User login
Novel platform harnesses 3D laser technology for skin treatments
in all skin types, according to speakers at a virtual course on laser and aesthetic skin therapy.
The products feature “focal point technology,” which pairs 3D laser targeting with an integrated high-resolution imaging system (IntelliView), to help the user guide treatments at selectable depths. They have been cleared by the Food and Drug Administration for use in skin resurfacing procedures, and to treat benign pigmented lesions of the skin, including hyperpigmentation, and were created by Dieter Manstein, MD, PhD, Rox Anderson, MD, and Henry Chan, MD, of the Wellman Center for Photomedicine at Massachusetts General Hospital, and Irina Erenburg, PhD, CEO of AVAVA, the company that markets the products.
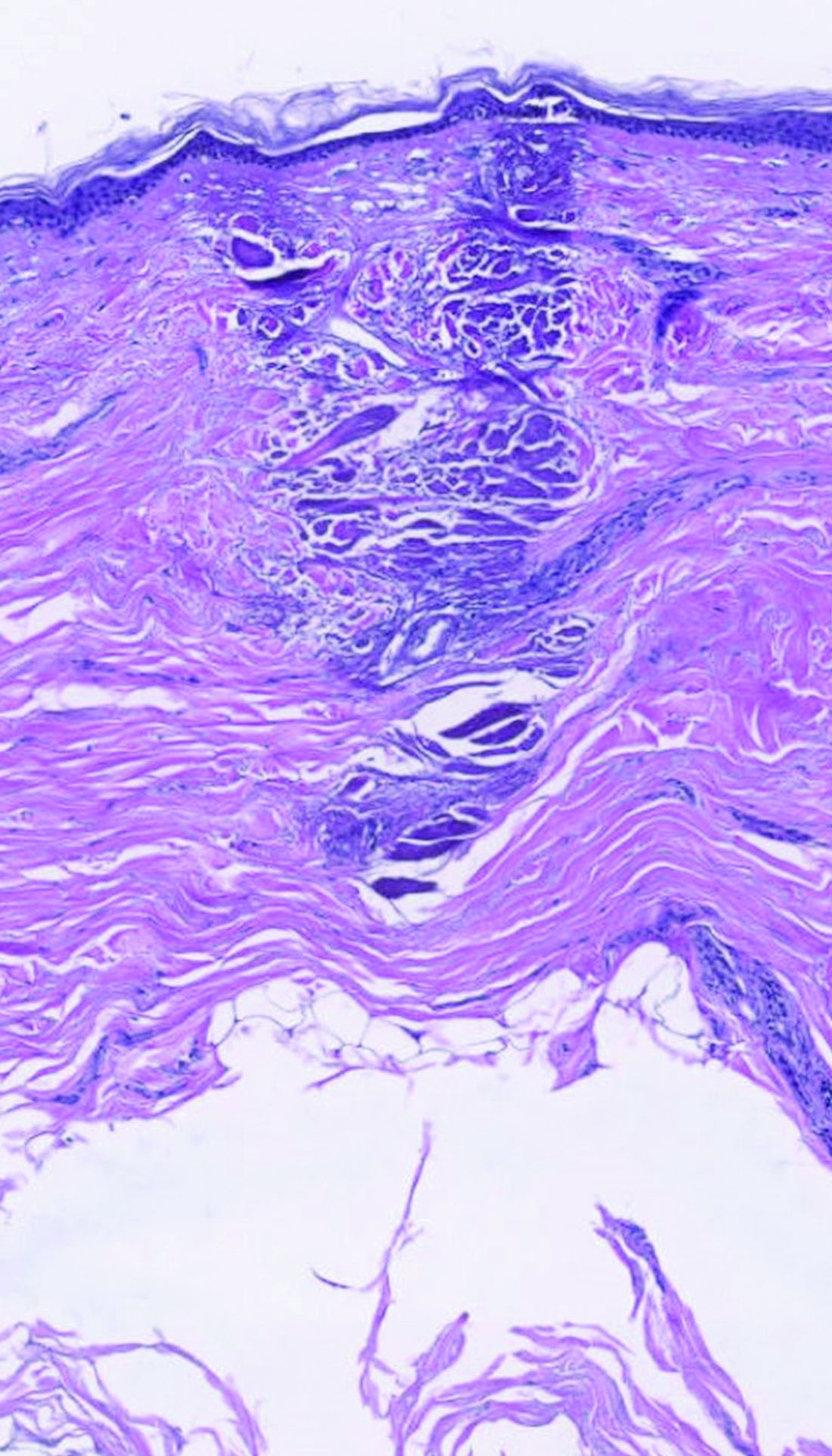
dermally focused treatment with Focal Point Technology. The coagulation zone, in dark purple, shows a deep conical lesion that extends 1.3 mm deep with significant epidermal sparing.
At the meeting, Mathew M. Avram, MD, JD, director of the Massachusetts General Hospital Dermatology Laser & Cosmetic Center, described focal point technology as an adjustable intradermally focused laser platform guided by real-time visual mapping to ensure the precise dose and depth of energy as the user performs treatments. “This is the key for rejuvenation,” he said. “You can go to different depths of the skin. You can be superficial for dyschromia and maybe a little bit different for wrinkles. If you want to treat scars, you go a little bit deeper. Coagulation occurs at these different depths.”
The collimated beam from conventional lasers affects all tissue in its path. The laser beam from the AVAVA product, however, creates a cone-shaped profile of injury in the dermis that minimizes the area of epidermal damage, making it safe in skin of color, according to Dr. Avram. “The beam comes to a focal point in the dermis at the depth that you want it to,” he explained during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s where the energy is going to focus and it bypasses the dermal/epidermal junction, which traditional fractional lasers cannot. What’s interesting about this platform is that you have a wavelength for skin rejuvenation, then you have wavelengths for pigment, which allows you to treat conditions like melasma at different depths.”
The AVAVA high-speed IntelliView imaging system features 10-micron resolution, “so you get exquisite imaging that can help guide your treatments,” he said. It also features image acquisition and storage with artificial intelligence algorithm interrogation and the ability to personalize treatments to the patient’s specific skin type. Commercial availability is expected in the first half of 2023, Dr. Avram said.
In a separate presentation, New York-based cosmetic dermatologist Roy G. Geronemus, MD, who has been involved in clinical trials of AVAVA’s focal point technology, said that patients “feel less pain and have less down time than we saw previously with other nonablative, fractional technologies.”
Downtime involves “just some mild redness,” he said, adding that he is encouraged by early results seen to date, and that “there appears to be some unique capabilities that will be borne out as the clinical studies progress.”
Dr. Avram disclosed that he has received consulting fees from Allergan, Galderma, and Revelle. He is an investigator for Endo and holds ownership and/or shareholder interest in Cytrellis and La Jolla NanoMedical. Dr. Geronemus disclosed having financial relationships with numerous device and pharmaceutical companies.
in all skin types, according to speakers at a virtual course on laser and aesthetic skin therapy.
The products feature “focal point technology,” which pairs 3D laser targeting with an integrated high-resolution imaging system (IntelliView), to help the user guide treatments at selectable depths. They have been cleared by the Food and Drug Administration for use in skin resurfacing procedures, and to treat benign pigmented lesions of the skin, including hyperpigmentation, and were created by Dieter Manstein, MD, PhD, Rox Anderson, MD, and Henry Chan, MD, of the Wellman Center for Photomedicine at Massachusetts General Hospital, and Irina Erenburg, PhD, CEO of AVAVA, the company that markets the products.
dermally focused treatment with Focal Point Technology. The coagulation zone, in dark purple, shows a deep conical lesion that extends 1.3 mm deep with significant epidermal sparing.
At the meeting, Mathew M. Avram, MD, JD, director of the Massachusetts General Hospital Dermatology Laser & Cosmetic Center, described focal point technology as an adjustable intradermally focused laser platform guided by real-time visual mapping to ensure the precise dose and depth of energy as the user performs treatments. “This is the key for rejuvenation,” he said. “You can go to different depths of the skin. You can be superficial for dyschromia and maybe a little bit different for wrinkles. If you want to treat scars, you go a little bit deeper. Coagulation occurs at these different depths.”
The collimated beam from conventional lasers affects all tissue in its path. The laser beam from the AVAVA product, however, creates a cone-shaped profile of injury in the dermis that minimizes the area of epidermal damage, making it safe in skin of color, according to Dr. Avram. “The beam comes to a focal point in the dermis at the depth that you want it to,” he explained during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s where the energy is going to focus and it bypasses the dermal/epidermal junction, which traditional fractional lasers cannot. What’s interesting about this platform is that you have a wavelength for skin rejuvenation, then you have wavelengths for pigment, which allows you to treat conditions like melasma at different depths.”
The AVAVA high-speed IntelliView imaging system features 10-micron resolution, “so you get exquisite imaging that can help guide your treatments,” he said. It also features image acquisition and storage with artificial intelligence algorithm interrogation and the ability to personalize treatments to the patient’s specific skin type. Commercial availability is expected in the first half of 2023, Dr. Avram said.
In a separate presentation, New York-based cosmetic dermatologist Roy G. Geronemus, MD, who has been involved in clinical trials of AVAVA’s focal point technology, said that patients “feel less pain and have less down time than we saw previously with other nonablative, fractional technologies.”
Downtime involves “just some mild redness,” he said, adding that he is encouraged by early results seen to date, and that “there appears to be some unique capabilities that will be borne out as the clinical studies progress.”
Dr. Avram disclosed that he has received consulting fees from Allergan, Galderma, and Revelle. He is an investigator for Endo and holds ownership and/or shareholder interest in Cytrellis and La Jolla NanoMedical. Dr. Geronemus disclosed having financial relationships with numerous device and pharmaceutical companies.
in all skin types, according to speakers at a virtual course on laser and aesthetic skin therapy.
The products feature “focal point technology,” which pairs 3D laser targeting with an integrated high-resolution imaging system (IntelliView), to help the user guide treatments at selectable depths. They have been cleared by the Food and Drug Administration for use in skin resurfacing procedures, and to treat benign pigmented lesions of the skin, including hyperpigmentation, and were created by Dieter Manstein, MD, PhD, Rox Anderson, MD, and Henry Chan, MD, of the Wellman Center for Photomedicine at Massachusetts General Hospital, and Irina Erenburg, PhD, CEO of AVAVA, the company that markets the products.
dermally focused treatment with Focal Point Technology. The coagulation zone, in dark purple, shows a deep conical lesion that extends 1.3 mm deep with significant epidermal sparing.
At the meeting, Mathew M. Avram, MD, JD, director of the Massachusetts General Hospital Dermatology Laser & Cosmetic Center, described focal point technology as an adjustable intradermally focused laser platform guided by real-time visual mapping to ensure the precise dose and depth of energy as the user performs treatments. “This is the key for rejuvenation,” he said. “You can go to different depths of the skin. You can be superficial for dyschromia and maybe a little bit different for wrinkles. If you want to treat scars, you go a little bit deeper. Coagulation occurs at these different depths.”
The collimated beam from conventional lasers affects all tissue in its path. The laser beam from the AVAVA product, however, creates a cone-shaped profile of injury in the dermis that minimizes the area of epidermal damage, making it safe in skin of color, according to Dr. Avram. “The beam comes to a focal point in the dermis at the depth that you want it to,” he explained during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s where the energy is going to focus and it bypasses the dermal/epidermal junction, which traditional fractional lasers cannot. What’s interesting about this platform is that you have a wavelength for skin rejuvenation, then you have wavelengths for pigment, which allows you to treat conditions like melasma at different depths.”
The AVAVA high-speed IntelliView imaging system features 10-micron resolution, “so you get exquisite imaging that can help guide your treatments,” he said. It also features image acquisition and storage with artificial intelligence algorithm interrogation and the ability to personalize treatments to the patient’s specific skin type. Commercial availability is expected in the first half of 2023, Dr. Avram said.
In a separate presentation, New York-based cosmetic dermatologist Roy G. Geronemus, MD, who has been involved in clinical trials of AVAVA’s focal point technology, said that patients “feel less pain and have less down time than we saw previously with other nonablative, fractional technologies.”
Downtime involves “just some mild redness,” he said, adding that he is encouraged by early results seen to date, and that “there appears to be some unique capabilities that will be borne out as the clinical studies progress.”
Dr. Avram disclosed that he has received consulting fees from Allergan, Galderma, and Revelle. He is an investigator for Endo and holds ownership and/or shareholder interest in Cytrellis and La Jolla NanoMedical. Dr. Geronemus disclosed having financial relationships with numerous device and pharmaceutical companies.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Rosacea and the gut: Looking into SIBO
, according to speakers at the annual Integrative Dermatology Symposium.
“SIBO is definitely something we test for and treat,” Raja Sivamani, MD, said in an interview after the meeting. Dr. Sivamani practices as an integrative dermatologist at the Pacific Skin Institute in Sacramento and is the director of clinical research at the institute’s research unit, Integrative Skin Science and Research. He led a panel discussion on rosacea and acne at the meeting.
Associations between SIBO and several dermatologic conditions, including systemic sclerosis, have been reported, but the strongest evidence to date involves rosacea. “There’s associative epidemiological evidence showing higher rates of SIBO among those with rosacea, and there are prospective studies” showing clearance of rosacea in patients treated for SIBO, said Dr. Sivamani, also adjunct associate professor of clinical dermatology at the University of California, Davis.
Studies are small, but are “well done and well-designed,” he said in the interview. “Do we need more studies? Absolutely. But what we have now is compelling [enough] for us to take a look at it.”
Findings of rosacea clearance
SIBO’s believed contribution to the pathophysiology of rosacea is part of the increasingly described gut microbiome-skin axis. SIBO has been recognized as a medical phenomenon for many decades and has been defined as an excessive bacterial load in the small bowel that causes gastrointestinal symptoms, according to the 2020 American College of Gastroenterology clinical guideline on SIBO.
Symptoms commonly associated with SIBO overlap with the cardinal symptoms of irritable bowel syndrome (IBS): abdominal pain; diarrhea, constipation, or both; bloating; and flatulence. SIBO can be diagnosed with several validated carbohydrate substrate (glucose or lactulose)–based breath tests that measure hydrogen and/or methane.
Hydrogen-positive breath tests suggest bacterial overgrowth, and methane-positive breath tests suggest small intestinal methanogen overgrowth. Methane is increasingly important and recognized, the AGA guideline says, though it creates a “nomenclature problem in the SIBO framework” because methanogens are not bacteria, the authors note.
In conventional practice, SIBO is typically treated with antibiotics such as rifaximin, and often with short-term dietary modification as well. Integrative medicine typically considers the use of supplements and botanicals in addition to or instead of antibiotics, as well as dietary change and increasingly, a close look at SIBO risk factors to prevent recurrence, Dr. Sivamani said. (His research unit is currently studying the use of herbal protocols as an alternative to antibiotics in patients with SIBO and dermatologic conditions.)
During a presentation on rosacea at the meeting, Neal Bhatia, MD, director of clinical dermatology at Therapeutics Clinical Research, a dermatology treatment and research center in San Diego, said that currently available breath tests for SIBO “are very interesting tools for understanding what may be happening in the gut” and that the “rifaximin data are good.”
He referred to a study reported in the Journal of the American Academy of Dermatology showing that patients with rosacea were significantly more likely to have SIBO (41.7% of 48 patients vs. 5.0% of 40 controls; P < .001), and that 64.5% of rosacea patients who completed treatment with rifaximin had remission of rosacea at a 3-year follow-up.
An earlier crossover study is also notable, he said. This study enrolled 113 consecutive patients with rosacea and 60 age- and sex-matched controls, and randomized those with SIBO (52 of the 113 with rosacea vs. 3 of the 60 controls) to rifaximin or placebo. Rosacea cleared in 20 of the 28 patients in the rifaximin group and greatly improved in 6 of the 28. Of 20 patients in the placebo group, rosacea remained unchanged in 18 and worsened in 2. When patients in the placebo group were switched to rifaximin, SIBO was eradicated in 17 of the 20, and rosacea completely resolved in 15 of those patients, Dr. Bhatia said.
In his view, it will take more time, greater awareness of the rosacea-SIBO link, and a willingness “to take chances” for more dermatologists to consider SIBO during rosacea care. “Breath tests are not something used in the [typical dermatology] clinic right now, but they may make their way in,” he said at the meeting.
In a follow-up interview, Dr. Bhatia emphasized that “it’s really a question of uptake, which always takes a while” and of willingness to “think through the disease from another angle ... especially in patients who are recalcitrant.”
Treatment
Dr. Sivamani said in the interview that a third type of SIBO – hydrogen sulfide–dominant SIBO – is now documented and worth considering when glucose and lactulose breath tests are negative in patients with rosacea who have gastrointestinal symptoms.
The use of breath tests to objectively diagnose SIBO is always best, Dr. Sivamani said, but he will consider empiric therapy in some patients. “I always tell patients [about] the benefits of testing, but if they can’t get the test covered or are unable to pay for the test, and they have symptoms consistent with SIBO, I’m okay doing a trial with therapy,” he said.
Rifaximin, one of the suggested antibiotics listed in the AGA guideline, is a nonabsorbable antibiotic that is FDA-approved for IBS with diarrhea (IBS-D); it has been shown to not negatively affect the growth of beneficial bacteria in the colon.
However, herbals are also an attractive option – alone or in combination with rifaximin or other antibiotics – speakers at the meeting said. In a multicenter retrospective chart review led by investigators at the Johns Hopkins Hospital, herbal therapies were at least as effective as rifaximin for treating SIBO, with similar safety profiles. The response rate for normalizing breath hydrogen testing in patients with SIBO was 46% for herbal therapies and 34% for rifaximin.
Dietary change is also part of treatment, with the reduction of fermentable carbohydrates – often through the Low FODMAP Diet and Specific Carbohydrate Diet – being the dominant theme in dietary intervention for SIBO, according to the AGA guideline.
“There are definitely some food choices you can shift,” said Dr. Sivamani. “I’ll work with patients on FODMAP, though it’s hard to sustain over the long-term and can induce psychological issues. You have to provide other options.”
Dr. Sivamani works with patients on using “a restrictive diet for a short amount of time, with the gradual reintroduction of foods to see [what] foods are and aren’t [causing] flares.” He also works to identify and eliminate risk factors and predisposing factors for SIBO so that recurrence will be less likely.
“SIBO is definitely an entity that is not on the fringes anymore ... it adds to inflammation in the body ... and if you have an inflamed gut, there’s a domino effect that will lead to inflammation elsewhere,” Dr. Sivamani said.
“You want to know, do your patients have SIBO? What subset do they have? Do they have risk factors you can eliminate?” he said. “And then what therapies will you use – pharmaceuticals, supplements and botanicals, or a combination? And finally, what will you do with diet?”
Dr. Bhatia disclosed he has affiliations with Abbvie, Almirall, Arcutis, Arena, Biofrontera, BMS, BI, Brickell, Dermavant, EPI Health, Ferndale, Galderma, Genentech, InCyte, ISDIN, Johnson & Johnson, LaRoche-Posay, Leo, Lilly, Novartis, Ortho, Pfizer, Proctor & Gamble, Regeneron, Sanofi, Stemline, SunPharma, and Verrica. Dr. Sivamani did not provide a disclosure statement.
, according to speakers at the annual Integrative Dermatology Symposium.
“SIBO is definitely something we test for and treat,” Raja Sivamani, MD, said in an interview after the meeting. Dr. Sivamani practices as an integrative dermatologist at the Pacific Skin Institute in Sacramento and is the director of clinical research at the institute’s research unit, Integrative Skin Science and Research. He led a panel discussion on rosacea and acne at the meeting.
Associations between SIBO and several dermatologic conditions, including systemic sclerosis, have been reported, but the strongest evidence to date involves rosacea. “There’s associative epidemiological evidence showing higher rates of SIBO among those with rosacea, and there are prospective studies” showing clearance of rosacea in patients treated for SIBO, said Dr. Sivamani, also adjunct associate professor of clinical dermatology at the University of California, Davis.
Studies are small, but are “well done and well-designed,” he said in the interview. “Do we need more studies? Absolutely. But what we have now is compelling [enough] for us to take a look at it.”
Findings of rosacea clearance
SIBO’s believed contribution to the pathophysiology of rosacea is part of the increasingly described gut microbiome-skin axis. SIBO has been recognized as a medical phenomenon for many decades and has been defined as an excessive bacterial load in the small bowel that causes gastrointestinal symptoms, according to the 2020 American College of Gastroenterology clinical guideline on SIBO.
Symptoms commonly associated with SIBO overlap with the cardinal symptoms of irritable bowel syndrome (IBS): abdominal pain; diarrhea, constipation, or both; bloating; and flatulence. SIBO can be diagnosed with several validated carbohydrate substrate (glucose or lactulose)–based breath tests that measure hydrogen and/or methane.
Hydrogen-positive breath tests suggest bacterial overgrowth, and methane-positive breath tests suggest small intestinal methanogen overgrowth. Methane is increasingly important and recognized, the AGA guideline says, though it creates a “nomenclature problem in the SIBO framework” because methanogens are not bacteria, the authors note.
In conventional practice, SIBO is typically treated with antibiotics such as rifaximin, and often with short-term dietary modification as well. Integrative medicine typically considers the use of supplements and botanicals in addition to or instead of antibiotics, as well as dietary change and increasingly, a close look at SIBO risk factors to prevent recurrence, Dr. Sivamani said. (His research unit is currently studying the use of herbal protocols as an alternative to antibiotics in patients with SIBO and dermatologic conditions.)
During a presentation on rosacea at the meeting, Neal Bhatia, MD, director of clinical dermatology at Therapeutics Clinical Research, a dermatology treatment and research center in San Diego, said that currently available breath tests for SIBO “are very interesting tools for understanding what may be happening in the gut” and that the “rifaximin data are good.”
He referred to a study reported in the Journal of the American Academy of Dermatology showing that patients with rosacea were significantly more likely to have SIBO (41.7% of 48 patients vs. 5.0% of 40 controls; P < .001), and that 64.5% of rosacea patients who completed treatment with rifaximin had remission of rosacea at a 3-year follow-up.
An earlier crossover study is also notable, he said. This study enrolled 113 consecutive patients with rosacea and 60 age- and sex-matched controls, and randomized those with SIBO (52 of the 113 with rosacea vs. 3 of the 60 controls) to rifaximin or placebo. Rosacea cleared in 20 of the 28 patients in the rifaximin group and greatly improved in 6 of the 28. Of 20 patients in the placebo group, rosacea remained unchanged in 18 and worsened in 2. When patients in the placebo group were switched to rifaximin, SIBO was eradicated in 17 of the 20, and rosacea completely resolved in 15 of those patients, Dr. Bhatia said.
In his view, it will take more time, greater awareness of the rosacea-SIBO link, and a willingness “to take chances” for more dermatologists to consider SIBO during rosacea care. “Breath tests are not something used in the [typical dermatology] clinic right now, but they may make their way in,” he said at the meeting.
In a follow-up interview, Dr. Bhatia emphasized that “it’s really a question of uptake, which always takes a while” and of willingness to “think through the disease from another angle ... especially in patients who are recalcitrant.”
Treatment
Dr. Sivamani said in the interview that a third type of SIBO – hydrogen sulfide–dominant SIBO – is now documented and worth considering when glucose and lactulose breath tests are negative in patients with rosacea who have gastrointestinal symptoms.
The use of breath tests to objectively diagnose SIBO is always best, Dr. Sivamani said, but he will consider empiric therapy in some patients. “I always tell patients [about] the benefits of testing, but if they can’t get the test covered or are unable to pay for the test, and they have symptoms consistent with SIBO, I’m okay doing a trial with therapy,” he said.
Rifaximin, one of the suggested antibiotics listed in the AGA guideline, is a nonabsorbable antibiotic that is FDA-approved for IBS with diarrhea (IBS-D); it has been shown to not negatively affect the growth of beneficial bacteria in the colon.
However, herbals are also an attractive option – alone or in combination with rifaximin or other antibiotics – speakers at the meeting said. In a multicenter retrospective chart review led by investigators at the Johns Hopkins Hospital, herbal therapies were at least as effective as rifaximin for treating SIBO, with similar safety profiles. The response rate for normalizing breath hydrogen testing in patients with SIBO was 46% for herbal therapies and 34% for rifaximin.
Dietary change is also part of treatment, with the reduction of fermentable carbohydrates – often through the Low FODMAP Diet and Specific Carbohydrate Diet – being the dominant theme in dietary intervention for SIBO, according to the AGA guideline.
“There are definitely some food choices you can shift,” said Dr. Sivamani. “I’ll work with patients on FODMAP, though it’s hard to sustain over the long-term and can induce psychological issues. You have to provide other options.”
Dr. Sivamani works with patients on using “a restrictive diet for a short amount of time, with the gradual reintroduction of foods to see [what] foods are and aren’t [causing] flares.” He also works to identify and eliminate risk factors and predisposing factors for SIBO so that recurrence will be less likely.
“SIBO is definitely an entity that is not on the fringes anymore ... it adds to inflammation in the body ... and if you have an inflamed gut, there’s a domino effect that will lead to inflammation elsewhere,” Dr. Sivamani said.
“You want to know, do your patients have SIBO? What subset do they have? Do they have risk factors you can eliminate?” he said. “And then what therapies will you use – pharmaceuticals, supplements and botanicals, or a combination? And finally, what will you do with diet?”
Dr. Bhatia disclosed he has affiliations with Abbvie, Almirall, Arcutis, Arena, Biofrontera, BMS, BI, Brickell, Dermavant, EPI Health, Ferndale, Galderma, Genentech, InCyte, ISDIN, Johnson & Johnson, LaRoche-Posay, Leo, Lilly, Novartis, Ortho, Pfizer, Proctor & Gamble, Regeneron, Sanofi, Stemline, SunPharma, and Verrica. Dr. Sivamani did not provide a disclosure statement.
, according to speakers at the annual Integrative Dermatology Symposium.
“SIBO is definitely something we test for and treat,” Raja Sivamani, MD, said in an interview after the meeting. Dr. Sivamani practices as an integrative dermatologist at the Pacific Skin Institute in Sacramento and is the director of clinical research at the institute’s research unit, Integrative Skin Science and Research. He led a panel discussion on rosacea and acne at the meeting.
Associations between SIBO and several dermatologic conditions, including systemic sclerosis, have been reported, but the strongest evidence to date involves rosacea. “There’s associative epidemiological evidence showing higher rates of SIBO among those with rosacea, and there are prospective studies” showing clearance of rosacea in patients treated for SIBO, said Dr. Sivamani, also adjunct associate professor of clinical dermatology at the University of California, Davis.
Studies are small, but are “well done and well-designed,” he said in the interview. “Do we need more studies? Absolutely. But what we have now is compelling [enough] for us to take a look at it.”
Findings of rosacea clearance
SIBO’s believed contribution to the pathophysiology of rosacea is part of the increasingly described gut microbiome-skin axis. SIBO has been recognized as a medical phenomenon for many decades and has been defined as an excessive bacterial load in the small bowel that causes gastrointestinal symptoms, according to the 2020 American College of Gastroenterology clinical guideline on SIBO.
Symptoms commonly associated with SIBO overlap with the cardinal symptoms of irritable bowel syndrome (IBS): abdominal pain; diarrhea, constipation, or both; bloating; and flatulence. SIBO can be diagnosed with several validated carbohydrate substrate (glucose or lactulose)–based breath tests that measure hydrogen and/or methane.
Hydrogen-positive breath tests suggest bacterial overgrowth, and methane-positive breath tests suggest small intestinal methanogen overgrowth. Methane is increasingly important and recognized, the AGA guideline says, though it creates a “nomenclature problem in the SIBO framework” because methanogens are not bacteria, the authors note.
In conventional practice, SIBO is typically treated with antibiotics such as rifaximin, and often with short-term dietary modification as well. Integrative medicine typically considers the use of supplements and botanicals in addition to or instead of antibiotics, as well as dietary change and increasingly, a close look at SIBO risk factors to prevent recurrence, Dr. Sivamani said. (His research unit is currently studying the use of herbal protocols as an alternative to antibiotics in patients with SIBO and dermatologic conditions.)
During a presentation on rosacea at the meeting, Neal Bhatia, MD, director of clinical dermatology at Therapeutics Clinical Research, a dermatology treatment and research center in San Diego, said that currently available breath tests for SIBO “are very interesting tools for understanding what may be happening in the gut” and that the “rifaximin data are good.”
He referred to a study reported in the Journal of the American Academy of Dermatology showing that patients with rosacea were significantly more likely to have SIBO (41.7% of 48 patients vs. 5.0% of 40 controls; P < .001), and that 64.5% of rosacea patients who completed treatment with rifaximin had remission of rosacea at a 3-year follow-up.
An earlier crossover study is also notable, he said. This study enrolled 113 consecutive patients with rosacea and 60 age- and sex-matched controls, and randomized those with SIBO (52 of the 113 with rosacea vs. 3 of the 60 controls) to rifaximin or placebo. Rosacea cleared in 20 of the 28 patients in the rifaximin group and greatly improved in 6 of the 28. Of 20 patients in the placebo group, rosacea remained unchanged in 18 and worsened in 2. When patients in the placebo group were switched to rifaximin, SIBO was eradicated in 17 of the 20, and rosacea completely resolved in 15 of those patients, Dr. Bhatia said.
In his view, it will take more time, greater awareness of the rosacea-SIBO link, and a willingness “to take chances” for more dermatologists to consider SIBO during rosacea care. “Breath tests are not something used in the [typical dermatology] clinic right now, but they may make their way in,” he said at the meeting.
In a follow-up interview, Dr. Bhatia emphasized that “it’s really a question of uptake, which always takes a while” and of willingness to “think through the disease from another angle ... especially in patients who are recalcitrant.”
Treatment
Dr. Sivamani said in the interview that a third type of SIBO – hydrogen sulfide–dominant SIBO – is now documented and worth considering when glucose and lactulose breath tests are negative in patients with rosacea who have gastrointestinal symptoms.
The use of breath tests to objectively diagnose SIBO is always best, Dr. Sivamani said, but he will consider empiric therapy in some patients. “I always tell patients [about] the benefits of testing, but if they can’t get the test covered or are unable to pay for the test, and they have symptoms consistent with SIBO, I’m okay doing a trial with therapy,” he said.
Rifaximin, one of the suggested antibiotics listed in the AGA guideline, is a nonabsorbable antibiotic that is FDA-approved for IBS with diarrhea (IBS-D); it has been shown to not negatively affect the growth of beneficial bacteria in the colon.
However, herbals are also an attractive option – alone or in combination with rifaximin or other antibiotics – speakers at the meeting said. In a multicenter retrospective chart review led by investigators at the Johns Hopkins Hospital, herbal therapies were at least as effective as rifaximin for treating SIBO, with similar safety profiles. The response rate for normalizing breath hydrogen testing in patients with SIBO was 46% for herbal therapies and 34% for rifaximin.
Dietary change is also part of treatment, with the reduction of fermentable carbohydrates – often through the Low FODMAP Diet and Specific Carbohydrate Diet – being the dominant theme in dietary intervention for SIBO, according to the AGA guideline.
“There are definitely some food choices you can shift,” said Dr. Sivamani. “I’ll work with patients on FODMAP, though it’s hard to sustain over the long-term and can induce psychological issues. You have to provide other options.”
Dr. Sivamani works with patients on using “a restrictive diet for a short amount of time, with the gradual reintroduction of foods to see [what] foods are and aren’t [causing] flares.” He also works to identify and eliminate risk factors and predisposing factors for SIBO so that recurrence will be less likely.
“SIBO is definitely an entity that is not on the fringes anymore ... it adds to inflammation in the body ... and if you have an inflamed gut, there’s a domino effect that will lead to inflammation elsewhere,” Dr. Sivamani said.
“You want to know, do your patients have SIBO? What subset do they have? Do they have risk factors you can eliminate?” he said. “And then what therapies will you use – pharmaceuticals, supplements and botanicals, or a combination? And finally, what will you do with diet?”
Dr. Bhatia disclosed he has affiliations with Abbvie, Almirall, Arcutis, Arena, Biofrontera, BMS, BI, Brickell, Dermavant, EPI Health, Ferndale, Galderma, Genentech, InCyte, ISDIN, Johnson & Johnson, LaRoche-Posay, Leo, Lilly, Novartis, Ortho, Pfizer, Proctor & Gamble, Regeneron, Sanofi, Stemline, SunPharma, and Verrica. Dr. Sivamani did not provide a disclosure statement.
REPORTING FROM IDS 2022
Advanced practice providers – an evolving role in pulmonary medicine
The integration of advanced practice providers (APPs) into pulmonology practice is in flux and deepening across numerous settings, from outpatient clinics to intensive care and inpatient pulmonary consult services – and as it evolves, so are issues of training.
Some institutions are developing pulmonary fellowship programs for APPs. This is a good indication that team-based pulmonology may be moving toward a time in the future when nurse practitioners (NPs) and physician assistants (PAs) join pulmonologists in practice after having undergone formal education in the subspecialty, rather than learning solely on the job from dedicated mentors.
Neither NPs nor PAs, who comprise almost all of the APP workforce in pulmonology, currently have a pulmonary tract for training. “Weight falls on the employer’s shoulders to train and educate their APPs,” said Corinne R. Young, MSN, FNP-C, FCCP, director of APP and clinical services at Colorado Springs Pulmonary Consultants and founder and president of the Association of Pulmonary Advanced Practice Providers, which launched in 2018.
The role that an APP plays and their scope of practice is determined not only by state policies and regulations – and by their prior experience, knowledge and motivation – but by “how much work a practice puts into [education and training],” she said.
An estimated 3,000-8,000 APPs are working in pulmonology, according to an analysis done by a marketing agency that has worked for the American College of Chest Physicians, Ms. Young said.
A 2021 APAPP survey of its several hundred members at the time showed them working in hospital systems (41%), private practice (28%), university systems (10%), and other health care systems (21%). They indicated practicing in pulmonary medicine, sleep medicine, or critical care – or some combination of these areas – and the vast majority (82%) indicated they were seeing both new and established patients in their roles.
“Nobody knows exactly how many of us are out there,” Ms. Young said. “But CHEST and APAPP are making great efforts to be beacons to APPs working in this realm and to bring them together to have a voice.”
The APAPP also wants to “close the education gap” and to “eventually develop a certification program to vet our knowledge in this area,” she said. “Right now, the closest we can get to vetting our knowledge is to become an FCCP through CHEST.”
Earning trust, seeking training
Omar Hussain, DO, has been practicing with an NP for over a decade in his role as an intensivist and knows what it’s like to train, supervise, and grow together. He and his private practice colleagues have a contract with Advocate Condell Hospital in Libertyville, Ill., to cover its ICU, and they hired their NP primarily to help care for shorter-stay, non–critically ill patients in the ICU (for example, patients receiving postoperative monitoring).
The NP has been invaluable. “We literally sit next to each other and in the mornings we make a game plan of which patients she will tackle first and which ones I’ll see first,” Dr. Hussain said. “When we’re called by the nurse for an ICU evaluation [on the floor], we’ll decide in real time who goes.”
The NP ensures that all guidelines and quality measures are followed in the ICU and, with a Monday-Friday schedule, she provides valuable continuity when there are handoffs from one intensivist to another, said Dr. Hussain, who serves as cochair of the joint CHEST/American Thoracic Society clinical practice committee, which deals with issues of physician-APP collaboration.
After working collaboratively for some time, Dr. Hussain and his partners decided to teach the NP how to intubate. It was a thoughtful and deliberate process, and “we used the same kind of mindset we’d used when we’ve supervised residents at other institutions,” he said.
Dr. Hussain and his partners have been fortunate in having such a long-term relationship with an APP. Their NP had worked as a nurse in the ICU before training as an adult gerontology–acute care NP and joining Dr. Hussain’s practice, so she was also “well known to us,” he added.
Rachel Adney, CPNP-PC, a certified pediatric NP in the division of pediatric pulmonology at Stanford (Calif.) Medicine Children’s Health, is an APP who actively sought advanced training. She joined Stanford in 2011 to provide ambulatory care, primarily, and having years of prior experience in asthma management and education, she fast became known as “the asthma person.”
After a physician colleague one day objected to her caring for a patient without asthma, Ms. Adney, the first APP in the division, approached John D. Mark, MD, program director of the pediatric fellowship program at Stanford, and inquired about training “so I could have more breadth and depth across the whole pulmonary milieu.”
Together they designed a “mini pediatric pulmonary fellowship” for Ms. Adney, incorporating elements of the first year of Stanford’s pediatric fellowship program as well as training materials from the University of Arizona’s Pediatric Pulmonary Center, Tucson, one of six federally funded PCCs that train various health care providers to care for pediatric patients with chronic pulmonary conditions. (Dr. Mark had previously been an educator at the center while serving on the University of Arizona faculty.)
Her curriculum consisted of 1,000 total hours of training, including 125 hours of didactic learning and 400 hours of both inpatient and outpatient clinical training in areas such as cystic fibrosis, sleep medicine, bronchopulmonary dysplasia (BPD), neuromuscular disorders, and general pulmonary medicine. “Rachel rotated through clinics, first as an observer, then as a trainee ... and she attended lectures that my fellows attended,” said Dr. Mark, who has long been a preceptor for APPs. “She became like a 1-year fellow in my division.”
Today, Ms. Adney sees patients independently in four outreach clinics along California’s central coast. “She sees very complicated pediatric pulmonary patients now” overall, and has become integral to Stanford’s interdisciplinary CRIB program (cardiac and respiratory care for infants with BPD), Dr. Mark said. “She follows these patients at Stanford along with the whole CRIB group, then sees them on her own for follow-up.”
As a result of her training, Ms. Adney said, “knowing that I have the knowledge and experience to take on more complex patients, my colleagues now trust me and are confident in my skills. They feel comfortable sending [patients] to me much earlier. ... And they know that if there’s something I need help with I will go to them instantly.”
Pulmonology “really spoke to my heart,” she said, recalling her pre-Stanford journey as an in-hospital medical-surgical nurse, and then, after her NP training, as a outpatient primary care PNP. “For the most part, it’s like putting a puzzle together, and being able to really impact the quality of life these patients have,” said Ms. Adney, who serves on the APAPP’s pediatric subcommittee.
It’s clear, Dr. Mark said, that “things are changing around the country” with increasing institutional interest in developing formal APP specialty training programs. “There’s no way [for an APP] to walk into a specialty and play an active role without additional training,” and institutions are frustrated with turnover and the loss of APPs who decide after 6-9 months of on-the-job training that they’re not interested in the field.
Stanford Medicine Children’s Health, in fact, has launched an internal Pediatric APP Fellowship Program that is training its first cohort of six newly graduated NPs and PAs in two clinical tracks, including a medical/surgical track that incorporates rotations in pulmonary medicine, said Raji Koppolu, CPNP-PC/AC, manager of advanced practice professional development for Stanford Medicine Children’s Health.
APP fellowship programs have been in existence since 2007 in a variety of clinical settings, she said, but more institutions are developing them as a way of recruiting and retaining APPs in areas of high need and of equipping them for successful transitions to their APP roles. Various national bodies accredit APP fellowship programs.
Most pulmonary fellowship programs, Ms. Young said, are also internal programs providing postgraduate education to their own newly hired APPs or recent NP/PA graduates. This limits their reach, but “it’s a step in the right direction toward standardizing education for pulmonary APPs.”
Defining APP competencies
In interventional pulmonology, training may soon be guided by newly defined “core clinical competencies” for APPs. The soon-to-be published and distributed competencies – the first such national APP competencies in pulmonology – were developed by an APP Leadership Council within the American Association of Bronchology and Interventional Pulmonology and cover the most common disease processes and practices in IP, from COPD and bronchoscopic lung volume reduction to pleural effusion and lung cancer screening.
Rebecca Priebe, ACNP-BC, who cochairs the AABIP’s APP chapter, organized the effort several years ago, bringing together a group of APPs and physician experts in advanced bronchoscopy and IP (some but not all of whom have worked with APPs), after fielding questions from pulmonologists at AABIP meetings about what to look for in an AAP and how to train them.
Physicians and institutions who are hiring and training APPs for IP can use any or all of the 11 core competencies to personalize and evaluate the training process for each APP’s needs, she said. “Someone looking to hire an APP for pleural disease, for instance, can pull up the content on plural effusion.”
APP interest in interventional pulmonology is growing rapidly, Ms. Priebe said, noting growth in the AABIP’s APP chapter from about 7-8 APPs 5 years ago to at least 60 currently.
Ms. Priebe was hired by Henry Ford Health in Detroit about 5 years ago to help establish and run an inpatient IP consult service, and more recently, she helped establish their inpatient pleural disease service and a bronchoscopic lung volume reduction program.
For the inpatient IP service, after several months of side-by-side training with an IP fellow and attending physicians, she began independently evaluating new patients, writing notes, and making recommendations.
For patients with pleural disease, she performs ultrasound examinations, chest tube insertions, and bedside thoracentesis independently. And for the bronchoscopic lung volume reduction program, she evaluates patients for candidate status, participates in valve placement, and sees patients independently through a year of follow-up.
“Physician colleagues often aren’t sure what an APP’s education and scope of practice is,” said Ms. Priebe, who was an ICU nurse before training as an acute care NP and then worked first with a private practice inpatient service and then with the University of Michigan, Ann Arbor, where she established and grew an APP-run program managing lung transplant patients and a step-down ICU unit.
“It’s a matter of knowing [your state’s policies], treating them like a fellow you would train, and then using them to the fullest extent of their education and training. If they’re given an opportunity to learn a subspecialty skill set, they can be an asset to any pulmonary program.”
‘We’re here to support,’ not replace
In her own practice, Ms. Young is one of seven APPs who work with nine physicians on a full range of inpatient care, outpatient care, critical care, sleep medicine, and procedures. Many new patients are seen first by the APP, who does the workup and orders tests, and by the physician on a follow-up visit. Most patients needing routine management of asthma and COPD are seen by the physician every third or fourth visit, she said.
Ms. Young also directs a 24-hour in-house APP service recently established by the practice, and she participates in research. In a practice across town, she noted, APPs see mainly established patients and do not practice as autonomously as the state permits. “Part of that difference may [stem from] the lack of a standard of education and variable amounts of work the practice puts into their APPs.”
The American Medical Association’s #StopScopeCreep social media messaging feels divisive and “sheds a negative light on APPs working in any area,” Ms. Young said. “One of the biggest things we want to convey [at APAPP] is that we’re not here for [physicians’] jobs.”
“We’re here to support those who are practicing, to support underserved populations, and to help bridge gaps” created by an aging pulmonologist workforce and real and projected physician shortages, Ms. Young said, referring to a 2016 report from the Health Resources and Services Administration and a 2017 report from Merritt Hawkins indicating that 73% of U.S. pulmonologists (the largest percentage of all subspecialties) were at least 55 years old.
Dr. Hussain said he has “seen scope creep” first-hand in his hospitals, in the form of noncollaborative practices and tasks performed by APPs without adequate training – most likely often stemming from poor decisions and oversight by physicians. But when constructed thoughtfully, APP-physician teams are “serving great needs” in many types of care, he said, from follow-up care and management of chronic conditions to inpatient rounding. “My [colleagues] are having great success,” he said.
He is watching with interest – and some concern – pending reimbursement changes from the Centers for Medicare & Medicaid Services that will make time the only defining feature of the “substantive” portion of a split/shared visit involving physicians and APPs in a facility setting. Medical decision-making will no longer be applicable.
For time-based services like critical care, time alone is currently the metric. (And in the nonfacility setting, physician-APP teams may still apply “incident to” billing practices). But in the facility setting, said Amy M. Ahasic, MD, MPH, a pulmonologist in Norwalk, Conn., who coauthored a 2022 commentary on the issue, the change (now planned for 2024) could be problematic for employed physicians whose contracts are based on productivity, and could create tension and possibly lead to reduced use of APPs rather than supporting collaborative care.
“The team model has been evolving so well over the past 10-15 years,” said Dr. Ahasic, who serves on the CHEST Health Policy and Advocacy Reimbursement Workgroup and cochairs the CHEST/American Thoracic Society clinical practice committee with Dr. Hussain. “It’s good for patient safety to have more [providers] involved ... and because APP salaries are lower health systems could do it and be able to have better care and better coverage.”
The pulmonology culture, said Dr. Hussain, has been increasingly embracing APPs and “it’s collegial.” Pulmonologists are “coming to CHEST meetings with their APPs. They’re learning the same things we’re learning, to manage the same patients we manage.”
The article sources reported that they had no relevant financial conflicts of interest to disclose.
The integration of advanced practice providers (APPs) into pulmonology practice is in flux and deepening across numerous settings, from outpatient clinics to intensive care and inpatient pulmonary consult services – and as it evolves, so are issues of training.
Some institutions are developing pulmonary fellowship programs for APPs. This is a good indication that team-based pulmonology may be moving toward a time in the future when nurse practitioners (NPs) and physician assistants (PAs) join pulmonologists in practice after having undergone formal education in the subspecialty, rather than learning solely on the job from dedicated mentors.
Neither NPs nor PAs, who comprise almost all of the APP workforce in pulmonology, currently have a pulmonary tract for training. “Weight falls on the employer’s shoulders to train and educate their APPs,” said Corinne R. Young, MSN, FNP-C, FCCP, director of APP and clinical services at Colorado Springs Pulmonary Consultants and founder and president of the Association of Pulmonary Advanced Practice Providers, which launched in 2018.
The role that an APP plays and their scope of practice is determined not only by state policies and regulations – and by their prior experience, knowledge and motivation – but by “how much work a practice puts into [education and training],” she said.
An estimated 3,000-8,000 APPs are working in pulmonology, according to an analysis done by a marketing agency that has worked for the American College of Chest Physicians, Ms. Young said.
A 2021 APAPP survey of its several hundred members at the time showed them working in hospital systems (41%), private practice (28%), university systems (10%), and other health care systems (21%). They indicated practicing in pulmonary medicine, sleep medicine, or critical care – or some combination of these areas – and the vast majority (82%) indicated they were seeing both new and established patients in their roles.
“Nobody knows exactly how many of us are out there,” Ms. Young said. “But CHEST and APAPP are making great efforts to be beacons to APPs working in this realm and to bring them together to have a voice.”
The APAPP also wants to “close the education gap” and to “eventually develop a certification program to vet our knowledge in this area,” she said. “Right now, the closest we can get to vetting our knowledge is to become an FCCP through CHEST.”
Earning trust, seeking training
Omar Hussain, DO, has been practicing with an NP for over a decade in his role as an intensivist and knows what it’s like to train, supervise, and grow together. He and his private practice colleagues have a contract with Advocate Condell Hospital in Libertyville, Ill., to cover its ICU, and they hired their NP primarily to help care for shorter-stay, non–critically ill patients in the ICU (for example, patients receiving postoperative monitoring).
The NP has been invaluable. “We literally sit next to each other and in the mornings we make a game plan of which patients she will tackle first and which ones I’ll see first,” Dr. Hussain said. “When we’re called by the nurse for an ICU evaluation [on the floor], we’ll decide in real time who goes.”
The NP ensures that all guidelines and quality measures are followed in the ICU and, with a Monday-Friday schedule, she provides valuable continuity when there are handoffs from one intensivist to another, said Dr. Hussain, who serves as cochair of the joint CHEST/American Thoracic Society clinical practice committee, which deals with issues of physician-APP collaboration.
After working collaboratively for some time, Dr. Hussain and his partners decided to teach the NP how to intubate. It was a thoughtful and deliberate process, and “we used the same kind of mindset we’d used when we’ve supervised residents at other institutions,” he said.
Dr. Hussain and his partners have been fortunate in having such a long-term relationship with an APP. Their NP had worked as a nurse in the ICU before training as an adult gerontology–acute care NP and joining Dr. Hussain’s practice, so she was also “well known to us,” he added.
Rachel Adney, CPNP-PC, a certified pediatric NP in the division of pediatric pulmonology at Stanford (Calif.) Medicine Children’s Health, is an APP who actively sought advanced training. She joined Stanford in 2011 to provide ambulatory care, primarily, and having years of prior experience in asthma management and education, she fast became known as “the asthma person.”
After a physician colleague one day objected to her caring for a patient without asthma, Ms. Adney, the first APP in the division, approached John D. Mark, MD, program director of the pediatric fellowship program at Stanford, and inquired about training “so I could have more breadth and depth across the whole pulmonary milieu.”
Together they designed a “mini pediatric pulmonary fellowship” for Ms. Adney, incorporating elements of the first year of Stanford’s pediatric fellowship program as well as training materials from the University of Arizona’s Pediatric Pulmonary Center, Tucson, one of six federally funded PCCs that train various health care providers to care for pediatric patients with chronic pulmonary conditions. (Dr. Mark had previously been an educator at the center while serving on the University of Arizona faculty.)
Her curriculum consisted of 1,000 total hours of training, including 125 hours of didactic learning and 400 hours of both inpatient and outpatient clinical training in areas such as cystic fibrosis, sleep medicine, bronchopulmonary dysplasia (BPD), neuromuscular disorders, and general pulmonary medicine. “Rachel rotated through clinics, first as an observer, then as a trainee ... and she attended lectures that my fellows attended,” said Dr. Mark, who has long been a preceptor for APPs. “She became like a 1-year fellow in my division.”
Today, Ms. Adney sees patients independently in four outreach clinics along California’s central coast. “She sees very complicated pediatric pulmonary patients now” overall, and has become integral to Stanford’s interdisciplinary CRIB program (cardiac and respiratory care for infants with BPD), Dr. Mark said. “She follows these patients at Stanford along with the whole CRIB group, then sees them on her own for follow-up.”
As a result of her training, Ms. Adney said, “knowing that I have the knowledge and experience to take on more complex patients, my colleagues now trust me and are confident in my skills. They feel comfortable sending [patients] to me much earlier. ... And they know that if there’s something I need help with I will go to them instantly.”
Pulmonology “really spoke to my heart,” she said, recalling her pre-Stanford journey as an in-hospital medical-surgical nurse, and then, after her NP training, as a outpatient primary care PNP. “For the most part, it’s like putting a puzzle together, and being able to really impact the quality of life these patients have,” said Ms. Adney, who serves on the APAPP’s pediatric subcommittee.
It’s clear, Dr. Mark said, that “things are changing around the country” with increasing institutional interest in developing formal APP specialty training programs. “There’s no way [for an APP] to walk into a specialty and play an active role without additional training,” and institutions are frustrated with turnover and the loss of APPs who decide after 6-9 months of on-the-job training that they’re not interested in the field.
Stanford Medicine Children’s Health, in fact, has launched an internal Pediatric APP Fellowship Program that is training its first cohort of six newly graduated NPs and PAs in two clinical tracks, including a medical/surgical track that incorporates rotations in pulmonary medicine, said Raji Koppolu, CPNP-PC/AC, manager of advanced practice professional development for Stanford Medicine Children’s Health.
APP fellowship programs have been in existence since 2007 in a variety of clinical settings, she said, but more institutions are developing them as a way of recruiting and retaining APPs in areas of high need and of equipping them for successful transitions to their APP roles. Various national bodies accredit APP fellowship programs.
Most pulmonary fellowship programs, Ms. Young said, are also internal programs providing postgraduate education to their own newly hired APPs or recent NP/PA graduates. This limits their reach, but “it’s a step in the right direction toward standardizing education for pulmonary APPs.”
Defining APP competencies
In interventional pulmonology, training may soon be guided by newly defined “core clinical competencies” for APPs. The soon-to-be published and distributed competencies – the first such national APP competencies in pulmonology – were developed by an APP Leadership Council within the American Association of Bronchology and Interventional Pulmonology and cover the most common disease processes and practices in IP, from COPD and bronchoscopic lung volume reduction to pleural effusion and lung cancer screening.
Rebecca Priebe, ACNP-BC, who cochairs the AABIP’s APP chapter, organized the effort several years ago, bringing together a group of APPs and physician experts in advanced bronchoscopy and IP (some but not all of whom have worked with APPs), after fielding questions from pulmonologists at AABIP meetings about what to look for in an AAP and how to train them.
Physicians and institutions who are hiring and training APPs for IP can use any or all of the 11 core competencies to personalize and evaluate the training process for each APP’s needs, she said. “Someone looking to hire an APP for pleural disease, for instance, can pull up the content on plural effusion.”
APP interest in interventional pulmonology is growing rapidly, Ms. Priebe said, noting growth in the AABIP’s APP chapter from about 7-8 APPs 5 years ago to at least 60 currently.
Ms. Priebe was hired by Henry Ford Health in Detroit about 5 years ago to help establish and run an inpatient IP consult service, and more recently, she helped establish their inpatient pleural disease service and a bronchoscopic lung volume reduction program.
For the inpatient IP service, after several months of side-by-side training with an IP fellow and attending physicians, she began independently evaluating new patients, writing notes, and making recommendations.
For patients with pleural disease, she performs ultrasound examinations, chest tube insertions, and bedside thoracentesis independently. And for the bronchoscopic lung volume reduction program, she evaluates patients for candidate status, participates in valve placement, and sees patients independently through a year of follow-up.
“Physician colleagues often aren’t sure what an APP’s education and scope of practice is,” said Ms. Priebe, who was an ICU nurse before training as an acute care NP and then worked first with a private practice inpatient service and then with the University of Michigan, Ann Arbor, where she established and grew an APP-run program managing lung transplant patients and a step-down ICU unit.
“It’s a matter of knowing [your state’s policies], treating them like a fellow you would train, and then using them to the fullest extent of their education and training. If they’re given an opportunity to learn a subspecialty skill set, they can be an asset to any pulmonary program.”
‘We’re here to support,’ not replace
In her own practice, Ms. Young is one of seven APPs who work with nine physicians on a full range of inpatient care, outpatient care, critical care, sleep medicine, and procedures. Many new patients are seen first by the APP, who does the workup and orders tests, and by the physician on a follow-up visit. Most patients needing routine management of asthma and COPD are seen by the physician every third or fourth visit, she said.
Ms. Young also directs a 24-hour in-house APP service recently established by the practice, and she participates in research. In a practice across town, she noted, APPs see mainly established patients and do not practice as autonomously as the state permits. “Part of that difference may [stem from] the lack of a standard of education and variable amounts of work the practice puts into their APPs.”
The American Medical Association’s #StopScopeCreep social media messaging feels divisive and “sheds a negative light on APPs working in any area,” Ms. Young said. “One of the biggest things we want to convey [at APAPP] is that we’re not here for [physicians’] jobs.”
“We’re here to support those who are practicing, to support underserved populations, and to help bridge gaps” created by an aging pulmonologist workforce and real and projected physician shortages, Ms. Young said, referring to a 2016 report from the Health Resources and Services Administration and a 2017 report from Merritt Hawkins indicating that 73% of U.S. pulmonologists (the largest percentage of all subspecialties) were at least 55 years old.
Dr. Hussain said he has “seen scope creep” first-hand in his hospitals, in the form of noncollaborative practices and tasks performed by APPs without adequate training – most likely often stemming from poor decisions and oversight by physicians. But when constructed thoughtfully, APP-physician teams are “serving great needs” in many types of care, he said, from follow-up care and management of chronic conditions to inpatient rounding. “My [colleagues] are having great success,” he said.
He is watching with interest – and some concern – pending reimbursement changes from the Centers for Medicare & Medicaid Services that will make time the only defining feature of the “substantive” portion of a split/shared visit involving physicians and APPs in a facility setting. Medical decision-making will no longer be applicable.
For time-based services like critical care, time alone is currently the metric. (And in the nonfacility setting, physician-APP teams may still apply “incident to” billing practices). But in the facility setting, said Amy M. Ahasic, MD, MPH, a pulmonologist in Norwalk, Conn., who coauthored a 2022 commentary on the issue, the change (now planned for 2024) could be problematic for employed physicians whose contracts are based on productivity, and could create tension and possibly lead to reduced use of APPs rather than supporting collaborative care.
“The team model has been evolving so well over the past 10-15 years,” said Dr. Ahasic, who serves on the CHEST Health Policy and Advocacy Reimbursement Workgroup and cochairs the CHEST/American Thoracic Society clinical practice committee with Dr. Hussain. “It’s good for patient safety to have more [providers] involved ... and because APP salaries are lower health systems could do it and be able to have better care and better coverage.”
The pulmonology culture, said Dr. Hussain, has been increasingly embracing APPs and “it’s collegial.” Pulmonologists are “coming to CHEST meetings with their APPs. They’re learning the same things we’re learning, to manage the same patients we manage.”
The article sources reported that they had no relevant financial conflicts of interest to disclose.
The integration of advanced practice providers (APPs) into pulmonology practice is in flux and deepening across numerous settings, from outpatient clinics to intensive care and inpatient pulmonary consult services – and as it evolves, so are issues of training.
Some institutions are developing pulmonary fellowship programs for APPs. This is a good indication that team-based pulmonology may be moving toward a time in the future when nurse practitioners (NPs) and physician assistants (PAs) join pulmonologists in practice after having undergone formal education in the subspecialty, rather than learning solely on the job from dedicated mentors.
Neither NPs nor PAs, who comprise almost all of the APP workforce in pulmonology, currently have a pulmonary tract for training. “Weight falls on the employer’s shoulders to train and educate their APPs,” said Corinne R. Young, MSN, FNP-C, FCCP, director of APP and clinical services at Colorado Springs Pulmonary Consultants and founder and president of the Association of Pulmonary Advanced Practice Providers, which launched in 2018.
The role that an APP plays and their scope of practice is determined not only by state policies and regulations – and by their prior experience, knowledge and motivation – but by “how much work a practice puts into [education and training],” she said.
An estimated 3,000-8,000 APPs are working in pulmonology, according to an analysis done by a marketing agency that has worked for the American College of Chest Physicians, Ms. Young said.
A 2021 APAPP survey of its several hundred members at the time showed them working in hospital systems (41%), private practice (28%), university systems (10%), and other health care systems (21%). They indicated practicing in pulmonary medicine, sleep medicine, or critical care – or some combination of these areas – and the vast majority (82%) indicated they were seeing both new and established patients in their roles.
“Nobody knows exactly how many of us are out there,” Ms. Young said. “But CHEST and APAPP are making great efforts to be beacons to APPs working in this realm and to bring them together to have a voice.”
The APAPP also wants to “close the education gap” and to “eventually develop a certification program to vet our knowledge in this area,” she said. “Right now, the closest we can get to vetting our knowledge is to become an FCCP through CHEST.”
Earning trust, seeking training
Omar Hussain, DO, has been practicing with an NP for over a decade in his role as an intensivist and knows what it’s like to train, supervise, and grow together. He and his private practice colleagues have a contract with Advocate Condell Hospital in Libertyville, Ill., to cover its ICU, and they hired their NP primarily to help care for shorter-stay, non–critically ill patients in the ICU (for example, patients receiving postoperative monitoring).
The NP has been invaluable. “We literally sit next to each other and in the mornings we make a game plan of which patients she will tackle first and which ones I’ll see first,” Dr. Hussain said. “When we’re called by the nurse for an ICU evaluation [on the floor], we’ll decide in real time who goes.”
The NP ensures that all guidelines and quality measures are followed in the ICU and, with a Monday-Friday schedule, she provides valuable continuity when there are handoffs from one intensivist to another, said Dr. Hussain, who serves as cochair of the joint CHEST/American Thoracic Society clinical practice committee, which deals with issues of physician-APP collaboration.
After working collaboratively for some time, Dr. Hussain and his partners decided to teach the NP how to intubate. It was a thoughtful and deliberate process, and “we used the same kind of mindset we’d used when we’ve supervised residents at other institutions,” he said.
Dr. Hussain and his partners have been fortunate in having such a long-term relationship with an APP. Their NP had worked as a nurse in the ICU before training as an adult gerontology–acute care NP and joining Dr. Hussain’s practice, so she was also “well known to us,” he added.
Rachel Adney, CPNP-PC, a certified pediatric NP in the division of pediatric pulmonology at Stanford (Calif.) Medicine Children’s Health, is an APP who actively sought advanced training. She joined Stanford in 2011 to provide ambulatory care, primarily, and having years of prior experience in asthma management and education, she fast became known as “the asthma person.”
After a physician colleague one day objected to her caring for a patient without asthma, Ms. Adney, the first APP in the division, approached John D. Mark, MD, program director of the pediatric fellowship program at Stanford, and inquired about training “so I could have more breadth and depth across the whole pulmonary milieu.”
Together they designed a “mini pediatric pulmonary fellowship” for Ms. Adney, incorporating elements of the first year of Stanford’s pediatric fellowship program as well as training materials from the University of Arizona’s Pediatric Pulmonary Center, Tucson, one of six federally funded PCCs that train various health care providers to care for pediatric patients with chronic pulmonary conditions. (Dr. Mark had previously been an educator at the center while serving on the University of Arizona faculty.)
Her curriculum consisted of 1,000 total hours of training, including 125 hours of didactic learning and 400 hours of both inpatient and outpatient clinical training in areas such as cystic fibrosis, sleep medicine, bronchopulmonary dysplasia (BPD), neuromuscular disorders, and general pulmonary medicine. “Rachel rotated through clinics, first as an observer, then as a trainee ... and she attended lectures that my fellows attended,” said Dr. Mark, who has long been a preceptor for APPs. “She became like a 1-year fellow in my division.”
Today, Ms. Adney sees patients independently in four outreach clinics along California’s central coast. “She sees very complicated pediatric pulmonary patients now” overall, and has become integral to Stanford’s interdisciplinary CRIB program (cardiac and respiratory care for infants with BPD), Dr. Mark said. “She follows these patients at Stanford along with the whole CRIB group, then sees them on her own for follow-up.”
As a result of her training, Ms. Adney said, “knowing that I have the knowledge and experience to take on more complex patients, my colleagues now trust me and are confident in my skills. They feel comfortable sending [patients] to me much earlier. ... And they know that if there’s something I need help with I will go to them instantly.”
Pulmonology “really spoke to my heart,” she said, recalling her pre-Stanford journey as an in-hospital medical-surgical nurse, and then, after her NP training, as a outpatient primary care PNP. “For the most part, it’s like putting a puzzle together, and being able to really impact the quality of life these patients have,” said Ms. Adney, who serves on the APAPP’s pediatric subcommittee.
It’s clear, Dr. Mark said, that “things are changing around the country” with increasing institutional interest in developing formal APP specialty training programs. “There’s no way [for an APP] to walk into a specialty and play an active role without additional training,” and institutions are frustrated with turnover and the loss of APPs who decide after 6-9 months of on-the-job training that they’re not interested in the field.
Stanford Medicine Children’s Health, in fact, has launched an internal Pediatric APP Fellowship Program that is training its first cohort of six newly graduated NPs and PAs in two clinical tracks, including a medical/surgical track that incorporates rotations in pulmonary medicine, said Raji Koppolu, CPNP-PC/AC, manager of advanced practice professional development for Stanford Medicine Children’s Health.
APP fellowship programs have been in existence since 2007 in a variety of clinical settings, she said, but more institutions are developing them as a way of recruiting and retaining APPs in areas of high need and of equipping them for successful transitions to their APP roles. Various national bodies accredit APP fellowship programs.
Most pulmonary fellowship programs, Ms. Young said, are also internal programs providing postgraduate education to their own newly hired APPs or recent NP/PA graduates. This limits their reach, but “it’s a step in the right direction toward standardizing education for pulmonary APPs.”
Defining APP competencies
In interventional pulmonology, training may soon be guided by newly defined “core clinical competencies” for APPs. The soon-to-be published and distributed competencies – the first such national APP competencies in pulmonology – were developed by an APP Leadership Council within the American Association of Bronchology and Interventional Pulmonology and cover the most common disease processes and practices in IP, from COPD and bronchoscopic lung volume reduction to pleural effusion and lung cancer screening.
Rebecca Priebe, ACNP-BC, who cochairs the AABIP’s APP chapter, organized the effort several years ago, bringing together a group of APPs and physician experts in advanced bronchoscopy and IP (some but not all of whom have worked with APPs), after fielding questions from pulmonologists at AABIP meetings about what to look for in an AAP and how to train them.
Physicians and institutions who are hiring and training APPs for IP can use any or all of the 11 core competencies to personalize and evaluate the training process for each APP’s needs, she said. “Someone looking to hire an APP for pleural disease, for instance, can pull up the content on plural effusion.”
APP interest in interventional pulmonology is growing rapidly, Ms. Priebe said, noting growth in the AABIP’s APP chapter from about 7-8 APPs 5 years ago to at least 60 currently.
Ms. Priebe was hired by Henry Ford Health in Detroit about 5 years ago to help establish and run an inpatient IP consult service, and more recently, she helped establish their inpatient pleural disease service and a bronchoscopic lung volume reduction program.
For the inpatient IP service, after several months of side-by-side training with an IP fellow and attending physicians, she began independently evaluating new patients, writing notes, and making recommendations.
For patients with pleural disease, she performs ultrasound examinations, chest tube insertions, and bedside thoracentesis independently. And for the bronchoscopic lung volume reduction program, she evaluates patients for candidate status, participates in valve placement, and sees patients independently through a year of follow-up.
“Physician colleagues often aren’t sure what an APP’s education and scope of practice is,” said Ms. Priebe, who was an ICU nurse before training as an acute care NP and then worked first with a private practice inpatient service and then with the University of Michigan, Ann Arbor, where she established and grew an APP-run program managing lung transplant patients and a step-down ICU unit.
“It’s a matter of knowing [your state’s policies], treating them like a fellow you would train, and then using them to the fullest extent of their education and training. If they’re given an opportunity to learn a subspecialty skill set, they can be an asset to any pulmonary program.”
‘We’re here to support,’ not replace
In her own practice, Ms. Young is one of seven APPs who work with nine physicians on a full range of inpatient care, outpatient care, critical care, sleep medicine, and procedures. Many new patients are seen first by the APP, who does the workup and orders tests, and by the physician on a follow-up visit. Most patients needing routine management of asthma and COPD are seen by the physician every third or fourth visit, she said.
Ms. Young also directs a 24-hour in-house APP service recently established by the practice, and she participates in research. In a practice across town, she noted, APPs see mainly established patients and do not practice as autonomously as the state permits. “Part of that difference may [stem from] the lack of a standard of education and variable amounts of work the practice puts into their APPs.”
The American Medical Association’s #StopScopeCreep social media messaging feels divisive and “sheds a negative light on APPs working in any area,” Ms. Young said. “One of the biggest things we want to convey [at APAPP] is that we’re not here for [physicians’] jobs.”
“We’re here to support those who are practicing, to support underserved populations, and to help bridge gaps” created by an aging pulmonologist workforce and real and projected physician shortages, Ms. Young said, referring to a 2016 report from the Health Resources and Services Administration and a 2017 report from Merritt Hawkins indicating that 73% of U.S. pulmonologists (the largest percentage of all subspecialties) were at least 55 years old.
Dr. Hussain said he has “seen scope creep” first-hand in his hospitals, in the form of noncollaborative practices and tasks performed by APPs without adequate training – most likely often stemming from poor decisions and oversight by physicians. But when constructed thoughtfully, APP-physician teams are “serving great needs” in many types of care, he said, from follow-up care and management of chronic conditions to inpatient rounding. “My [colleagues] are having great success,” he said.
He is watching with interest – and some concern – pending reimbursement changes from the Centers for Medicare & Medicaid Services that will make time the only defining feature of the “substantive” portion of a split/shared visit involving physicians and APPs in a facility setting. Medical decision-making will no longer be applicable.
For time-based services like critical care, time alone is currently the metric. (And in the nonfacility setting, physician-APP teams may still apply “incident to” billing practices). But in the facility setting, said Amy M. Ahasic, MD, MPH, a pulmonologist in Norwalk, Conn., who coauthored a 2022 commentary on the issue, the change (now planned for 2024) could be problematic for employed physicians whose contracts are based on productivity, and could create tension and possibly lead to reduced use of APPs rather than supporting collaborative care.
“The team model has been evolving so well over the past 10-15 years,” said Dr. Ahasic, who serves on the CHEST Health Policy and Advocacy Reimbursement Workgroup and cochairs the CHEST/American Thoracic Society clinical practice committee with Dr. Hussain. “It’s good for patient safety to have more [providers] involved ... and because APP salaries are lower health systems could do it and be able to have better care and better coverage.”
The pulmonology culture, said Dr. Hussain, has been increasingly embracing APPs and “it’s collegial.” Pulmonologists are “coming to CHEST meetings with their APPs. They’re learning the same things we’re learning, to manage the same patients we manage.”
The article sources reported that they had no relevant financial conflicts of interest to disclose.
Applications for laser-assisted drug delivery on the horizon, expert says
For those who view fractional ablative laser–assisted drug delivery as a pie-in-the-sky procedure that will take years to work its way into routine clinical practice, think again.
According to Merete Haedersdal, MD, PhD, DMSc, .
“The groundwork has been established over a decade with more than 100 publications available on PubMed,” Dr. Haedersdal, professor of dermatology at the University of Copenhagen, said during a virtual course on laser and aesthetic skin therapy. “There is no doubt that by drilling tiny little holes or channels with ablative fractional lasers, we enhance drug delivery to the skin, and we also empower different topical treatment regimens. Also, laser-assisted drug delivery holds the potential to bring new innovations into established medicine.”
Many studies have demonstrated that clinicians can enhance drug uptake into the skin with the fractional 10,600 nm CO2 laser, the fractional 2,940 nm erbium:YAG laser, and the 1,927 nm thulium laser, but proper tuning of the devices is key. The lower the density, the better, Dr. Haedersdal said.
“Typically, we use 5% density or 5% coverage, sometimes 10%-15%, but don’t go higher in order to avoid the risk of having a systemic uptake,” she said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Also, the pulse energy for channel depth needs to be tailored to the specific dermatologic disease being treated,” she said, noting that for melasma, for example, “very low pulse energies” would be used, but they would be higher for treating thicker lesions, such as a hypertrophic scar.
Treatment with ablative fractional lasers enhances drug accumulation in the skin of any drug or substance applied to the skin, and clinical indications are expanding rapidly. Established indications include combining ablative fractional lasers and photodynamic therapy (PDT) for AKs and combining ablative fractional lasers and triamcinolone or 5-FU for scars. “Although we have a good body of evidence, particularly for AKs, it’s still an off-label use,” she emphasized.
Evolving indications include concomitant use of ablative fractional laser and vitamins and cosmeceuticals for rejuvenation; lidocaine for local anesthetics; tranexamic acid and hydroquinone for melasma; antifungals for onychomycosis; Botox for hyperhidrosis; minoxidil for alopecia; and betamethasone for vitiligo. A promising treatment for skin cancer “on the horizon,” she said, is the “combination of ablative fractional laser with PD1 inhibitors and chemotherapy.”
Data on AKs
Evidence supporting laser-assisted drug delivery for AKs comes from more than 10 randomized, controlled trials in the dermatology literature involving 400-plus immunocompetent and immunosuppressed patients. These trials have found ablative fractional laser–assisted PDT to be significantly more efficacious than PDT alone up to 12 months postoperatively and to foster lower rates of AK recurrence.
In a meta-analysis and systematic review, German researchers concluded that PDT combined with ablative laser treatment for AKs is more efficient but not more painful than either therapy alone. They recommended the combined regimen for patients with severe photodamage, field cancerization, and multiple AKs.
In 2020, an international consensus panel of experts, including Dr. Haedersdal, published recommendations regarding laser treatment of traumatic scars and contractures. The panel members determined that laser-assisted delivery of corticosteroids and antimetabolites was recommended for hypertrophic scars and cited triamcinolone acetonide suspension (TAC) as the most common corticosteroid used in combination with ablative fractional lasers. “It can be applied in concentrations of 40 mg/mL or less depending on the degree of hypertrophy,” they wrote.
In addition, they stated that 5-FU solution is “most commonly applied in a concentration of 50 mg/mL alone, or mixed with TAC in ratios of 9:1 or 3:1.”
According to the best available evidence, the clinical approach for hypertrophic scars supports combination treatment with ablative fractional laser and triamcinolone acetonide either alone or in combination with 5-FU. For atrophic scars, laser-assisted delivery of poly-L-lactic acid has been shown to be efficient. “Both of these treatments improve texture and thickness but also dyschromia and scar functionality,” said Dr. Haedersdal, who is also a visiting scientist at the Wellman Center for Photomedicine, Boston.
Commenting on patient safety with laser-assisted drug delivery, “the combination of lasers and topicals can be a powerful cocktail,” she said. “You can expect intensified local skin reactions. When treating larger areas, consider the risk of systemic absorption and the risk of potential toxicity. There is also the potential for infection with pathogens such as Staphylococcus aureus. The take-home message here is that you should only use the type and amount of drug no higher than administered during intradermal injection.”
Dr. Haedersdal disclosed that she has received equipment from Cherry Imaging, Cynosure-Hologic, MiraDry, and PerfAction Technologies. She has also received research grants from Leo Pharma, Lutronic, Mirai Medical, Novoxel, and Venus Concept.
For those who view fractional ablative laser–assisted drug delivery as a pie-in-the-sky procedure that will take years to work its way into routine clinical practice, think again.
According to Merete Haedersdal, MD, PhD, DMSc, .
“The groundwork has been established over a decade with more than 100 publications available on PubMed,” Dr. Haedersdal, professor of dermatology at the University of Copenhagen, said during a virtual course on laser and aesthetic skin therapy. “There is no doubt that by drilling tiny little holes or channels with ablative fractional lasers, we enhance drug delivery to the skin, and we also empower different topical treatment regimens. Also, laser-assisted drug delivery holds the potential to bring new innovations into established medicine.”
Many studies have demonstrated that clinicians can enhance drug uptake into the skin with the fractional 10,600 nm CO2 laser, the fractional 2,940 nm erbium:YAG laser, and the 1,927 nm thulium laser, but proper tuning of the devices is key. The lower the density, the better, Dr. Haedersdal said.
“Typically, we use 5% density or 5% coverage, sometimes 10%-15%, but don’t go higher in order to avoid the risk of having a systemic uptake,” she said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Also, the pulse energy for channel depth needs to be tailored to the specific dermatologic disease being treated,” she said, noting that for melasma, for example, “very low pulse energies” would be used, but they would be higher for treating thicker lesions, such as a hypertrophic scar.
Treatment with ablative fractional lasers enhances drug accumulation in the skin of any drug or substance applied to the skin, and clinical indications are expanding rapidly. Established indications include combining ablative fractional lasers and photodynamic therapy (PDT) for AKs and combining ablative fractional lasers and triamcinolone or 5-FU for scars. “Although we have a good body of evidence, particularly for AKs, it’s still an off-label use,” she emphasized.
Evolving indications include concomitant use of ablative fractional laser and vitamins and cosmeceuticals for rejuvenation; lidocaine for local anesthetics; tranexamic acid and hydroquinone for melasma; antifungals for onychomycosis; Botox for hyperhidrosis; minoxidil for alopecia; and betamethasone for vitiligo. A promising treatment for skin cancer “on the horizon,” she said, is the “combination of ablative fractional laser with PD1 inhibitors and chemotherapy.”
Data on AKs
Evidence supporting laser-assisted drug delivery for AKs comes from more than 10 randomized, controlled trials in the dermatology literature involving 400-plus immunocompetent and immunosuppressed patients. These trials have found ablative fractional laser–assisted PDT to be significantly more efficacious than PDT alone up to 12 months postoperatively and to foster lower rates of AK recurrence.
In a meta-analysis and systematic review, German researchers concluded that PDT combined with ablative laser treatment for AKs is more efficient but not more painful than either therapy alone. They recommended the combined regimen for patients with severe photodamage, field cancerization, and multiple AKs.
In 2020, an international consensus panel of experts, including Dr. Haedersdal, published recommendations regarding laser treatment of traumatic scars and contractures. The panel members determined that laser-assisted delivery of corticosteroids and antimetabolites was recommended for hypertrophic scars and cited triamcinolone acetonide suspension (TAC) as the most common corticosteroid used in combination with ablative fractional lasers. “It can be applied in concentrations of 40 mg/mL or less depending on the degree of hypertrophy,” they wrote.
In addition, they stated that 5-FU solution is “most commonly applied in a concentration of 50 mg/mL alone, or mixed with TAC in ratios of 9:1 or 3:1.”
According to the best available evidence, the clinical approach for hypertrophic scars supports combination treatment with ablative fractional laser and triamcinolone acetonide either alone or in combination with 5-FU. For atrophic scars, laser-assisted delivery of poly-L-lactic acid has been shown to be efficient. “Both of these treatments improve texture and thickness but also dyschromia and scar functionality,” said Dr. Haedersdal, who is also a visiting scientist at the Wellman Center for Photomedicine, Boston.
Commenting on patient safety with laser-assisted drug delivery, “the combination of lasers and topicals can be a powerful cocktail,” she said. “You can expect intensified local skin reactions. When treating larger areas, consider the risk of systemic absorption and the risk of potential toxicity. There is also the potential for infection with pathogens such as Staphylococcus aureus. The take-home message here is that you should only use the type and amount of drug no higher than administered during intradermal injection.”
Dr. Haedersdal disclosed that she has received equipment from Cherry Imaging, Cynosure-Hologic, MiraDry, and PerfAction Technologies. She has also received research grants from Leo Pharma, Lutronic, Mirai Medical, Novoxel, and Venus Concept.
For those who view fractional ablative laser–assisted drug delivery as a pie-in-the-sky procedure that will take years to work its way into routine clinical practice, think again.
According to Merete Haedersdal, MD, PhD, DMSc, .
“The groundwork has been established over a decade with more than 100 publications available on PubMed,” Dr. Haedersdal, professor of dermatology at the University of Copenhagen, said during a virtual course on laser and aesthetic skin therapy. “There is no doubt that by drilling tiny little holes or channels with ablative fractional lasers, we enhance drug delivery to the skin, and we also empower different topical treatment regimens. Also, laser-assisted drug delivery holds the potential to bring new innovations into established medicine.”
Many studies have demonstrated that clinicians can enhance drug uptake into the skin with the fractional 10,600 nm CO2 laser, the fractional 2,940 nm erbium:YAG laser, and the 1,927 nm thulium laser, but proper tuning of the devices is key. The lower the density, the better, Dr. Haedersdal said.
“Typically, we use 5% density or 5% coverage, sometimes 10%-15%, but don’t go higher in order to avoid the risk of having a systemic uptake,” she said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Also, the pulse energy for channel depth needs to be tailored to the specific dermatologic disease being treated,” she said, noting that for melasma, for example, “very low pulse energies” would be used, but they would be higher for treating thicker lesions, such as a hypertrophic scar.
Treatment with ablative fractional lasers enhances drug accumulation in the skin of any drug or substance applied to the skin, and clinical indications are expanding rapidly. Established indications include combining ablative fractional lasers and photodynamic therapy (PDT) for AKs and combining ablative fractional lasers and triamcinolone or 5-FU for scars. “Although we have a good body of evidence, particularly for AKs, it’s still an off-label use,” she emphasized.
Evolving indications include concomitant use of ablative fractional laser and vitamins and cosmeceuticals for rejuvenation; lidocaine for local anesthetics; tranexamic acid and hydroquinone for melasma; antifungals for onychomycosis; Botox for hyperhidrosis; minoxidil for alopecia; and betamethasone for vitiligo. A promising treatment for skin cancer “on the horizon,” she said, is the “combination of ablative fractional laser with PD1 inhibitors and chemotherapy.”
Data on AKs
Evidence supporting laser-assisted drug delivery for AKs comes from more than 10 randomized, controlled trials in the dermatology literature involving 400-plus immunocompetent and immunosuppressed patients. These trials have found ablative fractional laser–assisted PDT to be significantly more efficacious than PDT alone up to 12 months postoperatively and to foster lower rates of AK recurrence.
In a meta-analysis and systematic review, German researchers concluded that PDT combined with ablative laser treatment for AKs is more efficient but not more painful than either therapy alone. They recommended the combined regimen for patients with severe photodamage, field cancerization, and multiple AKs.
In 2020, an international consensus panel of experts, including Dr. Haedersdal, published recommendations regarding laser treatment of traumatic scars and contractures. The panel members determined that laser-assisted delivery of corticosteroids and antimetabolites was recommended for hypertrophic scars and cited triamcinolone acetonide suspension (TAC) as the most common corticosteroid used in combination with ablative fractional lasers. “It can be applied in concentrations of 40 mg/mL or less depending on the degree of hypertrophy,” they wrote.
In addition, they stated that 5-FU solution is “most commonly applied in a concentration of 50 mg/mL alone, or mixed with TAC in ratios of 9:1 or 3:1.”
According to the best available evidence, the clinical approach for hypertrophic scars supports combination treatment with ablative fractional laser and triamcinolone acetonide either alone or in combination with 5-FU. For atrophic scars, laser-assisted delivery of poly-L-lactic acid has been shown to be efficient. “Both of these treatments improve texture and thickness but also dyschromia and scar functionality,” said Dr. Haedersdal, who is also a visiting scientist at the Wellman Center for Photomedicine, Boston.
Commenting on patient safety with laser-assisted drug delivery, “the combination of lasers and topicals can be a powerful cocktail,” she said. “You can expect intensified local skin reactions. When treating larger areas, consider the risk of systemic absorption and the risk of potential toxicity. There is also the potential for infection with pathogens such as Staphylococcus aureus. The take-home message here is that you should only use the type and amount of drug no higher than administered during intradermal injection.”
Dr. Haedersdal disclosed that she has received equipment from Cherry Imaging, Cynosure-Hologic, MiraDry, and PerfAction Technologies. She has also received research grants from Leo Pharma, Lutronic, Mirai Medical, Novoxel, and Venus Concept.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Everyone wins when losers get paid
Bribery really is the solution to all of life’s problems
Breaking news: The United States has a bit of an obesity epidemic. Okay, maybe not so breaking news. But it’s a problem we’ve been struggling with for a very long time. Part of the issue is that there really is no secret to weight loss. Pretty much anything can work if you’re committed. The millions of diets floating around are testament to this idea.
The problem of losing weight is amplified if you don’t rake in the big bucks. Lower-income individuals often can’t afford healthy superfoods, and they’re often too busy to spend time at classes, exercising, or following programs. A group of researchers at New York University has offered up an alternate solution to encourage weight loss in low-income people: Pay them.
Specifically, pay them for losing weight. A reward, if you will. The researchers recruited several hundred lower-income people and split them into three groups. All participants received a free 1-year membership to a gym and weight-loss program, as well as food journals and fitness devices, but one group received payment (on average, about $300 overall) for attending meetings, exercising a certain amount every week, or weighing themselves twice a week. About 40% of people in this group lost 5% of their body weight after 6 months, twice as many as in the group that did not receive payment for performing these tasks.
The big winners, however, were those in the third group. They also received the free stuff, but the researchers offered them a more simple and direct bribe: Lose 5% of your weight over 6 months and we’ll pay you. The reward? About $450 on average, and it worked very well, with half this group losing the weight after 6 months. That said, after a year something like a fifth of this group put the weight back on, bringing them in line with the group that was paid to perform tasks. Still, both groups outperformed the control group, which received no money.
The takeaway from this research is pretty obvious. Pay people a fair price to do something, and they’ll do it. This is a lesson that has absolutely no relevance in the modern world. Nope, none whatsoever. We all receive completely fair wages. We all have plenty of money to pay for things. Everything is fine.
More green space, less medicine
Have you heard of the 3-30-300 rule? Proposed by urban forester Cecil Konijnendijk, it’s become the rule of thumb for urban planners and other foresters into getting more green space in populated areas. A recent study has found that people who lived within this 3-30-300 rule had better mental health and less medication use.
If you’re not an urban forester, however, you may not know what the 3-30-300 rule is. But it’s pretty simple, people should be able to see at least three trees from their home, have 30% tree canopy in their neighborhood, and have 300 Spartans to defend against the Persian army.
We may have made that last one up. It’s actually have a green space or park within 300 meters of your home.
In the new study, only 4.7% of people surveyed lived in an area that followed all three rules. About 62% of the surveyed lived with a green space at least 300 meters away, 43% had at least three trees within 15 meters from their home, and a rather pitiful 9% had adequate tree canopy coverage in their neighborhood.
Greater adherence to the 3-30-300 rule was associated with fewer visits to the psychologist, with 8.3% of the participants reporting a psychologist visit in the last year. The data come from a sample of a little over 3,000 Barcelona residents aged 15-97 who were randomly selected to participate in the Barcelona Public Health Agency Survey.
“There is an urgent need to provide citizens with more green space,” said Mark Nieuwenhuijsen, lead author of the study. “We may need to tear out asphalt and plant more trees, which would not only improve health, but also reduce heat island effects and contribute to carbon capture.”
The main goal and message is that more green space is good for everyone. So if you’re feeling a little overwhelmed, take a breather and sit somewhere green. Or call those 300 Spartans and get them to start knocking some buildings down.
Said the toilet to the engineer: Do you hear what I hear?
A mythical hero’s journey took Dorothy along the yellow brick road to find the Wizard of Oz. Huckleberry Finn used a raft to float down the Mississippi River. Luke Skywalker did most of his traveling between planets. For the rest of us, the journey may be just a bit shorter.
Also a bit less heroic. Unless, of course, you’re prepping for a colonoscopy. Yup, we’re headed to the toilet, but not just any toilet. This toilet was the subject of a presentation at the annual meeting of the Acoustical Society of America, titled “The feces thesis: Using machine learning to detect diarrhea,” and that presentation was the hero’s journey of Maia Gatlin, PhD, a research engineer at the Georgia Institute of Technology.
She and her team attached a noninvasive microphone sensor to a toilet, and now they can identify bowel diseases without collecting any identifiable information.
The audio sample of an excretion event is “transformed into a spectrogram, which essentially captures the sound in an image. Different events produce different features in the audio and the spectrogram. For example, urination creates a consistent tone, while defecation may have a singular tone. In contrast, diarrhea is more random,” they explained in the written statement.
They used a machine learning algorithm to classify each spectrogram based on its features. “The algorithm’s performance was tested against data with and without background noises to make sure it was learning the right sound features, regardless of the sensor’s environment,” Dr. Gatlin and associates wrote.
Their goal is to use the toilet sensor in areas where cholera is common to prevent the spread of disease. After that, who knows? “Perhaps someday, our algorithm can be used with existing in-home smart devices to monitor one’s own bowel movements and health!” she suggested.
That would be a heroic toilet indeed.
Bribery really is the solution to all of life’s problems
Breaking news: The United States has a bit of an obesity epidemic. Okay, maybe not so breaking news. But it’s a problem we’ve been struggling with for a very long time. Part of the issue is that there really is no secret to weight loss. Pretty much anything can work if you’re committed. The millions of diets floating around are testament to this idea.
The problem of losing weight is amplified if you don’t rake in the big bucks. Lower-income individuals often can’t afford healthy superfoods, and they’re often too busy to spend time at classes, exercising, or following programs. A group of researchers at New York University has offered up an alternate solution to encourage weight loss in low-income people: Pay them.
Specifically, pay them for losing weight. A reward, if you will. The researchers recruited several hundred lower-income people and split them into three groups. All participants received a free 1-year membership to a gym and weight-loss program, as well as food journals and fitness devices, but one group received payment (on average, about $300 overall) for attending meetings, exercising a certain amount every week, or weighing themselves twice a week. About 40% of people in this group lost 5% of their body weight after 6 months, twice as many as in the group that did not receive payment for performing these tasks.
The big winners, however, were those in the third group. They also received the free stuff, but the researchers offered them a more simple and direct bribe: Lose 5% of your weight over 6 months and we’ll pay you. The reward? About $450 on average, and it worked very well, with half this group losing the weight after 6 months. That said, after a year something like a fifth of this group put the weight back on, bringing them in line with the group that was paid to perform tasks. Still, both groups outperformed the control group, which received no money.
The takeaway from this research is pretty obvious. Pay people a fair price to do something, and they’ll do it. This is a lesson that has absolutely no relevance in the modern world. Nope, none whatsoever. We all receive completely fair wages. We all have plenty of money to pay for things. Everything is fine.
More green space, less medicine
Have you heard of the 3-30-300 rule? Proposed by urban forester Cecil Konijnendijk, it’s become the rule of thumb for urban planners and other foresters into getting more green space in populated areas. A recent study has found that people who lived within this 3-30-300 rule had better mental health and less medication use.
If you’re not an urban forester, however, you may not know what the 3-30-300 rule is. But it’s pretty simple, people should be able to see at least three trees from their home, have 30% tree canopy in their neighborhood, and have 300 Spartans to defend against the Persian army.
We may have made that last one up. It’s actually have a green space or park within 300 meters of your home.
In the new study, only 4.7% of people surveyed lived in an area that followed all three rules. About 62% of the surveyed lived with a green space at least 300 meters away, 43% had at least three trees within 15 meters from their home, and a rather pitiful 9% had adequate tree canopy coverage in their neighborhood.
Greater adherence to the 3-30-300 rule was associated with fewer visits to the psychologist, with 8.3% of the participants reporting a psychologist visit in the last year. The data come from a sample of a little over 3,000 Barcelona residents aged 15-97 who were randomly selected to participate in the Barcelona Public Health Agency Survey.
“There is an urgent need to provide citizens with more green space,” said Mark Nieuwenhuijsen, lead author of the study. “We may need to tear out asphalt and plant more trees, which would not only improve health, but also reduce heat island effects and contribute to carbon capture.”
The main goal and message is that more green space is good for everyone. So if you’re feeling a little overwhelmed, take a breather and sit somewhere green. Or call those 300 Spartans and get them to start knocking some buildings down.
Said the toilet to the engineer: Do you hear what I hear?
A mythical hero’s journey took Dorothy along the yellow brick road to find the Wizard of Oz. Huckleberry Finn used a raft to float down the Mississippi River. Luke Skywalker did most of his traveling between planets. For the rest of us, the journey may be just a bit shorter.
Also a bit less heroic. Unless, of course, you’re prepping for a colonoscopy. Yup, we’re headed to the toilet, but not just any toilet. This toilet was the subject of a presentation at the annual meeting of the Acoustical Society of America, titled “The feces thesis: Using machine learning to detect diarrhea,” and that presentation was the hero’s journey of Maia Gatlin, PhD, a research engineer at the Georgia Institute of Technology.
She and her team attached a noninvasive microphone sensor to a toilet, and now they can identify bowel diseases without collecting any identifiable information.
The audio sample of an excretion event is “transformed into a spectrogram, which essentially captures the sound in an image. Different events produce different features in the audio and the spectrogram. For example, urination creates a consistent tone, while defecation may have a singular tone. In contrast, diarrhea is more random,” they explained in the written statement.
They used a machine learning algorithm to classify each spectrogram based on its features. “The algorithm’s performance was tested against data with and without background noises to make sure it was learning the right sound features, regardless of the sensor’s environment,” Dr. Gatlin and associates wrote.
Their goal is to use the toilet sensor in areas where cholera is common to prevent the spread of disease. After that, who knows? “Perhaps someday, our algorithm can be used with existing in-home smart devices to monitor one’s own bowel movements and health!” she suggested.
That would be a heroic toilet indeed.
Bribery really is the solution to all of life’s problems
Breaking news: The United States has a bit of an obesity epidemic. Okay, maybe not so breaking news. But it’s a problem we’ve been struggling with for a very long time. Part of the issue is that there really is no secret to weight loss. Pretty much anything can work if you’re committed. The millions of diets floating around are testament to this idea.
The problem of losing weight is amplified if you don’t rake in the big bucks. Lower-income individuals often can’t afford healthy superfoods, and they’re often too busy to spend time at classes, exercising, or following programs. A group of researchers at New York University has offered up an alternate solution to encourage weight loss in low-income people: Pay them.
Specifically, pay them for losing weight. A reward, if you will. The researchers recruited several hundred lower-income people and split them into three groups. All participants received a free 1-year membership to a gym and weight-loss program, as well as food journals and fitness devices, but one group received payment (on average, about $300 overall) for attending meetings, exercising a certain amount every week, or weighing themselves twice a week. About 40% of people in this group lost 5% of their body weight after 6 months, twice as many as in the group that did not receive payment for performing these tasks.
The big winners, however, were those in the third group. They also received the free stuff, but the researchers offered them a more simple and direct bribe: Lose 5% of your weight over 6 months and we’ll pay you. The reward? About $450 on average, and it worked very well, with half this group losing the weight after 6 months. That said, after a year something like a fifth of this group put the weight back on, bringing them in line with the group that was paid to perform tasks. Still, both groups outperformed the control group, which received no money.
The takeaway from this research is pretty obvious. Pay people a fair price to do something, and they’ll do it. This is a lesson that has absolutely no relevance in the modern world. Nope, none whatsoever. We all receive completely fair wages. We all have plenty of money to pay for things. Everything is fine.
More green space, less medicine
Have you heard of the 3-30-300 rule? Proposed by urban forester Cecil Konijnendijk, it’s become the rule of thumb for urban planners and other foresters into getting more green space in populated areas. A recent study has found that people who lived within this 3-30-300 rule had better mental health and less medication use.
If you’re not an urban forester, however, you may not know what the 3-30-300 rule is. But it’s pretty simple, people should be able to see at least three trees from their home, have 30% tree canopy in their neighborhood, and have 300 Spartans to defend against the Persian army.
We may have made that last one up. It’s actually have a green space or park within 300 meters of your home.
In the new study, only 4.7% of people surveyed lived in an area that followed all three rules. About 62% of the surveyed lived with a green space at least 300 meters away, 43% had at least three trees within 15 meters from their home, and a rather pitiful 9% had adequate tree canopy coverage in their neighborhood.
Greater adherence to the 3-30-300 rule was associated with fewer visits to the psychologist, with 8.3% of the participants reporting a psychologist visit in the last year. The data come from a sample of a little over 3,000 Barcelona residents aged 15-97 who were randomly selected to participate in the Barcelona Public Health Agency Survey.
“There is an urgent need to provide citizens with more green space,” said Mark Nieuwenhuijsen, lead author of the study. “We may need to tear out asphalt and plant more trees, which would not only improve health, but also reduce heat island effects and contribute to carbon capture.”
The main goal and message is that more green space is good for everyone. So if you’re feeling a little overwhelmed, take a breather and sit somewhere green. Or call those 300 Spartans and get them to start knocking some buildings down.
Said the toilet to the engineer: Do you hear what I hear?
A mythical hero’s journey took Dorothy along the yellow brick road to find the Wizard of Oz. Huckleberry Finn used a raft to float down the Mississippi River. Luke Skywalker did most of his traveling between planets. For the rest of us, the journey may be just a bit shorter.
Also a bit less heroic. Unless, of course, you’re prepping for a colonoscopy. Yup, we’re headed to the toilet, but not just any toilet. This toilet was the subject of a presentation at the annual meeting of the Acoustical Society of America, titled “The feces thesis: Using machine learning to detect diarrhea,” and that presentation was the hero’s journey of Maia Gatlin, PhD, a research engineer at the Georgia Institute of Technology.
She and her team attached a noninvasive microphone sensor to a toilet, and now they can identify bowel diseases without collecting any identifiable information.
The audio sample of an excretion event is “transformed into a spectrogram, which essentially captures the sound in an image. Different events produce different features in the audio and the spectrogram. For example, urination creates a consistent tone, while defecation may have a singular tone. In contrast, diarrhea is more random,” they explained in the written statement.
They used a machine learning algorithm to classify each spectrogram based on its features. “The algorithm’s performance was tested against data with and without background noises to make sure it was learning the right sound features, regardless of the sensor’s environment,” Dr. Gatlin and associates wrote.
Their goal is to use the toilet sensor in areas where cholera is common to prevent the spread of disease. After that, who knows? “Perhaps someday, our algorithm can be used with existing in-home smart devices to monitor one’s own bowel movements and health!” she suggested.
That would be a heroic toilet indeed.
CRT boosts heart failure survival in extended follow-up
CHICAGO – Extended follow-up of patients with heart failure enrolled in the RAFT trial strengthens the case for starting treatment early with a cardiac resynchronization therapy plus defibrillation (CRT-D) device in appropriate patients.
RAFT, which compared CRT-D with treatment with an implantable cardioverter defibrillator (ICD) alone, showed that the early survival benefit produced by CRT-D during an average 40-month follow-up in the original trial persisted during an additional mean follow-up of about 5 years. This result strengthens the case for starting treatment early with a CRT-D device in appropriate patients with heart failure.
During extended follow-up of more than half of the enrolled patients, out to an average of 7.6 years overall and to an average of 12.9 years among survivors, patients who received a CRT-D device had a significant 21% relative reduction in their rate of all-cause mortality compared with randomized patients who received an ICD and no cardiac resynchronization, John L. Sapp, MD, reported at the American Heart Association scientific sessions.
The primary results of RAFT were first reported in 2010.
This magnitude of a survival benefit among the patients originally randomized to CRT is “dramatic,” given that many of the comparator patients who initially received no CRT likely crossed over to receive a CRT-D device once the initial, randomized 4 years of the study finished, commented Lynne W. Stevenson, MD, director of cardiomyopathy and the Lisa M. Jacobson Professor of Cardiology at Vanderbilt University Medical Center in Nashville, Tenn., who was not involved with the study.
‘CRT can remap heart failure trajectory’
The new findings “strengthen our conviction that CRT can remap the trajectory” of selected patients with heart failure, and that “candidates for CRT should be vigorously identified,” Dr. Stevenson said in an interview.
She also noted that the benefit with extended follow-up was “strikingly parallel” to that seen at 12 years after the addition of an ACE inhibitor for mild heart failure during the 4 years of the landmark SOLVD trial. The new RAFT extended follow-up, as well as the 12-year follow-up of the SOLVD trial, “support the concept that longer follow-up reveals vital information not provided by the relatively short randomized trial period,” she said.
“The new data say ‘don’t delay starting CRT in appropriate patients with heart failure,’ and ‘don’t think of CRT as just a treatment that makes patients feel better.’
“The totality of these data shows that CRT also treats the underlying heart muscle weakness, which helps patients live longer. Previous data showed that patients with left bundle branch block eligible for CRT are unlikely to respond well to the usual, recommended heart medications so it is important to start treatment with CRT-D early,” declared Dr. Stevenson, who cochaired the session where Dr. Sapp gave his report.
RAFT randomized 1,798 patients with New York Heart Association (NYHA) class II or III heart failure, a left ventricular ejection fraction of 30% or less, and an intrinsic QRS duration of at least 120 msec to receive either a CRT-D or ICD device. The study’s primary endpoint was death from any cause or hospitalization for heart failure. After an average 40 months of randomized follow-up, the primary endpoint occurred in 40% of the patients with an ICD and in 33% of those with a CRT-D device, a significant 25% relative reduction linked with CRT-D use. Both endpoint components contributed to the combined result significantly and to about the same extent, and the incremental benefit from CRT-D was significant for patients with NYHA class II heart failure as well as for those with class III.
However, prespecified subgroup analyses showed that the incremental benefit from CRT-D was significantly limited to patients with an intrinsic QRS duration of at least 150 msec, while in those with a duration of 120-149 msec CRT-D had a neutral effect compared with ICD. The same pattern also appeared when the analysis split patients into those with a left bundle branch block, who significantly benefited from CRT-D, but the initial benefit was not apparent in patients with right bundle branch block.
A study subgroup with extended follow-up
The new, extended follow-up analysis presented by Dr. Sapp included 1,050 of the original 1,798 patients (58%) enrolled at any of eight participating Canadian centers that each enrolled at least 100 patients and followed them through the end of 2021 (the full study cohort came from 34 centers, including 10 centers outside Canada). This subgroup included 520 patients randomized to receive CRT-D and 530 who received an ICD. Although this was a post hoc subgroup analysis, the CRT-D and ICD arms matched closely in all measured baseline characteristics.
The prespecified primary outcome of this follow-up analysis was the rate of all-cause mortality. Because of their longer disease trajectory, this pared-down study cohort included many more patients with NYHA class II function, 803, and in this subgroup CRT-D exerted a significant 23% incremental reduction in mortality compared with ICD treatment. CRT-D also produced a 17% relative reduction in long-term mortality among patients with NYHA class III function at baseline, but this point estimate of relative benefit was not significant in this subgroup of just 247 patients, said Dr. Sapp, a cardiologist and professor at Dalhousie University & Nova Scotia Health in Halifax.
Based on the original RAFT results from 2010, as well as on evidence from several other trials, the current heart failure management guideline from the AHA, the American College of Cardiology, and the Heart Failure Society of America give the highest level of recommendation, level 1, for CRT in patients with a left ventricular ejection fraction of 35% or less, sinus rhythm with left bundle branch block, a QRS duration of at least 150 msec, and NYHA class II, III, or ambulatory IV symptoms while on guideline-directed medical therapy.
The guideline also gives class 2a (“can be useful”) or 2b (“may be considered”) recommendation for certain other heart failure patients, including those with a QRS duration of 120-149 msec, a left ventricular ejection fraction as high as 50%, no left bundle branch block, or NYHA class I symptoms.
Don’t wait to start CRT
Although this 2022 guideline, as well as earlier versions that had roughly similar recommendations for CRT for about a decade, have led to “common” use of CRT in appropriate patients in U.S. practice, “it has not been used as much as it should be, in part because there’s been a feeling that CRT mostly treats symptoms and so perhaps you can wait” to start it, said Dr. Stevenson.
The findings from the new, extended follow-up RAFT analysis give increased urgency to starting CRT “as soon as possible” in appropriate patients with heart failure, even before they stabilize on guideline-directed medical therapy, said Dr. Stevenson. She also downplayed any ambiguity in the RAFT findings about optimal medical therapy, which during the RAFT study included traditional triple therapy at a time before treatment with sacubitril/valsartan (Entresto) and sodium-glucose cotransporter 2 (SGLT2) inhibitors became recommended.
“There is no reason to think that these treatments will negate the benefit of CRT for patients with heart failure with reduced ejection fraction and a wide left bundle branch block,” Dr. Stevenson said.
She also believes that the extended follow-up results, which showed clear efficacy for CRT-D in patients with NYHA class II function, support the case for upgrading the current 2b recommendation for using CRT treatment in patients with NYHA class I function and ischemic heart failure to a 2a recommendation regardless of whether or not patients have coronary artery disease. “The difference between class I and class II depends more on a patient’s lifestyle rather than on the severity of their heart failure,” Dr. Stevenson noted. “The RAFT study results encourage us to reexamine the clinical class and timing for CRT” in the current heart failure guideline.
RAFT received partial sponsorship from Medtronic. Dr. Sapp has been a consultant to Abbott, Biosense Webster, Medtronic, and Varian and has received research funding from Abbott and Biosense Webster. Dr. Stevenson had no disclosures.
CHICAGO – Extended follow-up of patients with heart failure enrolled in the RAFT trial strengthens the case for starting treatment early with a cardiac resynchronization therapy plus defibrillation (CRT-D) device in appropriate patients.
RAFT, which compared CRT-D with treatment with an implantable cardioverter defibrillator (ICD) alone, showed that the early survival benefit produced by CRT-D during an average 40-month follow-up in the original trial persisted during an additional mean follow-up of about 5 years. This result strengthens the case for starting treatment early with a CRT-D device in appropriate patients with heart failure.
During extended follow-up of more than half of the enrolled patients, out to an average of 7.6 years overall and to an average of 12.9 years among survivors, patients who received a CRT-D device had a significant 21% relative reduction in their rate of all-cause mortality compared with randomized patients who received an ICD and no cardiac resynchronization, John L. Sapp, MD, reported at the American Heart Association scientific sessions.
The primary results of RAFT were first reported in 2010.
This magnitude of a survival benefit among the patients originally randomized to CRT is “dramatic,” given that many of the comparator patients who initially received no CRT likely crossed over to receive a CRT-D device once the initial, randomized 4 years of the study finished, commented Lynne W. Stevenson, MD, director of cardiomyopathy and the Lisa M. Jacobson Professor of Cardiology at Vanderbilt University Medical Center in Nashville, Tenn., who was not involved with the study.
‘CRT can remap heart failure trajectory’
The new findings “strengthen our conviction that CRT can remap the trajectory” of selected patients with heart failure, and that “candidates for CRT should be vigorously identified,” Dr. Stevenson said in an interview.
She also noted that the benefit with extended follow-up was “strikingly parallel” to that seen at 12 years after the addition of an ACE inhibitor for mild heart failure during the 4 years of the landmark SOLVD trial. The new RAFT extended follow-up, as well as the 12-year follow-up of the SOLVD trial, “support the concept that longer follow-up reveals vital information not provided by the relatively short randomized trial period,” she said.
“The new data say ‘don’t delay starting CRT in appropriate patients with heart failure,’ and ‘don’t think of CRT as just a treatment that makes patients feel better.’
“The totality of these data shows that CRT also treats the underlying heart muscle weakness, which helps patients live longer. Previous data showed that patients with left bundle branch block eligible for CRT are unlikely to respond well to the usual, recommended heart medications so it is important to start treatment with CRT-D early,” declared Dr. Stevenson, who cochaired the session where Dr. Sapp gave his report.
RAFT randomized 1,798 patients with New York Heart Association (NYHA) class II or III heart failure, a left ventricular ejection fraction of 30% or less, and an intrinsic QRS duration of at least 120 msec to receive either a CRT-D or ICD device. The study’s primary endpoint was death from any cause or hospitalization for heart failure. After an average 40 months of randomized follow-up, the primary endpoint occurred in 40% of the patients with an ICD and in 33% of those with a CRT-D device, a significant 25% relative reduction linked with CRT-D use. Both endpoint components contributed to the combined result significantly and to about the same extent, and the incremental benefit from CRT-D was significant for patients with NYHA class II heart failure as well as for those with class III.
However, prespecified subgroup analyses showed that the incremental benefit from CRT-D was significantly limited to patients with an intrinsic QRS duration of at least 150 msec, while in those with a duration of 120-149 msec CRT-D had a neutral effect compared with ICD. The same pattern also appeared when the analysis split patients into those with a left bundle branch block, who significantly benefited from CRT-D, but the initial benefit was not apparent in patients with right bundle branch block.
A study subgroup with extended follow-up
The new, extended follow-up analysis presented by Dr. Sapp included 1,050 of the original 1,798 patients (58%) enrolled at any of eight participating Canadian centers that each enrolled at least 100 patients and followed them through the end of 2021 (the full study cohort came from 34 centers, including 10 centers outside Canada). This subgroup included 520 patients randomized to receive CRT-D and 530 who received an ICD. Although this was a post hoc subgroup analysis, the CRT-D and ICD arms matched closely in all measured baseline characteristics.
The prespecified primary outcome of this follow-up analysis was the rate of all-cause mortality. Because of their longer disease trajectory, this pared-down study cohort included many more patients with NYHA class II function, 803, and in this subgroup CRT-D exerted a significant 23% incremental reduction in mortality compared with ICD treatment. CRT-D also produced a 17% relative reduction in long-term mortality among patients with NYHA class III function at baseline, but this point estimate of relative benefit was not significant in this subgroup of just 247 patients, said Dr. Sapp, a cardiologist and professor at Dalhousie University & Nova Scotia Health in Halifax.
Based on the original RAFT results from 2010, as well as on evidence from several other trials, the current heart failure management guideline from the AHA, the American College of Cardiology, and the Heart Failure Society of America give the highest level of recommendation, level 1, for CRT in patients with a left ventricular ejection fraction of 35% or less, sinus rhythm with left bundle branch block, a QRS duration of at least 150 msec, and NYHA class II, III, or ambulatory IV symptoms while on guideline-directed medical therapy.
The guideline also gives class 2a (“can be useful”) or 2b (“may be considered”) recommendation for certain other heart failure patients, including those with a QRS duration of 120-149 msec, a left ventricular ejection fraction as high as 50%, no left bundle branch block, or NYHA class I symptoms.
Don’t wait to start CRT
Although this 2022 guideline, as well as earlier versions that had roughly similar recommendations for CRT for about a decade, have led to “common” use of CRT in appropriate patients in U.S. practice, “it has not been used as much as it should be, in part because there’s been a feeling that CRT mostly treats symptoms and so perhaps you can wait” to start it, said Dr. Stevenson.
The findings from the new, extended follow-up RAFT analysis give increased urgency to starting CRT “as soon as possible” in appropriate patients with heart failure, even before they stabilize on guideline-directed medical therapy, said Dr. Stevenson. She also downplayed any ambiguity in the RAFT findings about optimal medical therapy, which during the RAFT study included traditional triple therapy at a time before treatment with sacubitril/valsartan (Entresto) and sodium-glucose cotransporter 2 (SGLT2) inhibitors became recommended.
“There is no reason to think that these treatments will negate the benefit of CRT for patients with heart failure with reduced ejection fraction and a wide left bundle branch block,” Dr. Stevenson said.
She also believes that the extended follow-up results, which showed clear efficacy for CRT-D in patients with NYHA class II function, support the case for upgrading the current 2b recommendation for using CRT treatment in patients with NYHA class I function and ischemic heart failure to a 2a recommendation regardless of whether or not patients have coronary artery disease. “The difference between class I and class II depends more on a patient’s lifestyle rather than on the severity of their heart failure,” Dr. Stevenson noted. “The RAFT study results encourage us to reexamine the clinical class and timing for CRT” in the current heart failure guideline.
RAFT received partial sponsorship from Medtronic. Dr. Sapp has been a consultant to Abbott, Biosense Webster, Medtronic, and Varian and has received research funding from Abbott and Biosense Webster. Dr. Stevenson had no disclosures.
CHICAGO – Extended follow-up of patients with heart failure enrolled in the RAFT trial strengthens the case for starting treatment early with a cardiac resynchronization therapy plus defibrillation (CRT-D) device in appropriate patients.
RAFT, which compared CRT-D with treatment with an implantable cardioverter defibrillator (ICD) alone, showed that the early survival benefit produced by CRT-D during an average 40-month follow-up in the original trial persisted during an additional mean follow-up of about 5 years. This result strengthens the case for starting treatment early with a CRT-D device in appropriate patients with heart failure.
During extended follow-up of more than half of the enrolled patients, out to an average of 7.6 years overall and to an average of 12.9 years among survivors, patients who received a CRT-D device had a significant 21% relative reduction in their rate of all-cause mortality compared with randomized patients who received an ICD and no cardiac resynchronization, John L. Sapp, MD, reported at the American Heart Association scientific sessions.
The primary results of RAFT were first reported in 2010.
This magnitude of a survival benefit among the patients originally randomized to CRT is “dramatic,” given that many of the comparator patients who initially received no CRT likely crossed over to receive a CRT-D device once the initial, randomized 4 years of the study finished, commented Lynne W. Stevenson, MD, director of cardiomyopathy and the Lisa M. Jacobson Professor of Cardiology at Vanderbilt University Medical Center in Nashville, Tenn., who was not involved with the study.
‘CRT can remap heart failure trajectory’
The new findings “strengthen our conviction that CRT can remap the trajectory” of selected patients with heart failure, and that “candidates for CRT should be vigorously identified,” Dr. Stevenson said in an interview.
She also noted that the benefit with extended follow-up was “strikingly parallel” to that seen at 12 years after the addition of an ACE inhibitor for mild heart failure during the 4 years of the landmark SOLVD trial. The new RAFT extended follow-up, as well as the 12-year follow-up of the SOLVD trial, “support the concept that longer follow-up reveals vital information not provided by the relatively short randomized trial period,” she said.
“The new data say ‘don’t delay starting CRT in appropriate patients with heart failure,’ and ‘don’t think of CRT as just a treatment that makes patients feel better.’
“The totality of these data shows that CRT also treats the underlying heart muscle weakness, which helps patients live longer. Previous data showed that patients with left bundle branch block eligible for CRT are unlikely to respond well to the usual, recommended heart medications so it is important to start treatment with CRT-D early,” declared Dr. Stevenson, who cochaired the session where Dr. Sapp gave his report.
RAFT randomized 1,798 patients with New York Heart Association (NYHA) class II or III heart failure, a left ventricular ejection fraction of 30% or less, and an intrinsic QRS duration of at least 120 msec to receive either a CRT-D or ICD device. The study’s primary endpoint was death from any cause or hospitalization for heart failure. After an average 40 months of randomized follow-up, the primary endpoint occurred in 40% of the patients with an ICD and in 33% of those with a CRT-D device, a significant 25% relative reduction linked with CRT-D use. Both endpoint components contributed to the combined result significantly and to about the same extent, and the incremental benefit from CRT-D was significant for patients with NYHA class II heart failure as well as for those with class III.
However, prespecified subgroup analyses showed that the incremental benefit from CRT-D was significantly limited to patients with an intrinsic QRS duration of at least 150 msec, while in those with a duration of 120-149 msec CRT-D had a neutral effect compared with ICD. The same pattern also appeared when the analysis split patients into those with a left bundle branch block, who significantly benefited from CRT-D, but the initial benefit was not apparent in patients with right bundle branch block.
A study subgroup with extended follow-up
The new, extended follow-up analysis presented by Dr. Sapp included 1,050 of the original 1,798 patients (58%) enrolled at any of eight participating Canadian centers that each enrolled at least 100 patients and followed them through the end of 2021 (the full study cohort came from 34 centers, including 10 centers outside Canada). This subgroup included 520 patients randomized to receive CRT-D and 530 who received an ICD. Although this was a post hoc subgroup analysis, the CRT-D and ICD arms matched closely in all measured baseline characteristics.
The prespecified primary outcome of this follow-up analysis was the rate of all-cause mortality. Because of their longer disease trajectory, this pared-down study cohort included many more patients with NYHA class II function, 803, and in this subgroup CRT-D exerted a significant 23% incremental reduction in mortality compared with ICD treatment. CRT-D also produced a 17% relative reduction in long-term mortality among patients with NYHA class III function at baseline, but this point estimate of relative benefit was not significant in this subgroup of just 247 patients, said Dr. Sapp, a cardiologist and professor at Dalhousie University & Nova Scotia Health in Halifax.
Based on the original RAFT results from 2010, as well as on evidence from several other trials, the current heart failure management guideline from the AHA, the American College of Cardiology, and the Heart Failure Society of America give the highest level of recommendation, level 1, for CRT in patients with a left ventricular ejection fraction of 35% or less, sinus rhythm with left bundle branch block, a QRS duration of at least 150 msec, and NYHA class II, III, or ambulatory IV symptoms while on guideline-directed medical therapy.
The guideline also gives class 2a (“can be useful”) or 2b (“may be considered”) recommendation for certain other heart failure patients, including those with a QRS duration of 120-149 msec, a left ventricular ejection fraction as high as 50%, no left bundle branch block, or NYHA class I symptoms.
Don’t wait to start CRT
Although this 2022 guideline, as well as earlier versions that had roughly similar recommendations for CRT for about a decade, have led to “common” use of CRT in appropriate patients in U.S. practice, “it has not been used as much as it should be, in part because there’s been a feeling that CRT mostly treats symptoms and so perhaps you can wait” to start it, said Dr. Stevenson.
The findings from the new, extended follow-up RAFT analysis give increased urgency to starting CRT “as soon as possible” in appropriate patients with heart failure, even before they stabilize on guideline-directed medical therapy, said Dr. Stevenson. She also downplayed any ambiguity in the RAFT findings about optimal medical therapy, which during the RAFT study included traditional triple therapy at a time before treatment with sacubitril/valsartan (Entresto) and sodium-glucose cotransporter 2 (SGLT2) inhibitors became recommended.
“There is no reason to think that these treatments will negate the benefit of CRT for patients with heart failure with reduced ejection fraction and a wide left bundle branch block,” Dr. Stevenson said.
She also believes that the extended follow-up results, which showed clear efficacy for CRT-D in patients with NYHA class II function, support the case for upgrading the current 2b recommendation for using CRT treatment in patients with NYHA class I function and ischemic heart failure to a 2a recommendation regardless of whether or not patients have coronary artery disease. “The difference between class I and class II depends more on a patient’s lifestyle rather than on the severity of their heart failure,” Dr. Stevenson noted. “The RAFT study results encourage us to reexamine the clinical class and timing for CRT” in the current heart failure guideline.
RAFT received partial sponsorship from Medtronic. Dr. Sapp has been a consultant to Abbott, Biosense Webster, Medtronic, and Varian and has received research funding from Abbott and Biosense Webster. Dr. Stevenson had no disclosures.
AT AHA 2022
Fungi that cause lung infections now found in most states: Study
Soil-dwelling fungi that can cause lung infections are more widespread than most doctors thought, sometimes leading to missed diagnoses, according to a new study.
Researchers studying fungi-linked lung infections realized that many infections were occurring in places the fungi weren’t thought to exist. They found that maps doctors use to know if the fungi are a threat in their area hadn’t been updated in half a century.
University of California, Davis infectious disease professor George Thompson, MD, said in a commentary published along with the study.
Published in the journal Clinical Infectious Diseases, the study sought to identify illnesses linked to three types of soil fungi in the United States that are known to cause lung infections. They are called histoplasma, blastomyces, and coccidioides, the latter of which causes an illness known as Valley fever, which has been on the rise in California.
Researchers used data for more than 45 million people who use Medicare and found that at least 1 of these 3 fungi are present in 48 of 50 U.S. states and Washington, D.C.
Symptoms after breathing in the fungi spores include fever and cough and can be similar to symptoms of other illnesses, according to the Centers for Disease Control.
The researchers said health care providers need to increase their suspicion for these fungi, which “would likely result in fewer missed diagnoses, fewer diagnostic delays, and improved patient outcomes.”
A version of this article first appeared on WebMD.com.
Soil-dwelling fungi that can cause lung infections are more widespread than most doctors thought, sometimes leading to missed diagnoses, according to a new study.
Researchers studying fungi-linked lung infections realized that many infections were occurring in places the fungi weren’t thought to exist. They found that maps doctors use to know if the fungi are a threat in their area hadn’t been updated in half a century.
University of California, Davis infectious disease professor George Thompson, MD, said in a commentary published along with the study.
Published in the journal Clinical Infectious Diseases, the study sought to identify illnesses linked to three types of soil fungi in the United States that are known to cause lung infections. They are called histoplasma, blastomyces, and coccidioides, the latter of which causes an illness known as Valley fever, which has been on the rise in California.
Researchers used data for more than 45 million people who use Medicare and found that at least 1 of these 3 fungi are present in 48 of 50 U.S. states and Washington, D.C.
Symptoms after breathing in the fungi spores include fever and cough and can be similar to symptoms of other illnesses, according to the Centers for Disease Control.
The researchers said health care providers need to increase their suspicion for these fungi, which “would likely result in fewer missed diagnoses, fewer diagnostic delays, and improved patient outcomes.”
A version of this article first appeared on WebMD.com.
Soil-dwelling fungi that can cause lung infections are more widespread than most doctors thought, sometimes leading to missed diagnoses, according to a new study.
Researchers studying fungi-linked lung infections realized that many infections were occurring in places the fungi weren’t thought to exist. They found that maps doctors use to know if the fungi are a threat in their area hadn’t been updated in half a century.
University of California, Davis infectious disease professor George Thompson, MD, said in a commentary published along with the study.
Published in the journal Clinical Infectious Diseases, the study sought to identify illnesses linked to three types of soil fungi in the United States that are known to cause lung infections. They are called histoplasma, blastomyces, and coccidioides, the latter of which causes an illness known as Valley fever, which has been on the rise in California.
Researchers used data for more than 45 million people who use Medicare and found that at least 1 of these 3 fungi are present in 48 of 50 U.S. states and Washington, D.C.
Symptoms after breathing in the fungi spores include fever and cough and can be similar to symptoms of other illnesses, according to the Centers for Disease Control.
The researchers said health care providers need to increase their suspicion for these fungi, which “would likely result in fewer missed diagnoses, fewer diagnostic delays, and improved patient outcomes.”
A version of this article first appeared on WebMD.com.
FROM CLINICAL INFECTIOUS DISEASE
‘Slugging’: A TikTok skin trend that has some merit
They’ve been around for a while and show no signs of going away: videos on TikTok of people, often teens, slathering their face with petroleum jelly and claiming that it’s transformed their skin, cured their acne, or given them an amazing “glow up.”
TikTok videos mentioning petrolatum increased by 46% and Instagram videos by 93% from 2021 to 2022, reported Gabriel Santos Malave, BA, of the Icahn School of Medicine at Mount Sinai, New York, and William D. James, MD, professor of dermatology, University of Pennsylvania, Philadelphia, in a review of petroleum jelly’s uses recently published in Cutis.
The authors said that after application of a moisturizer.
In a typical demonstration, a dermatologist in the United Kingdom showed how she incorporates slugging into her routine in a TikTok video that’s had more than 1 million views.
Unlike many TikTok trends, slugging may not be entirely bad, say dermatologists.
“I think it’s a great way to keep your skin protected and moisturized, especially in those dry, cold winter months,” said dermatologist Mamina Turegano, MD, in a video posted in February 2022. That TikTok video has had more than 6 million views.
Dr. Turegano, who is in private practice in the New Orleans suburb of Metairie, La., told this news organization that she decided to post about slugging after she’d noticed that the topic was trending. Also, she had tried the technique herself when she was a resident in Washington more than a decade ago.
At the time, Dr. Turegano said that she was aware that “putting petroleum jelly on your face was not a normal thing.” But, given its history of being used in dermatology, she gave it a try and found that it worked well for her dry skin, she said.
Dr. Turegano is one among many dermatologists who have joined TikTok to dispel myths, educate, and inform. It’s important for them to be there “to engage and empower the public to become a better consumer of information out there and take ownership of their skin health,” said Jean McGee, MD, PhD, a dermatologist at Beth Israel Deaconess Medical Center, Boston, and assistant professor of dermatology at Harvard Medical School, also in Boston.
Dr. McGee and colleagues studied TikTok content on slugging and found that by far, videos that were created by health care providers were more educational. Dermatologists who posted were more likely to discuss the risks and benefits, whereas so-called “influencers” rarely posted on the risks, according to the study, published in Clinics in Dermatology.
Slugging is generally safe and effective for those who have a compromised skin barrier or “for those who have sensitive skin and can’t tolerate other products but need some form of moisturization,” said Dr. Turegano.
“Its oil-based nature allows it to seal water in the skin by creating a hydrophobic barrier that decreases transepidermal water loss (TEWL),” write Mr. Malave and Dr. James in Cutis. They note that petrolatum reduces TEWL by 98%, compared with only 20% to 30% for other oil-based moisturizers.
Dermatologists have often recommended a “seal and trap” regimen for dry skin or eczema. It involves a short, lukewarm shower, followed by immediately moisturizing with a petrolatum-based ointment, said Dr. McGee.
This could be safe for the face, but “other variables need to be considered,” including use of other topical medications and other skin care practices, she added.
The concept of double-layering a moisturizer and an occlusive agent can be beneficial but more typically for the hands and feet, where the skin can be severely dry and cracked, said Adam Friedman, MD, professor and chair of dermatology, George Washington University, Washington. “I would not recommend that on the face,” Dr. Friedman told this news organization.
He and other dermatologists warned about the potential for slugging – given petroleum jelly’s occlusive nature – to enhance the action of any topical steroid, retinol, or exfoliating agent.
Muneeb Shah, MD, who practices in Mooresville, N.C., is one of the most popular dermatologists on TikTok, with more than 17 million followers. He also warned in a February 2022 video about potential downsides. “Be careful after using retinol or exfoliating acids because it may actually irritate your skin more,” he says in the video.
“Slugging is awesome for some people but not for others, and not for every night,” said Whitney Bowe, MD, on a TikTok video she posted in July. She recommended it for eczema or really dry skin. Dr. Bowe, who practices with Advanced Dermatology in New York, advised those with acne-prone skin to “skip this trend.”
On a web page aimed at the general public, the American Academy of Dermatology similarly cautioned, “Avoid putting petroleum jelly on your face if you are acne-prone, as this may cause breakouts in some people.”
Acne cure or pore clogger?
And yet, plenty of TikTok users claim that it has improved their acne.
One such user posted a before and after video purporting to show that slugging had almost completely eliminated her acne and prior scarring. Not surprisingly, it has been viewed some 9 million times and got 1.5 million “likes.”
Dr. Friedman notes that it’s theoretically possible – but not likely – that acne could improve by slugging, given that acne basically is a disease of barrier disruption. “The idea here is you have disrupted skin barrier throughout the face regardless of whether you have a pimple in that spot or not, so you need to repair it,” he said. “That’s where I think slugging is somewhat on the right track, because by putting an occlusive agent on the skin, you are restoring the barrier element,” he said.
However, applying a thick, greasy ointment on the face could block pores and cause a backup of sebum and dead skin cells, and it could trap bacteria, he said. “Skin barrier protection and repair is central to acne management, but you need to do it in a safe way,” he said. He noted that that means applying an oil-free moisturizer to damp skin.
Dr. Turegano said she has seen slugging improve acne, but it’s hard to say which people with acne-prone skin would be the best candidates. Those who have used harsh products to treat acne and subsequently experienced worsening acne could potentially benefit, she said.
Even so, she said, “I’d be very cautious in anyone with acne.”
Dr. Friedman, Dr. McGee, and Dr. Turegano reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
They’ve been around for a while and show no signs of going away: videos on TikTok of people, often teens, slathering their face with petroleum jelly and claiming that it’s transformed their skin, cured their acne, or given them an amazing “glow up.”
TikTok videos mentioning petrolatum increased by 46% and Instagram videos by 93% from 2021 to 2022, reported Gabriel Santos Malave, BA, of the Icahn School of Medicine at Mount Sinai, New York, and William D. James, MD, professor of dermatology, University of Pennsylvania, Philadelphia, in a review of petroleum jelly’s uses recently published in Cutis.
The authors said that after application of a moisturizer.
In a typical demonstration, a dermatologist in the United Kingdom showed how she incorporates slugging into her routine in a TikTok video that’s had more than 1 million views.
Unlike many TikTok trends, slugging may not be entirely bad, say dermatologists.
“I think it’s a great way to keep your skin protected and moisturized, especially in those dry, cold winter months,” said dermatologist Mamina Turegano, MD, in a video posted in February 2022. That TikTok video has had more than 6 million views.
Dr. Turegano, who is in private practice in the New Orleans suburb of Metairie, La., told this news organization that she decided to post about slugging after she’d noticed that the topic was trending. Also, she had tried the technique herself when she was a resident in Washington more than a decade ago.
At the time, Dr. Turegano said that she was aware that “putting petroleum jelly on your face was not a normal thing.” But, given its history of being used in dermatology, she gave it a try and found that it worked well for her dry skin, she said.
Dr. Turegano is one among many dermatologists who have joined TikTok to dispel myths, educate, and inform. It’s important for them to be there “to engage and empower the public to become a better consumer of information out there and take ownership of their skin health,” said Jean McGee, MD, PhD, a dermatologist at Beth Israel Deaconess Medical Center, Boston, and assistant professor of dermatology at Harvard Medical School, also in Boston.
Dr. McGee and colleagues studied TikTok content on slugging and found that by far, videos that were created by health care providers were more educational. Dermatologists who posted were more likely to discuss the risks and benefits, whereas so-called “influencers” rarely posted on the risks, according to the study, published in Clinics in Dermatology.
Slugging is generally safe and effective for those who have a compromised skin barrier or “for those who have sensitive skin and can’t tolerate other products but need some form of moisturization,” said Dr. Turegano.
“Its oil-based nature allows it to seal water in the skin by creating a hydrophobic barrier that decreases transepidermal water loss (TEWL),” write Mr. Malave and Dr. James in Cutis. They note that petrolatum reduces TEWL by 98%, compared with only 20% to 30% for other oil-based moisturizers.
Dermatologists have often recommended a “seal and trap” regimen for dry skin or eczema. It involves a short, lukewarm shower, followed by immediately moisturizing with a petrolatum-based ointment, said Dr. McGee.
This could be safe for the face, but “other variables need to be considered,” including use of other topical medications and other skin care practices, she added.
The concept of double-layering a moisturizer and an occlusive agent can be beneficial but more typically for the hands and feet, where the skin can be severely dry and cracked, said Adam Friedman, MD, professor and chair of dermatology, George Washington University, Washington. “I would not recommend that on the face,” Dr. Friedman told this news organization.
He and other dermatologists warned about the potential for slugging – given petroleum jelly’s occlusive nature – to enhance the action of any topical steroid, retinol, or exfoliating agent.
Muneeb Shah, MD, who practices in Mooresville, N.C., is one of the most popular dermatologists on TikTok, with more than 17 million followers. He also warned in a February 2022 video about potential downsides. “Be careful after using retinol or exfoliating acids because it may actually irritate your skin more,” he says in the video.
“Slugging is awesome for some people but not for others, and not for every night,” said Whitney Bowe, MD, on a TikTok video she posted in July. She recommended it for eczema or really dry skin. Dr. Bowe, who practices with Advanced Dermatology in New York, advised those with acne-prone skin to “skip this trend.”
On a web page aimed at the general public, the American Academy of Dermatology similarly cautioned, “Avoid putting petroleum jelly on your face if you are acne-prone, as this may cause breakouts in some people.”
Acne cure or pore clogger?
And yet, plenty of TikTok users claim that it has improved their acne.
One such user posted a before and after video purporting to show that slugging had almost completely eliminated her acne and prior scarring. Not surprisingly, it has been viewed some 9 million times and got 1.5 million “likes.”
Dr. Friedman notes that it’s theoretically possible – but not likely – that acne could improve by slugging, given that acne basically is a disease of barrier disruption. “The idea here is you have disrupted skin barrier throughout the face regardless of whether you have a pimple in that spot or not, so you need to repair it,” he said. “That’s where I think slugging is somewhat on the right track, because by putting an occlusive agent on the skin, you are restoring the barrier element,” he said.
However, applying a thick, greasy ointment on the face could block pores and cause a backup of sebum and dead skin cells, and it could trap bacteria, he said. “Skin barrier protection and repair is central to acne management, but you need to do it in a safe way,” he said. He noted that that means applying an oil-free moisturizer to damp skin.
Dr. Turegano said she has seen slugging improve acne, but it’s hard to say which people with acne-prone skin would be the best candidates. Those who have used harsh products to treat acne and subsequently experienced worsening acne could potentially benefit, she said.
Even so, she said, “I’d be very cautious in anyone with acne.”
Dr. Friedman, Dr. McGee, and Dr. Turegano reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
They’ve been around for a while and show no signs of going away: videos on TikTok of people, often teens, slathering their face with petroleum jelly and claiming that it’s transformed their skin, cured their acne, or given them an amazing “glow up.”
TikTok videos mentioning petrolatum increased by 46% and Instagram videos by 93% from 2021 to 2022, reported Gabriel Santos Malave, BA, of the Icahn School of Medicine at Mount Sinai, New York, and William D. James, MD, professor of dermatology, University of Pennsylvania, Philadelphia, in a review of petroleum jelly’s uses recently published in Cutis.
The authors said that after application of a moisturizer.
In a typical demonstration, a dermatologist in the United Kingdom showed how she incorporates slugging into her routine in a TikTok video that’s had more than 1 million views.
Unlike many TikTok trends, slugging may not be entirely bad, say dermatologists.
“I think it’s a great way to keep your skin protected and moisturized, especially in those dry, cold winter months,” said dermatologist Mamina Turegano, MD, in a video posted in February 2022. That TikTok video has had more than 6 million views.
Dr. Turegano, who is in private practice in the New Orleans suburb of Metairie, La., told this news organization that she decided to post about slugging after she’d noticed that the topic was trending. Also, she had tried the technique herself when she was a resident in Washington more than a decade ago.
At the time, Dr. Turegano said that she was aware that “putting petroleum jelly on your face was not a normal thing.” But, given its history of being used in dermatology, she gave it a try and found that it worked well for her dry skin, she said.
Dr. Turegano is one among many dermatologists who have joined TikTok to dispel myths, educate, and inform. It’s important for them to be there “to engage and empower the public to become a better consumer of information out there and take ownership of their skin health,” said Jean McGee, MD, PhD, a dermatologist at Beth Israel Deaconess Medical Center, Boston, and assistant professor of dermatology at Harvard Medical School, also in Boston.
Dr. McGee and colleagues studied TikTok content on slugging and found that by far, videos that were created by health care providers were more educational. Dermatologists who posted were more likely to discuss the risks and benefits, whereas so-called “influencers” rarely posted on the risks, according to the study, published in Clinics in Dermatology.
Slugging is generally safe and effective for those who have a compromised skin barrier or “for those who have sensitive skin and can’t tolerate other products but need some form of moisturization,” said Dr. Turegano.
“Its oil-based nature allows it to seal water in the skin by creating a hydrophobic barrier that decreases transepidermal water loss (TEWL),” write Mr. Malave and Dr. James in Cutis. They note that petrolatum reduces TEWL by 98%, compared with only 20% to 30% for other oil-based moisturizers.
Dermatologists have often recommended a “seal and trap” regimen for dry skin or eczema. It involves a short, lukewarm shower, followed by immediately moisturizing with a petrolatum-based ointment, said Dr. McGee.
This could be safe for the face, but “other variables need to be considered,” including use of other topical medications and other skin care practices, she added.
The concept of double-layering a moisturizer and an occlusive agent can be beneficial but more typically for the hands and feet, where the skin can be severely dry and cracked, said Adam Friedman, MD, professor and chair of dermatology, George Washington University, Washington. “I would not recommend that on the face,” Dr. Friedman told this news organization.
He and other dermatologists warned about the potential for slugging – given petroleum jelly’s occlusive nature – to enhance the action of any topical steroid, retinol, or exfoliating agent.
Muneeb Shah, MD, who practices in Mooresville, N.C., is one of the most popular dermatologists on TikTok, with more than 17 million followers. He also warned in a February 2022 video about potential downsides. “Be careful after using retinol or exfoliating acids because it may actually irritate your skin more,” he says in the video.
“Slugging is awesome for some people but not for others, and not for every night,” said Whitney Bowe, MD, on a TikTok video she posted in July. She recommended it for eczema or really dry skin. Dr. Bowe, who practices with Advanced Dermatology in New York, advised those with acne-prone skin to “skip this trend.”
On a web page aimed at the general public, the American Academy of Dermatology similarly cautioned, “Avoid putting petroleum jelly on your face if you are acne-prone, as this may cause breakouts in some people.”
Acne cure or pore clogger?
And yet, plenty of TikTok users claim that it has improved their acne.
One such user posted a before and after video purporting to show that slugging had almost completely eliminated her acne and prior scarring. Not surprisingly, it has been viewed some 9 million times and got 1.5 million “likes.”
Dr. Friedman notes that it’s theoretically possible – but not likely – that acne could improve by slugging, given that acne basically is a disease of barrier disruption. “The idea here is you have disrupted skin barrier throughout the face regardless of whether you have a pimple in that spot or not, so you need to repair it,” he said. “That’s where I think slugging is somewhat on the right track, because by putting an occlusive agent on the skin, you are restoring the barrier element,” he said.
However, applying a thick, greasy ointment on the face could block pores and cause a backup of sebum and dead skin cells, and it could trap bacteria, he said. “Skin barrier protection and repair is central to acne management, but you need to do it in a safe way,” he said. He noted that that means applying an oil-free moisturizer to damp skin.
Dr. Turegano said she has seen slugging improve acne, but it’s hard to say which people with acne-prone skin would be the best candidates. Those who have used harsh products to treat acne and subsequently experienced worsening acne could potentially benefit, she said.
Even so, she said, “I’d be very cautious in anyone with acne.”
Dr. Friedman, Dr. McGee, and Dr. Turegano reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Ohio measles outbreak sickens nearly 60 children
None of the children had been fully vaccinated against measles, and 23 of them have been hospitalized, local officials report.
“Measles can be very serious, especially for children under age 5,” Columbus Public Health spokesperson Kelli Newman told CNN.
Nearly all of the infected children are under age 5, with 12 of them being under 1 year old.
“Many children are hospitalized for dehydration,” Ms. Newman told CNN in an email. “Other serious complications also can include pneumonia and neurological conditions such as encephalitis. There’s no way of knowing which children will become so sick they have to be hospitalized. The safest way to protect children from measles is to make sure they are vaccinated with MMR.”
Of the 59 infected children, 56 were unvaccinated and three had been partially vaccinated. The MMR (measles, mumps, and rubella) vaccine is recommended for children beginning at 12 months old, according to the Centers for Disease Control and American Academy of Pediatrics. Two doses are needed to be considered fully vaccinated, and the second dose is usually given between 4 and 6 years old.
Measles “is one of the most infectious agents known to man,” the academy says.
It is so contagious that if one person has it, up to 9 out of 10 people around that person will also become infected if they are not protected, the CDC explains. Measles infection causes a rash and a fever that can spike beyond 104° F. Sometimes, the illness can lead to brain swelling, brain damage, or death.
Last month, the World Health Organization and CDC warned that 40 million children worldwide missed their measles vaccinations in 2021, partly due to pandemic disruptions. The American Academy of Pediatrics also notes that many parents choose not to vaccinate their children due to misinformation.
Infants are at heightened risk because they are too young to be vaccinated.
The academy offered several tips for protecting unvaccinated infants during a measles outbreak:
- Limit your baby’s exposure to crowds, other children, and people with cold symptoms.
- Disinfect objects and surfaces at home regularly, because the measles virus can live on surfaces or suspended in the air for 2 hours.
- If possible, feed your baby breast milk, because it has antibodies to prevent and fight infections.
A version of this article first appeared on WebMD.com.
None of the children had been fully vaccinated against measles, and 23 of them have been hospitalized, local officials report.
“Measles can be very serious, especially for children under age 5,” Columbus Public Health spokesperson Kelli Newman told CNN.
Nearly all of the infected children are under age 5, with 12 of them being under 1 year old.
“Many children are hospitalized for dehydration,” Ms. Newman told CNN in an email. “Other serious complications also can include pneumonia and neurological conditions such as encephalitis. There’s no way of knowing which children will become so sick they have to be hospitalized. The safest way to protect children from measles is to make sure they are vaccinated with MMR.”
Of the 59 infected children, 56 were unvaccinated and three had been partially vaccinated. The MMR (measles, mumps, and rubella) vaccine is recommended for children beginning at 12 months old, according to the Centers for Disease Control and American Academy of Pediatrics. Two doses are needed to be considered fully vaccinated, and the second dose is usually given between 4 and 6 years old.
Measles “is one of the most infectious agents known to man,” the academy says.
It is so contagious that if one person has it, up to 9 out of 10 people around that person will also become infected if they are not protected, the CDC explains. Measles infection causes a rash and a fever that can spike beyond 104° F. Sometimes, the illness can lead to brain swelling, brain damage, or death.
Last month, the World Health Organization and CDC warned that 40 million children worldwide missed their measles vaccinations in 2021, partly due to pandemic disruptions. The American Academy of Pediatrics also notes that many parents choose not to vaccinate their children due to misinformation.
Infants are at heightened risk because they are too young to be vaccinated.
The academy offered several tips for protecting unvaccinated infants during a measles outbreak:
- Limit your baby’s exposure to crowds, other children, and people with cold symptoms.
- Disinfect objects and surfaces at home regularly, because the measles virus can live on surfaces or suspended in the air for 2 hours.
- If possible, feed your baby breast milk, because it has antibodies to prevent and fight infections.
A version of this article first appeared on WebMD.com.
None of the children had been fully vaccinated against measles, and 23 of them have been hospitalized, local officials report.
“Measles can be very serious, especially for children under age 5,” Columbus Public Health spokesperson Kelli Newman told CNN.
Nearly all of the infected children are under age 5, with 12 of them being under 1 year old.
“Many children are hospitalized for dehydration,” Ms. Newman told CNN in an email. “Other serious complications also can include pneumonia and neurological conditions such as encephalitis. There’s no way of knowing which children will become so sick they have to be hospitalized. The safest way to protect children from measles is to make sure they are vaccinated with MMR.”
Of the 59 infected children, 56 were unvaccinated and three had been partially vaccinated. The MMR (measles, mumps, and rubella) vaccine is recommended for children beginning at 12 months old, according to the Centers for Disease Control and American Academy of Pediatrics. Two doses are needed to be considered fully vaccinated, and the second dose is usually given between 4 and 6 years old.
Measles “is one of the most infectious agents known to man,” the academy says.
It is so contagious that if one person has it, up to 9 out of 10 people around that person will also become infected if they are not protected, the CDC explains. Measles infection causes a rash and a fever that can spike beyond 104° F. Sometimes, the illness can lead to brain swelling, brain damage, or death.
Last month, the World Health Organization and CDC warned that 40 million children worldwide missed their measles vaccinations in 2021, partly due to pandemic disruptions. The American Academy of Pediatrics also notes that many parents choose not to vaccinate their children due to misinformation.
Infants are at heightened risk because they are too young to be vaccinated.
The academy offered several tips for protecting unvaccinated infants during a measles outbreak:
- Limit your baby’s exposure to crowds, other children, and people with cold symptoms.
- Disinfect objects and surfaces at home regularly, because the measles virus can live on surfaces or suspended in the air for 2 hours.
- If possible, feed your baby breast milk, because it has antibodies to prevent and fight infections.
A version of this article first appeared on WebMD.com.
A 9-year old female presented with 1 day of fever, fatigue, and sore throat
This condition typically presents in the setting of Streptococcus pyogenes pharyngitis, or strep throat, and is spread via mucosal transfer in close proximity such as classrooms and nurseries. The dermatologic symptoms are a result of the endotoxin produced by S. pyogenes, which is part of the group A Strep bacteria. Clinically, the presentation can be differentiated from an allergic eruption by its relation to acute pharyngitis, insidious onset, and lack of confluence of the lesions. Diagnosis is supported by a throat culture and rapid strep test, although a rapid test lacks reliability in older patients who are less commonly affected and likely to be carriers. First-line treatment is penicillin or amoxicillin, but first-generation cephalosporins, clindamycin, or erythromycin are sufficient if the patient is allergic to penicillins. Prognosis worsens as time between onset and treatment increases, but is overall excellent now with the introduction of antibiotics and improved hygiene.
Scarlet fever is among a list of many common childhood rashes, and it can be difficult to differentiate between these pathologies on clinical presentation. A few notable childhood dermatologic eruptions include erythema infectiosum (fifth disease), roseola (exanthema subitum or sixth disease), and measles. These cases can be distinguished clinically by the age of the patient, distribution, and quality of the symptoms. Laboratory testing may be used to confirm the diagnosis.
Erythema infectiosum is known as fifth disease or slapped-cheek rash because it commonly presents on the cheeks as a pink, maculopapular rash in a reticular pattern. The disease is caused by parvovirus B19 and is accompanied by low fever, malaise, headache, sore throat, and nausea, which precedes the erythematous rash. The facial rash appears first and is followed by patchy eruptions on the extremities. Appearance of the rash typically indicates the patient is no longer contagious, and patients are treated symptomatically with NSAIDs and antihistamines for associated pruritus.
Roseola infantum is commonly caused by human herpesvirus 6 and is usually found in children 3 years and younger. The defining symptom is a high fever, which is paired with a mild cough, runny nose, and diarrhea. A maculopapular rash appears after the fever subsides, starting centrally and spreading outward to the extremities. Although this rash is similar to measles, they can be differentiated by the order of onset. The rash caused by measles begins on the face and mouth (Koplik spots) and moves downward. Additionally, the patient appears generally healthy and the disease is self-limiting in roseola, while patients with measles will appear more ill and require further attention. Measles is caused by the measles virus of the genus Morbillivirus and is highly contagious. It is spread via respiratory route presenting with fever, cough, coryza, and conjunctivitis followed by the rash. Fortunately, the measles vaccine is in widespread use, so cases have declined over the years.
Our patient had a positive strep test. Influenza and coronavirus tests were negative. She was started on daily amoxicillin and the rash resolved within 2 days of taking the antibiotics.
This case and photo were submitted by Lucas Shapiro, BS, Nova Southeastern University, Tampa, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
Allmon A et al.. Am Fam Physician. 2015 Aug 1;92(3):211-6.
Moss WJ. Lancet. 2017 Dec 2;390(10111):2490-502.
Mullins TB and Krishnamurthy K. Roseola Infantum, in “StatPearls.” Treasure Islan, Fla.: StatPearls Publishing, 2022.
Pardo S and Perera TB. Scarlet Fever, in “StatPearls.” Treasure Island, Fla.: StatPearls Publishing, 2022.
This condition typically presents in the setting of Streptococcus pyogenes pharyngitis, or strep throat, and is spread via mucosal transfer in close proximity such as classrooms and nurseries. The dermatologic symptoms are a result of the endotoxin produced by S. pyogenes, which is part of the group A Strep bacteria. Clinically, the presentation can be differentiated from an allergic eruption by its relation to acute pharyngitis, insidious onset, and lack of confluence of the lesions. Diagnosis is supported by a throat culture and rapid strep test, although a rapid test lacks reliability in older patients who are less commonly affected and likely to be carriers. First-line treatment is penicillin or amoxicillin, but first-generation cephalosporins, clindamycin, or erythromycin are sufficient if the patient is allergic to penicillins. Prognosis worsens as time between onset and treatment increases, but is overall excellent now with the introduction of antibiotics and improved hygiene.
Scarlet fever is among a list of many common childhood rashes, and it can be difficult to differentiate between these pathologies on clinical presentation. A few notable childhood dermatologic eruptions include erythema infectiosum (fifth disease), roseola (exanthema subitum or sixth disease), and measles. These cases can be distinguished clinically by the age of the patient, distribution, and quality of the symptoms. Laboratory testing may be used to confirm the diagnosis.
Erythema infectiosum is known as fifth disease or slapped-cheek rash because it commonly presents on the cheeks as a pink, maculopapular rash in a reticular pattern. The disease is caused by parvovirus B19 and is accompanied by low fever, malaise, headache, sore throat, and nausea, which precedes the erythematous rash. The facial rash appears first and is followed by patchy eruptions on the extremities. Appearance of the rash typically indicates the patient is no longer contagious, and patients are treated symptomatically with NSAIDs and antihistamines for associated pruritus.
Roseola infantum is commonly caused by human herpesvirus 6 and is usually found in children 3 years and younger. The defining symptom is a high fever, which is paired with a mild cough, runny nose, and diarrhea. A maculopapular rash appears after the fever subsides, starting centrally and spreading outward to the extremities. Although this rash is similar to measles, they can be differentiated by the order of onset. The rash caused by measles begins on the face and mouth (Koplik spots) and moves downward. Additionally, the patient appears generally healthy and the disease is self-limiting in roseola, while patients with measles will appear more ill and require further attention. Measles is caused by the measles virus of the genus Morbillivirus and is highly contagious. It is spread via respiratory route presenting with fever, cough, coryza, and conjunctivitis followed by the rash. Fortunately, the measles vaccine is in widespread use, so cases have declined over the years.
Our patient had a positive strep test. Influenza and coronavirus tests were negative. She was started on daily amoxicillin and the rash resolved within 2 days of taking the antibiotics.
This case and photo were submitted by Lucas Shapiro, BS, Nova Southeastern University, Tampa, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
Allmon A et al.. Am Fam Physician. 2015 Aug 1;92(3):211-6.
Moss WJ. Lancet. 2017 Dec 2;390(10111):2490-502.
Mullins TB and Krishnamurthy K. Roseola Infantum, in “StatPearls.” Treasure Islan, Fla.: StatPearls Publishing, 2022.
Pardo S and Perera TB. Scarlet Fever, in “StatPearls.” Treasure Island, Fla.: StatPearls Publishing, 2022.
This condition typically presents in the setting of Streptococcus pyogenes pharyngitis, or strep throat, and is spread via mucosal transfer in close proximity such as classrooms and nurseries. The dermatologic symptoms are a result of the endotoxin produced by S. pyogenes, which is part of the group A Strep bacteria. Clinically, the presentation can be differentiated from an allergic eruption by its relation to acute pharyngitis, insidious onset, and lack of confluence of the lesions. Diagnosis is supported by a throat culture and rapid strep test, although a rapid test lacks reliability in older patients who are less commonly affected and likely to be carriers. First-line treatment is penicillin or amoxicillin, but first-generation cephalosporins, clindamycin, or erythromycin are sufficient if the patient is allergic to penicillins. Prognosis worsens as time between onset and treatment increases, but is overall excellent now with the introduction of antibiotics and improved hygiene.
Scarlet fever is among a list of many common childhood rashes, and it can be difficult to differentiate between these pathologies on clinical presentation. A few notable childhood dermatologic eruptions include erythema infectiosum (fifth disease), roseola (exanthema subitum or sixth disease), and measles. These cases can be distinguished clinically by the age of the patient, distribution, and quality of the symptoms. Laboratory testing may be used to confirm the diagnosis.
Erythema infectiosum is known as fifth disease or slapped-cheek rash because it commonly presents on the cheeks as a pink, maculopapular rash in a reticular pattern. The disease is caused by parvovirus B19 and is accompanied by low fever, malaise, headache, sore throat, and nausea, which precedes the erythematous rash. The facial rash appears first and is followed by patchy eruptions on the extremities. Appearance of the rash typically indicates the patient is no longer contagious, and patients are treated symptomatically with NSAIDs and antihistamines for associated pruritus.
Roseola infantum is commonly caused by human herpesvirus 6 and is usually found in children 3 years and younger. The defining symptom is a high fever, which is paired with a mild cough, runny nose, and diarrhea. A maculopapular rash appears after the fever subsides, starting centrally and spreading outward to the extremities. Although this rash is similar to measles, they can be differentiated by the order of onset. The rash caused by measles begins on the face and mouth (Koplik spots) and moves downward. Additionally, the patient appears generally healthy and the disease is self-limiting in roseola, while patients with measles will appear more ill and require further attention. Measles is caused by the measles virus of the genus Morbillivirus and is highly contagious. It is spread via respiratory route presenting with fever, cough, coryza, and conjunctivitis followed by the rash. Fortunately, the measles vaccine is in widespread use, so cases have declined over the years.
Our patient had a positive strep test. Influenza and coronavirus tests were negative. She was started on daily amoxicillin and the rash resolved within 2 days of taking the antibiotics.
This case and photo were submitted by Lucas Shapiro, BS, Nova Southeastern University, Tampa, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
Allmon A et al.. Am Fam Physician. 2015 Aug 1;92(3):211-6.
Moss WJ. Lancet. 2017 Dec 2;390(10111):2490-502.
Mullins TB and Krishnamurthy K. Roseola Infantum, in “StatPearls.” Treasure Islan, Fla.: StatPearls Publishing, 2022.
Pardo S and Perera TB. Scarlet Fever, in “StatPearls.” Treasure Island, Fla.: StatPearls Publishing, 2022.