implanted for those who want it, allowing sexual intercourse. Most individuals had orgasmic function, not because of reconnected nerves in the flap, but, Dr. Monstrey said he believes, because the clitoris, placed beneath the phallus, is denuded and stimulated during sexual activity. He said the problem is that the prostheses are usually intended for elderly men “who have sex a couple of times a month and who have a normal anatomy.” Young transmen may engage in more sexual activity, “so we have a lot of problems with exposure [of the prosthesis], infection, technical defects, and so on,” he said.
A technique gaining popularity is to use a skin flap from the groin area to make a urethra and one from the thigh to construct a penis. Although a penile transplant has recently been performed for a patient who had lost his penis to cancer, transplants are not being considered at this point, both for surgical technical reasons and because of a need for lifelong immunosuppressive drugs.
Proper referrals and counseling
The World Professional Association for Transgender Health in its Standard of Care guidelines 7 recommends one mental health professional referral for the breast surgery and two such referrals for genital surgery. The issue of possible parenthood should be discussed with patients, along with early counseling about fertility options. The age of majority and consent in different countries is important. Dr. Monstrey said genital surgery may be possible before the age of 18 years if all members of a multidisciplinary team of health professionals agree on a case by case basis that the adolescent can understand the risks, benefits, and alternatives to the surgery with the same degree of competence as someone 18 years of age or older.
Dr. Monstrey reported having no financial disclosures.
ORLANDO – Gender reassignment surgery is the most extreme step for those transgender individuals who wish to complete the transformation to the opposite sex. While many transgender people do not opt to take this step, it may be an option for people who still have gender dysphoria after a thorough diagnostic work-up by a mental health professional, hormonal treatment, and having lived in the desired gender role as a “real-life test.”
Dr. Stan Monstrey, of Ghent University Hospital, Belgium, is an experienced gender reassignment surgeon and reported at the annual meeting of the American Academy of Clinical Endocrinology that between 1995 and 2005, he saw about 20-30 new patients a year. But now, he said, “We operate on a weekly basis between a minimum of three and sometimes six or seven transsexuals, so ... in our practice, probably between 90% and 95% are still going the whole way, still want what was called initially binary surgery.”
Transwomen: Male to female
The transformation procedure for male to female begins with feminizing aesthetic procedures, such as reducing the Adam’s apple (laryngeal prominence of the thyroid cartilage) and chin, frontal boss of the forehead, and possibly other facial work such as rhinoplasty. “Sometimes minor changes can have a huge effect on the face of the patient,” Dr. Monstrey said. “This is becoming, in our opinion, increasingly important for transwomen.”
Then, in about 75% of cases, Dr. Monstrey performs at least two surgeries under the same anesthesia – breast augmentation and perineal transformation. He said even after years of hormone therapy, most such patients have only a limited amount of breast tissue but want more prominent breasts. Implants can be placed behind or in front of the pectoralis muscle via inframammary, transaxillary, or occasionally periareolar approaches. Results are immediate, and complications are rare.
Another technique, which has become very popular over the past 5-10 years, is lipofilling to fill defects and depressions in the breasts. Stem cells contained in the fat may help soften scars. But when faced with a patient who had a BRCA1 mutation, the surgeons would not use lipofilling, fearing the potential for breast cancer, and would use prostheses instead (J Sex Med. 2014 Oct;11:2496-9). Still, questions remain about even using hormone treatments in such a patient.
Dr. Monstrey mentioned that in Belgium, breast augmentation for transwomen is considered reconstructive surgery and is always reimbursed whereas it is considered aesthetic surgery and never reimbursed for non-transwomen who want larger breasts. (For transmen, breast amputation is similarly reimbursed.)
The second operation is genital transformation. Basically, the interior of the penis is removed and the skin is invaginated to form a vagina of 8-18.5 cm and a scrotal flap, along with castration and removal of the penile bulb erectile tissue (corpus spongiosum) posteriorly. It is important to protect the rectal wall, which is not very strong. The foreskin becomes the new clitoral hood and inner side of the labia minora, and the clitoris is formed by reducing and transposing the penile glans. If the patient had a small penis and not enough tissue for the reconstruction, skin flaps from various other sites can be used.
Among more than 1,200 patients, 92% could achieve orgasm. Rectovaginal fistulas occurred in 4 patients, 19 needed repositioning of the urethra, 21 needed an operation to lengthen the vagina, and 95 needed aesthetic correction of the vulva. Dr. Monstrey said many patients have asked him when they should tell their new boyfriends about their transformation, meaning that the surgery was quite convincing even with penetrative sex.
If the first operation does not work, another technique is to use an isolated piece of colon or sigmoid bowel, which has been performed completely laparoscopically by a very skilled gastroenterologic surgeon at the hospital in Ghent.
Speaking to a roomful of endocrinologists, Dr. Monstrey told them, “I’ll be the first one to agree with you that indeed puberty blockers are a very good thing. However, we as surgeons are not so enthusiastic about them because … it is impossible to create a normal vagina” because of a lack of available tissue from the underdeveloped penis.
Transmen: Female to male
“Transmen react much better to hormonal therapy than do transwomen,” he said. “If they hide their breasts they really look like men. The disadvantage is that the surgical treatment is much more complex.” The most important operation for them is subcutaneous mastectomy and male contouring. A small, semiareolar incision leaves almost no scar. Most patients still require excision of redundant skin of the breasts.
Phalloplasty is a complex operation aimed at giving the patient an aesthetic phallus, a normal scrotum, the ability to void while standing, and to perform sexual intercourse, all while protecting erogenous sensation, with minimal morbidity and mortality. Dr. Monstrey reported that he has performed 600-700 phalloplasties.
The most common technique has been to use a free vascularized flap from another bodily site with the artery, vein, and nerves to reconnect at the phalloplasty site. Because the skin is very thin on the inner forearm, it is often used and allows forming an inner tube for the urethra and an outer tube for the penis. The surgery may have to be done in three or four stages for the best results. From pictures that Dr. Monstrey showed, it was obvious that the constructed penises were not absolutely natural in appearance, but he said most patients were “rather happy” with them, despite many of these patients being quite demanding. A scrotum is constructed from transposition of the labia minora.
Unfortunately, voiding while standing is often a problem, with 197 out of 562 patients (35%) having a fistula and urine leakage, but this issue frequently corrects itself. “More difficult to treat are the strictures with stenosis, which can be a problem voiding,” he said (occurring in 78/562). Other complications were 5 complete and 43 partial flap failures, 4 cases of compression syndrome, 58 cases of delayed wound healing, and 15 cases of transient ischemia. Flap failures occurred mainly in smokers, “so we don’t operate on smokers anymore,” he said.
One year after the constructive surgery, a penile prosthesis is implanted for those who want it, allowing sexual intercourse. Most individuals had orgasmic function, not because of reconnected nerves in the flap, but, Dr. Monstrey said he believes, because the clitoris, placed beneath the phallus, is denuded and stimulated during sexual activity. He said the problem is that the prostheses are usually intended for elderly men “who have sex a couple of times a month and who have a normal anatomy.” Young transmen may engage in more sexual activity, “so we have a lot of problems with exposure [of the prosthesis], infection, technical defects, and so on,” he said.
A technique gaining popularity is to use a skin flap from the groin area to make a urethra and one from the thigh to construct a penis. Although a penile transplant has recently been performed for a patient who had lost his penis to cancer, transplants are not being considered at this point, both for surgical technical reasons and because of a need for lifelong immunosuppressive drugs.
Proper referrals and counseling
The World Professional Association for Transgender Health in its Standard of Care guidelines 7 recommends one mental health professional referral for the breast surgery and two such referrals for genital surgery. The issue of possible parenthood should be discussed with patients, along with early counseling about fertility options. The age of majority and consent in different countries is important. Dr. Monstrey said genital surgery may be possible before the age of 18 years if all members of a multidisciplinary team of health professionals agree on a case by case basis that the adolescent can understand the risks, benefits, and alternatives to the surgery with the same degree of competence as someone 18 years of age or older.
Dr. Monstrey reported having no financial disclosures.
ORLANDO – Gender reassignment surgery is the most extreme step for those transgender individuals who wish to complete the transformation to the opposite sex. While many transgender people do not opt to take this step, it may be an option for people who still have gender dysphoria after a thorough diagnostic work-up by a mental health professional, hormonal treatment, and having lived in the desired gender role as a “real-life test.”
Dr. Stan Monstrey, of Ghent University Hospital, Belgium, is an experienced gender reassignment surgeon and reported at the annual meeting of the American Academy of Clinical Endocrinology that between 1995 and 2005, he saw about 20-30 new patients a year. But now, he said, “We operate on a weekly basis between a minimum of three and sometimes six or seven transsexuals, so ... in our practice, probably between 90% and 95% are still going the whole way, still want what was called initially binary surgery.”
Transwomen: Male to female
The transformation procedure for male to female begins with feminizing aesthetic procedures, such as reducing the Adam’s apple (laryngeal prominence of the thyroid cartilage) and chin, frontal boss of the forehead, and possibly other facial work such as rhinoplasty. “Sometimes minor changes can have a huge effect on the face of the patient,” Dr. Monstrey said. “This is becoming, in our opinion, increasingly important for transwomen.”
Then, in about 75% of cases, Dr. Monstrey performs at least two surgeries under the same anesthesia – breast augmentation and perineal transformation. He said even after years of hormone therapy, most such patients have only a limited amount of breast tissue but want more prominent breasts. Implants can be placed behind or in front of the pectoralis muscle via inframammary, transaxillary, or occasionally periareolar approaches. Results are immediate, and complications are rare.
Another technique, which has become very popular over the past 5-10 years, is lipofilling to fill defects and depressions in the breasts. Stem cells contained in the fat may help soften scars. But when faced with a patient who had a BRCA1 mutation, the surgeons would not use lipofilling, fearing the potential for breast cancer, and would use prostheses instead (J Sex Med. 2014 Oct;11:2496-9). Still, questions remain about even using hormone treatments in such a patient.
Dr. Monstrey mentioned that in Belgium, breast augmentation for transwomen is considered reconstructive surgery and is always reimbursed whereas it is considered aesthetic surgery and never reimbursed for non-transwomen who want larger breasts. (For transmen, breast amputation is similarly reimbursed.)
The second operation is genital transformation. Basically, the interior of the penis is removed and the skin is invaginated to form a vagina of 8-18.5 cm and a scrotal flap, along with castration and removal of the penile bulb erectile tissue (corpus spongiosum) posteriorly. It is important to protect the rectal wall, which is not very strong. The foreskin becomes the new clitoral hood and inner side of the labia minora, and the clitoris is formed by reducing and transposing the penile glans. If the patient had a small penis and not enough tissue for the reconstruction, skin flaps from various other sites can be used.
Among more than 1,200 patients, 92% could achieve orgasm. Rectovaginal fistulas occurred in 4 patients, 19 needed repositioning of the urethra, 21 needed an operation to lengthen the vagina, and 95 needed aesthetic correction of the vulva. Dr. Monstrey said many patients have asked him when they should tell their new boyfriends about their transformation, meaning that the surgery was quite convincing even with penetrative sex.
If the first operation does not work, another technique is to use an isolated piece of colon or sigmoid bowel, which has been performed completely laparoscopically by a very skilled gastroenterologic surgeon at the hospital in Ghent.
Speaking to a roomful of endocrinologists, Dr. Monstrey told them, “I’ll be the first one to agree with you that indeed puberty blockers are a very good thing. However, we as surgeons are not so enthusiastic about them because … it is impossible to create a normal vagina” because of a lack of available tissue from the underdeveloped penis.
Transmen: Female to male
“Transmen react much better to hormonal therapy than do transwomen,” he said. “If they hide their breasts they really look like men. The disadvantage is that the surgical treatment is much more complex.” The most important operation for them is subcutaneous mastectomy and male contouring. A small, semiareolar incision leaves almost no scar. Most patients still require excision of redundant skin of the breasts.
Phalloplasty is a complex operation aimed at giving the patient an aesthetic phallus, a normal scrotum, the ability to void while standing, and to perform sexual intercourse, all while protecting erogenous sensation, with minimal morbidity and mortality. Dr. Monstrey reported that he has performed 600-700 phalloplasties.
The most common technique has been to use a free vascularized flap from another bodily site with the artery, vein, and nerves to reconnect at the phalloplasty site. Because the skin is very thin on the inner forearm, it is often used and allows forming an inner tube for the urethra and an outer tube for the penis. The surgery may have to be done in three or four stages for the best results. From pictures that Dr. Monstrey showed, it was obvious that the constructed penises were not absolutely natural in appearance, but he said most patients were “rather happy” with them, despite many of these patients being quite demanding. A scrotum is constructed from transposition of the labia minora.
Unfortunately, voiding while standing is often a problem, with 197 out of 562 patients (35%) having a fistula and urine leakage, but this issue frequently corrects itself. “More difficult to treat are the strictures with stenosis, which can be a problem voiding,” he said (occurring in 78/562). Other complications were 5 complete and 43 partial flap failures, 4 cases of compression syndrome, 58 cases of delayed wound healing, and 15 cases of transient ischemia. Flap failures occurred mainly in smokers, “so we don’t operate on smokers anymore,” he said.
One year after the constructive surgery, a penile prosthesis is implanted for those who want it, allowing sexual intercourse. Most individuals had orgasmic function, not because of reconnected nerves in the flap, but, Dr. Monstrey said he believes, because the clitoris, placed beneath the phallus, is denuded and stimulated during sexual activity. He said the problem is that the prostheses are usually intended for elderly men “who have sex a couple of times a month and who have a normal anatomy.” Young transmen may engage in more sexual activity, “so we have a lot of problems with exposure [of the prosthesis], infection, technical defects, and so on,” he said.
A technique gaining popularity is to use a skin flap from the groin area to make a urethra and one from the thigh to construct a penis. Although a penile transplant has recently been performed for a patient who had lost his penis to cancer, transplants are not being considered at this point, both for surgical technical reasons and because of a need for lifelong immunosuppressive drugs.
Proper referrals and counseling
The World Professional Association for Transgender Health in its Standard of Care guidelines 7 recommends one mental health professional referral for the breast surgery and two such referrals for genital surgery. The issue of possible parenthood should be discussed with patients, along with early counseling about fertility options. The age of majority and consent in different countries is important. Dr. Monstrey said genital surgery may be possible before the age of 18 years if all members of a multidisciplinary team of health professionals agree on a case by case basis that the adolescent can understand the risks, benefits, and alternatives to the surgery with the same degree of competence as someone 18 years of age or older.
Dr. Monstrey reported having no financial disclosures.
AACE 2016
Flu vaccination found safe in surgical patients
Immunizing surgical patients against seasonal influenza before they are discharged from the hospital appears safe and is a sound strategy for expanding vaccine coverage, especially among people at high risk, according to a report published online March 14 in Annals of Internal Medicine.
All health care contacts, including hospitalizations, are considered excellent opportunities for influenza vaccination, and current recommendations advise that eligible inpatients receive the immunization before discharge. However, surgical patients don’t often get the flu vaccine before they leave the hospital, likely because of concerns that potential adverse effects like fever and myalgia could be falsely attributed to surgical complications. This would lead to unnecessary patient evaluations and could interfere with postsurgical care, said Sara Y. Tartof, Ph.D., and her associates in the department of research and evaluation, Kaiser Permanente Southern California, Pasadena.
“Although this concern is understandable, few clinical data support it,” they noted.
“To provide clinical evidence that would either substantiate or refute” these concerns about perioperative flu vaccination, the investigators analyzed data in the electronic health records for 81,647 surgeries. All the study participants were deemed eligible for flu vaccination. They were socioeconomically and ethnically diverse, ranged in age from 6 months to 106 years, and underwent surgery at 14 hospitals during three consecutive flu seasons. Operations included general, cardiac, eye, dermatologic, ENT, neurologic, ob.gyn., oral/maxillofacial, orthopedic, plastic, podiatric, urologic, and vascular procedures.
Patients received a flu vaccine in 6,420 hospital stays for surgery – only 15% of 42,777 eligible hospitalizations – usually on the day of discharge. (The remaining 38,870 patients either had been vaccinated before hospital admission or were vaccinated more than a week after discharge and were not included in further analyses.)
Compared with eligible patients who didn’t receive a flu vaccine during hospitalization for surgery, those who did showed no increased risk for subsequent inpatient visits, ED visits, or clinical work-ups for infection. Patients who received the flu vaccine before discharge showed a minimally increased risk for outpatient visits during the week following hospitalization, but this was considered unlikely “to translate into substantial clinical impact,” especially when balanced against the benefit of immunization, Dr. Tartof and her associates said (Ann Intern Med. 2016 Mar 14. doi: 10.7326/M15-1667).
Giving the flu vaccine during a surgical hospitalization “is an opportunity to protect a high-risk population,” because surgery patients tend to be of an age, and to have comorbid conditions, that raise their risk for flu complications. In addition, previous research has reported that 39%-46% of adults hospitalized for influenza-related disease in a given year had been hospitalized during the preceding autumn, indicating that recent hospitalization also raises the risk for flu complications, the investigators said.
“Our data support the rationale for increasing vaccination rates among surgical inpatients,” they said.
This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
Immunizing surgical patients against seasonal influenza before they are discharged from the hospital appears safe and is a sound strategy for expanding vaccine coverage, especially among people at high risk, according to a report published online March 14 in Annals of Internal Medicine.
All health care contacts, including hospitalizations, are considered excellent opportunities for influenza vaccination, and current recommendations advise that eligible inpatients receive the immunization before discharge. However, surgical patients don’t often get the flu vaccine before they leave the hospital, likely because of concerns that potential adverse effects like fever and myalgia could be falsely attributed to surgical complications. This would lead to unnecessary patient evaluations and could interfere with postsurgical care, said Sara Y. Tartof, Ph.D., and her associates in the department of research and evaluation, Kaiser Permanente Southern California, Pasadena.
“Although this concern is understandable, few clinical data support it,” they noted.
“To provide clinical evidence that would either substantiate or refute” these concerns about perioperative flu vaccination, the investigators analyzed data in the electronic health records for 81,647 surgeries. All the study participants were deemed eligible for flu vaccination. They were socioeconomically and ethnically diverse, ranged in age from 6 months to 106 years, and underwent surgery at 14 hospitals during three consecutive flu seasons. Operations included general, cardiac, eye, dermatologic, ENT, neurologic, ob.gyn., oral/maxillofacial, orthopedic, plastic, podiatric, urologic, and vascular procedures.
Patients received a flu vaccine in 6,420 hospital stays for surgery – only 15% of 42,777 eligible hospitalizations – usually on the day of discharge. (The remaining 38,870 patients either had been vaccinated before hospital admission or were vaccinated more than a week after discharge and were not included in further analyses.)
Compared with eligible patients who didn’t receive a flu vaccine during hospitalization for surgery, those who did showed no increased risk for subsequent inpatient visits, ED visits, or clinical work-ups for infection. Patients who received the flu vaccine before discharge showed a minimally increased risk for outpatient visits during the week following hospitalization, but this was considered unlikely “to translate into substantial clinical impact,” especially when balanced against the benefit of immunization, Dr. Tartof and her associates said (Ann Intern Med. 2016 Mar 14. doi: 10.7326/M15-1667).
Giving the flu vaccine during a surgical hospitalization “is an opportunity to protect a high-risk population,” because surgery patients tend to be of an age, and to have comorbid conditions, that raise their risk for flu complications. In addition, previous research has reported that 39%-46% of adults hospitalized for influenza-related disease in a given year had been hospitalized during the preceding autumn, indicating that recent hospitalization also raises the risk for flu complications, the investigators said.
“Our data support the rationale for increasing vaccination rates among surgical inpatients,” they said.
This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
Immunizing surgical patients against seasonal influenza before they are discharged from the hospital appears safe and is a sound strategy for expanding vaccine coverage, especially among people at high risk, according to a report published online March 14 in Annals of Internal Medicine.
All health care contacts, including hospitalizations, are considered excellent opportunities for influenza vaccination, and current recommendations advise that eligible inpatients receive the immunization before discharge. However, surgical patients don’t often get the flu vaccine before they leave the hospital, likely because of concerns that potential adverse effects like fever and myalgia could be falsely attributed to surgical complications. This would lead to unnecessary patient evaluations and could interfere with postsurgical care, said Sara Y. Tartof, Ph.D., and her associates in the department of research and evaluation, Kaiser Permanente Southern California, Pasadena.
“Although this concern is understandable, few clinical data support it,” they noted.
“To provide clinical evidence that would either substantiate or refute” these concerns about perioperative flu vaccination, the investigators analyzed data in the electronic health records for 81,647 surgeries. All the study participants were deemed eligible for flu vaccination. They were socioeconomically and ethnically diverse, ranged in age from 6 months to 106 years, and underwent surgery at 14 hospitals during three consecutive flu seasons. Operations included general, cardiac, eye, dermatologic, ENT, neurologic, ob.gyn., oral/maxillofacial, orthopedic, plastic, podiatric, urologic, and vascular procedures.
Patients received a flu vaccine in 6,420 hospital stays for surgery – only 15% of 42,777 eligible hospitalizations – usually on the day of discharge. (The remaining 38,870 patients either had been vaccinated before hospital admission or were vaccinated more than a week after discharge and were not included in further analyses.)
Compared with eligible patients who didn’t receive a flu vaccine during hospitalization for surgery, those who did showed no increased risk for subsequent inpatient visits, ED visits, or clinical work-ups for infection. Patients who received the flu vaccine before discharge showed a minimally increased risk for outpatient visits during the week following hospitalization, but this was considered unlikely “to translate into substantial clinical impact,” especially when balanced against the benefit of immunization, Dr. Tartof and her associates said (Ann Intern Med. 2016 Mar 14. doi: 10.7326/M15-1667).
Giving the flu vaccine during a surgical hospitalization “is an opportunity to protect a high-risk population,” because surgery patients tend to be of an age, and to have comorbid conditions, that raise their risk for flu complications. In addition, previous research has reported that 39%-46% of adults hospitalized for influenza-related disease in a given year had been hospitalized during the preceding autumn, indicating that recent hospitalization also raises the risk for flu complications, the investigators said.
“Our data support the rationale for increasing vaccination rates among surgical inpatients,” they said.
This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Immunizing surgical patients against seasonal influenza before they leave the hospital appears safe.
Major finding: Patients received a flu vaccine in only 6,420 hospital stays for surgery, comprising only 15% of the patient hospitalizations that were eligible.
Data source: A retrospective cohort study involving 81,647 surgeries at 14 California hospitals during three consecutive flu seasons.
Disclosures: This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
Global Surgery: ‘Partnership Among Friends’
Surgery volunteerism has been on the rise for several decades. The American College of Surgeons is increasing its role in organizing and facilitating these programs via Operation Giving Back (OGB). And many ACS members are prominent participants in this endeavor.
A leader in global surgery is Michael L. Bentz, M.D., FAAP, FACS, professor of surgery, pediatrics, and neurosurgery, and chairman of the Division of Plastic and Reconstructive Surgery at the University of Wisconsin School of Medicine and Public Health. Dr. Bentz has led international missions in many countries of the world over nearly 20 years and has helped a team develop a long-term program of clinical care and training in Nicaragua. We talked with him about his experiences.
Q: You have been involved in international surgical missions for many years. Can you tell us something about your early projects?
I was first exposed to international work at the University of Pittsburgh. My mentor J. William Futrell, M.D., FACS, was a veteran of over 30 international surgical trips. I went on the first trip with him to Vietnam in the 1997 and have been going ever since. For that initial trip, we worked with a nonprofit organization called Interplast. I went with a large group of 20 people from the University that included plastic surgery attendings, plastic surgery residents, pediatric attendings, pediatric residents, and nursing and anesthesia staff.
In those days, many trips were based predominantly on clinical care – adult care and pediatric care. Teams would do a certain number of operations and then go home. We did cleft lip repairs, cleft palate repairs, burn reconstruction, congenital hand deformity surgery, and tumor management.
That would result in good outcomes for those who actually had a procedure done. But in any place I have ever worked overseas – Vietnam, China, Russia, Nicaragua – the need is overwhelming. The need far outstripped what surgical missions can provide in isolated, single trips back and forth.
Q: The years have brought changes to these missions. What are the most significant changes over the years in how these missions are conducted?
The scope and direction of global health is moving toward sustainable, long-term, and longitudinal education. In those earlier trips where there was an emphasis on doing as many operations as possible, people meant well – we meant well! But the real impact comes with the longitudinal education investment.
I have never been anywhere around the world where there weren’t interested, very capable, excellent surgeons committed to taking care of their patients who only need some support and facilitation.
If you compare the cases we are able to do on a trip with our partners with the cases they are able to do independently, it’s a logarithmic curve – they are far more productive than we could ever be on any number of trips. There is a multiplier effect that allows many more patients to be taken care of.
Q: Your institution has a long-term relationship with a hospital in Nicaragua. How does this work and what is the role of your team in the program?
The University of Wisconsin Division of Plastic Surgery and the Eduplast Foundation has a team of about 10 that goes to Nicaragua twice a year. Most importantly, we support a residency program in there. We move residents through a 3-year modular program much like programs in the U.S. and then examine them. We facilitate this educational process with trips there and we bring them to our institution in the U.S.
Over the past 10 years, we have been doing a weekly live webcast of our Plastic Surgery Grand Rounds which is received on several continents. This creates a very valuable bidirectional, and even tridirectional conversation. This webcast is simple, incredibly inexpensive, and has provided hundreds of hours of education over the years in addition to the on-site work we do.
There can be a language barrier in some cases, but we broadcast in English, with occasional translation support. In addition to Nicaragua, our webcast has been received in institutions in Thailand, China, Ecuador and across the United States. We keep records of cases performed. Our plastic surgery residents can get credit for the cases they do under faculty supervision at our international sites if we meet specific criteria set by our Resident Review Committee.
It is important to note that we take care of the patients in our partner institutions in Nicaragua exactly as we would care for patients in our institution in Wisconsin. There is no “practicing” as all operations are done by surgeons appropriately credentialed and trained for the task.
Q: Do you find that there is a cultural gap that you must bridge in working with colleagues and patients in Nicaragua?
Our program has an orientation session for team participants in advance of each trip, where we talk about the mechanics of the trip – safety, medical issues. We also talk about cultural considerations of each site. It is very important that the residents embed in the culture in which we are working. They also need to know the cultural norms of how to communicate with patients, parents, and children. Some of it is simply good manners – acting like your mother taught you!
The team can reside in a local hotel, but often stays in the homes of local hosts, and this can be a beautiful opportunity to learn about local norms and communication.
Q: What is your favorite part of these missions?
I have so many favorite parts! I like caring for people who otherwise might not receive medical care. This is “giving back” and I think all of the participants would agree that we come home feeling like we received much more than we gave. These experiences remind you of why you went to medical school. It is an opportunity to provide something in return for all the investment that has been made in us for our education. In working with colleagues from other countries, I learn as much as I teach. I come back a better surgeon.
The benefits to residents from our institution are many. They learn how to operate in a resource-limited setting, and they return with a greater appreciation for the equipment and supplies we have available at our institution in Madison. The cultural competence and awareness they also learn is an invaluable life skill.
I want to stress that the friendships with our fellow surgeons are what makes this work. We achieve a degree of continuity and even watch our pediatric patients grow up over the years because of our long-term relationship with the hospital in León and our dedicated colleagues there. This is a truly a partnership among friends.
Q: Do you have some advice for a surgeon interested in participating in an international program?
For those surgeons who were not exposed to these programs during residency, finding a mentor or mentoring organization is the way to begin. A beginner should consider making the first couple of trips with someone who knows the ropes in terms of understanding cultural competency, practical issues of safety, and relevant clinical issues. Almost every surgery discipline has an organization with the capability of identifying volunteer surgery groups in their specialty. ACS’ Operation Giving Back is a particularly important resource for helping Fellows find the right international program.
If you would like to learn more about global surgery programs, contact Operation Giving Back at [email protected]. Or if you would like to share your experiences as an international surgical volunteer, please email this publication at [email protected].
Surgery volunteerism has been on the rise for several decades. The American College of Surgeons is increasing its role in organizing and facilitating these programs via Operation Giving Back (OGB). And many ACS members are prominent participants in this endeavor.
A leader in global surgery is Michael L. Bentz, M.D., FAAP, FACS, professor of surgery, pediatrics, and neurosurgery, and chairman of the Division of Plastic and Reconstructive Surgery at the University of Wisconsin School of Medicine and Public Health. Dr. Bentz has led international missions in many countries of the world over nearly 20 years and has helped a team develop a long-term program of clinical care and training in Nicaragua. We talked with him about his experiences.
Q: You have been involved in international surgical missions for many years. Can you tell us something about your early projects?
I was first exposed to international work at the University of Pittsburgh. My mentor J. William Futrell, M.D., FACS, was a veteran of over 30 international surgical trips. I went on the first trip with him to Vietnam in the 1997 and have been going ever since. For that initial trip, we worked with a nonprofit organization called Interplast. I went with a large group of 20 people from the University that included plastic surgery attendings, plastic surgery residents, pediatric attendings, pediatric residents, and nursing and anesthesia staff.
In those days, many trips were based predominantly on clinical care – adult care and pediatric care. Teams would do a certain number of operations and then go home. We did cleft lip repairs, cleft palate repairs, burn reconstruction, congenital hand deformity surgery, and tumor management.
That would result in good outcomes for those who actually had a procedure done. But in any place I have ever worked overseas – Vietnam, China, Russia, Nicaragua – the need is overwhelming. The need far outstripped what surgical missions can provide in isolated, single trips back and forth.
Q: The years have brought changes to these missions. What are the most significant changes over the years in how these missions are conducted?
The scope and direction of global health is moving toward sustainable, long-term, and longitudinal education. In those earlier trips where there was an emphasis on doing as many operations as possible, people meant well – we meant well! But the real impact comes with the longitudinal education investment.
I have never been anywhere around the world where there weren’t interested, very capable, excellent surgeons committed to taking care of their patients who only need some support and facilitation.
If you compare the cases we are able to do on a trip with our partners with the cases they are able to do independently, it’s a logarithmic curve – they are far more productive than we could ever be on any number of trips. There is a multiplier effect that allows many more patients to be taken care of.
Q: Your institution has a long-term relationship with a hospital in Nicaragua. How does this work and what is the role of your team in the program?
The University of Wisconsin Division of Plastic Surgery and the Eduplast Foundation has a team of about 10 that goes to Nicaragua twice a year. Most importantly, we support a residency program in there. We move residents through a 3-year modular program much like programs in the U.S. and then examine them. We facilitate this educational process with trips there and we bring them to our institution in the U.S.
Over the past 10 years, we have been doing a weekly live webcast of our Plastic Surgery Grand Rounds which is received on several continents. This creates a very valuable bidirectional, and even tridirectional conversation. This webcast is simple, incredibly inexpensive, and has provided hundreds of hours of education over the years in addition to the on-site work we do.
There can be a language barrier in some cases, but we broadcast in English, with occasional translation support. In addition to Nicaragua, our webcast has been received in institutions in Thailand, China, Ecuador and across the United States. We keep records of cases performed. Our plastic surgery residents can get credit for the cases they do under faculty supervision at our international sites if we meet specific criteria set by our Resident Review Committee.
It is important to note that we take care of the patients in our partner institutions in Nicaragua exactly as we would care for patients in our institution in Wisconsin. There is no “practicing” as all operations are done by surgeons appropriately credentialed and trained for the task.
Q: Do you find that there is a cultural gap that you must bridge in working with colleagues and patients in Nicaragua?
Our program has an orientation session for team participants in advance of each trip, where we talk about the mechanics of the trip – safety, medical issues. We also talk about cultural considerations of each site. It is very important that the residents embed in the culture in which we are working. They also need to know the cultural norms of how to communicate with patients, parents, and children. Some of it is simply good manners – acting like your mother taught you!
The team can reside in a local hotel, but often stays in the homes of local hosts, and this can be a beautiful opportunity to learn about local norms and communication.
Q: What is your favorite part of these missions?
I have so many favorite parts! I like caring for people who otherwise might not receive medical care. This is “giving back” and I think all of the participants would agree that we come home feeling like we received much more than we gave. These experiences remind you of why you went to medical school. It is an opportunity to provide something in return for all the investment that has been made in us for our education. In working with colleagues from other countries, I learn as much as I teach. I come back a better surgeon.
The benefits to residents from our institution are many. They learn how to operate in a resource-limited setting, and they return with a greater appreciation for the equipment and supplies we have available at our institution in Madison. The cultural competence and awareness they also learn is an invaluable life skill.
I want to stress that the friendships with our fellow surgeons are what makes this work. We achieve a degree of continuity and even watch our pediatric patients grow up over the years because of our long-term relationship with the hospital in León and our dedicated colleagues there. This is a truly a partnership among friends.
Q: Do you have some advice for a surgeon interested in participating in an international program?
For those surgeons who were not exposed to these programs during residency, finding a mentor or mentoring organization is the way to begin. A beginner should consider making the first couple of trips with someone who knows the ropes in terms of understanding cultural competency, practical issues of safety, and relevant clinical issues. Almost every surgery discipline has an organization with the capability of identifying volunteer surgery groups in their specialty. ACS’ Operation Giving Back is a particularly important resource for helping Fellows find the right international program.
If you would like to learn more about global surgery programs, contact Operation Giving Back at [email protected]. Or if you would like to share your experiences as an international surgical volunteer, please email this publication at [email protected].
Surgery volunteerism has been on the rise for several decades. The American College of Surgeons is increasing its role in organizing and facilitating these programs via Operation Giving Back (OGB). And many ACS members are prominent participants in this endeavor.
A leader in global surgery is Michael L. Bentz, M.D., FAAP, FACS, professor of surgery, pediatrics, and neurosurgery, and chairman of the Division of Plastic and Reconstructive Surgery at the University of Wisconsin School of Medicine and Public Health. Dr. Bentz has led international missions in many countries of the world over nearly 20 years and has helped a team develop a long-term program of clinical care and training in Nicaragua. We talked with him about his experiences.
Q: You have been involved in international surgical missions for many years. Can you tell us something about your early projects?
I was first exposed to international work at the University of Pittsburgh. My mentor J. William Futrell, M.D., FACS, was a veteran of over 30 international surgical trips. I went on the first trip with him to Vietnam in the 1997 and have been going ever since. For that initial trip, we worked with a nonprofit organization called Interplast. I went with a large group of 20 people from the University that included plastic surgery attendings, plastic surgery residents, pediatric attendings, pediatric residents, and nursing and anesthesia staff.
In those days, many trips were based predominantly on clinical care – adult care and pediatric care. Teams would do a certain number of operations and then go home. We did cleft lip repairs, cleft palate repairs, burn reconstruction, congenital hand deformity surgery, and tumor management.
That would result in good outcomes for those who actually had a procedure done. But in any place I have ever worked overseas – Vietnam, China, Russia, Nicaragua – the need is overwhelming. The need far outstripped what surgical missions can provide in isolated, single trips back and forth.
Q: The years have brought changes to these missions. What are the most significant changes over the years in how these missions are conducted?
The scope and direction of global health is moving toward sustainable, long-term, and longitudinal education. In those earlier trips where there was an emphasis on doing as many operations as possible, people meant well – we meant well! But the real impact comes with the longitudinal education investment.
I have never been anywhere around the world where there weren’t interested, very capable, excellent surgeons committed to taking care of their patients who only need some support and facilitation.
If you compare the cases we are able to do on a trip with our partners with the cases they are able to do independently, it’s a logarithmic curve – they are far more productive than we could ever be on any number of trips. There is a multiplier effect that allows many more patients to be taken care of.
Q: Your institution has a long-term relationship with a hospital in Nicaragua. How does this work and what is the role of your team in the program?
The University of Wisconsin Division of Plastic Surgery and the Eduplast Foundation has a team of about 10 that goes to Nicaragua twice a year. Most importantly, we support a residency program in there. We move residents through a 3-year modular program much like programs in the U.S. and then examine them. We facilitate this educational process with trips there and we bring them to our institution in the U.S.
Over the past 10 years, we have been doing a weekly live webcast of our Plastic Surgery Grand Rounds which is received on several continents. This creates a very valuable bidirectional, and even tridirectional conversation. This webcast is simple, incredibly inexpensive, and has provided hundreds of hours of education over the years in addition to the on-site work we do.
There can be a language barrier in some cases, but we broadcast in English, with occasional translation support. In addition to Nicaragua, our webcast has been received in institutions in Thailand, China, Ecuador and across the United States. We keep records of cases performed. Our plastic surgery residents can get credit for the cases they do under faculty supervision at our international sites if we meet specific criteria set by our Resident Review Committee.
It is important to note that we take care of the patients in our partner institutions in Nicaragua exactly as we would care for patients in our institution in Wisconsin. There is no “practicing” as all operations are done by surgeons appropriately credentialed and trained for the task.
Q: Do you find that there is a cultural gap that you must bridge in working with colleagues and patients in Nicaragua?
Our program has an orientation session for team participants in advance of each trip, where we talk about the mechanics of the trip – safety, medical issues. We also talk about cultural considerations of each site. It is very important that the residents embed in the culture in which we are working. They also need to know the cultural norms of how to communicate with patients, parents, and children. Some of it is simply good manners – acting like your mother taught you!
The team can reside in a local hotel, but often stays in the homes of local hosts, and this can be a beautiful opportunity to learn about local norms and communication.
Q: What is your favorite part of these missions?
I have so many favorite parts! I like caring for people who otherwise might not receive medical care. This is “giving back” and I think all of the participants would agree that we come home feeling like we received much more than we gave. These experiences remind you of why you went to medical school. It is an opportunity to provide something in return for all the investment that has been made in us for our education. In working with colleagues from other countries, I learn as much as I teach. I come back a better surgeon.
The benefits to residents from our institution are many. They learn how to operate in a resource-limited setting, and they return with a greater appreciation for the equipment and supplies we have available at our institution in Madison. The cultural competence and awareness they also learn is an invaluable life skill.
I want to stress that the friendships with our fellow surgeons are what makes this work. We achieve a degree of continuity and even watch our pediatric patients grow up over the years because of our long-term relationship with the hospital in León and our dedicated colleagues there. This is a truly a partnership among friends.
Q: Do you have some advice for a surgeon interested in participating in an international program?
For those surgeons who were not exposed to these programs during residency, finding a mentor or mentoring organization is the way to begin. A beginner should consider making the first couple of trips with someone who knows the ropes in terms of understanding cultural competency, practical issues of safety, and relevant clinical issues. Almost every surgery discipline has an organization with the capability of identifying volunteer surgery groups in their specialty. ACS’ Operation Giving Back is a particularly important resource for helping Fellows find the right international program.
If you would like to learn more about global surgery programs, contact Operation Giving Back at [email protected]. Or if you would like to share your experiences as an international surgical volunteer, please email this publication at [email protected].
Closing large dermal defects much like a Victorian corset
EDINBURGH – Barbed absorbable sutures are a useful new tool to facilitate dermal closure of facial and nonfacial defects following tumor resection.
“These are not the bad old sutures that you might of heard about before, that were nonabsorbable sutures and attempted for use in cosmetic procedures,” Dr. John Strasswimmer said at the 15th World Congress on Cancers of the Skin.
Last year, Dr. Strasswimmer, medical director of melanoma and cutaneous oncology at the Lynn Cancer Institute in Boca Raton, Fla., reported his initial experience using a procedure he calls “Corseta” to close a large Mohs defect on the trunk of an 83-year-old man (JAMA Dermatol. 2013;149:853-4).
The procedure employs a barbed, bioabsorbable suture (Ethicon’s Stratafix and Covidien’s V-Loc) that is run in a continuous vertical looping manner in the subcutaneous layer, with minimal to no undermining of the wound. Undermining is typically used in cutaneous surgery to relieve tension or provide structure around anatomical landmarks, but it can increase the risk of bleeding, swelling, and patient discomfort, he said.
Instead, the first suture pass is placed in the deepest portion of the subcutaneous tissue and brought out within the more superficial subcutaneous layer. Each bite of the barbed suture extends peripherally at least 2.0 cm from the edge of the wound, so the point of tension is lateral to the wound margins. At every two passes, tension is placed evenly across the sutures to close the deepest layer of tissue and to engage the barbs, much like closing of a Victorian corset, Dr. Strasswimmer said.
The second arm of the suture is passed in a similar manner in the subcutaneous plane, superficial to the first pass.
“This is a lacing, not a suturing technique,” he said. “You get tissue approximation, but more importantly, because we’re bringing in all that deep tissue, you automatically get beautiful wound-edge eversion and very nice cosmetic results.”
Because the sutures have barbs cut into them, however, a 0-0 weight polydioxane or other absorbable material suture can have a breaking strength of a #2-0 suture. “You have to look very carefully at the manufacturer’s sizing and strength requirements,” Dr. Strasswimmer cautioned.
Since their initial case report, Dr. Strasswimmer and his colleagues have expanded use of the Corseta technique to more than 600 facial and nonfacial reconstructions. The Corseta procedure is not as helpful for curved topography such as the central face or scalp, he said in an interview. Still, of the 600 or so cases, none required conversion to another closure technique.
“The traditional closure technique would not have worked in those challenging cases,” Dr. Strasswimmer said. “In the most difficult situations, such as older patients with severely atrophic skin, even the best suturing won’t work. In that case, the Corseta at least produces a partial closure, thereby reducing the wound and accelerating healing.” The Corseta procedure is often coupled with tumescent anesthesia to decrease the risk of bleeding, particularly in patients on anticoagulation, he noted.
The conference was sponsored by the Skin Cancer Foundation.
EDINBURGH – Barbed absorbable sutures are a useful new tool to facilitate dermal closure of facial and nonfacial defects following tumor resection.
“These are not the bad old sutures that you might of heard about before, that were nonabsorbable sutures and attempted for use in cosmetic procedures,” Dr. John Strasswimmer said at the 15th World Congress on Cancers of the Skin.
Last year, Dr. Strasswimmer, medical director of melanoma and cutaneous oncology at the Lynn Cancer Institute in Boca Raton, Fla., reported his initial experience using a procedure he calls “Corseta” to close a large Mohs defect on the trunk of an 83-year-old man (JAMA Dermatol. 2013;149:853-4).
The procedure employs a barbed, bioabsorbable suture (Ethicon’s Stratafix and Covidien’s V-Loc) that is run in a continuous vertical looping manner in the subcutaneous layer, with minimal to no undermining of the wound. Undermining is typically used in cutaneous surgery to relieve tension or provide structure around anatomical landmarks, but it can increase the risk of bleeding, swelling, and patient discomfort, he said.
Instead, the first suture pass is placed in the deepest portion of the subcutaneous tissue and brought out within the more superficial subcutaneous layer. Each bite of the barbed suture extends peripherally at least 2.0 cm from the edge of the wound, so the point of tension is lateral to the wound margins. At every two passes, tension is placed evenly across the sutures to close the deepest layer of tissue and to engage the barbs, much like closing of a Victorian corset, Dr. Strasswimmer said.
The second arm of the suture is passed in a similar manner in the subcutaneous plane, superficial to the first pass.
“This is a lacing, not a suturing technique,” he said. “You get tissue approximation, but more importantly, because we’re bringing in all that deep tissue, you automatically get beautiful wound-edge eversion and very nice cosmetic results.”
Because the sutures have barbs cut into them, however, a 0-0 weight polydioxane or other absorbable material suture can have a breaking strength of a #2-0 suture. “You have to look very carefully at the manufacturer’s sizing and strength requirements,” Dr. Strasswimmer cautioned.
Since their initial case report, Dr. Strasswimmer and his colleagues have expanded use of the Corseta technique to more than 600 facial and nonfacial reconstructions. The Corseta procedure is not as helpful for curved topography such as the central face or scalp, he said in an interview. Still, of the 600 or so cases, none required conversion to another closure technique.
“The traditional closure technique would not have worked in those challenging cases,” Dr. Strasswimmer said. “In the most difficult situations, such as older patients with severely atrophic skin, even the best suturing won’t work. In that case, the Corseta at least produces a partial closure, thereby reducing the wound and accelerating healing.” The Corseta procedure is often coupled with tumescent anesthesia to decrease the risk of bleeding, particularly in patients on anticoagulation, he noted.
The conference was sponsored by the Skin Cancer Foundation.
EDINBURGH – Barbed absorbable sutures are a useful new tool to facilitate dermal closure of facial and nonfacial defects following tumor resection.
“These are not the bad old sutures that you might of heard about before, that were nonabsorbable sutures and attempted for use in cosmetic procedures,” Dr. John Strasswimmer said at the 15th World Congress on Cancers of the Skin.
Last year, Dr. Strasswimmer, medical director of melanoma and cutaneous oncology at the Lynn Cancer Institute in Boca Raton, Fla., reported his initial experience using a procedure he calls “Corseta” to close a large Mohs defect on the trunk of an 83-year-old man (JAMA Dermatol. 2013;149:853-4).
The procedure employs a barbed, bioabsorbable suture (Ethicon’s Stratafix and Covidien’s V-Loc) that is run in a continuous vertical looping manner in the subcutaneous layer, with minimal to no undermining of the wound. Undermining is typically used in cutaneous surgery to relieve tension or provide structure around anatomical landmarks, but it can increase the risk of bleeding, swelling, and patient discomfort, he said.
Instead, the first suture pass is placed in the deepest portion of the subcutaneous tissue and brought out within the more superficial subcutaneous layer. Each bite of the barbed suture extends peripherally at least 2.0 cm from the edge of the wound, so the point of tension is lateral to the wound margins. At every two passes, tension is placed evenly across the sutures to close the deepest layer of tissue and to engage the barbs, much like closing of a Victorian corset, Dr. Strasswimmer said.
The second arm of the suture is passed in a similar manner in the subcutaneous plane, superficial to the first pass.
“This is a lacing, not a suturing technique,” he said. “You get tissue approximation, but more importantly, because we’re bringing in all that deep tissue, you automatically get beautiful wound-edge eversion and very nice cosmetic results.”
Because the sutures have barbs cut into them, however, a 0-0 weight polydioxane or other absorbable material suture can have a breaking strength of a #2-0 suture. “You have to look very carefully at the manufacturer’s sizing and strength requirements,” Dr. Strasswimmer cautioned.
Since their initial case report, Dr. Strasswimmer and his colleagues have expanded use of the Corseta technique to more than 600 facial and nonfacial reconstructions. The Corseta procedure is not as helpful for curved topography such as the central face or scalp, he said in an interview. Still, of the 600 or so cases, none required conversion to another closure technique.
“The traditional closure technique would not have worked in those challenging cases,” Dr. Strasswimmer said. “In the most difficult situations, such as older patients with severely atrophic skin, even the best suturing won’t work. In that case, the Corseta at least produces a partial closure, thereby reducing the wound and accelerating healing.” The Corseta procedure is often coupled with tumescent anesthesia to decrease the risk of bleeding, particularly in patients on anticoagulation, he noted.
The conference was sponsored by the Skin Cancer Foundation.
EXPERT ANALYSIS FROM WCCS 2014
VIDEO: Laser's novel effect improves restrictive burn scars
PHOENIX – New techniques using very-low-density, very-high-energy ablative fractional carbon dioxide laser are helping thousands of patients – mostly soldiers – with restrictive scars from bombs or burns.
It’s a treatment to which the far larger number of civilian burn patients should have access, but few do, explained Dr. Nathan S. Uebelhoer, who received an award and a standing ovation at the annual meeting of the American Society for Laser Medicine and Surgery for his work in this area.
In an interview, Dr. Uebelhoer of Aroostook Medical Center, Presque Isle, Maine, describes the techniques used to achieve such promising results with restrictive scars, and he discusses what might be necessary to make the treatment more widely available.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
PHOENIX – New techniques using very-low-density, very-high-energy ablative fractional carbon dioxide laser are helping thousands of patients – mostly soldiers – with restrictive scars from bombs or burns.
It’s a treatment to which the far larger number of civilian burn patients should have access, but few do, explained Dr. Nathan S. Uebelhoer, who received an award and a standing ovation at the annual meeting of the American Society for Laser Medicine and Surgery for his work in this area.
In an interview, Dr. Uebelhoer of Aroostook Medical Center, Presque Isle, Maine, describes the techniques used to achieve such promising results with restrictive scars, and he discusses what might be necessary to make the treatment more widely available.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
PHOENIX – New techniques using very-low-density, very-high-energy ablative fractional carbon dioxide laser are helping thousands of patients – mostly soldiers – with restrictive scars from bombs or burns.
It’s a treatment to which the far larger number of civilian burn patients should have access, but few do, explained Dr. Nathan S. Uebelhoer, who received an award and a standing ovation at the annual meeting of the American Society for Laser Medicine and Surgery for his work in this area.
In an interview, Dr. Uebelhoer of Aroostook Medical Center, Presque Isle, Maine, describes the techniques used to achieve such promising results with restrictive scars, and he discusses what might be necessary to make the treatment more widely available.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT LASER 2014
















