User login
Commentary: New Results With DMARD in RA, October 2022
Interleukin (IL)–6 is known to be of great importance in the pathogenesis of rheumatoid arthritis (RA) owing to its role in the inflammatory response. Current IL-6-directed therapies in RA, namely sarilumab and tocilizumab, target the receptor. In a double-blind randomized controlled trial with both placebo and active comparators, Smolen and colleagues evaluated the efficacy of olokizumab, which directly binds and inhibits the activity of IL-6, in combination with methotrexate, in the treatment of people with RA. Patients were treated with methotrexate alone or in combination with adalimumab or olokizumab, and clinical outcomes were evaluated after 12 weeks, a relatively short time frame. Olokizumab was noninferior to adalimumab in terms of the proportion of patients achieving an American College of Rheumatology 20 response, with similar rates of serious adverse events, the most common of which was infection. Though this study included patients from across the globe, the percentage of Black and Asian patients was relatively low and thus may affect the generalizability of this study to a US population; the numbers of patients in each group was also relatively small. These results certainly warrant larger-scale and longer studies to evaluate olokizumab's efficacy.
For those patients with RA who achieve sustained disease remission, the question of medication tapering has been raised as a possible strategy for minimizing risks for therapy. Using insurance database information, Birkner and colleagues performed a prospective cohort study of over 400 patients in Germany. Using shared decision-making between patients and their rheumatologists, two groups of patients were followed: 237 people who elected to remain on therapy and 200 who decided to taper medication. Of note, similar proportions of patients in both groups were taking conventional and biologic disease-modifying antirheumatic drug (DMARD) monotherapy, but more patients in the tapering group were taking a combination therapy with both. Flares and loss of remission were more common in the continuation group, a difference that did not persist after adjusting for patient risk characteristics. Overall, results from this "real-world" study were consistent with prior studies and support the possibility of tapering with flare in a subset of patients. Although the authors address the potential for selection bias in terms of patients "assigned" to each group, this can also be viewed as part of the shared decision-making in determining the appropriateness of tapering therapy in individual patients.
Because people receiving rituximab have experienced more severe COVID-19, studies aimed at enhancing the protection of these patients are of current interest. Of note, in a follow-up to a prior observational study by van der Togt and colleagues on the response to COVID-19 vaccines in people with RA being treated with rituximab, they looked at responses to the third (booster) dose of the COVID-19 vaccine. Only about 20% of patients treated with rituximab developed a humoral response to a third vaccine dose, as defined by immunoglobulins (Ig; total, IgG, and IgM) against SARS-CoV-2. Patients treated with 200 mg rituximab had a higher response rate than did those treated with 500 mg or 1000 mg, though this difference was not statistically significant. The study lacked a control arm of people being treated with other DMARD and also did not measure B-cell counts, COVID-19, or outcomes. Reassuringly, those patients who did have a positive humoral response to the first two vaccine doses tended to maintain a humoral response to the third, regardless of rituximab dose or timing.
Interleukin (IL)–6 is known to be of great importance in the pathogenesis of rheumatoid arthritis (RA) owing to its role in the inflammatory response. Current IL-6-directed therapies in RA, namely sarilumab and tocilizumab, target the receptor. In a double-blind randomized controlled trial with both placebo and active comparators, Smolen and colleagues evaluated the efficacy of olokizumab, which directly binds and inhibits the activity of IL-6, in combination with methotrexate, in the treatment of people with RA. Patients were treated with methotrexate alone or in combination with adalimumab or olokizumab, and clinical outcomes were evaluated after 12 weeks, a relatively short time frame. Olokizumab was noninferior to adalimumab in terms of the proportion of patients achieving an American College of Rheumatology 20 response, with similar rates of serious adverse events, the most common of which was infection. Though this study included patients from across the globe, the percentage of Black and Asian patients was relatively low and thus may affect the generalizability of this study to a US population; the numbers of patients in each group was also relatively small. These results certainly warrant larger-scale and longer studies to evaluate olokizumab's efficacy.
For those patients with RA who achieve sustained disease remission, the question of medication tapering has been raised as a possible strategy for minimizing risks for therapy. Using insurance database information, Birkner and colleagues performed a prospective cohort study of over 400 patients in Germany. Using shared decision-making between patients and their rheumatologists, two groups of patients were followed: 237 people who elected to remain on therapy and 200 who decided to taper medication. Of note, similar proportions of patients in both groups were taking conventional and biologic disease-modifying antirheumatic drug (DMARD) monotherapy, but more patients in the tapering group were taking a combination therapy with both. Flares and loss of remission were more common in the continuation group, a difference that did not persist after adjusting for patient risk characteristics. Overall, results from this "real-world" study were consistent with prior studies and support the possibility of tapering with flare in a subset of patients. Although the authors address the potential for selection bias in terms of patients "assigned" to each group, this can also be viewed as part of the shared decision-making in determining the appropriateness of tapering therapy in individual patients.
Because people receiving rituximab have experienced more severe COVID-19, studies aimed at enhancing the protection of these patients are of current interest. Of note, in a follow-up to a prior observational study by van der Togt and colleagues on the response to COVID-19 vaccines in people with RA being treated with rituximab, they looked at responses to the third (booster) dose of the COVID-19 vaccine. Only about 20% of patients treated with rituximab developed a humoral response to a third vaccine dose, as defined by immunoglobulins (Ig; total, IgG, and IgM) against SARS-CoV-2. Patients treated with 200 mg rituximab had a higher response rate than did those treated with 500 mg or 1000 mg, though this difference was not statistically significant. The study lacked a control arm of people being treated with other DMARD and also did not measure B-cell counts, COVID-19, or outcomes. Reassuringly, those patients who did have a positive humoral response to the first two vaccine doses tended to maintain a humoral response to the third, regardless of rituximab dose or timing.
Interleukin (IL)–6 is known to be of great importance in the pathogenesis of rheumatoid arthritis (RA) owing to its role in the inflammatory response. Current IL-6-directed therapies in RA, namely sarilumab and tocilizumab, target the receptor. In a double-blind randomized controlled trial with both placebo and active comparators, Smolen and colleagues evaluated the efficacy of olokizumab, which directly binds and inhibits the activity of IL-6, in combination with methotrexate, in the treatment of people with RA. Patients were treated with methotrexate alone or in combination with adalimumab or olokizumab, and clinical outcomes were evaluated after 12 weeks, a relatively short time frame. Olokizumab was noninferior to adalimumab in terms of the proportion of patients achieving an American College of Rheumatology 20 response, with similar rates of serious adverse events, the most common of which was infection. Though this study included patients from across the globe, the percentage of Black and Asian patients was relatively low and thus may affect the generalizability of this study to a US population; the numbers of patients in each group was also relatively small. These results certainly warrant larger-scale and longer studies to evaluate olokizumab's efficacy.
For those patients with RA who achieve sustained disease remission, the question of medication tapering has been raised as a possible strategy for minimizing risks for therapy. Using insurance database information, Birkner and colleagues performed a prospective cohort study of over 400 patients in Germany. Using shared decision-making between patients and their rheumatologists, two groups of patients were followed: 237 people who elected to remain on therapy and 200 who decided to taper medication. Of note, similar proportions of patients in both groups were taking conventional and biologic disease-modifying antirheumatic drug (DMARD) monotherapy, but more patients in the tapering group were taking a combination therapy with both. Flares and loss of remission were more common in the continuation group, a difference that did not persist after adjusting for patient risk characteristics. Overall, results from this "real-world" study were consistent with prior studies and support the possibility of tapering with flare in a subset of patients. Although the authors address the potential for selection bias in terms of patients "assigned" to each group, this can also be viewed as part of the shared decision-making in determining the appropriateness of tapering therapy in individual patients.
Because people receiving rituximab have experienced more severe COVID-19, studies aimed at enhancing the protection of these patients are of current interest. Of note, in a follow-up to a prior observational study by van der Togt and colleagues on the response to COVID-19 vaccines in people with RA being treated with rituximab, they looked at responses to the third (booster) dose of the COVID-19 vaccine. Only about 20% of patients treated with rituximab developed a humoral response to a third vaccine dose, as defined by immunoglobulins (Ig; total, IgG, and IgM) against SARS-CoV-2. Patients treated with 200 mg rituximab had a higher response rate than did those treated with 500 mg or 1000 mg, though this difference was not statistically significant. The study lacked a control arm of people being treated with other DMARD and also did not measure B-cell counts, COVID-19, or outcomes. Reassuringly, those patients who did have a positive humoral response to the first two vaccine doses tended to maintain a humoral response to the third, regardless of rituximab dose or timing.
Meet the JCOM Author with Dr. Barkoudah: Improving Inpatient COVID-19 Vaccination Rates
Complete endoscopic healing key when stopping anti-TNFs in IBD
The level of remission in patients with remitting inflammatory bowel disease (IBD) appears to play a major role in whether they will relapse after treatment when biologic therapies are discontinued, according to a new prospective study.
Patients with complete endoscopic healing have half the rate of relapse after withdrawal of anti-tumor necrosis factor alpha (anti-TNF) treatment than those with only partial healing, according to a study published online in Clinical Gastroenterology and Hepatology.
“Applying strict criteria for endoscopic healing and mesalamine treatment ... may lower the risk of relapse after withdrawal of anti-TNF treatment,” write Bas Oldenburg, MD, PhD, a professor at University Medical Center Utrecht, the Netherlands, and colleagues in their analysis of 81 patients.
De-escalation of anti-TNF treatment in IBD patients in remission has the potential to “reduce side effects, including risks of serious infections and malignancies, decrease health care expenditures, and meet patients’ preferences,” they note.
However, withdrawal of the drugs increases the risk of relapse by 30%-45% at 12 months. When patients relapse, reintroduction of anti-TNF therapy returns over 80% to remission.
Although no consensus exists on how to select patients for therapy de-escalation, evidence suggests that persistent inflammation affects outcomes and that the “depth” of endoscopic healing is a key indicator, the authors note.
Study details
To further the knowledge base, they conducted a prospective study of patients in remission to determine the relapse rate following de-escalation of anti-TNF therapy; evaluate relapse factors, including degree of endoscopic healing; and assess outcomes after reintroduction of anti-TNF therapy.
The study was limited to adult patients with IBD with at least 6 months of corticosteroid-free clinical remission, confirmed baseline clinical remission and endoscopic healing, no current hospitalization, and no pregnancy.
The patients underwent elective discontinuation of anti-TNF therapy between 2018 and 2020. The recommended protocol was to measure C-reactive protein (CRP) and fecal calprotectin at 3, 6, 12, and 24 months and to perform endoscopy at 12 months.
Patients also completed questionnaires at baseline and at 3, 6, 12, and 24 months. The authors selected the patient–Harvey-Bradshaw Index for patients with Crohn’s disease and the patient–Simple Clinical Colitis Activity Index for patients with ulcerative colitis and unclassified IBD, as well as the short IBD Quality of Life measure.
Of the 81 patients from 13 centers who took part, 51% had Crohn’s disease. The median duration of remission at baseline was 3.5 years, and the median disease duration was 9.1 years.
All patients had evidence of endoscopic healing, and 88% met the strict criteria for complete endoscopic healing. In 34%, trough levels of anti-TNF treatments were judged to be subtherapeutic.
After withdrawal of the drugs, 25.9% of patients continued on immunomodulators.
Over a median follow-up of 2 years, 49% of patients relapsed, which was confirmed via endoscopy, fecal calprotectin, or CRP in 83% of cases and inferred from treatment escalation for clinical flare in 17%. Rates of relapse were comparable between patients with Crohn’s disease and ulcerative colitis or unclassified IBD and between those discontinuing adalimumab and those stopping infliximab.
Better healing, better outcomes
However, analysis showed that partial endoscopic healing was independently associated with a higher risk of relapse, at an adjusted hazard ratio versus complete endoscopic healing of 3.28.
At 12 months, 70% of patients with partial endoscopic healing had relapsed versus 35% of those with complete endoscopic healing.
Treatment with the anti-inflammatory agent mesalamine (multiple brands) was independently associated with a reduced risk of relapse, at an adjusted hazard ratio of 0.08. No other potential predictors of relapse were identified.
Of the patients who relapsed, 75% restarted anti-TNF treatment, and the majority (87%) were restarted on the same agent at a median of 0.9 years since its withdrawal and a median of 24 days since the onset of relapse.
Clinical remission was achieved at 3 months in 73% of patients who restarted anti-TNF therapy, which was found to restore quality of life and well-being in relapsed patients, the authors report.
Reluctance remains
Stephen B. Hanauer, MD, professor of medicine (gastroenterology and hepatology) at Northwestern University Feinberg School of Medicine, Chicago, said the findings “reinforce the benefits of the maintenance versus the withdrawal of therapy” and “the deeper the remission” the more likely it is to be sustained.
The 35% relapse rate at 12 months, even in patients with compete endoscopic healing, indicates that treatment should be maintained, Dr. Hanauer said.
“What is also relevant, but was not evaluated, is the additional endpoint of histologic healing, which is likely to sustain remissions even longer,” he added.
Nevertheless, Dr. Hanauer said, the “observed relapse rate is important to discuss in shared decision-making with patients.”
The findings are interesting, but the study didn’t follow the patients for long enough to understand why 35% of those with complete endoscopic healing relapsed, Miguel Regueiro, MD, chair of the Cleveland Clinic’s Digestive Disease & Surgery Institute, told this news organization.
“Are there predictors, factors, or other treatments that could be used to reduce that 35% risk of relapse further?” he questioned.
Although the study didn’t clear up that question for Dr. Regueiro, he found it compelling that mesalamine continuation resulted in higher rates of sustained remission after anti-TNF withdrawal among patients with ulcerative colitis.
Dr. Regueiro said that he will not begin recommending withdrawal of advanced therapies, including anti-TNF drugs, in patients who have achieved a stable remission.
“We have not yet found the cure for IBD, and my concern is that patients may relapse with more severe disease than previously and that recurrence of inflammation could have potential risks for complications,” he said.
“Nonetheless, this study is intriguing and important, and at least prompts the discussion of withdrawing therapy in those who have achieved a deep endoscopic remission for a sustained period of time,” Dr. Regueiro added.
The study received support from the Dutch Health Insurance Innovation Fund.
Dr. Oldenburg declares relationships with AbbVie, Celltrion, Ferring, Takeda, Galapagos, Pfizer, Cablon, PBMS, Janssen, and MSD. Other authors also declare numerous relationships. The full list can be found with the original article. Dr. Hanauer declares relationships with AbbVie, Janssen, Pfizer, and Boehringer Ingelheim. Dr. Regueiro declares relationships with AbbVie, Janssen, UCB, Takeda, Pfizer, Miraca Labs, Amgen, Celgene, Seres, Allergan, Genentech, Gilead, Salix, Prometheus, Lilly, TARGET Pharma Solutions, ALFASIGMA, S.p.A., BMS, CME Outfitters, Imedex, GI Health Foundation, Cornerstones, Remedy, MJH Life Sciences, Medscape, MDEducation, WebMD, and HMPGlobal.
Help your patients better understand their IBD treatment options by sharing AGA’s patient education, “Living with IBD,” in the AGA GI Patient Center at www.gastro.org/IBD.
A version of this article first appeared on Medscape.com.
The level of remission in patients with remitting inflammatory bowel disease (IBD) appears to play a major role in whether they will relapse after treatment when biologic therapies are discontinued, according to a new prospective study.
Patients with complete endoscopic healing have half the rate of relapse after withdrawal of anti-tumor necrosis factor alpha (anti-TNF) treatment than those with only partial healing, according to a study published online in Clinical Gastroenterology and Hepatology.
“Applying strict criteria for endoscopic healing and mesalamine treatment ... may lower the risk of relapse after withdrawal of anti-TNF treatment,” write Bas Oldenburg, MD, PhD, a professor at University Medical Center Utrecht, the Netherlands, and colleagues in their analysis of 81 patients.
De-escalation of anti-TNF treatment in IBD patients in remission has the potential to “reduce side effects, including risks of serious infections and malignancies, decrease health care expenditures, and meet patients’ preferences,” they note.
However, withdrawal of the drugs increases the risk of relapse by 30%-45% at 12 months. When patients relapse, reintroduction of anti-TNF therapy returns over 80% to remission.
Although no consensus exists on how to select patients for therapy de-escalation, evidence suggests that persistent inflammation affects outcomes and that the “depth” of endoscopic healing is a key indicator, the authors note.
Study details
To further the knowledge base, they conducted a prospective study of patients in remission to determine the relapse rate following de-escalation of anti-TNF therapy; evaluate relapse factors, including degree of endoscopic healing; and assess outcomes after reintroduction of anti-TNF therapy.
The study was limited to adult patients with IBD with at least 6 months of corticosteroid-free clinical remission, confirmed baseline clinical remission and endoscopic healing, no current hospitalization, and no pregnancy.
The patients underwent elective discontinuation of anti-TNF therapy between 2018 and 2020. The recommended protocol was to measure C-reactive protein (CRP) and fecal calprotectin at 3, 6, 12, and 24 months and to perform endoscopy at 12 months.
Patients also completed questionnaires at baseline and at 3, 6, 12, and 24 months. The authors selected the patient–Harvey-Bradshaw Index for patients with Crohn’s disease and the patient–Simple Clinical Colitis Activity Index for patients with ulcerative colitis and unclassified IBD, as well as the short IBD Quality of Life measure.
Of the 81 patients from 13 centers who took part, 51% had Crohn’s disease. The median duration of remission at baseline was 3.5 years, and the median disease duration was 9.1 years.
All patients had evidence of endoscopic healing, and 88% met the strict criteria for complete endoscopic healing. In 34%, trough levels of anti-TNF treatments were judged to be subtherapeutic.
After withdrawal of the drugs, 25.9% of patients continued on immunomodulators.
Over a median follow-up of 2 years, 49% of patients relapsed, which was confirmed via endoscopy, fecal calprotectin, or CRP in 83% of cases and inferred from treatment escalation for clinical flare in 17%. Rates of relapse were comparable between patients with Crohn’s disease and ulcerative colitis or unclassified IBD and between those discontinuing adalimumab and those stopping infliximab.
Better healing, better outcomes
However, analysis showed that partial endoscopic healing was independently associated with a higher risk of relapse, at an adjusted hazard ratio versus complete endoscopic healing of 3.28.
At 12 months, 70% of patients with partial endoscopic healing had relapsed versus 35% of those with complete endoscopic healing.
Treatment with the anti-inflammatory agent mesalamine (multiple brands) was independently associated with a reduced risk of relapse, at an adjusted hazard ratio of 0.08. No other potential predictors of relapse were identified.
Of the patients who relapsed, 75% restarted anti-TNF treatment, and the majority (87%) were restarted on the same agent at a median of 0.9 years since its withdrawal and a median of 24 days since the onset of relapse.
Clinical remission was achieved at 3 months in 73% of patients who restarted anti-TNF therapy, which was found to restore quality of life and well-being in relapsed patients, the authors report.
Reluctance remains
Stephen B. Hanauer, MD, professor of medicine (gastroenterology and hepatology) at Northwestern University Feinberg School of Medicine, Chicago, said the findings “reinforce the benefits of the maintenance versus the withdrawal of therapy” and “the deeper the remission” the more likely it is to be sustained.
The 35% relapse rate at 12 months, even in patients with compete endoscopic healing, indicates that treatment should be maintained, Dr. Hanauer said.
“What is also relevant, but was not evaluated, is the additional endpoint of histologic healing, which is likely to sustain remissions even longer,” he added.
Nevertheless, Dr. Hanauer said, the “observed relapse rate is important to discuss in shared decision-making with patients.”
The findings are interesting, but the study didn’t follow the patients for long enough to understand why 35% of those with complete endoscopic healing relapsed, Miguel Regueiro, MD, chair of the Cleveland Clinic’s Digestive Disease & Surgery Institute, told this news organization.
“Are there predictors, factors, or other treatments that could be used to reduce that 35% risk of relapse further?” he questioned.
Although the study didn’t clear up that question for Dr. Regueiro, he found it compelling that mesalamine continuation resulted in higher rates of sustained remission after anti-TNF withdrawal among patients with ulcerative colitis.
Dr. Regueiro said that he will not begin recommending withdrawal of advanced therapies, including anti-TNF drugs, in patients who have achieved a stable remission.
“We have not yet found the cure for IBD, and my concern is that patients may relapse with more severe disease than previously and that recurrence of inflammation could have potential risks for complications,” he said.
“Nonetheless, this study is intriguing and important, and at least prompts the discussion of withdrawing therapy in those who have achieved a deep endoscopic remission for a sustained period of time,” Dr. Regueiro added.
The study received support from the Dutch Health Insurance Innovation Fund.
Dr. Oldenburg declares relationships with AbbVie, Celltrion, Ferring, Takeda, Galapagos, Pfizer, Cablon, PBMS, Janssen, and MSD. Other authors also declare numerous relationships. The full list can be found with the original article. Dr. Hanauer declares relationships with AbbVie, Janssen, Pfizer, and Boehringer Ingelheim. Dr. Regueiro declares relationships with AbbVie, Janssen, UCB, Takeda, Pfizer, Miraca Labs, Amgen, Celgene, Seres, Allergan, Genentech, Gilead, Salix, Prometheus, Lilly, TARGET Pharma Solutions, ALFASIGMA, S.p.A., BMS, CME Outfitters, Imedex, GI Health Foundation, Cornerstones, Remedy, MJH Life Sciences, Medscape, MDEducation, WebMD, and HMPGlobal.
Help your patients better understand their IBD treatment options by sharing AGA’s patient education, “Living with IBD,” in the AGA GI Patient Center at www.gastro.org/IBD.
A version of this article first appeared on Medscape.com.
The level of remission in patients with remitting inflammatory bowel disease (IBD) appears to play a major role in whether they will relapse after treatment when biologic therapies are discontinued, according to a new prospective study.
Patients with complete endoscopic healing have half the rate of relapse after withdrawal of anti-tumor necrosis factor alpha (anti-TNF) treatment than those with only partial healing, according to a study published online in Clinical Gastroenterology and Hepatology.
“Applying strict criteria for endoscopic healing and mesalamine treatment ... may lower the risk of relapse after withdrawal of anti-TNF treatment,” write Bas Oldenburg, MD, PhD, a professor at University Medical Center Utrecht, the Netherlands, and colleagues in their analysis of 81 patients.
De-escalation of anti-TNF treatment in IBD patients in remission has the potential to “reduce side effects, including risks of serious infections and malignancies, decrease health care expenditures, and meet patients’ preferences,” they note.
However, withdrawal of the drugs increases the risk of relapse by 30%-45% at 12 months. When patients relapse, reintroduction of anti-TNF therapy returns over 80% to remission.
Although no consensus exists on how to select patients for therapy de-escalation, evidence suggests that persistent inflammation affects outcomes and that the “depth” of endoscopic healing is a key indicator, the authors note.
Study details
To further the knowledge base, they conducted a prospective study of patients in remission to determine the relapse rate following de-escalation of anti-TNF therapy; evaluate relapse factors, including degree of endoscopic healing; and assess outcomes after reintroduction of anti-TNF therapy.
The study was limited to adult patients with IBD with at least 6 months of corticosteroid-free clinical remission, confirmed baseline clinical remission and endoscopic healing, no current hospitalization, and no pregnancy.
The patients underwent elective discontinuation of anti-TNF therapy between 2018 and 2020. The recommended protocol was to measure C-reactive protein (CRP) and fecal calprotectin at 3, 6, 12, and 24 months and to perform endoscopy at 12 months.
Patients also completed questionnaires at baseline and at 3, 6, 12, and 24 months. The authors selected the patient–Harvey-Bradshaw Index for patients with Crohn’s disease and the patient–Simple Clinical Colitis Activity Index for patients with ulcerative colitis and unclassified IBD, as well as the short IBD Quality of Life measure.
Of the 81 patients from 13 centers who took part, 51% had Crohn’s disease. The median duration of remission at baseline was 3.5 years, and the median disease duration was 9.1 years.
All patients had evidence of endoscopic healing, and 88% met the strict criteria for complete endoscopic healing. In 34%, trough levels of anti-TNF treatments were judged to be subtherapeutic.
After withdrawal of the drugs, 25.9% of patients continued on immunomodulators.
Over a median follow-up of 2 years, 49% of patients relapsed, which was confirmed via endoscopy, fecal calprotectin, or CRP in 83% of cases and inferred from treatment escalation for clinical flare in 17%. Rates of relapse were comparable between patients with Crohn’s disease and ulcerative colitis or unclassified IBD and between those discontinuing adalimumab and those stopping infliximab.
Better healing, better outcomes
However, analysis showed that partial endoscopic healing was independently associated with a higher risk of relapse, at an adjusted hazard ratio versus complete endoscopic healing of 3.28.
At 12 months, 70% of patients with partial endoscopic healing had relapsed versus 35% of those with complete endoscopic healing.
Treatment with the anti-inflammatory agent mesalamine (multiple brands) was independently associated with a reduced risk of relapse, at an adjusted hazard ratio of 0.08. No other potential predictors of relapse were identified.
Of the patients who relapsed, 75% restarted anti-TNF treatment, and the majority (87%) were restarted on the same agent at a median of 0.9 years since its withdrawal and a median of 24 days since the onset of relapse.
Clinical remission was achieved at 3 months in 73% of patients who restarted anti-TNF therapy, which was found to restore quality of life and well-being in relapsed patients, the authors report.
Reluctance remains
Stephen B. Hanauer, MD, professor of medicine (gastroenterology and hepatology) at Northwestern University Feinberg School of Medicine, Chicago, said the findings “reinforce the benefits of the maintenance versus the withdrawal of therapy” and “the deeper the remission” the more likely it is to be sustained.
The 35% relapse rate at 12 months, even in patients with compete endoscopic healing, indicates that treatment should be maintained, Dr. Hanauer said.
“What is also relevant, but was not evaluated, is the additional endpoint of histologic healing, which is likely to sustain remissions even longer,” he added.
Nevertheless, Dr. Hanauer said, the “observed relapse rate is important to discuss in shared decision-making with patients.”
The findings are interesting, but the study didn’t follow the patients for long enough to understand why 35% of those with complete endoscopic healing relapsed, Miguel Regueiro, MD, chair of the Cleveland Clinic’s Digestive Disease & Surgery Institute, told this news organization.
“Are there predictors, factors, or other treatments that could be used to reduce that 35% risk of relapse further?” he questioned.
Although the study didn’t clear up that question for Dr. Regueiro, he found it compelling that mesalamine continuation resulted in higher rates of sustained remission after anti-TNF withdrawal among patients with ulcerative colitis.
Dr. Regueiro said that he will not begin recommending withdrawal of advanced therapies, including anti-TNF drugs, in patients who have achieved a stable remission.
“We have not yet found the cure for IBD, and my concern is that patients may relapse with more severe disease than previously and that recurrence of inflammation could have potential risks for complications,” he said.
“Nonetheless, this study is intriguing and important, and at least prompts the discussion of withdrawing therapy in those who have achieved a deep endoscopic remission for a sustained period of time,” Dr. Regueiro added.
The study received support from the Dutch Health Insurance Innovation Fund.
Dr. Oldenburg declares relationships with AbbVie, Celltrion, Ferring, Takeda, Galapagos, Pfizer, Cablon, PBMS, Janssen, and MSD. Other authors also declare numerous relationships. The full list can be found with the original article. Dr. Hanauer declares relationships with AbbVie, Janssen, Pfizer, and Boehringer Ingelheim. Dr. Regueiro declares relationships with AbbVie, Janssen, UCB, Takeda, Pfizer, Miraca Labs, Amgen, Celgene, Seres, Allergan, Genentech, Gilead, Salix, Prometheus, Lilly, TARGET Pharma Solutions, ALFASIGMA, S.p.A., BMS, CME Outfitters, Imedex, GI Health Foundation, Cornerstones, Remedy, MJH Life Sciences, Medscape, MDEducation, WebMD, and HMPGlobal.
Help your patients better understand their IBD treatment options by sharing AGA’s patient education, “Living with IBD,” in the AGA GI Patient Center at www.gastro.org/IBD.
A version of this article first appeared on Medscape.com.
GERD linked to increased risk of nontuberculous mycobacterial pulmonary disease
Patients with gastrointestinal esophageal reflux disease (GERD) have more than three times the risk of developing nontuberculous mycobacterial pulmonary disease (NTM-PD), compared with those without GERD, according to a population-based retrospective cohort study.
“GERD is a common comorbidity of nontuberculous mycobacterial pulmonary disease [but] whether GERD is associated with an increased risk of developing NTM-PD is unknown,” Hayoung Choi, MD, PhD, Hallym University, Seoul, Republic of Korea, and colleagues reported.
Dr. Choi added in an email. “What needs to be understood is that GERD increases health care utilization in patients with NTM pulmonary disease; hence, clinicians who treat patients with NTM pulmonary disease need to be aware of the burden of GERD and treat the gastrointestinal illness simultaneously,” he added.
The study was published online in the journal CHEST.
Sample cohort
Data from the Korean National Health Insurance Service-National Sample Cohort between 2002 and 2015 were used to assess the impact of GERD on NTM-PD. The incidence and risk of NTM-PD were compared between 17,424 patients with GERD and 69,000 patients without GERD in a matched cohort. GERD was defined as patients having received more than 3 months of proton pump inhibitors (PPIs).
During a median follow-up of 5.1 years, the age- and sex-adjusted incidence of NTM-PD was significantly higher in the GERD cohort, at a rate of 34.8/100,000 person-years, than in the matched cohort, at a rate of only 10.5/100,000 person-years (P < .001), the authors reported.
As for risk factors for NTM-PD, being 60 years of age and older was associated with a 3.5-times higher risk of NTM-PD at an adjusted hazard ratio of 3.57 (95% confidence interval, 1.58-8.07), while bronchiectasis was associated with over an 18-times higher risk of NTM-PD in the GERD cohort at an adjusted HR of 18.69 (95% CI, 6.68-552.28). Those with GERD who developed NTM-PD had higher all-cause and respiratory disease–related emergency department visits or hospitalizations compared with patients with GERD who did not develop NTM-PD (P = .011), the investigators noted.
As the authors pointed out, the incidence of NTM-PD in the Korean population ranged from 6 to 19 cases/100,000 between 2008 and 2016; thus, the burden of incident NTM-PD associated with GERD appears to be considerable. As Dr. Choi explained, a combination of three factors influenced the development of NTM infections. The first is environmental, from water source, climate, or region; the second is patient influences, including such factors as immunodeficiency and comorbidities (including bronchiectasis); and the third is microbiological factors, including various NTM species.
Bile aspirating into the lung during GERD may be another possible pathway, as the authors suggested. Even if acid secretion is suppressed by PPI treatment in patients with GERD, NTM-PD may be induced or aggravated through mechanisms such as bile reflux. The fact that patients over the age of 60 were more prone to develop NTM-PD suggests that a decrease in gastric emptying and increased micro-aspiration or reflux associated with impaired swallowing (which are more common in elderly patients) may also be at play.
“Bronchiectasis is also a very well known risk factor for NTM pulmonary disease,” Dr. Choi emphasized. Thus, he recommends clinicians carefully observe clinical, radiological, and microbiological changes to detect NTM pulmonary disease when managing patients with bronchiectasis.
“The results of the present study have several potential clinical implications,” Dr. Choi and colleagues observed. First, NTM-PD should be suspected when new-onset worsening of respiratory symptoms develops during regular follow-up in patients with GERD. Second, because results indicate that older age and bronchiectasis significantly increase the risk of NTM-PD, “more active strategies (e.g., screening of symptoms and regular chest x-rays)” might be helpful in patients with GERD and these risk factors, the authors suggested. Because patients with GERD who developed NTM-PD had more respiratory disease–related ED visits and hospitalizations than those who did not develop NTM-PD, when GERD and NTM-PD are combined, clinicians should focus on the variations of respiratory symptoms, they suggested.
The authors cautioned, however, that because the study was one in a Korean population, studies in other countries and different ethnicities are needed before findings can be generalized.
More common than TB
Asked to comment on the findings, NTM-PD expert Theodore Marras, MD, clinician investigator, Krembil Research Institute, Toronto, noted that non-TB M-PD is about 10 times more common than TB and that could be an underestimate as there have been very large increases in the incidence of NTM-PD in recent years. “It’s an environmental germ – it’s in our water – and certain people are particularly susceptible to it, typically older age women who have underlying bronchiectasis,” Dr. Marras told this news organization. “And while there are ethnic differences in incidence rates between East Asian people and Black African people, immigration is not the main driver for the increase as far as we can tell,” he said.
He personally treats a lot of NTM-PD and he also believes that GERD is an important risk factor for all types of lung infections including NTM lung disease. “So without a doubt, I believe that GERD should be treated in patients with NTM-PD,” Dr. Marras emphasized. The big question is how to treat GERD, as there may be concerns with acid-suppressive agents such as proton pump inhibitors that “the reflux that comes back up may harbor more germs in it and if that reflux comes up high enough, we are at risk of aspirating some of that fluid into our lungs, especially when we’re asleep,” he said.
Some experts therefore argue in favor of using motility agents instead of PPIs. However, if Dr. Marras has a patient with heartburn, “you have to treat it,” he stressed. Similarly, if a patient has evidence of esophageal erosions, physicians need to treat those as well. However, if neither feature is present, “I tend to like the motility agents preferentially or use them in combination with a PPI,” Dr. Marras said.
Dr. Marras also thinks the study is encouraging physicians involved in treating these patients to think about controlling GERD both when they are treating patients and after they are treated to try to reduce recurrence.
The authors had no financial disclosures to make. Dr. Marras has given several talks on NTM lung disease, one sponsored by AstraZeneca and the other by Novartis.
Patients with gastrointestinal esophageal reflux disease (GERD) have more than three times the risk of developing nontuberculous mycobacterial pulmonary disease (NTM-PD), compared with those without GERD, according to a population-based retrospective cohort study.
“GERD is a common comorbidity of nontuberculous mycobacterial pulmonary disease [but] whether GERD is associated with an increased risk of developing NTM-PD is unknown,” Hayoung Choi, MD, PhD, Hallym University, Seoul, Republic of Korea, and colleagues reported.
Dr. Choi added in an email. “What needs to be understood is that GERD increases health care utilization in patients with NTM pulmonary disease; hence, clinicians who treat patients with NTM pulmonary disease need to be aware of the burden of GERD and treat the gastrointestinal illness simultaneously,” he added.
The study was published online in the journal CHEST.
Sample cohort
Data from the Korean National Health Insurance Service-National Sample Cohort between 2002 and 2015 were used to assess the impact of GERD on NTM-PD. The incidence and risk of NTM-PD were compared between 17,424 patients with GERD and 69,000 patients without GERD in a matched cohort. GERD was defined as patients having received more than 3 months of proton pump inhibitors (PPIs).
During a median follow-up of 5.1 years, the age- and sex-adjusted incidence of NTM-PD was significantly higher in the GERD cohort, at a rate of 34.8/100,000 person-years, than in the matched cohort, at a rate of only 10.5/100,000 person-years (P < .001), the authors reported.
As for risk factors for NTM-PD, being 60 years of age and older was associated with a 3.5-times higher risk of NTM-PD at an adjusted hazard ratio of 3.57 (95% confidence interval, 1.58-8.07), while bronchiectasis was associated with over an 18-times higher risk of NTM-PD in the GERD cohort at an adjusted HR of 18.69 (95% CI, 6.68-552.28). Those with GERD who developed NTM-PD had higher all-cause and respiratory disease–related emergency department visits or hospitalizations compared with patients with GERD who did not develop NTM-PD (P = .011), the investigators noted.
As the authors pointed out, the incidence of NTM-PD in the Korean population ranged from 6 to 19 cases/100,000 between 2008 and 2016; thus, the burden of incident NTM-PD associated with GERD appears to be considerable. As Dr. Choi explained, a combination of three factors influenced the development of NTM infections. The first is environmental, from water source, climate, or region; the second is patient influences, including such factors as immunodeficiency and comorbidities (including bronchiectasis); and the third is microbiological factors, including various NTM species.
Bile aspirating into the lung during GERD may be another possible pathway, as the authors suggested. Even if acid secretion is suppressed by PPI treatment in patients with GERD, NTM-PD may be induced or aggravated through mechanisms such as bile reflux. The fact that patients over the age of 60 were more prone to develop NTM-PD suggests that a decrease in gastric emptying and increased micro-aspiration or reflux associated with impaired swallowing (which are more common in elderly patients) may also be at play.
“Bronchiectasis is also a very well known risk factor for NTM pulmonary disease,” Dr. Choi emphasized. Thus, he recommends clinicians carefully observe clinical, radiological, and microbiological changes to detect NTM pulmonary disease when managing patients with bronchiectasis.
“The results of the present study have several potential clinical implications,” Dr. Choi and colleagues observed. First, NTM-PD should be suspected when new-onset worsening of respiratory symptoms develops during regular follow-up in patients with GERD. Second, because results indicate that older age and bronchiectasis significantly increase the risk of NTM-PD, “more active strategies (e.g., screening of symptoms and regular chest x-rays)” might be helpful in patients with GERD and these risk factors, the authors suggested. Because patients with GERD who developed NTM-PD had more respiratory disease–related ED visits and hospitalizations than those who did not develop NTM-PD, when GERD and NTM-PD are combined, clinicians should focus on the variations of respiratory symptoms, they suggested.
The authors cautioned, however, that because the study was one in a Korean population, studies in other countries and different ethnicities are needed before findings can be generalized.
More common than TB
Asked to comment on the findings, NTM-PD expert Theodore Marras, MD, clinician investigator, Krembil Research Institute, Toronto, noted that non-TB M-PD is about 10 times more common than TB and that could be an underestimate as there have been very large increases in the incidence of NTM-PD in recent years. “It’s an environmental germ – it’s in our water – and certain people are particularly susceptible to it, typically older age women who have underlying bronchiectasis,” Dr. Marras told this news organization. “And while there are ethnic differences in incidence rates between East Asian people and Black African people, immigration is not the main driver for the increase as far as we can tell,” he said.
He personally treats a lot of NTM-PD and he also believes that GERD is an important risk factor for all types of lung infections including NTM lung disease. “So without a doubt, I believe that GERD should be treated in patients with NTM-PD,” Dr. Marras emphasized. The big question is how to treat GERD, as there may be concerns with acid-suppressive agents such as proton pump inhibitors that “the reflux that comes back up may harbor more germs in it and if that reflux comes up high enough, we are at risk of aspirating some of that fluid into our lungs, especially when we’re asleep,” he said.
Some experts therefore argue in favor of using motility agents instead of PPIs. However, if Dr. Marras has a patient with heartburn, “you have to treat it,” he stressed. Similarly, if a patient has evidence of esophageal erosions, physicians need to treat those as well. However, if neither feature is present, “I tend to like the motility agents preferentially or use them in combination with a PPI,” Dr. Marras said.
Dr. Marras also thinks the study is encouraging physicians involved in treating these patients to think about controlling GERD both when they are treating patients and after they are treated to try to reduce recurrence.
The authors had no financial disclosures to make. Dr. Marras has given several talks on NTM lung disease, one sponsored by AstraZeneca and the other by Novartis.
Patients with gastrointestinal esophageal reflux disease (GERD) have more than three times the risk of developing nontuberculous mycobacterial pulmonary disease (NTM-PD), compared with those without GERD, according to a population-based retrospective cohort study.
“GERD is a common comorbidity of nontuberculous mycobacterial pulmonary disease [but] whether GERD is associated with an increased risk of developing NTM-PD is unknown,” Hayoung Choi, MD, PhD, Hallym University, Seoul, Republic of Korea, and colleagues reported.
Dr. Choi added in an email. “What needs to be understood is that GERD increases health care utilization in patients with NTM pulmonary disease; hence, clinicians who treat patients with NTM pulmonary disease need to be aware of the burden of GERD and treat the gastrointestinal illness simultaneously,” he added.
The study was published online in the journal CHEST.
Sample cohort
Data from the Korean National Health Insurance Service-National Sample Cohort between 2002 and 2015 were used to assess the impact of GERD on NTM-PD. The incidence and risk of NTM-PD were compared between 17,424 patients with GERD and 69,000 patients without GERD in a matched cohort. GERD was defined as patients having received more than 3 months of proton pump inhibitors (PPIs).
During a median follow-up of 5.1 years, the age- and sex-adjusted incidence of NTM-PD was significantly higher in the GERD cohort, at a rate of 34.8/100,000 person-years, than in the matched cohort, at a rate of only 10.5/100,000 person-years (P < .001), the authors reported.
As for risk factors for NTM-PD, being 60 years of age and older was associated with a 3.5-times higher risk of NTM-PD at an adjusted hazard ratio of 3.57 (95% confidence interval, 1.58-8.07), while bronchiectasis was associated with over an 18-times higher risk of NTM-PD in the GERD cohort at an adjusted HR of 18.69 (95% CI, 6.68-552.28). Those with GERD who developed NTM-PD had higher all-cause and respiratory disease–related emergency department visits or hospitalizations compared with patients with GERD who did not develop NTM-PD (P = .011), the investigators noted.
As the authors pointed out, the incidence of NTM-PD in the Korean population ranged from 6 to 19 cases/100,000 between 2008 and 2016; thus, the burden of incident NTM-PD associated with GERD appears to be considerable. As Dr. Choi explained, a combination of three factors influenced the development of NTM infections. The first is environmental, from water source, climate, or region; the second is patient influences, including such factors as immunodeficiency and comorbidities (including bronchiectasis); and the third is microbiological factors, including various NTM species.
Bile aspirating into the lung during GERD may be another possible pathway, as the authors suggested. Even if acid secretion is suppressed by PPI treatment in patients with GERD, NTM-PD may be induced or aggravated through mechanisms such as bile reflux. The fact that patients over the age of 60 were more prone to develop NTM-PD suggests that a decrease in gastric emptying and increased micro-aspiration or reflux associated with impaired swallowing (which are more common in elderly patients) may also be at play.
“Bronchiectasis is also a very well known risk factor for NTM pulmonary disease,” Dr. Choi emphasized. Thus, he recommends clinicians carefully observe clinical, radiological, and microbiological changes to detect NTM pulmonary disease when managing patients with bronchiectasis.
“The results of the present study have several potential clinical implications,” Dr. Choi and colleagues observed. First, NTM-PD should be suspected when new-onset worsening of respiratory symptoms develops during regular follow-up in patients with GERD. Second, because results indicate that older age and bronchiectasis significantly increase the risk of NTM-PD, “more active strategies (e.g., screening of symptoms and regular chest x-rays)” might be helpful in patients with GERD and these risk factors, the authors suggested. Because patients with GERD who developed NTM-PD had more respiratory disease–related ED visits and hospitalizations than those who did not develop NTM-PD, when GERD and NTM-PD are combined, clinicians should focus on the variations of respiratory symptoms, they suggested.
The authors cautioned, however, that because the study was one in a Korean population, studies in other countries and different ethnicities are needed before findings can be generalized.
More common than TB
Asked to comment on the findings, NTM-PD expert Theodore Marras, MD, clinician investigator, Krembil Research Institute, Toronto, noted that non-TB M-PD is about 10 times more common than TB and that could be an underestimate as there have been very large increases in the incidence of NTM-PD in recent years. “It’s an environmental germ – it’s in our water – and certain people are particularly susceptible to it, typically older age women who have underlying bronchiectasis,” Dr. Marras told this news organization. “And while there are ethnic differences in incidence rates between East Asian people and Black African people, immigration is not the main driver for the increase as far as we can tell,” he said.
He personally treats a lot of NTM-PD and he also believes that GERD is an important risk factor for all types of lung infections including NTM lung disease. “So without a doubt, I believe that GERD should be treated in patients with NTM-PD,” Dr. Marras emphasized. The big question is how to treat GERD, as there may be concerns with acid-suppressive agents such as proton pump inhibitors that “the reflux that comes back up may harbor more germs in it and if that reflux comes up high enough, we are at risk of aspirating some of that fluid into our lungs, especially when we’re asleep,” he said.
Some experts therefore argue in favor of using motility agents instead of PPIs. However, if Dr. Marras has a patient with heartburn, “you have to treat it,” he stressed. Similarly, if a patient has evidence of esophageal erosions, physicians need to treat those as well. However, if neither feature is present, “I tend to like the motility agents preferentially or use them in combination with a PPI,” Dr. Marras said.
Dr. Marras also thinks the study is encouraging physicians involved in treating these patients to think about controlling GERD both when they are treating patients and after they are treated to try to reduce recurrence.
The authors had no financial disclosures to make. Dr. Marras has given several talks on NTM lung disease, one sponsored by AstraZeneca and the other by Novartis.
FROM CHEST
Safer opioid supply program in Canada helps those who face overdose risks
An analysis indicates that the program is associated with a reduction in emergency department visits, hospitalizations, and overall health care costs. In addition, there were no opioid-related deaths among participants who were at high risk of overdose.
“Not only did hospital engagements decline immediately after starting SOS programs, but also the risk of overdose did not change, and there were no opioid-related deaths in the 1-year follow-up,” study author Tara Gomes, PhD, an assistant professor of health policy, management, and evaluation at the University of Toronto and a scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, said in an interview.
Dr. Gomes is the lead principal investigator of the Ontario Drug Policy Research Network, a collaboration between researchers and drug policy decision-makers in the province.
“These changes were not seen in a group of similar individuals who lived in the same city – so were exposed to the same illicit drug supply – but who were not part of this program, helping to reinforce that these changes are specific to SOS participation,” she said.
The study was published in the Canadian Medical Association Journal.
Hospital admissions declined
More than 29,000 opioid-related toxicity deaths occurred in Canada between 2016 and 2021, often as a result of high levels of fentanyl in the drug supply, according to the investigators. In response, SOS programs have been launched in several provinces, including the first formal SOS program at the London (Ont.) InterCommunity Health Centre. As part of the program, clients are prescribed pharmaceutical opioids as an alternative to the fentanyl-adulterated drug supply and are given health and social supports.
Dr. Gomes and colleagues conducted an interrupted time series analysis of residents in London, Ont., who had received a diagnosis of opioid use disorder and had had a health care encounter related to the diagnosis between January 2016 and March 2019. They followed 82 participants who entered the SOS program, as well as a comparison group of 303 people who were matched on the basis of demographic and clinical characteristics but who did not participate in the program.
The research team focused on the population’s numbers of emergency department visits, hospital admissions, infection rates, and health care costs. They used autoregressive integrated moving average models to evaluate the effect of starting the SOS program and to compare the population’s outcome rates in the year before and after entering the program.
For participants who entered the program, the rate of emergency department visits declined by about 14 visits per 100 people. In addition, hospital admissions declined by about 5 admissions per 100 people. Health care costs that weren’t related to primary care or outpatient medications declined by about $922 per person. The rate of hospital admission for infections remained about the same; the investigators observed a decline of about 1.6 infections per 100 people.
In the year after entry into the program, emergency department visits, hospital admissions, infection-related admissions, and total health care costs declined significantly among SOS clients, compared with the year before.
Conversely, there were no significant changes in any of the measured outcomes among the 303 people who didn’t participate in the program.
Medication costs increased
DR. Gomes and colleagues noted that the findings provide preliminary evidence that SOS programs can play a role in the harm-reduction options available to those who are at high risk of drug poisoning and overdose. At the same time, many questions remain.
For instance, although total health care costs declined among those enrolled in the program, the medication-related costs increased. About 34% of participants had HIV, 69.5% had hepatitis C virus infection, and 28% had infectious complications in the year before entering the program. This finding may indicate that the participants had serious medical complications resulting from their drug use and were able to seek health care services.
“We interpret that to be a positive finding, because of the very high prevalence of HIV and hepatitis C in the SOS clients. Treatments for HIV and hepatitis C are lifesaving but expensive,” said Dr. Gomes. “Therefore, these higher medication costs are likely reflective of improved access to treatments for these infections, which can greatly improve people’s health and quality of life but also save the health care system money over the longer term.”
DR. Gomes and colleagues are now beginning to evaluate other SOS programs across Ontario. They hope to better understand the various approaches that are available and determine which models can best support people who face high risks because of drug use.
A limited solution?
Commenting on the study, Andrew Ivsins, PhD, a postdoctoral fellow in social medicine at the University of British Columbia in Vancouver and a research scientist at the British Columbia Centre on Substance Abuse, said, “This is an important study and one of the first to show how safe supply can help by building connections to the health care system that didn’t exist previously.”
Dr. Ivsins, who wasn’t involved with this study, has researched safe supply programs around Vancouver. He and colleagues found that among participants in these programs, the use of illicit street-purchased drugs decreased, which led to improved health and wellness.
“Safe supply is fundamentally, at the most basic level, a response to the highly toxic drug supply and out-of-control poisoning crisis in North America,” he said. “It’s a contentious issue, but it makes so much sense that, if what’s killing people is highly toxic drugs, we need to find a way to provide an option that doesn’t kill them.”
“Up to now, safer supply has mostly been used to reduce harms, including mortality and morbidity, in persons using illicit opioids. But if we really want to lower the risk linked to heavy contamination of the unregulated drug supply, safer supply programs will have to be extended to all substances potentially sold illegally,” Marie-Eve Goyer, MD, an assistant professor of family medicine at the University of Montreal, said in an interview.
Dr. Goyer, who wasn’t involved with this study, has conducted research about substance replacement therapy in Quebec. She found that many provinces are now reporting on new potent designer benzodiazepines that are being used or that are contaminating fentanyl, which calls for a broader approach to address the drug overdose crisis.
“Let’s realize that safer supply prescription is a very medicalized (and limited) solution to an epidemic that is made of stigma, criminalization, and repressive public policies,” she said. “Without true changes in the law, we will continue to see our people dying every day.”
The study was funded by grants from the Ontario Ministry of Health and the Canadian Institutes of Health Research. Dr. Gomes has received grants to support the research of both groups, and other authors have received support or fees related to the London InterCommunity Health Centre. Dr. Ivsins and Dr. Goyer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An analysis indicates that the program is associated with a reduction in emergency department visits, hospitalizations, and overall health care costs. In addition, there were no opioid-related deaths among participants who were at high risk of overdose.
“Not only did hospital engagements decline immediately after starting SOS programs, but also the risk of overdose did not change, and there were no opioid-related deaths in the 1-year follow-up,” study author Tara Gomes, PhD, an assistant professor of health policy, management, and evaluation at the University of Toronto and a scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, said in an interview.
Dr. Gomes is the lead principal investigator of the Ontario Drug Policy Research Network, a collaboration between researchers and drug policy decision-makers in the province.
“These changes were not seen in a group of similar individuals who lived in the same city – so were exposed to the same illicit drug supply – but who were not part of this program, helping to reinforce that these changes are specific to SOS participation,” she said.
The study was published in the Canadian Medical Association Journal.
Hospital admissions declined
More than 29,000 opioid-related toxicity deaths occurred in Canada between 2016 and 2021, often as a result of high levels of fentanyl in the drug supply, according to the investigators. In response, SOS programs have been launched in several provinces, including the first formal SOS program at the London (Ont.) InterCommunity Health Centre. As part of the program, clients are prescribed pharmaceutical opioids as an alternative to the fentanyl-adulterated drug supply and are given health and social supports.
Dr. Gomes and colleagues conducted an interrupted time series analysis of residents in London, Ont., who had received a diagnosis of opioid use disorder and had had a health care encounter related to the diagnosis between January 2016 and March 2019. They followed 82 participants who entered the SOS program, as well as a comparison group of 303 people who were matched on the basis of demographic and clinical characteristics but who did not participate in the program.
The research team focused on the population’s numbers of emergency department visits, hospital admissions, infection rates, and health care costs. They used autoregressive integrated moving average models to evaluate the effect of starting the SOS program and to compare the population’s outcome rates in the year before and after entering the program.
For participants who entered the program, the rate of emergency department visits declined by about 14 visits per 100 people. In addition, hospital admissions declined by about 5 admissions per 100 people. Health care costs that weren’t related to primary care or outpatient medications declined by about $922 per person. The rate of hospital admission for infections remained about the same; the investigators observed a decline of about 1.6 infections per 100 people.
In the year after entry into the program, emergency department visits, hospital admissions, infection-related admissions, and total health care costs declined significantly among SOS clients, compared with the year before.
Conversely, there were no significant changes in any of the measured outcomes among the 303 people who didn’t participate in the program.
Medication costs increased
DR. Gomes and colleagues noted that the findings provide preliminary evidence that SOS programs can play a role in the harm-reduction options available to those who are at high risk of drug poisoning and overdose. At the same time, many questions remain.
For instance, although total health care costs declined among those enrolled in the program, the medication-related costs increased. About 34% of participants had HIV, 69.5% had hepatitis C virus infection, and 28% had infectious complications in the year before entering the program. This finding may indicate that the participants had serious medical complications resulting from their drug use and were able to seek health care services.
“We interpret that to be a positive finding, because of the very high prevalence of HIV and hepatitis C in the SOS clients. Treatments for HIV and hepatitis C are lifesaving but expensive,” said Dr. Gomes. “Therefore, these higher medication costs are likely reflective of improved access to treatments for these infections, which can greatly improve people’s health and quality of life but also save the health care system money over the longer term.”
DR. Gomes and colleagues are now beginning to evaluate other SOS programs across Ontario. They hope to better understand the various approaches that are available and determine which models can best support people who face high risks because of drug use.
A limited solution?
Commenting on the study, Andrew Ivsins, PhD, a postdoctoral fellow in social medicine at the University of British Columbia in Vancouver and a research scientist at the British Columbia Centre on Substance Abuse, said, “This is an important study and one of the first to show how safe supply can help by building connections to the health care system that didn’t exist previously.”
Dr. Ivsins, who wasn’t involved with this study, has researched safe supply programs around Vancouver. He and colleagues found that among participants in these programs, the use of illicit street-purchased drugs decreased, which led to improved health and wellness.
“Safe supply is fundamentally, at the most basic level, a response to the highly toxic drug supply and out-of-control poisoning crisis in North America,” he said. “It’s a contentious issue, but it makes so much sense that, if what’s killing people is highly toxic drugs, we need to find a way to provide an option that doesn’t kill them.”
“Up to now, safer supply has mostly been used to reduce harms, including mortality and morbidity, in persons using illicit opioids. But if we really want to lower the risk linked to heavy contamination of the unregulated drug supply, safer supply programs will have to be extended to all substances potentially sold illegally,” Marie-Eve Goyer, MD, an assistant professor of family medicine at the University of Montreal, said in an interview.
Dr. Goyer, who wasn’t involved with this study, has conducted research about substance replacement therapy in Quebec. She found that many provinces are now reporting on new potent designer benzodiazepines that are being used or that are contaminating fentanyl, which calls for a broader approach to address the drug overdose crisis.
“Let’s realize that safer supply prescription is a very medicalized (and limited) solution to an epidemic that is made of stigma, criminalization, and repressive public policies,” she said. “Without true changes in the law, we will continue to see our people dying every day.”
The study was funded by grants from the Ontario Ministry of Health and the Canadian Institutes of Health Research. Dr. Gomes has received grants to support the research of both groups, and other authors have received support or fees related to the London InterCommunity Health Centre. Dr. Ivsins and Dr. Goyer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An analysis indicates that the program is associated with a reduction in emergency department visits, hospitalizations, and overall health care costs. In addition, there were no opioid-related deaths among participants who were at high risk of overdose.
“Not only did hospital engagements decline immediately after starting SOS programs, but also the risk of overdose did not change, and there were no opioid-related deaths in the 1-year follow-up,” study author Tara Gomes, PhD, an assistant professor of health policy, management, and evaluation at the University of Toronto and a scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, said in an interview.
Dr. Gomes is the lead principal investigator of the Ontario Drug Policy Research Network, a collaboration between researchers and drug policy decision-makers in the province.
“These changes were not seen in a group of similar individuals who lived in the same city – so were exposed to the same illicit drug supply – but who were not part of this program, helping to reinforce that these changes are specific to SOS participation,” she said.
The study was published in the Canadian Medical Association Journal.
Hospital admissions declined
More than 29,000 opioid-related toxicity deaths occurred in Canada between 2016 and 2021, often as a result of high levels of fentanyl in the drug supply, according to the investigators. In response, SOS programs have been launched in several provinces, including the first formal SOS program at the London (Ont.) InterCommunity Health Centre. As part of the program, clients are prescribed pharmaceutical opioids as an alternative to the fentanyl-adulterated drug supply and are given health and social supports.
Dr. Gomes and colleagues conducted an interrupted time series analysis of residents in London, Ont., who had received a diagnosis of opioid use disorder and had had a health care encounter related to the diagnosis between January 2016 and March 2019. They followed 82 participants who entered the SOS program, as well as a comparison group of 303 people who were matched on the basis of demographic and clinical characteristics but who did not participate in the program.
The research team focused on the population’s numbers of emergency department visits, hospital admissions, infection rates, and health care costs. They used autoregressive integrated moving average models to evaluate the effect of starting the SOS program and to compare the population’s outcome rates in the year before and after entering the program.
For participants who entered the program, the rate of emergency department visits declined by about 14 visits per 100 people. In addition, hospital admissions declined by about 5 admissions per 100 people. Health care costs that weren’t related to primary care or outpatient medications declined by about $922 per person. The rate of hospital admission for infections remained about the same; the investigators observed a decline of about 1.6 infections per 100 people.
In the year after entry into the program, emergency department visits, hospital admissions, infection-related admissions, and total health care costs declined significantly among SOS clients, compared with the year before.
Conversely, there were no significant changes in any of the measured outcomes among the 303 people who didn’t participate in the program.
Medication costs increased
DR. Gomes and colleagues noted that the findings provide preliminary evidence that SOS programs can play a role in the harm-reduction options available to those who are at high risk of drug poisoning and overdose. At the same time, many questions remain.
For instance, although total health care costs declined among those enrolled in the program, the medication-related costs increased. About 34% of participants had HIV, 69.5% had hepatitis C virus infection, and 28% had infectious complications in the year before entering the program. This finding may indicate that the participants had serious medical complications resulting from their drug use and were able to seek health care services.
“We interpret that to be a positive finding, because of the very high prevalence of HIV and hepatitis C in the SOS clients. Treatments for HIV and hepatitis C are lifesaving but expensive,” said Dr. Gomes. “Therefore, these higher medication costs are likely reflective of improved access to treatments for these infections, which can greatly improve people’s health and quality of life but also save the health care system money over the longer term.”
DR. Gomes and colleagues are now beginning to evaluate other SOS programs across Ontario. They hope to better understand the various approaches that are available and determine which models can best support people who face high risks because of drug use.
A limited solution?
Commenting on the study, Andrew Ivsins, PhD, a postdoctoral fellow in social medicine at the University of British Columbia in Vancouver and a research scientist at the British Columbia Centre on Substance Abuse, said, “This is an important study and one of the first to show how safe supply can help by building connections to the health care system that didn’t exist previously.”
Dr. Ivsins, who wasn’t involved with this study, has researched safe supply programs around Vancouver. He and colleagues found that among participants in these programs, the use of illicit street-purchased drugs decreased, which led to improved health and wellness.
“Safe supply is fundamentally, at the most basic level, a response to the highly toxic drug supply and out-of-control poisoning crisis in North America,” he said. “It’s a contentious issue, but it makes so much sense that, if what’s killing people is highly toxic drugs, we need to find a way to provide an option that doesn’t kill them.”
“Up to now, safer supply has mostly been used to reduce harms, including mortality and morbidity, in persons using illicit opioids. But if we really want to lower the risk linked to heavy contamination of the unregulated drug supply, safer supply programs will have to be extended to all substances potentially sold illegally,” Marie-Eve Goyer, MD, an assistant professor of family medicine at the University of Montreal, said in an interview.
Dr. Goyer, who wasn’t involved with this study, has conducted research about substance replacement therapy in Quebec. She found that many provinces are now reporting on new potent designer benzodiazepines that are being used or that are contaminating fentanyl, which calls for a broader approach to address the drug overdose crisis.
“Let’s realize that safer supply prescription is a very medicalized (and limited) solution to an epidemic that is made of stigma, criminalization, and repressive public policies,” she said. “Without true changes in the law, we will continue to see our people dying every day.”
The study was funded by grants from the Ontario Ministry of Health and the Canadian Institutes of Health Research. Dr. Gomes has received grants to support the research of both groups, and other authors have received support or fees related to the London InterCommunity Health Centre. Dr. Ivsins and Dr. Goyer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANADIAN MEDICAL ASSOCIATION JOURNAL
Continued monkeypox spread can lead to viral mutations
Monkeypox cases are declining in the United States and the United Kingdom, but experts are urging the public to continue efforts to stanch the spread of the virus. Continued transmission of monkeypox provides more opportunities for the virus to mutate, according to Philip Johnson, PhD, assistant professor of biology at the University of Maryland, College Park, and colleagues.
the authors wrote in a correspondence published in The Lancet.
When case numbers are lower – and therefore less of a public health concern – viral transmission chains can be longer without causing alarm, Dr. Johnson explained. “The more generations of transmission, the more opportunities there are for mutations to occur,” he told this news organization. While it is difficult to anticipate how mutations can affect a virus, these changes in genetic code could be advantageous to the virus, making it more transmissible from human to human and therefore much more difficult to control.
This applies to any virus. The large Ebola outbreak from 2013 to 2016 is an example; a retrospective analysis found that specific amino acid changes in the Ebola virus increased growth in human cells and may have made the virus more infectious. More recently, the Delta and Omicron variants of SARS-CoV-2 each contained mutations that were associated with higher transmissibility. A recent study suggested that monkeypox appears to be mutating faster than expected, though it is not clear if these genetic mutations have changed the virus’ behavior.
Zoonotic infections, or viruses that originate from nonhuman animals, at first are expected to be less adapted to people, but that can change over time. When a virus continues to jump from animals to humans – as monkeypox has done since it was first identified in humans in 1970 – chances are it will gain a mutation that allows it to spread more effectively between people, said Rachel Roper, PhD, a professor of microbiology and immunology at East Carolina University, Greenville, N.C. She was not involved with The Lancet article.
“We discounted monkeypox; we didn’t pay much attention to it because it had not been that big of a problem,” she said in an interview. “We think this virus has been circulating now since 2017 and we really just realized it in May.”
Although monkeypox received global attention this past summer, the outbreak is now receiving less news coverage, and the public’s attention may be waning. Furthermore, the U.S. Congress just dropped billions of dollars from a short-term spending bill that would have provided additional COVID-19 and monkeypox funding.
Although new cases are trending downward, now is not the time to take our foot off the gas, Dr. Johnson and colleagues warned. “The epidemic is far from over, and continued drive toward elimination is essential,” the authors wrote. Because the virus exists in rodent populations in areas of central and west Africa, it is not possible to eradicate monkeypox as we did smallpox; however, “we could, through vaccination, eliminate any significant human to human transmission,” Dr. Johnson said.
Dr. Johnson also urges a more proactive approach to combating emerging infectious diseases in the future. “We wrote this article to raise awareness about the importance of dedicating resources to controlling these diseases all the way down to ideally elimination in the countries where they develop, and not just waiting until [these diseases] reach wealthier countries,” he said.
Dr. Roper agrees that a more global perspective is needed in monitoring and controlling zoonotic disease, but resources are limited. “The problem is there are a whole bunch of virus groups and a whole bunch of viruses jumping into humans all the time,” she said. “We can’t predict which virus group is going to be the next one with a big hit. I worked on SARS-CoV-1 back in 2003 to 2009, and I would have predicted that a virus from some other group would have jumped into humans next, before COVID hit,” she added.
Dr. Johnson acknowledged that it is hard to know where to focus public health resources, considering the hundreds of thousands of zoonotic viruses that may exist. He thought the best approach was to target emerging diseases that already appear to have extended transmission chains, “not just things that are hopping from animals to humans and sputtering out and disappearing, but diseases that appear to have any sustained human to human transmission.”
Dr. Johnson and Dr. Roper report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Monkeypox cases are declining in the United States and the United Kingdom, but experts are urging the public to continue efforts to stanch the spread of the virus. Continued transmission of monkeypox provides more opportunities for the virus to mutate, according to Philip Johnson, PhD, assistant professor of biology at the University of Maryland, College Park, and colleagues.
the authors wrote in a correspondence published in The Lancet.
When case numbers are lower – and therefore less of a public health concern – viral transmission chains can be longer without causing alarm, Dr. Johnson explained. “The more generations of transmission, the more opportunities there are for mutations to occur,” he told this news organization. While it is difficult to anticipate how mutations can affect a virus, these changes in genetic code could be advantageous to the virus, making it more transmissible from human to human and therefore much more difficult to control.
This applies to any virus. The large Ebola outbreak from 2013 to 2016 is an example; a retrospective analysis found that specific amino acid changes in the Ebola virus increased growth in human cells and may have made the virus more infectious. More recently, the Delta and Omicron variants of SARS-CoV-2 each contained mutations that were associated with higher transmissibility. A recent study suggested that monkeypox appears to be mutating faster than expected, though it is not clear if these genetic mutations have changed the virus’ behavior.
Zoonotic infections, or viruses that originate from nonhuman animals, at first are expected to be less adapted to people, but that can change over time. When a virus continues to jump from animals to humans – as monkeypox has done since it was first identified in humans in 1970 – chances are it will gain a mutation that allows it to spread more effectively between people, said Rachel Roper, PhD, a professor of microbiology and immunology at East Carolina University, Greenville, N.C. She was not involved with The Lancet article.
“We discounted monkeypox; we didn’t pay much attention to it because it had not been that big of a problem,” she said in an interview. “We think this virus has been circulating now since 2017 and we really just realized it in May.”
Although monkeypox received global attention this past summer, the outbreak is now receiving less news coverage, and the public’s attention may be waning. Furthermore, the U.S. Congress just dropped billions of dollars from a short-term spending bill that would have provided additional COVID-19 and monkeypox funding.
Although new cases are trending downward, now is not the time to take our foot off the gas, Dr. Johnson and colleagues warned. “The epidemic is far from over, and continued drive toward elimination is essential,” the authors wrote. Because the virus exists in rodent populations in areas of central and west Africa, it is not possible to eradicate monkeypox as we did smallpox; however, “we could, through vaccination, eliminate any significant human to human transmission,” Dr. Johnson said.
Dr. Johnson also urges a more proactive approach to combating emerging infectious diseases in the future. “We wrote this article to raise awareness about the importance of dedicating resources to controlling these diseases all the way down to ideally elimination in the countries where they develop, and not just waiting until [these diseases] reach wealthier countries,” he said.
Dr. Roper agrees that a more global perspective is needed in monitoring and controlling zoonotic disease, but resources are limited. “The problem is there are a whole bunch of virus groups and a whole bunch of viruses jumping into humans all the time,” she said. “We can’t predict which virus group is going to be the next one with a big hit. I worked on SARS-CoV-1 back in 2003 to 2009, and I would have predicted that a virus from some other group would have jumped into humans next, before COVID hit,” she added.
Dr. Johnson acknowledged that it is hard to know where to focus public health resources, considering the hundreds of thousands of zoonotic viruses that may exist. He thought the best approach was to target emerging diseases that already appear to have extended transmission chains, “not just things that are hopping from animals to humans and sputtering out and disappearing, but diseases that appear to have any sustained human to human transmission.”
Dr. Johnson and Dr. Roper report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Monkeypox cases are declining in the United States and the United Kingdom, but experts are urging the public to continue efforts to stanch the spread of the virus. Continued transmission of monkeypox provides more opportunities for the virus to mutate, according to Philip Johnson, PhD, assistant professor of biology at the University of Maryland, College Park, and colleagues.
the authors wrote in a correspondence published in The Lancet.
When case numbers are lower – and therefore less of a public health concern – viral transmission chains can be longer without causing alarm, Dr. Johnson explained. “The more generations of transmission, the more opportunities there are for mutations to occur,” he told this news organization. While it is difficult to anticipate how mutations can affect a virus, these changes in genetic code could be advantageous to the virus, making it more transmissible from human to human and therefore much more difficult to control.
This applies to any virus. The large Ebola outbreak from 2013 to 2016 is an example; a retrospective analysis found that specific amino acid changes in the Ebola virus increased growth in human cells and may have made the virus more infectious. More recently, the Delta and Omicron variants of SARS-CoV-2 each contained mutations that were associated with higher transmissibility. A recent study suggested that monkeypox appears to be mutating faster than expected, though it is not clear if these genetic mutations have changed the virus’ behavior.
Zoonotic infections, or viruses that originate from nonhuman animals, at first are expected to be less adapted to people, but that can change over time. When a virus continues to jump from animals to humans – as monkeypox has done since it was first identified in humans in 1970 – chances are it will gain a mutation that allows it to spread more effectively between people, said Rachel Roper, PhD, a professor of microbiology and immunology at East Carolina University, Greenville, N.C. She was not involved with The Lancet article.
“We discounted monkeypox; we didn’t pay much attention to it because it had not been that big of a problem,” she said in an interview. “We think this virus has been circulating now since 2017 and we really just realized it in May.”
Although monkeypox received global attention this past summer, the outbreak is now receiving less news coverage, and the public’s attention may be waning. Furthermore, the U.S. Congress just dropped billions of dollars from a short-term spending bill that would have provided additional COVID-19 and monkeypox funding.
Although new cases are trending downward, now is not the time to take our foot off the gas, Dr. Johnson and colleagues warned. “The epidemic is far from over, and continued drive toward elimination is essential,” the authors wrote. Because the virus exists in rodent populations in areas of central and west Africa, it is not possible to eradicate monkeypox as we did smallpox; however, “we could, through vaccination, eliminate any significant human to human transmission,” Dr. Johnson said.
Dr. Johnson also urges a more proactive approach to combating emerging infectious diseases in the future. “We wrote this article to raise awareness about the importance of dedicating resources to controlling these diseases all the way down to ideally elimination in the countries where they develop, and not just waiting until [these diseases] reach wealthier countries,” he said.
Dr. Roper agrees that a more global perspective is needed in monitoring and controlling zoonotic disease, but resources are limited. “The problem is there are a whole bunch of virus groups and a whole bunch of viruses jumping into humans all the time,” she said. “We can’t predict which virus group is going to be the next one with a big hit. I worked on SARS-CoV-1 back in 2003 to 2009, and I would have predicted that a virus from some other group would have jumped into humans next, before COVID hit,” she added.
Dr. Johnson acknowledged that it is hard to know where to focus public health resources, considering the hundreds of thousands of zoonotic viruses that may exist. He thought the best approach was to target emerging diseases that already appear to have extended transmission chains, “not just things that are hopping from animals to humans and sputtering out and disappearing, but diseases that appear to have any sustained human to human transmission.”
Dr. Johnson and Dr. Roper report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Trial shows olokizumab’s effect in nonresponders to TNF inhibitors in RA
Treatment of rheumatoid arthritis with olokizumab combined with methotrexate led to significantly more patients with improved signs and symptoms than did methotrexate plus placebo in circumstances where previous treatment with one or more tumor necrosis factor (TNF) inhibitors yielded inadequate responses, results from a phase 3 randomized trial show.
At the week 12 primary endpoint, 40.6% of patients receiving placebo had at least 20% improvement in American College of Rheumatology response criteria (ACR 20), compared with 60.9% of patients receiving olokizumab 64 mg every 2 weeks and 59.6% of patients receiving olokizumab 64 mg every 4 weeks (P <.01 for both comparisons), senior author Roy M. Fleischmann, MD, of the University of Texas Southwestern Medical Center in Dallas and colleagues reported in Annals of the Rheumatic Diseases.
Dr. Fleischmann said that given the existing literature on the investigational interleukin (IL)-6 inhibitor olokizumab shows that it is superior to placebo and noninferior to adalimumab (Humira) in patients who have an inadequate response to methotrexate and that it was superior to methotrexate alone for patients who have failed one or more TNF inhibitors in this current trial, the most likely use of olokizumab in clinical practice if it is approved is for those with inadequate responses to TNF inhibitors.
“If olokizumab is approved in the U.S., it is a reasonable choice when considering an inhibitor of IL-6. As it does affect IL-6 directly, rather than the receptor, much less protein needs to be administered with a convenient dosing interval of either every 2 or 4 weeks subcutaneously,” Dr. Fleischmann said in an interview.
The 24-week, double-blind, multicenter study, dubbed Clinical Rheumatoid Arthritis Development for Olokizumab (CREDO 3), involved 161 patients receiving 64 mg of olokizumab subcutaneously every 4 weeks, 138 receiving 64 mg of olokizumab subcutaneously once every 2 weeks, and 69 receiving placebo. At week 16, the researchers randomized participants in the placebo group to receive either olokizumab regimen.
All patients received methotrexate, and NSAIDs and glucocorticoids (< 10 mg/day prednisone or equivalent) were allowed in stable doses. Mean age was about 53 years across all three arms, and females accounted for the majority for each arm.
Significantly more patients in both olokizumab arms achieved the main secondary endpoint of Disease Activity Score in 28 joints based on C-reactive protein less than 3.2 at week 12, compared with placebo.
Notably, patients who moved from placebo at week 16 experienced improvement that was sustained over the remaining 8 weeks.
Serious treatment-emergent adverse events with olokizumab occurred in 3.2% receiving the drug every 4 weeks and in 7% receiving it every 2 weeks but in none who received placebo.
The study’s limitations included the high placebo response rate, the short timeframe for placebo, and its fairly small sample size, which limits the generalizability of the results, the authors noted.
Expert commentary
There are currently two biologics on the market that inhibit the IL-6 receptor, tocilizumab (Actemra), and sarilumab (Kevzara), but olokizumab is unique in that “it does not block the receptor. It binds directly to the cytokine,” noted Larry Moreland, MD, a professor of medicine and orthopedics in the division of rheumatology at the University of Colorado at Denver in Aurora, who was not involved in the study.
Tocilizumab and sarilumab had a similar clinical trial portfolio when they were studied in people who failed anti-TNF therapy, so this is the standard study a company would do prior to seeking approval, Dr. Moreland said.
“The fact that there is another IL-6 blocker that is showing promise means that there are more opportunities for researchers and clinicians to use these agents not only for rheumatoid arthritis but also hopefully study them in other diseases,” he said.
The CREDO 3 trial was sponsored by R-Pharm. Some of the authors are employees of R-Pharm. Dr. Fleischmann and some of his coauthors reported financial ties to R-Pharm and other pharmaceutical companies. Dr. Moreland reported having no relevant competing interests.
Treatment of rheumatoid arthritis with olokizumab combined with methotrexate led to significantly more patients with improved signs and symptoms than did methotrexate plus placebo in circumstances where previous treatment with one or more tumor necrosis factor (TNF) inhibitors yielded inadequate responses, results from a phase 3 randomized trial show.
At the week 12 primary endpoint, 40.6% of patients receiving placebo had at least 20% improvement in American College of Rheumatology response criteria (ACR 20), compared with 60.9% of patients receiving olokizumab 64 mg every 2 weeks and 59.6% of patients receiving olokizumab 64 mg every 4 weeks (P <.01 for both comparisons), senior author Roy M. Fleischmann, MD, of the University of Texas Southwestern Medical Center in Dallas and colleagues reported in Annals of the Rheumatic Diseases.
Dr. Fleischmann said that given the existing literature on the investigational interleukin (IL)-6 inhibitor olokizumab shows that it is superior to placebo and noninferior to adalimumab (Humira) in patients who have an inadequate response to methotrexate and that it was superior to methotrexate alone for patients who have failed one or more TNF inhibitors in this current trial, the most likely use of olokizumab in clinical practice if it is approved is for those with inadequate responses to TNF inhibitors.
“If olokizumab is approved in the U.S., it is a reasonable choice when considering an inhibitor of IL-6. As it does affect IL-6 directly, rather than the receptor, much less protein needs to be administered with a convenient dosing interval of either every 2 or 4 weeks subcutaneously,” Dr. Fleischmann said in an interview.
The 24-week, double-blind, multicenter study, dubbed Clinical Rheumatoid Arthritis Development for Olokizumab (CREDO 3), involved 161 patients receiving 64 mg of olokizumab subcutaneously every 4 weeks, 138 receiving 64 mg of olokizumab subcutaneously once every 2 weeks, and 69 receiving placebo. At week 16, the researchers randomized participants in the placebo group to receive either olokizumab regimen.
All patients received methotrexate, and NSAIDs and glucocorticoids (< 10 mg/day prednisone or equivalent) were allowed in stable doses. Mean age was about 53 years across all three arms, and females accounted for the majority for each arm.
Significantly more patients in both olokizumab arms achieved the main secondary endpoint of Disease Activity Score in 28 joints based on C-reactive protein less than 3.2 at week 12, compared with placebo.
Notably, patients who moved from placebo at week 16 experienced improvement that was sustained over the remaining 8 weeks.
Serious treatment-emergent adverse events with olokizumab occurred in 3.2% receiving the drug every 4 weeks and in 7% receiving it every 2 weeks but in none who received placebo.
The study’s limitations included the high placebo response rate, the short timeframe for placebo, and its fairly small sample size, which limits the generalizability of the results, the authors noted.
Expert commentary
There are currently two biologics on the market that inhibit the IL-6 receptor, tocilizumab (Actemra), and sarilumab (Kevzara), but olokizumab is unique in that “it does not block the receptor. It binds directly to the cytokine,” noted Larry Moreland, MD, a professor of medicine and orthopedics in the division of rheumatology at the University of Colorado at Denver in Aurora, who was not involved in the study.
Tocilizumab and sarilumab had a similar clinical trial portfolio when they were studied in people who failed anti-TNF therapy, so this is the standard study a company would do prior to seeking approval, Dr. Moreland said.
“The fact that there is another IL-6 blocker that is showing promise means that there are more opportunities for researchers and clinicians to use these agents not only for rheumatoid arthritis but also hopefully study them in other diseases,” he said.
The CREDO 3 trial was sponsored by R-Pharm. Some of the authors are employees of R-Pharm. Dr. Fleischmann and some of his coauthors reported financial ties to R-Pharm and other pharmaceutical companies. Dr. Moreland reported having no relevant competing interests.
Treatment of rheumatoid arthritis with olokizumab combined with methotrexate led to significantly more patients with improved signs and symptoms than did methotrexate plus placebo in circumstances where previous treatment with one or more tumor necrosis factor (TNF) inhibitors yielded inadequate responses, results from a phase 3 randomized trial show.
At the week 12 primary endpoint, 40.6% of patients receiving placebo had at least 20% improvement in American College of Rheumatology response criteria (ACR 20), compared with 60.9% of patients receiving olokizumab 64 mg every 2 weeks and 59.6% of patients receiving olokizumab 64 mg every 4 weeks (P <.01 for both comparisons), senior author Roy M. Fleischmann, MD, of the University of Texas Southwestern Medical Center in Dallas and colleagues reported in Annals of the Rheumatic Diseases.
Dr. Fleischmann said that given the existing literature on the investigational interleukin (IL)-6 inhibitor olokizumab shows that it is superior to placebo and noninferior to adalimumab (Humira) in patients who have an inadequate response to methotrexate and that it was superior to methotrexate alone for patients who have failed one or more TNF inhibitors in this current trial, the most likely use of olokizumab in clinical practice if it is approved is for those with inadequate responses to TNF inhibitors.
“If olokizumab is approved in the U.S., it is a reasonable choice when considering an inhibitor of IL-6. As it does affect IL-6 directly, rather than the receptor, much less protein needs to be administered with a convenient dosing interval of either every 2 or 4 weeks subcutaneously,” Dr. Fleischmann said in an interview.
The 24-week, double-blind, multicenter study, dubbed Clinical Rheumatoid Arthritis Development for Olokizumab (CREDO 3), involved 161 patients receiving 64 mg of olokizumab subcutaneously every 4 weeks, 138 receiving 64 mg of olokizumab subcutaneously once every 2 weeks, and 69 receiving placebo. At week 16, the researchers randomized participants in the placebo group to receive either olokizumab regimen.
All patients received methotrexate, and NSAIDs and glucocorticoids (< 10 mg/day prednisone or equivalent) were allowed in stable doses. Mean age was about 53 years across all three arms, and females accounted for the majority for each arm.
Significantly more patients in both olokizumab arms achieved the main secondary endpoint of Disease Activity Score in 28 joints based on C-reactive protein less than 3.2 at week 12, compared with placebo.
Notably, patients who moved from placebo at week 16 experienced improvement that was sustained over the remaining 8 weeks.
Serious treatment-emergent adverse events with olokizumab occurred in 3.2% receiving the drug every 4 weeks and in 7% receiving it every 2 weeks but in none who received placebo.
The study’s limitations included the high placebo response rate, the short timeframe for placebo, and its fairly small sample size, which limits the generalizability of the results, the authors noted.
Expert commentary
There are currently two biologics on the market that inhibit the IL-6 receptor, tocilizumab (Actemra), and sarilumab (Kevzara), but olokizumab is unique in that “it does not block the receptor. It binds directly to the cytokine,” noted Larry Moreland, MD, a professor of medicine and orthopedics in the division of rheumatology at the University of Colorado at Denver in Aurora, who was not involved in the study.
Tocilizumab and sarilumab had a similar clinical trial portfolio when they were studied in people who failed anti-TNF therapy, so this is the standard study a company would do prior to seeking approval, Dr. Moreland said.
“The fact that there is another IL-6 blocker that is showing promise means that there are more opportunities for researchers and clinicians to use these agents not only for rheumatoid arthritis but also hopefully study them in other diseases,” he said.
The CREDO 3 trial was sponsored by R-Pharm. Some of the authors are employees of R-Pharm. Dr. Fleischmann and some of his coauthors reported financial ties to R-Pharm and other pharmaceutical companies. Dr. Moreland reported having no relevant competing interests.
FROM ANNALS OF THE RHEUMATIC DISEASES
Dual-Physician Marriages: Understanding the Challenges and Rewards
Dual-physician marriages are becoming increasingly common. The estimated median age of first marriage has been increasing; the US Census Bureau reported a median age of 30.4 years for men and 28.6 years for women in early 2021.1 According to the Association of American Medical Colleges 2020 Matriculating Student Questionnaire, the median age at matriculation for medical students was 23 years (N=16,956), and 92.4% (N=15,932) reported their marital status as single and never legally married.2 Thus, it is likely that the majority of physicians get married at some point during medical school or residency training. A survey of over 10,000 physicians in more than 29 specialties showed that 24% of female physicians and 15% of male physicians are married to other physicians.3
Challenges
There are common challenges to all dual-career households, including coordinating demanding career schedules that compete with each other, balancing childrearing with career advancement, and harmonizing economic and personal goals. However, there are challenges that can be amplified in and unique to dual-physician marriages.
The Couples Match—Medical students, trainees, and even physicians in later stages of their careers may have less autonomy over their schedules compared to professionals in other fields. An early obstacle that many dual-physician marriages must overcome is navigating the National Resident Matching Program as a couple. The number of individuals participating as a couple in the 2022 Main Residency Match was 2444, and the postgraduate year 1 (PGY-1) match rate for individuals participating as a couple was 93.7%. The overall PGY-1 match rate for MD seniors in the United States was 92.9%.4 Thus, entering the match as a couple does not necessarily pose a disadvantage to successfully matching, but these statistics may be misleading. When applicants participate in the Match as a couple, their rank order lists form pairs of program choices that are processed by the matching algorithm to match the couple to the most preferred pair of programs on their rank order lists where each partner has been offered a position. Although many couples coordinate their rank order lists geographically, there is no guarantee that the couple will actually match together in the same city, let alone in the same time zone. Also, the statistics do not take into account if an individual in the couple is only partially matched (eg, if one applicant matches to a preliminary year position but not to an advanced dermatology position). The couples’ Match is only available to partners in the same application cycle, and couples that are not in sync may be more restricted when applying for residency positions.
Lack of Synchronization—Dual-physician couples are challenged to achieve synchronization not only in their day-to-day lives but also over the course of their careers. After matching to residency, the dual-physician couple faces additional scheduling stressors during training. Varied demanding patient schedules and competing call schedules may take a toll on the ability to spend time together. Coordination between both training programs to ensure weekend schedules and vacations are aligned can be helpful to try to maximize time together. If the couple’s education is staggered, their training schedules may not align when proceeding to fellowship or starting off with a new job as an attending. It is not uncommon for couples in medicine to be long-distance for a period of time, and partners may find themselves sacrificing ideal positions or self-restricting application to certain programs or jobs to secure a position near a partner who is already in training in a certain geographic location.
Domestic Work-Life Balance—Juxtaposing 2 highly demanding careers in the same household can be associated with certain tensions, as the weight of household and childrearing responsibilities as well as professional productivity and advancement is divided by the couple. In a 2008 survey of the American College of Surgeons on burnout, work-home conflict, and career satisfaction, surgeons in dual-physician relationships experienced a recent career conflict with their domestic partner and a work-home conflict more often than surgeons whose partners were working nonphysicians.5 The hours worked between men and women in dual-physician families differed according to a national sample of 9868 physicians in dual-physician relationships. The study showed that weekly hours worked by women with children were lower than among those without children, whereas similar differences were not observed among men.6 It is not understood if this suggests that women in dual-physician families work fewer hours due to the pressures of historical gender norms and increased household responsibilities. A 1988 survey of female physicians (N=382) in which 247 respondents indicated that they had domestic partners showed that women physicians whose partners also were physicians (n=91) were more than twice as likely to interrupt their own careers for their partners’ careers compared to female physicians whose partners were not physicians (n=156)(25% vs 11%, respectively). In contrast, the male partners who were not physicians were significantly more likely to interrupt their careers than male partners who were physicians (41% vs 15%, respectively, P<.05).7
Divorce—There have been mixed reports on the incidence of divorce in physicians compared to the general population, but studies suggest that physicians’ marriages tend to be more stable than those of other societal groups.8 Of 203 respondents of a survey of female physician members of the Minnesota Medical Association who were or had been married to another physician, 11.3% (22/203) were divorced, and medicine was reported to play a role in 69.6% of those separations.9 A retrospective analysis of nationally representative surveys by the US Census showed that divorce among physicians is less common than among non–health care workers and several other health professions.10
Rewards
The benefits of medical marriages are multifold and include increased job satisfaction, stability, financial security, shared passions, and mutual understanding. Common passions and interests form the foundation for many relationships, which is true for the dual-physician marriage. In a 2009 study, Perlman et al11 performed qualitative interviews with 25 physicians and their partners—10 of which were in dual-physician relationships—about the challenges and strengths of their relationships. A key theme that emerged during the interviews was the acknowledgment of the benefits of being a physician to the relationship. Participants discussed both the financial security in a physician marriage and the security that medical knowledge adds to a relationship when caring for ill or injured family members. Other key themes identified were relying on mutual support in the relationship, recognizing the important role of each family member, and having shared values.11
Financial Security—The financial security attributed to being in a medical marriage was highlighted in a series of interviews with physicians and their spouses.11 A cross-sectional survey of a random sample of physicians showed that both men and women in dual-physician families had lower personal incomes than physicians married to nonphysicians. However, men and women in dual-physician families had spouses with higher incomes compared to spouses of physicians married to nonphysicians. Thus, the total family incomes were substantially higher in dual-physician households than the family incomes of physicians married to nonphysicians.12
Satisfaction—Dual-physician marriages benefit from a shared camaraderie and understanding of the joys and sacrifices that accompany pursuing a career in medicine. Medical spouses can communicate in mutually understood medical jargon. Compared to physicians married to nonphysicians, a statistically significant difference (P<.001) was found in physicians in dual-physicians families who more frequently reported enjoyment in discussing work with their spouses and more frequently reported satisfaction from shared work interests with their spouses.12
Final Thoughts
From the start of medical training, physicians and physicians-in-training experience unique benefits and challenges that are compounded in distinctive ways when 2 physicians get married. In an era where dual-physician marriage is becoming more common, it is important to acknowledge how this can both enrich and challenge the relationship.
Acknowledgment—The author thanks her husband Joshua L. Weinstock, MD (Camden, New Jersey), for his contribution to this article and their marriage.
- Census Bureau releases new estimates on America’s families and living arrangements. News release. US Census Bureau; November 29, 2021. Accessed September 23, 2022. https://www.census.gov/newsroom/press-releases/2021/families-and-living-arrangements.html
- Association of American Medical Colleges. Matriculating Student Questionnaire: 2020 All Schools Summary Report. Published December 2020. Accessed September 12, 2022. https://www.aamc.org/media/50081/download
- Baggett SM, Martin KL. Medscape physician lifestyle & happiness report 2022. Medscape. January 14, 2022. Accessed September 19, 2022. https://www.medscape.com/slideshow/2022-lifestyle-happiness-6014665
- National Resident Matching Program. Results and Data 2022 Main Residency Match. Published May 2022. Accessed September 12, 2022. https://www.nrmp.org/wp-content/uploads/2022/05/2022-Main-Match-Results-and-Data_Final.pdf
- Dyrbye LN, Shanafelt TD, Balch CM, et al. Physicians married or partnered to physicians: a comparative study in the American College of Surgeons. J Am Coll Surg. 2010;211:663-671. doi:10.1016/j.jamcollsurg.2010.03.032
- Ly DP, Seabury SA, Jena AB. Hours worked among US dual physician couples with children, 2000 to 2015. JAMA Intern Med. 2017;177:1524-1525. doi:10.1001/jamainternmed.2017.3437
- Tesch BJ, Osborne J, Simpson DE, et al. Women physicians in dual-physician relationships compared with those in other dual-career relationships. Acad Med. 1992;67:542-544. doi:10.1097/00001888-199208000-00014
- Doherty WJ, Burge SK. Divorce among physicians. comparisons with other occupational groups. JAMA. 1989;261:2374-2377.
- Smith C, Boulger J, Beattie K. Exploring the dual-physician marriage. Minn Med. 2002;85:39-43.
- Ly DP, Seabury SA, Jena AB. Divorce among physicians and other healthcare professionals in the United States: analysis of census survey data. BMJ. 2015;350:h706. doi:10.1136/bmj.h706
- Perlman RL, Ross PT, Lypson ML. Understanding the medical marriage: physicians and their partners share strategies for success. Acad Med. 2015;90:63-68. doi:10.1097/ACM.0000000000000449
- Sobecks NW, Justice AC, Hinze S, et al. When doctors marry doctors: a survey exploring the professional and family lives of young physicians. Ann Intern Med. 1999;130(4 pt 1):312-319. doi:10.7326/0003-4819-130-4-199902160-00017
Dual-physician marriages are becoming increasingly common. The estimated median age of first marriage has been increasing; the US Census Bureau reported a median age of 30.4 years for men and 28.6 years for women in early 2021.1 According to the Association of American Medical Colleges 2020 Matriculating Student Questionnaire, the median age at matriculation for medical students was 23 years (N=16,956), and 92.4% (N=15,932) reported their marital status as single and never legally married.2 Thus, it is likely that the majority of physicians get married at some point during medical school or residency training. A survey of over 10,000 physicians in more than 29 specialties showed that 24% of female physicians and 15% of male physicians are married to other physicians.3
Challenges
There are common challenges to all dual-career households, including coordinating demanding career schedules that compete with each other, balancing childrearing with career advancement, and harmonizing economic and personal goals. However, there are challenges that can be amplified in and unique to dual-physician marriages.
The Couples Match—Medical students, trainees, and even physicians in later stages of their careers may have less autonomy over their schedules compared to professionals in other fields. An early obstacle that many dual-physician marriages must overcome is navigating the National Resident Matching Program as a couple. The number of individuals participating as a couple in the 2022 Main Residency Match was 2444, and the postgraduate year 1 (PGY-1) match rate for individuals participating as a couple was 93.7%. The overall PGY-1 match rate for MD seniors in the United States was 92.9%.4 Thus, entering the match as a couple does not necessarily pose a disadvantage to successfully matching, but these statistics may be misleading. When applicants participate in the Match as a couple, their rank order lists form pairs of program choices that are processed by the matching algorithm to match the couple to the most preferred pair of programs on their rank order lists where each partner has been offered a position. Although many couples coordinate their rank order lists geographically, there is no guarantee that the couple will actually match together in the same city, let alone in the same time zone. Also, the statistics do not take into account if an individual in the couple is only partially matched (eg, if one applicant matches to a preliminary year position but not to an advanced dermatology position). The couples’ Match is only available to partners in the same application cycle, and couples that are not in sync may be more restricted when applying for residency positions.
Lack of Synchronization—Dual-physician couples are challenged to achieve synchronization not only in their day-to-day lives but also over the course of their careers. After matching to residency, the dual-physician couple faces additional scheduling stressors during training. Varied demanding patient schedules and competing call schedules may take a toll on the ability to spend time together. Coordination between both training programs to ensure weekend schedules and vacations are aligned can be helpful to try to maximize time together. If the couple’s education is staggered, their training schedules may not align when proceeding to fellowship or starting off with a new job as an attending. It is not uncommon for couples in medicine to be long-distance for a period of time, and partners may find themselves sacrificing ideal positions or self-restricting application to certain programs or jobs to secure a position near a partner who is already in training in a certain geographic location.
Domestic Work-Life Balance—Juxtaposing 2 highly demanding careers in the same household can be associated with certain tensions, as the weight of household and childrearing responsibilities as well as professional productivity and advancement is divided by the couple. In a 2008 survey of the American College of Surgeons on burnout, work-home conflict, and career satisfaction, surgeons in dual-physician relationships experienced a recent career conflict with their domestic partner and a work-home conflict more often than surgeons whose partners were working nonphysicians.5 The hours worked between men and women in dual-physician families differed according to a national sample of 9868 physicians in dual-physician relationships. The study showed that weekly hours worked by women with children were lower than among those without children, whereas similar differences were not observed among men.6 It is not understood if this suggests that women in dual-physician families work fewer hours due to the pressures of historical gender norms and increased household responsibilities. A 1988 survey of female physicians (N=382) in which 247 respondents indicated that they had domestic partners showed that women physicians whose partners also were physicians (n=91) were more than twice as likely to interrupt their own careers for their partners’ careers compared to female physicians whose partners were not physicians (n=156)(25% vs 11%, respectively). In contrast, the male partners who were not physicians were significantly more likely to interrupt their careers than male partners who were physicians (41% vs 15%, respectively, P<.05).7
Divorce—There have been mixed reports on the incidence of divorce in physicians compared to the general population, but studies suggest that physicians’ marriages tend to be more stable than those of other societal groups.8 Of 203 respondents of a survey of female physician members of the Minnesota Medical Association who were or had been married to another physician, 11.3% (22/203) were divorced, and medicine was reported to play a role in 69.6% of those separations.9 A retrospective analysis of nationally representative surveys by the US Census showed that divorce among physicians is less common than among non–health care workers and several other health professions.10
Rewards
The benefits of medical marriages are multifold and include increased job satisfaction, stability, financial security, shared passions, and mutual understanding. Common passions and interests form the foundation for many relationships, which is true for the dual-physician marriage. In a 2009 study, Perlman et al11 performed qualitative interviews with 25 physicians and their partners—10 of which were in dual-physician relationships—about the challenges and strengths of their relationships. A key theme that emerged during the interviews was the acknowledgment of the benefits of being a physician to the relationship. Participants discussed both the financial security in a physician marriage and the security that medical knowledge adds to a relationship when caring for ill or injured family members. Other key themes identified were relying on mutual support in the relationship, recognizing the important role of each family member, and having shared values.11
Financial Security—The financial security attributed to being in a medical marriage was highlighted in a series of interviews with physicians and their spouses.11 A cross-sectional survey of a random sample of physicians showed that both men and women in dual-physician families had lower personal incomes than physicians married to nonphysicians. However, men and women in dual-physician families had spouses with higher incomes compared to spouses of physicians married to nonphysicians. Thus, the total family incomes were substantially higher in dual-physician households than the family incomes of physicians married to nonphysicians.12
Satisfaction—Dual-physician marriages benefit from a shared camaraderie and understanding of the joys and sacrifices that accompany pursuing a career in medicine. Medical spouses can communicate in mutually understood medical jargon. Compared to physicians married to nonphysicians, a statistically significant difference (P<.001) was found in physicians in dual-physicians families who more frequently reported enjoyment in discussing work with their spouses and more frequently reported satisfaction from shared work interests with their spouses.12
Final Thoughts
From the start of medical training, physicians and physicians-in-training experience unique benefits and challenges that are compounded in distinctive ways when 2 physicians get married. In an era where dual-physician marriage is becoming more common, it is important to acknowledge how this can both enrich and challenge the relationship.
Acknowledgment—The author thanks her husband Joshua L. Weinstock, MD (Camden, New Jersey), for his contribution to this article and their marriage.
Dual-physician marriages are becoming increasingly common. The estimated median age of first marriage has been increasing; the US Census Bureau reported a median age of 30.4 years for men and 28.6 years for women in early 2021.1 According to the Association of American Medical Colleges 2020 Matriculating Student Questionnaire, the median age at matriculation for medical students was 23 years (N=16,956), and 92.4% (N=15,932) reported their marital status as single and never legally married.2 Thus, it is likely that the majority of physicians get married at some point during medical school or residency training. A survey of over 10,000 physicians in more than 29 specialties showed that 24% of female physicians and 15% of male physicians are married to other physicians.3
Challenges
There are common challenges to all dual-career households, including coordinating demanding career schedules that compete with each other, balancing childrearing with career advancement, and harmonizing economic and personal goals. However, there are challenges that can be amplified in and unique to dual-physician marriages.
The Couples Match—Medical students, trainees, and even physicians in later stages of their careers may have less autonomy over their schedules compared to professionals in other fields. An early obstacle that many dual-physician marriages must overcome is navigating the National Resident Matching Program as a couple. The number of individuals participating as a couple in the 2022 Main Residency Match was 2444, and the postgraduate year 1 (PGY-1) match rate for individuals participating as a couple was 93.7%. The overall PGY-1 match rate for MD seniors in the United States was 92.9%.4 Thus, entering the match as a couple does not necessarily pose a disadvantage to successfully matching, but these statistics may be misleading. When applicants participate in the Match as a couple, their rank order lists form pairs of program choices that are processed by the matching algorithm to match the couple to the most preferred pair of programs on their rank order lists where each partner has been offered a position. Although many couples coordinate their rank order lists geographically, there is no guarantee that the couple will actually match together in the same city, let alone in the same time zone. Also, the statistics do not take into account if an individual in the couple is only partially matched (eg, if one applicant matches to a preliminary year position but not to an advanced dermatology position). The couples’ Match is only available to partners in the same application cycle, and couples that are not in sync may be more restricted when applying for residency positions.
Lack of Synchronization—Dual-physician couples are challenged to achieve synchronization not only in their day-to-day lives but also over the course of their careers. After matching to residency, the dual-physician couple faces additional scheduling stressors during training. Varied demanding patient schedules and competing call schedules may take a toll on the ability to spend time together. Coordination between both training programs to ensure weekend schedules and vacations are aligned can be helpful to try to maximize time together. If the couple’s education is staggered, their training schedules may not align when proceeding to fellowship or starting off with a new job as an attending. It is not uncommon for couples in medicine to be long-distance for a period of time, and partners may find themselves sacrificing ideal positions or self-restricting application to certain programs or jobs to secure a position near a partner who is already in training in a certain geographic location.
Domestic Work-Life Balance—Juxtaposing 2 highly demanding careers in the same household can be associated with certain tensions, as the weight of household and childrearing responsibilities as well as professional productivity and advancement is divided by the couple. In a 2008 survey of the American College of Surgeons on burnout, work-home conflict, and career satisfaction, surgeons in dual-physician relationships experienced a recent career conflict with their domestic partner and a work-home conflict more often than surgeons whose partners were working nonphysicians.5 The hours worked between men and women in dual-physician families differed according to a national sample of 9868 physicians in dual-physician relationships. The study showed that weekly hours worked by women with children were lower than among those without children, whereas similar differences were not observed among men.6 It is not understood if this suggests that women in dual-physician families work fewer hours due to the pressures of historical gender norms and increased household responsibilities. A 1988 survey of female physicians (N=382) in which 247 respondents indicated that they had domestic partners showed that women physicians whose partners also were physicians (n=91) were more than twice as likely to interrupt their own careers for their partners’ careers compared to female physicians whose partners were not physicians (n=156)(25% vs 11%, respectively). In contrast, the male partners who were not physicians were significantly more likely to interrupt their careers than male partners who were physicians (41% vs 15%, respectively, P<.05).7
Divorce—There have been mixed reports on the incidence of divorce in physicians compared to the general population, but studies suggest that physicians’ marriages tend to be more stable than those of other societal groups.8 Of 203 respondents of a survey of female physician members of the Minnesota Medical Association who were or had been married to another physician, 11.3% (22/203) were divorced, and medicine was reported to play a role in 69.6% of those separations.9 A retrospective analysis of nationally representative surveys by the US Census showed that divorce among physicians is less common than among non–health care workers and several other health professions.10
Rewards
The benefits of medical marriages are multifold and include increased job satisfaction, stability, financial security, shared passions, and mutual understanding. Common passions and interests form the foundation for many relationships, which is true for the dual-physician marriage. In a 2009 study, Perlman et al11 performed qualitative interviews with 25 physicians and their partners—10 of which were in dual-physician relationships—about the challenges and strengths of their relationships. A key theme that emerged during the interviews was the acknowledgment of the benefits of being a physician to the relationship. Participants discussed both the financial security in a physician marriage and the security that medical knowledge adds to a relationship when caring for ill or injured family members. Other key themes identified were relying on mutual support in the relationship, recognizing the important role of each family member, and having shared values.11
Financial Security—The financial security attributed to being in a medical marriage was highlighted in a series of interviews with physicians and their spouses.11 A cross-sectional survey of a random sample of physicians showed that both men and women in dual-physician families had lower personal incomes than physicians married to nonphysicians. However, men and women in dual-physician families had spouses with higher incomes compared to spouses of physicians married to nonphysicians. Thus, the total family incomes were substantially higher in dual-physician households than the family incomes of physicians married to nonphysicians.12
Satisfaction—Dual-physician marriages benefit from a shared camaraderie and understanding of the joys and sacrifices that accompany pursuing a career in medicine. Medical spouses can communicate in mutually understood medical jargon. Compared to physicians married to nonphysicians, a statistically significant difference (P<.001) was found in physicians in dual-physicians families who more frequently reported enjoyment in discussing work with their spouses and more frequently reported satisfaction from shared work interests with their spouses.12
Final Thoughts
From the start of medical training, physicians and physicians-in-training experience unique benefits and challenges that are compounded in distinctive ways when 2 physicians get married. In an era where dual-physician marriage is becoming more common, it is important to acknowledge how this can both enrich and challenge the relationship.
Acknowledgment—The author thanks her husband Joshua L. Weinstock, MD (Camden, New Jersey), for his contribution to this article and their marriage.
- Census Bureau releases new estimates on America’s families and living arrangements. News release. US Census Bureau; November 29, 2021. Accessed September 23, 2022. https://www.census.gov/newsroom/press-releases/2021/families-and-living-arrangements.html
- Association of American Medical Colleges. Matriculating Student Questionnaire: 2020 All Schools Summary Report. Published December 2020. Accessed September 12, 2022. https://www.aamc.org/media/50081/download
- Baggett SM, Martin KL. Medscape physician lifestyle & happiness report 2022. Medscape. January 14, 2022. Accessed September 19, 2022. https://www.medscape.com/slideshow/2022-lifestyle-happiness-6014665
- National Resident Matching Program. Results and Data 2022 Main Residency Match. Published May 2022. Accessed September 12, 2022. https://www.nrmp.org/wp-content/uploads/2022/05/2022-Main-Match-Results-and-Data_Final.pdf
- Dyrbye LN, Shanafelt TD, Balch CM, et al. Physicians married or partnered to physicians: a comparative study in the American College of Surgeons. J Am Coll Surg. 2010;211:663-671. doi:10.1016/j.jamcollsurg.2010.03.032
- Ly DP, Seabury SA, Jena AB. Hours worked among US dual physician couples with children, 2000 to 2015. JAMA Intern Med. 2017;177:1524-1525. doi:10.1001/jamainternmed.2017.3437
- Tesch BJ, Osborne J, Simpson DE, et al. Women physicians in dual-physician relationships compared with those in other dual-career relationships. Acad Med. 1992;67:542-544. doi:10.1097/00001888-199208000-00014
- Doherty WJ, Burge SK. Divorce among physicians. comparisons with other occupational groups. JAMA. 1989;261:2374-2377.
- Smith C, Boulger J, Beattie K. Exploring the dual-physician marriage. Minn Med. 2002;85:39-43.
- Ly DP, Seabury SA, Jena AB. Divorce among physicians and other healthcare professionals in the United States: analysis of census survey data. BMJ. 2015;350:h706. doi:10.1136/bmj.h706
- Perlman RL, Ross PT, Lypson ML. Understanding the medical marriage: physicians and their partners share strategies for success. Acad Med. 2015;90:63-68. doi:10.1097/ACM.0000000000000449
- Sobecks NW, Justice AC, Hinze S, et al. When doctors marry doctors: a survey exploring the professional and family lives of young physicians. Ann Intern Med. 1999;130(4 pt 1):312-319. doi:10.7326/0003-4819-130-4-199902160-00017
- Census Bureau releases new estimates on America’s families and living arrangements. News release. US Census Bureau; November 29, 2021. Accessed September 23, 2022. https://www.census.gov/newsroom/press-releases/2021/families-and-living-arrangements.html
- Association of American Medical Colleges. Matriculating Student Questionnaire: 2020 All Schools Summary Report. Published December 2020. Accessed September 12, 2022. https://www.aamc.org/media/50081/download
- Baggett SM, Martin KL. Medscape physician lifestyle & happiness report 2022. Medscape. January 14, 2022. Accessed September 19, 2022. https://www.medscape.com/slideshow/2022-lifestyle-happiness-6014665
- National Resident Matching Program. Results and Data 2022 Main Residency Match. Published May 2022. Accessed September 12, 2022. https://www.nrmp.org/wp-content/uploads/2022/05/2022-Main-Match-Results-and-Data_Final.pdf
- Dyrbye LN, Shanafelt TD, Balch CM, et al. Physicians married or partnered to physicians: a comparative study in the American College of Surgeons. J Am Coll Surg. 2010;211:663-671. doi:10.1016/j.jamcollsurg.2010.03.032
- Ly DP, Seabury SA, Jena AB. Hours worked among US dual physician couples with children, 2000 to 2015. JAMA Intern Med. 2017;177:1524-1525. doi:10.1001/jamainternmed.2017.3437
- Tesch BJ, Osborne J, Simpson DE, et al. Women physicians in dual-physician relationships compared with those in other dual-career relationships. Acad Med. 1992;67:542-544. doi:10.1097/00001888-199208000-00014
- Doherty WJ, Burge SK. Divorce among physicians. comparisons with other occupational groups. JAMA. 1989;261:2374-2377.
- Smith C, Boulger J, Beattie K. Exploring the dual-physician marriage. Minn Med. 2002;85:39-43.
- Ly DP, Seabury SA, Jena AB. Divorce among physicians and other healthcare professionals in the United States: analysis of census survey data. BMJ. 2015;350:h706. doi:10.1136/bmj.h706
- Perlman RL, Ross PT, Lypson ML. Understanding the medical marriage: physicians and their partners share strategies for success. Acad Med. 2015;90:63-68. doi:10.1097/ACM.0000000000000449
- Sobecks NW, Justice AC, Hinze S, et al. When doctors marry doctors: a survey exploring the professional and family lives of young physicians. Ann Intern Med. 1999;130(4 pt 1):312-319. doi:10.7326/0003-4819-130-4-199902160-00017
Resident Pearl
- As more physicians marry other physicians, there is an increasing need to understand the challenges and rewards of these relationships.
HIV Pre-exposure Prophylaxis (PrEP): A Survey of Dermatologists’ Knowledge and Practice Patterns
To the Editor:
In a 2010 landmark paper, researchers reported that the Preexposure Prophylaxis Initiative (iPrEx) trial demonstrated that once-daily pre-exposure prophylaxis (PrEP) with emtricitabine plus tenofovir disoproxil fumarate, which was approved by the US Food and Drug Administration (FDA) and packaged together as Truvada (Gilead Sciences, Inc), achieved a 44% reduction in the incidence of HIV infection compared to the placebo arm of the study (64/1248 HIV infections in the placebo group vs 36/1251 in the intervention group).1 Subsequently, the US Department of Health and Human Services proposed an initiative to reduce new HIV infections by 90% by 2030.2 The Centers for Disease Control and Prevention estimates that 1.1 million Americans have an indication for PrEP, yet only approximately 400,000 individuals currently take PrEP.3,4
Increasing awareness of PrEP and its indications is essential because PrEP exerts its greatest benefit when used broadly. Awareness among primary care and infectious disease physicians was reported at 76%5; awareness among other medical specialists remains unknown. Awareness of PrEP among dermatologists is important because dermatologists play an important role in the diagnosis and treatment of many sexually transmitted infections (STIs), which are a risk factor for transmission of HIV. As providers who treat STIs, dermatologists are in a prime position to educate patients about PrEP, refer them for treatment, and prescribe the regimen. We conducted a survey to assess dermatologists’ knowledge about and attitudes toward PrEP. We also provide a brief summary of prescribing information about common PrEP regimens to fill in the knowledge gap among dermatologists as a way to promote its utilization.
An electronic survey was distributed to 486 members of the Association of Professors of Dermatology based in the United States using the web-based survey application REDCap. The study was approved by the New York University Grossman School of Medicine (New York, New York) institutional review board. Eighty-one anonymous survey responses were completed and returned (response rate, 16.6%). Data were analyzed using descriptive statistics.
The mean age (SD) of respondents was 39.1 (9.7) years; 49.4% (40/81) were male; and 74.1% (60/81) were attending physicians, with a mean (SD) of 9.4 (8.6) years of practice. Clinical practices were predominantly from the northeast (46.9% [38/81]) and mostly in an academic setting (74.1% [60/81]). As shown in Table 1, most surveyed dermatologists reported being aware of PrEP (93.8% [76/81]), but a minority (42.0% [34/81]) were familiar with indications for its use; even fewer (4.9% [4/81]) were current prescribers. Referral to other physicians for PrEP was reported by 58.0% (47/81) of respondents.
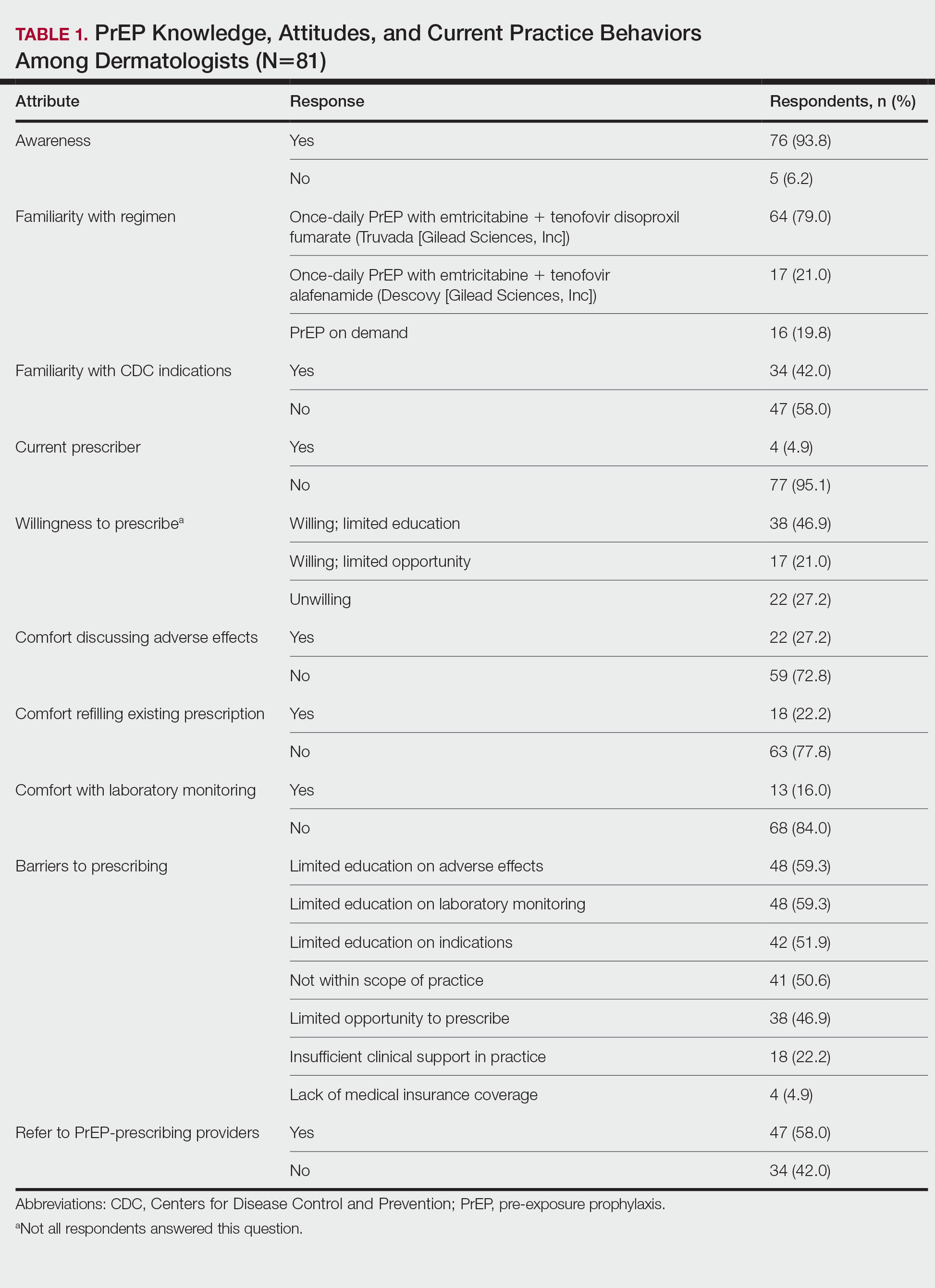
Despite respondents’ awareness of PrEP as a preventive measure (93.8% [76/81]) and their willingness to prescribe it (67.9% [55/81]), many reported being largely unfamiliar with its indications (58.0% [47/81]) and uncomfortable discussing its adverse effects (72.8% [59/81]), conducting appropriate laboratory monitoring (84.0% [68/81]), and refilling existing prescriptions (77.8% [63/81]). Respondents’ lack of education about PrEP was a barrier to prescribing (51.9% [42/81] to 59.3% [48/81]) and explains why a small minority (4.9% [4/81]) currently prescribe the regimen.
Our study sought to characterize current clinical knowledge about and practice patterns of PrEP among dermatologists. Dermatologists often encounter patients who present with an STI, which is a risk factor for HIV infection, but our survey respondents reported several barriers to utilizing PrEP. The difference in the degree of respondents’ willingness to prescribe PrEP (67.9%) and those who self-identified as prescribers (4.9%) suggests a role for dermatologists in prescribing or discussing PrEP with their patients—albeit a currently undefined role.
The results of our study suggested that half (41/81) of dermatologists believe that PrEP prescription is out of their scope of practice, likely due to a combination of scheduling, laboratory monitoring, and medicolegal concerns. For dermatologists who are interested in being PrEP prescribers, our results suggested that closing the knowledge gap around PrEP among dermatologists through training and education could improve comfort with this medication and lead to changes in practice to prevent the spread of HIV infection.
PrEP is indicated for HIV-negative patients who have HIV-positive sexual partners, utilize barrier protection methods inconsistently, or had a diagnosis of an STI in the last 6 months.6 In 2012, the FDA approved once-daily use of emtricitabine plus tenofovir for primary prevention of HIV infection. Post hoc analysis of iPrEx trial data revealed that once-daily PrEP taken regularly had a 92% to 100% protective effect against HIV.7
Regrettably, real-world uptake of PrEP has been slower than desired. The most recent data (2021) show that nearly 1 million individuals worldwide take PrEP; however, this represents only approximately one-third of those eligible.8 Utilization is notably lower among Black and Latino populations who stand to gain the most from PrEP given their higher risk of contracting HIV compared to their White counterparts.9 As such, improving access to PrEP through expanded provider awareness is essential to decrease the risk for HIV infection and transmission.
Emtricitabine plus tenofovir is safe and well tolerated; more common adverse effects are headache, nausea, vomiting, rash, and loss of appetite. Tenofovir likely decreases bone mineral density, even in HIV-negative patients10; mineralization seems to recover after the medication is discontinued.11 Rarely, tenofovir can increase the level of creatinine and hepatic transaminases; a recent report on its long-term side effects has shown small nonprogressive decreases in glomerular filtration rate.12 Monitoring kidney function is a component of prescribing PrEP (Table 2).
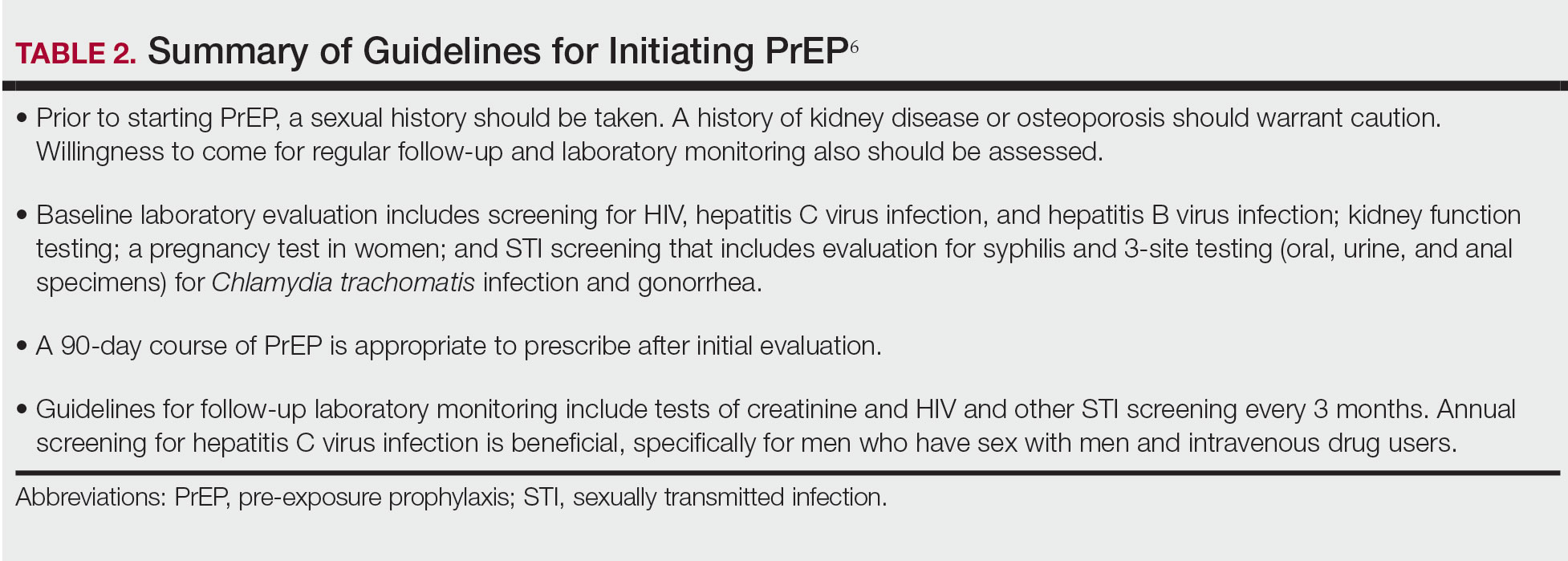
In 2019, emtricitabine plus tenofovir was reformulated with tenofovir alafenamide; the new combination regimen received FDA approval for once-daily PrEP under the brand name Descovy (Gilead Sciences, Inc). The new formulation results in a lower blood concentration of tenofovir and has been reported to present less of a risk for bone and kidney toxicity.13,14
Notably, emtricitabine plus tenofovir alafenamide might accumulate faster in peripheral lymphatic tissue than emtricitabine plus tenofovir disoproxil fumarate. This property has led to a new regimen known as “on-demand PrEP,” which follows a 2-1-1 dosing regimen: Patients take a double dose 2 to 24 hours before sexual activity, 1 dose on the day of sexual activity, and 1 dose the day after sexual activity.15 Because some patients at risk for HIV infection might not be consistently sexually active, on-demand PrEP allows them to cycle on and off the medication. Barriers to implementing on-demand PrEP include requiring that sexual activity be planned and an adverse effect profile similar to daily-use PrEP.16
The FDA recently approved a long-acting, once-monthly combination injectable PrEP of cabotegravir and rilpivirine.17 The long duration of action of this PrEP will benefit patients who report problems with medication adherence.
Our study demonstrates low frequency in prescribing patterns of PrEP among dermatologists and suggests that an addressable barrier to such prescribing is the lack of knowledge on how to prescribe it safely, which warrants further clinical investigation. We summarize an approach to prescribing PrEP in Table 2. Our study was limited by a small sample of mostly academic dermatologists and selection bias, which may diminish the generalizability of findings. A study of a larger, more representative group of dermatologists likely would show different prescribing patterns and degrees of knowledge about PrEP. Research is needed to study the impact of educational interventions that aim to increase both knowledge and prescribing of PrEP among dermatologists.
- Grant RM, Lama JR, Anderson PL, et al; iPrEx Study Team. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587-2599. doi:10.1056/NEJMoa1011205
- Fauci AS, Redfield RR, Sigounas G, et al. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321:844-845. doi:10.1001/jama.2019.1343
- Smith DK, Van Handel M, Grey J. Estimates of adults with indications for HIV pre-exposure prophylaxis by jurisdiction, transmission risk group, and race/ethnicity, United States, 2015. Ann Epidemiol. 2018;28:850-857.e9. doi:10.1016/j.annepidem.2018.05.003
- Song HJ, Squires P, Wilson D, et al. Trends in HIV preexposure prophylaxis prescribing in the United States, 2012-2018. JAMA. 2020;324:395-397. doi:10.1001/jama.2020.7312
- Petroll AE, Walsh JL, Owczarzak JL, et al. PrEP awareness, familiarity, comfort, and prescribing experience among US primary care providers and HIV specialists. AIDS Behav. 2017;21:1256-1267. doi:10.1007/s10461-016-1625-1
- US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 update. a clinical practice guideline. Centers for Disease Control and Prevention. Accessed September 15, 2022. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf
- Riddell J 4th, Amico KR, Mayer KH. HIV preexposure prophylaxis: a review. JAMA. 2018;319:1261-1268. doi:10.1001/JAMA.2018.1917
- Segal K, Fitch L, Riaz F, et al. The evolution of oral PrEP access: tracking trends in global oral PrEP use over time. J Int AIDS Soc. 2021;24:27-28.
- Elion RA, Kabiri M, Mayer KH, et al. Estimated impact of targeted pre-exposure prophylaxis: strategies for men who have sex with men in the United States. Int J Environ Res Public Health. 2019;16:1592. doi:10.3390/ijerph16091592
- Kasonde M, Niska RW, Rose C, et al. Bone mineral density changes among HIV-uninfected young adults in a randomised trial of pre-exposure prophylaxis with tenofovir-emtricitabine or placebo in Botswana. PLoS One. 2014;9:e90111. doi:10.1371/journal.pone.0090111
- Glidden DV, Mulligan K, McMahan V, et al. Brief report: recovery of bone mineral density after discontinuation of tenofovir-based HIV pre-exposure prophylaxis. J Acquir Immune Defic Syndr. 2017;76:177-182. doi:10.1097/QAI.0000000000001475
- Tang EC, Vittinghoff E, Anderson PL, et al. Changes in kidney function associated with daily tenofovir disoproxil fumarate/emtricitabine for HIV preexposure prophylaxis use in the United States Demonstration Project. J Acquir Immune Defic Syndr. 2018;77:193-198. doi:10.1097/QAI.0000000000001566
- Gupta SK, Post FA, Arribas JR, et al. Renal safety of tenofovir alafenamide vs. tenofovir disoproxil fumarate: a pooled analysis of 26 clinical trials. AIDS. 2019;33:1455-1465. doi:10.1097/QAD.0000000000002223
- Agarwal K, Brunetto M, Seto WK, et al; GS-US-320-0110; GS-US-320-0108 Investigators. 96 weeks treatment of tenofovir alafenamide vs. tenofovir disoproxil fumarate for hepatitis B virus infection [published online January 17, 2018]. J Hepatol. 2018;68:672-681. doi:10.1016/j.jhep.2017.11.039
- Molina JM, Capitant C, Spire B, et al; ANRS IPERGAY Study Group. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection [published online December 1, 2015]. N Engl J Med. 2015;3;2237-2246. doi:10.1056/NEJMoa1506273
- Saberi P, Scott HM. On-demand oral pre-exposure prophylaxis with tenofovir/emtricitabine: what every clinician needs to know. J Gen Intern Med. 2020;35:1285-1288. doi:10.1007/s11606-020-05651-2
- Landovitz RJ, Li S, Grinsztejn B, et al. Safety, tolerability, and pharmacokinetics of long-acting injectable cabotegravir in low-risk HIV-uninfected individuals: HPTN 077, a phase 2a randomized controlled trial. PLoS Med. 2018;15:e1002690. doi:10.1371/journal.pmed.1002690
To the Editor:
In a 2010 landmark paper, researchers reported that the Preexposure Prophylaxis Initiative (iPrEx) trial demonstrated that once-daily pre-exposure prophylaxis (PrEP) with emtricitabine plus tenofovir disoproxil fumarate, which was approved by the US Food and Drug Administration (FDA) and packaged together as Truvada (Gilead Sciences, Inc), achieved a 44% reduction in the incidence of HIV infection compared to the placebo arm of the study (64/1248 HIV infections in the placebo group vs 36/1251 in the intervention group).1 Subsequently, the US Department of Health and Human Services proposed an initiative to reduce new HIV infections by 90% by 2030.2 The Centers for Disease Control and Prevention estimates that 1.1 million Americans have an indication for PrEP, yet only approximately 400,000 individuals currently take PrEP.3,4
Increasing awareness of PrEP and its indications is essential because PrEP exerts its greatest benefit when used broadly. Awareness among primary care and infectious disease physicians was reported at 76%5; awareness among other medical specialists remains unknown. Awareness of PrEP among dermatologists is important because dermatologists play an important role in the diagnosis and treatment of many sexually transmitted infections (STIs), which are a risk factor for transmission of HIV. As providers who treat STIs, dermatologists are in a prime position to educate patients about PrEP, refer them for treatment, and prescribe the regimen. We conducted a survey to assess dermatologists’ knowledge about and attitudes toward PrEP. We also provide a brief summary of prescribing information about common PrEP regimens to fill in the knowledge gap among dermatologists as a way to promote its utilization.
An electronic survey was distributed to 486 members of the Association of Professors of Dermatology based in the United States using the web-based survey application REDCap. The study was approved by the New York University Grossman School of Medicine (New York, New York) institutional review board. Eighty-one anonymous survey responses were completed and returned (response rate, 16.6%). Data were analyzed using descriptive statistics.
The mean age (SD) of respondents was 39.1 (9.7) years; 49.4% (40/81) were male; and 74.1% (60/81) were attending physicians, with a mean (SD) of 9.4 (8.6) years of practice. Clinical practices were predominantly from the northeast (46.9% [38/81]) and mostly in an academic setting (74.1% [60/81]). As shown in Table 1, most surveyed dermatologists reported being aware of PrEP (93.8% [76/81]), but a minority (42.0% [34/81]) were familiar with indications for its use; even fewer (4.9% [4/81]) were current prescribers. Referral to other physicians for PrEP was reported by 58.0% (47/81) of respondents.
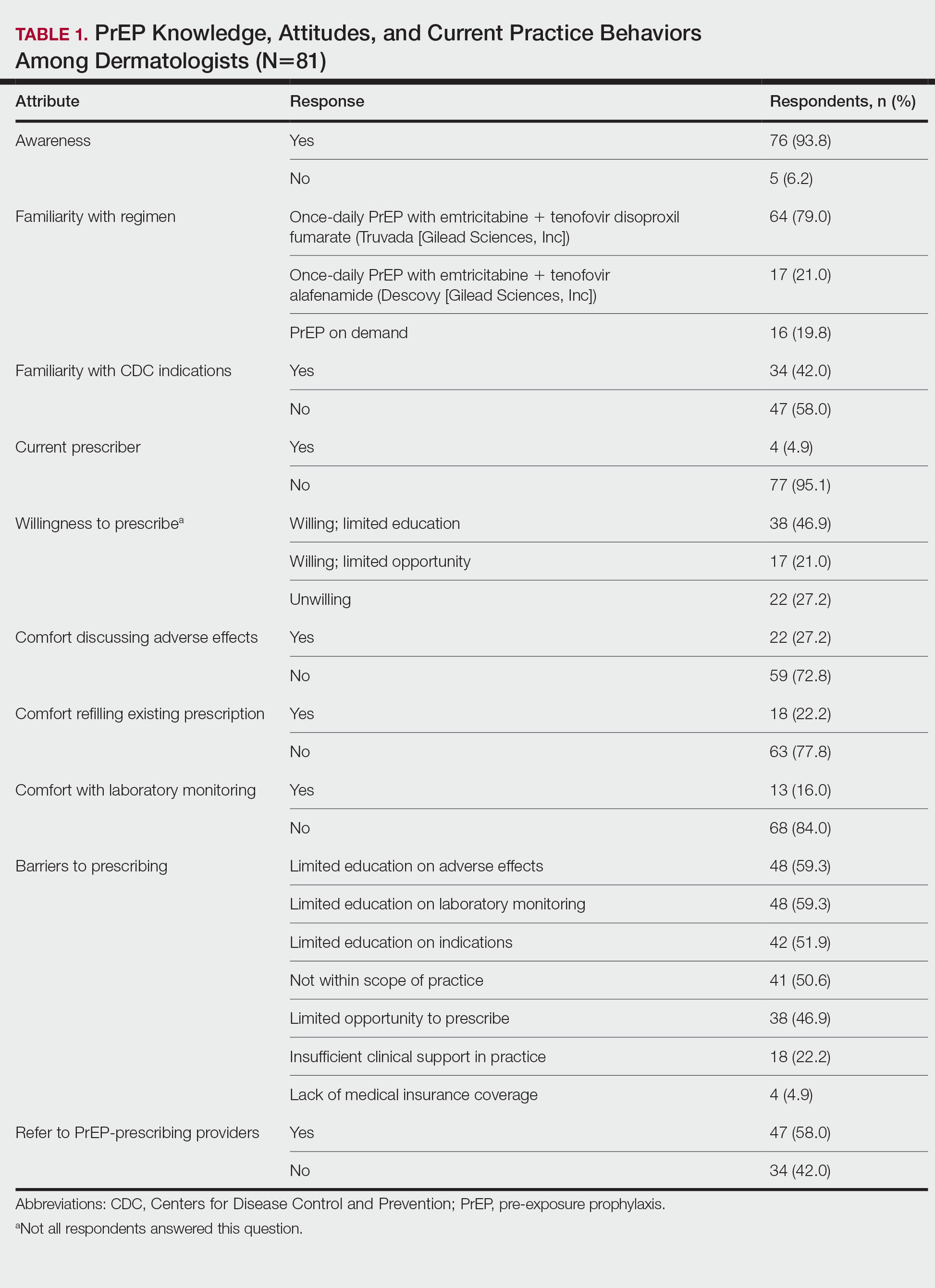
Despite respondents’ awareness of PrEP as a preventive measure (93.8% [76/81]) and their willingness to prescribe it (67.9% [55/81]), many reported being largely unfamiliar with its indications (58.0% [47/81]) and uncomfortable discussing its adverse effects (72.8% [59/81]), conducting appropriate laboratory monitoring (84.0% [68/81]), and refilling existing prescriptions (77.8% [63/81]). Respondents’ lack of education about PrEP was a barrier to prescribing (51.9% [42/81] to 59.3% [48/81]) and explains why a small minority (4.9% [4/81]) currently prescribe the regimen.
Our study sought to characterize current clinical knowledge about and practice patterns of PrEP among dermatologists. Dermatologists often encounter patients who present with an STI, which is a risk factor for HIV infection, but our survey respondents reported several barriers to utilizing PrEP. The difference in the degree of respondents’ willingness to prescribe PrEP (67.9%) and those who self-identified as prescribers (4.9%) suggests a role for dermatologists in prescribing or discussing PrEP with their patients—albeit a currently undefined role.
The results of our study suggested that half (41/81) of dermatologists believe that PrEP prescription is out of their scope of practice, likely due to a combination of scheduling, laboratory monitoring, and medicolegal concerns. For dermatologists who are interested in being PrEP prescribers, our results suggested that closing the knowledge gap around PrEP among dermatologists through training and education could improve comfort with this medication and lead to changes in practice to prevent the spread of HIV infection.
PrEP is indicated for HIV-negative patients who have HIV-positive sexual partners, utilize barrier protection methods inconsistently, or had a diagnosis of an STI in the last 6 months.6 In 2012, the FDA approved once-daily use of emtricitabine plus tenofovir for primary prevention of HIV infection. Post hoc analysis of iPrEx trial data revealed that once-daily PrEP taken regularly had a 92% to 100% protective effect against HIV.7
Regrettably, real-world uptake of PrEP has been slower than desired. The most recent data (2021) show that nearly 1 million individuals worldwide take PrEP; however, this represents only approximately one-third of those eligible.8 Utilization is notably lower among Black and Latino populations who stand to gain the most from PrEP given their higher risk of contracting HIV compared to their White counterparts.9 As such, improving access to PrEP through expanded provider awareness is essential to decrease the risk for HIV infection and transmission.
Emtricitabine plus tenofovir is safe and well tolerated; more common adverse effects are headache, nausea, vomiting, rash, and loss of appetite. Tenofovir likely decreases bone mineral density, even in HIV-negative patients10; mineralization seems to recover after the medication is discontinued.11 Rarely, tenofovir can increase the level of creatinine and hepatic transaminases; a recent report on its long-term side effects has shown small nonprogressive decreases in glomerular filtration rate.12 Monitoring kidney function is a component of prescribing PrEP (Table 2).
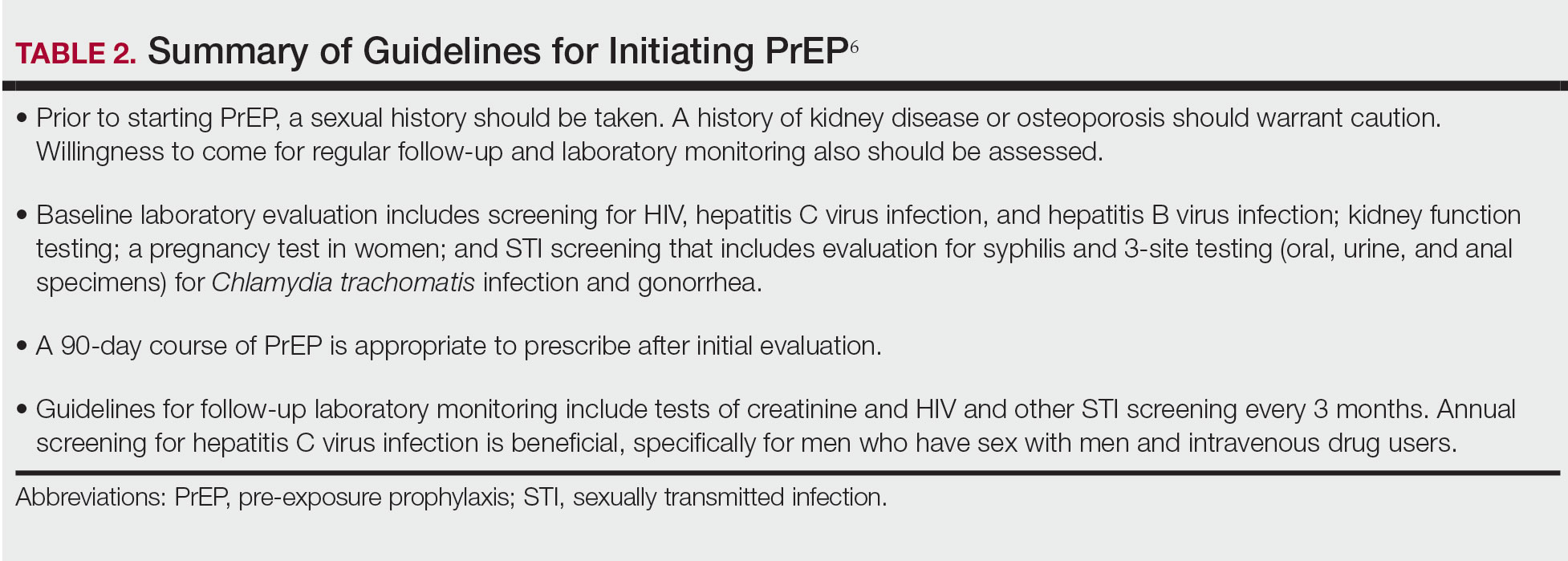
In 2019, emtricitabine plus tenofovir was reformulated with tenofovir alafenamide; the new combination regimen received FDA approval for once-daily PrEP under the brand name Descovy (Gilead Sciences, Inc). The new formulation results in a lower blood concentration of tenofovir and has been reported to present less of a risk for bone and kidney toxicity.13,14
Notably, emtricitabine plus tenofovir alafenamide might accumulate faster in peripheral lymphatic tissue than emtricitabine plus tenofovir disoproxil fumarate. This property has led to a new regimen known as “on-demand PrEP,” which follows a 2-1-1 dosing regimen: Patients take a double dose 2 to 24 hours before sexual activity, 1 dose on the day of sexual activity, and 1 dose the day after sexual activity.15 Because some patients at risk for HIV infection might not be consistently sexually active, on-demand PrEP allows them to cycle on and off the medication. Barriers to implementing on-demand PrEP include requiring that sexual activity be planned and an adverse effect profile similar to daily-use PrEP.16
The FDA recently approved a long-acting, once-monthly combination injectable PrEP of cabotegravir and rilpivirine.17 The long duration of action of this PrEP will benefit patients who report problems with medication adherence.
Our study demonstrates low frequency in prescribing patterns of PrEP among dermatologists and suggests that an addressable barrier to such prescribing is the lack of knowledge on how to prescribe it safely, which warrants further clinical investigation. We summarize an approach to prescribing PrEP in Table 2. Our study was limited by a small sample of mostly academic dermatologists and selection bias, which may diminish the generalizability of findings. A study of a larger, more representative group of dermatologists likely would show different prescribing patterns and degrees of knowledge about PrEP. Research is needed to study the impact of educational interventions that aim to increase both knowledge and prescribing of PrEP among dermatologists.
To the Editor:
In a 2010 landmark paper, researchers reported that the Preexposure Prophylaxis Initiative (iPrEx) trial demonstrated that once-daily pre-exposure prophylaxis (PrEP) with emtricitabine plus tenofovir disoproxil fumarate, which was approved by the US Food and Drug Administration (FDA) and packaged together as Truvada (Gilead Sciences, Inc), achieved a 44% reduction in the incidence of HIV infection compared to the placebo arm of the study (64/1248 HIV infections in the placebo group vs 36/1251 in the intervention group).1 Subsequently, the US Department of Health and Human Services proposed an initiative to reduce new HIV infections by 90% by 2030.2 The Centers for Disease Control and Prevention estimates that 1.1 million Americans have an indication for PrEP, yet only approximately 400,000 individuals currently take PrEP.3,4
Increasing awareness of PrEP and its indications is essential because PrEP exerts its greatest benefit when used broadly. Awareness among primary care and infectious disease physicians was reported at 76%5; awareness among other medical specialists remains unknown. Awareness of PrEP among dermatologists is important because dermatologists play an important role in the diagnosis and treatment of many sexually transmitted infections (STIs), which are a risk factor for transmission of HIV. As providers who treat STIs, dermatologists are in a prime position to educate patients about PrEP, refer them for treatment, and prescribe the regimen. We conducted a survey to assess dermatologists’ knowledge about and attitudes toward PrEP. We also provide a brief summary of prescribing information about common PrEP regimens to fill in the knowledge gap among dermatologists as a way to promote its utilization.
An electronic survey was distributed to 486 members of the Association of Professors of Dermatology based in the United States using the web-based survey application REDCap. The study was approved by the New York University Grossman School of Medicine (New York, New York) institutional review board. Eighty-one anonymous survey responses were completed and returned (response rate, 16.6%). Data were analyzed using descriptive statistics.
The mean age (SD) of respondents was 39.1 (9.7) years; 49.4% (40/81) were male; and 74.1% (60/81) were attending physicians, with a mean (SD) of 9.4 (8.6) years of practice. Clinical practices were predominantly from the northeast (46.9% [38/81]) and mostly in an academic setting (74.1% [60/81]). As shown in Table 1, most surveyed dermatologists reported being aware of PrEP (93.8% [76/81]), but a minority (42.0% [34/81]) were familiar with indications for its use; even fewer (4.9% [4/81]) were current prescribers. Referral to other physicians for PrEP was reported by 58.0% (47/81) of respondents.
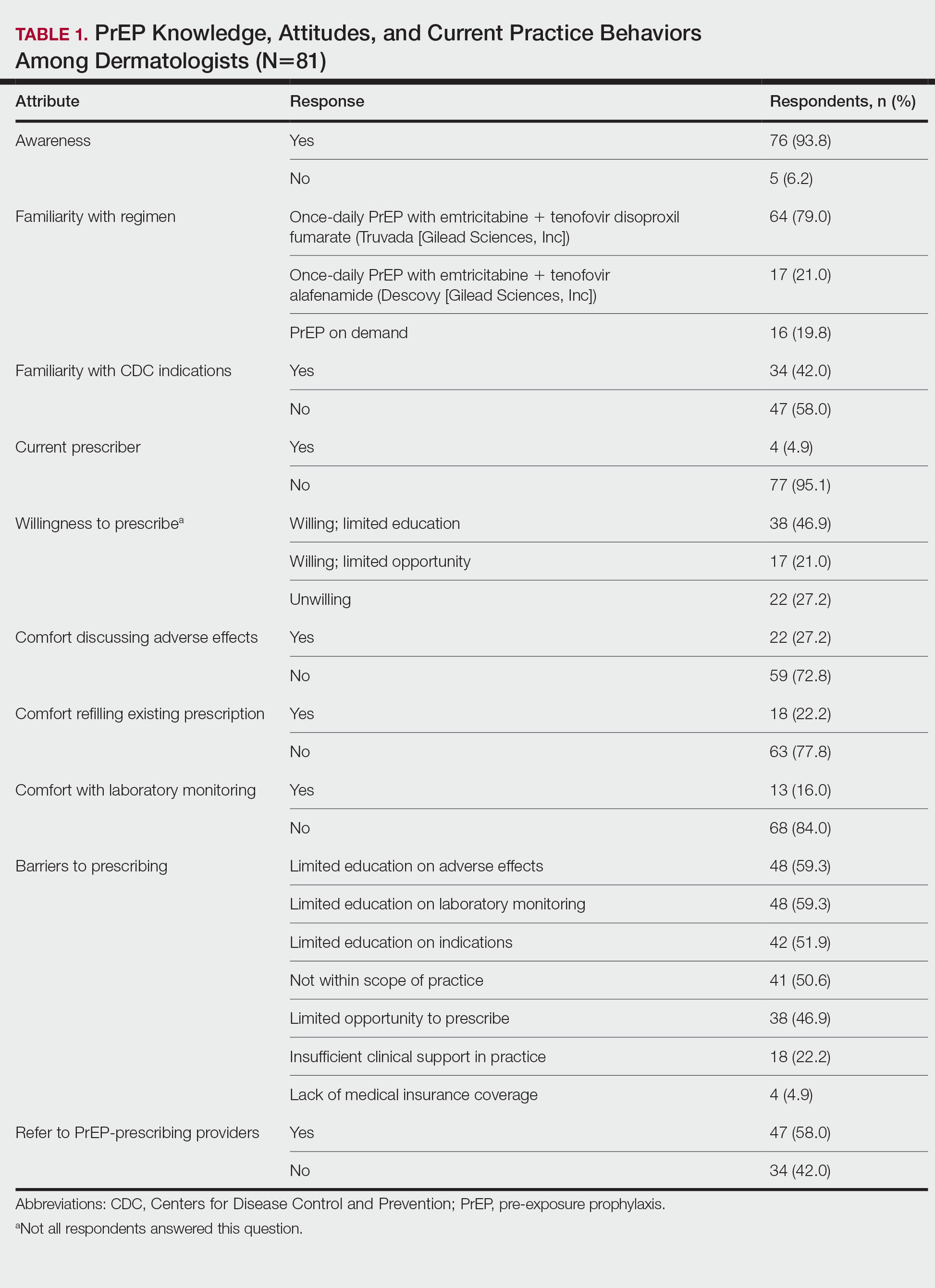
Despite respondents’ awareness of PrEP as a preventive measure (93.8% [76/81]) and their willingness to prescribe it (67.9% [55/81]), many reported being largely unfamiliar with its indications (58.0% [47/81]) and uncomfortable discussing its adverse effects (72.8% [59/81]), conducting appropriate laboratory monitoring (84.0% [68/81]), and refilling existing prescriptions (77.8% [63/81]). Respondents’ lack of education about PrEP was a barrier to prescribing (51.9% [42/81] to 59.3% [48/81]) and explains why a small minority (4.9% [4/81]) currently prescribe the regimen.
Our study sought to characterize current clinical knowledge about and practice patterns of PrEP among dermatologists. Dermatologists often encounter patients who present with an STI, which is a risk factor for HIV infection, but our survey respondents reported several barriers to utilizing PrEP. The difference in the degree of respondents’ willingness to prescribe PrEP (67.9%) and those who self-identified as prescribers (4.9%) suggests a role for dermatologists in prescribing or discussing PrEP with their patients—albeit a currently undefined role.
The results of our study suggested that half (41/81) of dermatologists believe that PrEP prescription is out of their scope of practice, likely due to a combination of scheduling, laboratory monitoring, and medicolegal concerns. For dermatologists who are interested in being PrEP prescribers, our results suggested that closing the knowledge gap around PrEP among dermatologists through training and education could improve comfort with this medication and lead to changes in practice to prevent the spread of HIV infection.
PrEP is indicated for HIV-negative patients who have HIV-positive sexual partners, utilize barrier protection methods inconsistently, or had a diagnosis of an STI in the last 6 months.6 In 2012, the FDA approved once-daily use of emtricitabine plus tenofovir for primary prevention of HIV infection. Post hoc analysis of iPrEx trial data revealed that once-daily PrEP taken regularly had a 92% to 100% protective effect against HIV.7
Regrettably, real-world uptake of PrEP has been slower than desired. The most recent data (2021) show that nearly 1 million individuals worldwide take PrEP; however, this represents only approximately one-third of those eligible.8 Utilization is notably lower among Black and Latino populations who stand to gain the most from PrEP given their higher risk of contracting HIV compared to their White counterparts.9 As such, improving access to PrEP through expanded provider awareness is essential to decrease the risk for HIV infection and transmission.
Emtricitabine plus tenofovir is safe and well tolerated; more common adverse effects are headache, nausea, vomiting, rash, and loss of appetite. Tenofovir likely decreases bone mineral density, even in HIV-negative patients10; mineralization seems to recover after the medication is discontinued.11 Rarely, tenofovir can increase the level of creatinine and hepatic transaminases; a recent report on its long-term side effects has shown small nonprogressive decreases in glomerular filtration rate.12 Monitoring kidney function is a component of prescribing PrEP (Table 2).
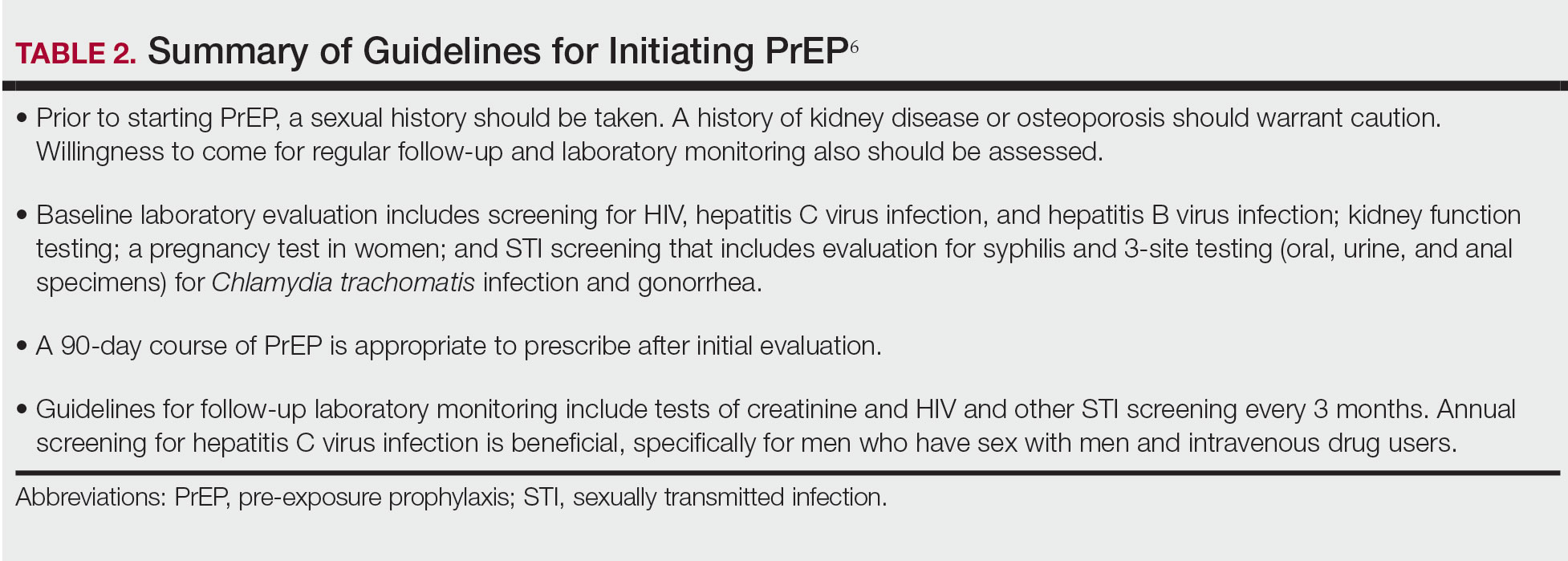
In 2019, emtricitabine plus tenofovir was reformulated with tenofovir alafenamide; the new combination regimen received FDA approval for once-daily PrEP under the brand name Descovy (Gilead Sciences, Inc). The new formulation results in a lower blood concentration of tenofovir and has been reported to present less of a risk for bone and kidney toxicity.13,14
Notably, emtricitabine plus tenofovir alafenamide might accumulate faster in peripheral lymphatic tissue than emtricitabine plus tenofovir disoproxil fumarate. This property has led to a new regimen known as “on-demand PrEP,” which follows a 2-1-1 dosing regimen: Patients take a double dose 2 to 24 hours before sexual activity, 1 dose on the day of sexual activity, and 1 dose the day after sexual activity.15 Because some patients at risk for HIV infection might not be consistently sexually active, on-demand PrEP allows them to cycle on and off the medication. Barriers to implementing on-demand PrEP include requiring that sexual activity be planned and an adverse effect profile similar to daily-use PrEP.16
The FDA recently approved a long-acting, once-monthly combination injectable PrEP of cabotegravir and rilpivirine.17 The long duration of action of this PrEP will benefit patients who report problems with medication adherence.
Our study demonstrates low frequency in prescribing patterns of PrEP among dermatologists and suggests that an addressable barrier to such prescribing is the lack of knowledge on how to prescribe it safely, which warrants further clinical investigation. We summarize an approach to prescribing PrEP in Table 2. Our study was limited by a small sample of mostly academic dermatologists and selection bias, which may diminish the generalizability of findings. A study of a larger, more representative group of dermatologists likely would show different prescribing patterns and degrees of knowledge about PrEP. Research is needed to study the impact of educational interventions that aim to increase both knowledge and prescribing of PrEP among dermatologists.
- Grant RM, Lama JR, Anderson PL, et al; iPrEx Study Team. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587-2599. doi:10.1056/NEJMoa1011205
- Fauci AS, Redfield RR, Sigounas G, et al. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321:844-845. doi:10.1001/jama.2019.1343
- Smith DK, Van Handel M, Grey J. Estimates of adults with indications for HIV pre-exposure prophylaxis by jurisdiction, transmission risk group, and race/ethnicity, United States, 2015. Ann Epidemiol. 2018;28:850-857.e9. doi:10.1016/j.annepidem.2018.05.003
- Song HJ, Squires P, Wilson D, et al. Trends in HIV preexposure prophylaxis prescribing in the United States, 2012-2018. JAMA. 2020;324:395-397. doi:10.1001/jama.2020.7312
- Petroll AE, Walsh JL, Owczarzak JL, et al. PrEP awareness, familiarity, comfort, and prescribing experience among US primary care providers and HIV specialists. AIDS Behav. 2017;21:1256-1267. doi:10.1007/s10461-016-1625-1
- US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 update. a clinical practice guideline. Centers for Disease Control and Prevention. Accessed September 15, 2022. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf
- Riddell J 4th, Amico KR, Mayer KH. HIV preexposure prophylaxis: a review. JAMA. 2018;319:1261-1268. doi:10.1001/JAMA.2018.1917
- Segal K, Fitch L, Riaz F, et al. The evolution of oral PrEP access: tracking trends in global oral PrEP use over time. J Int AIDS Soc. 2021;24:27-28.
- Elion RA, Kabiri M, Mayer KH, et al. Estimated impact of targeted pre-exposure prophylaxis: strategies for men who have sex with men in the United States. Int J Environ Res Public Health. 2019;16:1592. doi:10.3390/ijerph16091592
- Kasonde M, Niska RW, Rose C, et al. Bone mineral density changes among HIV-uninfected young adults in a randomised trial of pre-exposure prophylaxis with tenofovir-emtricitabine or placebo in Botswana. PLoS One. 2014;9:e90111. doi:10.1371/journal.pone.0090111
- Glidden DV, Mulligan K, McMahan V, et al. Brief report: recovery of bone mineral density after discontinuation of tenofovir-based HIV pre-exposure prophylaxis. J Acquir Immune Defic Syndr. 2017;76:177-182. doi:10.1097/QAI.0000000000001475
- Tang EC, Vittinghoff E, Anderson PL, et al. Changes in kidney function associated with daily tenofovir disoproxil fumarate/emtricitabine for HIV preexposure prophylaxis use in the United States Demonstration Project. J Acquir Immune Defic Syndr. 2018;77:193-198. doi:10.1097/QAI.0000000000001566
- Gupta SK, Post FA, Arribas JR, et al. Renal safety of tenofovir alafenamide vs. tenofovir disoproxil fumarate: a pooled analysis of 26 clinical trials. AIDS. 2019;33:1455-1465. doi:10.1097/QAD.0000000000002223
- Agarwal K, Brunetto M, Seto WK, et al; GS-US-320-0110; GS-US-320-0108 Investigators. 96 weeks treatment of tenofovir alafenamide vs. tenofovir disoproxil fumarate for hepatitis B virus infection [published online January 17, 2018]. J Hepatol. 2018;68:672-681. doi:10.1016/j.jhep.2017.11.039
- Molina JM, Capitant C, Spire B, et al; ANRS IPERGAY Study Group. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection [published online December 1, 2015]. N Engl J Med. 2015;3;2237-2246. doi:10.1056/NEJMoa1506273
- Saberi P, Scott HM. On-demand oral pre-exposure prophylaxis with tenofovir/emtricitabine: what every clinician needs to know. J Gen Intern Med. 2020;35:1285-1288. doi:10.1007/s11606-020-05651-2
- Landovitz RJ, Li S, Grinsztejn B, et al. Safety, tolerability, and pharmacokinetics of long-acting injectable cabotegravir in low-risk HIV-uninfected individuals: HPTN 077, a phase 2a randomized controlled trial. PLoS Med. 2018;15:e1002690. doi:10.1371/journal.pmed.1002690
- Grant RM, Lama JR, Anderson PL, et al; iPrEx Study Team. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587-2599. doi:10.1056/NEJMoa1011205
- Fauci AS, Redfield RR, Sigounas G, et al. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321:844-845. doi:10.1001/jama.2019.1343
- Smith DK, Van Handel M, Grey J. Estimates of adults with indications for HIV pre-exposure prophylaxis by jurisdiction, transmission risk group, and race/ethnicity, United States, 2015. Ann Epidemiol. 2018;28:850-857.e9. doi:10.1016/j.annepidem.2018.05.003
- Song HJ, Squires P, Wilson D, et al. Trends in HIV preexposure prophylaxis prescribing in the United States, 2012-2018. JAMA. 2020;324:395-397. doi:10.1001/jama.2020.7312
- Petroll AE, Walsh JL, Owczarzak JL, et al. PrEP awareness, familiarity, comfort, and prescribing experience among US primary care providers and HIV specialists. AIDS Behav. 2017;21:1256-1267. doi:10.1007/s10461-016-1625-1
- US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 update. a clinical practice guideline. Centers for Disease Control and Prevention. Accessed September 15, 2022. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf
- Riddell J 4th, Amico KR, Mayer KH. HIV preexposure prophylaxis: a review. JAMA. 2018;319:1261-1268. doi:10.1001/JAMA.2018.1917
- Segal K, Fitch L, Riaz F, et al. The evolution of oral PrEP access: tracking trends in global oral PrEP use over time. J Int AIDS Soc. 2021;24:27-28.
- Elion RA, Kabiri M, Mayer KH, et al. Estimated impact of targeted pre-exposure prophylaxis: strategies for men who have sex with men in the United States. Int J Environ Res Public Health. 2019;16:1592. doi:10.3390/ijerph16091592
- Kasonde M, Niska RW, Rose C, et al. Bone mineral density changes among HIV-uninfected young adults in a randomised trial of pre-exposure prophylaxis with tenofovir-emtricitabine or placebo in Botswana. PLoS One. 2014;9:e90111. doi:10.1371/journal.pone.0090111
- Glidden DV, Mulligan K, McMahan V, et al. Brief report: recovery of bone mineral density after discontinuation of tenofovir-based HIV pre-exposure prophylaxis. J Acquir Immune Defic Syndr. 2017;76:177-182. doi:10.1097/QAI.0000000000001475
- Tang EC, Vittinghoff E, Anderson PL, et al. Changes in kidney function associated with daily tenofovir disoproxil fumarate/emtricitabine for HIV preexposure prophylaxis use in the United States Demonstration Project. J Acquir Immune Defic Syndr. 2018;77:193-198. doi:10.1097/QAI.0000000000001566
- Gupta SK, Post FA, Arribas JR, et al. Renal safety of tenofovir alafenamide vs. tenofovir disoproxil fumarate: a pooled analysis of 26 clinical trials. AIDS. 2019;33:1455-1465. doi:10.1097/QAD.0000000000002223
- Agarwal K, Brunetto M, Seto WK, et al; GS-US-320-0110; GS-US-320-0108 Investigators. 96 weeks treatment of tenofovir alafenamide vs. tenofovir disoproxil fumarate for hepatitis B virus infection [published online January 17, 2018]. J Hepatol. 2018;68:672-681. doi:10.1016/j.jhep.2017.11.039
- Molina JM, Capitant C, Spire B, et al; ANRS IPERGAY Study Group. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection [published online December 1, 2015]. N Engl J Med. 2015;3;2237-2246. doi:10.1056/NEJMoa1506273
- Saberi P, Scott HM. On-demand oral pre-exposure prophylaxis with tenofovir/emtricitabine: what every clinician needs to know. J Gen Intern Med. 2020;35:1285-1288. doi:10.1007/s11606-020-05651-2
- Landovitz RJ, Li S, Grinsztejn B, et al. Safety, tolerability, and pharmacokinetics of long-acting injectable cabotegravir in low-risk HIV-uninfected individuals: HPTN 077, a phase 2a randomized controlled trial. PLoS Med. 2018;15:e1002690. doi:10.1371/journal.pmed.1002690
Practice Points
- Sexually transmitted infections (STIs) often have skin manifestations, with patients presenting to dermatologists.
- Pre-exposure prophylaxis (PrEP) uses antiretrovirals taken prophylactically to prevent transmission of and infection with HIV. Dermatologists are aware of PrEP, but several barriers prevent them from being prescribers.
- Patients with a history of an STI should be considered for PrEP.
Could a vaccine (and more) fix the fentanyl crisis?
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.



