User login
T2D: Superior glycemic control with once-weekly tirzepatide vs. insulin degludec
Key clinical point: Once-weekly tirzepatide vs insulin degludec effectuates superior glycemic control, as measured by continuous glucose monitoring, in patients with inadequately controlled type 2 diabetes (T2D) on metformin with or without a sodium-glucose cotransporter-2 (SGLT2) inhibitor.
Major finding: At 52 weeks, patients receiving 5 mg tirzepatide (estimated treatment difference [ETD] 12%; P = .031), 10 mg (ETD 24%; P < .0001), and 15 mg (ETD 25%; P < .0001) vs insulin degludec spent significantly more time in the tight target range (blood glucose concentration 71-140 mg/dL).
Study details: This substudy of the SURPASS-3 trial included 243 insulin-naive patients with type T2D inadequately controlled on metformin with or without an SGLT2 inhibitor who were randomly assigned to receive once-weekly tirzepatide (5, 10, or 15 mg; n = 188) or insulin degludec (n = 55).
Disclosures: The study was funded by Eli Lilly and Company. Two authors reported being consultants or receiving advisory board member or speaker honoraria from various sources, including Eli Lilly. The other authors are employees and shareholders of Eli Lilly.
Source: Battelino T et al. Efficacy of once-weekly tirzepatide versus once-daily insulin degludec on glycaemic control measured by continuous glucose monitoring in adults with type 2 diabetes (SURPASS-3 CGM): A substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol. 2022;10(6):407-417 (Apr 22). Doi: 10.1016/S2213-8587(22)00077-8
Key clinical point: Once-weekly tirzepatide vs insulin degludec effectuates superior glycemic control, as measured by continuous glucose monitoring, in patients with inadequately controlled type 2 diabetes (T2D) on metformin with or without a sodium-glucose cotransporter-2 (SGLT2) inhibitor.
Major finding: At 52 weeks, patients receiving 5 mg tirzepatide (estimated treatment difference [ETD] 12%; P = .031), 10 mg (ETD 24%; P < .0001), and 15 mg (ETD 25%; P < .0001) vs insulin degludec spent significantly more time in the tight target range (blood glucose concentration 71-140 mg/dL).
Study details: This substudy of the SURPASS-3 trial included 243 insulin-naive patients with type T2D inadequately controlled on metformin with or without an SGLT2 inhibitor who were randomly assigned to receive once-weekly tirzepatide (5, 10, or 15 mg; n = 188) or insulin degludec (n = 55).
Disclosures: The study was funded by Eli Lilly and Company. Two authors reported being consultants or receiving advisory board member or speaker honoraria from various sources, including Eli Lilly. The other authors are employees and shareholders of Eli Lilly.
Source: Battelino T et al. Efficacy of once-weekly tirzepatide versus once-daily insulin degludec on glycaemic control measured by continuous glucose monitoring in adults with type 2 diabetes (SURPASS-3 CGM): A substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol. 2022;10(6):407-417 (Apr 22). Doi: 10.1016/S2213-8587(22)00077-8
Key clinical point: Once-weekly tirzepatide vs insulin degludec effectuates superior glycemic control, as measured by continuous glucose monitoring, in patients with inadequately controlled type 2 diabetes (T2D) on metformin with or without a sodium-glucose cotransporter-2 (SGLT2) inhibitor.
Major finding: At 52 weeks, patients receiving 5 mg tirzepatide (estimated treatment difference [ETD] 12%; P = .031), 10 mg (ETD 24%; P < .0001), and 15 mg (ETD 25%; P < .0001) vs insulin degludec spent significantly more time in the tight target range (blood glucose concentration 71-140 mg/dL).
Study details: This substudy of the SURPASS-3 trial included 243 insulin-naive patients with type T2D inadequately controlled on metformin with or without an SGLT2 inhibitor who were randomly assigned to receive once-weekly tirzepatide (5, 10, or 15 mg; n = 188) or insulin degludec (n = 55).
Disclosures: The study was funded by Eli Lilly and Company. Two authors reported being consultants or receiving advisory board member or speaker honoraria from various sources, including Eli Lilly. The other authors are employees and shareholders of Eli Lilly.
Source: Battelino T et al. Efficacy of once-weekly tirzepatide versus once-daily insulin degludec on glycaemic control measured by continuous glucose monitoring in adults with type 2 diabetes (SURPASS-3 CGM): A substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol. 2022;10(6):407-417 (Apr 22). Doi: 10.1016/S2213-8587(22)00077-8
Advanced squamous NSCLC: NFE2L2 and KEAP1 mutations tied to worse real-world PFS
Key clinical point: NFE2L2 and KEAP1 mutations account for 31.6% of all advanced squamous cell non-small cell lung cancer (NSCLC) cases, and these mutations are associated with worse real-world progression-free survival (PFS) after first-line therapy.
Major finding: NFE2L2 and KEAP1 mutations were detected in 31.6% of patients. Patients harboring these mutations had a shorter real-world PFS after first-line therapy (4.54 vs 6.25 months with wild-type disease; P = .0027).
Study details: The data come from a retrospective cohort study of 703 patients with advanced squamous cell NSCLC from a real-world US clinicogenomic database.
Disclosures: The study was funded by Takeda Development Center Americas, Inc. Y Wu, Y Yin, V Crossland, S Vincent, N Lineberry, and DV Faller are employees of Takeda Development Center Americas, Inc. PK Paik reported ties with various pharmaceutical companies.
Source: Wu Y et al. Survival outcomes and treatment patterns in patients with NFE2L2 and/or KEAP1 mutation-positive advanced squamous cell NSCLC using a real-world clinico-genomic database. Clin Lung Cancer. 2022 (May 10). Doi: 10.1016/j.cllc.2022.05.008
Key clinical point: NFE2L2 and KEAP1 mutations account for 31.6% of all advanced squamous cell non-small cell lung cancer (NSCLC) cases, and these mutations are associated with worse real-world progression-free survival (PFS) after first-line therapy.
Major finding: NFE2L2 and KEAP1 mutations were detected in 31.6% of patients. Patients harboring these mutations had a shorter real-world PFS after first-line therapy (4.54 vs 6.25 months with wild-type disease; P = .0027).
Study details: The data come from a retrospective cohort study of 703 patients with advanced squamous cell NSCLC from a real-world US clinicogenomic database.
Disclosures: The study was funded by Takeda Development Center Americas, Inc. Y Wu, Y Yin, V Crossland, S Vincent, N Lineberry, and DV Faller are employees of Takeda Development Center Americas, Inc. PK Paik reported ties with various pharmaceutical companies.
Source: Wu Y et al. Survival outcomes and treatment patterns in patients with NFE2L2 and/or KEAP1 mutation-positive advanced squamous cell NSCLC using a real-world clinico-genomic database. Clin Lung Cancer. 2022 (May 10). Doi: 10.1016/j.cllc.2022.05.008
Key clinical point: NFE2L2 and KEAP1 mutations account for 31.6% of all advanced squamous cell non-small cell lung cancer (NSCLC) cases, and these mutations are associated with worse real-world progression-free survival (PFS) after first-line therapy.
Major finding: NFE2L2 and KEAP1 mutations were detected in 31.6% of patients. Patients harboring these mutations had a shorter real-world PFS after first-line therapy (4.54 vs 6.25 months with wild-type disease; P = .0027).
Study details: The data come from a retrospective cohort study of 703 patients with advanced squamous cell NSCLC from a real-world US clinicogenomic database.
Disclosures: The study was funded by Takeda Development Center Americas, Inc. Y Wu, Y Yin, V Crossland, S Vincent, N Lineberry, and DV Faller are employees of Takeda Development Center Americas, Inc. PK Paik reported ties with various pharmaceutical companies.
Source: Wu Y et al. Survival outcomes and treatment patterns in patients with NFE2L2 and/or KEAP1 mutation-positive advanced squamous cell NSCLC using a real-world clinico-genomic database. Clin Lung Cancer. 2022 (May 10). Doi: 10.1016/j.cllc.2022.05.008
Lung cancer: Diagnostic method using breath biomarkers shows promise
Key clinical point: A new breath biomarker-based diagnostic method shows promise by identifying 16 cancer-derived volatile organic compounds (VOC) that have high sensitivity and specificity in patients with lung cancer.
Major finding: In the discovery phase, 16 VOC with peak intensity most altered before vs after surgery were identified. In the validation phase, the 16 VOC-based diagnostic model demonstrated an area under the curve of 0.952, sensitivity of 89.2%, specificity of 89.1%, and accuracy of 89.1%.
Study details: The discovery phase involved a prospective cohort study of 84 patients with lung cancer who were tested for 28 VOC before and after surgery. The promising VOC were further assessed in the validation phase which included 157 patients with lung cancer and 368 healthy controls.
Disclosures: The research was funded by the National Natural Science Foundation of China and others. The authors declared no competing interests.
Source: Wang P et al. Identification of lung cancer breath biomarkers based on perioperative breathomics testing: A prospective observational study. EClinicalMedicine. 2022;47:101384 (Apr 26). Doi: 10.1016/j.eclinm.2022.101384
Key clinical point: A new breath biomarker-based diagnostic method shows promise by identifying 16 cancer-derived volatile organic compounds (VOC) that have high sensitivity and specificity in patients with lung cancer.
Major finding: In the discovery phase, 16 VOC with peak intensity most altered before vs after surgery were identified. In the validation phase, the 16 VOC-based diagnostic model demonstrated an area under the curve of 0.952, sensitivity of 89.2%, specificity of 89.1%, and accuracy of 89.1%.
Study details: The discovery phase involved a prospective cohort study of 84 patients with lung cancer who were tested for 28 VOC before and after surgery. The promising VOC were further assessed in the validation phase which included 157 patients with lung cancer and 368 healthy controls.
Disclosures: The research was funded by the National Natural Science Foundation of China and others. The authors declared no competing interests.
Source: Wang P et al. Identification of lung cancer breath biomarkers based on perioperative breathomics testing: A prospective observational study. EClinicalMedicine. 2022;47:101384 (Apr 26). Doi: 10.1016/j.eclinm.2022.101384
Key clinical point: A new breath biomarker-based diagnostic method shows promise by identifying 16 cancer-derived volatile organic compounds (VOC) that have high sensitivity and specificity in patients with lung cancer.
Major finding: In the discovery phase, 16 VOC with peak intensity most altered before vs after surgery were identified. In the validation phase, the 16 VOC-based diagnostic model demonstrated an area under the curve of 0.952, sensitivity of 89.2%, specificity of 89.1%, and accuracy of 89.1%.
Study details: The discovery phase involved a prospective cohort study of 84 patients with lung cancer who were tested for 28 VOC before and after surgery. The promising VOC were further assessed in the validation phase which included 157 patients with lung cancer and 368 healthy controls.
Disclosures: The research was funded by the National Natural Science Foundation of China and others. The authors declared no competing interests.
Source: Wang P et al. Identification of lung cancer breath biomarkers based on perioperative breathomics testing: A prospective observational study. EClinicalMedicine. 2022;47:101384 (Apr 26). Doi: 10.1016/j.eclinm.2022.101384
Lung cancer: Noncancerous chest CT features may boost survival prediction
Key clinical point: In patients with stage I lung cancer treated with stereotactic body radiation therapy (SBRT), a model incorporating noncancerous imaging features on chest computed tomography (CT) and clinical features vs clinical features alone performed better at predicting overall survival (OS).
Major finding: The model that incorporated both clinical and imaging features vs the model that incorporated only clinical features performed better at predicting 5-year OS (area under the curve 0.75 vs 0.61; P < .01). Independent risk factors for shorter OS were elevated coronary artery calcium score, increased pulmonary artery-to-aorta ratio, and decreased thoracic skeletal muscle index.
Study details: The data come from a retrospective study involving 282 patients with stage I lung cancer treated with SBRT. Several clinical markers were assessed from pretreatment chest CT images.
Disclosures: No funding information was available. The corresponding author FJ Fintelmann reported no relevant financial relationships.
Source: Tahir I et al. Utility of noncancerous chest CT features for predicting overall survival and noncancer death in patients with stage I lung cancer treated with stereotactic body radiotherapy. AJR Am J Roentgenol. 2022 (Apr 13). Doi: 10.2214/AJR.22.27484
Key clinical point: In patients with stage I lung cancer treated with stereotactic body radiation therapy (SBRT), a model incorporating noncancerous imaging features on chest computed tomography (CT) and clinical features vs clinical features alone performed better at predicting overall survival (OS).
Major finding: The model that incorporated both clinical and imaging features vs the model that incorporated only clinical features performed better at predicting 5-year OS (area under the curve 0.75 vs 0.61; P < .01). Independent risk factors for shorter OS were elevated coronary artery calcium score, increased pulmonary artery-to-aorta ratio, and decreased thoracic skeletal muscle index.
Study details: The data come from a retrospective study involving 282 patients with stage I lung cancer treated with SBRT. Several clinical markers were assessed from pretreatment chest CT images.
Disclosures: No funding information was available. The corresponding author FJ Fintelmann reported no relevant financial relationships.
Source: Tahir I et al. Utility of noncancerous chest CT features for predicting overall survival and noncancer death in patients with stage I lung cancer treated with stereotactic body radiotherapy. AJR Am J Roentgenol. 2022 (Apr 13). Doi: 10.2214/AJR.22.27484
Key clinical point: In patients with stage I lung cancer treated with stereotactic body radiation therapy (SBRT), a model incorporating noncancerous imaging features on chest computed tomography (CT) and clinical features vs clinical features alone performed better at predicting overall survival (OS).
Major finding: The model that incorporated both clinical and imaging features vs the model that incorporated only clinical features performed better at predicting 5-year OS (area under the curve 0.75 vs 0.61; P < .01). Independent risk factors for shorter OS were elevated coronary artery calcium score, increased pulmonary artery-to-aorta ratio, and decreased thoracic skeletal muscle index.
Study details: The data come from a retrospective study involving 282 patients with stage I lung cancer treated with SBRT. Several clinical markers were assessed from pretreatment chest CT images.
Disclosures: No funding information was available. The corresponding author FJ Fintelmann reported no relevant financial relationships.
Source: Tahir I et al. Utility of noncancerous chest CT features for predicting overall survival and noncancer death in patients with stage I lung cancer treated with stereotactic body radiotherapy. AJR Am J Roentgenol. 2022 (Apr 13). Doi: 10.2214/AJR.22.27484
Extensive-stage SCLC: Anlotinib plus platinum-etoposide shows promise
Key clinical point: Frontline therapy with anlotinib plus platinum-etoposide chemotherapy shows favorable outcomes in patients with extensive-stage (ES) small-cell lung cancer (SCLC).
Major finding: The median progression-free survival was 8.02 (95% CI 6.90-9.66) months and the overall survival was 15.87 (95% CI 10.38-18.89) months. The objective response rate was 85.71% (95% CI 69.74%-95.19%) and the disease control rate was 94.29% (95% CI 80.84%-99.30%). The incidence of grade 3-4 adverse events was 40%.
Study details: The data come from a phase 2 single-arm trial of anlotinib plus platinum-etoposide in 35 patients with ES-SCLC at a single center in China.
Disclosures: The trial was funded by Chia Tai Tianqing Pharmaceutical Group Co., Ltd. The authors declared no competing interests.
Source: Deng P et al. Anlotinib plus platinum-etoposide as a first-line treatment for extensive-stage small cell lung cancer: A single-arm trial. Cancer Med. 2022 (May 8). Doi: 10.1002/cam4.4736
Key clinical point: Frontline therapy with anlotinib plus platinum-etoposide chemotherapy shows favorable outcomes in patients with extensive-stage (ES) small-cell lung cancer (SCLC).
Major finding: The median progression-free survival was 8.02 (95% CI 6.90-9.66) months and the overall survival was 15.87 (95% CI 10.38-18.89) months. The objective response rate was 85.71% (95% CI 69.74%-95.19%) and the disease control rate was 94.29% (95% CI 80.84%-99.30%). The incidence of grade 3-4 adverse events was 40%.
Study details: The data come from a phase 2 single-arm trial of anlotinib plus platinum-etoposide in 35 patients with ES-SCLC at a single center in China.
Disclosures: The trial was funded by Chia Tai Tianqing Pharmaceutical Group Co., Ltd. The authors declared no competing interests.
Source: Deng P et al. Anlotinib plus platinum-etoposide as a first-line treatment for extensive-stage small cell lung cancer: A single-arm trial. Cancer Med. 2022 (May 8). Doi: 10.1002/cam4.4736
Key clinical point: Frontline therapy with anlotinib plus platinum-etoposide chemotherapy shows favorable outcomes in patients with extensive-stage (ES) small-cell lung cancer (SCLC).
Major finding: The median progression-free survival was 8.02 (95% CI 6.90-9.66) months and the overall survival was 15.87 (95% CI 10.38-18.89) months. The objective response rate was 85.71% (95% CI 69.74%-95.19%) and the disease control rate was 94.29% (95% CI 80.84%-99.30%). The incidence of grade 3-4 adverse events was 40%.
Study details: The data come from a phase 2 single-arm trial of anlotinib plus platinum-etoposide in 35 patients with ES-SCLC at a single center in China.
Disclosures: The trial was funded by Chia Tai Tianqing Pharmaceutical Group Co., Ltd. The authors declared no competing interests.
Source: Deng P et al. Anlotinib plus platinum-etoposide as a first-line treatment for extensive-stage small cell lung cancer: A single-arm trial. Cancer Med. 2022 (May 8). Doi: 10.1002/cam4.4736
Small-sized peripheral NSCLC: Segmentectomy noninferior to lobectomy for OS
Key clinical point: Segmentectomy is noninferior to lobectomy for overall survival (OS) in patients with small-sized peripheral nonsmall cell lung cancer (NSCLC).
Major finding: Segmentectomy was noninferior to lobectomy for 5-year OS (94.3% vs 91.1%; hazard ratio 0.663; 95% CI 0.474-0.927; 1-sided P < .0001 for noninferiority). There were no differences between the groups in 5-year relapse-free survival.
Study details: The data come from a Japanese randomized controlled, noninferiority phase 3 trial (n = 1106) of segmentectomy vs lobectomy for stage IA NSCLC.
Disclosures: The trial was funded by the National Cancer Center Research and the Ministry of Health, Labor, and Welfare of Japan. R Nakajima, T Aoki, J Okami, H Ito, N Okumura, M Yamaguchi, K Nakamura, and S Nakamura reported no competing interests. The other authors reported ties with one or more pharmaceutical companies outside this work.
Source: Saji H et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): A multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet. 2022;399(10335):1607-1617 (Apr 23). Doi: 10.1016/S0140-6736(21)02333-3
Key clinical point: Segmentectomy is noninferior to lobectomy for overall survival (OS) in patients with small-sized peripheral nonsmall cell lung cancer (NSCLC).
Major finding: Segmentectomy was noninferior to lobectomy for 5-year OS (94.3% vs 91.1%; hazard ratio 0.663; 95% CI 0.474-0.927; 1-sided P < .0001 for noninferiority). There were no differences between the groups in 5-year relapse-free survival.
Study details: The data come from a Japanese randomized controlled, noninferiority phase 3 trial (n = 1106) of segmentectomy vs lobectomy for stage IA NSCLC.
Disclosures: The trial was funded by the National Cancer Center Research and the Ministry of Health, Labor, and Welfare of Japan. R Nakajima, T Aoki, J Okami, H Ito, N Okumura, M Yamaguchi, K Nakamura, and S Nakamura reported no competing interests. The other authors reported ties with one or more pharmaceutical companies outside this work.
Source: Saji H et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): A multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet. 2022;399(10335):1607-1617 (Apr 23). Doi: 10.1016/S0140-6736(21)02333-3
Key clinical point: Segmentectomy is noninferior to lobectomy for overall survival (OS) in patients with small-sized peripheral nonsmall cell lung cancer (NSCLC).
Major finding: Segmentectomy was noninferior to lobectomy for 5-year OS (94.3% vs 91.1%; hazard ratio 0.663; 95% CI 0.474-0.927; 1-sided P < .0001 for noninferiority). There were no differences between the groups in 5-year relapse-free survival.
Study details: The data come from a Japanese randomized controlled, noninferiority phase 3 trial (n = 1106) of segmentectomy vs lobectomy for stage IA NSCLC.
Disclosures: The trial was funded by the National Cancer Center Research and the Ministry of Health, Labor, and Welfare of Japan. R Nakajima, T Aoki, J Okami, H Ito, N Okumura, M Yamaguchi, K Nakamura, and S Nakamura reported no competing interests. The other authors reported ties with one or more pharmaceutical companies outside this work.
Source: Saji H et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): A multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet. 2022;399(10335):1607-1617 (Apr 23). Doi: 10.1016/S0140-6736(21)02333-3
Children and COVID: Weekly cases keep rising past 100,000
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
New cases were up by 14.6% over the previous week to just over 107,000 reported during May 13-16, marking the sixth straight increase since April 1-7, when the count was almost 26,000. Over that period, weekly cases rose 313%, based on data in the latest weekly COVID report from the AAP and CHA.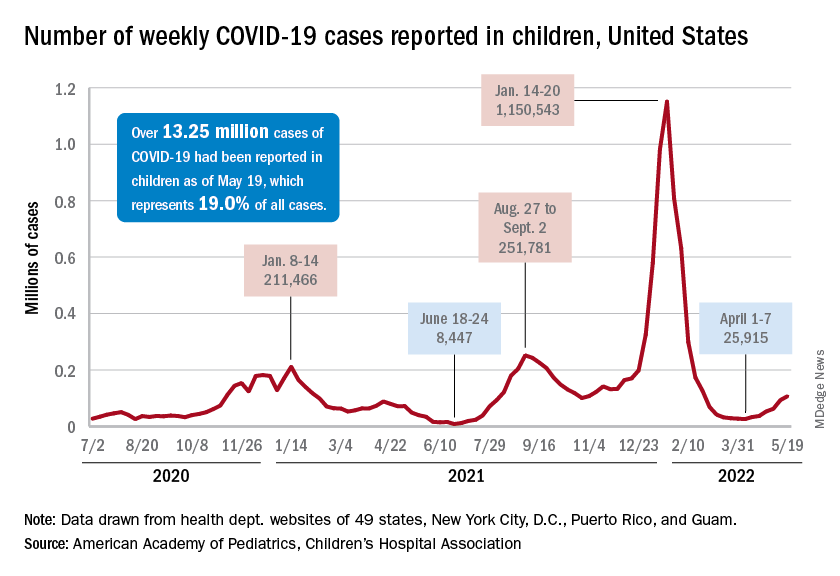
Rates reported by the Centers for Disease Control and Prevention show the same trend. Weekly cases per 100,000 population, which were down to 34.9 in children aged 0-4 years and 43.1 for those aged 5-11 on March 26, were up to 49.5 and 52.2, respectively, by April 16. The pace picked up right after that, and as of May 14, the rates of new cases were 125.4 per 100,000 in children aged 0-4 years and 143.1 in those aged 5-11, the CDC said.
Hospital admissions continue to rise as well. The rate of new admissions in children aged 0-17 was up to 0.25 per 100,000 population on May 18, nearly double the 0.13 per 100,000 recorded as late as April 13. The latest 7-day average count for new admissions, 163 per day from May 15-21, is down from the previous week’s 175 per day, but the CDC also acknowledges potential reporting delays in the most recent 7-day period.
Both of those weekly averages, however, are far below the peak rate for the pandemic, 914 per day, which occurred Jan. 10-16, 2022, during the Omicron surge. Since the CDC began keeping count at the beginning of August 2020, more than 125,000 children aged 0-17 years have been admitted with confirmed COVID-19, which is about 2.7% of all admissions over that period, the CDC’s data show.
Booster gets the green light
The week brought some positive news on the prevention side, though, as the CDC officially approved a COVID vaccine booster dose for children aged 5-11 years.
Even that good news came with a caveat, however. The vote by the CDC’s Advisory Committee on Immunization Practices was 11:1 in favor, with the negative vote cast by Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., who said that “boosters are great once we’ve gotten everyone their first round. That needs to be our priority in this.”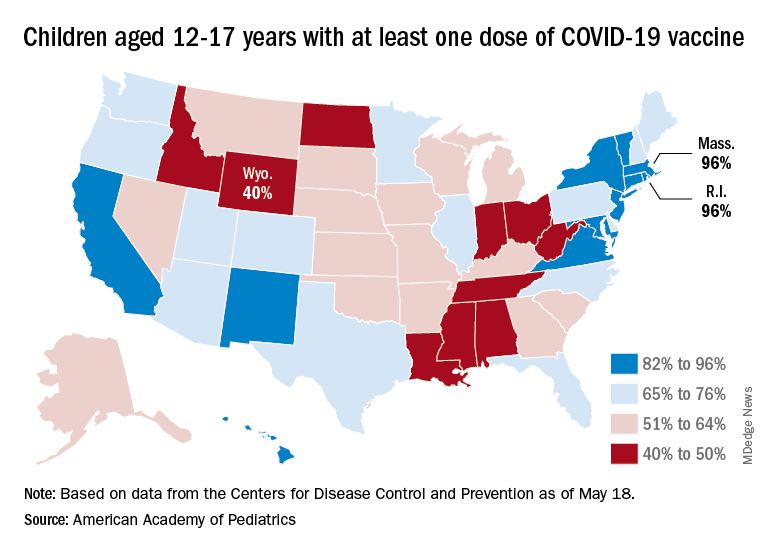
Nationally, in fact, just 35.7% of children aged 5-11 years have received at least one dose of the vaccine and only 29.0% are fully vaccinated. Those figures are nearly doubled among 12- to 17-year-olds: 69.3% have received at least one dose and 59.4% are fully vaccinated, the CDC said on its COVID Data Tracker.
Some states, meanwhile, are well below those national rates. In Wyoming, only 40% of children aged 12-17 have received an initial vaccine dose, and eight other states are below 50%. Among children aged 5-12, there are still five states below 20% in that measure, while the states on the other end of the spectrum – Vermont and Massachusetts – are above 60%, the AAP said in its separate vaccination report.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
New cases were up by 14.6% over the previous week to just over 107,000 reported during May 13-16, marking the sixth straight increase since April 1-7, when the count was almost 26,000. Over that period, weekly cases rose 313%, based on data in the latest weekly COVID report from the AAP and CHA.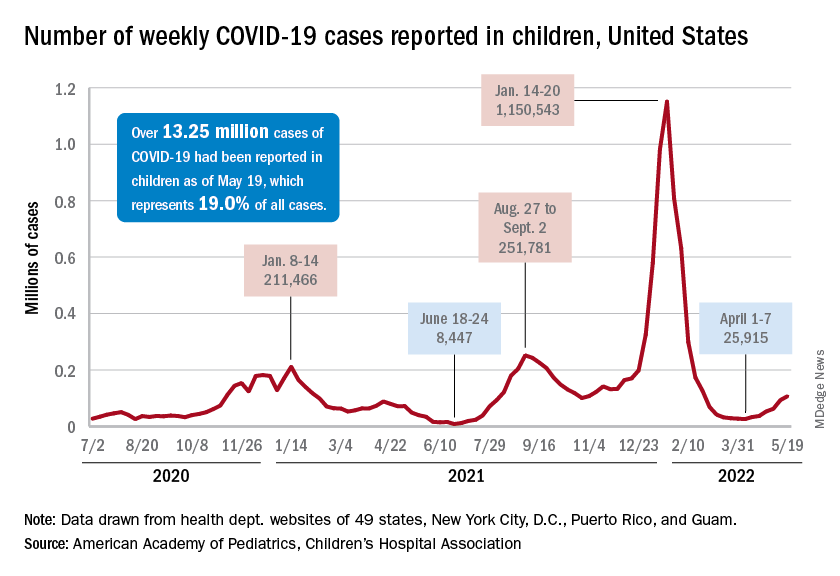
Rates reported by the Centers for Disease Control and Prevention show the same trend. Weekly cases per 100,000 population, which were down to 34.9 in children aged 0-4 years and 43.1 for those aged 5-11 on March 26, were up to 49.5 and 52.2, respectively, by April 16. The pace picked up right after that, and as of May 14, the rates of new cases were 125.4 per 100,000 in children aged 0-4 years and 143.1 in those aged 5-11, the CDC said.
Hospital admissions continue to rise as well. The rate of new admissions in children aged 0-17 was up to 0.25 per 100,000 population on May 18, nearly double the 0.13 per 100,000 recorded as late as April 13. The latest 7-day average count for new admissions, 163 per day from May 15-21, is down from the previous week’s 175 per day, but the CDC also acknowledges potential reporting delays in the most recent 7-day period.
Both of those weekly averages, however, are far below the peak rate for the pandemic, 914 per day, which occurred Jan. 10-16, 2022, during the Omicron surge. Since the CDC began keeping count at the beginning of August 2020, more than 125,000 children aged 0-17 years have been admitted with confirmed COVID-19, which is about 2.7% of all admissions over that period, the CDC’s data show.
Booster gets the green light
The week brought some positive news on the prevention side, though, as the CDC officially approved a COVID vaccine booster dose for children aged 5-11 years.
Even that good news came with a caveat, however. The vote by the CDC’s Advisory Committee on Immunization Practices was 11:1 in favor, with the negative vote cast by Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., who said that “boosters are great once we’ve gotten everyone their first round. That needs to be our priority in this.”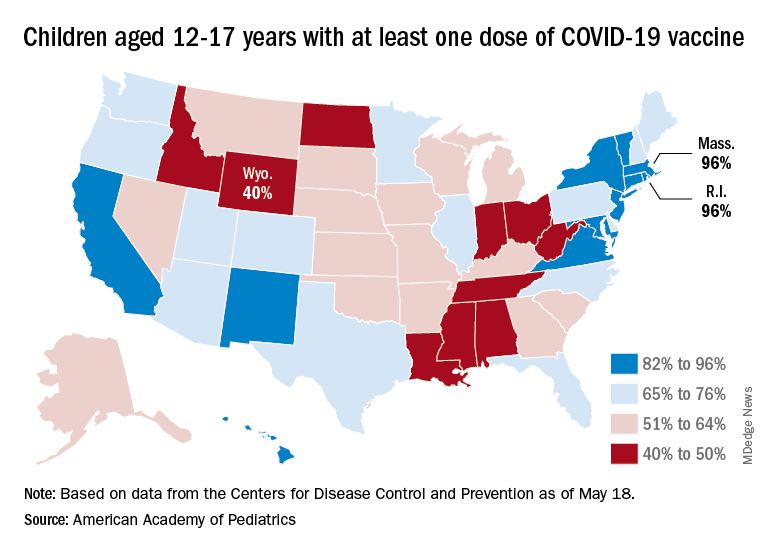
Nationally, in fact, just 35.7% of children aged 5-11 years have received at least one dose of the vaccine and only 29.0% are fully vaccinated. Those figures are nearly doubled among 12- to 17-year-olds: 69.3% have received at least one dose and 59.4% are fully vaccinated, the CDC said on its COVID Data Tracker.
Some states, meanwhile, are well below those national rates. In Wyoming, only 40% of children aged 12-17 have received an initial vaccine dose, and eight other states are below 50%. Among children aged 5-12, there are still five states below 20% in that measure, while the states on the other end of the spectrum – Vermont and Massachusetts – are above 60%, the AAP said in its separate vaccination report.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
New cases were up by 14.6% over the previous week to just over 107,000 reported during May 13-16, marking the sixth straight increase since April 1-7, when the count was almost 26,000. Over that period, weekly cases rose 313%, based on data in the latest weekly COVID report from the AAP and CHA.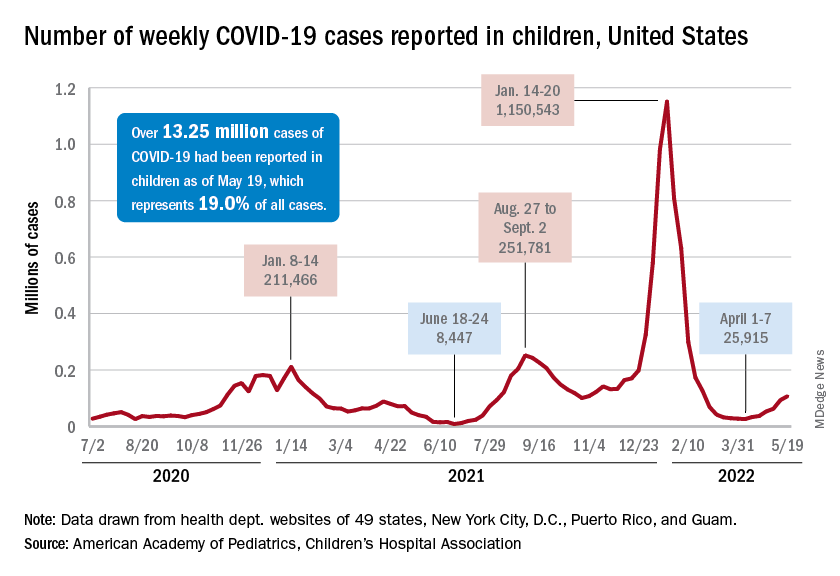
Rates reported by the Centers for Disease Control and Prevention show the same trend. Weekly cases per 100,000 population, which were down to 34.9 in children aged 0-4 years and 43.1 for those aged 5-11 on March 26, were up to 49.5 and 52.2, respectively, by April 16. The pace picked up right after that, and as of May 14, the rates of new cases were 125.4 per 100,000 in children aged 0-4 years and 143.1 in those aged 5-11, the CDC said.
Hospital admissions continue to rise as well. The rate of new admissions in children aged 0-17 was up to 0.25 per 100,000 population on May 18, nearly double the 0.13 per 100,000 recorded as late as April 13. The latest 7-day average count for new admissions, 163 per day from May 15-21, is down from the previous week’s 175 per day, but the CDC also acknowledges potential reporting delays in the most recent 7-day period.
Both of those weekly averages, however, are far below the peak rate for the pandemic, 914 per day, which occurred Jan. 10-16, 2022, during the Omicron surge. Since the CDC began keeping count at the beginning of August 2020, more than 125,000 children aged 0-17 years have been admitted with confirmed COVID-19, which is about 2.7% of all admissions over that period, the CDC’s data show.
Booster gets the green light
The week brought some positive news on the prevention side, though, as the CDC officially approved a COVID vaccine booster dose for children aged 5-11 years.
Even that good news came with a caveat, however. The vote by the CDC’s Advisory Committee on Immunization Practices was 11:1 in favor, with the negative vote cast by Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., who said that “boosters are great once we’ve gotten everyone their first round. That needs to be our priority in this.”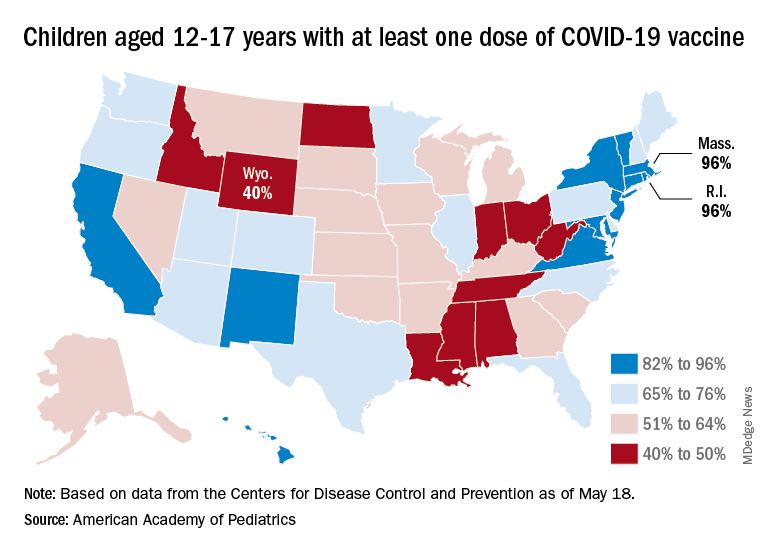
Nationally, in fact, just 35.7% of children aged 5-11 years have received at least one dose of the vaccine and only 29.0% are fully vaccinated. Those figures are nearly doubled among 12- to 17-year-olds: 69.3% have received at least one dose and 59.4% are fully vaccinated, the CDC said on its COVID Data Tracker.
Some states, meanwhile, are well below those national rates. In Wyoming, only 40% of children aged 12-17 have received an initial vaccine dose, and eight other states are below 50%. Among children aged 5-12, there are still five states below 20% in that measure, while the states on the other end of the spectrum – Vermont and Massachusetts – are above 60%, the AAP said in its separate vaccination report.
NSCLC with brain metastasis: ICI-radiotherapy combo prolongs OS vs chemoradiotherapy
Key clinical point: Immune checkpoint inhibitors (ICI) plus radiotherapy (RT) conferred an overall survival (OS) benefit over chemotherapy plus RT after resection of brain metastasis from non-small cell lung cancer (NSCLC).
Major finding: The chemotherapy plus RT group had a shorter median OS than the ICI plus RT group after neurosurgery (11.8 months; 95% CI 9.1-15.2 vs 23.0 months; 95% CI 20.3-53.8; P < .001).
Study details: The data come from a retrospective propensity score-matched cohort study involving 62 NSCLC patients treated with ICI plus RT and 62 treated with chemotherapy plus RT after neurosurgery for brain metastasis, from 2010 to 2021.
Disclosures: No funding information was available. N Frost reported receiving personal fees and nonfinancial support from pharmaceutical companies outside this work. The other authors declared no competing interests.
Source: Wasilewski D et al. Effectiveness of immune checkpoint inhibition vs chemotherapy in combination with radiation therapy among patients with non–small cell lung cancer and brain metastasis undergoing neurosurgical resection. JAMA Netw Open. 2022;5(4):e229553 (Apr 29). Doi: 10.1001/jamanetworkopen.2022.9553
Key clinical point: Immune checkpoint inhibitors (ICI) plus radiotherapy (RT) conferred an overall survival (OS) benefit over chemotherapy plus RT after resection of brain metastasis from non-small cell lung cancer (NSCLC).
Major finding: The chemotherapy plus RT group had a shorter median OS than the ICI plus RT group after neurosurgery (11.8 months; 95% CI 9.1-15.2 vs 23.0 months; 95% CI 20.3-53.8; P < .001).
Study details: The data come from a retrospective propensity score-matched cohort study involving 62 NSCLC patients treated with ICI plus RT and 62 treated with chemotherapy plus RT after neurosurgery for brain metastasis, from 2010 to 2021.
Disclosures: No funding information was available. N Frost reported receiving personal fees and nonfinancial support from pharmaceutical companies outside this work. The other authors declared no competing interests.
Source: Wasilewski D et al. Effectiveness of immune checkpoint inhibition vs chemotherapy in combination with radiation therapy among patients with non–small cell lung cancer and brain metastasis undergoing neurosurgical resection. JAMA Netw Open. 2022;5(4):e229553 (Apr 29). Doi: 10.1001/jamanetworkopen.2022.9553
Key clinical point: Immune checkpoint inhibitors (ICI) plus radiotherapy (RT) conferred an overall survival (OS) benefit over chemotherapy plus RT after resection of brain metastasis from non-small cell lung cancer (NSCLC).
Major finding: The chemotherapy plus RT group had a shorter median OS than the ICI plus RT group after neurosurgery (11.8 months; 95% CI 9.1-15.2 vs 23.0 months; 95% CI 20.3-53.8; P < .001).
Study details: The data come from a retrospective propensity score-matched cohort study involving 62 NSCLC patients treated with ICI plus RT and 62 treated with chemotherapy plus RT after neurosurgery for brain metastasis, from 2010 to 2021.
Disclosures: No funding information was available. N Frost reported receiving personal fees and nonfinancial support from pharmaceutical companies outside this work. The other authors declared no competing interests.
Source: Wasilewski D et al. Effectiveness of immune checkpoint inhibition vs chemotherapy in combination with radiation therapy among patients with non–small cell lung cancer and brain metastasis undergoing neurosurgical resection. JAMA Netw Open. 2022;5(4):e229553 (Apr 29). Doi: 10.1001/jamanetworkopen.2022.9553
Advanced NSCLC: Real-world long-term survival outcomes of ICI-treated patients
Key clinical point: In a real-world cohort of patients with advanced non-small cell lung cancer (NSCLC) treated with immune checkpoint inhibitor (ICI) monotherapy, the 4-year overall survival (OS) was nearly 18%.
Major finding: The mean progression-free survival (PFS) was 3.4 months and OS was 13.0 months. The 4-year OS rate was 17.9%. The predictors of favorable OS and PFS included age >70 years, a good Eastern Cooperative Oncology Group Performance Status score, programmed cell death-ligand 1 tumor proportion score of ≥50%, absence of bone metastasis, and presence of immune-related skin toxicity.
Study details: The data come from a real-world retrospective cohort study of 435 patients diagnosed with advanced, metastatic, or recurrent NSCLC and treated with ICI monotherapy across seven Japanese centers (2015-2018).
Disclosures: No information on funding and disclosures was available.
Source: Yoneda T et al. Long-term survival of patients with non-small cell lung cancer treated with immune checkpoint inhibitor monotherapy in real-world settings. Clin Lung Cancer. 2022 (May 1). Doi: 10.1016/j.cllc.2022.03.008
Key clinical point: In a real-world cohort of patients with advanced non-small cell lung cancer (NSCLC) treated with immune checkpoint inhibitor (ICI) monotherapy, the 4-year overall survival (OS) was nearly 18%.
Major finding: The mean progression-free survival (PFS) was 3.4 months and OS was 13.0 months. The 4-year OS rate was 17.9%. The predictors of favorable OS and PFS included age >70 years, a good Eastern Cooperative Oncology Group Performance Status score, programmed cell death-ligand 1 tumor proportion score of ≥50%, absence of bone metastasis, and presence of immune-related skin toxicity.
Study details: The data come from a real-world retrospective cohort study of 435 patients diagnosed with advanced, metastatic, or recurrent NSCLC and treated with ICI monotherapy across seven Japanese centers (2015-2018).
Disclosures: No information on funding and disclosures was available.
Source: Yoneda T et al. Long-term survival of patients with non-small cell lung cancer treated with immune checkpoint inhibitor monotherapy in real-world settings. Clin Lung Cancer. 2022 (May 1). Doi: 10.1016/j.cllc.2022.03.008
Key clinical point: In a real-world cohort of patients with advanced non-small cell lung cancer (NSCLC) treated with immune checkpoint inhibitor (ICI) monotherapy, the 4-year overall survival (OS) was nearly 18%.
Major finding: The mean progression-free survival (PFS) was 3.4 months and OS was 13.0 months. The 4-year OS rate was 17.9%. The predictors of favorable OS and PFS included age >70 years, a good Eastern Cooperative Oncology Group Performance Status score, programmed cell death-ligand 1 tumor proportion score of ≥50%, absence of bone metastasis, and presence of immune-related skin toxicity.
Study details: The data come from a real-world retrospective cohort study of 435 patients diagnosed with advanced, metastatic, or recurrent NSCLC and treated with ICI monotherapy across seven Japanese centers (2015-2018).
Disclosures: No information on funding and disclosures was available.
Source: Yoneda T et al. Long-term survival of patients with non-small cell lung cancer treated with immune checkpoint inhibitor monotherapy in real-world settings. Clin Lung Cancer. 2022 (May 1). Doi: 10.1016/j.cllc.2022.03.008
ALK- and ROS1-rearranged advanced NSCLC: Anticoagulants linked to worse outcomes
Key clinical point: Anticoagulant use is linked to worse progression-free survival (PFS) and objective response rate (ORR) in patients with ALK- and ROS1-rearranged advanced nonsmall cell lung cancer (NSCLC) treated with crizotinib.
Major finding: In the ROS1-rearranged group, anticoagulant use vs no use was associated with a shorter median PFS (5.1 vs 29 months) and poorer ORR (41.7% vs 80.5%). Similarly, in the ALK-rearranged group, anticoagulant use vs no use was associated with a shorter median PFS (7.1 vs 12 months) and poorer ORR (41% vs 74.3%).
Study details: The data come from a retrospective analysis of patients with ROS1- and ALK-rearranged advanced NSCLC (n = 206) who received crizotinib in the phase 1 PROFILE 1001 trial.
Disclosures: The study was funded by Pfizer. The authors reported receiving grants or personal fees from one or more pharmaceutical companies, including Pfizer, outside this work.
Source: Ng TL, Tsui DCC, et al. Association of anticoagulant use with clinical outcomes from crizotinib in ALK- and ROS1-rearranged advanced non-small cell lung cancers: A retrospective analysis of PROFILE 1001. Cancer Med. 2022 (May 5). Doi: 10.1002/cam4.4789
Key clinical point: Anticoagulant use is linked to worse progression-free survival (PFS) and objective response rate (ORR) in patients with ALK- and ROS1-rearranged advanced nonsmall cell lung cancer (NSCLC) treated with crizotinib.
Major finding: In the ROS1-rearranged group, anticoagulant use vs no use was associated with a shorter median PFS (5.1 vs 29 months) and poorer ORR (41.7% vs 80.5%). Similarly, in the ALK-rearranged group, anticoagulant use vs no use was associated with a shorter median PFS (7.1 vs 12 months) and poorer ORR (41% vs 74.3%).
Study details: The data come from a retrospective analysis of patients with ROS1- and ALK-rearranged advanced NSCLC (n = 206) who received crizotinib in the phase 1 PROFILE 1001 trial.
Disclosures: The study was funded by Pfizer. The authors reported receiving grants or personal fees from one or more pharmaceutical companies, including Pfizer, outside this work.
Source: Ng TL, Tsui DCC, et al. Association of anticoagulant use with clinical outcomes from crizotinib in ALK- and ROS1-rearranged advanced non-small cell lung cancers: A retrospective analysis of PROFILE 1001. Cancer Med. 2022 (May 5). Doi: 10.1002/cam4.4789
Key clinical point: Anticoagulant use is linked to worse progression-free survival (PFS) and objective response rate (ORR) in patients with ALK- and ROS1-rearranged advanced nonsmall cell lung cancer (NSCLC) treated with crizotinib.
Major finding: In the ROS1-rearranged group, anticoagulant use vs no use was associated with a shorter median PFS (5.1 vs 29 months) and poorer ORR (41.7% vs 80.5%). Similarly, in the ALK-rearranged group, anticoagulant use vs no use was associated with a shorter median PFS (7.1 vs 12 months) and poorer ORR (41% vs 74.3%).
Study details: The data come from a retrospective analysis of patients with ROS1- and ALK-rearranged advanced NSCLC (n = 206) who received crizotinib in the phase 1 PROFILE 1001 trial.
Disclosures: The study was funded by Pfizer. The authors reported receiving grants or personal fees from one or more pharmaceutical companies, including Pfizer, outside this work.
Source: Ng TL, Tsui DCC, et al. Association of anticoagulant use with clinical outcomes from crizotinib in ALK- and ROS1-rearranged advanced non-small cell lung cancers: A retrospective analysis of PROFILE 1001. Cancer Med. 2022 (May 5). Doi: 10.1002/cam4.4789