User login
Primary Care Shortage Reshaping How Patients Seek Care
By February of 2022, Ella, a 25-year-old behavioral interventionist in Colorado Springs, Colorado, was sick with strep-like symptoms for the third time in 3 months. She didn’t bother to call her doctor.
The first two times she had strep throat, she’d tried to schedule an appointment with her newest primary care doctor but couldn’t get in. They only had available appointments 5 and even 10 days out, but she’d already had symptoms for 3 days.
Until she graduated college, Ella had only known easy-access primary care. Her childhood family doctor and the nurse practitioners at her college clinic knew her. They anticipated her yearly allergies and knew about her predisposition for strep throat. Appointments were easy to schedule, and providers responded to her messages. But since entering the workforce and leaving her parent’s insurance, the kind of primary care she’d come to rely on was nearly impossible to find.
“I went to urgent care, and that became my primary care,” she told this news organization.
Patients Can’t Get Appointments
Primary care is in crisis. A growing number of Americans, like Ella, can’t access care when they need it. According to a 2024 report, 29% of adults and 14% of children don’t have a regular source of care. Those looking for a new primary care provider face extensive research and 6- to 9-month waits for a new patient appointment — if they can get in at all.
But even those with a primary care provider face long wait times: Days to weeks for a sick visit and months for a wellness checkup. Over one third of Medicare beneficiaries wait more than a month to see a doctor. Accessing primary care is more difficult than access to surgery, physical therapy, or rehabilitative care, according to a survey of Medicare beneficiaries by the Commonwealth Fund.
“Shortages tend to be in rural and urban underserved areas, but now, you’re hearing about primary care shortages in Boston, which is a mecca of healthcare,” said Ann Greiner, president and CEO of the Primary Care Coalition.
While retail clinics, urgent care, and telehealth help close the gap in acute needs, they miss one of primary care’s most critical benefits: A doctor who knows you. There’s strong evidence that ongoing treatment from a primary care physician (PCP) who knows your history, family, and context results in better long-term outcomes and fewer hospitalizations and emergency room visits.
If patients continue to find it too hard to break into primary care or set up an appointment, experts are concerned that they’ll stop pursuing primary care altogether.
Doctors’ Hands Are Tied
“I want to highlight that this is not an issue of primary care doctors not wanting to be accessible,” said Lisa Rotenstein, MD, MBA, a PCP and medical director of Ambulatory Quality and Safety at the University of California San Francisco Health. “These access issues are symptoms of the design of primary care in the United States.”
Across the United States, there’s a dearth of family medicine doctors, pediatricians, and internists. And without significantly more primary care providers, there’s simply no way for all Americans to get optimal primary care. The Health Resources and Services administration estimates a current shortage of 13,000 primary care providers. And that shortage will skyrocket to 68,000 by 2036 as the number of Americans needing care balloons and existing PCPs retire with too few trainees to fill their shoes.
The American Association of Medical Colleges predicts a slightly lower shortage in 2036 — between 20,000 and 40,000 primary care physicians — only if more residency positions are funded nationwide.
However, even with more positions, medical trainees see little incentive to pursue primary care. Young doctors are avoiding primary care because of the pressures, Dr. Rotenstein said. There’s incredible pressure to get reimbursement for primary care doctors. And the added administrative burden makes “the work life of these specialties not really manageable,” she said.
Continued Shortages of PCPs
“We know there’s a documented pajama time,” Ms. Greiner said. For every 1 hour spent with a patient, primary care must spend nearly 2 additional hours on electronic health records and desk work, according to a study by the American Medical Association. Even with all those additional hours devoted to getting paid, primary care doctors make an average of $103,000 less annually compared with their counterparts in surgery and oncology.
It’s not an attractive combination for a new doctor with medical debt. This year, Ms. Greiner said that residency positions in internal medicine and pediatrics went unfilled. Of those trainees who do go into a primary care specialty, many won’t last. Only half of primary care residents practice in primary care 3-5 years later. The rest choose to subspecialize or become hospitalists.
These untenable demands on a primary care provider don’t go unnoticed by patients. In Ella’s attempts to invest in a new primary care relationship, she often doesn’t feel heard and can tell the doctor is rushed. “[Urgent care is] probably not the best care because they don’t know me, but it does seem like they are able to listen to me better,” Ella said.
Patients Want to Invest in Primary Care
Primary care should work like putting money in a bank account, Dr. Rotenstein said. Young patients invest in the relationship and reap the benefits of a doctor who knows them later in life when they need more complex care. But if seeing a doctor is so difficult, many young people may stop investing in their PCP relationship.
“One thing ... that I worry about in this kind of situation where patients really have to put in a lot of work to get the care they need is in inequities of care,” Dr. Rotenstein said. “We know some of our patients are more able to undertake that work.”
Alternatively, the primary care shortage could be reshaping how patients seek care. A 2023 study showed the proportion of primary care preventative visits increased over 20 years. Policies under the Affordable Care Act were the driving force. But it’s also true that sick visits are being diverted to urgent care.
Ella told this news organization she doesn’t even consider primary care for sick visits at this point. “I can’t wait 5 days or a week and a half. Unless I have bigger issues, like I need tests, I’m not even going to go to primary care.” It’s possible that other patients also see primary care as a place for testing and wellness checks and leave sick visits to retail and urgent care.
The Road Ahead
There’s no single fix for primary care, but experts agree that the fee-for-service model is a core issue for the specialty. In a 2021 report, the National Association of Engineering and Medicine said that primary care reform needs to include higher reimbursement rates for primary care and that US primary care should be restructured so that payers “pay primary care teams to care for people, not doctors to deliver services.”
In the current model, the doctor-patient clinic time is the only income-generating part of a primary care practice. A better model would consider the communication, administration, teams, and support doctors have to fund to provide the best primary care.
“We need to change how we pay and how much we pay, so [primary care doctors] are properly incentivized to build out a team to provide the comprehensive care you need,” Ms. Greiner said.
In the meantime, primary care doctors are adapting. Some drop down to part-time to account for the additional administrative workload. Others are transitioning to concierge services to offer the quality of care they want while getting the income they need. Still, others specialize their practice, offering primary care to a subset of the population, like older adults.
Employers are also looking to improve care access for their employees, hiring in-house doctors to provide primary care on site. Ms. Greiner recently met with a group of chief medical officers from major companies to discuss expanding primary care access via the workplace.
The efforts to adapt amid a broken system are admirable, Dr. Rotenstein said. And whatever a PCP has to do to keep practicing in primary care is laudable. The only problem with these adaptations is they largely limit a doctor’s patient pool and, therefore, limit access, she said. More significant reforms that adequately reimburse primary care and incentivize new doctors are still needed.
As for Ella, she got married. Her wife is in the military, so now she has Tricare, which comes with a more streamlined process to access primary care. However, doctor shortages are just as evident in that system. The couple called to schedule new patient appointments after their recent move to Virginia. The first available ones were 6 weeks out.
A version of this article appeared on Medscape.com.
By February of 2022, Ella, a 25-year-old behavioral interventionist in Colorado Springs, Colorado, was sick with strep-like symptoms for the third time in 3 months. She didn’t bother to call her doctor.
The first two times she had strep throat, she’d tried to schedule an appointment with her newest primary care doctor but couldn’t get in. They only had available appointments 5 and even 10 days out, but she’d already had symptoms for 3 days.
Until she graduated college, Ella had only known easy-access primary care. Her childhood family doctor and the nurse practitioners at her college clinic knew her. They anticipated her yearly allergies and knew about her predisposition for strep throat. Appointments were easy to schedule, and providers responded to her messages. But since entering the workforce and leaving her parent’s insurance, the kind of primary care she’d come to rely on was nearly impossible to find.
“I went to urgent care, and that became my primary care,” she told this news organization.
Patients Can’t Get Appointments
Primary care is in crisis. A growing number of Americans, like Ella, can’t access care when they need it. According to a 2024 report, 29% of adults and 14% of children don’t have a regular source of care. Those looking for a new primary care provider face extensive research and 6- to 9-month waits for a new patient appointment — if they can get in at all.
But even those with a primary care provider face long wait times: Days to weeks for a sick visit and months for a wellness checkup. Over one third of Medicare beneficiaries wait more than a month to see a doctor. Accessing primary care is more difficult than access to surgery, physical therapy, or rehabilitative care, according to a survey of Medicare beneficiaries by the Commonwealth Fund.
“Shortages tend to be in rural and urban underserved areas, but now, you’re hearing about primary care shortages in Boston, which is a mecca of healthcare,” said Ann Greiner, president and CEO of the Primary Care Coalition.
While retail clinics, urgent care, and telehealth help close the gap in acute needs, they miss one of primary care’s most critical benefits: A doctor who knows you. There’s strong evidence that ongoing treatment from a primary care physician (PCP) who knows your history, family, and context results in better long-term outcomes and fewer hospitalizations and emergency room visits.
If patients continue to find it too hard to break into primary care or set up an appointment, experts are concerned that they’ll stop pursuing primary care altogether.
Doctors’ Hands Are Tied
“I want to highlight that this is not an issue of primary care doctors not wanting to be accessible,” said Lisa Rotenstein, MD, MBA, a PCP and medical director of Ambulatory Quality and Safety at the University of California San Francisco Health. “These access issues are symptoms of the design of primary care in the United States.”
Across the United States, there’s a dearth of family medicine doctors, pediatricians, and internists. And without significantly more primary care providers, there’s simply no way for all Americans to get optimal primary care. The Health Resources and Services administration estimates a current shortage of 13,000 primary care providers. And that shortage will skyrocket to 68,000 by 2036 as the number of Americans needing care balloons and existing PCPs retire with too few trainees to fill their shoes.
The American Association of Medical Colleges predicts a slightly lower shortage in 2036 — between 20,000 and 40,000 primary care physicians — only if more residency positions are funded nationwide.
However, even with more positions, medical trainees see little incentive to pursue primary care. Young doctors are avoiding primary care because of the pressures, Dr. Rotenstein said. There’s incredible pressure to get reimbursement for primary care doctors. And the added administrative burden makes “the work life of these specialties not really manageable,” she said.
Continued Shortages of PCPs
“We know there’s a documented pajama time,” Ms. Greiner said. For every 1 hour spent with a patient, primary care must spend nearly 2 additional hours on electronic health records and desk work, according to a study by the American Medical Association. Even with all those additional hours devoted to getting paid, primary care doctors make an average of $103,000 less annually compared with their counterparts in surgery and oncology.
It’s not an attractive combination for a new doctor with medical debt. This year, Ms. Greiner said that residency positions in internal medicine and pediatrics went unfilled. Of those trainees who do go into a primary care specialty, many won’t last. Only half of primary care residents practice in primary care 3-5 years later. The rest choose to subspecialize or become hospitalists.
These untenable demands on a primary care provider don’t go unnoticed by patients. In Ella’s attempts to invest in a new primary care relationship, she often doesn’t feel heard and can tell the doctor is rushed. “[Urgent care is] probably not the best care because they don’t know me, but it does seem like they are able to listen to me better,” Ella said.
Patients Want to Invest in Primary Care
Primary care should work like putting money in a bank account, Dr. Rotenstein said. Young patients invest in the relationship and reap the benefits of a doctor who knows them later in life when they need more complex care. But if seeing a doctor is so difficult, many young people may stop investing in their PCP relationship.
“One thing ... that I worry about in this kind of situation where patients really have to put in a lot of work to get the care they need is in inequities of care,” Dr. Rotenstein said. “We know some of our patients are more able to undertake that work.”
Alternatively, the primary care shortage could be reshaping how patients seek care. A 2023 study showed the proportion of primary care preventative visits increased over 20 years. Policies under the Affordable Care Act were the driving force. But it’s also true that sick visits are being diverted to urgent care.
Ella told this news organization she doesn’t even consider primary care for sick visits at this point. “I can’t wait 5 days or a week and a half. Unless I have bigger issues, like I need tests, I’m not even going to go to primary care.” It’s possible that other patients also see primary care as a place for testing and wellness checks and leave sick visits to retail and urgent care.
The Road Ahead
There’s no single fix for primary care, but experts agree that the fee-for-service model is a core issue for the specialty. In a 2021 report, the National Association of Engineering and Medicine said that primary care reform needs to include higher reimbursement rates for primary care and that US primary care should be restructured so that payers “pay primary care teams to care for people, not doctors to deliver services.”
In the current model, the doctor-patient clinic time is the only income-generating part of a primary care practice. A better model would consider the communication, administration, teams, and support doctors have to fund to provide the best primary care.
“We need to change how we pay and how much we pay, so [primary care doctors] are properly incentivized to build out a team to provide the comprehensive care you need,” Ms. Greiner said.
In the meantime, primary care doctors are adapting. Some drop down to part-time to account for the additional administrative workload. Others are transitioning to concierge services to offer the quality of care they want while getting the income they need. Still, others specialize their practice, offering primary care to a subset of the population, like older adults.
Employers are also looking to improve care access for their employees, hiring in-house doctors to provide primary care on site. Ms. Greiner recently met with a group of chief medical officers from major companies to discuss expanding primary care access via the workplace.
The efforts to adapt amid a broken system are admirable, Dr. Rotenstein said. And whatever a PCP has to do to keep practicing in primary care is laudable. The only problem with these adaptations is they largely limit a doctor’s patient pool and, therefore, limit access, she said. More significant reforms that adequately reimburse primary care and incentivize new doctors are still needed.
As for Ella, she got married. Her wife is in the military, so now she has Tricare, which comes with a more streamlined process to access primary care. However, doctor shortages are just as evident in that system. The couple called to schedule new patient appointments after their recent move to Virginia. The first available ones were 6 weeks out.
A version of this article appeared on Medscape.com.
By February of 2022, Ella, a 25-year-old behavioral interventionist in Colorado Springs, Colorado, was sick with strep-like symptoms for the third time in 3 months. She didn’t bother to call her doctor.
The first two times she had strep throat, she’d tried to schedule an appointment with her newest primary care doctor but couldn’t get in. They only had available appointments 5 and even 10 days out, but she’d already had symptoms for 3 days.
Until she graduated college, Ella had only known easy-access primary care. Her childhood family doctor and the nurse practitioners at her college clinic knew her. They anticipated her yearly allergies and knew about her predisposition for strep throat. Appointments were easy to schedule, and providers responded to her messages. But since entering the workforce and leaving her parent’s insurance, the kind of primary care she’d come to rely on was nearly impossible to find.
“I went to urgent care, and that became my primary care,” she told this news organization.
Patients Can’t Get Appointments
Primary care is in crisis. A growing number of Americans, like Ella, can’t access care when they need it. According to a 2024 report, 29% of adults and 14% of children don’t have a regular source of care. Those looking for a new primary care provider face extensive research and 6- to 9-month waits for a new patient appointment — if they can get in at all.
But even those with a primary care provider face long wait times: Days to weeks for a sick visit and months for a wellness checkup. Over one third of Medicare beneficiaries wait more than a month to see a doctor. Accessing primary care is more difficult than access to surgery, physical therapy, or rehabilitative care, according to a survey of Medicare beneficiaries by the Commonwealth Fund.
“Shortages tend to be in rural and urban underserved areas, but now, you’re hearing about primary care shortages in Boston, which is a mecca of healthcare,” said Ann Greiner, president and CEO of the Primary Care Coalition.
While retail clinics, urgent care, and telehealth help close the gap in acute needs, they miss one of primary care’s most critical benefits: A doctor who knows you. There’s strong evidence that ongoing treatment from a primary care physician (PCP) who knows your history, family, and context results in better long-term outcomes and fewer hospitalizations and emergency room visits.
If patients continue to find it too hard to break into primary care or set up an appointment, experts are concerned that they’ll stop pursuing primary care altogether.
Doctors’ Hands Are Tied
“I want to highlight that this is not an issue of primary care doctors not wanting to be accessible,” said Lisa Rotenstein, MD, MBA, a PCP and medical director of Ambulatory Quality and Safety at the University of California San Francisco Health. “These access issues are symptoms of the design of primary care in the United States.”
Across the United States, there’s a dearth of family medicine doctors, pediatricians, and internists. And without significantly more primary care providers, there’s simply no way for all Americans to get optimal primary care. The Health Resources and Services administration estimates a current shortage of 13,000 primary care providers. And that shortage will skyrocket to 68,000 by 2036 as the number of Americans needing care balloons and existing PCPs retire with too few trainees to fill their shoes.
The American Association of Medical Colleges predicts a slightly lower shortage in 2036 — between 20,000 and 40,000 primary care physicians — only if more residency positions are funded nationwide.
However, even with more positions, medical trainees see little incentive to pursue primary care. Young doctors are avoiding primary care because of the pressures, Dr. Rotenstein said. There’s incredible pressure to get reimbursement for primary care doctors. And the added administrative burden makes “the work life of these specialties not really manageable,” she said.
Continued Shortages of PCPs
“We know there’s a documented pajama time,” Ms. Greiner said. For every 1 hour spent with a patient, primary care must spend nearly 2 additional hours on electronic health records and desk work, according to a study by the American Medical Association. Even with all those additional hours devoted to getting paid, primary care doctors make an average of $103,000 less annually compared with their counterparts in surgery and oncology.
It’s not an attractive combination for a new doctor with medical debt. This year, Ms. Greiner said that residency positions in internal medicine and pediatrics went unfilled. Of those trainees who do go into a primary care specialty, many won’t last. Only half of primary care residents practice in primary care 3-5 years later. The rest choose to subspecialize or become hospitalists.
These untenable demands on a primary care provider don’t go unnoticed by patients. In Ella’s attempts to invest in a new primary care relationship, she often doesn’t feel heard and can tell the doctor is rushed. “[Urgent care is] probably not the best care because they don’t know me, but it does seem like they are able to listen to me better,” Ella said.
Patients Want to Invest in Primary Care
Primary care should work like putting money in a bank account, Dr. Rotenstein said. Young patients invest in the relationship and reap the benefits of a doctor who knows them later in life when they need more complex care. But if seeing a doctor is so difficult, many young people may stop investing in their PCP relationship.
“One thing ... that I worry about in this kind of situation where patients really have to put in a lot of work to get the care they need is in inequities of care,” Dr. Rotenstein said. “We know some of our patients are more able to undertake that work.”
Alternatively, the primary care shortage could be reshaping how patients seek care. A 2023 study showed the proportion of primary care preventative visits increased over 20 years. Policies under the Affordable Care Act were the driving force. But it’s also true that sick visits are being diverted to urgent care.
Ella told this news organization she doesn’t even consider primary care for sick visits at this point. “I can’t wait 5 days or a week and a half. Unless I have bigger issues, like I need tests, I’m not even going to go to primary care.” It’s possible that other patients also see primary care as a place for testing and wellness checks and leave sick visits to retail and urgent care.
The Road Ahead
There’s no single fix for primary care, but experts agree that the fee-for-service model is a core issue for the specialty. In a 2021 report, the National Association of Engineering and Medicine said that primary care reform needs to include higher reimbursement rates for primary care and that US primary care should be restructured so that payers “pay primary care teams to care for people, not doctors to deliver services.”
In the current model, the doctor-patient clinic time is the only income-generating part of a primary care practice. A better model would consider the communication, administration, teams, and support doctors have to fund to provide the best primary care.
“We need to change how we pay and how much we pay, so [primary care doctors] are properly incentivized to build out a team to provide the comprehensive care you need,” Ms. Greiner said.
In the meantime, primary care doctors are adapting. Some drop down to part-time to account for the additional administrative workload. Others are transitioning to concierge services to offer the quality of care they want while getting the income they need. Still, others specialize their practice, offering primary care to a subset of the population, like older adults.
Employers are also looking to improve care access for their employees, hiring in-house doctors to provide primary care on site. Ms. Greiner recently met with a group of chief medical officers from major companies to discuss expanding primary care access via the workplace.
The efforts to adapt amid a broken system are admirable, Dr. Rotenstein said. And whatever a PCP has to do to keep practicing in primary care is laudable. The only problem with these adaptations is they largely limit a doctor’s patient pool and, therefore, limit access, she said. More significant reforms that adequately reimburse primary care and incentivize new doctors are still needed.
As for Ella, she got married. Her wife is in the military, so now she has Tricare, which comes with a more streamlined process to access primary care. However, doctor shortages are just as evident in that system. The couple called to schedule new patient appointments after their recent move to Virginia. The first available ones were 6 weeks out.
A version of this article appeared on Medscape.com.
Metabolic Dysfunction–Associated Steatotic Liver Disease Plus HIV Ups Risk for CVD but Not Liver Disease
TOPLINE:
Metabolic dysfunction-associated steatotic liver disease (MASLD) co-occurring with HIV infection does not appear to increase the risk for cirrhosis or hepatocellular carcinoma (HCC) compared with MASLD alone. However, the incidence of major adverse cardiovascular events (MACE) is significantly increased among patients with MASLD and HIV, a large study suggested.
METHODOLOGY:
- MASLD is highly prevalent in people living with HIV, but the impact of HIV on liver and cardiovascular disease (CVD) outcomes in people with MASLD remains unclear.
- To investigate, researchers created a propensity score-matched cohort of veterans with noncirrhotic MASLD, with and without HIV (920 patients in each group).
- They evaluated the incidence of cirrhosis, HCC, and MACE, as well as overall survival, among the two groups. They also assessed these outcomes in MASLD patients with HIV on the basis of whether they were on antiretroviral therapy (ART).
TAKEAWAY:
- During a median follow-up of 10.4 years in the MASLD with HIV group and 11.8 years in the MASLD-only group, the overall incidence of cirrhosis and HCC was similar in MASLD with vs without HIV (cirrhosis: 0.97 vs 1.06 per 100 person-years, P = .54; HCC: 0.26 vs 0.17 per 100,000 person-years, P = .23), regardless of ART use.
- In contrast, the incidence of MACE was significantly higher in MASLD with vs without HIV (5.18 vs 4.48 per 100 person-years, P = .03). The incidence also was higher in patients with MASLD and HIV who were not on ART compared with those on ART (5.83 vs 4.7 per 100 person-years, P = .07).
- Compared with MASLD without HIV, the overall 5-year survival was significantly lower in MASLD with HIV (91.3% vs 85.7%). In MASLD with HIV, receipt of ART was associated with a significantly higher 5-year survival than no ART (87.4% vs 81.6%).
IN PRACTICE:
“Ensuring timely and appropriate initiation of HIV treatment is critical in patients with MASLD who have concurrent HIV infection, as well as optimizing metabolic comorbidities that may also contribute to increased risks of CVD and increased mortality,” the authors wrote.
SOURCE:
The study, led by Robert J. Wong, MD, Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Palo Alto, California, was published online in the American Journal of Gastroenterology.
LIMITATIONS:
The study cohort consisted predominantly of older men, which may limit generalizability to women and younger populations. Metabolic comorbidities are more common in veterans compared with the general population, potentially affecting the generalizability of the CVD risk findings.
DISCLOSURES:
The study was supported by an investigator-initiated research grant from Theratechnologies. Wong has received funding for his institution from Gilead Sciences, Exact Sciences, and Durect Corporation and has served as a consultant for Gilead Sciences.
A version of this article appeared on Medscape.com.
TOPLINE:
Metabolic dysfunction-associated steatotic liver disease (MASLD) co-occurring with HIV infection does not appear to increase the risk for cirrhosis or hepatocellular carcinoma (HCC) compared with MASLD alone. However, the incidence of major adverse cardiovascular events (MACE) is significantly increased among patients with MASLD and HIV, a large study suggested.
METHODOLOGY:
- MASLD is highly prevalent in people living with HIV, but the impact of HIV on liver and cardiovascular disease (CVD) outcomes in people with MASLD remains unclear.
- To investigate, researchers created a propensity score-matched cohort of veterans with noncirrhotic MASLD, with and without HIV (920 patients in each group).
- They evaluated the incidence of cirrhosis, HCC, and MACE, as well as overall survival, among the two groups. They also assessed these outcomes in MASLD patients with HIV on the basis of whether they were on antiretroviral therapy (ART).
TAKEAWAY:
- During a median follow-up of 10.4 years in the MASLD with HIV group and 11.8 years in the MASLD-only group, the overall incidence of cirrhosis and HCC was similar in MASLD with vs without HIV (cirrhosis: 0.97 vs 1.06 per 100 person-years, P = .54; HCC: 0.26 vs 0.17 per 100,000 person-years, P = .23), regardless of ART use.
- In contrast, the incidence of MACE was significantly higher in MASLD with vs without HIV (5.18 vs 4.48 per 100 person-years, P = .03). The incidence also was higher in patients with MASLD and HIV who were not on ART compared with those on ART (5.83 vs 4.7 per 100 person-years, P = .07).
- Compared with MASLD without HIV, the overall 5-year survival was significantly lower in MASLD with HIV (91.3% vs 85.7%). In MASLD with HIV, receipt of ART was associated with a significantly higher 5-year survival than no ART (87.4% vs 81.6%).
IN PRACTICE:
“Ensuring timely and appropriate initiation of HIV treatment is critical in patients with MASLD who have concurrent HIV infection, as well as optimizing metabolic comorbidities that may also contribute to increased risks of CVD and increased mortality,” the authors wrote.
SOURCE:
The study, led by Robert J. Wong, MD, Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Palo Alto, California, was published online in the American Journal of Gastroenterology.
LIMITATIONS:
The study cohort consisted predominantly of older men, which may limit generalizability to women and younger populations. Metabolic comorbidities are more common in veterans compared with the general population, potentially affecting the generalizability of the CVD risk findings.
DISCLOSURES:
The study was supported by an investigator-initiated research grant from Theratechnologies. Wong has received funding for his institution from Gilead Sciences, Exact Sciences, and Durect Corporation and has served as a consultant for Gilead Sciences.
A version of this article appeared on Medscape.com.
TOPLINE:
Metabolic dysfunction-associated steatotic liver disease (MASLD) co-occurring with HIV infection does not appear to increase the risk for cirrhosis or hepatocellular carcinoma (HCC) compared with MASLD alone. However, the incidence of major adverse cardiovascular events (MACE) is significantly increased among patients with MASLD and HIV, a large study suggested.
METHODOLOGY:
- MASLD is highly prevalent in people living with HIV, but the impact of HIV on liver and cardiovascular disease (CVD) outcomes in people with MASLD remains unclear.
- To investigate, researchers created a propensity score-matched cohort of veterans with noncirrhotic MASLD, with and without HIV (920 patients in each group).
- They evaluated the incidence of cirrhosis, HCC, and MACE, as well as overall survival, among the two groups. They also assessed these outcomes in MASLD patients with HIV on the basis of whether they were on antiretroviral therapy (ART).
TAKEAWAY:
- During a median follow-up of 10.4 years in the MASLD with HIV group and 11.8 years in the MASLD-only group, the overall incidence of cirrhosis and HCC was similar in MASLD with vs without HIV (cirrhosis: 0.97 vs 1.06 per 100 person-years, P = .54; HCC: 0.26 vs 0.17 per 100,000 person-years, P = .23), regardless of ART use.
- In contrast, the incidence of MACE was significantly higher in MASLD with vs without HIV (5.18 vs 4.48 per 100 person-years, P = .03). The incidence also was higher in patients with MASLD and HIV who were not on ART compared with those on ART (5.83 vs 4.7 per 100 person-years, P = .07).
- Compared with MASLD without HIV, the overall 5-year survival was significantly lower in MASLD with HIV (91.3% vs 85.7%). In MASLD with HIV, receipt of ART was associated with a significantly higher 5-year survival than no ART (87.4% vs 81.6%).
IN PRACTICE:
“Ensuring timely and appropriate initiation of HIV treatment is critical in patients with MASLD who have concurrent HIV infection, as well as optimizing metabolic comorbidities that may also contribute to increased risks of CVD and increased mortality,” the authors wrote.
SOURCE:
The study, led by Robert J. Wong, MD, Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Palo Alto, California, was published online in the American Journal of Gastroenterology.
LIMITATIONS:
The study cohort consisted predominantly of older men, which may limit generalizability to women and younger populations. Metabolic comorbidities are more common in veterans compared with the general population, potentially affecting the generalizability of the CVD risk findings.
DISCLOSURES:
The study was supported by an investigator-initiated research grant from Theratechnologies. Wong has received funding for his institution from Gilead Sciences, Exact Sciences, and Durect Corporation and has served as a consultant for Gilead Sciences.
A version of this article appeared on Medscape.com.
Avian Flu Threat Still Low and Vaccine Measures Are Ready
After cow-to-cow transmission of avian influenza A subtype H5N1 in US dairy herds led to a cow-to-human transmission in Texas, the Association of State and Territorial Health Officials convened a panel of experts for a scientific symposium on Thursday to talk about the public health implications.
From the sequencing data, “we can expect and anticipate that [the candidate vaccine viruses] will provide good protection,” she explained.
Establishing candidate vaccine viruses “are the precursor to moving into large-scale vaccine production,” Dr. Dugan explained. Should that be needed, the candidate viruses can be used by manufacturers to produce new vaccines.
The CDC is also actively partnering with commercial diagnostic developers and testing companies in case there is a need to scale-up testing, Dr. Dugan said.
The only current human case in the United States was reported on April 1 and confirmed by the CDC within 24 hours, reported Sonja Olsen, PhD, associate director for preparedness and response of the Influenza Division at the CDC.
The person had direct exposure to cattle and reported eye redness, consistent with conjunctivitis, as the only symptom. The person received treatment and has recovered, and there were no reports of illness among the person’s household contacts, Dr. Olsen said.
Person With the Virus Has Recovered
The only other detection of the virus in a human in the United States was in 2022 and it was associated with infected poultry exposure. That person also had mild illness and recovered, Dr. Olsen explained.
Since 1997, when the first case of human infection was reported globally, “there have been 909 [human cases] reported from 23 countries,” Dr. Olsen said. “About half [52%] of the human cases have resulted in death.” Only a small number of human cases have been reported since 2015, but since 2022, more than two dozen human cases have been reported to the World Health Organization.
Experience with the virus in the United States has been about a year behind that in Europe, said Rosemary Sifford, DVM, chief veterinary officer at the US Department of Agriculture. In the United States, the first detection — in January 2022 — was in wild birds; this was followed the next month by the first detection in a commercial poultry flock.
In March of this year, the United States had its first detection in cattle, specifically dairy cattle. But testing has shown that “it remains very much an avian virus. It’s not becoming a bovine virus,” Dr. Sifford reported.
Detected in Cattle
Earlier this week, in an effort to minimize the risk of disease spread, the USDA issued a federal order that requires the reporting of positive influenza tests in livestock and mandatory testing for influenza of dairy cattle before interstate movement.
“As of today, there are affected herds in 33 farms across eight states,” reported Dr. Olsen.
Tests are ongoing to determine how the virus is traveling, but “what we can say is that there’s a high viral load in the milk in the cattle, and it appears that the transmission is happening mostly within the lactating herds,” Dr. Sifford reported. It is unclear whether that is happening during the milking of the cows or whether contaminated milk from a cow with a high viral load is transmitting the virus to other cattle.
“We are strongly encouraging producers to limit the movement of cattle, particularly lactating cattle, as much as possible,” she says.
Milk Is Likely the Source of Transmission
“We haven’t seen anything that would change our assessment that the commercial milk supply is safe,” says Donald Prater, DVM, acting director of the Center for Food Safety and Applied Nutrition at the US Food and Drug Administration (FDA).
In the federal and state milk safety system, he explained, nearly 99% of the commercial milk supply comes from farms that participate in the Grade A program and follow the Pasteurized Milk Ordinance, which outlines pasteurization requirements.
Because detection of the virus in dairy cattle is new, there are many questions to be answered in research, he reported. Among them:
- What level of virus might be leaving the farms from shedding by apparently healthy cows?
- Does any live virus survive the pasteurization process?
- Do different methods of pasteurization and dairy production have different effects on the viability of H5N1?
- Are effects different in various forms of dairy products, such as cheese and cream?
A critical question regarding the potential risk to humans is how much milk would have to be consumed for the virus to become an established infection. That information is essential to determine “what type of pasteurization criteria” are needed to provide “acceptable public health outcomes,” Dr. Prater said.
The CDC is currently using the flu surveillance system to monitor for H5N1 activity in people. The systems show no current indicators of unusual influenza activity in people.
A version of this article appeared on Medscape.com.
After cow-to-cow transmission of avian influenza A subtype H5N1 in US dairy herds led to a cow-to-human transmission in Texas, the Association of State and Territorial Health Officials convened a panel of experts for a scientific symposium on Thursday to talk about the public health implications.
From the sequencing data, “we can expect and anticipate that [the candidate vaccine viruses] will provide good protection,” she explained.
Establishing candidate vaccine viruses “are the precursor to moving into large-scale vaccine production,” Dr. Dugan explained. Should that be needed, the candidate viruses can be used by manufacturers to produce new vaccines.
The CDC is also actively partnering with commercial diagnostic developers and testing companies in case there is a need to scale-up testing, Dr. Dugan said.
The only current human case in the United States was reported on April 1 and confirmed by the CDC within 24 hours, reported Sonja Olsen, PhD, associate director for preparedness and response of the Influenza Division at the CDC.
The person had direct exposure to cattle and reported eye redness, consistent with conjunctivitis, as the only symptom. The person received treatment and has recovered, and there were no reports of illness among the person’s household contacts, Dr. Olsen said.
Person With the Virus Has Recovered
The only other detection of the virus in a human in the United States was in 2022 and it was associated with infected poultry exposure. That person also had mild illness and recovered, Dr. Olsen explained.
Since 1997, when the first case of human infection was reported globally, “there have been 909 [human cases] reported from 23 countries,” Dr. Olsen said. “About half [52%] of the human cases have resulted in death.” Only a small number of human cases have been reported since 2015, but since 2022, more than two dozen human cases have been reported to the World Health Organization.
Experience with the virus in the United States has been about a year behind that in Europe, said Rosemary Sifford, DVM, chief veterinary officer at the US Department of Agriculture. In the United States, the first detection — in January 2022 — was in wild birds; this was followed the next month by the first detection in a commercial poultry flock.
In March of this year, the United States had its first detection in cattle, specifically dairy cattle. But testing has shown that “it remains very much an avian virus. It’s not becoming a bovine virus,” Dr. Sifford reported.
Detected in Cattle
Earlier this week, in an effort to minimize the risk of disease spread, the USDA issued a federal order that requires the reporting of positive influenza tests in livestock and mandatory testing for influenza of dairy cattle before interstate movement.
“As of today, there are affected herds in 33 farms across eight states,” reported Dr. Olsen.
Tests are ongoing to determine how the virus is traveling, but “what we can say is that there’s a high viral load in the milk in the cattle, and it appears that the transmission is happening mostly within the lactating herds,” Dr. Sifford reported. It is unclear whether that is happening during the milking of the cows or whether contaminated milk from a cow with a high viral load is transmitting the virus to other cattle.
“We are strongly encouraging producers to limit the movement of cattle, particularly lactating cattle, as much as possible,” she says.
Milk Is Likely the Source of Transmission
“We haven’t seen anything that would change our assessment that the commercial milk supply is safe,” says Donald Prater, DVM, acting director of the Center for Food Safety and Applied Nutrition at the US Food and Drug Administration (FDA).
In the federal and state milk safety system, he explained, nearly 99% of the commercial milk supply comes from farms that participate in the Grade A program and follow the Pasteurized Milk Ordinance, which outlines pasteurization requirements.
Because detection of the virus in dairy cattle is new, there are many questions to be answered in research, he reported. Among them:
- What level of virus might be leaving the farms from shedding by apparently healthy cows?
- Does any live virus survive the pasteurization process?
- Do different methods of pasteurization and dairy production have different effects on the viability of H5N1?
- Are effects different in various forms of dairy products, such as cheese and cream?
A critical question regarding the potential risk to humans is how much milk would have to be consumed for the virus to become an established infection. That information is essential to determine “what type of pasteurization criteria” are needed to provide “acceptable public health outcomes,” Dr. Prater said.
The CDC is currently using the flu surveillance system to monitor for H5N1 activity in people. The systems show no current indicators of unusual influenza activity in people.
A version of this article appeared on Medscape.com.
After cow-to-cow transmission of avian influenza A subtype H5N1 in US dairy herds led to a cow-to-human transmission in Texas, the Association of State and Territorial Health Officials convened a panel of experts for a scientific symposium on Thursday to talk about the public health implications.
From the sequencing data, “we can expect and anticipate that [the candidate vaccine viruses] will provide good protection,” she explained.
Establishing candidate vaccine viruses “are the precursor to moving into large-scale vaccine production,” Dr. Dugan explained. Should that be needed, the candidate viruses can be used by manufacturers to produce new vaccines.
The CDC is also actively partnering with commercial diagnostic developers and testing companies in case there is a need to scale-up testing, Dr. Dugan said.
The only current human case in the United States was reported on April 1 and confirmed by the CDC within 24 hours, reported Sonja Olsen, PhD, associate director for preparedness and response of the Influenza Division at the CDC.
The person had direct exposure to cattle and reported eye redness, consistent with conjunctivitis, as the only symptom. The person received treatment and has recovered, and there were no reports of illness among the person’s household contacts, Dr. Olsen said.
Person With the Virus Has Recovered
The only other detection of the virus in a human in the United States was in 2022 and it was associated with infected poultry exposure. That person also had mild illness and recovered, Dr. Olsen explained.
Since 1997, when the first case of human infection was reported globally, “there have been 909 [human cases] reported from 23 countries,” Dr. Olsen said. “About half [52%] of the human cases have resulted in death.” Only a small number of human cases have been reported since 2015, but since 2022, more than two dozen human cases have been reported to the World Health Organization.
Experience with the virus in the United States has been about a year behind that in Europe, said Rosemary Sifford, DVM, chief veterinary officer at the US Department of Agriculture. In the United States, the first detection — in January 2022 — was in wild birds; this was followed the next month by the first detection in a commercial poultry flock.
In March of this year, the United States had its first detection in cattle, specifically dairy cattle. But testing has shown that “it remains very much an avian virus. It’s not becoming a bovine virus,” Dr. Sifford reported.
Detected in Cattle
Earlier this week, in an effort to minimize the risk of disease spread, the USDA issued a federal order that requires the reporting of positive influenza tests in livestock and mandatory testing for influenza of dairy cattle before interstate movement.
“As of today, there are affected herds in 33 farms across eight states,” reported Dr. Olsen.
Tests are ongoing to determine how the virus is traveling, but “what we can say is that there’s a high viral load in the milk in the cattle, and it appears that the transmission is happening mostly within the lactating herds,” Dr. Sifford reported. It is unclear whether that is happening during the milking of the cows or whether contaminated milk from a cow with a high viral load is transmitting the virus to other cattle.
“We are strongly encouraging producers to limit the movement of cattle, particularly lactating cattle, as much as possible,” she says.
Milk Is Likely the Source of Transmission
“We haven’t seen anything that would change our assessment that the commercial milk supply is safe,” says Donald Prater, DVM, acting director of the Center for Food Safety and Applied Nutrition at the US Food and Drug Administration (FDA).
In the federal and state milk safety system, he explained, nearly 99% of the commercial milk supply comes from farms that participate in the Grade A program and follow the Pasteurized Milk Ordinance, which outlines pasteurization requirements.
Because detection of the virus in dairy cattle is new, there are many questions to be answered in research, he reported. Among them:
- What level of virus might be leaving the farms from shedding by apparently healthy cows?
- Does any live virus survive the pasteurization process?
- Do different methods of pasteurization and dairy production have different effects on the viability of H5N1?
- Are effects different in various forms of dairy products, such as cheese and cream?
A critical question regarding the potential risk to humans is how much milk would have to be consumed for the virus to become an established infection. That information is essential to determine “what type of pasteurization criteria” are needed to provide “acceptable public health outcomes,” Dr. Prater said.
The CDC is currently using the flu surveillance system to monitor for H5N1 activity in people. The systems show no current indicators of unusual influenza activity in people.
A version of this article appeared on Medscape.com.
Dermatologic Care for Refugees: Effective Management of Scabies and Pediculosis
Approximately 108 million individuals have been forcibly displaced across the globe as of 2022, 35 million of whom are formally designated as refugees.1,2 The United States has coordinated resettlement of more refugee populations than any other country; the most common countries of origin are the Democratic Republic of the Congo, Syria, Afghanistan, and Myanmar.3 In 2021, policy to increase the number of refugees resettled in the United States by more than 700% (from 15,000 up to 125,000) was established; since enactment, the United States has seen more than double the refugee arrivals in 2023 than the prior year, making medical care for this population increasingly relevant for the dermatologist.4
Understanding how to care for this population begins with an accurate understanding of the term refugee. The United Nations defines a refugee as a person who is unwilling or unable to return to their country of nationality because of persecution or well-founded fear of persecution due to race, religion, nationality, membership in a particular social group, or political opinion. This term grants a protected status under international law and encompasses access to travel assistance, housing, cultural orientation, and medical evaluation upon resettlement.5,6
The burden of treatable dermatologic conditions in refugee populations ranges from 19% to 96% in the literature7,8 and varies from inflammatory disorders to infectious and parasitic diseases.9 In one study of 6899 displaced individuals in Greece, the prevalence of dermatologic conditions was higher than traumatic injury, cardiac disease, psychological conditions, and dental disease.10
When outlining differential diagnoses for parasitic infestations of the skin that affect refugee populations, helpful considerations include the individual’s country of origin, route traveled, and method of travel.11 Parasitic infestations specifically are more common in refugee populations when there are barriers to basic hygiene, crowded living or travel conditions, or lack of access to health care, which they may experience at any point in their home country, during travel, or in resettlement housing.8
Even with limited examination and diagnostic resources, the skin is the most accessible first indication of patients’ overall well-being and often provides simple diagnostic clues—in combination with contextualization of the patient’s unique circumstances—necessary for successful diagnosis and treatment of scabies and pediculosis.12 The dermatologist working with refugee populations may be the first set of eyes available and trained to discern skin infestations and therefore has the potential to improve overall outcomes.
Some parasitic infestations in refugee populations may fall under the category of neglected tropical diseases, including scabies, ascariasis, trypanosomiasis, leishmaniasis, and schistosomiasis; they affect an estimated 1 billion individuals across the globe but historically have been underrepresented in the literature and in health policy due in part to limited access to care.13 This review will focus on infestations by the scabies mite (Sarcoptes scabiei var hominis) and the human louse, as these frequently are encountered, easily diagnosed, and treatable by trained clinicians, even in resource-limited settings.
Scabies
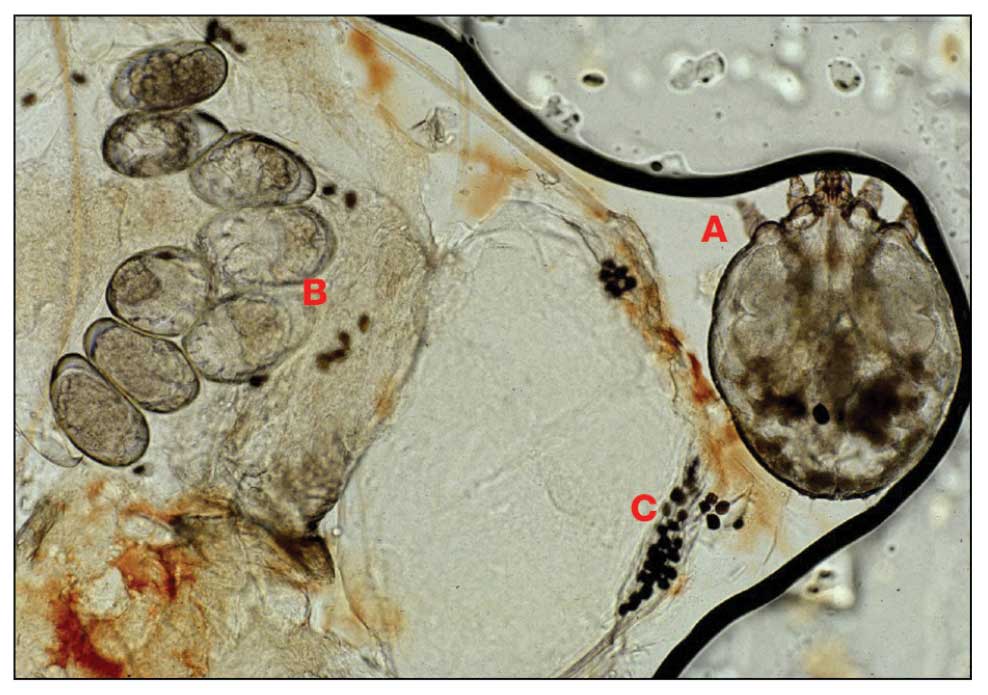
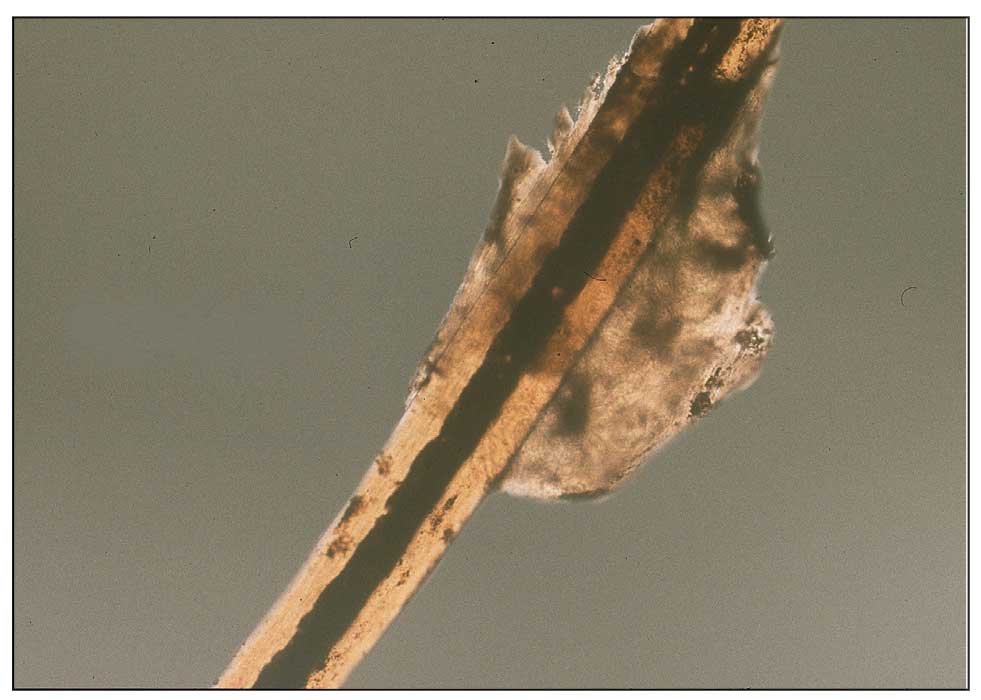
Scabies is a parasitic skin infestation caused by the 8-legged mite Sarcoptes scabiei var hominis. The female mite begins the infestation process via penetration of the epidermis, particularly the stratum corneum, and commences laying eggs (Figure 1). The subsequent larvae emerge 48 to 72 hours later and remain burrowed in the epidermis. The larvae mature over the next 10 to 14 days and continue the reproductive cycle.14,15 Symptoms of infestation occurs due to a hypersensitivity reaction to the mite and its by-products.16 Transmission of the mite primarily occurs via direct (skin-to-skin) contact with infected individuals or environmental surfaces for 24 to36 hours in specific conditions, though the latter source has been debated in the literature.
The method of transmission is particularly important when considering care for refugee populations. Scabies is found most often in those living in or traveling from tropical regions including East Asia, Southeast Asia, Oceania, and Latin America.17 In displaced or refugee populations, a lack of access to basic hygiene, extended travel in close quarters, and suboptimal health care access all may lead to an increased incidence of untreated scabies infestations.18 Scabies is more prevalent in children, with increased potential for secondary bacterial infections with Streptococcus and Staphylococcus species due to excoriation in unsanitary conditions. Secondary infection with Streptococcus pyogenes can lead to acute poststreptococcal glomerulonephritis, which accounts for a large burden of chronic kidney disease in affected populations.19 However, scabies may be found in any population, regardless of hygiene or health care access. Treating health care providers should keep a broad differential.
Presentation—The latency of scabies symptoms is 2 to 6 weeks in a primary outbreak and may be as short as 1 to 3 days with re-infestation, following the course of delayed-type hypersensitivity.20 The initial hallmark symptom is pruritus with increased severity in the evening. Visible lesions, excoriations, and burrows associated with scattered vesicles or pustules may be seen over the web spaces of the hands and feet, volar surfaces of the wrists, axillae, waist, genitalia, inner thighs, or buttocks.19 Chronic infestation often manifests with genital nodules. In populations with limited access to health care, there are reports of a sensitization phenomenon in which the individual may become less symptomatic after 4 to 6 weeks and yet be a potential carrier of the mite.21
Those with compromised immune function, such as individuals living with HIV or severe malnutrition, may present with crusted scabies, a variant that manifests as widespread hyperkeratotic scaling with more pronounced involvement of the head, neck, and acral areas. In contrast to classic scabies, crusted scabies is associated with minimal pruritus.22
Diagnosis—The diagnosis of scabies is largely clinical with confirmation through skin scrapings. The International Alliance for Control of Scabies has established diagnostic criteria that include a combination of clinical findings, history, and visualization of mites.23 A dermatologist working with refugee populations may employ any combination of history (eg, nocturnal itch, exposure to an affected individual) or clinical findings along with a high degree of suspicion in those with elevated risk. Visualization of mites is helpful to confirm the diagnosis and may be completed with the application of mineral oil at the terminal end of a burrow, skin scraping with a surgical blade or needle, and examination under light microscopy.
Treatment—First-line treatment for scabies consists of application of permethrin cream 5% on the skin of the neck to the soles of the feet, which is to be left on for 8 to 14 hours followed by rinsing. Re-application is recommended in 1 to 2 weeks. Oral ivermectin is a reasonable alternative to permethrin cream due to its low cost and easy administration in large affected groups. It is not labeled for use in pregnant women or children weighing less than 15 kg but has no selective fetal toxicity. Treatment of scabies with ivermectin has the benefit of treating many other parasitic infections. Both medications are on the World Health Organization Model List of Essential Medications and are widely available for treating providers, even in resource-limited settings.24
Much of the world still uses benzyl benzoate or precipitated sulfur ointment to treat scabies, and some botanicals used in folk medicine have genuine antiscabetic properties. Pruritus may persist for 1 to 4 weeks following treatment and does not indicate treatment failure. Topical camphor and menthol preparations, low-potency topical corticosteroids, or emollients all may be employed for relief.25 Sarna is a Spanish term for scabies and has become the proprietary name for topical antipruritic agents. Additional methods of treatment and prevention include washing clothes and linens in hot water and drying on high heat. If machine washing is not available, clothing and linens may be sealed in a plastic bag for 72 hours.
Pediculosis
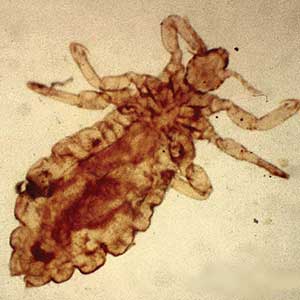
Pediculosis is an infestation caused by the ectoparasite Pediculus humanus, an obligate, sesame seed–sized louse that feeds exclusively on the blood of its host (Figure 2).26 Of the lice species, 2 require humans as hosts; one is P humanus and the other is Pthirus pubis (pubic lice). Pediculus humanus may be further classified into morphologies based largely on the affected area: body (P humanus corporis) or head (P humanus capitis), both of which will be discussed.27

Lice primarily attach to clothing and hair shafts, then transfer to the skin for blood feeds. Females lay eggs that hatch 6 to 10 days later, subsequently maturing into adults. The lifespan of these parasites with regular access to a host is 1 to 3 months for head lice and 18 days for body lice vs only 3 to 5 days without a host.28 Transmission of P humanus capitis primarily occurs via direct contact with affected individuals, either head-to-head contact or sharing of items such as brushes and headscarves; P humanus corporis also may be transmitted via direct contact with affected individuals or clothing.
Pediculosis is an important infestation to consider when providing care for refugee populations. Risk factors include lack of access to basic hygiene, including regular bathing or laundering of clothing, and crowded conditions that make direct person-to-person contact with affected individuals more likely.29 Body lice are associated more often with domestic turbulence and displaced populations30 in comparison to head lice, which have broad demographic variables, most often affecting females and children.28 Fatty acids in adult male sebum make the scalp less hospitable to lice.
Presentation—The most common clinical manifestation of pediculosis is pruritus. Cutaneous findings can include papules, wheals, or hemorrhagic puncta secondary to the louse bite. Due to the Tyndall effect of deep hemosiderin pigment, blue-grey macules termed maculae ceruleae (Figure 3) also may be present in chronic infestations of pediculosis pubis, in contrast to pediculosis capitis or corporis.31 Body louse infestation is associated with a general pruritus concentrated on the neck, shoulders, and waist—areas where clothing makes the most direct contact. Lesions may be visible and include eczematous patches with excoriation and possible secondary bacterial infection. Chronic infestation may exhibit lichenification or hyperpigmentation in associated areas. Head lice most often manifest with localized scalp pruritus and associated excoriation and cervical or occipital lymphadenopathy.32
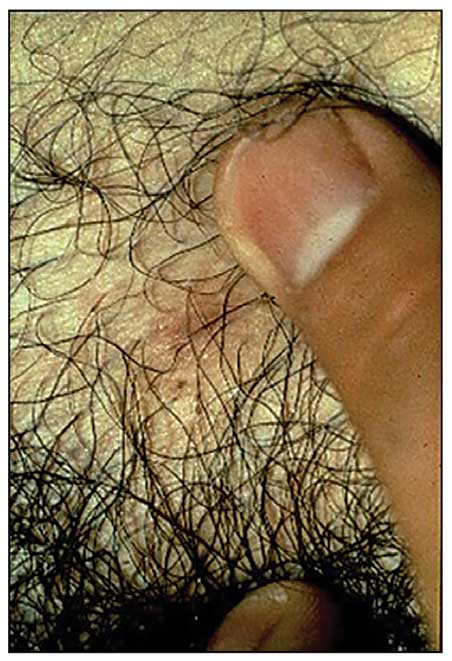
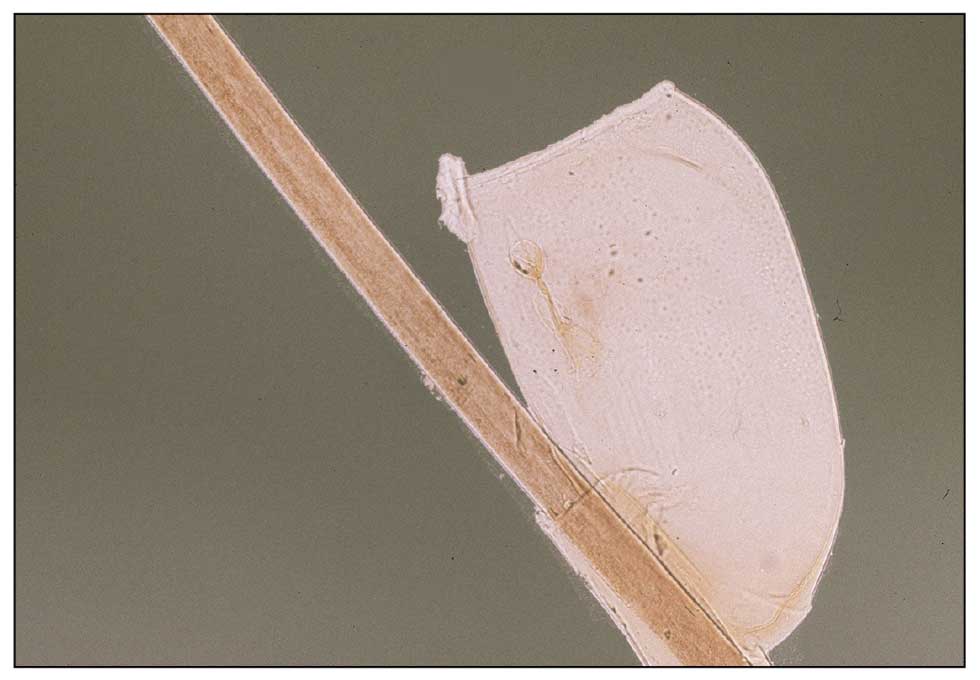
Diagnosis—The diagnosis of pediculosis is clinical, with confirmation requiring direct examination of the insect or nits (the egg case of the parasite)(Figure 4). Body lice and associated nits can be visualized on clothing seams near areas of highest body temperature, particularly the waistband. Head lice may be visualized crawling on hair shafts or on a louse comb. Nits are firmly attached to hair shafts and are visible to the naked eye, whereas pseudonits slide freely along the hair shaft and are not a manifestation of louse infestation (Figure 5).31
Treatment—Treatment varies by affected area. Pediculosis corporis may be treated with permethrin cream 5% applied to the entire body and left on for 8 to 10 hours, but this may not be necessary if facilities are available to wash and dry clothing.33 The use of oral ivermectin and permethrin-impregnated underwear both have been proposed.34,35 Treatment of pediculosis capitis may be accomplished with a variety of topical pediculicides including permethrin, pyrethrum with piperonyl butoxide, dimethicone, malathion, benzyl alcohol, spinosad, and topical ivermectin.22 Topical corticosteroids or emollients may be employed for residual pruritus.
Equally important is environmental elimination of infestation. Clothing should be discarded if possible or washed and dried using high heat. If neither approach is possible or appropriate, clothing may be sealed in a plastic bag for 2 weeks or treated with a pediculicide. Nit combing is an important adjunct in the treatment of pediculosis capitis.36 It is important to encourage return to work and/or school immediately after treatment. “No nit” policies are more harmful to education than helpful for prevention of investation.37
Pediculosis corporis may transmit infectious agents including Bartonella quintana, (trench fever, endocarditis, bacillary angiomatosis), Borrelia recurrentis (louse-borne relapsing fever), and Rickettsia prowazekii (epidemic typhus).31,38,39 Additionally, severe pediculosis infestations have the potential to cause chronic blood loss in affected populations. In a study of patients with active pediculosis infestation, mean hemoglobin values were found to be 2.5 g/dL lower than a matched population without infestation.40 It is important to consider pediculosis as a risk for iron-deficiency anemia in populations who are known to lack access to regular medical evaluation.41
Future Considerations
Increased access to tools and education for clinicians treating refugee populations is key to reducing the burden of parasitic skin disease and related morbidity and mortality in vulnerable groups both domestically and globally. One such tool, the Skin NTDs App, was launched by the World Health Organization in 2020. It is available for free for Android and iOS devices to assist clinicians in the field with the diagnosis and treatment of neglected tropical diseases—including scabies—that may affect refugee populations.42
Additionally, to both improve access and limit preventable sequelae, future investigations into appropriate models of community-based care are paramount. The model of community-based care is centered on the idea of care provision that prioritizes safety, accessibility, affordability, and acceptability in an environment closest to vulnerable populations. The largest dermatologic society, the International League of Dermatological Societies, formed a Migrant Health Dermatology Working Group that prioritizes understanding and improving care for refugee and migrant populations; this group hosted a summit in 2022, bringing together international subject matter leaders to discuss such models of care and set goals for the creation of tool kits for patients, frontline health care workers, and dermatologists.43
Conclusion
Improvement in dermatologic care of refugee populations includes provision of culturally and linguistically appropriate care by trained clinicians, adequate access to the most essential medications, and basic physical or legal access to health care systems in general.8,11,44 Parasitic infestations have the potential to remain asymptomatic for extended periods of time and result in spread to potentially nonendemic regions of resettlement.45 Additionally, the psychosocial well-being of refugee populations upon resettlement may be negatively affected by stigma of disease processes such as scabies and pediculosis, leading to additional barriers to successful re-entry into the patient’s new environment.46 Therefore, proper screening, diagnosis, and treatment of the most common parasitic infestations in this population have great potential to improve outcomes for large groups across the globe.
- Monin K, Batalova J, Lai T. Refugees and Asylees in the United States. Migration Information Source. Published May 13, 2021. Accessed April 4, 2024. https://www.migrationpolicy.org/article/refugees-and-asylees-united-states-2021
- UNHCR. Figures at a Glance. UNHCR USA. Update June 14, 2023. Accessed April 4, 2024. https://www.unhcr.org/en-us/figures-at-a-glance.html
- UNHCR. Refugee resettlement facts. Published October 2023. Accessed April 8, 2024. https://www.unhcr.org/us/media/refugee-resettlement-facts
- US Department of State. Report to Congress on Proposed Refugee Admissions for Fiscal Year 2024. Published November 3, 2023. Accessed April 8, 2024. https://www.state.gov/report-to-congress-on-proposed-refugee-admissions-for-fiscal-year-2024/
- UNHCR. Compact for Migration: Definitions. United Nations. Accessed April 4, 2024. https://refugeesmigrants.un.org/definitions
- United Nations High Commissioner for Refugees (UNHCR). Convention and Protocol Relating to the Status of Refugees. Published December 2010. Accessed January 11, 2024. https://www.unhcr.org/us/media/convention-and-protocol-relating-status-refugees
- Kibar Öztürk M. Skin diseases in rural Nyala, Sudan (in a rural hospital, in 12 orphanages, and in two refugee camps). Int J Dermatol. 2019;58:1341-1349. doi:10.1111/ijd.14619
- Padovese V, Knapp A. Challenges of managing skin diseases in refugees and migrants. Dermatol Clin. 2021;39:101-115. doi:10.1016/j.det.2020.08.010
- Saikal SL, Ge L, Mir A, et al. Skin disease profile of Syrian refugees in Jordan: a field-mission assessment. J Eur Acad Dermatol Venereol. 2020;34:419-425. doi:10.1111/jdv.15909
- Eonomopoulou A, Pavli A, Stasinopoulou P, et al. Migrant screening: lessons learned from the migrant holding level at the Greek-Turkish borders. J Infect Public Health. 2017;10:177-184. doi:10.1016/j.jiph.2016.04.012
- Marano N, Angelo KM, Merrill RD, et al. Expanding travel medicine in the 21st century to address the health needs of the world’s migrants.J Travel Med. 2018;25. doi:10.1093/jtm/tay067
- Hay RJ, Asiedu K. Skin-related neglected tropical diseases (skin NTDs)—a new challenge. Trop Med Infect Dis. 2018;4. doi:10.3390/tropicalmed4010004
- NIAID. Neglected tropical diseases. Updated July 11, 2016. Accessed April 4, 2024. https://www.niaid.nih.gov/research/neglected-tropical-diseases
- Arlian LG, Morgan MS. A review of Sarcoptes scabiei: past, present and future. Parasit Vectors. 2017;10:297. doi:10.1186/s13071-017-2234-1
- Arlian LG, Runyan RA, Achar S, et al. Survival and infectivity of Sarcoptes scabiei var. canis and var. hominis. J Am Acad Dermatol. 1984;11(2 pt 1):210-215. doi:10.1016/s0190-9622(84)70151-4
- Chandler DJ, Fuller LC. A review of scabies: an infestation more than skin deep. Dermatology. 2019;235:79-90. doi:10.1159/000495290
- Karimkhani C, Colombara DV, Drucker AM, et al. The global burden of scabies: a cross-sectional analysis from the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017;17:1247-1254. doi:10.1016/S1473-3099(17)30483-8
- Romani L, Steer AC, Whitfeld MJ, et al. Prevalence of scabies and impetigo worldwide: a systematic review. Lancet Infect Dis. 2015;15:960-967. doi:10.1016/S1473-3099(15)00132-2
- Thomas C, Coates SJ, Engelman D, et al. Ectoparasites: scabies. J Am Acad Dermatol. 2020;82:533-548. doi:10.1016/j.jaad.2019.05.109
- Mellanby K, Johnson CG, Bartley WC. Treatment of scabies. Br Med J. 1942;2:1-4. doi:10.1136/bmj.2.4252.1
- Walton SF. The immunology of susceptibility and resistance to scabies. Parasit Immunol. 2010;32:532-540. doi:10.1111/j.1365-3024.2010.01218.x
- Coates SJ, Thomas C, Chosidow O, et al. Ectoparasites: pediculosis and tungiasis. J Am Acad Dermatol. 2020;82:551-569. doi:10.1016/j.jaad.2019.05.110
- Engelman D, Fuller LC, Steer AC; International Alliance for the Control of Scabies Delphi p. Consensus criteria for the diagnosis of scabies: a Delphi study of international experts. PLoS Negl Trop Dis. 2018;12:E0006549. doi:10.1371/journal.pntd.0006549
- World Health Organization. WHO Model Lists of Essential Medicines—23rd list, 2023. Updated July 26, 2023. Accessed April 8, 2024. https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2023.02
- Salavastru CM, Chosidow O, Boffa MJ, et al. European guideline for the management of scabies. J Eur Acad Dermatol Venereol. 2017;31:1248-1253. doi:10.1111/jdv.14351
- Badiaga S, Brouqui P. Human louse-transmitted infectious diseases. Clin Microbiol Infect. 2012;18:332-337. doi:10.1111/j.1469-0691.2012.03778.x
- Leo NP, Campbell NJH, Yang X, et al. Evidence from mitochondrial DNA that head lice and body lice of humans (Phthiraptera: Pediculidae) are conspecific. J Med Entomol. 2002;39:662-666. doi:10.1603/0022-2585-39.4.662
- Chosidow O. Scabies and pediculosis. Lancet. 2000;355:819-826. doi:10.1016/S0140-6736(99)09458-1
- Arnaud A, Chosidow O, Détrez M-A, et al. Prevalences of scabies and pediculosis corporis among homeless people in the Paris region: results from two randomized cross-sectional surveys (HYTPEAC study). Br J Dermatol. 2016;174:104-112. doi:10.1111/bjd.14226
- Brouqui P. Arthropod-borne diseases associated with political and social disorder. Annu Rev Entomol. 2011;56:357-374. doi:10.1146/annurev-ento-120709-144739
- Ko CJ, Elston DM. Pediculosis. J Am Acad Dermatol. 2004;50:1-12. doi:10.1016/S0190-9622(03)02729-4
- Bloomfield D. Head lice. Pediatr Rev. 2002;23:34-35; discussion 34-35. doi:10.1542/pir.23-1-34
- Stone SP GJ, Bacelieri RE. Scabies, other mites, and pediculosis. In: Wolf K GL, Katz SI, et al (eds). Fitzpatrick’s Dermatology in General Medicine. McGraw Hill; 2008:2029.
- Foucault C, Ranque S, Badiaga S, et al. Oral ivermectin in the treatment of body lice. J Infect Dis. 2006;193:474-476. doi:10.1086/499279
- Benkouiten S, Drali R, Badiaga S, et al. Effect of permethrin-impregnated underwear on body lice in sheltered homeless persons: a randomized controlled trial. JAMA Dermatol. 2014;150:273-279. doi:10.1001/jamadermatol.2013.6398
- CDC. Parasites: Treatment. Updated October 15, 2019. Accessed April 4, 2024. https://www.cdc.gov/parasites/lice/head/treatment.html
- Devore CD, Schutze GE; Council on School Health and Committee on Infectious Diseases, American Academy of Pediatrics. Head lice. Pediatrics. 2015;135:e1355-e1365. doi:10.1542/peds.2015-0746
- Ohl ME, Spach DH. Bartonella quintana and urban trench fever. Clin Infect Dis. 2000;31:131-135. doi:10.1086/313890
- Drali R, Sangaré AK, Boutellis A, et al. Bartonella quintana in body lice from scalp hair of homeless persons, France. Emerg Infect Dis. 2014;20:907-908. doi:10.3201/eid2005.131242
- Rudd N, Zakaria A, Kohn MA, et al. Association of body lice infestation with hemoglobin values in hospitalized dermatology patients. JAMA Dermatol. 2022;158:691-693. doi:10.1001/jamadermatol.2022.0818
- Guss DA, Koenig M, Castillo EM. Severe iron deficiency anemia and lice infestation. J Emergency Med. 2011;41:362-365. doi:10.1016/j.jemermed.2010.05.030
- Neglected tropical diseases of the skin: WHO launches mobile application to facilitate diagnosis. News release. World Health Organization; July 16, 2020. Accessed April 4, 2024. https://www.who.int/news/item/16-07-2020-neglected-tropical-diseases-of-the-skin-who-launches-mobile-application-to-facilitate-diagnosis
- Padovese V, Fuller LC, Griffiths CEM, et al; Migrant Health Dermatology Working Group of the International Foundation for Dermatology. Migrant skin health: perspectives from the Migrant Health Summit, Malta, 2022. Br J Dermatology. 2023;188:553-554. doi:10.1093/bjd/ljad001
- Knapp AP, Rehmus W, Chang AY. Skin diseases in displaced populations: a review of contributing factors, challenges, and approaches to care. Int J Dermatol. 2020;59:1299-1311. doi:10.1111/ijd.15063
- Norman FF, Comeche B, Chamorro S, et al. Overcoming challenges in the diagnosis and treatment of parasitic infectious diseases in migrants. Expert Rev Anti-infective Therapy. 2020;18:127-143. doi:10.1080/14787210.2020.1713099
- Skin NTDs: prioritizing integrated approaches to reduce suffering, psychosocial impact and stigmatization. News release. World Health Organization; October 29, 2020. Accessed April 4, 2024. https://www.who.int/news/item/29-10-2020-skin-ntds-prioritizing-integrated-approaches-to-reduce-suffering-psychosocial-impact-and-stigmatization
Approximately 108 million individuals have been forcibly displaced across the globe as of 2022, 35 million of whom are formally designated as refugees.1,2 The United States has coordinated resettlement of more refugee populations than any other country; the most common countries of origin are the Democratic Republic of the Congo, Syria, Afghanistan, and Myanmar.3 In 2021, policy to increase the number of refugees resettled in the United States by more than 700% (from 15,000 up to 125,000) was established; since enactment, the United States has seen more than double the refugee arrivals in 2023 than the prior year, making medical care for this population increasingly relevant for the dermatologist.4
Understanding how to care for this population begins with an accurate understanding of the term refugee. The United Nations defines a refugee as a person who is unwilling or unable to return to their country of nationality because of persecution or well-founded fear of persecution due to race, religion, nationality, membership in a particular social group, or political opinion. This term grants a protected status under international law and encompasses access to travel assistance, housing, cultural orientation, and medical evaluation upon resettlement.5,6
The burden of treatable dermatologic conditions in refugee populations ranges from 19% to 96% in the literature7,8 and varies from inflammatory disorders to infectious and parasitic diseases.9 In one study of 6899 displaced individuals in Greece, the prevalence of dermatologic conditions was higher than traumatic injury, cardiac disease, psychological conditions, and dental disease.10
When outlining differential diagnoses for parasitic infestations of the skin that affect refugee populations, helpful considerations include the individual’s country of origin, route traveled, and method of travel.11 Parasitic infestations specifically are more common in refugee populations when there are barriers to basic hygiene, crowded living or travel conditions, or lack of access to health care, which they may experience at any point in their home country, during travel, or in resettlement housing.8
Even with limited examination and diagnostic resources, the skin is the most accessible first indication of patients’ overall well-being and often provides simple diagnostic clues—in combination with contextualization of the patient’s unique circumstances—necessary for successful diagnosis and treatment of scabies and pediculosis.12 The dermatologist working with refugee populations may be the first set of eyes available and trained to discern skin infestations and therefore has the potential to improve overall outcomes.
Some parasitic infestations in refugee populations may fall under the category of neglected tropical diseases, including scabies, ascariasis, trypanosomiasis, leishmaniasis, and schistosomiasis; they affect an estimated 1 billion individuals across the globe but historically have been underrepresented in the literature and in health policy due in part to limited access to care.13 This review will focus on infestations by the scabies mite (Sarcoptes scabiei var hominis) and the human louse, as these frequently are encountered, easily diagnosed, and treatable by trained clinicians, even in resource-limited settings.
Scabies
Scabies is a parasitic skin infestation caused by the 8-legged mite Sarcoptes scabiei var hominis. The female mite begins the infestation process via penetration of the epidermis, particularly the stratum corneum, and commences laying eggs (Figure 1). The subsequent larvae emerge 48 to 72 hours later and remain burrowed in the epidermis. The larvae mature over the next 10 to 14 days and continue the reproductive cycle.14,15 Symptoms of infestation occurs due to a hypersensitivity reaction to the mite and its by-products.16 Transmission of the mite primarily occurs via direct (skin-to-skin) contact with infected individuals or environmental surfaces for 24 to36 hours in specific conditions, though the latter source has been debated in the literature.
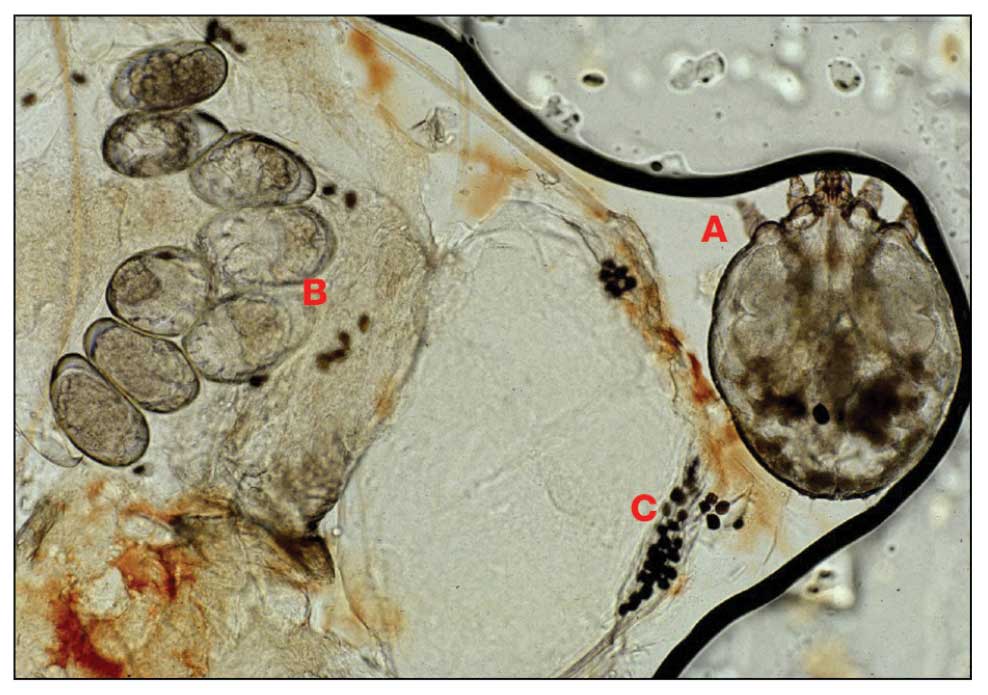
The method of transmission is particularly important when considering care for refugee populations. Scabies is found most often in those living in or traveling from tropical regions including East Asia, Southeast Asia, Oceania, and Latin America.17 In displaced or refugee populations, a lack of access to basic hygiene, extended travel in close quarters, and suboptimal health care access all may lead to an increased incidence of untreated scabies infestations.18 Scabies is more prevalent in children, with increased potential for secondary bacterial infections with Streptococcus and Staphylococcus species due to excoriation in unsanitary conditions. Secondary infection with Streptococcus pyogenes can lead to acute poststreptococcal glomerulonephritis, which accounts for a large burden of chronic kidney disease in affected populations.19 However, scabies may be found in any population, regardless of hygiene or health care access. Treating health care providers should keep a broad differential.
Presentation—The latency of scabies symptoms is 2 to 6 weeks in a primary outbreak and may be as short as 1 to 3 days with re-infestation, following the course of delayed-type hypersensitivity.20 The initial hallmark symptom is pruritus with increased severity in the evening. Visible lesions, excoriations, and burrows associated with scattered vesicles or pustules may be seen over the web spaces of the hands and feet, volar surfaces of the wrists, axillae, waist, genitalia, inner thighs, or buttocks.19 Chronic infestation often manifests with genital nodules. In populations with limited access to health care, there are reports of a sensitization phenomenon in which the individual may become less symptomatic after 4 to 6 weeks and yet be a potential carrier of the mite.21
Those with compromised immune function, such as individuals living with HIV or severe malnutrition, may present with crusted scabies, a variant that manifests as widespread hyperkeratotic scaling with more pronounced involvement of the head, neck, and acral areas. In contrast to classic scabies, crusted scabies is associated with minimal pruritus.22
Diagnosis—The diagnosis of scabies is largely clinical with confirmation through skin scrapings. The International Alliance for Control of Scabies has established diagnostic criteria that include a combination of clinical findings, history, and visualization of mites.23 A dermatologist working with refugee populations may employ any combination of history (eg, nocturnal itch, exposure to an affected individual) or clinical findings along with a high degree of suspicion in those with elevated risk. Visualization of mites is helpful to confirm the diagnosis and may be completed with the application of mineral oil at the terminal end of a burrow, skin scraping with a surgical blade or needle, and examination under light microscopy.
Treatment—First-line treatment for scabies consists of application of permethrin cream 5% on the skin of the neck to the soles of the feet, which is to be left on for 8 to 14 hours followed by rinsing. Re-application is recommended in 1 to 2 weeks. Oral ivermectin is a reasonable alternative to permethrin cream due to its low cost and easy administration in large affected groups. It is not labeled for use in pregnant women or children weighing less than 15 kg but has no selective fetal toxicity. Treatment of scabies with ivermectin has the benefit of treating many other parasitic infections. Both medications are on the World Health Organization Model List of Essential Medications and are widely available for treating providers, even in resource-limited settings.24
Much of the world still uses benzyl benzoate or precipitated sulfur ointment to treat scabies, and some botanicals used in folk medicine have genuine antiscabetic properties. Pruritus may persist for 1 to 4 weeks following treatment and does not indicate treatment failure. Topical camphor and menthol preparations, low-potency topical corticosteroids, or emollients all may be employed for relief.25 Sarna is a Spanish term for scabies and has become the proprietary name for topical antipruritic agents. Additional methods of treatment and prevention include washing clothes and linens in hot water and drying on high heat. If machine washing is not available, clothing and linens may be sealed in a plastic bag for 72 hours.
Pediculosis
Pediculosis is an infestation caused by the ectoparasite Pediculus humanus, an obligate, sesame seed–sized louse that feeds exclusively on the blood of its host (Figure 2).26 Of the lice species, 2 require humans as hosts; one is P humanus and the other is Pthirus pubis (pubic lice). Pediculus humanus may be further classified into morphologies based largely on the affected area: body (P humanus corporis) or head (P humanus capitis), both of which will be discussed.27

Lice primarily attach to clothing and hair shafts, then transfer to the skin for blood feeds. Females lay eggs that hatch 6 to 10 days later, subsequently maturing into adults. The lifespan of these parasites with regular access to a host is 1 to 3 months for head lice and 18 days for body lice vs only 3 to 5 days without a host.28 Transmission of P humanus capitis primarily occurs via direct contact with affected individuals, either head-to-head contact or sharing of items such as brushes and headscarves; P humanus corporis also may be transmitted via direct contact with affected individuals or clothing.
Pediculosis is an important infestation to consider when providing care for refugee populations. Risk factors include lack of access to basic hygiene, including regular bathing or laundering of clothing, and crowded conditions that make direct person-to-person contact with affected individuals more likely.29 Body lice are associated more often with domestic turbulence and displaced populations30 in comparison to head lice, which have broad demographic variables, most often affecting females and children.28 Fatty acids in adult male sebum make the scalp less hospitable to lice.
Presentation—The most common clinical manifestation of pediculosis is pruritus. Cutaneous findings can include papules, wheals, or hemorrhagic puncta secondary to the louse bite. Due to the Tyndall effect of deep hemosiderin pigment, blue-grey macules termed maculae ceruleae (Figure 3) also may be present in chronic infestations of pediculosis pubis, in contrast to pediculosis capitis or corporis.31 Body louse infestation is associated with a general pruritus concentrated on the neck, shoulders, and waist—areas where clothing makes the most direct contact. Lesions may be visible and include eczematous patches with excoriation and possible secondary bacterial infection. Chronic infestation may exhibit lichenification or hyperpigmentation in associated areas. Head lice most often manifest with localized scalp pruritus and associated excoriation and cervical or occipital lymphadenopathy.32
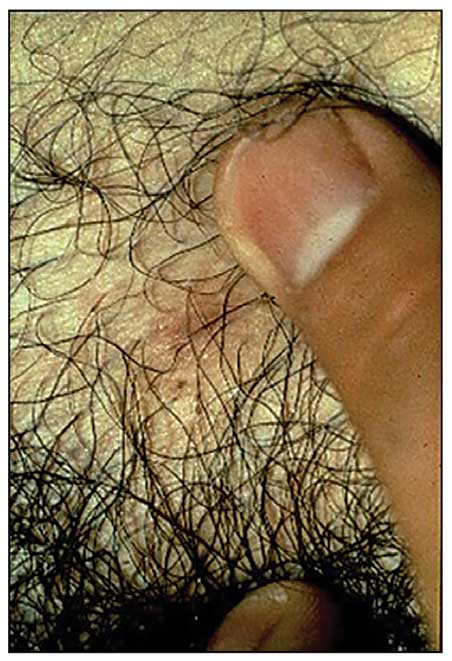
Diagnosis—The diagnosis of pediculosis is clinical, with confirmation requiring direct examination of the insect or nits (the egg case of the parasite)(Figure 4). Body lice and associated nits can be visualized on clothing seams near areas of highest body temperature, particularly the waistband. Head lice may be visualized crawling on hair shafts or on a louse comb. Nits are firmly attached to hair shafts and are visible to the naked eye, whereas pseudonits slide freely along the hair shaft and are not a manifestation of louse infestation (Figure 5).31
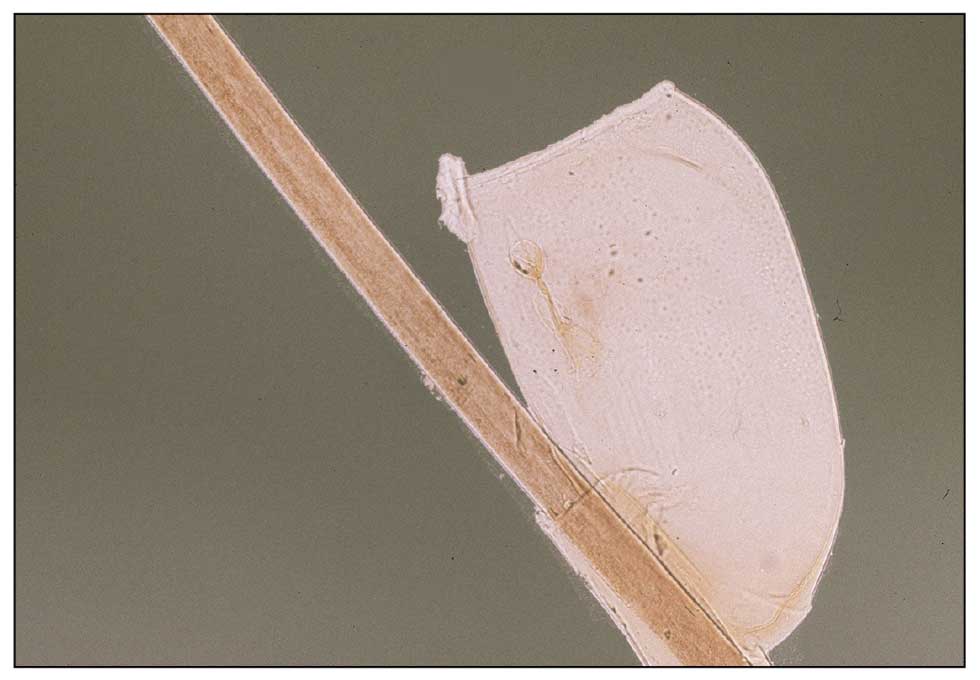
Treatment—Treatment varies by affected area. Pediculosis corporis may be treated with permethrin cream 5% applied to the entire body and left on for 8 to 10 hours, but this may not be necessary if facilities are available to wash and dry clothing.33 The use of oral ivermectin and permethrin-impregnated underwear both have been proposed.34,35 Treatment of pediculosis capitis may be accomplished with a variety of topical pediculicides including permethrin, pyrethrum with piperonyl butoxide, dimethicone, malathion, benzyl alcohol, spinosad, and topical ivermectin.22 Topical corticosteroids or emollients may be employed for residual pruritus.
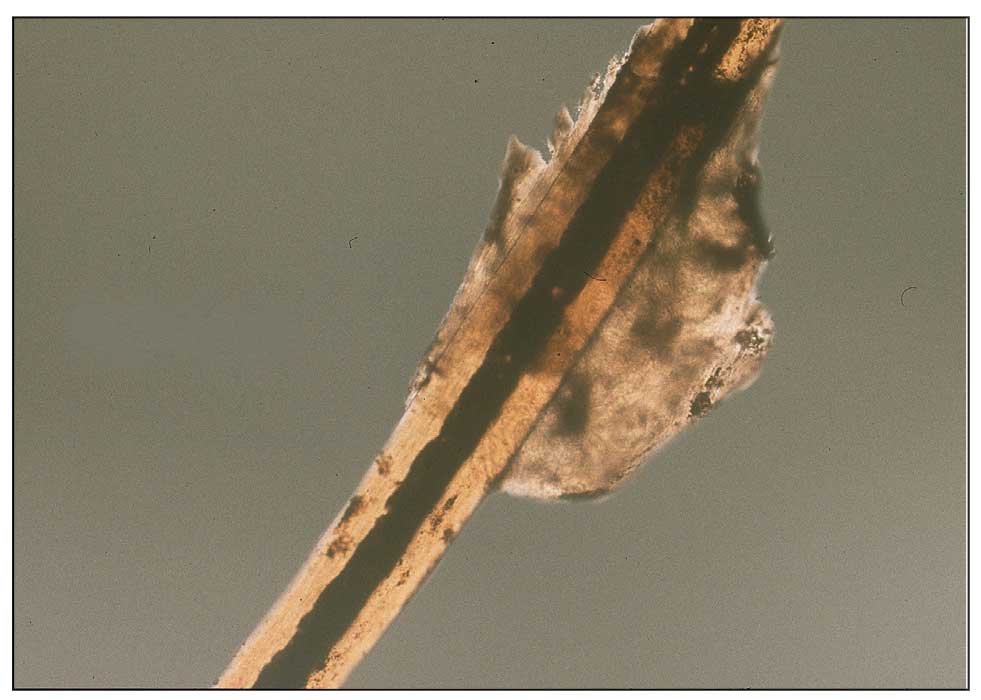
Equally important is environmental elimination of infestation. Clothing should be discarded if possible or washed and dried using high heat. If neither approach is possible or appropriate, clothing may be sealed in a plastic bag for 2 weeks or treated with a pediculicide. Nit combing is an important adjunct in the treatment of pediculosis capitis.36 It is important to encourage return to work and/or school immediately after treatment. “No nit” policies are more harmful to education than helpful for prevention of investation.37
Pediculosis corporis may transmit infectious agents including Bartonella quintana, (trench fever, endocarditis, bacillary angiomatosis), Borrelia recurrentis (louse-borne relapsing fever), and Rickettsia prowazekii (epidemic typhus).31,38,39 Additionally, severe pediculosis infestations have the potential to cause chronic blood loss in affected populations. In a study of patients with active pediculosis infestation, mean hemoglobin values were found to be 2.5 g/dL lower than a matched population without infestation.40 It is important to consider pediculosis as a risk for iron-deficiency anemia in populations who are known to lack access to regular medical evaluation.41
Future Considerations
Increased access to tools and education for clinicians treating refugee populations is key to reducing the burden of parasitic skin disease and related morbidity and mortality in vulnerable groups both domestically and globally. One such tool, the Skin NTDs App, was launched by the World Health Organization in 2020. It is available for free for Android and iOS devices to assist clinicians in the field with the diagnosis and treatment of neglected tropical diseases—including scabies—that may affect refugee populations.42
Additionally, to both improve access and limit preventable sequelae, future investigations into appropriate models of community-based care are paramount. The model of community-based care is centered on the idea of care provision that prioritizes safety, accessibility, affordability, and acceptability in an environment closest to vulnerable populations. The largest dermatologic society, the International League of Dermatological Societies, formed a Migrant Health Dermatology Working Group that prioritizes understanding and improving care for refugee and migrant populations; this group hosted a summit in 2022, bringing together international subject matter leaders to discuss such models of care and set goals for the creation of tool kits for patients, frontline health care workers, and dermatologists.43
Conclusion
Improvement in dermatologic care of refugee populations includes provision of culturally and linguistically appropriate care by trained clinicians, adequate access to the most essential medications, and basic physical or legal access to health care systems in general.8,11,44 Parasitic infestations have the potential to remain asymptomatic for extended periods of time and result in spread to potentially nonendemic regions of resettlement.45 Additionally, the psychosocial well-being of refugee populations upon resettlement may be negatively affected by stigma of disease processes such as scabies and pediculosis, leading to additional barriers to successful re-entry into the patient’s new environment.46 Therefore, proper screening, diagnosis, and treatment of the most common parasitic infestations in this population have great potential to improve outcomes for large groups across the globe.
Approximately 108 million individuals have been forcibly displaced across the globe as of 2022, 35 million of whom are formally designated as refugees.1,2 The United States has coordinated resettlement of more refugee populations than any other country; the most common countries of origin are the Democratic Republic of the Congo, Syria, Afghanistan, and Myanmar.3 In 2021, policy to increase the number of refugees resettled in the United States by more than 700% (from 15,000 up to 125,000) was established; since enactment, the United States has seen more than double the refugee arrivals in 2023 than the prior year, making medical care for this population increasingly relevant for the dermatologist.4
Understanding how to care for this population begins with an accurate understanding of the term refugee. The United Nations defines a refugee as a person who is unwilling or unable to return to their country of nationality because of persecution or well-founded fear of persecution due to race, religion, nationality, membership in a particular social group, or political opinion. This term grants a protected status under international law and encompasses access to travel assistance, housing, cultural orientation, and medical evaluation upon resettlement.5,6
The burden of treatable dermatologic conditions in refugee populations ranges from 19% to 96% in the literature7,8 and varies from inflammatory disorders to infectious and parasitic diseases.9 In one study of 6899 displaced individuals in Greece, the prevalence of dermatologic conditions was higher than traumatic injury, cardiac disease, psychological conditions, and dental disease.10
When outlining differential diagnoses for parasitic infestations of the skin that affect refugee populations, helpful considerations include the individual’s country of origin, route traveled, and method of travel.11 Parasitic infestations specifically are more common in refugee populations when there are barriers to basic hygiene, crowded living or travel conditions, or lack of access to health care, which they may experience at any point in their home country, during travel, or in resettlement housing.8
Even with limited examination and diagnostic resources, the skin is the most accessible first indication of patients’ overall well-being and often provides simple diagnostic clues—in combination with contextualization of the patient’s unique circumstances—necessary for successful diagnosis and treatment of scabies and pediculosis.12 The dermatologist working with refugee populations may be the first set of eyes available and trained to discern skin infestations and therefore has the potential to improve overall outcomes.
Some parasitic infestations in refugee populations may fall under the category of neglected tropical diseases, including scabies, ascariasis, trypanosomiasis, leishmaniasis, and schistosomiasis; they affect an estimated 1 billion individuals across the globe but historically have been underrepresented in the literature and in health policy due in part to limited access to care.13 This review will focus on infestations by the scabies mite (Sarcoptes scabiei var hominis) and the human louse, as these frequently are encountered, easily diagnosed, and treatable by trained clinicians, even in resource-limited settings.
Scabies
Scabies is a parasitic skin infestation caused by the 8-legged mite Sarcoptes scabiei var hominis. The female mite begins the infestation process via penetration of the epidermis, particularly the stratum corneum, and commences laying eggs (Figure 1). The subsequent larvae emerge 48 to 72 hours later and remain burrowed in the epidermis. The larvae mature over the next 10 to 14 days and continue the reproductive cycle.14,15 Symptoms of infestation occurs due to a hypersensitivity reaction to the mite and its by-products.16 Transmission of the mite primarily occurs via direct (skin-to-skin) contact with infected individuals or environmental surfaces for 24 to36 hours in specific conditions, though the latter source has been debated in the literature.
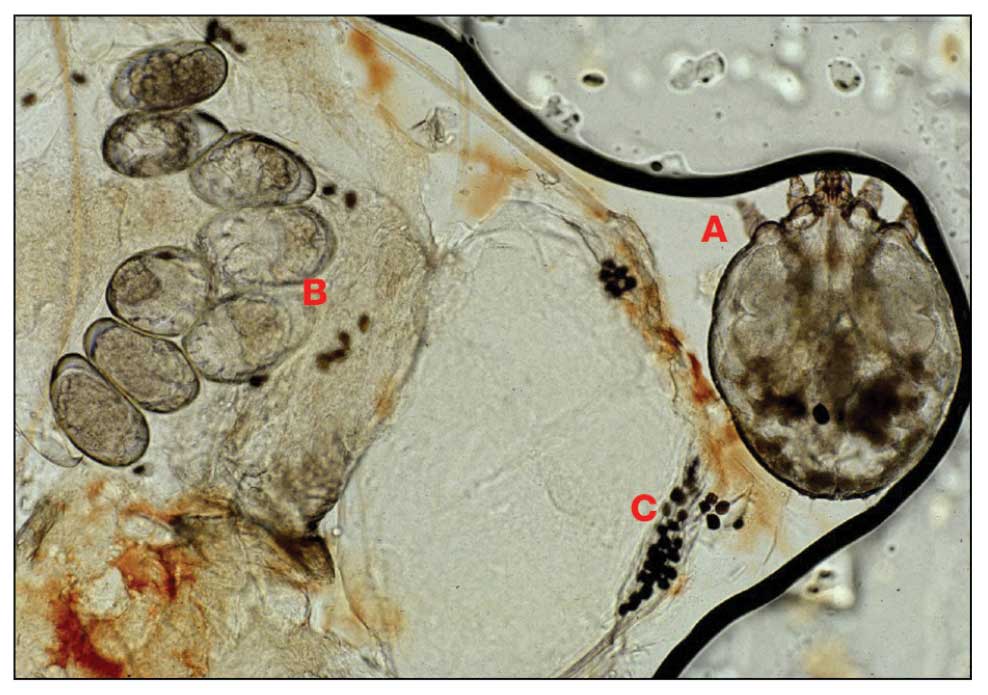
The method of transmission is particularly important when considering care for refugee populations. Scabies is found most often in those living in or traveling from tropical regions including East Asia, Southeast Asia, Oceania, and Latin America.17 In displaced or refugee populations, a lack of access to basic hygiene, extended travel in close quarters, and suboptimal health care access all may lead to an increased incidence of untreated scabies infestations.18 Scabies is more prevalent in children, with increased potential for secondary bacterial infections with Streptococcus and Staphylococcus species due to excoriation in unsanitary conditions. Secondary infection with Streptococcus pyogenes can lead to acute poststreptococcal glomerulonephritis, which accounts for a large burden of chronic kidney disease in affected populations.19 However, scabies may be found in any population, regardless of hygiene or health care access. Treating health care providers should keep a broad differential.
Presentation—The latency of scabies symptoms is 2 to 6 weeks in a primary outbreak and may be as short as 1 to 3 days with re-infestation, following the course of delayed-type hypersensitivity.20 The initial hallmark symptom is pruritus with increased severity in the evening. Visible lesions, excoriations, and burrows associated with scattered vesicles or pustules may be seen over the web spaces of the hands and feet, volar surfaces of the wrists, axillae, waist, genitalia, inner thighs, or buttocks.19 Chronic infestation often manifests with genital nodules. In populations with limited access to health care, there are reports of a sensitization phenomenon in which the individual may become less symptomatic after 4 to 6 weeks and yet be a potential carrier of the mite.21
Those with compromised immune function, such as individuals living with HIV or severe malnutrition, may present with crusted scabies, a variant that manifests as widespread hyperkeratotic scaling with more pronounced involvement of the head, neck, and acral areas. In contrast to classic scabies, crusted scabies is associated with minimal pruritus.22
Diagnosis—The diagnosis of scabies is largely clinical with confirmation through skin scrapings. The International Alliance for Control of Scabies has established diagnostic criteria that include a combination of clinical findings, history, and visualization of mites.23 A dermatologist working with refugee populations may employ any combination of history (eg, nocturnal itch, exposure to an affected individual) or clinical findings along with a high degree of suspicion in those with elevated risk. Visualization of mites is helpful to confirm the diagnosis and may be completed with the application of mineral oil at the terminal end of a burrow, skin scraping with a surgical blade or needle, and examination under light microscopy.
Treatment—First-line treatment for scabies consists of application of permethrin cream 5% on the skin of the neck to the soles of the feet, which is to be left on for 8 to 14 hours followed by rinsing. Re-application is recommended in 1 to 2 weeks. Oral ivermectin is a reasonable alternative to permethrin cream due to its low cost and easy administration in large affected groups. It is not labeled for use in pregnant women or children weighing less than 15 kg but has no selective fetal toxicity. Treatment of scabies with ivermectin has the benefit of treating many other parasitic infections. Both medications are on the World Health Organization Model List of Essential Medications and are widely available for treating providers, even in resource-limited settings.24
Much of the world still uses benzyl benzoate or precipitated sulfur ointment to treat scabies, and some botanicals used in folk medicine have genuine antiscabetic properties. Pruritus may persist for 1 to 4 weeks following treatment and does not indicate treatment failure. Topical camphor and menthol preparations, low-potency topical corticosteroids, or emollients all may be employed for relief.25 Sarna is a Spanish term for scabies and has become the proprietary name for topical antipruritic agents. Additional methods of treatment and prevention include washing clothes and linens in hot water and drying on high heat. If machine washing is not available, clothing and linens may be sealed in a plastic bag for 72 hours.
Pediculosis
Pediculosis is an infestation caused by the ectoparasite Pediculus humanus, an obligate, sesame seed–sized louse that feeds exclusively on the blood of its host (Figure 2).26 Of the lice species, 2 require humans as hosts; one is P humanus and the other is Pthirus pubis (pubic lice). Pediculus humanus may be further classified into morphologies based largely on the affected area: body (P humanus corporis) or head (P humanus capitis), both of which will be discussed.27

Lice primarily attach to clothing and hair shafts, then transfer to the skin for blood feeds. Females lay eggs that hatch 6 to 10 days later, subsequently maturing into adults. The lifespan of these parasites with regular access to a host is 1 to 3 months for head lice and 18 days for body lice vs only 3 to 5 days without a host.28 Transmission of P humanus capitis primarily occurs via direct contact with affected individuals, either head-to-head contact or sharing of items such as brushes and headscarves; P humanus corporis also may be transmitted via direct contact with affected individuals or clothing.
Pediculosis is an important infestation to consider when providing care for refugee populations. Risk factors include lack of access to basic hygiene, including regular bathing or laundering of clothing, and crowded conditions that make direct person-to-person contact with affected individuals more likely.29 Body lice are associated more often with domestic turbulence and displaced populations30 in comparison to head lice, which have broad demographic variables, most often affecting females and children.28 Fatty acids in adult male sebum make the scalp less hospitable to lice.
Presentation—The most common clinical manifestation of pediculosis is pruritus. Cutaneous findings can include papules, wheals, or hemorrhagic puncta secondary to the louse bite. Due to the Tyndall effect of deep hemosiderin pigment, blue-grey macules termed maculae ceruleae (Figure 3) also may be present in chronic infestations of pediculosis pubis, in contrast to pediculosis capitis or corporis.31 Body louse infestation is associated with a general pruritus concentrated on the neck, shoulders, and waist—areas where clothing makes the most direct contact. Lesions may be visible and include eczematous patches with excoriation and possible secondary bacterial infection. Chronic infestation may exhibit lichenification or hyperpigmentation in associated areas. Head lice most often manifest with localized scalp pruritus and associated excoriation and cervical or occipital lymphadenopathy.32
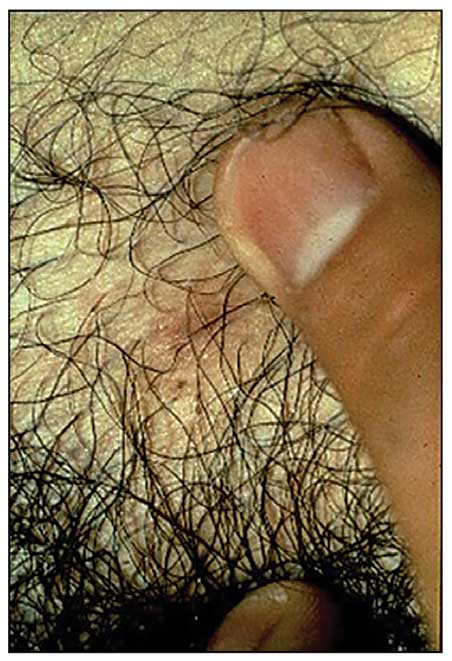
Diagnosis—The diagnosis of pediculosis is clinical, with confirmation requiring direct examination of the insect or nits (the egg case of the parasite)(Figure 4). Body lice and associated nits can be visualized on clothing seams near areas of highest body temperature, particularly the waistband. Head lice may be visualized crawling on hair shafts or on a louse comb. Nits are firmly attached to hair shafts and are visible to the naked eye, whereas pseudonits slide freely along the hair shaft and are not a manifestation of louse infestation (Figure 5).31
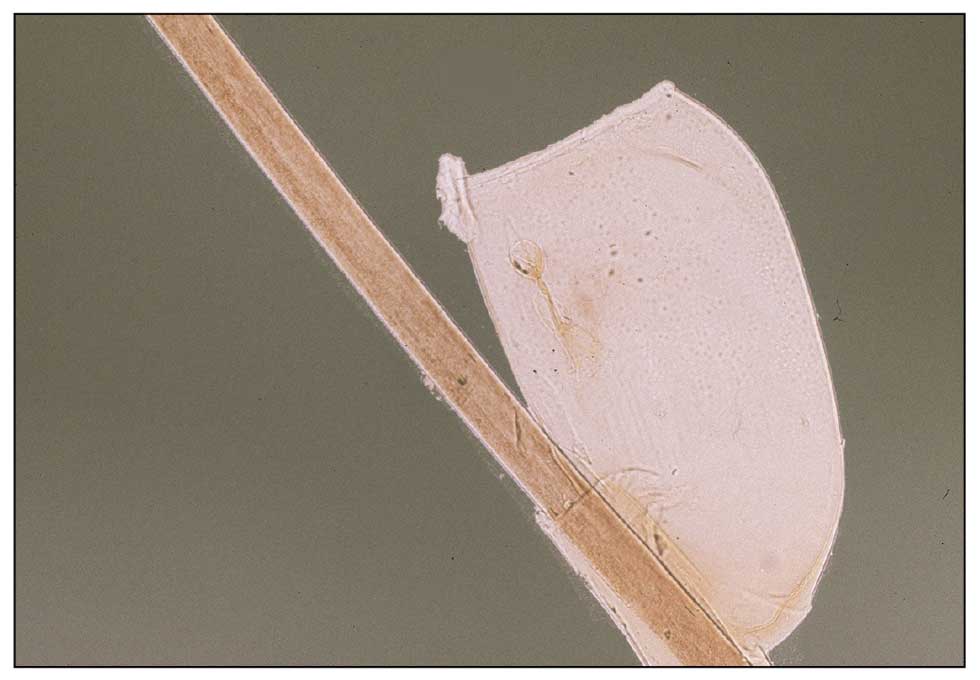
Treatment—Treatment varies by affected area. Pediculosis corporis may be treated with permethrin cream 5% applied to the entire body and left on for 8 to 10 hours, but this may not be necessary if facilities are available to wash and dry clothing.33 The use of oral ivermectin and permethrin-impregnated underwear both have been proposed.34,35 Treatment of pediculosis capitis may be accomplished with a variety of topical pediculicides including permethrin, pyrethrum with piperonyl butoxide, dimethicone, malathion, benzyl alcohol, spinosad, and topical ivermectin.22 Topical corticosteroids or emollients may be employed for residual pruritus.
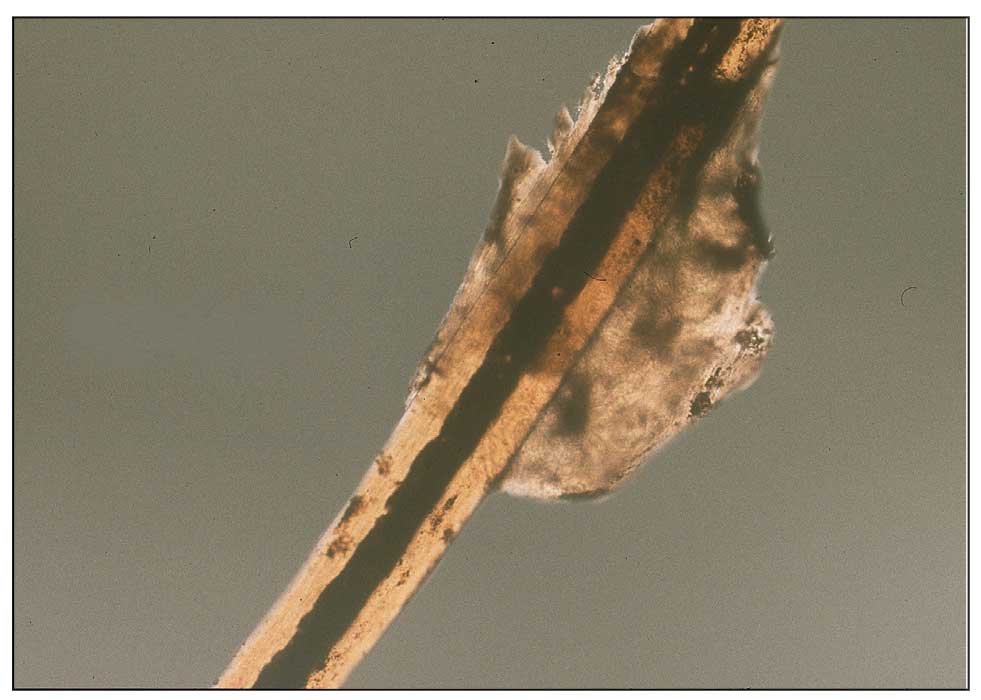
Equally important is environmental elimination of infestation. Clothing should be discarded if possible or washed and dried using high heat. If neither approach is possible or appropriate, clothing may be sealed in a plastic bag for 2 weeks or treated with a pediculicide. Nit combing is an important adjunct in the treatment of pediculosis capitis.36 It is important to encourage return to work and/or school immediately after treatment. “No nit” policies are more harmful to education than helpful for prevention of investation.37
Pediculosis corporis may transmit infectious agents including Bartonella quintana, (trench fever, endocarditis, bacillary angiomatosis), Borrelia recurrentis (louse-borne relapsing fever), and Rickettsia prowazekii (epidemic typhus).31,38,39 Additionally, severe pediculosis infestations have the potential to cause chronic blood loss in affected populations. In a study of patients with active pediculosis infestation, mean hemoglobin values were found to be 2.5 g/dL lower than a matched population without infestation.40 It is important to consider pediculosis as a risk for iron-deficiency anemia in populations who are known to lack access to regular medical evaluation.41
Future Considerations
Increased access to tools and education for clinicians treating refugee populations is key to reducing the burden of parasitic skin disease and related morbidity and mortality in vulnerable groups both domestically and globally. One such tool, the Skin NTDs App, was launched by the World Health Organization in 2020. It is available for free for Android and iOS devices to assist clinicians in the field with the diagnosis and treatment of neglected tropical diseases—including scabies—that may affect refugee populations.42
Additionally, to both improve access and limit preventable sequelae, future investigations into appropriate models of community-based care are paramount. The model of community-based care is centered on the idea of care provision that prioritizes safety, accessibility, affordability, and acceptability in an environment closest to vulnerable populations. The largest dermatologic society, the International League of Dermatological Societies, formed a Migrant Health Dermatology Working Group that prioritizes understanding and improving care for refugee and migrant populations; this group hosted a summit in 2022, bringing together international subject matter leaders to discuss such models of care and set goals for the creation of tool kits for patients, frontline health care workers, and dermatologists.43
Conclusion
Improvement in dermatologic care of refugee populations includes provision of culturally and linguistically appropriate care by trained clinicians, adequate access to the most essential medications, and basic physical or legal access to health care systems in general.8,11,44 Parasitic infestations have the potential to remain asymptomatic for extended periods of time and result in spread to potentially nonendemic regions of resettlement.45 Additionally, the psychosocial well-being of refugee populations upon resettlement may be negatively affected by stigma of disease processes such as scabies and pediculosis, leading to additional barriers to successful re-entry into the patient’s new environment.46 Therefore, proper screening, diagnosis, and treatment of the most common parasitic infestations in this population have great potential to improve outcomes for large groups across the globe.
- Monin K, Batalova J, Lai T. Refugees and Asylees in the United States. Migration Information Source. Published May 13, 2021. Accessed April 4, 2024. https://www.migrationpolicy.org/article/refugees-and-asylees-united-states-2021
- UNHCR. Figures at a Glance. UNHCR USA. Update June 14, 2023. Accessed April 4, 2024. https://www.unhcr.org/en-us/figures-at-a-glance.html
- UNHCR. Refugee resettlement facts. Published October 2023. Accessed April 8, 2024. https://www.unhcr.org/us/media/refugee-resettlement-facts
- US Department of State. Report to Congress on Proposed Refugee Admissions for Fiscal Year 2024. Published November 3, 2023. Accessed April 8, 2024. https://www.state.gov/report-to-congress-on-proposed-refugee-admissions-for-fiscal-year-2024/
- UNHCR. Compact for Migration: Definitions. United Nations. Accessed April 4, 2024. https://refugeesmigrants.un.org/definitions
- United Nations High Commissioner for Refugees (UNHCR). Convention and Protocol Relating to the Status of Refugees. Published December 2010. Accessed January 11, 2024. https://www.unhcr.org/us/media/convention-and-protocol-relating-status-refugees
- Kibar Öztürk M. Skin diseases in rural Nyala, Sudan (in a rural hospital, in 12 orphanages, and in two refugee camps). Int J Dermatol. 2019;58:1341-1349. doi:10.1111/ijd.14619
- Padovese V, Knapp A. Challenges of managing skin diseases in refugees and migrants. Dermatol Clin. 2021;39:101-115. doi:10.1016/j.det.2020.08.010
- Saikal SL, Ge L, Mir A, et al. Skin disease profile of Syrian refugees in Jordan: a field-mission assessment. J Eur Acad Dermatol Venereol. 2020;34:419-425. doi:10.1111/jdv.15909
- Eonomopoulou A, Pavli A, Stasinopoulou P, et al. Migrant screening: lessons learned from the migrant holding level at the Greek-Turkish borders. J Infect Public Health. 2017;10:177-184. doi:10.1016/j.jiph.2016.04.012
- Marano N, Angelo KM, Merrill RD, et al. Expanding travel medicine in the 21st century to address the health needs of the world’s migrants.J Travel Med. 2018;25. doi:10.1093/jtm/tay067
- Hay RJ, Asiedu K. Skin-related neglected tropical diseases (skin NTDs)—a new challenge. Trop Med Infect Dis. 2018;4. doi:10.3390/tropicalmed4010004
- NIAID. Neglected tropical diseases. Updated July 11, 2016. Accessed April 4, 2024. https://www.niaid.nih.gov/research/neglected-tropical-diseases
- Arlian LG, Morgan MS. A review of Sarcoptes scabiei: past, present and future. Parasit Vectors. 2017;10:297. doi:10.1186/s13071-017-2234-1
- Arlian LG, Runyan RA, Achar S, et al. Survival and infectivity of Sarcoptes scabiei var. canis and var. hominis. J Am Acad Dermatol. 1984;11(2 pt 1):210-215. doi:10.1016/s0190-9622(84)70151-4
- Chandler DJ, Fuller LC. A review of scabies: an infestation more than skin deep. Dermatology. 2019;235:79-90. doi:10.1159/000495290
- Karimkhani C, Colombara DV, Drucker AM, et al. The global burden of scabies: a cross-sectional analysis from the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017;17:1247-1254. doi:10.1016/S1473-3099(17)30483-8
- Romani L, Steer AC, Whitfeld MJ, et al. Prevalence of scabies and impetigo worldwide: a systematic review. Lancet Infect Dis. 2015;15:960-967. doi:10.1016/S1473-3099(15)00132-2
- Thomas C, Coates SJ, Engelman D, et al. Ectoparasites: scabies. J Am Acad Dermatol. 2020;82:533-548. doi:10.1016/j.jaad.2019.05.109
- Mellanby K, Johnson CG, Bartley WC. Treatment of scabies. Br Med J. 1942;2:1-4. doi:10.1136/bmj.2.4252.1
- Walton SF. The immunology of susceptibility and resistance to scabies. Parasit Immunol. 2010;32:532-540. doi:10.1111/j.1365-3024.2010.01218.x
- Coates SJ, Thomas C, Chosidow O, et al. Ectoparasites: pediculosis and tungiasis. J Am Acad Dermatol. 2020;82:551-569. doi:10.1016/j.jaad.2019.05.110
- Engelman D, Fuller LC, Steer AC; International Alliance for the Control of Scabies Delphi p. Consensus criteria for the diagnosis of scabies: a Delphi study of international experts. PLoS Negl Trop Dis. 2018;12:E0006549. doi:10.1371/journal.pntd.0006549
- World Health Organization. WHO Model Lists of Essential Medicines—23rd list, 2023. Updated July 26, 2023. Accessed April 8, 2024. https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2023.02
- Salavastru CM, Chosidow O, Boffa MJ, et al. European guideline for the management of scabies. J Eur Acad Dermatol Venereol. 2017;31:1248-1253. doi:10.1111/jdv.14351
- Badiaga S, Brouqui P. Human louse-transmitted infectious diseases. Clin Microbiol Infect. 2012;18:332-337. doi:10.1111/j.1469-0691.2012.03778.x
- Leo NP, Campbell NJH, Yang X, et al. Evidence from mitochondrial DNA that head lice and body lice of humans (Phthiraptera: Pediculidae) are conspecific. J Med Entomol. 2002;39:662-666. doi:10.1603/0022-2585-39.4.662
- Chosidow O. Scabies and pediculosis. Lancet. 2000;355:819-826. doi:10.1016/S0140-6736(99)09458-1
- Arnaud A, Chosidow O, Détrez M-A, et al. Prevalences of scabies and pediculosis corporis among homeless people in the Paris region: results from two randomized cross-sectional surveys (HYTPEAC study). Br J Dermatol. 2016;174:104-112. doi:10.1111/bjd.14226
- Brouqui P. Arthropod-borne diseases associated with political and social disorder. Annu Rev Entomol. 2011;56:357-374. doi:10.1146/annurev-ento-120709-144739
- Ko CJ, Elston DM. Pediculosis. J Am Acad Dermatol. 2004;50:1-12. doi:10.1016/S0190-9622(03)02729-4
- Bloomfield D. Head lice. Pediatr Rev. 2002;23:34-35; discussion 34-35. doi:10.1542/pir.23-1-34
- Stone SP GJ, Bacelieri RE. Scabies, other mites, and pediculosis. In: Wolf K GL, Katz SI, et al (eds). Fitzpatrick’s Dermatology in General Medicine. McGraw Hill; 2008:2029.
- Foucault C, Ranque S, Badiaga S, et al. Oral ivermectin in the treatment of body lice. J Infect Dis. 2006;193:474-476. doi:10.1086/499279
- Benkouiten S, Drali R, Badiaga S, et al. Effect of permethrin-impregnated underwear on body lice in sheltered homeless persons: a randomized controlled trial. JAMA Dermatol. 2014;150:273-279. doi:10.1001/jamadermatol.2013.6398
- CDC. Parasites: Treatment. Updated October 15, 2019. Accessed April 4, 2024. https://www.cdc.gov/parasites/lice/head/treatment.html
- Devore CD, Schutze GE; Council on School Health and Committee on Infectious Diseases, American Academy of Pediatrics. Head lice. Pediatrics. 2015;135:e1355-e1365. doi:10.1542/peds.2015-0746
- Ohl ME, Spach DH. Bartonella quintana and urban trench fever. Clin Infect Dis. 2000;31:131-135. doi:10.1086/313890
- Drali R, Sangaré AK, Boutellis A, et al. Bartonella quintana in body lice from scalp hair of homeless persons, France. Emerg Infect Dis. 2014;20:907-908. doi:10.3201/eid2005.131242
- Rudd N, Zakaria A, Kohn MA, et al. Association of body lice infestation with hemoglobin values in hospitalized dermatology patients. JAMA Dermatol. 2022;158:691-693. doi:10.1001/jamadermatol.2022.0818
- Guss DA, Koenig M, Castillo EM. Severe iron deficiency anemia and lice infestation. J Emergency Med. 2011;41:362-365. doi:10.1016/j.jemermed.2010.05.030
- Neglected tropical diseases of the skin: WHO launches mobile application to facilitate diagnosis. News release. World Health Organization; July 16, 2020. Accessed April 4, 2024. https://www.who.int/news/item/16-07-2020-neglected-tropical-diseases-of-the-skin-who-launches-mobile-application-to-facilitate-diagnosis
- Padovese V, Fuller LC, Griffiths CEM, et al; Migrant Health Dermatology Working Group of the International Foundation for Dermatology. Migrant skin health: perspectives from the Migrant Health Summit, Malta, 2022. Br J Dermatology. 2023;188:553-554. doi:10.1093/bjd/ljad001
- Knapp AP, Rehmus W, Chang AY. Skin diseases in displaced populations: a review of contributing factors, challenges, and approaches to care. Int J Dermatol. 2020;59:1299-1311. doi:10.1111/ijd.15063
- Norman FF, Comeche B, Chamorro S, et al. Overcoming challenges in the diagnosis and treatment of parasitic infectious diseases in migrants. Expert Rev Anti-infective Therapy. 2020;18:127-143. doi:10.1080/14787210.2020.1713099
- Skin NTDs: prioritizing integrated approaches to reduce suffering, psychosocial impact and stigmatization. News release. World Health Organization; October 29, 2020. Accessed April 4, 2024. https://www.who.int/news/item/29-10-2020-skin-ntds-prioritizing-integrated-approaches-to-reduce-suffering-psychosocial-impact-and-stigmatization
- Monin K, Batalova J, Lai T. Refugees and Asylees in the United States. Migration Information Source. Published May 13, 2021. Accessed April 4, 2024. https://www.migrationpolicy.org/article/refugees-and-asylees-united-states-2021
- UNHCR. Figures at a Glance. UNHCR USA. Update June 14, 2023. Accessed April 4, 2024. https://www.unhcr.org/en-us/figures-at-a-glance.html
- UNHCR. Refugee resettlement facts. Published October 2023. Accessed April 8, 2024. https://www.unhcr.org/us/media/refugee-resettlement-facts
- US Department of State. Report to Congress on Proposed Refugee Admissions for Fiscal Year 2024. Published November 3, 2023. Accessed April 8, 2024. https://www.state.gov/report-to-congress-on-proposed-refugee-admissions-for-fiscal-year-2024/
- UNHCR. Compact for Migration: Definitions. United Nations. Accessed April 4, 2024. https://refugeesmigrants.un.org/definitions
- United Nations High Commissioner for Refugees (UNHCR). Convention and Protocol Relating to the Status of Refugees. Published December 2010. Accessed January 11, 2024. https://www.unhcr.org/us/media/convention-and-protocol-relating-status-refugees
- Kibar Öztürk M. Skin diseases in rural Nyala, Sudan (in a rural hospital, in 12 orphanages, and in two refugee camps). Int J Dermatol. 2019;58:1341-1349. doi:10.1111/ijd.14619
- Padovese V, Knapp A. Challenges of managing skin diseases in refugees and migrants. Dermatol Clin. 2021;39:101-115. doi:10.1016/j.det.2020.08.010
- Saikal SL, Ge L, Mir A, et al. Skin disease profile of Syrian refugees in Jordan: a field-mission assessment. J Eur Acad Dermatol Venereol. 2020;34:419-425. doi:10.1111/jdv.15909
- Eonomopoulou A, Pavli A, Stasinopoulou P, et al. Migrant screening: lessons learned from the migrant holding level at the Greek-Turkish borders. J Infect Public Health. 2017;10:177-184. doi:10.1016/j.jiph.2016.04.012
- Marano N, Angelo KM, Merrill RD, et al. Expanding travel medicine in the 21st century to address the health needs of the world’s migrants.J Travel Med. 2018;25. doi:10.1093/jtm/tay067
- Hay RJ, Asiedu K. Skin-related neglected tropical diseases (skin NTDs)—a new challenge. Trop Med Infect Dis. 2018;4. doi:10.3390/tropicalmed4010004
- NIAID. Neglected tropical diseases. Updated July 11, 2016. Accessed April 4, 2024. https://www.niaid.nih.gov/research/neglected-tropical-diseases
- Arlian LG, Morgan MS. A review of Sarcoptes scabiei: past, present and future. Parasit Vectors. 2017;10:297. doi:10.1186/s13071-017-2234-1
- Arlian LG, Runyan RA, Achar S, et al. Survival and infectivity of Sarcoptes scabiei var. canis and var. hominis. J Am Acad Dermatol. 1984;11(2 pt 1):210-215. doi:10.1016/s0190-9622(84)70151-4
- Chandler DJ, Fuller LC. A review of scabies: an infestation more than skin deep. Dermatology. 2019;235:79-90. doi:10.1159/000495290
- Karimkhani C, Colombara DV, Drucker AM, et al. The global burden of scabies: a cross-sectional analysis from the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017;17:1247-1254. doi:10.1016/S1473-3099(17)30483-8
- Romani L, Steer AC, Whitfeld MJ, et al. Prevalence of scabies and impetigo worldwide: a systematic review. Lancet Infect Dis. 2015;15:960-967. doi:10.1016/S1473-3099(15)00132-2
- Thomas C, Coates SJ, Engelman D, et al. Ectoparasites: scabies. J Am Acad Dermatol. 2020;82:533-548. doi:10.1016/j.jaad.2019.05.109
- Mellanby K, Johnson CG, Bartley WC. Treatment of scabies. Br Med J. 1942;2:1-4. doi:10.1136/bmj.2.4252.1
- Walton SF. The immunology of susceptibility and resistance to scabies. Parasit Immunol. 2010;32:532-540. doi:10.1111/j.1365-3024.2010.01218.x
- Coates SJ, Thomas C, Chosidow O, et al. Ectoparasites: pediculosis and tungiasis. J Am Acad Dermatol. 2020;82:551-569. doi:10.1016/j.jaad.2019.05.110
- Engelman D, Fuller LC, Steer AC; International Alliance for the Control of Scabies Delphi p. Consensus criteria for the diagnosis of scabies: a Delphi study of international experts. PLoS Negl Trop Dis. 2018;12:E0006549. doi:10.1371/journal.pntd.0006549
- World Health Organization. WHO Model Lists of Essential Medicines—23rd list, 2023. Updated July 26, 2023. Accessed April 8, 2024. https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2023.02
- Salavastru CM, Chosidow O, Boffa MJ, et al. European guideline for the management of scabies. J Eur Acad Dermatol Venereol. 2017;31:1248-1253. doi:10.1111/jdv.14351
- Badiaga S, Brouqui P. Human louse-transmitted infectious diseases. Clin Microbiol Infect. 2012;18:332-337. doi:10.1111/j.1469-0691.2012.03778.x
- Leo NP, Campbell NJH, Yang X, et al. Evidence from mitochondrial DNA that head lice and body lice of humans (Phthiraptera: Pediculidae) are conspecific. J Med Entomol. 2002;39:662-666. doi:10.1603/0022-2585-39.4.662
- Chosidow O. Scabies and pediculosis. Lancet. 2000;355:819-826. doi:10.1016/S0140-6736(99)09458-1
- Arnaud A, Chosidow O, Détrez M-A, et al. Prevalences of scabies and pediculosis corporis among homeless people in the Paris region: results from two randomized cross-sectional surveys (HYTPEAC study). Br J Dermatol. 2016;174:104-112. doi:10.1111/bjd.14226
- Brouqui P. Arthropod-borne diseases associated with political and social disorder. Annu Rev Entomol. 2011;56:357-374. doi:10.1146/annurev-ento-120709-144739
- Ko CJ, Elston DM. Pediculosis. J Am Acad Dermatol. 2004;50:1-12. doi:10.1016/S0190-9622(03)02729-4
- Bloomfield D. Head lice. Pediatr Rev. 2002;23:34-35; discussion 34-35. doi:10.1542/pir.23-1-34
- Stone SP GJ, Bacelieri RE. Scabies, other mites, and pediculosis. In: Wolf K GL, Katz SI, et al (eds). Fitzpatrick’s Dermatology in General Medicine. McGraw Hill; 2008:2029.
- Foucault C, Ranque S, Badiaga S, et al. Oral ivermectin in the treatment of body lice. J Infect Dis. 2006;193:474-476. doi:10.1086/499279
- Benkouiten S, Drali R, Badiaga S, et al. Effect of permethrin-impregnated underwear on body lice in sheltered homeless persons: a randomized controlled trial. JAMA Dermatol. 2014;150:273-279. doi:10.1001/jamadermatol.2013.6398
- CDC. Parasites: Treatment. Updated October 15, 2019. Accessed April 4, 2024. https://www.cdc.gov/parasites/lice/head/treatment.html
- Devore CD, Schutze GE; Council on School Health and Committee on Infectious Diseases, American Academy of Pediatrics. Head lice. Pediatrics. 2015;135:e1355-e1365. doi:10.1542/peds.2015-0746
- Ohl ME, Spach DH. Bartonella quintana and urban trench fever. Clin Infect Dis. 2000;31:131-135. doi:10.1086/313890
- Drali R, Sangaré AK, Boutellis A, et al. Bartonella quintana in body lice from scalp hair of homeless persons, France. Emerg Infect Dis. 2014;20:907-908. doi:10.3201/eid2005.131242
- Rudd N, Zakaria A, Kohn MA, et al. Association of body lice infestation with hemoglobin values in hospitalized dermatology patients. JAMA Dermatol. 2022;158:691-693. doi:10.1001/jamadermatol.2022.0818
- Guss DA, Koenig M, Castillo EM. Severe iron deficiency anemia and lice infestation. J Emergency Med. 2011;41:362-365. doi:10.1016/j.jemermed.2010.05.030
- Neglected tropical diseases of the skin: WHO launches mobile application to facilitate diagnosis. News release. World Health Organization; July 16, 2020. Accessed April 4, 2024. https://www.who.int/news/item/16-07-2020-neglected-tropical-diseases-of-the-skin-who-launches-mobile-application-to-facilitate-diagnosis
- Padovese V, Fuller LC, Griffiths CEM, et al; Migrant Health Dermatology Working Group of the International Foundation for Dermatology. Migrant skin health: perspectives from the Migrant Health Summit, Malta, 2022. Br J Dermatology. 2023;188:553-554. doi:10.1093/bjd/ljad001
- Knapp AP, Rehmus W, Chang AY. Skin diseases in displaced populations: a review of contributing factors, challenges, and approaches to care. Int J Dermatol. 2020;59:1299-1311. doi:10.1111/ijd.15063
- Norman FF, Comeche B, Chamorro S, et al. Overcoming challenges in the diagnosis and treatment of parasitic infectious diseases in migrants. Expert Rev Anti-infective Therapy. 2020;18:127-143. doi:10.1080/14787210.2020.1713099
- Skin NTDs: prioritizing integrated approaches to reduce suffering, psychosocial impact and stigmatization. News release. World Health Organization; October 29, 2020. Accessed April 4, 2024. https://www.who.int/news/item/29-10-2020-skin-ntds-prioritizing-integrated-approaches-to-reduce-suffering-psychosocial-impact-and-stigmatization
Practice Points
- War and natural disasters displace populations and disrupt infrastructure and access to medical care.
- Infestations and cutaneous infections are common among refugee populations, and impetigo often is a sign of underlying scabies infestation.
- Body lice are important disease vectors inrefugee populations.
Hepatitis Kills 3500 People Each Day, Says WHO
The number of deaths from viral hepatitis worldwide increased from 1.1 million in 2019 to 1.3 million in 2022. These figures equate to approximately 3500 deaths per day due to the disease, which is the second leading cause of mortality from infectious agents globally.
These data are part of the recently released Global Hepatitis Report 2024, which was published by the World Health Organization (WHO) during the World Hepatitis Summit in Lisbon, Portugal.
“This report paints a concerning picture: Despite global progress in preventing hepatitis infections, deaths are increasing because very few people with hepatitis are being diagnosed and treated,” said WHO Director-General Tedros Adhanom Ghebreyesus, PhD.
Hepatitis B significantly is associated with the highest mortality rate. It accounted for 83% of deaths from the disease in 2022. Meanwhile, hepatitis C was responsible for 17% of deaths. The mortality of other, less common types of hepatitis was not considered in the ranking.
The report also indicates that more than 6000 people worldwide are infected with viral hepatitis every day. The 2.2 million new cases in 2022 represent a slight decrease from 2.5 million in 2019, but the WHO considers the incidence high.
The organization’s updated statistics indicate that about 254 million people had hepatitis B in 2022, while 50 million had type C.
“Besides the deaths, the number of new cases every year is also striking. These are diseases that continue to spread. In the case of hepatitis C, the spread results from lack of access to disposable or properly sterilized sharp materials,” said Thor Dantas, MD, PhD, a physician and director of the Brazilian Society of Hepatology’s Viral Hepatitis Committee.
The situation of hepatitis B is particularly problematic, given that there is a safe and effective vaccine against it, said Dantas. “It’s remarkable that we continue to have so many new cases worldwide. This shows that we are failing in access to preventive measures for control and spread.”
Half of chronic hepatitis B and C cases occur in people between ages 30 and 54 years, while 12% affect children. There are more infections among men, who represent 58% of all cases.
The WHO also drew attention to the difficulty of accessing diagnosis and treatment. Only 13% of people with chronic hepatitis B infection were diagnosed, while only 3% — equivalent to 7 million people — received antiviral therapy by the end of 2022. This result is well below the WHO’s global target, which aims to treat 80% of cases by 2030.
Brazil has a higher diagnostic rate than the global average but is still below the target. According to the report, in 2022, the country diagnosed 34.2% of all hepatitis B infections. However, treatment coverage remains low: 3.6% of the total.
For hepatitis C, the scenario is somewhat different. During the same period, Brazil diagnosed 36% of total cases, with a treatment rate of 24%.
In 2022, Brazil had 2578 deaths from hepatitis B and 2977 from hepatitis C.
Because hepatitis is a silent disease, diagnosis often comes late, when the disease is already quite advanced, said Dr. Dantas. “Viral hepatitis evolves over the years essentially asymptomatically. Malaria shows symptoms, and tuberculosis shows symptoms. Viral hepatitis does not. They are only discovered through active searching.”
The WHO report shows significant regional differences in infection rates. Almost two thirds of cases are concentrated in the following 10 countries: China, India, Indonesia, Nigeria, Pakistan, Ethiopia, Bangladesh, Vietnam, the Philippines, and Russia.
In terms of hepatitis C incidence, Brazil ranks 15th globally, with 536,000 cases in 2022, representing 1.1% of the global total. The list is led by Pakistan, with 8.8 million cases, equivalent to 17.8% of the total. Next are India, with 5.5 million (11.2%), and China, with 4 million (8.1%).
In addition to regional differences, the report also reveals profound disparities in the prices paid for major treatments.
“Price disparities between, and even within, WHO regions persist, with many countries paying above global reference values, including for nonpatented medications,” according to the report.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.A version of this article appeared on Medscape.com.
The number of deaths from viral hepatitis worldwide increased from 1.1 million in 2019 to 1.3 million in 2022. These figures equate to approximately 3500 deaths per day due to the disease, which is the second leading cause of mortality from infectious agents globally.
These data are part of the recently released Global Hepatitis Report 2024, which was published by the World Health Organization (WHO) during the World Hepatitis Summit in Lisbon, Portugal.
“This report paints a concerning picture: Despite global progress in preventing hepatitis infections, deaths are increasing because very few people with hepatitis are being diagnosed and treated,” said WHO Director-General Tedros Adhanom Ghebreyesus, PhD.
Hepatitis B significantly is associated with the highest mortality rate. It accounted for 83% of deaths from the disease in 2022. Meanwhile, hepatitis C was responsible for 17% of deaths. The mortality of other, less common types of hepatitis was not considered in the ranking.
The report also indicates that more than 6000 people worldwide are infected with viral hepatitis every day. The 2.2 million new cases in 2022 represent a slight decrease from 2.5 million in 2019, but the WHO considers the incidence high.
The organization’s updated statistics indicate that about 254 million people had hepatitis B in 2022, while 50 million had type C.
“Besides the deaths, the number of new cases every year is also striking. These are diseases that continue to spread. In the case of hepatitis C, the spread results from lack of access to disposable or properly sterilized sharp materials,” said Thor Dantas, MD, PhD, a physician and director of the Brazilian Society of Hepatology’s Viral Hepatitis Committee.
The situation of hepatitis B is particularly problematic, given that there is a safe and effective vaccine against it, said Dantas. “It’s remarkable that we continue to have so many new cases worldwide. This shows that we are failing in access to preventive measures for control and spread.”
Half of chronic hepatitis B and C cases occur in people between ages 30 and 54 years, while 12% affect children. There are more infections among men, who represent 58% of all cases.
The WHO also drew attention to the difficulty of accessing diagnosis and treatment. Only 13% of people with chronic hepatitis B infection were diagnosed, while only 3% — equivalent to 7 million people — received antiviral therapy by the end of 2022. This result is well below the WHO’s global target, which aims to treat 80% of cases by 2030.
Brazil has a higher diagnostic rate than the global average but is still below the target. According to the report, in 2022, the country diagnosed 34.2% of all hepatitis B infections. However, treatment coverage remains low: 3.6% of the total.
For hepatitis C, the scenario is somewhat different. During the same period, Brazil diagnosed 36% of total cases, with a treatment rate of 24%.
In 2022, Brazil had 2578 deaths from hepatitis B and 2977 from hepatitis C.
Because hepatitis is a silent disease, diagnosis often comes late, when the disease is already quite advanced, said Dr. Dantas. “Viral hepatitis evolves over the years essentially asymptomatically. Malaria shows symptoms, and tuberculosis shows symptoms. Viral hepatitis does not. They are only discovered through active searching.”
The WHO report shows significant regional differences in infection rates. Almost two thirds of cases are concentrated in the following 10 countries: China, India, Indonesia, Nigeria, Pakistan, Ethiopia, Bangladesh, Vietnam, the Philippines, and Russia.
In terms of hepatitis C incidence, Brazil ranks 15th globally, with 536,000 cases in 2022, representing 1.1% of the global total. The list is led by Pakistan, with 8.8 million cases, equivalent to 17.8% of the total. Next are India, with 5.5 million (11.2%), and China, with 4 million (8.1%).
In addition to regional differences, the report also reveals profound disparities in the prices paid for major treatments.
“Price disparities between, and even within, WHO regions persist, with many countries paying above global reference values, including for nonpatented medications,” according to the report.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.A version of this article appeared on Medscape.com.
The number of deaths from viral hepatitis worldwide increased from 1.1 million in 2019 to 1.3 million in 2022. These figures equate to approximately 3500 deaths per day due to the disease, which is the second leading cause of mortality from infectious agents globally.
These data are part of the recently released Global Hepatitis Report 2024, which was published by the World Health Organization (WHO) during the World Hepatitis Summit in Lisbon, Portugal.
“This report paints a concerning picture: Despite global progress in preventing hepatitis infections, deaths are increasing because very few people with hepatitis are being diagnosed and treated,” said WHO Director-General Tedros Adhanom Ghebreyesus, PhD.
Hepatitis B significantly is associated with the highest mortality rate. It accounted for 83% of deaths from the disease in 2022. Meanwhile, hepatitis C was responsible for 17% of deaths. The mortality of other, less common types of hepatitis was not considered in the ranking.
The report also indicates that more than 6000 people worldwide are infected with viral hepatitis every day. The 2.2 million new cases in 2022 represent a slight decrease from 2.5 million in 2019, but the WHO considers the incidence high.
The organization’s updated statistics indicate that about 254 million people had hepatitis B in 2022, while 50 million had type C.
“Besides the deaths, the number of new cases every year is also striking. These are diseases that continue to spread. In the case of hepatitis C, the spread results from lack of access to disposable or properly sterilized sharp materials,” said Thor Dantas, MD, PhD, a physician and director of the Brazilian Society of Hepatology’s Viral Hepatitis Committee.
The situation of hepatitis B is particularly problematic, given that there is a safe and effective vaccine against it, said Dantas. “It’s remarkable that we continue to have so many new cases worldwide. This shows that we are failing in access to preventive measures for control and spread.”
Half of chronic hepatitis B and C cases occur in people between ages 30 and 54 years, while 12% affect children. There are more infections among men, who represent 58% of all cases.
The WHO also drew attention to the difficulty of accessing diagnosis and treatment. Only 13% of people with chronic hepatitis B infection were diagnosed, while only 3% — equivalent to 7 million people — received antiviral therapy by the end of 2022. This result is well below the WHO’s global target, which aims to treat 80% of cases by 2030.
Brazil has a higher diagnostic rate than the global average but is still below the target. According to the report, in 2022, the country diagnosed 34.2% of all hepatitis B infections. However, treatment coverage remains low: 3.6% of the total.
For hepatitis C, the scenario is somewhat different. During the same period, Brazil diagnosed 36% of total cases, with a treatment rate of 24%.
In 2022, Brazil had 2578 deaths from hepatitis B and 2977 from hepatitis C.
Because hepatitis is a silent disease, diagnosis often comes late, when the disease is already quite advanced, said Dr. Dantas. “Viral hepatitis evolves over the years essentially asymptomatically. Malaria shows symptoms, and tuberculosis shows symptoms. Viral hepatitis does not. They are only discovered through active searching.”
The WHO report shows significant regional differences in infection rates. Almost two thirds of cases are concentrated in the following 10 countries: China, India, Indonesia, Nigeria, Pakistan, Ethiopia, Bangladesh, Vietnam, the Philippines, and Russia.
In terms of hepatitis C incidence, Brazil ranks 15th globally, with 536,000 cases in 2022, representing 1.1% of the global total. The list is led by Pakistan, with 8.8 million cases, equivalent to 17.8% of the total. Next are India, with 5.5 million (11.2%), and China, with 4 million (8.1%).
In addition to regional differences, the report also reveals profound disparities in the prices paid for major treatments.
“Price disparities between, and even within, WHO regions persist, with many countries paying above global reference values, including for nonpatented medications,” according to the report.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.A version of this article appeared on Medscape.com.
Syphilis Treatment Falls Short for Pregnant Patients
Approximately one third of pregnant individuals with syphilis were inadequately treated or not treated for syphilis despite receiving timely prenatal care, based on data from nearly 1500 patients.
Although congenital syphilis is preventable with treatment before or early in pregnancy, data from the Centers for Disease Control and Prevention (CDC) show a doubling of syphilis rates in the United States between 2018 and 2021 wrote Ayzsa Tannis, MPH, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
To better understand factors contributing to inadequate syphilis treatment during pregnancy, the researchers examined data from 1476 individuals with syphilis during pregnancy. The study population came from six jurisdictions that participated in the Surveillance for Emerging Threats to Pregnant People and Infants Network, and sources included case investigations, medical records, and links between laboratory data and vital records.
The researchers characterized the status of syphilis during pregnancy as adequate, inadequate, or not treated based on the CDC’s Sexually Transmitted Infections Treatment Guidelines, 2021. Prenatal care was defined as timely (at least 30 days prior to pregnancy outcome), nontimely (less than 30 days before pregnancy outcome), and no prenatal care. The findings were published in Obstetrics & Gynecology.
Of the 1476 individuals studied, 855 (57.9%) were adequately treated for syphilis and 621 (42.1%) were inadequately or not treated.
Overall, 82% of the study population received timely prenatal care. However, 32.1% of those who received timely prenatal care were inadequately treated, including 14.8% who received no syphilis treatment. Individuals with nontimely or no prenatal care were significantly more likely to receive inadequate or no treatment for syphilis than those who received timely care (risk ratio, 2.50 and 2.73, respectively).
The findings were consistent with previous studies of missed opportunities for prevention and treatment, the researchers noted. Factors behind nontimely treatment (less than 30 days before pregnancy outcome) may include intermittent shortages of benzathine penicillin G, the standard treatment for syphilis, as well as the lack of time and administrative support for clinicians to communicate with patients and health departments, and to expedite treatment, the researchers wrote.
The results were limited by several factors including the use of data from six US jurisdictions that may not generalize to other areas, the variations in reporting years for the different jurisdictions, and variation in mandates for syphilis screening during pregnancy, the researchers noted.
More research is needed to improve syphilis testing itself, and to develop more treatment options, the researchers concluded. Partnerships among public health, patient advocacy groups, prenatal care clinicians, and other clinicians outside the prenatal care setting also are needed for effective intervention in pregnant individuals with syphilis, they said.
The study was carried out as part of the regular work of the CDC, supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement and through contractual mechanisms including the Local Health Department Initiative to Chickasaw Health Consulting. The researchers had no financial conflicts to disclose.
Approximately one third of pregnant individuals with syphilis were inadequately treated or not treated for syphilis despite receiving timely prenatal care, based on data from nearly 1500 patients.
Although congenital syphilis is preventable with treatment before or early in pregnancy, data from the Centers for Disease Control and Prevention (CDC) show a doubling of syphilis rates in the United States between 2018 and 2021 wrote Ayzsa Tannis, MPH, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
To better understand factors contributing to inadequate syphilis treatment during pregnancy, the researchers examined data from 1476 individuals with syphilis during pregnancy. The study population came from six jurisdictions that participated in the Surveillance for Emerging Threats to Pregnant People and Infants Network, and sources included case investigations, medical records, and links between laboratory data and vital records.
The researchers characterized the status of syphilis during pregnancy as adequate, inadequate, or not treated based on the CDC’s Sexually Transmitted Infections Treatment Guidelines, 2021. Prenatal care was defined as timely (at least 30 days prior to pregnancy outcome), nontimely (less than 30 days before pregnancy outcome), and no prenatal care. The findings were published in Obstetrics & Gynecology.
Of the 1476 individuals studied, 855 (57.9%) were adequately treated for syphilis and 621 (42.1%) were inadequately or not treated.
Overall, 82% of the study population received timely prenatal care. However, 32.1% of those who received timely prenatal care were inadequately treated, including 14.8% who received no syphilis treatment. Individuals with nontimely or no prenatal care were significantly more likely to receive inadequate or no treatment for syphilis than those who received timely care (risk ratio, 2.50 and 2.73, respectively).
The findings were consistent with previous studies of missed opportunities for prevention and treatment, the researchers noted. Factors behind nontimely treatment (less than 30 days before pregnancy outcome) may include intermittent shortages of benzathine penicillin G, the standard treatment for syphilis, as well as the lack of time and administrative support for clinicians to communicate with patients and health departments, and to expedite treatment, the researchers wrote.
The results were limited by several factors including the use of data from six US jurisdictions that may not generalize to other areas, the variations in reporting years for the different jurisdictions, and variation in mandates for syphilis screening during pregnancy, the researchers noted.
More research is needed to improve syphilis testing itself, and to develop more treatment options, the researchers concluded. Partnerships among public health, patient advocacy groups, prenatal care clinicians, and other clinicians outside the prenatal care setting also are needed for effective intervention in pregnant individuals with syphilis, they said.
The study was carried out as part of the regular work of the CDC, supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement and through contractual mechanisms including the Local Health Department Initiative to Chickasaw Health Consulting. The researchers had no financial conflicts to disclose.
Approximately one third of pregnant individuals with syphilis were inadequately treated or not treated for syphilis despite receiving timely prenatal care, based on data from nearly 1500 patients.
Although congenital syphilis is preventable with treatment before or early in pregnancy, data from the Centers for Disease Control and Prevention (CDC) show a doubling of syphilis rates in the United States between 2018 and 2021 wrote Ayzsa Tannis, MPH, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
To better understand factors contributing to inadequate syphilis treatment during pregnancy, the researchers examined data from 1476 individuals with syphilis during pregnancy. The study population came from six jurisdictions that participated in the Surveillance for Emerging Threats to Pregnant People and Infants Network, and sources included case investigations, medical records, and links between laboratory data and vital records.
The researchers characterized the status of syphilis during pregnancy as adequate, inadequate, or not treated based on the CDC’s Sexually Transmitted Infections Treatment Guidelines, 2021. Prenatal care was defined as timely (at least 30 days prior to pregnancy outcome), nontimely (less than 30 days before pregnancy outcome), and no prenatal care. The findings were published in Obstetrics & Gynecology.
Of the 1476 individuals studied, 855 (57.9%) were adequately treated for syphilis and 621 (42.1%) were inadequately or not treated.
Overall, 82% of the study population received timely prenatal care. However, 32.1% of those who received timely prenatal care were inadequately treated, including 14.8% who received no syphilis treatment. Individuals with nontimely or no prenatal care were significantly more likely to receive inadequate or no treatment for syphilis than those who received timely care (risk ratio, 2.50 and 2.73, respectively).
The findings were consistent with previous studies of missed opportunities for prevention and treatment, the researchers noted. Factors behind nontimely treatment (less than 30 days before pregnancy outcome) may include intermittent shortages of benzathine penicillin G, the standard treatment for syphilis, as well as the lack of time and administrative support for clinicians to communicate with patients and health departments, and to expedite treatment, the researchers wrote.
The results were limited by several factors including the use of data from six US jurisdictions that may not generalize to other areas, the variations in reporting years for the different jurisdictions, and variation in mandates for syphilis screening during pregnancy, the researchers noted.
More research is needed to improve syphilis testing itself, and to develop more treatment options, the researchers concluded. Partnerships among public health, patient advocacy groups, prenatal care clinicians, and other clinicians outside the prenatal care setting also are needed for effective intervention in pregnant individuals with syphilis, they said.
The study was carried out as part of the regular work of the CDC, supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement and through contractual mechanisms including the Local Health Department Initiative to Chickasaw Health Consulting. The researchers had no financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY
Menopause, RSV, and More: 4 New Meds to Know
BOSTON — The US Food and Drug Administration (FDA) approved 55 new medications in 2023 and 11 more in 2024 to date.
A New First-Line for GERD?
Vonoprazan, an oral potassium-competitive acid blocker — which received FDA approval in November 2023 — may be a good alternative for patients whose symptoms continue to linger despite taking medications designated to treat gastroesophageal reflux disease (GERD).
GERD is the most common gastrointestinal symptom encountered by primary care physicians. Proton-pump inhibitors (PPIs) are the first-line treatment for the condition but can have long-term side effects such as Clostridioides difficile infection and kidney lesions.
“We know that not all patients are going to have symptom relief with H2 blockers and PPIs, so there’s an opportunity for patients who don’t get full symptom relief,” Dr. Smetana told attendees.
Vonoprazan blocks potassium binding to ATPase proton pumps and inhibits the secretion of gastric acid.
The approval of vonoprazan for erosive GERD was based on results from the phase 3 PHALCON-EE study, a randomized, double-blind, multicenter study that found the drug to be more effective than lansoprazole in treating erosive esophagitis.
Vonoprazan “has more rapid absorption than PPIs [and a] longer half-life and is more potent than PPIs, so theoretically it could be more effective in certain settings,” Dr. Smetana said.
Vonoprazan is FDA approved for only 6 months of use. Despite its efficacy, cost may be a barrier to many patients. H2 blockers generally cost patients less than $10 for 1 month’s supply, whereas vonoprazan can cost up to $650.
Nonhormonal Drug for Menopause
Fezolinetant, the first neurokinin receptor antagonist to receive approval from the FDA to treat vasomotor symptoms, may be an option for women concerned about hormone-based therapy for menopausal hot flashes.
“[Fezolinetant] specifically works in the area of the brain that’s involved in body temperature regulation and sweating,” Dr. Smetana said.
Results from the SKYLIGHT 1 randomized controlled trial of fezolinetant found the medication reduced the frequency and severity of hot flashes. Some of the side effects include abdominal pain, diarrhea, and insomnia.
Other nonestrogen treatments, including selective serotonin reuptake inhibitors (SSRIs), gabapentin, cognitive-behavioral therapy, and hypnosis, are modestly effective, according to the North American Menopause Society.
“[Fezolinetant] offers a different option that physicians may be more comfortable prescribing,” Dr. Smetana said. “And I think this will be an important addition to nonhormonal therapy.”
RSV Vaccine for Everyone
Once considered an illness that is more prevalent in young children, respiratory syncytial virus (RSV) has become more prevalent and severe among older adults. Between 60,000 and 120,000 older adults are hospitalized and 6000-10,000 die of RSV infection each year, according to the US Centers for Disease Control and Prevention.
The FDA has approved two RSV vaccines approved for older adults, but clinicians may find it challenging to get older patients vaccinated for this and other preventable illnesses.
Patients who received the RSV vaccine had an 83% relative risk reduction for the illness, according to a recent study, and an overall lower risk for hospitalization.
Moderna is developing an mRNA vaccine for RSV that is similar to many COVID-19 vaccines. A study published in 2023 in The New England Journal of Medicine found no cases of neuroinflammatory disorders among patients who received the mRNA RSV vaccine, with a median follow-up of 112 days.
“This is important given ongoing concerns of neurological safety,” among older adults who receive the RSV vaccine, Dr. Smetana said.
As of March 2024, the CDC recommends shared decision-making for adults older than 60 years and for healthcare providers to “consider” rather than “recommend” the vaccine for their patients. The agency’s Adult RSV Work Group plans to meet at June 2024 to reconsider whether shared clinical decision-making remains the preferred policy option.
New Antidepressants
A medication thrice rejected by the FDA is now heading a new class of drugs to treat major depressive disorder.
Gepirone, a 5-HT1A receptor agonist, has a different mechanism of action from that of SSRIs, which are currently considered the first-line treatment for depression.
Gepirone was rejected by the FDA in 2002, 2004, and 2007, with concerns that the efficacy studies were too small. In 2015, an FDA advisory committee agreed that the evidence to date did not support approval of an extended-release form of the drug. But the agency decided to approve the medication in September 2023.
“So why is this medication worth discussing now?” Dr. Smetana said. “It’s because the side effect profile is different from existing antidepressants.”
Many patients may stop using SSRIs because of side effects such as insomnia and loss of libido, Dr. Smetana said. Gepirone has the potential to avoid activation of other 5-HT receptors that mediate side effects, he said.
Studies suggest that gepirone reduces both anxiety and depression scores on the Hamilton Depression Rating Scale in patients who have both conditions and decreases rates of depression relapse compared with placebo through at least 48 weeks. The drug also may be less likely than SSRIs to cause sexual dysfunction in men, Dr. Smetana said.
Gepirone will be available to prescribe to patients in fall 2024.
Dr. Smetana reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
BOSTON — The US Food and Drug Administration (FDA) approved 55 new medications in 2023 and 11 more in 2024 to date.
A New First-Line for GERD?
Vonoprazan, an oral potassium-competitive acid blocker — which received FDA approval in November 2023 — may be a good alternative for patients whose symptoms continue to linger despite taking medications designated to treat gastroesophageal reflux disease (GERD).
GERD is the most common gastrointestinal symptom encountered by primary care physicians. Proton-pump inhibitors (PPIs) are the first-line treatment for the condition but can have long-term side effects such as Clostridioides difficile infection and kidney lesions.
“We know that not all patients are going to have symptom relief with H2 blockers and PPIs, so there’s an opportunity for patients who don’t get full symptom relief,” Dr. Smetana told attendees.
Vonoprazan blocks potassium binding to ATPase proton pumps and inhibits the secretion of gastric acid.
The approval of vonoprazan for erosive GERD was based on results from the phase 3 PHALCON-EE study, a randomized, double-blind, multicenter study that found the drug to be more effective than lansoprazole in treating erosive esophagitis.
Vonoprazan “has more rapid absorption than PPIs [and a] longer half-life and is more potent than PPIs, so theoretically it could be more effective in certain settings,” Dr. Smetana said.
Vonoprazan is FDA approved for only 6 months of use. Despite its efficacy, cost may be a barrier to many patients. H2 blockers generally cost patients less than $10 for 1 month’s supply, whereas vonoprazan can cost up to $650.
Nonhormonal Drug for Menopause
Fezolinetant, the first neurokinin receptor antagonist to receive approval from the FDA to treat vasomotor symptoms, may be an option for women concerned about hormone-based therapy for menopausal hot flashes.
“[Fezolinetant] specifically works in the area of the brain that’s involved in body temperature regulation and sweating,” Dr. Smetana said.
Results from the SKYLIGHT 1 randomized controlled trial of fezolinetant found the medication reduced the frequency and severity of hot flashes. Some of the side effects include abdominal pain, diarrhea, and insomnia.
Other nonestrogen treatments, including selective serotonin reuptake inhibitors (SSRIs), gabapentin, cognitive-behavioral therapy, and hypnosis, are modestly effective, according to the North American Menopause Society.
“[Fezolinetant] offers a different option that physicians may be more comfortable prescribing,” Dr. Smetana said. “And I think this will be an important addition to nonhormonal therapy.”
RSV Vaccine for Everyone
Once considered an illness that is more prevalent in young children, respiratory syncytial virus (RSV) has become more prevalent and severe among older adults. Between 60,000 and 120,000 older adults are hospitalized and 6000-10,000 die of RSV infection each year, according to the US Centers for Disease Control and Prevention.
The FDA has approved two RSV vaccines approved for older adults, but clinicians may find it challenging to get older patients vaccinated for this and other preventable illnesses.
Patients who received the RSV vaccine had an 83% relative risk reduction for the illness, according to a recent study, and an overall lower risk for hospitalization.
Moderna is developing an mRNA vaccine for RSV that is similar to many COVID-19 vaccines. A study published in 2023 in The New England Journal of Medicine found no cases of neuroinflammatory disorders among patients who received the mRNA RSV vaccine, with a median follow-up of 112 days.
“This is important given ongoing concerns of neurological safety,” among older adults who receive the RSV vaccine, Dr. Smetana said.
As of March 2024, the CDC recommends shared decision-making for adults older than 60 years and for healthcare providers to “consider” rather than “recommend” the vaccine for their patients. The agency’s Adult RSV Work Group plans to meet at June 2024 to reconsider whether shared clinical decision-making remains the preferred policy option.
New Antidepressants
A medication thrice rejected by the FDA is now heading a new class of drugs to treat major depressive disorder.
Gepirone, a 5-HT1A receptor agonist, has a different mechanism of action from that of SSRIs, which are currently considered the first-line treatment for depression.
Gepirone was rejected by the FDA in 2002, 2004, and 2007, with concerns that the efficacy studies were too small. In 2015, an FDA advisory committee agreed that the evidence to date did not support approval of an extended-release form of the drug. But the agency decided to approve the medication in September 2023.
“So why is this medication worth discussing now?” Dr. Smetana said. “It’s because the side effect profile is different from existing antidepressants.”
Many patients may stop using SSRIs because of side effects such as insomnia and loss of libido, Dr. Smetana said. Gepirone has the potential to avoid activation of other 5-HT receptors that mediate side effects, he said.
Studies suggest that gepirone reduces both anxiety and depression scores on the Hamilton Depression Rating Scale in patients who have both conditions and decreases rates of depression relapse compared with placebo through at least 48 weeks. The drug also may be less likely than SSRIs to cause sexual dysfunction in men, Dr. Smetana said.
Gepirone will be available to prescribe to patients in fall 2024.
Dr. Smetana reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
BOSTON — The US Food and Drug Administration (FDA) approved 55 new medications in 2023 and 11 more in 2024 to date.
A New First-Line for GERD?
Vonoprazan, an oral potassium-competitive acid blocker — which received FDA approval in November 2023 — may be a good alternative for patients whose symptoms continue to linger despite taking medications designated to treat gastroesophageal reflux disease (GERD).
GERD is the most common gastrointestinal symptom encountered by primary care physicians. Proton-pump inhibitors (PPIs) are the first-line treatment for the condition but can have long-term side effects such as Clostridioides difficile infection and kidney lesions.
“We know that not all patients are going to have symptom relief with H2 blockers and PPIs, so there’s an opportunity for patients who don’t get full symptom relief,” Dr. Smetana told attendees.
Vonoprazan blocks potassium binding to ATPase proton pumps and inhibits the secretion of gastric acid.
The approval of vonoprazan for erosive GERD was based on results from the phase 3 PHALCON-EE study, a randomized, double-blind, multicenter study that found the drug to be more effective than lansoprazole in treating erosive esophagitis.
Vonoprazan “has more rapid absorption than PPIs [and a] longer half-life and is more potent than PPIs, so theoretically it could be more effective in certain settings,” Dr. Smetana said.
Vonoprazan is FDA approved for only 6 months of use. Despite its efficacy, cost may be a barrier to many patients. H2 blockers generally cost patients less than $10 for 1 month’s supply, whereas vonoprazan can cost up to $650.
Nonhormonal Drug for Menopause
Fezolinetant, the first neurokinin receptor antagonist to receive approval from the FDA to treat vasomotor symptoms, may be an option for women concerned about hormone-based therapy for menopausal hot flashes.
“[Fezolinetant] specifically works in the area of the brain that’s involved in body temperature regulation and sweating,” Dr. Smetana said.
Results from the SKYLIGHT 1 randomized controlled trial of fezolinetant found the medication reduced the frequency and severity of hot flashes. Some of the side effects include abdominal pain, diarrhea, and insomnia.
Other nonestrogen treatments, including selective serotonin reuptake inhibitors (SSRIs), gabapentin, cognitive-behavioral therapy, and hypnosis, are modestly effective, according to the North American Menopause Society.
“[Fezolinetant] offers a different option that physicians may be more comfortable prescribing,” Dr. Smetana said. “And I think this will be an important addition to nonhormonal therapy.”
RSV Vaccine for Everyone
Once considered an illness that is more prevalent in young children, respiratory syncytial virus (RSV) has become more prevalent and severe among older adults. Between 60,000 and 120,000 older adults are hospitalized and 6000-10,000 die of RSV infection each year, according to the US Centers for Disease Control and Prevention.
The FDA has approved two RSV vaccines approved for older adults, but clinicians may find it challenging to get older patients vaccinated for this and other preventable illnesses.
Patients who received the RSV vaccine had an 83% relative risk reduction for the illness, according to a recent study, and an overall lower risk for hospitalization.
Moderna is developing an mRNA vaccine for RSV that is similar to many COVID-19 vaccines. A study published in 2023 in The New England Journal of Medicine found no cases of neuroinflammatory disorders among patients who received the mRNA RSV vaccine, with a median follow-up of 112 days.
“This is important given ongoing concerns of neurological safety,” among older adults who receive the RSV vaccine, Dr. Smetana said.
As of March 2024, the CDC recommends shared decision-making for adults older than 60 years and for healthcare providers to “consider” rather than “recommend” the vaccine for their patients. The agency’s Adult RSV Work Group plans to meet at June 2024 to reconsider whether shared clinical decision-making remains the preferred policy option.
New Antidepressants
A medication thrice rejected by the FDA is now heading a new class of drugs to treat major depressive disorder.
Gepirone, a 5-HT1A receptor agonist, has a different mechanism of action from that of SSRIs, which are currently considered the first-line treatment for depression.
Gepirone was rejected by the FDA in 2002, 2004, and 2007, with concerns that the efficacy studies were too small. In 2015, an FDA advisory committee agreed that the evidence to date did not support approval of an extended-release form of the drug. But the agency decided to approve the medication in September 2023.
“So why is this medication worth discussing now?” Dr. Smetana said. “It’s because the side effect profile is different from existing antidepressants.”
Many patients may stop using SSRIs because of side effects such as insomnia and loss of libido, Dr. Smetana said. Gepirone has the potential to avoid activation of other 5-HT receptors that mediate side effects, he said.
Studies suggest that gepirone reduces both anxiety and depression scores on the Hamilton Depression Rating Scale in patients who have both conditions and decreases rates of depression relapse compared with placebo through at least 48 weeks. The drug also may be less likely than SSRIs to cause sexual dysfunction in men, Dr. Smetana said.
Gepirone will be available to prescribe to patients in fall 2024.
Dr. Smetana reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
Ocular Microbiome May Be Dry Eye Culprit
A mix of microbes may help explain why some people develop dry eye disease, new research showed.
This finding suggests that bacteria may cause dry eye and could someday point to new treatments for the condition and related disorders, which affect an estimated 27 million Americans, according to researchers.
Current treatments aim to preserve and enhance tears and tear production to ease the grittiness and itchiness that accompany dry eye disease.
To examine the role of the ocular microbiome in dry eye disease, scientists in Texas analyzed swab samples from 30 men and women, nine of whom had dry eye.
They found Streptococcus and Pedobacter species were the most common bacteria in healthy eyes.
In people with dry eye, however, more Acinetobacter species were detected.
“We think the metabolites produced by these bacteria are responsible for dry eye conditions,” study coauthor Pallavi Sharma said in a news release about the findings.
Sharma, a graduate student at Stephen F. Austin State University in Nacogdoches, Texas, presented this research last month at the annual meeting of the American Society for Biochemistry and Molecular Biology. The research team was led by Alexandra Van Kley, PhD, a professor of biology at the university.
“Once we understand the eye microbiota properly, it will improve disease diagnosis at an early stage,” Van Kley predicted in the news release. “This knowledge can also serve as a catalyst for developing innovative therapies aimed at preventing and treating ocular disease as well as those that affect the central microbiome site: The gut.”
Investigators in Australia have conducted similar experiments in patients with meibomian gland dysfunction, a condition marked by underproduction of key oils in the eye.
One group reported in August 2023 the finding of “detectable differences in the bacterial richness, diversity, and community structure of the conjunctiva and eyelid margin between individuals with meibomian gland dysfunction with and without lacrimal dysfunction, as well as to healthy controls.”
More research is needed to confirm and understand the findings, though, and “to determine if manipulating the microbiome could be a potential treatment for the condition,” they wrote.
A version of this article appeared on Medscape.com.
A mix of microbes may help explain why some people develop dry eye disease, new research showed.
This finding suggests that bacteria may cause dry eye and could someday point to new treatments for the condition and related disorders, which affect an estimated 27 million Americans, according to researchers.
Current treatments aim to preserve and enhance tears and tear production to ease the grittiness and itchiness that accompany dry eye disease.
To examine the role of the ocular microbiome in dry eye disease, scientists in Texas analyzed swab samples from 30 men and women, nine of whom had dry eye.
They found Streptococcus and Pedobacter species were the most common bacteria in healthy eyes.
In people with dry eye, however, more Acinetobacter species were detected.
“We think the metabolites produced by these bacteria are responsible for dry eye conditions,” study coauthor Pallavi Sharma said in a news release about the findings.
Sharma, a graduate student at Stephen F. Austin State University in Nacogdoches, Texas, presented this research last month at the annual meeting of the American Society for Biochemistry and Molecular Biology. The research team was led by Alexandra Van Kley, PhD, a professor of biology at the university.
“Once we understand the eye microbiota properly, it will improve disease diagnosis at an early stage,” Van Kley predicted in the news release. “This knowledge can also serve as a catalyst for developing innovative therapies aimed at preventing and treating ocular disease as well as those that affect the central microbiome site: The gut.”
Investigators in Australia have conducted similar experiments in patients with meibomian gland dysfunction, a condition marked by underproduction of key oils in the eye.
One group reported in August 2023 the finding of “detectable differences in the bacterial richness, diversity, and community structure of the conjunctiva and eyelid margin between individuals with meibomian gland dysfunction with and without lacrimal dysfunction, as well as to healthy controls.”
More research is needed to confirm and understand the findings, though, and “to determine if manipulating the microbiome could be a potential treatment for the condition,” they wrote.
A version of this article appeared on Medscape.com.
A mix of microbes may help explain why some people develop dry eye disease, new research showed.
This finding suggests that bacteria may cause dry eye and could someday point to new treatments for the condition and related disorders, which affect an estimated 27 million Americans, according to researchers.
Current treatments aim to preserve and enhance tears and tear production to ease the grittiness and itchiness that accompany dry eye disease.
To examine the role of the ocular microbiome in dry eye disease, scientists in Texas analyzed swab samples from 30 men and women, nine of whom had dry eye.
They found Streptococcus and Pedobacter species were the most common bacteria in healthy eyes.
In people with dry eye, however, more Acinetobacter species were detected.
“We think the metabolites produced by these bacteria are responsible for dry eye conditions,” study coauthor Pallavi Sharma said in a news release about the findings.
Sharma, a graduate student at Stephen F. Austin State University in Nacogdoches, Texas, presented this research last month at the annual meeting of the American Society for Biochemistry and Molecular Biology. The research team was led by Alexandra Van Kley, PhD, a professor of biology at the university.
“Once we understand the eye microbiota properly, it will improve disease diagnosis at an early stage,” Van Kley predicted in the news release. “This knowledge can also serve as a catalyst for developing innovative therapies aimed at preventing and treating ocular disease as well as those that affect the central microbiome site: The gut.”
Investigators in Australia have conducted similar experiments in patients with meibomian gland dysfunction, a condition marked by underproduction of key oils in the eye.
One group reported in August 2023 the finding of “detectable differences in the bacterial richness, diversity, and community structure of the conjunctiva and eyelid margin between individuals with meibomian gland dysfunction with and without lacrimal dysfunction, as well as to healthy controls.”
More research is needed to confirm and understand the findings, though, and “to determine if manipulating the microbiome could be a potential treatment for the condition,” they wrote.
A version of this article appeared on Medscape.com.
Vaccine ‘Will Not Curb’ Dengue Epidemic, Says PAHO
The current tetravalent dengue vaccine TAK-003, from the Japanese laboratory Takeda, is not likely to control the ongoing epidemic, according to the Pan American Health Organization (PAHO). The organization emphasized the need to better understand the vaccine’s effectiveness against different serotypes and its safety under real-world clinical conditions.
The Americas are experiencing a record increase in dengue cases. Three times as many cases have been identified during 2024 (3.5 million) than were reported for the same period in 2023.
“The vaccine we have available will not curb the dengue epidemic; it should be used complementarily with other actions. The most important actions are field operations, vector control, prevention, and education,” said Daniel Salas, MD, executive manager of the PAHO Comprehensive Immunization Program, during a press conference on March 28.
“The vaccines we currently have are not the best response to reduce transmission and prevent deaths,” added Jarbas Barbosa, MD, PhD, PAHO’s director. The fatality rate remains below 0.05%, but this figure could be hard to maintain if the situation becomes more uncontrolled.
The TAK-003 regimen consists of two doses with a 3-month interval between applications, so “it is not a tool to control transmission at this moment. Studies have shown that only 8 years of [population-level] vaccination would have a significant impact on dengue transmission,” said Dr. Barbosa.
A new vaccine developed in Brazil in partnership with the company MSD, Butantan-DV, is in phase 3 trials and has the advantage of being a single-dose application, which could facilitate its use in situations with accelerated transmission. “But this vaccine will likely only be available in 2025,” said Dr. Barbosa.
PAHO officials also highlighted the need to better characterize the vaccine’s effectiveness and safety in the real world. They observed, for example, that when TAK-003 was investigated, the circulation of dengue serotype 3 was almost nonexistent, so the efficacy data against that serotype “are very limited.”
“The producer, Takeda, has very limited production capacity. Brazil is the country that uses this vaccine the most, followed by Argentina. Given that these countries have a good epidemiological surveillance system and adverse effect registration, they can conduct studies on how the vaccine performs in real life, which will greatly increase our knowledge about it. For example, we will see its effectiveness against serotype 3,” said Dr. Barbosa.
The PAHO Technical Advisory Group (TAG) on vaccine-preventable diseases recommended that any country using these vaccines have surveillance systems in place because it is important to promptly report and investigate any adverse events, said Dr. Salas. The organization also suggested that vaccination should ideally be administered in a “more controlled environment,” a phase 4 study, “to complete the safety and efficacy profile, especially in those who have not had dengue before and for dengue 3 and 4,” said Dr. Salas in response to a question from this news organization.
“People cannot expect that just because they were vaccinated, they will not get dengue. The vaccine has limited reach,” he emphasized.
Other research strategies for vector control, such as the use of the Wolbachia bacteria and mosquito sterilization, are future strategies and “not tools to control this outbreak,” noted Sylvain Aldighieri, MD, director of the Department of Prevention, Control, and Elimination of Transmissible Diseases at PAHO.
In his opening remarks, Dr. Barbosa urged the intensification of efforts with tools that are already available. These approaches include eliminating mosquito breeding sites (“80% are in or near homes”) and protecting against mosquito bites, preparing health services for early diagnosis and timely clinical management, and educating the population about dengue symptoms so they seek medical attention immediately.
Although dengue is increasing throughout Latin America and the Caribbean, the most affected countries are Brazil (83%), Paraguay (5.3%), and Argentina (3.7%), which account for 92% of the cases and 87% of the deaths, PAHO reported.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com .
The current tetravalent dengue vaccine TAK-003, from the Japanese laboratory Takeda, is not likely to control the ongoing epidemic, according to the Pan American Health Organization (PAHO). The organization emphasized the need to better understand the vaccine’s effectiveness against different serotypes and its safety under real-world clinical conditions.
The Americas are experiencing a record increase in dengue cases. Three times as many cases have been identified during 2024 (3.5 million) than were reported for the same period in 2023.
“The vaccine we have available will not curb the dengue epidemic; it should be used complementarily with other actions. The most important actions are field operations, vector control, prevention, and education,” said Daniel Salas, MD, executive manager of the PAHO Comprehensive Immunization Program, during a press conference on March 28.
“The vaccines we currently have are not the best response to reduce transmission and prevent deaths,” added Jarbas Barbosa, MD, PhD, PAHO’s director. The fatality rate remains below 0.05%, but this figure could be hard to maintain if the situation becomes more uncontrolled.
The TAK-003 regimen consists of two doses with a 3-month interval between applications, so “it is not a tool to control transmission at this moment. Studies have shown that only 8 years of [population-level] vaccination would have a significant impact on dengue transmission,” said Dr. Barbosa.
A new vaccine developed in Brazil in partnership with the company MSD, Butantan-DV, is in phase 3 trials and has the advantage of being a single-dose application, which could facilitate its use in situations with accelerated transmission. “But this vaccine will likely only be available in 2025,” said Dr. Barbosa.
PAHO officials also highlighted the need to better characterize the vaccine’s effectiveness and safety in the real world. They observed, for example, that when TAK-003 was investigated, the circulation of dengue serotype 3 was almost nonexistent, so the efficacy data against that serotype “are very limited.”
“The producer, Takeda, has very limited production capacity. Brazil is the country that uses this vaccine the most, followed by Argentina. Given that these countries have a good epidemiological surveillance system and adverse effect registration, they can conduct studies on how the vaccine performs in real life, which will greatly increase our knowledge about it. For example, we will see its effectiveness against serotype 3,” said Dr. Barbosa.
The PAHO Technical Advisory Group (TAG) on vaccine-preventable diseases recommended that any country using these vaccines have surveillance systems in place because it is important to promptly report and investigate any adverse events, said Dr. Salas. The organization also suggested that vaccination should ideally be administered in a “more controlled environment,” a phase 4 study, “to complete the safety and efficacy profile, especially in those who have not had dengue before and for dengue 3 and 4,” said Dr. Salas in response to a question from this news organization.
“People cannot expect that just because they were vaccinated, they will not get dengue. The vaccine has limited reach,” he emphasized.
Other research strategies for vector control, such as the use of the Wolbachia bacteria and mosquito sterilization, are future strategies and “not tools to control this outbreak,” noted Sylvain Aldighieri, MD, director of the Department of Prevention, Control, and Elimination of Transmissible Diseases at PAHO.
In his opening remarks, Dr. Barbosa urged the intensification of efforts with tools that are already available. These approaches include eliminating mosquito breeding sites (“80% are in or near homes”) and protecting against mosquito bites, preparing health services for early diagnosis and timely clinical management, and educating the population about dengue symptoms so they seek medical attention immediately.
Although dengue is increasing throughout Latin America and the Caribbean, the most affected countries are Brazil (83%), Paraguay (5.3%), and Argentina (3.7%), which account for 92% of the cases and 87% of the deaths, PAHO reported.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com .
The current tetravalent dengue vaccine TAK-003, from the Japanese laboratory Takeda, is not likely to control the ongoing epidemic, according to the Pan American Health Organization (PAHO). The organization emphasized the need to better understand the vaccine’s effectiveness against different serotypes and its safety under real-world clinical conditions.
The Americas are experiencing a record increase in dengue cases. Three times as many cases have been identified during 2024 (3.5 million) than were reported for the same period in 2023.
“The vaccine we have available will not curb the dengue epidemic; it should be used complementarily with other actions. The most important actions are field operations, vector control, prevention, and education,” said Daniel Salas, MD, executive manager of the PAHO Comprehensive Immunization Program, during a press conference on March 28.
“The vaccines we currently have are not the best response to reduce transmission and prevent deaths,” added Jarbas Barbosa, MD, PhD, PAHO’s director. The fatality rate remains below 0.05%, but this figure could be hard to maintain if the situation becomes more uncontrolled.
The TAK-003 regimen consists of two doses with a 3-month interval between applications, so “it is not a tool to control transmission at this moment. Studies have shown that only 8 years of [population-level] vaccination would have a significant impact on dengue transmission,” said Dr. Barbosa.
A new vaccine developed in Brazil in partnership with the company MSD, Butantan-DV, is in phase 3 trials and has the advantage of being a single-dose application, which could facilitate its use in situations with accelerated transmission. “But this vaccine will likely only be available in 2025,” said Dr. Barbosa.
PAHO officials also highlighted the need to better characterize the vaccine’s effectiveness and safety in the real world. They observed, for example, that when TAK-003 was investigated, the circulation of dengue serotype 3 was almost nonexistent, so the efficacy data against that serotype “are very limited.”
“The producer, Takeda, has very limited production capacity. Brazil is the country that uses this vaccine the most, followed by Argentina. Given that these countries have a good epidemiological surveillance system and adverse effect registration, they can conduct studies on how the vaccine performs in real life, which will greatly increase our knowledge about it. For example, we will see its effectiveness against serotype 3,” said Dr. Barbosa.
The PAHO Technical Advisory Group (TAG) on vaccine-preventable diseases recommended that any country using these vaccines have surveillance systems in place because it is important to promptly report and investigate any adverse events, said Dr. Salas. The organization also suggested that vaccination should ideally be administered in a “more controlled environment,” a phase 4 study, “to complete the safety and efficacy profile, especially in those who have not had dengue before and for dengue 3 and 4,” said Dr. Salas in response to a question from this news organization.
“People cannot expect that just because they were vaccinated, they will not get dengue. The vaccine has limited reach,” he emphasized.
Other research strategies for vector control, such as the use of the Wolbachia bacteria and mosquito sterilization, are future strategies and “not tools to control this outbreak,” noted Sylvain Aldighieri, MD, director of the Department of Prevention, Control, and Elimination of Transmissible Diseases at PAHO.
In his opening remarks, Dr. Barbosa urged the intensification of efforts with tools that are already available. These approaches include eliminating mosquito breeding sites (“80% are in or near homes”) and protecting against mosquito bites, preparing health services for early diagnosis and timely clinical management, and educating the population about dengue symptoms so they seek medical attention immediately.
Although dengue is increasing throughout Latin America and the Caribbean, the most affected countries are Brazil (83%), Paraguay (5.3%), and Argentina (3.7%), which account for 92% of the cases and 87% of the deaths, PAHO reported.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com .
FDA Approves AI Diagnostic Tool for Early Sepsis Detection
The US Food and Drug Administration (FDA) has approved a medical device named the Sepsis ImmunoScore, which is an artificial intelligence/machine learning software, to guide rapid diagnosis and prediction of sepsis. The authorization was granted through the FDA’s De Novo pathway.
Sepsis is a complex condition, so diagnosing it early is difficult and has been a decades-long challenge for the US healthcare system.
Using both biomarkers and clinical data with the assistance of AI, the Sepsis ImmunoScore helps assess the risk for the presence of or progression to sepsis within 24 hours of patient evaluation in the emergency department or hospital. By considering 22 diverse parameters, the AI-powered tool provides a comprehensive evaluation of the patient’s biological condition, resulting in a risk score and categorization into four distinct risk levels.
It’s important to note that this system is not an alert mechanism. These risk categories are correlated with the risk for patient deterioration, including length of hospital stay, in-hospital mortality, and the need for escalated care within 24 hours (such as intensive care unit admission, mechanical ventilation, or vasopressor use). The diagnostic software is integrated directly into hospital electronic medical records.
This is the first AI diagnostic tool for sepsis to receive marketing authorization from the FDA.
A version of this article appeared on Medscape.com.
The US Food and Drug Administration (FDA) has approved a medical device named the Sepsis ImmunoScore, which is an artificial intelligence/machine learning software, to guide rapid diagnosis and prediction of sepsis. The authorization was granted through the FDA’s De Novo pathway.
Sepsis is a complex condition, so diagnosing it early is difficult and has been a decades-long challenge for the US healthcare system.
Using both biomarkers and clinical data with the assistance of AI, the Sepsis ImmunoScore helps assess the risk for the presence of or progression to sepsis within 24 hours of patient evaluation in the emergency department or hospital. By considering 22 diverse parameters, the AI-powered tool provides a comprehensive evaluation of the patient’s biological condition, resulting in a risk score and categorization into four distinct risk levels.
It’s important to note that this system is not an alert mechanism. These risk categories are correlated with the risk for patient deterioration, including length of hospital stay, in-hospital mortality, and the need for escalated care within 24 hours (such as intensive care unit admission, mechanical ventilation, or vasopressor use). The diagnostic software is integrated directly into hospital electronic medical records.
This is the first AI diagnostic tool for sepsis to receive marketing authorization from the FDA.
A version of this article appeared on Medscape.com.
The US Food and Drug Administration (FDA) has approved a medical device named the Sepsis ImmunoScore, which is an artificial intelligence/machine learning software, to guide rapid diagnosis and prediction of sepsis. The authorization was granted through the FDA’s De Novo pathway.
Sepsis is a complex condition, so diagnosing it early is difficult and has been a decades-long challenge for the US healthcare system.
Using both biomarkers and clinical data with the assistance of AI, the Sepsis ImmunoScore helps assess the risk for the presence of or progression to sepsis within 24 hours of patient evaluation in the emergency department or hospital. By considering 22 diverse parameters, the AI-powered tool provides a comprehensive evaluation of the patient’s biological condition, resulting in a risk score and categorization into four distinct risk levels.
It’s important to note that this system is not an alert mechanism. These risk categories are correlated with the risk for patient deterioration, including length of hospital stay, in-hospital mortality, and the need for escalated care within 24 hours (such as intensive care unit admission, mechanical ventilation, or vasopressor use). The diagnostic software is integrated directly into hospital electronic medical records.
This is the first AI diagnostic tool for sepsis to receive marketing authorization from the FDA.
A version of this article appeared on Medscape.com.