User login
Unleashing Our Immune Response to Quash Cancer
This article was originally published on February 10 in Eric Topol’s substack “Ground Truths.”
It’s astounding how devious cancer cells and tumor tissue can be. This week in Science we learned how certain lung cancer cells can function like “Catch Me If You Can” — changing their driver mutation and cell identity to escape targeted therapy. This histologic transformation, as seen in an experimental model, is just one of so many cancer tricks that we are learning about.
Recently, as shown by single-cell sequencing, cancer cells can steal the mitochondria from T cells, a double whammy that turbocharges cancer cells with the hijacked fuel supply and, at the same time, dismantles the immune response.
Last week, we saw how tumor cells can release a virus-like protein that unleashes a vicious autoimmune response.
And then there’s the finding that cancer cell spread predominantly is occurring while we sleep.
As I previously reviewed, the ability for cancer cells to hijack neurons and neural circuits is now well established, no less their ability to reprogram neurons to become adrenergic and stimulate tumor progression, and interfere with the immune response. Stay tuned on that for a new Ground Truths podcast with Prof Michelle Monje, a leader in cancer neuroscience, which will post soon.
Add advancing age’s immunosenescence as yet another challenge to the long and growing list of formidable ways that cancer cells, and the tumor microenvironment, evade our immune response.
An Ever-Expanding Armamentarium
Immune Checkpoint Inhibitors
The field of immunotherapies took off with the immune checkpoint inhibitors, first approved by the FDA in 2011, that take the brakes off of T cells, with the programmed death-1 (PD-1), PD-ligand1, and anti-CTLA-4 monoclonal antibodies.
But we’re clearly learning they are not enough to prevail over cancer with common recurrences, only short term success in most patients, with some notable exceptions. Adding other immune response strategies, such as a vaccine, or antibody-drug conjugates, or engineered T cells, are showing improved chances for success.
Therapeutic Cancer Vaccines
There are many therapeutic cancer vaccines in the works, as reviewed in depth here.
Here’s a list of ongoing clinical trials of cancer vaccines. You’ll note most of these are on top of a checkpoint inhibitor and use personalized neoantigens (cancer cell surface proteins) derived from sequencing (whole-exome or whole genome, RNA-sequencing and HLA-profiling) the patient’s tumor.
An example of positive findings is with the combination of an mRNA-nanoparticle vaccine with up to 34 personalized neoantigens and pembrolizumab (Keytruda) vs pembrolizumab alone in advanced melanoma after resection, with improved outcomes at 3-year follow-up, cutting death or relapse rate in half.
Antibody-Drug Conjugates (ADC)
There is considerable excitement about antibody-drug conjugates (ADC) whereby a linker is used to attach a chemotherapy agent to the checkpoint inhibitor antibody, specifically targeting the cancer cell and facilitating entry of the chemotherapy into the cell. Akin to these are bispecific antibodies (BiTEs, binding to a tumor antigen and T cell receptor simultaneously), both of these conjugates acting as “biologic” or “guided” missiles.
A very good example of the potency of an ADC was seen in a “HER2-low” breast cancer randomized trial. The absence or very low expression or amplification of the HER2 receptor is common in breast cancer and successful treatment has been elusive. A randomized trial of an ADC (trastuzumab deruxtecan) compared to physician’s choice therapy demonstrated a marked success for progression-free survival in HER2-low patients, which was characterized as “unheard-of success” by media coverage.
This strategy is being used to target some of the most difficult cancer driver mutations such as TP53 and KRAS.
Oncolytic Viruses
Modifying viruses to infect the tumor and make it more visible to the immune system, potentiating anti-tumor responses, known as oncolytic viruses, have been proposed as a way to rev up the immune response for a long time but without positive Phase 3 clinical trials.
After decades of failure, a recent trial in refractory bladder cancer showed marked success, along with others, summarized here, now providing very encouraging results. It looks like oncolytic viruses are on a comeback path.
Engineering T Cells (Chimeric Antigen Receptor [CAR-T])
As I recently reviewed, there are over 500 ongoing clinical trials to build on the success of the first CAR-T approval for leukemia 7 years ago. I won’t go through that all again here, but to reiterate most of the success to date has been in “liquid” blood (leukemia and lymphoma) cancer tumors. This week in Nature is the discovery of a T cell cancer mutation, a gene fusion CARD11-PIK3R3, from a T cell lymphoma that can potentially be used to augment CAR-T efficacy. It has pronounced and prolonged effects in the experimental model. Instead of 1 million cells needed for treatment, even 20,000 were enough to melt the tumor. This is a noteworthy discovery since CAR-T work to date has largely not exploited such naturally occurring mutations, while instead concentrating on those seen in the patient’s set of key tumor mutations.
As currently conceived, CAR-T, and what is being referred to more broadly as adoptive cell therapies, involves removing T cells from the patient’s body and engineering their activation, then reintroducing them back to the patient. This is laborious, technically difficult, and very expensive. Recently, the idea of achieving all of this via an injection of virus that specifically infects T cells and inserts the genes needed, was advanced by two biotech companies with preclinical results, one in non-human primates.
Gearing up to meet the challenge of solid tumor CAR-T intervention, there’s more work using CRISPR genome editing of T cell receptors. A.I. is increasingly being exploited to process the data from sequencing and identify optimal neoantigens.
Instead of just CAR-T, we’re seeing the emergence of CAR-macrophage and CAR-natural killer (NK) cells strategies, and rapidly expanding potential combinations of all the strategies I’ve mentioned. No less, there’s been maturation of on-off suicide switches programmed in, to limit cytokine release and promote safety of these interventions. Overall, major side effects of immunotherapies are not only cytokine release syndromes, but also include interstitial pneumonitis and neurotoxicity.
Summary
Given the multitude of ways cancer cells and tumor tissue can evade our immune response, durably successful treatment remains a daunting challenge. But the ingenuity of so many different approaches to unleash our immune response, and their combinations, provides considerable hope that we’ll increasingly meet the challenge in the years ahead. We have clearly learned that combining different immunotherapy strategies will be essential for many patients with the most resilient solid tumors.
Of concern, as noted by a recent editorial in The Lancet, entitled “Cancer Research Equity: Innovations For The Many, Not The Few,” is that these individualized, sophisticated strategies are not scalable; they will have limited reach and benefit. The movement towards “off the shelf” CAR-T and inexpensive, orally active checkpoint inhibitors may help mitigate this issue.
Notwithstanding this important concern, we’re seeing an array of diverse and potent immunotherapy strategies that are providing highly encouraging results, engendering more excitement than we’ve seen in this space for some time. These should propel substantial improvements in outcomes for patients in the years ahead. It can’t happen soon enough.
Thanks for reading this edition of Ground Truths. If you found it informative, please share it with your colleagues.
Dr. Topol has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for Dexcom; Illumina; Molecular Stethoscope; Quest Diagnostics; Blue Cross Blue Shield Association. Received research grant from National Institutes of Health.
A version of this article appeared on Medscape.com.
This article was originally published on February 10 in Eric Topol’s substack “Ground Truths.”
It’s astounding how devious cancer cells and tumor tissue can be. This week in Science we learned how certain lung cancer cells can function like “Catch Me If You Can” — changing their driver mutation and cell identity to escape targeted therapy. This histologic transformation, as seen in an experimental model, is just one of so many cancer tricks that we are learning about.
Recently, as shown by single-cell sequencing, cancer cells can steal the mitochondria from T cells, a double whammy that turbocharges cancer cells with the hijacked fuel supply and, at the same time, dismantles the immune response.
Last week, we saw how tumor cells can release a virus-like protein that unleashes a vicious autoimmune response.
And then there’s the finding that cancer cell spread predominantly is occurring while we sleep.
As I previously reviewed, the ability for cancer cells to hijack neurons and neural circuits is now well established, no less their ability to reprogram neurons to become adrenergic and stimulate tumor progression, and interfere with the immune response. Stay tuned on that for a new Ground Truths podcast with Prof Michelle Monje, a leader in cancer neuroscience, which will post soon.
Add advancing age’s immunosenescence as yet another challenge to the long and growing list of formidable ways that cancer cells, and the tumor microenvironment, evade our immune response.
An Ever-Expanding Armamentarium
Immune Checkpoint Inhibitors
The field of immunotherapies took off with the immune checkpoint inhibitors, first approved by the FDA in 2011, that take the brakes off of T cells, with the programmed death-1 (PD-1), PD-ligand1, and anti-CTLA-4 monoclonal antibodies.
But we’re clearly learning they are not enough to prevail over cancer with common recurrences, only short term success in most patients, with some notable exceptions. Adding other immune response strategies, such as a vaccine, or antibody-drug conjugates, or engineered T cells, are showing improved chances for success.
Therapeutic Cancer Vaccines
There are many therapeutic cancer vaccines in the works, as reviewed in depth here.
Here’s a list of ongoing clinical trials of cancer vaccines. You’ll note most of these are on top of a checkpoint inhibitor and use personalized neoantigens (cancer cell surface proteins) derived from sequencing (whole-exome or whole genome, RNA-sequencing and HLA-profiling) the patient’s tumor.
An example of positive findings is with the combination of an mRNA-nanoparticle vaccine with up to 34 personalized neoantigens and pembrolizumab (Keytruda) vs pembrolizumab alone in advanced melanoma after resection, with improved outcomes at 3-year follow-up, cutting death or relapse rate in half.
Antibody-Drug Conjugates (ADC)
There is considerable excitement about antibody-drug conjugates (ADC) whereby a linker is used to attach a chemotherapy agent to the checkpoint inhibitor antibody, specifically targeting the cancer cell and facilitating entry of the chemotherapy into the cell. Akin to these are bispecific antibodies (BiTEs, binding to a tumor antigen and T cell receptor simultaneously), both of these conjugates acting as “biologic” or “guided” missiles.
A very good example of the potency of an ADC was seen in a “HER2-low” breast cancer randomized trial. The absence or very low expression or amplification of the HER2 receptor is common in breast cancer and successful treatment has been elusive. A randomized trial of an ADC (trastuzumab deruxtecan) compared to physician’s choice therapy demonstrated a marked success for progression-free survival in HER2-low patients, which was characterized as “unheard-of success” by media coverage.
This strategy is being used to target some of the most difficult cancer driver mutations such as TP53 and KRAS.
Oncolytic Viruses
Modifying viruses to infect the tumor and make it more visible to the immune system, potentiating anti-tumor responses, known as oncolytic viruses, have been proposed as a way to rev up the immune response for a long time but without positive Phase 3 clinical trials.
After decades of failure, a recent trial in refractory bladder cancer showed marked success, along with others, summarized here, now providing very encouraging results. It looks like oncolytic viruses are on a comeback path.
Engineering T Cells (Chimeric Antigen Receptor [CAR-T])
As I recently reviewed, there are over 500 ongoing clinical trials to build on the success of the first CAR-T approval for leukemia 7 years ago. I won’t go through that all again here, but to reiterate most of the success to date has been in “liquid” blood (leukemia and lymphoma) cancer tumors. This week in Nature is the discovery of a T cell cancer mutation, a gene fusion CARD11-PIK3R3, from a T cell lymphoma that can potentially be used to augment CAR-T efficacy. It has pronounced and prolonged effects in the experimental model. Instead of 1 million cells needed for treatment, even 20,000 were enough to melt the tumor. This is a noteworthy discovery since CAR-T work to date has largely not exploited such naturally occurring mutations, while instead concentrating on those seen in the patient’s set of key tumor mutations.
As currently conceived, CAR-T, and what is being referred to more broadly as adoptive cell therapies, involves removing T cells from the patient’s body and engineering their activation, then reintroducing them back to the patient. This is laborious, technically difficult, and very expensive. Recently, the idea of achieving all of this via an injection of virus that specifically infects T cells and inserts the genes needed, was advanced by two biotech companies with preclinical results, one in non-human primates.
Gearing up to meet the challenge of solid tumor CAR-T intervention, there’s more work using CRISPR genome editing of T cell receptors. A.I. is increasingly being exploited to process the data from sequencing and identify optimal neoantigens.
Instead of just CAR-T, we’re seeing the emergence of CAR-macrophage and CAR-natural killer (NK) cells strategies, and rapidly expanding potential combinations of all the strategies I’ve mentioned. No less, there’s been maturation of on-off suicide switches programmed in, to limit cytokine release and promote safety of these interventions. Overall, major side effects of immunotherapies are not only cytokine release syndromes, but also include interstitial pneumonitis and neurotoxicity.
Summary
Given the multitude of ways cancer cells and tumor tissue can evade our immune response, durably successful treatment remains a daunting challenge. But the ingenuity of so many different approaches to unleash our immune response, and their combinations, provides considerable hope that we’ll increasingly meet the challenge in the years ahead. We have clearly learned that combining different immunotherapy strategies will be essential for many patients with the most resilient solid tumors.
Of concern, as noted by a recent editorial in The Lancet, entitled “Cancer Research Equity: Innovations For The Many, Not The Few,” is that these individualized, sophisticated strategies are not scalable; they will have limited reach and benefit. The movement towards “off the shelf” CAR-T and inexpensive, orally active checkpoint inhibitors may help mitigate this issue.
Notwithstanding this important concern, we’re seeing an array of diverse and potent immunotherapy strategies that are providing highly encouraging results, engendering more excitement than we’ve seen in this space for some time. These should propel substantial improvements in outcomes for patients in the years ahead. It can’t happen soon enough.
Thanks for reading this edition of Ground Truths. If you found it informative, please share it with your colleagues.
Dr. Topol has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for Dexcom; Illumina; Molecular Stethoscope; Quest Diagnostics; Blue Cross Blue Shield Association. Received research grant from National Institutes of Health.
A version of this article appeared on Medscape.com.
This article was originally published on February 10 in Eric Topol’s substack “Ground Truths.”
It’s astounding how devious cancer cells and tumor tissue can be. This week in Science we learned how certain lung cancer cells can function like “Catch Me If You Can” — changing their driver mutation and cell identity to escape targeted therapy. This histologic transformation, as seen in an experimental model, is just one of so many cancer tricks that we are learning about.
Recently, as shown by single-cell sequencing, cancer cells can steal the mitochondria from T cells, a double whammy that turbocharges cancer cells with the hijacked fuel supply and, at the same time, dismantles the immune response.
Last week, we saw how tumor cells can release a virus-like protein that unleashes a vicious autoimmune response.
And then there’s the finding that cancer cell spread predominantly is occurring while we sleep.
As I previously reviewed, the ability for cancer cells to hijack neurons and neural circuits is now well established, no less their ability to reprogram neurons to become adrenergic and stimulate tumor progression, and interfere with the immune response. Stay tuned on that for a new Ground Truths podcast with Prof Michelle Monje, a leader in cancer neuroscience, which will post soon.
Add advancing age’s immunosenescence as yet another challenge to the long and growing list of formidable ways that cancer cells, and the tumor microenvironment, evade our immune response.
An Ever-Expanding Armamentarium
Immune Checkpoint Inhibitors
The field of immunotherapies took off with the immune checkpoint inhibitors, first approved by the FDA in 2011, that take the brakes off of T cells, with the programmed death-1 (PD-1), PD-ligand1, and anti-CTLA-4 monoclonal antibodies.
But we’re clearly learning they are not enough to prevail over cancer with common recurrences, only short term success in most patients, with some notable exceptions. Adding other immune response strategies, such as a vaccine, or antibody-drug conjugates, or engineered T cells, are showing improved chances for success.
Therapeutic Cancer Vaccines
There are many therapeutic cancer vaccines in the works, as reviewed in depth here.
Here’s a list of ongoing clinical trials of cancer vaccines. You’ll note most of these are on top of a checkpoint inhibitor and use personalized neoantigens (cancer cell surface proteins) derived from sequencing (whole-exome or whole genome, RNA-sequencing and HLA-profiling) the patient’s tumor.
An example of positive findings is with the combination of an mRNA-nanoparticle vaccine with up to 34 personalized neoantigens and pembrolizumab (Keytruda) vs pembrolizumab alone in advanced melanoma after resection, with improved outcomes at 3-year follow-up, cutting death or relapse rate in half.
Antibody-Drug Conjugates (ADC)
There is considerable excitement about antibody-drug conjugates (ADC) whereby a linker is used to attach a chemotherapy agent to the checkpoint inhibitor antibody, specifically targeting the cancer cell and facilitating entry of the chemotherapy into the cell. Akin to these are bispecific antibodies (BiTEs, binding to a tumor antigen and T cell receptor simultaneously), both of these conjugates acting as “biologic” or “guided” missiles.
A very good example of the potency of an ADC was seen in a “HER2-low” breast cancer randomized trial. The absence or very low expression or amplification of the HER2 receptor is common in breast cancer and successful treatment has been elusive. A randomized trial of an ADC (trastuzumab deruxtecan) compared to physician’s choice therapy demonstrated a marked success for progression-free survival in HER2-low patients, which was characterized as “unheard-of success” by media coverage.
This strategy is being used to target some of the most difficult cancer driver mutations such as TP53 and KRAS.
Oncolytic Viruses
Modifying viruses to infect the tumor and make it more visible to the immune system, potentiating anti-tumor responses, known as oncolytic viruses, have been proposed as a way to rev up the immune response for a long time but without positive Phase 3 clinical trials.
After decades of failure, a recent trial in refractory bladder cancer showed marked success, along with others, summarized here, now providing very encouraging results. It looks like oncolytic viruses are on a comeback path.
Engineering T Cells (Chimeric Antigen Receptor [CAR-T])
As I recently reviewed, there are over 500 ongoing clinical trials to build on the success of the first CAR-T approval for leukemia 7 years ago. I won’t go through that all again here, but to reiterate most of the success to date has been in “liquid” blood (leukemia and lymphoma) cancer tumors. This week in Nature is the discovery of a T cell cancer mutation, a gene fusion CARD11-PIK3R3, from a T cell lymphoma that can potentially be used to augment CAR-T efficacy. It has pronounced and prolonged effects in the experimental model. Instead of 1 million cells needed for treatment, even 20,000 were enough to melt the tumor. This is a noteworthy discovery since CAR-T work to date has largely not exploited such naturally occurring mutations, while instead concentrating on those seen in the patient’s set of key tumor mutations.
As currently conceived, CAR-T, and what is being referred to more broadly as adoptive cell therapies, involves removing T cells from the patient’s body and engineering their activation, then reintroducing them back to the patient. This is laborious, technically difficult, and very expensive. Recently, the idea of achieving all of this via an injection of virus that specifically infects T cells and inserts the genes needed, was advanced by two biotech companies with preclinical results, one in non-human primates.
Gearing up to meet the challenge of solid tumor CAR-T intervention, there’s more work using CRISPR genome editing of T cell receptors. A.I. is increasingly being exploited to process the data from sequencing and identify optimal neoantigens.
Instead of just CAR-T, we’re seeing the emergence of CAR-macrophage and CAR-natural killer (NK) cells strategies, and rapidly expanding potential combinations of all the strategies I’ve mentioned. No less, there’s been maturation of on-off suicide switches programmed in, to limit cytokine release and promote safety of these interventions. Overall, major side effects of immunotherapies are not only cytokine release syndromes, but also include interstitial pneumonitis and neurotoxicity.
Summary
Given the multitude of ways cancer cells and tumor tissue can evade our immune response, durably successful treatment remains a daunting challenge. But the ingenuity of so many different approaches to unleash our immune response, and their combinations, provides considerable hope that we’ll increasingly meet the challenge in the years ahead. We have clearly learned that combining different immunotherapy strategies will be essential for many patients with the most resilient solid tumors.
Of concern, as noted by a recent editorial in The Lancet, entitled “Cancer Research Equity: Innovations For The Many, Not The Few,” is that these individualized, sophisticated strategies are not scalable; they will have limited reach and benefit. The movement towards “off the shelf” CAR-T and inexpensive, orally active checkpoint inhibitors may help mitigate this issue.
Notwithstanding this important concern, we’re seeing an array of diverse and potent immunotherapy strategies that are providing highly encouraging results, engendering more excitement than we’ve seen in this space for some time. These should propel substantial improvements in outcomes for patients in the years ahead. It can’t happen soon enough.
Thanks for reading this edition of Ground Truths. If you found it informative, please share it with your colleagues.
Dr. Topol has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for Dexcom; Illumina; Molecular Stethoscope; Quest Diagnostics; Blue Cross Blue Shield Association. Received research grant from National Institutes of Health.
A version of this article appeared on Medscape.com.
Chemotherapy-induced peripheral neuropathy tied to compromised executive function
PHOENIX – , a new finding that may increase the risk for compromised mobility and fall risk.
“Among older cancer survivors treated with chemotherapy, the presence of CIPN was independently associated with reduced executive function,” said study investigator Brendan L. McNeish, MD, of the department of physical medicine and rehabilitation, University of Pittsburgh.
“Importantly, given the emerging relationship of executive function with mobility in this population, stakeholders and clinicians are called to acknowledge that chemotherapy-related mobility declines in CIPN survivors are likely due to both neuromuscular and executive dysfunction,” he said.
The findings were presented at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
Research gap
Characterized by numbness, tingling, pain, and motor impairment, CIPN affects up to 50% of all patients with cancer that is treated with taxane-, platinum-, or vinca alkaloid–based chemotherapy. The condition is among the leading dose-limiting toxicities, potentially increasing mortality risk.
Though the effects of chemotherapy on cognitive function are well-established, less is known about a potential relationship between this side effect and CIPN, Dr. McNeish said.
“Chemotherapy can be neurotoxic, but few studies have linked neurotoxicity to the central nervous system and peripheral nervous system,” Dr. McNeish said.
To compare cognitive outcomes in patients treated with chemotherapy who did and did not develop CIPN, the investigators conducted a cross-sectional study that included 50 chemotherapy-treated cancer survivors at a single time point post chemotherapy. The mean age of participants was 65.6 years, and 90% were women.
Twenty-two (44%) patients had CIPN on the basis of patient-reported distal paresthesias or numbness that started when chemotherapy was initiated and was present at the time of study enrollment.
Patients with CIPN had a greater decline in executive function, compared with those without the condition, as measured by the Trail Making Test Part B (TMT-B; CIPN-positive, 84.9 sec vs. 59.1 sec, respectively; P = .01) and the Stroop Color and Word Test (SCWT; CIPN-positive, 178.1 sec vs. CIPN-negative, 152.7 sec; P = .04), as well as lower rapid reaction accuracy (CIPN-positive, 60.3% vs. CIPN-negative, 70.6%; P = .01).
The association between CIPN and decreased executive function remained after multivariate adjusting for age, gender, depression, and benzodiazepine use for TMT-B (beta, 18.7; P = .046) and rapid reaction accuracy (beta, -.088; P = .018) but not SCWT (beta, 9.52; P = .233).
Clinical guidance
A recent study by the same investigators showed a link between executive function and balance in cancer survivors (mean age, 65.6 years; 88% women) treated with chemotherapy.
Another study of 116 patients treated with chemotherapy, including 32 who developed CIPN, showed that those with CIPN were nearly three times more likely to report a fall or near fall than were those without CIPN symptoms. In addition, those with CIPN symptoms were also more likely to have received medical care for falls.
Based on the current findings, the research suggests that “current clinical approaches to caring for this growing population [of cancer patients] should not assume that the well-known increased fall risk is solely related to CIPN.”
Dr. McNeish speculated that two potential hypotheses could explain the association between CIPN and reduced executive function in older cancer survivors.
“First, CIPN is associated with other conditions such as depression and anxiety, which are associated with reduced executive function,” he said.
“The second is that cancer-related cognitive dysfunction and CIPN share pathogenic mechanisms of neuronal injury, inflammation, and advanced aging, and thus some patients are vulnerable to both central (cancer-related cognitive function) and peripheral neurotoxicity.”
Either way, Dr. McNeish noted that “all interventions should measure both CIPN and executive function, as one could confound the other.”
Need for increased awareness
Commenting on the study, Ting Bao, MD, co-director of the Leonard P. Zakim Center for Integrative Therapies & Healthy Living at the Dana-Farber Cancer Institute, Boston, said that the findings underscore that “there is a need for increased awareness of the diverse manifestations of chemotherapy-induced neuropathy.”
These include the fact that “neurotoxic chemotherapy impacts both the peripheral and central nervous systems, affecting balance through distinct mechanisms.”
Although treatments routinely recommended for CIPN include duloxetine, tricyclic antidepressants, or gabapentin as well as topical agents such as lidocaine, evidence also shows benefits of nonpharmacologic approaches including exercise, acupuncture, and yoga. Dr. Bao’s own research has suggested that those benefits can extend improved balance and reduced fall risk.
Dr. Bao and colleagues recently conducted a randomized study that included 41 patients with CIPN to receive either yoga or usual care.
“The findings revealed that after eight biweekly sessions of yoga, there was a notable improvement in the far-reach test, which is a predictor of fall risk,” she said.
To validate these findings, the researchers are currently conducting a larger randomized controlled trial, she said.
In the meantime, “further research into the mechanisms and effective treatments for chemotherapy-induced neurotoxicity is essential,” added Dr. Bao.
Dr. McNeish and Dr. Bao report no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHOENIX – , a new finding that may increase the risk for compromised mobility and fall risk.
“Among older cancer survivors treated with chemotherapy, the presence of CIPN was independently associated with reduced executive function,” said study investigator Brendan L. McNeish, MD, of the department of physical medicine and rehabilitation, University of Pittsburgh.
“Importantly, given the emerging relationship of executive function with mobility in this population, stakeholders and clinicians are called to acknowledge that chemotherapy-related mobility declines in CIPN survivors are likely due to both neuromuscular and executive dysfunction,” he said.
The findings were presented at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
Research gap
Characterized by numbness, tingling, pain, and motor impairment, CIPN affects up to 50% of all patients with cancer that is treated with taxane-, platinum-, or vinca alkaloid–based chemotherapy. The condition is among the leading dose-limiting toxicities, potentially increasing mortality risk.
Though the effects of chemotherapy on cognitive function are well-established, less is known about a potential relationship between this side effect and CIPN, Dr. McNeish said.
“Chemotherapy can be neurotoxic, but few studies have linked neurotoxicity to the central nervous system and peripheral nervous system,” Dr. McNeish said.
To compare cognitive outcomes in patients treated with chemotherapy who did and did not develop CIPN, the investigators conducted a cross-sectional study that included 50 chemotherapy-treated cancer survivors at a single time point post chemotherapy. The mean age of participants was 65.6 years, and 90% were women.
Twenty-two (44%) patients had CIPN on the basis of patient-reported distal paresthesias or numbness that started when chemotherapy was initiated and was present at the time of study enrollment.
Patients with CIPN had a greater decline in executive function, compared with those without the condition, as measured by the Trail Making Test Part B (TMT-B; CIPN-positive, 84.9 sec vs. 59.1 sec, respectively; P = .01) and the Stroop Color and Word Test (SCWT; CIPN-positive, 178.1 sec vs. CIPN-negative, 152.7 sec; P = .04), as well as lower rapid reaction accuracy (CIPN-positive, 60.3% vs. CIPN-negative, 70.6%; P = .01).
The association between CIPN and decreased executive function remained after multivariate adjusting for age, gender, depression, and benzodiazepine use for TMT-B (beta, 18.7; P = .046) and rapid reaction accuracy (beta, -.088; P = .018) but not SCWT (beta, 9.52; P = .233).
Clinical guidance
A recent study by the same investigators showed a link between executive function and balance in cancer survivors (mean age, 65.6 years; 88% women) treated with chemotherapy.
Another study of 116 patients treated with chemotherapy, including 32 who developed CIPN, showed that those with CIPN were nearly three times more likely to report a fall or near fall than were those without CIPN symptoms. In addition, those with CIPN symptoms were also more likely to have received medical care for falls.
Based on the current findings, the research suggests that “current clinical approaches to caring for this growing population [of cancer patients] should not assume that the well-known increased fall risk is solely related to CIPN.”
Dr. McNeish speculated that two potential hypotheses could explain the association between CIPN and reduced executive function in older cancer survivors.
“First, CIPN is associated with other conditions such as depression and anxiety, which are associated with reduced executive function,” he said.
“The second is that cancer-related cognitive dysfunction and CIPN share pathogenic mechanisms of neuronal injury, inflammation, and advanced aging, and thus some patients are vulnerable to both central (cancer-related cognitive function) and peripheral neurotoxicity.”
Either way, Dr. McNeish noted that “all interventions should measure both CIPN and executive function, as one could confound the other.”
Need for increased awareness
Commenting on the study, Ting Bao, MD, co-director of the Leonard P. Zakim Center for Integrative Therapies & Healthy Living at the Dana-Farber Cancer Institute, Boston, said that the findings underscore that “there is a need for increased awareness of the diverse manifestations of chemotherapy-induced neuropathy.”
These include the fact that “neurotoxic chemotherapy impacts both the peripheral and central nervous systems, affecting balance through distinct mechanisms.”
Although treatments routinely recommended for CIPN include duloxetine, tricyclic antidepressants, or gabapentin as well as topical agents such as lidocaine, evidence also shows benefits of nonpharmacologic approaches including exercise, acupuncture, and yoga. Dr. Bao’s own research has suggested that those benefits can extend improved balance and reduced fall risk.
Dr. Bao and colleagues recently conducted a randomized study that included 41 patients with CIPN to receive either yoga or usual care.
“The findings revealed that after eight biweekly sessions of yoga, there was a notable improvement in the far-reach test, which is a predictor of fall risk,” she said.
To validate these findings, the researchers are currently conducting a larger randomized controlled trial, she said.
In the meantime, “further research into the mechanisms and effective treatments for chemotherapy-induced neurotoxicity is essential,” added Dr. Bao.
Dr. McNeish and Dr. Bao report no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHOENIX – , a new finding that may increase the risk for compromised mobility and fall risk.
“Among older cancer survivors treated with chemotherapy, the presence of CIPN was independently associated with reduced executive function,” said study investigator Brendan L. McNeish, MD, of the department of physical medicine and rehabilitation, University of Pittsburgh.
“Importantly, given the emerging relationship of executive function with mobility in this population, stakeholders and clinicians are called to acknowledge that chemotherapy-related mobility declines in CIPN survivors are likely due to both neuromuscular and executive dysfunction,” he said.
The findings were presented at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
Research gap
Characterized by numbness, tingling, pain, and motor impairment, CIPN affects up to 50% of all patients with cancer that is treated with taxane-, platinum-, or vinca alkaloid–based chemotherapy. The condition is among the leading dose-limiting toxicities, potentially increasing mortality risk.
Though the effects of chemotherapy on cognitive function are well-established, less is known about a potential relationship between this side effect and CIPN, Dr. McNeish said.
“Chemotherapy can be neurotoxic, but few studies have linked neurotoxicity to the central nervous system and peripheral nervous system,” Dr. McNeish said.
To compare cognitive outcomes in patients treated with chemotherapy who did and did not develop CIPN, the investigators conducted a cross-sectional study that included 50 chemotherapy-treated cancer survivors at a single time point post chemotherapy. The mean age of participants was 65.6 years, and 90% were women.
Twenty-two (44%) patients had CIPN on the basis of patient-reported distal paresthesias or numbness that started when chemotherapy was initiated and was present at the time of study enrollment.
Patients with CIPN had a greater decline in executive function, compared with those without the condition, as measured by the Trail Making Test Part B (TMT-B; CIPN-positive, 84.9 sec vs. 59.1 sec, respectively; P = .01) and the Stroop Color and Word Test (SCWT; CIPN-positive, 178.1 sec vs. CIPN-negative, 152.7 sec; P = .04), as well as lower rapid reaction accuracy (CIPN-positive, 60.3% vs. CIPN-negative, 70.6%; P = .01).
The association between CIPN and decreased executive function remained after multivariate adjusting for age, gender, depression, and benzodiazepine use for TMT-B (beta, 18.7; P = .046) and rapid reaction accuracy (beta, -.088; P = .018) but not SCWT (beta, 9.52; P = .233).
Clinical guidance
A recent study by the same investigators showed a link between executive function and balance in cancer survivors (mean age, 65.6 years; 88% women) treated with chemotherapy.
Another study of 116 patients treated with chemotherapy, including 32 who developed CIPN, showed that those with CIPN were nearly three times more likely to report a fall or near fall than were those without CIPN symptoms. In addition, those with CIPN symptoms were also more likely to have received medical care for falls.
Based on the current findings, the research suggests that “current clinical approaches to caring for this growing population [of cancer patients] should not assume that the well-known increased fall risk is solely related to CIPN.”
Dr. McNeish speculated that two potential hypotheses could explain the association between CIPN and reduced executive function in older cancer survivors.
“First, CIPN is associated with other conditions such as depression and anxiety, which are associated with reduced executive function,” he said.
“The second is that cancer-related cognitive dysfunction and CIPN share pathogenic mechanisms of neuronal injury, inflammation, and advanced aging, and thus some patients are vulnerable to both central (cancer-related cognitive function) and peripheral neurotoxicity.”
Either way, Dr. McNeish noted that “all interventions should measure both CIPN and executive function, as one could confound the other.”
Need for increased awareness
Commenting on the study, Ting Bao, MD, co-director of the Leonard P. Zakim Center for Integrative Therapies & Healthy Living at the Dana-Farber Cancer Institute, Boston, said that the findings underscore that “there is a need for increased awareness of the diverse manifestations of chemotherapy-induced neuropathy.”
These include the fact that “neurotoxic chemotherapy impacts both the peripheral and central nervous systems, affecting balance through distinct mechanisms.”
Although treatments routinely recommended for CIPN include duloxetine, tricyclic antidepressants, or gabapentin as well as topical agents such as lidocaine, evidence also shows benefits of nonpharmacologic approaches including exercise, acupuncture, and yoga. Dr. Bao’s own research has suggested that those benefits can extend improved balance and reduced fall risk.
Dr. Bao and colleagues recently conducted a randomized study that included 41 patients with CIPN to receive either yoga or usual care.
“The findings revealed that after eight biweekly sessions of yoga, there was a notable improvement in the far-reach test, which is a predictor of fall risk,” she said.
To validate these findings, the researchers are currently conducting a larger randomized controlled trial, she said.
In the meantime, “further research into the mechanisms and effective treatments for chemotherapy-induced neurotoxicity is essential,” added Dr. Bao.
Dr. McNeish and Dr. Bao report no relevant disclosures.
A version of this article first appeared on Medscape.com.
AT AANEM 2023
Can thermal biofeedback reduce pain and anxiety?
TOPLINE:
A novel handheld tool may hold promise for reducing anxiety and pain and improving sleep quality, according to research presented at Lifestyle Medicine 2023, the annual meeting of the American College of Lifestyle Medicine.
METHODOLOGY:
- Franklin Somchith Ly, a PhD candidate in mechanical engineering at the University of California, Santa Barbara, developed , a product that assesses blood flow to the hand with an infrared temperature sensor and changes color as blood vessels expand during relaxation.
- Exercises such as intentional breathwork, visualization, and muscle relaxation change the color displayed by the device.
- Mr. Ly examined how measures of anxiety, sleep quality, and chronic pain changed after participants used the instrument. Ten participants completed a study assessing anxiety. Eight participants were enrolled in a sleep study where they completed biofeedback sessions before bed for 2 weeks, and 15 participants performed biofeedback twice daily and reported their levels of anxiety and pain.
TAKEAWAY:
- Anxiety scores decreased by about 22% on average (P < .001).
- Seven of the eight participants in the sleep study had improved scores on the Pittsburgh Sleep Quality Index, with an average improvement of nearly 30% (P < .05). Daytime dysfunction improved by 58% (P < .01).
- In the chronic pain study, about 60% of the 350 biofeedback sessions led to reduced pain.
IN PRACTICE:
“These portable devices may aid lifestyle management by alleviating anxiety, chronic pain, and enhancing daytime energy,” Mr. Ly said. “The results support their integration into lifestyle medicine and integrative medicine.”
SOURCE:
Mr. Ly presented the findings as a poster at Lifestyle Medicine 2023, which took place Oct. 29 to Nov. 1 in Denver and online.
LIMITATIONS:
The studies were open label and did not include control groups.
DISCLOSURES:
Mr. Ly is the founder of CalmStone, which markets a thermal biofeedback device. The research was supported by the Bill and Melinda Gates Foundation and the U.S. Army Research Office and Institute for Collaborative Biotechnologies.
A version of this article first appeared on Medscape.com.
TOPLINE:
A novel handheld tool may hold promise for reducing anxiety and pain and improving sleep quality, according to research presented at Lifestyle Medicine 2023, the annual meeting of the American College of Lifestyle Medicine.
METHODOLOGY:
- Franklin Somchith Ly, a PhD candidate in mechanical engineering at the University of California, Santa Barbara, developed , a product that assesses blood flow to the hand with an infrared temperature sensor and changes color as blood vessels expand during relaxation.
- Exercises such as intentional breathwork, visualization, and muscle relaxation change the color displayed by the device.
- Mr. Ly examined how measures of anxiety, sleep quality, and chronic pain changed after participants used the instrument. Ten participants completed a study assessing anxiety. Eight participants were enrolled in a sleep study where they completed biofeedback sessions before bed for 2 weeks, and 15 participants performed biofeedback twice daily and reported their levels of anxiety and pain.
TAKEAWAY:
- Anxiety scores decreased by about 22% on average (P < .001).
- Seven of the eight participants in the sleep study had improved scores on the Pittsburgh Sleep Quality Index, with an average improvement of nearly 30% (P < .05). Daytime dysfunction improved by 58% (P < .01).
- In the chronic pain study, about 60% of the 350 biofeedback sessions led to reduced pain.
IN PRACTICE:
“These portable devices may aid lifestyle management by alleviating anxiety, chronic pain, and enhancing daytime energy,” Mr. Ly said. “The results support their integration into lifestyle medicine and integrative medicine.”
SOURCE:
Mr. Ly presented the findings as a poster at Lifestyle Medicine 2023, which took place Oct. 29 to Nov. 1 in Denver and online.
LIMITATIONS:
The studies were open label and did not include control groups.
DISCLOSURES:
Mr. Ly is the founder of CalmStone, which markets a thermal biofeedback device. The research was supported by the Bill and Melinda Gates Foundation and the U.S. Army Research Office and Institute for Collaborative Biotechnologies.
A version of this article first appeared on Medscape.com.
TOPLINE:
A novel handheld tool may hold promise for reducing anxiety and pain and improving sleep quality, according to research presented at Lifestyle Medicine 2023, the annual meeting of the American College of Lifestyle Medicine.
METHODOLOGY:
- Franklin Somchith Ly, a PhD candidate in mechanical engineering at the University of California, Santa Barbara, developed , a product that assesses blood flow to the hand with an infrared temperature sensor and changes color as blood vessels expand during relaxation.
- Exercises such as intentional breathwork, visualization, and muscle relaxation change the color displayed by the device.
- Mr. Ly examined how measures of anxiety, sleep quality, and chronic pain changed after participants used the instrument. Ten participants completed a study assessing anxiety. Eight participants were enrolled in a sleep study where they completed biofeedback sessions before bed for 2 weeks, and 15 participants performed biofeedback twice daily and reported their levels of anxiety and pain.
TAKEAWAY:
- Anxiety scores decreased by about 22% on average (P < .001).
- Seven of the eight participants in the sleep study had improved scores on the Pittsburgh Sleep Quality Index, with an average improvement of nearly 30% (P < .05). Daytime dysfunction improved by 58% (P < .01).
- In the chronic pain study, about 60% of the 350 biofeedback sessions led to reduced pain.
IN PRACTICE:
“These portable devices may aid lifestyle management by alleviating anxiety, chronic pain, and enhancing daytime energy,” Mr. Ly said. “The results support their integration into lifestyle medicine and integrative medicine.”
SOURCE:
Mr. Ly presented the findings as a poster at Lifestyle Medicine 2023, which took place Oct. 29 to Nov. 1 in Denver and online.
LIMITATIONS:
The studies were open label and did not include control groups.
DISCLOSURES:
Mr. Ly is the founder of CalmStone, which markets a thermal biofeedback device. The research was supported by the Bill and Melinda Gates Foundation and the U.S. Army Research Office and Institute for Collaborative Biotechnologies.
A version of this article first appeared on Medscape.com.
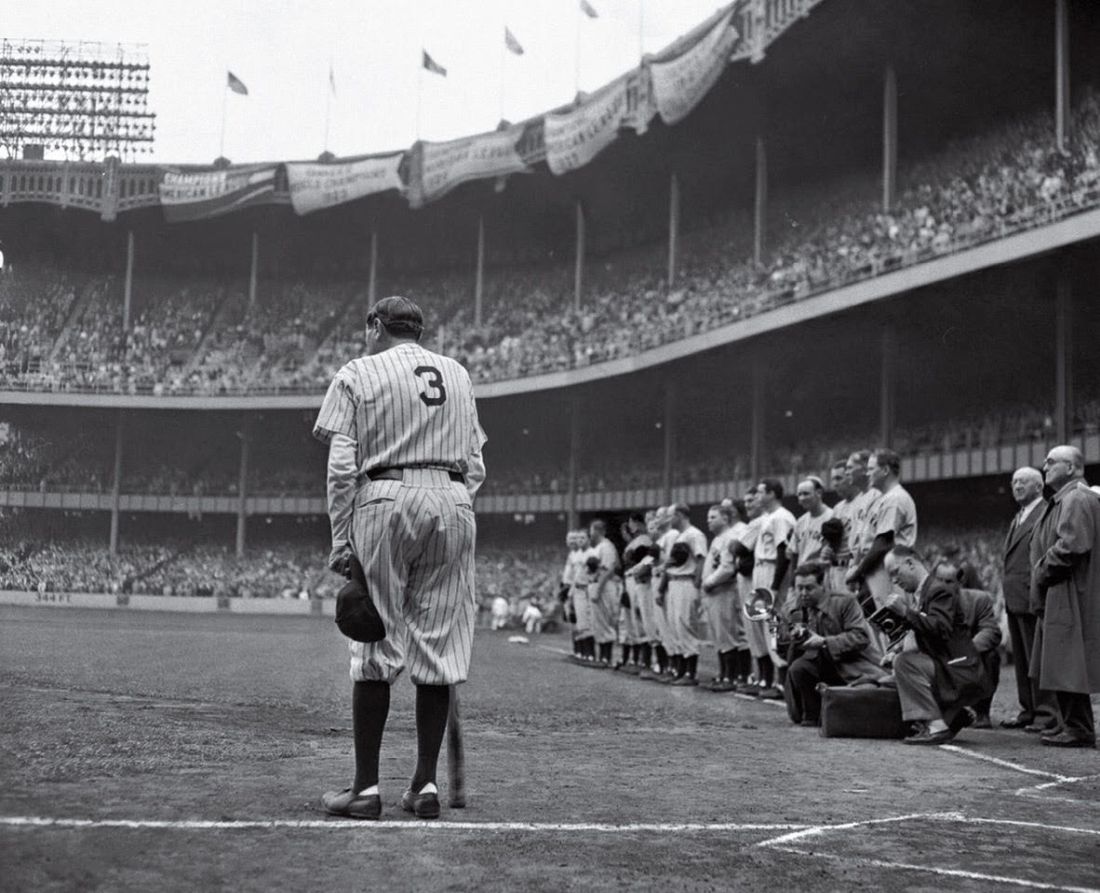
Babe Ruth’s unique cane, and why he used it
Babe Ruth was arguably the greatest athlete in American history.
Certainly, there have been, and always will be, many great figures in all sports. But none of them – Michael Jordan or LeBron James or Tom Brady – have ever, probably will never, dominate sports AND society in the way Babe Ruth did.
Ruth wasn’t an angel, nor did he claim to be. But he was a center of American life the way no athlete ever was or will be.
He was a remarkably good baseball player. In an era where home runs were rarities, he hit more than the entire rest of Major League Baseball combined. But he wasn’t just a slugger, he was an excellent play maker, fielder, and pitcher. (He was actually one of the best pitchers of his era, something else mostly forgotten today.)
Ruth retired in 1935. He never entirely left the limelight, with fans showing up even to watch him play golf in celebrity tournaments. In 1939 he spoke on July 4 at Lou Gehrig appreciation day as his former teammate was publicly dying of ALS.
In 1946 Ruth began having trouble swallowing and developed pain over his right eye. He was found to have nasopharyngeal carcinoma spreading down into his skull base and neck.
Even today surgery to remove cancer from that area is tricky. In 1946 it didn’t exist. An experimental treatment of combined radiation and chemotherapy – today standard – was tried, including a new folic acid derivative called teropterin. He improved somewhat – enough that he was an unnamed case study presented at a medical meeting – but had lost 80 pounds. After a brief respite he continued to go downhill. On June 13, 1948, he appeared at Yankee Stadium – the house that Ruth built – for the last time, where he was honored. He had difficulty walking and used a baseball bat as a cane. His pharynx was so damaged his voice could barely be heard. He died 2 months later on Aug. 16, 1948.
This isn’t a sports column, I’m not a sports writer, and this definitely ain’t Sport Illustrated. So why am I writing this?
Because Babe Ruth never knew he had cancer. Was never told he was dying. His family was afraid he’d harm himself if he knew, so his doctors were under strict instructions to keep the bad news from him.
Now, Ruth wasn’t stupid. Wild, unrepentant, hedonistic, and a lot of other things – but not stupid. He certainly must have figured it out with getting radiation, or chemotherapy, or his declining physical status. But none of his doctors or family ever told him he had cancer and was dying (what they did tell him I have no idea).
Let’s look at this as a case history: A 51-year-old male, possessed of all his mental faculties, presents with headaches, dysphonia, and dysphagia. Workup reveals advanced, inoperable, nasopharyngeal cancer. The family is willing to accept treatment, but understands the prognosis is poor. Family members request that, under no circumstances, he be told of the diagnosis or prognosis.
The fact that the patient is probably the biggest celebrity of his era shouldn’t make a difference, but it does.
I’m sure most of us would want to tell the patient. We live in an age of patient autonomy. . But what if the family has concerns that the patient would hurt himself, as Ruth’s family did?
This summer is 75 years since the Babe died. Medicine has changed a lot, but some questions never will.
What would you do?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Babe Ruth was arguably the greatest athlete in American history.
Certainly, there have been, and always will be, many great figures in all sports. But none of them – Michael Jordan or LeBron James or Tom Brady – have ever, probably will never, dominate sports AND society in the way Babe Ruth did.
Ruth wasn’t an angel, nor did he claim to be. But he was a center of American life the way no athlete ever was or will be.
He was a remarkably good baseball player. In an era where home runs were rarities, he hit more than the entire rest of Major League Baseball combined. But he wasn’t just a slugger, he was an excellent play maker, fielder, and pitcher. (He was actually one of the best pitchers of his era, something else mostly forgotten today.)
Ruth retired in 1935. He never entirely left the limelight, with fans showing up even to watch him play golf in celebrity tournaments. In 1939 he spoke on July 4 at Lou Gehrig appreciation day as his former teammate was publicly dying of ALS.
In 1946 Ruth began having trouble swallowing and developed pain over his right eye. He was found to have nasopharyngeal carcinoma spreading down into his skull base and neck.
Even today surgery to remove cancer from that area is tricky. In 1946 it didn’t exist. An experimental treatment of combined radiation and chemotherapy – today standard – was tried, including a new folic acid derivative called teropterin. He improved somewhat – enough that he was an unnamed case study presented at a medical meeting – but had lost 80 pounds. After a brief respite he continued to go downhill. On June 13, 1948, he appeared at Yankee Stadium – the house that Ruth built – for the last time, where he was honored. He had difficulty walking and used a baseball bat as a cane. His pharynx was so damaged his voice could barely be heard. He died 2 months later on Aug. 16, 1948.
This isn’t a sports column, I’m not a sports writer, and this definitely ain’t Sport Illustrated. So why am I writing this?
Because Babe Ruth never knew he had cancer. Was never told he was dying. His family was afraid he’d harm himself if he knew, so his doctors were under strict instructions to keep the bad news from him.
Now, Ruth wasn’t stupid. Wild, unrepentant, hedonistic, and a lot of other things – but not stupid. He certainly must have figured it out with getting radiation, or chemotherapy, or his declining physical status. But none of his doctors or family ever told him he had cancer and was dying (what they did tell him I have no idea).
Let’s look at this as a case history: A 51-year-old male, possessed of all his mental faculties, presents with headaches, dysphonia, and dysphagia. Workup reveals advanced, inoperable, nasopharyngeal cancer. The family is willing to accept treatment, but understands the prognosis is poor. Family members request that, under no circumstances, he be told of the diagnosis or prognosis.
The fact that the patient is probably the biggest celebrity of his era shouldn’t make a difference, but it does.
I’m sure most of us would want to tell the patient. We live in an age of patient autonomy. . But what if the family has concerns that the patient would hurt himself, as Ruth’s family did?
This summer is 75 years since the Babe died. Medicine has changed a lot, but some questions never will.
What would you do?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Babe Ruth was arguably the greatest athlete in American history.
Certainly, there have been, and always will be, many great figures in all sports. But none of them – Michael Jordan or LeBron James or Tom Brady – have ever, probably will never, dominate sports AND society in the way Babe Ruth did.
Ruth wasn’t an angel, nor did he claim to be. But he was a center of American life the way no athlete ever was or will be.
He was a remarkably good baseball player. In an era where home runs were rarities, he hit more than the entire rest of Major League Baseball combined. But he wasn’t just a slugger, he was an excellent play maker, fielder, and pitcher. (He was actually one of the best pitchers of his era, something else mostly forgotten today.)
Ruth retired in 1935. He never entirely left the limelight, with fans showing up even to watch him play golf in celebrity tournaments. In 1939 he spoke on July 4 at Lou Gehrig appreciation day as his former teammate was publicly dying of ALS.
In 1946 Ruth began having trouble swallowing and developed pain over his right eye. He was found to have nasopharyngeal carcinoma spreading down into his skull base and neck.
Even today surgery to remove cancer from that area is tricky. In 1946 it didn’t exist. An experimental treatment of combined radiation and chemotherapy – today standard – was tried, including a new folic acid derivative called teropterin. He improved somewhat – enough that he was an unnamed case study presented at a medical meeting – but had lost 80 pounds. After a brief respite he continued to go downhill. On June 13, 1948, he appeared at Yankee Stadium – the house that Ruth built – for the last time, where he was honored. He had difficulty walking and used a baseball bat as a cane. His pharynx was so damaged his voice could barely be heard. He died 2 months later on Aug. 16, 1948.
This isn’t a sports column, I’m not a sports writer, and this definitely ain’t Sport Illustrated. So why am I writing this?
Because Babe Ruth never knew he had cancer. Was never told he was dying. His family was afraid he’d harm himself if he knew, so his doctors were under strict instructions to keep the bad news from him.
Now, Ruth wasn’t stupid. Wild, unrepentant, hedonistic, and a lot of other things – but not stupid. He certainly must have figured it out with getting radiation, or chemotherapy, or his declining physical status. But none of his doctors or family ever told him he had cancer and was dying (what they did tell him I have no idea).
Let’s look at this as a case history: A 51-year-old male, possessed of all his mental faculties, presents with headaches, dysphonia, and dysphagia. Workup reveals advanced, inoperable, nasopharyngeal cancer. The family is willing to accept treatment, but understands the prognosis is poor. Family members request that, under no circumstances, he be told of the diagnosis or prognosis.
The fact that the patient is probably the biggest celebrity of his era shouldn’t make a difference, but it does.
I’m sure most of us would want to tell the patient. We live in an age of patient autonomy. . But what if the family has concerns that the patient would hurt himself, as Ruth’s family did?
This summer is 75 years since the Babe died. Medicine has changed a lot, but some questions never will.
What would you do?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Palliative radiation therapy improves QoL in high-grade glioma
Topline
Methodology
- Uncertainty persists about the value of palliative radiation, particularly longer regimens, among patients with high-grade gliomas.
- To address the uncertainty, investigators administered quality of life (QoL) questionnaires to patients before receiving 35 Gy of palliative radiation in 10 fractions over 2 weeks, then again 1 month after treatment, followed by every 3 months until disease progression or death.
- Overall, 49 of 55 patients (89%) completed radiation treatment, and 42 completed the surveys.
- QoL was assessed using the 100-point European Organization for Research and Treatment of Cancer QoL core questionnaire (QLQ-C30) and its brain cancer module (BN20).
- Two-thirds of patients were treated with temozolomide chemotherapy following radiation.
Takeaways
- There was clinically and statistically significant improvement 1 month after radiation therapy in patient-reported fatigue and dyspnea on the QLQ-C30.
- A clinically meaningful improvement – meaning a 10-point or greater improvement – was seen for insomnia. Other symptoms, such as nausea/vomiting, loss of appetite, constipation, diarrhea, and financial difficulty, remained stable over time.
- On the BN20, investigators reported clinically and statistically significant improvement in motor function; other symptoms remained stable.
- Median progression-free survival was 8.4 months; median overall survival was 10.5 months.
In practice
“Short-course palliative hypofractionated radiotherapy in patients with poor-prognosis [high-grade glioma] does not impair QoL in the short term; but is rather associated with stable and/or improved QoL scores in several domains/symptom scales” at 1-3 months after treatment, “making it a viable resource-sparing alternative regimen,” the authors concluded.
Source
The work, led by Y. Baviskar of the Tata Memorial Hospital department of radiation oncology in Mumbai, India, was published July 11 in Clinical Oncology.
Limitations
- It was a single-center study with no control arm.
- Fewer patients completed QoL forms over time, limiting longitudinal assessment to 3 months.
- Forms might have been completed by caregivers at times, raising questions about the veracity of responses.
Disclosures
- There was no external funding for the work.
- The investigators report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Topline
Methodology
- Uncertainty persists about the value of palliative radiation, particularly longer regimens, among patients with high-grade gliomas.
- To address the uncertainty, investigators administered quality of life (QoL) questionnaires to patients before receiving 35 Gy of palliative radiation in 10 fractions over 2 weeks, then again 1 month after treatment, followed by every 3 months until disease progression or death.
- Overall, 49 of 55 patients (89%) completed radiation treatment, and 42 completed the surveys.
- QoL was assessed using the 100-point European Organization for Research and Treatment of Cancer QoL core questionnaire (QLQ-C30) and its brain cancer module (BN20).
- Two-thirds of patients were treated with temozolomide chemotherapy following radiation.
Takeaways
- There was clinically and statistically significant improvement 1 month after radiation therapy in patient-reported fatigue and dyspnea on the QLQ-C30.
- A clinically meaningful improvement – meaning a 10-point or greater improvement – was seen for insomnia. Other symptoms, such as nausea/vomiting, loss of appetite, constipation, diarrhea, and financial difficulty, remained stable over time.
- On the BN20, investigators reported clinically and statistically significant improvement in motor function; other symptoms remained stable.
- Median progression-free survival was 8.4 months; median overall survival was 10.5 months.
In practice
“Short-course palliative hypofractionated radiotherapy in patients with poor-prognosis [high-grade glioma] does not impair QoL in the short term; but is rather associated with stable and/or improved QoL scores in several domains/symptom scales” at 1-3 months after treatment, “making it a viable resource-sparing alternative regimen,” the authors concluded.
Source
The work, led by Y. Baviskar of the Tata Memorial Hospital department of radiation oncology in Mumbai, India, was published July 11 in Clinical Oncology.
Limitations
- It was a single-center study with no control arm.
- Fewer patients completed QoL forms over time, limiting longitudinal assessment to 3 months.
- Forms might have been completed by caregivers at times, raising questions about the veracity of responses.
Disclosures
- There was no external funding for the work.
- The investigators report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Topline
Methodology
- Uncertainty persists about the value of palliative radiation, particularly longer regimens, among patients with high-grade gliomas.
- To address the uncertainty, investigators administered quality of life (QoL) questionnaires to patients before receiving 35 Gy of palliative radiation in 10 fractions over 2 weeks, then again 1 month after treatment, followed by every 3 months until disease progression or death.
- Overall, 49 of 55 patients (89%) completed radiation treatment, and 42 completed the surveys.
- QoL was assessed using the 100-point European Organization for Research and Treatment of Cancer QoL core questionnaire (QLQ-C30) and its brain cancer module (BN20).
- Two-thirds of patients were treated with temozolomide chemotherapy following radiation.
Takeaways
- There was clinically and statistically significant improvement 1 month after radiation therapy in patient-reported fatigue and dyspnea on the QLQ-C30.
- A clinically meaningful improvement – meaning a 10-point or greater improvement – was seen for insomnia. Other symptoms, such as nausea/vomiting, loss of appetite, constipation, diarrhea, and financial difficulty, remained stable over time.
- On the BN20, investigators reported clinically and statistically significant improvement in motor function; other symptoms remained stable.
- Median progression-free survival was 8.4 months; median overall survival was 10.5 months.
In practice
“Short-course palliative hypofractionated radiotherapy in patients with poor-prognosis [high-grade glioma] does not impair QoL in the short term; but is rather associated with stable and/or improved QoL scores in several domains/symptom scales” at 1-3 months after treatment, “making it a viable resource-sparing alternative regimen,” the authors concluded.
Source
The work, led by Y. Baviskar of the Tata Memorial Hospital department of radiation oncology in Mumbai, India, was published July 11 in Clinical Oncology.
Limitations
- It was a single-center study with no control arm.
- Fewer patients completed QoL forms over time, limiting longitudinal assessment to 3 months.
- Forms might have been completed by caregivers at times, raising questions about the veracity of responses.
Disclosures
- There was no external funding for the work.
- The investigators report no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM CLINICAL ONCOLOGY
Can a biodegradable brain implant deliver lifesaving cancer meds?
It’s the latest advance in a rapidly growing field using ultrasound – high-frequency sound waves undetectable to humans – to fight cancer and other diseases.
The problem addressed by the researchers is the blood-brain barrier, a nearly impenetrable blood vessel lining that keeps harmful molecules from passing into the brain from the blood. But this lining can also block chemo drugs from reaching cancer cells.
So the scientists implanted 1-cm2 devices into the skulls of mice, directly behind the tumor site. The implants generate ultrasound waves, loosening the barrier and allowing the drugs to reach the tumor. The sound waves leave healthy tissue undamaged.
“You inject the drug into the body and turn on the ultrasound at the same time. You’re going to hit precisely at the tumor area every single time you use it,” said lead study author Thanh Nguyen, PhD, an associate professor of mechanical engineering at the University of Connecticut, Storrs.
The drug used in the study was paclitaxel, which normally struggles to get through the blood-brain barrier. The tumors shrank, and the mice doubled their lifetime, compared with untreated mice. The mice showed no bad health effects 6 months later.
Breaking through the blood-brain barrier
The biodegradable implant is made of glycine, an amino acid that’s also strongly piezoelectric, meaning it vibrates when subjected to an electrical current. To make it, researchers cultivated glycine crystals, shattered them into pieces, and finally used a process called electrospinning, which applies a high electrical voltage to the nanocrystals.
Voltage flows to the implant via an external device. The resulting ultrasound causes the tightly adhered cells of the blood-brain barrier to vibrate, stretching them out and creating space for pores to form.
“That allows in very tiny particles, including chemo drugs,” said Dr. Nguyen.
His earlier biodegradable implant broke apart from the force, but the new glycine implant is more flexible, stable, and highly piezoelectric. It could be implanted after a patient has surgery to remove a brain tumor, to continue treating residual cancer cells. The implant dissolves harmlessly in the body over time, and doctors can control its lifespan.
A new wave of uses for ultrasound
Dr. Nguyen’s study builds on similar efforts, including a recent clinical trial of a nonbiodegradable implant for treating brain tumors. Ultrasound can focus energy on precise targets in the body.
It’s like “using a magnifying glass to focus multiple beams of light on a point and burn a hole in a leaf,” said Neal Kassell, MD, founder and chairman of the Focused Ultrasound Foundation. This approach spares adjacent normal tissue.
Doctors now understand more than 30 ways that ultrasound interacts with tissue – from destroying abnormal tissue to delivering drugs more effectively to stimulating an immune response. A decade ago, only five such interactions were known.
This opens the door for treating “a wide spectrum of medical disorders,” from neurodegenerative diseases like Alzheimer’s and Parkinson’s to difficult-to-treat cancers of the prostate and pancreas, and even addiction, said Dr. Kassell.
Dr. Kassell envisions using focused ultrasound to treat brain tumors as an alternative (or complement) to surgery, chemotherapy, immunotherapy, or radiation therapy. In the meantime, implants have helped show “the effectiveness of opening the blood-brain barrier.”
Dr. Nguyen’s team plans on testing the safety and efficacy of their implant in pigs next. Eventually, Dr. Nguyen hopes to develop a patch with an array of implants to target different areas of the brain.
One study coauthor is cofounder of PiezoBioMembrane and SingleTimeMicroneedles. The other study authors reported no conflicts of interest.
A version of this article originally appeared on WebMD.com.
It’s the latest advance in a rapidly growing field using ultrasound – high-frequency sound waves undetectable to humans – to fight cancer and other diseases.
The problem addressed by the researchers is the blood-brain barrier, a nearly impenetrable blood vessel lining that keeps harmful molecules from passing into the brain from the blood. But this lining can also block chemo drugs from reaching cancer cells.
So the scientists implanted 1-cm2 devices into the skulls of mice, directly behind the tumor site. The implants generate ultrasound waves, loosening the barrier and allowing the drugs to reach the tumor. The sound waves leave healthy tissue undamaged.
“You inject the drug into the body and turn on the ultrasound at the same time. You’re going to hit precisely at the tumor area every single time you use it,” said lead study author Thanh Nguyen, PhD, an associate professor of mechanical engineering at the University of Connecticut, Storrs.
The drug used in the study was paclitaxel, which normally struggles to get through the blood-brain barrier. The tumors shrank, and the mice doubled their lifetime, compared with untreated mice. The mice showed no bad health effects 6 months later.
Breaking through the blood-brain barrier
The biodegradable implant is made of glycine, an amino acid that’s also strongly piezoelectric, meaning it vibrates when subjected to an electrical current. To make it, researchers cultivated glycine crystals, shattered them into pieces, and finally used a process called electrospinning, which applies a high electrical voltage to the nanocrystals.
Voltage flows to the implant via an external device. The resulting ultrasound causes the tightly adhered cells of the blood-brain barrier to vibrate, stretching them out and creating space for pores to form.
“That allows in very tiny particles, including chemo drugs,” said Dr. Nguyen.
His earlier biodegradable implant broke apart from the force, but the new glycine implant is more flexible, stable, and highly piezoelectric. It could be implanted after a patient has surgery to remove a brain tumor, to continue treating residual cancer cells. The implant dissolves harmlessly in the body over time, and doctors can control its lifespan.
A new wave of uses for ultrasound
Dr. Nguyen’s study builds on similar efforts, including a recent clinical trial of a nonbiodegradable implant for treating brain tumors. Ultrasound can focus energy on precise targets in the body.
It’s like “using a magnifying glass to focus multiple beams of light on a point and burn a hole in a leaf,” said Neal Kassell, MD, founder and chairman of the Focused Ultrasound Foundation. This approach spares adjacent normal tissue.
Doctors now understand more than 30 ways that ultrasound interacts with tissue – from destroying abnormal tissue to delivering drugs more effectively to stimulating an immune response. A decade ago, only five such interactions were known.
This opens the door for treating “a wide spectrum of medical disorders,” from neurodegenerative diseases like Alzheimer’s and Parkinson’s to difficult-to-treat cancers of the prostate and pancreas, and even addiction, said Dr. Kassell.
Dr. Kassell envisions using focused ultrasound to treat brain tumors as an alternative (or complement) to surgery, chemotherapy, immunotherapy, or radiation therapy. In the meantime, implants have helped show “the effectiveness of opening the blood-brain barrier.”
Dr. Nguyen’s team plans on testing the safety and efficacy of their implant in pigs next. Eventually, Dr. Nguyen hopes to develop a patch with an array of implants to target different areas of the brain.
One study coauthor is cofounder of PiezoBioMembrane and SingleTimeMicroneedles. The other study authors reported no conflicts of interest.
A version of this article originally appeared on WebMD.com.
It’s the latest advance in a rapidly growing field using ultrasound – high-frequency sound waves undetectable to humans – to fight cancer and other diseases.
The problem addressed by the researchers is the blood-brain barrier, a nearly impenetrable blood vessel lining that keeps harmful molecules from passing into the brain from the blood. But this lining can also block chemo drugs from reaching cancer cells.
So the scientists implanted 1-cm2 devices into the skulls of mice, directly behind the tumor site. The implants generate ultrasound waves, loosening the barrier and allowing the drugs to reach the tumor. The sound waves leave healthy tissue undamaged.
“You inject the drug into the body and turn on the ultrasound at the same time. You’re going to hit precisely at the tumor area every single time you use it,” said lead study author Thanh Nguyen, PhD, an associate professor of mechanical engineering at the University of Connecticut, Storrs.
The drug used in the study was paclitaxel, which normally struggles to get through the blood-brain barrier. The tumors shrank, and the mice doubled their lifetime, compared with untreated mice. The mice showed no bad health effects 6 months later.
Breaking through the blood-brain barrier
The biodegradable implant is made of glycine, an amino acid that’s also strongly piezoelectric, meaning it vibrates when subjected to an electrical current. To make it, researchers cultivated glycine crystals, shattered them into pieces, and finally used a process called electrospinning, which applies a high electrical voltage to the nanocrystals.
Voltage flows to the implant via an external device. The resulting ultrasound causes the tightly adhered cells of the blood-brain barrier to vibrate, stretching them out and creating space for pores to form.
“That allows in very tiny particles, including chemo drugs,” said Dr. Nguyen.
His earlier biodegradable implant broke apart from the force, but the new glycine implant is more flexible, stable, and highly piezoelectric. It could be implanted after a patient has surgery to remove a brain tumor, to continue treating residual cancer cells. The implant dissolves harmlessly in the body over time, and doctors can control its lifespan.
A new wave of uses for ultrasound
Dr. Nguyen’s study builds on similar efforts, including a recent clinical trial of a nonbiodegradable implant for treating brain tumors. Ultrasound can focus energy on precise targets in the body.
It’s like “using a magnifying glass to focus multiple beams of light on a point and burn a hole in a leaf,” said Neal Kassell, MD, founder and chairman of the Focused Ultrasound Foundation. This approach spares adjacent normal tissue.
Doctors now understand more than 30 ways that ultrasound interacts with tissue – from destroying abnormal tissue to delivering drugs more effectively to stimulating an immune response. A decade ago, only five such interactions were known.
This opens the door for treating “a wide spectrum of medical disorders,” from neurodegenerative diseases like Alzheimer’s and Parkinson’s to difficult-to-treat cancers of the prostate and pancreas, and even addiction, said Dr. Kassell.
Dr. Kassell envisions using focused ultrasound to treat brain tumors as an alternative (or complement) to surgery, chemotherapy, immunotherapy, or radiation therapy. In the meantime, implants have helped show “the effectiveness of opening the blood-brain barrier.”
Dr. Nguyen’s team plans on testing the safety and efficacy of their implant in pigs next. Eventually, Dr. Nguyen hopes to develop a patch with an array of implants to target different areas of the brain.
One study coauthor is cofounder of PiezoBioMembrane and SingleTimeMicroneedles. The other study authors reported no conflicts of interest.
A version of this article originally appeared on WebMD.com.
FROM SCIENCE ADVANCES
CBSM phone app eases anxiety, depression in cancer patients
CHICAGO – One-third of patients with cancer also experience anxiety or depression, and an estimated 70% of the 18 million patients with cancer and cancer survivors in the US experience emotional symptoms, including fear of recurrence.
Despite many having these symptoms, few patients with cancer have access to psycho-oncologic support.
A digital cognitive-behavioral stress management (CBSM) application may help to ease some of the burden, reported Allison Ramiller, MPH, of Blue Note Therapeutics in San Francisco, which developed the app version of the program.
In addition, patients assigned to the CBSM app were twice as likely as control persons to report that their symptoms were “much” or “very much” improved after using the app for 12 weeks, Ms. Ramiller reported at an oral abstract session at the annual meeting of the American Society of Clinical Oncology (ASCO).
However, the investigators did not report baseline characteristics of patients in each of the study arms, which might have helped to clarify the depth of the effects they saw.
The CBSM program was developed by Michael H. Antoni, PhD, and colleagues in the University of Miami Health System. It is based on cognitive-behavioral therapy but also includes stress management and relaxation techniques to help patients cope with cancer-specific stress.
“”It has been clinically validated and shown to benefit patients with cancer,” Ms. Ramiller said. “However, access is a problem,” she said.
“There aren’t enough qualified, trained providers for the need, and patients with cancer encounter barriers to in-person participation, including things like transportation or financial barriers. So to overcome this, we developed a digitized version of CBSM,” she explained.
Impressive and elegant
“Everything about [the study] I thought was very impressive, very elegant, very nicely done,” said invited discussant Raymond U. Osarogiagbon, MBBS, FACP, chief scientist at Baptist Memorial Health Care Corp in Memphis, Tenn.
“They showed efficacy, they showed safety – very nice – user friendliness – very good. Certainly they look like they’re trying to address a highly important, unmet need in a very elegant way. Certainly, they pointed out it needs longer follow-up to see sustainability. We need to see will this work in other settings. Will this be cost-effective? You’ve gotta believe it probably will be,” he said.
CBSM has previously been shown to help patients with cancer reduce stress, improve general and cancer-specific quality of life at various stages of treatment, reduce symptom burden, and improve coping skills, Ms. Ramiller said.
To see whether these benefits could be conveyed digitally rather than in face-to-face encounters, Ms. Ramiller and colleagues worked with Dr. Antoni to develop the CBSM app.
Patients using the app received therapeutic content over 10 sessions with audio, video, and interactive tools that mimicked the sessions they would have received during in-person interventions.
They then compared the app against the control educational app in the randomized, decentralized RESTORE study.
High-quality control
Ms. Ramiller said that the control app set “a high bar.”
“The control also offered 10 interactive self-guided sessions. Both treatment apps were professionally designed and visually similar in styling, and they were presented as digital therapeutic-specific for cancer patients. And they were also in a match condition, meaning they received the same attention from study staff and cadence of reminders, but importantly, only the intervention app was based on CBSM,” she explained.
A total of 449 patients with cancers of stage I–III who were undergoing active systemic treatment or were planning to undergo such treatment within 6 months were randomly assigned to the CBSM app or the control app.
The CBSM app was superior to the control app for the primary outcome of anxiety reduction over baseline, as measured at 4, 8 and 12 weeks by the Patient-Reported Outcomes Measurement Information System Anxiety Scale (PROMIS-A) (beta = -.03; P = .019).
CBSM was also significantly better than the control app for the secondary endpoints of reducing symptoms of depression, as measured by the PROMIS-D scale (beta = -.02, P = .042), and also at increasing the percentage of patients who reported improvement in anxiety and depression symptoms on the Patient Global Impression of Change instrument (P < .001)
An extension study of the durability of the effects at 3 and 6 months is underway.
The investigators noted that the incremental cost of management of anxiety or depression is greater than $17,000 per patient per year.
“One of the big promises of a digital therapeutic like this is that it could potentially reduce costs,” Ms. Ramiller told the audience, but she acknowledged, “More work is really needed, however, to directly test the potential savings.”
The RESTORE study is funded by Blue Note Therapeutics. Dr. Osarogiagbon owns stock in Gilead, Lilly, and Pfizer, has received honoraria from Biodesix and Medscape, and has a consulting or advisory role for the American Cancer Society AstraZeneca, Genentech/Roche, LUNGevity, National Cancer Institute, and Triptych Health Partners.
A version of this article originally appeared on Medscape.com.
CHICAGO – One-third of patients with cancer also experience anxiety or depression, and an estimated 70% of the 18 million patients with cancer and cancer survivors in the US experience emotional symptoms, including fear of recurrence.
Despite many having these symptoms, few patients with cancer have access to psycho-oncologic support.
A digital cognitive-behavioral stress management (CBSM) application may help to ease some of the burden, reported Allison Ramiller, MPH, of Blue Note Therapeutics in San Francisco, which developed the app version of the program.
In addition, patients assigned to the CBSM app were twice as likely as control persons to report that their symptoms were “much” or “very much” improved after using the app for 12 weeks, Ms. Ramiller reported at an oral abstract session at the annual meeting of the American Society of Clinical Oncology (ASCO).
However, the investigators did not report baseline characteristics of patients in each of the study arms, which might have helped to clarify the depth of the effects they saw.
The CBSM program was developed by Michael H. Antoni, PhD, and colleagues in the University of Miami Health System. It is based on cognitive-behavioral therapy but also includes stress management and relaxation techniques to help patients cope with cancer-specific stress.
“”It has been clinically validated and shown to benefit patients with cancer,” Ms. Ramiller said. “However, access is a problem,” she said.
“There aren’t enough qualified, trained providers for the need, and patients with cancer encounter barriers to in-person participation, including things like transportation or financial barriers. So to overcome this, we developed a digitized version of CBSM,” she explained.
Impressive and elegant
“Everything about [the study] I thought was very impressive, very elegant, very nicely done,” said invited discussant Raymond U. Osarogiagbon, MBBS, FACP, chief scientist at Baptist Memorial Health Care Corp in Memphis, Tenn.
“They showed efficacy, they showed safety – very nice – user friendliness – very good. Certainly they look like they’re trying to address a highly important, unmet need in a very elegant way. Certainly, they pointed out it needs longer follow-up to see sustainability. We need to see will this work in other settings. Will this be cost-effective? You’ve gotta believe it probably will be,” he said.
CBSM has previously been shown to help patients with cancer reduce stress, improve general and cancer-specific quality of life at various stages of treatment, reduce symptom burden, and improve coping skills, Ms. Ramiller said.
To see whether these benefits could be conveyed digitally rather than in face-to-face encounters, Ms. Ramiller and colleagues worked with Dr. Antoni to develop the CBSM app.
Patients using the app received therapeutic content over 10 sessions with audio, video, and interactive tools that mimicked the sessions they would have received during in-person interventions.
They then compared the app against the control educational app in the randomized, decentralized RESTORE study.
High-quality control
Ms. Ramiller said that the control app set “a high bar.”
“The control also offered 10 interactive self-guided sessions. Both treatment apps were professionally designed and visually similar in styling, and they were presented as digital therapeutic-specific for cancer patients. And they were also in a match condition, meaning they received the same attention from study staff and cadence of reminders, but importantly, only the intervention app was based on CBSM,” she explained.
A total of 449 patients with cancers of stage I–III who were undergoing active systemic treatment or were planning to undergo such treatment within 6 months were randomly assigned to the CBSM app or the control app.
The CBSM app was superior to the control app for the primary outcome of anxiety reduction over baseline, as measured at 4, 8 and 12 weeks by the Patient-Reported Outcomes Measurement Information System Anxiety Scale (PROMIS-A) (beta = -.03; P = .019).
CBSM was also significantly better than the control app for the secondary endpoints of reducing symptoms of depression, as measured by the PROMIS-D scale (beta = -.02, P = .042), and also at increasing the percentage of patients who reported improvement in anxiety and depression symptoms on the Patient Global Impression of Change instrument (P < .001)
An extension study of the durability of the effects at 3 and 6 months is underway.
The investigators noted that the incremental cost of management of anxiety or depression is greater than $17,000 per patient per year.
“One of the big promises of a digital therapeutic like this is that it could potentially reduce costs,” Ms. Ramiller told the audience, but she acknowledged, “More work is really needed, however, to directly test the potential savings.”
The RESTORE study is funded by Blue Note Therapeutics. Dr. Osarogiagbon owns stock in Gilead, Lilly, and Pfizer, has received honoraria from Biodesix and Medscape, and has a consulting or advisory role for the American Cancer Society AstraZeneca, Genentech/Roche, LUNGevity, National Cancer Institute, and Triptych Health Partners.
A version of this article originally appeared on Medscape.com.
CHICAGO – One-third of patients with cancer also experience anxiety or depression, and an estimated 70% of the 18 million patients with cancer and cancer survivors in the US experience emotional symptoms, including fear of recurrence.
Despite many having these symptoms, few patients with cancer have access to psycho-oncologic support.
A digital cognitive-behavioral stress management (CBSM) application may help to ease some of the burden, reported Allison Ramiller, MPH, of Blue Note Therapeutics in San Francisco, which developed the app version of the program.
In addition, patients assigned to the CBSM app were twice as likely as control persons to report that their symptoms were “much” or “very much” improved after using the app for 12 weeks, Ms. Ramiller reported at an oral abstract session at the annual meeting of the American Society of Clinical Oncology (ASCO).
However, the investigators did not report baseline characteristics of patients in each of the study arms, which might have helped to clarify the depth of the effects they saw.
The CBSM program was developed by Michael H. Antoni, PhD, and colleagues in the University of Miami Health System. It is based on cognitive-behavioral therapy but also includes stress management and relaxation techniques to help patients cope with cancer-specific stress.
“”It has been clinically validated and shown to benefit patients with cancer,” Ms. Ramiller said. “However, access is a problem,” she said.
“There aren’t enough qualified, trained providers for the need, and patients with cancer encounter barriers to in-person participation, including things like transportation or financial barriers. So to overcome this, we developed a digitized version of CBSM,” she explained.
Impressive and elegant
“Everything about [the study] I thought was very impressive, very elegant, very nicely done,” said invited discussant Raymond U. Osarogiagbon, MBBS, FACP, chief scientist at Baptist Memorial Health Care Corp in Memphis, Tenn.
“They showed efficacy, they showed safety – very nice – user friendliness – very good. Certainly they look like they’re trying to address a highly important, unmet need in a very elegant way. Certainly, they pointed out it needs longer follow-up to see sustainability. We need to see will this work in other settings. Will this be cost-effective? You’ve gotta believe it probably will be,” he said.
CBSM has previously been shown to help patients with cancer reduce stress, improve general and cancer-specific quality of life at various stages of treatment, reduce symptom burden, and improve coping skills, Ms. Ramiller said.
To see whether these benefits could be conveyed digitally rather than in face-to-face encounters, Ms. Ramiller and colleagues worked with Dr. Antoni to develop the CBSM app.
Patients using the app received therapeutic content over 10 sessions with audio, video, and interactive tools that mimicked the sessions they would have received during in-person interventions.
They then compared the app against the control educational app in the randomized, decentralized RESTORE study.
High-quality control
Ms. Ramiller said that the control app set “a high bar.”
“The control also offered 10 interactive self-guided sessions. Both treatment apps were professionally designed and visually similar in styling, and they were presented as digital therapeutic-specific for cancer patients. And they were also in a match condition, meaning they received the same attention from study staff and cadence of reminders, but importantly, only the intervention app was based on CBSM,” she explained.
A total of 449 patients with cancers of stage I–III who were undergoing active systemic treatment or were planning to undergo such treatment within 6 months were randomly assigned to the CBSM app or the control app.
The CBSM app was superior to the control app for the primary outcome of anxiety reduction over baseline, as measured at 4, 8 and 12 weeks by the Patient-Reported Outcomes Measurement Information System Anxiety Scale (PROMIS-A) (beta = -.03; P = .019).
CBSM was also significantly better than the control app for the secondary endpoints of reducing symptoms of depression, as measured by the PROMIS-D scale (beta = -.02, P = .042), and also at increasing the percentage of patients who reported improvement in anxiety and depression symptoms on the Patient Global Impression of Change instrument (P < .001)
An extension study of the durability of the effects at 3 and 6 months is underway.
The investigators noted that the incremental cost of management of anxiety or depression is greater than $17,000 per patient per year.
“One of the big promises of a digital therapeutic like this is that it could potentially reduce costs,” Ms. Ramiller told the audience, but she acknowledged, “More work is really needed, however, to directly test the potential savings.”
The RESTORE study is funded by Blue Note Therapeutics. Dr. Osarogiagbon owns stock in Gilead, Lilly, and Pfizer, has received honoraria from Biodesix and Medscape, and has a consulting or advisory role for the American Cancer Society AstraZeneca, Genentech/Roche, LUNGevity, National Cancer Institute, and Triptych Health Partners.
A version of this article originally appeared on Medscape.com.
AT ASCO 2023
Drugmakers are abandoning cheap generics, and now U.S. cancer patients can’t get meds
On Nov. 22, three Food and Drug Administration inspectors arrived at the sprawling Intas Pharmaceuticals plant south of Ahmedabad, India, and found hundreds of trash bags full of shredded documents tossed into a garbage truck. Over the next 10 days, the inspectors assessed what looked like a systematic effort to conceal quality problems at the plant, which provided more than half of the U.S. supply of generic cisplatin and carboplatin, two cheap drugs used to treat as many as 500,000 new cancer cases every year.
Their decisions are likely to result in preventable deaths.
Cisplatin and carboplatin are among scores of drugs in shortage, including 12 other cancer drugs, ADHD pills, blood thinners, and antibiotics. COVID-hangover supply chain issues and limited FDA oversight are part of the problem, but the main cause, experts agree, is the underlying weakness of the generic drug industry. Made mostly overseas, these old but crucial drugs are often sold at a loss or for little profit. Domestic manufacturers have little interest in making them, setting their sights instead on high-priced drugs with plump profit margins.
The problem isn’t new, and that’s particularly infuriating to many clinicians. President Joe Biden, whose son Beau died of an aggressive brain cancer, has focused his Cancer Moonshot on discovering cures – undoubtedly expensive ones. Indeed, existing brand-name cancer drugs often cost tens of thousands of dollars a year.
But what about the thousands of patients today who can’t get a drug like cisplatin, approved by the FDA in 1978 and costing as little as $6 a dose?
“It’s just insane,” said Mark Ratain, MD, a cancer doctor and pharmacologist at the University of Chicago. “Your roof is caving in, but you want to build a basketball court in the backyard because your wife is pregnant with twin boys and you want them to be NBA stars when they grow up?”
“It’s just a travesty that this is the level of health care in the United States of America right now,” said Stephen Divers, MD, an oncologist in Hot Springs, Ark., who in recent weeks has had to delay or change treatment for numerous bladder, breast, and ovarian cancer patients because his clinic cannot find enough cisplatin and carboplatin. Results from a survey of academic cancer centers released June 7 found 93% couldn’t find enough carboplatin and 70% had cisplatin shortages.
“All day, in between patients, we hold staff meetings trying to figure this out,” said Bonny Moore, MD, an oncologist in Fredericksburg, Virginia. “It’s the most nauseous I’ve ever felt. Our office stayed open during COVID; we never had to stop treating patients. We got them vaccinated, kept them safe, and now I can’t get them a $10 drug.”
The cancer clinicians KFF Health News interviewed for this story said that, given current shortages, they prioritize patients who can be cured over later-stage patients, in whom the drugs generally can only slow the disease, and for whom alternatives – though sometimes less effective and often with more side effects – are available. But some doctors are even rationing doses intended to cure.
Isabella McDonald, then a junior at Utah Valley University, was diagnosed in April with a rare, often fatal bone cancer, whose sole treatment for young adults includes the drug methotrexate. When Isabella’s second cycle of treatment began June 5, clinicians advised that she would be getting less than the full dose because of a methotrexate shortage, said her father, Brent.
“They don’t think it will have a negative impact on her treatment, but as far as I am aware, there isn’t any scientific basis to make that conclusion,” he said. “As you can imagine, when they gave us such low odds of her beating this cancer, it feels like we want to give it everything we can and not something short of the standard.”
Mr. McDonald stressed that he didn’t blame the staffers at Intermountain Health who take care of Isabella. The family – his other daughter, Cate, made a TikTok video about her sister’s plight – were simply stunned at such a basic flaw in the health care system.
At Dr. Moore’s practice, in Virginia, clinicians gave 60% of the optimal dose of carboplatin to some uterine cancer patients during the week of May 16, then shifted to 80% after a small shipment came in the following week. The doctors had to omit carboplatin from normal combination treatments for patients with recurrent disease, she said.
On June 2, Dr. Moore and colleagues were glued to their drug distributor’s website, anxious as teenagers waiting for Taylor Swift tickets to go on sale – only with mortal consequences at stake.
She later emailed KFF Health News: “Carboplatin did NOT come back in stock today. Neither did cisplatin.”
Doses remained at 80%, she said. Things hadn’t changed 10 days later.
Generics manufacturers are pulling out
The causes of shortages are well established. Everyone wants to pay less, and the middlemen who procure and distribute generics keep driving down wholesale prices. The average net price of generic drugs fell by more than half between 2016 and 2022, according to research by Anthony Sardella, a business professor at Washington University in St. Louis.
As generics manufacturers compete to win sales contracts with the big negotiators of such purchases, such as Vizient and Premier, their profits sink. Some are going out of business. Akorn, which made 75 common generics, went bankrupt and closed in February. Israeli generics giant Teva, which has a portfolio of 3,600 medicines, announced May 18 it was shifting to brand-name drugs and “high-value generics.” Lannett, with about 120 generics, announced a Chapter 11 reorganization amid declining revenue. Other companies are in trouble too, said David Gaugh, interim CEO of the Association for Accessible Medicines, the leading generics trade group.
The generics industry used to lose money on about a third of the drugs it produced, but now it’s more like half, Mr. Gaugh said. So when a company stops making a drug, others do not necessarily step up, he said. Officials at Fresenius Kabi and Pfizer said they have increased their carboplatin production since March, but not enough to end the shortage. On June 2, FDA Commissioner Robert Califf announced the agency had given emergency authorization for Chinese-made cisplatin to enter the U.S. market, but the impact of the move wasn’t immediately clear.
Cisplatin and carboplatin are made in special production lines under sterile conditions, and expanding or changing the lines requires FDA approval. Bargain-basement prices have pushed production overseas, where it’s harder for the FDA to track quality standards. The Intas plant inspection was a relative rarity in India, where the FDA in 2022 reportedly inspected only 3% of sites that make drugs for the U.S. market. Mr. Sardella testified in May that a quarter of all U.S. drug prescriptions are filled by companies that received FDA warning letters in the past 26 months. And pharmaceutical industry product recalls are at their highest level in 18 years, reflecting fragile supply conditions.
The FDA listed 137 drugs in shortage as of June 13, including many essential medicines made by few companies.
Intas voluntarily shut down its Ahmedabad plant after the FDA inspection, and the agency posted its shocking inspection report in January. Accord Healthcare, the U.S. subsidiary of Intas, said in mid-June it had no date for restarting production.
Asked why it waited 2 months after its inspection to announce the cisplatin shortage, given that Intas supplied more than half the U.S. market for the drug, the FDA said via email that it doesn’t list a drug in shortage until it has “confirmed that overall market demand is not being met.”
Prices for carboplatin, cisplatin, and other drugs have skyrocketed on the so-called gray market, where speculators sell medicines they snapped up in anticipation of shortages. A 600-mg bottle of carboplatin, normally available for $30, was going for $185 in early May and $345 a week later, said Richard Scanlon, the pharmacist at dr. Moore’s clinic.
“It’s hard to have these conversations with patients – ‘I have your dose for this cycle, but not sure about next cycle,’” said Mark Einstein, MD, chair of the department of obstetrics, gynecology and reproductive health at New Jersey Medical School, Newark.
Should government step in?
Despite a drug shortage task force and numerous congressional hearings, progress has been slow at best. The 2020 CARES Act gave the FDA the power to require companies to have contingency plans enabling them to respond to shortages, but the agency has not yet implemented guidance to enforce the provisions.
As a result, neither Accord nor other cisplatin makers had a response plan in place when Intas’ plant was shut down, said Soumi Saha, senior vice president of government affairs for Premier, which arranges wholesale drug purchases for more than 4,400 hospitals and health systems.
Premier understood in December that the shutdown endangered the U.S. supply of cisplatin and carboplatin, but it also didn’t issue an immediate alarm. “It’s a fine balance,” she said. “You don’t want to create panic-buying or hoarding.”
More lasting solutions are under discussion. Mr. Sardella and others have proposed government subsidies to get U.S. generics plants running full time. Their capacity is now half-idle. If federal agencies like the Centers for Medicare & Medicaid Services paid more for more safely and efficiently produced drugs, it would promote a more stable supply chain, he said.
“At a certain point the system needs to recognize there’s a high cost to low-cost drugs,” said Allan Coukell, senior vice president for public policy at Civica Rx, a nonprofit funded by health systems, foundations, and the federal government that provides about 80 drugs to hospitals in its network. Civica is building a $140 million factory near Petersburg, Va., that will produce dozens more, Mr. Coukell said.
Dr. Ratain and his University of Chicago colleague Satyajit Kosuri, MD, recently called for the creation of a strategic inventory buffer for generic medications, something like the Strategic Petroleum Reserve, set up in 1975 in response to the OPEC oil crisis.
In fact, Dr. Ratain reckons, selling a quarter-million barrels of oil would probably generate enough cash to make and store 2 years’ worth of carboplatin and cisplatin.
“It would almost literally be a drop in the bucket.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – an independent source of health policy research, polling, and journalism. Learn more about KFF.
On Nov. 22, three Food and Drug Administration inspectors arrived at the sprawling Intas Pharmaceuticals plant south of Ahmedabad, India, and found hundreds of trash bags full of shredded documents tossed into a garbage truck. Over the next 10 days, the inspectors assessed what looked like a systematic effort to conceal quality problems at the plant, which provided more than half of the U.S. supply of generic cisplatin and carboplatin, two cheap drugs used to treat as many as 500,000 new cancer cases every year.
Their decisions are likely to result in preventable deaths.
Cisplatin and carboplatin are among scores of drugs in shortage, including 12 other cancer drugs, ADHD pills, blood thinners, and antibiotics. COVID-hangover supply chain issues and limited FDA oversight are part of the problem, but the main cause, experts agree, is the underlying weakness of the generic drug industry. Made mostly overseas, these old but crucial drugs are often sold at a loss or for little profit. Domestic manufacturers have little interest in making them, setting their sights instead on high-priced drugs with plump profit margins.
The problem isn’t new, and that’s particularly infuriating to many clinicians. President Joe Biden, whose son Beau died of an aggressive brain cancer, has focused his Cancer Moonshot on discovering cures – undoubtedly expensive ones. Indeed, existing brand-name cancer drugs often cost tens of thousands of dollars a year.
But what about the thousands of patients today who can’t get a drug like cisplatin, approved by the FDA in 1978 and costing as little as $6 a dose?
“It’s just insane,” said Mark Ratain, MD, a cancer doctor and pharmacologist at the University of Chicago. “Your roof is caving in, but you want to build a basketball court in the backyard because your wife is pregnant with twin boys and you want them to be NBA stars when they grow up?”
“It’s just a travesty that this is the level of health care in the United States of America right now,” said Stephen Divers, MD, an oncologist in Hot Springs, Ark., who in recent weeks has had to delay or change treatment for numerous bladder, breast, and ovarian cancer patients because his clinic cannot find enough cisplatin and carboplatin. Results from a survey of academic cancer centers released June 7 found 93% couldn’t find enough carboplatin and 70% had cisplatin shortages.
“All day, in between patients, we hold staff meetings trying to figure this out,” said Bonny Moore, MD, an oncologist in Fredericksburg, Virginia. “It’s the most nauseous I’ve ever felt. Our office stayed open during COVID; we never had to stop treating patients. We got them vaccinated, kept them safe, and now I can’t get them a $10 drug.”
The cancer clinicians KFF Health News interviewed for this story said that, given current shortages, they prioritize patients who can be cured over later-stage patients, in whom the drugs generally can only slow the disease, and for whom alternatives – though sometimes less effective and often with more side effects – are available. But some doctors are even rationing doses intended to cure.
Isabella McDonald, then a junior at Utah Valley University, was diagnosed in April with a rare, often fatal bone cancer, whose sole treatment for young adults includes the drug methotrexate. When Isabella’s second cycle of treatment began June 5, clinicians advised that she would be getting less than the full dose because of a methotrexate shortage, said her father, Brent.
“They don’t think it will have a negative impact on her treatment, but as far as I am aware, there isn’t any scientific basis to make that conclusion,” he said. “As you can imagine, when they gave us such low odds of her beating this cancer, it feels like we want to give it everything we can and not something short of the standard.”
Mr. McDonald stressed that he didn’t blame the staffers at Intermountain Health who take care of Isabella. The family – his other daughter, Cate, made a TikTok video about her sister’s plight – were simply stunned at such a basic flaw in the health care system.
At Dr. Moore’s practice, in Virginia, clinicians gave 60% of the optimal dose of carboplatin to some uterine cancer patients during the week of May 16, then shifted to 80% after a small shipment came in the following week. The doctors had to omit carboplatin from normal combination treatments for patients with recurrent disease, she said.
On June 2, Dr. Moore and colleagues were glued to their drug distributor’s website, anxious as teenagers waiting for Taylor Swift tickets to go on sale – only with mortal consequences at stake.
She later emailed KFF Health News: “Carboplatin did NOT come back in stock today. Neither did cisplatin.”
Doses remained at 80%, she said. Things hadn’t changed 10 days later.
Generics manufacturers are pulling out
The causes of shortages are well established. Everyone wants to pay less, and the middlemen who procure and distribute generics keep driving down wholesale prices. The average net price of generic drugs fell by more than half between 2016 and 2022, according to research by Anthony Sardella, a business professor at Washington University in St. Louis.
As generics manufacturers compete to win sales contracts with the big negotiators of such purchases, such as Vizient and Premier, their profits sink. Some are going out of business. Akorn, which made 75 common generics, went bankrupt and closed in February. Israeli generics giant Teva, which has a portfolio of 3,600 medicines, announced May 18 it was shifting to brand-name drugs and “high-value generics.” Lannett, with about 120 generics, announced a Chapter 11 reorganization amid declining revenue. Other companies are in trouble too, said David Gaugh, interim CEO of the Association for Accessible Medicines, the leading generics trade group.
The generics industry used to lose money on about a third of the drugs it produced, but now it’s more like half, Mr. Gaugh said. So when a company stops making a drug, others do not necessarily step up, he said. Officials at Fresenius Kabi and Pfizer said they have increased their carboplatin production since March, but not enough to end the shortage. On June 2, FDA Commissioner Robert Califf announced the agency had given emergency authorization for Chinese-made cisplatin to enter the U.S. market, but the impact of the move wasn’t immediately clear.
Cisplatin and carboplatin are made in special production lines under sterile conditions, and expanding or changing the lines requires FDA approval. Bargain-basement prices have pushed production overseas, where it’s harder for the FDA to track quality standards. The Intas plant inspection was a relative rarity in India, where the FDA in 2022 reportedly inspected only 3% of sites that make drugs for the U.S. market. Mr. Sardella testified in May that a quarter of all U.S. drug prescriptions are filled by companies that received FDA warning letters in the past 26 months. And pharmaceutical industry product recalls are at their highest level in 18 years, reflecting fragile supply conditions.
The FDA listed 137 drugs in shortage as of June 13, including many essential medicines made by few companies.
Intas voluntarily shut down its Ahmedabad plant after the FDA inspection, and the agency posted its shocking inspection report in January. Accord Healthcare, the U.S. subsidiary of Intas, said in mid-June it had no date for restarting production.
Asked why it waited 2 months after its inspection to announce the cisplatin shortage, given that Intas supplied more than half the U.S. market for the drug, the FDA said via email that it doesn’t list a drug in shortage until it has “confirmed that overall market demand is not being met.”
Prices for carboplatin, cisplatin, and other drugs have skyrocketed on the so-called gray market, where speculators sell medicines they snapped up in anticipation of shortages. A 600-mg bottle of carboplatin, normally available for $30, was going for $185 in early May and $345 a week later, said Richard Scanlon, the pharmacist at dr. Moore’s clinic.
“It’s hard to have these conversations with patients – ‘I have your dose for this cycle, but not sure about next cycle,’” said Mark Einstein, MD, chair of the department of obstetrics, gynecology and reproductive health at New Jersey Medical School, Newark.
Should government step in?
Despite a drug shortage task force and numerous congressional hearings, progress has been slow at best. The 2020 CARES Act gave the FDA the power to require companies to have contingency plans enabling them to respond to shortages, but the agency has not yet implemented guidance to enforce the provisions.
As a result, neither Accord nor other cisplatin makers had a response plan in place when Intas’ plant was shut down, said Soumi Saha, senior vice president of government affairs for Premier, which arranges wholesale drug purchases for more than 4,400 hospitals and health systems.
Premier understood in December that the shutdown endangered the U.S. supply of cisplatin and carboplatin, but it also didn’t issue an immediate alarm. “It’s a fine balance,” she said. “You don’t want to create panic-buying or hoarding.”
More lasting solutions are under discussion. Mr. Sardella and others have proposed government subsidies to get U.S. generics plants running full time. Their capacity is now half-idle. If federal agencies like the Centers for Medicare & Medicaid Services paid more for more safely and efficiently produced drugs, it would promote a more stable supply chain, he said.
“At a certain point the system needs to recognize there’s a high cost to low-cost drugs,” said Allan Coukell, senior vice president for public policy at Civica Rx, a nonprofit funded by health systems, foundations, and the federal government that provides about 80 drugs to hospitals in its network. Civica is building a $140 million factory near Petersburg, Va., that will produce dozens more, Mr. Coukell said.
Dr. Ratain and his University of Chicago colleague Satyajit Kosuri, MD, recently called for the creation of a strategic inventory buffer for generic medications, something like the Strategic Petroleum Reserve, set up in 1975 in response to the OPEC oil crisis.
In fact, Dr. Ratain reckons, selling a quarter-million barrels of oil would probably generate enough cash to make and store 2 years’ worth of carboplatin and cisplatin.
“It would almost literally be a drop in the bucket.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – an independent source of health policy research, polling, and journalism. Learn more about KFF.
On Nov. 22, three Food and Drug Administration inspectors arrived at the sprawling Intas Pharmaceuticals plant south of Ahmedabad, India, and found hundreds of trash bags full of shredded documents tossed into a garbage truck. Over the next 10 days, the inspectors assessed what looked like a systematic effort to conceal quality problems at the plant, which provided more than half of the U.S. supply of generic cisplatin and carboplatin, two cheap drugs used to treat as many as 500,000 new cancer cases every year.
Their decisions are likely to result in preventable deaths.
Cisplatin and carboplatin are among scores of drugs in shortage, including 12 other cancer drugs, ADHD pills, blood thinners, and antibiotics. COVID-hangover supply chain issues and limited FDA oversight are part of the problem, but the main cause, experts agree, is the underlying weakness of the generic drug industry. Made mostly overseas, these old but crucial drugs are often sold at a loss or for little profit. Domestic manufacturers have little interest in making them, setting their sights instead on high-priced drugs with plump profit margins.
The problem isn’t new, and that’s particularly infuriating to many clinicians. President Joe Biden, whose son Beau died of an aggressive brain cancer, has focused his Cancer Moonshot on discovering cures – undoubtedly expensive ones. Indeed, existing brand-name cancer drugs often cost tens of thousands of dollars a year.
But what about the thousands of patients today who can’t get a drug like cisplatin, approved by the FDA in 1978 and costing as little as $6 a dose?
“It’s just insane,” said Mark Ratain, MD, a cancer doctor and pharmacologist at the University of Chicago. “Your roof is caving in, but you want to build a basketball court in the backyard because your wife is pregnant with twin boys and you want them to be NBA stars when they grow up?”
“It’s just a travesty that this is the level of health care in the United States of America right now,” said Stephen Divers, MD, an oncologist in Hot Springs, Ark., who in recent weeks has had to delay or change treatment for numerous bladder, breast, and ovarian cancer patients because his clinic cannot find enough cisplatin and carboplatin. Results from a survey of academic cancer centers released June 7 found 93% couldn’t find enough carboplatin and 70% had cisplatin shortages.
“All day, in between patients, we hold staff meetings trying to figure this out,” said Bonny Moore, MD, an oncologist in Fredericksburg, Virginia. “It’s the most nauseous I’ve ever felt. Our office stayed open during COVID; we never had to stop treating patients. We got them vaccinated, kept them safe, and now I can’t get them a $10 drug.”
The cancer clinicians KFF Health News interviewed for this story said that, given current shortages, they prioritize patients who can be cured over later-stage patients, in whom the drugs generally can only slow the disease, and for whom alternatives – though sometimes less effective and often with more side effects – are available. But some doctors are even rationing doses intended to cure.
Isabella McDonald, then a junior at Utah Valley University, was diagnosed in April with a rare, often fatal bone cancer, whose sole treatment for young adults includes the drug methotrexate. When Isabella’s second cycle of treatment began June 5, clinicians advised that she would be getting less than the full dose because of a methotrexate shortage, said her father, Brent.
“They don’t think it will have a negative impact on her treatment, but as far as I am aware, there isn’t any scientific basis to make that conclusion,” he said. “As you can imagine, when they gave us such low odds of her beating this cancer, it feels like we want to give it everything we can and not something short of the standard.”
Mr. McDonald stressed that he didn’t blame the staffers at Intermountain Health who take care of Isabella. The family – his other daughter, Cate, made a TikTok video about her sister’s plight – were simply stunned at such a basic flaw in the health care system.
At Dr. Moore’s practice, in Virginia, clinicians gave 60% of the optimal dose of carboplatin to some uterine cancer patients during the week of May 16, then shifted to 80% after a small shipment came in the following week. The doctors had to omit carboplatin from normal combination treatments for patients with recurrent disease, she said.
On June 2, Dr. Moore and colleagues were glued to their drug distributor’s website, anxious as teenagers waiting for Taylor Swift tickets to go on sale – only with mortal consequences at stake.
She later emailed KFF Health News: “Carboplatin did NOT come back in stock today. Neither did cisplatin.”
Doses remained at 80%, she said. Things hadn’t changed 10 days later.
Generics manufacturers are pulling out
The causes of shortages are well established. Everyone wants to pay less, and the middlemen who procure and distribute generics keep driving down wholesale prices. The average net price of generic drugs fell by more than half between 2016 and 2022, according to research by Anthony Sardella, a business professor at Washington University in St. Louis.
As generics manufacturers compete to win sales contracts with the big negotiators of such purchases, such as Vizient and Premier, their profits sink. Some are going out of business. Akorn, which made 75 common generics, went bankrupt and closed in February. Israeli generics giant Teva, which has a portfolio of 3,600 medicines, announced May 18 it was shifting to brand-name drugs and “high-value generics.” Lannett, with about 120 generics, announced a Chapter 11 reorganization amid declining revenue. Other companies are in trouble too, said David Gaugh, interim CEO of the Association for Accessible Medicines, the leading generics trade group.
The generics industry used to lose money on about a third of the drugs it produced, but now it’s more like half, Mr. Gaugh said. So when a company stops making a drug, others do not necessarily step up, he said. Officials at Fresenius Kabi and Pfizer said they have increased their carboplatin production since March, but not enough to end the shortage. On June 2, FDA Commissioner Robert Califf announced the agency had given emergency authorization for Chinese-made cisplatin to enter the U.S. market, but the impact of the move wasn’t immediately clear.
Cisplatin and carboplatin are made in special production lines under sterile conditions, and expanding or changing the lines requires FDA approval. Bargain-basement prices have pushed production overseas, where it’s harder for the FDA to track quality standards. The Intas plant inspection was a relative rarity in India, where the FDA in 2022 reportedly inspected only 3% of sites that make drugs for the U.S. market. Mr. Sardella testified in May that a quarter of all U.S. drug prescriptions are filled by companies that received FDA warning letters in the past 26 months. And pharmaceutical industry product recalls are at their highest level in 18 years, reflecting fragile supply conditions.
The FDA listed 137 drugs in shortage as of June 13, including many essential medicines made by few companies.
Intas voluntarily shut down its Ahmedabad plant after the FDA inspection, and the agency posted its shocking inspection report in January. Accord Healthcare, the U.S. subsidiary of Intas, said in mid-June it had no date for restarting production.
Asked why it waited 2 months after its inspection to announce the cisplatin shortage, given that Intas supplied more than half the U.S. market for the drug, the FDA said via email that it doesn’t list a drug in shortage until it has “confirmed that overall market demand is not being met.”
Prices for carboplatin, cisplatin, and other drugs have skyrocketed on the so-called gray market, where speculators sell medicines they snapped up in anticipation of shortages. A 600-mg bottle of carboplatin, normally available for $30, was going for $185 in early May and $345 a week later, said Richard Scanlon, the pharmacist at dr. Moore’s clinic.
“It’s hard to have these conversations with patients – ‘I have your dose for this cycle, but not sure about next cycle,’” said Mark Einstein, MD, chair of the department of obstetrics, gynecology and reproductive health at New Jersey Medical School, Newark.
Should government step in?
Despite a drug shortage task force and numerous congressional hearings, progress has been slow at best. The 2020 CARES Act gave the FDA the power to require companies to have contingency plans enabling them to respond to shortages, but the agency has not yet implemented guidance to enforce the provisions.
As a result, neither Accord nor other cisplatin makers had a response plan in place when Intas’ plant was shut down, said Soumi Saha, senior vice president of government affairs for Premier, which arranges wholesale drug purchases for more than 4,400 hospitals and health systems.
Premier understood in December that the shutdown endangered the U.S. supply of cisplatin and carboplatin, but it also didn’t issue an immediate alarm. “It’s a fine balance,” she said. “You don’t want to create panic-buying or hoarding.”
More lasting solutions are under discussion. Mr. Sardella and others have proposed government subsidies to get U.S. generics plants running full time. Their capacity is now half-idle. If federal agencies like the Centers for Medicare & Medicaid Services paid more for more safely and efficiently produced drugs, it would promote a more stable supply chain, he said.
“At a certain point the system needs to recognize there’s a high cost to low-cost drugs,” said Allan Coukell, senior vice president for public policy at Civica Rx, a nonprofit funded by health systems, foundations, and the federal government that provides about 80 drugs to hospitals in its network. Civica is building a $140 million factory near Petersburg, Va., that will produce dozens more, Mr. Coukell said.
Dr. Ratain and his University of Chicago colleague Satyajit Kosuri, MD, recently called for the creation of a strategic inventory buffer for generic medications, something like the Strategic Petroleum Reserve, set up in 1975 in response to the OPEC oil crisis.
In fact, Dr. Ratain reckons, selling a quarter-million barrels of oil would probably generate enough cash to make and store 2 years’ worth of carboplatin and cisplatin.
“It would almost literally be a drop in the bucket.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – an independent source of health policy research, polling, and journalism. Learn more about KFF.
Oral drug for brain tumor could change treatment landscape
say researchers reporting new results that could potentially change the treatment landscape.
The investigational drug vorasidenib (Servier) is awaiting approval for use in gliomas bearing mutations in IDH1 and IDH2.
Results from the pivotal phase 3 INDIGO trial show that the drug was associated with a significant delay in time to disease progression when compared with placebo.
The median progression-free survival (PFS) was 27.7 months for patients on vorasidenib, compared with 11.1 months for patients assigned to placebo (hazard ratio for progression or death with vorasidenib of 0.39 (P < .0001).
Vorasidenib was also associated with significantly longer time to the next treatment, and patients generally tolerated the drug well, reported first author Ingo K. Mellinghoff, MD, from Memorial Sloan Kettering Cancer Center, New York.
The results show that “treatment with an oral precision medicine therapy can produce a reduction in the risk of tumor progression by 61%, so that is, we think, a significant sign of efficacy that has potential to change the landscape in this disease,” he commented.
Dr. Mellinghoff spoke at a media briefing prior to presenting the data at a plenary session at the annual meeting of the American Society of Clinical Oncology.
The study was published online in the New England Journal of Medicine to coincide with the presentation.
“What you just heard is a trial that was well done and well thought out: to use an oral, targeted, well-tolerated therapy to see if we could delay the use of our standard chemotherapy and radiation,” commented ASCO expert Glenn Lesser, MD, from Wake Forest Baptist Health in Winston-Salem, N.C., the invited discussant at the briefing.
“The results are quite striking and they’re statistically highly significant, and more importantly, they’re clinically very, very significant,” he continued.
“The results of this study really suggest that, in selected patients with IDH-mutant low-grade gliomas, we can potentially delay the use of these toxic chemotherapies and radiation, maybe for years if not many years, and as a result delay the long-term toxicities of those therapies in a group of patients who typically are experiencing long-term survival,” Dr. Lesser added.
Brain-penetrating oral drug
Vorasidenib is an oral inhibitor of the IDH1 and IDH2 enzymes, with the ability to cross the blood-brain barrier. Mutations in IDH1 are found in about 80% of grade 2 gliomas, and IDH2 mutations occur in about 4%.
Adjuvant chemoradiotherapy has become the standard of care for patients with IDH-mutant grade 3 gliomas and patients with IDH-mutant grade 2 tumors who are thought to be a high risk for early progression.
Many patients with IDH-mutant grade 2 gliomas are initially followed with serial MRI scans, with toxic therapies reserved for use after disease progression, Dr. Mellinghoff noted.
Vorasidenib offers the potential for delaying the use of more toxic therapies and the potential to alter the natural history of diffuse glioma while helping patients to maintain a good quality of life, he said.
Study details
The INDIGO trial involved 331 patients with grade 2 gliomas with IDH mutations, who were enrolled across 77 centers in 10 countries in North America, Europe, and the Middle East.
Patients were aged 12-80 years and had residual or recurrent grade 2 IDH1- or IDH2-mutated oligodendroglioma or astrocytoma, with measurable nonenhancing disease and no prior treatment for glioma (with the most recent surgery 1-5 years before randomization). They were eligible for the study if they were not in immediate need of chemotherapy and/or radiation.
After stratification by 1p/19q status and baseline tumor size, they were randomly assigned to receive either vorasidenib 40 mg daily or placebo in 28-day cycles.
At the second planned interim analysis data cutoff in September 2022, at a median follow-up of 14.2 months, 226 (68.3%) of the 331 patients remained on treatment.
The primary endpoint was median PFS by blinded independent central review, which as noted above was 16.6 months longer in those on the drug, compared with placebo.
The time to next therapy was also significantly longer with vorasidenib, with a median not yet reached, compared with 17.4 months for placebo (hazard ratio, 0.26, P < .001).
Adverse events of any grade occurring in more than 20% of those receiving vorasidenib were elevated liver enzymes, fatigue, headache, diarrhea, and nausea. Grade 3 or 4 ALT elevations occurred in 9.6% of patients assigned to vorasidenib, but not in the placebo group.
Vorasidenib received fast-track status from the Food and Drug Administration in March. It is currently being studied in a phase 1 trial in combination with pembrolizumab (Keytruda) in patients with grade 2/3 gliomas, and further exploration of the drug in combination with other agents is being considered.
The study was funded by Servier Pharmaceuticals, manufacturer of vorasidenib. Dr. Mellinghoff disclosed honoraria from Roche, a consulting or advisory role with Agios, Black Diamond Therapeutics, Debiopharm Group, Puma Biotechnology, Voyager Therapeutics, research funding from Amgen, General Electric, Lilly, and travel expenses from Agios, AstraZeneca, Puma Biotechnology, Roche, and Voyager Therapeutics. Dr. Lesser disclosed honoraria from SDP Oncology, consulting/advising for Cancer Expert Now, Agio, IN8bio, and Ono Pharmaceutical.
A version of this article first appeared on Medscape.com.
say researchers reporting new results that could potentially change the treatment landscape.
The investigational drug vorasidenib (Servier) is awaiting approval for use in gliomas bearing mutations in IDH1 and IDH2.
Results from the pivotal phase 3 INDIGO trial show that the drug was associated with a significant delay in time to disease progression when compared with placebo.
The median progression-free survival (PFS) was 27.7 months for patients on vorasidenib, compared with 11.1 months for patients assigned to placebo (hazard ratio for progression or death with vorasidenib of 0.39 (P < .0001).
Vorasidenib was also associated with significantly longer time to the next treatment, and patients generally tolerated the drug well, reported first author Ingo K. Mellinghoff, MD, from Memorial Sloan Kettering Cancer Center, New York.
The results show that “treatment with an oral precision medicine therapy can produce a reduction in the risk of tumor progression by 61%, so that is, we think, a significant sign of efficacy that has potential to change the landscape in this disease,” he commented.
Dr. Mellinghoff spoke at a media briefing prior to presenting the data at a plenary session at the annual meeting of the American Society of Clinical Oncology.
The study was published online in the New England Journal of Medicine to coincide with the presentation.
“What you just heard is a trial that was well done and well thought out: to use an oral, targeted, well-tolerated therapy to see if we could delay the use of our standard chemotherapy and radiation,” commented ASCO expert Glenn Lesser, MD, from Wake Forest Baptist Health in Winston-Salem, N.C., the invited discussant at the briefing.
“The results are quite striking and they’re statistically highly significant, and more importantly, they’re clinically very, very significant,” he continued.
“The results of this study really suggest that, in selected patients with IDH-mutant low-grade gliomas, we can potentially delay the use of these toxic chemotherapies and radiation, maybe for years if not many years, and as a result delay the long-term toxicities of those therapies in a group of patients who typically are experiencing long-term survival,” Dr. Lesser added.
Brain-penetrating oral drug
Vorasidenib is an oral inhibitor of the IDH1 and IDH2 enzymes, with the ability to cross the blood-brain barrier. Mutations in IDH1 are found in about 80% of grade 2 gliomas, and IDH2 mutations occur in about 4%.
Adjuvant chemoradiotherapy has become the standard of care for patients with IDH-mutant grade 3 gliomas and patients with IDH-mutant grade 2 tumors who are thought to be a high risk for early progression.
Many patients with IDH-mutant grade 2 gliomas are initially followed with serial MRI scans, with toxic therapies reserved for use after disease progression, Dr. Mellinghoff noted.
Vorasidenib offers the potential for delaying the use of more toxic therapies and the potential to alter the natural history of diffuse glioma while helping patients to maintain a good quality of life, he said.
Study details
The INDIGO trial involved 331 patients with grade 2 gliomas with IDH mutations, who were enrolled across 77 centers in 10 countries in North America, Europe, and the Middle East.
Patients were aged 12-80 years and had residual or recurrent grade 2 IDH1- or IDH2-mutated oligodendroglioma or astrocytoma, with measurable nonenhancing disease and no prior treatment for glioma (with the most recent surgery 1-5 years before randomization). They were eligible for the study if they were not in immediate need of chemotherapy and/or radiation.
After stratification by 1p/19q status and baseline tumor size, they were randomly assigned to receive either vorasidenib 40 mg daily or placebo in 28-day cycles.
At the second planned interim analysis data cutoff in September 2022, at a median follow-up of 14.2 months, 226 (68.3%) of the 331 patients remained on treatment.
The primary endpoint was median PFS by blinded independent central review, which as noted above was 16.6 months longer in those on the drug, compared with placebo.
The time to next therapy was also significantly longer with vorasidenib, with a median not yet reached, compared with 17.4 months for placebo (hazard ratio, 0.26, P < .001).
Adverse events of any grade occurring in more than 20% of those receiving vorasidenib were elevated liver enzymes, fatigue, headache, diarrhea, and nausea. Grade 3 or 4 ALT elevations occurred in 9.6% of patients assigned to vorasidenib, but not in the placebo group.
Vorasidenib received fast-track status from the Food and Drug Administration in March. It is currently being studied in a phase 1 trial in combination with pembrolizumab (Keytruda) in patients with grade 2/3 gliomas, and further exploration of the drug in combination with other agents is being considered.
The study was funded by Servier Pharmaceuticals, manufacturer of vorasidenib. Dr. Mellinghoff disclosed honoraria from Roche, a consulting or advisory role with Agios, Black Diamond Therapeutics, Debiopharm Group, Puma Biotechnology, Voyager Therapeutics, research funding from Amgen, General Electric, Lilly, and travel expenses from Agios, AstraZeneca, Puma Biotechnology, Roche, and Voyager Therapeutics. Dr. Lesser disclosed honoraria from SDP Oncology, consulting/advising for Cancer Expert Now, Agio, IN8bio, and Ono Pharmaceutical.
A version of this article first appeared on Medscape.com.
say researchers reporting new results that could potentially change the treatment landscape.
The investigational drug vorasidenib (Servier) is awaiting approval for use in gliomas bearing mutations in IDH1 and IDH2.
Results from the pivotal phase 3 INDIGO trial show that the drug was associated with a significant delay in time to disease progression when compared with placebo.
The median progression-free survival (PFS) was 27.7 months for patients on vorasidenib, compared with 11.1 months for patients assigned to placebo (hazard ratio for progression or death with vorasidenib of 0.39 (P < .0001).
Vorasidenib was also associated with significantly longer time to the next treatment, and patients generally tolerated the drug well, reported first author Ingo K. Mellinghoff, MD, from Memorial Sloan Kettering Cancer Center, New York.
The results show that “treatment with an oral precision medicine therapy can produce a reduction in the risk of tumor progression by 61%, so that is, we think, a significant sign of efficacy that has potential to change the landscape in this disease,” he commented.
Dr. Mellinghoff spoke at a media briefing prior to presenting the data at a plenary session at the annual meeting of the American Society of Clinical Oncology.
The study was published online in the New England Journal of Medicine to coincide with the presentation.
“What you just heard is a trial that was well done and well thought out: to use an oral, targeted, well-tolerated therapy to see if we could delay the use of our standard chemotherapy and radiation,” commented ASCO expert Glenn Lesser, MD, from Wake Forest Baptist Health in Winston-Salem, N.C., the invited discussant at the briefing.
“The results are quite striking and they’re statistically highly significant, and more importantly, they’re clinically very, very significant,” he continued.
“The results of this study really suggest that, in selected patients with IDH-mutant low-grade gliomas, we can potentially delay the use of these toxic chemotherapies and radiation, maybe for years if not many years, and as a result delay the long-term toxicities of those therapies in a group of patients who typically are experiencing long-term survival,” Dr. Lesser added.
Brain-penetrating oral drug
Vorasidenib is an oral inhibitor of the IDH1 and IDH2 enzymes, with the ability to cross the blood-brain barrier. Mutations in IDH1 are found in about 80% of grade 2 gliomas, and IDH2 mutations occur in about 4%.
Adjuvant chemoradiotherapy has become the standard of care for patients with IDH-mutant grade 3 gliomas and patients with IDH-mutant grade 2 tumors who are thought to be a high risk for early progression.
Many patients with IDH-mutant grade 2 gliomas are initially followed with serial MRI scans, with toxic therapies reserved for use after disease progression, Dr. Mellinghoff noted.
Vorasidenib offers the potential for delaying the use of more toxic therapies and the potential to alter the natural history of diffuse glioma while helping patients to maintain a good quality of life, he said.
Study details
The INDIGO trial involved 331 patients with grade 2 gliomas with IDH mutations, who were enrolled across 77 centers in 10 countries in North America, Europe, and the Middle East.
Patients were aged 12-80 years and had residual or recurrent grade 2 IDH1- or IDH2-mutated oligodendroglioma or astrocytoma, with measurable nonenhancing disease and no prior treatment for glioma (with the most recent surgery 1-5 years before randomization). They were eligible for the study if they were not in immediate need of chemotherapy and/or radiation.
After stratification by 1p/19q status and baseline tumor size, they were randomly assigned to receive either vorasidenib 40 mg daily or placebo in 28-day cycles.
At the second planned interim analysis data cutoff in September 2022, at a median follow-up of 14.2 months, 226 (68.3%) of the 331 patients remained on treatment.
The primary endpoint was median PFS by blinded independent central review, which as noted above was 16.6 months longer in those on the drug, compared with placebo.
The time to next therapy was also significantly longer with vorasidenib, with a median not yet reached, compared with 17.4 months for placebo (hazard ratio, 0.26, P < .001).
Adverse events of any grade occurring in more than 20% of those receiving vorasidenib were elevated liver enzymes, fatigue, headache, diarrhea, and nausea. Grade 3 or 4 ALT elevations occurred in 9.6% of patients assigned to vorasidenib, but not in the placebo group.
Vorasidenib received fast-track status from the Food and Drug Administration in March. It is currently being studied in a phase 1 trial in combination with pembrolizumab (Keytruda) in patients with grade 2/3 gliomas, and further exploration of the drug in combination with other agents is being considered.
The study was funded by Servier Pharmaceuticals, manufacturer of vorasidenib. Dr. Mellinghoff disclosed honoraria from Roche, a consulting or advisory role with Agios, Black Diamond Therapeutics, Debiopharm Group, Puma Biotechnology, Voyager Therapeutics, research funding from Amgen, General Electric, Lilly, and travel expenses from Agios, AstraZeneca, Puma Biotechnology, Roche, and Voyager Therapeutics. Dr. Lesser disclosed honoraria from SDP Oncology, consulting/advising for Cancer Expert Now, Agio, IN8bio, and Ono Pharmaceutical.
A version of this article first appeared on Medscape.com.
AT ASCO 2023
Number of cancer survivors with functional limitations doubled in 20 years
Vishal Patel, BS, a student at the Dell Medical School at The University of Texas at Austin, and colleagues identified 51,258 cancer survivors from the National Health Interview Survey, representing a weighted population of approximately 178.8 million from 1999 to 2018.
Most survivors were women (60.2%) and were at least 65 years old (55.4%). In 1999, 3.6 million weighted survivors reported functional limitation. In 2018, the number increased to 8.2 million, a 2.25-fold increase.
The number of survivors who reported no limitations also increased, but not by as much. That group grew 1.34-fold during the study period.
For context, “the 70% prevalence of functional limitation among survivors in 2018 is nearly twice that of the general population,” the authors wrote.
Patients surveyed on function
Functional limitation was defined as “self-reported difficulty performing any of 12 routine physical or social activities without assistance.” Examples of the activities included difficulty sitting for more than 2 hours, difficulty participating in social activities or difficulty pushing or pulling an object the size of a living room chair.
Over the 2 decades analyzed, the adjusted prevalence of functional limitation was highest among survivors of pancreatic cancer (80.3%) and lung cancer (76.5%). Prevalence was lowest for survivors of melanoma (62.2%), breast (61.8%) and prostate (59.5%) cancers.
Not just a result of living longer
Mr. Patel told this publication that one assumption people might make when they read these results is that people are just living longer with cancer and losing functional ability accordingly.
“But, in fact, we found that the youngest [– those less than 65 years–] actually contributed to this trend more than the oldest people, which means it’s not just [happening], because people are getting older,” he said.
Hispanic and Black individuals had disproportionately higher increases in functional limitation; percentage point increases over the 2 decades were 19.5 for Black people, 25.1 for Hispanic people and 12.5 for White people. There may be a couple of reasons for that, Mr. Patel noted.
Those who are Black or Hispanic tend to have less access to cancer survivorship care for reasons including insurance status and historic health care inequities, he noted.
“The other potential reason is that they have had less access to cancer care historically. And if, 20 years ago Black and Hispanic individuals didn’t have access to some chemotherapies, and now they do, maybe it’s the increased access to care that’s causing these functional limitations. Because chemotherapy can sometimes be very toxic. It may be sort of a catch-up toxicity,” he said.
Quality of life beyond survivorship
Mr. Patel said the results seem to call for building on improved survival rates by tracking and improving function.
“It’s good to celebrate that there are more survivors. But now that we can keep people alive longer, maybe we can shift gears to improving their quality of life,” he said.
The more-than-doubling of functional limitations over 2 decades “is a very sobering trend,” he noted, while pointing out that the functional limitations applied to 8 million people in the United States – people whose needs are not being met.
There’s no sign of the trend stopping, he continued. “We saw no downward trend, only an upward trend.”
Increasingly, including functionality as an endpoint in cancer trials, in addition to improvements in mortality, is one place to start, he added.
“Our findings suggest an urgent need for care teams to understand and address function, for researchers to evaluate function as a core outcome in trials, and for health systems and policy makers to reimagine survivorship care, recognizing the burden of cancer and its treatment on physical, psychosocial, and cognitive function,” the authors wrote in their paper. Limitations of the study include the potential for recall bias, lack of cancer staging or treatment information, and the subjective perception of function.
A coauthor reported personal fees from Astellas, AstraZeneca, AAA, Blue Earth, Janssen, Lantheus, Myovant, Myriad Genetics, Novartis, Telix, and Sanofi, as well as grants from Pfizer and Bayer during the conduct of the study. No other disclosures were reported.
Vishal Patel, BS, a student at the Dell Medical School at The University of Texas at Austin, and colleagues identified 51,258 cancer survivors from the National Health Interview Survey, representing a weighted population of approximately 178.8 million from 1999 to 2018.
Most survivors were women (60.2%) and were at least 65 years old (55.4%). In 1999, 3.6 million weighted survivors reported functional limitation. In 2018, the number increased to 8.2 million, a 2.25-fold increase.
The number of survivors who reported no limitations also increased, but not by as much. That group grew 1.34-fold during the study period.
For context, “the 70% prevalence of functional limitation among survivors in 2018 is nearly twice that of the general population,” the authors wrote.
Patients surveyed on function
Functional limitation was defined as “self-reported difficulty performing any of 12 routine physical or social activities without assistance.” Examples of the activities included difficulty sitting for more than 2 hours, difficulty participating in social activities or difficulty pushing or pulling an object the size of a living room chair.
Over the 2 decades analyzed, the adjusted prevalence of functional limitation was highest among survivors of pancreatic cancer (80.3%) and lung cancer (76.5%). Prevalence was lowest for survivors of melanoma (62.2%), breast (61.8%) and prostate (59.5%) cancers.
Not just a result of living longer
Mr. Patel told this publication that one assumption people might make when they read these results is that people are just living longer with cancer and losing functional ability accordingly.
“But, in fact, we found that the youngest [– those less than 65 years–] actually contributed to this trend more than the oldest people, which means it’s not just [happening], because people are getting older,” he said.
Hispanic and Black individuals had disproportionately higher increases in functional limitation; percentage point increases over the 2 decades were 19.5 for Black people, 25.1 for Hispanic people and 12.5 for White people. There may be a couple of reasons for that, Mr. Patel noted.
Those who are Black or Hispanic tend to have less access to cancer survivorship care for reasons including insurance status and historic health care inequities, he noted.
“The other potential reason is that they have had less access to cancer care historically. And if, 20 years ago Black and Hispanic individuals didn’t have access to some chemotherapies, and now they do, maybe it’s the increased access to care that’s causing these functional limitations. Because chemotherapy can sometimes be very toxic. It may be sort of a catch-up toxicity,” he said.
Quality of life beyond survivorship
Mr. Patel said the results seem to call for building on improved survival rates by tracking and improving function.
“It’s good to celebrate that there are more survivors. But now that we can keep people alive longer, maybe we can shift gears to improving their quality of life,” he said.
The more-than-doubling of functional limitations over 2 decades “is a very sobering trend,” he noted, while pointing out that the functional limitations applied to 8 million people in the United States – people whose needs are not being met.
There’s no sign of the trend stopping, he continued. “We saw no downward trend, only an upward trend.”
Increasingly, including functionality as an endpoint in cancer trials, in addition to improvements in mortality, is one place to start, he added.
“Our findings suggest an urgent need for care teams to understand and address function, for researchers to evaluate function as a core outcome in trials, and for health systems and policy makers to reimagine survivorship care, recognizing the burden of cancer and its treatment on physical, psychosocial, and cognitive function,” the authors wrote in their paper. Limitations of the study include the potential for recall bias, lack of cancer staging or treatment information, and the subjective perception of function.
A coauthor reported personal fees from Astellas, AstraZeneca, AAA, Blue Earth, Janssen, Lantheus, Myovant, Myriad Genetics, Novartis, Telix, and Sanofi, as well as grants from Pfizer and Bayer during the conduct of the study. No other disclosures were reported.
Vishal Patel, BS, a student at the Dell Medical School at The University of Texas at Austin, and colleagues identified 51,258 cancer survivors from the National Health Interview Survey, representing a weighted population of approximately 178.8 million from 1999 to 2018.
Most survivors were women (60.2%) and were at least 65 years old (55.4%). In 1999, 3.6 million weighted survivors reported functional limitation. In 2018, the number increased to 8.2 million, a 2.25-fold increase.
The number of survivors who reported no limitations also increased, but not by as much. That group grew 1.34-fold during the study period.
For context, “the 70% prevalence of functional limitation among survivors in 2018 is nearly twice that of the general population,” the authors wrote.
Patients surveyed on function
Functional limitation was defined as “self-reported difficulty performing any of 12 routine physical or social activities without assistance.” Examples of the activities included difficulty sitting for more than 2 hours, difficulty participating in social activities or difficulty pushing or pulling an object the size of a living room chair.
Over the 2 decades analyzed, the adjusted prevalence of functional limitation was highest among survivors of pancreatic cancer (80.3%) and lung cancer (76.5%). Prevalence was lowest for survivors of melanoma (62.2%), breast (61.8%) and prostate (59.5%) cancers.
Not just a result of living longer
Mr. Patel told this publication that one assumption people might make when they read these results is that people are just living longer with cancer and losing functional ability accordingly.
“But, in fact, we found that the youngest [– those less than 65 years–] actually contributed to this trend more than the oldest people, which means it’s not just [happening], because people are getting older,” he said.
Hispanic and Black individuals had disproportionately higher increases in functional limitation; percentage point increases over the 2 decades were 19.5 for Black people, 25.1 for Hispanic people and 12.5 for White people. There may be a couple of reasons for that, Mr. Patel noted.
Those who are Black or Hispanic tend to have less access to cancer survivorship care for reasons including insurance status and historic health care inequities, he noted.
“The other potential reason is that they have had less access to cancer care historically. And if, 20 years ago Black and Hispanic individuals didn’t have access to some chemotherapies, and now they do, maybe it’s the increased access to care that’s causing these functional limitations. Because chemotherapy can sometimes be very toxic. It may be sort of a catch-up toxicity,” he said.
Quality of life beyond survivorship
Mr. Patel said the results seem to call for building on improved survival rates by tracking and improving function.
“It’s good to celebrate that there are more survivors. But now that we can keep people alive longer, maybe we can shift gears to improving their quality of life,” he said.
The more-than-doubling of functional limitations over 2 decades “is a very sobering trend,” he noted, while pointing out that the functional limitations applied to 8 million people in the United States – people whose needs are not being met.
There’s no sign of the trend stopping, he continued. “We saw no downward trend, only an upward trend.”
Increasingly, including functionality as an endpoint in cancer trials, in addition to improvements in mortality, is one place to start, he added.
“Our findings suggest an urgent need for care teams to understand and address function, for researchers to evaluate function as a core outcome in trials, and for health systems and policy makers to reimagine survivorship care, recognizing the burden of cancer and its treatment on physical, psychosocial, and cognitive function,” the authors wrote in their paper. Limitations of the study include the potential for recall bias, lack of cancer staging or treatment information, and the subjective perception of function.
A coauthor reported personal fees from Astellas, AstraZeneca, AAA, Blue Earth, Janssen, Lantheus, Myovant, Myriad Genetics, Novartis, Telix, and Sanofi, as well as grants from Pfizer and Bayer during the conduct of the study. No other disclosures were reported.
FROM JAMA ONCOLOGY