User login
Why Do Minority Women Have a Higher Risk of Postpartum Depression?
About 10% to 15% of women in the US have postpartum depression (PPD)—but that estimate is based mostly on women of European ancestry. In black women the rates are doubled, and among Latinas the prevalence is 30% to 43%. But those 2 groups have been inadequately studied, say researchers from University of North Carolina. To help remedy the lack of information, they conducted a study with the largest and “most robustly phenotyped” cohort of minority women with PPD. Their study also is the first to examine genetic ancestry as it contributes to PPD risk.
The researchers recruited 549 women with PPD and 968 without PPD who were within 6 weeks of having given birth. Of those, 67.4% were black, 14.4% were Latina, and 18.2% were white. The median age was 26.7; nearly half of the participants were married. Only 3.6% had given birth for the first time.
The women completed a battery of tests, including the Abuse and Trauma Inventory, Everyday Stressors Index (ESI), Edinburgh Postnatal Depression Scale (EPDS), and Postpartum Bonding Questionnaire. The researchers also assessed estradiol, progesterone, brain-derived neurotrophic factor, oxytocin, and allopregnanolone.
The women with PPD had significantly higher rates of previous psychiatric diagnoses, significantly higher EPDS total scores, and higher rates of family history of PPD. They also had significantly higher rates of previous diagnoses of major depressive disorder (MDD) (53% vs 15%), although 47% were experiencing their first episode of MDD. Dramatically higher numbers of women with PPD vs without PPD had suicidal thoughts in the month prior to assessment: 36% vs 2%, respectively.
Genetic ancestry was not predictive of case status, nor were hormonal influences any different between the 2 groups. Instead, psychiatric history and exposure to adverse life events were significant predictors. Nearly half of all the women with PPD had a lifetime anxiety disorder diagnosis compared with 7% of the controls. And although 67% of all participants reported a history of ≥ 1 traumatic event, women with PPD had double the proportion of multiple events of abuse and trauma. Women who had experienced multiple adverse life events were 3 times more likely to have PPD. Childhood and adult sexual abuse and life-threatening attack were among the most predictive.
The women with PPD had an ESI score > 3 times higher than that of the controls (19% vs 6%, respectively). The researchers note that cumulative lifetime stress may lead to epigenetic modification, and thus to PPD. Women with PPD also had a significantly higher proportion of dysfunctional mother-infant relationships, although the numbers were low in both groups (7% vs 0.35%, respectively).
The researchers say that although genetic ancestry did not play a role in determining case status, there are important ethnic and cultural differences that do play a role in treatment. For instance, Latinas and black women may be less likely to accept antidepressants as therapy. And because socioeconomic status is a determinant of health care access, they also face major barriers to mental health care. However, neither insurance nor education status (markers of socioeconomic status) distinguished cases from controls, even when the researchers controlled for genetic ancestry.
Their data provide a set of risk factors that can be used in screening new mothers, the researchers say. A brief, single assessment for previous psychiatric and abuse/trauma history during the perinatal period, along with regular mood monitoring, could increase a clinician’s ability to predict the onset of PPD.
Source:
Guintivano J, Sullivan PF, Stuebe AM. Psychol Med. 2018;48(7):1190-1200.
doi: 10.1017/S0033291717002641.
About 10% to 15% of women in the US have postpartum depression (PPD)—but that estimate is based mostly on women of European ancestry. In black women the rates are doubled, and among Latinas the prevalence is 30% to 43%. But those 2 groups have been inadequately studied, say researchers from University of North Carolina. To help remedy the lack of information, they conducted a study with the largest and “most robustly phenotyped” cohort of minority women with PPD. Their study also is the first to examine genetic ancestry as it contributes to PPD risk.
The researchers recruited 549 women with PPD and 968 without PPD who were within 6 weeks of having given birth. Of those, 67.4% were black, 14.4% were Latina, and 18.2% were white. The median age was 26.7; nearly half of the participants were married. Only 3.6% had given birth for the first time.
The women completed a battery of tests, including the Abuse and Trauma Inventory, Everyday Stressors Index (ESI), Edinburgh Postnatal Depression Scale (EPDS), and Postpartum Bonding Questionnaire. The researchers also assessed estradiol, progesterone, brain-derived neurotrophic factor, oxytocin, and allopregnanolone.
The women with PPD had significantly higher rates of previous psychiatric diagnoses, significantly higher EPDS total scores, and higher rates of family history of PPD. They also had significantly higher rates of previous diagnoses of major depressive disorder (MDD) (53% vs 15%), although 47% were experiencing their first episode of MDD. Dramatically higher numbers of women with PPD vs without PPD had suicidal thoughts in the month prior to assessment: 36% vs 2%, respectively.
Genetic ancestry was not predictive of case status, nor were hormonal influences any different between the 2 groups. Instead, psychiatric history and exposure to adverse life events were significant predictors. Nearly half of all the women with PPD had a lifetime anxiety disorder diagnosis compared with 7% of the controls. And although 67% of all participants reported a history of ≥ 1 traumatic event, women with PPD had double the proportion of multiple events of abuse and trauma. Women who had experienced multiple adverse life events were 3 times more likely to have PPD. Childhood and adult sexual abuse and life-threatening attack were among the most predictive.
The women with PPD had an ESI score > 3 times higher than that of the controls (19% vs 6%, respectively). The researchers note that cumulative lifetime stress may lead to epigenetic modification, and thus to PPD. Women with PPD also had a significantly higher proportion of dysfunctional mother-infant relationships, although the numbers were low in both groups (7% vs 0.35%, respectively).
The researchers say that although genetic ancestry did not play a role in determining case status, there are important ethnic and cultural differences that do play a role in treatment. For instance, Latinas and black women may be less likely to accept antidepressants as therapy. And because socioeconomic status is a determinant of health care access, they also face major barriers to mental health care. However, neither insurance nor education status (markers of socioeconomic status) distinguished cases from controls, even when the researchers controlled for genetic ancestry.
Their data provide a set of risk factors that can be used in screening new mothers, the researchers say. A brief, single assessment for previous psychiatric and abuse/trauma history during the perinatal period, along with regular mood monitoring, could increase a clinician’s ability to predict the onset of PPD.
Source:
Guintivano J, Sullivan PF, Stuebe AM. Psychol Med. 2018;48(7):1190-1200.
doi: 10.1017/S0033291717002641.
About 10% to 15% of women in the US have postpartum depression (PPD)—but that estimate is based mostly on women of European ancestry. In black women the rates are doubled, and among Latinas the prevalence is 30% to 43%. But those 2 groups have been inadequately studied, say researchers from University of North Carolina. To help remedy the lack of information, they conducted a study with the largest and “most robustly phenotyped” cohort of minority women with PPD. Their study also is the first to examine genetic ancestry as it contributes to PPD risk.
The researchers recruited 549 women with PPD and 968 without PPD who were within 6 weeks of having given birth. Of those, 67.4% were black, 14.4% were Latina, and 18.2% were white. The median age was 26.7; nearly half of the participants were married. Only 3.6% had given birth for the first time.
The women completed a battery of tests, including the Abuse and Trauma Inventory, Everyday Stressors Index (ESI), Edinburgh Postnatal Depression Scale (EPDS), and Postpartum Bonding Questionnaire. The researchers also assessed estradiol, progesterone, brain-derived neurotrophic factor, oxytocin, and allopregnanolone.
The women with PPD had significantly higher rates of previous psychiatric diagnoses, significantly higher EPDS total scores, and higher rates of family history of PPD. They also had significantly higher rates of previous diagnoses of major depressive disorder (MDD) (53% vs 15%), although 47% were experiencing their first episode of MDD. Dramatically higher numbers of women with PPD vs without PPD had suicidal thoughts in the month prior to assessment: 36% vs 2%, respectively.
Genetic ancestry was not predictive of case status, nor were hormonal influences any different between the 2 groups. Instead, psychiatric history and exposure to adverse life events were significant predictors. Nearly half of all the women with PPD had a lifetime anxiety disorder diagnosis compared with 7% of the controls. And although 67% of all participants reported a history of ≥ 1 traumatic event, women with PPD had double the proportion of multiple events of abuse and trauma. Women who had experienced multiple adverse life events were 3 times more likely to have PPD. Childhood and adult sexual abuse and life-threatening attack were among the most predictive.
The women with PPD had an ESI score > 3 times higher than that of the controls (19% vs 6%, respectively). The researchers note that cumulative lifetime stress may lead to epigenetic modification, and thus to PPD. Women with PPD also had a significantly higher proportion of dysfunctional mother-infant relationships, although the numbers were low in both groups (7% vs 0.35%, respectively).
The researchers say that although genetic ancestry did not play a role in determining case status, there are important ethnic and cultural differences that do play a role in treatment. For instance, Latinas and black women may be less likely to accept antidepressants as therapy. And because socioeconomic status is a determinant of health care access, they also face major barriers to mental health care. However, neither insurance nor education status (markers of socioeconomic status) distinguished cases from controls, even when the researchers controlled for genetic ancestry.
Their data provide a set of risk factors that can be used in screening new mothers, the researchers say. A brief, single assessment for previous psychiatric and abuse/trauma history during the perinatal period, along with regular mood monitoring, could increase a clinician’s ability to predict the onset of PPD.
Source:
Guintivano J, Sullivan PF, Stuebe AM. Psychol Med. 2018;48(7):1190-1200.
doi: 10.1017/S0033291717002641.
Cost of imatinib still high despite generic options, team says
The availability of generic imatinib has had limited effects on costs of the drug, according to research published in Health Affairs.
Data suggest the cost of Gleevec in the US has more than doubled since the drug was approved in 2001, and the introduction of generic imatinib has reduced costs only slightly.
Two years after generic imatinib hit the market, a month’s supply of Gleevec cost about $9000, and the cost for generic imatinib was about $8000.
“Patients and providers have all looked forward to generic entry, expecting major price reductions,” said study author Stacie Dusetzina, PhD, of Vanderbilt University School of Medicine in Nashville, Tennessee.
“Unfortunately, we don’t see prices drop as quickly and as low as we would hope when generics are available.”
For this study, Dr Dusetzina and a colleague analyzed data from the MarketScan Commercial Research Database. The database contained records of 139,233 prescription fills for imatinib, which were made by 7201 patients from May 2001 through September 2017.
The researchers noted that Gleevec was priced at nearly $4000 for a 1-month (400 mg) supply when it came on the market in 2001. That price escalated to nearly $10,000 by 2015 before a generic competitor entered the market.
However, prices for Gleevec and generic imatinib remained high 2 years later. In 2017, a month’s supply of Gleevec cost about $9000, and the cost of generic imatinib was about $8000.
The researchers said the Gleevec case demonstrates several potential barriers to effective generic price competition, including shifts in prescribing toward more expensive brand-name treatments and smaller-than-expected price reductions.
Twenty-four percent of imatinib (Gleevec) prescriptions claims were for “dispense as written,” according to the researchers. This suggests that patients or providers specifically wanted to stay on the brand-name drug instead of switching to the generic.
“The more than doubling of the drug price over time and the lack of price reductions observed with nearly 2 years of generic drug competition is concerning,” Dr Dusetzina said.
“It begs the question whether we can rely on generic entry as a primary approach to address drug pricing for high-priced specialty medications. We need robust competition to move prices in this space.”
The availability of generic imatinib has had limited effects on costs of the drug, according to research published in Health Affairs.
Data suggest the cost of Gleevec in the US has more than doubled since the drug was approved in 2001, and the introduction of generic imatinib has reduced costs only slightly.
Two years after generic imatinib hit the market, a month’s supply of Gleevec cost about $9000, and the cost for generic imatinib was about $8000.
“Patients and providers have all looked forward to generic entry, expecting major price reductions,” said study author Stacie Dusetzina, PhD, of Vanderbilt University School of Medicine in Nashville, Tennessee.
“Unfortunately, we don’t see prices drop as quickly and as low as we would hope when generics are available.”
For this study, Dr Dusetzina and a colleague analyzed data from the MarketScan Commercial Research Database. The database contained records of 139,233 prescription fills for imatinib, which were made by 7201 patients from May 2001 through September 2017.
The researchers noted that Gleevec was priced at nearly $4000 for a 1-month (400 mg) supply when it came on the market in 2001. That price escalated to nearly $10,000 by 2015 before a generic competitor entered the market.
However, prices for Gleevec and generic imatinib remained high 2 years later. In 2017, a month’s supply of Gleevec cost about $9000, and the cost of generic imatinib was about $8000.
The researchers said the Gleevec case demonstrates several potential barriers to effective generic price competition, including shifts in prescribing toward more expensive brand-name treatments and smaller-than-expected price reductions.
Twenty-four percent of imatinib (Gleevec) prescriptions claims were for “dispense as written,” according to the researchers. This suggests that patients or providers specifically wanted to stay on the brand-name drug instead of switching to the generic.
“The more than doubling of the drug price over time and the lack of price reductions observed with nearly 2 years of generic drug competition is concerning,” Dr Dusetzina said.
“It begs the question whether we can rely on generic entry as a primary approach to address drug pricing for high-priced specialty medications. We need robust competition to move prices in this space.”
The availability of generic imatinib has had limited effects on costs of the drug, according to research published in Health Affairs.
Data suggest the cost of Gleevec in the US has more than doubled since the drug was approved in 2001, and the introduction of generic imatinib has reduced costs only slightly.
Two years after generic imatinib hit the market, a month’s supply of Gleevec cost about $9000, and the cost for generic imatinib was about $8000.
“Patients and providers have all looked forward to generic entry, expecting major price reductions,” said study author Stacie Dusetzina, PhD, of Vanderbilt University School of Medicine in Nashville, Tennessee.
“Unfortunately, we don’t see prices drop as quickly and as low as we would hope when generics are available.”
For this study, Dr Dusetzina and a colleague analyzed data from the MarketScan Commercial Research Database. The database contained records of 139,233 prescription fills for imatinib, which were made by 7201 patients from May 2001 through September 2017.
The researchers noted that Gleevec was priced at nearly $4000 for a 1-month (400 mg) supply when it came on the market in 2001. That price escalated to nearly $10,000 by 2015 before a generic competitor entered the market.
However, prices for Gleevec and generic imatinib remained high 2 years later. In 2017, a month’s supply of Gleevec cost about $9000, and the cost of generic imatinib was about $8000.
The researchers said the Gleevec case demonstrates several potential barriers to effective generic price competition, including shifts in prescribing toward more expensive brand-name treatments and smaller-than-expected price reductions.
Twenty-four percent of imatinib (Gleevec) prescriptions claims were for “dispense as written,” according to the researchers. This suggests that patients or providers specifically wanted to stay on the brand-name drug instead of switching to the generic.
“The more than doubling of the drug price over time and the lack of price reductions observed with nearly 2 years of generic drug competition is concerning,” Dr Dusetzina said.
“It begs the question whether we can rely on generic entry as a primary approach to address drug pricing for high-priced specialty medications. We need robust competition to move prices in this space.”
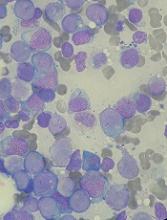
Y chromosome gene protects against AML
Researchers have discovered the first leukemia-protective gene that is specific to the Y chromosome, according to an article published in Nature Genetics.
The researchers were investigating how loss of the X-chromosome gene UTX hastens the development of acute myeloid leukemia (AML).
However, they found that UTY, a related gene on the Y chromosome, protected male mice lacking UTX from developing AML.
The researchers then found that, in AML and other cancers, loss of UTX is accompanied by loss of UTY.
“This is the first Y chromosome-specific gene that protects against AML,” said study author Malgorzata Gozdecka, PhD, of the Wellcome Sanger Institute in Hinxton, UK.
“Previously, it had been suggested that the only function of the Y chromosome is in creating male sexual characteristics, but our results indicate that the Y chromosome could also protect against AML and other cancers.”
For this work, Dr Gozdecka and her colleagues studied the UTX gene in human cells and mice.
In addition to their discovery that UTY acts as a tumor suppressor gene, the researchers uncovered a new mechanism for how loss of UTX leads to AML.
They discovered that UTX acts as a common scaffold, bringing together a large number of regulatory proteins that control access to DNA and gene expression, a function that can also be carried out by UTY.
Specifically, the team said UTX suppresses AML by repressing oncogenic ETS and upregulating tumor-suppressive GATA programs. And loss of UTX leads to “altered patterns of gene expression that induce and maintain” AML.
“Treatments for AML have not changed in decades, and there is a large unmet need for new therapies,” said study author George Vassiliou, PhD, of the Wellcome Sanger Institute.
“This study helps us understand the development of AML and gives us clues for developing new drug targets to disrupt leukemia-causing processes. We hope this study will enable new lines of research for the development of previously unforeseen treatments and improve the lives of patients with AML.”
Researchers have discovered the first leukemia-protective gene that is specific to the Y chromosome, according to an article published in Nature Genetics.
The researchers were investigating how loss of the X-chromosome gene UTX hastens the development of acute myeloid leukemia (AML).
However, they found that UTY, a related gene on the Y chromosome, protected male mice lacking UTX from developing AML.
The researchers then found that, in AML and other cancers, loss of UTX is accompanied by loss of UTY.
“This is the first Y chromosome-specific gene that protects against AML,” said study author Malgorzata Gozdecka, PhD, of the Wellcome Sanger Institute in Hinxton, UK.
“Previously, it had been suggested that the only function of the Y chromosome is in creating male sexual characteristics, but our results indicate that the Y chromosome could also protect against AML and other cancers.”
For this work, Dr Gozdecka and her colleagues studied the UTX gene in human cells and mice.
In addition to their discovery that UTY acts as a tumor suppressor gene, the researchers uncovered a new mechanism for how loss of UTX leads to AML.
They discovered that UTX acts as a common scaffold, bringing together a large number of regulatory proteins that control access to DNA and gene expression, a function that can also be carried out by UTY.
Specifically, the team said UTX suppresses AML by repressing oncogenic ETS and upregulating tumor-suppressive GATA programs. And loss of UTX leads to “altered patterns of gene expression that induce and maintain” AML.
“Treatments for AML have not changed in decades, and there is a large unmet need for new therapies,” said study author George Vassiliou, PhD, of the Wellcome Sanger Institute.
“This study helps us understand the development of AML and gives us clues for developing new drug targets to disrupt leukemia-causing processes. We hope this study will enable new lines of research for the development of previously unforeseen treatments and improve the lives of patients with AML.”
Researchers have discovered the first leukemia-protective gene that is specific to the Y chromosome, according to an article published in Nature Genetics.
The researchers were investigating how loss of the X-chromosome gene UTX hastens the development of acute myeloid leukemia (AML).
However, they found that UTY, a related gene on the Y chromosome, protected male mice lacking UTX from developing AML.
The researchers then found that, in AML and other cancers, loss of UTX is accompanied by loss of UTY.
“This is the first Y chromosome-specific gene that protects against AML,” said study author Malgorzata Gozdecka, PhD, of the Wellcome Sanger Institute in Hinxton, UK.
“Previously, it had been suggested that the only function of the Y chromosome is in creating male sexual characteristics, but our results indicate that the Y chromosome could also protect against AML and other cancers.”
For this work, Dr Gozdecka and her colleagues studied the UTX gene in human cells and mice.
In addition to their discovery that UTY acts as a tumor suppressor gene, the researchers uncovered a new mechanism for how loss of UTX leads to AML.
They discovered that UTX acts as a common scaffold, bringing together a large number of regulatory proteins that control access to DNA and gene expression, a function that can also be carried out by UTY.
Specifically, the team said UTX suppresses AML by repressing oncogenic ETS and upregulating tumor-suppressive GATA programs. And loss of UTX leads to “altered patterns of gene expression that induce and maintain” AML.
“Treatments for AML have not changed in decades, and there is a large unmet need for new therapies,” said study author George Vassiliou, PhD, of the Wellcome Sanger Institute.
“This study helps us understand the development of AML and gives us clues for developing new drug targets to disrupt leukemia-causing processes. We hope this study will enable new lines of research for the development of previously unforeseen treatments and improve the lives of patients with AML.”
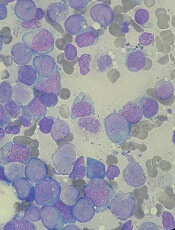
How ruxolitinib reduces thrombosis in MPNs
Preclinical research helps explain how the JAK1/2 inhibitor ruxolitinib can reduce thrombosis in patients with myeloproliferative neoplasms (MPNs).
Experiments revealed a link between JAK2V617F and the formation of neutrophil extracellular traps (NETs), which have been implicated in thrombosis.
Researchers found that ruxolitinib reduced NET formation and decreased thrombosis in JAK2-mutant mice.
Benjamin L. Ebert, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues reported these findings in Science Translational Medicine.
The researchers noted that patients with MPNs have an increased risk of thrombosis, and previous research linked thrombosis to the formation of NETs. NETs are structures that help trap pathogens but may also promote autoimmune responses and excessive blood clotting.
With the current study, Dr Ebert and his colleagues examined whether NET formation could promote thrombosis in patients with MPNs.
The team found that neutrophils from MPN patients were more likely to form NETs than neutrophils from healthy individuals. However, incubating neutrophils with ruxolitinib reduced NET formation.
The researchers also found that mice with JAK2V617F were more likely to form NETs and develop thrombosis when compared to wild-type mice. However, treatment with ruxolitinib reduced rates of thrombosis and prevented NET formation in the mice.
The researchers noted that expression of PAD4, a protein required for NET formation, is increased in JAK2V617F-expressing neutrophils. And the team found that PAD4 is required for JAK2V617F-driven NET formation and thrombosis in mouse models of MPNs.
Lastly, the researchers looked at data from 10,893 human subjects. None of these subjects had MPNs, but some had JAK2V617F.
Subjects who were JAK2V617F-positive had a significantly higher risk of thrombotic events than subjects without the mutation (P=0.0003).
Taken together, these findings suggest that JAK2 inhibition can reduce NET formation and ameliorate thrombosis in patients with MPNs or the JAK2V617F mutation.
The researchers noted that, in the phase 3 RESPONSE trial, patients with polycythemia vera had a lower rate of thromboembolic events if they received ruxolitinib rather than standard therapy.
Preclinical research helps explain how the JAK1/2 inhibitor ruxolitinib can reduce thrombosis in patients with myeloproliferative neoplasms (MPNs).
Experiments revealed a link between JAK2V617F and the formation of neutrophil extracellular traps (NETs), which have been implicated in thrombosis.
Researchers found that ruxolitinib reduced NET formation and decreased thrombosis in JAK2-mutant mice.
Benjamin L. Ebert, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues reported these findings in Science Translational Medicine.
The researchers noted that patients with MPNs have an increased risk of thrombosis, and previous research linked thrombosis to the formation of NETs. NETs are structures that help trap pathogens but may also promote autoimmune responses and excessive blood clotting.
With the current study, Dr Ebert and his colleagues examined whether NET formation could promote thrombosis in patients with MPNs.
The team found that neutrophils from MPN patients were more likely to form NETs than neutrophils from healthy individuals. However, incubating neutrophils with ruxolitinib reduced NET formation.
The researchers also found that mice with JAK2V617F were more likely to form NETs and develop thrombosis when compared to wild-type mice. However, treatment with ruxolitinib reduced rates of thrombosis and prevented NET formation in the mice.
The researchers noted that expression of PAD4, a protein required for NET formation, is increased in JAK2V617F-expressing neutrophils. And the team found that PAD4 is required for JAK2V617F-driven NET formation and thrombosis in mouse models of MPNs.
Lastly, the researchers looked at data from 10,893 human subjects. None of these subjects had MPNs, but some had JAK2V617F.
Subjects who were JAK2V617F-positive had a significantly higher risk of thrombotic events than subjects without the mutation (P=0.0003).
Taken together, these findings suggest that JAK2 inhibition can reduce NET formation and ameliorate thrombosis in patients with MPNs or the JAK2V617F mutation.
The researchers noted that, in the phase 3 RESPONSE trial, patients with polycythemia vera had a lower rate of thromboembolic events if they received ruxolitinib rather than standard therapy.
Preclinical research helps explain how the JAK1/2 inhibitor ruxolitinib can reduce thrombosis in patients with myeloproliferative neoplasms (MPNs).
Experiments revealed a link between JAK2V617F and the formation of neutrophil extracellular traps (NETs), which have been implicated in thrombosis.
Researchers found that ruxolitinib reduced NET formation and decreased thrombosis in JAK2-mutant mice.
Benjamin L. Ebert, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues reported these findings in Science Translational Medicine.
The researchers noted that patients with MPNs have an increased risk of thrombosis, and previous research linked thrombosis to the formation of NETs. NETs are structures that help trap pathogens but may also promote autoimmune responses and excessive blood clotting.
With the current study, Dr Ebert and his colleagues examined whether NET formation could promote thrombosis in patients with MPNs.
The team found that neutrophils from MPN patients were more likely to form NETs than neutrophils from healthy individuals. However, incubating neutrophils with ruxolitinib reduced NET formation.
The researchers also found that mice with JAK2V617F were more likely to form NETs and develop thrombosis when compared to wild-type mice. However, treatment with ruxolitinib reduced rates of thrombosis and prevented NET formation in the mice.
The researchers noted that expression of PAD4, a protein required for NET formation, is increased in JAK2V617F-expressing neutrophils. And the team found that PAD4 is required for JAK2V617F-driven NET formation and thrombosis in mouse models of MPNs.
Lastly, the researchers looked at data from 10,893 human subjects. None of these subjects had MPNs, but some had JAK2V617F.
Subjects who were JAK2V617F-positive had a significantly higher risk of thrombotic events than subjects without the mutation (P=0.0003).
Taken together, these findings suggest that JAK2 inhibition can reduce NET formation and ameliorate thrombosis in patients with MPNs or the JAK2V617F mutation.
The researchers noted that, in the phase 3 RESPONSE trial, patients with polycythemia vera had a lower rate of thromboembolic events if they received ruxolitinib rather than standard therapy.
About sex, adults aren’t talking or kids aren’t listening
TORONTO – Almost half of adolescents (45%) reported that their primary care providers (PCPs) do not routinely ask them about sex, and only 13% report they’ve been offered screening for sexually transmitted infections (STIs), according to a survey study presented at the Pediatric Academic Societies meeting.
And it appears the teenagers aren’t even listening to much of what their parents are saying on the subject: The survey also found that 90% of parents reported that they talk to their adolescents about sex, but only 39% of adolescents reported the same.
Regarding the discrepancy between the parents’ and adolescents’ responses, “Our best guess is that parents may have mentioned sex with their adolescents at some point, but the conversation was not meaningful enough to register on the adolescents’ radars! That type of discussion is probably best had more than once and in more than one way,”she said in an interview.
The adolescents, aged 13-17 years, and parents of adolescents attending the 2017 Minnesota State Fair were invited to complete an 18-question anonymous survey. The teens were queried whether they had seen a PCP in the last year and asked about their discussions about sexual activity and STIs with their physicians and parents. Parents were asked about their knowledge of discussions the teens had with their PCPs and their own discussions with their children. A total of 582 adolescents and 516 parents completed the survey.
One-quarter of parents who completed the survey felt that PCPs should not discuss sex with their teens.
“I think that primary care physicians have a lot to cover when doing preventive health visits with adolescents, and talking about sex is not necessarily an easy or comfortable thing to do and so may be something that falls to a lower priority. And it certainly doesn’t help if parents are not supportive of the concept of confidential adolescent care,” Dr. Schneider related.
“We were very surprised to see that 25% of parents did not feel that PCPs should be discussing sex with their child. I think that we need to next work on getting the parents on board and building an expectation that adolescents, when visiting their PCP, will have confidential discussions about sexual health,” she said.
TORONTO – Almost half of adolescents (45%) reported that their primary care providers (PCPs) do not routinely ask them about sex, and only 13% report they’ve been offered screening for sexually transmitted infections (STIs), according to a survey study presented at the Pediatric Academic Societies meeting.
And it appears the teenagers aren’t even listening to much of what their parents are saying on the subject: The survey also found that 90% of parents reported that they talk to their adolescents about sex, but only 39% of adolescents reported the same.
Regarding the discrepancy between the parents’ and adolescents’ responses, “Our best guess is that parents may have mentioned sex with their adolescents at some point, but the conversation was not meaningful enough to register on the adolescents’ radars! That type of discussion is probably best had more than once and in more than one way,”she said in an interview.
The adolescents, aged 13-17 years, and parents of adolescents attending the 2017 Minnesota State Fair were invited to complete an 18-question anonymous survey. The teens were queried whether they had seen a PCP in the last year and asked about their discussions about sexual activity and STIs with their physicians and parents. Parents were asked about their knowledge of discussions the teens had with their PCPs and their own discussions with their children. A total of 582 adolescents and 516 parents completed the survey.
One-quarter of parents who completed the survey felt that PCPs should not discuss sex with their teens.
“I think that primary care physicians have a lot to cover when doing preventive health visits with adolescents, and talking about sex is not necessarily an easy or comfortable thing to do and so may be something that falls to a lower priority. And it certainly doesn’t help if parents are not supportive of the concept of confidential adolescent care,” Dr. Schneider related.
“We were very surprised to see that 25% of parents did not feel that PCPs should be discussing sex with their child. I think that we need to next work on getting the parents on board and building an expectation that adolescents, when visiting their PCP, will have confidential discussions about sexual health,” she said.
TORONTO – Almost half of adolescents (45%) reported that their primary care providers (PCPs) do not routinely ask them about sex, and only 13% report they’ve been offered screening for sexually transmitted infections (STIs), according to a survey study presented at the Pediatric Academic Societies meeting.
And it appears the teenagers aren’t even listening to much of what their parents are saying on the subject: The survey also found that 90% of parents reported that they talk to their adolescents about sex, but only 39% of adolescents reported the same.
Regarding the discrepancy between the parents’ and adolescents’ responses, “Our best guess is that parents may have mentioned sex with their adolescents at some point, but the conversation was not meaningful enough to register on the adolescents’ radars! That type of discussion is probably best had more than once and in more than one way,”she said in an interview.
The adolescents, aged 13-17 years, and parents of adolescents attending the 2017 Minnesota State Fair were invited to complete an 18-question anonymous survey. The teens were queried whether they had seen a PCP in the last year and asked about their discussions about sexual activity and STIs with their physicians and parents. Parents were asked about their knowledge of discussions the teens had with their PCPs and their own discussions with their children. A total of 582 adolescents and 516 parents completed the survey.
One-quarter of parents who completed the survey felt that PCPs should not discuss sex with their teens.
“I think that primary care physicians have a lot to cover when doing preventive health visits with adolescents, and talking about sex is not necessarily an easy or comfortable thing to do and so may be something that falls to a lower priority. And it certainly doesn’t help if parents are not supportive of the concept of confidential adolescent care,” Dr. Schneider related.
“We were very surprised to see that 25% of parents did not feel that PCPs should be discussing sex with their child. I think that we need to next work on getting the parents on board and building an expectation that adolescents, when visiting their PCP, will have confidential discussions about sexual health,” she said.
Key clinical point:
Major finding: Of the adolescents who responded to the survey, 45% said their PCPs don’t routinely discuss sex with them, and only 13% reported being offered screening for STIs.
Study details: Survey study including 582 adolescents aged 13-17 years and 516 parents of adolescents.
Disclosures: Dr. Schneider reported no financial conflicts of interest.
Consider heterogeneous experiences among veteran cohorts when treating PTSD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW YORK – Veterans are not a homogeneous group, and when treating them for posttraumatic stress, it helps to consider their specific cohort, according to Elspeth Cameron Ritchie, MD.
Veterans from the first Gulf War, for example, have lingering concerns regarding medical illness (Gulf War syndrome); those from Vietnam are aging and might have medical problems or find that while they did well while working, now they are experiencing PTSD symptoms for the first time; and those returning from the conflicts in Iraq and Afghanistan might have physical injuries from blasts – the “signature weapon” of those wars. Such blasts can cause amputations, genital injuries, head trauma, and PTSD, said Dr. Ritchie, of the Uniformed Services University of the Health Sciences, Bethesda, Md.
In this video interview, Dr. Ritchie discusses these and other issues related to the treatment of PTSD among veterans as presented during a workshop entitled “Psychiatry and U.S. Veterans,” which she chaired at the annual meeting of the American Psychiatric Association.
The workshop covered the spectrum of treatments that might be helpful for veterans.
“ They don’t want it to just be the doctor giving them a pill,” she said. “Veterans are resilient; they’re tough; they don’t like to be thought of as victims ... and when you’re working with them, it’s very important to link into that dynamic resilient piece and capitalize on their strengths.”
Dr. Ritchie reported having no disclosures.
SOURCE: Ritchie EC et al. APA Workshop.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW YORK – Veterans are not a homogeneous group, and when treating them for posttraumatic stress, it helps to consider their specific cohort, according to Elspeth Cameron Ritchie, MD.
Veterans from the first Gulf War, for example, have lingering concerns regarding medical illness (Gulf War syndrome); those from Vietnam are aging and might have medical problems or find that while they did well while working, now they are experiencing PTSD symptoms for the first time; and those returning from the conflicts in Iraq and Afghanistan might have physical injuries from blasts – the “signature weapon” of those wars. Such blasts can cause amputations, genital injuries, head trauma, and PTSD, said Dr. Ritchie, of the Uniformed Services University of the Health Sciences, Bethesda, Md.
In this video interview, Dr. Ritchie discusses these and other issues related to the treatment of PTSD among veterans as presented during a workshop entitled “Psychiatry and U.S. Veterans,” which she chaired at the annual meeting of the American Psychiatric Association.
The workshop covered the spectrum of treatments that might be helpful for veterans.
“ They don’t want it to just be the doctor giving them a pill,” she said. “Veterans are resilient; they’re tough; they don’t like to be thought of as victims ... and when you’re working with them, it’s very important to link into that dynamic resilient piece and capitalize on their strengths.”
Dr. Ritchie reported having no disclosures.
SOURCE: Ritchie EC et al. APA Workshop.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW YORK – Veterans are not a homogeneous group, and when treating them for posttraumatic stress, it helps to consider their specific cohort, according to Elspeth Cameron Ritchie, MD.
Veterans from the first Gulf War, for example, have lingering concerns regarding medical illness (Gulf War syndrome); those from Vietnam are aging and might have medical problems or find that while they did well while working, now they are experiencing PTSD symptoms for the first time; and those returning from the conflicts in Iraq and Afghanistan might have physical injuries from blasts – the “signature weapon” of those wars. Such blasts can cause amputations, genital injuries, head trauma, and PTSD, said Dr. Ritchie, of the Uniformed Services University of the Health Sciences, Bethesda, Md.
In this video interview, Dr. Ritchie discusses these and other issues related to the treatment of PTSD among veterans as presented during a workshop entitled “Psychiatry and U.S. Veterans,” which she chaired at the annual meeting of the American Psychiatric Association.
The workshop covered the spectrum of treatments that might be helpful for veterans.
“ They don’t want it to just be the doctor giving them a pill,” she said. “Veterans are resilient; they’re tough; they don’t like to be thought of as victims ... and when you’re working with them, it’s very important to link into that dynamic resilient piece and capitalize on their strengths.”
Dr. Ritchie reported having no disclosures.
SOURCE: Ritchie EC et al. APA Workshop.
REPORTING FROM APA
Ivacaftor reduced hospitalizations in CF
with a variety of mutations, according to results published May 7 in Health Affairs.
The study involved 143 patients being treated with ivacaftor between February 2012 and February 2015. In 2014, the FDA expanded its approval for the use of ivacaftor by cystic fibrosis patients to include nine additional mutations, and patients with these mutations were included in this study.
Ms. Feng, who is senior director for policy and advocacy at the Cystic Fibrosis Foundation and her colleagues analyzed administrative claims data from the Truven Health Analytics Market Scan Commercial Research Database. All of the claims were for patients from the United States with employer-sponsored insurance plans. Eligibility criteria included an ICD-9 CM diagnosis of cystic fibrosis on one or more inpatient claims or two or more outpatient claims at least 30 days apart, a prescription claim for ivacaftor monotherapy, being at least 6 years of age at the time of the first filled prescription, and 12 months of continuous enrollment before and after the first filled prescription.
The “pre-ivacaftor” period was defined as the 12 months before the first filled prescription. The “post-ivacaftor” period was defined as the 12 months after the first filled prescription. For each period, the numbers and percentages of patients hospitalized were calculated, for any reason and for cystic fibrosis–related reasons. Hospitalization rates also were calculated as numbers of admissions per person-year, the authors said.
Data also were analyzed for two subcohorts: the 86 patients who started using ivacaftor between Feb. 6, 2012, and Feb. 21, 2014, under the initial Food and Drug Administration label; and the 57 patients who initiated use between Feb. 22, 2014, and Dec. 31, 2015, under the expanded FDA label, which included nine additional genetic mutations.
Of the 143 patients who had filled prescriptions for ivacaftor, 63% were aged 18 years or older. The rate of overall inpatient admissions decreased 55%, from 0.57 admissions per person-year in the pre-ivacaftor period to 0.26 admissions per person-year in the post-ivacaftor period, the investigators reported.
The declines in hospital admissions also were similar between the initial label and the expanded FDA label groups, with declines in overall admissions of 59% and 57%, respectively.
Hospital admissions related to cystic fibrosis also decreased significantly, by 78%. Admissions with principal diagnosis codes for cystic fibrosis decreased from 42 in the preprescription period, to 8 after filling the prescription. Rates per person per year decreased by 82% in patients aged 6-17 years and 80% among adults aged 18 years and older. Additionally, patients who filled at least 10 prescriptions during the study period experienced a 68% reduction in inpatient admissions, compared with 45% for those with three to nine prescriptions filled.
Ivacaftor also was associated with 60% lower per-person inpatient spending overall, with a greater proportional reduction in hospital costs for adults (68%) than for children (45%), and an absolute per-person reduction of $10,567, the authors reported.
“Treatments that target the protein defect that causes cystic fibrosis illustrate the promise of precision medicine,” the authors wrote. “To deliver the right care to the right patient, cystic fibrosis care must continue to account for other aspects unique to individuals such as environment, physiology, patients’ preferences, and lifestyle,” they concluded.
Ivacaftor (Kalydeco) is manufactured for Vertex Pharmaceuticals. No disclosures or conflicts of interest were reported.
SOURCE: Feng LB et al. Health Aff. 2018 May 8. doi: 10.1377/hlthaff.2017.1554
with a variety of mutations, according to results published May 7 in Health Affairs.
The study involved 143 patients being treated with ivacaftor between February 2012 and February 2015. In 2014, the FDA expanded its approval for the use of ivacaftor by cystic fibrosis patients to include nine additional mutations, and patients with these mutations were included in this study.
Ms. Feng, who is senior director for policy and advocacy at the Cystic Fibrosis Foundation and her colleagues analyzed administrative claims data from the Truven Health Analytics Market Scan Commercial Research Database. All of the claims were for patients from the United States with employer-sponsored insurance plans. Eligibility criteria included an ICD-9 CM diagnosis of cystic fibrosis on one or more inpatient claims or two or more outpatient claims at least 30 days apart, a prescription claim for ivacaftor monotherapy, being at least 6 years of age at the time of the first filled prescription, and 12 months of continuous enrollment before and after the first filled prescription.
The “pre-ivacaftor” period was defined as the 12 months before the first filled prescription. The “post-ivacaftor” period was defined as the 12 months after the first filled prescription. For each period, the numbers and percentages of patients hospitalized were calculated, for any reason and for cystic fibrosis–related reasons. Hospitalization rates also were calculated as numbers of admissions per person-year, the authors said.
Data also were analyzed for two subcohorts: the 86 patients who started using ivacaftor between Feb. 6, 2012, and Feb. 21, 2014, under the initial Food and Drug Administration label; and the 57 patients who initiated use between Feb. 22, 2014, and Dec. 31, 2015, under the expanded FDA label, which included nine additional genetic mutations.
Of the 143 patients who had filled prescriptions for ivacaftor, 63% were aged 18 years or older. The rate of overall inpatient admissions decreased 55%, from 0.57 admissions per person-year in the pre-ivacaftor period to 0.26 admissions per person-year in the post-ivacaftor period, the investigators reported.
The declines in hospital admissions also were similar between the initial label and the expanded FDA label groups, with declines in overall admissions of 59% and 57%, respectively.
Hospital admissions related to cystic fibrosis also decreased significantly, by 78%. Admissions with principal diagnosis codes for cystic fibrosis decreased from 42 in the preprescription period, to 8 after filling the prescription. Rates per person per year decreased by 82% in patients aged 6-17 years and 80% among adults aged 18 years and older. Additionally, patients who filled at least 10 prescriptions during the study period experienced a 68% reduction in inpatient admissions, compared with 45% for those with three to nine prescriptions filled.
Ivacaftor also was associated with 60% lower per-person inpatient spending overall, with a greater proportional reduction in hospital costs for adults (68%) than for children (45%), and an absolute per-person reduction of $10,567, the authors reported.
“Treatments that target the protein defect that causes cystic fibrosis illustrate the promise of precision medicine,” the authors wrote. “To deliver the right care to the right patient, cystic fibrosis care must continue to account for other aspects unique to individuals such as environment, physiology, patients’ preferences, and lifestyle,” they concluded.
Ivacaftor (Kalydeco) is manufactured for Vertex Pharmaceuticals. No disclosures or conflicts of interest were reported.
SOURCE: Feng LB et al. Health Aff. 2018 May 8. doi: 10.1377/hlthaff.2017.1554
with a variety of mutations, according to results published May 7 in Health Affairs.
The study involved 143 patients being treated with ivacaftor between February 2012 and February 2015. In 2014, the FDA expanded its approval for the use of ivacaftor by cystic fibrosis patients to include nine additional mutations, and patients with these mutations were included in this study.
Ms. Feng, who is senior director for policy and advocacy at the Cystic Fibrosis Foundation and her colleagues analyzed administrative claims data from the Truven Health Analytics Market Scan Commercial Research Database. All of the claims were for patients from the United States with employer-sponsored insurance plans. Eligibility criteria included an ICD-9 CM diagnosis of cystic fibrosis on one or more inpatient claims or two or more outpatient claims at least 30 days apart, a prescription claim for ivacaftor monotherapy, being at least 6 years of age at the time of the first filled prescription, and 12 months of continuous enrollment before and after the first filled prescription.
The “pre-ivacaftor” period was defined as the 12 months before the first filled prescription. The “post-ivacaftor” period was defined as the 12 months after the first filled prescription. For each period, the numbers and percentages of patients hospitalized were calculated, for any reason and for cystic fibrosis–related reasons. Hospitalization rates also were calculated as numbers of admissions per person-year, the authors said.
Data also were analyzed for two subcohorts: the 86 patients who started using ivacaftor between Feb. 6, 2012, and Feb. 21, 2014, under the initial Food and Drug Administration label; and the 57 patients who initiated use between Feb. 22, 2014, and Dec. 31, 2015, under the expanded FDA label, which included nine additional genetic mutations.
Of the 143 patients who had filled prescriptions for ivacaftor, 63% were aged 18 years or older. The rate of overall inpatient admissions decreased 55%, from 0.57 admissions per person-year in the pre-ivacaftor period to 0.26 admissions per person-year in the post-ivacaftor period, the investigators reported.
The declines in hospital admissions also were similar between the initial label and the expanded FDA label groups, with declines in overall admissions of 59% and 57%, respectively.
Hospital admissions related to cystic fibrosis also decreased significantly, by 78%. Admissions with principal diagnosis codes for cystic fibrosis decreased from 42 in the preprescription period, to 8 after filling the prescription. Rates per person per year decreased by 82% in patients aged 6-17 years and 80% among adults aged 18 years and older. Additionally, patients who filled at least 10 prescriptions during the study period experienced a 68% reduction in inpatient admissions, compared with 45% for those with three to nine prescriptions filled.
Ivacaftor also was associated with 60% lower per-person inpatient spending overall, with a greater proportional reduction in hospital costs for adults (68%) than for children (45%), and an absolute per-person reduction of $10,567, the authors reported.
“Treatments that target the protein defect that causes cystic fibrosis illustrate the promise of precision medicine,” the authors wrote. “To deliver the right care to the right patient, cystic fibrosis care must continue to account for other aspects unique to individuals such as environment, physiology, patients’ preferences, and lifestyle,” they concluded.
Ivacaftor (Kalydeco) is manufactured for Vertex Pharmaceuticals. No disclosures or conflicts of interest were reported.
SOURCE: Feng LB et al. Health Aff. 2018 May 8. doi: 10.1377/hlthaff.2017.1554
FROM HEALTH AFFAIRS
Key clinical point: Ivacaftor significantly reduced hospital admission rates in patients with cystic fibrosis.
Major finding: Overall rate of inpatient admissions dropped by 55% and cystic fibrosis related admissions rates by 78% (P less than .0001).
Study details: A study of 143 patients treated with ivacaftor between February 2012 and February 2015.
Disclosures: No disclosures or conflicts of interest were reported.
Source: Feng LB et al. Health Aff. 2018 May 8. doi: 10.1377/hlthaff.2017.1554.
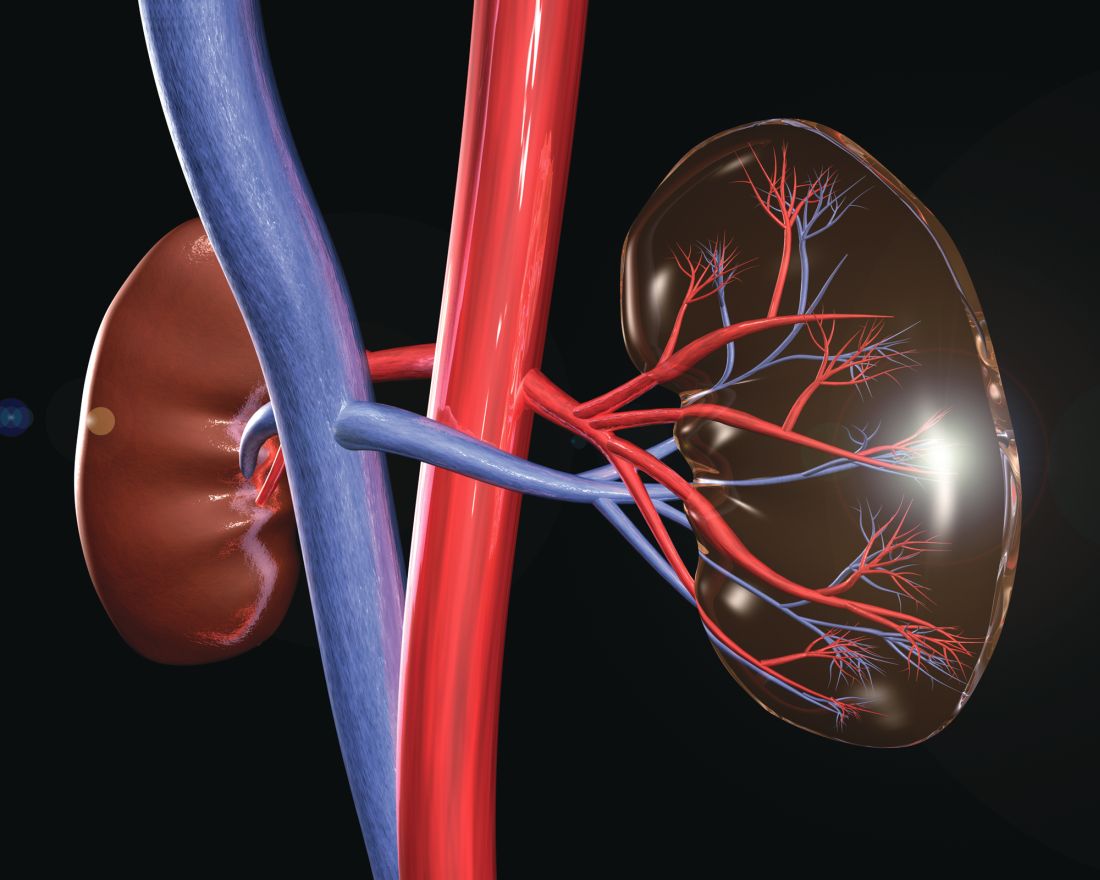
New trial to assess HIV+/HIV+ kidney transplants
The HOPE in Action Multicenter Kidney Study, the first large-scale clinical trial to study kidney transplantations between people with HIV, has begun at clinical centers across the United States, according to an announcement by the National Institutes of Health. The study, sponsored by the National Institute of Allergy and Infectious Diseases and NIH, will assess the safety of HIV-positive donor to HIV-positive recipient kidney transplantation. This form of transplantation was made legal by the passage of the HOPE (HIV Organ Policy Equity) Act, which permits the transplantation of organs from donors with HIV into qualified HIV-positive recipients with end-stage organ failure.
Outcomes to be studied in the multicenter trial will include potential transplant-related and HIV-related complications following surgery, as well as organ rejection, organ failure, and failure of previously effective HIV medications. The study is currently enrolling and is expected to include 360 participants, with an estimated completion date of Aug. 1, 2022.
“The HOPE Act of 2013 opened the door for researchers to explore a potential new source of donor organs for those living with HIV – a population with a significant and growing need for transplants. This study offers a chance to improve the health of those living with HIV, and increase the overall supply of transplantable organs,” said NIAID Director Anthony S. Fauci, MD, in the NIH news release. Transplantation of organs from HIV-positive donors to HIV-negative recipients remains illegal in the United States.
More information about the study can be found at ClinicalTrials.gov using the identifier NCT03500315. A similar trial to examine liver transplantation, the HOPE in Action Multicenter Liver Study, is expected to launch later in 2018.
The HOPE in Action Multicenter Kidney Study, the first large-scale clinical trial to study kidney transplantations between people with HIV, has begun at clinical centers across the United States, according to an announcement by the National Institutes of Health. The study, sponsored by the National Institute of Allergy and Infectious Diseases and NIH, will assess the safety of HIV-positive donor to HIV-positive recipient kidney transplantation. This form of transplantation was made legal by the passage of the HOPE (HIV Organ Policy Equity) Act, which permits the transplantation of organs from donors with HIV into qualified HIV-positive recipients with end-stage organ failure.
Outcomes to be studied in the multicenter trial will include potential transplant-related and HIV-related complications following surgery, as well as organ rejection, organ failure, and failure of previously effective HIV medications. The study is currently enrolling and is expected to include 360 participants, with an estimated completion date of Aug. 1, 2022.
“The HOPE Act of 2013 opened the door for researchers to explore a potential new source of donor organs for those living with HIV – a population with a significant and growing need for transplants. This study offers a chance to improve the health of those living with HIV, and increase the overall supply of transplantable organs,” said NIAID Director Anthony S. Fauci, MD, in the NIH news release. Transplantation of organs from HIV-positive donors to HIV-negative recipients remains illegal in the United States.
More information about the study can be found at ClinicalTrials.gov using the identifier NCT03500315. A similar trial to examine liver transplantation, the HOPE in Action Multicenter Liver Study, is expected to launch later in 2018.
The HOPE in Action Multicenter Kidney Study, the first large-scale clinical trial to study kidney transplantations between people with HIV, has begun at clinical centers across the United States, according to an announcement by the National Institutes of Health. The study, sponsored by the National Institute of Allergy and Infectious Diseases and NIH, will assess the safety of HIV-positive donor to HIV-positive recipient kidney transplantation. This form of transplantation was made legal by the passage of the HOPE (HIV Organ Policy Equity) Act, which permits the transplantation of organs from donors with HIV into qualified HIV-positive recipients with end-stage organ failure.
Outcomes to be studied in the multicenter trial will include potential transplant-related and HIV-related complications following surgery, as well as organ rejection, organ failure, and failure of previously effective HIV medications. The study is currently enrolling and is expected to include 360 participants, with an estimated completion date of Aug. 1, 2022.
“The HOPE Act of 2013 opened the door for researchers to explore a potential new source of donor organs for those living with HIV – a population with a significant and growing need for transplants. This study offers a chance to improve the health of those living with HIV, and increase the overall supply of transplantable organs,” said NIAID Director Anthony S. Fauci, MD, in the NIH news release. Transplantation of organs from HIV-positive donors to HIV-negative recipients remains illegal in the United States.
More information about the study can be found at ClinicalTrials.gov using the identifier NCT03500315. A similar trial to examine liver transplantation, the HOPE in Action Multicenter Liver Study, is expected to launch later in 2018.
In PAH trials, clinical worsening risk rose with time
Current clinical trials evaluating combination therapy for pulmonary artery hypertension (PAH) may be longer than what is needed to demonstrate treatment benefit, results of a recent meta-analysis suggest.
, according to results of the study published in the May issue of the journal Chest®.
The meta-analysis by Dr. Lajoie and her colleagues included 3,801 patients enrolled in one of 15 previously published randomized clinical trials. Of those trials, four were long-term, event driven studies, with a mean duration of 87 weeks, while the remainder were shorter studies with a mean duration of 15 weeks.
For the long-term, event-driven trials, the mean number needed to treat (NNT) was 17.4 at week 16, gradually decreasing to 8.8 at 52 weeks of follow-up, remaining stable after that, according to investigators.
Consistent with that finding, the mean relative risk of clinical worsening was 0.38 at 16 weeks, and similarly, 0.41 at 26 weeks, investigators reported. After that, the relative risk progressively increased to 0.54 at 52 weeks and 0.68 at 104 weeks.
Looking at all trials combined, Dr. Lajoie and her colleagues observed that longer trial duration had a positive correlation with relative risk of clinical worsening (P = .0002).
Pragmatically, these results raise the possibility that PAH combination therapy trials could be shorter in duration. Some recent event-driven studies have lasted up to 6 years, with patients on treatment for about 2 of those years, investigators noted.
“In the context of an orphan disease with limited and competing recruitment for trials and the rapidly changing treatment paradigm in PAH, the optimal duration of future trials should be revisited,” Dr. Lajoie and her colleagues wrote in a discussion of their findings.
They also cautioned that NNT, a measure of how many patient treatments are needed to prevent one additional adverse event, could be “misleading” despite its value as a simple measure of treatment impact.
Likewise, relative risk can be misleading; for example, a treatment reducing event risk from 30% to 20% represents a relative risk reduction of approximately 35%, but so does a treatment reducing event risk from 3% to 2%, the researchers noted.
“Multiple factors, in addition to the efficacy of the therapy and the comparator, may directly influence the NNT and relative risk and should be taken into account in their interpretation,” they said in their report.
Dr. Lajoie had no disclosures related to the study. Her coauthors had disclosures related to Actelion Pharmaceuticals, Bayer, and GlaxoSmithKline, among others.
SOURCE: Lajoie AC et al. Chest. 2017 May;153(5):1142-52.
Key clinical point: A meta-analysis calls into question the need to perform pulmonary arterial hypertension (PAH) trials beyond 6 to 12 months of treatment in the future.
Major finding: The mean number needed to treat was stable at 52 weeks of follow-up and thereafter, while the mean relative risk of clinical worsening progressively increased from approximately 0.38 at week 16 to 0.68 at week 104.
Study details: A systematic review of 3,801 patients enrolled in 15 randomized clinical trials.
Disclosures: The authors reported disclosures related to Actelion Pharmaceuticals, Bayer, and GlaxoSmithKline, among other entities.
Source: Lajoie AC et al. Chest. 2017 May;153(5):1142-52.
Key clinical point: A meta-analysis calls into question the need to perform pulmonary arterial hypertension (PAH) trials beyond 6 to 12 months of treatment in the future.
Major finding: The mean number needed to treat was stable at 52 weeks of follow-up and thereafter, while the mean relative risk of clinical worsening progressively increased from approximately 0.38 at week 16 to 0.68 at week 104.
Study details: A systematic review of 3,801 patients enrolled in 15 randomized clinical trials.
Disclosures: The authors reported disclosures related to Actelion Pharmaceuticals, Bayer, and GlaxoSmithKline, among other entities.
Source: Lajoie AC et al. Chest. 2017 May;153(5):1142-52.
Key clinical point: A meta-analysis calls into question the need to perform pulmonary arterial hypertension (PAH) trials beyond 6 to 12 months of treatment in the future.
Major finding: The mean number needed to treat was stable at 52 weeks of follow-up and thereafter, while the mean relative risk of clinical worsening progressively increased from approximately 0.38 at week 16 to 0.68 at week 104.
Study details: A systematic review of 3,801 patients enrolled in 15 randomized clinical trials.
Disclosures: The authors reported disclosures related to Actelion Pharmaceuticals, Bayer, and GlaxoSmithKline, among other entities.
Source: Lajoie AC et al. Chest. 2017 May;153(5):1142-52.
Current clinical trials evaluating combination therapy for pulmonary artery hypertension (PAH) may be longer than what is needed to demonstrate treatment benefit, results of a recent meta-analysis suggest.
, according to results of the study published in the May issue of the journal Chest®.
The meta-analysis by Dr. Lajoie and her colleagues included 3,801 patients enrolled in one of 15 previously published randomized clinical trials. Of those trials, four were long-term, event driven studies, with a mean duration of 87 weeks, while the remainder were shorter studies with a mean duration of 15 weeks.
For the long-term, event-driven trials, the mean number needed to treat (NNT) was 17.4 at week 16, gradually decreasing to 8.8 at 52 weeks of follow-up, remaining stable after that, according to investigators.
Consistent with that finding, the mean relative risk of clinical worsening was 0.38 at 16 weeks, and similarly, 0.41 at 26 weeks, investigators reported. After that, the relative risk progressively increased to 0.54 at 52 weeks and 0.68 at 104 weeks.
Looking at all trials combined, Dr. Lajoie and her colleagues observed that longer trial duration had a positive correlation with relative risk of clinical worsening (P = .0002).
Pragmatically, these results raise the possibility that PAH combination therapy trials could be shorter in duration. Some recent event-driven studies have lasted up to 6 years, with patients on treatment for about 2 of those years, investigators noted.
“In the context of an orphan disease with limited and competing recruitment for trials and the rapidly changing treatment paradigm in PAH, the optimal duration of future trials should be revisited,” Dr. Lajoie and her colleagues wrote in a discussion of their findings.
They also cautioned that NNT, a measure of how many patient treatments are needed to prevent one additional adverse event, could be “misleading” despite its value as a simple measure of treatment impact.
Likewise, relative risk can be misleading; for example, a treatment reducing event risk from 30% to 20% represents a relative risk reduction of approximately 35%, but so does a treatment reducing event risk from 3% to 2%, the researchers noted.
“Multiple factors, in addition to the efficacy of the therapy and the comparator, may directly influence the NNT and relative risk and should be taken into account in their interpretation,” they said in their report.
Dr. Lajoie had no disclosures related to the study. Her coauthors had disclosures related to Actelion Pharmaceuticals, Bayer, and GlaxoSmithKline, among others.
SOURCE: Lajoie AC et al. Chest. 2017 May;153(5):1142-52.
Current clinical trials evaluating combination therapy for pulmonary artery hypertension (PAH) may be longer than what is needed to demonstrate treatment benefit, results of a recent meta-analysis suggest.
, according to results of the study published in the May issue of the journal Chest®.
The meta-analysis by Dr. Lajoie and her colleagues included 3,801 patients enrolled in one of 15 previously published randomized clinical trials. Of those trials, four were long-term, event driven studies, with a mean duration of 87 weeks, while the remainder were shorter studies with a mean duration of 15 weeks.
For the long-term, event-driven trials, the mean number needed to treat (NNT) was 17.4 at week 16, gradually decreasing to 8.8 at 52 weeks of follow-up, remaining stable after that, according to investigators.
Consistent with that finding, the mean relative risk of clinical worsening was 0.38 at 16 weeks, and similarly, 0.41 at 26 weeks, investigators reported. After that, the relative risk progressively increased to 0.54 at 52 weeks and 0.68 at 104 weeks.
Looking at all trials combined, Dr. Lajoie and her colleagues observed that longer trial duration had a positive correlation with relative risk of clinical worsening (P = .0002).
Pragmatically, these results raise the possibility that PAH combination therapy trials could be shorter in duration. Some recent event-driven studies have lasted up to 6 years, with patients on treatment for about 2 of those years, investigators noted.
“In the context of an orphan disease with limited and competing recruitment for trials and the rapidly changing treatment paradigm in PAH, the optimal duration of future trials should be revisited,” Dr. Lajoie and her colleagues wrote in a discussion of their findings.
They also cautioned that NNT, a measure of how many patient treatments are needed to prevent one additional adverse event, could be “misleading” despite its value as a simple measure of treatment impact.
Likewise, relative risk can be misleading; for example, a treatment reducing event risk from 30% to 20% represents a relative risk reduction of approximately 35%, but so does a treatment reducing event risk from 3% to 2%, the researchers noted.
“Multiple factors, in addition to the efficacy of the therapy and the comparator, may directly influence the NNT and relative risk and should be taken into account in their interpretation,” they said in their report.
Dr. Lajoie had no disclosures related to the study. Her coauthors had disclosures related to Actelion Pharmaceuticals, Bayer, and GlaxoSmithKline, among others.
SOURCE: Lajoie AC et al. Chest. 2017 May;153(5):1142-52.
FROM CHEST®
When and how to suspect asthma misdiagnosis
NEW ORLEANS – Kyle I. Happel, MD, said at the annual meeting of the American College of Physicians.
“Asthma is a disease whose symptoms are caused by variable airflow obstruction. It varies throughout the day, usually, and certainly by the week or by the month. I want you to think about the variability of a patient’s disease symptoms in forming your index of suspicion for this disease,” urged Dr. Happel, of the section of pulmonary, critical care, and allergy/immunology at Louisiana State University Medical Center in New Orleans.
These phenomena occur often. In a Canadian multicenter study of more than 700 patients with a history of physician-diagnosed asthma within the past 5 years, current asthma was ruled out in fully 33% of them on the basis of no deterioration of asthma symptoms, no evidence of reversible airway obstruction, and no bronchial hyperresponsiveness after all asthma drugs were tapered off (JAMA. 2017 Jan 17;317[3]:269-79).
Wheezing is the most specific symptom of asthma, although it is not, in fact, terribly specific. In descending order, the next most specific symptoms are breathlessness, chest tightness, and cough.
The top seven diseases that mimic asthma symptoms are chronic obstructive pulmonary disease, rhinosinusitis, heart failure with preserved or reduced ejection fraction, gastroesophageal reflux disease, angina, anxiety, and vocal cord dysfunction syndrome.
Strike two for an asthma diagnosis is a patient’s report that albuterol doesn’t improve the symptoms. That definitely raises questions about the diagnosis.
“Most asthmatics get symptomatic relief from their disease,” Dr. Happel observed.
And, if there is no indication in the patient’s chart that the asthma diagnosis was based upon demonstration of airflow obstruction on spirometry, the diagnosis is thrown further into doubt. In the recent Canadian study, patients who didn’t undergo pulmonary function testing (PFT) to establish airflow limitation at their time of diagnosis were significantly less likely to have current asthma.
“I would strongly suggest everyone with the diagnosis of asthma get spirometry with bronchodilator testing,” Dr. Happel said. “Good-quality PFTs are critical in forming a solid diagnosis of asthma.”
In a patient who has symptoms consistent with asthma, a 200-cc and 12% or more improvement in forced expiratory volume in 1 second (FEV1) in response to bronchodilator challenge is supportive of the diagnosis. However, absence of reversible airway obstruction doesn’t exclude the possibility of asthma.
In the setting of low to-moderate clinical suspicion of asthma plus no demonstrable obstruction on spirometry, Dr. Happel recommends moving on to bronchial hyperreactivity testing via a methacholine challenge.
“The beauty of a methacholine challenge is that is has a high negative predictive value to help exclude the diagnosis of asthma, particularly in people who are having symptoms suggestive of asthma,” Dr. Happel explained. “If it takes more than 8 mg/mL of methacholine to elicit a 20% or greater decrease in FEV1, it’s probably something else. It’s not a particularly specific test, though; you can get false positives from a methacholine challenge.”
NEW ORLEANS – Kyle I. Happel, MD, said at the annual meeting of the American College of Physicians.
“Asthma is a disease whose symptoms are caused by variable airflow obstruction. It varies throughout the day, usually, and certainly by the week or by the month. I want you to think about the variability of a patient’s disease symptoms in forming your index of suspicion for this disease,” urged Dr. Happel, of the section of pulmonary, critical care, and allergy/immunology at Louisiana State University Medical Center in New Orleans.
These phenomena occur often. In a Canadian multicenter study of more than 700 patients with a history of physician-diagnosed asthma within the past 5 years, current asthma was ruled out in fully 33% of them on the basis of no deterioration of asthma symptoms, no evidence of reversible airway obstruction, and no bronchial hyperresponsiveness after all asthma drugs were tapered off (JAMA. 2017 Jan 17;317[3]:269-79).
Wheezing is the most specific symptom of asthma, although it is not, in fact, terribly specific. In descending order, the next most specific symptoms are breathlessness, chest tightness, and cough.
The top seven diseases that mimic asthma symptoms are chronic obstructive pulmonary disease, rhinosinusitis, heart failure with preserved or reduced ejection fraction, gastroesophageal reflux disease, angina, anxiety, and vocal cord dysfunction syndrome.
Strike two for an asthma diagnosis is a patient’s report that albuterol doesn’t improve the symptoms. That definitely raises questions about the diagnosis.
“Most asthmatics get symptomatic relief from their disease,” Dr. Happel observed.
And, if there is no indication in the patient’s chart that the asthma diagnosis was based upon demonstration of airflow obstruction on spirometry, the diagnosis is thrown further into doubt. In the recent Canadian study, patients who didn’t undergo pulmonary function testing (PFT) to establish airflow limitation at their time of diagnosis were significantly less likely to have current asthma.
“I would strongly suggest everyone with the diagnosis of asthma get spirometry with bronchodilator testing,” Dr. Happel said. “Good-quality PFTs are critical in forming a solid diagnosis of asthma.”
In a patient who has symptoms consistent with asthma, a 200-cc and 12% or more improvement in forced expiratory volume in 1 second (FEV1) in response to bronchodilator challenge is supportive of the diagnosis. However, absence of reversible airway obstruction doesn’t exclude the possibility of asthma.
In the setting of low to-moderate clinical suspicion of asthma plus no demonstrable obstruction on spirometry, Dr. Happel recommends moving on to bronchial hyperreactivity testing via a methacholine challenge.
“The beauty of a methacholine challenge is that is has a high negative predictive value to help exclude the diagnosis of asthma, particularly in people who are having symptoms suggestive of asthma,” Dr. Happel explained. “If it takes more than 8 mg/mL of methacholine to elicit a 20% or greater decrease in FEV1, it’s probably something else. It’s not a particularly specific test, though; you can get false positives from a methacholine challenge.”
NEW ORLEANS – Kyle I. Happel, MD, said at the annual meeting of the American College of Physicians.
“Asthma is a disease whose symptoms are caused by variable airflow obstruction. It varies throughout the day, usually, and certainly by the week or by the month. I want you to think about the variability of a patient’s disease symptoms in forming your index of suspicion for this disease,” urged Dr. Happel, of the section of pulmonary, critical care, and allergy/immunology at Louisiana State University Medical Center in New Orleans.
These phenomena occur often. In a Canadian multicenter study of more than 700 patients with a history of physician-diagnosed asthma within the past 5 years, current asthma was ruled out in fully 33% of them on the basis of no deterioration of asthma symptoms, no evidence of reversible airway obstruction, and no bronchial hyperresponsiveness after all asthma drugs were tapered off (JAMA. 2017 Jan 17;317[3]:269-79).
Wheezing is the most specific symptom of asthma, although it is not, in fact, terribly specific. In descending order, the next most specific symptoms are breathlessness, chest tightness, and cough.
The top seven diseases that mimic asthma symptoms are chronic obstructive pulmonary disease, rhinosinusitis, heart failure with preserved or reduced ejection fraction, gastroesophageal reflux disease, angina, anxiety, and vocal cord dysfunction syndrome.
Strike two for an asthma diagnosis is a patient’s report that albuterol doesn’t improve the symptoms. That definitely raises questions about the diagnosis.
“Most asthmatics get symptomatic relief from their disease,” Dr. Happel observed.
And, if there is no indication in the patient’s chart that the asthma diagnosis was based upon demonstration of airflow obstruction on spirometry, the diagnosis is thrown further into doubt. In the recent Canadian study, patients who didn’t undergo pulmonary function testing (PFT) to establish airflow limitation at their time of diagnosis were significantly less likely to have current asthma.
“I would strongly suggest everyone with the diagnosis of asthma get spirometry with bronchodilator testing,” Dr. Happel said. “Good-quality PFTs are critical in forming a solid diagnosis of asthma.”
In a patient who has symptoms consistent with asthma, a 200-cc and 12% or more improvement in forced expiratory volume in 1 second (FEV1) in response to bronchodilator challenge is supportive of the diagnosis. However, absence of reversible airway obstruction doesn’t exclude the possibility of asthma.
In the setting of low to-moderate clinical suspicion of asthma plus no demonstrable obstruction on spirometry, Dr. Happel recommends moving on to bronchial hyperreactivity testing via a methacholine challenge.
“The beauty of a methacholine challenge is that is has a high negative predictive value to help exclude the diagnosis of asthma, particularly in people who are having symptoms suggestive of asthma,” Dr. Happel explained. “If it takes more than 8 mg/mL of methacholine to elicit a 20% or greater decrease in FEV1, it’s probably something else. It’s not a particularly specific test, though; you can get false positives from a methacholine challenge.”
REPORTING FROM ACP INTERNAL MEDICINE