User login
Inhibitor could overcome TKI resistance in Ph+ B-ALL

Results of preclinical research indicate that combining 2 kinase inhibitors may be a promising treatment strategy for Philadelphia chromosome-positive B-cell acute lymphoblastic leukemia (Ph+ B-ALL).
Researchers found that combining a tyrosine kinase inhibitor (TKI) and an inhibitor of focal adhesion kinase (FAK) was “remarkably effective” against Ph+ B-ALL in vitro and in vivo.
The TKI dasatinib and the FAK inhibitor VS-4718 decreased leukemic cell survival and adhesion, inhibited tumor growth, and prolonged survival in mouse models of Ph+ B-ALL.
Charles Mullighan, MBBS, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues conducted this research and reported their results in JCI Insight.
The researchers noted that patients with Ph+ ALL have shown resistance to TKI therapy, and this resistance has been tied to alterations in IKZF1.
As FAK expression is elevated in IKZF1-mutated leukemias, the team speculated that adding a FAK inhibitor to TKI therapy might lead to better results.
First, the researchers set out to confirm that FAK is overexpressed in Ph+ B-ALL. Their experiments revealed upregulation of the FAK pathway in Ph+ B-ALL cells, with further overexpression of FAK in IKZF1-mutated Ph+ B-ALL cells.
When they inhibited FAK with VS-4718, the team observed decreases in the survival, clonogenicity, and adhesion of IKZF1-mutated Ph+ B-ALL cells from both mice and humans.
Next, the researchers found that VS-4718 synergizes with the TKI dasatinib in vitro and in vivo.
In in vitro experiments with both mouse and human Ph+ B-ALL cells, the combination decreased cell survival and adhesion and inhibited downstream targets of FAK.
In mouse models of Ph+ B-ALL, VS-4718 proved ineffective when given alone.
However, the researchers said the combination of VS-4718 and dasatinib “dramatically” decreased leukemic burden and extended the lives of mice.
In fact, 1 long-term survivor achieved a complete remission that endured after treatment was stopped.
The researchers said these results suggest that targeting FAK with VS-4718 can overcome the deleterious effects of FAK overexpression in Ph+ B-ALL, potentiating responsiveness to TKIs. ![]()

Results of preclinical research indicate that combining 2 kinase inhibitors may be a promising treatment strategy for Philadelphia chromosome-positive B-cell acute lymphoblastic leukemia (Ph+ B-ALL).
Researchers found that combining a tyrosine kinase inhibitor (TKI) and an inhibitor of focal adhesion kinase (FAK) was “remarkably effective” against Ph+ B-ALL in vitro and in vivo.
The TKI dasatinib and the FAK inhibitor VS-4718 decreased leukemic cell survival and adhesion, inhibited tumor growth, and prolonged survival in mouse models of Ph+ B-ALL.
Charles Mullighan, MBBS, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues conducted this research and reported their results in JCI Insight.
The researchers noted that patients with Ph+ ALL have shown resistance to TKI therapy, and this resistance has been tied to alterations in IKZF1.
As FAK expression is elevated in IKZF1-mutated leukemias, the team speculated that adding a FAK inhibitor to TKI therapy might lead to better results.
First, the researchers set out to confirm that FAK is overexpressed in Ph+ B-ALL. Their experiments revealed upregulation of the FAK pathway in Ph+ B-ALL cells, with further overexpression of FAK in IKZF1-mutated Ph+ B-ALL cells.
When they inhibited FAK with VS-4718, the team observed decreases in the survival, clonogenicity, and adhesion of IKZF1-mutated Ph+ B-ALL cells from both mice and humans.
Next, the researchers found that VS-4718 synergizes with the TKI dasatinib in vitro and in vivo.
In in vitro experiments with both mouse and human Ph+ B-ALL cells, the combination decreased cell survival and adhesion and inhibited downstream targets of FAK.
In mouse models of Ph+ B-ALL, VS-4718 proved ineffective when given alone.
However, the researchers said the combination of VS-4718 and dasatinib “dramatically” decreased leukemic burden and extended the lives of mice.
In fact, 1 long-term survivor achieved a complete remission that endured after treatment was stopped.
The researchers said these results suggest that targeting FAK with VS-4718 can overcome the deleterious effects of FAK overexpression in Ph+ B-ALL, potentiating responsiveness to TKIs. ![]()

Results of preclinical research indicate that combining 2 kinase inhibitors may be a promising treatment strategy for Philadelphia chromosome-positive B-cell acute lymphoblastic leukemia (Ph+ B-ALL).
Researchers found that combining a tyrosine kinase inhibitor (TKI) and an inhibitor of focal adhesion kinase (FAK) was “remarkably effective” against Ph+ B-ALL in vitro and in vivo.
The TKI dasatinib and the FAK inhibitor VS-4718 decreased leukemic cell survival and adhesion, inhibited tumor growth, and prolonged survival in mouse models of Ph+ B-ALL.
Charles Mullighan, MBBS, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues conducted this research and reported their results in JCI Insight.
The researchers noted that patients with Ph+ ALL have shown resistance to TKI therapy, and this resistance has been tied to alterations in IKZF1.
As FAK expression is elevated in IKZF1-mutated leukemias, the team speculated that adding a FAK inhibitor to TKI therapy might lead to better results.
First, the researchers set out to confirm that FAK is overexpressed in Ph+ B-ALL. Their experiments revealed upregulation of the FAK pathway in Ph+ B-ALL cells, with further overexpression of FAK in IKZF1-mutated Ph+ B-ALL cells.
When they inhibited FAK with VS-4718, the team observed decreases in the survival, clonogenicity, and adhesion of IKZF1-mutated Ph+ B-ALL cells from both mice and humans.
Next, the researchers found that VS-4718 synergizes with the TKI dasatinib in vitro and in vivo.
In in vitro experiments with both mouse and human Ph+ B-ALL cells, the combination decreased cell survival and adhesion and inhibited downstream targets of FAK.
In mouse models of Ph+ B-ALL, VS-4718 proved ineffective when given alone.
However, the researchers said the combination of VS-4718 and dasatinib “dramatically” decreased leukemic burden and extended the lives of mice.
In fact, 1 long-term survivor achieved a complete remission that endured after treatment was stopped.
The researchers said these results suggest that targeting FAK with VS-4718 can overcome the deleterious effects of FAK overexpression in Ph+ B-ALL, potentiating responsiveness to TKIs. ![]()
Postoperative Clostridium Difficile Infection Associated with Number of Antibiotics, Surgical Procedure Complexity
Clinical question: What are the factors that increase risk of Clostridium difficile infection (CDI) in postoperative patients?
Background: CDI has become an important infectious etiology for morbidity, lengthy and costly hospital admissions, and mortality. This study focused on the risks for postoperative patients to be infected with C. diff. Awareness of the risk factors for CDI allows for processes to be implemented that can decrease the rate of infection.
Study design: Retrospective, observational study.
Setting: Multiple Veterans Health Administration surgery programs.
Synopsis: The study investigated 468,386 surgical procedures in 134 surgical programs in 12 subspecialties over a four-year period. Overall, the postoperative CDI rate was 0.4% per year. Rates were higher in emergency or complex procedures, older patients, patients with longer preoperative hospital stays, and those who received three or more classes of antibiotics. CDI in postoperative patients was associated with five times higher risk of mortality, a 12 times higher risk of morbidity, and longer hospital stays (17.9 versus 3.6 days) compared with those without CDI. Further studies with a larger population size will confirm the findings of this study.
The study was conducted on middle-aged to elderly male veterans, and it can only be assumed that these results will translate to other populations. Nevertheless, CDI can lead to significant morbidity and mortality, and the study reinforces the importance of infection control and prevention to reduce CDI incidence and disease severity.
Bottom line: Postoperative CDI is significantly associated with the number of postoperative antibiotics, surgical procedure complexity, preoperative length of stay, and patient comorbidities.
Citation: Li X, Wilson M, Nylander W, Smith T, Lynn M, Gunnar W. Analysis of morbidity and mortality outcomes in postoperative Clostridium difficile infection in the Veterans Health Administration. JAMA Surg. 2015;25:1-9.
Clinical question: What are the factors that increase risk of Clostridium difficile infection (CDI) in postoperative patients?
Background: CDI has become an important infectious etiology for morbidity, lengthy and costly hospital admissions, and mortality. This study focused on the risks for postoperative patients to be infected with C. diff. Awareness of the risk factors for CDI allows for processes to be implemented that can decrease the rate of infection.
Study design: Retrospective, observational study.
Setting: Multiple Veterans Health Administration surgery programs.
Synopsis: The study investigated 468,386 surgical procedures in 134 surgical programs in 12 subspecialties over a four-year period. Overall, the postoperative CDI rate was 0.4% per year. Rates were higher in emergency or complex procedures, older patients, patients with longer preoperative hospital stays, and those who received three or more classes of antibiotics. CDI in postoperative patients was associated with five times higher risk of mortality, a 12 times higher risk of morbidity, and longer hospital stays (17.9 versus 3.6 days) compared with those without CDI. Further studies with a larger population size will confirm the findings of this study.
The study was conducted on middle-aged to elderly male veterans, and it can only be assumed that these results will translate to other populations. Nevertheless, CDI can lead to significant morbidity and mortality, and the study reinforces the importance of infection control and prevention to reduce CDI incidence and disease severity.
Bottom line: Postoperative CDI is significantly associated with the number of postoperative antibiotics, surgical procedure complexity, preoperative length of stay, and patient comorbidities.
Citation: Li X, Wilson M, Nylander W, Smith T, Lynn M, Gunnar W. Analysis of morbidity and mortality outcomes in postoperative Clostridium difficile infection in the Veterans Health Administration. JAMA Surg. 2015;25:1-9.
Clinical question: What are the factors that increase risk of Clostridium difficile infection (CDI) in postoperative patients?
Background: CDI has become an important infectious etiology for morbidity, lengthy and costly hospital admissions, and mortality. This study focused on the risks for postoperative patients to be infected with C. diff. Awareness of the risk factors for CDI allows for processes to be implemented that can decrease the rate of infection.
Study design: Retrospective, observational study.
Setting: Multiple Veterans Health Administration surgery programs.
Synopsis: The study investigated 468,386 surgical procedures in 134 surgical programs in 12 subspecialties over a four-year period. Overall, the postoperative CDI rate was 0.4% per year. Rates were higher in emergency or complex procedures, older patients, patients with longer preoperative hospital stays, and those who received three or more classes of antibiotics. CDI in postoperative patients was associated with five times higher risk of mortality, a 12 times higher risk of morbidity, and longer hospital stays (17.9 versus 3.6 days) compared with those without CDI. Further studies with a larger population size will confirm the findings of this study.
The study was conducted on middle-aged to elderly male veterans, and it can only be assumed that these results will translate to other populations. Nevertheless, CDI can lead to significant morbidity and mortality, and the study reinforces the importance of infection control and prevention to reduce CDI incidence and disease severity.
Bottom line: Postoperative CDI is significantly associated with the number of postoperative antibiotics, surgical procedure complexity, preoperative length of stay, and patient comorbidities.
Citation: Li X, Wilson M, Nylander W, Smith T, Lynn M, Gunnar W. Analysis of morbidity and mortality outcomes in postoperative Clostridium difficile infection in the Veterans Health Administration. JAMA Surg. 2015;25:1-9.
Most Postoperative Readmissions Due to Patient Factors
Clinical question: What is the etiology of 30-day readmissions in postoperative patients?
Background: As the focus of healthcare changes to a quality-focused model, readmissions impact physicians, reimbursements, and patients. Understanding the cause of readmissions becomes essential to preventing them. The etiology of 30-day readmissions in postoperative patients has not specifically been studied.
Study design: Retrospective analysis.
Setting: Academic tertiary-care center.
Synopsis: Using administrative claims data, an analysis of 22,559 patients who underwent a major surgical procedure between 2009 and 2013 was performed. A total of 56 surgeons within eight surgical subspecialties were analyzed, showing that variation in 30-day readmissions was largely due to patient-specific factors (82.8%) while only a minority were attributable to surgical subspecialty (14.5%) and individual surgeon levels (2.8%). Factors associated with readmission included race/ethnicity, comorbidities, postoperative complications, and extended length of stay.
Further studies within this area will need to be conducted focusing on one specific subspecialty and one surgeon to exclude confounding factors. Additional meta-analysis can then compare these individual studies. A larger population and multiple care centers will also further validate the findings. Understanding the cause of the readmissions in postoperative patients can prevent further readmissions, improve quality of care, and decrease healthcare costs. If patient factors are identified as a major cause for readmissions in postoperative patients, changes in preoperative management may need to be made.
Bottom line: Postoperative readmissions are more dependent on patient factors than surgeon- or surgical subspecialty-specific factors.
Citation: Gani F, Lucas DJ, Kim Y, Schneider EB, Pawlik TM. Understanding variation in 30-day surgical readmission in the era of accountable care: effect of the patient, surgeon, and surgical subspecialties. JAMA Surg. 2015;150(11):1042-1049.
Clinical question: What is the etiology of 30-day readmissions in postoperative patients?
Background: As the focus of healthcare changes to a quality-focused model, readmissions impact physicians, reimbursements, and patients. Understanding the cause of readmissions becomes essential to preventing them. The etiology of 30-day readmissions in postoperative patients has not specifically been studied.
Study design: Retrospective analysis.
Setting: Academic tertiary-care center.
Synopsis: Using administrative claims data, an analysis of 22,559 patients who underwent a major surgical procedure between 2009 and 2013 was performed. A total of 56 surgeons within eight surgical subspecialties were analyzed, showing that variation in 30-day readmissions was largely due to patient-specific factors (82.8%) while only a minority were attributable to surgical subspecialty (14.5%) and individual surgeon levels (2.8%). Factors associated with readmission included race/ethnicity, comorbidities, postoperative complications, and extended length of stay.
Further studies within this area will need to be conducted focusing on one specific subspecialty and one surgeon to exclude confounding factors. Additional meta-analysis can then compare these individual studies. A larger population and multiple care centers will also further validate the findings. Understanding the cause of the readmissions in postoperative patients can prevent further readmissions, improve quality of care, and decrease healthcare costs. If patient factors are identified as a major cause for readmissions in postoperative patients, changes in preoperative management may need to be made.
Bottom line: Postoperative readmissions are more dependent on patient factors than surgeon- or surgical subspecialty-specific factors.
Citation: Gani F, Lucas DJ, Kim Y, Schneider EB, Pawlik TM. Understanding variation in 30-day surgical readmission in the era of accountable care: effect of the patient, surgeon, and surgical subspecialties. JAMA Surg. 2015;150(11):1042-1049.
Clinical question: What is the etiology of 30-day readmissions in postoperative patients?
Background: As the focus of healthcare changes to a quality-focused model, readmissions impact physicians, reimbursements, and patients. Understanding the cause of readmissions becomes essential to preventing them. The etiology of 30-day readmissions in postoperative patients has not specifically been studied.
Study design: Retrospective analysis.
Setting: Academic tertiary-care center.
Synopsis: Using administrative claims data, an analysis of 22,559 patients who underwent a major surgical procedure between 2009 and 2013 was performed. A total of 56 surgeons within eight surgical subspecialties were analyzed, showing that variation in 30-day readmissions was largely due to patient-specific factors (82.8%) while only a minority were attributable to surgical subspecialty (14.5%) and individual surgeon levels (2.8%). Factors associated with readmission included race/ethnicity, comorbidities, postoperative complications, and extended length of stay.
Further studies within this area will need to be conducted focusing on one specific subspecialty and one surgeon to exclude confounding factors. Additional meta-analysis can then compare these individual studies. A larger population and multiple care centers will also further validate the findings. Understanding the cause of the readmissions in postoperative patients can prevent further readmissions, improve quality of care, and decrease healthcare costs. If patient factors are identified as a major cause for readmissions in postoperative patients, changes in preoperative management may need to be made.
Bottom line: Postoperative readmissions are more dependent on patient factors than surgeon- or surgical subspecialty-specific factors.
Citation: Gani F, Lucas DJ, Kim Y, Schneider EB, Pawlik TM. Understanding variation in 30-day surgical readmission in the era of accountable care: effect of the patient, surgeon, and surgical subspecialties. JAMA Surg. 2015;150(11):1042-1049.
U.S. Hospitals Should Prepare for "ransomeware" Attacks by Cyber Criminals
(Reuters) - U.S. hospitals should brace for a surge in "ransomware" attacks by cyber criminals who infect and shut down computer networks, then demand payment in return for unlocking them, a non-profit healthcare group warned on Friday.
The Health Information Trust Alliance conducted a study of some 30 mid-sized U.S. hospitals late last year and found that 52 percent of them were infected with malicious software, HITRUST Chief Executive Daniel Nutkis told Reuters.
The most common type of malware was ransomware, Nutkis said, which was present in 35 percent of the hospitals included in the study of network traffic conducted by security software maker Trend Micro Inc.
Ransomware is malicious software that locks up data in computers and leaves messages demanding payment to recover the data. Last month, Hollywood Presbyterian Hospital in Los Angeles paid a ransom of $17,000 to regain access to its systems.
This week, an attack on MedStar Health forced the largest healthcare provider in Washington, D.C., to shut down much of its computer network. The Baltimore Sun reported a ransom of $18,500 was sought. MedStar declined to comment.
HITRUST said it expects such attacks to become more frequent because ransomware has turned into a profitable business for cyber criminals.
The results of the study, which HITRUST has yet to share with the public, demonstrate that hackers have moved away from focusing on stealing patient data, Nutkis said.
"If stuff isn't working, they move on. If stuff is working, they keep doing it," said Nutkis. "Organizations that are paying have considered their options, and unfortunately they don't have a lot of options."
Extortion has become more popular with cyber criminals because it is seen as a way to generate fast money, said Larry Whiteside, a healthcare expert with cyber security firm Optiv.
Stealing healthcare data is far more labour intensive, requiring attackers to keep their presence in a victim's network undetected for months as they steal data, then they need to find buyers, he added.
"With ransomware I'm going to get paid immediately," Whiteside said.
Frisco, Texas-based HITRUST's board includes executives from Anthem, Health Care Services, Humana, UnitedHealth and Walgreens.
(Reuters) - U.S. hospitals should brace for a surge in "ransomware" attacks by cyber criminals who infect and shut down computer networks, then demand payment in return for unlocking them, a non-profit healthcare group warned on Friday.
The Health Information Trust Alliance conducted a study of some 30 mid-sized U.S. hospitals late last year and found that 52 percent of them were infected with malicious software, HITRUST Chief Executive Daniel Nutkis told Reuters.
The most common type of malware was ransomware, Nutkis said, which was present in 35 percent of the hospitals included in the study of network traffic conducted by security software maker Trend Micro Inc.
Ransomware is malicious software that locks up data in computers and leaves messages demanding payment to recover the data. Last month, Hollywood Presbyterian Hospital in Los Angeles paid a ransom of $17,000 to regain access to its systems.
This week, an attack on MedStar Health forced the largest healthcare provider in Washington, D.C., to shut down much of its computer network. The Baltimore Sun reported a ransom of $18,500 was sought. MedStar declined to comment.
HITRUST said it expects such attacks to become more frequent because ransomware has turned into a profitable business for cyber criminals.
The results of the study, which HITRUST has yet to share with the public, demonstrate that hackers have moved away from focusing on stealing patient data, Nutkis said.
"If stuff isn't working, they move on. If stuff is working, they keep doing it," said Nutkis. "Organizations that are paying have considered their options, and unfortunately they don't have a lot of options."
Extortion has become more popular with cyber criminals because it is seen as a way to generate fast money, said Larry Whiteside, a healthcare expert with cyber security firm Optiv.
Stealing healthcare data is far more labour intensive, requiring attackers to keep their presence in a victim's network undetected for months as they steal data, then they need to find buyers, he added.
"With ransomware I'm going to get paid immediately," Whiteside said.
Frisco, Texas-based HITRUST's board includes executives from Anthem, Health Care Services, Humana, UnitedHealth and Walgreens.
(Reuters) - U.S. hospitals should brace for a surge in "ransomware" attacks by cyber criminals who infect and shut down computer networks, then demand payment in return for unlocking them, a non-profit healthcare group warned on Friday.
The Health Information Trust Alliance conducted a study of some 30 mid-sized U.S. hospitals late last year and found that 52 percent of them were infected with malicious software, HITRUST Chief Executive Daniel Nutkis told Reuters.
The most common type of malware was ransomware, Nutkis said, which was present in 35 percent of the hospitals included in the study of network traffic conducted by security software maker Trend Micro Inc.
Ransomware is malicious software that locks up data in computers and leaves messages demanding payment to recover the data. Last month, Hollywood Presbyterian Hospital in Los Angeles paid a ransom of $17,000 to regain access to its systems.
This week, an attack on MedStar Health forced the largest healthcare provider in Washington, D.C., to shut down much of its computer network. The Baltimore Sun reported a ransom of $18,500 was sought. MedStar declined to comment.
HITRUST said it expects such attacks to become more frequent because ransomware has turned into a profitable business for cyber criminals.
The results of the study, which HITRUST has yet to share with the public, demonstrate that hackers have moved away from focusing on stealing patient data, Nutkis said.
"If stuff isn't working, they move on. If stuff is working, they keep doing it," said Nutkis. "Organizations that are paying have considered their options, and unfortunately they don't have a lot of options."
Extortion has become more popular with cyber criminals because it is seen as a way to generate fast money, said Larry Whiteside, a healthcare expert with cyber security firm Optiv.
Stealing healthcare data is far more labour intensive, requiring attackers to keep their presence in a victim's network undetected for months as they steal data, then they need to find buyers, he added.
"With ransomware I'm going to get paid immediately," Whiteside said.
Frisco, Texas-based HITRUST's board includes executives from Anthem, Health Care Services, Humana, UnitedHealth and Walgreens.
Slowing the progression of sickle cell disease
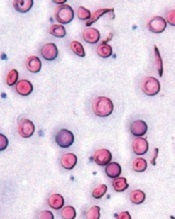
Image courtesy of the
University of Michigan
Activating the antioxidant regulator Nrf2 may slow the progression of sickle cell disease (SCD), according to preclinical research published in JCI Insight.
Investigators found the severity of hemolytic anemia, vascular inflammation, and lung injury increased with age in mice with SCD.
However, activating Nrf2 in young animals had a prophylactic effect, reducing the severity of these adverse effects and improving survival.
To uncover these findings, Solomon Ofori-Acquah, PhD, of the University of Pittsburgh in Pennsylvania, and his colleagues conducted a 10-month longitudinal observational study of mice with SCD.
The team found that, in mice with homozygous SCD (SS), there was a link between intravascular hemolysis, vascular inflammation, lung injury, and early death.
Mice as young as 2 months showed exacerbation of intravascular hemolysis. And additional investigation linked worsening intravascular hemolysis and oxidative stress to the release of VE-cadherin and progressive lung damage in aging SS mice.
The investigators knew that Nrf2 regulates the expression of genes that protect against the effects of intravascular hemolysis. So they decided to see if activating Nrf2 in young mice with SCD would slow the disease progression that occurs with age.
The team took SS mice that were about a month old and randomized them to receive 3H-1, 2-dithiole-3-thione (D3T) or a DMSO vehicle for 3 months or longer.
Treatment with D3T stabilized the concentration of hemoglobin, increased white blood cell counts, increased reticulocyte counts (though not significantly), kept HO-1 levels stable, increased levels of NQO1 and ferritin, and impeded the progression of endothelial dysfunction.
The investigators also looked at the role of Nrf2 in nonhematopoietic tissues and were surprised to find that Nrf2 deficiency in nonhematopoietic tissues exacerbated anemia and caused premature pulmonary edema in mice with SCD.
The team said this suggests a dominant protective role for nonhematopoietic Nrf2 against tissue damage in both erythroid and nonerythroid tissues in SCD.
And, when taken together, the results of this research indicate that activating Nrf2 can impede the onset of the severe adult phenotype of SCD in mice. ![]()
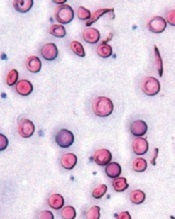
Image courtesy of the
University of Michigan
Activating the antioxidant regulator Nrf2 may slow the progression of sickle cell disease (SCD), according to preclinical research published in JCI Insight.
Investigators found the severity of hemolytic anemia, vascular inflammation, and lung injury increased with age in mice with SCD.
However, activating Nrf2 in young animals had a prophylactic effect, reducing the severity of these adverse effects and improving survival.
To uncover these findings, Solomon Ofori-Acquah, PhD, of the University of Pittsburgh in Pennsylvania, and his colleagues conducted a 10-month longitudinal observational study of mice with SCD.
The team found that, in mice with homozygous SCD (SS), there was a link between intravascular hemolysis, vascular inflammation, lung injury, and early death.
Mice as young as 2 months showed exacerbation of intravascular hemolysis. And additional investigation linked worsening intravascular hemolysis and oxidative stress to the release of VE-cadherin and progressive lung damage in aging SS mice.
The investigators knew that Nrf2 regulates the expression of genes that protect against the effects of intravascular hemolysis. So they decided to see if activating Nrf2 in young mice with SCD would slow the disease progression that occurs with age.
The team took SS mice that were about a month old and randomized them to receive 3H-1, 2-dithiole-3-thione (D3T) or a DMSO vehicle for 3 months or longer.
Treatment with D3T stabilized the concentration of hemoglobin, increased white blood cell counts, increased reticulocyte counts (though not significantly), kept HO-1 levels stable, increased levels of NQO1 and ferritin, and impeded the progression of endothelial dysfunction.
The investigators also looked at the role of Nrf2 in nonhematopoietic tissues and were surprised to find that Nrf2 deficiency in nonhematopoietic tissues exacerbated anemia and caused premature pulmonary edema in mice with SCD.
The team said this suggests a dominant protective role for nonhematopoietic Nrf2 against tissue damage in both erythroid and nonerythroid tissues in SCD.
And, when taken together, the results of this research indicate that activating Nrf2 can impede the onset of the severe adult phenotype of SCD in mice. ![]()
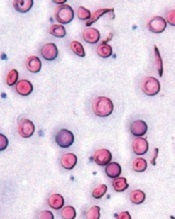
Image courtesy of the
University of Michigan
Activating the antioxidant regulator Nrf2 may slow the progression of sickle cell disease (SCD), according to preclinical research published in JCI Insight.
Investigators found the severity of hemolytic anemia, vascular inflammation, and lung injury increased with age in mice with SCD.
However, activating Nrf2 in young animals had a prophylactic effect, reducing the severity of these adverse effects and improving survival.
To uncover these findings, Solomon Ofori-Acquah, PhD, of the University of Pittsburgh in Pennsylvania, and his colleagues conducted a 10-month longitudinal observational study of mice with SCD.
The team found that, in mice with homozygous SCD (SS), there was a link between intravascular hemolysis, vascular inflammation, lung injury, and early death.
Mice as young as 2 months showed exacerbation of intravascular hemolysis. And additional investigation linked worsening intravascular hemolysis and oxidative stress to the release of VE-cadherin and progressive lung damage in aging SS mice.
The investigators knew that Nrf2 regulates the expression of genes that protect against the effects of intravascular hemolysis. So they decided to see if activating Nrf2 in young mice with SCD would slow the disease progression that occurs with age.
The team took SS mice that were about a month old and randomized them to receive 3H-1, 2-dithiole-3-thione (D3T) or a DMSO vehicle for 3 months or longer.
Treatment with D3T stabilized the concentration of hemoglobin, increased white blood cell counts, increased reticulocyte counts (though not significantly), kept HO-1 levels stable, increased levels of NQO1 and ferritin, and impeded the progression of endothelial dysfunction.
The investigators also looked at the role of Nrf2 in nonhematopoietic tissues and were surprised to find that Nrf2 deficiency in nonhematopoietic tissues exacerbated anemia and caused premature pulmonary edema in mice with SCD.
The team said this suggests a dominant protective role for nonhematopoietic Nrf2 against tissue damage in both erythroid and nonerythroid tissues in SCD.
And, when taken together, the results of this research indicate that activating Nrf2 can impede the onset of the severe adult phenotype of SCD in mice. ![]()
EC approves drug for pediatric ITP

Photo by Logan Tuttle
The European Commission (EC) has approved eltrombopag (Revolade), a once-daily oral thrombopoietin receptor agonist, to treat pediatric patients (age 1 and older) with chronic immune thrombocytopenia (ITP) that is refractory to other therapies.
This approval includes the use of tablets and a new oral suspension formulation of eltrombopag, which is designed for younger children who may not be able to swallow tablets.
The approval applies to all 28 member states of the European Union plus Iceland, Norway, and Liechtenstein.
Eltrombopag was previously approved by the EC for use in adults with refractory chronic ITP. The drug is also approved in the EC to treat adults with severe aplastic anemia and adults with chronic hepatitis C virus infection who have thrombocytopenia.
Eltrombopag is made by Novartis. For more details on the drug, see the full Summary of Product Characteristics, available on the European Medicines Agency’s website.
The EC’s latest approval of eltrombopag was based on data from 2 double-blind, placebo-controlled trials—the phase 2 PETIT trial and the phase 3 PETIT2 trial.
PETIT trials: Efficacy
The PETIT trial included 67 ITP patients stratified by age cohort (12-17 years, 6-11 years, and 1-5 years). They were randomized (2:1) to receive eltrombopag or placebo for 7 weeks. The eltrombopag dose was titrated to a target platelet count of 50-200 x 109/L.
The primary efficacy endpoint was the proportion of subjects achieving platelet counts of 50 x 109/L or higher at least once between days 8 and 43 of the randomized period of the study.
Significantly more patients in the eltrombopag arm met this endpoint—62.2%—compared to 31.8% in the placebo arm (P=0.011).
The PETIT2 trial enrolled 92 patients with chronic ITP who were randomized (2:1) to receive eltrombopag or placebo for 13 weeks. The eltrombopag dose was titrated to a target platelet count of 50-200 x 109/L.
The primary efficacy endpoint was the proportion of subjects who achieved platelet counts of 50 x 109/L or higher for at least 6 out of 8 weeks, between weeks 5 and 12 of the randomized period.
Significantly more patients in the eltrombopag arm met this endpoint—41.3%—compared to 3.4% of patients in the placebo arm (P<0.001).
PETIT trials: Safety
For both trials, there were 107 eltrombopag-treated patients evaluable for safety.
The most common adverse events that occurred more frequently in the eltrombopag arms than the placebo arms were upper respiratory tract infection, nasopharyngitis, cough, diarrhea, pyrexia, rhinitis, abdominal pain, oropharyngeal pain, toothache, increased ALT/AST, rash, and rhinorrhea.
Serious adverse events were reported in 8% of patients during the randomized part of both trials, although no serious adverse event occurred in more than 1 patient.
An ALT elevation of at least 3 times the upper limit of normal occurred in 5% of eltrombopag-treated patients. Of those patients, 2% had ALT increases of at least 5 times the upper limit of normal.
There were no deaths or thromboembolic events during either study. ![]()

Photo by Logan Tuttle
The European Commission (EC) has approved eltrombopag (Revolade), a once-daily oral thrombopoietin receptor agonist, to treat pediatric patients (age 1 and older) with chronic immune thrombocytopenia (ITP) that is refractory to other therapies.
This approval includes the use of tablets and a new oral suspension formulation of eltrombopag, which is designed for younger children who may not be able to swallow tablets.
The approval applies to all 28 member states of the European Union plus Iceland, Norway, and Liechtenstein.
Eltrombopag was previously approved by the EC for use in adults with refractory chronic ITP. The drug is also approved in the EC to treat adults with severe aplastic anemia and adults with chronic hepatitis C virus infection who have thrombocytopenia.
Eltrombopag is made by Novartis. For more details on the drug, see the full Summary of Product Characteristics, available on the European Medicines Agency’s website.
The EC’s latest approval of eltrombopag was based on data from 2 double-blind, placebo-controlled trials—the phase 2 PETIT trial and the phase 3 PETIT2 trial.
PETIT trials: Efficacy
The PETIT trial included 67 ITP patients stratified by age cohort (12-17 years, 6-11 years, and 1-5 years). They were randomized (2:1) to receive eltrombopag or placebo for 7 weeks. The eltrombopag dose was titrated to a target platelet count of 50-200 x 109/L.
The primary efficacy endpoint was the proportion of subjects achieving platelet counts of 50 x 109/L or higher at least once between days 8 and 43 of the randomized period of the study.
Significantly more patients in the eltrombopag arm met this endpoint—62.2%—compared to 31.8% in the placebo arm (P=0.011).
The PETIT2 trial enrolled 92 patients with chronic ITP who were randomized (2:1) to receive eltrombopag or placebo for 13 weeks. The eltrombopag dose was titrated to a target platelet count of 50-200 x 109/L.
The primary efficacy endpoint was the proportion of subjects who achieved platelet counts of 50 x 109/L or higher for at least 6 out of 8 weeks, between weeks 5 and 12 of the randomized period.
Significantly more patients in the eltrombopag arm met this endpoint—41.3%—compared to 3.4% of patients in the placebo arm (P<0.001).
PETIT trials: Safety
For both trials, there were 107 eltrombopag-treated patients evaluable for safety.
The most common adverse events that occurred more frequently in the eltrombopag arms than the placebo arms were upper respiratory tract infection, nasopharyngitis, cough, diarrhea, pyrexia, rhinitis, abdominal pain, oropharyngeal pain, toothache, increased ALT/AST, rash, and rhinorrhea.
Serious adverse events were reported in 8% of patients during the randomized part of both trials, although no serious adverse event occurred in more than 1 patient.
An ALT elevation of at least 3 times the upper limit of normal occurred in 5% of eltrombopag-treated patients. Of those patients, 2% had ALT increases of at least 5 times the upper limit of normal.
There were no deaths or thromboembolic events during either study. ![]()

Photo by Logan Tuttle
The European Commission (EC) has approved eltrombopag (Revolade), a once-daily oral thrombopoietin receptor agonist, to treat pediatric patients (age 1 and older) with chronic immune thrombocytopenia (ITP) that is refractory to other therapies.
This approval includes the use of tablets and a new oral suspension formulation of eltrombopag, which is designed for younger children who may not be able to swallow tablets.
The approval applies to all 28 member states of the European Union plus Iceland, Norway, and Liechtenstein.
Eltrombopag was previously approved by the EC for use in adults with refractory chronic ITP. The drug is also approved in the EC to treat adults with severe aplastic anemia and adults with chronic hepatitis C virus infection who have thrombocytopenia.
Eltrombopag is made by Novartis. For more details on the drug, see the full Summary of Product Characteristics, available on the European Medicines Agency’s website.
The EC’s latest approval of eltrombopag was based on data from 2 double-blind, placebo-controlled trials—the phase 2 PETIT trial and the phase 3 PETIT2 trial.
PETIT trials: Efficacy
The PETIT trial included 67 ITP patients stratified by age cohort (12-17 years, 6-11 years, and 1-5 years). They were randomized (2:1) to receive eltrombopag or placebo for 7 weeks. The eltrombopag dose was titrated to a target platelet count of 50-200 x 109/L.
The primary efficacy endpoint was the proportion of subjects achieving platelet counts of 50 x 109/L or higher at least once between days 8 and 43 of the randomized period of the study.
Significantly more patients in the eltrombopag arm met this endpoint—62.2%—compared to 31.8% in the placebo arm (P=0.011).
The PETIT2 trial enrolled 92 patients with chronic ITP who were randomized (2:1) to receive eltrombopag or placebo for 13 weeks. The eltrombopag dose was titrated to a target platelet count of 50-200 x 109/L.
The primary efficacy endpoint was the proportion of subjects who achieved platelet counts of 50 x 109/L or higher for at least 6 out of 8 weeks, between weeks 5 and 12 of the randomized period.
Significantly more patients in the eltrombopag arm met this endpoint—41.3%—compared to 3.4% of patients in the placebo arm (P<0.001).
PETIT trials: Safety
For both trials, there were 107 eltrombopag-treated patients evaluable for safety.
The most common adverse events that occurred more frequently in the eltrombopag arms than the placebo arms were upper respiratory tract infection, nasopharyngitis, cough, diarrhea, pyrexia, rhinitis, abdominal pain, oropharyngeal pain, toothache, increased ALT/AST, rash, and rhinorrhea.
Serious adverse events were reported in 8% of patients during the randomized part of both trials, although no serious adverse event occurred in more than 1 patient.
An ALT elevation of at least 3 times the upper limit of normal occurred in 5% of eltrombopag-treated patients. Of those patients, 2% had ALT increases of at least 5 times the upper limit of normal.
There were no deaths or thromboembolic events during either study. ![]()
Study suggests iPSCs pose no cancer risk

Image from the Salk Institute
In tracking the mutational history of somatic cells and induced pluripotent stem cells (iPSCs), researchers found that somatic cells accumulate mutations more frequently than iPSCs.
And none of the mutations found in iPSCs were associated with cancers.
“None of the mutations we found in induced pluripotent stem cells were cancer-driver mutations or mutations in cancer-causing genes,” said Foad Rouhani, of the Wellcome Trust Sanger Institute in the UK.
“We didn’t find anything that would preclude the use of [iPSCs] in therapeutic medicine.”
Rouhani and his colleagues reported these findings in PLOS Genetics.
The researchers generated iPSCs using cells from healthy individuals, then sequenced the genomes of the somatic cells and the derived iPSCs.
They found that somatic cells had a mutation rate of 14 single nucleotide variants per cell per generation, and the mutation rate for iPSCs was 10-fold lower.
The researchers said this is the first time that mutation rates of both types of cells, the donor cell and iPSC, have been calculated and compared.
“Until now, the question of whether generating [iPSCs] and growing them in cell culture creates mutations has not been addressed in detail,” said study author Allan Bradley, PhD, of the Wellcome Trust Sanger Institute.
“If human cells are really to be reprogrammed on a large scale for use in regenerative medicine, then understanding the mutations the donor cells carry will be a crucial step. We now have the tools to do this.”
The researchers also used the iPSCs to trace the history of every mutation that one endothelial progenitor cell had developed from the time it was a fertilized egg to the moment it was taken out of the body.
They said the ability to track the genetic changes in cells over a lifetime could improve scientists’ understanding of how, when, and why mutations lead to cancer. ![]()

Image from the Salk Institute
In tracking the mutational history of somatic cells and induced pluripotent stem cells (iPSCs), researchers found that somatic cells accumulate mutations more frequently than iPSCs.
And none of the mutations found in iPSCs were associated with cancers.
“None of the mutations we found in induced pluripotent stem cells were cancer-driver mutations or mutations in cancer-causing genes,” said Foad Rouhani, of the Wellcome Trust Sanger Institute in the UK.
“We didn’t find anything that would preclude the use of [iPSCs] in therapeutic medicine.”
Rouhani and his colleagues reported these findings in PLOS Genetics.
The researchers generated iPSCs using cells from healthy individuals, then sequenced the genomes of the somatic cells and the derived iPSCs.
They found that somatic cells had a mutation rate of 14 single nucleotide variants per cell per generation, and the mutation rate for iPSCs was 10-fold lower.
The researchers said this is the first time that mutation rates of both types of cells, the donor cell and iPSC, have been calculated and compared.
“Until now, the question of whether generating [iPSCs] and growing them in cell culture creates mutations has not been addressed in detail,” said study author Allan Bradley, PhD, of the Wellcome Trust Sanger Institute.
“If human cells are really to be reprogrammed on a large scale for use in regenerative medicine, then understanding the mutations the donor cells carry will be a crucial step. We now have the tools to do this.”
The researchers also used the iPSCs to trace the history of every mutation that one endothelial progenitor cell had developed from the time it was a fertilized egg to the moment it was taken out of the body.
They said the ability to track the genetic changes in cells over a lifetime could improve scientists’ understanding of how, when, and why mutations lead to cancer. ![]()

Image from the Salk Institute
In tracking the mutational history of somatic cells and induced pluripotent stem cells (iPSCs), researchers found that somatic cells accumulate mutations more frequently than iPSCs.
And none of the mutations found in iPSCs were associated with cancers.
“None of the mutations we found in induced pluripotent stem cells were cancer-driver mutations or mutations in cancer-causing genes,” said Foad Rouhani, of the Wellcome Trust Sanger Institute in the UK.
“We didn’t find anything that would preclude the use of [iPSCs] in therapeutic medicine.”
Rouhani and his colleagues reported these findings in PLOS Genetics.
The researchers generated iPSCs using cells from healthy individuals, then sequenced the genomes of the somatic cells and the derived iPSCs.
They found that somatic cells had a mutation rate of 14 single nucleotide variants per cell per generation, and the mutation rate for iPSCs was 10-fold lower.
The researchers said this is the first time that mutation rates of both types of cells, the donor cell and iPSC, have been calculated and compared.
“Until now, the question of whether generating [iPSCs] and growing them in cell culture creates mutations has not been addressed in detail,” said study author Allan Bradley, PhD, of the Wellcome Trust Sanger Institute.
“If human cells are really to be reprogrammed on a large scale for use in regenerative medicine, then understanding the mutations the donor cells carry will be a crucial step. We now have the tools to do this.”
The researchers also used the iPSCs to trace the history of every mutation that one endothelial progenitor cell had developed from the time it was a fertilized egg to the moment it was taken out of the body.
They said the ability to track the genetic changes in cells over a lifetime could improve scientists’ understanding of how, when, and why mutations lead to cancer. ![]()
Platelet-Rich Plasma for Androgenetic Alopecia
Many male and female patients seek therapy for androgenetic alopecia (AGA) at some point. Results are rarely achieved with single-modality therapy. In fact, the treatment of AGA often requires a combination approach of systemic medications and supplements; topical therapy; and if indicated, some type of minimally invasive procedure or surgical option.
The use of platelet-rich plasma (PRP) to pretreat follicular unit hair grafts may increase hair growth and density. Although the method by which PRP helps promote hair growth remains a source of speculation, it is known that platelets contain many growth factors in the platelet α granules. When these granules become activated, they release many types of growth factors ranging from vascular endothelial growth factor, transforming growth factor ß, epidermal growth factor, platelet-derived growth factor, and insulinlike growth factor.
Injection or topical application of PRP has become a popular treatment for skin rejuvenation, alopecia, and autologous fat grafting; however, many of these treatments are being done without the studies to support them.
Alves and Grimalt (Dermatol Surg. 2016;42:491-497) conducted a prospective, split-scalp, placebo-controlled study evaluating the use of PRP injections in the treatment of AGA in 25 patients (12 men, 13 women) with a mean age of 39 years (age range, 21–62 years). Photographs were taken and 4 areas per split scalp were marked with red tattoo dots. The patients were randomized to receive PRP on 1 side and saline injections on the other side. Patients were blinded, but the physician performing the treatment was not blinded. Treatments were performed monthly for 3 sessions. Follow-up photographs and hair density counts were performed at 3 and 6 months after treatment.
Results showed that after 6 months there was a statistically significant (P<.05) increase in the total hair density and terminal hair counts on the PRP-treated side compared to baseline and to the placebo-treated side. When broken down by demographics, patients who did best were men 40 years or younger with AGA beginning at 25 years or older, a positive family history of AGA, and AGA duration of greater than 10 years.
What’s the issue?
The results of this study suggest that PRP has a mild to modest effect (approximately 10% increase) on increasing hair density in a specific patient population. This split-scalp, placebo-controlled study is one of the few of its kind in the field of PRP research and the authors should be applauded for the design of this study. However, it would be beneficial to have a 1-year follow-up to see if the results are maintained and to better help determine if maintenance injections would be needed to sustain the results.
The field of hair restoration and regeneration will continue to grow as newer technologies in hair stem cell injections come to the forefront as well. Rigorous studies will be needed to better help physicians and patients make the right treatment decisions.
Have patients been asking you about PRP for skin rejuvenation and hair restoration?
Many male and female patients seek therapy for androgenetic alopecia (AGA) at some point. Results are rarely achieved with single-modality therapy. In fact, the treatment of AGA often requires a combination approach of systemic medications and supplements; topical therapy; and if indicated, some type of minimally invasive procedure or surgical option.
The use of platelet-rich plasma (PRP) to pretreat follicular unit hair grafts may increase hair growth and density. Although the method by which PRP helps promote hair growth remains a source of speculation, it is known that platelets contain many growth factors in the platelet α granules. When these granules become activated, they release many types of growth factors ranging from vascular endothelial growth factor, transforming growth factor ß, epidermal growth factor, platelet-derived growth factor, and insulinlike growth factor.
Injection or topical application of PRP has become a popular treatment for skin rejuvenation, alopecia, and autologous fat grafting; however, many of these treatments are being done without the studies to support them.
Alves and Grimalt (Dermatol Surg. 2016;42:491-497) conducted a prospective, split-scalp, placebo-controlled study evaluating the use of PRP injections in the treatment of AGA in 25 patients (12 men, 13 women) with a mean age of 39 years (age range, 21–62 years). Photographs were taken and 4 areas per split scalp were marked with red tattoo dots. The patients were randomized to receive PRP on 1 side and saline injections on the other side. Patients were blinded, but the physician performing the treatment was not blinded. Treatments were performed monthly for 3 sessions. Follow-up photographs and hair density counts were performed at 3 and 6 months after treatment.
Results showed that after 6 months there was a statistically significant (P<.05) increase in the total hair density and terminal hair counts on the PRP-treated side compared to baseline and to the placebo-treated side. When broken down by demographics, patients who did best were men 40 years or younger with AGA beginning at 25 years or older, a positive family history of AGA, and AGA duration of greater than 10 years.
What’s the issue?
The results of this study suggest that PRP has a mild to modest effect (approximately 10% increase) on increasing hair density in a specific patient population. This split-scalp, placebo-controlled study is one of the few of its kind in the field of PRP research and the authors should be applauded for the design of this study. However, it would be beneficial to have a 1-year follow-up to see if the results are maintained and to better help determine if maintenance injections would be needed to sustain the results.
The field of hair restoration and regeneration will continue to grow as newer technologies in hair stem cell injections come to the forefront as well. Rigorous studies will be needed to better help physicians and patients make the right treatment decisions.
Have patients been asking you about PRP for skin rejuvenation and hair restoration?
Many male and female patients seek therapy for androgenetic alopecia (AGA) at some point. Results are rarely achieved with single-modality therapy. In fact, the treatment of AGA often requires a combination approach of systemic medications and supplements; topical therapy; and if indicated, some type of minimally invasive procedure or surgical option.
The use of platelet-rich plasma (PRP) to pretreat follicular unit hair grafts may increase hair growth and density. Although the method by which PRP helps promote hair growth remains a source of speculation, it is known that platelets contain many growth factors in the platelet α granules. When these granules become activated, they release many types of growth factors ranging from vascular endothelial growth factor, transforming growth factor ß, epidermal growth factor, platelet-derived growth factor, and insulinlike growth factor.
Injection or topical application of PRP has become a popular treatment for skin rejuvenation, alopecia, and autologous fat grafting; however, many of these treatments are being done without the studies to support them.
Alves and Grimalt (Dermatol Surg. 2016;42:491-497) conducted a prospective, split-scalp, placebo-controlled study evaluating the use of PRP injections in the treatment of AGA in 25 patients (12 men, 13 women) with a mean age of 39 years (age range, 21–62 years). Photographs were taken and 4 areas per split scalp were marked with red tattoo dots. The patients were randomized to receive PRP on 1 side and saline injections on the other side. Patients were blinded, but the physician performing the treatment was not blinded. Treatments were performed monthly for 3 sessions. Follow-up photographs and hair density counts were performed at 3 and 6 months after treatment.
Results showed that after 6 months there was a statistically significant (P<.05) increase in the total hair density and terminal hair counts on the PRP-treated side compared to baseline and to the placebo-treated side. When broken down by demographics, patients who did best were men 40 years or younger with AGA beginning at 25 years or older, a positive family history of AGA, and AGA duration of greater than 10 years.
What’s the issue?
The results of this study suggest that PRP has a mild to modest effect (approximately 10% increase) on increasing hair density in a specific patient population. This split-scalp, placebo-controlled study is one of the few of its kind in the field of PRP research and the authors should be applauded for the design of this study. However, it would be beneficial to have a 1-year follow-up to see if the results are maintained and to better help determine if maintenance injections would be needed to sustain the results.
The field of hair restoration and regeneration will continue to grow as newer technologies in hair stem cell injections come to the forefront as well. Rigorous studies will be needed to better help physicians and patients make the right treatment decisions.
Have patients been asking you about PRP for skin rejuvenation and hair restoration?
The brief thrill of catching a zebra
Life in a general neurology practice, over time, becomes a routine. Migraines, dementia, strokes, neuropathy, back and neck pain … the things that are, as they say, the “bread and butter” of the job. So much of this job is spent thinking inside the box that some days it’s hard to remember we have to keep an eye on the outside of it, too.
Unlike my academic colleagues, I’m not a huge fan of zebras. I prefer my life, practice, and cases uncomplicated and straightforward. Horses suit me better. But, like everyone else in this job, I occasionally find a zebra. Recently, a fellow was referred to me for imbalance, but his appearance concerned me enough that I thought something outside the usual considerations was there. When all was said and done, he’d been diagnosed with myotonic dystrophy.
And, as much as uncommon diagnoses can drive you nuts, when you stumble across one AND get it right, it’s exhilarating – like a home run, a 3-point shot, or an interception returned for a touchdown. That’s especially true if it’s something treatable, and you can make a real difference in someone’s life.
A key part of medical training is the differential game – where an attending repeatedly grills you with the question, “And what else could this be?” making you think of both obvious and far-fetched possibilities.
This part is probably one of the most hated during training, yet very appreciated years later. Where I trained, it was the focus of a much-dreaded conference held every Thursday morning around a huge table. You were forced to think of the unordinary things that are the pitfalls of medicine. Today, I realize how valuable those 90-minute, weekly sessions were.
Although none of us realizes it at the time, those are the things that make you a better doctor. The brief thrill of catching a zebra never gets old. And it’s always coupled with a deep appreciation for those who taught me to hunt them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Life in a general neurology practice, over time, becomes a routine. Migraines, dementia, strokes, neuropathy, back and neck pain … the things that are, as they say, the “bread and butter” of the job. So much of this job is spent thinking inside the box that some days it’s hard to remember we have to keep an eye on the outside of it, too.
Unlike my academic colleagues, I’m not a huge fan of zebras. I prefer my life, practice, and cases uncomplicated and straightforward. Horses suit me better. But, like everyone else in this job, I occasionally find a zebra. Recently, a fellow was referred to me for imbalance, but his appearance concerned me enough that I thought something outside the usual considerations was there. When all was said and done, he’d been diagnosed with myotonic dystrophy.
And, as much as uncommon diagnoses can drive you nuts, when you stumble across one AND get it right, it’s exhilarating – like a home run, a 3-point shot, or an interception returned for a touchdown. That’s especially true if it’s something treatable, and you can make a real difference in someone’s life.
A key part of medical training is the differential game – where an attending repeatedly grills you with the question, “And what else could this be?” making you think of both obvious and far-fetched possibilities.
This part is probably one of the most hated during training, yet very appreciated years later. Where I trained, it was the focus of a much-dreaded conference held every Thursday morning around a huge table. You were forced to think of the unordinary things that are the pitfalls of medicine. Today, I realize how valuable those 90-minute, weekly sessions were.
Although none of us realizes it at the time, those are the things that make you a better doctor. The brief thrill of catching a zebra never gets old. And it’s always coupled with a deep appreciation for those who taught me to hunt them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Life in a general neurology practice, over time, becomes a routine. Migraines, dementia, strokes, neuropathy, back and neck pain … the things that are, as they say, the “bread and butter” of the job. So much of this job is spent thinking inside the box that some days it’s hard to remember we have to keep an eye on the outside of it, too.
Unlike my academic colleagues, I’m not a huge fan of zebras. I prefer my life, practice, and cases uncomplicated and straightforward. Horses suit me better. But, like everyone else in this job, I occasionally find a zebra. Recently, a fellow was referred to me for imbalance, but his appearance concerned me enough that I thought something outside the usual considerations was there. When all was said and done, he’d been diagnosed with myotonic dystrophy.
And, as much as uncommon diagnoses can drive you nuts, when you stumble across one AND get it right, it’s exhilarating – like a home run, a 3-point shot, or an interception returned for a touchdown. That’s especially true if it’s something treatable, and you can make a real difference in someone’s life.
A key part of medical training is the differential game – where an attending repeatedly grills you with the question, “And what else could this be?” making you think of both obvious and far-fetched possibilities.
This part is probably one of the most hated during training, yet very appreciated years later. Where I trained, it was the focus of a much-dreaded conference held every Thursday morning around a huge table. You were forced to think of the unordinary things that are the pitfalls of medicine. Today, I realize how valuable those 90-minute, weekly sessions were.
Although none of us realizes it at the time, those are the things that make you a better doctor. The brief thrill of catching a zebra never gets old. And it’s always coupled with a deep appreciation for those who taught me to hunt them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Early antiarrhythmic drugs boost survival in shock-refractory cardiac arrest
CHICAGO – Paramedic-administered amiodarone or lidocaine during resuscitation of patients with shock-refractory ventricular fibrillation or ventricular tachycardia of out-of-hospital cardiac arrest significantly improves survival, according to the findings of the largest-ever clinical trial of out-of-hospital cardiac arrest.
However, the survival advantage was limited to bystander-witnessed arrest. The reason for this difference in the Amiodarone, Lidocaine or Placebo Study (ALPS) is that observed arrest is a good surrogate for earlier recognition and treatment of an out-of-hospital cardiac arrest (OHCA), Dr. Peter J. Kudenchuk explained in presenting the study findings at the annual meeting of the American College of Cardiology.
“The message from this trial is that, if you give these drugs to everyone across the board with out-of-hospital shock-refractory VF/VT cardiac arrest, you’ll help those who can be helped and you won’t hurt those who are beyond help,” said Dr. Kudenchuk, professor of medicine at the University of Washington, Seattle.
ALPS was a randomized, blinded, placebo-controlled clinical trial of 3,026 patients with shock-refractory VF/VT OHCA at 10 U.S. and Canadian sites participating in the Resuscitation Outcomes Consortium. Subjects were randomized to paramedic-administered treatment with prefilled syringes of amiodarone, lidocaine, or placebo. Time to treatment averaged 19 minutes from the initial call made to emergency services.
The primary endpoint in ALPS was survival to hospital discharge. Rates were 24.4% in the amiodarone group, 23.7% with lidocaine, and 21% with placebo. Differences in survival rates between the antiarrhythmic drug and placebo groups approached but did not achieve statistical significance.
Survival to hospital discharge in the 1,934 participants with bystander-witnessed arrest was a prespecified secondary endpoint. That outcome was achieved in 27.7% of the amiodarone group and 27.8% who got lidocaine, compared with 22.7% of placebo-treated patients. Those differences were statistically significant and clinically meaningful, Dr. Kudenchuk asserted.
“Though these differences – an absolute 5% improvement over placebo – may seem small, were we to implement this as policy, upwards of 1,800 more lives could potentially be saved each year in the United States alone,” said Dr. Kudenchuk, an electrophysiologist and cardiologist.
Bystander-witnessed OHCA was 2.3-fold more common than unwitnessed arrest. In the unwitnessed arrest subgroup there was no hint of benefit for either amiodarone or lidocaine.
“Many patients with unwitnessed arrest have already sustained mortal ischemic damage by the time they’re found,” he observed. “If you go into a morgue and give the best drug in the world, you’re not going to save anybody.”
Moreover, among the roughly 5% of patients whose OHCA was witnessed by EMS personnel, survival to hospital discharge was a whopping absolute 22% greater with antiarrhythmic drug therapy than with placebo.
“Taken together, these findings suggest that treatment sooner after heart collapse may be a critical determinant of drug effect,” Dr. Kudenchuk continued.
He said the ALPS findings are generalizable to all communities across North America where the local EMS system follows the Resuscitation Outcomes Consortium philosophy that early defibrillation and good CPR are the cornerstones of effective management of OHCA, without which no treatment can be effective.
Current use of these drugs across the United States is not standardized. “It is really a free-for-all,” according to Dr. Kudenchuk. “Some agencies strictly use lidocaine, others may use amiodarone. Some use both. And some use neither. I think in part that’s because current guideline recommendations give these drugs a class IIb recommendation – meaning they’re optional – because up until this point there have been no data to support their effectiveness in changing outcome.”
In his view, the ALPS data clearly warrant upgrading the strength of the recommendation for antiarrhythmic drug therapy in the next iteration of the guidelines. Although he is on the guideline committee, Dr. Kudenchuk added, he cannot predict what the committee as a whole will decide.
ALPS will not lead to a change in practice such that paramedic-administered antiarrhythmic agents are given only to patients with witnessed arrest, Dr. Kudenchuk said. It’s not practical for rescue personnel in the midst of the fray to try to figure out whether an OHCA was witnessed or not. Plus, there’s an ethical issue involved.
“If we’d wanted to hit the headlines with a major trial with a positive outcome we would have selected only people with witnessed cardiac arrest from the get-go to do this trial, since we guessed that’s where the money was going to be. The reality is you can’t treat people that way. Everyone has to have a chance,” he said.
Asked which antiarrhythmic drug the next edition of the resuscitation guidelines should recommend preferentially, he said ALPS wasn’t powered to distinguish between amiodarone and lidocaine. “If I were writing the guidelines, I would simply say either or both happens to be okay.”
An important footnote is that ALPS utilized a new, Food and Drug Administration–approved formulation of amiodarone, known as Nexterone, designed to reduce hypotensive effects. Had investigators employed the more familiar version of the drug, the safety results wouldn’t have been as good.
Out-of-hospital cardiac arrest accounts for roughly 350,000 deaths per year in the United States
Simultaneously with Dr. Kudenchuk’s presentation of the ALPS findings at ACC 16 in Chicago, the results were published online (N Engl J Med. 2016 Apr 4; doi: 10.1056/NEJMoa1514204).
He reported having no financial conflicts regarding the ALPS study, which was funded by the National Heart, Lung, and Blood Institute, the Canadian Institutes of Health Research, the American Heart Association, the U.S. Army, and Defense Research and Development Canada.
CHICAGO – Paramedic-administered amiodarone or lidocaine during resuscitation of patients with shock-refractory ventricular fibrillation or ventricular tachycardia of out-of-hospital cardiac arrest significantly improves survival, according to the findings of the largest-ever clinical trial of out-of-hospital cardiac arrest.
However, the survival advantage was limited to bystander-witnessed arrest. The reason for this difference in the Amiodarone, Lidocaine or Placebo Study (ALPS) is that observed arrest is a good surrogate for earlier recognition and treatment of an out-of-hospital cardiac arrest (OHCA), Dr. Peter J. Kudenchuk explained in presenting the study findings at the annual meeting of the American College of Cardiology.
“The message from this trial is that, if you give these drugs to everyone across the board with out-of-hospital shock-refractory VF/VT cardiac arrest, you’ll help those who can be helped and you won’t hurt those who are beyond help,” said Dr. Kudenchuk, professor of medicine at the University of Washington, Seattle.
ALPS was a randomized, blinded, placebo-controlled clinical trial of 3,026 patients with shock-refractory VF/VT OHCA at 10 U.S. and Canadian sites participating in the Resuscitation Outcomes Consortium. Subjects were randomized to paramedic-administered treatment with prefilled syringes of amiodarone, lidocaine, or placebo. Time to treatment averaged 19 minutes from the initial call made to emergency services.
The primary endpoint in ALPS was survival to hospital discharge. Rates were 24.4% in the amiodarone group, 23.7% with lidocaine, and 21% with placebo. Differences in survival rates between the antiarrhythmic drug and placebo groups approached but did not achieve statistical significance.
Survival to hospital discharge in the 1,934 participants with bystander-witnessed arrest was a prespecified secondary endpoint. That outcome was achieved in 27.7% of the amiodarone group and 27.8% who got lidocaine, compared with 22.7% of placebo-treated patients. Those differences were statistically significant and clinically meaningful, Dr. Kudenchuk asserted.
“Though these differences – an absolute 5% improvement over placebo – may seem small, were we to implement this as policy, upwards of 1,800 more lives could potentially be saved each year in the United States alone,” said Dr. Kudenchuk, an electrophysiologist and cardiologist.
Bystander-witnessed OHCA was 2.3-fold more common than unwitnessed arrest. In the unwitnessed arrest subgroup there was no hint of benefit for either amiodarone or lidocaine.
“Many patients with unwitnessed arrest have already sustained mortal ischemic damage by the time they’re found,” he observed. “If you go into a morgue and give the best drug in the world, you’re not going to save anybody.”
Moreover, among the roughly 5% of patients whose OHCA was witnessed by EMS personnel, survival to hospital discharge was a whopping absolute 22% greater with antiarrhythmic drug therapy than with placebo.
“Taken together, these findings suggest that treatment sooner after heart collapse may be a critical determinant of drug effect,” Dr. Kudenchuk continued.
He said the ALPS findings are generalizable to all communities across North America where the local EMS system follows the Resuscitation Outcomes Consortium philosophy that early defibrillation and good CPR are the cornerstones of effective management of OHCA, without which no treatment can be effective.
Current use of these drugs across the United States is not standardized. “It is really a free-for-all,” according to Dr. Kudenchuk. “Some agencies strictly use lidocaine, others may use amiodarone. Some use both. And some use neither. I think in part that’s because current guideline recommendations give these drugs a class IIb recommendation – meaning they’re optional – because up until this point there have been no data to support their effectiveness in changing outcome.”
In his view, the ALPS data clearly warrant upgrading the strength of the recommendation for antiarrhythmic drug therapy in the next iteration of the guidelines. Although he is on the guideline committee, Dr. Kudenchuk added, he cannot predict what the committee as a whole will decide.
ALPS will not lead to a change in practice such that paramedic-administered antiarrhythmic agents are given only to patients with witnessed arrest, Dr. Kudenchuk said. It’s not practical for rescue personnel in the midst of the fray to try to figure out whether an OHCA was witnessed or not. Plus, there’s an ethical issue involved.
“If we’d wanted to hit the headlines with a major trial with a positive outcome we would have selected only people with witnessed cardiac arrest from the get-go to do this trial, since we guessed that’s where the money was going to be. The reality is you can’t treat people that way. Everyone has to have a chance,” he said.
Asked which antiarrhythmic drug the next edition of the resuscitation guidelines should recommend preferentially, he said ALPS wasn’t powered to distinguish between amiodarone and lidocaine. “If I were writing the guidelines, I would simply say either or both happens to be okay.”
An important footnote is that ALPS utilized a new, Food and Drug Administration–approved formulation of amiodarone, known as Nexterone, designed to reduce hypotensive effects. Had investigators employed the more familiar version of the drug, the safety results wouldn’t have been as good.
Out-of-hospital cardiac arrest accounts for roughly 350,000 deaths per year in the United States
Simultaneously with Dr. Kudenchuk’s presentation of the ALPS findings at ACC 16 in Chicago, the results were published online (N Engl J Med. 2016 Apr 4; doi: 10.1056/NEJMoa1514204).
He reported having no financial conflicts regarding the ALPS study, which was funded by the National Heart, Lung, and Blood Institute, the Canadian Institutes of Health Research, the American Heart Association, the U.S. Army, and Defense Research and Development Canada.
CHICAGO – Paramedic-administered amiodarone or lidocaine during resuscitation of patients with shock-refractory ventricular fibrillation or ventricular tachycardia of out-of-hospital cardiac arrest significantly improves survival, according to the findings of the largest-ever clinical trial of out-of-hospital cardiac arrest.
However, the survival advantage was limited to bystander-witnessed arrest. The reason for this difference in the Amiodarone, Lidocaine or Placebo Study (ALPS) is that observed arrest is a good surrogate for earlier recognition and treatment of an out-of-hospital cardiac arrest (OHCA), Dr. Peter J. Kudenchuk explained in presenting the study findings at the annual meeting of the American College of Cardiology.
“The message from this trial is that, if you give these drugs to everyone across the board with out-of-hospital shock-refractory VF/VT cardiac arrest, you’ll help those who can be helped and you won’t hurt those who are beyond help,” said Dr. Kudenchuk, professor of medicine at the University of Washington, Seattle.
ALPS was a randomized, blinded, placebo-controlled clinical trial of 3,026 patients with shock-refractory VF/VT OHCA at 10 U.S. and Canadian sites participating in the Resuscitation Outcomes Consortium. Subjects were randomized to paramedic-administered treatment with prefilled syringes of amiodarone, lidocaine, or placebo. Time to treatment averaged 19 minutes from the initial call made to emergency services.
The primary endpoint in ALPS was survival to hospital discharge. Rates were 24.4% in the amiodarone group, 23.7% with lidocaine, and 21% with placebo. Differences in survival rates between the antiarrhythmic drug and placebo groups approached but did not achieve statistical significance.
Survival to hospital discharge in the 1,934 participants with bystander-witnessed arrest was a prespecified secondary endpoint. That outcome was achieved in 27.7% of the amiodarone group and 27.8% who got lidocaine, compared with 22.7% of placebo-treated patients. Those differences were statistically significant and clinically meaningful, Dr. Kudenchuk asserted.
“Though these differences – an absolute 5% improvement over placebo – may seem small, were we to implement this as policy, upwards of 1,800 more lives could potentially be saved each year in the United States alone,” said Dr. Kudenchuk, an electrophysiologist and cardiologist.
Bystander-witnessed OHCA was 2.3-fold more common than unwitnessed arrest. In the unwitnessed arrest subgroup there was no hint of benefit for either amiodarone or lidocaine.
“Many patients with unwitnessed arrest have already sustained mortal ischemic damage by the time they’re found,” he observed. “If you go into a morgue and give the best drug in the world, you’re not going to save anybody.”
Moreover, among the roughly 5% of patients whose OHCA was witnessed by EMS personnel, survival to hospital discharge was a whopping absolute 22% greater with antiarrhythmic drug therapy than with placebo.
“Taken together, these findings suggest that treatment sooner after heart collapse may be a critical determinant of drug effect,” Dr. Kudenchuk continued.
He said the ALPS findings are generalizable to all communities across North America where the local EMS system follows the Resuscitation Outcomes Consortium philosophy that early defibrillation and good CPR are the cornerstones of effective management of OHCA, without which no treatment can be effective.
Current use of these drugs across the United States is not standardized. “It is really a free-for-all,” according to Dr. Kudenchuk. “Some agencies strictly use lidocaine, others may use amiodarone. Some use both. And some use neither. I think in part that’s because current guideline recommendations give these drugs a class IIb recommendation – meaning they’re optional – because up until this point there have been no data to support their effectiveness in changing outcome.”
In his view, the ALPS data clearly warrant upgrading the strength of the recommendation for antiarrhythmic drug therapy in the next iteration of the guidelines. Although he is on the guideline committee, Dr. Kudenchuk added, he cannot predict what the committee as a whole will decide.
ALPS will not lead to a change in practice such that paramedic-administered antiarrhythmic agents are given only to patients with witnessed arrest, Dr. Kudenchuk said. It’s not practical for rescue personnel in the midst of the fray to try to figure out whether an OHCA was witnessed or not. Plus, there’s an ethical issue involved.
“If we’d wanted to hit the headlines with a major trial with a positive outcome we would have selected only people with witnessed cardiac arrest from the get-go to do this trial, since we guessed that’s where the money was going to be. The reality is you can’t treat people that way. Everyone has to have a chance,” he said.
Asked which antiarrhythmic drug the next edition of the resuscitation guidelines should recommend preferentially, he said ALPS wasn’t powered to distinguish between amiodarone and lidocaine. “If I were writing the guidelines, I would simply say either or both happens to be okay.”
An important footnote is that ALPS utilized a new, Food and Drug Administration–approved formulation of amiodarone, known as Nexterone, designed to reduce hypotensive effects. Had investigators employed the more familiar version of the drug, the safety results wouldn’t have been as good.
Out-of-hospital cardiac arrest accounts for roughly 350,000 deaths per year in the United States
Simultaneously with Dr. Kudenchuk’s presentation of the ALPS findings at ACC 16 in Chicago, the results were published online (N Engl J Med. 2016 Apr 4; doi: 10.1056/NEJMoa1514204).
He reported having no financial conflicts regarding the ALPS study, which was funded by the National Heart, Lung, and Blood Institute, the Canadian Institutes of Health Research, the American Heart Association, the U.S. Army, and Defense Research and Development Canada.
AT ACC 16
Key clinical point: Routine use of injectable amiodarone or lidocaine by paramedics in cases of shock-refractory VF/VT out-of-hospital cardiac arrest would save at least 1,800 lives per year in the U.S.
Major finding: Survival to hospital discharge was an absolute 5% greater when such patients got the antiarrhythmic compared with placebo.
Data source: A blinded, randomized, placebo-controlled clinical trial of 3,026 subjects at 10 sites.
Disclosures: The National Heart, Lung, and Blood Institute, the Canadian Institutes of Health Research, the American Heart Association, the U.S. Army, and Defense Research and Development Canada funded the ALPS trial. The presenter reported having no financial conflicts of interest.