User login
Psychiatry can help reduce prison violence
The news has been filled lately with stories of violence within correctional facilities, often involving prisoners or detainees who are alleged to have mental illness. The California prison system recently announced an initiative to reduce the use of force against mentally ill prisoners and to require correctional officers to consider an inmate’s mental health status prior to any use of force.
This is an excellent initiative, and close collaboration between security and mental health services is crucial for effective treatment of some mentally ill offenders.
However, this would be a good time to remember that not all seriously mentally ill prisoners are disruptive and that violence is a behavior rather than a diagnostic criterion. The nonsymptomatic causes of violence are important to consider as well: Is the inmate defending himself from attack by more aggressive peers? Is he taking a stand and making a display of force in order to make the point that he won’t be intimidated? Is he delirious from an unrecognized or treated medical condition? Is he having a seizure, suffering from withdrawal, or medically compromised in some other way? Or is the violence instrumental, a means to an end by a sociopathic inmate who needs to enforce his chain of command or protect his prison drug distribution channels? While for some, violence may be an outward sign of psychosis, for others it’s part of the cost of doing business.
In addition to looking at violence on an individual level, we also need to consider it from an institutional perspective. Violence may be a sign that there are serious problems not only on an individual level but possibly on an institutional one as well. Increased sensitivity to the mental status of the prisoner is only one piece of the puzzle.
Correctional officers are exposed to an environment unlike anything most civilians can imagine. They are exposed daily to threats, actual or implied assault, harassment, and sometimes even flying bodily fluids. When the prison budget doesn’t keep up with the daily institutional census, they may be required to work repeated overtime shifts or to work on tiers in which they are greatly outnumbered by the prisoners they are supposed to supervise and protect. Even when a correctional officer is not directly the subject of violence, the officer is required to respond to traumatic events like inmate-on-inmate assaults or completed suicides.
It’s not surprising, then, that many new officers leave the profession within the first 5 years, and that those who stay longer may be prone to stress-related absenteeism, substance abuse, and depression. Officers (or "guards" as the traditional media repeatedly misidentifies them) who show a change in personality or an unusually low tolerance for inmate misbehavior may be showing early signs of posttraumatic stress disorder or clinical depression. If this is being taken out on an inmate, it may also be a problem at home, leading to relationship problems or domestic violence. Officers who are cruel to a prisoner may not be particularly pleasant to civilian staff, either.
Changing a violent prison environment requires more than additional staff training and another redundant prison directive about the use of force. It requires change in a prison culture that values toughness and bravado. Access to mental health should be rapid and confidential, and not seen as an indication that an officer wants an "easy way out" through medical retirement. Security and psychiatry must work together for the care of the prisoner, but they also need to work on behalf of one another.
Dr. Hanson is a forensic psychiatrist and coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011). The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health & Mental Hygiene or the Maryland State Division of Correction.
The news has been filled lately with stories of violence within correctional facilities, often involving prisoners or detainees who are alleged to have mental illness. The California prison system recently announced an initiative to reduce the use of force against mentally ill prisoners and to require correctional officers to consider an inmate’s mental health status prior to any use of force.
This is an excellent initiative, and close collaboration between security and mental health services is crucial for effective treatment of some mentally ill offenders.
However, this would be a good time to remember that not all seriously mentally ill prisoners are disruptive and that violence is a behavior rather than a diagnostic criterion. The nonsymptomatic causes of violence are important to consider as well: Is the inmate defending himself from attack by more aggressive peers? Is he taking a stand and making a display of force in order to make the point that he won’t be intimidated? Is he delirious from an unrecognized or treated medical condition? Is he having a seizure, suffering from withdrawal, or medically compromised in some other way? Or is the violence instrumental, a means to an end by a sociopathic inmate who needs to enforce his chain of command or protect his prison drug distribution channels? While for some, violence may be an outward sign of psychosis, for others it’s part of the cost of doing business.
In addition to looking at violence on an individual level, we also need to consider it from an institutional perspective. Violence may be a sign that there are serious problems not only on an individual level but possibly on an institutional one as well. Increased sensitivity to the mental status of the prisoner is only one piece of the puzzle.
Correctional officers are exposed to an environment unlike anything most civilians can imagine. They are exposed daily to threats, actual or implied assault, harassment, and sometimes even flying bodily fluids. When the prison budget doesn’t keep up with the daily institutional census, they may be required to work repeated overtime shifts or to work on tiers in which they are greatly outnumbered by the prisoners they are supposed to supervise and protect. Even when a correctional officer is not directly the subject of violence, the officer is required to respond to traumatic events like inmate-on-inmate assaults or completed suicides.
It’s not surprising, then, that many new officers leave the profession within the first 5 years, and that those who stay longer may be prone to stress-related absenteeism, substance abuse, and depression. Officers (or "guards" as the traditional media repeatedly misidentifies them) who show a change in personality or an unusually low tolerance for inmate misbehavior may be showing early signs of posttraumatic stress disorder or clinical depression. If this is being taken out on an inmate, it may also be a problem at home, leading to relationship problems or domestic violence. Officers who are cruel to a prisoner may not be particularly pleasant to civilian staff, either.
Changing a violent prison environment requires more than additional staff training and another redundant prison directive about the use of force. It requires change in a prison culture that values toughness and bravado. Access to mental health should be rapid and confidential, and not seen as an indication that an officer wants an "easy way out" through medical retirement. Security and psychiatry must work together for the care of the prisoner, but they also need to work on behalf of one another.
Dr. Hanson is a forensic psychiatrist and coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011). The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health & Mental Hygiene or the Maryland State Division of Correction.
The news has been filled lately with stories of violence within correctional facilities, often involving prisoners or detainees who are alleged to have mental illness. The California prison system recently announced an initiative to reduce the use of force against mentally ill prisoners and to require correctional officers to consider an inmate’s mental health status prior to any use of force.
This is an excellent initiative, and close collaboration between security and mental health services is crucial for effective treatment of some mentally ill offenders.
However, this would be a good time to remember that not all seriously mentally ill prisoners are disruptive and that violence is a behavior rather than a diagnostic criterion. The nonsymptomatic causes of violence are important to consider as well: Is the inmate defending himself from attack by more aggressive peers? Is he taking a stand and making a display of force in order to make the point that he won’t be intimidated? Is he delirious from an unrecognized or treated medical condition? Is he having a seizure, suffering from withdrawal, or medically compromised in some other way? Or is the violence instrumental, a means to an end by a sociopathic inmate who needs to enforce his chain of command or protect his prison drug distribution channels? While for some, violence may be an outward sign of psychosis, for others it’s part of the cost of doing business.
In addition to looking at violence on an individual level, we also need to consider it from an institutional perspective. Violence may be a sign that there are serious problems not only on an individual level but possibly on an institutional one as well. Increased sensitivity to the mental status of the prisoner is only one piece of the puzzle.
Correctional officers are exposed to an environment unlike anything most civilians can imagine. They are exposed daily to threats, actual or implied assault, harassment, and sometimes even flying bodily fluids. When the prison budget doesn’t keep up with the daily institutional census, they may be required to work repeated overtime shifts or to work on tiers in which they are greatly outnumbered by the prisoners they are supposed to supervise and protect. Even when a correctional officer is not directly the subject of violence, the officer is required to respond to traumatic events like inmate-on-inmate assaults or completed suicides.
It’s not surprising, then, that many new officers leave the profession within the first 5 years, and that those who stay longer may be prone to stress-related absenteeism, substance abuse, and depression. Officers (or "guards" as the traditional media repeatedly misidentifies them) who show a change in personality or an unusually low tolerance for inmate misbehavior may be showing early signs of posttraumatic stress disorder or clinical depression. If this is being taken out on an inmate, it may also be a problem at home, leading to relationship problems or domestic violence. Officers who are cruel to a prisoner may not be particularly pleasant to civilian staff, either.
Changing a violent prison environment requires more than additional staff training and another redundant prison directive about the use of force. It requires change in a prison culture that values toughness and bravado. Access to mental health should be rapid and confidential, and not seen as an indication that an officer wants an "easy way out" through medical retirement. Security and psychiatry must work together for the care of the prisoner, but they also need to work on behalf of one another.
Dr. Hanson is a forensic psychiatrist and coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011). The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health & Mental Hygiene or the Maryland State Division of Correction.
Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with seizures
Definitions for the strength of evidence (Class I-III) and strength of recommendations (Level A-C) are provided at the end of the "Major Recommendations" field.
- In patients with a first generalized convulsive seizure who have returned to their baseline clinical status, should antiepileptic therapy be initiated in the emergency department (ED) to prevent additional seizures?
Patient Management Recommendations
Level A recommendations. None specified.
Level B recommendations. None specified.
Level C recommendations.
- Emergency physicians need not initiate antiepileptic medication* in the ED for patients who have had a first provoked seizure. Precipitating medical conditions should be identified and treated.
- Emergency physicians need not initiate antiepileptic medication* in the ED for patients who have had a first unprovoked seizure without evidence of brain disease or injury.
- Emergency physicians may initiate antiepileptic medication* in the ED, or defer in coordination with other providers, for patients who experienced a first unprovoked seizure with a remote history of brain disease or injury.
*Antiepileptic medication in this document refers to medications prescribed for seizure prevention.
- In patients with a first unprovoked seizure who have returned to their baseline clinical status in the ED, should the patient be admitted to the hospital to prevent adverse events?
Patient Management Recommendations
Level A recommendations. None specified.
Level B recommendations. None specified.
Level C recommendations. Emergency physicians need not admit patients with a first unprovoked seizure who have returned to their clinical baseline in the ED.
- In patients with a known seizure disorder in which resuming their antiepileptic medication in the ED is deemed appropriate, does the route of administration impact recurrence of seizures?
Patient Management Recommendations
Level A recommendations. None specified.
Level B recommendations. None specified.
Level C recommendations. When resuming antiepileptic medication in the ED is deemed appropriate, the emergency physician may administer intravenous (IV) or oral medication at their discretion.
- In ED patients with generalized convulsive status epilepticus who continue to have seizures despite receiving optimal dosing of a benzodiazepine, which agent or agents should be administered next to terminate seizures?
Patient Management Recommendations
Level A recommendations. Emergency physicians should administer an additional antiepileptic medication in ED patients with refractory status epilepticus who have failed treatment with benzodiazepines.
Level B recommendations. Emergency physicians may administer IV phenytoin, fosphenytoin, or valproate in ED patients with refractory status epilepticus who have failed treatment with benzodiazepines.
Level C recommendations. Emergency physicians may administer IV levetiracetam, propofol, or barbiturates in ED patients with refractory status epilepticus who have failed treatment with benzodiazepines.
Definitions:
Strength of Evidence
Literature Classification Schema*
Design/Class Therapy† Diagnosis‡ Prognosis§ 1 Randomized, controlled trial or meta-analysis of randomized trials Prospective cohort using a criterion standard or meta-analysis of prospective studies Population prospective cohort or meta-analysis of prospective studies 2 Nonrandomized trial Retrospective observational Retrospective cohort
Case control3 Case series
Case report
Other (e.g., consensus, review)Case series
Case report
Other (e.g., consensus, review)Case series
Case report
Other (e.g., consensus, review)*Some designs (e.g., surveys) will not fit this schema and should be assessed individually.
†Objective is to measure therapeutic efficacy comparing interventions.
‡Objective is to determine the sensitivity and specificity of diagnostic tests.
§Objective is to predict outcome including mortality and morbidity.
Approach to Downgrading Strength of Evidence*
Design/Class Downgrading 1 2 3 None I II III 1 level II III X 2 levels III X X Fatally flawed X X X *See the "Description of Methods Used to Analyze the Evidence" field for more information.
Strength of recommendations regarding each critical question were made by subcommittee members using results from strength of evidence grading, expert opinion, and consensus among subcommittee members according to the following guidelines:
Strength of Recommendations
Level A recommendations. Generally accepted principles for patient care that reflect a high degree of clinical certainty (i.e., based on evidence from 1 or more Class of Evidence I or multiple Class of Evidence II studies).
Level B recommendations. Recommendations for patient care that may identify a particular strategy or range of strategies that reflect moderate clinical certainty (i.e., based on evidence from 1 or more Class of Evidence II studies or strong consensus of Class of Evidence III studies).
Level C recommendations. Recommendations for patient care that are based on evidence from Class of Evidence III studies or, in the absence of any adequate published literature, based on expert consensus. In instances where consensus recommendations are made, "consensus" is placed in parentheses at the end of the recommendation.
There are certain circumstances in which the recommendations stemming from a body of evidence should not be rated as highly as the individual studies on which they are based. Factors such as heterogeneity of results, uncertainty about effect magnitude and consequences, and publication bias, among others, might lead to such a downgrading of recommendations.
Definitions for the strength of evidence (Class I-III) and strength of recommendations (Level A-C) are provided at the end of the "Major Recommendations" field.
- In patients with a first generalized convulsive seizure who have returned to their baseline clinical status, should antiepileptic therapy be initiated in the emergency department (ED) to prevent additional seizures?
Patient Management Recommendations
Level A recommendations. None specified.
Level B recommendations. None specified.
Level C recommendations.
- Emergency physicians need not initiate antiepileptic medication* in the ED for patients who have had a first provoked seizure. Precipitating medical conditions should be identified and treated.
- Emergency physicians need not initiate antiepileptic medication* in the ED for patients who have had a first unprovoked seizure without evidence of brain disease or injury.
- Emergency physicians may initiate antiepileptic medication* in the ED, or defer in coordination with other providers, for patients who experienced a first unprovoked seizure with a remote history of brain disease or injury.
*Antiepileptic medication in this document refers to medications prescribed for seizure prevention.
- In patients with a first unprovoked seizure who have returned to their baseline clinical status in the ED, should the patient be admitted to the hospital to prevent adverse events?
Patient Management Recommendations
Level A recommendations. None specified.
Level B recommendations. None specified.
Level C recommendations. Emergency physicians need not admit patients with a first unprovoked seizure who have returned to their clinical baseline in the ED.
- In patients with a known seizure disorder in which resuming their antiepileptic medication in the ED is deemed appropriate, does the route of administration impact recurrence of seizures?
Patient Management Recommendations
Level A recommendations. None specified.
Level B recommendations. None specified.
Level C recommendations. When resuming antiepileptic medication in the ED is deemed appropriate, the emergency physician may administer intravenous (IV) or oral medication at their discretion.
- In ED patients with generalized convulsive status epilepticus who continue to have seizures despite receiving optimal dosing of a benzodiazepine, which agent or agents should be administered next to terminate seizures?
Patient Management Recommendations
Level A recommendations. Emergency physicians should administer an additional antiepileptic medication in ED patients with refractory status epilepticus who have failed treatment with benzodiazepines.
Level B recommendations. Emergency physicians may administer IV phenytoin, fosphenytoin, or valproate in ED patients with refractory status epilepticus who have failed treatment with benzodiazepines.
Level C recommendations. Emergency physicians may administer IV levetiracetam, propofol, or barbiturates in ED patients with refractory status epilepticus who have failed treatment with benzodiazepines.
Definitions:
Strength of Evidence
Literature Classification Schema*
Design/Class Therapy† Diagnosis‡ Prognosis§ 1 Randomized, controlled trial or meta-analysis of randomized trials Prospective cohort using a criterion standard or meta-analysis of prospective studies Population prospective cohort or meta-analysis of prospective studies 2 Nonrandomized trial Retrospective observational Retrospective cohort
Case control3 Case series
Case report
Other (e.g., consensus, review)Case series
Case report
Other (e.g., consensus, review)Case series
Case report
Other (e.g., consensus, review)*Some designs (e.g., surveys) will not fit this schema and should be assessed individually.
†Objective is to measure therapeutic efficacy comparing interventions.
‡Objective is to determine the sensitivity and specificity of diagnostic tests.
§Objective is to predict outcome including mortality and morbidity.
Approach to Downgrading Strength of Evidence*
Design/Class Downgrading 1 2 3 None I II III 1 level II III X 2 levels III X X Fatally flawed X X X *See the "Description of Methods Used to Analyze the Evidence" field for more information.
Strength of recommendations regarding each critical question were made by subcommittee members using results from strength of evidence grading, expert opinion, and consensus among subcommittee members according to the following guidelines:
Strength of Recommendations
Level A recommendations. Generally accepted principles for patient care that reflect a high degree of clinical certainty (i.e., based on evidence from 1 or more Class of Evidence I or multiple Class of Evidence II studies).
Level B recommendations. Recommendations for patient care that may identify a particular strategy or range of strategies that reflect moderate clinical certainty (i.e., based on evidence from 1 or more Class of Evidence II studies or strong consensus of Class of Evidence III studies).
Level C recommendations. Recommendations for patient care that are based on evidence from Class of Evidence III studies or, in the absence of any adequate published literature, based on expert consensus. In instances where consensus recommendations are made, "consensus" is placed in parentheses at the end of the recommendation.
There are certain circumstances in which the recommendations stemming from a body of evidence should not be rated as highly as the individual studies on which they are based. Factors such as heterogeneity of results, uncertainty about effect magnitude and consequences, and publication bias, among others, might lead to such a downgrading of recommendations.
Definitions for the strength of evidence (Class I-III) and strength of recommendations (Level A-C) are provided at the end of the "Major Recommendations" field.
- In patients with a first generalized convulsive seizure who have returned to their baseline clinical status, should antiepileptic therapy be initiated in the emergency department (ED) to prevent additional seizures?
Patient Management Recommendations
Level A recommendations. None specified.
Level B recommendations. None specified.
Level C recommendations.
- Emergency physicians need not initiate antiepileptic medication* in the ED for patients who have had a first provoked seizure. Precipitating medical conditions should be identified and treated.
- Emergency physicians need not initiate antiepileptic medication* in the ED for patients who have had a first unprovoked seizure without evidence of brain disease or injury.
- Emergency physicians may initiate antiepileptic medication* in the ED, or defer in coordination with other providers, for patients who experienced a first unprovoked seizure with a remote history of brain disease or injury.
*Antiepileptic medication in this document refers to medications prescribed for seizure prevention.
- In patients with a first unprovoked seizure who have returned to their baseline clinical status in the ED, should the patient be admitted to the hospital to prevent adverse events?
Patient Management Recommendations
Level A recommendations. None specified.
Level B recommendations. None specified.
Level C recommendations. Emergency physicians need not admit patients with a first unprovoked seizure who have returned to their clinical baseline in the ED.
- In patients with a known seizure disorder in which resuming their antiepileptic medication in the ED is deemed appropriate, does the route of administration impact recurrence of seizures?
Patient Management Recommendations
Level A recommendations. None specified.
Level B recommendations. None specified.
Level C recommendations. When resuming antiepileptic medication in the ED is deemed appropriate, the emergency physician may administer intravenous (IV) or oral medication at their discretion.
- In ED patients with generalized convulsive status epilepticus who continue to have seizures despite receiving optimal dosing of a benzodiazepine, which agent or agents should be administered next to terminate seizures?
Patient Management Recommendations
Level A recommendations. Emergency physicians should administer an additional antiepileptic medication in ED patients with refractory status epilepticus who have failed treatment with benzodiazepines.
Level B recommendations. Emergency physicians may administer IV phenytoin, fosphenytoin, or valproate in ED patients with refractory status epilepticus who have failed treatment with benzodiazepines.
Level C recommendations. Emergency physicians may administer IV levetiracetam, propofol, or barbiturates in ED patients with refractory status epilepticus who have failed treatment with benzodiazepines.
Definitions:
Strength of Evidence
Literature Classification Schema*
Design/Class Therapy† Diagnosis‡ Prognosis§ 1 Randomized, controlled trial or meta-analysis of randomized trials Prospective cohort using a criterion standard or meta-analysis of prospective studies Population prospective cohort or meta-analysis of prospective studies 2 Nonrandomized trial Retrospective observational Retrospective cohort
Case control3 Case series
Case report
Other (e.g., consensus, review)Case series
Case report
Other (e.g., consensus, review)Case series
Case report
Other (e.g., consensus, review)*Some designs (e.g., surveys) will not fit this schema and should be assessed individually.
†Objective is to measure therapeutic efficacy comparing interventions.
‡Objective is to determine the sensitivity and specificity of diagnostic tests.
§Objective is to predict outcome including mortality and morbidity.
Approach to Downgrading Strength of Evidence*
Design/Class Downgrading 1 2 3 None I II III 1 level II III X 2 levels III X X Fatally flawed X X X *See the "Description of Methods Used to Analyze the Evidence" field for more information.
Strength of recommendations regarding each critical question were made by subcommittee members using results from strength of evidence grading, expert opinion, and consensus among subcommittee members according to the following guidelines:
Strength of Recommendations
Level A recommendations. Generally accepted principles for patient care that reflect a high degree of clinical certainty (i.e., based on evidence from 1 or more Class of Evidence I or multiple Class of Evidence II studies).
Level B recommendations. Recommendations for patient care that may identify a particular strategy or range of strategies that reflect moderate clinical certainty (i.e., based on evidence from 1 or more Class of Evidence II studies or strong consensus of Class of Evidence III studies).
Level C recommendations. Recommendations for patient care that are based on evidence from Class of Evidence III studies or, in the absence of any adequate published literature, based on expert consensus. In instances where consensus recommendations are made, "consensus" is placed in parentheses at the end of the recommendation.
There are certain circumstances in which the recommendations stemming from a body of evidence should not be rated as highly as the individual studies on which they are based. Factors such as heterogeneity of results, uncertainty about effect magnitude and consequences, and publication bias, among others, might lead to such a downgrading of recommendations.
This clinical policy from the American College of Emergency Physicians is the revision of a 2004 policy on critical issues in the evaluation and management of adult patients with seizures in the emergency department. A writing subcommittee reviewed the literature to derive evidence-based recommendations to help clinicians answer four critical questions. A literature search was performed, the evidence was graded, and recommendations were given based on the strength of the available data in the medical literature.
Guidelines are copyright © 2014 American College of Emergency Physicians. All rights reserved. The summary is provided by the Agency for Healthcare Research and Quality.
Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis
Note from the National Guideline Clearinghouse (NGC): This document is the first section in a series of four and covers methods for diagnosis and assessment of atopic dermatitis (AD). The second guideline in the series will address the management and treatment of AD with pharmacologic and nonpharmacologic topical modalities; the third section will cover phototherapy and systemic treatment options; and the fourth section will address the minimization of disease flares, educational interventions, and use of adjunctive approaches.
Features to Be Considered in the Diagnosis of Patients with AD
| Essential Features—Must be present:
*Patterns Include:
Important Features—Seen in most cases, adding support to the diagnosis:
Associated Features—These clinical associations help to suggest the diagnosis of AD but are too nonspecific to be used for defining or detecting AD for research and epidemiologic studies:
Exclusionary Conditions—It should be noted that a diagnosis of AD depends on excluding conditions, such as:
Adapted from Eichenfield LF, Hanifin JM, Luger TA, Stevens SR, Pride HB. Consensus conference on pediatric atopic dermatitis. J Am Acad Dermatol 2003;49:1088-95. Used with permission of the American Academy of Dermatology. |
Recommendation for the Diagnosis of AD
Patients with presumed AD should have their diagnosis based on the criteria summarized in the box above. On occasion, skin biopsy specimens or other tests (such as serum immunoglobulin E, potassium hydroxide preparation, patch testing, and/or genetic testing) may be helpful to rule out other or associated skin conditions.
Strength of Recommendations for the Diagnosis and Assessment of AD
| Recommendation | Strength of Recommendation | Level of Evidence | References |
|---|---|---|---|
| Diagnosis made using criteria in the box above | C | III | Mevorah et al., 1988; Gu et al., 2001; Lan et al., 2009; Diepgen, Sauerbrei, & Fartasch, 1996; De, Kanwar, & Handa, 2006; Loden, Andersson, & Lindberg, 1998; Samochocki & Dejewska, 2012; Samochocki, Paulochowska, & Zabielski, 2000; Chalmers et al., 2007; Firooz et al., 1999; Saeki et al., 2007; Firooz & Kashani, 2008; Hamada et al., 2005; Williams et al., 1994; Williams et al., 1996 |
| No specific biomarkers for diagnosis or severity assessment | B | II | Murat-Susic et al., 2006; Schulte-Herbruggen et al., 2007; Amon et al., 2000; Dhar et al., 2005; Gerdes, Kurrat, & Mrowietz, 2009; Aral et al, 2006; Di Lorenzo et al., 2003; El Mongy et al., 2008; Ezzat, Hasan, & Shaheen, 2011; Jahnz-Rozyk et al., 2005; Nakazato et al., 2008; Belloni Fortina et al., 2006; Gutgesell et al., 2002; Hirai et al., 1996; Hon et al., 2007; Horikawa et al., 2002; Kakinuma et al., 2003; La Grutta et al., 2005; Leung et al., 2003; Mostafa et al., 2008; Oflazoglu et al., "CD30 expression," 2008; Oflazoglu et al., "CD40 expression," 2008; Ott et al., 2010; Raap et al., 2006; Song et al., 2006; Wolkerstorfer et al., 1998 |
| Immunoglobulin E levels not routinely recommended | A | I | Schneider et al., 2013; Murat-Susic et al., 2006; Schulte-Herbruggen et al., 2007; Gerdes, Kurrat, & Mrowietz, 2009; Aral et al., 2006; Vakirlis et al., 2011; Wu et al., 2011 |
| Available disease severity scales not for routine clinical use | C | II | Schmitt, Langan, & Williams, 2007; Schram et al., 2012; Sprikkelman et al., 1997; Angelova-Fischer et al., 2005; Wolkerstorfer et al., 1999; Linnet & Jemec, 1999; Hon et al., 2006; Barbier et al., 2004; Charman, Venn, & Williams, 2002; Charman, Venn, & Williams, 2004; Charman et al., 1999; Cosickic et al., 2010; Emerson, Charman, & Williams, 2000; Hanifin et al., 2001; Holm et al., 2007; Oranje et al., 1997; Rullo et al., 2008 |
| Available quality of life severity scales not for routine clinical use | C | II | Chamlin et al., 2007; Augustin et al., 2004; Hon et al, 2006; Misery et al., 2007 |
| Should query itch, sleep, impact on daily activity, and disease persistence | C | III | Chamlin et al., 2005; Hon et al., 2008; Dawn et al., 2009; Lewis-Jones, 2006; Weisshaar et al., 2008; Ricci et al., 2007; Bender et al., 2008; Ben-Gashir, Seed, & Hay, 2002 |
| Awareness and discussion of common associations | C | I and II | Chamlin et al., 2005; Hon et al., 2008; Batlles-Garrido et al., 2010; Chawes et al., 2010; Sultesz et al., 2010; Kyllonen et al., 2006; Hwang et al., 2010; Hyvarinen et al., 2005; Eller et al., 2009; Horwitz, Hossain, & Yousef, 2009; Bashir, Dar, & Rao, 2010; Schmitt et al., "Psychiatric comorbidity," 2009; Schmitt et al., "Atopic eczema," 2009; Yaghmaie, Koudelka, & Simpson, 2013; Harding et al., 2008; Synnerstad et al., 2008; Vajdic et al., 2009; Kajbaf, Asar, & Alipoor, 2011; Vlaski et al., 2006 |
| Integrated, multidisciplinary approach to care | C | III | Boguniewicz et al., 2008; Ricci et al., 2009 |
Recommendations for the Use of Biomarkers in the Assessment of AD
- For patients with presumed AD, there are no specific biomarkers that can be recommended for diagnosis and/or assessment of disease severity.
- Monitoring of immunoglobulin E levels is not recommended for the routine assessment of disease severity.
Recommendations for Disease Severity and Clinical Outcomes Assessment
- For the general management of patients with AD, available disease severity measurement scales are not recommended for routine clinical practice, because they were not usually designed for this purpose.
- For the general management of patients with AD, available patient quality of life measurement scales are not recommended for routine clinical practice.
- It is recommended that clinicians ask general questions about itch, sleep, impact on daily activity, and persistence of disease, and currently available scales be used mainly when practical.
Recommendations for the Assessment of Clinical Associations of AD
- Physicians should be aware of and assess for conditions associated with AD, such as rhinitis/rhinoconjunctivitis, asthma, food allergy, sleep disturbance, depression, and other neuropsychiatric conditions, and it is recommended that physicians discuss them with the patient as part of the treatment/management plan, when appropriate.
- An integrated, multidisciplinary approach to care may be valuable and is suggested for AD patients who present with common associations.
Definitions:
Levels of Evidence
- Good-quality patient-oriented evidence (i.e., evidence measuring outcomes that matter to patients: morbidity, mortality, symptom improvement, cost reduction, and quality of life)
- Limited-quality patient-oriented evidence
- Other evidence including consensus guidelines, opinion, case studies, or disease-oriented evidence (i.e., evidence measuring intermediate, physiologic, or surrogate end points that may or may not reflect improvements in patient outcomes)
Grades of Recommendation
- Recommendation based on consistent and good quality patient-oriented evidence
- Recommendation based on inconsistent or limited quality patient-oriented evidence
- Recommendation based on consensus, opinion, case studies, or disease-oriented evidence
Note from the National Guideline Clearinghouse (NGC): This document is the first section in a series of four and covers methods for diagnosis and assessment of atopic dermatitis (AD). The second guideline in the series will address the management and treatment of AD with pharmacologic and nonpharmacologic topical modalities; the third section will cover phototherapy and systemic treatment options; and the fourth section will address the minimization of disease flares, educational interventions, and use of adjunctive approaches.
Features to Be Considered in the Diagnosis of Patients with AD
| Essential Features—Must be present:
*Patterns Include:
Important Features—Seen in most cases, adding support to the diagnosis:
Associated Features—These clinical associations help to suggest the diagnosis of AD but are too nonspecific to be used for defining or detecting AD for research and epidemiologic studies:
Exclusionary Conditions—It should be noted that a diagnosis of AD depends on excluding conditions, such as:
Adapted from Eichenfield LF, Hanifin JM, Luger TA, Stevens SR, Pride HB. Consensus conference on pediatric atopic dermatitis. J Am Acad Dermatol 2003;49:1088-95. Used with permission of the American Academy of Dermatology. |
Recommendation for the Diagnosis of AD
Patients with presumed AD should have their diagnosis based on the criteria summarized in the box above. On occasion, skin biopsy specimens or other tests (such as serum immunoglobulin E, potassium hydroxide preparation, patch testing, and/or genetic testing) may be helpful to rule out other or associated skin conditions.
Strength of Recommendations for the Diagnosis and Assessment of AD
| Recommendation | Strength of Recommendation | Level of Evidence | References |
|---|---|---|---|
| Diagnosis made using criteria in the box above | C | III | Mevorah et al., 1988; Gu et al., 2001; Lan et al., 2009; Diepgen, Sauerbrei, & Fartasch, 1996; De, Kanwar, & Handa, 2006; Loden, Andersson, & Lindberg, 1998; Samochocki & Dejewska, 2012; Samochocki, Paulochowska, & Zabielski, 2000; Chalmers et al., 2007; Firooz et al., 1999; Saeki et al., 2007; Firooz & Kashani, 2008; Hamada et al., 2005; Williams et al., 1994; Williams et al., 1996 |
| No specific biomarkers for diagnosis or severity assessment | B | II | Murat-Susic et al., 2006; Schulte-Herbruggen et al., 2007; Amon et al., 2000; Dhar et al., 2005; Gerdes, Kurrat, & Mrowietz, 2009; Aral et al, 2006; Di Lorenzo et al., 2003; El Mongy et al., 2008; Ezzat, Hasan, & Shaheen, 2011; Jahnz-Rozyk et al., 2005; Nakazato et al., 2008; Belloni Fortina et al., 2006; Gutgesell et al., 2002; Hirai et al., 1996; Hon et al., 2007; Horikawa et al., 2002; Kakinuma et al., 2003; La Grutta et al., 2005; Leung et al., 2003; Mostafa et al., 2008; Oflazoglu et al., "CD30 expression," 2008; Oflazoglu et al., "CD40 expression," 2008; Ott et al., 2010; Raap et al., 2006; Song et al., 2006; Wolkerstorfer et al., 1998 |
| Immunoglobulin E levels not routinely recommended | A | I | Schneider et al., 2013; Murat-Susic et al., 2006; Schulte-Herbruggen et al., 2007; Gerdes, Kurrat, & Mrowietz, 2009; Aral et al., 2006; Vakirlis et al., 2011; Wu et al., 2011 |
| Available disease severity scales not for routine clinical use | C | II | Schmitt, Langan, & Williams, 2007; Schram et al., 2012; Sprikkelman et al., 1997; Angelova-Fischer et al., 2005; Wolkerstorfer et al., 1999; Linnet & Jemec, 1999; Hon et al., 2006; Barbier et al., 2004; Charman, Venn, & Williams, 2002; Charman, Venn, & Williams, 2004; Charman et al., 1999; Cosickic et al., 2010; Emerson, Charman, & Williams, 2000; Hanifin et al., 2001; Holm et al., 2007; Oranje et al., 1997; Rullo et al., 2008 |
| Available quality of life severity scales not for routine clinical use | C | II | Chamlin et al., 2007; Augustin et al., 2004; Hon et al, 2006; Misery et al., 2007 |
| Should query itch, sleep, impact on daily activity, and disease persistence | C | III | Chamlin et al., 2005; Hon et al., 2008; Dawn et al., 2009; Lewis-Jones, 2006; Weisshaar et al., 2008; Ricci et al., 2007; Bender et al., 2008; Ben-Gashir, Seed, & Hay, 2002 |
| Awareness and discussion of common associations | C | I and II | Chamlin et al., 2005; Hon et al., 2008; Batlles-Garrido et al., 2010; Chawes et al., 2010; Sultesz et al., 2010; Kyllonen et al., 2006; Hwang et al., 2010; Hyvarinen et al., 2005; Eller et al., 2009; Horwitz, Hossain, & Yousef, 2009; Bashir, Dar, & Rao, 2010; Schmitt et al., "Psychiatric comorbidity," 2009; Schmitt et al., "Atopic eczema," 2009; Yaghmaie, Koudelka, & Simpson, 2013; Harding et al., 2008; Synnerstad et al., 2008; Vajdic et al., 2009; Kajbaf, Asar, & Alipoor, 2011; Vlaski et al., 2006 |
| Integrated, multidisciplinary approach to care | C | III | Boguniewicz et al., 2008; Ricci et al., 2009 |
Recommendations for the Use of Biomarkers in the Assessment of AD
- For patients with presumed AD, there are no specific biomarkers that can be recommended for diagnosis and/or assessment of disease severity.
- Monitoring of immunoglobulin E levels is not recommended for the routine assessment of disease severity.
Recommendations for Disease Severity and Clinical Outcomes Assessment
- For the general management of patients with AD, available disease severity measurement scales are not recommended for routine clinical practice, because they were not usually designed for this purpose.
- For the general management of patients with AD, available patient quality of life measurement scales are not recommended for routine clinical practice.
- It is recommended that clinicians ask general questions about itch, sleep, impact on daily activity, and persistence of disease, and currently available scales be used mainly when practical.
Recommendations for the Assessment of Clinical Associations of AD
- Physicians should be aware of and assess for conditions associated with AD, such as rhinitis/rhinoconjunctivitis, asthma, food allergy, sleep disturbance, depression, and other neuropsychiatric conditions, and it is recommended that physicians discuss them with the patient as part of the treatment/management plan, when appropriate.
- An integrated, multidisciplinary approach to care may be valuable and is suggested for AD patients who present with common associations.
Definitions:
Levels of Evidence
- Good-quality patient-oriented evidence (i.e., evidence measuring outcomes that matter to patients: morbidity, mortality, symptom improvement, cost reduction, and quality of life)
- Limited-quality patient-oriented evidence
- Other evidence including consensus guidelines, opinion, case studies, or disease-oriented evidence (i.e., evidence measuring intermediate, physiologic, or surrogate end points that may or may not reflect improvements in patient outcomes)
Grades of Recommendation
- Recommendation based on consistent and good quality patient-oriented evidence
- Recommendation based on inconsistent or limited quality patient-oriented evidence
- Recommendation based on consensus, opinion, case studies, or disease-oriented evidence
Note from the National Guideline Clearinghouse (NGC): This document is the first section in a series of four and covers methods for diagnosis and assessment of atopic dermatitis (AD). The second guideline in the series will address the management and treatment of AD with pharmacologic and nonpharmacologic topical modalities; the third section will cover phototherapy and systemic treatment options; and the fourth section will address the minimization of disease flares, educational interventions, and use of adjunctive approaches.
Features to Be Considered in the Diagnosis of Patients with AD
| Essential Features—Must be present:
*Patterns Include:
Important Features—Seen in most cases, adding support to the diagnosis:
Associated Features—These clinical associations help to suggest the diagnosis of AD but are too nonspecific to be used for defining or detecting AD for research and epidemiologic studies:
Exclusionary Conditions—It should be noted that a diagnosis of AD depends on excluding conditions, such as:
Adapted from Eichenfield LF, Hanifin JM, Luger TA, Stevens SR, Pride HB. Consensus conference on pediatric atopic dermatitis. J Am Acad Dermatol 2003;49:1088-95. Used with permission of the American Academy of Dermatology. |
Recommendation for the Diagnosis of AD
Patients with presumed AD should have their diagnosis based on the criteria summarized in the box above. On occasion, skin biopsy specimens or other tests (such as serum immunoglobulin E, potassium hydroxide preparation, patch testing, and/or genetic testing) may be helpful to rule out other or associated skin conditions.
Strength of Recommendations for the Diagnosis and Assessment of AD
| Recommendation | Strength of Recommendation | Level of Evidence | References |
|---|---|---|---|
| Diagnosis made using criteria in the box above | C | III | Mevorah et al., 1988; Gu et al., 2001; Lan et al., 2009; Diepgen, Sauerbrei, & Fartasch, 1996; De, Kanwar, & Handa, 2006; Loden, Andersson, & Lindberg, 1998; Samochocki & Dejewska, 2012; Samochocki, Paulochowska, & Zabielski, 2000; Chalmers et al., 2007; Firooz et al., 1999; Saeki et al., 2007; Firooz & Kashani, 2008; Hamada et al., 2005; Williams et al., 1994; Williams et al., 1996 |
| No specific biomarkers for diagnosis or severity assessment | B | II | Murat-Susic et al., 2006; Schulte-Herbruggen et al., 2007; Amon et al., 2000; Dhar et al., 2005; Gerdes, Kurrat, & Mrowietz, 2009; Aral et al, 2006; Di Lorenzo et al., 2003; El Mongy et al., 2008; Ezzat, Hasan, & Shaheen, 2011; Jahnz-Rozyk et al., 2005; Nakazato et al., 2008; Belloni Fortina et al., 2006; Gutgesell et al., 2002; Hirai et al., 1996; Hon et al., 2007; Horikawa et al., 2002; Kakinuma et al., 2003; La Grutta et al., 2005; Leung et al., 2003; Mostafa et al., 2008; Oflazoglu et al., "CD30 expression," 2008; Oflazoglu et al., "CD40 expression," 2008; Ott et al., 2010; Raap et al., 2006; Song et al., 2006; Wolkerstorfer et al., 1998 |
| Immunoglobulin E levels not routinely recommended | A | I | Schneider et al., 2013; Murat-Susic et al., 2006; Schulte-Herbruggen et al., 2007; Gerdes, Kurrat, & Mrowietz, 2009; Aral et al., 2006; Vakirlis et al., 2011; Wu et al., 2011 |
| Available disease severity scales not for routine clinical use | C | II | Schmitt, Langan, & Williams, 2007; Schram et al., 2012; Sprikkelman et al., 1997; Angelova-Fischer et al., 2005; Wolkerstorfer et al., 1999; Linnet & Jemec, 1999; Hon et al., 2006; Barbier et al., 2004; Charman, Venn, & Williams, 2002; Charman, Venn, & Williams, 2004; Charman et al., 1999; Cosickic et al., 2010; Emerson, Charman, & Williams, 2000; Hanifin et al., 2001; Holm et al., 2007; Oranje et al., 1997; Rullo et al., 2008 |
| Available quality of life severity scales not for routine clinical use | C | II | Chamlin et al., 2007; Augustin et al., 2004; Hon et al, 2006; Misery et al., 2007 |
| Should query itch, sleep, impact on daily activity, and disease persistence | C | III | Chamlin et al., 2005; Hon et al., 2008; Dawn et al., 2009; Lewis-Jones, 2006; Weisshaar et al., 2008; Ricci et al., 2007; Bender et al., 2008; Ben-Gashir, Seed, & Hay, 2002 |
| Awareness and discussion of common associations | C | I and II | Chamlin et al., 2005; Hon et al., 2008; Batlles-Garrido et al., 2010; Chawes et al., 2010; Sultesz et al., 2010; Kyllonen et al., 2006; Hwang et al., 2010; Hyvarinen et al., 2005; Eller et al., 2009; Horwitz, Hossain, & Yousef, 2009; Bashir, Dar, & Rao, 2010; Schmitt et al., "Psychiatric comorbidity," 2009; Schmitt et al., "Atopic eczema," 2009; Yaghmaie, Koudelka, & Simpson, 2013; Harding et al., 2008; Synnerstad et al., 2008; Vajdic et al., 2009; Kajbaf, Asar, & Alipoor, 2011; Vlaski et al., 2006 |
| Integrated, multidisciplinary approach to care | C | III | Boguniewicz et al., 2008; Ricci et al., 2009 |
Recommendations for the Use of Biomarkers in the Assessment of AD
- For patients with presumed AD, there are no specific biomarkers that can be recommended for diagnosis and/or assessment of disease severity.
- Monitoring of immunoglobulin E levels is not recommended for the routine assessment of disease severity.
Recommendations for Disease Severity and Clinical Outcomes Assessment
- For the general management of patients with AD, available disease severity measurement scales are not recommended for routine clinical practice, because they were not usually designed for this purpose.
- For the general management of patients with AD, available patient quality of life measurement scales are not recommended for routine clinical practice.
- It is recommended that clinicians ask general questions about itch, sleep, impact on daily activity, and persistence of disease, and currently available scales be used mainly when practical.
Recommendations for the Assessment of Clinical Associations of AD
- Physicians should be aware of and assess for conditions associated with AD, such as rhinitis/rhinoconjunctivitis, asthma, food allergy, sleep disturbance, depression, and other neuropsychiatric conditions, and it is recommended that physicians discuss them with the patient as part of the treatment/management plan, when appropriate.
- An integrated, multidisciplinary approach to care may be valuable and is suggested for AD patients who present with common associations.
Definitions:
Levels of Evidence
- Good-quality patient-oriented evidence (i.e., evidence measuring outcomes that matter to patients: morbidity, mortality, symptom improvement, cost reduction, and quality of life)
- Limited-quality patient-oriented evidence
- Other evidence including consensus guidelines, opinion, case studies, or disease-oriented evidence (i.e., evidence measuring intermediate, physiologic, or surrogate end points that may or may not reflect improvements in patient outcomes)
Grades of Recommendation
- Recommendation based on consistent and good quality patient-oriented evidence
- Recommendation based on inconsistent or limited quality patient-oriented evidence
- Recommendation based on consensus, opinion, case studies, or disease-oriented evidence
Atopic dermatitis affects up to 25% of children and 2% to 3% of adults. This guideline addresses methods for the diagnosis and monitoring of disease, outcomes measures for assessment, and common clinical associations that affect patients with AD are discussed.
Guidelines are copyright © 2013 American Academy of Dermatology, Inc. Published by Mosby, Inc. All rights reserved. The summary is provided by the Agency for Healthcare Research and Quality
Finding the Best Approach to Autoimmune Connective Tissue Disease Diagnosis
Jenny Cabas-Vargas, MD
Rheumatologist
Institute for Rheumatic and Autoimmune Diseases
Overlook Medical Center
Summit, New Jersey
Puja Chitkara, MD
Rheumatologist
Center for Arthritis and Rheumatologic Excellence (CARE)
San Diego, California
Stratos Christianakis, MD
Rheumatologist
Assistant Professor of Clinical Medicine
Keck School of Medicine of USC
Los Angeles, California
Chaim Putterman, MD
Professor of Medicine
(Rheumatology) and Microbiology & Immunology
Chief, Division of Rheumatology
Albert Einstein College of Medicine
Bronx, New York
Part 1
Part 2
Part 3
Part 4
Part 5
Part 6
Part 7
Part 8
Jenny Cabas-Vargas, MD
Rheumatologist
Institute for Rheumatic and Autoimmune Diseases
Overlook Medical Center
Summit, New Jersey
Puja Chitkara, MD
Rheumatologist
Center for Arthritis and Rheumatologic Excellence (CARE)
San Diego, California
Stratos Christianakis, MD
Rheumatologist
Assistant Professor of Clinical Medicine
Keck School of Medicine of USC
Los Angeles, California
Chaim Putterman, MD
Professor of Medicine
(Rheumatology) and Microbiology & Immunology
Chief, Division of Rheumatology
Albert Einstein College of Medicine
Bronx, New York
Part 1
Part 2
Part 3
Part 4
Part 5
Part 6
Part 7
Part 8
Jenny Cabas-Vargas, MD
Rheumatologist
Institute for Rheumatic and Autoimmune Diseases
Overlook Medical Center
Summit, New Jersey
Puja Chitkara, MD
Rheumatologist
Center for Arthritis and Rheumatologic Excellence (CARE)
San Diego, California
Stratos Christianakis, MD
Rheumatologist
Assistant Professor of Clinical Medicine
Keck School of Medicine of USC
Los Angeles, California
Chaim Putterman, MD
Professor of Medicine
(Rheumatology) and Microbiology & Immunology
Chief, Division of Rheumatology
Albert Einstein College of Medicine
Bronx, New York
Part 1
Part 2
Part 3
Part 4
Part 5
Part 6
Part 7
Part 8
Gene Expression Signatures in Breast Cancer: A Surgical Oncologist’s Perspective
The use of systemic chemotherapy and estrogen ablation (EA) for the treatment of breast cancer historically have been based on both the histologic prognostic parameters of the invasive breast cancer and on traditional estimates of recurrence risk. These estimates take into account the patient’s age, tumor size, grade, lymphovascular invasion, hormonal receptor status (estrogen receptor/progesterone receptor [ER/PR]), and human epidermal growth factor receptor 2 (HER2) overexpression.1
The recent description of 4 primary breast cancer subtypes on the basis of gene expression profiles has led to the identification of more specific gene prognostic signatures.2 These may serve to supplement, and possibly supersede, the assessment of recurrence risk currently employed as the basis for chemotherapy or EA recommendations for patients with breast cancer. As a result, many
patients who would have been treated with chemotherapy previously may now safely avoid it. The information provided by these prognostic signatures may also alter surgical decision making for many patients and, consequently, should be within the purview of dedicated cancer surgeons.
BREAST CANCER SUBTYPES
The 4 breast cancer subtypes are (1) the HER2 type, these can be ER/PR positive or negative; (2) basal-like tumors, typically ER, PR, and HER2 negative (ER-, PR-, and HER2-); and ER-positive (ER+) or luminal tumors, usually divided into (3) luminal A and (4) luminal B.2
HER2 Type
The advent of the first targeted breast cancer therapy, trastuzumab, and its immense salutary effect on survival of patients with previously poor prognoses has made the use of chemotherapy in combination with trastuzumab nearly mandatory in all HER2+ patients with breast cancer. Remarkably, the huge improvement in survival of these formerly doomed patients has led to the recommendation that trastuzumab-containing chemotherapy regimens should be used in the management of even subcentimeter, node-negative patients.3 This recommendation represents a clear change from the traditional recommendations for chemotherapy, which held that the benefits of systemic chemotherapy were more likely to be seen in patients with tumors in excess of 1 cm and/or who were node positive.
Basal-like Tumors
The discovery of trastuzumab made the basal-like tumor, which is usually ER-, PR-, and HER2- (triple negative), the subtype with the worst prognosis. Further, the natural course of this illness is markedly different from that of ER+/PR+ breast cancer. Nearly all basal-like or triple-negative patients with breast cancer who experience a recurrence do so within the first 5 years after diagnosis.4 In contrast, nearly 40% of ER+/PR+ HER2- breast cancer survivors experience their first recurrence beyond the 5-year milestone, with many even later in their course.5 Thus, the patient with triple-negative breast cancer is more likely to benefit from chemotherapy predominantly during the first 5 post-diagnosis years, as suggested by the Early Breast Cancer Trialists’ Collaborative Group meta-analyses.1
HER2+ and triple-negative breast cancers account for 20% and 15% of all breast cancers, respectively.6,7 In both subtypes, the benefit of chemotherapy is immense and chemotherapy will rarely be omitted from the treatment plan. Many of these patients are considered ideal candidates for preoperative chemotherapy (PCT), which results in increased rates of breast-conserving surgery (BCS), decreased positive margin rates at BCS, and decreased need for axillary node dissection. In the setting of PCT, a pathologic complete response (pCR) in the breast and axilla is increasingly recognized as a marker for improved disease-free survival (DFS) and overall survival (OS).8 For these reasons, preoperative consultation with medical oncologists is now even more important. Many of these patients will benefit from the use of PCT before any surgical treatment is undertaken.
Luminal Type (A and B)
The remaining two-thirds of all patients with breast cancer are ER+, primarily postmenopausal, and fall within the 2 remaining molecular subtypes: luminal A and luminal B. It is for these patients that the relative benefits of chemotherapy vs EA, or both, are currently being debated. For these patients the use of gene prognostic signatures, in concert with traditional histopathologic and clinical risk factors, may alter estimates of recurrence risk and the impact of chemotherapy on survival and recurrence estimates.
It is now evident that even the strongest predictors for breast cancer recurrence—histologic grade, patient age, and nodal status—are inconsistent predictors of the behavior of any individual tumor. While the use of chemotherapy can reduce the risk of metastases in these luminal-type patients with breast cancer, the majority of patients so stratified would survive without chemotherapy.9
GENE EXPRESSION SIGNATURE ASSAYS
One of the best demonstrations of the shortcomings of the standard risk predictors for ER+, HER2- breast cancers is provided by the Oncotype DX breast cancer assay’s recurrence score (RS) or gene expression signature (GES).10,11
Oncotype DX
The Oncotype DX assay is the first commercially available GES assay to illustrate the variability in survival of patients with node-negative, ER+ breast tumors. Sixteen selected cancer proliferative genes are paired with 5 control nonproliferative genes whose relative activity can be measured in paraffin-embedded breast cancer tissue. The ability to retrieve reliable ribonucleic acid (RNA) expression from cancer cells embedded in paraffin was a stroke of genius; it enabled the investigators to correlate the gene expression profile of patient subgroups treated decades earlier with their long-term clinical outcomes and survival.
The normalized summation of the proliferative activity of the 16 cancerproliferation genes in the Oncotype DX assay is expressed as the RS. The RS increases linearly and so does the average rate of distant recurrence in 10 years as a function of the RS. Three risk recurrence groups are defined by the RS: low risk (RS < 18); intermediate risk (RS > 18 to 30); and high risk (RS > 31).10,11
Clinical Trials
In the National Surgical Adjuvant Breast and Bowel Project (NSABP) clinical trial B-14, ER+ node-negative patients were randomized to observation or tamoxifen. In the untreated control patients, a low RS (< 18) was accompanied by a 6.8% risk of metastasis at 10 years, and a high RS (> 31) was accompanied by a 30.5% rate of distant recurrence.11 In another study, the low RS tamoxifen-treated arm showed a 2.8% risk of breast cancer death at 10 years vs a 15.5% risk in the high RS cohort.12
The remarkable significance of the RS is demonstrated when the RS is plotted against patient age, grade, or tumor size.10 This illustrates the huge variability in these traditional histopathologic and clinical features within a given RS group. For any patient with a low RS, there is marked variability in patient age, tumor grade, or tumor size. A very small or low-grade tumor can have a very high 10-year recurrence rate, as measured by the gene prognostic signature or RS. Similarly, a very large tumor in a young patient can have a very low 10-year recurrence rate or RS. This is due to the heterogeneity of the biology of these cancers, regardless of their favorable or unfavorable histologic features.
In most cases, decisions about chemotherapy in patient who are postmenopausal, node-negative, and ER+ are made by risk estimates based on patient age, tumor grade, and tumor size, without knowledge of their RS. However, the large variability in 10-year rates of metastases and death among patients clearly demonstrates that, for some, chemotherapy affords no benefit. Their RS suggest that their risk of metastases at 10 years is only 2.8% when treated with EA (ie, tamoxifen) and no chemotherapy. In fact, 51% of the patients who are postmenopausal, node-negative, and ER+ in NSABP B-14 fell within the low risk RS category for 10-year distant recurrence, whereas about 27% fell within the high risk (RS > 31) category.13
Confidence in the Oncotype DX assay RS stems from the ability of investigators to plot the recurrence rates of distant metastases in patientstreated with tamoxifen vs placebo in the NSABP B-14 trial. Their clinicaloutcomes could be correlated with their GES samples retrieved from paraffin-embedded archival tissue many years after treatment. Corresponding plotting was done for similar patient cohorts treated with chemotherapy with or without tamoxifen in NSABP Trial B-20.
Among patients with low RS, the distant recurrence rate at 10 years was 2.2%, whether treated with systemic chemotherapy plus tamoxifenor with tamoxifen alone. Thus, in study participants with low RS, regardless of tumor size, grade, or patient age, 10-year recurrence rates were not affected by the addition of chemotherapy.13
Note that, in the absence of the new information provided by the Oncotype gene prognostic signature, nearly all these patients would be treated with systemic chemotherapy. Studies have shown that the additional risk assessment estimate provided by the Oncotype assay causes a change in systemic therapy recommendations from chemotherapy to no chemotherapy in 30% of patients.14,15 Among patients with high RS, 10-year distant recurrence rates decreased by an absolute 27% with the addition of chemotherapy to tamoxifen. These patients clearly benefited from chemotherapy.13
The relative benefits of chemotherapy vs tamoxifen in a third RS group with an intermediate RS of 18-21 awaits publication of the now-closed Trial Assigning Individualized Options for Treatment (TAILORx) trial. This group accounts for 22% of patients who are postmenopausal, node-negative, and ER+ identified by the Oncotype DX assay. Initial reports show no significant benefit from the addition of chemotherapy to tamoxifen in this group.10
MammaPrint
Other gene prognostic signatures have recently been validated. Of these, the MammaPrint assay is the best established and validated.16 The MammaPrint uses a panel of 70 proliferation genes that were selected without bias by scanning the entire human genome. Unlike the Oncotype DX, the MammaPrint panel was randomly selected without any prior knowledge of the role of the proliferation genes in breast carcinogenesis. Furthermore, the reliability of the MammaPrint gene signature is independent of nodal status.17 This suggests that the intrinsic genetic makeup of the cancer establishes its biologic behavior and supersedes the impact of the traditional assessment of nodal involvement as a significant risk factor for distant metastases.
The MammaPrint GES was developed to identify patients at high risk of recurrence within 5 years of diagnosis; those for whom, as noted earlier, the salutary effect of chemotherapy is most evident.18 The assay is reliable for both pre- and postmenopausal women and stratifies patients into 2 risk groups only: high vs low.19-21 The probability of remaining free of recurrent disease at 10 years is 85% in the low risk GES patients vs 50.6% in those with high risk MammaPrint prognosis signatures.17
Subsequent validation trials examined the accuracy of the MammaPrint as a prognostic indicator as well as a predictor of response to chemotherapy. These studies included node-negative, node-positive, pre- and postmenopausal women.18-23 The risk of metastatic disease within the first 5 years after diagnosis was more significant in the high-risk than in the low-risk group. However, because the MammaPrint signature is independent of ER status, not all MammaPrint low-risk signatures are ER+. This reflects the contribution of unselected proliferation genes to the MammaPrint signature that results in the luminal A and luminal B breast cancer subtypes. In postmenopausal, node-negative patients, 61% may have good prognosis signatures, regardless of ER status.18,22
A poor prognosis signature, then, would suggest the use of chemotherapy to prevent early (< 5 years from diagnosis) breast cancer deaths, but would still allow for EA to prevent late (> 5 years after diagnosis) recurrence for patients whose tumors were ER+. It should be noted that these findings also apply to patients treated with contemporary anthracycline chemotherapy regimens.22 The MammaPrint poor prognostic signature identifies patients at risk for early recurrence who may therefore benefit from chemotherapy, whereas the good prognostic signature identifies patients with a very low risk of distant metastases < 5 years.22 In the latter group, this low risk may not warrant use of systemic chemotherapy, but treatment with EA would confer a decrease in systemic metastases.
THE SURGEON’S PERSPECTIVE
To the surgeon, as suggested earlier, perhaps more pertinent is the available information on the use of chemotherapy before planned surgery for basal-type triple negative and HER-2+ breast cancers in the setting of luminal ER+ tumors. Mounting evidence suggests that the GES, such as those determined via the Oncotype and MammaPrint assays, can provide a very reliable indication of an individual patient’s response to PCT or chemotherapy in the neoadjuvant setting.24,25 These clinical responses are easily quantitated on physical examination or by imaging in the few months during which a patient can receive PCT.
Furthermore, the absence of residual microscopic tumor in the breast and axilla (ie, pCR) after PCT can be predicted by the Oncotype DX RS and the MammaPrint GES. More than 11 reports (5,210 patients) have demonstrated a higher DFS and OS in patients who achieve a pCR after PCT.8 A pCR in a locally advanced patient with breast cancer can provide the surgeon with a margin-negative surgical procedure (BCS or mastectomy) and inform the patient of the potential for a much better DFS or OS than anticipated from the stage of breast cancer at presentation.
In some patients amenable to BCS at presentation but whose tumor is too close to the chest wall or is proximate to a silicone augmentation prosthesis, the predicted response to systemic chemotherapy or hormonal ablation provided by GES can lead to a decrease in margin-positive rates and salvage of the previous cosmetic augmentation.
In patients at risk for carrying a BRCA mutation, the interval of PCT can be used for appropriate genetic testing and counseling and plastic surgery and gynecologic oncology consultations. Identified BRCA gene carriers may benefit from risk reduction surgery because of their increased breast and ovarian cancerrisk. Non-BRCA patients can consider BCS as an option, with decreased margin-positive rates and improved cosmesis. Information provided by GES can be essential to a good surgical outcome and underlines the need for preoperative consultation with medical oncology.26
CONCLUSION
Gene expression signatures provide information about the biologic behavior of each individual patient’s breast cancer. As new GES are introduced into clinical practice, surgeons must become fully informed about these advances in order to provide truly personalized cancer care plans to our patients.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect an endorsement by or opinion of Federal Practitioner, Frontline Medical Communications, the U.S. Air Force, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drug combinations–including indications, contraindications, warnings, and adverse effects–before administering pharmacologic therapy to patients.
1. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687-1717.
2. Sørlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinoma distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98(19):10869-10874.
3. Goldhirsch A, Winer EP, Coates AS, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013;24(9):2206-2223.
4. Pagoda K, Niwinska A, Murawska M, Pienkowski T. Analysis of pattern, time, and risk factors influencing recurrence in triple-negative breast cancer patients. Med Oncol. 2013;30(1):388.
5. Brewster AM, Hortobagyi GN, Broglio KR. Residual risk of breast cancer recurrence 5 years after adjuvant therapy. J Natl Cancer Inst. 2008;100(16):1179-1183.
6. Reynolds S. Triple-negative breast cancer disproportionately affects african american and Hispanic women. NCI Cancer Bulletin. 2007;4(22). www.cancer.gov/ncicancerbulletin/archive/2007/072407/page7. Accessed July 17, 2014.
7. Phillips C. Treatment Options for HER2-positive breast cancer expand and evolve. NCI Cancer Bulletin. 2012;9(20). www.cancer.gov/ncicancerbulletin/101612/page2. Accessed July 17, 2014.
8. Kaufmann M, von Minckwitz G, Mamounas EP, et al. Recommendations from an international conference on the current status and future of neoadjuvant systemic therapy in primary breast cancer. Ann Surg Oncol. 2012;19(5):1508-1516.
9. Coates AS, Colleoni M, Goldhirsch A. Is adjuvant chemotherapy useful for women with luminal A breast cancer? J Clin Oncol. 2012;30(12):1260-1263.
10. Paik S, Tang G, Kim C, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24(23):3726-3734.
11. Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351(27):2817-2826.
12. Habel LA, Shak S, Jacobs MK, et al. A population-based study of tumor gene expression and risk of breast cancer death among lymph node-negative patients. Breast Cancer Res. 2006;8(3):1-15.
13. Sparano JA, Paik S. Development of the 21-gene assay and its application in clinical practice and clinical trials. J Clin Oncol. 2008;26(5):721-728.
14. Lo SS, Mumby PB, Norton J, et al. Prospective multicenter study of the impact of the 21-gene recurrence score assay on medical oncologists and patient adjuvant breast cancer treatment selection. J Clin Oncol. 2010;28(10):1671-1676.
15. Hassett MJ, Silver SM, Hughes ME, et al. Adoption of gene expression profile testing and association with the use of chemotherapy among women with breast cancer. J Clin Oncol. 2012;30(18):2218-2226.
16. van’t Veer LJ, Dai H, van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415(6871):530-536.
17. van de Vijver MJ, He YD, van’t Veer LJ, et al. A gene expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002;347(25):1999-2009.
18. Mook S, Schmidt MK, Weigelt B, et al. The 70-gene prognostic signature predicts early metastasis in breast cancer patients between 55 and 70 years of age. Ann Oncol. 2010;21(4):717-722.
19. Drukker CA, Bueno-de-Mesquita JM, Retél VP, et al. A prospective evaluation of a breast cancer prognostic signature in the observational RASTER study. Intl J Cancer. 2013;133(4):929-936.
20. Buyse M, Loi S, van’t Veer L, et al. Validation and clinical utility of a 70-gene prognostic signature for women with node-negative breast cancer. J Natl Cancer Inst. 2006;98(17): 1183-1192.
21. Bueno-de-Mesquita JM, Linn SC, Keijzer R, et al. Validation of 70-gene prognostic signature in node-negative breast cancer. Breast Cancer Res Treat. 2009;117(3):483-495.
22. Knauer M, Mook S, Rutgers EJ, et al. The predictive value of the 70-gene signature for adjuvant chemotherapy in early breast cancer. Breast Cancer Res Treat. 2010;120(3):655-661.
23. Mook S, Schmidt MK, Viale G, et al; TRANSBIG Consortium. The 70-gene prognosis-signature predicts disease outcome in breast cancer patients with 1-3 positive lymph nodes in an independent validation study. Breast Cancer Res Treat. 2009;116(2):295-302.
24. Gianni L, Zambetti M, Clark K, et al. Gene expression profiles in paraffin-embedded core biopsy tissue predicts response to chemotherapy in women with locally advanced breast cancer. J Clin Oncol. 2005;23(29):7265-7277.
25. Straver ME, Glas AM, Hannemann J, et al. The 70-gene signature as a response predictor for neoadjuvant chemotherapy in breast cancer. Breast Cancer Res Treat. 2010;119(3):551-558.
26. Silva E. Targeted tailored management of the breast cancer patient at risk for harboring a germline mutation: current trends affecting the selection of patients considering surgical prophylaxis. Breast J. 2009;15(suppl 1):S76-S80.
The use of systemic chemotherapy and estrogen ablation (EA) for the treatment of breast cancer historically have been based on both the histologic prognostic parameters of the invasive breast cancer and on traditional estimates of recurrence risk. These estimates take into account the patient’s age, tumor size, grade, lymphovascular invasion, hormonal receptor status (estrogen receptor/progesterone receptor [ER/PR]), and human epidermal growth factor receptor 2 (HER2) overexpression.1
The recent description of 4 primary breast cancer subtypes on the basis of gene expression profiles has led to the identification of more specific gene prognostic signatures.2 These may serve to supplement, and possibly supersede, the assessment of recurrence risk currently employed as the basis for chemotherapy or EA recommendations for patients with breast cancer. As a result, many
patients who would have been treated with chemotherapy previously may now safely avoid it. The information provided by these prognostic signatures may also alter surgical decision making for many patients and, consequently, should be within the purview of dedicated cancer surgeons.
BREAST CANCER SUBTYPES
The 4 breast cancer subtypes are (1) the HER2 type, these can be ER/PR positive or negative; (2) basal-like tumors, typically ER, PR, and HER2 negative (ER-, PR-, and HER2-); and ER-positive (ER+) or luminal tumors, usually divided into (3) luminal A and (4) luminal B.2
HER2 Type
The advent of the first targeted breast cancer therapy, trastuzumab, and its immense salutary effect on survival of patients with previously poor prognoses has made the use of chemotherapy in combination with trastuzumab nearly mandatory in all HER2+ patients with breast cancer. Remarkably, the huge improvement in survival of these formerly doomed patients has led to the recommendation that trastuzumab-containing chemotherapy regimens should be used in the management of even subcentimeter, node-negative patients.3 This recommendation represents a clear change from the traditional recommendations for chemotherapy, which held that the benefits of systemic chemotherapy were more likely to be seen in patients with tumors in excess of 1 cm and/or who were node positive.
Basal-like Tumors
The discovery of trastuzumab made the basal-like tumor, which is usually ER-, PR-, and HER2- (triple negative), the subtype with the worst prognosis. Further, the natural course of this illness is markedly different from that of ER+/PR+ breast cancer. Nearly all basal-like or triple-negative patients with breast cancer who experience a recurrence do so within the first 5 years after diagnosis.4 In contrast, nearly 40% of ER+/PR+ HER2- breast cancer survivors experience their first recurrence beyond the 5-year milestone, with many even later in their course.5 Thus, the patient with triple-negative breast cancer is more likely to benefit from chemotherapy predominantly during the first 5 post-diagnosis years, as suggested by the Early Breast Cancer Trialists’ Collaborative Group meta-analyses.1
HER2+ and triple-negative breast cancers account for 20% and 15% of all breast cancers, respectively.6,7 In both subtypes, the benefit of chemotherapy is immense and chemotherapy will rarely be omitted from the treatment plan. Many of these patients are considered ideal candidates for preoperative chemotherapy (PCT), which results in increased rates of breast-conserving surgery (BCS), decreased positive margin rates at BCS, and decreased need for axillary node dissection. In the setting of PCT, a pathologic complete response (pCR) in the breast and axilla is increasingly recognized as a marker for improved disease-free survival (DFS) and overall survival (OS).8 For these reasons, preoperative consultation with medical oncologists is now even more important. Many of these patients will benefit from the use of PCT before any surgical treatment is undertaken.
Luminal Type (A and B)
The remaining two-thirds of all patients with breast cancer are ER+, primarily postmenopausal, and fall within the 2 remaining molecular subtypes: luminal A and luminal B. It is for these patients that the relative benefits of chemotherapy vs EA, or both, are currently being debated. For these patients the use of gene prognostic signatures, in concert with traditional histopathologic and clinical risk factors, may alter estimates of recurrence risk and the impact of chemotherapy on survival and recurrence estimates.
It is now evident that even the strongest predictors for breast cancer recurrence—histologic grade, patient age, and nodal status—are inconsistent predictors of the behavior of any individual tumor. While the use of chemotherapy can reduce the risk of metastases in these luminal-type patients with breast cancer, the majority of patients so stratified would survive without chemotherapy.9
GENE EXPRESSION SIGNATURE ASSAYS
One of the best demonstrations of the shortcomings of the standard risk predictors for ER+, HER2- breast cancers is provided by the Oncotype DX breast cancer assay’s recurrence score (RS) or gene expression signature (GES).10,11
Oncotype DX
The Oncotype DX assay is the first commercially available GES assay to illustrate the variability in survival of patients with node-negative, ER+ breast tumors. Sixteen selected cancer proliferative genes are paired with 5 control nonproliferative genes whose relative activity can be measured in paraffin-embedded breast cancer tissue. The ability to retrieve reliable ribonucleic acid (RNA) expression from cancer cells embedded in paraffin was a stroke of genius; it enabled the investigators to correlate the gene expression profile of patient subgroups treated decades earlier with their long-term clinical outcomes and survival.
The normalized summation of the proliferative activity of the 16 cancerproliferation genes in the Oncotype DX assay is expressed as the RS. The RS increases linearly and so does the average rate of distant recurrence in 10 years as a function of the RS. Three risk recurrence groups are defined by the RS: low risk (RS < 18); intermediate risk (RS > 18 to 30); and high risk (RS > 31).10,11
Clinical Trials
In the National Surgical Adjuvant Breast and Bowel Project (NSABP) clinical trial B-14, ER+ node-negative patients were randomized to observation or tamoxifen. In the untreated control patients, a low RS (< 18) was accompanied by a 6.8% risk of metastasis at 10 years, and a high RS (> 31) was accompanied by a 30.5% rate of distant recurrence.11 In another study, the low RS tamoxifen-treated arm showed a 2.8% risk of breast cancer death at 10 years vs a 15.5% risk in the high RS cohort.12
The remarkable significance of the RS is demonstrated when the RS is plotted against patient age, grade, or tumor size.10 This illustrates the huge variability in these traditional histopathologic and clinical features within a given RS group. For any patient with a low RS, there is marked variability in patient age, tumor grade, or tumor size. A very small or low-grade tumor can have a very high 10-year recurrence rate, as measured by the gene prognostic signature or RS. Similarly, a very large tumor in a young patient can have a very low 10-year recurrence rate or RS. This is due to the heterogeneity of the biology of these cancers, regardless of their favorable or unfavorable histologic features.
In most cases, decisions about chemotherapy in patient who are postmenopausal, node-negative, and ER+ are made by risk estimates based on patient age, tumor grade, and tumor size, without knowledge of their RS. However, the large variability in 10-year rates of metastases and death among patients clearly demonstrates that, for some, chemotherapy affords no benefit. Their RS suggest that their risk of metastases at 10 years is only 2.8% when treated with EA (ie, tamoxifen) and no chemotherapy. In fact, 51% of the patients who are postmenopausal, node-negative, and ER+ in NSABP B-14 fell within the low risk RS category for 10-year distant recurrence, whereas about 27% fell within the high risk (RS > 31) category.13
Confidence in the Oncotype DX assay RS stems from the ability of investigators to plot the recurrence rates of distant metastases in patientstreated with tamoxifen vs placebo in the NSABP B-14 trial. Their clinicaloutcomes could be correlated with their GES samples retrieved from paraffin-embedded archival tissue many years after treatment. Corresponding plotting was done for similar patient cohorts treated with chemotherapy with or without tamoxifen in NSABP Trial B-20.
Among patients with low RS, the distant recurrence rate at 10 years was 2.2%, whether treated with systemic chemotherapy plus tamoxifenor with tamoxifen alone. Thus, in study participants with low RS, regardless of tumor size, grade, or patient age, 10-year recurrence rates were not affected by the addition of chemotherapy.13
Note that, in the absence of the new information provided by the Oncotype gene prognostic signature, nearly all these patients would be treated with systemic chemotherapy. Studies have shown that the additional risk assessment estimate provided by the Oncotype assay causes a change in systemic therapy recommendations from chemotherapy to no chemotherapy in 30% of patients.14,15 Among patients with high RS, 10-year distant recurrence rates decreased by an absolute 27% with the addition of chemotherapy to tamoxifen. These patients clearly benefited from chemotherapy.13
The relative benefits of chemotherapy vs tamoxifen in a third RS group with an intermediate RS of 18-21 awaits publication of the now-closed Trial Assigning Individualized Options for Treatment (TAILORx) trial. This group accounts for 22% of patients who are postmenopausal, node-negative, and ER+ identified by the Oncotype DX assay. Initial reports show no significant benefit from the addition of chemotherapy to tamoxifen in this group.10
MammaPrint
Other gene prognostic signatures have recently been validated. Of these, the MammaPrint assay is the best established and validated.16 The MammaPrint uses a panel of 70 proliferation genes that were selected without bias by scanning the entire human genome. Unlike the Oncotype DX, the MammaPrint panel was randomly selected without any prior knowledge of the role of the proliferation genes in breast carcinogenesis. Furthermore, the reliability of the MammaPrint gene signature is independent of nodal status.17 This suggests that the intrinsic genetic makeup of the cancer establishes its biologic behavior and supersedes the impact of the traditional assessment of nodal involvement as a significant risk factor for distant metastases.
The MammaPrint GES was developed to identify patients at high risk of recurrence within 5 years of diagnosis; those for whom, as noted earlier, the salutary effect of chemotherapy is most evident.18 The assay is reliable for both pre- and postmenopausal women and stratifies patients into 2 risk groups only: high vs low.19-21 The probability of remaining free of recurrent disease at 10 years is 85% in the low risk GES patients vs 50.6% in those with high risk MammaPrint prognosis signatures.17
Subsequent validation trials examined the accuracy of the MammaPrint as a prognostic indicator as well as a predictor of response to chemotherapy. These studies included node-negative, node-positive, pre- and postmenopausal women.18-23 The risk of metastatic disease within the first 5 years after diagnosis was more significant in the high-risk than in the low-risk group. However, because the MammaPrint signature is independent of ER status, not all MammaPrint low-risk signatures are ER+. This reflects the contribution of unselected proliferation genes to the MammaPrint signature that results in the luminal A and luminal B breast cancer subtypes. In postmenopausal, node-negative patients, 61% may have good prognosis signatures, regardless of ER status.18,22
A poor prognosis signature, then, would suggest the use of chemotherapy to prevent early (< 5 years from diagnosis) breast cancer deaths, but would still allow for EA to prevent late (> 5 years after diagnosis) recurrence for patients whose tumors were ER+. It should be noted that these findings also apply to patients treated with contemporary anthracycline chemotherapy regimens.22 The MammaPrint poor prognostic signature identifies patients at risk for early recurrence who may therefore benefit from chemotherapy, whereas the good prognostic signature identifies patients with a very low risk of distant metastases < 5 years.22 In the latter group, this low risk may not warrant use of systemic chemotherapy, but treatment with EA would confer a decrease in systemic metastases.
THE SURGEON’S PERSPECTIVE
To the surgeon, as suggested earlier, perhaps more pertinent is the available information on the use of chemotherapy before planned surgery for basal-type triple negative and HER-2+ breast cancers in the setting of luminal ER+ tumors. Mounting evidence suggests that the GES, such as those determined via the Oncotype and MammaPrint assays, can provide a very reliable indication of an individual patient’s response to PCT or chemotherapy in the neoadjuvant setting.24,25 These clinical responses are easily quantitated on physical examination or by imaging in the few months during which a patient can receive PCT.
Furthermore, the absence of residual microscopic tumor in the breast and axilla (ie, pCR) after PCT can be predicted by the Oncotype DX RS and the MammaPrint GES. More than 11 reports (5,210 patients) have demonstrated a higher DFS and OS in patients who achieve a pCR after PCT.8 A pCR in a locally advanced patient with breast cancer can provide the surgeon with a margin-negative surgical procedure (BCS or mastectomy) and inform the patient of the potential for a much better DFS or OS than anticipated from the stage of breast cancer at presentation.
In some patients amenable to BCS at presentation but whose tumor is too close to the chest wall or is proximate to a silicone augmentation prosthesis, the predicted response to systemic chemotherapy or hormonal ablation provided by GES can lead to a decrease in margin-positive rates and salvage of the previous cosmetic augmentation.
In patients at risk for carrying a BRCA mutation, the interval of PCT can be used for appropriate genetic testing and counseling and plastic surgery and gynecologic oncology consultations. Identified BRCA gene carriers may benefit from risk reduction surgery because of their increased breast and ovarian cancerrisk. Non-BRCA patients can consider BCS as an option, with decreased margin-positive rates and improved cosmesis. Information provided by GES can be essential to a good surgical outcome and underlines the need for preoperative consultation with medical oncology.26
CONCLUSION
Gene expression signatures provide information about the biologic behavior of each individual patient’s breast cancer. As new GES are introduced into clinical practice, surgeons must become fully informed about these advances in order to provide truly personalized cancer care plans to our patients.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect an endorsement by or opinion of Federal Practitioner, Frontline Medical Communications, the U.S. Air Force, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drug combinations–including indications, contraindications, warnings, and adverse effects–before administering pharmacologic therapy to patients.
The use of systemic chemotherapy and estrogen ablation (EA) for the treatment of breast cancer historically have been based on both the histologic prognostic parameters of the invasive breast cancer and on traditional estimates of recurrence risk. These estimates take into account the patient’s age, tumor size, grade, lymphovascular invasion, hormonal receptor status (estrogen receptor/progesterone receptor [ER/PR]), and human epidermal growth factor receptor 2 (HER2) overexpression.1
The recent description of 4 primary breast cancer subtypes on the basis of gene expression profiles has led to the identification of more specific gene prognostic signatures.2 These may serve to supplement, and possibly supersede, the assessment of recurrence risk currently employed as the basis for chemotherapy or EA recommendations for patients with breast cancer. As a result, many
patients who would have been treated with chemotherapy previously may now safely avoid it. The information provided by these prognostic signatures may also alter surgical decision making for many patients and, consequently, should be within the purview of dedicated cancer surgeons.
BREAST CANCER SUBTYPES
The 4 breast cancer subtypes are (1) the HER2 type, these can be ER/PR positive or negative; (2) basal-like tumors, typically ER, PR, and HER2 negative (ER-, PR-, and HER2-); and ER-positive (ER+) or luminal tumors, usually divided into (3) luminal A and (4) luminal B.2
HER2 Type
The advent of the first targeted breast cancer therapy, trastuzumab, and its immense salutary effect on survival of patients with previously poor prognoses has made the use of chemotherapy in combination with trastuzumab nearly mandatory in all HER2+ patients with breast cancer. Remarkably, the huge improvement in survival of these formerly doomed patients has led to the recommendation that trastuzumab-containing chemotherapy regimens should be used in the management of even subcentimeter, node-negative patients.3 This recommendation represents a clear change from the traditional recommendations for chemotherapy, which held that the benefits of systemic chemotherapy were more likely to be seen in patients with tumors in excess of 1 cm and/or who were node positive.
Basal-like Tumors
The discovery of trastuzumab made the basal-like tumor, which is usually ER-, PR-, and HER2- (triple negative), the subtype with the worst prognosis. Further, the natural course of this illness is markedly different from that of ER+/PR+ breast cancer. Nearly all basal-like or triple-negative patients with breast cancer who experience a recurrence do so within the first 5 years after diagnosis.4 In contrast, nearly 40% of ER+/PR+ HER2- breast cancer survivors experience their first recurrence beyond the 5-year milestone, with many even later in their course.5 Thus, the patient with triple-negative breast cancer is more likely to benefit from chemotherapy predominantly during the first 5 post-diagnosis years, as suggested by the Early Breast Cancer Trialists’ Collaborative Group meta-analyses.1
HER2+ and triple-negative breast cancers account for 20% and 15% of all breast cancers, respectively.6,7 In both subtypes, the benefit of chemotherapy is immense and chemotherapy will rarely be omitted from the treatment plan. Many of these patients are considered ideal candidates for preoperative chemotherapy (PCT), which results in increased rates of breast-conserving surgery (BCS), decreased positive margin rates at BCS, and decreased need for axillary node dissection. In the setting of PCT, a pathologic complete response (pCR) in the breast and axilla is increasingly recognized as a marker for improved disease-free survival (DFS) and overall survival (OS).8 For these reasons, preoperative consultation with medical oncologists is now even more important. Many of these patients will benefit from the use of PCT before any surgical treatment is undertaken.
Luminal Type (A and B)
The remaining two-thirds of all patients with breast cancer are ER+, primarily postmenopausal, and fall within the 2 remaining molecular subtypes: luminal A and luminal B. It is for these patients that the relative benefits of chemotherapy vs EA, or both, are currently being debated. For these patients the use of gene prognostic signatures, in concert with traditional histopathologic and clinical risk factors, may alter estimates of recurrence risk and the impact of chemotherapy on survival and recurrence estimates.
It is now evident that even the strongest predictors for breast cancer recurrence—histologic grade, patient age, and nodal status—are inconsistent predictors of the behavior of any individual tumor. While the use of chemotherapy can reduce the risk of metastases in these luminal-type patients with breast cancer, the majority of patients so stratified would survive without chemotherapy.9
GENE EXPRESSION SIGNATURE ASSAYS
One of the best demonstrations of the shortcomings of the standard risk predictors for ER+, HER2- breast cancers is provided by the Oncotype DX breast cancer assay’s recurrence score (RS) or gene expression signature (GES).10,11
Oncotype DX
The Oncotype DX assay is the first commercially available GES assay to illustrate the variability in survival of patients with node-negative, ER+ breast tumors. Sixteen selected cancer proliferative genes are paired with 5 control nonproliferative genes whose relative activity can be measured in paraffin-embedded breast cancer tissue. The ability to retrieve reliable ribonucleic acid (RNA) expression from cancer cells embedded in paraffin was a stroke of genius; it enabled the investigators to correlate the gene expression profile of patient subgroups treated decades earlier with their long-term clinical outcomes and survival.
The normalized summation of the proliferative activity of the 16 cancerproliferation genes in the Oncotype DX assay is expressed as the RS. The RS increases linearly and so does the average rate of distant recurrence in 10 years as a function of the RS. Three risk recurrence groups are defined by the RS: low risk (RS < 18); intermediate risk (RS > 18 to 30); and high risk (RS > 31).10,11
Clinical Trials
In the National Surgical Adjuvant Breast and Bowel Project (NSABP) clinical trial B-14, ER+ node-negative patients were randomized to observation or tamoxifen. In the untreated control patients, a low RS (< 18) was accompanied by a 6.8% risk of metastasis at 10 years, and a high RS (> 31) was accompanied by a 30.5% rate of distant recurrence.11 In another study, the low RS tamoxifen-treated arm showed a 2.8% risk of breast cancer death at 10 years vs a 15.5% risk in the high RS cohort.12
The remarkable significance of the RS is demonstrated when the RS is plotted against patient age, grade, or tumor size.10 This illustrates the huge variability in these traditional histopathologic and clinical features within a given RS group. For any patient with a low RS, there is marked variability in patient age, tumor grade, or tumor size. A very small or low-grade tumor can have a very high 10-year recurrence rate, as measured by the gene prognostic signature or RS. Similarly, a very large tumor in a young patient can have a very low 10-year recurrence rate or RS. This is due to the heterogeneity of the biology of these cancers, regardless of their favorable or unfavorable histologic features.
In most cases, decisions about chemotherapy in patient who are postmenopausal, node-negative, and ER+ are made by risk estimates based on patient age, tumor grade, and tumor size, without knowledge of their RS. However, the large variability in 10-year rates of metastases and death among patients clearly demonstrates that, for some, chemotherapy affords no benefit. Their RS suggest that their risk of metastases at 10 years is only 2.8% when treated with EA (ie, tamoxifen) and no chemotherapy. In fact, 51% of the patients who are postmenopausal, node-negative, and ER+ in NSABP B-14 fell within the low risk RS category for 10-year distant recurrence, whereas about 27% fell within the high risk (RS > 31) category.13
Confidence in the Oncotype DX assay RS stems from the ability of investigators to plot the recurrence rates of distant metastases in patientstreated with tamoxifen vs placebo in the NSABP B-14 trial. Their clinicaloutcomes could be correlated with their GES samples retrieved from paraffin-embedded archival tissue many years after treatment. Corresponding plotting was done for similar patient cohorts treated with chemotherapy with or without tamoxifen in NSABP Trial B-20.
Among patients with low RS, the distant recurrence rate at 10 years was 2.2%, whether treated with systemic chemotherapy plus tamoxifenor with tamoxifen alone. Thus, in study participants with low RS, regardless of tumor size, grade, or patient age, 10-year recurrence rates were not affected by the addition of chemotherapy.13
Note that, in the absence of the new information provided by the Oncotype gene prognostic signature, nearly all these patients would be treated with systemic chemotherapy. Studies have shown that the additional risk assessment estimate provided by the Oncotype assay causes a change in systemic therapy recommendations from chemotherapy to no chemotherapy in 30% of patients.14,15 Among patients with high RS, 10-year distant recurrence rates decreased by an absolute 27% with the addition of chemotherapy to tamoxifen. These patients clearly benefited from chemotherapy.13
The relative benefits of chemotherapy vs tamoxifen in a third RS group with an intermediate RS of 18-21 awaits publication of the now-closed Trial Assigning Individualized Options for Treatment (TAILORx) trial. This group accounts for 22% of patients who are postmenopausal, node-negative, and ER+ identified by the Oncotype DX assay. Initial reports show no significant benefit from the addition of chemotherapy to tamoxifen in this group.10
MammaPrint
Other gene prognostic signatures have recently been validated. Of these, the MammaPrint assay is the best established and validated.16 The MammaPrint uses a panel of 70 proliferation genes that were selected without bias by scanning the entire human genome. Unlike the Oncotype DX, the MammaPrint panel was randomly selected without any prior knowledge of the role of the proliferation genes in breast carcinogenesis. Furthermore, the reliability of the MammaPrint gene signature is independent of nodal status.17 This suggests that the intrinsic genetic makeup of the cancer establishes its biologic behavior and supersedes the impact of the traditional assessment of nodal involvement as a significant risk factor for distant metastases.
The MammaPrint GES was developed to identify patients at high risk of recurrence within 5 years of diagnosis; those for whom, as noted earlier, the salutary effect of chemotherapy is most evident.18 The assay is reliable for both pre- and postmenopausal women and stratifies patients into 2 risk groups only: high vs low.19-21 The probability of remaining free of recurrent disease at 10 years is 85% in the low risk GES patients vs 50.6% in those with high risk MammaPrint prognosis signatures.17
Subsequent validation trials examined the accuracy of the MammaPrint as a prognostic indicator as well as a predictor of response to chemotherapy. These studies included node-negative, node-positive, pre- and postmenopausal women.18-23 The risk of metastatic disease within the first 5 years after diagnosis was more significant in the high-risk than in the low-risk group. However, because the MammaPrint signature is independent of ER status, not all MammaPrint low-risk signatures are ER+. This reflects the contribution of unselected proliferation genes to the MammaPrint signature that results in the luminal A and luminal B breast cancer subtypes. In postmenopausal, node-negative patients, 61% may have good prognosis signatures, regardless of ER status.18,22
A poor prognosis signature, then, would suggest the use of chemotherapy to prevent early (< 5 years from diagnosis) breast cancer deaths, but would still allow for EA to prevent late (> 5 years after diagnosis) recurrence for patients whose tumors were ER+. It should be noted that these findings also apply to patients treated with contemporary anthracycline chemotherapy regimens.22 The MammaPrint poor prognostic signature identifies patients at risk for early recurrence who may therefore benefit from chemotherapy, whereas the good prognostic signature identifies patients with a very low risk of distant metastases < 5 years.22 In the latter group, this low risk may not warrant use of systemic chemotherapy, but treatment with EA would confer a decrease in systemic metastases.
THE SURGEON’S PERSPECTIVE
To the surgeon, as suggested earlier, perhaps more pertinent is the available information on the use of chemotherapy before planned surgery for basal-type triple negative and HER-2+ breast cancers in the setting of luminal ER+ tumors. Mounting evidence suggests that the GES, such as those determined via the Oncotype and MammaPrint assays, can provide a very reliable indication of an individual patient’s response to PCT or chemotherapy in the neoadjuvant setting.24,25 These clinical responses are easily quantitated on physical examination or by imaging in the few months during which a patient can receive PCT.
Furthermore, the absence of residual microscopic tumor in the breast and axilla (ie, pCR) after PCT can be predicted by the Oncotype DX RS and the MammaPrint GES. More than 11 reports (5,210 patients) have demonstrated a higher DFS and OS in patients who achieve a pCR after PCT.8 A pCR in a locally advanced patient with breast cancer can provide the surgeon with a margin-negative surgical procedure (BCS or mastectomy) and inform the patient of the potential for a much better DFS or OS than anticipated from the stage of breast cancer at presentation.
In some patients amenable to BCS at presentation but whose tumor is too close to the chest wall or is proximate to a silicone augmentation prosthesis, the predicted response to systemic chemotherapy or hormonal ablation provided by GES can lead to a decrease in margin-positive rates and salvage of the previous cosmetic augmentation.
In patients at risk for carrying a BRCA mutation, the interval of PCT can be used for appropriate genetic testing and counseling and plastic surgery and gynecologic oncology consultations. Identified BRCA gene carriers may benefit from risk reduction surgery because of their increased breast and ovarian cancerrisk. Non-BRCA patients can consider BCS as an option, with decreased margin-positive rates and improved cosmesis. Information provided by GES can be essential to a good surgical outcome and underlines the need for preoperative consultation with medical oncology.26
CONCLUSION
Gene expression signatures provide information about the biologic behavior of each individual patient’s breast cancer. As new GES are introduced into clinical practice, surgeons must become fully informed about these advances in order to provide truly personalized cancer care plans to our patients.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect an endorsement by or opinion of Federal Practitioner, Frontline Medical Communications, the U.S. Air Force, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drug combinations–including indications, contraindications, warnings, and adverse effects–before administering pharmacologic therapy to patients.
1. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687-1717.
2. Sørlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinoma distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98(19):10869-10874.
3. Goldhirsch A, Winer EP, Coates AS, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013;24(9):2206-2223.
4. Pagoda K, Niwinska A, Murawska M, Pienkowski T. Analysis of pattern, time, and risk factors influencing recurrence in triple-negative breast cancer patients. Med Oncol. 2013;30(1):388.
5. Brewster AM, Hortobagyi GN, Broglio KR. Residual risk of breast cancer recurrence 5 years after adjuvant therapy. J Natl Cancer Inst. 2008;100(16):1179-1183.
6. Reynolds S. Triple-negative breast cancer disproportionately affects african american and Hispanic women. NCI Cancer Bulletin. 2007;4(22). www.cancer.gov/ncicancerbulletin/archive/2007/072407/page7. Accessed July 17, 2014.
7. Phillips C. Treatment Options for HER2-positive breast cancer expand and evolve. NCI Cancer Bulletin. 2012;9(20). www.cancer.gov/ncicancerbulletin/101612/page2. Accessed July 17, 2014.
8. Kaufmann M, von Minckwitz G, Mamounas EP, et al. Recommendations from an international conference on the current status and future of neoadjuvant systemic therapy in primary breast cancer. Ann Surg Oncol. 2012;19(5):1508-1516.
9. Coates AS, Colleoni M, Goldhirsch A. Is adjuvant chemotherapy useful for women with luminal A breast cancer? J Clin Oncol. 2012;30(12):1260-1263.
10. Paik S, Tang G, Kim C, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24(23):3726-3734.
11. Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351(27):2817-2826.
12. Habel LA, Shak S, Jacobs MK, et al. A population-based study of tumor gene expression and risk of breast cancer death among lymph node-negative patients. Breast Cancer Res. 2006;8(3):1-15.
13. Sparano JA, Paik S. Development of the 21-gene assay and its application in clinical practice and clinical trials. J Clin Oncol. 2008;26(5):721-728.
14. Lo SS, Mumby PB, Norton J, et al. Prospective multicenter study of the impact of the 21-gene recurrence score assay on medical oncologists and patient adjuvant breast cancer treatment selection. J Clin Oncol. 2010;28(10):1671-1676.
15. Hassett MJ, Silver SM, Hughes ME, et al. Adoption of gene expression profile testing and association with the use of chemotherapy among women with breast cancer. J Clin Oncol. 2012;30(18):2218-2226.
16. van’t Veer LJ, Dai H, van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415(6871):530-536.
17. van de Vijver MJ, He YD, van’t Veer LJ, et al. A gene expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002;347(25):1999-2009.
18. Mook S, Schmidt MK, Weigelt B, et al. The 70-gene prognostic signature predicts early metastasis in breast cancer patients between 55 and 70 years of age. Ann Oncol. 2010;21(4):717-722.
19. Drukker CA, Bueno-de-Mesquita JM, Retél VP, et al. A prospective evaluation of a breast cancer prognostic signature in the observational RASTER study. Intl J Cancer. 2013;133(4):929-936.
20. Buyse M, Loi S, van’t Veer L, et al. Validation and clinical utility of a 70-gene prognostic signature for women with node-negative breast cancer. J Natl Cancer Inst. 2006;98(17): 1183-1192.
21. Bueno-de-Mesquita JM, Linn SC, Keijzer R, et al. Validation of 70-gene prognostic signature in node-negative breast cancer. Breast Cancer Res Treat. 2009;117(3):483-495.
22. Knauer M, Mook S, Rutgers EJ, et al. The predictive value of the 70-gene signature for adjuvant chemotherapy in early breast cancer. Breast Cancer Res Treat. 2010;120(3):655-661.
23. Mook S, Schmidt MK, Viale G, et al; TRANSBIG Consortium. The 70-gene prognosis-signature predicts disease outcome in breast cancer patients with 1-3 positive lymph nodes in an independent validation study. Breast Cancer Res Treat. 2009;116(2):295-302.
24. Gianni L, Zambetti M, Clark K, et al. Gene expression profiles in paraffin-embedded core biopsy tissue predicts response to chemotherapy in women with locally advanced breast cancer. J Clin Oncol. 2005;23(29):7265-7277.
25. Straver ME, Glas AM, Hannemann J, et al. The 70-gene signature as a response predictor for neoadjuvant chemotherapy in breast cancer. Breast Cancer Res Treat. 2010;119(3):551-558.
26. Silva E. Targeted tailored management of the breast cancer patient at risk for harboring a germline mutation: current trends affecting the selection of patients considering surgical prophylaxis. Breast J. 2009;15(suppl 1):S76-S80.
1. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687-1717.
2. Sørlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinoma distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98(19):10869-10874.
3. Goldhirsch A, Winer EP, Coates AS, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013;24(9):2206-2223.
4. Pagoda K, Niwinska A, Murawska M, Pienkowski T. Analysis of pattern, time, and risk factors influencing recurrence in triple-negative breast cancer patients. Med Oncol. 2013;30(1):388.
5. Brewster AM, Hortobagyi GN, Broglio KR. Residual risk of breast cancer recurrence 5 years after adjuvant therapy. J Natl Cancer Inst. 2008;100(16):1179-1183.
6. Reynolds S. Triple-negative breast cancer disproportionately affects african american and Hispanic women. NCI Cancer Bulletin. 2007;4(22). www.cancer.gov/ncicancerbulletin/archive/2007/072407/page7. Accessed July 17, 2014.
7. Phillips C. Treatment Options for HER2-positive breast cancer expand and evolve. NCI Cancer Bulletin. 2012;9(20). www.cancer.gov/ncicancerbulletin/101612/page2. Accessed July 17, 2014.
8. Kaufmann M, von Minckwitz G, Mamounas EP, et al. Recommendations from an international conference on the current status and future of neoadjuvant systemic therapy in primary breast cancer. Ann Surg Oncol. 2012;19(5):1508-1516.
9. Coates AS, Colleoni M, Goldhirsch A. Is adjuvant chemotherapy useful for women with luminal A breast cancer? J Clin Oncol. 2012;30(12):1260-1263.
10. Paik S, Tang G, Kim C, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24(23):3726-3734.
11. Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351(27):2817-2826.
12. Habel LA, Shak S, Jacobs MK, et al. A population-based study of tumor gene expression and risk of breast cancer death among lymph node-negative patients. Breast Cancer Res. 2006;8(3):1-15.
13. Sparano JA, Paik S. Development of the 21-gene assay and its application in clinical practice and clinical trials. J Clin Oncol. 2008;26(5):721-728.
14. Lo SS, Mumby PB, Norton J, et al. Prospective multicenter study of the impact of the 21-gene recurrence score assay on medical oncologists and patient adjuvant breast cancer treatment selection. J Clin Oncol. 2010;28(10):1671-1676.
15. Hassett MJ, Silver SM, Hughes ME, et al. Adoption of gene expression profile testing and association with the use of chemotherapy among women with breast cancer. J Clin Oncol. 2012;30(18):2218-2226.
16. van’t Veer LJ, Dai H, van de Vijver MJ, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415(6871):530-536.
17. van de Vijver MJ, He YD, van’t Veer LJ, et al. A gene expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002;347(25):1999-2009.
18. Mook S, Schmidt MK, Weigelt B, et al. The 70-gene prognostic signature predicts early metastasis in breast cancer patients between 55 and 70 years of age. Ann Oncol. 2010;21(4):717-722.
19. Drukker CA, Bueno-de-Mesquita JM, Retél VP, et al. A prospective evaluation of a breast cancer prognostic signature in the observational RASTER study. Intl J Cancer. 2013;133(4):929-936.
20. Buyse M, Loi S, van’t Veer L, et al. Validation and clinical utility of a 70-gene prognostic signature for women with node-negative breast cancer. J Natl Cancer Inst. 2006;98(17): 1183-1192.
21. Bueno-de-Mesquita JM, Linn SC, Keijzer R, et al. Validation of 70-gene prognostic signature in node-negative breast cancer. Breast Cancer Res Treat. 2009;117(3):483-495.
22. Knauer M, Mook S, Rutgers EJ, et al. The predictive value of the 70-gene signature for adjuvant chemotherapy in early breast cancer. Breast Cancer Res Treat. 2010;120(3):655-661.
23. Mook S, Schmidt MK, Viale G, et al; TRANSBIG Consortium. The 70-gene prognosis-signature predicts disease outcome in breast cancer patients with 1-3 positive lymph nodes in an independent validation study. Breast Cancer Res Treat. 2009;116(2):295-302.
24. Gianni L, Zambetti M, Clark K, et al. Gene expression profiles in paraffin-embedded core biopsy tissue predicts response to chemotherapy in women with locally advanced breast cancer. J Clin Oncol. 2005;23(29):7265-7277.
25. Straver ME, Glas AM, Hannemann J, et al. The 70-gene signature as a response predictor for neoadjuvant chemotherapy in breast cancer. Breast Cancer Res Treat. 2010;119(3):551-558.
26. Silva E. Targeted tailored management of the breast cancer patient at risk for harboring a germline mutation: current trends affecting the selection of patients considering surgical prophylaxis. Breast J. 2009;15(suppl 1):S76-S80.
New insight into stem cell differentiation
Adam Engler, UC San Diego
Jacobs School of Engineering
The stiffness of the extracellular matrix may play a larger role in stem cell differentiation than we thought, according to a new study.
Scientists have recently suggested that protein tethering and matrix porosity, as well as matrix stiffness and ligand type, regulate stem cell differentiation.
However, new research published in Nature Materials indicates that matrix stiffness regulates stem cell differentiation independently of tethering and porosity.
Adam Engler, PhD, of the University of California, San Diego, and his colleagues discovered that human adipose stromal cells and mesenchymal stromal cells underwent osteogenic differentiation if placed in a stiff hydrogel. But the cells underwent adipogenesis if placed in a soft hydrogel.
The protein binding the stem cell to the hydrogel was not a factor in the differentiation process. Results suggested the protein layer was merely an adhesive.
The researchers found that stem cell differentiation is a response to the mechanical deformation of the hydrogel from the force exerted by the cell. With a series of experiments, the team showed that this happens whether the protein tethering the cell to the matrix is tight, loose, or nonexistent.
Across multiple samples using a stiff matrix, varying the degree of tethering made no significant difference in the rate of osteogenic or adipogenic differentiation.
Likewise, the size of the pores in the matrix had no effect on stem cell differentiation, as long as the stiffness of the hydrogel remained the same.
However, Dr Engler pointed out that matrix stiffness is only “one cue out of dozens that are important in stem cell differentiation.”
“That doesn’t mean the other cues are irrelevant,” he noted. “They may still push the cells into a specific cell type. We have just ruled out porosity and tethering, and further emphasized stiffness in this process.” ![]()
Adam Engler, UC San Diego
Jacobs School of Engineering
The stiffness of the extracellular matrix may play a larger role in stem cell differentiation than we thought, according to a new study.
Scientists have recently suggested that protein tethering and matrix porosity, as well as matrix stiffness and ligand type, regulate stem cell differentiation.
However, new research published in Nature Materials indicates that matrix stiffness regulates stem cell differentiation independently of tethering and porosity.
Adam Engler, PhD, of the University of California, San Diego, and his colleagues discovered that human adipose stromal cells and mesenchymal stromal cells underwent osteogenic differentiation if placed in a stiff hydrogel. But the cells underwent adipogenesis if placed in a soft hydrogel.
The protein binding the stem cell to the hydrogel was not a factor in the differentiation process. Results suggested the protein layer was merely an adhesive.
The researchers found that stem cell differentiation is a response to the mechanical deformation of the hydrogel from the force exerted by the cell. With a series of experiments, the team showed that this happens whether the protein tethering the cell to the matrix is tight, loose, or nonexistent.
Across multiple samples using a stiff matrix, varying the degree of tethering made no significant difference in the rate of osteogenic or adipogenic differentiation.
Likewise, the size of the pores in the matrix had no effect on stem cell differentiation, as long as the stiffness of the hydrogel remained the same.
However, Dr Engler pointed out that matrix stiffness is only “one cue out of dozens that are important in stem cell differentiation.”
“That doesn’t mean the other cues are irrelevant,” he noted. “They may still push the cells into a specific cell type. We have just ruled out porosity and tethering, and further emphasized stiffness in this process.” ![]()
Adam Engler, UC San Diego
Jacobs School of Engineering
The stiffness of the extracellular matrix may play a larger role in stem cell differentiation than we thought, according to a new study.
Scientists have recently suggested that protein tethering and matrix porosity, as well as matrix stiffness and ligand type, regulate stem cell differentiation.
However, new research published in Nature Materials indicates that matrix stiffness regulates stem cell differentiation independently of tethering and porosity.
Adam Engler, PhD, of the University of California, San Diego, and his colleagues discovered that human adipose stromal cells and mesenchymal stromal cells underwent osteogenic differentiation if placed in a stiff hydrogel. But the cells underwent adipogenesis if placed in a soft hydrogel.
The protein binding the stem cell to the hydrogel was not a factor in the differentiation process. Results suggested the protein layer was merely an adhesive.
The researchers found that stem cell differentiation is a response to the mechanical deformation of the hydrogel from the force exerted by the cell. With a series of experiments, the team showed that this happens whether the protein tethering the cell to the matrix is tight, loose, or nonexistent.
Across multiple samples using a stiff matrix, varying the degree of tethering made no significant difference in the rate of osteogenic or adipogenic differentiation.
Likewise, the size of the pores in the matrix had no effect on stem cell differentiation, as long as the stiffness of the hydrogel remained the same.
However, Dr Engler pointed out that matrix stiffness is only “one cue out of dozens that are important in stem cell differentiation.”
“That doesn’t mean the other cues are irrelevant,” he noted. “They may still push the cells into a specific cell type. We have just ruled out porosity and tethering, and further emphasized stiffness in this process.” ![]()
Current Options and Future Directions in the Systemic Treatment of Metastatic Melanoma
This article has been adapted from an article originally published in The Journal of Supportive and Community Oncology (jcso-online.com). Schindler K, Postow M. Current options and future directions in the systemic treatment of metastatic melanoma. J Community Support Oncol. 2014;12(1):20-26.
The incidence of melanoma, a highly aggressive tumor arising from melanocytes, continues to rise by about 3% a year in the U.S. with about 76,000 patients being diagnosed every year and 9,000 patients dying of the disease.1 Complete surgical resection is the standard for localized melanoma, with surgical excision margins depending on tumor thickness. For patients with involved sentinel lymph nodes, complete lymphadenectomy is typically recommended, although the benefits of completion lymphadenectomy are being evaluated in an ongoing randomized trial.2,3
For patients with surgically resected, high-risk melanoma, the only approved adjuvant therapy is interferon-a (IFN-a).4 Use of IFN-a, however, remains controversial because of the associated adverse effects (AEs) and controversial effects on overall survival (OS).5,6 Unfortunately, many patients with localized disease will ultimately experience a recurrence, and the prognosis of patients with metastatic disease is poor with a historical 5-year survival rate of 10%.7
Chemotherapy and interleukin 2
For more than 3 decades, conventional cytotoxic chemotherapy was used to treat metastatic melanoma. Typical agents included alkylating agents (dacarbazine, temozolomide, nitrosoureas), platinum analogs (cisplatin and carboplatin), and microtubular toxins (vinblastine and paclitaxel). Despite the clinical use and investigation of a number of these chemotherapies for patients with metastatic melanoma, the only treatment approved by the FDA is dacarbazine, which is administered intravenously every 3 to 4 weeks at a dose of 800 to 1,000 mg/m2.
Monotherapy with dacarbazine is generally well tolerated with only mild AEs such as nausea, myelosuppression, and fatigue. In a pooled analysis, the overall response rate (RR) for dacarbazine was approximately 9%.8 Temozolomide, the oral analog of dacarbazine, penetrates into the central nervous system and has been compared with dacarbazine in randomized trials. These agents are believed to have similar efficacy, but temozolomide has been associated with a higher rate of lymphopenia.9,10
Investigation of chemotherapy combinations such as cisplatin, vinblastine, and dacarbazine or carboplatin and paclitaxel have shown promising RRs but unfortunately no prolongation of OS compared with single-agent dacarbazine.11-13 Despite its modest efficacy, chemotherapy still has a place in the palliative treatment for some patients.
In addition to dacarbazine, the immunotherapeutic strategy, high-dose recombinant interleukin-2 (IL-2), had also been a mainstay treatment for advanced melanoma for many years. IL-2 is administered as an IV infusion every 8 hours at a dose of 600,000 to 720,000 IU/kg on days 1 to 5 and days 15 to 19, with a maximum of 14 such biphasic cycles. Because of the significant acute toxicity profile, including capillary leak syndrome, cardiovascular complications, and seizures, IL-2 treatment requires hospitalization and is generally only performed at specialized centers for patients with good performance status. Though the overall RR in pooled analysis was low at 16%, the durability of responses in some responders that appeared to last many years led to the FDA approval of IL-2 in 1998.14,15
IL-2 continues to be investigated. In a randomized trial, an improved RR and progression-free survival (PFS) were seen when IL-2 was combined with the glycoprotein 100 (gp100) peptide vaccine compared with IL-2 alone.16 Other approaches have sought to improve the safety of IL-2 by selectively delivering it to tumor sites. The fusion protein L19-IL2 couples IL-2 with the recombinant human vascular targeting antibody L19 and has preliminarily been shown to be safe in phase 1 evaluation and in combination with dacarbazine.17,18
Antibodies that block immunologic checkpoints
Melanoma has long been recognized as an immunogenic malignancy but the efficacy of immunotherapeutic strategies has generally been modest. The precise etiology of why immunotherapy historically was not more successful is not completely understood, but it is possible that patients with advanced malignancy have predominant immune inhibitory circuits that prevent otherwise effective antitumor immune responses.
In recent years, research has illuminated some of these immunologic inhibitory elements, termed “immunologic checkpoints,” which include cytotoxic T-lymphocyte antigen 4 (CTLA-4) and programmed death-1 (PD-1). Antibodies that target these checkpoints have resulted in durable responses in some patients and a unique pattern of immune-mediated AEs. Though an ongoing area of research, no pre- or on-treatment biomarkers have been sufficiently validated to enable specific patient selection for these therapies.
Antibodies Blocking CTLA-4
CTLA-4 is expressed on activated T cells and typically functions as a negative regulator of T-cell activity preserving normal immunologic homeostasis. Blocking CTLA-4 with therapeutic antibodies such as ipilimumab and tremelimumab prevents normal CTLA-4–mediated T-cell downregulation and thereby enhances the ability of T cells to exert their full antitumor immune effects (Figure 1). Ipilimumab was the first drug in the management of metastatic melanoma to show an improvement in OS in phase 3 studies, and although a phase 3 study of tremelimumab did not demonstrate an improvement in OS, durable responses were similarly seen.19-21
The first phase 3 trial investigating ipilimumab randomized previously pretreated patients with advanced melanoma to ipilimumab at a dose of 3 mg/kg with or without the gp100 peptide vaccine. The median OS was 10.0 months among patients receiving ipilimumab plus gp100, compared with 6.4 months among patients receiving gp100 alone. There was no difference in OS between the ipilimumab groups.19 The outcome of this study has led to the approval of ipilimumab at a dose of 3 mg/kg in patients with advanced melanoma by regulatory agencies in the U.S., European Union, and Australia.
For treatment-naive patients, a second phase 3 trial investigating dacarbazine in combination with ipilimumab compared with dacarbazine in combination with placebo also demonstrated improvement of OS in patients treated with dacarbazine in combination with ipilimumab.20 The estimated 1-year, 2-year, and 3-year survival rates were 47.3%, 28.5%, and 20.8%, respectively, in the dacarbazine plus ipilimumab group, compared with 36.3%, 17.9%, and 12.2% in the dacarbazine alone group. This second trial used a higher dose of ipilimumab (10 mg/kg) and though it confirmed ipilimumab’s beneficial effects on OS, ipilimumab is not approved at 10 mg/kg and is not routinely recommended to be used in combination with dacarbazine given hepatic toxicity concerns.
Though the median OS was improved in these phase 3 trials, perhaps the greatest activity of ipilimumab lies in the increased number of patients who can achieve long-term OS. In a recently published updated survival analysis, the 4-year survival rates for previously treated patients who received ipilimumab at 3 or 10 mg/kg were 18.2% and 19.7% to 28.4%. For treatment-naive patients receiving ipilimumab at 10 mg/kg, 4-year survival rates were between 37.7% and 49.5%.22 These values appear superior to historical data from prior chemotherapy trials.
An important consideration in the clinical use of CTLA-4 blocking antibodies is the possible occurrence of toxicities that differ from those associated with traditional chemotherapy. These AEs are termed immune-related AEs (irAEs), and they most commonly manifest as diarrhea, dermatitis, hepatitis, and endocrinopathies but less commonly can involve other organs, resulting in uveitis, nephritis, myopathy, and neuropathy.
In general, the onset of irAEs follows a certain pattern with cutaneous manifestations often presenting early in treatment, followed by gastrointestinal and hepatic events occurring about 2 months into therapy and endocrinopathies appearing even later.23 In rare cases, severe AEs (eg, perforating colitis, toxic epidermal necrolysis) can occur and may require hospitalization.24
Clinicians must be attentive to early signs of these AEs and promptly initiate immunosuppression with steroids or other immunosuppressive medications, which do not appear to diminish the antitumor immune effects.25 Established management algorithms exist to guide clinicians. Given the occasional need for immunosuppression in this patient population, awareness of the possibility of opportunistic or rare infections is also important.
In phase 3 evaluation, the number of patients who had long-term survival exceeded the number of patients who had a classically defined disease response to treatment. Durable stable disease and late responses have been observed clinically and may be responsible for some of the beneficial outcomes.26 If patients are asymptomatic and have minimal radiographic progression, it is reasonable to repeat imaging 1 to 2 months later to confirm progression before considering additional lines of therapy.
Antibodies Blocking the Programmed Death-1 Axis
Programmed death-1 (PD-1) is a receptor on the surface of T cells that is upregulated at later stages of T-cell activation as opposed to the early upregulation of CTLA-4. Normally, engagement of PD-1 attenuates T-cell activity at several phases of an immune response. Tumors are believed to escape immune attack by similarly inhibiting T-cell activity by upregulating one of the ligands of PD-1, PD-L1.27,28 Several antibodies that inhibit PD-1 activity, either by blocking the PD-1 molecule itself or PD-L1, are demonstrating significant promise in ongoing clinical trials.
Nivolumab (previously, BMS-936558) is a fully human monoclonal antibody targeting PD-1. In a large phase 1 study in patients with a variety of malignancies, nivolumab demonstrated a 31% RR in patients with advanced melanoma.29 Subsequent follow-up data indicates these responses are generally durable with a median duration of response of 24 months and a 3-year OS rate of 40%.30 Adverse effects of nivolumab appear less frequently than with CTLA-4 blockade but have included vitiligo, colitis, hepatitis, hypophysitis, and thyroiditis. Unique to PD-1 blockade appears to be the AE of an inflammatory pneumonitis, which can present with a dry cough, dyspnea, and ground-glass opacities and can be potentially lethal.29
On the basis of complementary regulatory roles of CTLA-4 and PD-1 checkpoint inhibition, a trial investigating combined nivolumab and ipilimumab was completed. In the small group of patients treated, a high RR was seen with a generally acceptable safety profile.31 Ongoing phase 2 and 3 trials are assessing nivolumab alone and in combination with other agents for the treatment of advanced melanoma and other malignancies (Table 1).
Another PD-1 blocking antibody, MK-3475, has been evaluated in patients with advanced melanoma, and promising RRs have been described.32 In a small group of patients, the confirmed RR at a dose of 10 mg/kg every 2 weeks was 52% and appeared similar in patients who had and who had not been previously treated with ipilimumab. The AEs of MK-3475 seem to resemble nivolumab. MK-3475 is similarly being evaluated in large phase 2 and 3 trials for both patients with melanoma and additional malignancies.
In addition to antibodies targeting PD-1, clinical activity has also been observed with several different antibodies (BMS-936559, MPDL3280A, and MEDI4736) that target PD-L1. Though some data have been published for this therapeutic strategy,33 ongoing trials will continue to clarify the role of targeting PD-L1 in patients with advanced melanoma.
Targeted Therapies That Block Oncogenic Signaling Pathways
The mitogen-activated protein kinase (MAPK) pathway responds to extracellular growth signals and regulates cell proliferation and survival. In many patients with melanoma, the MAPK pathway is constitutively activated as a result of molecular alterations in genes encoding key regulators or components of the pathway such as BRAF, NRAS, and KIT.34,35 The most common mutation arising in melanoma is the BRAF mutation, occurring in nearly half of melanomas, and typically involves a missense mutation in which glutamic acid is substituted for valine at codon 600 (BRAF V600E mutation).36 Less frequent BRAF mutations include V600K, V600R, and K601E.37 Strategies that directly inhibit oncogenic BRAF or disable downstream elements such as MEK have recently shown dramatic results in patients with melanoma (Figure 2).
BRAF inhibitors
Vemurafenib is a potent inhibitor of mutated BRAF with marked antitumor effects against melanoma cell lines with the BRAF V600E mutation.38 The first striking results of tumor regression with this strategy in patients were seen in a phase 1 study in patients with melanoma characterized by a BRAF V600E mutation but not in patients whose melanomas did not have a BRAF mutation.39
Subsequent phase 3 trials confirmed the high RRs of this agent in patients with BRAF-mutant melanoma and demonstrated superiority in OS compared with dacarbazine chemotherapy.40 The results of this phase 3 trial led to the approval of vemurafenib by the FDA in August 2011 with treatment exclusively limited to patients with BRAF mutant melanoma. Updated OS data from this phase 3 study revealed a median OS of 13.2 months for vemurafenib, compared with 9.6 months for dacarbazine, with an overall RR in patients treated with vemurafenib of 57% and a median PFS of 6.9 months.41 General AEs with vemurafenib include arthralgia, fatigue, aminotransferase elevations, nausea and vomiting, and decreased kidney function. In general, toxicities are manageable with dose reduction or temporary drug cessation.
One characteristic of vemurafenib and other BRAF-targeted agents is the frequent development of hyperproliferative skin AEs. Skin lesions, including follicular and palmo-plantar hyperkeratosis, papillomas, and also cutaneous squamous-cell carcinomas and keratoacanthomas, have commonly been observed under treatment with vemurafenib, and close evaluation by a dermatologist is important.42 The mechanism of this phenomenon is believed to be a paradoxical activation of the MAPK pathway in nonmelanoma BRAF wild-type cells when systemic treatment with a BRAF inhibitor is administered.43
The phenomenon of hyperproliferation of non–BRAF-mutant tissues with ongoing BRAF-inhibitor therapy has also been seen in patients with lymphoproliferative disorders and may be a mechanism involved in the discovery that patients have a high rate of new primary melanomas while on therapy.44,45 These findings warrant special attention, particularly as BRAF inhibitors are undergoing evaluation as adjuvant therapy.
Another active BRAF kinase inhibitor with a similar efficacy profile as vemurafenib is dabrafenib, which was approved in May 2013 based on the demonstration of improved PFS in a phase 3 trial comparing dabrafenib 150 mg orally twice daily and dacarbazine 1,000 mg/m2 intravenously once every 3 weeks in previously untreated patients with BRAF V600E mutant melanoma. The median PFS times were 5.1 and 2.7 months in the dabrafenib and dacarbazine arms, respectively, with an objective RR of 52% in patients treated with dabrafenib.46 Follow-up time was too short to make a determination of the impact of dabrafenib on OS. In a separate study, dabrafenib was also shown to be effective for patients with brain metastases and remains an excellent therapeutic choice for this particular patient population.47
Generally, dabrafenib is believed to have similar efficacy to vemurafenib. Nevertheless, EAs with of dabrafenib differ somewhat from those observed with vemurafenib: The rate of proliferative skin lesions, including squamous cell carcinomas and keratoacanthomas appears to be lower for dabrafenib than vemurafenib. However, AEs particular to dabrafenib have been seen such as pyrexia, which were recorded in about 11% of patients.46
MEK inhibitors
Though targeting oncogenic BRAF directly has been incredibly successful for patients with BRAF-mutant metastatic melanoma, additional success has been observed by blocking the MAPK pathway at a downstream component, MEK. Trametinib is an MEK inhibitor that was approved by the FDA in June 2013 as a single agent for patients with BRAF V600E or V600K mutant melanoma. Trametinib is administered at a dose of 2 mg once daily and was shown to improve PFS and OS compared with dacarbazine and paclitaxel chemotherapies.47 Despite the improvement in PFS and OS compared with chemotherapy, the objective RR for trametinib was somewhat lower (22%) than that seen with BRAF inhibitors.
Trametinib also is associated with a different AE profile from BRAF inhibitors and includes diarrhea, peripheral edema, hypertension, and fatigue, typical of other MEK inhibitors as well.48 Asymptomatic and reversible reduction of the cardiac ejection fraction and ocular toxic effects also occur infrequently. Unlike with BRAF-inhibitor treatment, the development of cutaneous squamous-cell carcinomas or other hyperproliferative skin lesions was not noted.49
Despite the significant benefits of targeted therapy disrupting overly active MAPK signaling in patients with BRAF-mutant metastatic melanoma, almost all patients treated with these targeted inhibitors who achieve an initial response will ultimately progress. Several mechanisms of resistance have been proposed, and most relate to reactivation of the MAPK pathway.50,51 As a result, efforts to maintain suppression of the MAPK pathway have been pursued to delay the onset of resistance. In a phase 2 trial that combined dabrafenib with trametinib, there was a longer PFS than there was with dabrafenib monotherapy.52
Furthermore, the addition of trametinib to dabrafenib reduced the incidence of squamous-cell carcinoma, providing further evidence that reactivation of the MAPK pathway is involved in these hyperproliferative skin lesions arising under BRAF-directed therapy. A higher rate of febrile episodes was seen, however. An ongoing phase 3 study is looking at whether or not combining BRAF and MEK inhibitors results in improved OS compared with single-agent BRAF. It is premature at this juncture to recommend combining dabrafenib and trametinib until the results of the ongoing phase 3 studies more thoroughly describe the risks and benefits of this approach (Table 2).
KIT inhibitors
In a subset of melanomas, particularly those that arise from mucosal, acral, or chronically sun-damaged skin, mutations are found in the receptor-tyrosine kinase KIT.35 A number of agents directed against KIT, such as imatinib, have been tested in clinical trials. Initial phase 2 studies revealed poor RRs with KIT inhibition in molecularly unselected patients.53-55 Subsequent studies selected patients with KIT genetic aberrations, including mutations and amplifications, and some responses were seen.56-58
Importantly, not all KIT genetic aberrations are believed to be considered equal. Preliminarily, it appears that mutations in exon 11 (L576P) and exon 13 (K642E) appear to be most closely associated with response and may be true driver mutations. Other KIT mutations may have less functional significance but additional research is needed. Imatinib is a reasonable therapeutic choice in patients with a KIT mutation, particularly when an L576P or K642E mutation is present.
conclusions
Since 2011, 4 new drugs—ipilimumab, vemurafenib, dabrafenib, and trametinib—have been approved for the treatment of metastatic melanoma. Exciting early data from PD-1 clinical trials suggest that agents that disrupt PD-1 may also become important therapeutic modalities. Future studies will continue to evaluate combinations of these therapeutic modalities, but caution should be exercised in combining these drugs prior to data from ongoing clinical trials revealing the true benefits and risks of combination therapy. Excessive toxicity was seen in an early phase trial when vemurafenib was combined with ipilimumab.59
Additional research will also explore biomarkers that may help clinicians apply immunotherapy to the most appropriate patients and better understand mechanisms of resistance to targeted therapies. Clinical trials of novel agents or combinations should be considered at every treatment juncture to continue the rapid pace of developing the most innovative and tailored treatment approaches.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10-29.
2. Garbe C, Peris K, Hauschild A, et al; European Dermatology Forum, European Association of Dermato-Oncology, European Organization of Research and Treatment of Cancer. Diagnosis and treatment of melanoma. European consensus-based interdisciplinary guideline—Update 2012. Eur J Cancer. 2012;48(15):2375-2390.
3. Coit DG, Andtbacka R, Bichakjian CK, et al; NCCN Melanoma Panel. Melanoma. J Natl Compr Canc Netw. 2009;7(3):250-275.
4. Molife R, Hancock BW. Adjuvant therapy of malignant melanoma. Crit Rev Oncol Hematol. 2002;44(1):81-102.
5. Wheatley K, Ives N, Hancock B, Gore M, Eggermont A, Suciu S. Does adjuvant interferon-alpha for high-risk melanoma provide a worthwhile benefit? A meta-analysis of the randomised trials. Cancer Treat Rev. 2003;29(4):241-252.
6. Mocellin S, Pasquali S, Rossi CR, Nitti D. Interferon alpha adjuvant therapy in patients with high-risk melanoma: A systematic review and meta-analysis. J Natl Cancer Inst. 2010;102(7):493-501.
7. Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27(36):6199-6206.
8. Luke JJ, Rubinstein LV, Smith GL, Ivy SP, Harris PJ. Similar efficacy for phase I trials in comparison with DTIC for advanced malignant melanoma: an analysis of melanoma outcomes in CTEP-sponsored phase I trials 1995-2011. Melanoma Res. 2013;23(2):152-158.
9. Middleton MR, Grob JJ, Aaronson N, et al. Randomized phase III study of temozolomide versus dacarbazine in the treatment of patients with advanced metastatic malignant melanoma. J Clin Oncol. 2000;18(1):158-166.
10. Teimouri F, Nikfar S, Abdollahi M. Efficacy and side effects of dacarbazine in comparison with temozolomide in the treatment of malignant melanoma: A meta-analysis consisting of 1314 patients. Melanoma Res. 2013;23(5):381-389.
11. Chapman PB, Einhorn LH, Meyers ML, et al. Phase III multicenter randomized trial of the Dartmouth regimen versus dacarbazine in patients with metastatic melanoma. J Clin Oncol. 1999;17(9):2745-2751.
12. Legha SS, Ring S, Papadopoulos N, Plager C, Chawla S, Benjamin R. A prospective evaluation of a triple-drug regimen containing cisplatin, vinblastine, and dacarbazine (CVD) for metastatic melanoma. Cancer. 1989;64(10):2024-2029.
13. Rao RD, Holtan SG, Ingle JN, et al. Combination of paclitaxel and carboplatin as second-line therapy for patients with metastatic melanoma. Cancer. 2006;106(2):375-382.
14. Atkins MB, Kunkel L, Sznol M, Rosenberg SA. High-dose recombinant interleukin-2 therapy in patients with metastatic melanoma: Long-term survival update. Cancer J Sci Am. 2000;6(suppl 1):S11-S14.
15. Atkins MB, Lotze MT, Dutcher JP, et al. High-dose recombinant interleukin 2 therapy for patients with metastatic melanoma: Analysis of 270 patients treated between 1985 and 1993. J Clin Oncol. 1999;17(7):2105-2116.
16. Schwartzentruber DJ, Lawson DH, Richards JM, et al. gp100 peptide vaccine and interleukin-2 in patients with advanced melanoma. N Engl J Med. 2011;364(22):2119-2127.
17. Johannsen M, Spitaleri G, Curigliano G, et al. The tumour-targeting human L19-IL2 immunocytokine: Preclinical safety studies, phase I clinical trial in patients with solid tumours and expansion into patients with advanced renal cell carcinoma. Eur J Cancer. 2010;46(16):2926-2935.
18. Eigentler TK, Weide B, de Braud F, et al. A dose-escalation and signal-generating study of the immunocytokine L19-IL2 in combination with dacarbazine for the therapy of patients with metastatic melanoma. Clin Cancer Res. 2011;17(24):7732-7742.
19. Hodi FS, O'Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711-723.
20. Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364(26):2517-2526.
21. Ribas A, Kefford R, Marshall MA, et al. Phase III randomized clinical trial comparing tremelimumab with standard-of-care chemotherapy in patients with advanced melanoma. J Clin Oncol. 2013;31(5):616-622.
22. Wolchok JD, Weber JS, Maio M, et al. Four-year survival rates for patients with metastatic melanoma who received ipilimumab in phase II clinical trials. Ann Oncol. 2013;24(8):2174-2180.
23. Weber JS, Kähler KC, Hauschild A. Management of immune-related adverse events and kinetics of response with ipilimumab. J Clin Oncol. 2012;30(21):2691-2697.
24. Di Giacomo AM, Biagioli M, Maio M. The emerging toxicity profiles of anti-CTLA-4 antibodies across clinical indications. Semin Oncol. 2010;37(5):499-507.
25. Harmankaya K, Erasim C, Koelblinger C, et al. Continuous systemic corticosteroids do not affect the ongoing regression of metastatic melanoma for more than two years following ipilimumab therapy. Med Oncol. 2011;28(4):1140-1144.
26. Wolchok JD, Hoos A, O’Day S, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: Immune-related response criteria. Clin Cancer Res. 2009;15(23):7412-7420.
27. Zou W, Chen L. Inhibitory B7-family molecules in the tumour microenvironment. Nat Rev Immunol. 2008;8(6):467-477.
28. Keir ME, Liang SC, Guleria I, et al. Tissue expression of PD-L1 mediates peripheral T cell tolerance. J Exp Med. 2006;203(4):883-895.
29. Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443-2454.
30. Sznol M, Kluger HM, Hodi FS, et al. Survival and long-term follow-up of safety and response in patients (pts) with advanced melanoma (MEL) in a phase I trial of nivolumab (anti-PD-1; BMS-936558; ONO-4538) [ASCO abstract CRA9006]. ASCO Meet Abstr. 2013;31(18_suppl):CRA9006. http://meetinglibrary.asco.org/content/80822. Accessed July 23, 2014.
31. Wolchok JD, Kluger H, Callahan MK, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369(2):122-133.
32. Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369(2):134-144.
33. Brahmer JR, Tykodi SS, Chow LQ, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455-2465.
34. McCubrey JA, Steelman LS, Chappell WH, et al. Roles of the Raf/MEK/ERK pathway in cell growth, malignant transformation and drug resistance.
Biochim Biophys Acta. 2007;1773(8):1263-1284.
35. Curtin JA, Busam K, Pinkel D, Bastian BC. Somatic activation of KIT in distinct subtypes of melanoma. J Clin Oncol. 2006;24(26):4340-4346.
36. Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949-954.
37. Long GV, Menzies AM, Nagrial AM, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29(10):1239-1246.
38. Bollag G, Hirth P, Tsai J, et al. Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma. Nature. 2010;467(7315):596-599.
39. Flaherty KT, Puzanov I, Kim KB, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010;363(9):809-819.
40. Chapman PB, Hauschild A, Robert C, et al; BRIM-3 Study Group. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364(26):2507-2516.
41. Chapman PB, Hauschild A, Robert C, et al. Updated overall survival (OS) results for BRIM-3, a phase III randomized, open-label, multicenter trial comparing BRAF inhibitor vemurafenib (vem) with dacarbazine (DTIC) in previously untreated patients with BRAF(V600E)-mutated melanoma [ASCO abstract 8502]. ASCO Meet Abstr. 2012;30(15_suppl):8502. http://meetinglibrary.asco.org/content/70533?media=vm. Accessed July 23, 2014.
42. Lacouture ME, O’Reilly K, Rosen N, Solit DB. Induction of cutaneous squamous cell carcinomas by RAF inhibitors: Cause for concern? J Clin Oncol. 2012;30(3):329-330.
43. Su F, Viros A, Milagre C, et al. RAS mutations in cutaneous squamous-cell carcinomas in patients treated with BRAF inhibitors. New Engl J Med. 2012;366(3):207-215.
44. Callahan MK, Rampal R, Harding JJ, et al. Progression of RAS-mutant leukemia during RAF inhibitor treatment. New Engl J Med. 2012;367(24):2316-2321.
45. Zimmer L, Hillen U, Livingstone E, et al. Atypical melanocytic proliferations and new primary melanomas in patients with advanced melanoma undergoing selective BRAF inhibition. J Clin Oncol. 2012;30(19):2375-2383.
46. Hauschild A, Grob JJ, Demidov LV, et al. Dabrafenib in BRAF-mutated metastatic melanoma: A multicentre, open-label phase 3 randomised clinical trial. Lancet 2012;380(9839):358-365.
47. Long GV, Trefzer U, Davies MA, et al. Dabrafenib in patients with Val600Glu or Val600Lys BRAF-mutant melanoma metastatic to the brain (BREAK-MB): A multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13(11):1087-1095.
48. Kirkwood JM, Bastholt L, Robert C, et al. Phase II, open-label, randomized trial of the MEK1/2 inhibitor selumetinib as monotherapy versus temozolomide in patients with advanced melanoma. Clin Cancer Res. 2012;18(2):555-567.
49. Flaherty KT, Robert C, Hersey P, et al; METRIC Study Group. Improved survival with MEK inhibition in BRAF-mutated melanoma. New Engl J Med. 2012;367(2):107-114.
50. Poulikakos PI, Persaud Y, Janakiraman M, et al. RAF inhibitor resistance is mediated by dimerization of aberrantly spliced BRAF(V600E). Nature. 2011;480(7377):387-390.
51. Nazarian R, Shi H, Wang Q, et al. Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature. 2010;468(7326):973-977.
52. Flaherty KT, Infante JR, Daud A, et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. New Engl J Med. 2012;367(18):1694-1703.
53. Ugurel S, Hildenbrand R, Zimpfer A, et al. Lack of clinical efficacy of imatinib in metastatic melanoma. Br J Cancer. 2005;9(8):1398-1405.
54. Wyman K, Atkins MB, Prieto V, et al. Multicenter Phase II trial of high-dose imatinib mesylate in metastatic melanoma: Significant toxicity with no clinical efficacy. Cancer. 2006;106(9):2005-2011.
55. Kim KB, Eton O, Davis DW, et al. Phase II trial of imatinib mesylate in patients with metastatic melanoma. Br J Cancer. 2008;99(5):734-740.
56. Carvajal RD, Antonescu CR, Wolchok JD, et al. KIT as a therapeutic target in metastatic melanoma. JAMA. 2011;305(22):2327-2334.
57. Hodi FS, Corless CL, Giobbie-Hurder A, et al. Imatinib for melanomas harboring mutationally activated or amplified KIT arising on mucosal, acral, and chronically sun-damaged skin. J Clin Oncol. 2013;31(26):3182-3190.
58. Guo J, Si L, Kong Y, et al. Phase II, open-label, single-arm trial of imatinib mesylate in patients with metastatic melanoma harboring c-Kit mutation or amplification. J Clin Oncol. 2011;29(21):2904-2909.
59. Ribas A, Hodi FS, Callahan M, et al. Hepatotoxicity with combination of vemurafenib and ipilimumab. N Engl J Med. 2013;368(14):1365-1366.
This article has been adapted from an article originally published in The Journal of Supportive and Community Oncology (jcso-online.com). Schindler K, Postow M. Current options and future directions in the systemic treatment of metastatic melanoma. J Community Support Oncol. 2014;12(1):20-26.
The incidence of melanoma, a highly aggressive tumor arising from melanocytes, continues to rise by about 3% a year in the U.S. with about 76,000 patients being diagnosed every year and 9,000 patients dying of the disease.1 Complete surgical resection is the standard for localized melanoma, with surgical excision margins depending on tumor thickness. For patients with involved sentinel lymph nodes, complete lymphadenectomy is typically recommended, although the benefits of completion lymphadenectomy are being evaluated in an ongoing randomized trial.2,3
For patients with surgically resected, high-risk melanoma, the only approved adjuvant therapy is interferon-a (IFN-a).4 Use of IFN-a, however, remains controversial because of the associated adverse effects (AEs) and controversial effects on overall survival (OS).5,6 Unfortunately, many patients with localized disease will ultimately experience a recurrence, and the prognosis of patients with metastatic disease is poor with a historical 5-year survival rate of 10%.7
Chemotherapy and interleukin 2
For more than 3 decades, conventional cytotoxic chemotherapy was used to treat metastatic melanoma. Typical agents included alkylating agents (dacarbazine, temozolomide, nitrosoureas), platinum analogs (cisplatin and carboplatin), and microtubular toxins (vinblastine and paclitaxel). Despite the clinical use and investigation of a number of these chemotherapies for patients with metastatic melanoma, the only treatment approved by the FDA is dacarbazine, which is administered intravenously every 3 to 4 weeks at a dose of 800 to 1,000 mg/m2.
Monotherapy with dacarbazine is generally well tolerated with only mild AEs such as nausea, myelosuppression, and fatigue. In a pooled analysis, the overall response rate (RR) for dacarbazine was approximately 9%.8 Temozolomide, the oral analog of dacarbazine, penetrates into the central nervous system and has been compared with dacarbazine in randomized trials. These agents are believed to have similar efficacy, but temozolomide has been associated with a higher rate of lymphopenia.9,10
Investigation of chemotherapy combinations such as cisplatin, vinblastine, and dacarbazine or carboplatin and paclitaxel have shown promising RRs but unfortunately no prolongation of OS compared with single-agent dacarbazine.11-13 Despite its modest efficacy, chemotherapy still has a place in the palliative treatment for some patients.
In addition to dacarbazine, the immunotherapeutic strategy, high-dose recombinant interleukin-2 (IL-2), had also been a mainstay treatment for advanced melanoma for many years. IL-2 is administered as an IV infusion every 8 hours at a dose of 600,000 to 720,000 IU/kg on days 1 to 5 and days 15 to 19, with a maximum of 14 such biphasic cycles. Because of the significant acute toxicity profile, including capillary leak syndrome, cardiovascular complications, and seizures, IL-2 treatment requires hospitalization and is generally only performed at specialized centers for patients with good performance status. Though the overall RR in pooled analysis was low at 16%, the durability of responses in some responders that appeared to last many years led to the FDA approval of IL-2 in 1998.14,15
IL-2 continues to be investigated. In a randomized trial, an improved RR and progression-free survival (PFS) were seen when IL-2 was combined with the glycoprotein 100 (gp100) peptide vaccine compared with IL-2 alone.16 Other approaches have sought to improve the safety of IL-2 by selectively delivering it to tumor sites. The fusion protein L19-IL2 couples IL-2 with the recombinant human vascular targeting antibody L19 and has preliminarily been shown to be safe in phase 1 evaluation and in combination with dacarbazine.17,18
Antibodies that block immunologic checkpoints
Melanoma has long been recognized as an immunogenic malignancy but the efficacy of immunotherapeutic strategies has generally been modest. The precise etiology of why immunotherapy historically was not more successful is not completely understood, but it is possible that patients with advanced malignancy have predominant immune inhibitory circuits that prevent otherwise effective antitumor immune responses.
In recent years, research has illuminated some of these immunologic inhibitory elements, termed “immunologic checkpoints,” which include cytotoxic T-lymphocyte antigen 4 (CTLA-4) and programmed death-1 (PD-1). Antibodies that target these checkpoints have resulted in durable responses in some patients and a unique pattern of immune-mediated AEs. Though an ongoing area of research, no pre- or on-treatment biomarkers have been sufficiently validated to enable specific patient selection for these therapies.
Antibodies Blocking CTLA-4
CTLA-4 is expressed on activated T cells and typically functions as a negative regulator of T-cell activity preserving normal immunologic homeostasis. Blocking CTLA-4 with therapeutic antibodies such as ipilimumab and tremelimumab prevents normal CTLA-4–mediated T-cell downregulation and thereby enhances the ability of T cells to exert their full antitumor immune effects (Figure 1). Ipilimumab was the first drug in the management of metastatic melanoma to show an improvement in OS in phase 3 studies, and although a phase 3 study of tremelimumab did not demonstrate an improvement in OS, durable responses were similarly seen.19-21
The first phase 3 trial investigating ipilimumab randomized previously pretreated patients with advanced melanoma to ipilimumab at a dose of 3 mg/kg with or without the gp100 peptide vaccine. The median OS was 10.0 months among patients receiving ipilimumab plus gp100, compared with 6.4 months among patients receiving gp100 alone. There was no difference in OS between the ipilimumab groups.19 The outcome of this study has led to the approval of ipilimumab at a dose of 3 mg/kg in patients with advanced melanoma by regulatory agencies in the U.S., European Union, and Australia.
For treatment-naive patients, a second phase 3 trial investigating dacarbazine in combination with ipilimumab compared with dacarbazine in combination with placebo also demonstrated improvement of OS in patients treated with dacarbazine in combination with ipilimumab.20 The estimated 1-year, 2-year, and 3-year survival rates were 47.3%, 28.5%, and 20.8%, respectively, in the dacarbazine plus ipilimumab group, compared with 36.3%, 17.9%, and 12.2% in the dacarbazine alone group. This second trial used a higher dose of ipilimumab (10 mg/kg) and though it confirmed ipilimumab’s beneficial effects on OS, ipilimumab is not approved at 10 mg/kg and is not routinely recommended to be used in combination with dacarbazine given hepatic toxicity concerns.
Though the median OS was improved in these phase 3 trials, perhaps the greatest activity of ipilimumab lies in the increased number of patients who can achieve long-term OS. In a recently published updated survival analysis, the 4-year survival rates for previously treated patients who received ipilimumab at 3 or 10 mg/kg were 18.2% and 19.7% to 28.4%. For treatment-naive patients receiving ipilimumab at 10 mg/kg, 4-year survival rates were between 37.7% and 49.5%.22 These values appear superior to historical data from prior chemotherapy trials.
An important consideration in the clinical use of CTLA-4 blocking antibodies is the possible occurrence of toxicities that differ from those associated with traditional chemotherapy. These AEs are termed immune-related AEs (irAEs), and they most commonly manifest as diarrhea, dermatitis, hepatitis, and endocrinopathies but less commonly can involve other organs, resulting in uveitis, nephritis, myopathy, and neuropathy.
In general, the onset of irAEs follows a certain pattern with cutaneous manifestations often presenting early in treatment, followed by gastrointestinal and hepatic events occurring about 2 months into therapy and endocrinopathies appearing even later.23 In rare cases, severe AEs (eg, perforating colitis, toxic epidermal necrolysis) can occur and may require hospitalization.24
Clinicians must be attentive to early signs of these AEs and promptly initiate immunosuppression with steroids or other immunosuppressive medications, which do not appear to diminish the antitumor immune effects.25 Established management algorithms exist to guide clinicians. Given the occasional need for immunosuppression in this patient population, awareness of the possibility of opportunistic or rare infections is also important.
In phase 3 evaluation, the number of patients who had long-term survival exceeded the number of patients who had a classically defined disease response to treatment. Durable stable disease and late responses have been observed clinically and may be responsible for some of the beneficial outcomes.26 If patients are asymptomatic and have minimal radiographic progression, it is reasonable to repeat imaging 1 to 2 months later to confirm progression before considering additional lines of therapy.
Antibodies Blocking the Programmed Death-1 Axis
Programmed death-1 (PD-1) is a receptor on the surface of T cells that is upregulated at later stages of T-cell activation as opposed to the early upregulation of CTLA-4. Normally, engagement of PD-1 attenuates T-cell activity at several phases of an immune response. Tumors are believed to escape immune attack by similarly inhibiting T-cell activity by upregulating one of the ligands of PD-1, PD-L1.27,28 Several antibodies that inhibit PD-1 activity, either by blocking the PD-1 molecule itself or PD-L1, are demonstrating significant promise in ongoing clinical trials.
Nivolumab (previously, BMS-936558) is a fully human monoclonal antibody targeting PD-1. In a large phase 1 study in patients with a variety of malignancies, nivolumab demonstrated a 31% RR in patients with advanced melanoma.29 Subsequent follow-up data indicates these responses are generally durable with a median duration of response of 24 months and a 3-year OS rate of 40%.30 Adverse effects of nivolumab appear less frequently than with CTLA-4 blockade but have included vitiligo, colitis, hepatitis, hypophysitis, and thyroiditis. Unique to PD-1 blockade appears to be the AE of an inflammatory pneumonitis, which can present with a dry cough, dyspnea, and ground-glass opacities and can be potentially lethal.29
On the basis of complementary regulatory roles of CTLA-4 and PD-1 checkpoint inhibition, a trial investigating combined nivolumab and ipilimumab was completed. In the small group of patients treated, a high RR was seen with a generally acceptable safety profile.31 Ongoing phase 2 and 3 trials are assessing nivolumab alone and in combination with other agents for the treatment of advanced melanoma and other malignancies (Table 1).
Another PD-1 blocking antibody, MK-3475, has been evaluated in patients with advanced melanoma, and promising RRs have been described.32 In a small group of patients, the confirmed RR at a dose of 10 mg/kg every 2 weeks was 52% and appeared similar in patients who had and who had not been previously treated with ipilimumab. The AEs of MK-3475 seem to resemble nivolumab. MK-3475 is similarly being evaluated in large phase 2 and 3 trials for both patients with melanoma and additional malignancies.
In addition to antibodies targeting PD-1, clinical activity has also been observed with several different antibodies (BMS-936559, MPDL3280A, and MEDI4736) that target PD-L1. Though some data have been published for this therapeutic strategy,33 ongoing trials will continue to clarify the role of targeting PD-L1 in patients with advanced melanoma.
Targeted Therapies That Block Oncogenic Signaling Pathways
The mitogen-activated protein kinase (MAPK) pathway responds to extracellular growth signals and regulates cell proliferation and survival. In many patients with melanoma, the MAPK pathway is constitutively activated as a result of molecular alterations in genes encoding key regulators or components of the pathway such as BRAF, NRAS, and KIT.34,35 The most common mutation arising in melanoma is the BRAF mutation, occurring in nearly half of melanomas, and typically involves a missense mutation in which glutamic acid is substituted for valine at codon 600 (BRAF V600E mutation).36 Less frequent BRAF mutations include V600K, V600R, and K601E.37 Strategies that directly inhibit oncogenic BRAF or disable downstream elements such as MEK have recently shown dramatic results in patients with melanoma (Figure 2).
BRAF inhibitors
Vemurafenib is a potent inhibitor of mutated BRAF with marked antitumor effects against melanoma cell lines with the BRAF V600E mutation.38 The first striking results of tumor regression with this strategy in patients were seen in a phase 1 study in patients with melanoma characterized by a BRAF V600E mutation but not in patients whose melanomas did not have a BRAF mutation.39
Subsequent phase 3 trials confirmed the high RRs of this agent in patients with BRAF-mutant melanoma and demonstrated superiority in OS compared with dacarbazine chemotherapy.40 The results of this phase 3 trial led to the approval of vemurafenib by the FDA in August 2011 with treatment exclusively limited to patients with BRAF mutant melanoma. Updated OS data from this phase 3 study revealed a median OS of 13.2 months for vemurafenib, compared with 9.6 months for dacarbazine, with an overall RR in patients treated with vemurafenib of 57% and a median PFS of 6.9 months.41 General AEs with vemurafenib include arthralgia, fatigue, aminotransferase elevations, nausea and vomiting, and decreased kidney function. In general, toxicities are manageable with dose reduction or temporary drug cessation.
One characteristic of vemurafenib and other BRAF-targeted agents is the frequent development of hyperproliferative skin AEs. Skin lesions, including follicular and palmo-plantar hyperkeratosis, papillomas, and also cutaneous squamous-cell carcinomas and keratoacanthomas, have commonly been observed under treatment with vemurafenib, and close evaluation by a dermatologist is important.42 The mechanism of this phenomenon is believed to be a paradoxical activation of the MAPK pathway in nonmelanoma BRAF wild-type cells when systemic treatment with a BRAF inhibitor is administered.43
The phenomenon of hyperproliferation of non–BRAF-mutant tissues with ongoing BRAF-inhibitor therapy has also been seen in patients with lymphoproliferative disorders and may be a mechanism involved in the discovery that patients have a high rate of new primary melanomas while on therapy.44,45 These findings warrant special attention, particularly as BRAF inhibitors are undergoing evaluation as adjuvant therapy.
Another active BRAF kinase inhibitor with a similar efficacy profile as vemurafenib is dabrafenib, which was approved in May 2013 based on the demonstration of improved PFS in a phase 3 trial comparing dabrafenib 150 mg orally twice daily and dacarbazine 1,000 mg/m2 intravenously once every 3 weeks in previously untreated patients with BRAF V600E mutant melanoma. The median PFS times were 5.1 and 2.7 months in the dabrafenib and dacarbazine arms, respectively, with an objective RR of 52% in patients treated with dabrafenib.46 Follow-up time was too short to make a determination of the impact of dabrafenib on OS. In a separate study, dabrafenib was also shown to be effective for patients with brain metastases and remains an excellent therapeutic choice for this particular patient population.47
Generally, dabrafenib is believed to have similar efficacy to vemurafenib. Nevertheless, EAs with of dabrafenib differ somewhat from those observed with vemurafenib: The rate of proliferative skin lesions, including squamous cell carcinomas and keratoacanthomas appears to be lower for dabrafenib than vemurafenib. However, AEs particular to dabrafenib have been seen such as pyrexia, which were recorded in about 11% of patients.46
MEK inhibitors
Though targeting oncogenic BRAF directly has been incredibly successful for patients with BRAF-mutant metastatic melanoma, additional success has been observed by blocking the MAPK pathway at a downstream component, MEK. Trametinib is an MEK inhibitor that was approved by the FDA in June 2013 as a single agent for patients with BRAF V600E or V600K mutant melanoma. Trametinib is administered at a dose of 2 mg once daily and was shown to improve PFS and OS compared with dacarbazine and paclitaxel chemotherapies.47 Despite the improvement in PFS and OS compared with chemotherapy, the objective RR for trametinib was somewhat lower (22%) than that seen with BRAF inhibitors.
Trametinib also is associated with a different AE profile from BRAF inhibitors and includes diarrhea, peripheral edema, hypertension, and fatigue, typical of other MEK inhibitors as well.48 Asymptomatic and reversible reduction of the cardiac ejection fraction and ocular toxic effects also occur infrequently. Unlike with BRAF-inhibitor treatment, the development of cutaneous squamous-cell carcinomas or other hyperproliferative skin lesions was not noted.49
Despite the significant benefits of targeted therapy disrupting overly active MAPK signaling in patients with BRAF-mutant metastatic melanoma, almost all patients treated with these targeted inhibitors who achieve an initial response will ultimately progress. Several mechanisms of resistance have been proposed, and most relate to reactivation of the MAPK pathway.50,51 As a result, efforts to maintain suppression of the MAPK pathway have been pursued to delay the onset of resistance. In a phase 2 trial that combined dabrafenib with trametinib, there was a longer PFS than there was with dabrafenib monotherapy.52
Furthermore, the addition of trametinib to dabrafenib reduced the incidence of squamous-cell carcinoma, providing further evidence that reactivation of the MAPK pathway is involved in these hyperproliferative skin lesions arising under BRAF-directed therapy. A higher rate of febrile episodes was seen, however. An ongoing phase 3 study is looking at whether or not combining BRAF and MEK inhibitors results in improved OS compared with single-agent BRAF. It is premature at this juncture to recommend combining dabrafenib and trametinib until the results of the ongoing phase 3 studies more thoroughly describe the risks and benefits of this approach (Table 2).
KIT inhibitors
In a subset of melanomas, particularly those that arise from mucosal, acral, or chronically sun-damaged skin, mutations are found in the receptor-tyrosine kinase KIT.35 A number of agents directed against KIT, such as imatinib, have been tested in clinical trials. Initial phase 2 studies revealed poor RRs with KIT inhibition in molecularly unselected patients.53-55 Subsequent studies selected patients with KIT genetic aberrations, including mutations and amplifications, and some responses were seen.56-58
Importantly, not all KIT genetic aberrations are believed to be considered equal. Preliminarily, it appears that mutations in exon 11 (L576P) and exon 13 (K642E) appear to be most closely associated with response and may be true driver mutations. Other KIT mutations may have less functional significance but additional research is needed. Imatinib is a reasonable therapeutic choice in patients with a KIT mutation, particularly when an L576P or K642E mutation is present.
conclusions
Since 2011, 4 new drugs—ipilimumab, vemurafenib, dabrafenib, and trametinib—have been approved for the treatment of metastatic melanoma. Exciting early data from PD-1 clinical trials suggest that agents that disrupt PD-1 may also become important therapeutic modalities. Future studies will continue to evaluate combinations of these therapeutic modalities, but caution should be exercised in combining these drugs prior to data from ongoing clinical trials revealing the true benefits and risks of combination therapy. Excessive toxicity was seen in an early phase trial when vemurafenib was combined with ipilimumab.59
Additional research will also explore biomarkers that may help clinicians apply immunotherapy to the most appropriate patients and better understand mechanisms of resistance to targeted therapies. Clinical trials of novel agents or combinations should be considered at every treatment juncture to continue the rapid pace of developing the most innovative and tailored treatment approaches.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
This article has been adapted from an article originally published in The Journal of Supportive and Community Oncology (jcso-online.com). Schindler K, Postow M. Current options and future directions in the systemic treatment of metastatic melanoma. J Community Support Oncol. 2014;12(1):20-26.
The incidence of melanoma, a highly aggressive tumor arising from melanocytes, continues to rise by about 3% a year in the U.S. with about 76,000 patients being diagnosed every year and 9,000 patients dying of the disease.1 Complete surgical resection is the standard for localized melanoma, with surgical excision margins depending on tumor thickness. For patients with involved sentinel lymph nodes, complete lymphadenectomy is typically recommended, although the benefits of completion lymphadenectomy are being evaluated in an ongoing randomized trial.2,3
For patients with surgically resected, high-risk melanoma, the only approved adjuvant therapy is interferon-a (IFN-a).4 Use of IFN-a, however, remains controversial because of the associated adverse effects (AEs) and controversial effects on overall survival (OS).5,6 Unfortunately, many patients with localized disease will ultimately experience a recurrence, and the prognosis of patients with metastatic disease is poor with a historical 5-year survival rate of 10%.7
Chemotherapy and interleukin 2
For more than 3 decades, conventional cytotoxic chemotherapy was used to treat metastatic melanoma. Typical agents included alkylating agents (dacarbazine, temozolomide, nitrosoureas), platinum analogs (cisplatin and carboplatin), and microtubular toxins (vinblastine and paclitaxel). Despite the clinical use and investigation of a number of these chemotherapies for patients with metastatic melanoma, the only treatment approved by the FDA is dacarbazine, which is administered intravenously every 3 to 4 weeks at a dose of 800 to 1,000 mg/m2.
Monotherapy with dacarbazine is generally well tolerated with only mild AEs such as nausea, myelosuppression, and fatigue. In a pooled analysis, the overall response rate (RR) for dacarbazine was approximately 9%.8 Temozolomide, the oral analog of dacarbazine, penetrates into the central nervous system and has been compared with dacarbazine in randomized trials. These agents are believed to have similar efficacy, but temozolomide has been associated with a higher rate of lymphopenia.9,10
Investigation of chemotherapy combinations such as cisplatin, vinblastine, and dacarbazine or carboplatin and paclitaxel have shown promising RRs but unfortunately no prolongation of OS compared with single-agent dacarbazine.11-13 Despite its modest efficacy, chemotherapy still has a place in the palliative treatment for some patients.
In addition to dacarbazine, the immunotherapeutic strategy, high-dose recombinant interleukin-2 (IL-2), had also been a mainstay treatment for advanced melanoma for many years. IL-2 is administered as an IV infusion every 8 hours at a dose of 600,000 to 720,000 IU/kg on days 1 to 5 and days 15 to 19, with a maximum of 14 such biphasic cycles. Because of the significant acute toxicity profile, including capillary leak syndrome, cardiovascular complications, and seizures, IL-2 treatment requires hospitalization and is generally only performed at specialized centers for patients with good performance status. Though the overall RR in pooled analysis was low at 16%, the durability of responses in some responders that appeared to last many years led to the FDA approval of IL-2 in 1998.14,15
IL-2 continues to be investigated. In a randomized trial, an improved RR and progression-free survival (PFS) were seen when IL-2 was combined with the glycoprotein 100 (gp100) peptide vaccine compared with IL-2 alone.16 Other approaches have sought to improve the safety of IL-2 by selectively delivering it to tumor sites. The fusion protein L19-IL2 couples IL-2 with the recombinant human vascular targeting antibody L19 and has preliminarily been shown to be safe in phase 1 evaluation and in combination with dacarbazine.17,18
Antibodies that block immunologic checkpoints
Melanoma has long been recognized as an immunogenic malignancy but the efficacy of immunotherapeutic strategies has generally been modest. The precise etiology of why immunotherapy historically was not more successful is not completely understood, but it is possible that patients with advanced malignancy have predominant immune inhibitory circuits that prevent otherwise effective antitumor immune responses.
In recent years, research has illuminated some of these immunologic inhibitory elements, termed “immunologic checkpoints,” which include cytotoxic T-lymphocyte antigen 4 (CTLA-4) and programmed death-1 (PD-1). Antibodies that target these checkpoints have resulted in durable responses in some patients and a unique pattern of immune-mediated AEs. Though an ongoing area of research, no pre- or on-treatment biomarkers have been sufficiently validated to enable specific patient selection for these therapies.
Antibodies Blocking CTLA-4
CTLA-4 is expressed on activated T cells and typically functions as a negative regulator of T-cell activity preserving normal immunologic homeostasis. Blocking CTLA-4 with therapeutic antibodies such as ipilimumab and tremelimumab prevents normal CTLA-4–mediated T-cell downregulation and thereby enhances the ability of T cells to exert their full antitumor immune effects (Figure 1). Ipilimumab was the first drug in the management of metastatic melanoma to show an improvement in OS in phase 3 studies, and although a phase 3 study of tremelimumab did not demonstrate an improvement in OS, durable responses were similarly seen.19-21
The first phase 3 trial investigating ipilimumab randomized previously pretreated patients with advanced melanoma to ipilimumab at a dose of 3 mg/kg with or without the gp100 peptide vaccine. The median OS was 10.0 months among patients receiving ipilimumab plus gp100, compared with 6.4 months among patients receiving gp100 alone. There was no difference in OS between the ipilimumab groups.19 The outcome of this study has led to the approval of ipilimumab at a dose of 3 mg/kg in patients with advanced melanoma by regulatory agencies in the U.S., European Union, and Australia.
For treatment-naive patients, a second phase 3 trial investigating dacarbazine in combination with ipilimumab compared with dacarbazine in combination with placebo also demonstrated improvement of OS in patients treated with dacarbazine in combination with ipilimumab.20 The estimated 1-year, 2-year, and 3-year survival rates were 47.3%, 28.5%, and 20.8%, respectively, in the dacarbazine plus ipilimumab group, compared with 36.3%, 17.9%, and 12.2% in the dacarbazine alone group. This second trial used a higher dose of ipilimumab (10 mg/kg) and though it confirmed ipilimumab’s beneficial effects on OS, ipilimumab is not approved at 10 mg/kg and is not routinely recommended to be used in combination with dacarbazine given hepatic toxicity concerns.
Though the median OS was improved in these phase 3 trials, perhaps the greatest activity of ipilimumab lies in the increased number of patients who can achieve long-term OS. In a recently published updated survival analysis, the 4-year survival rates for previously treated patients who received ipilimumab at 3 or 10 mg/kg were 18.2% and 19.7% to 28.4%. For treatment-naive patients receiving ipilimumab at 10 mg/kg, 4-year survival rates were between 37.7% and 49.5%.22 These values appear superior to historical data from prior chemotherapy trials.
An important consideration in the clinical use of CTLA-4 blocking antibodies is the possible occurrence of toxicities that differ from those associated with traditional chemotherapy. These AEs are termed immune-related AEs (irAEs), and they most commonly manifest as diarrhea, dermatitis, hepatitis, and endocrinopathies but less commonly can involve other organs, resulting in uveitis, nephritis, myopathy, and neuropathy.
In general, the onset of irAEs follows a certain pattern with cutaneous manifestations often presenting early in treatment, followed by gastrointestinal and hepatic events occurring about 2 months into therapy and endocrinopathies appearing even later.23 In rare cases, severe AEs (eg, perforating colitis, toxic epidermal necrolysis) can occur and may require hospitalization.24
Clinicians must be attentive to early signs of these AEs and promptly initiate immunosuppression with steroids or other immunosuppressive medications, which do not appear to diminish the antitumor immune effects.25 Established management algorithms exist to guide clinicians. Given the occasional need for immunosuppression in this patient population, awareness of the possibility of opportunistic or rare infections is also important.
In phase 3 evaluation, the number of patients who had long-term survival exceeded the number of patients who had a classically defined disease response to treatment. Durable stable disease and late responses have been observed clinically and may be responsible for some of the beneficial outcomes.26 If patients are asymptomatic and have minimal radiographic progression, it is reasonable to repeat imaging 1 to 2 months later to confirm progression before considering additional lines of therapy.
Antibodies Blocking the Programmed Death-1 Axis
Programmed death-1 (PD-1) is a receptor on the surface of T cells that is upregulated at later stages of T-cell activation as opposed to the early upregulation of CTLA-4. Normally, engagement of PD-1 attenuates T-cell activity at several phases of an immune response. Tumors are believed to escape immune attack by similarly inhibiting T-cell activity by upregulating one of the ligands of PD-1, PD-L1.27,28 Several antibodies that inhibit PD-1 activity, either by blocking the PD-1 molecule itself or PD-L1, are demonstrating significant promise in ongoing clinical trials.
Nivolumab (previously, BMS-936558) is a fully human monoclonal antibody targeting PD-1. In a large phase 1 study in patients with a variety of malignancies, nivolumab demonstrated a 31% RR in patients with advanced melanoma.29 Subsequent follow-up data indicates these responses are generally durable with a median duration of response of 24 months and a 3-year OS rate of 40%.30 Adverse effects of nivolumab appear less frequently than with CTLA-4 blockade but have included vitiligo, colitis, hepatitis, hypophysitis, and thyroiditis. Unique to PD-1 blockade appears to be the AE of an inflammatory pneumonitis, which can present with a dry cough, dyspnea, and ground-glass opacities and can be potentially lethal.29
On the basis of complementary regulatory roles of CTLA-4 and PD-1 checkpoint inhibition, a trial investigating combined nivolumab and ipilimumab was completed. In the small group of patients treated, a high RR was seen with a generally acceptable safety profile.31 Ongoing phase 2 and 3 trials are assessing nivolumab alone and in combination with other agents for the treatment of advanced melanoma and other malignancies (Table 1).
Another PD-1 blocking antibody, MK-3475, has been evaluated in patients with advanced melanoma, and promising RRs have been described.32 In a small group of patients, the confirmed RR at a dose of 10 mg/kg every 2 weeks was 52% and appeared similar in patients who had and who had not been previously treated with ipilimumab. The AEs of MK-3475 seem to resemble nivolumab. MK-3475 is similarly being evaluated in large phase 2 and 3 trials for both patients with melanoma and additional malignancies.
In addition to antibodies targeting PD-1, clinical activity has also been observed with several different antibodies (BMS-936559, MPDL3280A, and MEDI4736) that target PD-L1. Though some data have been published for this therapeutic strategy,33 ongoing trials will continue to clarify the role of targeting PD-L1 in patients with advanced melanoma.
Targeted Therapies That Block Oncogenic Signaling Pathways
The mitogen-activated protein kinase (MAPK) pathway responds to extracellular growth signals and regulates cell proliferation and survival. In many patients with melanoma, the MAPK pathway is constitutively activated as a result of molecular alterations in genes encoding key regulators or components of the pathway such as BRAF, NRAS, and KIT.34,35 The most common mutation arising in melanoma is the BRAF mutation, occurring in nearly half of melanomas, and typically involves a missense mutation in which glutamic acid is substituted for valine at codon 600 (BRAF V600E mutation).36 Less frequent BRAF mutations include V600K, V600R, and K601E.37 Strategies that directly inhibit oncogenic BRAF or disable downstream elements such as MEK have recently shown dramatic results in patients with melanoma (Figure 2).
BRAF inhibitors
Vemurafenib is a potent inhibitor of mutated BRAF with marked antitumor effects against melanoma cell lines with the BRAF V600E mutation.38 The first striking results of tumor regression with this strategy in patients were seen in a phase 1 study in patients with melanoma characterized by a BRAF V600E mutation but not in patients whose melanomas did not have a BRAF mutation.39
Subsequent phase 3 trials confirmed the high RRs of this agent in patients with BRAF-mutant melanoma and demonstrated superiority in OS compared with dacarbazine chemotherapy.40 The results of this phase 3 trial led to the approval of vemurafenib by the FDA in August 2011 with treatment exclusively limited to patients with BRAF mutant melanoma. Updated OS data from this phase 3 study revealed a median OS of 13.2 months for vemurafenib, compared with 9.6 months for dacarbazine, with an overall RR in patients treated with vemurafenib of 57% and a median PFS of 6.9 months.41 General AEs with vemurafenib include arthralgia, fatigue, aminotransferase elevations, nausea and vomiting, and decreased kidney function. In general, toxicities are manageable with dose reduction or temporary drug cessation.
One characteristic of vemurafenib and other BRAF-targeted agents is the frequent development of hyperproliferative skin AEs. Skin lesions, including follicular and palmo-plantar hyperkeratosis, papillomas, and also cutaneous squamous-cell carcinomas and keratoacanthomas, have commonly been observed under treatment with vemurafenib, and close evaluation by a dermatologist is important.42 The mechanism of this phenomenon is believed to be a paradoxical activation of the MAPK pathway in nonmelanoma BRAF wild-type cells when systemic treatment with a BRAF inhibitor is administered.43
The phenomenon of hyperproliferation of non–BRAF-mutant tissues with ongoing BRAF-inhibitor therapy has also been seen in patients with lymphoproliferative disorders and may be a mechanism involved in the discovery that patients have a high rate of new primary melanomas while on therapy.44,45 These findings warrant special attention, particularly as BRAF inhibitors are undergoing evaluation as adjuvant therapy.
Another active BRAF kinase inhibitor with a similar efficacy profile as vemurafenib is dabrafenib, which was approved in May 2013 based on the demonstration of improved PFS in a phase 3 trial comparing dabrafenib 150 mg orally twice daily and dacarbazine 1,000 mg/m2 intravenously once every 3 weeks in previously untreated patients with BRAF V600E mutant melanoma. The median PFS times were 5.1 and 2.7 months in the dabrafenib and dacarbazine arms, respectively, with an objective RR of 52% in patients treated with dabrafenib.46 Follow-up time was too short to make a determination of the impact of dabrafenib on OS. In a separate study, dabrafenib was also shown to be effective for patients with brain metastases and remains an excellent therapeutic choice for this particular patient population.47
Generally, dabrafenib is believed to have similar efficacy to vemurafenib. Nevertheless, EAs with of dabrafenib differ somewhat from those observed with vemurafenib: The rate of proliferative skin lesions, including squamous cell carcinomas and keratoacanthomas appears to be lower for dabrafenib than vemurafenib. However, AEs particular to dabrafenib have been seen such as pyrexia, which were recorded in about 11% of patients.46
MEK inhibitors
Though targeting oncogenic BRAF directly has been incredibly successful for patients with BRAF-mutant metastatic melanoma, additional success has been observed by blocking the MAPK pathway at a downstream component, MEK. Trametinib is an MEK inhibitor that was approved by the FDA in June 2013 as a single agent for patients with BRAF V600E or V600K mutant melanoma. Trametinib is administered at a dose of 2 mg once daily and was shown to improve PFS and OS compared with dacarbazine and paclitaxel chemotherapies.47 Despite the improvement in PFS and OS compared with chemotherapy, the objective RR for trametinib was somewhat lower (22%) than that seen with BRAF inhibitors.
Trametinib also is associated with a different AE profile from BRAF inhibitors and includes diarrhea, peripheral edema, hypertension, and fatigue, typical of other MEK inhibitors as well.48 Asymptomatic and reversible reduction of the cardiac ejection fraction and ocular toxic effects also occur infrequently. Unlike with BRAF-inhibitor treatment, the development of cutaneous squamous-cell carcinomas or other hyperproliferative skin lesions was not noted.49
Despite the significant benefits of targeted therapy disrupting overly active MAPK signaling in patients with BRAF-mutant metastatic melanoma, almost all patients treated with these targeted inhibitors who achieve an initial response will ultimately progress. Several mechanisms of resistance have been proposed, and most relate to reactivation of the MAPK pathway.50,51 As a result, efforts to maintain suppression of the MAPK pathway have been pursued to delay the onset of resistance. In a phase 2 trial that combined dabrafenib with trametinib, there was a longer PFS than there was with dabrafenib monotherapy.52
Furthermore, the addition of trametinib to dabrafenib reduced the incidence of squamous-cell carcinoma, providing further evidence that reactivation of the MAPK pathway is involved in these hyperproliferative skin lesions arising under BRAF-directed therapy. A higher rate of febrile episodes was seen, however. An ongoing phase 3 study is looking at whether or not combining BRAF and MEK inhibitors results in improved OS compared with single-agent BRAF. It is premature at this juncture to recommend combining dabrafenib and trametinib until the results of the ongoing phase 3 studies more thoroughly describe the risks and benefits of this approach (Table 2).
KIT inhibitors
In a subset of melanomas, particularly those that arise from mucosal, acral, or chronically sun-damaged skin, mutations are found in the receptor-tyrosine kinase KIT.35 A number of agents directed against KIT, such as imatinib, have been tested in clinical trials. Initial phase 2 studies revealed poor RRs with KIT inhibition in molecularly unselected patients.53-55 Subsequent studies selected patients with KIT genetic aberrations, including mutations and amplifications, and some responses were seen.56-58
Importantly, not all KIT genetic aberrations are believed to be considered equal. Preliminarily, it appears that mutations in exon 11 (L576P) and exon 13 (K642E) appear to be most closely associated with response and may be true driver mutations. Other KIT mutations may have less functional significance but additional research is needed. Imatinib is a reasonable therapeutic choice in patients with a KIT mutation, particularly when an L576P or K642E mutation is present.
conclusions
Since 2011, 4 new drugs—ipilimumab, vemurafenib, dabrafenib, and trametinib—have been approved for the treatment of metastatic melanoma. Exciting early data from PD-1 clinical trials suggest that agents that disrupt PD-1 may also become important therapeutic modalities. Future studies will continue to evaluate combinations of these therapeutic modalities, but caution should be exercised in combining these drugs prior to data from ongoing clinical trials revealing the true benefits and risks of combination therapy. Excessive toxicity was seen in an early phase trial when vemurafenib was combined with ipilimumab.59
Additional research will also explore biomarkers that may help clinicians apply immunotherapy to the most appropriate patients and better understand mechanisms of resistance to targeted therapies. Clinical trials of novel agents or combinations should be considered at every treatment juncture to continue the rapid pace of developing the most innovative and tailored treatment approaches.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10-29.
2. Garbe C, Peris K, Hauschild A, et al; European Dermatology Forum, European Association of Dermato-Oncology, European Organization of Research and Treatment of Cancer. Diagnosis and treatment of melanoma. European consensus-based interdisciplinary guideline—Update 2012. Eur J Cancer. 2012;48(15):2375-2390.
3. Coit DG, Andtbacka R, Bichakjian CK, et al; NCCN Melanoma Panel. Melanoma. J Natl Compr Canc Netw. 2009;7(3):250-275.
4. Molife R, Hancock BW. Adjuvant therapy of malignant melanoma. Crit Rev Oncol Hematol. 2002;44(1):81-102.
5. Wheatley K, Ives N, Hancock B, Gore M, Eggermont A, Suciu S. Does adjuvant interferon-alpha for high-risk melanoma provide a worthwhile benefit? A meta-analysis of the randomised trials. Cancer Treat Rev. 2003;29(4):241-252.
6. Mocellin S, Pasquali S, Rossi CR, Nitti D. Interferon alpha adjuvant therapy in patients with high-risk melanoma: A systematic review and meta-analysis. J Natl Cancer Inst. 2010;102(7):493-501.
7. Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27(36):6199-6206.
8. Luke JJ, Rubinstein LV, Smith GL, Ivy SP, Harris PJ. Similar efficacy for phase I trials in comparison with DTIC for advanced malignant melanoma: an analysis of melanoma outcomes in CTEP-sponsored phase I trials 1995-2011. Melanoma Res. 2013;23(2):152-158.
9. Middleton MR, Grob JJ, Aaronson N, et al. Randomized phase III study of temozolomide versus dacarbazine in the treatment of patients with advanced metastatic malignant melanoma. J Clin Oncol. 2000;18(1):158-166.
10. Teimouri F, Nikfar S, Abdollahi M. Efficacy and side effects of dacarbazine in comparison with temozolomide in the treatment of malignant melanoma: A meta-analysis consisting of 1314 patients. Melanoma Res. 2013;23(5):381-389.
11. Chapman PB, Einhorn LH, Meyers ML, et al. Phase III multicenter randomized trial of the Dartmouth regimen versus dacarbazine in patients with metastatic melanoma. J Clin Oncol. 1999;17(9):2745-2751.
12. Legha SS, Ring S, Papadopoulos N, Plager C, Chawla S, Benjamin R. A prospective evaluation of a triple-drug regimen containing cisplatin, vinblastine, and dacarbazine (CVD) for metastatic melanoma. Cancer. 1989;64(10):2024-2029.
13. Rao RD, Holtan SG, Ingle JN, et al. Combination of paclitaxel and carboplatin as second-line therapy for patients with metastatic melanoma. Cancer. 2006;106(2):375-382.
14. Atkins MB, Kunkel L, Sznol M, Rosenberg SA. High-dose recombinant interleukin-2 therapy in patients with metastatic melanoma: Long-term survival update. Cancer J Sci Am. 2000;6(suppl 1):S11-S14.
15. Atkins MB, Lotze MT, Dutcher JP, et al. High-dose recombinant interleukin 2 therapy for patients with metastatic melanoma: Analysis of 270 patients treated between 1985 and 1993. J Clin Oncol. 1999;17(7):2105-2116.
16. Schwartzentruber DJ, Lawson DH, Richards JM, et al. gp100 peptide vaccine and interleukin-2 in patients with advanced melanoma. N Engl J Med. 2011;364(22):2119-2127.
17. Johannsen M, Spitaleri G, Curigliano G, et al. The tumour-targeting human L19-IL2 immunocytokine: Preclinical safety studies, phase I clinical trial in patients with solid tumours and expansion into patients with advanced renal cell carcinoma. Eur J Cancer. 2010;46(16):2926-2935.
18. Eigentler TK, Weide B, de Braud F, et al. A dose-escalation and signal-generating study of the immunocytokine L19-IL2 in combination with dacarbazine for the therapy of patients with metastatic melanoma. Clin Cancer Res. 2011;17(24):7732-7742.
19. Hodi FS, O'Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711-723.
20. Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364(26):2517-2526.
21. Ribas A, Kefford R, Marshall MA, et al. Phase III randomized clinical trial comparing tremelimumab with standard-of-care chemotherapy in patients with advanced melanoma. J Clin Oncol. 2013;31(5):616-622.
22. Wolchok JD, Weber JS, Maio M, et al. Four-year survival rates for patients with metastatic melanoma who received ipilimumab in phase II clinical trials. Ann Oncol. 2013;24(8):2174-2180.
23. Weber JS, Kähler KC, Hauschild A. Management of immune-related adverse events and kinetics of response with ipilimumab. J Clin Oncol. 2012;30(21):2691-2697.
24. Di Giacomo AM, Biagioli M, Maio M. The emerging toxicity profiles of anti-CTLA-4 antibodies across clinical indications. Semin Oncol. 2010;37(5):499-507.
25. Harmankaya K, Erasim C, Koelblinger C, et al. Continuous systemic corticosteroids do not affect the ongoing regression of metastatic melanoma for more than two years following ipilimumab therapy. Med Oncol. 2011;28(4):1140-1144.
26. Wolchok JD, Hoos A, O’Day S, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: Immune-related response criteria. Clin Cancer Res. 2009;15(23):7412-7420.
27. Zou W, Chen L. Inhibitory B7-family molecules in the tumour microenvironment. Nat Rev Immunol. 2008;8(6):467-477.
28. Keir ME, Liang SC, Guleria I, et al. Tissue expression of PD-L1 mediates peripheral T cell tolerance. J Exp Med. 2006;203(4):883-895.
29. Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443-2454.
30. Sznol M, Kluger HM, Hodi FS, et al. Survival and long-term follow-up of safety and response in patients (pts) with advanced melanoma (MEL) in a phase I trial of nivolumab (anti-PD-1; BMS-936558; ONO-4538) [ASCO abstract CRA9006]. ASCO Meet Abstr. 2013;31(18_suppl):CRA9006. http://meetinglibrary.asco.org/content/80822. Accessed July 23, 2014.
31. Wolchok JD, Kluger H, Callahan MK, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369(2):122-133.
32. Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369(2):134-144.
33. Brahmer JR, Tykodi SS, Chow LQ, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455-2465.
34. McCubrey JA, Steelman LS, Chappell WH, et al. Roles of the Raf/MEK/ERK pathway in cell growth, malignant transformation and drug resistance.
Biochim Biophys Acta. 2007;1773(8):1263-1284.
35. Curtin JA, Busam K, Pinkel D, Bastian BC. Somatic activation of KIT in distinct subtypes of melanoma. J Clin Oncol. 2006;24(26):4340-4346.
36. Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949-954.
37. Long GV, Menzies AM, Nagrial AM, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29(10):1239-1246.
38. Bollag G, Hirth P, Tsai J, et al. Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma. Nature. 2010;467(7315):596-599.
39. Flaherty KT, Puzanov I, Kim KB, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010;363(9):809-819.
40. Chapman PB, Hauschild A, Robert C, et al; BRIM-3 Study Group. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364(26):2507-2516.
41. Chapman PB, Hauschild A, Robert C, et al. Updated overall survival (OS) results for BRIM-3, a phase III randomized, open-label, multicenter trial comparing BRAF inhibitor vemurafenib (vem) with dacarbazine (DTIC) in previously untreated patients with BRAF(V600E)-mutated melanoma [ASCO abstract 8502]. ASCO Meet Abstr. 2012;30(15_suppl):8502. http://meetinglibrary.asco.org/content/70533?media=vm. Accessed July 23, 2014.
42. Lacouture ME, O’Reilly K, Rosen N, Solit DB. Induction of cutaneous squamous cell carcinomas by RAF inhibitors: Cause for concern? J Clin Oncol. 2012;30(3):329-330.
43. Su F, Viros A, Milagre C, et al. RAS mutations in cutaneous squamous-cell carcinomas in patients treated with BRAF inhibitors. New Engl J Med. 2012;366(3):207-215.
44. Callahan MK, Rampal R, Harding JJ, et al. Progression of RAS-mutant leukemia during RAF inhibitor treatment. New Engl J Med. 2012;367(24):2316-2321.
45. Zimmer L, Hillen U, Livingstone E, et al. Atypical melanocytic proliferations and new primary melanomas in patients with advanced melanoma undergoing selective BRAF inhibition. J Clin Oncol. 2012;30(19):2375-2383.
46. Hauschild A, Grob JJ, Demidov LV, et al. Dabrafenib in BRAF-mutated metastatic melanoma: A multicentre, open-label phase 3 randomised clinical trial. Lancet 2012;380(9839):358-365.
47. Long GV, Trefzer U, Davies MA, et al. Dabrafenib in patients with Val600Glu or Val600Lys BRAF-mutant melanoma metastatic to the brain (BREAK-MB): A multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13(11):1087-1095.
48. Kirkwood JM, Bastholt L, Robert C, et al. Phase II, open-label, randomized trial of the MEK1/2 inhibitor selumetinib as monotherapy versus temozolomide in patients with advanced melanoma. Clin Cancer Res. 2012;18(2):555-567.
49. Flaherty KT, Robert C, Hersey P, et al; METRIC Study Group. Improved survival with MEK inhibition in BRAF-mutated melanoma. New Engl J Med. 2012;367(2):107-114.
50. Poulikakos PI, Persaud Y, Janakiraman M, et al. RAF inhibitor resistance is mediated by dimerization of aberrantly spliced BRAF(V600E). Nature. 2011;480(7377):387-390.
51. Nazarian R, Shi H, Wang Q, et al. Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature. 2010;468(7326):973-977.
52. Flaherty KT, Infante JR, Daud A, et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. New Engl J Med. 2012;367(18):1694-1703.
53. Ugurel S, Hildenbrand R, Zimpfer A, et al. Lack of clinical efficacy of imatinib in metastatic melanoma. Br J Cancer. 2005;9(8):1398-1405.
54. Wyman K, Atkins MB, Prieto V, et al. Multicenter Phase II trial of high-dose imatinib mesylate in metastatic melanoma: Significant toxicity with no clinical efficacy. Cancer. 2006;106(9):2005-2011.
55. Kim KB, Eton O, Davis DW, et al. Phase II trial of imatinib mesylate in patients with metastatic melanoma. Br J Cancer. 2008;99(5):734-740.
56. Carvajal RD, Antonescu CR, Wolchok JD, et al. KIT as a therapeutic target in metastatic melanoma. JAMA. 2011;305(22):2327-2334.
57. Hodi FS, Corless CL, Giobbie-Hurder A, et al. Imatinib for melanomas harboring mutationally activated or amplified KIT arising on mucosal, acral, and chronically sun-damaged skin. J Clin Oncol. 2013;31(26):3182-3190.
58. Guo J, Si L, Kong Y, et al. Phase II, open-label, single-arm trial of imatinib mesylate in patients with metastatic melanoma harboring c-Kit mutation or amplification. J Clin Oncol. 2011;29(21):2904-2909.
59. Ribas A, Hodi FS, Callahan M, et al. Hepatotoxicity with combination of vemurafenib and ipilimumab. N Engl J Med. 2013;368(14):1365-1366.
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10-29.
2. Garbe C, Peris K, Hauschild A, et al; European Dermatology Forum, European Association of Dermato-Oncology, European Organization of Research and Treatment of Cancer. Diagnosis and treatment of melanoma. European consensus-based interdisciplinary guideline—Update 2012. Eur J Cancer. 2012;48(15):2375-2390.
3. Coit DG, Andtbacka R, Bichakjian CK, et al; NCCN Melanoma Panel. Melanoma. J Natl Compr Canc Netw. 2009;7(3):250-275.
4. Molife R, Hancock BW. Adjuvant therapy of malignant melanoma. Crit Rev Oncol Hematol. 2002;44(1):81-102.
5. Wheatley K, Ives N, Hancock B, Gore M, Eggermont A, Suciu S. Does adjuvant interferon-alpha for high-risk melanoma provide a worthwhile benefit? A meta-analysis of the randomised trials. Cancer Treat Rev. 2003;29(4):241-252.
6. Mocellin S, Pasquali S, Rossi CR, Nitti D. Interferon alpha adjuvant therapy in patients with high-risk melanoma: A systematic review and meta-analysis. J Natl Cancer Inst. 2010;102(7):493-501.
7. Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27(36):6199-6206.
8. Luke JJ, Rubinstein LV, Smith GL, Ivy SP, Harris PJ. Similar efficacy for phase I trials in comparison with DTIC for advanced malignant melanoma: an analysis of melanoma outcomes in CTEP-sponsored phase I trials 1995-2011. Melanoma Res. 2013;23(2):152-158.
9. Middleton MR, Grob JJ, Aaronson N, et al. Randomized phase III study of temozolomide versus dacarbazine in the treatment of patients with advanced metastatic malignant melanoma. J Clin Oncol. 2000;18(1):158-166.
10. Teimouri F, Nikfar S, Abdollahi M. Efficacy and side effects of dacarbazine in comparison with temozolomide in the treatment of malignant melanoma: A meta-analysis consisting of 1314 patients. Melanoma Res. 2013;23(5):381-389.
11. Chapman PB, Einhorn LH, Meyers ML, et al. Phase III multicenter randomized trial of the Dartmouth regimen versus dacarbazine in patients with metastatic melanoma. J Clin Oncol. 1999;17(9):2745-2751.
12. Legha SS, Ring S, Papadopoulos N, Plager C, Chawla S, Benjamin R. A prospective evaluation of a triple-drug regimen containing cisplatin, vinblastine, and dacarbazine (CVD) for metastatic melanoma. Cancer. 1989;64(10):2024-2029.
13. Rao RD, Holtan SG, Ingle JN, et al. Combination of paclitaxel and carboplatin as second-line therapy for patients with metastatic melanoma. Cancer. 2006;106(2):375-382.
14. Atkins MB, Kunkel L, Sznol M, Rosenberg SA. High-dose recombinant interleukin-2 therapy in patients with metastatic melanoma: Long-term survival update. Cancer J Sci Am. 2000;6(suppl 1):S11-S14.
15. Atkins MB, Lotze MT, Dutcher JP, et al. High-dose recombinant interleukin 2 therapy for patients with metastatic melanoma: Analysis of 270 patients treated between 1985 and 1993. J Clin Oncol. 1999;17(7):2105-2116.
16. Schwartzentruber DJ, Lawson DH, Richards JM, et al. gp100 peptide vaccine and interleukin-2 in patients with advanced melanoma. N Engl J Med. 2011;364(22):2119-2127.
17. Johannsen M, Spitaleri G, Curigliano G, et al. The tumour-targeting human L19-IL2 immunocytokine: Preclinical safety studies, phase I clinical trial in patients with solid tumours and expansion into patients with advanced renal cell carcinoma. Eur J Cancer. 2010;46(16):2926-2935.
18. Eigentler TK, Weide B, de Braud F, et al. A dose-escalation and signal-generating study of the immunocytokine L19-IL2 in combination with dacarbazine for the therapy of patients with metastatic melanoma. Clin Cancer Res. 2011;17(24):7732-7742.
19. Hodi FS, O'Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711-723.
20. Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364(26):2517-2526.
21. Ribas A, Kefford R, Marshall MA, et al. Phase III randomized clinical trial comparing tremelimumab with standard-of-care chemotherapy in patients with advanced melanoma. J Clin Oncol. 2013;31(5):616-622.
22. Wolchok JD, Weber JS, Maio M, et al. Four-year survival rates for patients with metastatic melanoma who received ipilimumab in phase II clinical trials. Ann Oncol. 2013;24(8):2174-2180.
23. Weber JS, Kähler KC, Hauschild A. Management of immune-related adverse events and kinetics of response with ipilimumab. J Clin Oncol. 2012;30(21):2691-2697.
24. Di Giacomo AM, Biagioli M, Maio M. The emerging toxicity profiles of anti-CTLA-4 antibodies across clinical indications. Semin Oncol. 2010;37(5):499-507.
25. Harmankaya K, Erasim C, Koelblinger C, et al. Continuous systemic corticosteroids do not affect the ongoing regression of metastatic melanoma for more than two years following ipilimumab therapy. Med Oncol. 2011;28(4):1140-1144.
26. Wolchok JD, Hoos A, O’Day S, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: Immune-related response criteria. Clin Cancer Res. 2009;15(23):7412-7420.
27. Zou W, Chen L. Inhibitory B7-family molecules in the tumour microenvironment. Nat Rev Immunol. 2008;8(6):467-477.
28. Keir ME, Liang SC, Guleria I, et al. Tissue expression of PD-L1 mediates peripheral T cell tolerance. J Exp Med. 2006;203(4):883-895.
29. Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443-2454.
30. Sznol M, Kluger HM, Hodi FS, et al. Survival and long-term follow-up of safety and response in patients (pts) with advanced melanoma (MEL) in a phase I trial of nivolumab (anti-PD-1; BMS-936558; ONO-4538) [ASCO abstract CRA9006]. ASCO Meet Abstr. 2013;31(18_suppl):CRA9006. http://meetinglibrary.asco.org/content/80822. Accessed July 23, 2014.
31. Wolchok JD, Kluger H, Callahan MK, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369(2):122-133.
32. Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369(2):134-144.
33. Brahmer JR, Tykodi SS, Chow LQ, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455-2465.
34. McCubrey JA, Steelman LS, Chappell WH, et al. Roles of the Raf/MEK/ERK pathway in cell growth, malignant transformation and drug resistance.
Biochim Biophys Acta. 2007;1773(8):1263-1284.
35. Curtin JA, Busam K, Pinkel D, Bastian BC. Somatic activation of KIT in distinct subtypes of melanoma. J Clin Oncol. 2006;24(26):4340-4346.
36. Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949-954.
37. Long GV, Menzies AM, Nagrial AM, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29(10):1239-1246.
38. Bollag G, Hirth P, Tsai J, et al. Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma. Nature. 2010;467(7315):596-599.
39. Flaherty KT, Puzanov I, Kim KB, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010;363(9):809-819.
40. Chapman PB, Hauschild A, Robert C, et al; BRIM-3 Study Group. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364(26):2507-2516.
41. Chapman PB, Hauschild A, Robert C, et al. Updated overall survival (OS) results for BRIM-3, a phase III randomized, open-label, multicenter trial comparing BRAF inhibitor vemurafenib (vem) with dacarbazine (DTIC) in previously untreated patients with BRAF(V600E)-mutated melanoma [ASCO abstract 8502]. ASCO Meet Abstr. 2012;30(15_suppl):8502. http://meetinglibrary.asco.org/content/70533?media=vm. Accessed July 23, 2014.
42. Lacouture ME, O’Reilly K, Rosen N, Solit DB. Induction of cutaneous squamous cell carcinomas by RAF inhibitors: Cause for concern? J Clin Oncol. 2012;30(3):329-330.
43. Su F, Viros A, Milagre C, et al. RAS mutations in cutaneous squamous-cell carcinomas in patients treated with BRAF inhibitors. New Engl J Med. 2012;366(3):207-215.
44. Callahan MK, Rampal R, Harding JJ, et al. Progression of RAS-mutant leukemia during RAF inhibitor treatment. New Engl J Med. 2012;367(24):2316-2321.
45. Zimmer L, Hillen U, Livingstone E, et al. Atypical melanocytic proliferations and new primary melanomas in patients with advanced melanoma undergoing selective BRAF inhibition. J Clin Oncol. 2012;30(19):2375-2383.
46. Hauschild A, Grob JJ, Demidov LV, et al. Dabrafenib in BRAF-mutated metastatic melanoma: A multicentre, open-label phase 3 randomised clinical trial. Lancet 2012;380(9839):358-365.
47. Long GV, Trefzer U, Davies MA, et al. Dabrafenib in patients with Val600Glu or Val600Lys BRAF-mutant melanoma metastatic to the brain (BREAK-MB): A multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13(11):1087-1095.
48. Kirkwood JM, Bastholt L, Robert C, et al. Phase II, open-label, randomized trial of the MEK1/2 inhibitor selumetinib as monotherapy versus temozolomide in patients with advanced melanoma. Clin Cancer Res. 2012;18(2):555-567.
49. Flaherty KT, Robert C, Hersey P, et al; METRIC Study Group. Improved survival with MEK inhibition in BRAF-mutated melanoma. New Engl J Med. 2012;367(2):107-114.
50. Poulikakos PI, Persaud Y, Janakiraman M, et al. RAF inhibitor resistance is mediated by dimerization of aberrantly spliced BRAF(V600E). Nature. 2011;480(7377):387-390.
51. Nazarian R, Shi H, Wang Q, et al. Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature. 2010;468(7326):973-977.
52. Flaherty KT, Infante JR, Daud A, et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. New Engl J Med. 2012;367(18):1694-1703.
53. Ugurel S, Hildenbrand R, Zimpfer A, et al. Lack of clinical efficacy of imatinib in metastatic melanoma. Br J Cancer. 2005;9(8):1398-1405.
54. Wyman K, Atkins MB, Prieto V, et al. Multicenter Phase II trial of high-dose imatinib mesylate in metastatic melanoma: Significant toxicity with no clinical efficacy. Cancer. 2006;106(9):2005-2011.
55. Kim KB, Eton O, Davis DW, et al. Phase II trial of imatinib mesylate in patients with metastatic melanoma. Br J Cancer. 2008;99(5):734-740.
56. Carvajal RD, Antonescu CR, Wolchok JD, et al. KIT as a therapeutic target in metastatic melanoma. JAMA. 2011;305(22):2327-2334.
57. Hodi FS, Corless CL, Giobbie-Hurder A, et al. Imatinib for melanomas harboring mutationally activated or amplified KIT arising on mucosal, acral, and chronically sun-damaged skin. J Clin Oncol. 2013;31(26):3182-3190.
58. Guo J, Si L, Kong Y, et al. Phase II, open-label, single-arm trial of imatinib mesylate in patients with metastatic melanoma harboring c-Kit mutation or amplification. J Clin Oncol. 2011;29(21):2904-2909.
59. Ribas A, Hodi FS, Callahan M, et al. Hepatotoxicity with combination of vemurafenib and ipilimumab. N Engl J Med. 2013;368(14):1365-1366.
FDA approves bortezomib retreatment in MM
The US Food and Drug Administration (FDA) has approved bortezomib (Velcade) for the retreatment of adults with multiple myeloma (MM) who previously responded to bortezomib and relapsed at least 6 months after that treatment.
Bortezomib’s label has been updated to include dosing guidelines and safety and efficacy findings for single-agent bortezomib and bortezomib in combination with dexamethasone in patients previously treated with bortezomib.
Bortezomib retreatment may be started at the last dose the patient tolerated.
The FDA approved bortezomib retreatment based on results of the phase 2 RETRIEVE study and other supportive data.
The single-arm RETRIEVE trial included 130 MM patients aged 18 years and older who had previously responded to bortezomib-based therapy and relapsed at least 6 months after the treatment. The patients had received a median of 2 prior therapies (range, 1 to 7).
In this study, 94 of the patients received bortezomib in combination with dexamethasone.
One patient achieved complete response to treatment, and 49 achieved partial responses, for an overall response rate of 38.5%. The median duration of response was 6.5 months (range, 0.6 to 19.3 months).
The safety profile with bortezomib retreatment was consistent with the known safety profile of intravenous bortezomib in relapsed MM. Researchers did not observer cumulative toxicities upon retreatment.
The most common adverse event was thrombocytopenia, which occurred in 52% of patients. The incidence of grade 3 or higher thrombocytopenia was 24%.
Peripheral neuropathy was also common, occurring in 28% of patients. Grade 3 or higher peripheral neuropathy occurred in 6% of patients.
The rate of serious adverse events was 12.3%. The most commonly reported serious adverse events were thrombocytopenia (3.8%), diarrhea (2.3%), herpes zoster (1.5%), and pneumonia (1.5%). Adverse events leading to discontinuation occurred in 13% of patients.
Bortezomib is co-developed by Millennium/Takeda and Janssen Pharmaceutical Companies. Millennium is responsible for commercialization of bortezomib in the US. Janssen Pharmaceutical Companies are responsible for commercialization in Europe and the rest of the world.
Takeda Pharmaceutical Company Limited and Janssen Pharmaceutical K.K. co-promote bortezomib in Japan. Bortezomib is approved in more than 90 countries.
The US Food and Drug Administration (FDA) has approved bortezomib (Velcade) for the retreatment of adults with multiple myeloma (MM) who previously responded to bortezomib and relapsed at least 6 months after that treatment.
Bortezomib’s label has been updated to include dosing guidelines and safety and efficacy findings for single-agent bortezomib and bortezomib in combination with dexamethasone in patients previously treated with bortezomib.
Bortezomib retreatment may be started at the last dose the patient tolerated.
The FDA approved bortezomib retreatment based on results of the phase 2 RETRIEVE study and other supportive data.
The single-arm RETRIEVE trial included 130 MM patients aged 18 years and older who had previously responded to bortezomib-based therapy and relapsed at least 6 months after the treatment. The patients had received a median of 2 prior therapies (range, 1 to 7).
In this study, 94 of the patients received bortezomib in combination with dexamethasone.
One patient achieved complete response to treatment, and 49 achieved partial responses, for an overall response rate of 38.5%. The median duration of response was 6.5 months (range, 0.6 to 19.3 months).
The safety profile with bortezomib retreatment was consistent with the known safety profile of intravenous bortezomib in relapsed MM. Researchers did not observer cumulative toxicities upon retreatment.
The most common adverse event was thrombocytopenia, which occurred in 52% of patients. The incidence of grade 3 or higher thrombocytopenia was 24%.
Peripheral neuropathy was also common, occurring in 28% of patients. Grade 3 or higher peripheral neuropathy occurred in 6% of patients.
The rate of serious adverse events was 12.3%. The most commonly reported serious adverse events were thrombocytopenia (3.8%), diarrhea (2.3%), herpes zoster (1.5%), and pneumonia (1.5%). Adverse events leading to discontinuation occurred in 13% of patients.
Bortezomib is co-developed by Millennium/Takeda and Janssen Pharmaceutical Companies. Millennium is responsible for commercialization of bortezomib in the US. Janssen Pharmaceutical Companies are responsible for commercialization in Europe and the rest of the world.
Takeda Pharmaceutical Company Limited and Janssen Pharmaceutical K.K. co-promote bortezomib in Japan. Bortezomib is approved in more than 90 countries.
The US Food and Drug Administration (FDA) has approved bortezomib (Velcade) for the retreatment of adults with multiple myeloma (MM) who previously responded to bortezomib and relapsed at least 6 months after that treatment.
Bortezomib’s label has been updated to include dosing guidelines and safety and efficacy findings for single-agent bortezomib and bortezomib in combination with dexamethasone in patients previously treated with bortezomib.
Bortezomib retreatment may be started at the last dose the patient tolerated.
The FDA approved bortezomib retreatment based on results of the phase 2 RETRIEVE study and other supportive data.
The single-arm RETRIEVE trial included 130 MM patients aged 18 years and older who had previously responded to bortezomib-based therapy and relapsed at least 6 months after the treatment. The patients had received a median of 2 prior therapies (range, 1 to 7).
In this study, 94 of the patients received bortezomib in combination with dexamethasone.
One patient achieved complete response to treatment, and 49 achieved partial responses, for an overall response rate of 38.5%. The median duration of response was 6.5 months (range, 0.6 to 19.3 months).
The safety profile with bortezomib retreatment was consistent with the known safety profile of intravenous bortezomib in relapsed MM. Researchers did not observer cumulative toxicities upon retreatment.
The most common adverse event was thrombocytopenia, which occurred in 52% of patients. The incidence of grade 3 or higher thrombocytopenia was 24%.
Peripheral neuropathy was also common, occurring in 28% of patients. Grade 3 or higher peripheral neuropathy occurred in 6% of patients.
The rate of serious adverse events was 12.3%. The most commonly reported serious adverse events were thrombocytopenia (3.8%), diarrhea (2.3%), herpes zoster (1.5%), and pneumonia (1.5%). Adverse events leading to discontinuation occurred in 13% of patients.
Bortezomib is co-developed by Millennium/Takeda and Janssen Pharmaceutical Companies. Millennium is responsible for commercialization of bortezomib in the US. Janssen Pharmaceutical Companies are responsible for commercialization in Europe and the rest of the world.
Takeda Pharmaceutical Company Limited and Janssen Pharmaceutical K.K. co-promote bortezomib in Japan. Bortezomib is approved in more than 90 countries.
Secure Texting Improves Hospital Communication
Pagers, though reliable and familiar technology, can be suboptimal for facilitating healthcare team communication.[1, 2] Most paging systems utilize single‐function pagers and only allow one‐way communication, requiring recipients to disrupt workflow to respond to pages. Paging transmissions can also be intercepted, and the information presented on pager displays can be viewed by anyone in possession of the pager.
Smartphones allow for instantaneous two‐way and group communication through advanced technological features. Their use is widespread; over 81% of American physicians owned a smartphone in 2011.[3] Previous studies demonstrate that healthcare providers rate smartphone‐based email positively, and that team smartphones can facilitate communication between nurses and physicians.[4, 5] However, these studies specifically examined the utility of smartphone‐based email and voice calls, and did not include text messaging. Limitations of traditional smartphone‐based text messaging include Health Insurance Portability and Accountability Act (HIPAA) noncompliance and dependence on in‐hospital cellular reception, which can be unreliable. HIPAA is a 1996 US federal law that established a set of privacy and security rules governing not only what is considered protected health information (PHI), but also minimum standards for the protection of such information. HIPAA compliance is defined as meeting these minimum standards for physical, network, and process security.[6, 7] Though PHI is often transmitted via paging systems and commercial carrier‐based text messaging, these modalities are not secure and are thus not HIPAA‐compliant.
Text messaging applications that address these security and reliability issues have the potential to greatly enhance in‐hospital communication. We hypothesized that a smartphone‐based HIPAA‐compliant group messaging application could improve in‐hospital communication on the inpatient medicine service. To our knowledge, our study is the first to examine a HIPAA‐compliant text messaging system, and also the first to compare a combination paging/HIPAA‐compliant group messaging (HCGM) system with a paging‐only system in assessing healthcare provider perception of communication efficiency.
METHODS
Intervention
This study utilized Medigram (Medigram, Inc.,
Study Design
In an eight‐week prospective, cluster‐randomized, controlled trial conducted at Stanford Hospital (June 25, 2012August 17, 2012), three of five inpatient medicine teams were randomized to use Medigram in addition to the existing hospital paging system (HCGM teams); the remaining two teams were assigned to use hospital paging only (control teams). Each team included one attending physician, one resident, two interns, two medical students, and a case manager. According to prescheduled rotations, attendings rotated every two weeks, and residents, interns, and medical students rotated every four weeks. All rotations were either off‐service or off‐site, with the exception of two attendings who rotated between study teams but within their experimental designations. Case managers remained with the same team. Additionally, the satellite pharmacy was provided with an HCGM‐equipped smartphone to communicate with experimental teams.
Participation was voluntary, with a 96% participation rate (n=75). HCGM teams downloaded the free application onto their smartphones. Participants without smartphones were provided with one for the duration of the study. Proper application use was demonstrated by one researcher in a 10‐minute standardized presentation. HCGM teams were encouraged to use the application in lieu of paging, except when patient care could be compromised.
All participants completed linked baseline and post‐study surveys. Gift cards valued at $10 were provided on completion of each survey. Though participants were assigned to either HCGM or control groups based on the randomized assignment of their preset cluster (hospital team) to an HCGM or control group, analysis was performed on the individual level due to the hospital's set rotation schedule, which resulted in dynamic, frequently changing clusters. We also compared average length of stay and time of discharge for patients treated by control versus HCGM teams. Clinical outcome data were obtained from the hospital's database using Midas+ Statit Solutions (Midas+ Statit Solutions Group, Tucson, AZ). Survey and clinical outcome data were analyzed in Stata (StataCorp, College Station, TX) and R (R Foundation for Statistical Computing, Vienna, Austria).
Survey Design and Analysis
Identical, anonymous baseline surveys were administered to control and HCGM teams. These surveys assessed attitudes toward the hospital paging system using a 5‐point Likert scale (1=low, 5=high) to evaluate perceived measures of effectiveness, workflow integration, and overall satisfaction. Wilcoxon rank sum tests were used to compare control and HCGM group responses to these questions. Free response questions asked participants to list the most effective and ineffective aspects of the paging system.
Post‐study surveys included all baseline survey questions, as well as questions about personal texting behavior. Post‐study HCGM surveys also included a parallel set of questions rating the HCGM application on the same measures of perceived effectiveness, workflow integration, and overall satisfaction. Wilcoxon signed rank tests were used to compare HCGM participants' baseline evaluations of paging to their post‐study evaluations of the HCGM application. Baseline and post‐study surveys were linked by the last four digits of respondent cell phone numbers. To compare control and HCGM group perceptions of the hospital paging system at study completion, post‐study survey responses were evaluated using Wilcoxon rank sum tests. The family‐wise error rate was left unadjusted due to concerns around inflated type II errors, given the high degree of correlation between survey questions.
All free response questions were analyzed using thematic analysis and grounded theory. After reviewing responses to each question, a list of overarching themes was constructed. Two researchers then independently reviewed each free‐response entry to assign it to one or more of these themes (some responses included several ideas with distinct themes). Entries with concordant theme assignments (90%) were coded as such; nonconcordant entries required an additional round of review to reach concordance. Finally, objective outcome measures including length of stay and time of discharge were analyzed by two‐sample t test.
| Control Group | HCGM Group | |
|---|---|---|
| ||
| Paired surveys collected (completion rate) | 22 (85%) | 41 (84%) |
| Average age 95% CI | 30.10 1.71 | 30.95 2.94 |
| Gender | ||
| Male | 13 (59%) | 24 (59%) |
| Female | 9 (41%) | 17 (41%) |
| Role | ||
| Medical students | 6 (27%) | 11 (27%) |
| Interns (PGY 1) | 7 (32%) | 12 (29%) |
| Residents (PGY2 and 3) | 3 (14%) | 6 (15%) |
| Attending physicians | 5 (23%) | 5 (12%) |
| Case managers | 1 (5%) | 3 (7%) |
| Pharmacists | 0 (0%) | 4 (10%) |
Information Security
The HCGM application in this study features 256‐bit encryption technology and requires a six‐digit password to access texts. For added security, a study‐dedicated server (HP ProLiant DL 180 G6; Hewlett‐Packard Co., Palo Alto, CA) with 4‐TB hard drive capacity (4 Seagate Barracuda ST1000DM003 1 TB 7200 RPM internal hard drives; Seagate Technology PLC, Cupertino, CA) was installed in the Stanford School of Medicine Data Center to store encrypted text messages. Data stored on the phones/server were accessible only to study participants, not researchers. These security measures were approved by Stanford Hospital and Stanford School of Medicine's security and privacy review process.
Hospital Paging System
Stanford Hospital and Clinics is a quaternary care academic medical center with 613 beds, 49 operating rooms, and over 25,000 inpatient admissions per year.[8] The institution uses one‐way alphanumeric pagers (primary model: Daviscomm BR802 Flex Pager from USA Mobility, secondary model: Sun Telecom Titan 3 Plus from USA Mobility; USA Mobility Inc., Springfield, VA). USA Mobility operates the largest one‐ and two‐way paging networks in the United States.[9]
RESULTS
Of 26 control and 49 HCGM group members participating in the study, linked baseline and post‐study surveys were collected for 22 control and 41 HCGM participants (completion rates of 84.6% and 83.7%, respectively). To minimize recall bias, surveys not completed within a prespecified timeframe upon entering or leaving a team (two days attendings, four days others) were excluded.
Control and HCGM Group Characteristics
Control and HCGM groups were well matched demographically (Table 1). The average ages of control and HCGM group members were 30.10 and 30.95, respectively. Both groups were 59% male and 41% female.
| What do you find effective about the current hospital paging system? | What do you find ineffective about the current hospital paging system? | ||||
|---|---|---|---|---|---|
| Theme | No. of Respondents, (% of Total) | Response Example | Theme | No. of Respondents, (% of Total) | Response Example |
| |||||
| Reliability of message transmission | 17 (30.4%) | Everyone is able to receive the pages I send, regardless of service | Time wasted waiting for a response | 17 (29.3%) | Inefficient use of time waiting for reply |
| Ability to text page | 14 (25.0%) | Text paging allows targeted questions | One‐way nature of communication | 14 (24.1%) | Cannot text back instantly |
| Ease of use | 8 (14.3%) | Easy to use | Needing to find a computer to send a text page | 12 (20.7%) | Have to find an available computer to send a page |
| Search function | 5 (8.9%) | Search function is pretty effective in finding the people you're looking for | Character limitation | 10 (17.2%) | Length of text allowed too short |
| Ubiquity | 5 (8.9%) | Everyone is on paging system | Search function | 6 (10.3%) | Delay in looking people up in the system |
| Speed | 4 (7.1%) | Fast | Finding a phone to return a page | 5 (8.6%) | When you receive a page you need to find a phone |
| Loud alerts | 4 (7.1%) | Pager loud enough to hear all the time | Receipt of page uncertain | 3 (5.2%) | Unknown if page received |
| Staff responsiveness to pages | 4 (7.1%) | I know MD has to be onsite or covering the pager so someone eventually will call back | Sender's pager number not always included in page | 3 (5.2%) | Not everyone puts their pager number when they page. Then it's impossible to get back to them. |
| Brevity of messages | 3 (5.4%) | Requires very brief messages (easier for recipient) | Needing to remain near a phone while waiting for a page response | 3 (5.2%) | Wait by a phone for someone to call back; sometimes they do not call back |
| Helpful page operators | 2 (3.6%) | Page operators very helpful | Reliability of message transmission | 3 (5.2%) | Sometimes messages don't go through |
| Other | 10 (17.9%) | It's online and allows paging from anywhere there's internet access | Other | 11 (19.0%) | You cannot text with patient info on it |
A similar distribution of team member roles was observed in both groups, with two exceptions. First, the proportion of attending respondents in the HCGM group was lower than in the control group. This was due to the fact that several HCGM attendings entered discrepant ID codes on their surveys, thus making it impossible to link baseline and post‐study responses; these data were excluded. Additionally, two HCGM attendings were on service for four, rather than the standard two weeks, meaning two additional data points from unique attendings could not be obtained. Second, the experimental group included four pharmacists, whereas the control group did not. As a sensitivity test, we analyzed the data excluding the pharmacists, and this did not change our results.
Baseline Evaluations of the Hospital Paging System
At baseline, there were no significant differences between control and HCGM participants' perceptions of paging effectiveness (see Supporting Table 1, in the online version of this article). On a 5‐point rating scale (1=low, 5=high), 63 subjects rated their overall satisfaction with the paging system an average of 2.79 (95% confidence interval: 2.55‐3.03).
In free response questions, components of the paging system most frequently cited as effective included: reliability of message transmission, alphanumeric text paging, and ease of use (30.4%, 25.0%, and 14.3% of 56 respondents, respectively) (Table 2). Ineffective aspects included: time wasted waiting for responses to pages, the unidirectional nature of pagers, and needing to find a computer to send a text page (29.3%, 24.1%, and 20.7% of 58 respondents, respectively) (Table 2).
| Question | Baseline Average Rating of Paging System* | Post‐Study Average Rating of HCGM Application | P Value |
|---|---|---|---|
| |||
| Rate the effectiveness of each in allowing you to | |||
| Communicate your thoughts clearly | 3.194 | 3.806 | 0.010 |
| Communicate your thoughts efficiently | 3.200 | 3.829 | 0.009 |
| Send messages to other hospital staff | 3.543 | 3.571 | 0.480 |
| Receive messages/stay informed in real time | 3.222 | 3.306 | 0.405 |
| Rate the effectiveness of each in integrating into your workflow during | |||
| Work rounds | 2.313 | 3.000 | 0.018 |
| Patient discharge | 2.448 | 3.276 | 0.012 |
| Patient admissions | 2.862 | 2.621 | 0.238 |
| Teaching sessions | 2.292 | 2.458 | 0.448 |
| Overall satisfaction | 2.811 | 3.459 | 0.003 |
Baseline Utilization of Text Messaging
The majority of participants were familiar with text messaging and regularly used it personally and professionally prior to the start of the study. 90.5% of participants (n = 63) reported sending an average of 1 personal text messages per day, with the largest proportion (39.7%) sending 1‐5 texts per day (see Supporting Figure 1A in the online version of this article). 58.1% of respondents (n=62) reported sending an average of 1 text messages per day related to patient care (see Supporting Figure 1B in the online version of this article), with the largest fraction (58.3%) sending 1‐5 texts per day.
HCGM Adoption and Usage Patterns
Active use of HCGM was defined as using the application to send or receive an average of 1 text messages per day. Of HCGM participants, 67% self‐reported 1 week of active use of the application, indicating a strong compliance rate. Among non‐attendings, 70% reported sending 1 or more texts to other team members per day; this percentage increased to 86% among those whose attendings texted them at least once per day (47% of non‐attendings). Respondents who text frequently in their personal lives (>5 texts/day) were more likely to use the application; 90% of these respondents sent 1 or more HCGM texts per day.
Among 12 subjects who did not report sending or receiving 1 HCGM text/day, the top three reasons were: other team members were not using it (67%), no need to use it given the close proximity of other team members (67%), and other (33%). A Wilcoxon rank sum test was used to compare the ages of active versus nonactive users; no significant age difference was found (P=0.200).
To provide an objective measure of application adoption, usage data for each HCGM participant were obtained from the application developers. Because much of the study's first week was spent onboarding and instructing participant, the first week was not included in the analysis. Of 43 individuals enrolled in the study for at least one of the seven remaining weeks, 56% sent a total of 5 texts, 44% sent 10 texts, and 28% sent 20 texts. HCGM users on three teams sent an aggregate mean of 123 texts/week. Data on number of messages received by each user were not available.
Perceived Effectiveness: Paging Versus HCGM
In post‐study surveys, HCGM participants rated HCGM significantly higher (P<0.05) than paging (Table 3) in terms of ability to communicate thoughts clearly (P=0.010) and efficiently (P=0.009). HCGM was also deemed more effective at integrating into workflow during rounds (P=0.018) and patient discharge (P=0.012). Overall satisfaction with HCGM was also significantly higher (P=0.003).
| Control (n=22) | HCGM (n=41) | |||||
|---|---|---|---|---|---|---|
| Baseline Mean | Post‐Study Mean | P Value* | Baseline Mean | Post‐Study Mean | P Value* | |
| ||||||
| Rate the effectiveness of each in allowing you to | ||||||
| Communicate your thoughts clearly | 2.905 | 2.619 | 0.103 | 3.250 | 2.850 | 0.004 |
| Communicate your thoughts efficiently | 2.952 | 2.762 | 0.106 | 3.250 | 2.825 | 0.018 |
| Send messages to other hospital staff | 3.762 | 3.190 | 0.019 | 3.550 | 3.450 | 0.253 |
| Receive messages/stay informed in real time | 3.667 | 2.857 | 0.002 | 3.300 | 2.900 | 0.031 |
| Rate the effectiveness of each in integrating into your workflow during | ||||||
| Work rounds | 2.429 | 2.476 | 0.303 | 2.410 | 2.718 | 0.078 |
| Patient discharge | 2.500 | 2.350 | 0.251 | 2.472 | 2.861 | 0.071 |
| Patient admissions | 2.905 | 2.524 | 0.020 | 2.889 | 3.000 | 0.384 |
| Teaching sessions | 2.143 | 2.200 | 0.386 | 2.367 | 2.400 | 0.418 |
Comparison of Pre‐ and Post‐study Perceived Effectiveness of the Hospital Paging System
In post‐study evaluations, both control and HCGM participants rated the paging system's effectiveness less favorably (P<0.05) compared to baseline in terms of ability to receive messages/stay informed in real time (control P=0.002, HCGM P=0.031) (Table 4). Controls also reported a decrease from baseline in perceived effectiveness of paging in terms of ability to send messages (P=0.019) and integrate into workflow during patient admissions (P=0.020). HCGM participants found paging less effective at communicating thoughts clearly (P=0.004) and efficiently (P=0.018). No significant differences existed between control and HCGM groups' average assessments of paging at the conclusion of the study (see Supporting Table 2, in the online version of this article).
| What do you find effective about the Medigram system? | What do you find ineffective about the Medigram system? | ||||
|---|---|---|---|---|---|
| Theme | No. of Respondents, (% of Total) | Response Example | Theme | No. of Respondents, (% of Total) | Response Example |
| |||||
| Ease of use | 11 (32.4%) | Easy to use | Lack of ubiquity | 10 (30.3%) | Not enough people using it |
| Group texting feature | 11 (32.4%) | Ability to communicate with entire teameveryone seeing same message | Inconsistent usage | 8 (24.2%) | No one used it reliably |
| Speed | 8 (23.5%) | Faster than a page to send a message | Reliability of message transmission | 5 (15.2%) | Big negative is it requires Wi‐Fi |
| Accessibility | 5 (14.7%) | Able to get messages across quickly and anywhere without a computer | Missed message alerts | 4 (12.1%) | Unable to reliably know message was received if phone on silent |
| Efficiency | 4 (11.8%) | Very efficient way to communicate | Password login | 3 (9.1%) | Having to type a 6‐digit password in |
| Real‐time communication | 2 (5.9%) | Real‐time results | User interface | 2 (6.1%) | Interface is a little convoluted |
| No character limitation | 2 (5.9%) | No limit on words | Other | 10 (30.3%) | Not sure if all of the texts were relevant |
| Other | 4 (11.8%) | Great UI | |||
HCGM User Experience
When asked if they would recommend using an HCGM system to facilitate communication on the internal medicine wards, 85% of HCGM participants replied yes, 15% reported not sure, and 0% reported no. Based on free response entries, HCGM's most effective features (Table 5) included ease of use, group texting capacity, and speed (32.4%, 32.4%, and 23.5% of 34 respondents, respectively); its most ineffective aspects (Table 5) included lack of ubiquity, inconsistent usage by those with access to the application, and reliability of message transmission (30.3%, 24.2%, and 15.2% of 33 respondents, respectively).
DISCUSSION
We are the first to report that smartphone‐based, HIPAA‐compliant, group messaging applications improve provider perception of in‐hospital communication, while providing the information security that paging and commercial cellular networks do not. HCGM participants rated the application more favorably than paging in terms of clarity and efficiency of communication. These findings may be attributed to the expanded functionality offered by the application, including no character limit per HCGM text, the ability to use special characters such as slashes and ampersands, group texting, and the ability to reply immediately. HCGM may result in more efficient communication by facilitating direct two‐way communication via smartphones, whereas sending or returning pages requires a landline or computer.
HCGM participants rated the application higher than paging in terms of workflow integration during rounds and patient discharge, but not during patient admissions and teaching sessions. We had hypothesized that HCGM would integrate better into participants' workflows because HCGM texts could be replied to immediately. The reasons for the equivalence of HCGM and paging for workflow integration during patient admissions and teaching sessions may have been due to weak Wi‐Fi in certain areas of the hospital, and may warrant further investigation.
Analysis of HCGM utilization indicated that there were factors that made participants more or less likely to use the application. Individuals who reported that their attendings used HCGM regularly were more likely to use it themselves. Attending usage may legitimize use of HCGM for housestaff and medical students, who may otherwise feel that texting appears unprofessional. Participants who texted frequently in their personal lives were also more likely to utilize HCGM regularly, perhaps due to increased familiarity with/affinity for the platform.
HCGM participants who did not utilize the application regularly most often cited the fact that other team members did not use it. Among all users, the most frequently noted ineffective aspects of the application were its lack of ubiquity (HCGM was made available only to the small subset of individuals involved in the study) and inconsistent usage by those who did have access to the application. These findings suggest that HCGM effectiveness may be maximized with unrestricted access and mandated use; patchwork implementation, as in this study, detracts from perceived effectiveness.
Though objective outcome measures (average length of stay and average time of discharge) for patients of control attendings and HCGM attendings were examined, no significant differences were observed (P=0.089 and 0.494, respectively). These results may be due to the small size and short duration of the study.
Limitations
Our study had several limitations. HCGM was available only to individuals in the experimental arm of the study; most members of the internal medicine department and all other departments were not reachable through the application. This lack of ubiquity was a frequently cited frustration. Among individuals to whom HCGM was made available, barriers to adoption included: close proximity to would‐be message recipients, concern that smartphone usage in front of patients might appear unprofessional, and inconsistent or dropped service (weak or no Wi‐Fi signal in some areas). A technical problem with the Android platform midway through the study served as a potential frustration to several participants.
Due to the aforementioned issues, some participants used the HCGM application in a very limited way. We also did not replace hospital pagers (infeasible in this hospital setting); the HCGM application was added as a supplemental system. Future studies might explore the replacement of paging systems with HCGM‐type applications, as well as delve further into quantitative patient care outcomes.
It should be noted that the start of the study unintentionally coincided with the start of new interns and medical students in the hospital. Although it is possible that their relative unfamiliarity with the hospital may have made them more amenable to adopting a new technology, it is also possible that they may have been less likely to do so in the midst of such a major transitional period. Finally, this was a single‐site study, and as such, its findings may not be broadly generalizable. More research on such interventions is warranted, particularly in the context of current insecure communication methods such as paging that may make hospital‐wide adoption of new methods of secure communication, such as HCGM, mandatory.
CONCLUSION
Our study is the first to demonstrate that HCGM applications improve healthcare provider perception of multiple measures of in‐hospital communication, including efficiency of communication, workflow integration, and overall satisfaction. Notably, 85% of HCGM team respondents said they would recommend using an HCGM system on the wards. As smartphone use is expected to continue to increase among physicians and the general population, it is increasingly important to understand how to utilize these powerful communication tools to improve healthcare in an effective and secure manner.
Acknowledgements
The authors would like to thank the Stanford Medicine Residency Program and Stanford Hospital and Clinics for allowing them to perform the study, as well as Medigram, Inc., for supplying gift cards to incentivize survey completion and loaner iPhones to allow individuals without smartphones to participate in the study.
Disclosures: Stanford University School of Medicine's Medical Scholars Program provided financial support to the first author over the course of the study. Medigram, Inc. funded gift cards given to both control and HCGM participants upon survey completion and provided loaner iPhones to allow individuals without smartphones to participate in the study. Medigram, Inc. has also paid the fee for OnlineOpen to provide open access to this article. This study received an institutional review board exemption as quality improvement research. Participation was voluntary, and all participants signed a consent form. The authors report no conflicts of interest.
- . Communication systems in healthcare. Clin Biochem Rev. 2006;27:89–98.
- , , . Alphanumeric paging: a potential source of problems in patient care and communication. J Surg Educ. 2011;68:447–451.
- Manhattan Research. Taking the pulse: US market research report. Available at: http://manhattanresearch.com/Products‐and‐Services/Physician/Physician‐Research‐Modules. Accessed February 6, 2013.
- , , , et al. The use of wireless e‐mail to improve healthcare team communication. J Am Med Inform Assoc. 2009;16:705–713.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5:553–559.
- US Department of Health and Human Services. Summary of the HIPAA privacy rule. Available at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/summary/. Accessed May 11, 2013.
- United States Department of Health and Human Services. Summary of the HIPAA security rule. Available at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/srsummary.html. Accessed May 11, 2013.
- Stanford University. Stanford facts: about Stanford. Available at: http://facts.stanford.edu/about/hospital. Accessed October 12, 2013.
- Wikinvest. USA mobility. Available at: http://www.wikinvest.com/stock/USA_Mobility_(USMO). Accessed February 6, 2013.
Pagers, though reliable and familiar technology, can be suboptimal for facilitating healthcare team communication.[1, 2] Most paging systems utilize single‐function pagers and only allow one‐way communication, requiring recipients to disrupt workflow to respond to pages. Paging transmissions can also be intercepted, and the information presented on pager displays can be viewed by anyone in possession of the pager.
Smartphones allow for instantaneous two‐way and group communication through advanced technological features. Their use is widespread; over 81% of American physicians owned a smartphone in 2011.[3] Previous studies demonstrate that healthcare providers rate smartphone‐based email positively, and that team smartphones can facilitate communication between nurses and physicians.[4, 5] However, these studies specifically examined the utility of smartphone‐based email and voice calls, and did not include text messaging. Limitations of traditional smartphone‐based text messaging include Health Insurance Portability and Accountability Act (HIPAA) noncompliance and dependence on in‐hospital cellular reception, which can be unreliable. HIPAA is a 1996 US federal law that established a set of privacy and security rules governing not only what is considered protected health information (PHI), but also minimum standards for the protection of such information. HIPAA compliance is defined as meeting these minimum standards for physical, network, and process security.[6, 7] Though PHI is often transmitted via paging systems and commercial carrier‐based text messaging, these modalities are not secure and are thus not HIPAA‐compliant.
Text messaging applications that address these security and reliability issues have the potential to greatly enhance in‐hospital communication. We hypothesized that a smartphone‐based HIPAA‐compliant group messaging application could improve in‐hospital communication on the inpatient medicine service. To our knowledge, our study is the first to examine a HIPAA‐compliant text messaging system, and also the first to compare a combination paging/HIPAA‐compliant group messaging (HCGM) system with a paging‐only system in assessing healthcare provider perception of communication efficiency.
METHODS
Intervention
This study utilized Medigram (Medigram, Inc.,
Study Design
In an eight‐week prospective, cluster‐randomized, controlled trial conducted at Stanford Hospital (June 25, 2012August 17, 2012), three of five inpatient medicine teams were randomized to use Medigram in addition to the existing hospital paging system (HCGM teams); the remaining two teams were assigned to use hospital paging only (control teams). Each team included one attending physician, one resident, two interns, two medical students, and a case manager. According to prescheduled rotations, attendings rotated every two weeks, and residents, interns, and medical students rotated every four weeks. All rotations were either off‐service or off‐site, with the exception of two attendings who rotated between study teams but within their experimental designations. Case managers remained with the same team. Additionally, the satellite pharmacy was provided with an HCGM‐equipped smartphone to communicate with experimental teams.
Participation was voluntary, with a 96% participation rate (n=75). HCGM teams downloaded the free application onto their smartphones. Participants without smartphones were provided with one for the duration of the study. Proper application use was demonstrated by one researcher in a 10‐minute standardized presentation. HCGM teams were encouraged to use the application in lieu of paging, except when patient care could be compromised.
All participants completed linked baseline and post‐study surveys. Gift cards valued at $10 were provided on completion of each survey. Though participants were assigned to either HCGM or control groups based on the randomized assignment of their preset cluster (hospital team) to an HCGM or control group, analysis was performed on the individual level due to the hospital's set rotation schedule, which resulted in dynamic, frequently changing clusters. We also compared average length of stay and time of discharge for patients treated by control versus HCGM teams. Clinical outcome data were obtained from the hospital's database using Midas+ Statit Solutions (Midas+ Statit Solutions Group, Tucson, AZ). Survey and clinical outcome data were analyzed in Stata (StataCorp, College Station, TX) and R (R Foundation for Statistical Computing, Vienna, Austria).
Survey Design and Analysis
Identical, anonymous baseline surveys were administered to control and HCGM teams. These surveys assessed attitudes toward the hospital paging system using a 5‐point Likert scale (1=low, 5=high) to evaluate perceived measures of effectiveness, workflow integration, and overall satisfaction. Wilcoxon rank sum tests were used to compare control and HCGM group responses to these questions. Free response questions asked participants to list the most effective and ineffective aspects of the paging system.
Post‐study surveys included all baseline survey questions, as well as questions about personal texting behavior. Post‐study HCGM surveys also included a parallel set of questions rating the HCGM application on the same measures of perceived effectiveness, workflow integration, and overall satisfaction. Wilcoxon signed rank tests were used to compare HCGM participants' baseline evaluations of paging to their post‐study evaluations of the HCGM application. Baseline and post‐study surveys were linked by the last four digits of respondent cell phone numbers. To compare control and HCGM group perceptions of the hospital paging system at study completion, post‐study survey responses were evaluated using Wilcoxon rank sum tests. The family‐wise error rate was left unadjusted due to concerns around inflated type II errors, given the high degree of correlation between survey questions.
All free response questions were analyzed using thematic analysis and grounded theory. After reviewing responses to each question, a list of overarching themes was constructed. Two researchers then independently reviewed each free‐response entry to assign it to one or more of these themes (some responses included several ideas with distinct themes). Entries with concordant theme assignments (90%) were coded as such; nonconcordant entries required an additional round of review to reach concordance. Finally, objective outcome measures including length of stay and time of discharge were analyzed by two‐sample t test.
| Control Group | HCGM Group | |
|---|---|---|
| ||
| Paired surveys collected (completion rate) | 22 (85%) | 41 (84%) |
| Average age 95% CI | 30.10 1.71 | 30.95 2.94 |
| Gender | ||
| Male | 13 (59%) | 24 (59%) |
| Female | 9 (41%) | 17 (41%) |
| Role | ||
| Medical students | 6 (27%) | 11 (27%) |
| Interns (PGY 1) | 7 (32%) | 12 (29%) |
| Residents (PGY2 and 3) | 3 (14%) | 6 (15%) |
| Attending physicians | 5 (23%) | 5 (12%) |
| Case managers | 1 (5%) | 3 (7%) |
| Pharmacists | 0 (0%) | 4 (10%) |
Information Security
The HCGM application in this study features 256‐bit encryption technology and requires a six‐digit password to access texts. For added security, a study‐dedicated server (HP ProLiant DL 180 G6; Hewlett‐Packard Co., Palo Alto, CA) with 4‐TB hard drive capacity (4 Seagate Barracuda ST1000DM003 1 TB 7200 RPM internal hard drives; Seagate Technology PLC, Cupertino, CA) was installed in the Stanford School of Medicine Data Center to store encrypted text messages. Data stored on the phones/server were accessible only to study participants, not researchers. These security measures were approved by Stanford Hospital and Stanford School of Medicine's security and privacy review process.
Hospital Paging System
Stanford Hospital and Clinics is a quaternary care academic medical center with 613 beds, 49 operating rooms, and over 25,000 inpatient admissions per year.[8] The institution uses one‐way alphanumeric pagers (primary model: Daviscomm BR802 Flex Pager from USA Mobility, secondary model: Sun Telecom Titan 3 Plus from USA Mobility; USA Mobility Inc., Springfield, VA). USA Mobility operates the largest one‐ and two‐way paging networks in the United States.[9]
RESULTS
Of 26 control and 49 HCGM group members participating in the study, linked baseline and post‐study surveys were collected for 22 control and 41 HCGM participants (completion rates of 84.6% and 83.7%, respectively). To minimize recall bias, surveys not completed within a prespecified timeframe upon entering or leaving a team (two days attendings, four days others) were excluded.
Control and HCGM Group Characteristics
Control and HCGM groups were well matched demographically (Table 1). The average ages of control and HCGM group members were 30.10 and 30.95, respectively. Both groups were 59% male and 41% female.
| What do you find effective about the current hospital paging system? | What do you find ineffective about the current hospital paging system? | ||||
|---|---|---|---|---|---|
| Theme | No. of Respondents, (% of Total) | Response Example | Theme | No. of Respondents, (% of Total) | Response Example |
| |||||
| Reliability of message transmission | 17 (30.4%) | Everyone is able to receive the pages I send, regardless of service | Time wasted waiting for a response | 17 (29.3%) | Inefficient use of time waiting for reply |
| Ability to text page | 14 (25.0%) | Text paging allows targeted questions | One‐way nature of communication | 14 (24.1%) | Cannot text back instantly |
| Ease of use | 8 (14.3%) | Easy to use | Needing to find a computer to send a text page | 12 (20.7%) | Have to find an available computer to send a page |
| Search function | 5 (8.9%) | Search function is pretty effective in finding the people you're looking for | Character limitation | 10 (17.2%) | Length of text allowed too short |
| Ubiquity | 5 (8.9%) | Everyone is on paging system | Search function | 6 (10.3%) | Delay in looking people up in the system |
| Speed | 4 (7.1%) | Fast | Finding a phone to return a page | 5 (8.6%) | When you receive a page you need to find a phone |
| Loud alerts | 4 (7.1%) | Pager loud enough to hear all the time | Receipt of page uncertain | 3 (5.2%) | Unknown if page received |
| Staff responsiveness to pages | 4 (7.1%) | I know MD has to be onsite or covering the pager so someone eventually will call back | Sender's pager number not always included in page | 3 (5.2%) | Not everyone puts their pager number when they page. Then it's impossible to get back to them. |
| Brevity of messages | 3 (5.4%) | Requires very brief messages (easier for recipient) | Needing to remain near a phone while waiting for a page response | 3 (5.2%) | Wait by a phone for someone to call back; sometimes they do not call back |
| Helpful page operators | 2 (3.6%) | Page operators very helpful | Reliability of message transmission | 3 (5.2%) | Sometimes messages don't go through |
| Other | 10 (17.9%) | It's online and allows paging from anywhere there's internet access | Other | 11 (19.0%) | You cannot text with patient info on it |
A similar distribution of team member roles was observed in both groups, with two exceptions. First, the proportion of attending respondents in the HCGM group was lower than in the control group. This was due to the fact that several HCGM attendings entered discrepant ID codes on their surveys, thus making it impossible to link baseline and post‐study responses; these data were excluded. Additionally, two HCGM attendings were on service for four, rather than the standard two weeks, meaning two additional data points from unique attendings could not be obtained. Second, the experimental group included four pharmacists, whereas the control group did not. As a sensitivity test, we analyzed the data excluding the pharmacists, and this did not change our results.
Baseline Evaluations of the Hospital Paging System
At baseline, there were no significant differences between control and HCGM participants' perceptions of paging effectiveness (see Supporting Table 1, in the online version of this article). On a 5‐point rating scale (1=low, 5=high), 63 subjects rated their overall satisfaction with the paging system an average of 2.79 (95% confidence interval: 2.55‐3.03).
In free response questions, components of the paging system most frequently cited as effective included: reliability of message transmission, alphanumeric text paging, and ease of use (30.4%, 25.0%, and 14.3% of 56 respondents, respectively) (Table 2). Ineffective aspects included: time wasted waiting for responses to pages, the unidirectional nature of pagers, and needing to find a computer to send a text page (29.3%, 24.1%, and 20.7% of 58 respondents, respectively) (Table 2).
| Question | Baseline Average Rating of Paging System* | Post‐Study Average Rating of HCGM Application | P Value |
|---|---|---|---|
| |||
| Rate the effectiveness of each in allowing you to | |||
| Communicate your thoughts clearly | 3.194 | 3.806 | 0.010 |
| Communicate your thoughts efficiently | 3.200 | 3.829 | 0.009 |
| Send messages to other hospital staff | 3.543 | 3.571 | 0.480 |
| Receive messages/stay informed in real time | 3.222 | 3.306 | 0.405 |
| Rate the effectiveness of each in integrating into your workflow during | |||
| Work rounds | 2.313 | 3.000 | 0.018 |
| Patient discharge | 2.448 | 3.276 | 0.012 |
| Patient admissions | 2.862 | 2.621 | 0.238 |
| Teaching sessions | 2.292 | 2.458 | 0.448 |
| Overall satisfaction | 2.811 | 3.459 | 0.003 |
Baseline Utilization of Text Messaging
The majority of participants were familiar with text messaging and regularly used it personally and professionally prior to the start of the study. 90.5% of participants (n = 63) reported sending an average of 1 personal text messages per day, with the largest proportion (39.7%) sending 1‐5 texts per day (see Supporting Figure 1A in the online version of this article). 58.1% of respondents (n=62) reported sending an average of 1 text messages per day related to patient care (see Supporting Figure 1B in the online version of this article), with the largest fraction (58.3%) sending 1‐5 texts per day.
HCGM Adoption and Usage Patterns
Active use of HCGM was defined as using the application to send or receive an average of 1 text messages per day. Of HCGM participants, 67% self‐reported 1 week of active use of the application, indicating a strong compliance rate. Among non‐attendings, 70% reported sending 1 or more texts to other team members per day; this percentage increased to 86% among those whose attendings texted them at least once per day (47% of non‐attendings). Respondents who text frequently in their personal lives (>5 texts/day) were more likely to use the application; 90% of these respondents sent 1 or more HCGM texts per day.
Among 12 subjects who did not report sending or receiving 1 HCGM text/day, the top three reasons were: other team members were not using it (67%), no need to use it given the close proximity of other team members (67%), and other (33%). A Wilcoxon rank sum test was used to compare the ages of active versus nonactive users; no significant age difference was found (P=0.200).
To provide an objective measure of application adoption, usage data for each HCGM participant were obtained from the application developers. Because much of the study's first week was spent onboarding and instructing participant, the first week was not included in the analysis. Of 43 individuals enrolled in the study for at least one of the seven remaining weeks, 56% sent a total of 5 texts, 44% sent 10 texts, and 28% sent 20 texts. HCGM users on three teams sent an aggregate mean of 123 texts/week. Data on number of messages received by each user were not available.
Perceived Effectiveness: Paging Versus HCGM
In post‐study surveys, HCGM participants rated HCGM significantly higher (P<0.05) than paging (Table 3) in terms of ability to communicate thoughts clearly (P=0.010) and efficiently (P=0.009). HCGM was also deemed more effective at integrating into workflow during rounds (P=0.018) and patient discharge (P=0.012). Overall satisfaction with HCGM was also significantly higher (P=0.003).
| Control (n=22) | HCGM (n=41) | |||||
|---|---|---|---|---|---|---|
| Baseline Mean | Post‐Study Mean | P Value* | Baseline Mean | Post‐Study Mean | P Value* | |
| ||||||
| Rate the effectiveness of each in allowing you to | ||||||
| Communicate your thoughts clearly | 2.905 | 2.619 | 0.103 | 3.250 | 2.850 | 0.004 |
| Communicate your thoughts efficiently | 2.952 | 2.762 | 0.106 | 3.250 | 2.825 | 0.018 |
| Send messages to other hospital staff | 3.762 | 3.190 | 0.019 | 3.550 | 3.450 | 0.253 |
| Receive messages/stay informed in real time | 3.667 | 2.857 | 0.002 | 3.300 | 2.900 | 0.031 |
| Rate the effectiveness of each in integrating into your workflow during | ||||||
| Work rounds | 2.429 | 2.476 | 0.303 | 2.410 | 2.718 | 0.078 |
| Patient discharge | 2.500 | 2.350 | 0.251 | 2.472 | 2.861 | 0.071 |
| Patient admissions | 2.905 | 2.524 | 0.020 | 2.889 | 3.000 | 0.384 |
| Teaching sessions | 2.143 | 2.200 | 0.386 | 2.367 | 2.400 | 0.418 |
Comparison of Pre‐ and Post‐study Perceived Effectiveness of the Hospital Paging System
In post‐study evaluations, both control and HCGM participants rated the paging system's effectiveness less favorably (P<0.05) compared to baseline in terms of ability to receive messages/stay informed in real time (control P=0.002, HCGM P=0.031) (Table 4). Controls also reported a decrease from baseline in perceived effectiveness of paging in terms of ability to send messages (P=0.019) and integrate into workflow during patient admissions (P=0.020). HCGM participants found paging less effective at communicating thoughts clearly (P=0.004) and efficiently (P=0.018). No significant differences existed between control and HCGM groups' average assessments of paging at the conclusion of the study (see Supporting Table 2, in the online version of this article).
| What do you find effective about the Medigram system? | What do you find ineffective about the Medigram system? | ||||
|---|---|---|---|---|---|
| Theme | No. of Respondents, (% of Total) | Response Example | Theme | No. of Respondents, (% of Total) | Response Example |
| |||||
| Ease of use | 11 (32.4%) | Easy to use | Lack of ubiquity | 10 (30.3%) | Not enough people using it |
| Group texting feature | 11 (32.4%) | Ability to communicate with entire teameveryone seeing same message | Inconsistent usage | 8 (24.2%) | No one used it reliably |
| Speed | 8 (23.5%) | Faster than a page to send a message | Reliability of message transmission | 5 (15.2%) | Big negative is it requires Wi‐Fi |
| Accessibility | 5 (14.7%) | Able to get messages across quickly and anywhere without a computer | Missed message alerts | 4 (12.1%) | Unable to reliably know message was received if phone on silent |
| Efficiency | 4 (11.8%) | Very efficient way to communicate | Password login | 3 (9.1%) | Having to type a 6‐digit password in |
| Real‐time communication | 2 (5.9%) | Real‐time results | User interface | 2 (6.1%) | Interface is a little convoluted |
| No character limitation | 2 (5.9%) | No limit on words | Other | 10 (30.3%) | Not sure if all of the texts were relevant |
| Other | 4 (11.8%) | Great UI | |||
HCGM User Experience
When asked if they would recommend using an HCGM system to facilitate communication on the internal medicine wards, 85% of HCGM participants replied yes, 15% reported not sure, and 0% reported no. Based on free response entries, HCGM's most effective features (Table 5) included ease of use, group texting capacity, and speed (32.4%, 32.4%, and 23.5% of 34 respondents, respectively); its most ineffective aspects (Table 5) included lack of ubiquity, inconsistent usage by those with access to the application, and reliability of message transmission (30.3%, 24.2%, and 15.2% of 33 respondents, respectively).
DISCUSSION
We are the first to report that smartphone‐based, HIPAA‐compliant, group messaging applications improve provider perception of in‐hospital communication, while providing the information security that paging and commercial cellular networks do not. HCGM participants rated the application more favorably than paging in terms of clarity and efficiency of communication. These findings may be attributed to the expanded functionality offered by the application, including no character limit per HCGM text, the ability to use special characters such as slashes and ampersands, group texting, and the ability to reply immediately. HCGM may result in more efficient communication by facilitating direct two‐way communication via smartphones, whereas sending or returning pages requires a landline or computer.
HCGM participants rated the application higher than paging in terms of workflow integration during rounds and patient discharge, but not during patient admissions and teaching sessions. We had hypothesized that HCGM would integrate better into participants' workflows because HCGM texts could be replied to immediately. The reasons for the equivalence of HCGM and paging for workflow integration during patient admissions and teaching sessions may have been due to weak Wi‐Fi in certain areas of the hospital, and may warrant further investigation.
Analysis of HCGM utilization indicated that there were factors that made participants more or less likely to use the application. Individuals who reported that their attendings used HCGM regularly were more likely to use it themselves. Attending usage may legitimize use of HCGM for housestaff and medical students, who may otherwise feel that texting appears unprofessional. Participants who texted frequently in their personal lives were also more likely to utilize HCGM regularly, perhaps due to increased familiarity with/affinity for the platform.
HCGM participants who did not utilize the application regularly most often cited the fact that other team members did not use it. Among all users, the most frequently noted ineffective aspects of the application were its lack of ubiquity (HCGM was made available only to the small subset of individuals involved in the study) and inconsistent usage by those who did have access to the application. These findings suggest that HCGM effectiveness may be maximized with unrestricted access and mandated use; patchwork implementation, as in this study, detracts from perceived effectiveness.
Though objective outcome measures (average length of stay and average time of discharge) for patients of control attendings and HCGM attendings were examined, no significant differences were observed (P=0.089 and 0.494, respectively). These results may be due to the small size and short duration of the study.
Limitations
Our study had several limitations. HCGM was available only to individuals in the experimental arm of the study; most members of the internal medicine department and all other departments were not reachable through the application. This lack of ubiquity was a frequently cited frustration. Among individuals to whom HCGM was made available, barriers to adoption included: close proximity to would‐be message recipients, concern that smartphone usage in front of patients might appear unprofessional, and inconsistent or dropped service (weak or no Wi‐Fi signal in some areas). A technical problem with the Android platform midway through the study served as a potential frustration to several participants.
Due to the aforementioned issues, some participants used the HCGM application in a very limited way. We also did not replace hospital pagers (infeasible in this hospital setting); the HCGM application was added as a supplemental system. Future studies might explore the replacement of paging systems with HCGM‐type applications, as well as delve further into quantitative patient care outcomes.
It should be noted that the start of the study unintentionally coincided with the start of new interns and medical students in the hospital. Although it is possible that their relative unfamiliarity with the hospital may have made them more amenable to adopting a new technology, it is also possible that they may have been less likely to do so in the midst of such a major transitional period. Finally, this was a single‐site study, and as such, its findings may not be broadly generalizable. More research on such interventions is warranted, particularly in the context of current insecure communication methods such as paging that may make hospital‐wide adoption of new methods of secure communication, such as HCGM, mandatory.
CONCLUSION
Our study is the first to demonstrate that HCGM applications improve healthcare provider perception of multiple measures of in‐hospital communication, including efficiency of communication, workflow integration, and overall satisfaction. Notably, 85% of HCGM team respondents said they would recommend using an HCGM system on the wards. As smartphone use is expected to continue to increase among physicians and the general population, it is increasingly important to understand how to utilize these powerful communication tools to improve healthcare in an effective and secure manner.
Acknowledgements
The authors would like to thank the Stanford Medicine Residency Program and Stanford Hospital and Clinics for allowing them to perform the study, as well as Medigram, Inc., for supplying gift cards to incentivize survey completion and loaner iPhones to allow individuals without smartphones to participate in the study.
Disclosures: Stanford University School of Medicine's Medical Scholars Program provided financial support to the first author over the course of the study. Medigram, Inc. funded gift cards given to both control and HCGM participants upon survey completion and provided loaner iPhones to allow individuals without smartphones to participate in the study. Medigram, Inc. has also paid the fee for OnlineOpen to provide open access to this article. This study received an institutional review board exemption as quality improvement research. Participation was voluntary, and all participants signed a consent form. The authors report no conflicts of interest.
Pagers, though reliable and familiar technology, can be suboptimal for facilitating healthcare team communication.[1, 2] Most paging systems utilize single‐function pagers and only allow one‐way communication, requiring recipients to disrupt workflow to respond to pages. Paging transmissions can also be intercepted, and the information presented on pager displays can be viewed by anyone in possession of the pager.
Smartphones allow for instantaneous two‐way and group communication through advanced technological features. Their use is widespread; over 81% of American physicians owned a smartphone in 2011.[3] Previous studies demonstrate that healthcare providers rate smartphone‐based email positively, and that team smartphones can facilitate communication between nurses and physicians.[4, 5] However, these studies specifically examined the utility of smartphone‐based email and voice calls, and did not include text messaging. Limitations of traditional smartphone‐based text messaging include Health Insurance Portability and Accountability Act (HIPAA) noncompliance and dependence on in‐hospital cellular reception, which can be unreliable. HIPAA is a 1996 US federal law that established a set of privacy and security rules governing not only what is considered protected health information (PHI), but also minimum standards for the protection of such information. HIPAA compliance is defined as meeting these minimum standards for physical, network, and process security.[6, 7] Though PHI is often transmitted via paging systems and commercial carrier‐based text messaging, these modalities are not secure and are thus not HIPAA‐compliant.
Text messaging applications that address these security and reliability issues have the potential to greatly enhance in‐hospital communication. We hypothesized that a smartphone‐based HIPAA‐compliant group messaging application could improve in‐hospital communication on the inpatient medicine service. To our knowledge, our study is the first to examine a HIPAA‐compliant text messaging system, and also the first to compare a combination paging/HIPAA‐compliant group messaging (HCGM) system with a paging‐only system in assessing healthcare provider perception of communication efficiency.
METHODS
Intervention
This study utilized Medigram (Medigram, Inc.,
Study Design
In an eight‐week prospective, cluster‐randomized, controlled trial conducted at Stanford Hospital (June 25, 2012August 17, 2012), three of five inpatient medicine teams were randomized to use Medigram in addition to the existing hospital paging system (HCGM teams); the remaining two teams were assigned to use hospital paging only (control teams). Each team included one attending physician, one resident, two interns, two medical students, and a case manager. According to prescheduled rotations, attendings rotated every two weeks, and residents, interns, and medical students rotated every four weeks. All rotations were either off‐service or off‐site, with the exception of two attendings who rotated between study teams but within their experimental designations. Case managers remained with the same team. Additionally, the satellite pharmacy was provided with an HCGM‐equipped smartphone to communicate with experimental teams.
Participation was voluntary, with a 96% participation rate (n=75). HCGM teams downloaded the free application onto their smartphones. Participants without smartphones were provided with one for the duration of the study. Proper application use was demonstrated by one researcher in a 10‐minute standardized presentation. HCGM teams were encouraged to use the application in lieu of paging, except when patient care could be compromised.
All participants completed linked baseline and post‐study surveys. Gift cards valued at $10 were provided on completion of each survey. Though participants were assigned to either HCGM or control groups based on the randomized assignment of their preset cluster (hospital team) to an HCGM or control group, analysis was performed on the individual level due to the hospital's set rotation schedule, which resulted in dynamic, frequently changing clusters. We also compared average length of stay and time of discharge for patients treated by control versus HCGM teams. Clinical outcome data were obtained from the hospital's database using Midas+ Statit Solutions (Midas+ Statit Solutions Group, Tucson, AZ). Survey and clinical outcome data were analyzed in Stata (StataCorp, College Station, TX) and R (R Foundation for Statistical Computing, Vienna, Austria).
Survey Design and Analysis
Identical, anonymous baseline surveys were administered to control and HCGM teams. These surveys assessed attitudes toward the hospital paging system using a 5‐point Likert scale (1=low, 5=high) to evaluate perceived measures of effectiveness, workflow integration, and overall satisfaction. Wilcoxon rank sum tests were used to compare control and HCGM group responses to these questions. Free response questions asked participants to list the most effective and ineffective aspects of the paging system.
Post‐study surveys included all baseline survey questions, as well as questions about personal texting behavior. Post‐study HCGM surveys also included a parallel set of questions rating the HCGM application on the same measures of perceived effectiveness, workflow integration, and overall satisfaction. Wilcoxon signed rank tests were used to compare HCGM participants' baseline evaluations of paging to their post‐study evaluations of the HCGM application. Baseline and post‐study surveys were linked by the last four digits of respondent cell phone numbers. To compare control and HCGM group perceptions of the hospital paging system at study completion, post‐study survey responses were evaluated using Wilcoxon rank sum tests. The family‐wise error rate was left unadjusted due to concerns around inflated type II errors, given the high degree of correlation between survey questions.
All free response questions were analyzed using thematic analysis and grounded theory. After reviewing responses to each question, a list of overarching themes was constructed. Two researchers then independently reviewed each free‐response entry to assign it to one or more of these themes (some responses included several ideas with distinct themes). Entries with concordant theme assignments (90%) were coded as such; nonconcordant entries required an additional round of review to reach concordance. Finally, objective outcome measures including length of stay and time of discharge were analyzed by two‐sample t test.
| Control Group | HCGM Group | |
|---|---|---|
| ||
| Paired surveys collected (completion rate) | 22 (85%) | 41 (84%) |
| Average age 95% CI | 30.10 1.71 | 30.95 2.94 |
| Gender | ||
| Male | 13 (59%) | 24 (59%) |
| Female | 9 (41%) | 17 (41%) |
| Role | ||
| Medical students | 6 (27%) | 11 (27%) |
| Interns (PGY 1) | 7 (32%) | 12 (29%) |
| Residents (PGY2 and 3) | 3 (14%) | 6 (15%) |
| Attending physicians | 5 (23%) | 5 (12%) |
| Case managers | 1 (5%) | 3 (7%) |
| Pharmacists | 0 (0%) | 4 (10%) |
Information Security
The HCGM application in this study features 256‐bit encryption technology and requires a six‐digit password to access texts. For added security, a study‐dedicated server (HP ProLiant DL 180 G6; Hewlett‐Packard Co., Palo Alto, CA) with 4‐TB hard drive capacity (4 Seagate Barracuda ST1000DM003 1 TB 7200 RPM internal hard drives; Seagate Technology PLC, Cupertino, CA) was installed in the Stanford School of Medicine Data Center to store encrypted text messages. Data stored on the phones/server were accessible only to study participants, not researchers. These security measures were approved by Stanford Hospital and Stanford School of Medicine's security and privacy review process.
Hospital Paging System
Stanford Hospital and Clinics is a quaternary care academic medical center with 613 beds, 49 operating rooms, and over 25,000 inpatient admissions per year.[8] The institution uses one‐way alphanumeric pagers (primary model: Daviscomm BR802 Flex Pager from USA Mobility, secondary model: Sun Telecom Titan 3 Plus from USA Mobility; USA Mobility Inc., Springfield, VA). USA Mobility operates the largest one‐ and two‐way paging networks in the United States.[9]
RESULTS
Of 26 control and 49 HCGM group members participating in the study, linked baseline and post‐study surveys were collected for 22 control and 41 HCGM participants (completion rates of 84.6% and 83.7%, respectively). To minimize recall bias, surveys not completed within a prespecified timeframe upon entering or leaving a team (two days attendings, four days others) were excluded.
Control and HCGM Group Characteristics
Control and HCGM groups were well matched demographically (Table 1). The average ages of control and HCGM group members were 30.10 and 30.95, respectively. Both groups were 59% male and 41% female.
| What do you find effective about the current hospital paging system? | What do you find ineffective about the current hospital paging system? | ||||
|---|---|---|---|---|---|
| Theme | No. of Respondents, (% of Total) | Response Example | Theme | No. of Respondents, (% of Total) | Response Example |
| |||||
| Reliability of message transmission | 17 (30.4%) | Everyone is able to receive the pages I send, regardless of service | Time wasted waiting for a response | 17 (29.3%) | Inefficient use of time waiting for reply |
| Ability to text page | 14 (25.0%) | Text paging allows targeted questions | One‐way nature of communication | 14 (24.1%) | Cannot text back instantly |
| Ease of use | 8 (14.3%) | Easy to use | Needing to find a computer to send a text page | 12 (20.7%) | Have to find an available computer to send a page |
| Search function | 5 (8.9%) | Search function is pretty effective in finding the people you're looking for | Character limitation | 10 (17.2%) | Length of text allowed too short |
| Ubiquity | 5 (8.9%) | Everyone is on paging system | Search function | 6 (10.3%) | Delay in looking people up in the system |
| Speed | 4 (7.1%) | Fast | Finding a phone to return a page | 5 (8.6%) | When you receive a page you need to find a phone |
| Loud alerts | 4 (7.1%) | Pager loud enough to hear all the time | Receipt of page uncertain | 3 (5.2%) | Unknown if page received |
| Staff responsiveness to pages | 4 (7.1%) | I know MD has to be onsite or covering the pager so someone eventually will call back | Sender's pager number not always included in page | 3 (5.2%) | Not everyone puts their pager number when they page. Then it's impossible to get back to them. |
| Brevity of messages | 3 (5.4%) | Requires very brief messages (easier for recipient) | Needing to remain near a phone while waiting for a page response | 3 (5.2%) | Wait by a phone for someone to call back; sometimes they do not call back |
| Helpful page operators | 2 (3.6%) | Page operators very helpful | Reliability of message transmission | 3 (5.2%) | Sometimes messages don't go through |
| Other | 10 (17.9%) | It's online and allows paging from anywhere there's internet access | Other | 11 (19.0%) | You cannot text with patient info on it |
A similar distribution of team member roles was observed in both groups, with two exceptions. First, the proportion of attending respondents in the HCGM group was lower than in the control group. This was due to the fact that several HCGM attendings entered discrepant ID codes on their surveys, thus making it impossible to link baseline and post‐study responses; these data were excluded. Additionally, two HCGM attendings were on service for four, rather than the standard two weeks, meaning two additional data points from unique attendings could not be obtained. Second, the experimental group included four pharmacists, whereas the control group did not. As a sensitivity test, we analyzed the data excluding the pharmacists, and this did not change our results.
Baseline Evaluations of the Hospital Paging System
At baseline, there were no significant differences between control and HCGM participants' perceptions of paging effectiveness (see Supporting Table 1, in the online version of this article). On a 5‐point rating scale (1=low, 5=high), 63 subjects rated their overall satisfaction with the paging system an average of 2.79 (95% confidence interval: 2.55‐3.03).
In free response questions, components of the paging system most frequently cited as effective included: reliability of message transmission, alphanumeric text paging, and ease of use (30.4%, 25.0%, and 14.3% of 56 respondents, respectively) (Table 2). Ineffective aspects included: time wasted waiting for responses to pages, the unidirectional nature of pagers, and needing to find a computer to send a text page (29.3%, 24.1%, and 20.7% of 58 respondents, respectively) (Table 2).
| Question | Baseline Average Rating of Paging System* | Post‐Study Average Rating of HCGM Application | P Value |
|---|---|---|---|
| |||
| Rate the effectiveness of each in allowing you to | |||
| Communicate your thoughts clearly | 3.194 | 3.806 | 0.010 |
| Communicate your thoughts efficiently | 3.200 | 3.829 | 0.009 |
| Send messages to other hospital staff | 3.543 | 3.571 | 0.480 |
| Receive messages/stay informed in real time | 3.222 | 3.306 | 0.405 |
| Rate the effectiveness of each in integrating into your workflow during | |||
| Work rounds | 2.313 | 3.000 | 0.018 |
| Patient discharge | 2.448 | 3.276 | 0.012 |
| Patient admissions | 2.862 | 2.621 | 0.238 |
| Teaching sessions | 2.292 | 2.458 | 0.448 |
| Overall satisfaction | 2.811 | 3.459 | 0.003 |
Baseline Utilization of Text Messaging
The majority of participants were familiar with text messaging and regularly used it personally and professionally prior to the start of the study. 90.5% of participants (n = 63) reported sending an average of 1 personal text messages per day, with the largest proportion (39.7%) sending 1‐5 texts per day (see Supporting Figure 1A in the online version of this article). 58.1% of respondents (n=62) reported sending an average of 1 text messages per day related to patient care (see Supporting Figure 1B in the online version of this article), with the largest fraction (58.3%) sending 1‐5 texts per day.
HCGM Adoption and Usage Patterns
Active use of HCGM was defined as using the application to send or receive an average of 1 text messages per day. Of HCGM participants, 67% self‐reported 1 week of active use of the application, indicating a strong compliance rate. Among non‐attendings, 70% reported sending 1 or more texts to other team members per day; this percentage increased to 86% among those whose attendings texted them at least once per day (47% of non‐attendings). Respondents who text frequently in their personal lives (>5 texts/day) were more likely to use the application; 90% of these respondents sent 1 or more HCGM texts per day.
Among 12 subjects who did not report sending or receiving 1 HCGM text/day, the top three reasons were: other team members were not using it (67%), no need to use it given the close proximity of other team members (67%), and other (33%). A Wilcoxon rank sum test was used to compare the ages of active versus nonactive users; no significant age difference was found (P=0.200).
To provide an objective measure of application adoption, usage data for each HCGM participant were obtained from the application developers. Because much of the study's first week was spent onboarding and instructing participant, the first week was not included in the analysis. Of 43 individuals enrolled in the study for at least one of the seven remaining weeks, 56% sent a total of 5 texts, 44% sent 10 texts, and 28% sent 20 texts. HCGM users on three teams sent an aggregate mean of 123 texts/week. Data on number of messages received by each user were not available.
Perceived Effectiveness: Paging Versus HCGM
In post‐study surveys, HCGM participants rated HCGM significantly higher (P<0.05) than paging (Table 3) in terms of ability to communicate thoughts clearly (P=0.010) and efficiently (P=0.009). HCGM was also deemed more effective at integrating into workflow during rounds (P=0.018) and patient discharge (P=0.012). Overall satisfaction with HCGM was also significantly higher (P=0.003).
| Control (n=22) | HCGM (n=41) | |||||
|---|---|---|---|---|---|---|
| Baseline Mean | Post‐Study Mean | P Value* | Baseline Mean | Post‐Study Mean | P Value* | |
| ||||||
| Rate the effectiveness of each in allowing you to | ||||||
| Communicate your thoughts clearly | 2.905 | 2.619 | 0.103 | 3.250 | 2.850 | 0.004 |
| Communicate your thoughts efficiently | 2.952 | 2.762 | 0.106 | 3.250 | 2.825 | 0.018 |
| Send messages to other hospital staff | 3.762 | 3.190 | 0.019 | 3.550 | 3.450 | 0.253 |
| Receive messages/stay informed in real time | 3.667 | 2.857 | 0.002 | 3.300 | 2.900 | 0.031 |
| Rate the effectiveness of each in integrating into your workflow during | ||||||
| Work rounds | 2.429 | 2.476 | 0.303 | 2.410 | 2.718 | 0.078 |
| Patient discharge | 2.500 | 2.350 | 0.251 | 2.472 | 2.861 | 0.071 |
| Patient admissions | 2.905 | 2.524 | 0.020 | 2.889 | 3.000 | 0.384 |
| Teaching sessions | 2.143 | 2.200 | 0.386 | 2.367 | 2.400 | 0.418 |
Comparison of Pre‐ and Post‐study Perceived Effectiveness of the Hospital Paging System
In post‐study evaluations, both control and HCGM participants rated the paging system's effectiveness less favorably (P<0.05) compared to baseline in terms of ability to receive messages/stay informed in real time (control P=0.002, HCGM P=0.031) (Table 4). Controls also reported a decrease from baseline in perceived effectiveness of paging in terms of ability to send messages (P=0.019) and integrate into workflow during patient admissions (P=0.020). HCGM participants found paging less effective at communicating thoughts clearly (P=0.004) and efficiently (P=0.018). No significant differences existed between control and HCGM groups' average assessments of paging at the conclusion of the study (see Supporting Table 2, in the online version of this article).
| What do you find effective about the Medigram system? | What do you find ineffective about the Medigram system? | ||||
|---|---|---|---|---|---|
| Theme | No. of Respondents, (% of Total) | Response Example | Theme | No. of Respondents, (% of Total) | Response Example |
| |||||
| Ease of use | 11 (32.4%) | Easy to use | Lack of ubiquity | 10 (30.3%) | Not enough people using it |
| Group texting feature | 11 (32.4%) | Ability to communicate with entire teameveryone seeing same message | Inconsistent usage | 8 (24.2%) | No one used it reliably |
| Speed | 8 (23.5%) | Faster than a page to send a message | Reliability of message transmission | 5 (15.2%) | Big negative is it requires Wi‐Fi |
| Accessibility | 5 (14.7%) | Able to get messages across quickly and anywhere without a computer | Missed message alerts | 4 (12.1%) | Unable to reliably know message was received if phone on silent |
| Efficiency | 4 (11.8%) | Very efficient way to communicate | Password login | 3 (9.1%) | Having to type a 6‐digit password in |
| Real‐time communication | 2 (5.9%) | Real‐time results | User interface | 2 (6.1%) | Interface is a little convoluted |
| No character limitation | 2 (5.9%) | No limit on words | Other | 10 (30.3%) | Not sure if all of the texts were relevant |
| Other | 4 (11.8%) | Great UI | |||
HCGM User Experience
When asked if they would recommend using an HCGM system to facilitate communication on the internal medicine wards, 85% of HCGM participants replied yes, 15% reported not sure, and 0% reported no. Based on free response entries, HCGM's most effective features (Table 5) included ease of use, group texting capacity, and speed (32.4%, 32.4%, and 23.5% of 34 respondents, respectively); its most ineffective aspects (Table 5) included lack of ubiquity, inconsistent usage by those with access to the application, and reliability of message transmission (30.3%, 24.2%, and 15.2% of 33 respondents, respectively).
DISCUSSION
We are the first to report that smartphone‐based, HIPAA‐compliant, group messaging applications improve provider perception of in‐hospital communication, while providing the information security that paging and commercial cellular networks do not. HCGM participants rated the application more favorably than paging in terms of clarity and efficiency of communication. These findings may be attributed to the expanded functionality offered by the application, including no character limit per HCGM text, the ability to use special characters such as slashes and ampersands, group texting, and the ability to reply immediately. HCGM may result in more efficient communication by facilitating direct two‐way communication via smartphones, whereas sending or returning pages requires a landline or computer.
HCGM participants rated the application higher than paging in terms of workflow integration during rounds and patient discharge, but not during patient admissions and teaching sessions. We had hypothesized that HCGM would integrate better into participants' workflows because HCGM texts could be replied to immediately. The reasons for the equivalence of HCGM and paging for workflow integration during patient admissions and teaching sessions may have been due to weak Wi‐Fi in certain areas of the hospital, and may warrant further investigation.
Analysis of HCGM utilization indicated that there were factors that made participants more or less likely to use the application. Individuals who reported that their attendings used HCGM regularly were more likely to use it themselves. Attending usage may legitimize use of HCGM for housestaff and medical students, who may otherwise feel that texting appears unprofessional. Participants who texted frequently in their personal lives were also more likely to utilize HCGM regularly, perhaps due to increased familiarity with/affinity for the platform.
HCGM participants who did not utilize the application regularly most often cited the fact that other team members did not use it. Among all users, the most frequently noted ineffective aspects of the application were its lack of ubiquity (HCGM was made available only to the small subset of individuals involved in the study) and inconsistent usage by those who did have access to the application. These findings suggest that HCGM effectiveness may be maximized with unrestricted access and mandated use; patchwork implementation, as in this study, detracts from perceived effectiveness.
Though objective outcome measures (average length of stay and average time of discharge) for patients of control attendings and HCGM attendings were examined, no significant differences were observed (P=0.089 and 0.494, respectively). These results may be due to the small size and short duration of the study.
Limitations
Our study had several limitations. HCGM was available only to individuals in the experimental arm of the study; most members of the internal medicine department and all other departments were not reachable through the application. This lack of ubiquity was a frequently cited frustration. Among individuals to whom HCGM was made available, barriers to adoption included: close proximity to would‐be message recipients, concern that smartphone usage in front of patients might appear unprofessional, and inconsistent or dropped service (weak or no Wi‐Fi signal in some areas). A technical problem with the Android platform midway through the study served as a potential frustration to several participants.
Due to the aforementioned issues, some participants used the HCGM application in a very limited way. We also did not replace hospital pagers (infeasible in this hospital setting); the HCGM application was added as a supplemental system. Future studies might explore the replacement of paging systems with HCGM‐type applications, as well as delve further into quantitative patient care outcomes.
It should be noted that the start of the study unintentionally coincided with the start of new interns and medical students in the hospital. Although it is possible that their relative unfamiliarity with the hospital may have made them more amenable to adopting a new technology, it is also possible that they may have been less likely to do so in the midst of such a major transitional period. Finally, this was a single‐site study, and as such, its findings may not be broadly generalizable. More research on such interventions is warranted, particularly in the context of current insecure communication methods such as paging that may make hospital‐wide adoption of new methods of secure communication, such as HCGM, mandatory.
CONCLUSION
Our study is the first to demonstrate that HCGM applications improve healthcare provider perception of multiple measures of in‐hospital communication, including efficiency of communication, workflow integration, and overall satisfaction. Notably, 85% of HCGM team respondents said they would recommend using an HCGM system on the wards. As smartphone use is expected to continue to increase among physicians and the general population, it is increasingly important to understand how to utilize these powerful communication tools to improve healthcare in an effective and secure manner.
Acknowledgements
The authors would like to thank the Stanford Medicine Residency Program and Stanford Hospital and Clinics for allowing them to perform the study, as well as Medigram, Inc., for supplying gift cards to incentivize survey completion and loaner iPhones to allow individuals without smartphones to participate in the study.
Disclosures: Stanford University School of Medicine's Medical Scholars Program provided financial support to the first author over the course of the study. Medigram, Inc. funded gift cards given to both control and HCGM participants upon survey completion and provided loaner iPhones to allow individuals without smartphones to participate in the study. Medigram, Inc. has also paid the fee for OnlineOpen to provide open access to this article. This study received an institutional review board exemption as quality improvement research. Participation was voluntary, and all participants signed a consent form. The authors report no conflicts of interest.
- . Communication systems in healthcare. Clin Biochem Rev. 2006;27:89–98.
- , , . Alphanumeric paging: a potential source of problems in patient care and communication. J Surg Educ. 2011;68:447–451.
- Manhattan Research. Taking the pulse: US market research report. Available at: http://manhattanresearch.com/Products‐and‐Services/Physician/Physician‐Research‐Modules. Accessed February 6, 2013.
- , , , et al. The use of wireless e‐mail to improve healthcare team communication. J Am Med Inform Assoc. 2009;16:705–713.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5:553–559.
- US Department of Health and Human Services. Summary of the HIPAA privacy rule. Available at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/summary/. Accessed May 11, 2013.
- United States Department of Health and Human Services. Summary of the HIPAA security rule. Available at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/srsummary.html. Accessed May 11, 2013.
- Stanford University. Stanford facts: about Stanford. Available at: http://facts.stanford.edu/about/hospital. Accessed October 12, 2013.
- Wikinvest. USA mobility. Available at: http://www.wikinvest.com/stock/USA_Mobility_(USMO). Accessed February 6, 2013.
- . Communication systems in healthcare. Clin Biochem Rev. 2006;27:89–98.
- , , . Alphanumeric paging: a potential source of problems in patient care and communication. J Surg Educ. 2011;68:447–451.
- Manhattan Research. Taking the pulse: US market research report. Available at: http://manhattanresearch.com/Products‐and‐Services/Physician/Physician‐Research‐Modules. Accessed February 6, 2013.
- , , , et al. The use of wireless e‐mail to improve healthcare team communication. J Am Med Inform Assoc. 2009;16:705–713.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5:553–559.
- US Department of Health and Human Services. Summary of the HIPAA privacy rule. Available at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/summary/. Accessed May 11, 2013.
- United States Department of Health and Human Services. Summary of the HIPAA security rule. Available at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/srsummary.html. Accessed May 11, 2013.
- Stanford University. Stanford facts: about Stanford. Available at: http://facts.stanford.edu/about/hospital. Accessed October 12, 2013.
- Wikinvest. USA mobility. Available at: http://www.wikinvest.com/stock/USA_Mobility_(USMO). Accessed February 6, 2013.
© 2014 The Authors Journal of Hospital Medicine published by Wiley Periodicals, Inc. on behalf of Society of Hospital Medicine
Generating Mortality Predictions
The systematic deployment of prediction rules within health systems remains a challenge, although such decision aids have been available for decades.[1, 2] We previously developed and validated a prediction rule for 30‐day mortality in a retrospective cohort, noting that the mortality risk is associated with a number of other clinical events.[3] These relationships suggest risk strata, defined by the predicted probability of 30‐day mortality, and could trigger a number of coordinated care processes proportional to the level of risk.[4] For example, patients within the higher‐risk strata could be considered for placement into an intermediate or intensive care unit (ICU), be monitored more closely by physician and nurse team members for clinical deterioration, be seen by a physician within a few days of hospital discharge, and be considered for advance care planning discussions.[3, 4, 5, 6, 7] Patients within the lower‐risk strata might not need the same intensity of these processes routinely unless some other indication were present.
However attractive this conceptual framework may be, its realization is dependent on the willingness of clinical staff to generate predictions consistently on a substantial portion of the patient population, and on the accuracy of the predictions when the risk factors are determined with some level of uncertainty at the beginning of the hospitalization.[2, 8] Skepticism is justified, because the work involved in completing the prediction rule might be incompatible with existing workflow. A patient might not be scored if the emergency physician lacks time or if technical issues arise with the information system and computation process.[9] There is also a generic concern that the predictions will prove to be less accurate outside of the original study population.[8, 9, 10] A more specific concern for our rule is how well present on admission diagnoses can be determined during the relatively short emergency department or presurgery evaluation period. For example, a final diagnosis of heart failure might not be established until later in the hospitalization, after the results of diagnostic testing and clinical response to treatment are known. Moreover, our retrospective prediction rule requires an assessment of the presence or absence of sepsis and respiratory failure. These diagnoses appear to be susceptible to secular trends in medical record coding practices, suggesting the rule's accuracy might not be stable over time.[11]
We report the feasibility of having emergency physicians and the surgical preparation center team generate mortality predictions before an inpatient bed is assigned. We evaluate and report the accuracy of these prospective predictions.
METHODS
The study population consisted of all patients 18 years of age or less than 100 years who were admitted from the emergency department or assigned an inpatient bed following elective surgery at a tertiary, community teaching hospital in the Midwestern United States from September 1, 2012 through February 15, 2013. Although patients entering the hospital from these 2 pathways would be expected to have different levels of mortality risk, we used the original prediction rule for both because such distinctions were not made in its derivation and validation. Patients were not considered if they were admitted for childbirth or other obstetrical reasons, admitted directly from physician offices, the cardiac catheterization laboratory, hemodialysis unit, or from another hospital. The site institutional review board approved this study.
The implementation process began with presentations to the administrative and medical staff leadership on the accuracy of the retrospectively generated mortality predictions and risk of other adverse events.[3] The chief medical and nursing officers became project champions, secured internal funding for the technical components, and arranged to have 2 project comanagers available. A multidisciplinary task force endorsed the implementation details at biweekly meetings throughout the planning year. The leadership of the emergency department and surgical preparation center committed their colleagues to generate the predictions. The support of the emergency leadership was contingent on the completion of the entire prediction generating process in a very short time (within the time a physician could hold his/her breath). The chief medical officer, with the support of the leadership of the hospitalists and emergency physicians, made the administrative decision that a prediction must be generated prior to the assignment of a hospital room.
During the consensus‐building phase, a Web‐based application was developed to generate the predictions. Emergency physicians and surgical preparation staff were trained on the definitions of the risk factors (see Supporting Information, Appendix, in the online version of this article) and how to use the Web application. Three supporting databases were created. Each midnight, a past medical history database was updated, identifying those who had been discharged from the study hospital in the previous 365 days, and whether or not their diagnoses included atrial fibrillation, leukemia/lymphoma, metastatic cancer, cancer other than leukemia, lymphoma, cognitive disorder, or other neurological conditions (eg, Parkinson's, multiple sclerosis, epilepsy, coma, and stupor). Similarly, a clinical laboratory results database was created and updated real time through an HL7 (Health Level Seven, a standard data exchange format[12]) interface with the laboratory information system for the following tests performed in the preceding 30 days at a hospital‐affiliated facility: hemoglobin, platelet count, white blood count, serum troponin, blood urea nitrogen, serum albumin, serum lactate, arterial pH, arterial partial pressure of oxygen values. The third database, admission‐discharge‐transfer, was created and updated every 15 minutes to identify patients currently in the emergency room or scheduled for surgery. When a patient registration event was added to this database, the Web application created a record, retrieved all relevant data, and displayed the patient name for scoring. When the decision for hospitalization was made, the clinician selected the patient's name and reviewed the pre‐populated medical diagnoses of interest, which could be overwritten based on his/her own assessment (Figure 1A,B). The clinician then indicated (yes, no, or unknown) if the patient currently had or was being treated for each of the following: injury, heart failure, sepsis, respiratory failure, and whether or not the admitting service would be medicine (ie, nonsurgical, nonobstetrical). We considered unknown status to indicate the patient did not have the condition. When laboratory values were not available, a normal value was imputed using a previously developed algorithm.[3] Two additional questions, not used in the current prediction process, were answered to provide data for a future analysis: 1 concerning the change in the patient's condition while in the emergency department and the other concerning the presence of abnormal vital signs. The probability of 30‐day mortality was calculated via the Web application using the risk information supplied and the scoring weights (ie, parameter estimates) provided in the Appendices of our original publication.[3] Predictions were updated every minute as new laboratory values became available, and flagged with an alert if a more severe score resulted.
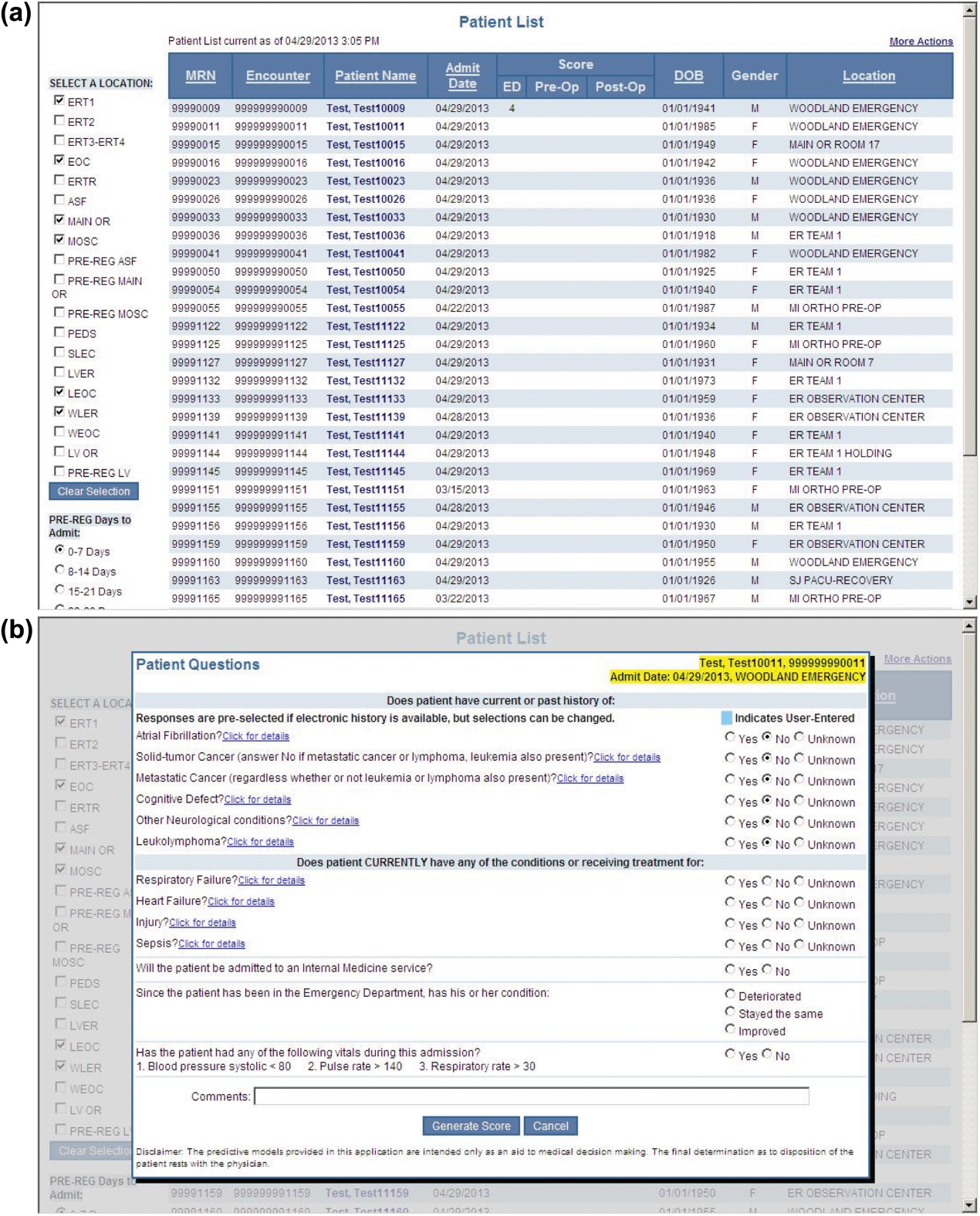
For the analyses of this study, the last prospective prediction viewed by emergency department personnel, a hospital bed manager, or surgical suite staff prior to arrival on the nursing unit is the one referenced as prospective. Once the patient had been discharged from the hospital, we generated a second mortality prediction based on previously published parameter estimates applied to risk factor data ascertained retrospectively as was done in the original article[3]; we subsequently refer to this prediction as retrospective. We will report on the group of patients who had both prospective and retrospective scores (1 patient had a prospective but not retrospective score available).
The prediction scores were made available to the clinical teams gradually during the study period. All scores were viewable by the midpoint of the study for emergency department admissions and near the end of the study for elective‐surgery patients. Only 2 changes in care processes based on level of risk were introduced during the study period. The first required initial placement of patients having a probability of dying of 0.3 or greater into an intensive or intermediate care unit unless the patient or family requested a less aggressive approach. The second occurred in the final 2 months of the study when a large multispecialty practice began routinely arranging for high‐risk patients to be seen within 3 or 7 days of hospital discharge.
Statistical Analyses
SAS version 9.3 (SAS Institute Inc., Cary, NC) was used to build the datasets and perform the analyses. Feasibility was evaluated by the number of patients who were candidates for prospective scoring with a score available at the time of admission. The validity was assessed with the primary outcome of death within 30 days from the date of hospital admission, as determined from hospital administrative data and the Social Security Death Index. The primary statistical metric is the area under the receiver operating characteristic curve (AROC) and the corresponding 95% Wald confidence limits. We needed some context for understanding the performance of the prospective predictions, assuming the accuracy could deteriorate due to the instability of the prediction rule over time and/or due to imperfect clinical information at the time the risk factors were determined. Accordingly, we also calculated an AROC based on retrospectively derived covariates (but using the same set of parameter estimates) as done in our original publication so we could gauge the stability of the original prediction rule. However, the motivation was not to determine whether retrospective versus prospective predictions were more accurate, given that only prospective predictions are useful in the context of developing real‐time care processes. Rather, we wanted to know if the prospective predictions would be sufficiently accurate for use in clinical practice. A priori, we assumed the prospective predictions should have an AROC of approximately 0.80. Therefore, a target sample size of 8660 hospitalizations was determined to be adequate to assess validity, assuming a 30‐day mortality rate of 5%, a desired lower 95% confidence boundary for the area under the prospective curve at or above 0.80, with a total confidence interval width of 0.07.[13] Calibration was assessed by comparing the actual proportion of patients dying (with 95% binomial confidence intervals) with the mean predicted mortality level within 5 percentile increments of predicted risk.
Risk Strata
We categorize the probability of 30‐day mortality into strata, with the understanding that the thresholds for defining these are a work in progress. Our hospital currently has 5 strata ranging from level 1 (highest mortality risk) to level 5 (lowest risk). The corresponding thresholds (at probabilities of death of 0.005, 0.02, 0.07, 0.20) were determined by visual inspection of the event rates and slope of curves displayed in Figure 1 of the original publication.[3]
Relationship to Secondary Clinical Outcomes of Interest
The choice of clinical care processes triggered per level of risk may be informed by understanding the frequency of events that increase with the mortality risk. We therefore examined the AROC from logistic regression models for the following outcomes using the prospectively generated probability as an explanatory variable: unplanned transfer to an ICU within the first 24 hours for patients not admitted to an ICU initially, ICU use at some point during the hospitalization, the development of a condition not present on admission (complication), receipt of palliative care by the end of the hospitalization, death during the hospitalization, 30‐day readmission, and death within 180 days. The definition of these outcomes and statistical approach used has been previously reported.[3]
RESULTS
Mortality predictions were generated on demand for 7291 out of 7777 (93.8%) eligible patients admitted from the emergency department, and for 2021 out of 2250 (89.8%) eligible elective surgical cases, for a total of 9312 predictions generated out of a possible 10,027 hospitalizations (92.9%). Table 1 displays the characteristics of the study population. The mean age was 65.2 years and 53.8% were women. The most common risk factors were atrial fibrillation (16.4%) and cancer (14.6%). Orders for a comfort care approach (rather than curative) were entered within 4 hours of admission for 32/9312 patients (0.34%), and 9/9312 (0.1%) were hospice patients on admission.
| Risk Factors | No. | Without Imputation | No. | With Imputation |
|---|---|---|---|---|
| ||||
| Clinical laboratory values within preceding 30 days | ||||
| Maximum serum blood urea nitrogen (mg/dL) | 8,484 | 22.7 (17.7) | 9,312 | 22.3 (16.9) |
| Minimum hemoglobin, g/dL, | 8,750 | 12.5 (2.4) | 9,312 | 12.4 (2.4) |
| Minimum platelet count, 1,000/UL | 8,737 | 224.1 (87.4) | 9,312 | 225.2 (84.7) |
| Maximum white blood count, 1,000/UL | 8,750 | 10.3 (5.8) | 9,312 | 10.3 (5.6) |
| Maximum serum lactate, mEq/L | 1,749 | 2.2 (1.8) | 9,312 | 0.7 (1.1) |
| Minimum serum albumin, g/dL | 4,057 | 3.4 (0.7) | 9,312 | 3.2 (0.5) |
| Minimum arterial pH | 509 | 7.36 (0.10) | 9,312 | 7.36 (0.02) |
| Minimum arterial pO2, mm Hg | 509 | 73.6 (25.2) | 9,312 | 98.6 (8.4) |
| Maximum serum troponin, ng/mL | 3,217 | 0.5 (9.3) | 9,312 | 0.2 (5.4) |
| Demographics and diagnoses | ||||
| Age, y | 9,312 | 65.2 (17.0) | ||
| Female sex | 9,312 | 5,006 (53.8%) | ||
| Previous hospitalization within past 365 days | 9,312 | 3,995 (42.9%) | ||
| Emergent admission | 9,312 | 7,288 (78.3%) | ||
| Admitted to a medicine service | 9,312 | 5,840 (62.7%) | ||
| Current or past atrial fibrillation | 9,312 | 1,526 (16.4%) | ||
| Current or past cancer without metastases, excluding leukemia or lymphoma | 9,312 | 1,356 (14.6%) | ||
| Current or past history of leukemia or lymphoma | 9,312 | 145 (1.6%) | ||
| Current or past metastatic cancer | 9,312 | 363 (3.9%) | ||
| Current or past cognitive deficiency | 9,312 | 844 (9.1%) | ||
| Current or past history of other neurological conditions (eg, Parkinson's disease, multiple sclerosis, epilepsy, coma, stupor, brain damage) | 9,312 | 952 (10.2%) | ||
| Injury such as fractures or trauma at the time of admission | 9,312 | 656 (7.0%) | ||
| Sepsis at the time of admission | 9,312 | 406 (4.4%) | ||
| Heart failure at the time of admission | 9,312 | 776 (8.3%) | ||
| Respiratory failure on admission | 9,312 | 557 (6.0%) | ||
| Outcomes of interest | ||||
| Unplanned transfer to an ICU (for those not admitted to an ICU) within 24 hours of admission | 8,377 | 86 (1.0%) | ||
| Ever in an ICU during the hospitalization | 9,312 | 1,267 (13.6%) | ||
| Development of a condition not present on admission (complication) | 9,312 | 834 (9.0%) | ||
| Within hospital mortality | 9,312 | 188 (2.0%) | ||
| Mortality within 30 days of admission | 9,312 | 466 (5.0%) | ||
| Mortality within 180 days of admission | 9,312 | 1,070 (11.5%) | ||
| Receipt of palliative care by the end of the hospitalization | 9,312 | 314 (3.4%) | ||
| Readmitted to the hospital within 30 days of discharge (patients alive at discharge) | 9,124 | 1,302 (14.3%) | ||
| Readmitted to the hospital within 30 days of discharge (patients alive on admission) | 9,312 | 1,302 (14.0%) | ||
Evaluation of Prediction Accuracy
The AROC for 30‐day mortality was 0.850 (95% confidence interval [CI]: 0.833‐0.866) for prospectively collected covariates, and 0.870 (95% CI: 0.855‐0.885) for retrospectively determined risk factors. These AROCs are not substantively different from each other, demonstrating comparable prediction performance. Calibration was excellent, as indicated in Figure 2, in which the predicted level of risk lay within the 95% confidence limits of the actual 30‐day mortality for 19 out of 20 intervals of 5 percentile increments.
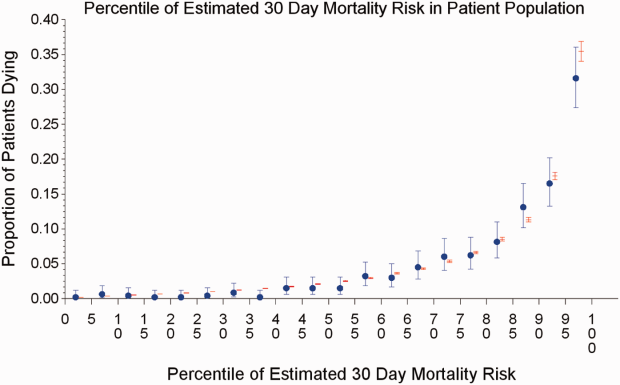
Relationship to Secondary Clinical Outcomes of Interest
The relationship between the prospectively generated probability of dying within 30 days and other events is quantified by the AROC displayed in Table 2. The 30‐day mortality risk has a strong association with the receipt of palliative care by hospital discharge, in‐hospital mortality, and 180‐day mortality, a fair association with the risk for 30‐day readmissions and unplanned transfers to intensive care, and weak associations with receipt of intensive unit care ever within the hospitalization or the development of a new diagnosis that was not present on admission (complication). The frequency of these events per mortality risk strata is shown in Table 3. The level 1 stratum contains a higher frequency of these events, whereas the level 5 stratum contains relatively few, reflecting the Pareto principle by which a relatively small proportion of patients contribute a disproportionate frequency of the events of interest.
| |
| In‐hospital mortality | 0.841 (0.8140.869) |
| 180day mortality | 0.836 (0.8250.848) |
| Receipt of palliative care by discharge | 0.875 (0.8580.891) |
| 30day readmission (patients alive at discharge) | 0.649 (0.6340.664) |
| Unplanned transfer to an ICU (for those not admitted to an ICU) within 24 hours | 0.643 (0.5900.696) |
| Ever in an ICU during the hospitalization | 0.605 (0.5880.621) |
| Development of a condition not present on admission (complication) | 0.555 (0.5350.575) |
| Risk Strata | 30‐Day Mortality, Count/Cases (%) | Unplanned Transfers to ICU Within 24 Hours, Count/Cases (%) | Diagnosis Not Present on Admission, Complication, Count/Cases (%) | Palliative Status at Discharge, Count/Cases (%) | Death in Hospital, Count/Cases (%) |
|---|---|---|---|---|---|
| Risk Strata | Ever in ICU, Count/Cases (%) | 30‐Day Readmission, Count/Cases (%) | Death or Readmission Within 30 Days, Count/Cases (%) | 180‐Day Mortality, Count/Cases (%) | |
| |||||
| 1 | 155/501 (30.9%) | 6/358 (1.7%) | 58/501 (11.6%) | 110/501 (22.0%) | 72/501 (14.4%) |
| 2 | 166/1,316 (12.6%) | 22/1,166 (1.9%) | 148/1,316 (11.3%) | 121/1,316 (9.2%) | 58/1,316 (4.4%) |
| 3 | 117/2,977 (3.9%) | 35/2,701 (1.3%) | 271/2,977 (9.1%) | 75/2,977 (2.5%) | 43/2,977 (1.4%) |
| 4 | 24/3,350 (0.7%) | 20/3,042 (0.7%) | 293/3,350 (8.8%) | 6/3,350 (0.2%) | 13/3,350 (0.4%) |
| 5 | 4/1,168 (0.3%) | 3/1,110 (0.3%) | 64/1,168 (5.5%) | 2/1,168 (0.2%) | 2/1,168 (0.2%) |
| Total | 466/9,312 (5.0%) | 86/8,377 (1.0%) | 834/9,312 (9.0%) | 314/9,312 (3.4%) | 188/9,312 (2.0%) |
| 1 | 165/501 (32.9%) | 106/429 (24.7%) | 243/501 (48.5%) | 240/501 (47.9%) | |
| 2 | 213/1,316 (16.2%) | 275/1,258 (21.9%) | 418/1,316 (31.8%) | 403/1,316 (30.6%) | |
| 3 | 412/2,977 (13.8%) | 521/2,934 (17.8%) | 612/2,977 (20.6%) | 344/2,977 (11.6%) | |
| 4 | 406/3,350 (12.1%) | 348/3,337 (10.4%) | 368/3,350 (11.0%) | 77/3,350 (2.3%) | |
| 5 | 71/1,168 (6.1%) | 52/1,166 (4.5%) | 56/1,168 (4.8%) | 6/1,168 (0.5%) | |
| Total | 1,267/9,312 (13.6%) | 1,302/9,124 (14.3%) | 1,697/9,312 (18.2%) | 1,070/9,312 (11.5%) | |
DISCUSSION
Emergency physicians and surgical preparation center nurses generated predictions by the time of hospital admission for over 90% of the target population during usual workflow, without the addition of staff or resources. The discrimination of the prospectively generated predictions was very good to excellent, with an AROC of 0.850 (95% CI: 0.833‐0.866), similar to that obtained from the retrospective version. Calibration was excellent. The prospectively calculated mortality risk was associated with a number of other events. As shown in Table 3, the differing frequency of events within the risk strata support the development of differing intensities of multidisciplinary strategies according to the level of risk.[5] Our study provides useful experience for others who anticipate generating real‐time predictions. We consider the key reasons for success to be the considerable time spent achieving consensus, the technical development of the Web application, the brief clinician time required for the scoring process, the leadership of the chief medical and nursing officers, and the requirement that a prediction be generated before assignment of a hospital room.
Our study has a number of limitations, some of which were noted in our original publication, and although still relevant, will not be repeated here for space considerations. This is a single‐site study that used a prediction rule developed by the same site, albeit on a patient population 4 to 5 years earlier. It is not known how well the specific rule might perform in other hospital populations; any such use should therefore be accompanied by independent validation studies prior to implementation. Our successful experience should motivate future validation studies. Second, because the prognoses of patients scored from the emergency department are likely to be worse than those of elective surgery patients, our rule should be recalibrated for each subgroup separately. We plan to do this in the near future, as well as consider additional risk factors. Third, the other events of interest might be predicted more accurately if rules specifically developed for each were deployed. The mortality risk by itself is unlikely to be a sufficiently accurate predictor, particularly for complications and intensive care use, for reasons outlined in our original publication.[3] However, the varying levels of events within the higher versus lower strata should be noted by the clinical team as they design their team‐based processes. A follow‐up visit with a physician within a few days of discharge could address the concurrent risk of dying as well as readmission, for example. Finally, it is too early to determine if the availability of mortality predictions from this rule will benefit patients.[2, 8, 10] During the study period, we implemented only 2 new care processes based on the level of risk. This lack of interventions allowed us to evaluate the prediction accuracy with minimal additional confounding, but at the expense of not yet knowing the clinical impact of this work. After the study period, we implemented a number of other interventions and plan on evaluating their effectiveness in the future. We are also considering an evaluation of the potential information gained by updating the predictions throughout the course of the hospitalization.[14]
In conclusion, it is feasible to have a reasonably accurate prediction of mortality risk for most adult patients at the beginning of their hospitalizations. The availability of this prognostic information provides an opportunity to develop proactive care plans for high‐ and low‐risk subsets of patients.
Acknowledgements
The authors acknowledge the technical assistance of Nehal Sanghvi and Ben Sutton in the development of the Web application and related databases, and the support of the Chief Nursing Officer, Joyce Young, RN, PhD, the emergency department medical staff, Mohammad Salameh, MD, David Vandenberg, MD, and the surgical preparation center staff.
Disclosure: Nothing to report.
- , , , et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845–850.
- , . Methodological standards for the development of clinical decision rules in emergency medicine. Ann Emerg Med. 1999;33:437–447.
- , , , , . Mortality predictions on admission as a context for organizing care activities. J Hosp Med. 2013;8:229–235.
- , . The simple clinical score predicts mortality for 30 days after admission to an acute medical unit. QJM. 2006;99:771–781.
- , , , et al. Allocating scare resources in real‐time to reduce heart failure readmissions: a prospective, controlled study. BMJ Qual Saf. 2013;22:998–1005.
- , . Interventions to decrease hospital readmissions: keys for cost‐effectiveness. JAMA Intern Med. 2013;173:695–698.
- , , , et.al. A validated value‐based model to improve hospital‐wide perioperative outcomes. Ann Surg. 2010;252:486–498.
- , . Why is a good clinical prediction rule so hard to find? Arch Intern Med. 2011;171:1701–1702.
- , , , , , . Early detection of impending physiologic deterioration among patients who are not in intensive care: development of predictive models using data from an automated electronic medical record. J Hosp Med. 2012;7(5):388–395.
- , , . Predicting death: an empirical evaluation of predictive tools for mortality. Arch Intern Med. 2011;171:1721–1726.
- , , , , . Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA. 2012;307:1405–1413.
- Health Level Seven International website. Available at: http://www.hl7.org/. Accessed June 21, 2014.
- . Bounding sample size projections for the area under a ROC curve. J Stat Plan Inference. 2009;139:711–721.
- , , , , . Derivation and validation of a model to predict daily risk of death in hospital. Med Care. 2011;49:734–743.
The systematic deployment of prediction rules within health systems remains a challenge, although such decision aids have been available for decades.[1, 2] We previously developed and validated a prediction rule for 30‐day mortality in a retrospective cohort, noting that the mortality risk is associated with a number of other clinical events.[3] These relationships suggest risk strata, defined by the predicted probability of 30‐day mortality, and could trigger a number of coordinated care processes proportional to the level of risk.[4] For example, patients within the higher‐risk strata could be considered for placement into an intermediate or intensive care unit (ICU), be monitored more closely by physician and nurse team members for clinical deterioration, be seen by a physician within a few days of hospital discharge, and be considered for advance care planning discussions.[3, 4, 5, 6, 7] Patients within the lower‐risk strata might not need the same intensity of these processes routinely unless some other indication were present.
However attractive this conceptual framework may be, its realization is dependent on the willingness of clinical staff to generate predictions consistently on a substantial portion of the patient population, and on the accuracy of the predictions when the risk factors are determined with some level of uncertainty at the beginning of the hospitalization.[2, 8] Skepticism is justified, because the work involved in completing the prediction rule might be incompatible with existing workflow. A patient might not be scored if the emergency physician lacks time or if technical issues arise with the information system and computation process.[9] There is also a generic concern that the predictions will prove to be less accurate outside of the original study population.[8, 9, 10] A more specific concern for our rule is how well present on admission diagnoses can be determined during the relatively short emergency department or presurgery evaluation period. For example, a final diagnosis of heart failure might not be established until later in the hospitalization, after the results of diagnostic testing and clinical response to treatment are known. Moreover, our retrospective prediction rule requires an assessment of the presence or absence of sepsis and respiratory failure. These diagnoses appear to be susceptible to secular trends in medical record coding practices, suggesting the rule's accuracy might not be stable over time.[11]
We report the feasibility of having emergency physicians and the surgical preparation center team generate mortality predictions before an inpatient bed is assigned. We evaluate and report the accuracy of these prospective predictions.
METHODS
The study population consisted of all patients 18 years of age or less than 100 years who were admitted from the emergency department or assigned an inpatient bed following elective surgery at a tertiary, community teaching hospital in the Midwestern United States from September 1, 2012 through February 15, 2013. Although patients entering the hospital from these 2 pathways would be expected to have different levels of mortality risk, we used the original prediction rule for both because such distinctions were not made in its derivation and validation. Patients were not considered if they were admitted for childbirth or other obstetrical reasons, admitted directly from physician offices, the cardiac catheterization laboratory, hemodialysis unit, or from another hospital. The site institutional review board approved this study.
The implementation process began with presentations to the administrative and medical staff leadership on the accuracy of the retrospectively generated mortality predictions and risk of other adverse events.[3] The chief medical and nursing officers became project champions, secured internal funding for the technical components, and arranged to have 2 project comanagers available. A multidisciplinary task force endorsed the implementation details at biweekly meetings throughout the planning year. The leadership of the emergency department and surgical preparation center committed their colleagues to generate the predictions. The support of the emergency leadership was contingent on the completion of the entire prediction generating process in a very short time (within the time a physician could hold his/her breath). The chief medical officer, with the support of the leadership of the hospitalists and emergency physicians, made the administrative decision that a prediction must be generated prior to the assignment of a hospital room.
During the consensus‐building phase, a Web‐based application was developed to generate the predictions. Emergency physicians and surgical preparation staff were trained on the definitions of the risk factors (see Supporting Information, Appendix, in the online version of this article) and how to use the Web application. Three supporting databases were created. Each midnight, a past medical history database was updated, identifying those who had been discharged from the study hospital in the previous 365 days, and whether or not their diagnoses included atrial fibrillation, leukemia/lymphoma, metastatic cancer, cancer other than leukemia, lymphoma, cognitive disorder, or other neurological conditions (eg, Parkinson's, multiple sclerosis, epilepsy, coma, and stupor). Similarly, a clinical laboratory results database was created and updated real time through an HL7 (Health Level Seven, a standard data exchange format[12]) interface with the laboratory information system for the following tests performed in the preceding 30 days at a hospital‐affiliated facility: hemoglobin, platelet count, white blood count, serum troponin, blood urea nitrogen, serum albumin, serum lactate, arterial pH, arterial partial pressure of oxygen values. The third database, admission‐discharge‐transfer, was created and updated every 15 minutes to identify patients currently in the emergency room or scheduled for surgery. When a patient registration event was added to this database, the Web application created a record, retrieved all relevant data, and displayed the patient name for scoring. When the decision for hospitalization was made, the clinician selected the patient's name and reviewed the pre‐populated medical diagnoses of interest, which could be overwritten based on his/her own assessment (Figure 1A,B). The clinician then indicated (yes, no, or unknown) if the patient currently had or was being treated for each of the following: injury, heart failure, sepsis, respiratory failure, and whether or not the admitting service would be medicine (ie, nonsurgical, nonobstetrical). We considered unknown status to indicate the patient did not have the condition. When laboratory values were not available, a normal value was imputed using a previously developed algorithm.[3] Two additional questions, not used in the current prediction process, were answered to provide data for a future analysis: 1 concerning the change in the patient's condition while in the emergency department and the other concerning the presence of abnormal vital signs. The probability of 30‐day mortality was calculated via the Web application using the risk information supplied and the scoring weights (ie, parameter estimates) provided in the Appendices of our original publication.[3] Predictions were updated every minute as new laboratory values became available, and flagged with an alert if a more severe score resulted.
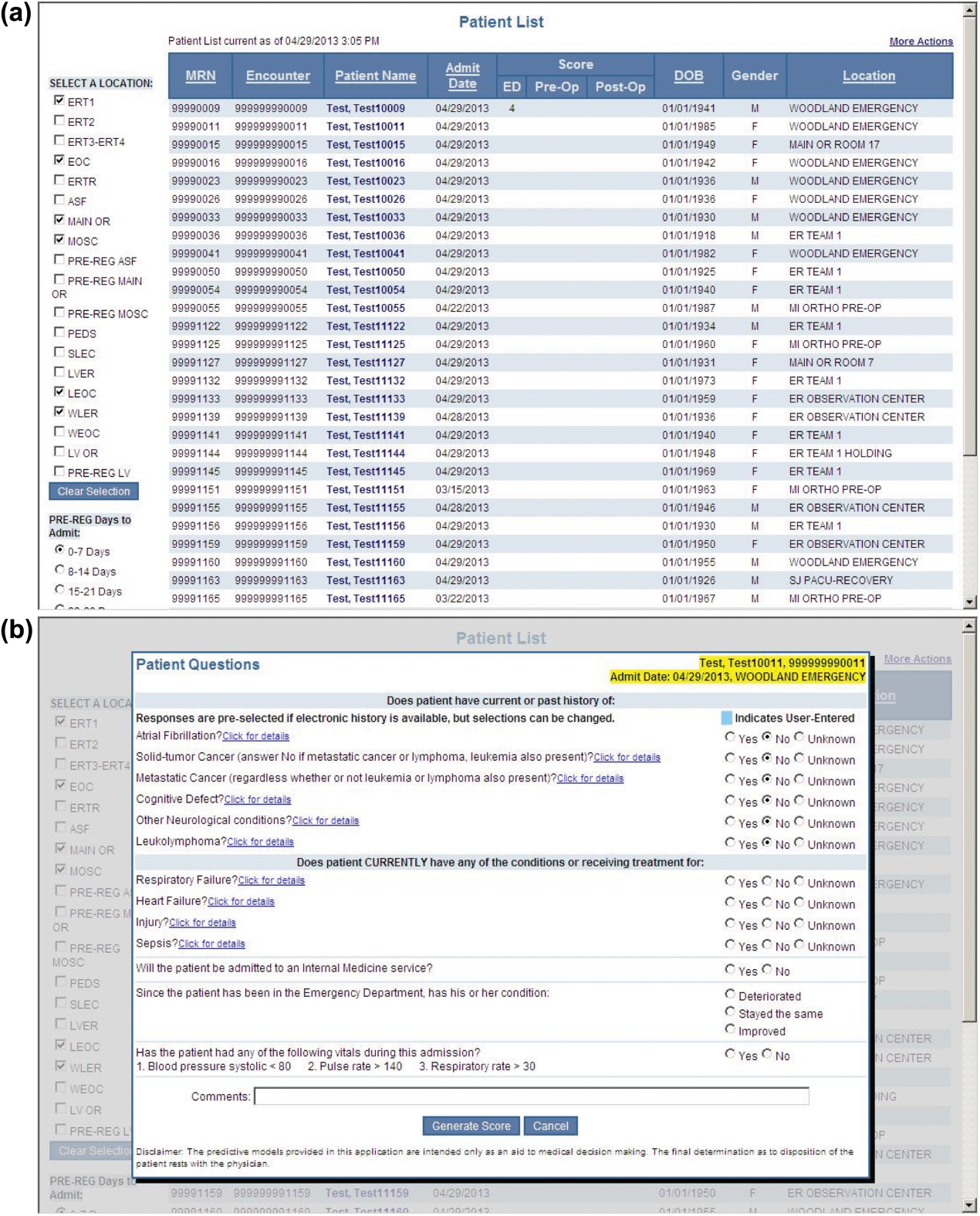
For the analyses of this study, the last prospective prediction viewed by emergency department personnel, a hospital bed manager, or surgical suite staff prior to arrival on the nursing unit is the one referenced as prospective. Once the patient had been discharged from the hospital, we generated a second mortality prediction based on previously published parameter estimates applied to risk factor data ascertained retrospectively as was done in the original article[3]; we subsequently refer to this prediction as retrospective. We will report on the group of patients who had both prospective and retrospective scores (1 patient had a prospective but not retrospective score available).
The prediction scores were made available to the clinical teams gradually during the study period. All scores were viewable by the midpoint of the study for emergency department admissions and near the end of the study for elective‐surgery patients. Only 2 changes in care processes based on level of risk were introduced during the study period. The first required initial placement of patients having a probability of dying of 0.3 or greater into an intensive or intermediate care unit unless the patient or family requested a less aggressive approach. The second occurred in the final 2 months of the study when a large multispecialty practice began routinely arranging for high‐risk patients to be seen within 3 or 7 days of hospital discharge.
Statistical Analyses
SAS version 9.3 (SAS Institute Inc., Cary, NC) was used to build the datasets and perform the analyses. Feasibility was evaluated by the number of patients who were candidates for prospective scoring with a score available at the time of admission. The validity was assessed with the primary outcome of death within 30 days from the date of hospital admission, as determined from hospital administrative data and the Social Security Death Index. The primary statistical metric is the area under the receiver operating characteristic curve (AROC) and the corresponding 95% Wald confidence limits. We needed some context for understanding the performance of the prospective predictions, assuming the accuracy could deteriorate due to the instability of the prediction rule over time and/or due to imperfect clinical information at the time the risk factors were determined. Accordingly, we also calculated an AROC based on retrospectively derived covariates (but using the same set of parameter estimates) as done in our original publication so we could gauge the stability of the original prediction rule. However, the motivation was not to determine whether retrospective versus prospective predictions were more accurate, given that only prospective predictions are useful in the context of developing real‐time care processes. Rather, we wanted to know if the prospective predictions would be sufficiently accurate for use in clinical practice. A priori, we assumed the prospective predictions should have an AROC of approximately 0.80. Therefore, a target sample size of 8660 hospitalizations was determined to be adequate to assess validity, assuming a 30‐day mortality rate of 5%, a desired lower 95% confidence boundary for the area under the prospective curve at or above 0.80, with a total confidence interval width of 0.07.[13] Calibration was assessed by comparing the actual proportion of patients dying (with 95% binomial confidence intervals) with the mean predicted mortality level within 5 percentile increments of predicted risk.
Risk Strata
We categorize the probability of 30‐day mortality into strata, with the understanding that the thresholds for defining these are a work in progress. Our hospital currently has 5 strata ranging from level 1 (highest mortality risk) to level 5 (lowest risk). The corresponding thresholds (at probabilities of death of 0.005, 0.02, 0.07, 0.20) were determined by visual inspection of the event rates and slope of curves displayed in Figure 1 of the original publication.[3]
Relationship to Secondary Clinical Outcomes of Interest
The choice of clinical care processes triggered per level of risk may be informed by understanding the frequency of events that increase with the mortality risk. We therefore examined the AROC from logistic regression models for the following outcomes using the prospectively generated probability as an explanatory variable: unplanned transfer to an ICU within the first 24 hours for patients not admitted to an ICU initially, ICU use at some point during the hospitalization, the development of a condition not present on admission (complication), receipt of palliative care by the end of the hospitalization, death during the hospitalization, 30‐day readmission, and death within 180 days. The definition of these outcomes and statistical approach used has been previously reported.[3]
RESULTS
Mortality predictions were generated on demand for 7291 out of 7777 (93.8%) eligible patients admitted from the emergency department, and for 2021 out of 2250 (89.8%) eligible elective surgical cases, for a total of 9312 predictions generated out of a possible 10,027 hospitalizations (92.9%). Table 1 displays the characteristics of the study population. The mean age was 65.2 years and 53.8% were women. The most common risk factors were atrial fibrillation (16.4%) and cancer (14.6%). Orders for a comfort care approach (rather than curative) were entered within 4 hours of admission for 32/9312 patients (0.34%), and 9/9312 (0.1%) were hospice patients on admission.
| Risk Factors | No. | Without Imputation | No. | With Imputation |
|---|---|---|---|---|
| ||||
| Clinical laboratory values within preceding 30 days | ||||
| Maximum serum blood urea nitrogen (mg/dL) | 8,484 | 22.7 (17.7) | 9,312 | 22.3 (16.9) |
| Minimum hemoglobin, g/dL, | 8,750 | 12.5 (2.4) | 9,312 | 12.4 (2.4) |
| Minimum platelet count, 1,000/UL | 8,737 | 224.1 (87.4) | 9,312 | 225.2 (84.7) |
| Maximum white blood count, 1,000/UL | 8,750 | 10.3 (5.8) | 9,312 | 10.3 (5.6) |
| Maximum serum lactate, mEq/L | 1,749 | 2.2 (1.8) | 9,312 | 0.7 (1.1) |
| Minimum serum albumin, g/dL | 4,057 | 3.4 (0.7) | 9,312 | 3.2 (0.5) |
| Minimum arterial pH | 509 | 7.36 (0.10) | 9,312 | 7.36 (0.02) |
| Minimum arterial pO2, mm Hg | 509 | 73.6 (25.2) | 9,312 | 98.6 (8.4) |
| Maximum serum troponin, ng/mL | 3,217 | 0.5 (9.3) | 9,312 | 0.2 (5.4) |
| Demographics and diagnoses | ||||
| Age, y | 9,312 | 65.2 (17.0) | ||
| Female sex | 9,312 | 5,006 (53.8%) | ||
| Previous hospitalization within past 365 days | 9,312 | 3,995 (42.9%) | ||
| Emergent admission | 9,312 | 7,288 (78.3%) | ||
| Admitted to a medicine service | 9,312 | 5,840 (62.7%) | ||
| Current or past atrial fibrillation | 9,312 | 1,526 (16.4%) | ||
| Current or past cancer without metastases, excluding leukemia or lymphoma | 9,312 | 1,356 (14.6%) | ||
| Current or past history of leukemia or lymphoma | 9,312 | 145 (1.6%) | ||
| Current or past metastatic cancer | 9,312 | 363 (3.9%) | ||
| Current or past cognitive deficiency | 9,312 | 844 (9.1%) | ||
| Current or past history of other neurological conditions (eg, Parkinson's disease, multiple sclerosis, epilepsy, coma, stupor, brain damage) | 9,312 | 952 (10.2%) | ||
| Injury such as fractures or trauma at the time of admission | 9,312 | 656 (7.0%) | ||
| Sepsis at the time of admission | 9,312 | 406 (4.4%) | ||
| Heart failure at the time of admission | 9,312 | 776 (8.3%) | ||
| Respiratory failure on admission | 9,312 | 557 (6.0%) | ||
| Outcomes of interest | ||||
| Unplanned transfer to an ICU (for those not admitted to an ICU) within 24 hours of admission | 8,377 | 86 (1.0%) | ||
| Ever in an ICU during the hospitalization | 9,312 | 1,267 (13.6%) | ||
| Development of a condition not present on admission (complication) | 9,312 | 834 (9.0%) | ||
| Within hospital mortality | 9,312 | 188 (2.0%) | ||
| Mortality within 30 days of admission | 9,312 | 466 (5.0%) | ||
| Mortality within 180 days of admission | 9,312 | 1,070 (11.5%) | ||
| Receipt of palliative care by the end of the hospitalization | 9,312 | 314 (3.4%) | ||
| Readmitted to the hospital within 30 days of discharge (patients alive at discharge) | 9,124 | 1,302 (14.3%) | ||
| Readmitted to the hospital within 30 days of discharge (patients alive on admission) | 9,312 | 1,302 (14.0%) | ||
Evaluation of Prediction Accuracy
The AROC for 30‐day mortality was 0.850 (95% confidence interval [CI]: 0.833‐0.866) for prospectively collected covariates, and 0.870 (95% CI: 0.855‐0.885) for retrospectively determined risk factors. These AROCs are not substantively different from each other, demonstrating comparable prediction performance. Calibration was excellent, as indicated in Figure 2, in which the predicted level of risk lay within the 95% confidence limits of the actual 30‐day mortality for 19 out of 20 intervals of 5 percentile increments.
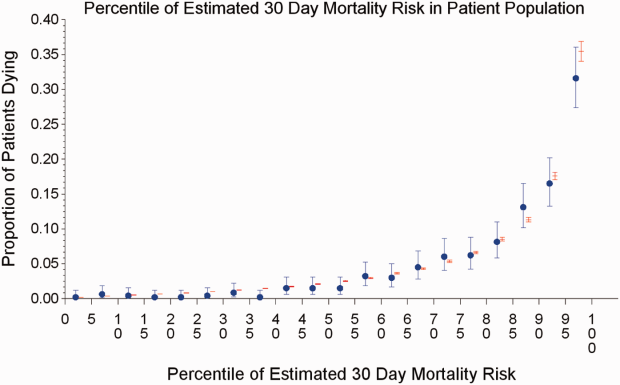
Relationship to Secondary Clinical Outcomes of Interest
The relationship between the prospectively generated probability of dying within 30 days and other events is quantified by the AROC displayed in Table 2. The 30‐day mortality risk has a strong association with the receipt of palliative care by hospital discharge, in‐hospital mortality, and 180‐day mortality, a fair association with the risk for 30‐day readmissions and unplanned transfers to intensive care, and weak associations with receipt of intensive unit care ever within the hospitalization or the development of a new diagnosis that was not present on admission (complication). The frequency of these events per mortality risk strata is shown in Table 3. The level 1 stratum contains a higher frequency of these events, whereas the level 5 stratum contains relatively few, reflecting the Pareto principle by which a relatively small proportion of patients contribute a disproportionate frequency of the events of interest.
| |
| In‐hospital mortality | 0.841 (0.8140.869) |
| 180day mortality | 0.836 (0.8250.848) |
| Receipt of palliative care by discharge | 0.875 (0.8580.891) |
| 30day readmission (patients alive at discharge) | 0.649 (0.6340.664) |
| Unplanned transfer to an ICU (for those not admitted to an ICU) within 24 hours | 0.643 (0.5900.696) |
| Ever in an ICU during the hospitalization | 0.605 (0.5880.621) |
| Development of a condition not present on admission (complication) | 0.555 (0.5350.575) |
| Risk Strata | 30‐Day Mortality, Count/Cases (%) | Unplanned Transfers to ICU Within 24 Hours, Count/Cases (%) | Diagnosis Not Present on Admission, Complication, Count/Cases (%) | Palliative Status at Discharge, Count/Cases (%) | Death in Hospital, Count/Cases (%) |
|---|---|---|---|---|---|
| Risk Strata | Ever in ICU, Count/Cases (%) | 30‐Day Readmission, Count/Cases (%) | Death or Readmission Within 30 Days, Count/Cases (%) | 180‐Day Mortality, Count/Cases (%) | |
| |||||
| 1 | 155/501 (30.9%) | 6/358 (1.7%) | 58/501 (11.6%) | 110/501 (22.0%) | 72/501 (14.4%) |
| 2 | 166/1,316 (12.6%) | 22/1,166 (1.9%) | 148/1,316 (11.3%) | 121/1,316 (9.2%) | 58/1,316 (4.4%) |
| 3 | 117/2,977 (3.9%) | 35/2,701 (1.3%) | 271/2,977 (9.1%) | 75/2,977 (2.5%) | 43/2,977 (1.4%) |
| 4 | 24/3,350 (0.7%) | 20/3,042 (0.7%) | 293/3,350 (8.8%) | 6/3,350 (0.2%) | 13/3,350 (0.4%) |
| 5 | 4/1,168 (0.3%) | 3/1,110 (0.3%) | 64/1,168 (5.5%) | 2/1,168 (0.2%) | 2/1,168 (0.2%) |
| Total | 466/9,312 (5.0%) | 86/8,377 (1.0%) | 834/9,312 (9.0%) | 314/9,312 (3.4%) | 188/9,312 (2.0%) |
| 1 | 165/501 (32.9%) | 106/429 (24.7%) | 243/501 (48.5%) | 240/501 (47.9%) | |
| 2 | 213/1,316 (16.2%) | 275/1,258 (21.9%) | 418/1,316 (31.8%) | 403/1,316 (30.6%) | |
| 3 | 412/2,977 (13.8%) | 521/2,934 (17.8%) | 612/2,977 (20.6%) | 344/2,977 (11.6%) | |
| 4 | 406/3,350 (12.1%) | 348/3,337 (10.4%) | 368/3,350 (11.0%) | 77/3,350 (2.3%) | |
| 5 | 71/1,168 (6.1%) | 52/1,166 (4.5%) | 56/1,168 (4.8%) | 6/1,168 (0.5%) | |
| Total | 1,267/9,312 (13.6%) | 1,302/9,124 (14.3%) | 1,697/9,312 (18.2%) | 1,070/9,312 (11.5%) | |
DISCUSSION
Emergency physicians and surgical preparation center nurses generated predictions by the time of hospital admission for over 90% of the target population during usual workflow, without the addition of staff or resources. The discrimination of the prospectively generated predictions was very good to excellent, with an AROC of 0.850 (95% CI: 0.833‐0.866), similar to that obtained from the retrospective version. Calibration was excellent. The prospectively calculated mortality risk was associated with a number of other events. As shown in Table 3, the differing frequency of events within the risk strata support the development of differing intensities of multidisciplinary strategies according to the level of risk.[5] Our study provides useful experience for others who anticipate generating real‐time predictions. We consider the key reasons for success to be the considerable time spent achieving consensus, the technical development of the Web application, the brief clinician time required for the scoring process, the leadership of the chief medical and nursing officers, and the requirement that a prediction be generated before assignment of a hospital room.
Our study has a number of limitations, some of which were noted in our original publication, and although still relevant, will not be repeated here for space considerations. This is a single‐site study that used a prediction rule developed by the same site, albeit on a patient population 4 to 5 years earlier. It is not known how well the specific rule might perform in other hospital populations; any such use should therefore be accompanied by independent validation studies prior to implementation. Our successful experience should motivate future validation studies. Second, because the prognoses of patients scored from the emergency department are likely to be worse than those of elective surgery patients, our rule should be recalibrated for each subgroup separately. We plan to do this in the near future, as well as consider additional risk factors. Third, the other events of interest might be predicted more accurately if rules specifically developed for each were deployed. The mortality risk by itself is unlikely to be a sufficiently accurate predictor, particularly for complications and intensive care use, for reasons outlined in our original publication.[3] However, the varying levels of events within the higher versus lower strata should be noted by the clinical team as they design their team‐based processes. A follow‐up visit with a physician within a few days of discharge could address the concurrent risk of dying as well as readmission, for example. Finally, it is too early to determine if the availability of mortality predictions from this rule will benefit patients.[2, 8, 10] During the study period, we implemented only 2 new care processes based on the level of risk. This lack of interventions allowed us to evaluate the prediction accuracy with minimal additional confounding, but at the expense of not yet knowing the clinical impact of this work. After the study period, we implemented a number of other interventions and plan on evaluating their effectiveness in the future. We are also considering an evaluation of the potential information gained by updating the predictions throughout the course of the hospitalization.[14]
In conclusion, it is feasible to have a reasonably accurate prediction of mortality risk for most adult patients at the beginning of their hospitalizations. The availability of this prognostic information provides an opportunity to develop proactive care plans for high‐ and low‐risk subsets of patients.
Acknowledgements
The authors acknowledge the technical assistance of Nehal Sanghvi and Ben Sutton in the development of the Web application and related databases, and the support of the Chief Nursing Officer, Joyce Young, RN, PhD, the emergency department medical staff, Mohammad Salameh, MD, David Vandenberg, MD, and the surgical preparation center staff.
Disclosure: Nothing to report.
The systematic deployment of prediction rules within health systems remains a challenge, although such decision aids have been available for decades.[1, 2] We previously developed and validated a prediction rule for 30‐day mortality in a retrospective cohort, noting that the mortality risk is associated with a number of other clinical events.[3] These relationships suggest risk strata, defined by the predicted probability of 30‐day mortality, and could trigger a number of coordinated care processes proportional to the level of risk.[4] For example, patients within the higher‐risk strata could be considered for placement into an intermediate or intensive care unit (ICU), be monitored more closely by physician and nurse team members for clinical deterioration, be seen by a physician within a few days of hospital discharge, and be considered for advance care planning discussions.[3, 4, 5, 6, 7] Patients within the lower‐risk strata might not need the same intensity of these processes routinely unless some other indication were present.
However attractive this conceptual framework may be, its realization is dependent on the willingness of clinical staff to generate predictions consistently on a substantial portion of the patient population, and on the accuracy of the predictions when the risk factors are determined with some level of uncertainty at the beginning of the hospitalization.[2, 8] Skepticism is justified, because the work involved in completing the prediction rule might be incompatible with existing workflow. A patient might not be scored if the emergency physician lacks time or if technical issues arise with the information system and computation process.[9] There is also a generic concern that the predictions will prove to be less accurate outside of the original study population.[8, 9, 10] A more specific concern for our rule is how well present on admission diagnoses can be determined during the relatively short emergency department or presurgery evaluation period. For example, a final diagnosis of heart failure might not be established until later in the hospitalization, after the results of diagnostic testing and clinical response to treatment are known. Moreover, our retrospective prediction rule requires an assessment of the presence or absence of sepsis and respiratory failure. These diagnoses appear to be susceptible to secular trends in medical record coding practices, suggesting the rule's accuracy might not be stable over time.[11]
We report the feasibility of having emergency physicians and the surgical preparation center team generate mortality predictions before an inpatient bed is assigned. We evaluate and report the accuracy of these prospective predictions.
METHODS
The study population consisted of all patients 18 years of age or less than 100 years who were admitted from the emergency department or assigned an inpatient bed following elective surgery at a tertiary, community teaching hospital in the Midwestern United States from September 1, 2012 through February 15, 2013. Although patients entering the hospital from these 2 pathways would be expected to have different levels of mortality risk, we used the original prediction rule for both because such distinctions were not made in its derivation and validation. Patients were not considered if they were admitted for childbirth or other obstetrical reasons, admitted directly from physician offices, the cardiac catheterization laboratory, hemodialysis unit, or from another hospital. The site institutional review board approved this study.
The implementation process began with presentations to the administrative and medical staff leadership on the accuracy of the retrospectively generated mortality predictions and risk of other adverse events.[3] The chief medical and nursing officers became project champions, secured internal funding for the technical components, and arranged to have 2 project comanagers available. A multidisciplinary task force endorsed the implementation details at biweekly meetings throughout the planning year. The leadership of the emergency department and surgical preparation center committed their colleagues to generate the predictions. The support of the emergency leadership was contingent on the completion of the entire prediction generating process in a very short time (within the time a physician could hold his/her breath). The chief medical officer, with the support of the leadership of the hospitalists and emergency physicians, made the administrative decision that a prediction must be generated prior to the assignment of a hospital room.
During the consensus‐building phase, a Web‐based application was developed to generate the predictions. Emergency physicians and surgical preparation staff were trained on the definitions of the risk factors (see Supporting Information, Appendix, in the online version of this article) and how to use the Web application. Three supporting databases were created. Each midnight, a past medical history database was updated, identifying those who had been discharged from the study hospital in the previous 365 days, and whether or not their diagnoses included atrial fibrillation, leukemia/lymphoma, metastatic cancer, cancer other than leukemia, lymphoma, cognitive disorder, or other neurological conditions (eg, Parkinson's, multiple sclerosis, epilepsy, coma, and stupor). Similarly, a clinical laboratory results database was created and updated real time through an HL7 (Health Level Seven, a standard data exchange format[12]) interface with the laboratory information system for the following tests performed in the preceding 30 days at a hospital‐affiliated facility: hemoglobin, platelet count, white blood count, serum troponin, blood urea nitrogen, serum albumin, serum lactate, arterial pH, arterial partial pressure of oxygen values. The third database, admission‐discharge‐transfer, was created and updated every 15 minutes to identify patients currently in the emergency room or scheduled for surgery. When a patient registration event was added to this database, the Web application created a record, retrieved all relevant data, and displayed the patient name for scoring. When the decision for hospitalization was made, the clinician selected the patient's name and reviewed the pre‐populated medical diagnoses of interest, which could be overwritten based on his/her own assessment (Figure 1A,B). The clinician then indicated (yes, no, or unknown) if the patient currently had or was being treated for each of the following: injury, heart failure, sepsis, respiratory failure, and whether or not the admitting service would be medicine (ie, nonsurgical, nonobstetrical). We considered unknown status to indicate the patient did not have the condition. When laboratory values were not available, a normal value was imputed using a previously developed algorithm.[3] Two additional questions, not used in the current prediction process, were answered to provide data for a future analysis: 1 concerning the change in the patient's condition while in the emergency department and the other concerning the presence of abnormal vital signs. The probability of 30‐day mortality was calculated via the Web application using the risk information supplied and the scoring weights (ie, parameter estimates) provided in the Appendices of our original publication.[3] Predictions were updated every minute as new laboratory values became available, and flagged with an alert if a more severe score resulted.
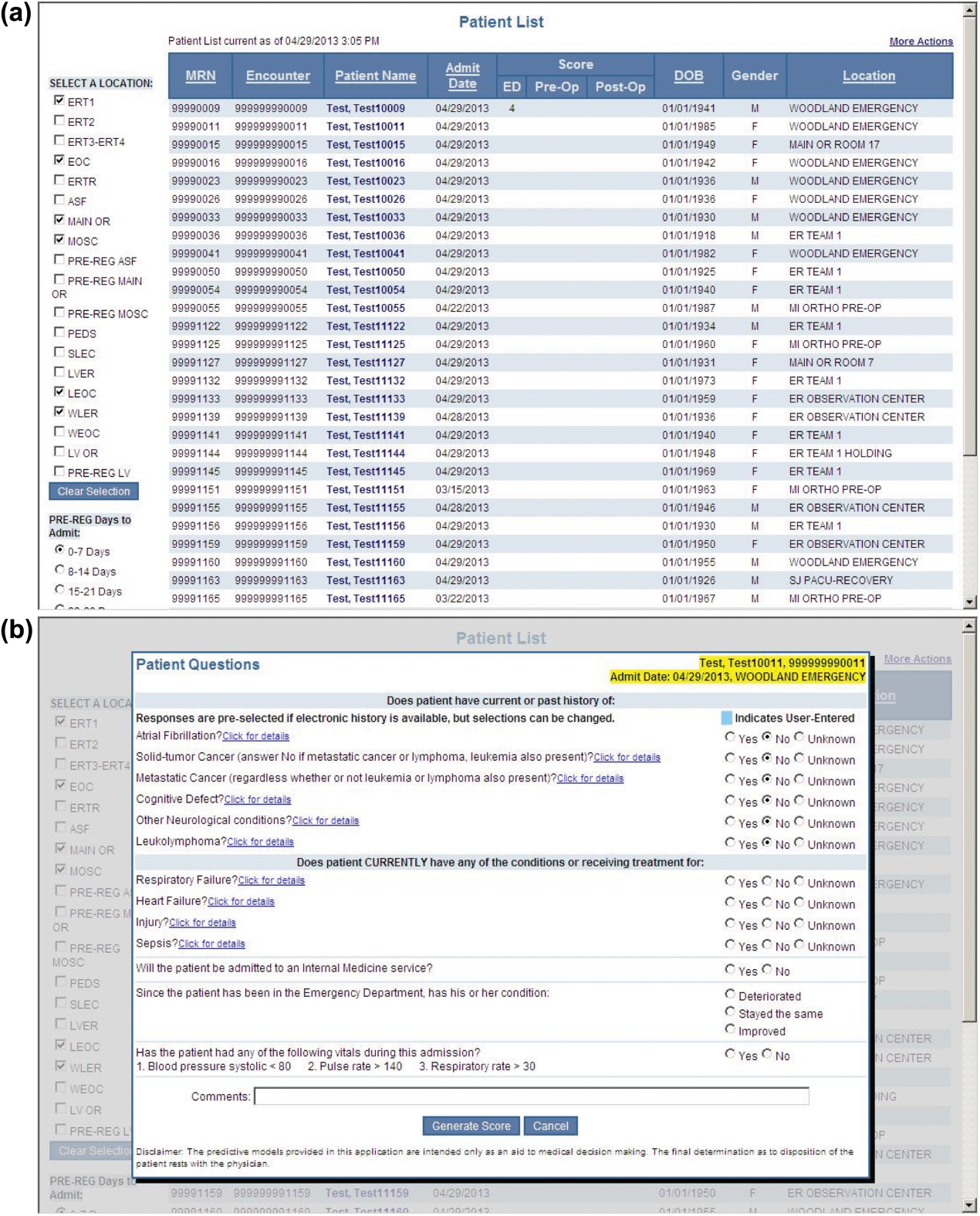
For the analyses of this study, the last prospective prediction viewed by emergency department personnel, a hospital bed manager, or surgical suite staff prior to arrival on the nursing unit is the one referenced as prospective. Once the patient had been discharged from the hospital, we generated a second mortality prediction based on previously published parameter estimates applied to risk factor data ascertained retrospectively as was done in the original article[3]; we subsequently refer to this prediction as retrospective. We will report on the group of patients who had both prospective and retrospective scores (1 patient had a prospective but not retrospective score available).
The prediction scores were made available to the clinical teams gradually during the study period. All scores were viewable by the midpoint of the study for emergency department admissions and near the end of the study for elective‐surgery patients. Only 2 changes in care processes based on level of risk were introduced during the study period. The first required initial placement of patients having a probability of dying of 0.3 or greater into an intensive or intermediate care unit unless the patient or family requested a less aggressive approach. The second occurred in the final 2 months of the study when a large multispecialty practice began routinely arranging for high‐risk patients to be seen within 3 or 7 days of hospital discharge.
Statistical Analyses
SAS version 9.3 (SAS Institute Inc., Cary, NC) was used to build the datasets and perform the analyses. Feasibility was evaluated by the number of patients who were candidates for prospective scoring with a score available at the time of admission. The validity was assessed with the primary outcome of death within 30 days from the date of hospital admission, as determined from hospital administrative data and the Social Security Death Index. The primary statistical metric is the area under the receiver operating characteristic curve (AROC) and the corresponding 95% Wald confidence limits. We needed some context for understanding the performance of the prospective predictions, assuming the accuracy could deteriorate due to the instability of the prediction rule over time and/or due to imperfect clinical information at the time the risk factors were determined. Accordingly, we also calculated an AROC based on retrospectively derived covariates (but using the same set of parameter estimates) as done in our original publication so we could gauge the stability of the original prediction rule. However, the motivation was not to determine whether retrospective versus prospective predictions were more accurate, given that only prospective predictions are useful in the context of developing real‐time care processes. Rather, we wanted to know if the prospective predictions would be sufficiently accurate for use in clinical practice. A priori, we assumed the prospective predictions should have an AROC of approximately 0.80. Therefore, a target sample size of 8660 hospitalizations was determined to be adequate to assess validity, assuming a 30‐day mortality rate of 5%, a desired lower 95% confidence boundary for the area under the prospective curve at or above 0.80, with a total confidence interval width of 0.07.[13] Calibration was assessed by comparing the actual proportion of patients dying (with 95% binomial confidence intervals) with the mean predicted mortality level within 5 percentile increments of predicted risk.
Risk Strata
We categorize the probability of 30‐day mortality into strata, with the understanding that the thresholds for defining these are a work in progress. Our hospital currently has 5 strata ranging from level 1 (highest mortality risk) to level 5 (lowest risk). The corresponding thresholds (at probabilities of death of 0.005, 0.02, 0.07, 0.20) were determined by visual inspection of the event rates and slope of curves displayed in Figure 1 of the original publication.[3]
Relationship to Secondary Clinical Outcomes of Interest
The choice of clinical care processes triggered per level of risk may be informed by understanding the frequency of events that increase with the mortality risk. We therefore examined the AROC from logistic regression models for the following outcomes using the prospectively generated probability as an explanatory variable: unplanned transfer to an ICU within the first 24 hours for patients not admitted to an ICU initially, ICU use at some point during the hospitalization, the development of a condition not present on admission (complication), receipt of palliative care by the end of the hospitalization, death during the hospitalization, 30‐day readmission, and death within 180 days. The definition of these outcomes and statistical approach used has been previously reported.[3]
RESULTS
Mortality predictions were generated on demand for 7291 out of 7777 (93.8%) eligible patients admitted from the emergency department, and for 2021 out of 2250 (89.8%) eligible elective surgical cases, for a total of 9312 predictions generated out of a possible 10,027 hospitalizations (92.9%). Table 1 displays the characteristics of the study population. The mean age was 65.2 years and 53.8% were women. The most common risk factors were atrial fibrillation (16.4%) and cancer (14.6%). Orders for a comfort care approach (rather than curative) were entered within 4 hours of admission for 32/9312 patients (0.34%), and 9/9312 (0.1%) were hospice patients on admission.
| Risk Factors | No. | Without Imputation | No. | With Imputation |
|---|---|---|---|---|
| ||||
| Clinical laboratory values within preceding 30 days | ||||
| Maximum serum blood urea nitrogen (mg/dL) | 8,484 | 22.7 (17.7) | 9,312 | 22.3 (16.9) |
| Minimum hemoglobin, g/dL, | 8,750 | 12.5 (2.4) | 9,312 | 12.4 (2.4) |
| Minimum platelet count, 1,000/UL | 8,737 | 224.1 (87.4) | 9,312 | 225.2 (84.7) |
| Maximum white blood count, 1,000/UL | 8,750 | 10.3 (5.8) | 9,312 | 10.3 (5.6) |
| Maximum serum lactate, mEq/L | 1,749 | 2.2 (1.8) | 9,312 | 0.7 (1.1) |
| Minimum serum albumin, g/dL | 4,057 | 3.4 (0.7) | 9,312 | 3.2 (0.5) |
| Minimum arterial pH | 509 | 7.36 (0.10) | 9,312 | 7.36 (0.02) |
| Minimum arterial pO2, mm Hg | 509 | 73.6 (25.2) | 9,312 | 98.6 (8.4) |
| Maximum serum troponin, ng/mL | 3,217 | 0.5 (9.3) | 9,312 | 0.2 (5.4) |
| Demographics and diagnoses | ||||
| Age, y | 9,312 | 65.2 (17.0) | ||
| Female sex | 9,312 | 5,006 (53.8%) | ||
| Previous hospitalization within past 365 days | 9,312 | 3,995 (42.9%) | ||
| Emergent admission | 9,312 | 7,288 (78.3%) | ||
| Admitted to a medicine service | 9,312 | 5,840 (62.7%) | ||
| Current or past atrial fibrillation | 9,312 | 1,526 (16.4%) | ||
| Current or past cancer without metastases, excluding leukemia or lymphoma | 9,312 | 1,356 (14.6%) | ||
| Current or past history of leukemia or lymphoma | 9,312 | 145 (1.6%) | ||
| Current or past metastatic cancer | 9,312 | 363 (3.9%) | ||
| Current or past cognitive deficiency | 9,312 | 844 (9.1%) | ||
| Current or past history of other neurological conditions (eg, Parkinson's disease, multiple sclerosis, epilepsy, coma, stupor, brain damage) | 9,312 | 952 (10.2%) | ||
| Injury such as fractures or trauma at the time of admission | 9,312 | 656 (7.0%) | ||
| Sepsis at the time of admission | 9,312 | 406 (4.4%) | ||
| Heart failure at the time of admission | 9,312 | 776 (8.3%) | ||
| Respiratory failure on admission | 9,312 | 557 (6.0%) | ||
| Outcomes of interest | ||||
| Unplanned transfer to an ICU (for those not admitted to an ICU) within 24 hours of admission | 8,377 | 86 (1.0%) | ||
| Ever in an ICU during the hospitalization | 9,312 | 1,267 (13.6%) | ||
| Development of a condition not present on admission (complication) | 9,312 | 834 (9.0%) | ||
| Within hospital mortality | 9,312 | 188 (2.0%) | ||
| Mortality within 30 days of admission | 9,312 | 466 (5.0%) | ||
| Mortality within 180 days of admission | 9,312 | 1,070 (11.5%) | ||
| Receipt of palliative care by the end of the hospitalization | 9,312 | 314 (3.4%) | ||
| Readmitted to the hospital within 30 days of discharge (patients alive at discharge) | 9,124 | 1,302 (14.3%) | ||
| Readmitted to the hospital within 30 days of discharge (patients alive on admission) | 9,312 | 1,302 (14.0%) | ||
Evaluation of Prediction Accuracy
The AROC for 30‐day mortality was 0.850 (95% confidence interval [CI]: 0.833‐0.866) for prospectively collected covariates, and 0.870 (95% CI: 0.855‐0.885) for retrospectively determined risk factors. These AROCs are not substantively different from each other, demonstrating comparable prediction performance. Calibration was excellent, as indicated in Figure 2, in which the predicted level of risk lay within the 95% confidence limits of the actual 30‐day mortality for 19 out of 20 intervals of 5 percentile increments.
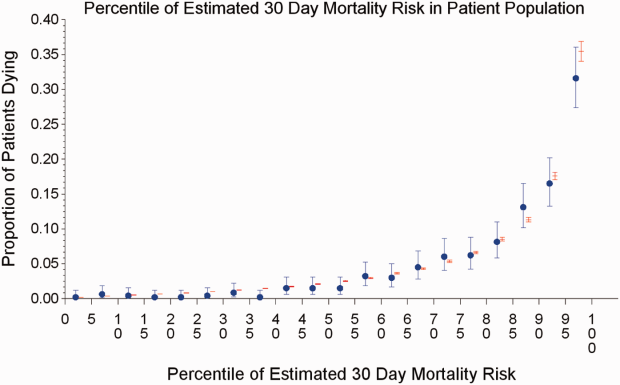
Relationship to Secondary Clinical Outcomes of Interest
The relationship between the prospectively generated probability of dying within 30 days and other events is quantified by the AROC displayed in Table 2. The 30‐day mortality risk has a strong association with the receipt of palliative care by hospital discharge, in‐hospital mortality, and 180‐day mortality, a fair association with the risk for 30‐day readmissions and unplanned transfers to intensive care, and weak associations with receipt of intensive unit care ever within the hospitalization or the development of a new diagnosis that was not present on admission (complication). The frequency of these events per mortality risk strata is shown in Table 3. The level 1 stratum contains a higher frequency of these events, whereas the level 5 stratum contains relatively few, reflecting the Pareto principle by which a relatively small proportion of patients contribute a disproportionate frequency of the events of interest.
| |
| In‐hospital mortality | 0.841 (0.8140.869) |
| 180day mortality | 0.836 (0.8250.848) |
| Receipt of palliative care by discharge | 0.875 (0.8580.891) |
| 30day readmission (patients alive at discharge) | 0.649 (0.6340.664) |
| Unplanned transfer to an ICU (for those not admitted to an ICU) within 24 hours | 0.643 (0.5900.696) |
| Ever in an ICU during the hospitalization | 0.605 (0.5880.621) |
| Development of a condition not present on admission (complication) | 0.555 (0.5350.575) |
| Risk Strata | 30‐Day Mortality, Count/Cases (%) | Unplanned Transfers to ICU Within 24 Hours, Count/Cases (%) | Diagnosis Not Present on Admission, Complication, Count/Cases (%) | Palliative Status at Discharge, Count/Cases (%) | Death in Hospital, Count/Cases (%) |
|---|---|---|---|---|---|
| Risk Strata | Ever in ICU, Count/Cases (%) | 30‐Day Readmission, Count/Cases (%) | Death or Readmission Within 30 Days, Count/Cases (%) | 180‐Day Mortality, Count/Cases (%) | |
| |||||
| 1 | 155/501 (30.9%) | 6/358 (1.7%) | 58/501 (11.6%) | 110/501 (22.0%) | 72/501 (14.4%) |
| 2 | 166/1,316 (12.6%) | 22/1,166 (1.9%) | 148/1,316 (11.3%) | 121/1,316 (9.2%) | 58/1,316 (4.4%) |
| 3 | 117/2,977 (3.9%) | 35/2,701 (1.3%) | 271/2,977 (9.1%) | 75/2,977 (2.5%) | 43/2,977 (1.4%) |
| 4 | 24/3,350 (0.7%) | 20/3,042 (0.7%) | 293/3,350 (8.8%) | 6/3,350 (0.2%) | 13/3,350 (0.4%) |
| 5 | 4/1,168 (0.3%) | 3/1,110 (0.3%) | 64/1,168 (5.5%) | 2/1,168 (0.2%) | 2/1,168 (0.2%) |
| Total | 466/9,312 (5.0%) | 86/8,377 (1.0%) | 834/9,312 (9.0%) | 314/9,312 (3.4%) | 188/9,312 (2.0%) |
| 1 | 165/501 (32.9%) | 106/429 (24.7%) | 243/501 (48.5%) | 240/501 (47.9%) | |
| 2 | 213/1,316 (16.2%) | 275/1,258 (21.9%) | 418/1,316 (31.8%) | 403/1,316 (30.6%) | |
| 3 | 412/2,977 (13.8%) | 521/2,934 (17.8%) | 612/2,977 (20.6%) | 344/2,977 (11.6%) | |
| 4 | 406/3,350 (12.1%) | 348/3,337 (10.4%) | 368/3,350 (11.0%) | 77/3,350 (2.3%) | |
| 5 | 71/1,168 (6.1%) | 52/1,166 (4.5%) | 56/1,168 (4.8%) | 6/1,168 (0.5%) | |
| Total | 1,267/9,312 (13.6%) | 1,302/9,124 (14.3%) | 1,697/9,312 (18.2%) | 1,070/9,312 (11.5%) | |
DISCUSSION
Emergency physicians and surgical preparation center nurses generated predictions by the time of hospital admission for over 90% of the target population during usual workflow, without the addition of staff or resources. The discrimination of the prospectively generated predictions was very good to excellent, with an AROC of 0.850 (95% CI: 0.833‐0.866), similar to that obtained from the retrospective version. Calibration was excellent. The prospectively calculated mortality risk was associated with a number of other events. As shown in Table 3, the differing frequency of events within the risk strata support the development of differing intensities of multidisciplinary strategies according to the level of risk.[5] Our study provides useful experience for others who anticipate generating real‐time predictions. We consider the key reasons for success to be the considerable time spent achieving consensus, the technical development of the Web application, the brief clinician time required for the scoring process, the leadership of the chief medical and nursing officers, and the requirement that a prediction be generated before assignment of a hospital room.
Our study has a number of limitations, some of which were noted in our original publication, and although still relevant, will not be repeated here for space considerations. This is a single‐site study that used a prediction rule developed by the same site, albeit on a patient population 4 to 5 years earlier. It is not known how well the specific rule might perform in other hospital populations; any such use should therefore be accompanied by independent validation studies prior to implementation. Our successful experience should motivate future validation studies. Second, because the prognoses of patients scored from the emergency department are likely to be worse than those of elective surgery patients, our rule should be recalibrated for each subgroup separately. We plan to do this in the near future, as well as consider additional risk factors. Third, the other events of interest might be predicted more accurately if rules specifically developed for each were deployed. The mortality risk by itself is unlikely to be a sufficiently accurate predictor, particularly for complications and intensive care use, for reasons outlined in our original publication.[3] However, the varying levels of events within the higher versus lower strata should be noted by the clinical team as they design their team‐based processes. A follow‐up visit with a physician within a few days of discharge could address the concurrent risk of dying as well as readmission, for example. Finally, it is too early to determine if the availability of mortality predictions from this rule will benefit patients.[2, 8, 10] During the study period, we implemented only 2 new care processes based on the level of risk. This lack of interventions allowed us to evaluate the prediction accuracy with minimal additional confounding, but at the expense of not yet knowing the clinical impact of this work. After the study period, we implemented a number of other interventions and plan on evaluating their effectiveness in the future. We are also considering an evaluation of the potential information gained by updating the predictions throughout the course of the hospitalization.[14]
In conclusion, it is feasible to have a reasonably accurate prediction of mortality risk for most adult patients at the beginning of their hospitalizations. The availability of this prognostic information provides an opportunity to develop proactive care plans for high‐ and low‐risk subsets of patients.
Acknowledgements
The authors acknowledge the technical assistance of Nehal Sanghvi and Ben Sutton in the development of the Web application and related databases, and the support of the Chief Nursing Officer, Joyce Young, RN, PhD, the emergency department medical staff, Mohammad Salameh, MD, David Vandenberg, MD, and the surgical preparation center staff.
Disclosure: Nothing to report.
- , , , et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845–850.
- , . Methodological standards for the development of clinical decision rules in emergency medicine. Ann Emerg Med. 1999;33:437–447.
- , , , , . Mortality predictions on admission as a context for organizing care activities. J Hosp Med. 2013;8:229–235.
- , . The simple clinical score predicts mortality for 30 days after admission to an acute medical unit. QJM. 2006;99:771–781.
- , , , et al. Allocating scare resources in real‐time to reduce heart failure readmissions: a prospective, controlled study. BMJ Qual Saf. 2013;22:998–1005.
- , . Interventions to decrease hospital readmissions: keys for cost‐effectiveness. JAMA Intern Med. 2013;173:695–698.
- , , , et.al. A validated value‐based model to improve hospital‐wide perioperative outcomes. Ann Surg. 2010;252:486–498.
- , . Why is a good clinical prediction rule so hard to find? Arch Intern Med. 2011;171:1701–1702.
- , , , , , . Early detection of impending physiologic deterioration among patients who are not in intensive care: development of predictive models using data from an automated electronic medical record. J Hosp Med. 2012;7(5):388–395.
- , , . Predicting death: an empirical evaluation of predictive tools for mortality. Arch Intern Med. 2011;171:1721–1726.
- , , , , . Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA. 2012;307:1405–1413.
- Health Level Seven International website. Available at: http://www.hl7.org/. Accessed June 21, 2014.
- . Bounding sample size projections for the area under a ROC curve. J Stat Plan Inference. 2009;139:711–721.
- , , , , . Derivation and validation of a model to predict daily risk of death in hospital. Med Care. 2011;49:734–743.
- , , , et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845–850.
- , . Methodological standards for the development of clinical decision rules in emergency medicine. Ann Emerg Med. 1999;33:437–447.
- , , , , . Mortality predictions on admission as a context for organizing care activities. J Hosp Med. 2013;8:229–235.
- , . The simple clinical score predicts mortality for 30 days after admission to an acute medical unit. QJM. 2006;99:771–781.
- , , , et al. Allocating scare resources in real‐time to reduce heart failure readmissions: a prospective, controlled study. BMJ Qual Saf. 2013;22:998–1005.
- , . Interventions to decrease hospital readmissions: keys for cost‐effectiveness. JAMA Intern Med. 2013;173:695–698.
- , , , et.al. A validated value‐based model to improve hospital‐wide perioperative outcomes. Ann Surg. 2010;252:486–498.
- , . Why is a good clinical prediction rule so hard to find? Arch Intern Med. 2011;171:1701–1702.
- , , , , , . Early detection of impending physiologic deterioration among patients who are not in intensive care: development of predictive models using data from an automated electronic medical record. J Hosp Med. 2012;7(5):388–395.
- , , . Predicting death: an empirical evaluation of predictive tools for mortality. Arch Intern Med. 2011;171:1721–1726.
- , , , , . Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA. 2012;307:1405–1413.
- Health Level Seven International website. Available at: http://www.hl7.org/. Accessed June 21, 2014.
- . Bounding sample size projections for the area under a ROC curve. J Stat Plan Inference. 2009;139:711–721.
- , , , , . Derivation and validation of a model to predict daily risk of death in hospital. Med Care. 2011;49:734–743.
© 2014 Society of Hospital Medicine