User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Hospital Dermatology: Review of Research in 2023-2024
Inpatient consultative dermatology has advanced as a subspecialty and increasingly gained recognition in recent years. Since its founding in 2009, the Society of Dermatology Hospitalists has fostered research and education in hospital dermatology. Last year, we reviewed the 2022-2023 literature with a focus on developments in severe cutaneous adverse reactions, supportive oncodermatology, cost of inpatient services, and teledermatology.1 In this review, we highlight 3 areas of interest from the 2023-2024 literature: severe cutaneous adverse drug reactions, skin and soft tissue infections, and autoimmune blistering diseases (AIBDs).
Severe Cutaneous Adverse Drug Reactions
Adverse drug reactions are among the most common diagnoses encountered by inpatient dermatology consultants.2,3 Severe cutaneous adverse drug reactions are associated with substantial morbidity and mortality. Efforts to characterize these conditions and standardize their diagnosis and management continue to be a major focus of ongoing research.
A single-center retrospective analysis of 102 cases of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome evaluated differences in clinical manifestations depending on the culprit drug, offering insights into the heterogeneity of DRESS syndrome and the potential for diagnostic uncertainty.4 The shortest median latency was observed in a case caused by penicillin and cephalosporins (12 and 18 days, respectively), while DRESS syndrome secondary to allopurinol had the longest median latency (36 days). Nonsteroidal anti-inflammatory drug–induced DRESS syndrome was associated with the shortest hospital stay (6.5 days), while cephalosporin and vancomycin cases had the highest mortality rates.4
In the first international Delphi consensus study on the diagnostic workup, severity assessment, and management of DRESS syndrome, 54 dermatology and/or allergy experts reached consensus on 93 statements.5 Specific recommendations included basic evaluation with complete blood count with differential, kidney and liver function parameters, and electrocardiogram for all patients with suspected DRESS syndrome, with additional complementary workup considered in patients with evidence of specific organ damage and/or severe disease. In the proposed DRESS syndrome severity grading scheme, laboratory values that reached consensus for inclusion were hemoglobin, neutrophil, and platelet counts and creatinine, transaminases, and alkaline phosphatase levels. Although treatment of DRESS syndrome should be based on assessed disease severity, treatment with corticosteroids should be initiated in all patients with confirmed DRESS syndrome. Cyclosporine, antibodies interfering with the IL-5 axis, and intravenous immunoglobulins can be considered in patients with corticosteroid-refractory DRESS syndrome, and antiviral treatment can be considered in patients with a high serum cytomegalovirus viral load. Regularly following up with laboratory evaluation of involved organs; screening for autoantibodies, thyroid dysfunction, and steroid adverse effects; and offering of psychological support also were consensus recommendations.5
Identifying causative agents in drug hypersensitivity reactions remains challenging. A retrospective cohort study of 48 patients with Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN) highlighted the need for a systematic unbiased approach to identifying culprit drugs. Using the RegiSCAR database and algorithm for drug causality for epidermal necrolysis to analyze the cohort, more than half of causative agents were determined to be different from those initially identified by the treating physicians. Nine additional suspected culprit drugs were identified, while 43 drugs initially identified as allergens were exonerated.6
Etiology-associated definitions for blistering reactions in children have been proposed to replace the existing terms Stevens-Johnson syndrome, toxic epidermal necrolysis, and others.7 Investigators in a recent study reclassified cases of SJS and TEN as reactive infectious mucocutaneous eruption (RIME) or drug-induced epidermal necrolysis (DEN), respectively. In RIME cases, Mycoplasma pneumoniae was the most commonly identified trigger, and in DEN cases, anticonvulsants were the most common class of culprit medications. Cases of RIME were less severe and were most often treated with antibiotics, whereas patients with DEN were more likely to receive supportive care, corticosteroids, intravenous immunoglobulins, and other immunosuppressive therapies.7
In addition to causing acute devastating mucocutaneous complications, SJS and TEN have long-lasting effects that require ongoing care. In a cohort of 6552 incident SJS/TEN cases over an 11-year period, survivors of SJS/TEN endured a mean loss of 9.4 years in life expectancy and excess health care expenditures of $3752 per year compared with age- and sex-matched controls. Patients with more severe disease, comorbid malignancy, diabetes, end-stage renal disease, or SJS/TEN sequelae experienced greater loss in life expectancy and lifetime health care expenditures.8 Separately, a qualitative study investigating the psychological impact of SJS/TEN in pediatric patients described sequelae including night terrors, posttraumatic stress disorder, depression, and anxiety for many years after the acute phase. Many patients reported a desire for increased support for their physical and emotional needs following hospital discharge.9
Skin and Soft Tissue Infections: Diagnosis, Management, and Prevention
Dermatology consultation has been shown to be a cost-effective intervention to improve outcomes in hospitalized patients with skin and soft tissue infections.10,11 In particular, cellulitis frequently is misdiagnosed, leading to unnecessary antibiotic use, hospitalizations, and major health care expenditures.12 Recognizing this challenge, researchers have worked to develop objective tools to improve diagnostic accuracy. In a large prospective prognostic validation study, Pulia et al13 found that thermal imaging alone or in combination with the ALT-70 prediction model (asymmetry, leukocytosis, tachycardia, and age ≥70 years) could be used successfully to reduce overdiagnosis of cellulitis. Both thermal imaging and the ALT-70 prediction model demonstrated robust sensitivity (93.5% and 98.8%, respectively) but low specificity (38.4% and 22.0%, respectively, and 53.9% when combined).13
In a systematic review, Kovacs et al14 analyzed case reports of pseudocellulitis caused by chemotherapeutic medications. Of the 81 cases selected, 58 (71.6%) were associated with gemcitabine, with the remaining 23 (28.4%) attributed to pemetrexed. Within this group, two-thirds of the patients received antibiotic treatment prior to receiving the correct diagnosis, and 36% experienced interruptions to their oncologic therapies. In contrast to infectious cellulitis, which tends to be unilateral and associated with elevated erythrocyte sedimentation rate or C-reactive protein, most chemotherapy-induced pseudocellulitis cases occurred bilaterally on the lower extremities, while erythrocyte sedimentation rate and C-reactive protein seldom were elevated.14
Necrotizing soft tissue infections (NSTIs) are severe life-threatening conditions characterized by widespread tissue destruction, signs of systemic toxicity, hemodynamic collapse, organ failure, and high mortality. Surgical inspection along with intraoperative tissue culture is the gold standard for diagnosis. Early detection, prompt surgical intervention, and appropriate antibiotic treatment are essential to reduce mortality and improve outcomes.15 A retrospective study of patients with surgically confirmed NSTIs assessed the incidence and risk factors for recurrence within 1 year following an initial NSTI of the lower extremity. Among 93 included patients, 32 (34.4%) had recurrence within 1 year, and more than half of recurrences occurred in the first 3 months (median, 66 days). The comparison of patients with and without recurrence showed similar proportions of antibiotic prophylaxis use after the first NSTI. There was significantly less compression therapy use (33.3% vs 62.3%; P=.13) and more negative pressure wound therapy use (83.3% vs 63.3%; P=.03) in the recurrence group, though the authors acknowledged that factors such as severity of pain and size of soft tissue defect may have affected the decisions for compression and negative pressure wound therapy.16
Residents of nursing homes are a particularly vulnerable population at high risk for health care–associated infections due to older age and a higher likelihood of having wounds, indwelling medical devices, and/or coexisting conditions.17 One cluster-randomized trial compared universal decolonization with routine-care bathing practices in nursing homes (N=28,956 residents). Decolonization entailed the use of chlorhexidine for all routine bathing and showering and administration of nasal povidone-iodine twice daily for the first 5 days after admission and then twice daily for 5 days every other week. Transfer to a hospital due to infection decreased from 62.9% to 52.2% with decolonization, for a difference in risk ratio of 16.6% (P<.001) compared with routine care. Additionally, the difference in risk ratio of the secondary end point (transfer to a hospital for any reason) was 14.6%. The number needed to treat was 9.7 to prevent 1 infection-related hospitalization and 8.9 to prevent 1 hospitalization for any reason.17
Autoimmune Blistering Diseases
Although rare, AIBDs are potentially life-threatening cutaneous diseases that often require inpatient management. While corticosteroids remain the mainstay of initial AIBD management, rituximab is now well recognized as the steroid-sparing treatment of choice for patients with moderate to severe pemphigus. In a long-term follow-up study of Ritux 318—the trial that led to the US Food and Drug Administration approval of rituximab in the treatment of moderate to severe pemphigus vulgaris—researchers assessed the long-term efficacy and safety of rituximab as a first-line treatment in patients with pemphigus.19 The 5- and 7-year disease-free survival rates without corticosteroid therapy for patients treated with rituximab were 76.7% and 72.1%, respectively, compared with 35.3% and 35.3% in those treated with prednisone alone (P<.001). Fewer serious adverse events were reported in those treated with rituximab plus prednisone compared with those treated with prednisone alone. None of the patients who maintained complete remission off corticosteroid therapy received any additional maintenance infusions of rituximab after the end of the Ritux 3 regimen (1 g of rituximab at day 0 and day 14, then 500 mg at months 12 and 18).19
By contrast, treatment of severe bullous pemphigoid (BP) often is less clear-cut, as no single therapeutic option has been shown to be superior to other immunomodulatory and immunosuppressive regimens, and the medical comorbidities of elderly patients with BP can be limiting. Fortunately, newer therapies with favorable safety profiles have emerged in recent years. In a multicenter retrospective study, 100 patients with BP received omalizumab after previously failing to respond to at least one alternative therapy. Disease control was obtained after a median of 10 days, and complete remission was achieved in 77% of patients in a median time of 3 months.20 In a multicenter retrospective cohort study of 146 patients with BP treated with dupilumab following the atopic dermatitis dosing schedule (one 600-mg dose followed by 300 mg every 2 weeks), disease control was achieved in a median of 14 days, while complete remission was achieved in 35.6% of patients, with 8.9% relapsing during the observation period.21 A retrospective case series of 30 patients with BP treated with dupilumab with maintenance dosing frequency tailored to individual patient response showed complete remission or marked response in 76.7% (23/30) of patients.22 A phase 2/3 randomized controlled trial of dupilumab in BP is currently ongoing (ClinicalTrials.gov identifier NCT04206553).
Pemphigoid gestationis is a rare autoimmune subepidermal bullous dermatosis of pregnancy that may be difficult to distinguish clinically from polymorphic eruption of pregnancy but confers notably different maternal and fetal risks. Researchers developed and validated a scoring system using clinical factors—history of pemphigoid gestationis, primigravidae, timing of rash onset, and specific clinical examination findings—that was able to differentiate between the 2 diseases with 79% sensitivity, 95% specificity, and an area under the curve of 0.93 without the need for advanced immunologic testing.23
Final Thoughts
Highlights of the literature from 2023-2024 demonstrate advancements in hospital-based dermatology as well as ongoing challenges. This year’s review emphasizes key developments in severe cutaneous adverse drug reactions, skin and soft tissue infections, and AIBDs. Continued expansion of knowledge in these areas and others informs patient care and demonstrates the value of dermatologic expertise in the inpatient setting.
- Berk-Krauss J, Micheletti RG. Hospital dermatology: review of research in 2022-2023. Cutis. 2023;112:236-239.
- Falanga V, Schachner LA, Rae V, et al. Dermatologic consultations in the hospital setting. Arch Dermatol. 1994;130:1022-1025.
- Kroshinsky D, Cotliar J, Hughey LC, et al. Association of dermatology consultation with accuracy of cutaneous disorder diagnoses in hospitalized patients: a multicenter analysis. JAMA Dermatol. 2016;152:477-480.
- Blumenthal KG, Alvarez-Arango S, Kroshinsky D, et al. Drug reaction eosinophilia and systemic symptoms: clinical phenotypic patterns according to causative drug. J Am Acad Dermatol. 2024;90:1240-1242.
- Brüggen MC, Walsh S, Ameri MM, et al. Management of adult patients with drug reaction with eosinophilia and systemic symptoms: a Delphi-based international consensus. JAMA Dermatol. 2024;160:37-44.
- Li DJ, Velasquez GA, Romar GA, et al. Assessment of need for improved identification of a culprit drug in Stevens-Johnson syndrome/toxic epidermal necrolysis. JAMA Dermatol. 2023;159:830-836.
- Martinez-Cabriales S, Coulombe J, Aaron M, et al. Preliminary summary and reclassification of cases from the Pediatric Research of Management in Stevens-Johnson syndrome and Epidermonecrolysis (PROMISE) study: a North American, multisite retrospective cohort. J Am Acad Dermatol. 2024;90:635-637.
- Chiu YM, Chiu HY. Lifetime risk, life expectancy, loss-of-life expectancy and lifetime healthcare expenditure for Stevens-Johnson syndrome/toxic epidermal necrolysis in Taiwan: follow-up of a nationwide cohort from 2008 to 2019. Br J Dermatol. 2023;189:553-560.
- Phillips C, Russell E, McNiven A, et al. A qualitative study of psychological morbidity in paediatric survivors of Stevens-Johnson syndrome/toxic epidermal necrolysis. Br J Dermatol. 2024;191:293-295.
- Li DG, Xia FD, Khosravi H, et al. Outcomes of early dermatology consultation for inpatients diagnosed with cellulitis. JAMA Dermatol. 2018;154:537-543.
- Milani-Nejad N, Zhang M, Kaffenberger BH. Association of dermatology consultations with patient care outcomes in hospitalized patients with inflammatory skin diseases. JAMA Dermatol. 2017;153:523-528.
- Weng QY, Raff AB, Cohen JM, et al. Costs and consequences associated with misdiagnosed lower extremity cellulitis. JAMA Dermatol. 2017;153:141-146.
- Pulia MS, Schwei RJ, Alexandridis R, et al. Validation of thermal imaging and the ALT-70 prediction model to differentiate cellulitis from pseudocellulitis. JAMA Dermatol. 2024;160:511-517.
- Kovacs LD, O’Donoghue M, Cogen AL. Chemotherapy-induced pseudocellulitis without prior radiation exposure: a systematic review. JAMA Dermatol. 2023;159:870-874.
- Yildiz H, Yombi JC. Necrotizing soft-tissue infections. comment. N Engl J Med. 2018;378:970.
- Traineau H, Charpentier C, Lepeule R, et al. First-year recurrence rate of skin and soft tissue infections following an initial necrotizing soft tissue infection of the lower extremities: a retrospective cohort study of 93 patients. J Am Acad Dermatol. 2023;88:1360-1363.
- Miller LG, McKinnell JA, Singh RD, et al. Decolonization in nursing homes to prevent infection and hospitalization. N Engl J Med. 2023;389:1766-1777.
- Joly P, Maho-Vaillant M, Prost-Squarcioni C, et al; French Study Group on Autoimmune Bullous Skin Diseases. First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): a prospective, multicentre, parallel-group, open-label randomised trial. Lancet. 2017;389:2031-2040.
- Tedbirt B, Maho-Vaillant M, Houivet E, et al; French Reference Center for Autoimmune Blistering Diseases MALIBUL. Sustained remission without corticosteroids among patients with pemphigus who had rituximab as first-line therapy: follow-up of the Ritux 3 Trial. JAMA Dermatol. 2024;160:290-296.
- Chebani R, Lombart F, Chaby G, et al; French Study Group on Autoimmune Bullous Diseases. Omalizumab in the treatment of bullous pemphigoid resistant to first-line therapy: a French national multicentre retrospective study of 100 patients. Br J Dermatol. 2024;190:258-265.
- Zhao L, Wang Q, Liang G, et al. Evaluation of dupilumab in patients with bullous pemphigoid. JAMA Dermatol. 2023;159:953-960.
- Miller AC, Temiz LA, Adjei S, et al. Treatment of bullous pemphigoid with dupilumab: a case series of 30 patients. J Drugs Dermatol. 2024;23:E144-E148.
- Xie F, Davis DMR, Baban F, et al. Development and multicenter international validation of a diagnostic tool to differentiate between pemphigoid gestationis and polymorphic eruption of pregnancy. J Am Acad Dermatol. 2023;89:106-113.
Inpatient consultative dermatology has advanced as a subspecialty and increasingly gained recognition in recent years. Since its founding in 2009, the Society of Dermatology Hospitalists has fostered research and education in hospital dermatology. Last year, we reviewed the 2022-2023 literature with a focus on developments in severe cutaneous adverse reactions, supportive oncodermatology, cost of inpatient services, and teledermatology.1 In this review, we highlight 3 areas of interest from the 2023-2024 literature: severe cutaneous adverse drug reactions, skin and soft tissue infections, and autoimmune blistering diseases (AIBDs).
Severe Cutaneous Adverse Drug Reactions
Adverse drug reactions are among the most common diagnoses encountered by inpatient dermatology consultants.2,3 Severe cutaneous adverse drug reactions are associated with substantial morbidity and mortality. Efforts to characterize these conditions and standardize their diagnosis and management continue to be a major focus of ongoing research.
A single-center retrospective analysis of 102 cases of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome evaluated differences in clinical manifestations depending on the culprit drug, offering insights into the heterogeneity of DRESS syndrome and the potential for diagnostic uncertainty.4 The shortest median latency was observed in a case caused by penicillin and cephalosporins (12 and 18 days, respectively), while DRESS syndrome secondary to allopurinol had the longest median latency (36 days). Nonsteroidal anti-inflammatory drug–induced DRESS syndrome was associated with the shortest hospital stay (6.5 days), while cephalosporin and vancomycin cases had the highest mortality rates.4
In the first international Delphi consensus study on the diagnostic workup, severity assessment, and management of DRESS syndrome, 54 dermatology and/or allergy experts reached consensus on 93 statements.5 Specific recommendations included basic evaluation with complete blood count with differential, kidney and liver function parameters, and electrocardiogram for all patients with suspected DRESS syndrome, with additional complementary workup considered in patients with evidence of specific organ damage and/or severe disease. In the proposed DRESS syndrome severity grading scheme, laboratory values that reached consensus for inclusion were hemoglobin, neutrophil, and platelet counts and creatinine, transaminases, and alkaline phosphatase levels. Although treatment of DRESS syndrome should be based on assessed disease severity, treatment with corticosteroids should be initiated in all patients with confirmed DRESS syndrome. Cyclosporine, antibodies interfering with the IL-5 axis, and intravenous immunoglobulins can be considered in patients with corticosteroid-refractory DRESS syndrome, and antiviral treatment can be considered in patients with a high serum cytomegalovirus viral load. Regularly following up with laboratory evaluation of involved organs; screening for autoantibodies, thyroid dysfunction, and steroid adverse effects; and offering of psychological support also were consensus recommendations.5
Identifying causative agents in drug hypersensitivity reactions remains challenging. A retrospective cohort study of 48 patients with Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN) highlighted the need for a systematic unbiased approach to identifying culprit drugs. Using the RegiSCAR database and algorithm for drug causality for epidermal necrolysis to analyze the cohort, more than half of causative agents were determined to be different from those initially identified by the treating physicians. Nine additional suspected culprit drugs were identified, while 43 drugs initially identified as allergens were exonerated.6
Etiology-associated definitions for blistering reactions in children have been proposed to replace the existing terms Stevens-Johnson syndrome, toxic epidermal necrolysis, and others.7 Investigators in a recent study reclassified cases of SJS and TEN as reactive infectious mucocutaneous eruption (RIME) or drug-induced epidermal necrolysis (DEN), respectively. In RIME cases, Mycoplasma pneumoniae was the most commonly identified trigger, and in DEN cases, anticonvulsants were the most common class of culprit medications. Cases of RIME were less severe and were most often treated with antibiotics, whereas patients with DEN were more likely to receive supportive care, corticosteroids, intravenous immunoglobulins, and other immunosuppressive therapies.7
In addition to causing acute devastating mucocutaneous complications, SJS and TEN have long-lasting effects that require ongoing care. In a cohort of 6552 incident SJS/TEN cases over an 11-year period, survivors of SJS/TEN endured a mean loss of 9.4 years in life expectancy and excess health care expenditures of $3752 per year compared with age- and sex-matched controls. Patients with more severe disease, comorbid malignancy, diabetes, end-stage renal disease, or SJS/TEN sequelae experienced greater loss in life expectancy and lifetime health care expenditures.8 Separately, a qualitative study investigating the psychological impact of SJS/TEN in pediatric patients described sequelae including night terrors, posttraumatic stress disorder, depression, and anxiety for many years after the acute phase. Many patients reported a desire for increased support for their physical and emotional needs following hospital discharge.9
Skin and Soft Tissue Infections: Diagnosis, Management, and Prevention
Dermatology consultation has been shown to be a cost-effective intervention to improve outcomes in hospitalized patients with skin and soft tissue infections.10,11 In particular, cellulitis frequently is misdiagnosed, leading to unnecessary antibiotic use, hospitalizations, and major health care expenditures.12 Recognizing this challenge, researchers have worked to develop objective tools to improve diagnostic accuracy. In a large prospective prognostic validation study, Pulia et al13 found that thermal imaging alone or in combination with the ALT-70 prediction model (asymmetry, leukocytosis, tachycardia, and age ≥70 years) could be used successfully to reduce overdiagnosis of cellulitis. Both thermal imaging and the ALT-70 prediction model demonstrated robust sensitivity (93.5% and 98.8%, respectively) but low specificity (38.4% and 22.0%, respectively, and 53.9% when combined).13
In a systematic review, Kovacs et al14 analyzed case reports of pseudocellulitis caused by chemotherapeutic medications. Of the 81 cases selected, 58 (71.6%) were associated with gemcitabine, with the remaining 23 (28.4%) attributed to pemetrexed. Within this group, two-thirds of the patients received antibiotic treatment prior to receiving the correct diagnosis, and 36% experienced interruptions to their oncologic therapies. In contrast to infectious cellulitis, which tends to be unilateral and associated with elevated erythrocyte sedimentation rate or C-reactive protein, most chemotherapy-induced pseudocellulitis cases occurred bilaterally on the lower extremities, while erythrocyte sedimentation rate and C-reactive protein seldom were elevated.14
Necrotizing soft tissue infections (NSTIs) are severe life-threatening conditions characterized by widespread tissue destruction, signs of systemic toxicity, hemodynamic collapse, organ failure, and high mortality. Surgical inspection along with intraoperative tissue culture is the gold standard for diagnosis. Early detection, prompt surgical intervention, and appropriate antibiotic treatment are essential to reduce mortality and improve outcomes.15 A retrospective study of patients with surgically confirmed NSTIs assessed the incidence and risk factors for recurrence within 1 year following an initial NSTI of the lower extremity. Among 93 included patients, 32 (34.4%) had recurrence within 1 year, and more than half of recurrences occurred in the first 3 months (median, 66 days). The comparison of patients with and without recurrence showed similar proportions of antibiotic prophylaxis use after the first NSTI. There was significantly less compression therapy use (33.3% vs 62.3%; P=.13) and more negative pressure wound therapy use (83.3% vs 63.3%; P=.03) in the recurrence group, though the authors acknowledged that factors such as severity of pain and size of soft tissue defect may have affected the decisions for compression and negative pressure wound therapy.16
Residents of nursing homes are a particularly vulnerable population at high risk for health care–associated infections due to older age and a higher likelihood of having wounds, indwelling medical devices, and/or coexisting conditions.17 One cluster-randomized trial compared universal decolonization with routine-care bathing practices in nursing homes (N=28,956 residents). Decolonization entailed the use of chlorhexidine for all routine bathing and showering and administration of nasal povidone-iodine twice daily for the first 5 days after admission and then twice daily for 5 days every other week. Transfer to a hospital due to infection decreased from 62.9% to 52.2% with decolonization, for a difference in risk ratio of 16.6% (P<.001) compared with routine care. Additionally, the difference in risk ratio of the secondary end point (transfer to a hospital for any reason) was 14.6%. The number needed to treat was 9.7 to prevent 1 infection-related hospitalization and 8.9 to prevent 1 hospitalization for any reason.17
Autoimmune Blistering Diseases
Although rare, AIBDs are potentially life-threatening cutaneous diseases that often require inpatient management. While corticosteroids remain the mainstay of initial AIBD management, rituximab is now well recognized as the steroid-sparing treatment of choice for patients with moderate to severe pemphigus. In a long-term follow-up study of Ritux 318—the trial that led to the US Food and Drug Administration approval of rituximab in the treatment of moderate to severe pemphigus vulgaris—researchers assessed the long-term efficacy and safety of rituximab as a first-line treatment in patients with pemphigus.19 The 5- and 7-year disease-free survival rates without corticosteroid therapy for patients treated with rituximab were 76.7% and 72.1%, respectively, compared with 35.3% and 35.3% in those treated with prednisone alone (P<.001). Fewer serious adverse events were reported in those treated with rituximab plus prednisone compared with those treated with prednisone alone. None of the patients who maintained complete remission off corticosteroid therapy received any additional maintenance infusions of rituximab after the end of the Ritux 3 regimen (1 g of rituximab at day 0 and day 14, then 500 mg at months 12 and 18).19
By contrast, treatment of severe bullous pemphigoid (BP) often is less clear-cut, as no single therapeutic option has been shown to be superior to other immunomodulatory and immunosuppressive regimens, and the medical comorbidities of elderly patients with BP can be limiting. Fortunately, newer therapies with favorable safety profiles have emerged in recent years. In a multicenter retrospective study, 100 patients with BP received omalizumab after previously failing to respond to at least one alternative therapy. Disease control was obtained after a median of 10 days, and complete remission was achieved in 77% of patients in a median time of 3 months.20 In a multicenter retrospective cohort study of 146 patients with BP treated with dupilumab following the atopic dermatitis dosing schedule (one 600-mg dose followed by 300 mg every 2 weeks), disease control was achieved in a median of 14 days, while complete remission was achieved in 35.6% of patients, with 8.9% relapsing during the observation period.21 A retrospective case series of 30 patients with BP treated with dupilumab with maintenance dosing frequency tailored to individual patient response showed complete remission or marked response in 76.7% (23/30) of patients.22 A phase 2/3 randomized controlled trial of dupilumab in BP is currently ongoing (ClinicalTrials.gov identifier NCT04206553).
Pemphigoid gestationis is a rare autoimmune subepidermal bullous dermatosis of pregnancy that may be difficult to distinguish clinically from polymorphic eruption of pregnancy but confers notably different maternal and fetal risks. Researchers developed and validated a scoring system using clinical factors—history of pemphigoid gestationis, primigravidae, timing of rash onset, and specific clinical examination findings—that was able to differentiate between the 2 diseases with 79% sensitivity, 95% specificity, and an area under the curve of 0.93 without the need for advanced immunologic testing.23
Final Thoughts
Highlights of the literature from 2023-2024 demonstrate advancements in hospital-based dermatology as well as ongoing challenges. This year’s review emphasizes key developments in severe cutaneous adverse drug reactions, skin and soft tissue infections, and AIBDs. Continued expansion of knowledge in these areas and others informs patient care and demonstrates the value of dermatologic expertise in the inpatient setting.
Inpatient consultative dermatology has advanced as a subspecialty and increasingly gained recognition in recent years. Since its founding in 2009, the Society of Dermatology Hospitalists has fostered research and education in hospital dermatology. Last year, we reviewed the 2022-2023 literature with a focus on developments in severe cutaneous adverse reactions, supportive oncodermatology, cost of inpatient services, and teledermatology.1 In this review, we highlight 3 areas of interest from the 2023-2024 literature: severe cutaneous adverse drug reactions, skin and soft tissue infections, and autoimmune blistering diseases (AIBDs).
Severe Cutaneous Adverse Drug Reactions
Adverse drug reactions are among the most common diagnoses encountered by inpatient dermatology consultants.2,3 Severe cutaneous adverse drug reactions are associated with substantial morbidity and mortality. Efforts to characterize these conditions and standardize their diagnosis and management continue to be a major focus of ongoing research.
A single-center retrospective analysis of 102 cases of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome evaluated differences in clinical manifestations depending on the culprit drug, offering insights into the heterogeneity of DRESS syndrome and the potential for diagnostic uncertainty.4 The shortest median latency was observed in a case caused by penicillin and cephalosporins (12 and 18 days, respectively), while DRESS syndrome secondary to allopurinol had the longest median latency (36 days). Nonsteroidal anti-inflammatory drug–induced DRESS syndrome was associated with the shortest hospital stay (6.5 days), while cephalosporin and vancomycin cases had the highest mortality rates.4
In the first international Delphi consensus study on the diagnostic workup, severity assessment, and management of DRESS syndrome, 54 dermatology and/or allergy experts reached consensus on 93 statements.5 Specific recommendations included basic evaluation with complete blood count with differential, kidney and liver function parameters, and electrocardiogram for all patients with suspected DRESS syndrome, with additional complementary workup considered in patients with evidence of specific organ damage and/or severe disease. In the proposed DRESS syndrome severity grading scheme, laboratory values that reached consensus for inclusion were hemoglobin, neutrophil, and platelet counts and creatinine, transaminases, and alkaline phosphatase levels. Although treatment of DRESS syndrome should be based on assessed disease severity, treatment with corticosteroids should be initiated in all patients with confirmed DRESS syndrome. Cyclosporine, antibodies interfering with the IL-5 axis, and intravenous immunoglobulins can be considered in patients with corticosteroid-refractory DRESS syndrome, and antiviral treatment can be considered in patients with a high serum cytomegalovirus viral load. Regularly following up with laboratory evaluation of involved organs; screening for autoantibodies, thyroid dysfunction, and steroid adverse effects; and offering of psychological support also were consensus recommendations.5
Identifying causative agents in drug hypersensitivity reactions remains challenging. A retrospective cohort study of 48 patients with Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN) highlighted the need for a systematic unbiased approach to identifying culprit drugs. Using the RegiSCAR database and algorithm for drug causality for epidermal necrolysis to analyze the cohort, more than half of causative agents were determined to be different from those initially identified by the treating physicians. Nine additional suspected culprit drugs were identified, while 43 drugs initially identified as allergens were exonerated.6
Etiology-associated definitions for blistering reactions in children have been proposed to replace the existing terms Stevens-Johnson syndrome, toxic epidermal necrolysis, and others.7 Investigators in a recent study reclassified cases of SJS and TEN as reactive infectious mucocutaneous eruption (RIME) or drug-induced epidermal necrolysis (DEN), respectively. In RIME cases, Mycoplasma pneumoniae was the most commonly identified trigger, and in DEN cases, anticonvulsants were the most common class of culprit medications. Cases of RIME were less severe and were most often treated with antibiotics, whereas patients with DEN were more likely to receive supportive care, corticosteroids, intravenous immunoglobulins, and other immunosuppressive therapies.7
In addition to causing acute devastating mucocutaneous complications, SJS and TEN have long-lasting effects that require ongoing care. In a cohort of 6552 incident SJS/TEN cases over an 11-year period, survivors of SJS/TEN endured a mean loss of 9.4 years in life expectancy and excess health care expenditures of $3752 per year compared with age- and sex-matched controls. Patients with more severe disease, comorbid malignancy, diabetes, end-stage renal disease, or SJS/TEN sequelae experienced greater loss in life expectancy and lifetime health care expenditures.8 Separately, a qualitative study investigating the psychological impact of SJS/TEN in pediatric patients described sequelae including night terrors, posttraumatic stress disorder, depression, and anxiety for many years after the acute phase. Many patients reported a desire for increased support for their physical and emotional needs following hospital discharge.9
Skin and Soft Tissue Infections: Diagnosis, Management, and Prevention
Dermatology consultation has been shown to be a cost-effective intervention to improve outcomes in hospitalized patients with skin and soft tissue infections.10,11 In particular, cellulitis frequently is misdiagnosed, leading to unnecessary antibiotic use, hospitalizations, and major health care expenditures.12 Recognizing this challenge, researchers have worked to develop objective tools to improve diagnostic accuracy. In a large prospective prognostic validation study, Pulia et al13 found that thermal imaging alone or in combination with the ALT-70 prediction model (asymmetry, leukocytosis, tachycardia, and age ≥70 years) could be used successfully to reduce overdiagnosis of cellulitis. Both thermal imaging and the ALT-70 prediction model demonstrated robust sensitivity (93.5% and 98.8%, respectively) but low specificity (38.4% and 22.0%, respectively, and 53.9% when combined).13
In a systematic review, Kovacs et al14 analyzed case reports of pseudocellulitis caused by chemotherapeutic medications. Of the 81 cases selected, 58 (71.6%) were associated with gemcitabine, with the remaining 23 (28.4%) attributed to pemetrexed. Within this group, two-thirds of the patients received antibiotic treatment prior to receiving the correct diagnosis, and 36% experienced interruptions to their oncologic therapies. In contrast to infectious cellulitis, which tends to be unilateral and associated with elevated erythrocyte sedimentation rate or C-reactive protein, most chemotherapy-induced pseudocellulitis cases occurred bilaterally on the lower extremities, while erythrocyte sedimentation rate and C-reactive protein seldom were elevated.14
Necrotizing soft tissue infections (NSTIs) are severe life-threatening conditions characterized by widespread tissue destruction, signs of systemic toxicity, hemodynamic collapse, organ failure, and high mortality. Surgical inspection along with intraoperative tissue culture is the gold standard for diagnosis. Early detection, prompt surgical intervention, and appropriate antibiotic treatment are essential to reduce mortality and improve outcomes.15 A retrospective study of patients with surgically confirmed NSTIs assessed the incidence and risk factors for recurrence within 1 year following an initial NSTI of the lower extremity. Among 93 included patients, 32 (34.4%) had recurrence within 1 year, and more than half of recurrences occurred in the first 3 months (median, 66 days). The comparison of patients with and without recurrence showed similar proportions of antibiotic prophylaxis use after the first NSTI. There was significantly less compression therapy use (33.3% vs 62.3%; P=.13) and more negative pressure wound therapy use (83.3% vs 63.3%; P=.03) in the recurrence group, though the authors acknowledged that factors such as severity of pain and size of soft tissue defect may have affected the decisions for compression and negative pressure wound therapy.16
Residents of nursing homes are a particularly vulnerable population at high risk for health care–associated infections due to older age and a higher likelihood of having wounds, indwelling medical devices, and/or coexisting conditions.17 One cluster-randomized trial compared universal decolonization with routine-care bathing practices in nursing homes (N=28,956 residents). Decolonization entailed the use of chlorhexidine for all routine bathing and showering and administration of nasal povidone-iodine twice daily for the first 5 days after admission and then twice daily for 5 days every other week. Transfer to a hospital due to infection decreased from 62.9% to 52.2% with decolonization, for a difference in risk ratio of 16.6% (P<.001) compared with routine care. Additionally, the difference in risk ratio of the secondary end point (transfer to a hospital for any reason) was 14.6%. The number needed to treat was 9.7 to prevent 1 infection-related hospitalization and 8.9 to prevent 1 hospitalization for any reason.17
Autoimmune Blistering Diseases
Although rare, AIBDs are potentially life-threatening cutaneous diseases that often require inpatient management. While corticosteroids remain the mainstay of initial AIBD management, rituximab is now well recognized as the steroid-sparing treatment of choice for patients with moderate to severe pemphigus. In a long-term follow-up study of Ritux 318—the trial that led to the US Food and Drug Administration approval of rituximab in the treatment of moderate to severe pemphigus vulgaris—researchers assessed the long-term efficacy and safety of rituximab as a first-line treatment in patients with pemphigus.19 The 5- and 7-year disease-free survival rates without corticosteroid therapy for patients treated with rituximab were 76.7% and 72.1%, respectively, compared with 35.3% and 35.3% in those treated with prednisone alone (P<.001). Fewer serious adverse events were reported in those treated with rituximab plus prednisone compared with those treated with prednisone alone. None of the patients who maintained complete remission off corticosteroid therapy received any additional maintenance infusions of rituximab after the end of the Ritux 3 regimen (1 g of rituximab at day 0 and day 14, then 500 mg at months 12 and 18).19
By contrast, treatment of severe bullous pemphigoid (BP) often is less clear-cut, as no single therapeutic option has been shown to be superior to other immunomodulatory and immunosuppressive regimens, and the medical comorbidities of elderly patients with BP can be limiting. Fortunately, newer therapies with favorable safety profiles have emerged in recent years. In a multicenter retrospective study, 100 patients with BP received omalizumab after previously failing to respond to at least one alternative therapy. Disease control was obtained after a median of 10 days, and complete remission was achieved in 77% of patients in a median time of 3 months.20 In a multicenter retrospective cohort study of 146 patients with BP treated with dupilumab following the atopic dermatitis dosing schedule (one 600-mg dose followed by 300 mg every 2 weeks), disease control was achieved in a median of 14 days, while complete remission was achieved in 35.6% of patients, with 8.9% relapsing during the observation period.21 A retrospective case series of 30 patients with BP treated with dupilumab with maintenance dosing frequency tailored to individual patient response showed complete remission or marked response in 76.7% (23/30) of patients.22 A phase 2/3 randomized controlled trial of dupilumab in BP is currently ongoing (ClinicalTrials.gov identifier NCT04206553).
Pemphigoid gestationis is a rare autoimmune subepidermal bullous dermatosis of pregnancy that may be difficult to distinguish clinically from polymorphic eruption of pregnancy but confers notably different maternal and fetal risks. Researchers developed and validated a scoring system using clinical factors—history of pemphigoid gestationis, primigravidae, timing of rash onset, and specific clinical examination findings—that was able to differentiate between the 2 diseases with 79% sensitivity, 95% specificity, and an area under the curve of 0.93 without the need for advanced immunologic testing.23
Final Thoughts
Highlights of the literature from 2023-2024 demonstrate advancements in hospital-based dermatology as well as ongoing challenges. This year’s review emphasizes key developments in severe cutaneous adverse drug reactions, skin and soft tissue infections, and AIBDs. Continued expansion of knowledge in these areas and others informs patient care and demonstrates the value of dermatologic expertise in the inpatient setting.
- Berk-Krauss J, Micheletti RG. Hospital dermatology: review of research in 2022-2023. Cutis. 2023;112:236-239.
- Falanga V, Schachner LA, Rae V, et al. Dermatologic consultations in the hospital setting. Arch Dermatol. 1994;130:1022-1025.
- Kroshinsky D, Cotliar J, Hughey LC, et al. Association of dermatology consultation with accuracy of cutaneous disorder diagnoses in hospitalized patients: a multicenter analysis. JAMA Dermatol. 2016;152:477-480.
- Blumenthal KG, Alvarez-Arango S, Kroshinsky D, et al. Drug reaction eosinophilia and systemic symptoms: clinical phenotypic patterns according to causative drug. J Am Acad Dermatol. 2024;90:1240-1242.
- Brüggen MC, Walsh S, Ameri MM, et al. Management of adult patients with drug reaction with eosinophilia and systemic symptoms: a Delphi-based international consensus. JAMA Dermatol. 2024;160:37-44.
- Li DJ, Velasquez GA, Romar GA, et al. Assessment of need for improved identification of a culprit drug in Stevens-Johnson syndrome/toxic epidermal necrolysis. JAMA Dermatol. 2023;159:830-836.
- Martinez-Cabriales S, Coulombe J, Aaron M, et al. Preliminary summary and reclassification of cases from the Pediatric Research of Management in Stevens-Johnson syndrome and Epidermonecrolysis (PROMISE) study: a North American, multisite retrospective cohort. J Am Acad Dermatol. 2024;90:635-637.
- Chiu YM, Chiu HY. Lifetime risk, life expectancy, loss-of-life expectancy and lifetime healthcare expenditure for Stevens-Johnson syndrome/toxic epidermal necrolysis in Taiwan: follow-up of a nationwide cohort from 2008 to 2019. Br J Dermatol. 2023;189:553-560.
- Phillips C, Russell E, McNiven A, et al. A qualitative study of psychological morbidity in paediatric survivors of Stevens-Johnson syndrome/toxic epidermal necrolysis. Br J Dermatol. 2024;191:293-295.
- Li DG, Xia FD, Khosravi H, et al. Outcomes of early dermatology consultation for inpatients diagnosed with cellulitis. JAMA Dermatol. 2018;154:537-543.
- Milani-Nejad N, Zhang M, Kaffenberger BH. Association of dermatology consultations with patient care outcomes in hospitalized patients with inflammatory skin diseases. JAMA Dermatol. 2017;153:523-528.
- Weng QY, Raff AB, Cohen JM, et al. Costs and consequences associated with misdiagnosed lower extremity cellulitis. JAMA Dermatol. 2017;153:141-146.
- Pulia MS, Schwei RJ, Alexandridis R, et al. Validation of thermal imaging and the ALT-70 prediction model to differentiate cellulitis from pseudocellulitis. JAMA Dermatol. 2024;160:511-517.
- Kovacs LD, O’Donoghue M, Cogen AL. Chemotherapy-induced pseudocellulitis without prior radiation exposure: a systematic review. JAMA Dermatol. 2023;159:870-874.
- Yildiz H, Yombi JC. Necrotizing soft-tissue infections. comment. N Engl J Med. 2018;378:970.
- Traineau H, Charpentier C, Lepeule R, et al. First-year recurrence rate of skin and soft tissue infections following an initial necrotizing soft tissue infection of the lower extremities: a retrospective cohort study of 93 patients. J Am Acad Dermatol. 2023;88:1360-1363.
- Miller LG, McKinnell JA, Singh RD, et al. Decolonization in nursing homes to prevent infection and hospitalization. N Engl J Med. 2023;389:1766-1777.
- Joly P, Maho-Vaillant M, Prost-Squarcioni C, et al; French Study Group on Autoimmune Bullous Skin Diseases. First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): a prospective, multicentre, parallel-group, open-label randomised trial. Lancet. 2017;389:2031-2040.
- Tedbirt B, Maho-Vaillant M, Houivet E, et al; French Reference Center for Autoimmune Blistering Diseases MALIBUL. Sustained remission without corticosteroids among patients with pemphigus who had rituximab as first-line therapy: follow-up of the Ritux 3 Trial. JAMA Dermatol. 2024;160:290-296.
- Chebani R, Lombart F, Chaby G, et al; French Study Group on Autoimmune Bullous Diseases. Omalizumab in the treatment of bullous pemphigoid resistant to first-line therapy: a French national multicentre retrospective study of 100 patients. Br J Dermatol. 2024;190:258-265.
- Zhao L, Wang Q, Liang G, et al. Evaluation of dupilumab in patients with bullous pemphigoid. JAMA Dermatol. 2023;159:953-960.
- Miller AC, Temiz LA, Adjei S, et al. Treatment of bullous pemphigoid with dupilumab: a case series of 30 patients. J Drugs Dermatol. 2024;23:E144-E148.
- Xie F, Davis DMR, Baban F, et al. Development and multicenter international validation of a diagnostic tool to differentiate between pemphigoid gestationis and polymorphic eruption of pregnancy. J Am Acad Dermatol. 2023;89:106-113.
- Berk-Krauss J, Micheletti RG. Hospital dermatology: review of research in 2022-2023. Cutis. 2023;112:236-239.
- Falanga V, Schachner LA, Rae V, et al. Dermatologic consultations in the hospital setting. Arch Dermatol. 1994;130:1022-1025.
- Kroshinsky D, Cotliar J, Hughey LC, et al. Association of dermatology consultation with accuracy of cutaneous disorder diagnoses in hospitalized patients: a multicenter analysis. JAMA Dermatol. 2016;152:477-480.
- Blumenthal KG, Alvarez-Arango S, Kroshinsky D, et al. Drug reaction eosinophilia and systemic symptoms: clinical phenotypic patterns according to causative drug. J Am Acad Dermatol. 2024;90:1240-1242.
- Brüggen MC, Walsh S, Ameri MM, et al. Management of adult patients with drug reaction with eosinophilia and systemic symptoms: a Delphi-based international consensus. JAMA Dermatol. 2024;160:37-44.
- Li DJ, Velasquez GA, Romar GA, et al. Assessment of need for improved identification of a culprit drug in Stevens-Johnson syndrome/toxic epidermal necrolysis. JAMA Dermatol. 2023;159:830-836.
- Martinez-Cabriales S, Coulombe J, Aaron M, et al. Preliminary summary and reclassification of cases from the Pediatric Research of Management in Stevens-Johnson syndrome and Epidermonecrolysis (PROMISE) study: a North American, multisite retrospective cohort. J Am Acad Dermatol. 2024;90:635-637.
- Chiu YM, Chiu HY. Lifetime risk, life expectancy, loss-of-life expectancy and lifetime healthcare expenditure for Stevens-Johnson syndrome/toxic epidermal necrolysis in Taiwan: follow-up of a nationwide cohort from 2008 to 2019. Br J Dermatol. 2023;189:553-560.
- Phillips C, Russell E, McNiven A, et al. A qualitative study of psychological morbidity in paediatric survivors of Stevens-Johnson syndrome/toxic epidermal necrolysis. Br J Dermatol. 2024;191:293-295.
- Li DG, Xia FD, Khosravi H, et al. Outcomes of early dermatology consultation for inpatients diagnosed with cellulitis. JAMA Dermatol. 2018;154:537-543.
- Milani-Nejad N, Zhang M, Kaffenberger BH. Association of dermatology consultations with patient care outcomes in hospitalized patients with inflammatory skin diseases. JAMA Dermatol. 2017;153:523-528.
- Weng QY, Raff AB, Cohen JM, et al. Costs and consequences associated with misdiagnosed lower extremity cellulitis. JAMA Dermatol. 2017;153:141-146.
- Pulia MS, Schwei RJ, Alexandridis R, et al. Validation of thermal imaging and the ALT-70 prediction model to differentiate cellulitis from pseudocellulitis. JAMA Dermatol. 2024;160:511-517.
- Kovacs LD, O’Donoghue M, Cogen AL. Chemotherapy-induced pseudocellulitis without prior radiation exposure: a systematic review. JAMA Dermatol. 2023;159:870-874.
- Yildiz H, Yombi JC. Necrotizing soft-tissue infections. comment. N Engl J Med. 2018;378:970.
- Traineau H, Charpentier C, Lepeule R, et al. First-year recurrence rate of skin and soft tissue infections following an initial necrotizing soft tissue infection of the lower extremities: a retrospective cohort study of 93 patients. J Am Acad Dermatol. 2023;88:1360-1363.
- Miller LG, McKinnell JA, Singh RD, et al. Decolonization in nursing homes to prevent infection and hospitalization. N Engl J Med. 2023;389:1766-1777.
- Joly P, Maho-Vaillant M, Prost-Squarcioni C, et al; French Study Group on Autoimmune Bullous Skin Diseases. First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): a prospective, multicentre, parallel-group, open-label randomised trial. Lancet. 2017;389:2031-2040.
- Tedbirt B, Maho-Vaillant M, Houivet E, et al; French Reference Center for Autoimmune Blistering Diseases MALIBUL. Sustained remission without corticosteroids among patients with pemphigus who had rituximab as first-line therapy: follow-up of the Ritux 3 Trial. JAMA Dermatol. 2024;160:290-296.
- Chebani R, Lombart F, Chaby G, et al; French Study Group on Autoimmune Bullous Diseases. Omalizumab in the treatment of bullous pemphigoid resistant to first-line therapy: a French national multicentre retrospective study of 100 patients. Br J Dermatol. 2024;190:258-265.
- Zhao L, Wang Q, Liang G, et al. Evaluation of dupilumab in patients with bullous pemphigoid. JAMA Dermatol. 2023;159:953-960.
- Miller AC, Temiz LA, Adjei S, et al. Treatment of bullous pemphigoid with dupilumab: a case series of 30 patients. J Drugs Dermatol. 2024;23:E144-E148.
- Xie F, Davis DMR, Baban F, et al. Development and multicenter international validation of a diagnostic tool to differentiate between pemphigoid gestationis and polymorphic eruption of pregnancy. J Am Acad Dermatol. 2023;89:106-113.
Practice Points
- An international Delphi study reached consensus on 93 statements regarding workup, severity assessment, and management of DRESS syndrome.
- In nursing homes, universal decolonization with chlorhexidine and nasal iodophor greatly reduced the risk for hospital transfers due to infection compared to routine care.
- Rituximab as the first-line therapy for pemphigus vulgaris is associated with long-term sustained complete remission without corticosteroid therapy.
- Dupilumab and omalizumab are emerging safe and effective treatment options for bullous pemphigoid.
Emerging Insights in Keloid Pathogenesis and Therapeutics
Keloids are fibroproliferative lesions caused by aberrant wound healing in predisposed individuals.1 While keloids have been reported in patients of all races and ethnicities, they most commonly develop in individuals of African or Asian descent.2 Often associated with symptoms such as pain and itching, keloids can be disfiguring and result in poorer quality of life.3 There is a paucity of research on keloid pathogenesis and efficacious therapeutics, particularly in patients with skin of color (SOC). Herein, we outline the current research on keloid treatment and highlight promising new therapies ranging from innovative intralesional techniques to advanced laser-based and biologic therapies.
Deficiencies in Skin of Color Research
Although keloids are 17 times more prevalent in patients with SOC,4 there is a considerable lack of focus on this population in the literature.5 Studies on keloids that include individuals with SOC often group patients of all skin types together, and subgroup analyses are not always performed.6,7 As a result, dermatologists may face considerable challenges in providing effective treatments for keloids in patients with SOC. With few evidence-based options available, patients with SOC who have keloids continue to experience impairments in quality of life.
Common Keloid Therapies
There currently is no gold-standard treatment for keloids. Common therapeutic modalities include intralesional corticosteroids (ILCs), antineoplastic agents and neuromodulators, laser-based devices, and surgical therapies (eg, excision), as well as combined medical and surgical techniques.8
Intralesional Corticosteroids—Minimally invasive ILCs are the first-line treatment in all patients with keloids, regardless of skin phototype. Because keloid formation results from trauma to the skin, ILCs often are recommended to minimize further skin damage.5 One meta-analysis found that ILCs have demonstrated success rates of 50% to 100%9; however, these studies frequently combine ILCs with other treatment modalities, and few studies have focused on the efficacy of ILC monotherapy in patients with SOC.6,10-13
Antineoplastic Agents and Neuromodulators—Certain antineoplastic agents (eg, 5-fluorouracil [5-FU] and bleomycin) and neuromodulators (eg, botulinum toxin A [BTA]) also have been studied in keloid management.8
5-Fluorouracil frequently is combined with ILCs such as triamcinolone (TAC). Combined therapy is more effective than TAC monotherapy in scar height reduction.14,15 Rates of adverse events such as dyspigmentation, atrophy, and telangiectasias also were lower in patients who received combined therapy.14,15 A systematic review found that intralesional bleomycin may be more effective than TAC alone, 5-FU alone, TAC combined with 5-FU, and TAC combined with cryotherapy; however, hyperpigmentation was a common adverse event, occurring in roughly 70% (42/60) of patients.16,17 Additionally, a 2024 meta-analysis evaluated 20 randomized controlled trials comprising 1114 patients treated with intralesional TAC, 5-FU, BTA, verapamil, and/or bleomycin. Botulinum toxin A and TAC plus 5-FU were found to have outstanding therapeutic efficacy for keloids, and rates of adverse events were similar among users of TAC, 5-FU, BTA, and TAC plus 5-FU.18
While antineoplastic agents and BTA may be promising keloid therapies, further studies demonstrating their efficacy and safety profiles are necessary, particularly regarding dyspigmentation as a potential adverse event, as this may be of concern in patients with darker phototypes.
Laser Therapies—Of all treatment modalities, laser-based keloid therapies have been the most robustly studied in SOC. The 2 main types are ablative (eg, CO2, Er:YAG) and nonablative (eg, pulsed dye, Nd:YAG) lasers. Ablative lasers rapidly heat water molecules within the skin, thereby vaporizing the skin cells in a controlled precise process that reduces scar tissue by removing layers of skin. Nonablative lasers target hemoglobin in blood vessels, reducing oxygen supply and inducing collagen remodeling without damaging the epidermis.19
For patients with SOC, lasers carry a risk for postinflammatory hyperpigmentation.20 To address this risk, recent advancements in laser technology and procedural protocols have aimed to minimize the number of passes and utilize cooling devices21; however, many of these recommendations are based on retrospective reviews and small case series. A 2024 meta-analysis comprising 550 patients found that the combination of fractional CO2 laser therapy and 5-FU was the most effective intervention, markedly reducing Vancouver Scar Scale and pliability scores as well as keloid thickness.22 Conversely, pulsed dye lasers were the least effective in terms of improving scar thickness, pigmentation, and pliability when compared to other treatments.
Randomized controlled trials of laser-based therapies in patients with SOC are lacking in the literature. Future studies should focus on calibrating laser-based therapies for those with darker skin tones and examine the efficacy and adverse effects of ablative and nonablative lasers in patients with SOC.
Promising New Keloid Therapies
Keloid disease pathogenesis is incompletely understood, but several new therapeutic targets have been highlighted in the literature, including dupilumab, pentoxifylline, sirtuin 6 (SIRT6) modulators, remdesivir, and needle-assisted electrocoagulation plus pharmacotherapy.
Dupilumab—An anti–IL-4 and IL-13 monoclonal antibody, dupilumab was first approved for the treatment of severe atopic dermatitis. Its use has broadened since its approval, and keloids have been identified as a potential therapeutic target. A 2019 case study described a 53-year-old Black man with severe atopic dermatitis and chronic keloids that regressed with systemic dupilumab therapy.23 This prompted a follow-up case-control study using real-time polymerase chain reaction testing to evaluate Th2 gene expression (IL-4R, IL-13, and CCL18) of lesional and nonlesional tissue in 3 Black patients with chronic keloids and no concurrent atopic dermatitis vs 5 healthy Black controls. Despite the limited sample size, a significant increase in IL-13 and the Th2 chemokine CCL18 was found in patients with keloids compared to controls (P<.05), suggesting that the entire integument of patients with severe keloids is abnormal.23 This finding supports the use of systemic treatments for chronic and multifocal keloid disease. Several subsequent case reports have corroborated the efficacy of systemic and/or intralesional dupilumab.24,25 However, some studies have reported contradictory findings, suggesting the need for high-quality clinical trials.26,27
Pentoxifylline—Pentoxifylline is a methylated xanthine derivative and a nonspecific phosphodiesterase inhibitor used to treat claudication from peripheral artery disease. It also inhibits the proliferation and rate of collagen synthesis of fibroblasts from keloids in vitro.28,29 A 2019 retrospective, open-label pilot study analyzed postsurgical keloid recurrence in 45 patients with 67 unique keloids that were stratified into low- and high-risk groups based on clinical factors including multiple symptomatic keloids, history of recurrence, and family history.30 Both the low- and the high-risk groups were treated with 40 mg/mL intralesional triamcinolone acetonide monthly for 6 months; however, some of the high-risk keloids also received pentoxifylline 300 mg 3 times daily for 6 months. There was a statistically significant decrease in keloid recurrence rate between the high-risk group treated with pentoxifylline and the low-risk group for whom pentoxifylline was not prescribed (P=.015).
Similarly, a randomized clinical trial comparing the efficacy of combination intralesional pentoxifylline and intralesional triamcinolone vs monotherapy with pentoxifylline or triamcinolone found the most significant improvement in the combination cohort with reduction in keloid height (P=.04), pliability (P=.003), and vascularity (P=.05).31 These findings highlight the need for supplementary studies on the use of pentoxifylline for keloid therapy.
SIRT6 Modulators—SIRT6 modulators are an exciting future therapeutic target. In a recent case-control study evaluating the histologic milieu of keloid tissue vs normal skin specimens, the researchers found that selective overexpression of SIRT6 via the use of a recombinant adenovirus in keloid fibroblasts attenuated proliferation, invasion, and collagen synthesis while fostering apoptosis, likely through the suppression of MAPK/ERK pathway activity.32
Remdesivir—The antiviral drug remdesivir has been reported to have pharmacologic activities in a wide range of fibrotic diseases, including keloids. A 2024 study explored the potential effect and mechanisms of remdesivir on skin fibrosis both in vitro and in rodents.33 Remdesivir was found to decrease skin fibrosis and attenuate the gross weight of keloid tissues in vivo, suppress fibroblast activation and autophagy both in vivo and in vitro, dampen fibroblast activation by the TGF-β1/Smad signaling pathway, and inhibit fibroblasts autophagy by the PI3K/Akt/mTOR signaling pathway. These results demonstrate the therapeutic potential of remdesivir for keloid management.
Needle-Assisted Electrocoagulation Plus Pharmacotherapy—A novel needle-assisted electrocoagulation technique combined with pharmacotherapy (corticosteroid and 5-FU injections) was effective in a Chinese clinical trial involving 6 patients with keloids.34 Investigators used Vancouver Scar Scale and both Patient and Observer Scar Assessment Scale scores to grade patients’ scars before treatment and 1 month after the first treatment cycle. They found that ablation combined with pharmacotherapy significantly reduced all 3 scores without any obvious adverse events (P=.004, P=.006, and P=.017, respectively). This novel combination treatment may serve as a safe and effective therapeutic approach for keloid removal.
Final Thoughts
Emerging treatments offer promising new horizons in keloid management; however, the lack of robust, high-quality clinical trials, especially those focusing on
- Téot L, Mustoe TA, Middelkoop E, eds. Textbook on Scar Management: State of the Art Management and Emerging Technologies. Springer; 2020.
- Davis SA, Feldman SR, McMichael AJ. Management of keloids in the United States, 1990-2009: an analysis of the National Ambulatory Medical Care Survey. Dermatol Surg. 2013;39:988-994. doi:10.1111/dsu.12182
- Kassi K, Kouame K, Kouassi A, et al. Quality of life in black African patients with keloid scars. Dermatol Reports. 2020;12:8312. doi:10.4081/dr.2020.8312
- Delaleu J, Charvet E, Petit A. Keloid disease: review with clinical atlas. part I: definitions, history, epidemiology, clinics and diagnosis. Ann Dermatol Venereol. 2023;150:3-15.
doi:10.1016/j.annder.2022.08.010 - Bronte J, Zhou C, Vempati A, et al. A comprehensive review of non-surgical treatments for hypertrophic and keloid scars in skin of color. Clin Cosmet Investig Dermatol.
2024;17:1459-1469. doi:10.2147/CCID.S470997 - Davison SP, Dayan JH, Clemens MW, et al. Efficacy of intralesional 5-fluorouracil and triamcinolone in the treatment of keloids. Aesthet Surg J. 2009;29:40-46. doi:10.1016/j.asj.2008.11.006
- Azzam OA, Bassiouny DA, El-Hawary MS, et al. Treatment of hypertrophic scars and keloids by fractional carbon dioxide laser: a clinical, histological, and immunohistochemical study. Lasers Med Sci. 2016;31:9-18. doi:10.1007/s10103-015-1824-4
- Ekstein SF, Wyles SP, Moran SL, et al. Keloids: a review of therapeutic management. Int J Dermatol. 2021;60:661-671. doi:10.1111/ijd.15159
- Morelli Coppola M, Salzillo R, Segreto F, et al. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:387-396. doi:10.2147/CCID.S133672
- Kant SB, van den Kerckhove E, Colla C, et al. A new treatment of hypertrophic and keloid scars with combined triamcinolone and verapamil: a retrospective study. Eur J Plast Surg. 2018;41:69-80. doi:10.1007/s00238-017-1322-y
- Cohen AJ, Talasila S, Lazarevic B, et al. Combination cryotherapy and intralesional corticosteroid versus steroid monotherapy in the treatment of keloids. J Cosmet Dermatol. 2023;22:932-936. doi:10.1111/jocd.15520
- Tawaranurak N, Pliensiri P, Tawaranurak K. Combination of fractional carbon dioxide laser and topical triamcinolone vs intralesional triamcinolone for keloid treatment: a randomised clinical trial. Int Wound J. 2022;19:1729-1735. doi:10.1111/iwj.13775
- Belie O, Ugburo AO, Mofikoya BO, et al. A comparison of intralesional verapamil and triamcinolone monotherapy in the treatment of keloids in an African population. Niger J Clin Pract. 2021;24:986-992. doi:10.4103/njcp.njcp_474_20
- Khalid FA, Mehrose MY, Saleem M, et al. Comparison of efficacy and safety of intralesional triamcinolone and combination of triamcinolone with 5-fluorouracil in the treatment of keloids and hypertrophic scars: randomised control trial. Burns. 2019;45:69-75. doi:10.1016/j.burns.2018.08.011
- Asilian A, Darougheh A, Shariati F. New combination of triamcinolone, 5-Fluorouracil, and pulsed-dye laser for treatment of keloid and hypertrophic scars. Dermatol Surg. 2006;32:907-915. doi:10.1111/j.1524-4725.2006.32195.x
- Kim WI, Kim S, Cho SW, et al. The efficacy of bleomycin for treating keloid and hypertrophic scar: a systematic review and meta-analysis. J Cosmet Dermatol. 2020;19:3357-3366. doi:10.1111/jocd.13390
- Kabel A, Sabry H, Sorour N, et al. Comparative study between intralesional injection of bleomycin and 5-fluorouracil in the treatment of keloids and hypertrophic scars. J Dermatol Dermatol Surg. 2016;20:32-38.
- Yang HA, Jheng WL, Yu J, et al. Comparative efficacy of drug interventions for keloids: a network meta-analysis. Ann Plast Surg. 2024;92(1S suppl 1
):S52-S59. doi:10.1097/SAP.0000000000003759 - Preissig J, Hamilton K, Markus R. Current laser resurfacing technologies: a review that delves beneath the surface. Semin Plast Surg. 2012;26:109-116. doi:10.1055/s-0032-1329413
- Bin Dakhil A, Shadid A, Altalhab S. Post-inflammatory hyperpigmentation after carbon dioxide laser: review of prevention and risk factors. Dermatol Reports. 2023;15:9703. doi:10.4081/dr.2023.9703
- Kaushik SB, Alexis AF. Nonablative fractional laser resurfacing in skin of color: evidence-based review. J Clin Aesthet Dermatol. 2017;10:51-67.
- Foppiani JA, Khaity A, Al-Dardery NM, et al. Laser therapy in hypertrophic and keloid scars: a systematic review and network meta-analysis. Aesthetic Plast Surg. Published May 17, 2024. doi:10.1007/s00266-024-04027-9
- Diaz A, Tan K, He H, et al. Keloid lesions show increased IL-4/IL-13 signaling and respond to Th2-targeting dupilumab therapy. J Eur Acad Dermatol Venereol. 2020;34:E161-E164. doi:10.1111/jdv.16097
- Min MS,
Mazori DR, Lee MS, et al. Successful treatment of keloids and hypertrophic scars with systemic and intralesional dupilumab. J Drugs Dermatol. 2023;22:1220-1222. doi:10.36849/JDD.6385 - Wittmer A, Finklea L, Joseph J. Effects of dupilumab on keloid stabilization and prevention. JAAD Case Rep. 2023;37:103-105. doi:10.1016/j.jdcr.2023.05.001
- Luk K, Fakhoury J, Ozog D. Nonresponse and progression of diffuse keloids to dupilumab therapy. J Drugs Dermatol. 2022;21:197-199. doi:10.36849/jdd.6252
- Tirgan MH, Uitto J. Lack of efficacy of dupilumab in the treatment of keloid disorder. J Eur Acad Dermatol Venereol. 2022;36:E120-E122. doi:10.1111/jdv.17669
- Berman B, Duncan MR. Pentoxifylline inhibits the proliferation of human fibroblasts derived from keloid, scleroderma and morphoea skin and their production of collagen, glycosaminoglycans and fibronectin. Br J Dermatol. 1990;123:339-346. doi:10.1111/j.1365-
2133.1990.tb06294.x - Berman B, Duncan MR. Pentoxifylline inhibits normal human dermal fibroblast in vitro proliferation, collagen, glycosaminoglycan, and fibronectin production, and increases collagenase activity. J Invest Dermatol. 1989;92:605-610.
- Tan A, Martinez Luna O, Glass DA 2nd. Pentoxifylline for the prevention of postsurgical keloid recurrence. Dermatol Surg. 2020;46:1353-1356. doi:10.1097/DSS.0000000000002090
- Serag-Eldin YMA, Mahmoud WH, Gamea MM, et al. Intralesional pentoxifylline, triamcinolone acetonide, and their combination for treatment of keloid scars. J Cosmet Dermatol. 2021;20:3330-3340. doi:10.1111/jocd.14305
- Zhou T, Chen Y, Wang C, et al. SIRT6 inhibits the proliferation and collagen synthesis of keloid fibroblasts through MAPK/ERK pathway. Discov Med. 2024;36:1430-1440. doi:10.24976/Discov.Med.202436186.133
- Zhang J, Zhang X, Guo X, et al. Remdesivir alleviates skin fibrosis by suppressing TGF-β1 signaling pathway. PLoS One. 2024;19:E0305927.
doi:10.1371/journal.pone.0305927 - Zhao J, Zhai X, Xu Z, et al. Novel needle-type electrocoagulation and combination pharmacotherapy: basic and clinical studies on efficacy and safety in treating keloids. J Cosmet Dermatol. doi:10.1111/jocd.16453
Keloids are fibroproliferative lesions caused by aberrant wound healing in predisposed individuals.1 While keloids have been reported in patients of all races and ethnicities, they most commonly develop in individuals of African or Asian descent.2 Often associated with symptoms such as pain and itching, keloids can be disfiguring and result in poorer quality of life.3 There is a paucity of research on keloid pathogenesis and efficacious therapeutics, particularly in patients with skin of color (SOC). Herein, we outline the current research on keloid treatment and highlight promising new therapies ranging from innovative intralesional techniques to advanced laser-based and biologic therapies.
Deficiencies in Skin of Color Research
Although keloids are 17 times more prevalent in patients with SOC,4 there is a considerable lack of focus on this population in the literature.5 Studies on keloids that include individuals with SOC often group patients of all skin types together, and subgroup analyses are not always performed.6,7 As a result, dermatologists may face considerable challenges in providing effective treatments for keloids in patients with SOC. With few evidence-based options available, patients with SOC who have keloids continue to experience impairments in quality of life.
Common Keloid Therapies
There currently is no gold-standard treatment for keloids. Common therapeutic modalities include intralesional corticosteroids (ILCs), antineoplastic agents and neuromodulators, laser-based devices, and surgical therapies (eg, excision), as well as combined medical and surgical techniques.8
Intralesional Corticosteroids—Minimally invasive ILCs are the first-line treatment in all patients with keloids, regardless of skin phototype. Because keloid formation results from trauma to the skin, ILCs often are recommended to minimize further skin damage.5 One meta-analysis found that ILCs have demonstrated success rates of 50% to 100%9; however, these studies frequently combine ILCs with other treatment modalities, and few studies have focused on the efficacy of ILC monotherapy in patients with SOC.6,10-13
Antineoplastic Agents and Neuromodulators—Certain antineoplastic agents (eg, 5-fluorouracil [5-FU] and bleomycin) and neuromodulators (eg, botulinum toxin A [BTA]) also have been studied in keloid management.8
5-Fluorouracil frequently is combined with ILCs such as triamcinolone (TAC). Combined therapy is more effective than TAC monotherapy in scar height reduction.14,15 Rates of adverse events such as dyspigmentation, atrophy, and telangiectasias also were lower in patients who received combined therapy.14,15 A systematic review found that intralesional bleomycin may be more effective than TAC alone, 5-FU alone, TAC combined with 5-FU, and TAC combined with cryotherapy; however, hyperpigmentation was a common adverse event, occurring in roughly 70% (42/60) of patients.16,17 Additionally, a 2024 meta-analysis evaluated 20 randomized controlled trials comprising 1114 patients treated with intralesional TAC, 5-FU, BTA, verapamil, and/or bleomycin. Botulinum toxin A and TAC plus 5-FU were found to have outstanding therapeutic efficacy for keloids, and rates of adverse events were similar among users of TAC, 5-FU, BTA, and TAC plus 5-FU.18
While antineoplastic agents and BTA may be promising keloid therapies, further studies demonstrating their efficacy and safety profiles are necessary, particularly regarding dyspigmentation as a potential adverse event, as this may be of concern in patients with darker phototypes.
Laser Therapies—Of all treatment modalities, laser-based keloid therapies have been the most robustly studied in SOC. The 2 main types are ablative (eg, CO2, Er:YAG) and nonablative (eg, pulsed dye, Nd:YAG) lasers. Ablative lasers rapidly heat water molecules within the skin, thereby vaporizing the skin cells in a controlled precise process that reduces scar tissue by removing layers of skin. Nonablative lasers target hemoglobin in blood vessels, reducing oxygen supply and inducing collagen remodeling without damaging the epidermis.19
For patients with SOC, lasers carry a risk for postinflammatory hyperpigmentation.20 To address this risk, recent advancements in laser technology and procedural protocols have aimed to minimize the number of passes and utilize cooling devices21; however, many of these recommendations are based on retrospective reviews and small case series. A 2024 meta-analysis comprising 550 patients found that the combination of fractional CO2 laser therapy and 5-FU was the most effective intervention, markedly reducing Vancouver Scar Scale and pliability scores as well as keloid thickness.22 Conversely, pulsed dye lasers were the least effective in terms of improving scar thickness, pigmentation, and pliability when compared to other treatments.
Randomized controlled trials of laser-based therapies in patients with SOC are lacking in the literature. Future studies should focus on calibrating laser-based therapies for those with darker skin tones and examine the efficacy and adverse effects of ablative and nonablative lasers in patients with SOC.
Promising New Keloid Therapies
Keloid disease pathogenesis is incompletely understood, but several new therapeutic targets have been highlighted in the literature, including dupilumab, pentoxifylline, sirtuin 6 (SIRT6) modulators, remdesivir, and needle-assisted electrocoagulation plus pharmacotherapy.
Dupilumab—An anti–IL-4 and IL-13 monoclonal antibody, dupilumab was first approved for the treatment of severe atopic dermatitis. Its use has broadened since its approval, and keloids have been identified as a potential therapeutic target. A 2019 case study described a 53-year-old Black man with severe atopic dermatitis and chronic keloids that regressed with systemic dupilumab therapy.23 This prompted a follow-up case-control study using real-time polymerase chain reaction testing to evaluate Th2 gene expression (IL-4R, IL-13, and CCL18) of lesional and nonlesional tissue in 3 Black patients with chronic keloids and no concurrent atopic dermatitis vs 5 healthy Black controls. Despite the limited sample size, a significant increase in IL-13 and the Th2 chemokine CCL18 was found in patients with keloids compared to controls (P<.05), suggesting that the entire integument of patients with severe keloids is abnormal.23 This finding supports the use of systemic treatments for chronic and multifocal keloid disease. Several subsequent case reports have corroborated the efficacy of systemic and/or intralesional dupilumab.24,25 However, some studies have reported contradictory findings, suggesting the need for high-quality clinical trials.26,27
Pentoxifylline—Pentoxifylline is a methylated xanthine derivative and a nonspecific phosphodiesterase inhibitor used to treat claudication from peripheral artery disease. It also inhibits the proliferation and rate of collagen synthesis of fibroblasts from keloids in vitro.28,29 A 2019 retrospective, open-label pilot study analyzed postsurgical keloid recurrence in 45 patients with 67 unique keloids that were stratified into low- and high-risk groups based on clinical factors including multiple symptomatic keloids, history of recurrence, and family history.30 Both the low- and the high-risk groups were treated with 40 mg/mL intralesional triamcinolone acetonide monthly for 6 months; however, some of the high-risk keloids also received pentoxifylline 300 mg 3 times daily for 6 months. There was a statistically significant decrease in keloid recurrence rate between the high-risk group treated with pentoxifylline and the low-risk group for whom pentoxifylline was not prescribed (P=.015).
Similarly, a randomized clinical trial comparing the efficacy of combination intralesional pentoxifylline and intralesional triamcinolone vs monotherapy with pentoxifylline or triamcinolone found the most significant improvement in the combination cohort with reduction in keloid height (P=.04), pliability (P=.003), and vascularity (P=.05).31 These findings highlight the need for supplementary studies on the use of pentoxifylline for keloid therapy.
SIRT6 Modulators—SIRT6 modulators are an exciting future therapeutic target. In a recent case-control study evaluating the histologic milieu of keloid tissue vs normal skin specimens, the researchers found that selective overexpression of SIRT6 via the use of a recombinant adenovirus in keloid fibroblasts attenuated proliferation, invasion, and collagen synthesis while fostering apoptosis, likely through the suppression of MAPK/ERK pathway activity.32
Remdesivir—The antiviral drug remdesivir has been reported to have pharmacologic activities in a wide range of fibrotic diseases, including keloids. A 2024 study explored the potential effect and mechanisms of remdesivir on skin fibrosis both in vitro and in rodents.33 Remdesivir was found to decrease skin fibrosis and attenuate the gross weight of keloid tissues in vivo, suppress fibroblast activation and autophagy both in vivo and in vitro, dampen fibroblast activation by the TGF-β1/Smad signaling pathway, and inhibit fibroblasts autophagy by the PI3K/Akt/mTOR signaling pathway. These results demonstrate the therapeutic potential of remdesivir for keloid management.
Needle-Assisted Electrocoagulation Plus Pharmacotherapy—A novel needle-assisted electrocoagulation technique combined with pharmacotherapy (corticosteroid and 5-FU injections) was effective in a Chinese clinical trial involving 6 patients with keloids.34 Investigators used Vancouver Scar Scale and both Patient and Observer Scar Assessment Scale scores to grade patients’ scars before treatment and 1 month after the first treatment cycle. They found that ablation combined with pharmacotherapy significantly reduced all 3 scores without any obvious adverse events (P=.004, P=.006, and P=.017, respectively). This novel combination treatment may serve as a safe and effective therapeutic approach for keloid removal.
Final Thoughts
Emerging treatments offer promising new horizons in keloid management; however, the lack of robust, high-quality clinical trials, especially those focusing on
Keloids are fibroproliferative lesions caused by aberrant wound healing in predisposed individuals.1 While keloids have been reported in patients of all races and ethnicities, they most commonly develop in individuals of African or Asian descent.2 Often associated with symptoms such as pain and itching, keloids can be disfiguring and result in poorer quality of life.3 There is a paucity of research on keloid pathogenesis and efficacious therapeutics, particularly in patients with skin of color (SOC). Herein, we outline the current research on keloid treatment and highlight promising new therapies ranging from innovative intralesional techniques to advanced laser-based and biologic therapies.
Deficiencies in Skin of Color Research
Although keloids are 17 times more prevalent in patients with SOC,4 there is a considerable lack of focus on this population in the literature.5 Studies on keloids that include individuals with SOC often group patients of all skin types together, and subgroup analyses are not always performed.6,7 As a result, dermatologists may face considerable challenges in providing effective treatments for keloids in patients with SOC. With few evidence-based options available, patients with SOC who have keloids continue to experience impairments in quality of life.
Common Keloid Therapies
There currently is no gold-standard treatment for keloids. Common therapeutic modalities include intralesional corticosteroids (ILCs), antineoplastic agents and neuromodulators, laser-based devices, and surgical therapies (eg, excision), as well as combined medical and surgical techniques.8
Intralesional Corticosteroids—Minimally invasive ILCs are the first-line treatment in all patients with keloids, regardless of skin phototype. Because keloid formation results from trauma to the skin, ILCs often are recommended to minimize further skin damage.5 One meta-analysis found that ILCs have demonstrated success rates of 50% to 100%9; however, these studies frequently combine ILCs with other treatment modalities, and few studies have focused on the efficacy of ILC monotherapy in patients with SOC.6,10-13
Antineoplastic Agents and Neuromodulators—Certain antineoplastic agents (eg, 5-fluorouracil [5-FU] and bleomycin) and neuromodulators (eg, botulinum toxin A [BTA]) also have been studied in keloid management.8
5-Fluorouracil frequently is combined with ILCs such as triamcinolone (TAC). Combined therapy is more effective than TAC monotherapy in scar height reduction.14,15 Rates of adverse events such as dyspigmentation, atrophy, and telangiectasias also were lower in patients who received combined therapy.14,15 A systematic review found that intralesional bleomycin may be more effective than TAC alone, 5-FU alone, TAC combined with 5-FU, and TAC combined with cryotherapy; however, hyperpigmentation was a common adverse event, occurring in roughly 70% (42/60) of patients.16,17 Additionally, a 2024 meta-analysis evaluated 20 randomized controlled trials comprising 1114 patients treated with intralesional TAC, 5-FU, BTA, verapamil, and/or bleomycin. Botulinum toxin A and TAC plus 5-FU were found to have outstanding therapeutic efficacy for keloids, and rates of adverse events were similar among users of TAC, 5-FU, BTA, and TAC plus 5-FU.18
While antineoplastic agents and BTA may be promising keloid therapies, further studies demonstrating their efficacy and safety profiles are necessary, particularly regarding dyspigmentation as a potential adverse event, as this may be of concern in patients with darker phototypes.
Laser Therapies—Of all treatment modalities, laser-based keloid therapies have been the most robustly studied in SOC. The 2 main types are ablative (eg, CO2, Er:YAG) and nonablative (eg, pulsed dye, Nd:YAG) lasers. Ablative lasers rapidly heat water molecules within the skin, thereby vaporizing the skin cells in a controlled precise process that reduces scar tissue by removing layers of skin. Nonablative lasers target hemoglobin in blood vessels, reducing oxygen supply and inducing collagen remodeling without damaging the epidermis.19
For patients with SOC, lasers carry a risk for postinflammatory hyperpigmentation.20 To address this risk, recent advancements in laser technology and procedural protocols have aimed to minimize the number of passes and utilize cooling devices21; however, many of these recommendations are based on retrospective reviews and small case series. A 2024 meta-analysis comprising 550 patients found that the combination of fractional CO2 laser therapy and 5-FU was the most effective intervention, markedly reducing Vancouver Scar Scale and pliability scores as well as keloid thickness.22 Conversely, pulsed dye lasers were the least effective in terms of improving scar thickness, pigmentation, and pliability when compared to other treatments.
Randomized controlled trials of laser-based therapies in patients with SOC are lacking in the literature. Future studies should focus on calibrating laser-based therapies for those with darker skin tones and examine the efficacy and adverse effects of ablative and nonablative lasers in patients with SOC.
Promising New Keloid Therapies
Keloid disease pathogenesis is incompletely understood, but several new therapeutic targets have been highlighted in the literature, including dupilumab, pentoxifylline, sirtuin 6 (SIRT6) modulators, remdesivir, and needle-assisted electrocoagulation plus pharmacotherapy.
Dupilumab—An anti–IL-4 and IL-13 monoclonal antibody, dupilumab was first approved for the treatment of severe atopic dermatitis. Its use has broadened since its approval, and keloids have been identified as a potential therapeutic target. A 2019 case study described a 53-year-old Black man with severe atopic dermatitis and chronic keloids that regressed with systemic dupilumab therapy.23 This prompted a follow-up case-control study using real-time polymerase chain reaction testing to evaluate Th2 gene expression (IL-4R, IL-13, and CCL18) of lesional and nonlesional tissue in 3 Black patients with chronic keloids and no concurrent atopic dermatitis vs 5 healthy Black controls. Despite the limited sample size, a significant increase in IL-13 and the Th2 chemokine CCL18 was found in patients with keloids compared to controls (P<.05), suggesting that the entire integument of patients with severe keloids is abnormal.23 This finding supports the use of systemic treatments for chronic and multifocal keloid disease. Several subsequent case reports have corroborated the efficacy of systemic and/or intralesional dupilumab.24,25 However, some studies have reported contradictory findings, suggesting the need for high-quality clinical trials.26,27
Pentoxifylline—Pentoxifylline is a methylated xanthine derivative and a nonspecific phosphodiesterase inhibitor used to treat claudication from peripheral artery disease. It also inhibits the proliferation and rate of collagen synthesis of fibroblasts from keloids in vitro.28,29 A 2019 retrospective, open-label pilot study analyzed postsurgical keloid recurrence in 45 patients with 67 unique keloids that were stratified into low- and high-risk groups based on clinical factors including multiple symptomatic keloids, history of recurrence, and family history.30 Both the low- and the high-risk groups were treated with 40 mg/mL intralesional triamcinolone acetonide monthly for 6 months; however, some of the high-risk keloids also received pentoxifylline 300 mg 3 times daily for 6 months. There was a statistically significant decrease in keloid recurrence rate between the high-risk group treated with pentoxifylline and the low-risk group for whom pentoxifylline was not prescribed (P=.015).
Similarly, a randomized clinical trial comparing the efficacy of combination intralesional pentoxifylline and intralesional triamcinolone vs monotherapy with pentoxifylline or triamcinolone found the most significant improvement in the combination cohort with reduction in keloid height (P=.04), pliability (P=.003), and vascularity (P=.05).31 These findings highlight the need for supplementary studies on the use of pentoxifylline for keloid therapy.
SIRT6 Modulators—SIRT6 modulators are an exciting future therapeutic target. In a recent case-control study evaluating the histologic milieu of keloid tissue vs normal skin specimens, the researchers found that selective overexpression of SIRT6 via the use of a recombinant adenovirus in keloid fibroblasts attenuated proliferation, invasion, and collagen synthesis while fostering apoptosis, likely through the suppression of MAPK/ERK pathway activity.32
Remdesivir—The antiviral drug remdesivir has been reported to have pharmacologic activities in a wide range of fibrotic diseases, including keloids. A 2024 study explored the potential effect and mechanisms of remdesivir on skin fibrosis both in vitro and in rodents.33 Remdesivir was found to decrease skin fibrosis and attenuate the gross weight of keloid tissues in vivo, suppress fibroblast activation and autophagy both in vivo and in vitro, dampen fibroblast activation by the TGF-β1/Smad signaling pathway, and inhibit fibroblasts autophagy by the PI3K/Akt/mTOR signaling pathway. These results demonstrate the therapeutic potential of remdesivir for keloid management.
Needle-Assisted Electrocoagulation Plus Pharmacotherapy—A novel needle-assisted electrocoagulation technique combined with pharmacotherapy (corticosteroid and 5-FU injections) was effective in a Chinese clinical trial involving 6 patients with keloids.34 Investigators used Vancouver Scar Scale and both Patient and Observer Scar Assessment Scale scores to grade patients’ scars before treatment and 1 month after the first treatment cycle. They found that ablation combined with pharmacotherapy significantly reduced all 3 scores without any obvious adverse events (P=.004, P=.006, and P=.017, respectively). This novel combination treatment may serve as a safe and effective therapeutic approach for keloid removal.
Final Thoughts
Emerging treatments offer promising new horizons in keloid management; however, the lack of robust, high-quality clinical trials, especially those focusing on
- Téot L, Mustoe TA, Middelkoop E, eds. Textbook on Scar Management: State of the Art Management and Emerging Technologies. Springer; 2020.
- Davis SA, Feldman SR, McMichael AJ. Management of keloids in the United States, 1990-2009: an analysis of the National Ambulatory Medical Care Survey. Dermatol Surg. 2013;39:988-994. doi:10.1111/dsu.12182
- Kassi K, Kouame K, Kouassi A, et al. Quality of life in black African patients with keloid scars. Dermatol Reports. 2020;12:8312. doi:10.4081/dr.2020.8312
- Delaleu J, Charvet E, Petit A. Keloid disease: review with clinical atlas. part I: definitions, history, epidemiology, clinics and diagnosis. Ann Dermatol Venereol. 2023;150:3-15.
doi:10.1016/j.annder.2022.08.010 - Bronte J, Zhou C, Vempati A, et al. A comprehensive review of non-surgical treatments for hypertrophic and keloid scars in skin of color. Clin Cosmet Investig Dermatol.
2024;17:1459-1469. doi:10.2147/CCID.S470997 - Davison SP, Dayan JH, Clemens MW, et al. Efficacy of intralesional 5-fluorouracil and triamcinolone in the treatment of keloids. Aesthet Surg J. 2009;29:40-46. doi:10.1016/j.asj.2008.11.006
- Azzam OA, Bassiouny DA, El-Hawary MS, et al. Treatment of hypertrophic scars and keloids by fractional carbon dioxide laser: a clinical, histological, and immunohistochemical study. Lasers Med Sci. 2016;31:9-18. doi:10.1007/s10103-015-1824-4
- Ekstein SF, Wyles SP, Moran SL, et al. Keloids: a review of therapeutic management. Int J Dermatol. 2021;60:661-671. doi:10.1111/ijd.15159
- Morelli Coppola M, Salzillo R, Segreto F, et al. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:387-396. doi:10.2147/CCID.S133672
- Kant SB, van den Kerckhove E, Colla C, et al. A new treatment of hypertrophic and keloid scars with combined triamcinolone and verapamil: a retrospective study. Eur J Plast Surg. 2018;41:69-80. doi:10.1007/s00238-017-1322-y
- Cohen AJ, Talasila S, Lazarevic B, et al. Combination cryotherapy and intralesional corticosteroid versus steroid monotherapy in the treatment of keloids. J Cosmet Dermatol. 2023;22:932-936. doi:10.1111/jocd.15520
- Tawaranurak N, Pliensiri P, Tawaranurak K. Combination of fractional carbon dioxide laser and topical triamcinolone vs intralesional triamcinolone for keloid treatment: a randomised clinical trial. Int Wound J. 2022;19:1729-1735. doi:10.1111/iwj.13775
- Belie O, Ugburo AO, Mofikoya BO, et al. A comparison of intralesional verapamil and triamcinolone monotherapy in the treatment of keloids in an African population. Niger J Clin Pract. 2021;24:986-992. doi:10.4103/njcp.njcp_474_20
- Khalid FA, Mehrose MY, Saleem M, et al. Comparison of efficacy and safety of intralesional triamcinolone and combination of triamcinolone with 5-fluorouracil in the treatment of keloids and hypertrophic scars: randomised control trial. Burns. 2019;45:69-75. doi:10.1016/j.burns.2018.08.011
- Asilian A, Darougheh A, Shariati F. New combination of triamcinolone, 5-Fluorouracil, and pulsed-dye laser for treatment of keloid and hypertrophic scars. Dermatol Surg. 2006;32:907-915. doi:10.1111/j.1524-4725.2006.32195.x
- Kim WI, Kim S, Cho SW, et al. The efficacy of bleomycin for treating keloid and hypertrophic scar: a systematic review and meta-analysis. J Cosmet Dermatol. 2020;19:3357-3366. doi:10.1111/jocd.13390
- Kabel A, Sabry H, Sorour N, et al. Comparative study between intralesional injection of bleomycin and 5-fluorouracil in the treatment of keloids and hypertrophic scars. J Dermatol Dermatol Surg. 2016;20:32-38.
- Yang HA, Jheng WL, Yu J, et al. Comparative efficacy of drug interventions for keloids: a network meta-analysis. Ann Plast Surg. 2024;92(1S suppl 1
):S52-S59. doi:10.1097/SAP.0000000000003759 - Preissig J, Hamilton K, Markus R. Current laser resurfacing technologies: a review that delves beneath the surface. Semin Plast Surg. 2012;26:109-116. doi:10.1055/s-0032-1329413
- Bin Dakhil A, Shadid A, Altalhab S. Post-inflammatory hyperpigmentation after carbon dioxide laser: review of prevention and risk factors. Dermatol Reports. 2023;15:9703. doi:10.4081/dr.2023.9703
- Kaushik SB, Alexis AF. Nonablative fractional laser resurfacing in skin of color: evidence-based review. J Clin Aesthet Dermatol. 2017;10:51-67.
- Foppiani JA, Khaity A, Al-Dardery NM, et al. Laser therapy in hypertrophic and keloid scars: a systematic review and network meta-analysis. Aesthetic Plast Surg. Published May 17, 2024. doi:10.1007/s00266-024-04027-9
- Diaz A, Tan K, He H, et al. Keloid lesions show increased IL-4/IL-13 signaling and respond to Th2-targeting dupilumab therapy. J Eur Acad Dermatol Venereol. 2020;34:E161-E164. doi:10.1111/jdv.16097
- Min MS,
Mazori DR, Lee MS, et al. Successful treatment of keloids and hypertrophic scars with systemic and intralesional dupilumab. J Drugs Dermatol. 2023;22:1220-1222. doi:10.36849/JDD.6385 - Wittmer A, Finklea L, Joseph J. Effects of dupilumab on keloid stabilization and prevention. JAAD Case Rep. 2023;37:103-105. doi:10.1016/j.jdcr.2023.05.001
- Luk K, Fakhoury J, Ozog D. Nonresponse and progression of diffuse keloids to dupilumab therapy. J Drugs Dermatol. 2022;21:197-199. doi:10.36849/jdd.6252
- Tirgan MH, Uitto J. Lack of efficacy of dupilumab in the treatment of keloid disorder. J Eur Acad Dermatol Venereol. 2022;36:E120-E122. doi:10.1111/jdv.17669
- Berman B, Duncan MR. Pentoxifylline inhibits the proliferation of human fibroblasts derived from keloid, scleroderma and morphoea skin and their production of collagen, glycosaminoglycans and fibronectin. Br J Dermatol. 1990;123:339-346. doi:10.1111/j.1365-
2133.1990.tb06294.x - Berman B, Duncan MR. Pentoxifylline inhibits normal human dermal fibroblast in vitro proliferation, collagen, glycosaminoglycan, and fibronectin production, and increases collagenase activity. J Invest Dermatol. 1989;92:605-610.
- Tan A, Martinez Luna O, Glass DA 2nd. Pentoxifylline for the prevention of postsurgical keloid recurrence. Dermatol Surg. 2020;46:1353-1356. doi:10.1097/DSS.0000000000002090
- Serag-Eldin YMA, Mahmoud WH, Gamea MM, et al. Intralesional pentoxifylline, triamcinolone acetonide, and their combination for treatment of keloid scars. J Cosmet Dermatol. 2021;20:3330-3340. doi:10.1111/jocd.14305
- Zhou T, Chen Y, Wang C, et al. SIRT6 inhibits the proliferation and collagen synthesis of keloid fibroblasts through MAPK/ERK pathway. Discov Med. 2024;36:1430-1440. doi:10.24976/Discov.Med.202436186.133
- Zhang J, Zhang X, Guo X, et al. Remdesivir alleviates skin fibrosis by suppressing TGF-β1 signaling pathway. PLoS One. 2024;19:E0305927.
doi:10.1371/journal.pone.0305927 - Zhao J, Zhai X, Xu Z, et al. Novel needle-type electrocoagulation and combination pharmacotherapy: basic and clinical studies on efficacy and safety in treating keloids. J Cosmet Dermatol. doi:10.1111/jocd.16453
- Téot L, Mustoe TA, Middelkoop E, eds. Textbook on Scar Management: State of the Art Management and Emerging Technologies. Springer; 2020.
- Davis SA, Feldman SR, McMichael AJ. Management of keloids in the United States, 1990-2009: an analysis of the National Ambulatory Medical Care Survey. Dermatol Surg. 2013;39:988-994. doi:10.1111/dsu.12182
- Kassi K, Kouame K, Kouassi A, et al. Quality of life in black African patients with keloid scars. Dermatol Reports. 2020;12:8312. doi:10.4081/dr.2020.8312
- Delaleu J, Charvet E, Petit A. Keloid disease: review with clinical atlas. part I: definitions, history, epidemiology, clinics and diagnosis. Ann Dermatol Venereol. 2023;150:3-15.
doi:10.1016/j.annder.2022.08.010 - Bronte J, Zhou C, Vempati A, et al. A comprehensive review of non-surgical treatments for hypertrophic and keloid scars in skin of color. Clin Cosmet Investig Dermatol.
2024;17:1459-1469. doi:10.2147/CCID.S470997 - Davison SP, Dayan JH, Clemens MW, et al. Efficacy of intralesional 5-fluorouracil and triamcinolone in the treatment of keloids. Aesthet Surg J. 2009;29:40-46. doi:10.1016/j.asj.2008.11.006
- Azzam OA, Bassiouny DA, El-Hawary MS, et al. Treatment of hypertrophic scars and keloids by fractional carbon dioxide laser: a clinical, histological, and immunohistochemical study. Lasers Med Sci. 2016;31:9-18. doi:10.1007/s10103-015-1824-4
- Ekstein SF, Wyles SP, Moran SL, et al. Keloids: a review of therapeutic management. Int J Dermatol. 2021;60:661-671. doi:10.1111/ijd.15159
- Morelli Coppola M, Salzillo R, Segreto F, et al. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:387-396. doi:10.2147/CCID.S133672
- Kant SB, van den Kerckhove E, Colla C, et al. A new treatment of hypertrophic and keloid scars with combined triamcinolone and verapamil: a retrospective study. Eur J Plast Surg. 2018;41:69-80. doi:10.1007/s00238-017-1322-y
- Cohen AJ, Talasila S, Lazarevic B, et al. Combination cryotherapy and intralesional corticosteroid versus steroid monotherapy in the treatment of keloids. J Cosmet Dermatol. 2023;22:932-936. doi:10.1111/jocd.15520
- Tawaranurak N, Pliensiri P, Tawaranurak K. Combination of fractional carbon dioxide laser and topical triamcinolone vs intralesional triamcinolone for keloid treatment: a randomised clinical trial. Int Wound J. 2022;19:1729-1735. doi:10.1111/iwj.13775
- Belie O, Ugburo AO, Mofikoya BO, et al. A comparison of intralesional verapamil and triamcinolone monotherapy in the treatment of keloids in an African population. Niger J Clin Pract. 2021;24:986-992. doi:10.4103/njcp.njcp_474_20
- Khalid FA, Mehrose MY, Saleem M, et al. Comparison of efficacy and safety of intralesional triamcinolone and combination of triamcinolone with 5-fluorouracil in the treatment of keloids and hypertrophic scars: randomised control trial. Burns. 2019;45:69-75. doi:10.1016/j.burns.2018.08.011
- Asilian A, Darougheh A, Shariati F. New combination of triamcinolone, 5-Fluorouracil, and pulsed-dye laser for treatment of keloid and hypertrophic scars. Dermatol Surg. 2006;32:907-915. doi:10.1111/j.1524-4725.2006.32195.x
- Kim WI, Kim S, Cho SW, et al. The efficacy of bleomycin for treating keloid and hypertrophic scar: a systematic review and meta-analysis. J Cosmet Dermatol. 2020;19:3357-3366. doi:10.1111/jocd.13390
- Kabel A, Sabry H, Sorour N, et al. Comparative study between intralesional injection of bleomycin and 5-fluorouracil in the treatment of keloids and hypertrophic scars. J Dermatol Dermatol Surg. 2016;20:32-38.
- Yang HA, Jheng WL, Yu J, et al. Comparative efficacy of drug interventions for keloids: a network meta-analysis. Ann Plast Surg. 2024;92(1S suppl 1
):S52-S59. doi:10.1097/SAP.0000000000003759 - Preissig J, Hamilton K, Markus R. Current laser resurfacing technologies: a review that delves beneath the surface. Semin Plast Surg. 2012;26:109-116. doi:10.1055/s-0032-1329413
- Bin Dakhil A, Shadid A, Altalhab S. Post-inflammatory hyperpigmentation after carbon dioxide laser: review of prevention and risk factors. Dermatol Reports. 2023;15:9703. doi:10.4081/dr.2023.9703
- Kaushik SB, Alexis AF. Nonablative fractional laser resurfacing in skin of color: evidence-based review. J Clin Aesthet Dermatol. 2017;10:51-67.
- Foppiani JA, Khaity A, Al-Dardery NM, et al. Laser therapy in hypertrophic and keloid scars: a systematic review and network meta-analysis. Aesthetic Plast Surg. Published May 17, 2024. doi:10.1007/s00266-024-04027-9
- Diaz A, Tan K, He H, et al. Keloid lesions show increased IL-4/IL-13 signaling and respond to Th2-targeting dupilumab therapy. J Eur Acad Dermatol Venereol. 2020;34:E161-E164. doi:10.1111/jdv.16097
- Min MS,
Mazori DR, Lee MS, et al. Successful treatment of keloids and hypertrophic scars with systemic and intralesional dupilumab. J Drugs Dermatol. 2023;22:1220-1222. doi:10.36849/JDD.6385 - Wittmer A, Finklea L, Joseph J. Effects of dupilumab on keloid stabilization and prevention. JAAD Case Rep. 2023;37:103-105. doi:10.1016/j.jdcr.2023.05.001
- Luk K, Fakhoury J, Ozog D. Nonresponse and progression of diffuse keloids to dupilumab therapy. J Drugs Dermatol. 2022;21:197-199. doi:10.36849/jdd.6252
- Tirgan MH, Uitto J. Lack of efficacy of dupilumab in the treatment of keloid disorder. J Eur Acad Dermatol Venereol. 2022;36:E120-E122. doi:10.1111/jdv.17669
- Berman B, Duncan MR. Pentoxifylline inhibits the proliferation of human fibroblasts derived from keloid, scleroderma and morphoea skin and their production of collagen, glycosaminoglycans and fibronectin. Br J Dermatol. 1990;123:339-346. doi:10.1111/j.1365-
2133.1990.tb06294.x - Berman B, Duncan MR. Pentoxifylline inhibits normal human dermal fibroblast in vitro proliferation, collagen, glycosaminoglycan, and fibronectin production, and increases collagenase activity. J Invest Dermatol. 1989;92:605-610.
- Tan A, Martinez Luna O, Glass DA 2nd. Pentoxifylline for the prevention of postsurgical keloid recurrence. Dermatol Surg. 2020;46:1353-1356. doi:10.1097/DSS.0000000000002090
- Serag-Eldin YMA, Mahmoud WH, Gamea MM, et al. Intralesional pentoxifylline, triamcinolone acetonide, and their combination for treatment of keloid scars. J Cosmet Dermatol. 2021;20:3330-3340. doi:10.1111/jocd.14305
- Zhou T, Chen Y, Wang C, et al. SIRT6 inhibits the proliferation and collagen synthesis of keloid fibroblasts through MAPK/ERK pathway. Discov Med. 2024;36:1430-1440. doi:10.24976/Discov.Med.202436186.133
- Zhang J, Zhang X, Guo X, et al. Remdesivir alleviates skin fibrosis by suppressing TGF-β1 signaling pathway. PLoS One. 2024;19:E0305927.
doi:10.1371/journal.pone.0305927 - Zhao J, Zhai X, Xu Z, et al. Novel needle-type electrocoagulation and combination pharmacotherapy: basic and clinical studies on efficacy and safety in treating keloids. J Cosmet Dermatol. doi:10.1111/jocd.16453
When Your Malpractice Insurer Investigates You: What to Know
When psychiatrist Paul Sartain, MD (not his real name), received a letter from his state’s medical board, he was concerned. A patient’s family complained that he made sexual advances to a young woman he treated for psychotic depression.
“There was absolutely no evidence, and the claims were vague,” he said. “I think the family was angry at me and with the system — the woman had not gotten better.” Sartain reviewed his medical records and then called his malpractice insurer.
The insurer asked about his involvement with the patient’s case, if there was anything credible to the patient’s complaint, and if he had thorough documentation. Then, the carrier offered Sartain his choice of several attorneys who could represent him. The medical board ultimately closed the case with no findings against him, and the patient’s family never sued him.
“If I’m wrongly accused, I’m defended (by the carrier). If I had stolen money or had a sexual relationship with the patient, then you’re acting outside the bounds of what is protected (by the carrier),” he said.
How Medical Board and Malpractice Insurer Investigations Differ
Medical board complaints differ from malpractice claims, in which patients seek damages. The investigation process also varies.
When a patient reports a doctor to a state medical board, they may also sue the doctor for monetary damages in civil court. The medical board responds to patient complaints made directly to them, but it also may also initiate its own investigations. Those can be prompted by a malpractice claim resolution, with a court verdict against the doctor, or a settlement recorded in the National Practitioner Data Bank.
Malpractice insurers may offer limited legal representation for medical board investigations, requiring the doctor to report the medical board issue to them before the doctor takes any action. Often, they will cover up to $50,000 in defense costs but not cover any subsequent medical board fines or required classes or medical board fees.
When a doctor contacts the carrier about a medical board investigation, the carrier may ask for the medical board document and the medical records, said Alex Keoskey, a partner in Frier Levitt’s life sciences group.
The carrier may want to ask about the patient, staff members involved, the doctor’s background, if there have been previous medical board investigations or lawsuits against this doctor, and the doctor’s opinion of the allegations. The doctor should be transparent with the carrier, Keoskey said.
Some carriers conduct more in-depth investigations, examining record-keeping, prescription practices, patient consent processes, and continuing medical education status. That’s because the medical board may inquire about these as well should its own investigation expand.
Not all carriers explore cases like these, even if reimbursing for defense costs, said Karen Frisella, director of professional liability claims at BETA Healthcare Group in California. In her experience, a licensing investigation usually follows a claim resolution that was already worked up by the carrier. If a complaint was made directly to the licensing board without an accompanying liability claim, the carrier’s ability to initiate an investigation on the incident depends on the policy terms or coverage available.
“Typically, a professional liability policy requires that the insured report a claim to trigger coverage. The carrier can’t unilaterally decide to open a claim,” she said. A licensing board investigation is not a claim by definition and therefore does not provide a mechanism for the carrier to open a liability claim file, she added.
If the medical board ultimately restricts the doctor’s license or puts the doctor on probation, that becomes public, and the underwriting department may then look into it.
Malpractice insurers routinely monitor licensing board discipline notices. A reprimand or restrictions on a doctor’s license could trigger a review of the physician’s future insurability and lead to higher premiums or even nonrenewal, Frisella said.
If a carrier investigates a reported claim and determines there are issues with the care rendered, whether there is an accompanying medical board action, that also can affect underwriting decisions, Frisella said.
Who Is Your Attorney Really Working for?
The doctor should understand whose interests the attorney represents. In a medical board claim, the attorney — even if defense is paid by the carrier — represents the doctor.
Frisella said her organization provides pass-through coverage, meaning it reimburses the doctor for medical board defense costs. “Because the carrier isn’t directing the medical board defense, it is not generally privy to the work product.”
If a patient files a malpractice claim, however, the attorney ultimately represents the insurance company.
“The panel counsel who works for the insurer does not work for the doctor, and that’s always important to remember,” Keoskey said. While the attorney will do their best to aggressively defend the doctor, “he’s going to protect the insurer’s interest before the doctor’s.”
Physicians who find any conflict of interest with their insurer should seek counsel.
Such conflicts could include:
- Disagreements over the case’s ultimate worth. For example, a physician might want a case to settle for less than their carrier is willing to pay.
- The legal judgment may exceed the carrier’s policy limits, or there are punitive damages or allegations of criminal acts that the insurer does not cover.
In these cases, the insurance company should recommend the doctor get personal counsel. They will send a reservation of rights letter saying they will defend the doctor for now, but if the facts show the doctor committed some type of misconduct, they may decline coverage, said Keoskey. Some states, including California, require that the carrier pay for this independent counsel.
Unless there is a conflict of interest, though, having a personal attorney just makes the situation more complicated, said Frisella.
A version of this article first appeared on Medscape.com.
When psychiatrist Paul Sartain, MD (not his real name), received a letter from his state’s medical board, he was concerned. A patient’s family complained that he made sexual advances to a young woman he treated for psychotic depression.
“There was absolutely no evidence, and the claims were vague,” he said. “I think the family was angry at me and with the system — the woman had not gotten better.” Sartain reviewed his medical records and then called his malpractice insurer.
The insurer asked about his involvement with the patient’s case, if there was anything credible to the patient’s complaint, and if he had thorough documentation. Then, the carrier offered Sartain his choice of several attorneys who could represent him. The medical board ultimately closed the case with no findings against him, and the patient’s family never sued him.
“If I’m wrongly accused, I’m defended (by the carrier). If I had stolen money or had a sexual relationship with the patient, then you’re acting outside the bounds of what is protected (by the carrier),” he said.
How Medical Board and Malpractice Insurer Investigations Differ
Medical board complaints differ from malpractice claims, in which patients seek damages. The investigation process also varies.
When a patient reports a doctor to a state medical board, they may also sue the doctor for monetary damages in civil court. The medical board responds to patient complaints made directly to them, but it also may also initiate its own investigations. Those can be prompted by a malpractice claim resolution, with a court verdict against the doctor, or a settlement recorded in the National Practitioner Data Bank.
Malpractice insurers may offer limited legal representation for medical board investigations, requiring the doctor to report the medical board issue to them before the doctor takes any action. Often, they will cover up to $50,000 in defense costs but not cover any subsequent medical board fines or required classes or medical board fees.
When a doctor contacts the carrier about a medical board investigation, the carrier may ask for the medical board document and the medical records, said Alex Keoskey, a partner in Frier Levitt’s life sciences group.
The carrier may want to ask about the patient, staff members involved, the doctor’s background, if there have been previous medical board investigations or lawsuits against this doctor, and the doctor’s opinion of the allegations. The doctor should be transparent with the carrier, Keoskey said.
Some carriers conduct more in-depth investigations, examining record-keeping, prescription practices, patient consent processes, and continuing medical education status. That’s because the medical board may inquire about these as well should its own investigation expand.
Not all carriers explore cases like these, even if reimbursing for defense costs, said Karen Frisella, director of professional liability claims at BETA Healthcare Group in California. In her experience, a licensing investigation usually follows a claim resolution that was already worked up by the carrier. If a complaint was made directly to the licensing board without an accompanying liability claim, the carrier’s ability to initiate an investigation on the incident depends on the policy terms or coverage available.
“Typically, a professional liability policy requires that the insured report a claim to trigger coverage. The carrier can’t unilaterally decide to open a claim,” she said. A licensing board investigation is not a claim by definition and therefore does not provide a mechanism for the carrier to open a liability claim file, she added.
If the medical board ultimately restricts the doctor’s license or puts the doctor on probation, that becomes public, and the underwriting department may then look into it.
Malpractice insurers routinely monitor licensing board discipline notices. A reprimand or restrictions on a doctor’s license could trigger a review of the physician’s future insurability and lead to higher premiums or even nonrenewal, Frisella said.
If a carrier investigates a reported claim and determines there are issues with the care rendered, whether there is an accompanying medical board action, that also can affect underwriting decisions, Frisella said.
Who Is Your Attorney Really Working for?
The doctor should understand whose interests the attorney represents. In a medical board claim, the attorney — even if defense is paid by the carrier — represents the doctor.
Frisella said her organization provides pass-through coverage, meaning it reimburses the doctor for medical board defense costs. “Because the carrier isn’t directing the medical board defense, it is not generally privy to the work product.”
If a patient files a malpractice claim, however, the attorney ultimately represents the insurance company.
“The panel counsel who works for the insurer does not work for the doctor, and that’s always important to remember,” Keoskey said. While the attorney will do their best to aggressively defend the doctor, “he’s going to protect the insurer’s interest before the doctor’s.”
Physicians who find any conflict of interest with their insurer should seek counsel.
Such conflicts could include:
- Disagreements over the case’s ultimate worth. For example, a physician might want a case to settle for less than their carrier is willing to pay.
- The legal judgment may exceed the carrier’s policy limits, or there are punitive damages or allegations of criminal acts that the insurer does not cover.
In these cases, the insurance company should recommend the doctor get personal counsel. They will send a reservation of rights letter saying they will defend the doctor for now, but if the facts show the doctor committed some type of misconduct, they may decline coverage, said Keoskey. Some states, including California, require that the carrier pay for this independent counsel.
Unless there is a conflict of interest, though, having a personal attorney just makes the situation more complicated, said Frisella.
A version of this article first appeared on Medscape.com.
When psychiatrist Paul Sartain, MD (not his real name), received a letter from his state’s medical board, he was concerned. A patient’s family complained that he made sexual advances to a young woman he treated for psychotic depression.
“There was absolutely no evidence, and the claims were vague,” he said. “I think the family was angry at me and with the system — the woman had not gotten better.” Sartain reviewed his medical records and then called his malpractice insurer.
The insurer asked about his involvement with the patient’s case, if there was anything credible to the patient’s complaint, and if he had thorough documentation. Then, the carrier offered Sartain his choice of several attorneys who could represent him. The medical board ultimately closed the case with no findings against him, and the patient’s family never sued him.
“If I’m wrongly accused, I’m defended (by the carrier). If I had stolen money or had a sexual relationship with the patient, then you’re acting outside the bounds of what is protected (by the carrier),” he said.
How Medical Board and Malpractice Insurer Investigations Differ
Medical board complaints differ from malpractice claims, in which patients seek damages. The investigation process also varies.
When a patient reports a doctor to a state medical board, they may also sue the doctor for monetary damages in civil court. The medical board responds to patient complaints made directly to them, but it also may also initiate its own investigations. Those can be prompted by a malpractice claim resolution, with a court verdict against the doctor, or a settlement recorded in the National Practitioner Data Bank.
Malpractice insurers may offer limited legal representation for medical board investigations, requiring the doctor to report the medical board issue to them before the doctor takes any action. Often, they will cover up to $50,000 in defense costs but not cover any subsequent medical board fines or required classes or medical board fees.
When a doctor contacts the carrier about a medical board investigation, the carrier may ask for the medical board document and the medical records, said Alex Keoskey, a partner in Frier Levitt’s life sciences group.
The carrier may want to ask about the patient, staff members involved, the doctor’s background, if there have been previous medical board investigations or lawsuits against this doctor, and the doctor’s opinion of the allegations. The doctor should be transparent with the carrier, Keoskey said.
Some carriers conduct more in-depth investigations, examining record-keeping, prescription practices, patient consent processes, and continuing medical education status. That’s because the medical board may inquire about these as well should its own investigation expand.
Not all carriers explore cases like these, even if reimbursing for defense costs, said Karen Frisella, director of professional liability claims at BETA Healthcare Group in California. In her experience, a licensing investigation usually follows a claim resolution that was already worked up by the carrier. If a complaint was made directly to the licensing board without an accompanying liability claim, the carrier’s ability to initiate an investigation on the incident depends on the policy terms or coverage available.
“Typically, a professional liability policy requires that the insured report a claim to trigger coverage. The carrier can’t unilaterally decide to open a claim,” she said. A licensing board investigation is not a claim by definition and therefore does not provide a mechanism for the carrier to open a liability claim file, she added.
If the medical board ultimately restricts the doctor’s license or puts the doctor on probation, that becomes public, and the underwriting department may then look into it.
Malpractice insurers routinely monitor licensing board discipline notices. A reprimand or restrictions on a doctor’s license could trigger a review of the physician’s future insurability and lead to higher premiums or even nonrenewal, Frisella said.
If a carrier investigates a reported claim and determines there are issues with the care rendered, whether there is an accompanying medical board action, that also can affect underwriting decisions, Frisella said.
Who Is Your Attorney Really Working for?
The doctor should understand whose interests the attorney represents. In a medical board claim, the attorney — even if defense is paid by the carrier — represents the doctor.
Frisella said her organization provides pass-through coverage, meaning it reimburses the doctor for medical board defense costs. “Because the carrier isn’t directing the medical board defense, it is not generally privy to the work product.”
If a patient files a malpractice claim, however, the attorney ultimately represents the insurance company.
“The panel counsel who works for the insurer does not work for the doctor, and that’s always important to remember,” Keoskey said. While the attorney will do their best to aggressively defend the doctor, “he’s going to protect the insurer’s interest before the doctor’s.”
Physicians who find any conflict of interest with their insurer should seek counsel.
Such conflicts could include:
- Disagreements over the case’s ultimate worth. For example, a physician might want a case to settle for less than their carrier is willing to pay.
- The legal judgment may exceed the carrier’s policy limits, or there are punitive damages or allegations of criminal acts that the insurer does not cover.
In these cases, the insurance company should recommend the doctor get personal counsel. They will send a reservation of rights letter saying they will defend the doctor for now, but if the facts show the doctor committed some type of misconduct, they may decline coverage, said Keoskey. Some states, including California, require that the carrier pay for this independent counsel.
Unless there is a conflict of interest, though, having a personal attorney just makes the situation more complicated, said Frisella.
A version of this article first appeared on Medscape.com.
The Rise of Sham Peer Reviews
While a medical peer review occurs once a patient, fellow doctor, or staff member reports that a physician failed to treat a patient up to standards or acted improperly, a “sham peer review” is undertaken for ulterior motives.
They’re typically undertaken due to professional competition or institutional politics rather than to promote quality care or uphold professional standards.
Physicians should be concerned. In a soon-to-be-published Medscape report on peer reviews, 56% of US physicians surveyed expressed higher levels of concern that a peer review could be misused to punish a physician for reasons unrelated to the matter being reviewed.
This is a troublesome issue, and many doctors may not be aware of it or how often it occurs.
“The biggest misconception about sham peer reviews is a denial of how pervasive they are,” said Andy Schlafly, general counsel for the Association of American Physicians and Surgeons (AAPS), which offers a free legal consultation service for physicians facing a sham peer review. “Many hospital administrations are as dangerous to good physicians as street gangs can be in a crime-ridden neighborhood.”
“Physicians should become aware of whether sham peer reviews are prevalent at their hospital and, if so, those physicians should look to practice somewhere else,” Schlafly said in an interview.
Unfortunately, there are limited data on how often this happens. When it does, it can be a career killer, said Lawrence Huntoon, MD, PhD, who has run the AAPS sham peer review hotline for over 20 years.
The physicians at the most risk for a sham peer review tend to be those who work for large hospital systems — as this is one way for hospitals to get rid of the doctors they don’t want to retain on staff, Huntoon said.
“Hospitals want a model whereby every physician on the medical staff is an employee,” Huntoon added. “This gives them complete power and control over these physicians, including the way they practice and how many patients they see per day, which, for some, is 20-50 a day to generate sufficient revenue.”
Complaints are generally filed via incident reporting software.
“The complaint could be that the physician is ‘disruptive,’ which can include facial expression, tone of voice, and body language — for example, ‘I found his facial expression demeaning’ or ‘I found her tone condescending’ — and this can be used to prosecute a doctor,” Huntoon said.
After the complaint is filed, the leaders of a hospital’s peer review committee meet to discuss the incident, followed by a panel of fellow physicians convened to review the matter. Once the date for a meeting is set, the accused doctor is allowed to testify, offer evidence, and have attorney representation.
The entire experience can take a physician by surprise.
“A sham peer review is difficult to prepare for because no physician thinks this is going to happen to them,” said Laurie L. York, a medical law attorney in Austin, Texas.
York added that there may also be a misperception of what is actually happening.
“When a physician becomes aware of an investigation, it initially may look like a regular peer review, and the physician may feel there has been a ‘misunderstanding’ that they can make right by explaining things,” York said. “The window of opportunity to shut down a sham peer review happens quickly. That’s why the physician needs the help of an experienced attorney as early in the process as possible.”
If You’re a Victim of a Sham Peer Review
Be vigilant. The most important thing you should think about when it comes to sham peer reviews is that this can, indeed, happen to you, Huntoon said. “I’ve written articles to help educate physicians about the tactics that are used,” he said. “You need to be educated and read medical staff bylaws to know your rights before something bad happens.”
Stay in your job. No matter what, if you’re under review, do not resign your position, no matter how difficult this may be. “A resignation during a sham peer review triggers an adverse report to the National Practitioner Data Bank [NPDB],” Schlafly said. The NPDB is a flagging system created by Congress to improve healthcare quality and reduce healthcare fraud and abuse. “A resignation also waives the physician’s right to contest the unfair review. In addition, leverage to negotiate a favorable settlement is lost if the physician simply resigns.”
Get a lawyer on board early. This is the only way to protect your rights. “Don’t wait a year to get an attorney involved,” Huntoon said. But this also can’t be any lawyer. It’s critical to find someone who specializes in sham peer reviews, so be sure to ask about their experience in handling peer review matters in hospitals and how knowledgeable they are about databank reporting requirements. “Sometimes, doctors will hire a malpractice attorney with no knowledge of what happens with sham peer reviews, and they may give bad advice,” he said. “Others may hire an employment attorney and that attorney will be up on employment law but has no experience with peer review matters in hospitals.”
Given the seriousness of a sham peer review, following these guidelines can help.
Contact the AAPA right away. There are things that can be done early on like getting a withdrawal of the request for corrective action as well as obtaining a preliminary injunction. Preparing for the fallout that may occur can be just as challenging.
“After this situation, the doctor is damaged goods,” Huntoon said. “What hospital will want to hire damaged goods to be part of their medical staff? Finding employment is going to be challenging and opening your own practice may also be difficult because the insurers have access to data bank reports.”
Ultimately, the best advice Huntoon can offer is to do your best to stay one step ahead of any work issues that could even lead to a sham peer review.
“Try and shield yourself from a sham peer review and be prepared should it happen,” he said. “I’ve seen careers end in the blink of an eye — wrongfully.”
A version of this article first appeared on Medscape.com.
While a medical peer review occurs once a patient, fellow doctor, or staff member reports that a physician failed to treat a patient up to standards or acted improperly, a “sham peer review” is undertaken for ulterior motives.
They’re typically undertaken due to professional competition or institutional politics rather than to promote quality care or uphold professional standards.
Physicians should be concerned. In a soon-to-be-published Medscape report on peer reviews, 56% of US physicians surveyed expressed higher levels of concern that a peer review could be misused to punish a physician for reasons unrelated to the matter being reviewed.
This is a troublesome issue, and many doctors may not be aware of it or how often it occurs.
“The biggest misconception about sham peer reviews is a denial of how pervasive they are,” said Andy Schlafly, general counsel for the Association of American Physicians and Surgeons (AAPS), which offers a free legal consultation service for physicians facing a sham peer review. “Many hospital administrations are as dangerous to good physicians as street gangs can be in a crime-ridden neighborhood.”
“Physicians should become aware of whether sham peer reviews are prevalent at their hospital and, if so, those physicians should look to practice somewhere else,” Schlafly said in an interview.
Unfortunately, there are limited data on how often this happens. When it does, it can be a career killer, said Lawrence Huntoon, MD, PhD, who has run the AAPS sham peer review hotline for over 20 years.
The physicians at the most risk for a sham peer review tend to be those who work for large hospital systems — as this is one way for hospitals to get rid of the doctors they don’t want to retain on staff, Huntoon said.
“Hospitals want a model whereby every physician on the medical staff is an employee,” Huntoon added. “This gives them complete power and control over these physicians, including the way they practice and how many patients they see per day, which, for some, is 20-50 a day to generate sufficient revenue.”
Complaints are generally filed via incident reporting software.
“The complaint could be that the physician is ‘disruptive,’ which can include facial expression, tone of voice, and body language — for example, ‘I found his facial expression demeaning’ or ‘I found her tone condescending’ — and this can be used to prosecute a doctor,” Huntoon said.
After the complaint is filed, the leaders of a hospital’s peer review committee meet to discuss the incident, followed by a panel of fellow physicians convened to review the matter. Once the date for a meeting is set, the accused doctor is allowed to testify, offer evidence, and have attorney representation.
The entire experience can take a physician by surprise.
“A sham peer review is difficult to prepare for because no physician thinks this is going to happen to them,” said Laurie L. York, a medical law attorney in Austin, Texas.
York added that there may also be a misperception of what is actually happening.
“When a physician becomes aware of an investigation, it initially may look like a regular peer review, and the physician may feel there has been a ‘misunderstanding’ that they can make right by explaining things,” York said. “The window of opportunity to shut down a sham peer review happens quickly. That’s why the physician needs the help of an experienced attorney as early in the process as possible.”
If You’re a Victim of a Sham Peer Review
Be vigilant. The most important thing you should think about when it comes to sham peer reviews is that this can, indeed, happen to you, Huntoon said. “I’ve written articles to help educate physicians about the tactics that are used,” he said. “You need to be educated and read medical staff bylaws to know your rights before something bad happens.”
Stay in your job. No matter what, if you’re under review, do not resign your position, no matter how difficult this may be. “A resignation during a sham peer review triggers an adverse report to the National Practitioner Data Bank [NPDB],” Schlafly said. The NPDB is a flagging system created by Congress to improve healthcare quality and reduce healthcare fraud and abuse. “A resignation also waives the physician’s right to contest the unfair review. In addition, leverage to negotiate a favorable settlement is lost if the physician simply resigns.”
Get a lawyer on board early. This is the only way to protect your rights. “Don’t wait a year to get an attorney involved,” Huntoon said. But this also can’t be any lawyer. It’s critical to find someone who specializes in sham peer reviews, so be sure to ask about their experience in handling peer review matters in hospitals and how knowledgeable they are about databank reporting requirements. “Sometimes, doctors will hire a malpractice attorney with no knowledge of what happens with sham peer reviews, and they may give bad advice,” he said. “Others may hire an employment attorney and that attorney will be up on employment law but has no experience with peer review matters in hospitals.”
Given the seriousness of a sham peer review, following these guidelines can help.
Contact the AAPA right away. There are things that can be done early on like getting a withdrawal of the request for corrective action as well as obtaining a preliminary injunction. Preparing for the fallout that may occur can be just as challenging.
“After this situation, the doctor is damaged goods,” Huntoon said. “What hospital will want to hire damaged goods to be part of their medical staff? Finding employment is going to be challenging and opening your own practice may also be difficult because the insurers have access to data bank reports.”
Ultimately, the best advice Huntoon can offer is to do your best to stay one step ahead of any work issues that could even lead to a sham peer review.
“Try and shield yourself from a sham peer review and be prepared should it happen,” he said. “I’ve seen careers end in the blink of an eye — wrongfully.”
A version of this article first appeared on Medscape.com.
While a medical peer review occurs once a patient, fellow doctor, or staff member reports that a physician failed to treat a patient up to standards or acted improperly, a “sham peer review” is undertaken for ulterior motives.
They’re typically undertaken due to professional competition or institutional politics rather than to promote quality care or uphold professional standards.
Physicians should be concerned. In a soon-to-be-published Medscape report on peer reviews, 56% of US physicians surveyed expressed higher levels of concern that a peer review could be misused to punish a physician for reasons unrelated to the matter being reviewed.
This is a troublesome issue, and many doctors may not be aware of it or how often it occurs.
“The biggest misconception about sham peer reviews is a denial of how pervasive they are,” said Andy Schlafly, general counsel for the Association of American Physicians and Surgeons (AAPS), which offers a free legal consultation service for physicians facing a sham peer review. “Many hospital administrations are as dangerous to good physicians as street gangs can be in a crime-ridden neighborhood.”
“Physicians should become aware of whether sham peer reviews are prevalent at their hospital and, if so, those physicians should look to practice somewhere else,” Schlafly said in an interview.
Unfortunately, there are limited data on how often this happens. When it does, it can be a career killer, said Lawrence Huntoon, MD, PhD, who has run the AAPS sham peer review hotline for over 20 years.
The physicians at the most risk for a sham peer review tend to be those who work for large hospital systems — as this is one way for hospitals to get rid of the doctors they don’t want to retain on staff, Huntoon said.
“Hospitals want a model whereby every physician on the medical staff is an employee,” Huntoon added. “This gives them complete power and control over these physicians, including the way they practice and how many patients they see per day, which, for some, is 20-50 a day to generate sufficient revenue.”
Complaints are generally filed via incident reporting software.
“The complaint could be that the physician is ‘disruptive,’ which can include facial expression, tone of voice, and body language — for example, ‘I found his facial expression demeaning’ or ‘I found her tone condescending’ — and this can be used to prosecute a doctor,” Huntoon said.
After the complaint is filed, the leaders of a hospital’s peer review committee meet to discuss the incident, followed by a panel of fellow physicians convened to review the matter. Once the date for a meeting is set, the accused doctor is allowed to testify, offer evidence, and have attorney representation.
The entire experience can take a physician by surprise.
“A sham peer review is difficult to prepare for because no physician thinks this is going to happen to them,” said Laurie L. York, a medical law attorney in Austin, Texas.
York added that there may also be a misperception of what is actually happening.
“When a physician becomes aware of an investigation, it initially may look like a regular peer review, and the physician may feel there has been a ‘misunderstanding’ that they can make right by explaining things,” York said. “The window of opportunity to shut down a sham peer review happens quickly. That’s why the physician needs the help of an experienced attorney as early in the process as possible.”
If You’re a Victim of a Sham Peer Review
Be vigilant. The most important thing you should think about when it comes to sham peer reviews is that this can, indeed, happen to you, Huntoon said. “I’ve written articles to help educate physicians about the tactics that are used,” he said. “You need to be educated and read medical staff bylaws to know your rights before something bad happens.”
Stay in your job. No matter what, if you’re under review, do not resign your position, no matter how difficult this may be. “A resignation during a sham peer review triggers an adverse report to the National Practitioner Data Bank [NPDB],” Schlafly said. The NPDB is a flagging system created by Congress to improve healthcare quality and reduce healthcare fraud and abuse. “A resignation also waives the physician’s right to contest the unfair review. In addition, leverage to negotiate a favorable settlement is lost if the physician simply resigns.”
Get a lawyer on board early. This is the only way to protect your rights. “Don’t wait a year to get an attorney involved,” Huntoon said. But this also can’t be any lawyer. It’s critical to find someone who specializes in sham peer reviews, so be sure to ask about their experience in handling peer review matters in hospitals and how knowledgeable they are about databank reporting requirements. “Sometimes, doctors will hire a malpractice attorney with no knowledge of what happens with sham peer reviews, and they may give bad advice,” he said. “Others may hire an employment attorney and that attorney will be up on employment law but has no experience with peer review matters in hospitals.”
Given the seriousness of a sham peer review, following these guidelines can help.
Contact the AAPA right away. There are things that can be done early on like getting a withdrawal of the request for corrective action as well as obtaining a preliminary injunction. Preparing for the fallout that may occur can be just as challenging.
“After this situation, the doctor is damaged goods,” Huntoon said. “What hospital will want to hire damaged goods to be part of their medical staff? Finding employment is going to be challenging and opening your own practice may also be difficult because the insurers have access to data bank reports.”
Ultimately, the best advice Huntoon can offer is to do your best to stay one step ahead of any work issues that could even lead to a sham peer review.
“Try and shield yourself from a sham peer review and be prepared should it happen,” he said. “I’ve seen careers end in the blink of an eye — wrongfully.”
A version of this article first appeared on Medscape.com.
Sulfites: The 2024 American Contact Dermatitis Society Allergen of the Year
The American Contact Dermatitis Society (ACDS) selected sulfites as the 2024 Allergen of the Year.1 Due to their preservative and antioxidant properties, sulfites are prevalent in a variety of foods, beverages, medications, and personal care products; however, sulfites also have been implicated as a potential contact allergen. In this article, we review common sources of sulfite exposure, clinical manifestations of allergic contact dermatitis (ACD) to sulfites, and patch testing considerations for this emerging allergen.
What Are Sulfites?
Sulfiting agents are compounds that contain the sulfite ion SO32-, including sulfur dioxide, sodium disulfite (sodium metabisulfite), and potassium metabisulfite.2 Sulfites occur naturally in the environment and commonly are used as preservatives, antibrowning agents, and antioxidants in various foods, beverages, medications, cosmetics, and skin care products. As antibrowning agents and antioxidants, sulfites help maintain the natural appearance of foods and other products and prevent premature spoiling by inactivating oxidative enzymes.3 It should be noted that sulfites and sulfates are distinct and unrelated compounds that do not cross-react.1
Common Sources of Sulfite Exposure
From a morning glass of juice to an evening shower, in the pharmacy and at the hair salon, sulfite exposure is ubiquitous in most daily routines. Sulfites are present in many foods and beverages, either as a byproduct of natural fermentation or as an additive to prevent spoiling and color change. The Table provides examples of foods with high sulfite content.1,4-6 In particular, dried fruit, bottled lemon juice, wine, grape juice, sauerkraut juice, and pickled onions have high sulfite content.
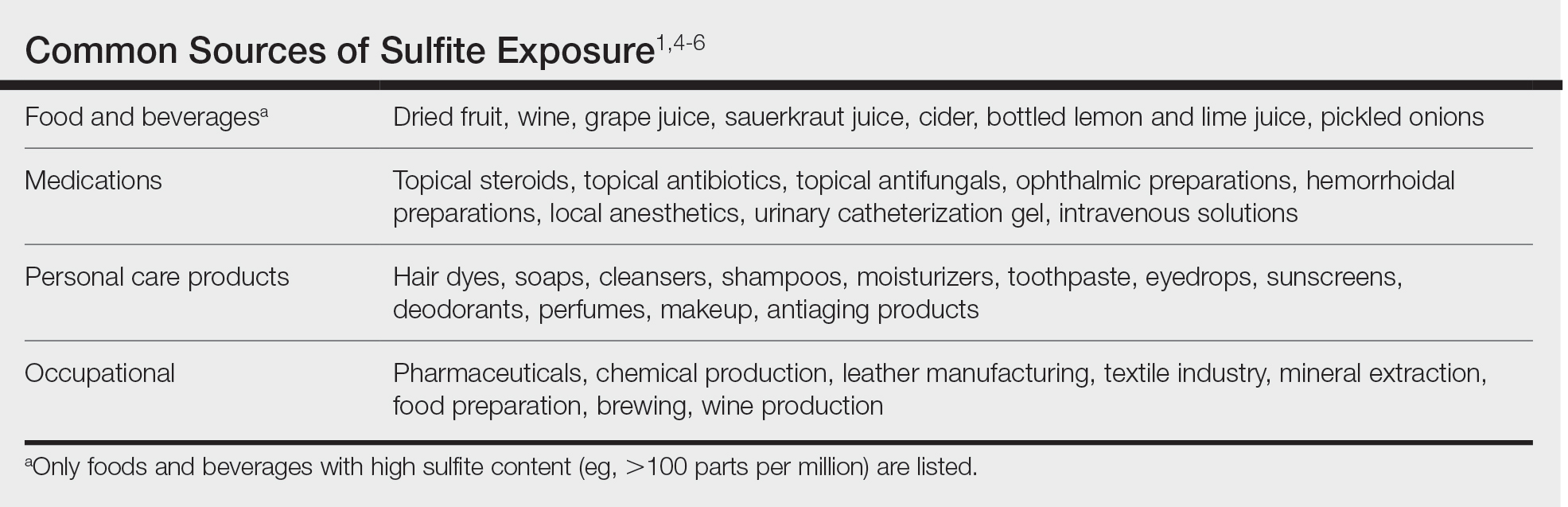
Topical medications and personal care products represent other potential sources of sulfite exposure. A number of reports have shown that sulfites may be included in topical steroids,7 antibiotics,8 antifungals,9 hemorrhoidal preparations,10 local anesthetics,11 and urinary catheterization gel,12 highlighting their many potential applications. In addition, a comprehensive ingredient analysis of 264 ophthalmic medications found that 3.8% of the products contained sodium disulfite.13 Sulfites may be found in personal care products, including facial and hand cleansers, shampoos, moisturizers, and toothpastes. Hair dyes also commonly contain sulfites,7 which are listed in as many as 90% of hair dye kits in the ACDS Contact Allergen Management Program database.1
Occupational exposures also are widespread, as sulfites are extensively utilized across diverse industries such as pharmaceuticals, health care, leather manufacturing, mineral extraction, food preparation, chemical manufacturing, textiles, alcohol brewing, and wine production.1
Sulfites also are used in the rubber industry—particularly in gloves—due to their anticoagulant and preservative properties.4 This is relevant to health care providers, who may use dozens of disposable gloves in a single day. In an experimental pilot study, researchers detected sulfites in 83% (5/6) of natural rubber latex gloves, 96% (23/24) of synthetic (nitrile) gloves, and 0% (0/5) of polyvinyl chloride gloves.14 While this study was limited to a small sample size, it demonstrates the common use of sulfites in certain rubber gloves and encourages future studies to determine whether there is a quantitative threshold to elicit allergic reactions.
Sulfite Allergy
In 1968, an early case report of ACD to sulfites was published involving a pharmaceutical worker who developed hand eczema after working at a factory for 3 months and had a positive patch test to potassium metabisulfite.15 There have been other cases published in the literature since then, including localized ACD as well as less common cases of systemic contact dermatitis following oral, injectable, and rectal sulfite exposures.16
The North American Contact Dermatitis Group found that, among 132 (2.7%) of 4885 patients with positive patch tests to sodium disulfite from 2017 to 2018, the most commonly involved body sites were the face (28.8%) and hands (20.5%) followed by a scattered/generalized distribution (13.6%). Involvement of the face and hands may correlate with the most frequent sources of exposure that were identified, including personal care products (particularly hair dyes)(18.9%), medications (9.1%), and foods (7.6%).17 A multicenter analysis of patch test results from Germany, Austria, and Switzerland from 1999 to 2013 showed that 357 (2.9%) of 12,156 patients had positive reactions to sodium disulfite, with the most commonly identified exposure sources being topical pharmaceutical agents (59.3%); cosmetics, creams, and sunscreens (13.6%); and systemic drugs (6.8%).18 However, it is not always possible to determine the clinical relevance of a positive patch test to sulfites.1
Other than the face and hands, there have been other unexpected anatomic locations for sulfite ACD (eg, the lower back), and systemic contact dermatitis has manifested with widespread rashes due to oral, rectal, and parenteral exposure.4,16,19 There is no definitive link between sulfite contact allergy and patient sex, but there seems to be a higher prevalence in patients older than 40 years, perhaps related to overall lifetime exposure.1
Immediate hypersensitivity reactions to sulfites also have been reported, including urticaria, angioedema, and anaphylaxis.4 Due to multiple cases of severe dermatologic and respiratory reactions to food products containing sulfites,20 the US Food and Drug Administration prohibited their use in fresh fruit and vegetables as antibrowning agents in 1986 and required labels on packaged foods that contained sulfites at more than 10 parts per million.21 However, food and drinks produced in restaurants, bakeries, and cafes as well as those that are distributed directly to consumers from the preparation site are exempt from these rules.17
In addition, consuming high amounts of dietary sulfites has been linked to headaches through unclear (ie, not necessarily allergic) mechanisms.4,22 One study found that wine with a higher sulfite concentration was associated with increased risk for headaches in participants who had a history of headaches related to wine consumption.22
Patch Testing to Sulfites
The North American Contact Dermatitis Group has tested sodium disulfite since 2017 and found an increased frequency of positive patch tests from 2.7% (N=4885) in 2017 and 201817 to 3.3% (N=4115) in 2019 and 202023 among patients referred for testing. Similarly, patch testing to sodium disulfite in nearly 40,000 patients in 9 European countries showed a pooled prevalence of reactions of 3.1%.17 However, this contact allergy may go unrecognized, as sulfites are not included in common patch test series, including the thin-layer rapid use epicutaneous test and the ACDS Core Allergen Series.24,25 The relatively high patch test positivity to sulfites along with the prevalence of daily exposures supports the addition of sulfites to more patch test screening series.
The recommended patch test concentration for sodium disulfite is 1% in petrolatum.5 Testing in aqueous solutions is not recommended because they can cause sulfites to break down, potentially producing false-positive or irritant patch test reactions.7,26,27
Recommendations for Patients With Sulfite Allergies
Individuals with contact allergies to sulfites should be counseled on exposure sources and should be given resources providing a list of safe products, such as the ACDS Contact Allergen Management Program (https://www.acdscamp.org/login) or SkinSAFE (https://www.skinsafeproducts.com/). Prescribers should be cognizant of sulfites that are present in prescription medications. Just because a patient has a positive patch test to sulfites does not automatically imply that they will need to modify their diet to avoid sulfite-containing foods; in the absence of cheilitis or a distribution suggestive of systemic contact dermatitis (eg, vesicular hand/foot dermatitis, intertriginous eruptions), this step may be unnecessary. On the other hand, individuals who have experienced immediate hypersensitivity reactions to sulfites should avoid sulfite-containing foods and carry an epinephrine autoinjector.
Final Interpretation
Sulfites are ubiquitous compounds found in various foods, beverages, medications, and personal care products in addition to a range of occupational exposures. The face and hands are the most common sites of sulfite ACD. Despite patch test positivity in as many as 3% of tested patients,17,23 sulfite allergy may be missed due to lack of routine testing on standard screening series.
- Ekstein SF, Warshaw EM. Sulfites: allergen of the year 2024. Dermatitis. 2024;35:6-12. doi:10.1089/derm.2023.0154
- Gunnison AF, Jacobsen DW. Sulfite hypersensitivity. a critical review. CRC Crit Rev Toxicol. 1987;17:185-214. doi:10.3109/10408448709071208
- Clough SR. Sodium sulfite. In: Wexler P, ed. Encyclopedia of Toxicology. 3rd ed. Academic Press; 2014: 341-343.
- Vally H, Misso NL, Madan V. Clinical effects of sulphite additives. Clin Exp Allergy. 2009;39:1643-1651. doi:10.1111/j.1365-2222.2009.03362.x
- Ralph N, Verma S, Merry S, et al. What is the relevance of contact allergy to sodium metabisulfite and which concentration of the allergen should we use? Dermatitis. 2015;26:162-165. doi:10.1097/der.0000000000000120
- Madan V, Walker SL, Beck MH. Sodium metabisulfite allergy is common but is it relevant? Contact Dermatitis. 2007;57:173-176. doi:10.1111/j.1600-0536.2007.01188.x
- García-Gavín J, Parente J, Goossens A. Allergic contact dermatitis caused by sodium metabisulfite: a challenging allergen. a case series and literature review. Contact Dermatitis. 2012;67:260-269. doi:10.1111/j.1600-0536.2012.02135.x
- Milpied B, van Wassenhove L, Larousse C, et al. Contact dermatitis from rifamycin. Contact Dermatitis. 1986;14:252-253. doi:10.1111/j.1600-0536.1986.tb01240.x
- Lodi A, Chiarelli G, Mancini LL, et al. Contact allergy to sodium sulfite contained in an antifungal preparation. Contact Dermatitis. 1993;29:97. doi:10.1111/j.1600-0536.1993.tb03493.x
- Sánchez-Pérez J, Abajo P, Córdoba S, et al. Allergic contact dermatitis from sodium metabisulfite in an antihemorrhoidal cream. Contact Dermatitis. 2000;42:176-177.
- Boyd AH, Warshaw EM. Sulfites: no longer a zebra? Dermatitis. 2017;28:364-366. doi:10.1097/der.0000000000000312
- Grosch E, Mahler V. Allergic contact dermatitis caused by a catheter system containing sodium metabisulfite. Contact Dermatitis. 2017;76:186-187. doi:10.1111/cod.12675
- Shaver RL, Warshaw EM. Contact allergens in prescription topical ophthalmic medications. Dermatitis. 2022;33:135-143. doi:10.1097/der.0000000000000751
- Dendooven E, Darrigade AS, Foubert K, et al. The presence of sulfites in ‘natural rubber latex’ and ‘synthetic’ rubber gloves: an experimental pilot study. Br J Dermatol. 2020;182:1054-1055. doi:10.1111/bjd.18608
- Nater JP. Allergic contact dermatitis caused by potassium metabisulfite. Dermatologica. 1968;136:477-478. doi:10.1159/000254143
- Borges AS, Valejo Coelho MM, Fernandes C, et al. Systemic allergic dermatitis caused by sodium metabisulfite in rectal enemas. Contact Dermatitis. 2018;78:429-430. doi:10.1111/cod.12971
- Warshaw EM, Buonomo M, DeKoven JG, et al. Patch testing with sodium disulfite: North American Contact Dermatitis Group experience, 2017 to 2018. Contact Dermatitis. 2021;85:285-296. doi:10.1111/cod.13860
- Häberle M, Geier J, Mahler V. Contact allergy to sulfites: clinical and occupational relevance—new data from the German Contact Dermatitis Research Group and the Information Network of Departments of Dermatology (IVDK). J Dtsch Dermatol Ges. 2016;14:938-941. doi:10.1111/ddg.13009
- Tan MG, Li HO, Pratt MD. Systemic allergic dermatitis to sodium metabisulfite in local anesthetic solution. Contact Dermatitis. 2022;86:120-121. doi:10.1111/cod.13978
- D’Amore T, Di Taranto A, Berardi G, et al. Sulfites in meat: occurrence, activity, toxicity, regulation, and detection. a comprehensive review. Compr Rev Food Sci Food Saf. 2020;19:2701-2720. doi:10.1111/1541-4337.12607
- Grotheer P, Marshall M, Simonne A. Sulfites: separating fact from fiction. May 11, 2022. UF IFAS Extension. University of Florida. Accessed October 4, 2024. https://edis.ifas.ufl.edu/publication/FY731
- Silva M, Gama J, Pinto N, et al. Sulfite concentration and the occurrence of headache in young adults: a prospective study. Eur J Clin Nutr. 2019;73:1316-1322. doi:10.1038/s41430-019-0420-2
- DeKoven JG, Warshaw EM, Reeder MJ, et al. North American Contact Dermatitis Group patch test results: 2019-2020. Dermatitis. 2023;34:90-104. doi:10.1089/derm.2022.29017.jdk
- T.R.U.E. Test. Thin-layer rapid use epicutaneous patch test. SmartPractice Dermatology Allergy. Accessed October 4, 2024. https://www.smartpractice.com/shop/category?id=581719&m=SPA
- Schalock PC, Dunnick CA, Nedorost, et al; American Contact Dermatitis Society Core Allergen Series Committee. American Contact Dermatitis Society Core Allergen Series: 2020 update. Dermatitis. 2020;31:279-282.
- Kaaman AC, Boman A, Wrangsjö K, et al. Contact allergy to sodium metabisulfite: an occupational problem. Contact Dermatitis. 2010;63:110-112. doi:10.1111/j.1600-0536.2010.01756.x
- Vena GA, Foti C, Angelini G. Sulfite contact allergy. Contact Dermatitis. 1994;31:172-175. doi:10.1111/j.1600-0536.1994.tb01959.x
The American Contact Dermatitis Society (ACDS) selected sulfites as the 2024 Allergen of the Year.1 Due to their preservative and antioxidant properties, sulfites are prevalent in a variety of foods, beverages, medications, and personal care products; however, sulfites also have been implicated as a potential contact allergen. In this article, we review common sources of sulfite exposure, clinical manifestations of allergic contact dermatitis (ACD) to sulfites, and patch testing considerations for this emerging allergen.
What Are Sulfites?
Sulfiting agents are compounds that contain the sulfite ion SO32-, including sulfur dioxide, sodium disulfite (sodium metabisulfite), and potassium metabisulfite.2 Sulfites occur naturally in the environment and commonly are used as preservatives, antibrowning agents, and antioxidants in various foods, beverages, medications, cosmetics, and skin care products. As antibrowning agents and antioxidants, sulfites help maintain the natural appearance of foods and other products and prevent premature spoiling by inactivating oxidative enzymes.3 It should be noted that sulfites and sulfates are distinct and unrelated compounds that do not cross-react.1
Common Sources of Sulfite Exposure
From a morning glass of juice to an evening shower, in the pharmacy and at the hair salon, sulfite exposure is ubiquitous in most daily routines. Sulfites are present in many foods and beverages, either as a byproduct of natural fermentation or as an additive to prevent spoiling and color change. The Table provides examples of foods with high sulfite content.1,4-6 In particular, dried fruit, bottled lemon juice, wine, grape juice, sauerkraut juice, and pickled onions have high sulfite content.
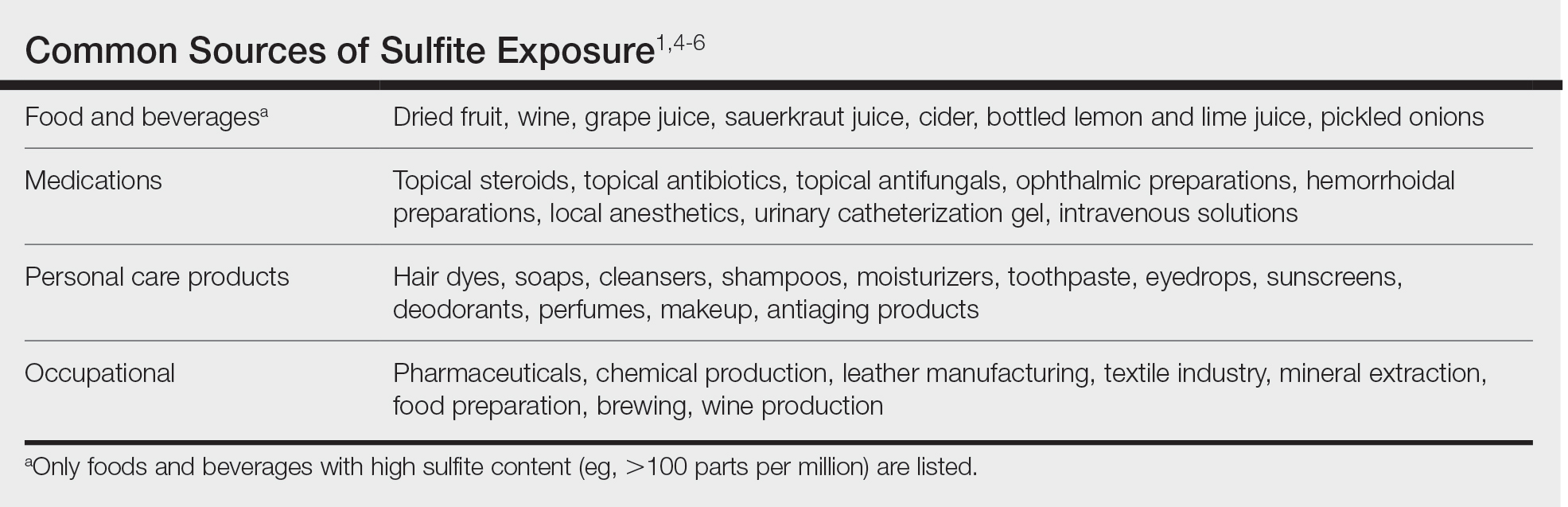
Topical medications and personal care products represent other potential sources of sulfite exposure. A number of reports have shown that sulfites may be included in topical steroids,7 antibiotics,8 antifungals,9 hemorrhoidal preparations,10 local anesthetics,11 and urinary catheterization gel,12 highlighting their many potential applications. In addition, a comprehensive ingredient analysis of 264 ophthalmic medications found that 3.8% of the products contained sodium disulfite.13 Sulfites may be found in personal care products, including facial and hand cleansers, shampoos, moisturizers, and toothpastes. Hair dyes also commonly contain sulfites,7 which are listed in as many as 90% of hair dye kits in the ACDS Contact Allergen Management Program database.1
Occupational exposures also are widespread, as sulfites are extensively utilized across diverse industries such as pharmaceuticals, health care, leather manufacturing, mineral extraction, food preparation, chemical manufacturing, textiles, alcohol brewing, and wine production.1
Sulfites also are used in the rubber industry—particularly in gloves—due to their anticoagulant and preservative properties.4 This is relevant to health care providers, who may use dozens of disposable gloves in a single day. In an experimental pilot study, researchers detected sulfites in 83% (5/6) of natural rubber latex gloves, 96% (23/24) of synthetic (nitrile) gloves, and 0% (0/5) of polyvinyl chloride gloves.14 While this study was limited to a small sample size, it demonstrates the common use of sulfites in certain rubber gloves and encourages future studies to determine whether there is a quantitative threshold to elicit allergic reactions.
Sulfite Allergy
In 1968, an early case report of ACD to sulfites was published involving a pharmaceutical worker who developed hand eczema after working at a factory for 3 months and had a positive patch test to potassium metabisulfite.15 There have been other cases published in the literature since then, including localized ACD as well as less common cases of systemic contact dermatitis following oral, injectable, and rectal sulfite exposures.16
The North American Contact Dermatitis Group found that, among 132 (2.7%) of 4885 patients with positive patch tests to sodium disulfite from 2017 to 2018, the most commonly involved body sites were the face (28.8%) and hands (20.5%) followed by a scattered/generalized distribution (13.6%). Involvement of the face and hands may correlate with the most frequent sources of exposure that were identified, including personal care products (particularly hair dyes)(18.9%), medications (9.1%), and foods (7.6%).17 A multicenter analysis of patch test results from Germany, Austria, and Switzerland from 1999 to 2013 showed that 357 (2.9%) of 12,156 patients had positive reactions to sodium disulfite, with the most commonly identified exposure sources being topical pharmaceutical agents (59.3%); cosmetics, creams, and sunscreens (13.6%); and systemic drugs (6.8%).18 However, it is not always possible to determine the clinical relevance of a positive patch test to sulfites.1
Other than the face and hands, there have been other unexpected anatomic locations for sulfite ACD (eg, the lower back), and systemic contact dermatitis has manifested with widespread rashes due to oral, rectal, and parenteral exposure.4,16,19 There is no definitive link between sulfite contact allergy and patient sex, but there seems to be a higher prevalence in patients older than 40 years, perhaps related to overall lifetime exposure.1
Immediate hypersensitivity reactions to sulfites also have been reported, including urticaria, angioedema, and anaphylaxis.4 Due to multiple cases of severe dermatologic and respiratory reactions to food products containing sulfites,20 the US Food and Drug Administration prohibited their use in fresh fruit and vegetables as antibrowning agents in 1986 and required labels on packaged foods that contained sulfites at more than 10 parts per million.21 However, food and drinks produced in restaurants, bakeries, and cafes as well as those that are distributed directly to consumers from the preparation site are exempt from these rules.17
In addition, consuming high amounts of dietary sulfites has been linked to headaches through unclear (ie, not necessarily allergic) mechanisms.4,22 One study found that wine with a higher sulfite concentration was associated with increased risk for headaches in participants who had a history of headaches related to wine consumption.22
Patch Testing to Sulfites
The North American Contact Dermatitis Group has tested sodium disulfite since 2017 and found an increased frequency of positive patch tests from 2.7% (N=4885) in 2017 and 201817 to 3.3% (N=4115) in 2019 and 202023 among patients referred for testing. Similarly, patch testing to sodium disulfite in nearly 40,000 patients in 9 European countries showed a pooled prevalence of reactions of 3.1%.17 However, this contact allergy may go unrecognized, as sulfites are not included in common patch test series, including the thin-layer rapid use epicutaneous test and the ACDS Core Allergen Series.24,25 The relatively high patch test positivity to sulfites along with the prevalence of daily exposures supports the addition of sulfites to more patch test screening series.
The recommended patch test concentration for sodium disulfite is 1% in petrolatum.5 Testing in aqueous solutions is not recommended because they can cause sulfites to break down, potentially producing false-positive or irritant patch test reactions.7,26,27
Recommendations for Patients With Sulfite Allergies
Individuals with contact allergies to sulfites should be counseled on exposure sources and should be given resources providing a list of safe products, such as the ACDS Contact Allergen Management Program (https://www.acdscamp.org/login) or SkinSAFE (https://www.skinsafeproducts.com/). Prescribers should be cognizant of sulfites that are present in prescription medications. Just because a patient has a positive patch test to sulfites does not automatically imply that they will need to modify their diet to avoid sulfite-containing foods; in the absence of cheilitis or a distribution suggestive of systemic contact dermatitis (eg, vesicular hand/foot dermatitis, intertriginous eruptions), this step may be unnecessary. On the other hand, individuals who have experienced immediate hypersensitivity reactions to sulfites should avoid sulfite-containing foods and carry an epinephrine autoinjector.
Final Interpretation
Sulfites are ubiquitous compounds found in various foods, beverages, medications, and personal care products in addition to a range of occupational exposures. The face and hands are the most common sites of sulfite ACD. Despite patch test positivity in as many as 3% of tested patients,17,23 sulfite allergy may be missed due to lack of routine testing on standard screening series.
The American Contact Dermatitis Society (ACDS) selected sulfites as the 2024 Allergen of the Year.1 Due to their preservative and antioxidant properties, sulfites are prevalent in a variety of foods, beverages, medications, and personal care products; however, sulfites also have been implicated as a potential contact allergen. In this article, we review common sources of sulfite exposure, clinical manifestations of allergic contact dermatitis (ACD) to sulfites, and patch testing considerations for this emerging allergen.
What Are Sulfites?
Sulfiting agents are compounds that contain the sulfite ion SO32-, including sulfur dioxide, sodium disulfite (sodium metabisulfite), and potassium metabisulfite.2 Sulfites occur naturally in the environment and commonly are used as preservatives, antibrowning agents, and antioxidants in various foods, beverages, medications, cosmetics, and skin care products. As antibrowning agents and antioxidants, sulfites help maintain the natural appearance of foods and other products and prevent premature spoiling by inactivating oxidative enzymes.3 It should be noted that sulfites and sulfates are distinct and unrelated compounds that do not cross-react.1
Common Sources of Sulfite Exposure
From a morning glass of juice to an evening shower, in the pharmacy and at the hair salon, sulfite exposure is ubiquitous in most daily routines. Sulfites are present in many foods and beverages, either as a byproduct of natural fermentation or as an additive to prevent spoiling and color change. The Table provides examples of foods with high sulfite content.1,4-6 In particular, dried fruit, bottled lemon juice, wine, grape juice, sauerkraut juice, and pickled onions have high sulfite content.
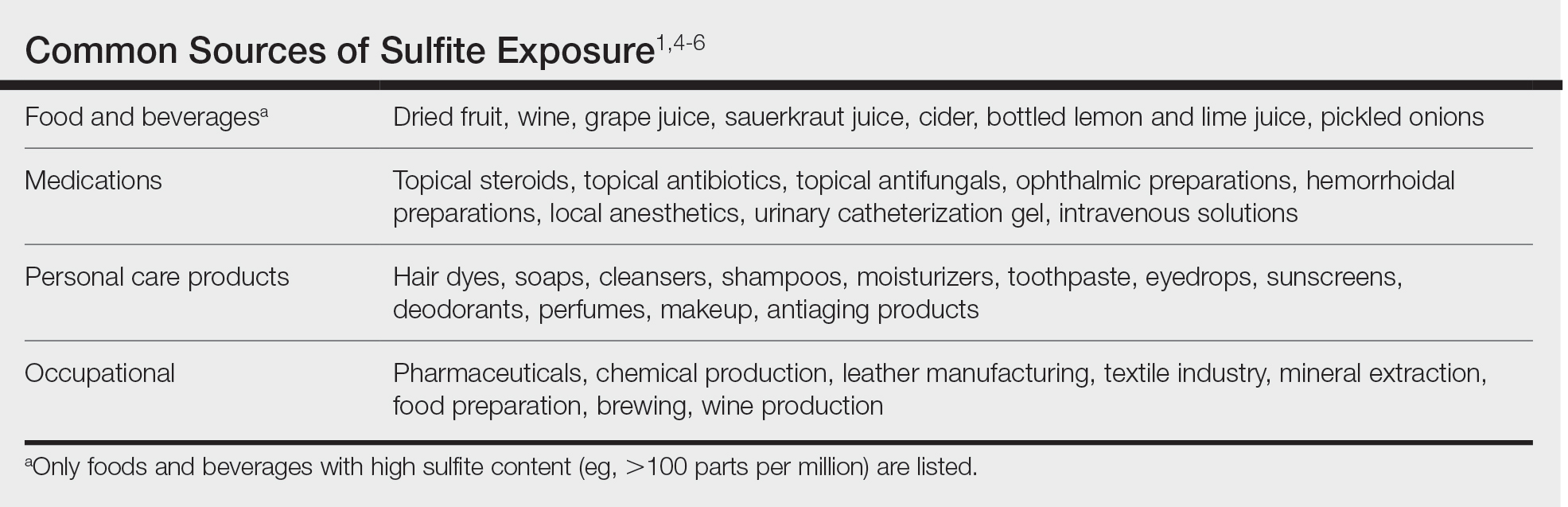
Topical medications and personal care products represent other potential sources of sulfite exposure. A number of reports have shown that sulfites may be included in topical steroids,7 antibiotics,8 antifungals,9 hemorrhoidal preparations,10 local anesthetics,11 and urinary catheterization gel,12 highlighting their many potential applications. In addition, a comprehensive ingredient analysis of 264 ophthalmic medications found that 3.8% of the products contained sodium disulfite.13 Sulfites may be found in personal care products, including facial and hand cleansers, shampoos, moisturizers, and toothpastes. Hair dyes also commonly contain sulfites,7 which are listed in as many as 90% of hair dye kits in the ACDS Contact Allergen Management Program database.1
Occupational exposures also are widespread, as sulfites are extensively utilized across diverse industries such as pharmaceuticals, health care, leather manufacturing, mineral extraction, food preparation, chemical manufacturing, textiles, alcohol brewing, and wine production.1
Sulfites also are used in the rubber industry—particularly in gloves—due to their anticoagulant and preservative properties.4 This is relevant to health care providers, who may use dozens of disposable gloves in a single day. In an experimental pilot study, researchers detected sulfites in 83% (5/6) of natural rubber latex gloves, 96% (23/24) of synthetic (nitrile) gloves, and 0% (0/5) of polyvinyl chloride gloves.14 While this study was limited to a small sample size, it demonstrates the common use of sulfites in certain rubber gloves and encourages future studies to determine whether there is a quantitative threshold to elicit allergic reactions.
Sulfite Allergy
In 1968, an early case report of ACD to sulfites was published involving a pharmaceutical worker who developed hand eczema after working at a factory for 3 months and had a positive patch test to potassium metabisulfite.15 There have been other cases published in the literature since then, including localized ACD as well as less common cases of systemic contact dermatitis following oral, injectable, and rectal sulfite exposures.16
The North American Contact Dermatitis Group found that, among 132 (2.7%) of 4885 patients with positive patch tests to sodium disulfite from 2017 to 2018, the most commonly involved body sites were the face (28.8%) and hands (20.5%) followed by a scattered/generalized distribution (13.6%). Involvement of the face and hands may correlate with the most frequent sources of exposure that were identified, including personal care products (particularly hair dyes)(18.9%), medications (9.1%), and foods (7.6%).17 A multicenter analysis of patch test results from Germany, Austria, and Switzerland from 1999 to 2013 showed that 357 (2.9%) of 12,156 patients had positive reactions to sodium disulfite, with the most commonly identified exposure sources being topical pharmaceutical agents (59.3%); cosmetics, creams, and sunscreens (13.6%); and systemic drugs (6.8%).18 However, it is not always possible to determine the clinical relevance of a positive patch test to sulfites.1
Other than the face and hands, there have been other unexpected anatomic locations for sulfite ACD (eg, the lower back), and systemic contact dermatitis has manifested with widespread rashes due to oral, rectal, and parenteral exposure.4,16,19 There is no definitive link between sulfite contact allergy and patient sex, but there seems to be a higher prevalence in patients older than 40 years, perhaps related to overall lifetime exposure.1
Immediate hypersensitivity reactions to sulfites also have been reported, including urticaria, angioedema, and anaphylaxis.4 Due to multiple cases of severe dermatologic and respiratory reactions to food products containing sulfites,20 the US Food and Drug Administration prohibited their use in fresh fruit and vegetables as antibrowning agents in 1986 and required labels on packaged foods that contained sulfites at more than 10 parts per million.21 However, food and drinks produced in restaurants, bakeries, and cafes as well as those that are distributed directly to consumers from the preparation site are exempt from these rules.17
In addition, consuming high amounts of dietary sulfites has been linked to headaches through unclear (ie, not necessarily allergic) mechanisms.4,22 One study found that wine with a higher sulfite concentration was associated with increased risk for headaches in participants who had a history of headaches related to wine consumption.22
Patch Testing to Sulfites
The North American Contact Dermatitis Group has tested sodium disulfite since 2017 and found an increased frequency of positive patch tests from 2.7% (N=4885) in 2017 and 201817 to 3.3% (N=4115) in 2019 and 202023 among patients referred for testing. Similarly, patch testing to sodium disulfite in nearly 40,000 patients in 9 European countries showed a pooled prevalence of reactions of 3.1%.17 However, this contact allergy may go unrecognized, as sulfites are not included in common patch test series, including the thin-layer rapid use epicutaneous test and the ACDS Core Allergen Series.24,25 The relatively high patch test positivity to sulfites along with the prevalence of daily exposures supports the addition of sulfites to more patch test screening series.
The recommended patch test concentration for sodium disulfite is 1% in petrolatum.5 Testing in aqueous solutions is not recommended because they can cause sulfites to break down, potentially producing false-positive or irritant patch test reactions.7,26,27
Recommendations for Patients With Sulfite Allergies
Individuals with contact allergies to sulfites should be counseled on exposure sources and should be given resources providing a list of safe products, such as the ACDS Contact Allergen Management Program (https://www.acdscamp.org/login) or SkinSAFE (https://www.skinsafeproducts.com/). Prescribers should be cognizant of sulfites that are present in prescription medications. Just because a patient has a positive patch test to sulfites does not automatically imply that they will need to modify their diet to avoid sulfite-containing foods; in the absence of cheilitis or a distribution suggestive of systemic contact dermatitis (eg, vesicular hand/foot dermatitis, intertriginous eruptions), this step may be unnecessary. On the other hand, individuals who have experienced immediate hypersensitivity reactions to sulfites should avoid sulfite-containing foods and carry an epinephrine autoinjector.
Final Interpretation
Sulfites are ubiquitous compounds found in various foods, beverages, medications, and personal care products in addition to a range of occupational exposures. The face and hands are the most common sites of sulfite ACD. Despite patch test positivity in as many as 3% of tested patients,17,23 sulfite allergy may be missed due to lack of routine testing on standard screening series.
- Ekstein SF, Warshaw EM. Sulfites: allergen of the year 2024. Dermatitis. 2024;35:6-12. doi:10.1089/derm.2023.0154
- Gunnison AF, Jacobsen DW. Sulfite hypersensitivity. a critical review. CRC Crit Rev Toxicol. 1987;17:185-214. doi:10.3109/10408448709071208
- Clough SR. Sodium sulfite. In: Wexler P, ed. Encyclopedia of Toxicology. 3rd ed. Academic Press; 2014: 341-343.
- Vally H, Misso NL, Madan V. Clinical effects of sulphite additives. Clin Exp Allergy. 2009;39:1643-1651. doi:10.1111/j.1365-2222.2009.03362.x
- Ralph N, Verma S, Merry S, et al. What is the relevance of contact allergy to sodium metabisulfite and which concentration of the allergen should we use? Dermatitis. 2015;26:162-165. doi:10.1097/der.0000000000000120
- Madan V, Walker SL, Beck MH. Sodium metabisulfite allergy is common but is it relevant? Contact Dermatitis. 2007;57:173-176. doi:10.1111/j.1600-0536.2007.01188.x
- García-Gavín J, Parente J, Goossens A. Allergic contact dermatitis caused by sodium metabisulfite: a challenging allergen. a case series and literature review. Contact Dermatitis. 2012;67:260-269. doi:10.1111/j.1600-0536.2012.02135.x
- Milpied B, van Wassenhove L, Larousse C, et al. Contact dermatitis from rifamycin. Contact Dermatitis. 1986;14:252-253. doi:10.1111/j.1600-0536.1986.tb01240.x
- Lodi A, Chiarelli G, Mancini LL, et al. Contact allergy to sodium sulfite contained in an antifungal preparation. Contact Dermatitis. 1993;29:97. doi:10.1111/j.1600-0536.1993.tb03493.x
- Sánchez-Pérez J, Abajo P, Córdoba S, et al. Allergic contact dermatitis from sodium metabisulfite in an antihemorrhoidal cream. Contact Dermatitis. 2000;42:176-177.
- Boyd AH, Warshaw EM. Sulfites: no longer a zebra? Dermatitis. 2017;28:364-366. doi:10.1097/der.0000000000000312
- Grosch E, Mahler V. Allergic contact dermatitis caused by a catheter system containing sodium metabisulfite. Contact Dermatitis. 2017;76:186-187. doi:10.1111/cod.12675
- Shaver RL, Warshaw EM. Contact allergens in prescription topical ophthalmic medications. Dermatitis. 2022;33:135-143. doi:10.1097/der.0000000000000751
- Dendooven E, Darrigade AS, Foubert K, et al. The presence of sulfites in ‘natural rubber latex’ and ‘synthetic’ rubber gloves: an experimental pilot study. Br J Dermatol. 2020;182:1054-1055. doi:10.1111/bjd.18608
- Nater JP. Allergic contact dermatitis caused by potassium metabisulfite. Dermatologica. 1968;136:477-478. doi:10.1159/000254143
- Borges AS, Valejo Coelho MM, Fernandes C, et al. Systemic allergic dermatitis caused by sodium metabisulfite in rectal enemas. Contact Dermatitis. 2018;78:429-430. doi:10.1111/cod.12971
- Warshaw EM, Buonomo M, DeKoven JG, et al. Patch testing with sodium disulfite: North American Contact Dermatitis Group experience, 2017 to 2018. Contact Dermatitis. 2021;85:285-296. doi:10.1111/cod.13860
- Häberle M, Geier J, Mahler V. Contact allergy to sulfites: clinical and occupational relevance—new data from the German Contact Dermatitis Research Group and the Information Network of Departments of Dermatology (IVDK). J Dtsch Dermatol Ges. 2016;14:938-941. doi:10.1111/ddg.13009
- Tan MG, Li HO, Pratt MD. Systemic allergic dermatitis to sodium metabisulfite in local anesthetic solution. Contact Dermatitis. 2022;86:120-121. doi:10.1111/cod.13978
- D’Amore T, Di Taranto A, Berardi G, et al. Sulfites in meat: occurrence, activity, toxicity, regulation, and detection. a comprehensive review. Compr Rev Food Sci Food Saf. 2020;19:2701-2720. doi:10.1111/1541-4337.12607
- Grotheer P, Marshall M, Simonne A. Sulfites: separating fact from fiction. May 11, 2022. UF IFAS Extension. University of Florida. Accessed October 4, 2024. https://edis.ifas.ufl.edu/publication/FY731
- Silva M, Gama J, Pinto N, et al. Sulfite concentration and the occurrence of headache in young adults: a prospective study. Eur J Clin Nutr. 2019;73:1316-1322. doi:10.1038/s41430-019-0420-2
- DeKoven JG, Warshaw EM, Reeder MJ, et al. North American Contact Dermatitis Group patch test results: 2019-2020. Dermatitis. 2023;34:90-104. doi:10.1089/derm.2022.29017.jdk
- T.R.U.E. Test. Thin-layer rapid use epicutaneous patch test. SmartPractice Dermatology Allergy. Accessed October 4, 2024. https://www.smartpractice.com/shop/category?id=581719&m=SPA
- Schalock PC, Dunnick CA, Nedorost, et al; American Contact Dermatitis Society Core Allergen Series Committee. American Contact Dermatitis Society Core Allergen Series: 2020 update. Dermatitis. 2020;31:279-282.
- Kaaman AC, Boman A, Wrangsjö K, et al. Contact allergy to sodium metabisulfite: an occupational problem. Contact Dermatitis. 2010;63:110-112. doi:10.1111/j.1600-0536.2010.01756.x
- Vena GA, Foti C, Angelini G. Sulfite contact allergy. Contact Dermatitis. 1994;31:172-175. doi:10.1111/j.1600-0536.1994.tb01959.x
- Ekstein SF, Warshaw EM. Sulfites: allergen of the year 2024. Dermatitis. 2024;35:6-12. doi:10.1089/derm.2023.0154
- Gunnison AF, Jacobsen DW. Sulfite hypersensitivity. a critical review. CRC Crit Rev Toxicol. 1987;17:185-214. doi:10.3109/10408448709071208
- Clough SR. Sodium sulfite. In: Wexler P, ed. Encyclopedia of Toxicology. 3rd ed. Academic Press; 2014: 341-343.
- Vally H, Misso NL, Madan V. Clinical effects of sulphite additives. Clin Exp Allergy. 2009;39:1643-1651. doi:10.1111/j.1365-2222.2009.03362.x
- Ralph N, Verma S, Merry S, et al. What is the relevance of contact allergy to sodium metabisulfite and which concentration of the allergen should we use? Dermatitis. 2015;26:162-165. doi:10.1097/der.0000000000000120
- Madan V, Walker SL, Beck MH. Sodium metabisulfite allergy is common but is it relevant? Contact Dermatitis. 2007;57:173-176. doi:10.1111/j.1600-0536.2007.01188.x
- García-Gavín J, Parente J, Goossens A. Allergic contact dermatitis caused by sodium metabisulfite: a challenging allergen. a case series and literature review. Contact Dermatitis. 2012;67:260-269. doi:10.1111/j.1600-0536.2012.02135.x
- Milpied B, van Wassenhove L, Larousse C, et al. Contact dermatitis from rifamycin. Contact Dermatitis. 1986;14:252-253. doi:10.1111/j.1600-0536.1986.tb01240.x
- Lodi A, Chiarelli G, Mancini LL, et al. Contact allergy to sodium sulfite contained in an antifungal preparation. Contact Dermatitis. 1993;29:97. doi:10.1111/j.1600-0536.1993.tb03493.x
- Sánchez-Pérez J, Abajo P, Córdoba S, et al. Allergic contact dermatitis from sodium metabisulfite in an antihemorrhoidal cream. Contact Dermatitis. 2000;42:176-177.
- Boyd AH, Warshaw EM. Sulfites: no longer a zebra? Dermatitis. 2017;28:364-366. doi:10.1097/der.0000000000000312
- Grosch E, Mahler V. Allergic contact dermatitis caused by a catheter system containing sodium metabisulfite. Contact Dermatitis. 2017;76:186-187. doi:10.1111/cod.12675
- Shaver RL, Warshaw EM. Contact allergens in prescription topical ophthalmic medications. Dermatitis. 2022;33:135-143. doi:10.1097/der.0000000000000751
- Dendooven E, Darrigade AS, Foubert K, et al. The presence of sulfites in ‘natural rubber latex’ and ‘synthetic’ rubber gloves: an experimental pilot study. Br J Dermatol. 2020;182:1054-1055. doi:10.1111/bjd.18608
- Nater JP. Allergic contact dermatitis caused by potassium metabisulfite. Dermatologica. 1968;136:477-478. doi:10.1159/000254143
- Borges AS, Valejo Coelho MM, Fernandes C, et al. Systemic allergic dermatitis caused by sodium metabisulfite in rectal enemas. Contact Dermatitis. 2018;78:429-430. doi:10.1111/cod.12971
- Warshaw EM, Buonomo M, DeKoven JG, et al. Patch testing with sodium disulfite: North American Contact Dermatitis Group experience, 2017 to 2018. Contact Dermatitis. 2021;85:285-296. doi:10.1111/cod.13860
- Häberle M, Geier J, Mahler V. Contact allergy to sulfites: clinical and occupational relevance—new data from the German Contact Dermatitis Research Group and the Information Network of Departments of Dermatology (IVDK). J Dtsch Dermatol Ges. 2016;14:938-941. doi:10.1111/ddg.13009
- Tan MG, Li HO, Pratt MD. Systemic allergic dermatitis to sodium metabisulfite in local anesthetic solution. Contact Dermatitis. 2022;86:120-121. doi:10.1111/cod.13978
- D’Amore T, Di Taranto A, Berardi G, et al. Sulfites in meat: occurrence, activity, toxicity, regulation, and detection. a comprehensive review. Compr Rev Food Sci Food Saf. 2020;19:2701-2720. doi:10.1111/1541-4337.12607
- Grotheer P, Marshall M, Simonne A. Sulfites: separating fact from fiction. May 11, 2022. UF IFAS Extension. University of Florida. Accessed October 4, 2024. https://edis.ifas.ufl.edu/publication/FY731
- Silva M, Gama J, Pinto N, et al. Sulfite concentration and the occurrence of headache in young adults: a prospective study. Eur J Clin Nutr. 2019;73:1316-1322. doi:10.1038/s41430-019-0420-2
- DeKoven JG, Warshaw EM, Reeder MJ, et al. North American Contact Dermatitis Group patch test results: 2019-2020. Dermatitis. 2023;34:90-104. doi:10.1089/derm.2022.29017.jdk
- T.R.U.E. Test. Thin-layer rapid use epicutaneous patch test. SmartPractice Dermatology Allergy. Accessed October 4, 2024. https://www.smartpractice.com/shop/category?id=581719&m=SPA
- Schalock PC, Dunnick CA, Nedorost, et al; American Contact Dermatitis Society Core Allergen Series Committee. American Contact Dermatitis Society Core Allergen Series: 2020 update. Dermatitis. 2020;31:279-282.
- Kaaman AC, Boman A, Wrangsjö K, et al. Contact allergy to sodium metabisulfite: an occupational problem. Contact Dermatitis. 2010;63:110-112. doi:10.1111/j.1600-0536.2010.01756.x
- Vena GA, Foti C, Angelini G. Sulfite contact allergy. Contact Dermatitis. 1994;31:172-175. doi:10.1111/j.1600-0536.1994.tb01959.x
Practice Points
- Sulfites are ubiquitous compounds that serve as preservatives and antioxidants in various foods, beverages, medications, and personal care products.
- Allergic contact dermatitis to sulfites most commonly affects the face and hands.
- Because sulfites are not included in most patch test screening series, contact allergy to sulfites may be missed unless expanded testing is performed.
Longitudinal Depression on the Right Thumbnail
THE DIAGNOSIS: Habit-Tic Deformity
Habit-tic deformity is a cause of nail dystrophy that commonly arises in children and adults due to subconscious repetitive and self-injurious manipulation of the nail bed or cuticle, which ultimately damages the nail matrix.1,2 It can be considered a variant of onychotillomania.1
Characteristic features of habit-tic deformity include a longitudinal depression on the central nail plate with transverse ridges,1 which can be more prominent on the dominant hand.3 Patients typically note a long duration of nail deformity, often without insight into its etiology.2 Diagnosis relies on careful assessment of the clinical presentation and the patient’s history to rule out other differential diagnoses. Based on our patient’s clinical presentation and history, we excluded wart, squamous cell carcinoma, eczema, psoriasis, lichen planus, autoimmune connective tissue disease, onychomycosis, paronychia, pincer nail deformity, and Beau line as potential diagnoses. Biopsy also can be performed to exclude these diagnoses from the differential if the cause is unclear following clinical examination.
Treatment for habit-tic deformity involves identifying and addressing the underlying habit. Barrier methods such as bandages and cyanoacrylate adhesives that prevent further manipulation of the nail matrix are effective treatments for habit-tic deformity.2 A multidisciplinary approach with psychiatry may be optimal to identify underlying psychological comorbidities and break the habit through behavior interventions and medications.4 Nail dystrophy generally improves once the habit is disrupted; however, a younger age of onset may carry a worse prognosis.3 Patients should be counseled that the affected nail may never grow normally.
Our patient was advised to use fluocinonide ointment 0.05% to reduce inflammation of the proximal nail fold and to cover the thumbnail with a bandage to prevent picking. He also was counseled that the nail may show ongoing abnormal growth. Minimal improvement was noted after 6 months.
- Rieder EA, Tosti A. Onychotillomania: an underrecognized disorder. J Am Acad Dermatol. 2016;75:1245-1250.doi:10.1016/j.jaad.2016
- Ring DS. Inexpensive solution for habit-tic deformity. Arch Dermatol. 2010;146:1222-1223. doi:10.1001/archdermatol.2010.287
- Horne MI, Utzig JB, Rieder EA, et al. Alopecia areata and habit tic deformities. Skin Appendage Disord. 2018;4:323-325. doi:10.1159/000486540
- Sonthalia S, Sharma P, Kapoor J, et al. Habit tic deformity: need fora comprehensive approach. Skin Appendage Disord. 2019;5:117-118.doi:10.1159/000489320 .05.036
THE DIAGNOSIS: Habit-Tic Deformity
Habit-tic deformity is a cause of nail dystrophy that commonly arises in children and adults due to subconscious repetitive and self-injurious manipulation of the nail bed or cuticle, which ultimately damages the nail matrix.1,2 It can be considered a variant of onychotillomania.1
Characteristic features of habit-tic deformity include a longitudinal depression on the central nail plate with transverse ridges,1 which can be more prominent on the dominant hand.3 Patients typically note a long duration of nail deformity, often without insight into its etiology.2 Diagnosis relies on careful assessment of the clinical presentation and the patient’s history to rule out other differential diagnoses. Based on our patient’s clinical presentation and history, we excluded wart, squamous cell carcinoma, eczema, psoriasis, lichen planus, autoimmune connective tissue disease, onychomycosis, paronychia, pincer nail deformity, and Beau line as potential diagnoses. Biopsy also can be performed to exclude these diagnoses from the differential if the cause is unclear following clinical examination.
Treatment for habit-tic deformity involves identifying and addressing the underlying habit. Barrier methods such as bandages and cyanoacrylate adhesives that prevent further manipulation of the nail matrix are effective treatments for habit-tic deformity.2 A multidisciplinary approach with psychiatry may be optimal to identify underlying psychological comorbidities and break the habit through behavior interventions and medications.4 Nail dystrophy generally improves once the habit is disrupted; however, a younger age of onset may carry a worse prognosis.3 Patients should be counseled that the affected nail may never grow normally.
Our patient was advised to use fluocinonide ointment 0.05% to reduce inflammation of the proximal nail fold and to cover the thumbnail with a bandage to prevent picking. He also was counseled that the nail may show ongoing abnormal growth. Minimal improvement was noted after 6 months.
THE DIAGNOSIS: Habit-Tic Deformity
Habit-tic deformity is a cause of nail dystrophy that commonly arises in children and adults due to subconscious repetitive and self-injurious manipulation of the nail bed or cuticle, which ultimately damages the nail matrix.1,2 It can be considered a variant of onychotillomania.1
Characteristic features of habit-tic deformity include a longitudinal depression on the central nail plate with transverse ridges,1 which can be more prominent on the dominant hand.3 Patients typically note a long duration of nail deformity, often without insight into its etiology.2 Diagnosis relies on careful assessment of the clinical presentation and the patient’s history to rule out other differential diagnoses. Based on our patient’s clinical presentation and history, we excluded wart, squamous cell carcinoma, eczema, psoriasis, lichen planus, autoimmune connective tissue disease, onychomycosis, paronychia, pincer nail deformity, and Beau line as potential diagnoses. Biopsy also can be performed to exclude these diagnoses from the differential if the cause is unclear following clinical examination.
Treatment for habit-tic deformity involves identifying and addressing the underlying habit. Barrier methods such as bandages and cyanoacrylate adhesives that prevent further manipulation of the nail matrix are effective treatments for habit-tic deformity.2 A multidisciplinary approach with psychiatry may be optimal to identify underlying psychological comorbidities and break the habit through behavior interventions and medications.4 Nail dystrophy generally improves once the habit is disrupted; however, a younger age of onset may carry a worse prognosis.3 Patients should be counseled that the affected nail may never grow normally.
Our patient was advised to use fluocinonide ointment 0.05% to reduce inflammation of the proximal nail fold and to cover the thumbnail with a bandage to prevent picking. He also was counseled that the nail may show ongoing abnormal growth. Minimal improvement was noted after 6 months.
- Rieder EA, Tosti A. Onychotillomania: an underrecognized disorder. J Am Acad Dermatol. 2016;75:1245-1250.doi:10.1016/j.jaad.2016
- Ring DS. Inexpensive solution for habit-tic deformity. Arch Dermatol. 2010;146:1222-1223. doi:10.1001/archdermatol.2010.287
- Horne MI, Utzig JB, Rieder EA, et al. Alopecia areata and habit tic deformities. Skin Appendage Disord. 2018;4:323-325. doi:10.1159/000486540
- Sonthalia S, Sharma P, Kapoor J, et al. Habit tic deformity: need fora comprehensive approach. Skin Appendage Disord. 2019;5:117-118.doi:10.1159/000489320 .05.036
- Rieder EA, Tosti A. Onychotillomania: an underrecognized disorder. J Am Acad Dermatol. 2016;75:1245-1250.doi:10.1016/j.jaad.2016
- Ring DS. Inexpensive solution for habit-tic deformity. Arch Dermatol. 2010;146:1222-1223. doi:10.1001/archdermatol.2010.287
- Horne MI, Utzig JB, Rieder EA, et al. Alopecia areata and habit tic deformities. Skin Appendage Disord. 2018;4:323-325. doi:10.1159/000486540
- Sonthalia S, Sharma P, Kapoor J, et al. Habit tic deformity: need fora comprehensive approach. Skin Appendage Disord. 2019;5:117-118.doi:10.1159/000489320 .05.036
A healthy 13-year-old boy presented to the dermatology department with dystrophy of the right thumbnail of 3 to 4 years’ duration. A 5-mm-wide, depressed median longitudinal groove with a fir tree pattern was noted on the central nail plate. The patient noted that the groove had been gradually deepening. There was erythema, edema, and lichenification of the proximal nailfold without vascular changes, and the lunula was enlarged. No hyperkeratosis, subungual debris, erythematous nail folds, or inward curvature of the lateral aspects of the nail were noted. The patient denied any pruritus, pain, discomfort, or bleeding; he also denied any recent illness or trauma to the nail. None of the other nails were affected, and no other lesions or rashes were observed elsewhere on the body. The patient was unsure if he picked at the nail but acknowledged that he may have done so subconsciously. He had no history of eczema, psoriasis, or autoimmune connective tissue disorders.

Sea Buckthorn
A member of the Elaeagnaceae family, Hippophae rhamnoides, better known as sea buckthorn, is a high-altitude wild shrub endemic to Europe and Asia with edible fruits and a lengthy record of use in traditional Chinese medicine.1-6 Used as a health supplement and consumed in the diet throughout the world,5 sea buckthorn berries, seeds, and leaves have been used in traditional medicine to treat burns/injuries, edema, hypertension, inflammation, skin grafts, ulcers, and wounds.4,7
This hardy plant is associated with a wide range of biologic activities, including anti-atherogenic, anti-atopic dermatitis, antibacterial, anticancer, antifungal, anti-inflammatory, antimicrobial, antioxidant, anti-psoriasis, anti-sebum, anti-stress, anti-tumor, cytoprotective, hepatoprotective, immunomodulatory, neuroprotective, radioprotective, and tissue regenerative functions.4,5,8-11
Key Constituents
Functional constituents identified in sea buckthorn include alkaloids, carotenoids, flavonoids, lignans, organic acids, phenolic acids, proanthocyanidins, polyunsaturated acids (including omega-3, -6, -7, and -9), steroids, tannins, terpenoids, and volatile oils, as well as nutritional compounds such as minerals, proteins, and vitamins.4,5,11 Sea buckthorn pericarp oil contains copious amounts of saturated palmitic acid (29%-36%) and omega-7 unsaturated palmitoleic acid (36%-48%), which fosters cutaneous and mucosal epithelialization, as well as linoleic (10%-12%) and oleic (4%-6%) acids.12,6 Significant amounts of carotenoids as well as alpha‐linolenic fatty acid (38%), linoleic (36%), oleic (13%), and palmitic (7%) acids are present in sea buckthorn seed oil.6
Polysaccharides
In an expansive review on the pharmacological activities of sea buckthorn polysaccharides, Teng and colleagues reported in April 2024 that 20 diverse polysaccharides have been culled from sea buckthorn and exhibited various healthy activities, including antioxidant, anti-fatigue, anti-inflammatory, anti-obesity, anti-tumor, hepatoprotective, hypoglycemic, and immunoregulation, and regulation of intestinal flora activities.1
Proanthocyanidins and Anti-Aging
In 2023, Liu and colleagues investigated the anti–skin aging impact of sea buckthorn proanthocyanidins in D-galactose-induced aging in mice given the known free radical scavenging activity of these compounds. They found the proanthocyanidins mitigated D-galactose-induced aging and can augment the total antioxidant capacity of the body. Sea buckthorn proanthocyanidins can further attenuate the effects of skin aging by regulating the TGF-beta1/Smads pathway and MMPs/TIMP system, thus amplifying collagen I and tropoelastin content.13
A year earlier, many of the same investigators assessed the possible protective activity of sea buckthorn proanthocyanidins against cutaneous aging engendered by oxidative stress from hydrogen peroxide. The compounds amplified superoxide dismutase and glutathione antioxidant functions. The extracts also fostered collagen I production in aging human skin fibroblasts via the TGF-beta1/Smads pathway and hindered collagen I degradation by regulating the MMPs/TIMPs system, which maintained extracellular matrix integrity. Senescent cell migration was also promoted with 100 mcg/mL of sea buckthorn proanthocyanidins. The researchers concluded that this sets the stage for investigating how sea buckthorn proanthocyanidins can be incorporated in cosmetic formulations.14 In a separate study, Liu and colleagues demonstrated that sea buckthorn proanthocyanidins can attenuate oxidative damage and protect mitochondrial function.9
Acne and Barrier Functions
The extracts of H rhamnoides and Cassia fistula in a combined formulation were found to be effective in lowering skin sebum content in humans with grade I and grade II acne vulgaris in a 2014 single-blind, randomized, placebo-controlled, split-face study with two groups of 25 patients each (aged 18-37 years).15 Khan and colleagues have also reported that a sea buckthorn oil-in-water emulsion improved barrier function in human skin as tested by a tewameter and corneometer (noninvasive probes) in 13 healthy males with a mean age of 27 ± 4.8 years.16
Anti-Aging, Antioxidant, Antibacterial, Skin-Whitening Activity
Zaman and colleagues reported in 2011 that results from an in vivo study of the effects of a sea buckthorn fruit extract topical cream on stratum corneum water content and transepidermal water loss indicated that the formulation enhanced cell surface integrin expression thus facilitating collagen contraction.17
In 2012, Khan and colleagues reported amelioration in skin elasticity, thus achieving an anti-aging result, from the use of a water-in-oil–based hydroalcoholic cream loaded with fruit extract of H rhamnoides, as measured with a Cutometer.18 The previous year, some of the same researchers reported that the antioxidants and flavonoids found in a topical sea buckthorn formulation could decrease cutaneous melanin and erythema levels.
More recently, Gęgotek and colleagues found that sea buckthorn seed oil prevented redox balance and lipid metabolism disturbances in skin fibroblasts and keratinocytes caused by UVA or UVB. They suggested that such findings point to the potential of this natural agent to confer anti-inflammatory properties and photoprotection to the skin.19
In 2020, Ivanišová and colleagues investigated the antioxidant and antimicrobial activities of H rhamnoides 100% oil, 100% juice, dry berries, and tea (dry berries, leaves, and twigs). They found that all of the studied sea buckthorn products displayed high antioxidant activity (identified through DPPH radical scavenging and molybdenum reducing antioxidant power tests). Sea buckthorn juice contained the highest total content of polyphenols, flavonoids, and carotenoids. All of the tested products also exhibited substantial antibacterial activity against the tested microbes.20
Burns and Wound Healing
In a preclinical study of the effects of sea buckthorn leaf extracts on wound healing in albino rats using an excision-punch wound model in 2005, Gupta and colleagues found that twice daily topical application of the aqueous leaf extract fostered wound healing. This was indicated by higher hydroxyproline and protein levels, a diminished wound area, and lower lipid peroxide levels. The investigators suggested that sea buckthorn may facilitate wound healing at least in part because of elevated antioxidant activity in the granulation tissue.3
A year later, Wang and colleagues reported on observations of using H rhamnoides oil, a traditional Chinese herbal medicine derived from sea buckthorn fruit, as a burn treatment. In the study, 151 burn patients received an H rhamnoides oil dressing (changed every other day until wound healing) that was covered with a disinfecting dressing. The dressing reduced swelling and effusion, and alleviated pain, with patients receiving the sea buckthorn dressing experiencing greater apparent exudation reduction, pain reduction, and more rapid epithelial cell growth and wound healing than controls (treated only with Vaseline gauze). The difference between the two groups was statistically significant.21
Conclusion
Sea buckthorn has been used for hundreds if not thousands of years in traditional medical applications, including for dermatologic purposes. Emerging data appear to support the use of this dynamic plant for consideration in dermatologic applications. As is often the case, much more work is necessary in the form of randomized controlled trials to determine the effectiveness of sea buckthorn formulations as well as the most appropriate avenues of research or uses for dermatologic application of this traditionally used botanical agent.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions, a SaaS company used to generate skin care routines in office and as a e-commerce solution. Write to her at [email protected].
References
1. Teng H et al. J Ethnopharmacol. 2024 Apr 24;324:117809. doi: 10.1016/j.jep.2024.117809.
2. Wang Z et al. Int J Biol Macromol. 2024 Apr;263(Pt 1):130206. doi: 10.1016/j.ijbiomac.2024.130206.
3. Gupta A et al. Int J Low Extrem Wounds. 2005 Jun;4(2):88-92. doi: 10.1177/1534734605277401.
4. Pundir S et al. J Ethnopharmacol. 2021 Feb 10;266:113434. doi: 10.1016/j.jep.2020.113434.
5. Ma QG et al. J Agric Food Chem. 2023 Mar 29;71(12):4769-4788. doi: 10.1021/acs.jafc.2c06916.
6. Poljšak N et al. Phytother Res. 2020 Feb;34(2):254-269. doi: 10.1002/ptr.6524. doi: 10.1002/ptr.6524.
7. Upadhyay NK et al. Evid Based Complement Alternat Med. 2011;2011:659705. doi: 10.1093/ecam/nep189.
8. Suryakumar G, Gupta A. J Ethnopharmacol. 2011 Nov 18;138(2):268-78. doi: 10.1016/j.jep.2011.09.024.
9. Liu K et al. Front Pharmacol. 2022 Jul 8;13:914146. doi: 10.3389/fphar.2022.914146.
10. Akhtar N et al. J Pharm Bioallied Sci. 2010 Jan;2(1):13-7. doi: 10.4103/0975-7406.62698.
11. Ren R et al. RSC Adv. 2020 Dec 17;10(73):44654-44671. doi: 10.1039/d0ra06488b.
12. Ito H et al. Burns. 2014 May;40(3):511-9. doi: 10.1016/j.burns.2013.08.011.
13. Liu X et al. Food Sci Nutr. 2023 Dec 7;12(2):1082-1094. doi: 10.1002/fsn3.3823.
14. Liu X at al. Antioxidants (Basel). 2022 Sep 25;11(10):1900. doi: 10.3390/antiox11101900.
15. Khan BA, Akhtar N. Postepy Dermatol Alergol. 2014 Aug;31(4):229-234. doi: 10.5114/pdia.2014.40934.
16. Khan BA, Akhtar N. Pak J Pharm Sci. 2014 Nov;27(6):1919-22.
17. Khan AB et al. African J Pharm Pharmacol. 2011 Aug;5(8):1092-5.
18. Khan BA, Akhtar N, Braga VA. Trop J Pharm Res. 2012;11(6):955-62.
19. Gęgotek A et al. Antioxidants (Basel). 2018 Aug 23;7(9):110. doi: 10.3390/antiox7090110.
20. Ivanišová E et al. Acta Sci Pol Technol Aliment. 2020 Apr-Jun;19(2):195-205. doi: 10.17306/J.AFS.0809.
21. Wang ZY, Luo XL, He CP. Nan Fang Yi Ke Da Xue Xue Bao. 2006 Jan;26(1):124-5.
A member of the Elaeagnaceae family, Hippophae rhamnoides, better known as sea buckthorn, is a high-altitude wild shrub endemic to Europe and Asia with edible fruits and a lengthy record of use in traditional Chinese medicine.1-6 Used as a health supplement and consumed in the diet throughout the world,5 sea buckthorn berries, seeds, and leaves have been used in traditional medicine to treat burns/injuries, edema, hypertension, inflammation, skin grafts, ulcers, and wounds.4,7
This hardy plant is associated with a wide range of biologic activities, including anti-atherogenic, anti-atopic dermatitis, antibacterial, anticancer, antifungal, anti-inflammatory, antimicrobial, antioxidant, anti-psoriasis, anti-sebum, anti-stress, anti-tumor, cytoprotective, hepatoprotective, immunomodulatory, neuroprotective, radioprotective, and tissue regenerative functions.4,5,8-11
Key Constituents
Functional constituents identified in sea buckthorn include alkaloids, carotenoids, flavonoids, lignans, organic acids, phenolic acids, proanthocyanidins, polyunsaturated acids (including omega-3, -6, -7, and -9), steroids, tannins, terpenoids, and volatile oils, as well as nutritional compounds such as minerals, proteins, and vitamins.4,5,11 Sea buckthorn pericarp oil contains copious amounts of saturated palmitic acid (29%-36%) and omega-7 unsaturated palmitoleic acid (36%-48%), which fosters cutaneous and mucosal epithelialization, as well as linoleic (10%-12%) and oleic (4%-6%) acids.12,6 Significant amounts of carotenoids as well as alpha‐linolenic fatty acid (38%), linoleic (36%), oleic (13%), and palmitic (7%) acids are present in sea buckthorn seed oil.6
Polysaccharides
In an expansive review on the pharmacological activities of sea buckthorn polysaccharides, Teng and colleagues reported in April 2024 that 20 diverse polysaccharides have been culled from sea buckthorn and exhibited various healthy activities, including antioxidant, anti-fatigue, anti-inflammatory, anti-obesity, anti-tumor, hepatoprotective, hypoglycemic, and immunoregulation, and regulation of intestinal flora activities.1
Proanthocyanidins and Anti-Aging
In 2023, Liu and colleagues investigated the anti–skin aging impact of sea buckthorn proanthocyanidins in D-galactose-induced aging in mice given the known free radical scavenging activity of these compounds. They found the proanthocyanidins mitigated D-galactose-induced aging and can augment the total antioxidant capacity of the body. Sea buckthorn proanthocyanidins can further attenuate the effects of skin aging by regulating the TGF-beta1/Smads pathway and MMPs/TIMP system, thus amplifying collagen I and tropoelastin content.13
A year earlier, many of the same investigators assessed the possible protective activity of sea buckthorn proanthocyanidins against cutaneous aging engendered by oxidative stress from hydrogen peroxide. The compounds amplified superoxide dismutase and glutathione antioxidant functions. The extracts also fostered collagen I production in aging human skin fibroblasts via the TGF-beta1/Smads pathway and hindered collagen I degradation by regulating the MMPs/TIMPs system, which maintained extracellular matrix integrity. Senescent cell migration was also promoted with 100 mcg/mL of sea buckthorn proanthocyanidins. The researchers concluded that this sets the stage for investigating how sea buckthorn proanthocyanidins can be incorporated in cosmetic formulations.14 In a separate study, Liu and colleagues demonstrated that sea buckthorn proanthocyanidins can attenuate oxidative damage and protect mitochondrial function.9
Acne and Barrier Functions
The extracts of H rhamnoides and Cassia fistula in a combined formulation were found to be effective in lowering skin sebum content in humans with grade I and grade II acne vulgaris in a 2014 single-blind, randomized, placebo-controlled, split-face study with two groups of 25 patients each (aged 18-37 years).15 Khan and colleagues have also reported that a sea buckthorn oil-in-water emulsion improved barrier function in human skin as tested by a tewameter and corneometer (noninvasive probes) in 13 healthy males with a mean age of 27 ± 4.8 years.16
Anti-Aging, Antioxidant, Antibacterial, Skin-Whitening Activity
Zaman and colleagues reported in 2011 that results from an in vivo study of the effects of a sea buckthorn fruit extract topical cream on stratum corneum water content and transepidermal water loss indicated that the formulation enhanced cell surface integrin expression thus facilitating collagen contraction.17
In 2012, Khan and colleagues reported amelioration in skin elasticity, thus achieving an anti-aging result, from the use of a water-in-oil–based hydroalcoholic cream loaded with fruit extract of H rhamnoides, as measured with a Cutometer.18 The previous year, some of the same researchers reported that the antioxidants and flavonoids found in a topical sea buckthorn formulation could decrease cutaneous melanin and erythema levels.
More recently, Gęgotek and colleagues found that sea buckthorn seed oil prevented redox balance and lipid metabolism disturbances in skin fibroblasts and keratinocytes caused by UVA or UVB. They suggested that such findings point to the potential of this natural agent to confer anti-inflammatory properties and photoprotection to the skin.19
In 2020, Ivanišová and colleagues investigated the antioxidant and antimicrobial activities of H rhamnoides 100% oil, 100% juice, dry berries, and tea (dry berries, leaves, and twigs). They found that all of the studied sea buckthorn products displayed high antioxidant activity (identified through DPPH radical scavenging and molybdenum reducing antioxidant power tests). Sea buckthorn juice contained the highest total content of polyphenols, flavonoids, and carotenoids. All of the tested products also exhibited substantial antibacterial activity against the tested microbes.20
Burns and Wound Healing
In a preclinical study of the effects of sea buckthorn leaf extracts on wound healing in albino rats using an excision-punch wound model in 2005, Gupta and colleagues found that twice daily topical application of the aqueous leaf extract fostered wound healing. This was indicated by higher hydroxyproline and protein levels, a diminished wound area, and lower lipid peroxide levels. The investigators suggested that sea buckthorn may facilitate wound healing at least in part because of elevated antioxidant activity in the granulation tissue.3
A year later, Wang and colleagues reported on observations of using H rhamnoides oil, a traditional Chinese herbal medicine derived from sea buckthorn fruit, as a burn treatment. In the study, 151 burn patients received an H rhamnoides oil dressing (changed every other day until wound healing) that was covered with a disinfecting dressing. The dressing reduced swelling and effusion, and alleviated pain, with patients receiving the sea buckthorn dressing experiencing greater apparent exudation reduction, pain reduction, and more rapid epithelial cell growth and wound healing than controls (treated only with Vaseline gauze). The difference between the two groups was statistically significant.21
Conclusion
Sea buckthorn has been used for hundreds if not thousands of years in traditional medical applications, including for dermatologic purposes. Emerging data appear to support the use of this dynamic plant for consideration in dermatologic applications. As is often the case, much more work is necessary in the form of randomized controlled trials to determine the effectiveness of sea buckthorn formulations as well as the most appropriate avenues of research or uses for dermatologic application of this traditionally used botanical agent.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions, a SaaS company used to generate skin care routines in office and as a e-commerce solution. Write to her at [email protected].
References
1. Teng H et al. J Ethnopharmacol. 2024 Apr 24;324:117809. doi: 10.1016/j.jep.2024.117809.
2. Wang Z et al. Int J Biol Macromol. 2024 Apr;263(Pt 1):130206. doi: 10.1016/j.ijbiomac.2024.130206.
3. Gupta A et al. Int J Low Extrem Wounds. 2005 Jun;4(2):88-92. doi: 10.1177/1534734605277401.
4. Pundir S et al. J Ethnopharmacol. 2021 Feb 10;266:113434. doi: 10.1016/j.jep.2020.113434.
5. Ma QG et al. J Agric Food Chem. 2023 Mar 29;71(12):4769-4788. doi: 10.1021/acs.jafc.2c06916.
6. Poljšak N et al. Phytother Res. 2020 Feb;34(2):254-269. doi: 10.1002/ptr.6524. doi: 10.1002/ptr.6524.
7. Upadhyay NK et al. Evid Based Complement Alternat Med. 2011;2011:659705. doi: 10.1093/ecam/nep189.
8. Suryakumar G, Gupta A. J Ethnopharmacol. 2011 Nov 18;138(2):268-78. doi: 10.1016/j.jep.2011.09.024.
9. Liu K et al. Front Pharmacol. 2022 Jul 8;13:914146. doi: 10.3389/fphar.2022.914146.
10. Akhtar N et al. J Pharm Bioallied Sci. 2010 Jan;2(1):13-7. doi: 10.4103/0975-7406.62698.
11. Ren R et al. RSC Adv. 2020 Dec 17;10(73):44654-44671. doi: 10.1039/d0ra06488b.
12. Ito H et al. Burns. 2014 May;40(3):511-9. doi: 10.1016/j.burns.2013.08.011.
13. Liu X et al. Food Sci Nutr. 2023 Dec 7;12(2):1082-1094. doi: 10.1002/fsn3.3823.
14. Liu X at al. Antioxidants (Basel). 2022 Sep 25;11(10):1900. doi: 10.3390/antiox11101900.
15. Khan BA, Akhtar N. Postepy Dermatol Alergol. 2014 Aug;31(4):229-234. doi: 10.5114/pdia.2014.40934.
16. Khan BA, Akhtar N. Pak J Pharm Sci. 2014 Nov;27(6):1919-22.
17. Khan AB et al. African J Pharm Pharmacol. 2011 Aug;5(8):1092-5.
18. Khan BA, Akhtar N, Braga VA. Trop J Pharm Res. 2012;11(6):955-62.
19. Gęgotek A et al. Antioxidants (Basel). 2018 Aug 23;7(9):110. doi: 10.3390/antiox7090110.
20. Ivanišová E et al. Acta Sci Pol Technol Aliment. 2020 Apr-Jun;19(2):195-205. doi: 10.17306/J.AFS.0809.
21. Wang ZY, Luo XL, He CP. Nan Fang Yi Ke Da Xue Xue Bao. 2006 Jan;26(1):124-5.
A member of the Elaeagnaceae family, Hippophae rhamnoides, better known as sea buckthorn, is a high-altitude wild shrub endemic to Europe and Asia with edible fruits and a lengthy record of use in traditional Chinese medicine.1-6 Used as a health supplement and consumed in the diet throughout the world,5 sea buckthorn berries, seeds, and leaves have been used in traditional medicine to treat burns/injuries, edema, hypertension, inflammation, skin grafts, ulcers, and wounds.4,7
This hardy plant is associated with a wide range of biologic activities, including anti-atherogenic, anti-atopic dermatitis, antibacterial, anticancer, antifungal, anti-inflammatory, antimicrobial, antioxidant, anti-psoriasis, anti-sebum, anti-stress, anti-tumor, cytoprotective, hepatoprotective, immunomodulatory, neuroprotective, radioprotective, and tissue regenerative functions.4,5,8-11
Key Constituents
Functional constituents identified in sea buckthorn include alkaloids, carotenoids, flavonoids, lignans, organic acids, phenolic acids, proanthocyanidins, polyunsaturated acids (including omega-3, -6, -7, and -9), steroids, tannins, terpenoids, and volatile oils, as well as nutritional compounds such as minerals, proteins, and vitamins.4,5,11 Sea buckthorn pericarp oil contains copious amounts of saturated palmitic acid (29%-36%) and omega-7 unsaturated palmitoleic acid (36%-48%), which fosters cutaneous and mucosal epithelialization, as well as linoleic (10%-12%) and oleic (4%-6%) acids.12,6 Significant amounts of carotenoids as well as alpha‐linolenic fatty acid (38%), linoleic (36%), oleic (13%), and palmitic (7%) acids are present in sea buckthorn seed oil.6
Polysaccharides
In an expansive review on the pharmacological activities of sea buckthorn polysaccharides, Teng and colleagues reported in April 2024 that 20 diverse polysaccharides have been culled from sea buckthorn and exhibited various healthy activities, including antioxidant, anti-fatigue, anti-inflammatory, anti-obesity, anti-tumor, hepatoprotective, hypoglycemic, and immunoregulation, and regulation of intestinal flora activities.1
Proanthocyanidins and Anti-Aging
In 2023, Liu and colleagues investigated the anti–skin aging impact of sea buckthorn proanthocyanidins in D-galactose-induced aging in mice given the known free radical scavenging activity of these compounds. They found the proanthocyanidins mitigated D-galactose-induced aging and can augment the total antioxidant capacity of the body. Sea buckthorn proanthocyanidins can further attenuate the effects of skin aging by regulating the TGF-beta1/Smads pathway and MMPs/TIMP system, thus amplifying collagen I and tropoelastin content.13
A year earlier, many of the same investigators assessed the possible protective activity of sea buckthorn proanthocyanidins against cutaneous aging engendered by oxidative stress from hydrogen peroxide. The compounds amplified superoxide dismutase and glutathione antioxidant functions. The extracts also fostered collagen I production in aging human skin fibroblasts via the TGF-beta1/Smads pathway and hindered collagen I degradation by regulating the MMPs/TIMPs system, which maintained extracellular matrix integrity. Senescent cell migration was also promoted with 100 mcg/mL of sea buckthorn proanthocyanidins. The researchers concluded that this sets the stage for investigating how sea buckthorn proanthocyanidins can be incorporated in cosmetic formulations.14 In a separate study, Liu and colleagues demonstrated that sea buckthorn proanthocyanidins can attenuate oxidative damage and protect mitochondrial function.9
Acne and Barrier Functions
The extracts of H rhamnoides and Cassia fistula in a combined formulation were found to be effective in lowering skin sebum content in humans with grade I and grade II acne vulgaris in a 2014 single-blind, randomized, placebo-controlled, split-face study with two groups of 25 patients each (aged 18-37 years).15 Khan and colleagues have also reported that a sea buckthorn oil-in-water emulsion improved barrier function in human skin as tested by a tewameter and corneometer (noninvasive probes) in 13 healthy males with a mean age of 27 ± 4.8 years.16
Anti-Aging, Antioxidant, Antibacterial, Skin-Whitening Activity
Zaman and colleagues reported in 2011 that results from an in vivo study of the effects of a sea buckthorn fruit extract topical cream on stratum corneum water content and transepidermal water loss indicated that the formulation enhanced cell surface integrin expression thus facilitating collagen contraction.17
In 2012, Khan and colleagues reported amelioration in skin elasticity, thus achieving an anti-aging result, from the use of a water-in-oil–based hydroalcoholic cream loaded with fruit extract of H rhamnoides, as measured with a Cutometer.18 The previous year, some of the same researchers reported that the antioxidants and flavonoids found in a topical sea buckthorn formulation could decrease cutaneous melanin and erythema levels.
More recently, Gęgotek and colleagues found that sea buckthorn seed oil prevented redox balance and lipid metabolism disturbances in skin fibroblasts and keratinocytes caused by UVA or UVB. They suggested that such findings point to the potential of this natural agent to confer anti-inflammatory properties and photoprotection to the skin.19
In 2020, Ivanišová and colleagues investigated the antioxidant and antimicrobial activities of H rhamnoides 100% oil, 100% juice, dry berries, and tea (dry berries, leaves, and twigs). They found that all of the studied sea buckthorn products displayed high antioxidant activity (identified through DPPH radical scavenging and molybdenum reducing antioxidant power tests). Sea buckthorn juice contained the highest total content of polyphenols, flavonoids, and carotenoids. All of the tested products also exhibited substantial antibacterial activity against the tested microbes.20
Burns and Wound Healing
In a preclinical study of the effects of sea buckthorn leaf extracts on wound healing in albino rats using an excision-punch wound model in 2005, Gupta and colleagues found that twice daily topical application of the aqueous leaf extract fostered wound healing. This was indicated by higher hydroxyproline and protein levels, a diminished wound area, and lower lipid peroxide levels. The investigators suggested that sea buckthorn may facilitate wound healing at least in part because of elevated antioxidant activity in the granulation tissue.3
A year later, Wang and colleagues reported on observations of using H rhamnoides oil, a traditional Chinese herbal medicine derived from sea buckthorn fruit, as a burn treatment. In the study, 151 burn patients received an H rhamnoides oil dressing (changed every other day until wound healing) that was covered with a disinfecting dressing. The dressing reduced swelling and effusion, and alleviated pain, with patients receiving the sea buckthorn dressing experiencing greater apparent exudation reduction, pain reduction, and more rapid epithelial cell growth and wound healing than controls (treated only with Vaseline gauze). The difference between the two groups was statistically significant.21
Conclusion
Sea buckthorn has been used for hundreds if not thousands of years in traditional medical applications, including for dermatologic purposes. Emerging data appear to support the use of this dynamic plant for consideration in dermatologic applications. As is often the case, much more work is necessary in the form of randomized controlled trials to determine the effectiveness of sea buckthorn formulations as well as the most appropriate avenues of research or uses for dermatologic application of this traditionally used botanical agent.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions, a SaaS company used to generate skin care routines in office and as a e-commerce solution. Write to her at [email protected].
References
1. Teng H et al. J Ethnopharmacol. 2024 Apr 24;324:117809. doi: 10.1016/j.jep.2024.117809.
2. Wang Z et al. Int J Biol Macromol. 2024 Apr;263(Pt 1):130206. doi: 10.1016/j.ijbiomac.2024.130206.
3. Gupta A et al. Int J Low Extrem Wounds. 2005 Jun;4(2):88-92. doi: 10.1177/1534734605277401.
4. Pundir S et al. J Ethnopharmacol. 2021 Feb 10;266:113434. doi: 10.1016/j.jep.2020.113434.
5. Ma QG et al. J Agric Food Chem. 2023 Mar 29;71(12):4769-4788. doi: 10.1021/acs.jafc.2c06916.
6. Poljšak N et al. Phytother Res. 2020 Feb;34(2):254-269. doi: 10.1002/ptr.6524. doi: 10.1002/ptr.6524.
7. Upadhyay NK et al. Evid Based Complement Alternat Med. 2011;2011:659705. doi: 10.1093/ecam/nep189.
8. Suryakumar G, Gupta A. J Ethnopharmacol. 2011 Nov 18;138(2):268-78. doi: 10.1016/j.jep.2011.09.024.
9. Liu K et al. Front Pharmacol. 2022 Jul 8;13:914146. doi: 10.3389/fphar.2022.914146.
10. Akhtar N et al. J Pharm Bioallied Sci. 2010 Jan;2(1):13-7. doi: 10.4103/0975-7406.62698.
11. Ren R et al. RSC Adv. 2020 Dec 17;10(73):44654-44671. doi: 10.1039/d0ra06488b.
12. Ito H et al. Burns. 2014 May;40(3):511-9. doi: 10.1016/j.burns.2013.08.011.
13. Liu X et al. Food Sci Nutr. 2023 Dec 7;12(2):1082-1094. doi: 10.1002/fsn3.3823.
14. Liu X at al. Antioxidants (Basel). 2022 Sep 25;11(10):1900. doi: 10.3390/antiox11101900.
15. Khan BA, Akhtar N. Postepy Dermatol Alergol. 2014 Aug;31(4):229-234. doi: 10.5114/pdia.2014.40934.
16. Khan BA, Akhtar N. Pak J Pharm Sci. 2014 Nov;27(6):1919-22.
17. Khan AB et al. African J Pharm Pharmacol. 2011 Aug;5(8):1092-5.
18. Khan BA, Akhtar N, Braga VA. Trop J Pharm Res. 2012;11(6):955-62.
19. Gęgotek A et al. Antioxidants (Basel). 2018 Aug 23;7(9):110. doi: 10.3390/antiox7090110.
20. Ivanišová E et al. Acta Sci Pol Technol Aliment. 2020 Apr-Jun;19(2):195-205. doi: 10.17306/J.AFS.0809.
21. Wang ZY, Luo XL, He CP. Nan Fang Yi Ke Da Xue Xue Bao. 2006 Jan;26(1):124-5.
Skin Fungal Infections Increasing in the United States
TOPLINE:
. Tinea unguium, tinea pedis, and tinea corporis were among the most common infections.
METHODOLOGY:
- Researchers analyzed data from the National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey from 2005 to 2016, to evaluate trends in the prevalence of SCFIs during this period.
- The analysis included over 13 billion ambulatory visits to nonfederally funded community, office-based physician practices, and emergency or outpatient departments in the United States, with an estimated 1,104,258,333 annual average.
- The Jonckheere-Terpstra nonparametric test for trend was used to determine the pattern of SCFI prevalence over the 12-year period.
TAKEAWAY:
- SCFIs constituted approximately 0.54% of all annual ambulatory visits, with an estimated 6,001,852 visits for SCFIs per year and over 72 million total visits for the infections during the study period.
- Tinea unguium, tinea pedis, and tinea corporis were the most common infections, comprising 20.5%, 12.2%, and 12.0% of the total visits, respectively.
- Researchers noted an increasing trend in annual SCFIs (P = .03).
IN PRACTICE:
“We observed a high burden of SCFIs among outpatient visits in the United States and an increasing trend in their prevalence,” the authors wrote. These results, they added, “highlight the importance of healthcare providers being able to identify, treat, and, when necessary, refer patients with SCFIs, as a high burden of disease is associated with a significant negative impact on the individual and population levels.”
SOURCE:
The study was co-led by Sarah L. Spaulding, BS, and A. Mitchel Wride, BA, from the Yale School of Medicine, New Haven, Connecticut, and was published online October 30 in the Journal of the American Academy of Dermatology.
LIMITATIONS:
The authors did not list any study limitations.
DISCLOSURES:
The lead authors were supported by Yale School of Medicine Medical Student Research Fellowships. Two other authors declared receiving consulting fees, research funding, and licensing fees outside the submitted work and also served on a data and safety monitoring board for Advarra Inc.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
. Tinea unguium, tinea pedis, and tinea corporis were among the most common infections.
METHODOLOGY:
- Researchers analyzed data from the National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey from 2005 to 2016, to evaluate trends in the prevalence of SCFIs during this period.
- The analysis included over 13 billion ambulatory visits to nonfederally funded community, office-based physician practices, and emergency or outpatient departments in the United States, with an estimated 1,104,258,333 annual average.
- The Jonckheere-Terpstra nonparametric test for trend was used to determine the pattern of SCFI prevalence over the 12-year period.
TAKEAWAY:
- SCFIs constituted approximately 0.54% of all annual ambulatory visits, with an estimated 6,001,852 visits for SCFIs per year and over 72 million total visits for the infections during the study period.
- Tinea unguium, tinea pedis, and tinea corporis were the most common infections, comprising 20.5%, 12.2%, and 12.0% of the total visits, respectively.
- Researchers noted an increasing trend in annual SCFIs (P = .03).
IN PRACTICE:
“We observed a high burden of SCFIs among outpatient visits in the United States and an increasing trend in their prevalence,” the authors wrote. These results, they added, “highlight the importance of healthcare providers being able to identify, treat, and, when necessary, refer patients with SCFIs, as a high burden of disease is associated with a significant negative impact on the individual and population levels.”
SOURCE:
The study was co-led by Sarah L. Spaulding, BS, and A. Mitchel Wride, BA, from the Yale School of Medicine, New Haven, Connecticut, and was published online October 30 in the Journal of the American Academy of Dermatology.
LIMITATIONS:
The authors did not list any study limitations.
DISCLOSURES:
The lead authors were supported by Yale School of Medicine Medical Student Research Fellowships. Two other authors declared receiving consulting fees, research funding, and licensing fees outside the submitted work and also served on a data and safety monitoring board for Advarra Inc.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
. Tinea unguium, tinea pedis, and tinea corporis were among the most common infections.
METHODOLOGY:
- Researchers analyzed data from the National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey from 2005 to 2016, to evaluate trends in the prevalence of SCFIs during this period.
- The analysis included over 13 billion ambulatory visits to nonfederally funded community, office-based physician practices, and emergency or outpatient departments in the United States, with an estimated 1,104,258,333 annual average.
- The Jonckheere-Terpstra nonparametric test for trend was used to determine the pattern of SCFI prevalence over the 12-year period.
TAKEAWAY:
- SCFIs constituted approximately 0.54% of all annual ambulatory visits, with an estimated 6,001,852 visits for SCFIs per year and over 72 million total visits for the infections during the study period.
- Tinea unguium, tinea pedis, and tinea corporis were the most common infections, comprising 20.5%, 12.2%, and 12.0% of the total visits, respectively.
- Researchers noted an increasing trend in annual SCFIs (P = .03).
IN PRACTICE:
“We observed a high burden of SCFIs among outpatient visits in the United States and an increasing trend in their prevalence,” the authors wrote. These results, they added, “highlight the importance of healthcare providers being able to identify, treat, and, when necessary, refer patients with SCFIs, as a high burden of disease is associated with a significant negative impact on the individual and population levels.”
SOURCE:
The study was co-led by Sarah L. Spaulding, BS, and A. Mitchel Wride, BA, from the Yale School of Medicine, New Haven, Connecticut, and was published online October 30 in the Journal of the American Academy of Dermatology.
LIMITATIONS:
The authors did not list any study limitations.
DISCLOSURES:
The lead authors were supported by Yale School of Medicine Medical Student Research Fellowships. Two other authors declared receiving consulting fees, research funding, and licensing fees outside the submitted work and also served on a data and safety monitoring board for Advarra Inc.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Study Finds Link to Increased Risk for Bulimia, Binge Eating and HS
“Clinicians should actively screen for eating disorders,” particularly bulimia nervosa and binge eating disorder, in patients with HS,” lead study author Christopher Guirguis, DMD, a student at Georgetown University School of Medicine, Washington, DC, told this news organization in advance of the annual Symposium on Hidradenitis Suppurative Advances, where the study was presented during an oral abstract session. “The significant psychological burden in these patients requires a holistic approach that integrates both dermatologic and psychosocial care. Addressing their mental health needs is essential for improving overall patient outcomes and quality of life,” he added.
In collaboration with fellow Georgetown medical student and first author Lauren Chin and Mikael Horissian, MD, a dermatologist and director of the HS Clinic at Gesinger Health System, Danville, Pennsylvania, Guirguis drew from the National Institutes of Health’s All of Us Research Program to identify 1653 individuals with a diagnosis of HS and a control group of 8265 individuals without a diagnosis of HS. They used the Observational Medical Outcomes Partnership to identify anorexia nervosa, bulimia nervosa, body dysmorphic disorder, binge eating disorder, and eating disorder, unspecified. Obsessive-compulsive disorder (OCD) was also included because of its association with bulimia. They used statistical models to compare cohorts and comorbidities. “What makes this work unique is its focus on the link between HS and eating disorders, a relationship previously underexplored,” he said.
The mean age of the overall study cohort was 46.8 years, and 78.6% were female. Univariate analysis revealed that, compared with controls, individuals in the HS cohort showed significantly increased diagnoses of bulimia, binge eating disorder, OCD, and eating disorder, unspecified, by 2.6, 5.48, 2.50, and 2.43 times, respectively (P < .05 for all associations). After adjusting for age, race, sex, and ethnicity, the researchers observed that patients with HS were 4.46 times as likely to have a diagnosis of binge eating disorder and 3.51 times as likely to have a diagnosis of bulimia as those who did not have HS (P < .05 for both associations).
Guirguis said that the absence of body dysmorphic disorder diagnoses in the HS cohort was unexpected. “Given HS’s known association with body image issues, we anticipated a higher prevalence of BDD,” he said. “This discrepancy may reflect underreporting or diagnostic overshadowing, where the physical symptoms of HS dominate clinical attention, potentially masking or complicating the identification of psychological conditions like BDD.”
He acknowledged certain limitations of the study, including the potential for variations in documentation practices in the database. “Additionally, there may be bias due to underrepresentation of certain demographic groups or underreporting of psychological comorbidities, which could influence the findings.”
Patricia M. Richey, MD, assistant professor of dermatology, at Boston University School of Medicine in Massachusetts, who was asked to comment on the study, said the results “should affect how physicians discuss lifestyle recommendations in those already at increased risk of psychiatric disease and disrupted body image.” The findings should also “prompt physicians to screen this patient population more thoroughly for eating disorders as we know they are an underrecognized and often undertreated entity,” she added.
Neither the study authors nor Richey reported having relevant disclosures.
A version of this article appeared on Medscape.com.
“Clinicians should actively screen for eating disorders,” particularly bulimia nervosa and binge eating disorder, in patients with HS,” lead study author Christopher Guirguis, DMD, a student at Georgetown University School of Medicine, Washington, DC, told this news organization in advance of the annual Symposium on Hidradenitis Suppurative Advances, where the study was presented during an oral abstract session. “The significant psychological burden in these patients requires a holistic approach that integrates both dermatologic and psychosocial care. Addressing their mental health needs is essential for improving overall patient outcomes and quality of life,” he added.
In collaboration with fellow Georgetown medical student and first author Lauren Chin and Mikael Horissian, MD, a dermatologist and director of the HS Clinic at Gesinger Health System, Danville, Pennsylvania, Guirguis drew from the National Institutes of Health’s All of Us Research Program to identify 1653 individuals with a diagnosis of HS and a control group of 8265 individuals without a diagnosis of HS. They used the Observational Medical Outcomes Partnership to identify anorexia nervosa, bulimia nervosa, body dysmorphic disorder, binge eating disorder, and eating disorder, unspecified. Obsessive-compulsive disorder (OCD) was also included because of its association with bulimia. They used statistical models to compare cohorts and comorbidities. “What makes this work unique is its focus on the link between HS and eating disorders, a relationship previously underexplored,” he said.
The mean age of the overall study cohort was 46.8 years, and 78.6% were female. Univariate analysis revealed that, compared with controls, individuals in the HS cohort showed significantly increased diagnoses of bulimia, binge eating disorder, OCD, and eating disorder, unspecified, by 2.6, 5.48, 2.50, and 2.43 times, respectively (P < .05 for all associations). After adjusting for age, race, sex, and ethnicity, the researchers observed that patients with HS were 4.46 times as likely to have a diagnosis of binge eating disorder and 3.51 times as likely to have a diagnosis of bulimia as those who did not have HS (P < .05 for both associations).
Guirguis said that the absence of body dysmorphic disorder diagnoses in the HS cohort was unexpected. “Given HS’s known association with body image issues, we anticipated a higher prevalence of BDD,” he said. “This discrepancy may reflect underreporting or diagnostic overshadowing, where the physical symptoms of HS dominate clinical attention, potentially masking or complicating the identification of psychological conditions like BDD.”
He acknowledged certain limitations of the study, including the potential for variations in documentation practices in the database. “Additionally, there may be bias due to underrepresentation of certain demographic groups or underreporting of psychological comorbidities, which could influence the findings.”
Patricia M. Richey, MD, assistant professor of dermatology, at Boston University School of Medicine in Massachusetts, who was asked to comment on the study, said the results “should affect how physicians discuss lifestyle recommendations in those already at increased risk of psychiatric disease and disrupted body image.” The findings should also “prompt physicians to screen this patient population more thoroughly for eating disorders as we know they are an underrecognized and often undertreated entity,” she added.
Neither the study authors nor Richey reported having relevant disclosures.
A version of this article appeared on Medscape.com.
“Clinicians should actively screen for eating disorders,” particularly bulimia nervosa and binge eating disorder, in patients with HS,” lead study author Christopher Guirguis, DMD, a student at Georgetown University School of Medicine, Washington, DC, told this news organization in advance of the annual Symposium on Hidradenitis Suppurative Advances, where the study was presented during an oral abstract session. “The significant psychological burden in these patients requires a holistic approach that integrates both dermatologic and psychosocial care. Addressing their mental health needs is essential for improving overall patient outcomes and quality of life,” he added.
In collaboration with fellow Georgetown medical student and first author Lauren Chin and Mikael Horissian, MD, a dermatologist and director of the HS Clinic at Gesinger Health System, Danville, Pennsylvania, Guirguis drew from the National Institutes of Health’s All of Us Research Program to identify 1653 individuals with a diagnosis of HS and a control group of 8265 individuals without a diagnosis of HS. They used the Observational Medical Outcomes Partnership to identify anorexia nervosa, bulimia nervosa, body dysmorphic disorder, binge eating disorder, and eating disorder, unspecified. Obsessive-compulsive disorder (OCD) was also included because of its association with bulimia. They used statistical models to compare cohorts and comorbidities. “What makes this work unique is its focus on the link between HS and eating disorders, a relationship previously underexplored,” he said.
The mean age of the overall study cohort was 46.8 years, and 78.6% were female. Univariate analysis revealed that, compared with controls, individuals in the HS cohort showed significantly increased diagnoses of bulimia, binge eating disorder, OCD, and eating disorder, unspecified, by 2.6, 5.48, 2.50, and 2.43 times, respectively (P < .05 for all associations). After adjusting for age, race, sex, and ethnicity, the researchers observed that patients with HS were 4.46 times as likely to have a diagnosis of binge eating disorder and 3.51 times as likely to have a diagnosis of bulimia as those who did not have HS (P < .05 for both associations).
Guirguis said that the absence of body dysmorphic disorder diagnoses in the HS cohort was unexpected. “Given HS’s known association with body image issues, we anticipated a higher prevalence of BDD,” he said. “This discrepancy may reflect underreporting or diagnostic overshadowing, where the physical symptoms of HS dominate clinical attention, potentially masking or complicating the identification of psychological conditions like BDD.”
He acknowledged certain limitations of the study, including the potential for variations in documentation practices in the database. “Additionally, there may be bias due to underrepresentation of certain demographic groups or underreporting of psychological comorbidities, which could influence the findings.”
Patricia M. Richey, MD, assistant professor of dermatology, at Boston University School of Medicine in Massachusetts, who was asked to comment on the study, said the results “should affect how physicians discuss lifestyle recommendations in those already at increased risk of psychiatric disease and disrupted body image.” The findings should also “prompt physicians to screen this patient population more thoroughly for eating disorders as we know they are an underrecognized and often undertreated entity,” she added.
Neither the study authors nor Richey reported having relevant disclosures.
A version of this article appeared on Medscape.com.
Effects of Bimekizumab Durable for HS Through One Year
AMSTERDAM — The monoclonal antibody according to new data from an open-label extension period.
“Efficacy and health-related quality-of-life outcomes were maintained through 2 years of treatment,” study presenter Christos C. Zouboulis, MD, professor of dermatology, venereology, and allergology, Brandenburg Medical School Theodor Fontane, Dessau, Germany, said at the European Academy of Dermatology and Venereology (EADV) 2024 Congress.
“No new safety signals were observed,” he added. “These data highlight the durability and consistency of bimekizumab treatment in patients with moderate to severe hidradenitis suppurativa,” Zouboulis concluded.
Efficacy Maintained
“This is the type of long-term data that clinicians hope to see in large phase 3 trials for hidradenitis suppurativa medications,” commented Jennifer L. Hsiao, MD, clinical associate professor of dermatology, University of Southern California, Los Angeles, who was not involved in the study.
She told this news organization that, beyond maintained improvement of patient-reported quality of life, the results are “raising the bar in terms of measuring treatment success,” with over three quarters of patients achieving a high level of response on the Hidradenitis Suppurativa Clinical Response (HiSCR) scale at the final 96-week follow-up.
“Clinicians and patients have struggled with maintaining treatment efficacy over time with the first [Food and Drug Administration]–approved class of biologics for hidradenitis suppurativa — TNF [tumor necrosis factor]–alpha antagonists,” Hsiao said. She emphasized that sustained treatment efficacy will reduce the need for continued treatment switching and “hopefully improve treatment adherence.”
“It was also helpful to see that, consistent with studies of bimekizumab in psoriasis, rates of oral candidiasis appear to decrease with prolonged exposure over 2 years, though as with any open-label extension study, study dropout is a limitation,” she said.
“The availability of long-term efficacy and safety data, such as those shown in this study, will help guide shared decision-making discussions with our patients.” Overall, Hsiao believes there is “much to be excited about in the field of hidradenitis suppurativa, with a robust pipeline of potential treatments.”
One-Year Extension Study
HS is a “chronic and debilitating inflammatory skin disease,” Zouboulis told the audience. He noted that interleukin (IL)–17F and IL-17A are highly expressed in lesional skin and play a role in the disease immunopathogenesis.
Bimekizumab is a humanized immunoglobulin G1 monoclonal antibody that selectively inhibits both IL-17F and IL-17A. It has previously demonstrated clinically meaningful improvements in patients with moderate to severe HS in the phase 3 BE HEARD I and BE HEARD II trials evaluating several dosing regimens.
Zouboulis said the current analysis combines data from the two phase 3 studies with the BE HEARD EXT open-label extension study, in which patients from both trials were continued on bimekizumab 320 mg every 2 weeks.
Of the 1014 patients initially enrolled in the two trials, 556 continued into the open-label extension. Their average age was 36.6 years, and 53.8% were women. The majority (80.6%) were White. Of the 556 patients enrolled in the extension, 446 completed the 1-year extension study.
The average draining tunnel count at baseline was 3.8, and 54.5% had Hurley stage II disease; the remaining 45.5% had stage III disease. The mean total Dermatology Life Quality Index (DLQI) score at baseline was 11.0, indicating the HS was having a very large impact on the patients’ lives.
After the 16-week initial treatment period and the maintenance treatment period out to 48 weeks, 64.0% of patients achieved HiSCR75, indicating at least a 75% reduction from baseline in the total abscess and inflammatory nodule count, rising to 77.1% at the end of the open-label extension, after a total follow-up of 96 weeks.
HiSCR100 scores, indicating a 100% reduction in total abscess and inflammatory nodule counts, were achieved by 30.2% of 556 patients after 48 weeks and 44.2% of 446 at the 96-week follow-up.
These findings were mirrored by substantial reductions on the International HS Severity Score System, with a 70.3% reduction over baseline at 48 weeks and a 79.8% reduction at the final follow-up.
There were also “clinically meaningful” reductions in the total draining tunnel count at 1 year that were further reduced at 2 years, Zouboulis reported, at a 57.5% reduction over baseline, increasing to 73.7% by 96 weeks. The mean draining tunnel count at the end of follow-up was 1.1.
Over the full 96 weeks, the mean DLQI score reduced from 11.0 to 4.7, with 33.9% of patients achieving a score of 0 or 1 on the scale, which he said is basically patients saying: “I don’t have disease now.”
Finally, the safety data showed that there were “no differences compared to what we knew before,” Zouboulis said, with the most common treatment-related adverse events being hidradenitis, coronavirus infection, and oral candidiasis. There were few serious and severe treatment-related adverse events, and few that led to treatment discontinuation.
The study was funded by UCB.Zouboulis declared relationships with AstraZeneca, Boehringer Ingelheim, Brandenburg Medical School Theodor Fontane, EAD, European Union, German Federal Ministry of Education and Research, GSK, InflaRx, MSD, Novartis, Relaxera, UCB, Almirall, Boehringer Ingelheim, Eli Lilly, Idorsia, Incyte, L’Oréal, NAOS-BIODERMA, Pfizer, PM, Sanofi. Hsiao is on the board of directors for the Hidradenitis Suppurativa Foundation and has declared relationships with AbbVie, Aclaris Therapeutics, Amgen, Boehringer Ingelheim, Incyte, Novartis, Sanofi-Regeneron, and UCB.
A version of this article appeared on Medscape.com.
AMSTERDAM — The monoclonal antibody according to new data from an open-label extension period.
“Efficacy and health-related quality-of-life outcomes were maintained through 2 years of treatment,” study presenter Christos C. Zouboulis, MD, professor of dermatology, venereology, and allergology, Brandenburg Medical School Theodor Fontane, Dessau, Germany, said at the European Academy of Dermatology and Venereology (EADV) 2024 Congress.
“No new safety signals were observed,” he added. “These data highlight the durability and consistency of bimekizumab treatment in patients with moderate to severe hidradenitis suppurativa,” Zouboulis concluded.
Efficacy Maintained
“This is the type of long-term data that clinicians hope to see in large phase 3 trials for hidradenitis suppurativa medications,” commented Jennifer L. Hsiao, MD, clinical associate professor of dermatology, University of Southern California, Los Angeles, who was not involved in the study.
She told this news organization that, beyond maintained improvement of patient-reported quality of life, the results are “raising the bar in terms of measuring treatment success,” with over three quarters of patients achieving a high level of response on the Hidradenitis Suppurativa Clinical Response (HiSCR) scale at the final 96-week follow-up.
“Clinicians and patients have struggled with maintaining treatment efficacy over time with the first [Food and Drug Administration]–approved class of biologics for hidradenitis suppurativa — TNF [tumor necrosis factor]–alpha antagonists,” Hsiao said. She emphasized that sustained treatment efficacy will reduce the need for continued treatment switching and “hopefully improve treatment adherence.”
“It was also helpful to see that, consistent with studies of bimekizumab in psoriasis, rates of oral candidiasis appear to decrease with prolonged exposure over 2 years, though as with any open-label extension study, study dropout is a limitation,” she said.
“The availability of long-term efficacy and safety data, such as those shown in this study, will help guide shared decision-making discussions with our patients.” Overall, Hsiao believes there is “much to be excited about in the field of hidradenitis suppurativa, with a robust pipeline of potential treatments.”
One-Year Extension Study
HS is a “chronic and debilitating inflammatory skin disease,” Zouboulis told the audience. He noted that interleukin (IL)–17F and IL-17A are highly expressed in lesional skin and play a role in the disease immunopathogenesis.
Bimekizumab is a humanized immunoglobulin G1 monoclonal antibody that selectively inhibits both IL-17F and IL-17A. It has previously demonstrated clinically meaningful improvements in patients with moderate to severe HS in the phase 3 BE HEARD I and BE HEARD II trials evaluating several dosing regimens.
Zouboulis said the current analysis combines data from the two phase 3 studies with the BE HEARD EXT open-label extension study, in which patients from both trials were continued on bimekizumab 320 mg every 2 weeks.
Of the 1014 patients initially enrolled in the two trials, 556 continued into the open-label extension. Their average age was 36.6 years, and 53.8% were women. The majority (80.6%) were White. Of the 556 patients enrolled in the extension, 446 completed the 1-year extension study.
The average draining tunnel count at baseline was 3.8, and 54.5% had Hurley stage II disease; the remaining 45.5% had stage III disease. The mean total Dermatology Life Quality Index (DLQI) score at baseline was 11.0, indicating the HS was having a very large impact on the patients’ lives.
After the 16-week initial treatment period and the maintenance treatment period out to 48 weeks, 64.0% of patients achieved HiSCR75, indicating at least a 75% reduction from baseline in the total abscess and inflammatory nodule count, rising to 77.1% at the end of the open-label extension, after a total follow-up of 96 weeks.
HiSCR100 scores, indicating a 100% reduction in total abscess and inflammatory nodule counts, were achieved by 30.2% of 556 patients after 48 weeks and 44.2% of 446 at the 96-week follow-up.
These findings were mirrored by substantial reductions on the International HS Severity Score System, with a 70.3% reduction over baseline at 48 weeks and a 79.8% reduction at the final follow-up.
There were also “clinically meaningful” reductions in the total draining tunnel count at 1 year that were further reduced at 2 years, Zouboulis reported, at a 57.5% reduction over baseline, increasing to 73.7% by 96 weeks. The mean draining tunnel count at the end of follow-up was 1.1.
Over the full 96 weeks, the mean DLQI score reduced from 11.0 to 4.7, with 33.9% of patients achieving a score of 0 or 1 on the scale, which he said is basically patients saying: “I don’t have disease now.”
Finally, the safety data showed that there were “no differences compared to what we knew before,” Zouboulis said, with the most common treatment-related adverse events being hidradenitis, coronavirus infection, and oral candidiasis. There were few serious and severe treatment-related adverse events, and few that led to treatment discontinuation.
The study was funded by UCB.Zouboulis declared relationships with AstraZeneca, Boehringer Ingelheim, Brandenburg Medical School Theodor Fontane, EAD, European Union, German Federal Ministry of Education and Research, GSK, InflaRx, MSD, Novartis, Relaxera, UCB, Almirall, Boehringer Ingelheim, Eli Lilly, Idorsia, Incyte, L’Oréal, NAOS-BIODERMA, Pfizer, PM, Sanofi. Hsiao is on the board of directors for the Hidradenitis Suppurativa Foundation and has declared relationships with AbbVie, Aclaris Therapeutics, Amgen, Boehringer Ingelheim, Incyte, Novartis, Sanofi-Regeneron, and UCB.
A version of this article appeared on Medscape.com.
AMSTERDAM — The monoclonal antibody according to new data from an open-label extension period.
“Efficacy and health-related quality-of-life outcomes were maintained through 2 years of treatment,” study presenter Christos C. Zouboulis, MD, professor of dermatology, venereology, and allergology, Brandenburg Medical School Theodor Fontane, Dessau, Germany, said at the European Academy of Dermatology and Venereology (EADV) 2024 Congress.
“No new safety signals were observed,” he added. “These data highlight the durability and consistency of bimekizumab treatment in patients with moderate to severe hidradenitis suppurativa,” Zouboulis concluded.
Efficacy Maintained
“This is the type of long-term data that clinicians hope to see in large phase 3 trials for hidradenitis suppurativa medications,” commented Jennifer L. Hsiao, MD, clinical associate professor of dermatology, University of Southern California, Los Angeles, who was not involved in the study.
She told this news organization that, beyond maintained improvement of patient-reported quality of life, the results are “raising the bar in terms of measuring treatment success,” with over three quarters of patients achieving a high level of response on the Hidradenitis Suppurativa Clinical Response (HiSCR) scale at the final 96-week follow-up.
“Clinicians and patients have struggled with maintaining treatment efficacy over time with the first [Food and Drug Administration]–approved class of biologics for hidradenitis suppurativa — TNF [tumor necrosis factor]–alpha antagonists,” Hsiao said. She emphasized that sustained treatment efficacy will reduce the need for continued treatment switching and “hopefully improve treatment adherence.”
“It was also helpful to see that, consistent with studies of bimekizumab in psoriasis, rates of oral candidiasis appear to decrease with prolonged exposure over 2 years, though as with any open-label extension study, study dropout is a limitation,” she said.
“The availability of long-term efficacy and safety data, such as those shown in this study, will help guide shared decision-making discussions with our patients.” Overall, Hsiao believes there is “much to be excited about in the field of hidradenitis suppurativa, with a robust pipeline of potential treatments.”
One-Year Extension Study
HS is a “chronic and debilitating inflammatory skin disease,” Zouboulis told the audience. He noted that interleukin (IL)–17F and IL-17A are highly expressed in lesional skin and play a role in the disease immunopathogenesis.
Bimekizumab is a humanized immunoglobulin G1 monoclonal antibody that selectively inhibits both IL-17F and IL-17A. It has previously demonstrated clinically meaningful improvements in patients with moderate to severe HS in the phase 3 BE HEARD I and BE HEARD II trials evaluating several dosing regimens.
Zouboulis said the current analysis combines data from the two phase 3 studies with the BE HEARD EXT open-label extension study, in which patients from both trials were continued on bimekizumab 320 mg every 2 weeks.
Of the 1014 patients initially enrolled in the two trials, 556 continued into the open-label extension. Their average age was 36.6 years, and 53.8% were women. The majority (80.6%) were White. Of the 556 patients enrolled in the extension, 446 completed the 1-year extension study.
The average draining tunnel count at baseline was 3.8, and 54.5% had Hurley stage II disease; the remaining 45.5% had stage III disease. The mean total Dermatology Life Quality Index (DLQI) score at baseline was 11.0, indicating the HS was having a very large impact on the patients’ lives.
After the 16-week initial treatment period and the maintenance treatment period out to 48 weeks, 64.0% of patients achieved HiSCR75, indicating at least a 75% reduction from baseline in the total abscess and inflammatory nodule count, rising to 77.1% at the end of the open-label extension, after a total follow-up of 96 weeks.
HiSCR100 scores, indicating a 100% reduction in total abscess and inflammatory nodule counts, were achieved by 30.2% of 556 patients after 48 weeks and 44.2% of 446 at the 96-week follow-up.
These findings were mirrored by substantial reductions on the International HS Severity Score System, with a 70.3% reduction over baseline at 48 weeks and a 79.8% reduction at the final follow-up.
There were also “clinically meaningful” reductions in the total draining tunnel count at 1 year that were further reduced at 2 years, Zouboulis reported, at a 57.5% reduction over baseline, increasing to 73.7% by 96 weeks. The mean draining tunnel count at the end of follow-up was 1.1.
Over the full 96 weeks, the mean DLQI score reduced from 11.0 to 4.7, with 33.9% of patients achieving a score of 0 or 1 on the scale, which he said is basically patients saying: “I don’t have disease now.”
Finally, the safety data showed that there were “no differences compared to what we knew before,” Zouboulis said, with the most common treatment-related adverse events being hidradenitis, coronavirus infection, and oral candidiasis. There were few serious and severe treatment-related adverse events, and few that led to treatment discontinuation.
The study was funded by UCB.Zouboulis declared relationships with AstraZeneca, Boehringer Ingelheim, Brandenburg Medical School Theodor Fontane, EAD, European Union, German Federal Ministry of Education and Research, GSK, InflaRx, MSD, Novartis, Relaxera, UCB, Almirall, Boehringer Ingelheim, Eli Lilly, Idorsia, Incyte, L’Oréal, NAOS-BIODERMA, Pfizer, PM, Sanofi. Hsiao is on the board of directors for the Hidradenitis Suppurativa Foundation and has declared relationships with AbbVie, Aclaris Therapeutics, Amgen, Boehringer Ingelheim, Incyte, Novartis, Sanofi-Regeneron, and UCB.
A version of this article appeared on Medscape.com.
FROM EADV 2024






