User login
Nicotinamide cuts rate of nonmelanoma skin cancer in those at high risk
Nicotinamide, an inexpensive, over-the-counter form of vitamin B3, is safe and efficacious for the chemoprevention of nonmelanoma skin cancer in patients at high risk, according to data from the Australian Oral Nicotinamide to Reduce Actinic Cancer (ONTRAC) Study.
Results reported in a press briefing held before the annual meeting of the American Society of Clinical Oncology showed that patients taking nicotinamide were about one-fourth less likely than peers taking a placebo to develop new basal cell and squamous cell skin cancers. They also had a smaller reduction in new actinic keratoses.
“Nicotinamide, vitamin B3, significantly reduced nonmelanoma skin cancers and keratoses in just 12 months in a group of pretty high-risk patients. It’s safe, it’s almost obscenely inexpensive, and it’s already widely commercially available, so this one’s ready to go straight into the clinic,” commented senior investigator Dr. Diona Damian, professor of dermatology at the University of Sydney.
She cautioned that the results apply only to the population studied: adults who had experienced two or more nonmelanoma skin cancers in the past 5 years.
“These are the people we’d be recommending it for – people who have already got a skin cancer track record. It’s not something that we’d recommend at this stage for the general population,” she said. Likewise, the findings do not speak to patients at the other end of the spectrum who are in treatment for advanced or metastatic skin cancer, as they also were excluded.
That said, the researchers are planning additional studies in other populations, such patients who are at high risk because they have immunosuppression, according to Dr. Damian.
“We still need the overall skin cancer prevention strategies of sun-safe behavior, sunscreen, and regular skin surveillance,” she stressed, “but we now have an additional exciting opportunity for affordable skin cancer chemoprevention which we can instantly translate into clinical practice.”
Dr. Peter Paul Yu, ASCO President and a medical oncologist and hematologist who is director of cancer research at the Palo Alto Medical Foundation, Sunnyvale, Calif., commented, “This is a very exciting prevention trial. We all know that we clamor for preventing rather than treating diseases, and this is a major advance for us.”
Exposure to ultraviolet light packs a one-two punch to the skin, both damaging cellular DNA and suppressing the skin’s immune response, according to Dr. Damian. The investigators opted to test nicotinamide as it counters both of these events.
The 386 patients in ONTRAC had heavily sun damaged skin, with a mean of 8 nonmelanoma skin cancers in the past 5 years and 50 keratoses at baseline. They were randomized evenly to receive nicotinamide (500 mg twice daily) or placebo for 12 months.
Results showed that the average number of new nonmelanoma skin cancers per patient during the treatment period was 1.77 in the nicotinamide group and 2.42 in the placebo group. The difference translated to a 23% lower rate of new cancers with the vitamin.
“There were comparable reductions seen for both basal and squamous cell carcinomas,” Dr. Damian noted. “Interestingly, this reduction in skin cancers seemed to start as early as the first 3-month visit. And then when people stopped taking their tablets after 12 months, the benefit was no longer seen. In other words, you need to continue taking the tablets in order for them to be effective.”
The nicotinamide group also had a roughly 15% lower rate of new actinic keratoses, compared with the placebo group.
“Nicotinamide was very well tolerated. There was no difference in adverse events, blood parameters, or blood pressure in the two arms” of the study, reported Dr. Damian. She stressed that it is critically important to distinguish nicotinamide from niacin (nicotinic acid), another form of vitamin B3 that has a host of side effects such as headache and flushing.
“One of the great things about [nicotinamide] is that it really has hardly any drug interactions, which means that elderly patients who may be taking a whole cocktail of medications for their heart disease and their hypertension, and whatever else, the nicotinamide won’t interact with those,” she added.
Some evidence also has shown nonsteroidal anti-inflammatory drugs to reduce the risk of skin cancer. “The advantage of nicotinamide is that it doesn’t have the potential gastrointestinal bleeding or renal side effects of nonsteroidals, so it may be suitable for a group of people who aren’t suitable for taking nonsteroidals,” she said. “In our ONTRAC study, we didn’t find synergy or additional benefit in people who were coincidentally taking nonsteroidals for other indications.”
The trial’s results should be generalizable to similar high-risk patients in less sunny parts of the world, Dr. Damian said. “If their skin has shown that degree of damage to get skin cancer, then we suspect nicotinamide would offer benefits to them as well.”
Dr. Damian disclosed no relevant conflicts of interest. The study was funded by the National Health & Medical Research Council.
Nicotinamide, an inexpensive, over-the-counter form of vitamin B3, is safe and efficacious for the chemoprevention of nonmelanoma skin cancer in patients at high risk, according to data from the Australian Oral Nicotinamide to Reduce Actinic Cancer (ONTRAC) Study.
Results reported in a press briefing held before the annual meeting of the American Society of Clinical Oncology showed that patients taking nicotinamide were about one-fourth less likely than peers taking a placebo to develop new basal cell and squamous cell skin cancers. They also had a smaller reduction in new actinic keratoses.
“Nicotinamide, vitamin B3, significantly reduced nonmelanoma skin cancers and keratoses in just 12 months in a group of pretty high-risk patients. It’s safe, it’s almost obscenely inexpensive, and it’s already widely commercially available, so this one’s ready to go straight into the clinic,” commented senior investigator Dr. Diona Damian, professor of dermatology at the University of Sydney.
She cautioned that the results apply only to the population studied: adults who had experienced two or more nonmelanoma skin cancers in the past 5 years.
“These are the people we’d be recommending it for – people who have already got a skin cancer track record. It’s not something that we’d recommend at this stage for the general population,” she said. Likewise, the findings do not speak to patients at the other end of the spectrum who are in treatment for advanced or metastatic skin cancer, as they also were excluded.
That said, the researchers are planning additional studies in other populations, such patients who are at high risk because they have immunosuppression, according to Dr. Damian.
“We still need the overall skin cancer prevention strategies of sun-safe behavior, sunscreen, and regular skin surveillance,” she stressed, “but we now have an additional exciting opportunity for affordable skin cancer chemoprevention which we can instantly translate into clinical practice.”
Dr. Peter Paul Yu, ASCO President and a medical oncologist and hematologist who is director of cancer research at the Palo Alto Medical Foundation, Sunnyvale, Calif., commented, “This is a very exciting prevention trial. We all know that we clamor for preventing rather than treating diseases, and this is a major advance for us.”
Exposure to ultraviolet light packs a one-two punch to the skin, both damaging cellular DNA and suppressing the skin’s immune response, according to Dr. Damian. The investigators opted to test nicotinamide as it counters both of these events.
The 386 patients in ONTRAC had heavily sun damaged skin, with a mean of 8 nonmelanoma skin cancers in the past 5 years and 50 keratoses at baseline. They were randomized evenly to receive nicotinamide (500 mg twice daily) or placebo for 12 months.
Results showed that the average number of new nonmelanoma skin cancers per patient during the treatment period was 1.77 in the nicotinamide group and 2.42 in the placebo group. The difference translated to a 23% lower rate of new cancers with the vitamin.
“There were comparable reductions seen for both basal and squamous cell carcinomas,” Dr. Damian noted. “Interestingly, this reduction in skin cancers seemed to start as early as the first 3-month visit. And then when people stopped taking their tablets after 12 months, the benefit was no longer seen. In other words, you need to continue taking the tablets in order for them to be effective.”
The nicotinamide group also had a roughly 15% lower rate of new actinic keratoses, compared with the placebo group.
“Nicotinamide was very well tolerated. There was no difference in adverse events, blood parameters, or blood pressure in the two arms” of the study, reported Dr. Damian. She stressed that it is critically important to distinguish nicotinamide from niacin (nicotinic acid), another form of vitamin B3 that has a host of side effects such as headache and flushing.
“One of the great things about [nicotinamide] is that it really has hardly any drug interactions, which means that elderly patients who may be taking a whole cocktail of medications for their heart disease and their hypertension, and whatever else, the nicotinamide won’t interact with those,” she added.
Some evidence also has shown nonsteroidal anti-inflammatory drugs to reduce the risk of skin cancer. “The advantage of nicotinamide is that it doesn’t have the potential gastrointestinal bleeding or renal side effects of nonsteroidals, so it may be suitable for a group of people who aren’t suitable for taking nonsteroidals,” she said. “In our ONTRAC study, we didn’t find synergy or additional benefit in people who were coincidentally taking nonsteroidals for other indications.”
The trial’s results should be generalizable to similar high-risk patients in less sunny parts of the world, Dr. Damian said. “If their skin has shown that degree of damage to get skin cancer, then we suspect nicotinamide would offer benefits to them as well.”
Dr. Damian disclosed no relevant conflicts of interest. The study was funded by the National Health & Medical Research Council.
Nicotinamide, an inexpensive, over-the-counter form of vitamin B3, is safe and efficacious for the chemoprevention of nonmelanoma skin cancer in patients at high risk, according to data from the Australian Oral Nicotinamide to Reduce Actinic Cancer (ONTRAC) Study.
Results reported in a press briefing held before the annual meeting of the American Society of Clinical Oncology showed that patients taking nicotinamide were about one-fourth less likely than peers taking a placebo to develop new basal cell and squamous cell skin cancers. They also had a smaller reduction in new actinic keratoses.
“Nicotinamide, vitamin B3, significantly reduced nonmelanoma skin cancers and keratoses in just 12 months in a group of pretty high-risk patients. It’s safe, it’s almost obscenely inexpensive, and it’s already widely commercially available, so this one’s ready to go straight into the clinic,” commented senior investigator Dr. Diona Damian, professor of dermatology at the University of Sydney.
She cautioned that the results apply only to the population studied: adults who had experienced two or more nonmelanoma skin cancers in the past 5 years.
“These are the people we’d be recommending it for – people who have already got a skin cancer track record. It’s not something that we’d recommend at this stage for the general population,” she said. Likewise, the findings do not speak to patients at the other end of the spectrum who are in treatment for advanced or metastatic skin cancer, as they also were excluded.
That said, the researchers are planning additional studies in other populations, such patients who are at high risk because they have immunosuppression, according to Dr. Damian.
“We still need the overall skin cancer prevention strategies of sun-safe behavior, sunscreen, and regular skin surveillance,” she stressed, “but we now have an additional exciting opportunity for affordable skin cancer chemoprevention which we can instantly translate into clinical practice.”
Dr. Peter Paul Yu, ASCO President and a medical oncologist and hematologist who is director of cancer research at the Palo Alto Medical Foundation, Sunnyvale, Calif., commented, “This is a very exciting prevention trial. We all know that we clamor for preventing rather than treating diseases, and this is a major advance for us.”
Exposure to ultraviolet light packs a one-two punch to the skin, both damaging cellular DNA and suppressing the skin’s immune response, according to Dr. Damian. The investigators opted to test nicotinamide as it counters both of these events.
The 386 patients in ONTRAC had heavily sun damaged skin, with a mean of 8 nonmelanoma skin cancers in the past 5 years and 50 keratoses at baseline. They were randomized evenly to receive nicotinamide (500 mg twice daily) or placebo for 12 months.
Results showed that the average number of new nonmelanoma skin cancers per patient during the treatment period was 1.77 in the nicotinamide group and 2.42 in the placebo group. The difference translated to a 23% lower rate of new cancers with the vitamin.
“There were comparable reductions seen for both basal and squamous cell carcinomas,” Dr. Damian noted. “Interestingly, this reduction in skin cancers seemed to start as early as the first 3-month visit. And then when people stopped taking their tablets after 12 months, the benefit was no longer seen. In other words, you need to continue taking the tablets in order for them to be effective.”
The nicotinamide group also had a roughly 15% lower rate of new actinic keratoses, compared with the placebo group.
“Nicotinamide was very well tolerated. There was no difference in adverse events, blood parameters, or blood pressure in the two arms” of the study, reported Dr. Damian. She stressed that it is critically important to distinguish nicotinamide from niacin (nicotinic acid), another form of vitamin B3 that has a host of side effects such as headache and flushing.
“One of the great things about [nicotinamide] is that it really has hardly any drug interactions, which means that elderly patients who may be taking a whole cocktail of medications for their heart disease and their hypertension, and whatever else, the nicotinamide won’t interact with those,” she added.
Some evidence also has shown nonsteroidal anti-inflammatory drugs to reduce the risk of skin cancer. “The advantage of nicotinamide is that it doesn’t have the potential gastrointestinal bleeding or renal side effects of nonsteroidals, so it may be suitable for a group of people who aren’t suitable for taking nonsteroidals,” she said. “In our ONTRAC study, we didn’t find synergy or additional benefit in people who were coincidentally taking nonsteroidals for other indications.”
The trial’s results should be generalizable to similar high-risk patients in less sunny parts of the world, Dr. Damian said. “If their skin has shown that degree of damage to get skin cancer, then we suspect nicotinamide would offer benefits to them as well.”
Dr. Damian disclosed no relevant conflicts of interest. The study was funded by the National Health & Medical Research Council.
FROM THE ASCO 2015 PRESSCAST
Key clinical point: Nicotinamide, an inexpensive oral vitamin, protects against nonmelanoma skin cancer in patients at high risk.
Major finding: Patients taking nicotinamide had a 23% lower rate of new basal cell and squamous cell carcinomas.
Data source: A randomized, placebo-controlled phase III trial among 386 patients with past nonmelanoma skin cancers.
Disclosures: Dr. Damian disclosed no relevant conflicts of interest. The study was funded by the National Health & Medical Research Council.
Managing open wounds in ob.gyn.
Negative pressure wound therapy is a wound management system for chronic open subcutaneous or intra-abdominal wounds. Some popular commercial systems include V.A.C. therapy (KCI, San Antonio) and the Chariker-Jeter wound-sealing kit (Smith and Nephew, London). Within ob.gyn. and gynecologic oncology, they have use in the management of postoperative superficial wound dehiscence from routine surgery and in the management of the open abdomen.
The primary benefit of negative pressure wound therapy (NPWT) is the acceleration of wound healing. Postoperative superficial wound dehiscence can occur as a result of surgical factors such as wound infection and subcutaneous seroma/hematoma or systematic factors such as poor nutrition and wound ischemia.
Acceleration of wound healing results from the design of the NPWT systems. They consist of semipermeable dressings (foam), sealed with an adhesive sheet that is connected to a portable pump. By the application of –50 to –175 mm Hg of continuous or intermittent suction, the edges of the wound are drawn together, and this deforming process promotes tissue remodeling at the cellular level. Other potential benefits of negative pressure are increased blood flow, a decrease in mediators of inflammation, and an increase in collagen organization via changes in wound biochemistry.
An alternative to NPWT would be traditional gauze dressings, which can also be applied in the case of superficial wound dehiscence. These are changed up to three times a day, however, and this can result in significant patient discomfort, caregiver difficulties, and prolonged healing of weeks to months. In contrast, NPWT dressings are changed once every 2-3 days. They are also versatile and can be fit to traditionally shaped abdominal wounds, as well as difficult to dress vulvar and groin wounds (J. Obstet. Gynaecol. Can. 2011;33:1031-7).
In a series of 27 gynecologic oncology patients in whom NPWT was employed after primary wound–healing failure, there was a 96% reduction in the size of the wounds with a median number of therapy days of 32 (range, 3-88). The majority of these patients were also managed as outpatients without complication (Gynecol. Oncol. 2004;92:586-91).
There are some contraindications to NPWT that should be considered. The major, and perhaps most common, is an ongoing wound infection.
A wound that needs to be evaluated at least daily to assess the response to antibiotic therapy or need for debridement should not be managed with NPWT until the wound is deemed stable. There should be no devitalized tissue present in the wound upon application of the NPWT. If any necrotic tissue is present, then wound debridement is warranted until only well-vascularized tissue remains.
Another contraindication is the presence of malignant tissue in the wound. Negative pressure can promote this tissue growth and lead to chronic nonhealing. Other considerations would include adhesive allergies and fragile skin due to chronic steroid use or collagen vascular disorders, as NPWT can lead to skin necrosis.
Finally, the involvement of vital organs, such as exposed bowel, is a contraindication to the NPWT systems, as constant suction can promote fistula formation or hemorrhage. However, in the setting of an open abdomen after trauma surgery, there has been the development of intra-abdominal wound management systems that may be appropriate.
Although rare in obstetrics, gynecology, and gynecologic oncology, delayed abdominal closure may be necessary. This can occur after reoperation for bowel injury, in cases where bowel wall edema and increased intra-abdominal pressure preclude closure, or in cases of massive hemorrhage (for example, ruptured ectopic pregnancy) where patient instability necessitates rapid termination of the surgical case. These wounds can be managed with temporary abdominal closure techniques such as retention sutures, a Bogota bag, or loose packing (World. J. Surg. 2015; 39: 912-25).
The negative pressure systems developed for these instances are the V.A.C. abdominal dressing (KCI), Renasys NPWT (Smith and Nephew), and ABThera open abdomen negative pressure therapy (KCI). They consist of a perforated plastic sheet with foam attachments that is placed directly in the abdomen to cover the intestine. This is then covered with an adhesive dressing that is cut to accommodate the suction attachment for the negative pressure pump. This setup is easily applied and taken down, and therefore facilitates frequent abdominal washouts until true facial closure can be achieved.
There are many benefits to NPWT for the management of superficial and deep wound dehiscence in the ob.gyn. or gynecologic oncology patient. NPWT should be considered primarily with any surgical wound healing by secondary intention.
Dr. Doll is a third-year fellow in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. The authors reported having no relevant financial disclosures.
Negative pressure wound therapy is a wound management system for chronic open subcutaneous or intra-abdominal wounds. Some popular commercial systems include V.A.C. therapy (KCI, San Antonio) and the Chariker-Jeter wound-sealing kit (Smith and Nephew, London). Within ob.gyn. and gynecologic oncology, they have use in the management of postoperative superficial wound dehiscence from routine surgery and in the management of the open abdomen.
The primary benefit of negative pressure wound therapy (NPWT) is the acceleration of wound healing. Postoperative superficial wound dehiscence can occur as a result of surgical factors such as wound infection and subcutaneous seroma/hematoma or systematic factors such as poor nutrition and wound ischemia.
Acceleration of wound healing results from the design of the NPWT systems. They consist of semipermeable dressings (foam), sealed with an adhesive sheet that is connected to a portable pump. By the application of –50 to –175 mm Hg of continuous or intermittent suction, the edges of the wound are drawn together, and this deforming process promotes tissue remodeling at the cellular level. Other potential benefits of negative pressure are increased blood flow, a decrease in mediators of inflammation, and an increase in collagen organization via changes in wound biochemistry.
An alternative to NPWT would be traditional gauze dressings, which can also be applied in the case of superficial wound dehiscence. These are changed up to three times a day, however, and this can result in significant patient discomfort, caregiver difficulties, and prolonged healing of weeks to months. In contrast, NPWT dressings are changed once every 2-3 days. They are also versatile and can be fit to traditionally shaped abdominal wounds, as well as difficult to dress vulvar and groin wounds (J. Obstet. Gynaecol. Can. 2011;33:1031-7).
In a series of 27 gynecologic oncology patients in whom NPWT was employed after primary wound–healing failure, there was a 96% reduction in the size of the wounds with a median number of therapy days of 32 (range, 3-88). The majority of these patients were also managed as outpatients without complication (Gynecol. Oncol. 2004;92:586-91).
There are some contraindications to NPWT that should be considered. The major, and perhaps most common, is an ongoing wound infection.
A wound that needs to be evaluated at least daily to assess the response to antibiotic therapy or need for debridement should not be managed with NPWT until the wound is deemed stable. There should be no devitalized tissue present in the wound upon application of the NPWT. If any necrotic tissue is present, then wound debridement is warranted until only well-vascularized tissue remains.
Another contraindication is the presence of malignant tissue in the wound. Negative pressure can promote this tissue growth and lead to chronic nonhealing. Other considerations would include adhesive allergies and fragile skin due to chronic steroid use or collagen vascular disorders, as NPWT can lead to skin necrosis.
Finally, the involvement of vital organs, such as exposed bowel, is a contraindication to the NPWT systems, as constant suction can promote fistula formation or hemorrhage. However, in the setting of an open abdomen after trauma surgery, there has been the development of intra-abdominal wound management systems that may be appropriate.
Although rare in obstetrics, gynecology, and gynecologic oncology, delayed abdominal closure may be necessary. This can occur after reoperation for bowel injury, in cases where bowel wall edema and increased intra-abdominal pressure preclude closure, or in cases of massive hemorrhage (for example, ruptured ectopic pregnancy) where patient instability necessitates rapid termination of the surgical case. These wounds can be managed with temporary abdominal closure techniques such as retention sutures, a Bogota bag, or loose packing (World. J. Surg. 2015; 39: 912-25).
The negative pressure systems developed for these instances are the V.A.C. abdominal dressing (KCI), Renasys NPWT (Smith and Nephew), and ABThera open abdomen negative pressure therapy (KCI). They consist of a perforated plastic sheet with foam attachments that is placed directly in the abdomen to cover the intestine. This is then covered with an adhesive dressing that is cut to accommodate the suction attachment for the negative pressure pump. This setup is easily applied and taken down, and therefore facilitates frequent abdominal washouts until true facial closure can be achieved.
There are many benefits to NPWT for the management of superficial and deep wound dehiscence in the ob.gyn. or gynecologic oncology patient. NPWT should be considered primarily with any surgical wound healing by secondary intention.
Dr. Doll is a third-year fellow in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. The authors reported having no relevant financial disclosures.
Negative pressure wound therapy is a wound management system for chronic open subcutaneous or intra-abdominal wounds. Some popular commercial systems include V.A.C. therapy (KCI, San Antonio) and the Chariker-Jeter wound-sealing kit (Smith and Nephew, London). Within ob.gyn. and gynecologic oncology, they have use in the management of postoperative superficial wound dehiscence from routine surgery and in the management of the open abdomen.
The primary benefit of negative pressure wound therapy (NPWT) is the acceleration of wound healing. Postoperative superficial wound dehiscence can occur as a result of surgical factors such as wound infection and subcutaneous seroma/hematoma or systematic factors such as poor nutrition and wound ischemia.
Acceleration of wound healing results from the design of the NPWT systems. They consist of semipermeable dressings (foam), sealed with an adhesive sheet that is connected to a portable pump. By the application of –50 to –175 mm Hg of continuous or intermittent suction, the edges of the wound are drawn together, and this deforming process promotes tissue remodeling at the cellular level. Other potential benefits of negative pressure are increased blood flow, a decrease in mediators of inflammation, and an increase in collagen organization via changes in wound biochemistry.
An alternative to NPWT would be traditional gauze dressings, which can also be applied in the case of superficial wound dehiscence. These are changed up to three times a day, however, and this can result in significant patient discomfort, caregiver difficulties, and prolonged healing of weeks to months. In contrast, NPWT dressings are changed once every 2-3 days. They are also versatile and can be fit to traditionally shaped abdominal wounds, as well as difficult to dress vulvar and groin wounds (J. Obstet. Gynaecol. Can. 2011;33:1031-7).
In a series of 27 gynecologic oncology patients in whom NPWT was employed after primary wound–healing failure, there was a 96% reduction in the size of the wounds with a median number of therapy days of 32 (range, 3-88). The majority of these patients were also managed as outpatients without complication (Gynecol. Oncol. 2004;92:586-91).
There are some contraindications to NPWT that should be considered. The major, and perhaps most common, is an ongoing wound infection.
A wound that needs to be evaluated at least daily to assess the response to antibiotic therapy or need for debridement should not be managed with NPWT until the wound is deemed stable. There should be no devitalized tissue present in the wound upon application of the NPWT. If any necrotic tissue is present, then wound debridement is warranted until only well-vascularized tissue remains.
Another contraindication is the presence of malignant tissue in the wound. Negative pressure can promote this tissue growth and lead to chronic nonhealing. Other considerations would include adhesive allergies and fragile skin due to chronic steroid use or collagen vascular disorders, as NPWT can lead to skin necrosis.
Finally, the involvement of vital organs, such as exposed bowel, is a contraindication to the NPWT systems, as constant suction can promote fistula formation or hemorrhage. However, in the setting of an open abdomen after trauma surgery, there has been the development of intra-abdominal wound management systems that may be appropriate.
Although rare in obstetrics, gynecology, and gynecologic oncology, delayed abdominal closure may be necessary. This can occur after reoperation for bowel injury, in cases where bowel wall edema and increased intra-abdominal pressure preclude closure, or in cases of massive hemorrhage (for example, ruptured ectopic pregnancy) where patient instability necessitates rapid termination of the surgical case. These wounds can be managed with temporary abdominal closure techniques such as retention sutures, a Bogota bag, or loose packing (World. J. Surg. 2015; 39: 912-25).
The negative pressure systems developed for these instances are the V.A.C. abdominal dressing (KCI), Renasys NPWT (Smith and Nephew), and ABThera open abdomen negative pressure therapy (KCI). They consist of a perforated plastic sheet with foam attachments that is placed directly in the abdomen to cover the intestine. This is then covered with an adhesive dressing that is cut to accommodate the suction attachment for the negative pressure pump. This setup is easily applied and taken down, and therefore facilitates frequent abdominal washouts until true facial closure can be achieved.
There are many benefits to NPWT for the management of superficial and deep wound dehiscence in the ob.gyn. or gynecologic oncology patient. NPWT should be considered primarily with any surgical wound healing by secondary intention.
Dr. Doll is a third-year fellow in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. The authors reported having no relevant financial disclosures.
Adding mAb to treatment extends PFS in MM

Photo by Linda Bartlett
The monoclonal antibody (mAb) elotuzumab may be a useful addition to the multiple myeloma (MM) arsenal, according to investigators involved in the phase 3 ELOQUENT-2 trial.
The trial showed that adding elotuzumab to treatment with lenalidomide and dexamethasone extended progression-free survival (PFS) in relapsed MM patients by about 5 months, on average, when compared to treatment with just lenalidomide and dexamethasone.
“It appears that, for patients with relapsed multiple myeloma who would otherwise be offered lenalidomide and dexamethasone, addition of this new targeted drug makes the outcomes even better,” said study investigator Sagar Lonial, MD, of Emory University in Atlanta, Georgia.
Dr Lonial presented data from ELOQUENT-2 at a presscast in advance of the 2015 ASCO Annual Meeting. Full data from the study will be presented at the meeting on June 2 as abstract 8508.
The study was funded by Bristol-Myers Squibb and AbbVie, the companies developing elotuzumab.
Dr Lonial explained that elotuzumab attaches to the cell surface protein SLAMF7, which is found on MM cells and natural killer (NK) cells. Scientists believe that elotuzumab mounts a 2-pronged attack on MM by targeting myeloma cells directly and by enhancing NK cells’ ability to kill myeloma cells.
In ELOQUENT-2, 646 patients with recurrent MM were randomized to receive elotuzumab plus lenalidomide and dexamethasone or only lenalidomide and dexamethasone (control).
The patients’ median age was 66. They had failed 1 to 3 prior treatments, and 35% of them were refractory to their last therapy. Thirty-two percent of patients had del(17p), and 9% had t[4;14].
At a median follow-up of 24 months, elotuzumab had reduced the risk of MM progression and death by 30%. Patients in the elotuzumab arm had significantly longer PFS than patients in the control arm—a median of 19.4 months and 14.9 months, respectively (P=0.0004).
The 1-year PFS was 68% in the elotuzumab arm and 57% in the control arm. The 2-year PFS was 41% and 27%, respectively. Dr Lonial pointed out that, unlike some other therapies, elotuzumab continued to improve PFS over time.
“[T]he idea of the maintenance of benefit over time really speaks to the power of an immune-based approach when we treat cancer,” he said.
“Patients who received elotuzumab had a longer duration of remission [and] a higher overall response rate, and this improvement in clinical parameters occurred without a significant increase in adverse events or toxicity. In fact, there was no reduction in quality of life for [patients in the] 3-drug arm.”
Mild infusion reactions occurred after the first few doses in 10% of patients who received elotuzumab. Most of these reactions were grade 1 or 2.
Common grade 3-4 adverse events (occurring in ≥ 15% of patients) in both the elotuzumab and control arms were neutropenia (25% and 33%, respectively) and anemia (15% and 16%, respectively).
In all, 210 patients died, 94 in the elotuzumab arm and 116 in the control arm.
“Based on this randomized, phase 3 trial, we hope that we will soon have a new treatment option for patients with relapsed or refractory myeloma . . . ,” Dr Lonial said.
The US Food and Drug Administration has already granted elotuzumab breakthrough therapy designation to treat MM patients who have received at least 1 prior therapy. ![]()

Photo by Linda Bartlett
The monoclonal antibody (mAb) elotuzumab may be a useful addition to the multiple myeloma (MM) arsenal, according to investigators involved in the phase 3 ELOQUENT-2 trial.
The trial showed that adding elotuzumab to treatment with lenalidomide and dexamethasone extended progression-free survival (PFS) in relapsed MM patients by about 5 months, on average, when compared to treatment with just lenalidomide and dexamethasone.
“It appears that, for patients with relapsed multiple myeloma who would otherwise be offered lenalidomide and dexamethasone, addition of this new targeted drug makes the outcomes even better,” said study investigator Sagar Lonial, MD, of Emory University in Atlanta, Georgia.
Dr Lonial presented data from ELOQUENT-2 at a presscast in advance of the 2015 ASCO Annual Meeting. Full data from the study will be presented at the meeting on June 2 as abstract 8508.
The study was funded by Bristol-Myers Squibb and AbbVie, the companies developing elotuzumab.
Dr Lonial explained that elotuzumab attaches to the cell surface protein SLAMF7, which is found on MM cells and natural killer (NK) cells. Scientists believe that elotuzumab mounts a 2-pronged attack on MM by targeting myeloma cells directly and by enhancing NK cells’ ability to kill myeloma cells.
In ELOQUENT-2, 646 patients with recurrent MM were randomized to receive elotuzumab plus lenalidomide and dexamethasone or only lenalidomide and dexamethasone (control).
The patients’ median age was 66. They had failed 1 to 3 prior treatments, and 35% of them were refractory to their last therapy. Thirty-two percent of patients had del(17p), and 9% had t[4;14].
At a median follow-up of 24 months, elotuzumab had reduced the risk of MM progression and death by 30%. Patients in the elotuzumab arm had significantly longer PFS than patients in the control arm—a median of 19.4 months and 14.9 months, respectively (P=0.0004).
The 1-year PFS was 68% in the elotuzumab arm and 57% in the control arm. The 2-year PFS was 41% and 27%, respectively. Dr Lonial pointed out that, unlike some other therapies, elotuzumab continued to improve PFS over time.
“[T]he idea of the maintenance of benefit over time really speaks to the power of an immune-based approach when we treat cancer,” he said.
“Patients who received elotuzumab had a longer duration of remission [and] a higher overall response rate, and this improvement in clinical parameters occurred without a significant increase in adverse events or toxicity. In fact, there was no reduction in quality of life for [patients in the] 3-drug arm.”
Mild infusion reactions occurred after the first few doses in 10% of patients who received elotuzumab. Most of these reactions were grade 1 or 2.
Common grade 3-4 adverse events (occurring in ≥ 15% of patients) in both the elotuzumab and control arms were neutropenia (25% and 33%, respectively) and anemia (15% and 16%, respectively).
In all, 210 patients died, 94 in the elotuzumab arm and 116 in the control arm.
“Based on this randomized, phase 3 trial, we hope that we will soon have a new treatment option for patients with relapsed or refractory myeloma . . . ,” Dr Lonial said.
The US Food and Drug Administration has already granted elotuzumab breakthrough therapy designation to treat MM patients who have received at least 1 prior therapy. ![]()

Photo by Linda Bartlett
The monoclonal antibody (mAb) elotuzumab may be a useful addition to the multiple myeloma (MM) arsenal, according to investigators involved in the phase 3 ELOQUENT-2 trial.
The trial showed that adding elotuzumab to treatment with lenalidomide and dexamethasone extended progression-free survival (PFS) in relapsed MM patients by about 5 months, on average, when compared to treatment with just lenalidomide and dexamethasone.
“It appears that, for patients with relapsed multiple myeloma who would otherwise be offered lenalidomide and dexamethasone, addition of this new targeted drug makes the outcomes even better,” said study investigator Sagar Lonial, MD, of Emory University in Atlanta, Georgia.
Dr Lonial presented data from ELOQUENT-2 at a presscast in advance of the 2015 ASCO Annual Meeting. Full data from the study will be presented at the meeting on June 2 as abstract 8508.
The study was funded by Bristol-Myers Squibb and AbbVie, the companies developing elotuzumab.
Dr Lonial explained that elotuzumab attaches to the cell surface protein SLAMF7, which is found on MM cells and natural killer (NK) cells. Scientists believe that elotuzumab mounts a 2-pronged attack on MM by targeting myeloma cells directly and by enhancing NK cells’ ability to kill myeloma cells.
In ELOQUENT-2, 646 patients with recurrent MM were randomized to receive elotuzumab plus lenalidomide and dexamethasone or only lenalidomide and dexamethasone (control).
The patients’ median age was 66. They had failed 1 to 3 prior treatments, and 35% of them were refractory to their last therapy. Thirty-two percent of patients had del(17p), and 9% had t[4;14].
At a median follow-up of 24 months, elotuzumab had reduced the risk of MM progression and death by 30%. Patients in the elotuzumab arm had significantly longer PFS than patients in the control arm—a median of 19.4 months and 14.9 months, respectively (P=0.0004).
The 1-year PFS was 68% in the elotuzumab arm and 57% in the control arm. The 2-year PFS was 41% and 27%, respectively. Dr Lonial pointed out that, unlike some other therapies, elotuzumab continued to improve PFS over time.
“[T]he idea of the maintenance of benefit over time really speaks to the power of an immune-based approach when we treat cancer,” he said.
“Patients who received elotuzumab had a longer duration of remission [and] a higher overall response rate, and this improvement in clinical parameters occurred without a significant increase in adverse events or toxicity. In fact, there was no reduction in quality of life for [patients in the] 3-drug arm.”
Mild infusion reactions occurred after the first few doses in 10% of patients who received elotuzumab. Most of these reactions were grade 1 or 2.
Common grade 3-4 adverse events (occurring in ≥ 15% of patients) in both the elotuzumab and control arms were neutropenia (25% and 33%, respectively) and anemia (15% and 16%, respectively).
In all, 210 patients died, 94 in the elotuzumab arm and 116 in the control arm.
“Based on this randomized, phase 3 trial, we hope that we will soon have a new treatment option for patients with relapsed or refractory myeloma . . . ,” Dr Lonial said.
The US Food and Drug Administration has already granted elotuzumab breakthrough therapy designation to treat MM patients who have received at least 1 prior therapy. ![]()
Modified T cells may treat GVHD
Image from PLOS ONE
A T-cell therapy designed to mitigate graft-vs-host disease (GVHD) is both feasible and safe, according to results of a pilot study published in Molecular Therapy.
To create this therapy, researchers transduced donor T cells with γ-retroviruses carrying a CD34-TK75 fusion gene.
The team said this allows them to track the cells via PET/CT and induce apoptosis by administering the antiviral drug ganciclovir if patients begin showing signs of GVHD.
“If donor T cells expand and cause severe graft-vs-host disease, we can give the patient ganciclovir, and it should kill the T cells and stop the process,” said study author John F. DiPersio, MD, PhD, of the Washington University School of Medicine in St Louis, Missouri.
Dr DiPersio and his colleagues tested the CD34-TK75-enriched T cells in 8 patients—4 with acute myeloid leukemia and 4 with myelodysplastic syndromes—who relapsed after allogeneic transplant. Six patients underwent [18F]FHBG PET/CT to track the T cells at several time points after infusion.
Patients received T-cell infusions ranging from 0.1 × 106 cells/kg to 1.3 × 106 cells/kg. Seven of the 8 patients received chemotherapy before T-cell infusion.
Four patients achieved a complete remission, 1 had progressive disease, and 3 patients died before the researchers could evaluate them for response.
Two patients developed GVHD—1 before T-cell infusion and 1 after. The patient who developed GVHD before infusion had grade 2 liver GVHD that resolved after an increased dose of steroids. The patient ultimately died of relapsed leukemia.
The patient who developed GVHD after T-cell infusion did not respond to chemotherapy or T-cell infusion. At 64 days after infusion, he exhibited symptoms consistent with grade 4 liver GVHD. He was treated with high-dose steroids and ganciclovir but did not respond. His primary cause of death was relapsed/progressive disease.
The mean overall survival after T-cell infusion was 165 days, 4 patients were still alive at 6 months, and 1 patient lived 408 days. All of the patients ultimately died.
The researchers said they did not detect any replication competent retrovirus or any antibodies against CD34-TK in any of the patients. The team also said there were no toxicities related to the CD34-TK75-enriched T cells.
Among patients who underwent imaging, there was no clear distinction between the [18F]FHBG biodistribution at baseline and later time points. And there was no difference between images in the patient who developed GVHD after infusion and patients who did not.
Past work from Dr DiPersio’s lab showed that leukemic mice that receive donor T cells and go on to develop GVHD show a characteristic migration pattern of the T cells through the body. When the cells gather early in the thymus, the mice develop GVHD. When T cells don’t migrate to the thymus, GVHD doesn’t occur.
In the current study, the patients received a relatively small number of CD34-TK75-enriched T cells, so the researchers were not able to show whether the migration patterns in mice were similar in humans.
However, based on the results of this study, Dr DiPersio and his colleagues are participating in a larger trial in partnership with a company based in Italy. The researchers are planning to include patients from multiple medical centers, and each participant should receive about 50 times more of the CD34-TK75-enriched T cells than were administered in this trial.
Washington University is the only center in the new trial that will be able to perform the imaging studies examining migration patterns of the T cells. ![]()
Image from PLOS ONE
A T-cell therapy designed to mitigate graft-vs-host disease (GVHD) is both feasible and safe, according to results of a pilot study published in Molecular Therapy.
To create this therapy, researchers transduced donor T cells with γ-retroviruses carrying a CD34-TK75 fusion gene.
The team said this allows them to track the cells via PET/CT and induce apoptosis by administering the antiviral drug ganciclovir if patients begin showing signs of GVHD.
“If donor T cells expand and cause severe graft-vs-host disease, we can give the patient ganciclovir, and it should kill the T cells and stop the process,” said study author John F. DiPersio, MD, PhD, of the Washington University School of Medicine in St Louis, Missouri.
Dr DiPersio and his colleagues tested the CD34-TK75-enriched T cells in 8 patients—4 with acute myeloid leukemia and 4 with myelodysplastic syndromes—who relapsed after allogeneic transplant. Six patients underwent [18F]FHBG PET/CT to track the T cells at several time points after infusion.
Patients received T-cell infusions ranging from 0.1 × 106 cells/kg to 1.3 × 106 cells/kg. Seven of the 8 patients received chemotherapy before T-cell infusion.
Four patients achieved a complete remission, 1 had progressive disease, and 3 patients died before the researchers could evaluate them for response.
Two patients developed GVHD—1 before T-cell infusion and 1 after. The patient who developed GVHD before infusion had grade 2 liver GVHD that resolved after an increased dose of steroids. The patient ultimately died of relapsed leukemia.
The patient who developed GVHD after T-cell infusion did not respond to chemotherapy or T-cell infusion. At 64 days after infusion, he exhibited symptoms consistent with grade 4 liver GVHD. He was treated with high-dose steroids and ganciclovir but did not respond. His primary cause of death was relapsed/progressive disease.
The mean overall survival after T-cell infusion was 165 days, 4 patients were still alive at 6 months, and 1 patient lived 408 days. All of the patients ultimately died.
The researchers said they did not detect any replication competent retrovirus or any antibodies against CD34-TK in any of the patients. The team also said there were no toxicities related to the CD34-TK75-enriched T cells.
Among patients who underwent imaging, there was no clear distinction between the [18F]FHBG biodistribution at baseline and later time points. And there was no difference between images in the patient who developed GVHD after infusion and patients who did not.
Past work from Dr DiPersio’s lab showed that leukemic mice that receive donor T cells and go on to develop GVHD show a characteristic migration pattern of the T cells through the body. When the cells gather early in the thymus, the mice develop GVHD. When T cells don’t migrate to the thymus, GVHD doesn’t occur.
In the current study, the patients received a relatively small number of CD34-TK75-enriched T cells, so the researchers were not able to show whether the migration patterns in mice were similar in humans.
However, based on the results of this study, Dr DiPersio and his colleagues are participating in a larger trial in partnership with a company based in Italy. The researchers are planning to include patients from multiple medical centers, and each participant should receive about 50 times more of the CD34-TK75-enriched T cells than were administered in this trial.
Washington University is the only center in the new trial that will be able to perform the imaging studies examining migration patterns of the T cells. ![]()
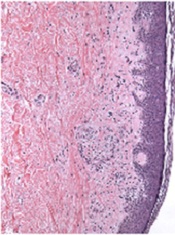
Image from PLOS ONE
A T-cell therapy designed to mitigate graft-vs-host disease (GVHD) is both feasible and safe, according to results of a pilot study published in Molecular Therapy.
To create this therapy, researchers transduced donor T cells with γ-retroviruses carrying a CD34-TK75 fusion gene.
The team said this allows them to track the cells via PET/CT and induce apoptosis by administering the antiviral drug ganciclovir if patients begin showing signs of GVHD.
“If donor T cells expand and cause severe graft-vs-host disease, we can give the patient ganciclovir, and it should kill the T cells and stop the process,” said study author John F. DiPersio, MD, PhD, of the Washington University School of Medicine in St Louis, Missouri.
Dr DiPersio and his colleagues tested the CD34-TK75-enriched T cells in 8 patients—4 with acute myeloid leukemia and 4 with myelodysplastic syndromes—who relapsed after allogeneic transplant. Six patients underwent [18F]FHBG PET/CT to track the T cells at several time points after infusion.
Patients received T-cell infusions ranging from 0.1 × 106 cells/kg to 1.3 × 106 cells/kg. Seven of the 8 patients received chemotherapy before T-cell infusion.
Four patients achieved a complete remission, 1 had progressive disease, and 3 patients died before the researchers could evaluate them for response.
Two patients developed GVHD—1 before T-cell infusion and 1 after. The patient who developed GVHD before infusion had grade 2 liver GVHD that resolved after an increased dose of steroids. The patient ultimately died of relapsed leukemia.
The patient who developed GVHD after T-cell infusion did not respond to chemotherapy or T-cell infusion. At 64 days after infusion, he exhibited symptoms consistent with grade 4 liver GVHD. He was treated with high-dose steroids and ganciclovir but did not respond. His primary cause of death was relapsed/progressive disease.
The mean overall survival after T-cell infusion was 165 days, 4 patients were still alive at 6 months, and 1 patient lived 408 days. All of the patients ultimately died.
The researchers said they did not detect any replication competent retrovirus or any antibodies against CD34-TK in any of the patients. The team also said there were no toxicities related to the CD34-TK75-enriched T cells.
Among patients who underwent imaging, there was no clear distinction between the [18F]FHBG biodistribution at baseline and later time points. And there was no difference between images in the patient who developed GVHD after infusion and patients who did not.
Past work from Dr DiPersio’s lab showed that leukemic mice that receive donor T cells and go on to develop GVHD show a characteristic migration pattern of the T cells through the body. When the cells gather early in the thymus, the mice develop GVHD. When T cells don’t migrate to the thymus, GVHD doesn’t occur.
In the current study, the patients received a relatively small number of CD34-TK75-enriched T cells, so the researchers were not able to show whether the migration patterns in mice were similar in humans.
However, based on the results of this study, Dr DiPersio and his colleagues are participating in a larger trial in partnership with a company based in Italy. The researchers are planning to include patients from multiple medical centers, and each participant should receive about 50 times more of the CD34-TK75-enriched T cells than were administered in this trial.
Washington University is the only center in the new trial that will be able to perform the imaging studies examining migration patterns of the T cells. ![]()
Company stops phase 3 PTCL trial

for use in a clinical trial
Photo by Esther Dyson
Takeda Pharmaceutical Company Limited has announced its decision to discontinue its phase 3 trial of the aurora A kinase inhibitor alisertib (MLN8237) in patients with relapsed or refractory peripheral T-cell lymphoma (PTCL).
Results of a pre-specified interim analysis indicated that alisertib was unlikely to meet the study’s primary endpoint: providing superior progression-free survival over the standard of care for PTCL.
Takeda said patients enrolled in the trial may continue to receive alisertib if they are thought to be benefitting from it and no safety concerns are present.
The company is encouraging patients to consult their study investigators to address any questions and before making any changes to their medication.
Takeda is working with trial investigators and local regulatory authorities to ensure that PTCL patients who participated in the study receive appropriate care.
The company is still investigating alisertib for use in small-cell lung cancer.
“While we are disappointed that alisertib will not be further investigated for relapsed or refractory peripheral T-cell lymphoma, we are optimistic about alisertib’s clinical development program in small-cell lung cancer,” said Michael Vasconcelles, MD, global head of the Takeda Oncology Therapeutic Unit.
“The randomized, phase 2 study of alisertib in small-cell lung cancer will continue as planned and is currently underway. Takeda also continues to support investigator-initiated research with alisertib and will evaluate its potential use in other oncology indications going forward.” ![]()

for use in a clinical trial
Photo by Esther Dyson
Takeda Pharmaceutical Company Limited has announced its decision to discontinue its phase 3 trial of the aurora A kinase inhibitor alisertib (MLN8237) in patients with relapsed or refractory peripheral T-cell lymphoma (PTCL).
Results of a pre-specified interim analysis indicated that alisertib was unlikely to meet the study’s primary endpoint: providing superior progression-free survival over the standard of care for PTCL.
Takeda said patients enrolled in the trial may continue to receive alisertib if they are thought to be benefitting from it and no safety concerns are present.
The company is encouraging patients to consult their study investigators to address any questions and before making any changes to their medication.
Takeda is working with trial investigators and local regulatory authorities to ensure that PTCL patients who participated in the study receive appropriate care.
The company is still investigating alisertib for use in small-cell lung cancer.
“While we are disappointed that alisertib will not be further investigated for relapsed or refractory peripheral T-cell lymphoma, we are optimistic about alisertib’s clinical development program in small-cell lung cancer,” said Michael Vasconcelles, MD, global head of the Takeda Oncology Therapeutic Unit.
“The randomized, phase 2 study of alisertib in small-cell lung cancer will continue as planned and is currently underway. Takeda also continues to support investigator-initiated research with alisertib and will evaluate its potential use in other oncology indications going forward.” ![]()

for use in a clinical trial
Photo by Esther Dyson
Takeda Pharmaceutical Company Limited has announced its decision to discontinue its phase 3 trial of the aurora A kinase inhibitor alisertib (MLN8237) in patients with relapsed or refractory peripheral T-cell lymphoma (PTCL).
Results of a pre-specified interim analysis indicated that alisertib was unlikely to meet the study’s primary endpoint: providing superior progression-free survival over the standard of care for PTCL.
Takeda said patients enrolled in the trial may continue to receive alisertib if they are thought to be benefitting from it and no safety concerns are present.
The company is encouraging patients to consult their study investigators to address any questions and before making any changes to their medication.
Takeda is working with trial investigators and local regulatory authorities to ensure that PTCL patients who participated in the study receive appropriate care.
The company is still investigating alisertib for use in small-cell lung cancer.
“While we are disappointed that alisertib will not be further investigated for relapsed or refractory peripheral T-cell lymphoma, we are optimistic about alisertib’s clinical development program in small-cell lung cancer,” said Michael Vasconcelles, MD, global head of the Takeda Oncology Therapeutic Unit.
“The randomized, phase 2 study of alisertib in small-cell lung cancer will continue as planned and is currently underway. Takeda also continues to support investigator-initiated research with alisertib and will evaluate its potential use in other oncology indications going forward.” ![]()
Equation provides new insight into blood flow

Engineers have devised an equation that yields simple predictions as to how quickly blood cells will migrate away from blood-vessel walls, how they will behave when they collide with each other, and how they will segregate during flow.
In the long run, these insights could help practitioners manipulate the mechanics of blood to design better blood transfusions, new techniques for drug delivery, and new processes for isolating blood-borne tumor cells.
Mike Graham, PhD, of the University of Wisconsin-Madison, and his colleagues described this work in Physical Review Letters.
“I’m really excited about this paper because it’s the first analytical theory for this phenomenon,” Dr Graham said. “It’s not very common that theory is ahead of experiments, but we’re in that position now.”
Dr Graham and his colleagues created complex computer simulations that showed how relatively stiff white blood cells and platelets interact with more flexible red blood cells.
As the different cells collide during blood flow, white cells tend to be pushed toward the walls of a blood vessel. This segregation process, called margination, creates some advantages; for example, letting white blood cells quickly exit the blood vessel to head to the site of an injury or infection.
However, the mechanical details of blood could spell both good news and bad in areas ranging from drug delivery to blood disorders to the spread of disease.
“I view my role as providing a fundamental basis of understanding for practitioners and for other engineers who are more directly connected with applications,” Dr Graham said.
Now, he is aiming to draw a firmer connection between mechanical insights and the biological functions they might impact. His group is working to refine the new equation to suit more complex flow situations and pursuing an experimental collaboration with Wilbur Lam, MD, PhD, a hematologist at Georgia Tech and Emory University in Atlanta.
Building on Dr Graham’s theoretical and simulation work, Dr Lam’s research group is creating microfluidic devices to study the behavior of blood cells. Dr Lam has developed a way to grow endothelial cells inside the artificial channels of the microfluidic devices.
“I think, together, our labs have really stumbled on how fluid mechanics may be able to explain a lot of the biological phenomena we see in blood,” Dr Lam said. “This can be related to a new way of understanding inflammation, infections, even transfusion medicine. It really pervades many different problems we see in hematology.”
Dr Graham said that capturing the physical nuances of blood vessels’ shape, size, and relative stiffness has tremendous value, even given the myriad other forces at work in the human body.
“We’d like to be able to convince practitioners that you don’t have to worry about all the details to capture the fundamental understanding of what’s going on,” Dr Graham said. “It’s extremely challenging to incorporate all the phenomena that might be important into a simulation. You have to make your case convincingly—if you want somebody to apply this research—that you’ve kept the important parts.”
Both researchers pointed out that sickle cell anemia has long been understood as both a mechanical and a biological problem. The defective red blood cells the disease causes are not only misshapen, but also stiffer than healthy red blood cells, meaning they block blood flow.
Yet, on a more detailed mechanical level, Drs Graham and Lam believe that sickle cells may literally poke and irritate the inner walls of blood vessels. If so, that would make sickle cell anemia not just a blood disorder but a disorder of the entire circulatory system. Their combined research strengths now create an opportunity to test that hypothesis.
“Biologists and hematologists have known for decades that these cells can get stuck, but what is less understood is that the blood vessel walls in the entire patient are really inflamed, and we don’t really know why,” Dr Lam said.
The researchers noted that a better understanding of blood-flow mechanics could help to make blood transfusions safer as well. Transfusions can sometimes set off heart attacks or lung damage, and the medical community isn’t entirely sure why. Dr Lam wants to find out if certain cells in stored, donated blood have mechanical properties that put patients at greater risk.
Though the collaboration between Drs Graham and Lam is still in an early stage, both researchers see the possibility of opening a new frontier in blood research.
“This would be a whole new category of things we could be looking at, and that’s why it’s so exciting,” Dr Lam said. “Suddenly, we have applications where the mechanics can be just as important.” ![]()

Engineers have devised an equation that yields simple predictions as to how quickly blood cells will migrate away from blood-vessel walls, how they will behave when they collide with each other, and how they will segregate during flow.
In the long run, these insights could help practitioners manipulate the mechanics of blood to design better blood transfusions, new techniques for drug delivery, and new processes for isolating blood-borne tumor cells.
Mike Graham, PhD, of the University of Wisconsin-Madison, and his colleagues described this work in Physical Review Letters.
“I’m really excited about this paper because it’s the first analytical theory for this phenomenon,” Dr Graham said. “It’s not very common that theory is ahead of experiments, but we’re in that position now.”
Dr Graham and his colleagues created complex computer simulations that showed how relatively stiff white blood cells and platelets interact with more flexible red blood cells.
As the different cells collide during blood flow, white cells tend to be pushed toward the walls of a blood vessel. This segregation process, called margination, creates some advantages; for example, letting white blood cells quickly exit the blood vessel to head to the site of an injury or infection.
However, the mechanical details of blood could spell both good news and bad in areas ranging from drug delivery to blood disorders to the spread of disease.
“I view my role as providing a fundamental basis of understanding for practitioners and for other engineers who are more directly connected with applications,” Dr Graham said.
Now, he is aiming to draw a firmer connection between mechanical insights and the biological functions they might impact. His group is working to refine the new equation to suit more complex flow situations and pursuing an experimental collaboration with Wilbur Lam, MD, PhD, a hematologist at Georgia Tech and Emory University in Atlanta.
Building on Dr Graham’s theoretical and simulation work, Dr Lam’s research group is creating microfluidic devices to study the behavior of blood cells. Dr Lam has developed a way to grow endothelial cells inside the artificial channels of the microfluidic devices.
“I think, together, our labs have really stumbled on how fluid mechanics may be able to explain a lot of the biological phenomena we see in blood,” Dr Lam said. “This can be related to a new way of understanding inflammation, infections, even transfusion medicine. It really pervades many different problems we see in hematology.”
Dr Graham said that capturing the physical nuances of blood vessels’ shape, size, and relative stiffness has tremendous value, even given the myriad other forces at work in the human body.
“We’d like to be able to convince practitioners that you don’t have to worry about all the details to capture the fundamental understanding of what’s going on,” Dr Graham said. “It’s extremely challenging to incorporate all the phenomena that might be important into a simulation. You have to make your case convincingly—if you want somebody to apply this research—that you’ve kept the important parts.”
Both researchers pointed out that sickle cell anemia has long been understood as both a mechanical and a biological problem. The defective red blood cells the disease causes are not only misshapen, but also stiffer than healthy red blood cells, meaning they block blood flow.
Yet, on a more detailed mechanical level, Drs Graham and Lam believe that sickle cells may literally poke and irritate the inner walls of blood vessels. If so, that would make sickle cell anemia not just a blood disorder but a disorder of the entire circulatory system. Their combined research strengths now create an opportunity to test that hypothesis.
“Biologists and hematologists have known for decades that these cells can get stuck, but what is less understood is that the blood vessel walls in the entire patient are really inflamed, and we don’t really know why,” Dr Lam said.
The researchers noted that a better understanding of blood-flow mechanics could help to make blood transfusions safer as well. Transfusions can sometimes set off heart attacks or lung damage, and the medical community isn’t entirely sure why. Dr Lam wants to find out if certain cells in stored, donated blood have mechanical properties that put patients at greater risk.
Though the collaboration between Drs Graham and Lam is still in an early stage, both researchers see the possibility of opening a new frontier in blood research.
“This would be a whole new category of things we could be looking at, and that’s why it’s so exciting,” Dr Lam said. “Suddenly, we have applications where the mechanics can be just as important.” ![]()

Engineers have devised an equation that yields simple predictions as to how quickly blood cells will migrate away from blood-vessel walls, how they will behave when they collide with each other, and how they will segregate during flow.
In the long run, these insights could help practitioners manipulate the mechanics of blood to design better blood transfusions, new techniques for drug delivery, and new processes for isolating blood-borne tumor cells.
Mike Graham, PhD, of the University of Wisconsin-Madison, and his colleagues described this work in Physical Review Letters.
“I’m really excited about this paper because it’s the first analytical theory for this phenomenon,” Dr Graham said. “It’s not very common that theory is ahead of experiments, but we’re in that position now.”
Dr Graham and his colleagues created complex computer simulations that showed how relatively stiff white blood cells and platelets interact with more flexible red blood cells.
As the different cells collide during blood flow, white cells tend to be pushed toward the walls of a blood vessel. This segregation process, called margination, creates some advantages; for example, letting white blood cells quickly exit the blood vessel to head to the site of an injury or infection.
However, the mechanical details of blood could spell both good news and bad in areas ranging from drug delivery to blood disorders to the spread of disease.
“I view my role as providing a fundamental basis of understanding for practitioners and for other engineers who are more directly connected with applications,” Dr Graham said.
Now, he is aiming to draw a firmer connection between mechanical insights and the biological functions they might impact. His group is working to refine the new equation to suit more complex flow situations and pursuing an experimental collaboration with Wilbur Lam, MD, PhD, a hematologist at Georgia Tech and Emory University in Atlanta.
Building on Dr Graham’s theoretical and simulation work, Dr Lam’s research group is creating microfluidic devices to study the behavior of blood cells. Dr Lam has developed a way to grow endothelial cells inside the artificial channels of the microfluidic devices.
“I think, together, our labs have really stumbled on how fluid mechanics may be able to explain a lot of the biological phenomena we see in blood,” Dr Lam said. “This can be related to a new way of understanding inflammation, infections, even transfusion medicine. It really pervades many different problems we see in hematology.”
Dr Graham said that capturing the physical nuances of blood vessels’ shape, size, and relative stiffness has tremendous value, even given the myriad other forces at work in the human body.
“We’d like to be able to convince practitioners that you don’t have to worry about all the details to capture the fundamental understanding of what’s going on,” Dr Graham said. “It’s extremely challenging to incorporate all the phenomena that might be important into a simulation. You have to make your case convincingly—if you want somebody to apply this research—that you’ve kept the important parts.”
Both researchers pointed out that sickle cell anemia has long been understood as both a mechanical and a biological problem. The defective red blood cells the disease causes are not only misshapen, but also stiffer than healthy red blood cells, meaning they block blood flow.
Yet, on a more detailed mechanical level, Drs Graham and Lam believe that sickle cells may literally poke and irritate the inner walls of blood vessels. If so, that would make sickle cell anemia not just a blood disorder but a disorder of the entire circulatory system. Their combined research strengths now create an opportunity to test that hypothesis.
“Biologists and hematologists have known for decades that these cells can get stuck, but what is less understood is that the blood vessel walls in the entire patient are really inflamed, and we don’t really know why,” Dr Lam said.
The researchers noted that a better understanding of blood-flow mechanics could help to make blood transfusions safer as well. Transfusions can sometimes set off heart attacks or lung damage, and the medical community isn’t entirely sure why. Dr Lam wants to find out if certain cells in stored, donated blood have mechanical properties that put patients at greater risk.
Though the collaboration between Drs Graham and Lam is still in an early stage, both researchers see the possibility of opening a new frontier in blood research.
“This would be a whole new category of things we could be looking at, and that’s why it’s so exciting,” Dr Lam said. “Suddenly, we have applications where the mechanics can be just as important.” ![]()
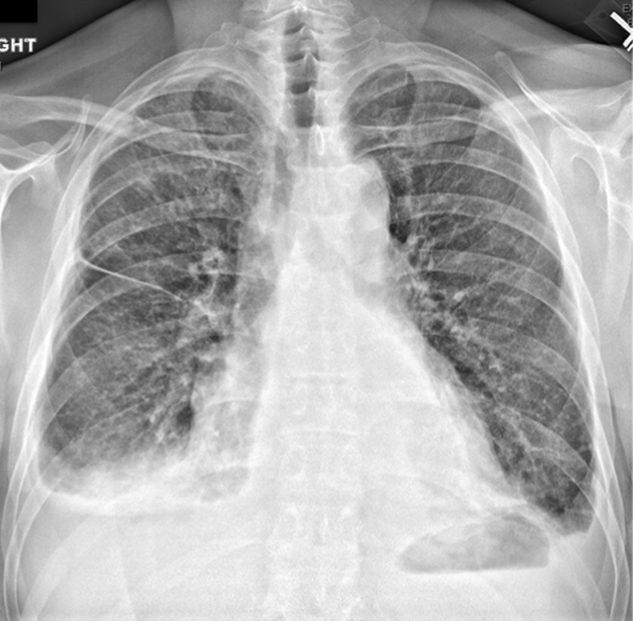
A coat with a clue
A 59‐year‐old man with a history of hypertension was admitted with 6 months of shortness of breath, night sweats, and debilitating fatigue. His symptoms were initially mild and would persist for weeks at a time, after which he would feel better for several days. Over the 2 weeks prior to admission his symptoms had progressed, and he had become dyspneic with minimal exertion.
Progressive dyspnea has a broad differential that includes diseases of the heart (eg, congestive heart failure, aortic stenosis, constrictive pericarditis), lung (eg, chronic obstructive pulmonary disease, interstitial lung disease, pulmonary hypertension, pleural effusion), and blood (eg, anemia).
Night sweats suggest an inflammatory condition, but do not help prioritize infection, malignancy, or autoimmunity. Any of those conditions can be relapsing and remitting, at least in their early phases, but the return to normalcy raises the possibility of hypersensitivity pneumonitis from a periodic exposure.
The 6‐month duration makes typical bacterial and viral infections less likely and suggests indolent infections such as mycobacteria, fungi, or human immunodeficiency virus. Lymphoma or chronic leukemia could cause dyspnea through pleural or pulmonary involvement or from anemia. Autoimmune conditions such as systemic lupus erythematosus or adult Still's disease could also present with this course.
On admission, he described progressive orthopnea, lower extremity edema, and a 15‐lb weight gain. He denied chest pain or palpitations. His symptoms did not correlate with environmental or occupational exposures. He had been diagnosed with essential hypertension a few years earlier but was not taking any medications. He worked as an editor for a newspaper and had traveled throughout California. He never used tobacco and drank alcohol in moderation. He previously smoked marijuana. His father died of Alzheimer's disease, and his mother and 2 siblings were healthy.
Orthopnea, lower extremity edema, and weight gain suggest volume overload, which can result from heart failure, cirrhosis, renal failure, or nephrotic syndrome. The untreated hypertension is a principal risk factor for heart failure. Subacute bacterial endocarditis is an important consideration in a patient with suspected heart failure and night sweats. Travel through the central valley of California may have exposed him to coccidiodomycosis, which can cause chronic pulmonary and extrapulmonary infection.
Physical examination revealed a chronically ill‐appearing man in mild respiratory distress. His temperature was 37.2C, heart rate was 83 bpm, and blood pressure was 168/81 mm Hg. His oxygen saturation was 97% with a respiratory rate of 17 while breathing ambient air. Bilateral chemosis was present. He had crackles at the lung bases. There was a 2/6 systolic murmur loudest at the left lower sternal border with apical radiation. His jugular venous pressure was 2 cm above the sternal angle at 45. He had mild pitting edema of both lower extremities. His abdomen was soft and nondistended. He demonstrated full range of motion of all extremities and had no rashes. He was alert and oriented to person, place, and time. There were no cranial nerve deficits. His strength, sensation and coordination were intact, and he had a normal gait.
Chemosis (conjunctival edema) usually represents conjunctival irritation from an allergic, infectious, or toxic process. It can also be seen in cases of increased ophthalmic venous pressure such as hyperthyroid ophthalmopathy, superior vena cava syndrome, or carotid‐cavernous sinus fistula. The crackles, weight gain, borderline jugular venous distention, and edema suggest some systemic volume overload, but not enough to produce chemosis.
The location and timing of the murmur suggests regurgitation through the mitral or tricuspid valve, a ventricular septal defect, or hypertrophic cardiomyopathy. Tricuspid regurgitation may indicate pulmonary hypertension with right ventricular failure. Despite the absence of fever, subacute bacterial endocarditis remains a concern.
Laboratory evaluation revealed a white blood cell count of 9600/L, hemoglobin of 8.7 g/dL, and platelet count of 522,000/L. Mean corpuscular volume was 88 fL. Serum chemistries were normal; serum creatinine was 1.2 mg/dL. Serum albumin was 2.6 g/dL. A urinalysis was normal. An electrocardiogram demonstrated normal sinus rhythm and left ventricular hypertrophy (LVH). A chest x‐ray revealed interstitial edema and small bilateral pleural effusions. A transthoracic echocardiogram demonstrated normal left ventricular systolic function, an ejection fraction of 65%, mild LVH, and mild diastolic dysfunction. Mild mitral regurgitation, a mildly dilated left atrium, and a minimal pericardial effusion were also noted. A renal ultrasound revealed an atrophic left kidney without arterial flow. He was treated with diuretics for presumed heart failure related to diastolic dysfunction. His dyspnea partially improved, and he was discharged.
Heart failure with preserved ejection fraction may be contributing to his dyspnea but is unlikely to be entirely explanatory given the laboratory abnormalities. The absence of valvular vegetations on transthoracic echocardiogram lowers the probability of bacterial endocarditis. The interstitial pulmonary markings may represent pulmonary edema but alternatively could reflect interstitial lung disease, lymphangitic spread of cancer, infection (eg, Pneumocystis jiroveci), or diffuse alveolar hemorrhage.
Anemia may also be contributing to his dyspnea. There is no evidence of bleeding on history, examination, or imaging. Hemolysis is unlikely given the absence of jaundice, splenomegaly, or a known predisposing condition. The normocytic anemia may also arise from chronic inflammation. Severe anemia can cause high output heart failure, but usually the hemoglobin level is much lower and the echocardiogram would have suggestive findings. Thrombocytosis suggests inflammation, a primary myeloproliferative disorder, or severe iron deficiency (not suspected here). His hypoalbuminemia is further evidence of chronic inflammation especially in the absence of nephropathy, hepatopathy, or a protein‐losing enteropathy.
An atrophic kidney may be congenital or result from long‐standing unilateral renal ischemia, infection, or obstruction. Diminished arterial flow in a middle‐aged man with hypertension may simply reflect atherosclerotic renal artery stenosis, but mass effect within the left renal artery from thrombus, infection, or cancer cannot be ruled out.
Four weeks later he was readmitted for progressive dyspnea and persistent night sweats. He was afebrile, fatigued, and in marked respiratory distress. The remainder of his physical examination was unchanged. Laboratory evaluation revealed a white blood cell count of 20,000/L with neutrophilic predominance, hemoglobin of 11 g/dL, and platelet count of 614,000/L. Creatinine was 1.4 mg/dL. Erythrocyte sedimentation rate (ESR) was greater than 100 mm/h, and C‐reactive protein (CRP) was 44 mg/L. Blood cultures were negative. Chest x‐ray (Figure 1) revealed persistent interstitial edema and increased bilateral pleural effusions.
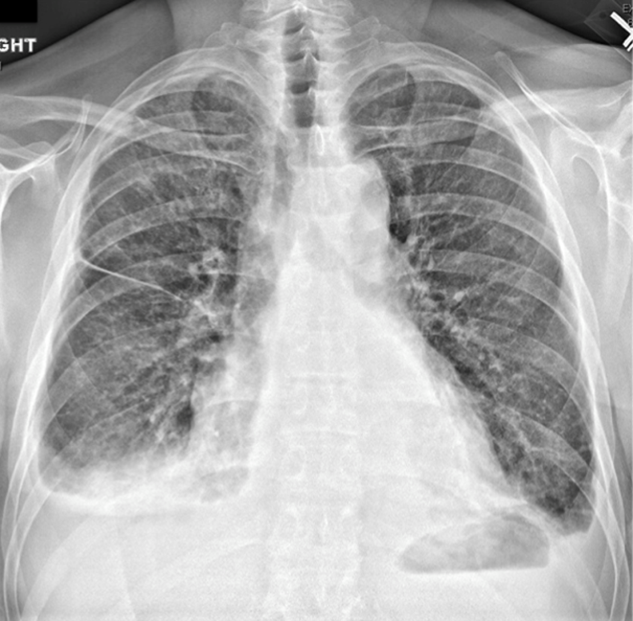
Although clinical and radiologic features continue to suggest heart failure, the marked respiratory distress and persistent chest x‐ray abnormalities imply that a superimposed process is affecting the lungs. The night sweats, neutrophilia, and elevated ESR and CRP strongly suggest an inflammatory state from infection, malignancy, or autoimmunity.
A computed tomography (CT) scan of the lungs would help assess for interstitial lung disease, lymphangitic carcinomatosis and septic emboli. Blood cultures should be repeated to definitively exclude subacute endocarditis. A peripheral blood smear is needed to evaluate for hematologic malignancy. Finally, human immunodeficiency virus antibody testing is indicated.
CT of the abdomen and pelvis demonstrated left renal artery stenosis, an atrophic left kidney, right kidney edema with mild perinephric stranding, and mild‐to‐moderate right hydroureter without an obstructing mass or calculus. There was mild splenomegaly and mesenteric lymphadenopathy up to 3 cm in diameter. The distal thoracic and suprarenal abdominal aorta had crescentic high‐density wall thickening. There were small sclerotic densities of the proximal femora, pelvic girdle, and thoracolumbar spine (Figure 2). Contrast chest CT demonstrated severe wall thickening of his entire thoracic aorta. There was also cardiomegaly, mild interlobular septal thickening, small bilateral pleural effusions, a 3.2‐cm right upper lobe paratracheal lymph node, and nodular pleural thickening (Figure 3).
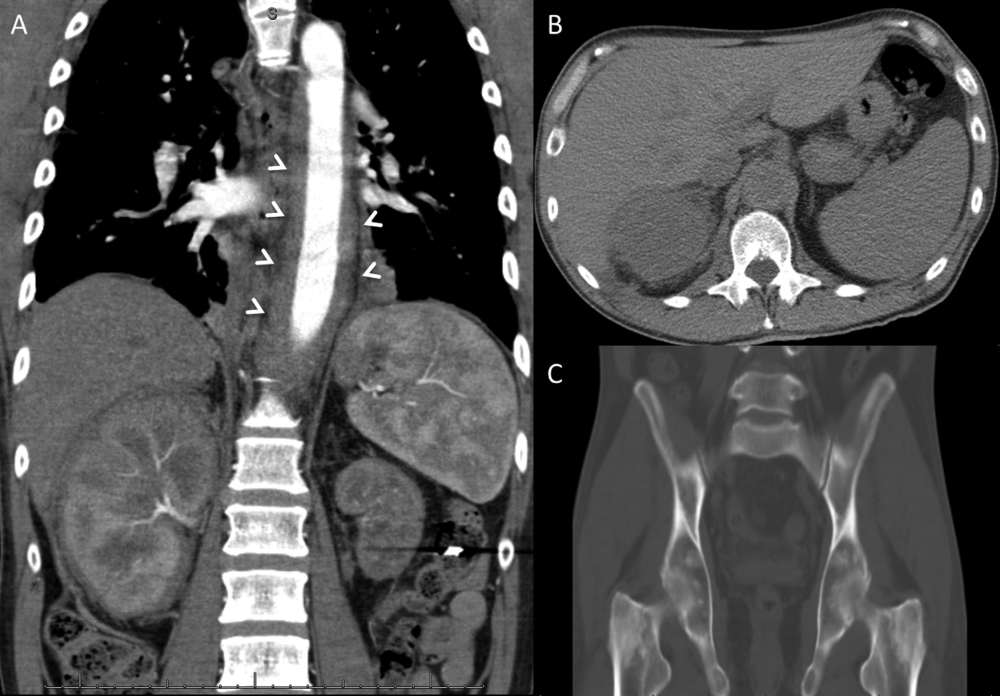
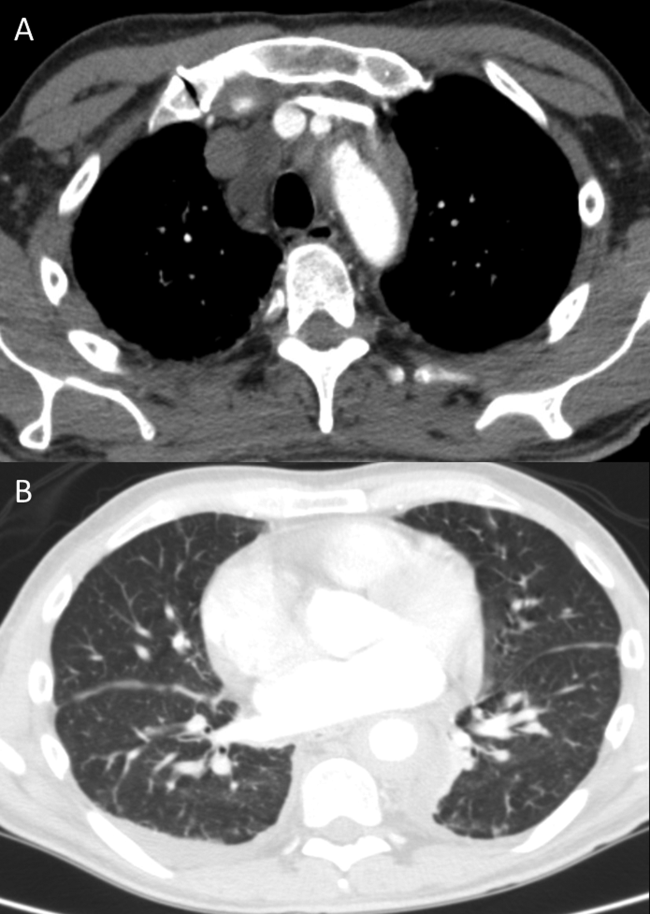
Diffuse aortopathy is caused by inflammatory, infectious, or infiltrative processes. Large vessel vasculitides such as Behet's disease, giant cell arteritis, and Takayasu's arteritis are unlikely, as the patient lacks the associated clinical findings or epidemiology. Imaging does not reveal preexisting aortic pathology, such as an aneurysm or atherosclerotic plaque, which could predispose him to bacterial endovascular infection.
Urinary system dilation without an obvious obstruction could be explained by retroperitoneal fibrosis. Generalized lymphadenopathy, (suspected) retroperitoneal fibrosis, sclerotic bone lesions, and cardiopulmonary disease collectively suggest a widespread infiltrative process. Lymphoma may lead to lymphadenopathy and bone lesions but would not explain the aortopathy. He lacks risk factors for infections like tuberculosis or tertiary syphilis, a well‐known cause of aortopathy in the past.
Widespread multisystem involvement invites consideration of nonmalignant, noninfectious infiltrative disorders such as immunoglobulin G4‐related disease (IgG4‐RD), histiocytoses such as Erdheim‐Chester disease (ECD), systemic mastocytosis (SM), and sarcoidosis. ECD is a disorder of non‐Langerhans histiocytes that infiltrate the aorta, bones, retroperitoneum, lungs, myocardium, and periorbital structures. Perinephric stranding is sometimes seen in this condition. The lymphoplasmacytes in IgG4‐RD and noncaseating granulomas of sarcoidosis infiltrate many of the same organs. Common sites infiltrated by mast cells in SM include the bone and lymph nodes. Among these diseases, ECD and IgG4‐RD more commonly manifest with aortic and retroperitoneal infiltration and thus are prioritized on this differential diagnosis.
A positron emission tomography (PET) scan revealed abnormal fluordeoxyglucose uptake involving the thoracic aorta, right apical pleural surface, perinephric soft tissue, and various marrow spaces. Core needle biopsy of a sclerotic lesion in the right ischium demonstrated focal marrow replacement by a fibrohistiocytic process. No malignant cells or pathogenic organisms were identified. Biopsy of the right kidney revealed chronic interstitial nephritis with features of megalocytic interstitial nephritis (histiocytic inflammation) and arteriolar nephrosclerosis. A transbronchial biopsy demonstrated alveolar tissue with focal intra‐alveolar hemorrhage and organization, but no malignancy, atypia, or pathogenic organisms.
The biopsy results do not support infection, lymphoma, or carcinoma. The absence of noncaseating granulomas and mastocytes on multiple biopsies essentially rules out sarcoidosis and SM, respectively. None of the characteristic pathologic features of IgG4‐RDlymphoplasmacytic infiltrate, obliterative phlebitis, and fibrosiswere observed. The pulmonary pathology points to injury, but not the underlying cause. The bone and kidney tissue samples reveal histiocytic infiltration.
The abnormalities of the aorta, bone, lung, kidney, and retroperitoneum can be explained by the diffuse histiocytic involvement seen in ECD. The perinephric stranding detected on CT and perinephric inflammation on the PET scan may reflect the hairy kidney of ECD, which is a result of histiocytic infiltration. It is possible that the chemosis relates to exophthalmos from histiocytic orbital infiltrates. Sensitivity for detecting orbital pathology on a PET scan is limited because of the high signal from the adjacent brain.
ECD should be distinguished from Langerhans cell histiocytosis (LCH) by immunohistologic staining and microscopic characteristics of the histiocytes. LCH usually does not involve the aorta, and it more commonly involves the skin.
Serum IgG4 was within normal limits, and immunohistochemical staining of pathology specimens for IgG4 was negative. The BRAF V600E mutation, which is present in the majority of patients with ECD, was detected in a subsequent right perinephric biopsy specimen. The patient was diagnosed with ECD.
Prednisone and pegylated interferon‐ led to a rapid improvement in his symptoms. As the prednisone was tapered, he developed bilateral periorbital swelling. Magnetic resonance imaging (MRI) revealed well‐circumscribed, intraorbital soft tissue masses with partial encasement of his optic nerves and superior ophthalmic veins, as well as infiltration of his transverse sinuses, consistent with intracranial manifestations of ECD. There was no evidence of pituitary, hypothalamic, or other brain parenchymal infiltration. His dyspnea, night sweats, and hypertension improved; however, 3 months into therapy he developed an extensive rash. Interferon was discontinued. Vemurafinib, a serine kinase inhibitor that targets the BRAF mutation, was prescribed with subsequent resolution of the rash.
COMMENTARY
This patient suffered from a chronic, progressive, inflammatory illness. Although the disease initially appeared to be confined to the heart and lungs, laboratory testing signaled a more systemic condition, and subsequent imaging demonstrated involvement of a disparate group of organs. Subacute disease processes with elevated markers of inflammation and diffuse organ involvement often fall into 1 of 3 categories: infectious, autoimmune, or neoplastic. The histiocytoses inhabit a fourth and easily overlooked category that can be described as infiltrative. Infiltrative diseases are a heterogeneous group of conditions that cause illness when cells or substances not normally found in tissues lead to organ dysfunction.
Although traditional teaching has focused on sarcoidosis, amyloidosis, and hemochromatosis as the primary representatives of this category, the medical literature describes a number of other infiltrative disease processes. IgG4‐RD is a fibroinflammatory disorder characterized by space‐occupying lesions, a lymphoplasmacytic infiltrate of IgG4‐positive plasma cells, and storiform (matted and irregularly whorled microscopic pattern) fibrosis.[1] IgG4‐RD, like sarcoidosis, blurs the categorical line between infiltrative and autoimmune diseases. Other infiltrative cellular disorders, such as histiocytosis and mastocytosis, exist on a spectrum between monoclonal proliferation and neoplastic invasion.
The histiocytoses represent a diverse group of disorders with an evolving nomenclature, characterized by localized or diffuse infiltration of macrophages, monocytes, and dendritic cells (Table 1). ECD is a rare, non‐Langerhans histiocytosis characterized by excessive recruitment and activation of histiocytes through kinase signaling pathways.[2, 3] Immunohistochemical staining for CD68, CD163, and Factor XIIIa, with lack of staining for CD1a, S100, and CD207, supports the diagnosis.[3] Mutations in the BRAF V600E gene (a protein kinase involved in cell proliferation) represent the most likely etiology of this overactivation. An estimated 38% to 100% of patients with ECD harbor this mutation, with detection rates influenced by the sensitivity of testing techniques.[3] The serine kinase inhibitor vemurafinib targets this mutation, and early experience with this agent in ECD demonstrates encouraging results.[4]
| Dendritic cell disorders |
| Langerhans cell histiocytosis |
| Secondary dendritic cell processes |
| Juvenile xanthogranuloma and related disorders (including Erdheim‐Chester disease) |
| Solitary histiocytomas with a dendritic phenotype |
| Macrophage‐related disorders |
| Primary hemophagocytic lymphohistiocytosis (familial and sporadic) |
| Secondary hemophagocytic syndromes |
| Sinus histiocytosis with massive lymphadenopathy (Rosai‐Dorfman disease) |
| Solitary histiocytoma with a macrophage phenotype |
| Malignant histiocytic disorders |
| Monocyte‐related leukemias |
| Extramedullary monocytic tumor or sarcoma |
| Dendritic cell‐related histiocytic sarcoma |
| Macrophage‐related histiocytic sarcoma |
ECD presents heterogeneously, occurring most commonly between the ages of 40 and 70 years. Nonspecific symptoms include weakness, fatigue, fever, chills, weight loss, and night sweats. Typical sites of involvement include the bone, central nervous system, cardiovascular system, lungs, and retroperitoneum. Bone involvement is nearly universal, and bone pain is the most common presenting symptom. Symmetric diaphyseal and metaphyseal osteosclerotic lesions may be seen on x‐rays, bone scan, PET, CT, and MRI.[3] Approximately 50% of patients have extraskeletal involvement at diagnosis.[5] Neurologic manifestations may result from invasion of histiocytes into the facial bones, orbits, meninges, and intracranial vessels, as eventually developed in this patient. Diabetes insipidus is the most common neurologic manifestation of ECD, followed by exophthalmos, cerebellar ataxia, panhypopituitarism, and papilledema.[6, 7] Approximately 75% of patients eventually suffer from cardiovascular disease, including hypertension, congestive heart failure, acute myocardial infarction, valvular dysfunction, pericardial infiltration, and cardiac tamponade.[8] Vascular involvement includes perivascular infiltration and periaortic fibrosis, resulting in the coated aorta seen in 20% of patients with ECD.[3] Pulmonary manifestations of ECD include interstitial, pleural, and consolidative lung disease. A review of high‐resolution chest CTs of patients with ECD demonstrated that greater than half had evidence of parenchymal lung disease, with interlobular septal thickening being the most common finding.[9] Infiltration and fibrosis of retroperitoneal structures is common. Infiltration of perinephric fat creates irregular renal borders, appearing radiographically as hairy kidneys.
Arriving at the diagnosis in this case proved to be challenging because the early presentation was consistent with congestive heart failure. As the patient's conditioned deteriorated, imaging suggested multisystem involvement. It was the extensive aortopathy in particularnot the less specific bone, kidney, lymph node, or pulmonary findingsthat allowed the clinicians to hone the extensive differential diagnosis. The coated aorta is a finding that has been strongly associated with ECD; few other conditions coat the aorta in a similar fashion.[10] In most mysteries, the perpetrator's coat conceals his identity; however, in this story the coat gave it away.
KEY LEARNING POINTS
- Subacute, inflammatory, multiorgan disease is usually explained by 3 categoriesinfection, autoimmunity, and neoplasiabut a fourth category, infiltrative disorders, sometimes warrants consideration.
- ECD presents heterogeneously, ranging from localized disease to widespread organ infiltration. The classic presentation includes bone pain, diabetes insipidus, and exophthalmos.
- Characteristic radiological findings that suggest ECD include long bone osteosclerosis, a coated aorta from periaortic infiltration, and hairy kidneys from perinephric infiltration.
Disclosure
Nothing to report
- , , IgG4‐related disease. N Engl J Med. 2012;366(6):539–551.
- , , , Diagnosing Erdheim‐Chester disease. Ann Rheum Dis. 2013;72(7):e19.
- , , , et al. Consensus guidelines for the diagnosis and clinical management of Erdheim‐Chester disease. Blood. 2014;124(4):483–492.
- , , , et al. The efficacy of vemurafenib in Erdheim‐Chester Disease and Langerhans Cell Histiocytosis: preliminary results from VE‐Basket Study. Blood. 2014;124(21):635.
- , , , et al. Erdheim‐Chester disease. Clinical and radiologic characteristics of 59 cases. Medicine (Baltimore). 1996;75(3):157–169.
- , , , et al. Neurological manifestations and neuroradiological presentation of Erdheim‐Chester disease: report of 6 cases and systematic review of the literature. J Neurol. 2006;253(10):1267–1277.
- , , , et al. Cerebral, facial, and orbital involvement in Erdheim‐Chester disease: CT and MR imaging findings. Radiology. 2010;255(2):586–594.
- , , , et al. Images in cardiovascular medicine. Cardiac involvement in Erdheim‐Chester disease: magnetic resonance and computed tomographic scan imaging in a monocentric series of 37 patients. Circulation. 2009;119(25):e597–e598.
- , , , et al. Pulmonary involvement in Erdheim‐Chester disease: a single‐center study of thirty‐four patients and a review of the literature. Arthritis Rheum. 2010;62(11):3504–3512.
- , , , et al. “Coated aorta”: a new sign of Erdheim‐Chester disease. J Rheumatol. 2000;27(6):1550–1553.
A 59‐year‐old man with a history of hypertension was admitted with 6 months of shortness of breath, night sweats, and debilitating fatigue. His symptoms were initially mild and would persist for weeks at a time, after which he would feel better for several days. Over the 2 weeks prior to admission his symptoms had progressed, and he had become dyspneic with minimal exertion.
Progressive dyspnea has a broad differential that includes diseases of the heart (eg, congestive heart failure, aortic stenosis, constrictive pericarditis), lung (eg, chronic obstructive pulmonary disease, interstitial lung disease, pulmonary hypertension, pleural effusion), and blood (eg, anemia).
Night sweats suggest an inflammatory condition, but do not help prioritize infection, malignancy, or autoimmunity. Any of those conditions can be relapsing and remitting, at least in their early phases, but the return to normalcy raises the possibility of hypersensitivity pneumonitis from a periodic exposure.
The 6‐month duration makes typical bacterial and viral infections less likely and suggests indolent infections such as mycobacteria, fungi, or human immunodeficiency virus. Lymphoma or chronic leukemia could cause dyspnea through pleural or pulmonary involvement or from anemia. Autoimmune conditions such as systemic lupus erythematosus or adult Still's disease could also present with this course.
On admission, he described progressive orthopnea, lower extremity edema, and a 15‐lb weight gain. He denied chest pain or palpitations. His symptoms did not correlate with environmental or occupational exposures. He had been diagnosed with essential hypertension a few years earlier but was not taking any medications. He worked as an editor for a newspaper and had traveled throughout California. He never used tobacco and drank alcohol in moderation. He previously smoked marijuana. His father died of Alzheimer's disease, and his mother and 2 siblings were healthy.
Orthopnea, lower extremity edema, and weight gain suggest volume overload, which can result from heart failure, cirrhosis, renal failure, or nephrotic syndrome. The untreated hypertension is a principal risk factor for heart failure. Subacute bacterial endocarditis is an important consideration in a patient with suspected heart failure and night sweats. Travel through the central valley of California may have exposed him to coccidiodomycosis, which can cause chronic pulmonary and extrapulmonary infection.
Physical examination revealed a chronically ill‐appearing man in mild respiratory distress. His temperature was 37.2C, heart rate was 83 bpm, and blood pressure was 168/81 mm Hg. His oxygen saturation was 97% with a respiratory rate of 17 while breathing ambient air. Bilateral chemosis was present. He had crackles at the lung bases. There was a 2/6 systolic murmur loudest at the left lower sternal border with apical radiation. His jugular venous pressure was 2 cm above the sternal angle at 45. He had mild pitting edema of both lower extremities. His abdomen was soft and nondistended. He demonstrated full range of motion of all extremities and had no rashes. He was alert and oriented to person, place, and time. There were no cranial nerve deficits. His strength, sensation and coordination were intact, and he had a normal gait.
Chemosis (conjunctival edema) usually represents conjunctival irritation from an allergic, infectious, or toxic process. It can also be seen in cases of increased ophthalmic venous pressure such as hyperthyroid ophthalmopathy, superior vena cava syndrome, or carotid‐cavernous sinus fistula. The crackles, weight gain, borderline jugular venous distention, and edema suggest some systemic volume overload, but not enough to produce chemosis.
The location and timing of the murmur suggests regurgitation through the mitral or tricuspid valve, a ventricular septal defect, or hypertrophic cardiomyopathy. Tricuspid regurgitation may indicate pulmonary hypertension with right ventricular failure. Despite the absence of fever, subacute bacterial endocarditis remains a concern.
Laboratory evaluation revealed a white blood cell count of 9600/L, hemoglobin of 8.7 g/dL, and platelet count of 522,000/L. Mean corpuscular volume was 88 fL. Serum chemistries were normal; serum creatinine was 1.2 mg/dL. Serum albumin was 2.6 g/dL. A urinalysis was normal. An electrocardiogram demonstrated normal sinus rhythm and left ventricular hypertrophy (LVH). A chest x‐ray revealed interstitial edema and small bilateral pleural effusions. A transthoracic echocardiogram demonstrated normal left ventricular systolic function, an ejection fraction of 65%, mild LVH, and mild diastolic dysfunction. Mild mitral regurgitation, a mildly dilated left atrium, and a minimal pericardial effusion were also noted. A renal ultrasound revealed an atrophic left kidney without arterial flow. He was treated with diuretics for presumed heart failure related to diastolic dysfunction. His dyspnea partially improved, and he was discharged.
Heart failure with preserved ejection fraction may be contributing to his dyspnea but is unlikely to be entirely explanatory given the laboratory abnormalities. The absence of valvular vegetations on transthoracic echocardiogram lowers the probability of bacterial endocarditis. The interstitial pulmonary markings may represent pulmonary edema but alternatively could reflect interstitial lung disease, lymphangitic spread of cancer, infection (eg, Pneumocystis jiroveci), or diffuse alveolar hemorrhage.
Anemia may also be contributing to his dyspnea. There is no evidence of bleeding on history, examination, or imaging. Hemolysis is unlikely given the absence of jaundice, splenomegaly, or a known predisposing condition. The normocytic anemia may also arise from chronic inflammation. Severe anemia can cause high output heart failure, but usually the hemoglobin level is much lower and the echocardiogram would have suggestive findings. Thrombocytosis suggests inflammation, a primary myeloproliferative disorder, or severe iron deficiency (not suspected here). His hypoalbuminemia is further evidence of chronic inflammation especially in the absence of nephropathy, hepatopathy, or a protein‐losing enteropathy.
An atrophic kidney may be congenital or result from long‐standing unilateral renal ischemia, infection, or obstruction. Diminished arterial flow in a middle‐aged man with hypertension may simply reflect atherosclerotic renal artery stenosis, but mass effect within the left renal artery from thrombus, infection, or cancer cannot be ruled out.
Four weeks later he was readmitted for progressive dyspnea and persistent night sweats. He was afebrile, fatigued, and in marked respiratory distress. The remainder of his physical examination was unchanged. Laboratory evaluation revealed a white blood cell count of 20,000/L with neutrophilic predominance, hemoglobin of 11 g/dL, and platelet count of 614,000/L. Creatinine was 1.4 mg/dL. Erythrocyte sedimentation rate (ESR) was greater than 100 mm/h, and C‐reactive protein (CRP) was 44 mg/L. Blood cultures were negative. Chest x‐ray (Figure 1) revealed persistent interstitial edema and increased bilateral pleural effusions.
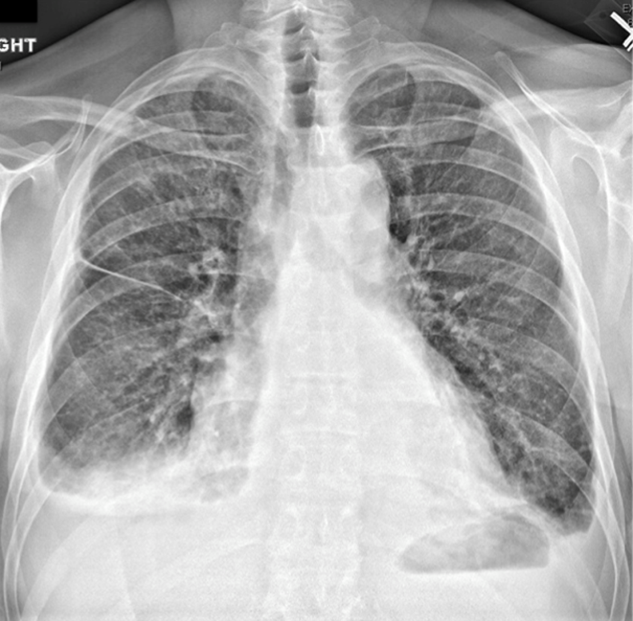
Although clinical and radiologic features continue to suggest heart failure, the marked respiratory distress and persistent chest x‐ray abnormalities imply that a superimposed process is affecting the lungs. The night sweats, neutrophilia, and elevated ESR and CRP strongly suggest an inflammatory state from infection, malignancy, or autoimmunity.
A computed tomography (CT) scan of the lungs would help assess for interstitial lung disease, lymphangitic carcinomatosis and septic emboli. Blood cultures should be repeated to definitively exclude subacute endocarditis. A peripheral blood smear is needed to evaluate for hematologic malignancy. Finally, human immunodeficiency virus antibody testing is indicated.
CT of the abdomen and pelvis demonstrated left renal artery stenosis, an atrophic left kidney, right kidney edema with mild perinephric stranding, and mild‐to‐moderate right hydroureter without an obstructing mass or calculus. There was mild splenomegaly and mesenteric lymphadenopathy up to 3 cm in diameter. The distal thoracic and suprarenal abdominal aorta had crescentic high‐density wall thickening. There were small sclerotic densities of the proximal femora, pelvic girdle, and thoracolumbar spine (Figure 2). Contrast chest CT demonstrated severe wall thickening of his entire thoracic aorta. There was also cardiomegaly, mild interlobular septal thickening, small bilateral pleural effusions, a 3.2‐cm right upper lobe paratracheal lymph node, and nodular pleural thickening (Figure 3).
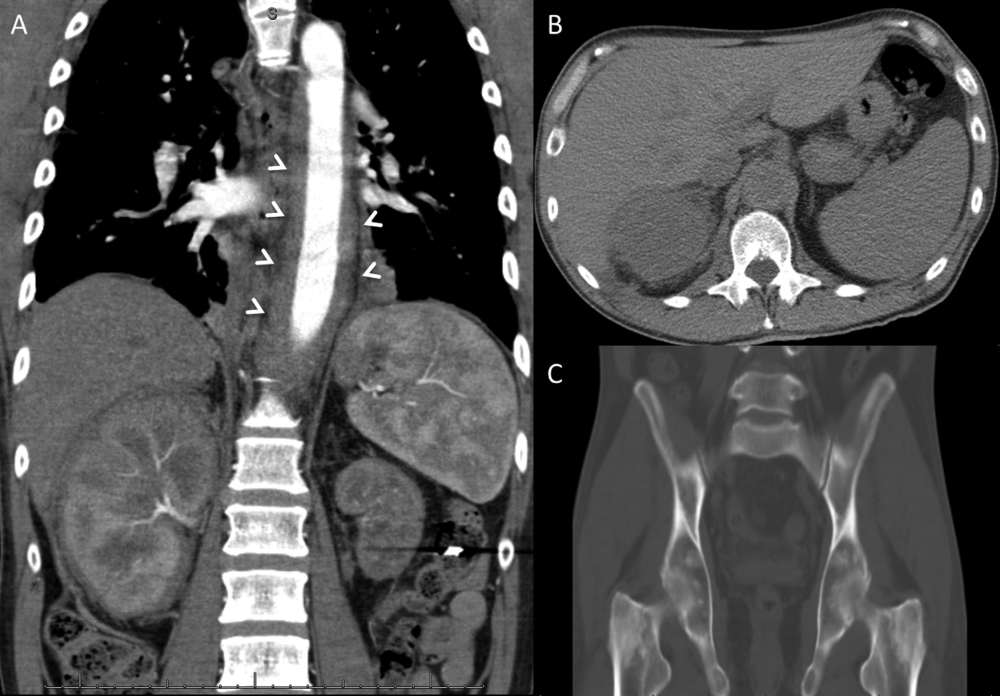
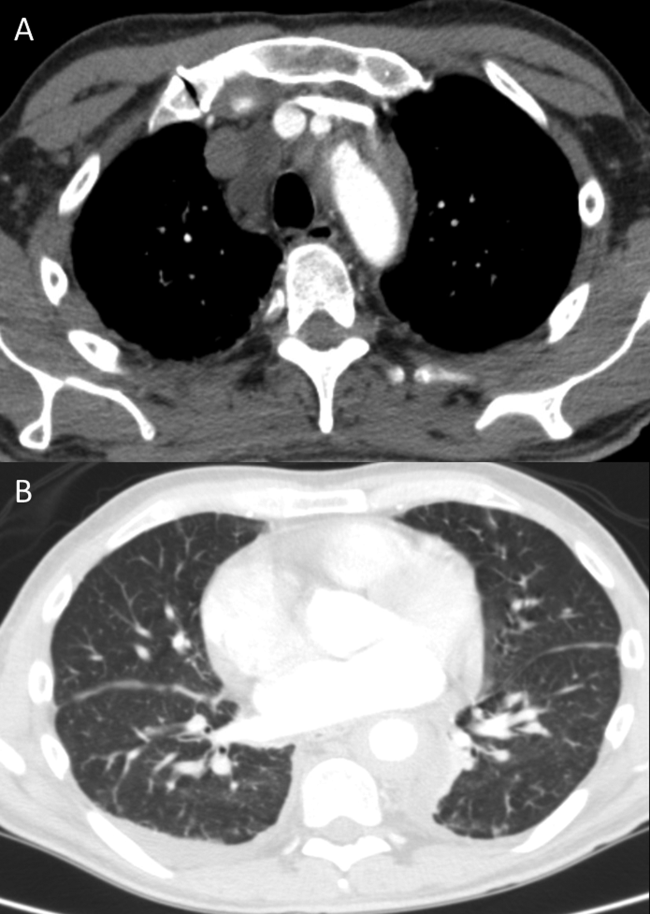
Diffuse aortopathy is caused by inflammatory, infectious, or infiltrative processes. Large vessel vasculitides such as Behet's disease, giant cell arteritis, and Takayasu's arteritis are unlikely, as the patient lacks the associated clinical findings or epidemiology. Imaging does not reveal preexisting aortic pathology, such as an aneurysm or atherosclerotic plaque, which could predispose him to bacterial endovascular infection.
Urinary system dilation without an obvious obstruction could be explained by retroperitoneal fibrosis. Generalized lymphadenopathy, (suspected) retroperitoneal fibrosis, sclerotic bone lesions, and cardiopulmonary disease collectively suggest a widespread infiltrative process. Lymphoma may lead to lymphadenopathy and bone lesions but would not explain the aortopathy. He lacks risk factors for infections like tuberculosis or tertiary syphilis, a well‐known cause of aortopathy in the past.
Widespread multisystem involvement invites consideration of nonmalignant, noninfectious infiltrative disorders such as immunoglobulin G4‐related disease (IgG4‐RD), histiocytoses such as Erdheim‐Chester disease (ECD), systemic mastocytosis (SM), and sarcoidosis. ECD is a disorder of non‐Langerhans histiocytes that infiltrate the aorta, bones, retroperitoneum, lungs, myocardium, and periorbital structures. Perinephric stranding is sometimes seen in this condition. The lymphoplasmacytes in IgG4‐RD and noncaseating granulomas of sarcoidosis infiltrate many of the same organs. Common sites infiltrated by mast cells in SM include the bone and lymph nodes. Among these diseases, ECD and IgG4‐RD more commonly manifest with aortic and retroperitoneal infiltration and thus are prioritized on this differential diagnosis.
A positron emission tomography (PET) scan revealed abnormal fluordeoxyglucose uptake involving the thoracic aorta, right apical pleural surface, perinephric soft tissue, and various marrow spaces. Core needle biopsy of a sclerotic lesion in the right ischium demonstrated focal marrow replacement by a fibrohistiocytic process. No malignant cells or pathogenic organisms were identified. Biopsy of the right kidney revealed chronic interstitial nephritis with features of megalocytic interstitial nephritis (histiocytic inflammation) and arteriolar nephrosclerosis. A transbronchial biopsy demonstrated alveolar tissue with focal intra‐alveolar hemorrhage and organization, but no malignancy, atypia, or pathogenic organisms.
The biopsy results do not support infection, lymphoma, or carcinoma. The absence of noncaseating granulomas and mastocytes on multiple biopsies essentially rules out sarcoidosis and SM, respectively. None of the characteristic pathologic features of IgG4‐RDlymphoplasmacytic infiltrate, obliterative phlebitis, and fibrosiswere observed. The pulmonary pathology points to injury, but not the underlying cause. The bone and kidney tissue samples reveal histiocytic infiltration.
The abnormalities of the aorta, bone, lung, kidney, and retroperitoneum can be explained by the diffuse histiocytic involvement seen in ECD. The perinephric stranding detected on CT and perinephric inflammation on the PET scan may reflect the hairy kidney of ECD, which is a result of histiocytic infiltration. It is possible that the chemosis relates to exophthalmos from histiocytic orbital infiltrates. Sensitivity for detecting orbital pathology on a PET scan is limited because of the high signal from the adjacent brain.
ECD should be distinguished from Langerhans cell histiocytosis (LCH) by immunohistologic staining and microscopic characteristics of the histiocytes. LCH usually does not involve the aorta, and it more commonly involves the skin.
Serum IgG4 was within normal limits, and immunohistochemical staining of pathology specimens for IgG4 was negative. The BRAF V600E mutation, which is present in the majority of patients with ECD, was detected in a subsequent right perinephric biopsy specimen. The patient was diagnosed with ECD.
Prednisone and pegylated interferon‐ led to a rapid improvement in his symptoms. As the prednisone was tapered, he developed bilateral periorbital swelling. Magnetic resonance imaging (MRI) revealed well‐circumscribed, intraorbital soft tissue masses with partial encasement of his optic nerves and superior ophthalmic veins, as well as infiltration of his transverse sinuses, consistent with intracranial manifestations of ECD. There was no evidence of pituitary, hypothalamic, or other brain parenchymal infiltration. His dyspnea, night sweats, and hypertension improved; however, 3 months into therapy he developed an extensive rash. Interferon was discontinued. Vemurafinib, a serine kinase inhibitor that targets the BRAF mutation, was prescribed with subsequent resolution of the rash.
COMMENTARY
This patient suffered from a chronic, progressive, inflammatory illness. Although the disease initially appeared to be confined to the heart and lungs, laboratory testing signaled a more systemic condition, and subsequent imaging demonstrated involvement of a disparate group of organs. Subacute disease processes with elevated markers of inflammation and diffuse organ involvement often fall into 1 of 3 categories: infectious, autoimmune, or neoplastic. The histiocytoses inhabit a fourth and easily overlooked category that can be described as infiltrative. Infiltrative diseases are a heterogeneous group of conditions that cause illness when cells or substances not normally found in tissues lead to organ dysfunction.
Although traditional teaching has focused on sarcoidosis, amyloidosis, and hemochromatosis as the primary representatives of this category, the medical literature describes a number of other infiltrative disease processes. IgG4‐RD is a fibroinflammatory disorder characterized by space‐occupying lesions, a lymphoplasmacytic infiltrate of IgG4‐positive plasma cells, and storiform (matted and irregularly whorled microscopic pattern) fibrosis.[1] IgG4‐RD, like sarcoidosis, blurs the categorical line between infiltrative and autoimmune diseases. Other infiltrative cellular disorders, such as histiocytosis and mastocytosis, exist on a spectrum between monoclonal proliferation and neoplastic invasion.
The histiocytoses represent a diverse group of disorders with an evolving nomenclature, characterized by localized or diffuse infiltration of macrophages, monocytes, and dendritic cells (Table 1). ECD is a rare, non‐Langerhans histiocytosis characterized by excessive recruitment and activation of histiocytes through kinase signaling pathways.[2, 3] Immunohistochemical staining for CD68, CD163, and Factor XIIIa, with lack of staining for CD1a, S100, and CD207, supports the diagnosis.[3] Mutations in the BRAF V600E gene (a protein kinase involved in cell proliferation) represent the most likely etiology of this overactivation. An estimated 38% to 100% of patients with ECD harbor this mutation, with detection rates influenced by the sensitivity of testing techniques.[3] The serine kinase inhibitor vemurafinib targets this mutation, and early experience with this agent in ECD demonstrates encouraging results.[4]
| Dendritic cell disorders |
| Langerhans cell histiocytosis |
| Secondary dendritic cell processes |
| Juvenile xanthogranuloma and related disorders (including Erdheim‐Chester disease) |
| Solitary histiocytomas with a dendritic phenotype |
| Macrophage‐related disorders |
| Primary hemophagocytic lymphohistiocytosis (familial and sporadic) |
| Secondary hemophagocytic syndromes |
| Sinus histiocytosis with massive lymphadenopathy (Rosai‐Dorfman disease) |
| Solitary histiocytoma with a macrophage phenotype |
| Malignant histiocytic disorders |
| Monocyte‐related leukemias |
| Extramedullary monocytic tumor or sarcoma |
| Dendritic cell‐related histiocytic sarcoma |
| Macrophage‐related histiocytic sarcoma |
ECD presents heterogeneously, occurring most commonly between the ages of 40 and 70 years. Nonspecific symptoms include weakness, fatigue, fever, chills, weight loss, and night sweats. Typical sites of involvement include the bone, central nervous system, cardiovascular system, lungs, and retroperitoneum. Bone involvement is nearly universal, and bone pain is the most common presenting symptom. Symmetric diaphyseal and metaphyseal osteosclerotic lesions may be seen on x‐rays, bone scan, PET, CT, and MRI.[3] Approximately 50% of patients have extraskeletal involvement at diagnosis.[5] Neurologic manifestations may result from invasion of histiocytes into the facial bones, orbits, meninges, and intracranial vessels, as eventually developed in this patient. Diabetes insipidus is the most common neurologic manifestation of ECD, followed by exophthalmos, cerebellar ataxia, panhypopituitarism, and papilledema.[6, 7] Approximately 75% of patients eventually suffer from cardiovascular disease, including hypertension, congestive heart failure, acute myocardial infarction, valvular dysfunction, pericardial infiltration, and cardiac tamponade.[8] Vascular involvement includes perivascular infiltration and periaortic fibrosis, resulting in the coated aorta seen in 20% of patients with ECD.[3] Pulmonary manifestations of ECD include interstitial, pleural, and consolidative lung disease. A review of high‐resolution chest CTs of patients with ECD demonstrated that greater than half had evidence of parenchymal lung disease, with interlobular septal thickening being the most common finding.[9] Infiltration and fibrosis of retroperitoneal structures is common. Infiltration of perinephric fat creates irregular renal borders, appearing radiographically as hairy kidneys.
Arriving at the diagnosis in this case proved to be challenging because the early presentation was consistent with congestive heart failure. As the patient's conditioned deteriorated, imaging suggested multisystem involvement. It was the extensive aortopathy in particularnot the less specific bone, kidney, lymph node, or pulmonary findingsthat allowed the clinicians to hone the extensive differential diagnosis. The coated aorta is a finding that has been strongly associated with ECD; few other conditions coat the aorta in a similar fashion.[10] In most mysteries, the perpetrator's coat conceals his identity; however, in this story the coat gave it away.
KEY LEARNING POINTS
- Subacute, inflammatory, multiorgan disease is usually explained by 3 categoriesinfection, autoimmunity, and neoplasiabut a fourth category, infiltrative disorders, sometimes warrants consideration.
- ECD presents heterogeneously, ranging from localized disease to widespread organ infiltration. The classic presentation includes bone pain, diabetes insipidus, and exophthalmos.
- Characteristic radiological findings that suggest ECD include long bone osteosclerosis, a coated aorta from periaortic infiltration, and hairy kidneys from perinephric infiltration.
Disclosure
Nothing to report
A 59‐year‐old man with a history of hypertension was admitted with 6 months of shortness of breath, night sweats, and debilitating fatigue. His symptoms were initially mild and would persist for weeks at a time, after which he would feel better for several days. Over the 2 weeks prior to admission his symptoms had progressed, and he had become dyspneic with minimal exertion.
Progressive dyspnea has a broad differential that includes diseases of the heart (eg, congestive heart failure, aortic stenosis, constrictive pericarditis), lung (eg, chronic obstructive pulmonary disease, interstitial lung disease, pulmonary hypertension, pleural effusion), and blood (eg, anemia).
Night sweats suggest an inflammatory condition, but do not help prioritize infection, malignancy, or autoimmunity. Any of those conditions can be relapsing and remitting, at least in their early phases, but the return to normalcy raises the possibility of hypersensitivity pneumonitis from a periodic exposure.
The 6‐month duration makes typical bacterial and viral infections less likely and suggests indolent infections such as mycobacteria, fungi, or human immunodeficiency virus. Lymphoma or chronic leukemia could cause dyspnea through pleural or pulmonary involvement or from anemia. Autoimmune conditions such as systemic lupus erythematosus or adult Still's disease could also present with this course.
On admission, he described progressive orthopnea, lower extremity edema, and a 15‐lb weight gain. He denied chest pain or palpitations. His symptoms did not correlate with environmental or occupational exposures. He had been diagnosed with essential hypertension a few years earlier but was not taking any medications. He worked as an editor for a newspaper and had traveled throughout California. He never used tobacco and drank alcohol in moderation. He previously smoked marijuana. His father died of Alzheimer's disease, and his mother and 2 siblings were healthy.
Orthopnea, lower extremity edema, and weight gain suggest volume overload, which can result from heart failure, cirrhosis, renal failure, or nephrotic syndrome. The untreated hypertension is a principal risk factor for heart failure. Subacute bacterial endocarditis is an important consideration in a patient with suspected heart failure and night sweats. Travel through the central valley of California may have exposed him to coccidiodomycosis, which can cause chronic pulmonary and extrapulmonary infection.
Physical examination revealed a chronically ill‐appearing man in mild respiratory distress. His temperature was 37.2C, heart rate was 83 bpm, and blood pressure was 168/81 mm Hg. His oxygen saturation was 97% with a respiratory rate of 17 while breathing ambient air. Bilateral chemosis was present. He had crackles at the lung bases. There was a 2/6 systolic murmur loudest at the left lower sternal border with apical radiation. His jugular venous pressure was 2 cm above the sternal angle at 45. He had mild pitting edema of both lower extremities. His abdomen was soft and nondistended. He demonstrated full range of motion of all extremities and had no rashes. He was alert and oriented to person, place, and time. There were no cranial nerve deficits. His strength, sensation and coordination were intact, and he had a normal gait.
Chemosis (conjunctival edema) usually represents conjunctival irritation from an allergic, infectious, or toxic process. It can also be seen in cases of increased ophthalmic venous pressure such as hyperthyroid ophthalmopathy, superior vena cava syndrome, or carotid‐cavernous sinus fistula. The crackles, weight gain, borderline jugular venous distention, and edema suggest some systemic volume overload, but not enough to produce chemosis.
The location and timing of the murmur suggests regurgitation through the mitral or tricuspid valve, a ventricular septal defect, or hypertrophic cardiomyopathy. Tricuspid regurgitation may indicate pulmonary hypertension with right ventricular failure. Despite the absence of fever, subacute bacterial endocarditis remains a concern.
Laboratory evaluation revealed a white blood cell count of 9600/L, hemoglobin of 8.7 g/dL, and platelet count of 522,000/L. Mean corpuscular volume was 88 fL. Serum chemistries were normal; serum creatinine was 1.2 mg/dL. Serum albumin was 2.6 g/dL. A urinalysis was normal. An electrocardiogram demonstrated normal sinus rhythm and left ventricular hypertrophy (LVH). A chest x‐ray revealed interstitial edema and small bilateral pleural effusions. A transthoracic echocardiogram demonstrated normal left ventricular systolic function, an ejection fraction of 65%, mild LVH, and mild diastolic dysfunction. Mild mitral regurgitation, a mildly dilated left atrium, and a minimal pericardial effusion were also noted. A renal ultrasound revealed an atrophic left kidney without arterial flow. He was treated with diuretics for presumed heart failure related to diastolic dysfunction. His dyspnea partially improved, and he was discharged.
Heart failure with preserved ejection fraction may be contributing to his dyspnea but is unlikely to be entirely explanatory given the laboratory abnormalities. The absence of valvular vegetations on transthoracic echocardiogram lowers the probability of bacterial endocarditis. The interstitial pulmonary markings may represent pulmonary edema but alternatively could reflect interstitial lung disease, lymphangitic spread of cancer, infection (eg, Pneumocystis jiroveci), or diffuse alveolar hemorrhage.
Anemia may also be contributing to his dyspnea. There is no evidence of bleeding on history, examination, or imaging. Hemolysis is unlikely given the absence of jaundice, splenomegaly, or a known predisposing condition. The normocytic anemia may also arise from chronic inflammation. Severe anemia can cause high output heart failure, but usually the hemoglobin level is much lower and the echocardiogram would have suggestive findings. Thrombocytosis suggests inflammation, a primary myeloproliferative disorder, or severe iron deficiency (not suspected here). His hypoalbuminemia is further evidence of chronic inflammation especially in the absence of nephropathy, hepatopathy, or a protein‐losing enteropathy.
An atrophic kidney may be congenital or result from long‐standing unilateral renal ischemia, infection, or obstruction. Diminished arterial flow in a middle‐aged man with hypertension may simply reflect atherosclerotic renal artery stenosis, but mass effect within the left renal artery from thrombus, infection, or cancer cannot be ruled out.
Four weeks later he was readmitted for progressive dyspnea and persistent night sweats. He was afebrile, fatigued, and in marked respiratory distress. The remainder of his physical examination was unchanged. Laboratory evaluation revealed a white blood cell count of 20,000/L with neutrophilic predominance, hemoglobin of 11 g/dL, and platelet count of 614,000/L. Creatinine was 1.4 mg/dL. Erythrocyte sedimentation rate (ESR) was greater than 100 mm/h, and C‐reactive protein (CRP) was 44 mg/L. Blood cultures were negative. Chest x‐ray (Figure 1) revealed persistent interstitial edema and increased bilateral pleural effusions.
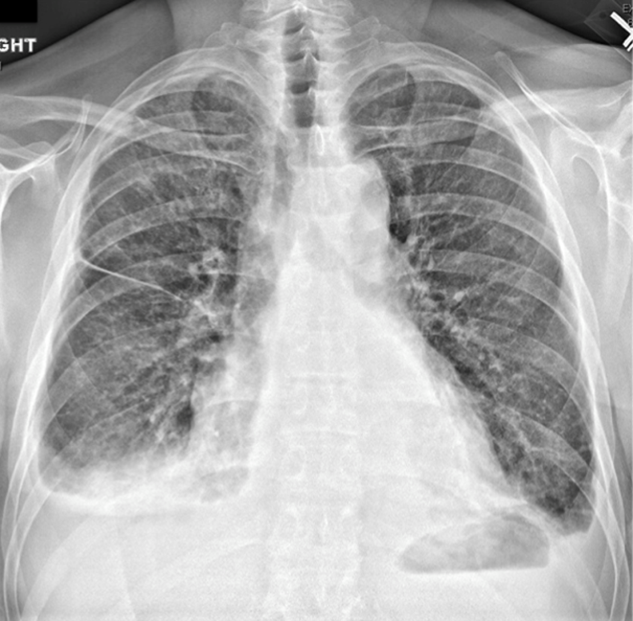
Although clinical and radiologic features continue to suggest heart failure, the marked respiratory distress and persistent chest x‐ray abnormalities imply that a superimposed process is affecting the lungs. The night sweats, neutrophilia, and elevated ESR and CRP strongly suggest an inflammatory state from infection, malignancy, or autoimmunity.
A computed tomography (CT) scan of the lungs would help assess for interstitial lung disease, lymphangitic carcinomatosis and septic emboli. Blood cultures should be repeated to definitively exclude subacute endocarditis. A peripheral blood smear is needed to evaluate for hematologic malignancy. Finally, human immunodeficiency virus antibody testing is indicated.
CT of the abdomen and pelvis demonstrated left renal artery stenosis, an atrophic left kidney, right kidney edema with mild perinephric stranding, and mild‐to‐moderate right hydroureter without an obstructing mass or calculus. There was mild splenomegaly and mesenteric lymphadenopathy up to 3 cm in diameter. The distal thoracic and suprarenal abdominal aorta had crescentic high‐density wall thickening. There were small sclerotic densities of the proximal femora, pelvic girdle, and thoracolumbar spine (Figure 2). Contrast chest CT demonstrated severe wall thickening of his entire thoracic aorta. There was also cardiomegaly, mild interlobular septal thickening, small bilateral pleural effusions, a 3.2‐cm right upper lobe paratracheal lymph node, and nodular pleural thickening (Figure 3).
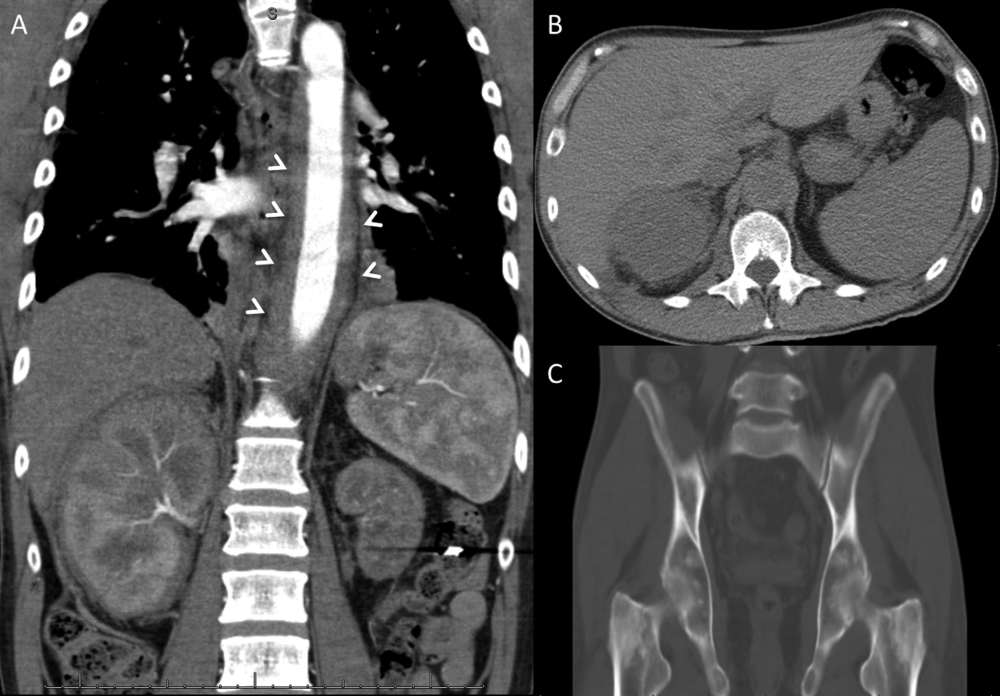
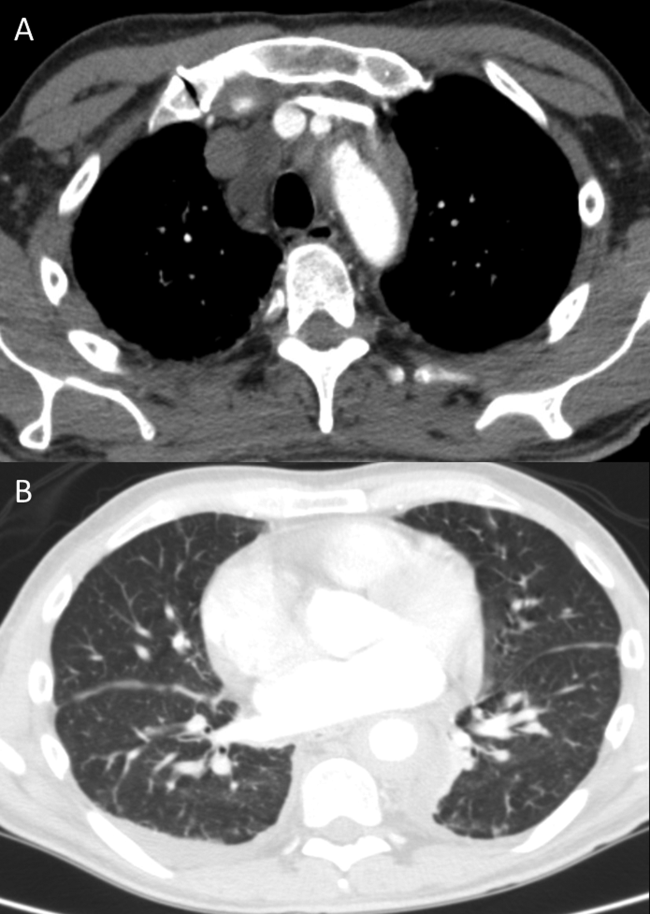
Diffuse aortopathy is caused by inflammatory, infectious, or infiltrative processes. Large vessel vasculitides such as Behet's disease, giant cell arteritis, and Takayasu's arteritis are unlikely, as the patient lacks the associated clinical findings or epidemiology. Imaging does not reveal preexisting aortic pathology, such as an aneurysm or atherosclerotic plaque, which could predispose him to bacterial endovascular infection.
Urinary system dilation without an obvious obstruction could be explained by retroperitoneal fibrosis. Generalized lymphadenopathy, (suspected) retroperitoneal fibrosis, sclerotic bone lesions, and cardiopulmonary disease collectively suggest a widespread infiltrative process. Lymphoma may lead to lymphadenopathy and bone lesions but would not explain the aortopathy. He lacks risk factors for infections like tuberculosis or tertiary syphilis, a well‐known cause of aortopathy in the past.
Widespread multisystem involvement invites consideration of nonmalignant, noninfectious infiltrative disorders such as immunoglobulin G4‐related disease (IgG4‐RD), histiocytoses such as Erdheim‐Chester disease (ECD), systemic mastocytosis (SM), and sarcoidosis. ECD is a disorder of non‐Langerhans histiocytes that infiltrate the aorta, bones, retroperitoneum, lungs, myocardium, and periorbital structures. Perinephric stranding is sometimes seen in this condition. The lymphoplasmacytes in IgG4‐RD and noncaseating granulomas of sarcoidosis infiltrate many of the same organs. Common sites infiltrated by mast cells in SM include the bone and lymph nodes. Among these diseases, ECD and IgG4‐RD more commonly manifest with aortic and retroperitoneal infiltration and thus are prioritized on this differential diagnosis.
A positron emission tomography (PET) scan revealed abnormal fluordeoxyglucose uptake involving the thoracic aorta, right apical pleural surface, perinephric soft tissue, and various marrow spaces. Core needle biopsy of a sclerotic lesion in the right ischium demonstrated focal marrow replacement by a fibrohistiocytic process. No malignant cells or pathogenic organisms were identified. Biopsy of the right kidney revealed chronic interstitial nephritis with features of megalocytic interstitial nephritis (histiocytic inflammation) and arteriolar nephrosclerosis. A transbronchial biopsy demonstrated alveolar tissue with focal intra‐alveolar hemorrhage and organization, but no malignancy, atypia, or pathogenic organisms.
The biopsy results do not support infection, lymphoma, or carcinoma. The absence of noncaseating granulomas and mastocytes on multiple biopsies essentially rules out sarcoidosis and SM, respectively. None of the characteristic pathologic features of IgG4‐RDlymphoplasmacytic infiltrate, obliterative phlebitis, and fibrosiswere observed. The pulmonary pathology points to injury, but not the underlying cause. The bone and kidney tissue samples reveal histiocytic infiltration.
The abnormalities of the aorta, bone, lung, kidney, and retroperitoneum can be explained by the diffuse histiocytic involvement seen in ECD. The perinephric stranding detected on CT and perinephric inflammation on the PET scan may reflect the hairy kidney of ECD, which is a result of histiocytic infiltration. It is possible that the chemosis relates to exophthalmos from histiocytic orbital infiltrates. Sensitivity for detecting orbital pathology on a PET scan is limited because of the high signal from the adjacent brain.
ECD should be distinguished from Langerhans cell histiocytosis (LCH) by immunohistologic staining and microscopic characteristics of the histiocytes. LCH usually does not involve the aorta, and it more commonly involves the skin.
Serum IgG4 was within normal limits, and immunohistochemical staining of pathology specimens for IgG4 was negative. The BRAF V600E mutation, which is present in the majority of patients with ECD, was detected in a subsequent right perinephric biopsy specimen. The patient was diagnosed with ECD.
Prednisone and pegylated interferon‐ led to a rapid improvement in his symptoms. As the prednisone was tapered, he developed bilateral periorbital swelling. Magnetic resonance imaging (MRI) revealed well‐circumscribed, intraorbital soft tissue masses with partial encasement of his optic nerves and superior ophthalmic veins, as well as infiltration of his transverse sinuses, consistent with intracranial manifestations of ECD. There was no evidence of pituitary, hypothalamic, or other brain parenchymal infiltration. His dyspnea, night sweats, and hypertension improved; however, 3 months into therapy he developed an extensive rash. Interferon was discontinued. Vemurafinib, a serine kinase inhibitor that targets the BRAF mutation, was prescribed with subsequent resolution of the rash.
COMMENTARY
This patient suffered from a chronic, progressive, inflammatory illness. Although the disease initially appeared to be confined to the heart and lungs, laboratory testing signaled a more systemic condition, and subsequent imaging demonstrated involvement of a disparate group of organs. Subacute disease processes with elevated markers of inflammation and diffuse organ involvement often fall into 1 of 3 categories: infectious, autoimmune, or neoplastic. The histiocytoses inhabit a fourth and easily overlooked category that can be described as infiltrative. Infiltrative diseases are a heterogeneous group of conditions that cause illness when cells or substances not normally found in tissues lead to organ dysfunction.
Although traditional teaching has focused on sarcoidosis, amyloidosis, and hemochromatosis as the primary representatives of this category, the medical literature describes a number of other infiltrative disease processes. IgG4‐RD is a fibroinflammatory disorder characterized by space‐occupying lesions, a lymphoplasmacytic infiltrate of IgG4‐positive plasma cells, and storiform (matted and irregularly whorled microscopic pattern) fibrosis.[1] IgG4‐RD, like sarcoidosis, blurs the categorical line between infiltrative and autoimmune diseases. Other infiltrative cellular disorders, such as histiocytosis and mastocytosis, exist on a spectrum between monoclonal proliferation and neoplastic invasion.
The histiocytoses represent a diverse group of disorders with an evolving nomenclature, characterized by localized or diffuse infiltration of macrophages, monocytes, and dendritic cells (Table 1). ECD is a rare, non‐Langerhans histiocytosis characterized by excessive recruitment and activation of histiocytes through kinase signaling pathways.[2, 3] Immunohistochemical staining for CD68, CD163, and Factor XIIIa, with lack of staining for CD1a, S100, and CD207, supports the diagnosis.[3] Mutations in the BRAF V600E gene (a protein kinase involved in cell proliferation) represent the most likely etiology of this overactivation. An estimated 38% to 100% of patients with ECD harbor this mutation, with detection rates influenced by the sensitivity of testing techniques.[3] The serine kinase inhibitor vemurafinib targets this mutation, and early experience with this agent in ECD demonstrates encouraging results.[4]
| Dendritic cell disorders |
| Langerhans cell histiocytosis |
| Secondary dendritic cell processes |
| Juvenile xanthogranuloma and related disorders (including Erdheim‐Chester disease) |
| Solitary histiocytomas with a dendritic phenotype |
| Macrophage‐related disorders |
| Primary hemophagocytic lymphohistiocytosis (familial and sporadic) |
| Secondary hemophagocytic syndromes |
| Sinus histiocytosis with massive lymphadenopathy (Rosai‐Dorfman disease) |
| Solitary histiocytoma with a macrophage phenotype |
| Malignant histiocytic disorders |
| Monocyte‐related leukemias |
| Extramedullary monocytic tumor or sarcoma |
| Dendritic cell‐related histiocytic sarcoma |
| Macrophage‐related histiocytic sarcoma |
ECD presents heterogeneously, occurring most commonly between the ages of 40 and 70 years. Nonspecific symptoms include weakness, fatigue, fever, chills, weight loss, and night sweats. Typical sites of involvement include the bone, central nervous system, cardiovascular system, lungs, and retroperitoneum. Bone involvement is nearly universal, and bone pain is the most common presenting symptom. Symmetric diaphyseal and metaphyseal osteosclerotic lesions may be seen on x‐rays, bone scan, PET, CT, and MRI.[3] Approximately 50% of patients have extraskeletal involvement at diagnosis.[5] Neurologic manifestations may result from invasion of histiocytes into the facial bones, orbits, meninges, and intracranial vessels, as eventually developed in this patient. Diabetes insipidus is the most common neurologic manifestation of ECD, followed by exophthalmos, cerebellar ataxia, panhypopituitarism, and papilledema.[6, 7] Approximately 75% of patients eventually suffer from cardiovascular disease, including hypertension, congestive heart failure, acute myocardial infarction, valvular dysfunction, pericardial infiltration, and cardiac tamponade.[8] Vascular involvement includes perivascular infiltration and periaortic fibrosis, resulting in the coated aorta seen in 20% of patients with ECD.[3] Pulmonary manifestations of ECD include interstitial, pleural, and consolidative lung disease. A review of high‐resolution chest CTs of patients with ECD demonstrated that greater than half had evidence of parenchymal lung disease, with interlobular septal thickening being the most common finding.[9] Infiltration and fibrosis of retroperitoneal structures is common. Infiltration of perinephric fat creates irregular renal borders, appearing radiographically as hairy kidneys.
Arriving at the diagnosis in this case proved to be challenging because the early presentation was consistent with congestive heart failure. As the patient's conditioned deteriorated, imaging suggested multisystem involvement. It was the extensive aortopathy in particularnot the less specific bone, kidney, lymph node, or pulmonary findingsthat allowed the clinicians to hone the extensive differential diagnosis. The coated aorta is a finding that has been strongly associated with ECD; few other conditions coat the aorta in a similar fashion.[10] In most mysteries, the perpetrator's coat conceals his identity; however, in this story the coat gave it away.
KEY LEARNING POINTS
- Subacute, inflammatory, multiorgan disease is usually explained by 3 categoriesinfection, autoimmunity, and neoplasiabut a fourth category, infiltrative disorders, sometimes warrants consideration.
- ECD presents heterogeneously, ranging from localized disease to widespread organ infiltration. The classic presentation includes bone pain, diabetes insipidus, and exophthalmos.
- Characteristic radiological findings that suggest ECD include long bone osteosclerosis, a coated aorta from periaortic infiltration, and hairy kidneys from perinephric infiltration.
Disclosure
Nothing to report
- , , IgG4‐related disease. N Engl J Med. 2012;366(6):539–551.
- , , , Diagnosing Erdheim‐Chester disease. Ann Rheum Dis. 2013;72(7):e19.
- , , , et al. Consensus guidelines for the diagnosis and clinical management of Erdheim‐Chester disease. Blood. 2014;124(4):483–492.
- , , , et al. The efficacy of vemurafenib in Erdheim‐Chester Disease and Langerhans Cell Histiocytosis: preliminary results from VE‐Basket Study. Blood. 2014;124(21):635.
- , , , et al. Erdheim‐Chester disease. Clinical and radiologic characteristics of 59 cases. Medicine (Baltimore). 1996;75(3):157–169.
- , , , et al. Neurological manifestations and neuroradiological presentation of Erdheim‐Chester disease: report of 6 cases and systematic review of the literature. J Neurol. 2006;253(10):1267–1277.
- , , , et al. Cerebral, facial, and orbital involvement in Erdheim‐Chester disease: CT and MR imaging findings. Radiology. 2010;255(2):586–594.
- , , , et al. Images in cardiovascular medicine. Cardiac involvement in Erdheim‐Chester disease: magnetic resonance and computed tomographic scan imaging in a monocentric series of 37 patients. Circulation. 2009;119(25):e597–e598.
- , , , et al. Pulmonary involvement in Erdheim‐Chester disease: a single‐center study of thirty‐four patients and a review of the literature. Arthritis Rheum. 2010;62(11):3504–3512.
- , , , et al. “Coated aorta”: a new sign of Erdheim‐Chester disease. J Rheumatol. 2000;27(6):1550–1553.
- , , IgG4‐related disease. N Engl J Med. 2012;366(6):539–551.
- , , , Diagnosing Erdheim‐Chester disease. Ann Rheum Dis. 2013;72(7):e19.
- , , , et al. Consensus guidelines for the diagnosis and clinical management of Erdheim‐Chester disease. Blood. 2014;124(4):483–492.
- , , , et al. The efficacy of vemurafenib in Erdheim‐Chester Disease and Langerhans Cell Histiocytosis: preliminary results from VE‐Basket Study. Blood. 2014;124(21):635.
- , , , et al. Erdheim‐Chester disease. Clinical and radiologic characteristics of 59 cases. Medicine (Baltimore). 1996;75(3):157–169.
- , , , et al. Neurological manifestations and neuroradiological presentation of Erdheim‐Chester disease: report of 6 cases and systematic review of the literature. J Neurol. 2006;253(10):1267–1277.
- , , , et al. Cerebral, facial, and orbital involvement in Erdheim‐Chester disease: CT and MR imaging findings. Radiology. 2010;255(2):586–594.
- , , , et al. Images in cardiovascular medicine. Cardiac involvement in Erdheim‐Chester disease: magnetic resonance and computed tomographic scan imaging in a monocentric series of 37 patients. Circulation. 2009;119(25):e597–e598.
- , , , et al. Pulmonary involvement in Erdheim‐Chester disease: a single‐center study of thirty‐four patients and a review of the literature. Arthritis Rheum. 2010;62(11):3504–3512.
- , , , et al. “Coated aorta”: a new sign of Erdheim‐Chester disease. J Rheumatol. 2000;27(6):1550–1553.
EVB in Hospitalized Cirrhotic Patients
Cirrhosis is a leading cause of death in the United States. In 2010, cirrhosis resulted in an estimated 49,500 deaths, which represented a significant increase from 35,500 deaths 2 decades ago.[1] Cirrhotic patients are susceptible to numerous disease‐specific complications including ascites, esophageal varices, hepatic encephalopathy (HE), and hepatorenal syndrome (HRS).[2]
Esophageal varices develop in approximately 50% of patient with cirrhosis, and their presence correlates with the severity of liver disease.[3] In cirrhotic patients, esophageal variceal bleeding (EVB) occurs at an annual rate of 5% to 15% and results in substantial morbidity and mortality.[3] Utilizing US national data, Jamal et al. reported a decline in the rate of hospitalizations related to EVB from 1988 to 2002.[4] However, recent large‐scale studies relating to the epidemiology of EVB are lacking. We conducted a retrospective analysis using a national US database to study the differences in demographic characteristics, rate of complications, outcomes, and temporal trends in hospitalized cirrhotic patients with and without EVB.
METHODS
We utilized biennial data (20022012) from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample using methods described earlier.[5] Initially, we extracted all entries with any discharge diagnosis of cirrhosis (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD‐9‐CM] codes: 571.2, 571.5, 571.6) in adult patients ages 18 years and older.[6] Within this cirrhotic population, we next extracted all entries with any discharge diagnosis of EVB (ICD‐9‐CM codes: 456.0., 456.20).[6] Population‐based rates relating to hospital discharges were reported as per 100,000 population/year.
The outcome variables of interest were in‐hospital mortality, total charges (rounded to the nearest $1000) and length of stay (LOS). Demographic details and hospital characteristics were also extracted. Cases were queried for complications well recognized in cirrhotic patients. These included urinary tract infection (UTI) (ICD‐9‐CM codes: 1122, 59010‐11, 5902‐03, 59080‐81, 5950, 5970, 5990), skin and subcutaneous tissue infections (SSCI) (ICD‐9‐CM codes: 680‐82, 684, 686), spontaneous bacterial peritonitis (SBP) (ICD‐9‐CM codes: 56723, 5672), Clostridium difficile infection (ICD‐9‐CM code: 00845), or pneumonia (ICD‐9‐CM codes: 480‐83, 487).[6] Also queried were HE (ICD‐9‐CM code: 572.2)[7] and HRS (ICD‐9‐CM code: 572.4).[8] Comorbid conditions were assessed using the Elixhauser comorbidity index minus the presence of liver disorders but including alcohol abuse.[9]
Statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC). To determine the independent association of EVB on outcome variables, we performed case‐control matching (EVB vs no EVB). We used high‐dimensional propensity scores in a 1:5 matching ratio with a greedy matching algorithm generated by regression analysis of patients with EVB based on demographics details (age, gender, insurance status), comorbid conditions, alcohol abuse, infections as detailed above, HE, and HRS. The 2 test and the Mann‐Whitney U test compared categorical and continuous variables. For trend analysis, we used the Cochrane‐Armitage test. The threshold for significance for all analyses was P0.01.
RESULTS
In 2012, there were 570,020 hospital discharges related to cirrhosis in patients 18 years of age and older. Within this cohort, EVB occurred in 32,945 discharges (5.78%). Table 1 details differences between cirrhotic patients with and without EVB. Comparatively, patients with EVB were younger (median age 55 years, interquartile range [IQR] 13 years vs median age 58 years, IQR 15 years; P0.01), more likely to be male (70.1% vs 60.4%; P0.01), and without health insurance (21.0% vs 12.50%; P0.01). Minor differences between the 2 groups were observed in respect to hospital region, location, teaching status, and household income quartile. There was no difference in the number of comorbid conditions (median 4 comorbid conditions in each group).
| Study Group | P Value | ||
|---|---|---|---|
| Cirrhosis Without Variceal Bleeding | Cirrhosis With Variceal Bleeding | ||
| |||
| Total 570,220 (100%) | 537,275 (94.22%) | 32,945 (5.78%) | |
| Age, y, median (IQR) | 58 (15) | 55 (13) | |
| Gender | |||
| Male | 60.40% | 70.10% | |
| Female | 39.60% | 29.90% | |
| Mortality | 5.80% | 9.90% | |
| Insurance | |||
| Private | 19.70% | 22.40% | |
| Medicare/Medicaid | 67.80% | 56.60% | |
| None | 12.50% | 21.00% | |
| Length of stay, median (IQR) | 4 (5) | 4 (4) | |
| Hospital charges, median (IQR) | 28 (39) | 41 (49) | |
| Associated comorbidities, median (IQR) | 4 (2) | 4 (3) | |
| Alcohol consumption | 48.80% | 63.90% | |
| Infections | |||
| Overall | 24.10% | 13.50% | |
| UTI | 13.10% | 6.90% | |
| Pneumonia | 1.50% | 1.40% | 0.03 |
| SBP | 3.40% | 3.40% | 0.45 |
| SSCI | 6.30% | 1.70% | |
| CDI | 2.20% | 1.40% | |
| Hepatic encephalopathy | 17.70% | 18.80% | |
| Hepatorenal syndrome | 3.70% | 4.30% | |
| EVL | 66.40% | ||
| TIPS | 4.90% | ||
| Blood transfusions | 56.90% | ||
Patients with EVB suffered a significantly higher rate of alcohol abuse (63.90% vs 48.80%; P0.01). EVB was also associated with an overall lower incidence of infection (13.50% vs 24.10%; P0.01). Specifically, the greatest difference in rates of infection were observed for UTI (6.90% vs 13.10%; P0.01) and SSCI (1.70% vs 6.30%; P0.01). Also, patients with EVB demonstrated a small, yet significant increased incidence of HE (18.80% vs 17.70%; P0.01) and HRS (4.30% vs 3.70%; P0.01).
Cirrhotic patients with EVB demonstrated worse overall outcomes compared to their counterparts without EVB. This manifested in an unadjusted higher mortality rate (9.90% vs 5.80%; P0.01) and increased hospital charges (median $41,000 [IQR $49,000] vs $28,000 [IQR $39,000]; P0.01). LOS between the 2 groups did not differ (median 4 days). After adjusting for demographic differences, complications, and comorbid conditions, EVB in patients with cirrhosis continued to be independently associated with a higher mortality rate (10.00% vs 5.00%; P0.01) and increased hospital charges (median $41,000 [IQR $49,000] vs $26,000 [IQR $34,000]; P0.01). Again, LOS was similar for the 2 groups (median 4 days).
Between the years 2002 and 2012, the number of hospital discharges related to cirrhosis increased from 337,956 to 570,220 (P0.01). Concurrently, the incidence of EVB in this population declined from 8.60% to 5.78% (Figure 1), representing an overall decrease of 33.0% with a significant decreased trend (P0.01).
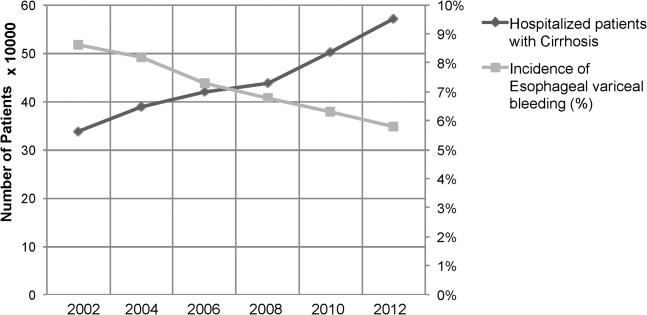
We also calculated population‐adjusted hospitalization rates for discharges related to cirrhosis and EVB. The rate of cirrhosis‐related discharges continued to demonstrate an increased trend from 157.42/100,000 population in 2002 to 237.43/100,000 population in 2012 (P0.01). However, no significant trend was observed for EVB‐related hospital discharges in the same period of time (13.60/100,000 population in 2002 to 13.72/100,000 population in 2012; P=0.91).
DISCUSSION
Our results indicated a significantly higher rate of alcohol abuse in cirrhotic patients with EVB. Alcohol consumption is an independent risk factor for esophageal variceal bleeding.[10, 11] Continued alcohol consumption not only increases the risk for development of varices but may also precipitate variceal rupture.[10] Other risk factors associated with EVB in this study (younger age, male, lower economic status) are likely related to a higher incidence of alcohol abuse in this demographic.[12]
Patients with EVB were also noted to have a lower overall incidence of infection, especially UTI and SSCI. The use of broad‐spectrum antibiotics decreases mortality from secondary infection and improves the prognosis of cirrhotic patients with EVB.[13, 14] The American Association for the Study of Liver Diseases recommends the use of third‐generation cephalosporins in the setting of EVB.[3] The widespread adoption of this in clinical practice may have contributed to a decreased rate of infection in patients with EVB. The difference in the incidence rates of HE and HRS, although statistically significant, were small, and likely the consequence of the large numbers involved in our study.
Our results also indicate that cirrhotic patients with EVB were twice as likely to die compared to matched counterparts without EVB. The increased mortality associated with EVB could be related to hemorrhagic/hypovolemic shock and cardiovascular collapse, aspiration into airway, multiorgan dysfunction due to poor perfusion, infections including SBP, and HE. Although prior studies have demonstrated the relationship between EVB and increased mortality, typically they have been restricted to small single‐center studies involving fewer than 200 patients.[6, 7, 8, 9] Cirrhotic patients with EVB also incurred significantly higher hospital charges compared to matched counterparts. Interestingly, the hospital LOS did not differ between the 2 groups. Intensive care and procedural costs were likely a major contributor to the higher charges; cirrhotic patients with EVB underwent a median of 3 procedures (IQR 2) during their hospital stay compared to a median of 1 procedure (IQR 3) for cirrhotic patients without EVB (P0.01; data not shown).
In contrast to trends from earlier decades,[4] the population‐adjusted rate of EVB‐related hospital discharges did not change significantly from 2002 to 2012. However, these data are confounded in their interpretation by a substantial increase in the prevalence of cirrhosis in the United States during the same time period.[15] Therefore, it may be more meaningful to state that there was a contemporaneous decline in EVB‐related hospital discharges when considered in the context of a complicating rate in hospitalized cirrhotic patients. These results are consistent with a recent single‐center study[16] and are very likely the fruition of intensive screening programs with primary and secondary prophylaxis for EVB involving esophageal variceal ligation and pharmacotherapy (‐blockers) as well as the increased acceptance of transjugular intrahepatic portosystemic shunt placement.[17, 18, 19]
There are limitations to our study. First, we relied exclusively on ICD‐9‐CM codes for case identification. Second, there is a nonavailability of data pertaining to Model for End‐Stage Liver Disease score calculations, medication, and antibiotic usage. Third, the Nationwide Inpatient Sample database does not allow for distinguishing individual patients with repeat admissions. Finally, our results represent a weighted estimate of national data.
CONCLUSION
EVB in cirrhotic patients was associated with significantly higher mortality and increased hospital charges. Also, the rate of EVB‐related hospital discharges as a complicating factor in patients with cirrhosis declined significantly during the decade 2002 to 2012. This likely reflects the ongoing effectiveness of primary and secondary prophylaxis.
Acknowledgements
The authors acknowledge the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample, sponsored by the Agency for Healthcare Research and Quality, which contributes to HCUP (
Disclosures: C.P., the first author and corresponding author, conceptualized the study, and with A.D. gathered and analyzed the data. C.P. and M.D. wrote, edited, and proofread the manuscript as well as created the bibliography and formulated the table and figure. R.G., R.T., and M.O. edited, commented on, and reviewed the manuscript. All of the authors reviewed and agreed on the final version of the manuscript for submission. The authors report no conflicts of interest.
- US Burden of Disease Collaborators. The state of US health, 1990‐2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608.
- , Complications of cirrhosis. Curr Opin Gastroenterol. 2012;28(3):223–229.
- , , , , Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922–938.
- , , , Declining hospitalization rate of esophageal variceal bleeding in the United States. Clin Gastroenterol Hepatol. 2008;6(6):689–695; quiz 605.
- , , , , , Association of Clostridium difficile infection with outcomes of hospitalized solid organ transplant recipients: results from the 2009 Nationwide Inpatient Sample database. Transpl Infect Dis. 2012;14(5):540–547.
- , , Prevalence and in‐hospital mortality trends of infections among patients with cirrhosis: a nationwide study of hospitalised patients in the United States. Aliment Pharmacol Ther. 2014;40(1):105–112.
- , , Racial disparities in the management of hospitalized patients with cirrhosis and complications of portal hypertension: a national study. Hepatology. 2007;45(5):1282–1289.
- , Protein‐calorie malnutrition as a prognostic indicator of mortality among patients hospitalized with cirrhosis and portal hypertension. Liver Int. 2009;29(9):1396–1402.
- , , , Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
- , , , , , Potential precipitating factors of esophageal variceal bleeding: a case‐control study. Am J Gastroenterol. 2011;106(1):96–103.
- , , , et al. Effects of ethanol consumption on hepatic hemodynamics in patients with alcoholic cirrhosis. Gastroenterology. 1997;112(4):1284–1289.
- , , , Prevalence, correlates, disability, and comorbidity of DSM‐IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–842.
- , , Role of prophylactic antibiotics in cirrhotic patients with variceal bleeding. World J Gastroenterol. 2014;20(7):1790–1796.
- , , , et al. Meta‐analysis: antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding—an updated Cochrane review. Aliment Pharmacol Ther. 2011;34(5):509–518.
- , , , et al. The epidemiology of cirrhosis in the United States: a population‐based study [published online ahead of print October 8, 2014]. J Clin Gastroenterol. doi: 10.1097/MCG.0000000000000208.
- , , , Hospitalization for variceal hemorrhage in an era with more prevalent cirrhosis. World J Gastroenterol. 2014;20(32):11326–11332.
- , Banding ligation versus beta‐blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012;8:CD004544.
- , , , et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362(25):2370–2379.
- , , , Meta‐analysis: banding ligation and medical interventions for the prevention of rebleeding from oesophageal varices. Aliment Pharmacol Ther. 2012;35(10):1155–1165.
Cirrhosis is a leading cause of death in the United States. In 2010, cirrhosis resulted in an estimated 49,500 deaths, which represented a significant increase from 35,500 deaths 2 decades ago.[1] Cirrhotic patients are susceptible to numerous disease‐specific complications including ascites, esophageal varices, hepatic encephalopathy (HE), and hepatorenal syndrome (HRS).[2]
Esophageal varices develop in approximately 50% of patient with cirrhosis, and their presence correlates with the severity of liver disease.[3] In cirrhotic patients, esophageal variceal bleeding (EVB) occurs at an annual rate of 5% to 15% and results in substantial morbidity and mortality.[3] Utilizing US national data, Jamal et al. reported a decline in the rate of hospitalizations related to EVB from 1988 to 2002.[4] However, recent large‐scale studies relating to the epidemiology of EVB are lacking. We conducted a retrospective analysis using a national US database to study the differences in demographic characteristics, rate of complications, outcomes, and temporal trends in hospitalized cirrhotic patients with and without EVB.
METHODS
We utilized biennial data (20022012) from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample using methods described earlier.[5] Initially, we extracted all entries with any discharge diagnosis of cirrhosis (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD‐9‐CM] codes: 571.2, 571.5, 571.6) in adult patients ages 18 years and older.[6] Within this cirrhotic population, we next extracted all entries with any discharge diagnosis of EVB (ICD‐9‐CM codes: 456.0., 456.20).[6] Population‐based rates relating to hospital discharges were reported as per 100,000 population/year.
The outcome variables of interest were in‐hospital mortality, total charges (rounded to the nearest $1000) and length of stay (LOS). Demographic details and hospital characteristics were also extracted. Cases were queried for complications well recognized in cirrhotic patients. These included urinary tract infection (UTI) (ICD‐9‐CM codes: 1122, 59010‐11, 5902‐03, 59080‐81, 5950, 5970, 5990), skin and subcutaneous tissue infections (SSCI) (ICD‐9‐CM codes: 680‐82, 684, 686), spontaneous bacterial peritonitis (SBP) (ICD‐9‐CM codes: 56723, 5672), Clostridium difficile infection (ICD‐9‐CM code: 00845), or pneumonia (ICD‐9‐CM codes: 480‐83, 487).[6] Also queried were HE (ICD‐9‐CM code: 572.2)[7] and HRS (ICD‐9‐CM code: 572.4).[8] Comorbid conditions were assessed using the Elixhauser comorbidity index minus the presence of liver disorders but including alcohol abuse.[9]
Statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC). To determine the independent association of EVB on outcome variables, we performed case‐control matching (EVB vs no EVB). We used high‐dimensional propensity scores in a 1:5 matching ratio with a greedy matching algorithm generated by regression analysis of patients with EVB based on demographics details (age, gender, insurance status), comorbid conditions, alcohol abuse, infections as detailed above, HE, and HRS. The 2 test and the Mann‐Whitney U test compared categorical and continuous variables. For trend analysis, we used the Cochrane‐Armitage test. The threshold for significance for all analyses was P0.01.
RESULTS
In 2012, there were 570,020 hospital discharges related to cirrhosis in patients 18 years of age and older. Within this cohort, EVB occurred in 32,945 discharges (5.78%). Table 1 details differences between cirrhotic patients with and without EVB. Comparatively, patients with EVB were younger (median age 55 years, interquartile range [IQR] 13 years vs median age 58 years, IQR 15 years; P0.01), more likely to be male (70.1% vs 60.4%; P0.01), and without health insurance (21.0% vs 12.50%; P0.01). Minor differences between the 2 groups were observed in respect to hospital region, location, teaching status, and household income quartile. There was no difference in the number of comorbid conditions (median 4 comorbid conditions in each group).
| Study Group | P Value | ||
|---|---|---|---|
| Cirrhosis Without Variceal Bleeding | Cirrhosis With Variceal Bleeding | ||
| |||
| Total 570,220 (100%) | 537,275 (94.22%) | 32,945 (5.78%) | |
| Age, y, median (IQR) | 58 (15) | 55 (13) | |
| Gender | |||
| Male | 60.40% | 70.10% | |
| Female | 39.60% | 29.90% | |
| Mortality | 5.80% | 9.90% | |
| Insurance | |||
| Private | 19.70% | 22.40% | |
| Medicare/Medicaid | 67.80% | 56.60% | |
| None | 12.50% | 21.00% | |
| Length of stay, median (IQR) | 4 (5) | 4 (4) | |
| Hospital charges, median (IQR) | 28 (39) | 41 (49) | |
| Associated comorbidities, median (IQR) | 4 (2) | 4 (3) | |
| Alcohol consumption | 48.80% | 63.90% | |
| Infections | |||
| Overall | 24.10% | 13.50% | |
| UTI | 13.10% | 6.90% | |
| Pneumonia | 1.50% | 1.40% | 0.03 |
| SBP | 3.40% | 3.40% | 0.45 |
| SSCI | 6.30% | 1.70% | |
| CDI | 2.20% | 1.40% | |
| Hepatic encephalopathy | 17.70% | 18.80% | |
| Hepatorenal syndrome | 3.70% | 4.30% | |
| EVL | 66.40% | ||
| TIPS | 4.90% | ||
| Blood transfusions | 56.90% | ||
Patients with EVB suffered a significantly higher rate of alcohol abuse (63.90% vs 48.80%; P0.01). EVB was also associated with an overall lower incidence of infection (13.50% vs 24.10%; P0.01). Specifically, the greatest difference in rates of infection were observed for UTI (6.90% vs 13.10%; P0.01) and SSCI (1.70% vs 6.30%; P0.01). Also, patients with EVB demonstrated a small, yet significant increased incidence of HE (18.80% vs 17.70%; P0.01) and HRS (4.30% vs 3.70%; P0.01).
Cirrhotic patients with EVB demonstrated worse overall outcomes compared to their counterparts without EVB. This manifested in an unadjusted higher mortality rate (9.90% vs 5.80%; P0.01) and increased hospital charges (median $41,000 [IQR $49,000] vs $28,000 [IQR $39,000]; P0.01). LOS between the 2 groups did not differ (median 4 days). After adjusting for demographic differences, complications, and comorbid conditions, EVB in patients with cirrhosis continued to be independently associated with a higher mortality rate (10.00% vs 5.00%; P0.01) and increased hospital charges (median $41,000 [IQR $49,000] vs $26,000 [IQR $34,000]; P0.01). Again, LOS was similar for the 2 groups (median 4 days).
Between the years 2002 and 2012, the number of hospital discharges related to cirrhosis increased from 337,956 to 570,220 (P0.01). Concurrently, the incidence of EVB in this population declined from 8.60% to 5.78% (Figure 1), representing an overall decrease of 33.0% with a significant decreased trend (P0.01).
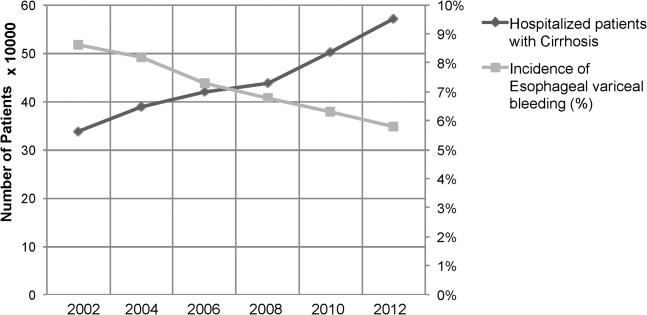
We also calculated population‐adjusted hospitalization rates for discharges related to cirrhosis and EVB. The rate of cirrhosis‐related discharges continued to demonstrate an increased trend from 157.42/100,000 population in 2002 to 237.43/100,000 population in 2012 (P0.01). However, no significant trend was observed for EVB‐related hospital discharges in the same period of time (13.60/100,000 population in 2002 to 13.72/100,000 population in 2012; P=0.91).
DISCUSSION
Our results indicated a significantly higher rate of alcohol abuse in cirrhotic patients with EVB. Alcohol consumption is an independent risk factor for esophageal variceal bleeding.[10, 11] Continued alcohol consumption not only increases the risk for development of varices but may also precipitate variceal rupture.[10] Other risk factors associated with EVB in this study (younger age, male, lower economic status) are likely related to a higher incidence of alcohol abuse in this demographic.[12]
Patients with EVB were also noted to have a lower overall incidence of infection, especially UTI and SSCI. The use of broad‐spectrum antibiotics decreases mortality from secondary infection and improves the prognosis of cirrhotic patients with EVB.[13, 14] The American Association for the Study of Liver Diseases recommends the use of third‐generation cephalosporins in the setting of EVB.[3] The widespread adoption of this in clinical practice may have contributed to a decreased rate of infection in patients with EVB. The difference in the incidence rates of HE and HRS, although statistically significant, were small, and likely the consequence of the large numbers involved in our study.
Our results also indicate that cirrhotic patients with EVB were twice as likely to die compared to matched counterparts without EVB. The increased mortality associated with EVB could be related to hemorrhagic/hypovolemic shock and cardiovascular collapse, aspiration into airway, multiorgan dysfunction due to poor perfusion, infections including SBP, and HE. Although prior studies have demonstrated the relationship between EVB and increased mortality, typically they have been restricted to small single‐center studies involving fewer than 200 patients.[6, 7, 8, 9] Cirrhotic patients with EVB also incurred significantly higher hospital charges compared to matched counterparts. Interestingly, the hospital LOS did not differ between the 2 groups. Intensive care and procedural costs were likely a major contributor to the higher charges; cirrhotic patients with EVB underwent a median of 3 procedures (IQR 2) during their hospital stay compared to a median of 1 procedure (IQR 3) for cirrhotic patients without EVB (P0.01; data not shown).
In contrast to trends from earlier decades,[4] the population‐adjusted rate of EVB‐related hospital discharges did not change significantly from 2002 to 2012. However, these data are confounded in their interpretation by a substantial increase in the prevalence of cirrhosis in the United States during the same time period.[15] Therefore, it may be more meaningful to state that there was a contemporaneous decline in EVB‐related hospital discharges when considered in the context of a complicating rate in hospitalized cirrhotic patients. These results are consistent with a recent single‐center study[16] and are very likely the fruition of intensive screening programs with primary and secondary prophylaxis for EVB involving esophageal variceal ligation and pharmacotherapy (‐blockers) as well as the increased acceptance of transjugular intrahepatic portosystemic shunt placement.[17, 18, 19]
There are limitations to our study. First, we relied exclusively on ICD‐9‐CM codes for case identification. Second, there is a nonavailability of data pertaining to Model for End‐Stage Liver Disease score calculations, medication, and antibiotic usage. Third, the Nationwide Inpatient Sample database does not allow for distinguishing individual patients with repeat admissions. Finally, our results represent a weighted estimate of national data.
CONCLUSION
EVB in cirrhotic patients was associated with significantly higher mortality and increased hospital charges. Also, the rate of EVB‐related hospital discharges as a complicating factor in patients with cirrhosis declined significantly during the decade 2002 to 2012. This likely reflects the ongoing effectiveness of primary and secondary prophylaxis.
Acknowledgements
The authors acknowledge the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample, sponsored by the Agency for Healthcare Research and Quality, which contributes to HCUP (
Disclosures: C.P., the first author and corresponding author, conceptualized the study, and with A.D. gathered and analyzed the data. C.P. and M.D. wrote, edited, and proofread the manuscript as well as created the bibliography and formulated the table and figure. R.G., R.T., and M.O. edited, commented on, and reviewed the manuscript. All of the authors reviewed and agreed on the final version of the manuscript for submission. The authors report no conflicts of interest.
Cirrhosis is a leading cause of death in the United States. In 2010, cirrhosis resulted in an estimated 49,500 deaths, which represented a significant increase from 35,500 deaths 2 decades ago.[1] Cirrhotic patients are susceptible to numerous disease‐specific complications including ascites, esophageal varices, hepatic encephalopathy (HE), and hepatorenal syndrome (HRS).[2]
Esophageal varices develop in approximately 50% of patient with cirrhosis, and their presence correlates with the severity of liver disease.[3] In cirrhotic patients, esophageal variceal bleeding (EVB) occurs at an annual rate of 5% to 15% and results in substantial morbidity and mortality.[3] Utilizing US national data, Jamal et al. reported a decline in the rate of hospitalizations related to EVB from 1988 to 2002.[4] However, recent large‐scale studies relating to the epidemiology of EVB are lacking. We conducted a retrospective analysis using a national US database to study the differences in demographic characteristics, rate of complications, outcomes, and temporal trends in hospitalized cirrhotic patients with and without EVB.
METHODS
We utilized biennial data (20022012) from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample using methods described earlier.[5] Initially, we extracted all entries with any discharge diagnosis of cirrhosis (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD‐9‐CM] codes: 571.2, 571.5, 571.6) in adult patients ages 18 years and older.[6] Within this cirrhotic population, we next extracted all entries with any discharge diagnosis of EVB (ICD‐9‐CM codes: 456.0., 456.20).[6] Population‐based rates relating to hospital discharges were reported as per 100,000 population/year.
The outcome variables of interest were in‐hospital mortality, total charges (rounded to the nearest $1000) and length of stay (LOS). Demographic details and hospital characteristics were also extracted. Cases were queried for complications well recognized in cirrhotic patients. These included urinary tract infection (UTI) (ICD‐9‐CM codes: 1122, 59010‐11, 5902‐03, 59080‐81, 5950, 5970, 5990), skin and subcutaneous tissue infections (SSCI) (ICD‐9‐CM codes: 680‐82, 684, 686), spontaneous bacterial peritonitis (SBP) (ICD‐9‐CM codes: 56723, 5672), Clostridium difficile infection (ICD‐9‐CM code: 00845), or pneumonia (ICD‐9‐CM codes: 480‐83, 487).[6] Also queried were HE (ICD‐9‐CM code: 572.2)[7] and HRS (ICD‐9‐CM code: 572.4).[8] Comorbid conditions were assessed using the Elixhauser comorbidity index minus the presence of liver disorders but including alcohol abuse.[9]
Statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC). To determine the independent association of EVB on outcome variables, we performed case‐control matching (EVB vs no EVB). We used high‐dimensional propensity scores in a 1:5 matching ratio with a greedy matching algorithm generated by regression analysis of patients with EVB based on demographics details (age, gender, insurance status), comorbid conditions, alcohol abuse, infections as detailed above, HE, and HRS. The 2 test and the Mann‐Whitney U test compared categorical and continuous variables. For trend analysis, we used the Cochrane‐Armitage test. The threshold for significance for all analyses was P0.01.
RESULTS
In 2012, there were 570,020 hospital discharges related to cirrhosis in patients 18 years of age and older. Within this cohort, EVB occurred in 32,945 discharges (5.78%). Table 1 details differences between cirrhotic patients with and without EVB. Comparatively, patients with EVB were younger (median age 55 years, interquartile range [IQR] 13 years vs median age 58 years, IQR 15 years; P0.01), more likely to be male (70.1% vs 60.4%; P0.01), and without health insurance (21.0% vs 12.50%; P0.01). Minor differences between the 2 groups were observed in respect to hospital region, location, teaching status, and household income quartile. There was no difference in the number of comorbid conditions (median 4 comorbid conditions in each group).
| Study Group | P Value | ||
|---|---|---|---|
| Cirrhosis Without Variceal Bleeding | Cirrhosis With Variceal Bleeding | ||
| |||
| Total 570,220 (100%) | 537,275 (94.22%) | 32,945 (5.78%) | |
| Age, y, median (IQR) | 58 (15) | 55 (13) | |
| Gender | |||
| Male | 60.40% | 70.10% | |
| Female | 39.60% | 29.90% | |
| Mortality | 5.80% | 9.90% | |
| Insurance | |||
| Private | 19.70% | 22.40% | |
| Medicare/Medicaid | 67.80% | 56.60% | |
| None | 12.50% | 21.00% | |
| Length of stay, median (IQR) | 4 (5) | 4 (4) | |
| Hospital charges, median (IQR) | 28 (39) | 41 (49) | |
| Associated comorbidities, median (IQR) | 4 (2) | 4 (3) | |
| Alcohol consumption | 48.80% | 63.90% | |
| Infections | |||
| Overall | 24.10% | 13.50% | |
| UTI | 13.10% | 6.90% | |
| Pneumonia | 1.50% | 1.40% | 0.03 |
| SBP | 3.40% | 3.40% | 0.45 |
| SSCI | 6.30% | 1.70% | |
| CDI | 2.20% | 1.40% | |
| Hepatic encephalopathy | 17.70% | 18.80% | |
| Hepatorenal syndrome | 3.70% | 4.30% | |
| EVL | 66.40% | ||
| TIPS | 4.90% | ||
| Blood transfusions | 56.90% | ||
Patients with EVB suffered a significantly higher rate of alcohol abuse (63.90% vs 48.80%; P0.01). EVB was also associated with an overall lower incidence of infection (13.50% vs 24.10%; P0.01). Specifically, the greatest difference in rates of infection were observed for UTI (6.90% vs 13.10%; P0.01) and SSCI (1.70% vs 6.30%; P0.01). Also, patients with EVB demonstrated a small, yet significant increased incidence of HE (18.80% vs 17.70%; P0.01) and HRS (4.30% vs 3.70%; P0.01).
Cirrhotic patients with EVB demonstrated worse overall outcomes compared to their counterparts without EVB. This manifested in an unadjusted higher mortality rate (9.90% vs 5.80%; P0.01) and increased hospital charges (median $41,000 [IQR $49,000] vs $28,000 [IQR $39,000]; P0.01). LOS between the 2 groups did not differ (median 4 days). After adjusting for demographic differences, complications, and comorbid conditions, EVB in patients with cirrhosis continued to be independently associated with a higher mortality rate (10.00% vs 5.00%; P0.01) and increased hospital charges (median $41,000 [IQR $49,000] vs $26,000 [IQR $34,000]; P0.01). Again, LOS was similar for the 2 groups (median 4 days).
Between the years 2002 and 2012, the number of hospital discharges related to cirrhosis increased from 337,956 to 570,220 (P0.01). Concurrently, the incidence of EVB in this population declined from 8.60% to 5.78% (Figure 1), representing an overall decrease of 33.0% with a significant decreased trend (P0.01).
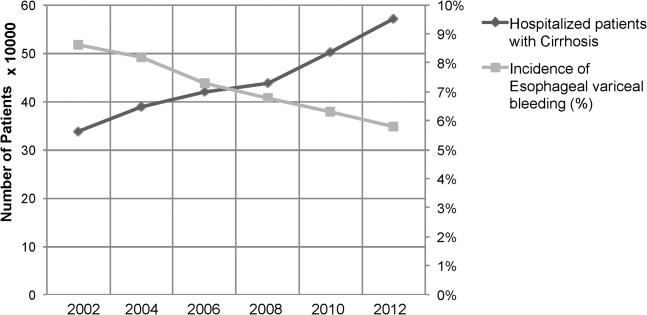
We also calculated population‐adjusted hospitalization rates for discharges related to cirrhosis and EVB. The rate of cirrhosis‐related discharges continued to demonstrate an increased trend from 157.42/100,000 population in 2002 to 237.43/100,000 population in 2012 (P0.01). However, no significant trend was observed for EVB‐related hospital discharges in the same period of time (13.60/100,000 population in 2002 to 13.72/100,000 population in 2012; P=0.91).
DISCUSSION
Our results indicated a significantly higher rate of alcohol abuse in cirrhotic patients with EVB. Alcohol consumption is an independent risk factor for esophageal variceal bleeding.[10, 11] Continued alcohol consumption not only increases the risk for development of varices but may also precipitate variceal rupture.[10] Other risk factors associated with EVB in this study (younger age, male, lower economic status) are likely related to a higher incidence of alcohol abuse in this demographic.[12]
Patients with EVB were also noted to have a lower overall incidence of infection, especially UTI and SSCI. The use of broad‐spectrum antibiotics decreases mortality from secondary infection and improves the prognosis of cirrhotic patients with EVB.[13, 14] The American Association for the Study of Liver Diseases recommends the use of third‐generation cephalosporins in the setting of EVB.[3] The widespread adoption of this in clinical practice may have contributed to a decreased rate of infection in patients with EVB. The difference in the incidence rates of HE and HRS, although statistically significant, were small, and likely the consequence of the large numbers involved in our study.
Our results also indicate that cirrhotic patients with EVB were twice as likely to die compared to matched counterparts without EVB. The increased mortality associated with EVB could be related to hemorrhagic/hypovolemic shock and cardiovascular collapse, aspiration into airway, multiorgan dysfunction due to poor perfusion, infections including SBP, and HE. Although prior studies have demonstrated the relationship between EVB and increased mortality, typically they have been restricted to small single‐center studies involving fewer than 200 patients.[6, 7, 8, 9] Cirrhotic patients with EVB also incurred significantly higher hospital charges compared to matched counterparts. Interestingly, the hospital LOS did not differ between the 2 groups. Intensive care and procedural costs were likely a major contributor to the higher charges; cirrhotic patients with EVB underwent a median of 3 procedures (IQR 2) during their hospital stay compared to a median of 1 procedure (IQR 3) for cirrhotic patients without EVB (P0.01; data not shown).
In contrast to trends from earlier decades,[4] the population‐adjusted rate of EVB‐related hospital discharges did not change significantly from 2002 to 2012. However, these data are confounded in their interpretation by a substantial increase in the prevalence of cirrhosis in the United States during the same time period.[15] Therefore, it may be more meaningful to state that there was a contemporaneous decline in EVB‐related hospital discharges when considered in the context of a complicating rate in hospitalized cirrhotic patients. These results are consistent with a recent single‐center study[16] and are very likely the fruition of intensive screening programs with primary and secondary prophylaxis for EVB involving esophageal variceal ligation and pharmacotherapy (‐blockers) as well as the increased acceptance of transjugular intrahepatic portosystemic shunt placement.[17, 18, 19]
There are limitations to our study. First, we relied exclusively on ICD‐9‐CM codes for case identification. Second, there is a nonavailability of data pertaining to Model for End‐Stage Liver Disease score calculations, medication, and antibiotic usage. Third, the Nationwide Inpatient Sample database does not allow for distinguishing individual patients with repeat admissions. Finally, our results represent a weighted estimate of national data.
CONCLUSION
EVB in cirrhotic patients was associated with significantly higher mortality and increased hospital charges. Also, the rate of EVB‐related hospital discharges as a complicating factor in patients with cirrhosis declined significantly during the decade 2002 to 2012. This likely reflects the ongoing effectiveness of primary and secondary prophylaxis.
Acknowledgements
The authors acknowledge the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample, sponsored by the Agency for Healthcare Research and Quality, which contributes to HCUP (
Disclosures: C.P., the first author and corresponding author, conceptualized the study, and with A.D. gathered and analyzed the data. C.P. and M.D. wrote, edited, and proofread the manuscript as well as created the bibliography and formulated the table and figure. R.G., R.T., and M.O. edited, commented on, and reviewed the manuscript. All of the authors reviewed and agreed on the final version of the manuscript for submission. The authors report no conflicts of interest.
- US Burden of Disease Collaborators. The state of US health, 1990‐2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608.
- , Complications of cirrhosis. Curr Opin Gastroenterol. 2012;28(3):223–229.
- , , , , Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922–938.
- , , , Declining hospitalization rate of esophageal variceal bleeding in the United States. Clin Gastroenterol Hepatol. 2008;6(6):689–695; quiz 605.
- , , , , , Association of Clostridium difficile infection with outcomes of hospitalized solid organ transplant recipients: results from the 2009 Nationwide Inpatient Sample database. Transpl Infect Dis. 2012;14(5):540–547.
- , , Prevalence and in‐hospital mortality trends of infections among patients with cirrhosis: a nationwide study of hospitalised patients in the United States. Aliment Pharmacol Ther. 2014;40(1):105–112.
- , , Racial disparities in the management of hospitalized patients with cirrhosis and complications of portal hypertension: a national study. Hepatology. 2007;45(5):1282–1289.
- , Protein‐calorie malnutrition as a prognostic indicator of mortality among patients hospitalized with cirrhosis and portal hypertension. Liver Int. 2009;29(9):1396–1402.
- , , , Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
- , , , , , Potential precipitating factors of esophageal variceal bleeding: a case‐control study. Am J Gastroenterol. 2011;106(1):96–103.
- , , , et al. Effects of ethanol consumption on hepatic hemodynamics in patients with alcoholic cirrhosis. Gastroenterology. 1997;112(4):1284–1289.
- , , , Prevalence, correlates, disability, and comorbidity of DSM‐IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–842.
- , , Role of prophylactic antibiotics in cirrhotic patients with variceal bleeding. World J Gastroenterol. 2014;20(7):1790–1796.
- , , , et al. Meta‐analysis: antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding—an updated Cochrane review. Aliment Pharmacol Ther. 2011;34(5):509–518.
- , , , et al. The epidemiology of cirrhosis in the United States: a population‐based study [published online ahead of print October 8, 2014]. J Clin Gastroenterol. doi: 10.1097/MCG.0000000000000208.
- , , , Hospitalization for variceal hemorrhage in an era with more prevalent cirrhosis. World J Gastroenterol. 2014;20(32):11326–11332.
- , Banding ligation versus beta‐blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012;8:CD004544.
- , , , et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362(25):2370–2379.
- , , , Meta‐analysis: banding ligation and medical interventions for the prevention of rebleeding from oesophageal varices. Aliment Pharmacol Ther. 2012;35(10):1155–1165.
- US Burden of Disease Collaborators. The state of US health, 1990‐2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608.
- , Complications of cirrhosis. Curr Opin Gastroenterol. 2012;28(3):223–229.
- , , , , Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922–938.
- , , , Declining hospitalization rate of esophageal variceal bleeding in the United States. Clin Gastroenterol Hepatol. 2008;6(6):689–695; quiz 605.
- , , , , , Association of Clostridium difficile infection with outcomes of hospitalized solid organ transplant recipients: results from the 2009 Nationwide Inpatient Sample database. Transpl Infect Dis. 2012;14(5):540–547.
- , , Prevalence and in‐hospital mortality trends of infections among patients with cirrhosis: a nationwide study of hospitalised patients in the United States. Aliment Pharmacol Ther. 2014;40(1):105–112.
- , , Racial disparities in the management of hospitalized patients with cirrhosis and complications of portal hypertension: a national study. Hepatology. 2007;45(5):1282–1289.
- , Protein‐calorie malnutrition as a prognostic indicator of mortality among patients hospitalized with cirrhosis and portal hypertension. Liver Int. 2009;29(9):1396–1402.
- , , , Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
- , , , , , Potential precipitating factors of esophageal variceal bleeding: a case‐control study. Am J Gastroenterol. 2011;106(1):96–103.
- , , , et al. Effects of ethanol consumption on hepatic hemodynamics in patients with alcoholic cirrhosis. Gastroenterology. 1997;112(4):1284–1289.
- , , , Prevalence, correlates, disability, and comorbidity of DSM‐IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–842.
- , , Role of prophylactic antibiotics in cirrhotic patients with variceal bleeding. World J Gastroenterol. 2014;20(7):1790–1796.
- , , , et al. Meta‐analysis: antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding—an updated Cochrane review. Aliment Pharmacol Ther. 2011;34(5):509–518.
- , , , et al. The epidemiology of cirrhosis in the United States: a population‐based study [published online ahead of print October 8, 2014]. J Clin Gastroenterol. doi: 10.1097/MCG.0000000000000208.
- , , , Hospitalization for variceal hemorrhage in an era with more prevalent cirrhosis. World J Gastroenterol. 2014;20(32):11326–11332.
- , Banding ligation versus beta‐blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012;8:CD004544.
- , , , et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362(25):2370–2379.
- , , , Meta‐analysis: banding ligation and medical interventions for the prevention of rebleeding from oesophageal varices. Aliment Pharmacol Ther. 2012;35(10):1155–1165.
Letter to the Editor
The recently published article by Schouten et al.[1] showed no difference in measured patient outcomes with the use of face‐to‐face handoffs. The authors bring several potential explanations for this observation, all of which might be relevant. Another potential explanation could be the human brain's very predisposition for cognitive biases, and face‐to‐face interaction only increases this possibility. The "framing effect" is a cognitive bias when people make decisions differently depending how information is presented, and "anchoring" describes the human tendency to rely heavily on the first piece of information provided. In our case, the daytime physicians who received face‐to‐face handoffs could have been biased with additional information provided and how this information was provided, and this could have increased the rate of measured adverse patient outcome for this group, eliminating the between group difference. More research is needed to study the influence of the cognitive biases in the medical field.
- , , , , . Association of face‐to‐face handoffs and outcomes of hospitalized internal medicine patients. J Hosp Med. 2015;10(3):137–141.
The recently published article by Schouten et al.[1] showed no difference in measured patient outcomes with the use of face‐to‐face handoffs. The authors bring several potential explanations for this observation, all of which might be relevant. Another potential explanation could be the human brain's very predisposition for cognitive biases, and face‐to‐face interaction only increases this possibility. The "framing effect" is a cognitive bias when people make decisions differently depending how information is presented, and "anchoring" describes the human tendency to rely heavily on the first piece of information provided. In our case, the daytime physicians who received face‐to‐face handoffs could have been biased with additional information provided and how this information was provided, and this could have increased the rate of measured adverse patient outcome for this group, eliminating the between group difference. More research is needed to study the influence of the cognitive biases in the medical field.
The recently published article by Schouten et al.[1] showed no difference in measured patient outcomes with the use of face‐to‐face handoffs. The authors bring several potential explanations for this observation, all of which might be relevant. Another potential explanation could be the human brain's very predisposition for cognitive biases, and face‐to‐face interaction only increases this possibility. The "framing effect" is a cognitive bias when people make decisions differently depending how information is presented, and "anchoring" describes the human tendency to rely heavily on the first piece of information provided. In our case, the daytime physicians who received face‐to‐face handoffs could have been biased with additional information provided and how this information was provided, and this could have increased the rate of measured adverse patient outcome for this group, eliminating the between group difference. More research is needed to study the influence of the cognitive biases in the medical field.
- , , , , . Association of face‐to‐face handoffs and outcomes of hospitalized internal medicine patients. J Hosp Med. 2015;10(3):137–141.
- , , , , . Association of face‐to‐face handoffs and outcomes of hospitalized internal medicine patients. J Hosp Med. 2015;10(3):137–141.
Letter to the Editor/
As a practicing hospitalist, I enjoyed the recently published research article by Schouten et al.[1] Their findings are not surprising to our hospitalist group. We evolved over the years from mandatory face‐to‐face or verbal handoffs to secured e‐mail communications. The night physician transfers care through a secured hospital‐provided email by 7 am. This information is supplemented by a phone call, originating from the day hospitalist on an as‐needed basis. This system works best for most community hospitalist programs, because it provides flexibility, improved communication, and saves a lot of time. In the era of electronic medical records and constantly updated tests results, a face‐to‐face communication is less important. We used to spend 45 to 60 minutes on the handoffs, sometimes even longer due to people being late or not answering phone calls right away. It squeezed time out of patient encounters. The accepting day hospitalist needed to review electronic records (including dictated history and physical information if completed) during the course of the day regardless of the sign out from the night physician. Now, the information flow is smoother and it leaves more time for patient encounters. The day hospitalist keeps printed e‐mail with him or her so that information is readily accessible.
For the relatively smaller community hospitalist groups, it is difficult to ensure that all hospitalists will be available for the face‐to‐face handoffs. The hospitalist who is supposed to take sign‐outs could also be on call for the admissions or responsible for codes or rapid responses, which may interrupt or delay the sign‐out process. The Society of Hospital Medicine recommends both written and verbal sign‐outs.[2] This goal could be achieved more efficiently by the model followed by our group as discussed above. The verbal component could be over the phone rather than face‐to‐face meetings.
- , , , , . Association of face‐to‐face handoffs and outcomes of hospitalized internal medicine patients. J Hosp Med. 2015;10(3):137–141.
- , , , , , . Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7):433–440.
As a practicing hospitalist, I enjoyed the recently published research article by Schouten et al.[1] Their findings are not surprising to our hospitalist group. We evolved over the years from mandatory face‐to‐face or verbal handoffs to secured e‐mail communications. The night physician transfers care through a secured hospital‐provided email by 7 am. This information is supplemented by a phone call, originating from the day hospitalist on an as‐needed basis. This system works best for most community hospitalist programs, because it provides flexibility, improved communication, and saves a lot of time. In the era of electronic medical records and constantly updated tests results, a face‐to‐face communication is less important. We used to spend 45 to 60 minutes on the handoffs, sometimes even longer due to people being late or not answering phone calls right away. It squeezed time out of patient encounters. The accepting day hospitalist needed to review electronic records (including dictated history and physical information if completed) during the course of the day regardless of the sign out from the night physician. Now, the information flow is smoother and it leaves more time for patient encounters. The day hospitalist keeps printed e‐mail with him or her so that information is readily accessible.
For the relatively smaller community hospitalist groups, it is difficult to ensure that all hospitalists will be available for the face‐to‐face handoffs. The hospitalist who is supposed to take sign‐outs could also be on call for the admissions or responsible for codes or rapid responses, which may interrupt or delay the sign‐out process. The Society of Hospital Medicine recommends both written and verbal sign‐outs.[2] This goal could be achieved more efficiently by the model followed by our group as discussed above. The verbal component could be over the phone rather than face‐to‐face meetings.
As a practicing hospitalist, I enjoyed the recently published research article by Schouten et al.[1] Their findings are not surprising to our hospitalist group. We evolved over the years from mandatory face‐to‐face or verbal handoffs to secured e‐mail communications. The night physician transfers care through a secured hospital‐provided email by 7 am. This information is supplemented by a phone call, originating from the day hospitalist on an as‐needed basis. This system works best for most community hospitalist programs, because it provides flexibility, improved communication, and saves a lot of time. In the era of electronic medical records and constantly updated tests results, a face‐to‐face communication is less important. We used to spend 45 to 60 minutes on the handoffs, sometimes even longer due to people being late or not answering phone calls right away. It squeezed time out of patient encounters. The accepting day hospitalist needed to review electronic records (including dictated history and physical information if completed) during the course of the day regardless of the sign out from the night physician. Now, the information flow is smoother and it leaves more time for patient encounters. The day hospitalist keeps printed e‐mail with him or her so that information is readily accessible.
For the relatively smaller community hospitalist groups, it is difficult to ensure that all hospitalists will be available for the face‐to‐face handoffs. The hospitalist who is supposed to take sign‐outs could also be on call for the admissions or responsible for codes or rapid responses, which may interrupt or delay the sign‐out process. The Society of Hospital Medicine recommends both written and verbal sign‐outs.[2] This goal could be achieved more efficiently by the model followed by our group as discussed above. The verbal component could be over the phone rather than face‐to‐face meetings.
- , , , , . Association of face‐to‐face handoffs and outcomes of hospitalized internal medicine patients. J Hosp Med. 2015;10(3):137–141.
- , , , , , . Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7):433–440.
- , , , , . Association of face‐to‐face handoffs and outcomes of hospitalized internal medicine patients. J Hosp Med. 2015;10(3):137–141.
- , , , , , . Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7):433–440.