User login
Obesity interventions tied to colon cancer risk reduction
LAS VEGAS – People with obesity may be able to reduce their risk of colorectal cancer with weight loss surgery or medication, researchers say.
“We need to have conversations with our patients in the clinic and educate them that they have these resources available,” said Aakash Desai, MD, a hospitalist at MetroHealth Medical Center, Cleveland, in an interview with this news organization.
Dr. Desai and colleagues found that sleeve gastrectomy and four medications were associated with a reduced risk of colorectal cancer but Roux-en-Y gastrojejunostomy and orlistat were not.
Coauthor Zryan Shwani, MD, a gastroenterology fellow at Sibley Memorial Hospital, Washington, D.C., presented the findings here at the American College of Gastroenterology (ACG) 2021 Annual Scientific Meeting.
Working with an underserved population with high rates of obesity in northeastern Ohio, the researchers wondered how surgery and medication could affect these patients.
They analyzed data from the IBM Explorys clinical database, which compiles and standardizes data from electronic medical records on about 74 million patients from more than 300 U.S. hospitals. Consistent with previous studies, they determined that patients with obesity in the database were 2.5 times more likely than people with a healthy weight to be diagnosed with colorectal cancer (odds ratio, 2.48; 95% CI, 2.45-2.51).
Zeroing in on people who had weight loss interventions, they included adults aged 18-75 years who had undergone either Roux-en-Y gastrojejunostomy or sleeve gastrectomy, or had taken the medications liraglutide, orlistat, phentermine/topiramate, bupropion/naltrexone, or lorcaserin.
They excluded patients with Lynch syndrome, intestinal polyposis syndrome, a family history of gastrointestinal malignancy, inflammatory bowel disease, or tobacco or alcohol abuse. Patients who had taken one of the weight loss medications and also had type 2 diabetes were excluded. They did not include patients who had undergone gastric banding because it has become less popular.
For the weight loss medication group, they found 117,730 patients who met their criteria. For the surgery group, 43,050 patients met the criteria.
In analyzing the colorectal cancer rates, they included only diagnoses of malignant neoplasms made 2 years after the interventions.
They compared these patients to a control group of 52,540 people matched in age, with a body mass index (BMI) greater than 30 kg/m2 who did not undergo weight loss surgery or take weight loss medication.
Among the 9,370 patients who underwent Roux-en-Y gastrojejunostomy, 50 were diagnosed with colorectal cancer and 400 had benign polyps. Their rate of colorectal cancer was not statistically different from people who didn’t have surgery (OR, 1.09; 95% CI, 0.82-1.43). The rate of benign polyps after Roux-en-Y gastrojejunostomy was greater (OR, 1.72; 95% CI, 1.55-1.90).
On the other hand, among the 33,680 patients who underwent sleeve gastrectomy, 50 were diagnosed with colorectal cancer, a lower rate than in the population who didn’t have surgery (OR, 0.30; 95% CI, 0.22-0.39). Their risk of benign polyps was also reduced (OR, 0.45; 95% CI, 0.40-0.50).
All of the medications were significantly associated with a lower risk of colorectal cancer, except orlistat (OR, 0.94; 95% CI, 0.72-1.25).
The finding on Roux-en-Y gastrojejunostomy agreed with studies from England and Nordic countries showing double the risk of colorectal cancer in those patients but conflicted with a French study showing decreased risk, Dr. Shwani said.
While the study doesn’t establish a reason why Roux-en-Y gastrojejunostomy was less beneficial, other researchers have associated the procedure with biomarkers of inflammation, Dr. Shwani said. “It’s inconsistent, and I don’t think we have a clear answer why.”
As a retrospective analysis, the study could not establish a cause-and-effect relationship between surgery or medication and cancer, or adjust for such factors as diet, exercise, or genes, he acknowledged.
Colorectal cancer is just one outcome to consider when deciding whether to undergo weight loss surgery or take weight loss drugs, said session moderator Mohammad Yaghoobi, MD, an associate professor of medicine at McMaster University, Hamilton, Ont.
“The most important outcome that should be investigated is the survival of the patients after obesity surgery,” he told this news organization. “The second would be the quality of life of those patients. Colon cancer is preventable if you are having regular colonoscopies.”
Other studies have not shown much difference between patients who have weight loss surgery and those who don’t, he added.
The study was funded by Merck. Dr. Desai and Dr. Shwani have reported receiving grant funding from Merck. Dr. Yaghoobi has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LAS VEGAS – People with obesity may be able to reduce their risk of colorectal cancer with weight loss surgery or medication, researchers say.
“We need to have conversations with our patients in the clinic and educate them that they have these resources available,” said Aakash Desai, MD, a hospitalist at MetroHealth Medical Center, Cleveland, in an interview with this news organization.
Dr. Desai and colleagues found that sleeve gastrectomy and four medications were associated with a reduced risk of colorectal cancer but Roux-en-Y gastrojejunostomy and orlistat were not.
Coauthor Zryan Shwani, MD, a gastroenterology fellow at Sibley Memorial Hospital, Washington, D.C., presented the findings here at the American College of Gastroenterology (ACG) 2021 Annual Scientific Meeting.
Working with an underserved population with high rates of obesity in northeastern Ohio, the researchers wondered how surgery and medication could affect these patients.
They analyzed data from the IBM Explorys clinical database, which compiles and standardizes data from electronic medical records on about 74 million patients from more than 300 U.S. hospitals. Consistent with previous studies, they determined that patients with obesity in the database were 2.5 times more likely than people with a healthy weight to be diagnosed with colorectal cancer (odds ratio, 2.48; 95% CI, 2.45-2.51).
Zeroing in on people who had weight loss interventions, they included adults aged 18-75 years who had undergone either Roux-en-Y gastrojejunostomy or sleeve gastrectomy, or had taken the medications liraglutide, orlistat, phentermine/topiramate, bupropion/naltrexone, or lorcaserin.
They excluded patients with Lynch syndrome, intestinal polyposis syndrome, a family history of gastrointestinal malignancy, inflammatory bowel disease, or tobacco or alcohol abuse. Patients who had taken one of the weight loss medications and also had type 2 diabetes were excluded. They did not include patients who had undergone gastric banding because it has become less popular.
For the weight loss medication group, they found 117,730 patients who met their criteria. For the surgery group, 43,050 patients met the criteria.
In analyzing the colorectal cancer rates, they included only diagnoses of malignant neoplasms made 2 years after the interventions.
They compared these patients to a control group of 52,540 people matched in age, with a body mass index (BMI) greater than 30 kg/m2 who did not undergo weight loss surgery or take weight loss medication.
Among the 9,370 patients who underwent Roux-en-Y gastrojejunostomy, 50 were diagnosed with colorectal cancer and 400 had benign polyps. Their rate of colorectal cancer was not statistically different from people who didn’t have surgery (OR, 1.09; 95% CI, 0.82-1.43). The rate of benign polyps after Roux-en-Y gastrojejunostomy was greater (OR, 1.72; 95% CI, 1.55-1.90).
On the other hand, among the 33,680 patients who underwent sleeve gastrectomy, 50 were diagnosed with colorectal cancer, a lower rate than in the population who didn’t have surgery (OR, 0.30; 95% CI, 0.22-0.39). Their risk of benign polyps was also reduced (OR, 0.45; 95% CI, 0.40-0.50).
All of the medications were significantly associated with a lower risk of colorectal cancer, except orlistat (OR, 0.94; 95% CI, 0.72-1.25).
The finding on Roux-en-Y gastrojejunostomy agreed with studies from England and Nordic countries showing double the risk of colorectal cancer in those patients but conflicted with a French study showing decreased risk, Dr. Shwani said.
While the study doesn’t establish a reason why Roux-en-Y gastrojejunostomy was less beneficial, other researchers have associated the procedure with biomarkers of inflammation, Dr. Shwani said. “It’s inconsistent, and I don’t think we have a clear answer why.”
As a retrospective analysis, the study could not establish a cause-and-effect relationship between surgery or medication and cancer, or adjust for such factors as diet, exercise, or genes, he acknowledged.
Colorectal cancer is just one outcome to consider when deciding whether to undergo weight loss surgery or take weight loss drugs, said session moderator Mohammad Yaghoobi, MD, an associate professor of medicine at McMaster University, Hamilton, Ont.
“The most important outcome that should be investigated is the survival of the patients after obesity surgery,” he told this news organization. “The second would be the quality of life of those patients. Colon cancer is preventable if you are having regular colonoscopies.”
Other studies have not shown much difference between patients who have weight loss surgery and those who don’t, he added.
The study was funded by Merck. Dr. Desai and Dr. Shwani have reported receiving grant funding from Merck. Dr. Yaghoobi has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LAS VEGAS – People with obesity may be able to reduce their risk of colorectal cancer with weight loss surgery or medication, researchers say.
“We need to have conversations with our patients in the clinic and educate them that they have these resources available,” said Aakash Desai, MD, a hospitalist at MetroHealth Medical Center, Cleveland, in an interview with this news organization.
Dr. Desai and colleagues found that sleeve gastrectomy and four medications were associated with a reduced risk of colorectal cancer but Roux-en-Y gastrojejunostomy and orlistat were not.
Coauthor Zryan Shwani, MD, a gastroenterology fellow at Sibley Memorial Hospital, Washington, D.C., presented the findings here at the American College of Gastroenterology (ACG) 2021 Annual Scientific Meeting.
Working with an underserved population with high rates of obesity in northeastern Ohio, the researchers wondered how surgery and medication could affect these patients.
They analyzed data from the IBM Explorys clinical database, which compiles and standardizes data from electronic medical records on about 74 million patients from more than 300 U.S. hospitals. Consistent with previous studies, they determined that patients with obesity in the database were 2.5 times more likely than people with a healthy weight to be diagnosed with colorectal cancer (odds ratio, 2.48; 95% CI, 2.45-2.51).
Zeroing in on people who had weight loss interventions, they included adults aged 18-75 years who had undergone either Roux-en-Y gastrojejunostomy or sleeve gastrectomy, or had taken the medications liraglutide, orlistat, phentermine/topiramate, bupropion/naltrexone, or lorcaserin.
They excluded patients with Lynch syndrome, intestinal polyposis syndrome, a family history of gastrointestinal malignancy, inflammatory bowel disease, or tobacco or alcohol abuse. Patients who had taken one of the weight loss medications and also had type 2 diabetes were excluded. They did not include patients who had undergone gastric banding because it has become less popular.
For the weight loss medication group, they found 117,730 patients who met their criteria. For the surgery group, 43,050 patients met the criteria.
In analyzing the colorectal cancer rates, they included only diagnoses of malignant neoplasms made 2 years after the interventions.
They compared these patients to a control group of 52,540 people matched in age, with a body mass index (BMI) greater than 30 kg/m2 who did not undergo weight loss surgery or take weight loss medication.
Among the 9,370 patients who underwent Roux-en-Y gastrojejunostomy, 50 were diagnosed with colorectal cancer and 400 had benign polyps. Their rate of colorectal cancer was not statistically different from people who didn’t have surgery (OR, 1.09; 95% CI, 0.82-1.43). The rate of benign polyps after Roux-en-Y gastrojejunostomy was greater (OR, 1.72; 95% CI, 1.55-1.90).
On the other hand, among the 33,680 patients who underwent sleeve gastrectomy, 50 were diagnosed with colorectal cancer, a lower rate than in the population who didn’t have surgery (OR, 0.30; 95% CI, 0.22-0.39). Their risk of benign polyps was also reduced (OR, 0.45; 95% CI, 0.40-0.50).
All of the medications were significantly associated with a lower risk of colorectal cancer, except orlistat (OR, 0.94; 95% CI, 0.72-1.25).
The finding on Roux-en-Y gastrojejunostomy agreed with studies from England and Nordic countries showing double the risk of colorectal cancer in those patients but conflicted with a French study showing decreased risk, Dr. Shwani said.
While the study doesn’t establish a reason why Roux-en-Y gastrojejunostomy was less beneficial, other researchers have associated the procedure with biomarkers of inflammation, Dr. Shwani said. “It’s inconsistent, and I don’t think we have a clear answer why.”
As a retrospective analysis, the study could not establish a cause-and-effect relationship between surgery or medication and cancer, or adjust for such factors as diet, exercise, or genes, he acknowledged.
Colorectal cancer is just one outcome to consider when deciding whether to undergo weight loss surgery or take weight loss drugs, said session moderator Mohammad Yaghoobi, MD, an associate professor of medicine at McMaster University, Hamilton, Ont.
“The most important outcome that should be investigated is the survival of the patients after obesity surgery,” he told this news organization. “The second would be the quality of life of those patients. Colon cancer is preventable if you are having regular colonoscopies.”
Other studies have not shown much difference between patients who have weight loss surgery and those who don’t, he added.
The study was funded by Merck. Dr. Desai and Dr. Shwani have reported receiving grant funding from Merck. Dr. Yaghoobi has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ACG 2021
Early peanut feeding guidelines still not reaching families
Four years after new infant feeding guidelines were issued to prevent allergies to peanut and other foods, 70% of surveyed parents and caregivers in the United States said they had never heard about the new recommendation.
Food allergies in developed countries have doubled in each of the last decades and now affect 7.6% of U.S. children. About 1 in 50 are allergic to peanut. Data from the 2015 LEAP study and other research has convincingly shown that early, sustained feeding of peanuts, eggs, and other allergens can prevent babies from developing allergies to these foods.
Based on those findings, the National Institute of Allergy and Infectious Diseases (NIAID) updated its feeding guidelines in 2017, urging parents to introduce these foods to babies around 4-6 months of age rather than wait until 1-3 years of age, as previously recommended. The American Academy of Pediatrics approved those guidelines too, and in 2019 changed its own feeding recommendations.
To assess awareness of this new guidance and to what extent these recommendations are being translated into clinical practice, researchers surveyed a demographically representative U.S. sample of 3,062 parents and caregivers with children between 7 months and 3½ years old. The survey was conducted in English and Spanish over the web or by phone.
More than one-third reported that their child’s primary care physician never discussed when to start feeding peanut-containing foods. And among those whose doctors did offer guidance, fewer than 1 in 4 specifically recommended introducing peanut by 6 months of age.
These data show that “despite strong evidence that early introduction of peanut within the first year of life can prevent the development of peanut allergy, this evidence is simply not making its way to parents of infants,” said Christopher Warren, PhD, assistant professor of preventive medicine at the Northwestern University Feinberg School of Medicine, Chicago. Dr. Warren led the study and presented the findings on a poster at this year’s American College of Allergy, Asthma & Immunology annual meeting in New Orleans.
In addition to caregivers, the Northwestern team surveyed U.S. allergists and pediatricians about the new feeding guidelines. Uptake was fairly good among allergists, with 65% reporting full implementation. On the other hand, while most pediatricians seemed familiar with the 2017 recommendations, fewer than one-third said they were following them.
“What’s unique about this challenge is that it’s not just a guideline change – it’s a guideline reversal,” said Wendy Sue Swanson, MD, chief medical officer for SpoonfulONE, a company that makes mix-ins and other products for multi-allergen feeding. After telling families for years to avoid these allergens in early life because food allergies were rising, “it’s harder advice to say, actually, we were wrong. Not only should you not wait, you should get peanut in while your baby’s immune system has this critical moment to learn and develop, and you should keep getting it in,” Dr. Swanson said in an interview.
Making matters worse, pediatricians are time pressed. Typically, at 4- to 6-month-old well-check visits, “they’re talking about sleep and development and feeding and milestones,” said Ruchi Gupta, MD, MPH, professor of pediatrics and medicine at Northwestern Feinberg, who led the allergist and pediatrician analyses.
Another challenge: Guidelines differ depending on the child’s level of food allergy risk, so it’s hard to explain them clearly and quickly. Babies at highest risk – as judged by having severe eczema, egg allergy, or both – should get peanut IgE blood testing and, if negative, begin regular consumption of peanut by 4-6 months. Intermediate-risk babies who have mild-to-moderate eczema are recommended to start peanut-containing foods by 6 months. And for low-risk babies with no eczema or known food allergies, the guidance is simply to introduce peanut-containing foods “in accordance with family preferences and cultural practices.”
As for pediatricians who say it’s hard to distinguish mild-to-moderate from severe eczema, “any eczema puts you at some risk,” Dr. Gupta told this news organization. “If they’ve required steroid creams to clear up their skin, or if you look at their skin, and you think it’s severe, don’t hesitate. Go ahead and draw the IgE and send them to an allergist.”
Australia, which has the highest rate of confirmed food allergy, has had more success implementing early feeding guidelines, said Dr. Swanson. Unlike the United States’ tiered approach, she said, they “had a national guideline that very crisply, years ago, told parents what to do.” Australia also has nurse educators that follow up with new moms to make sure they understand and follow the recommendations.
Dr. Gupta receives research support from the National Institutes of Health, Food Allergy Research and Education, the Melchiorre Family Foundation, the Sunshine Charitable Foundation, the Walder Foundation, the UnitedHealth Group, Thermo Fisher Scientific, and Genentech. She serves as a medical consultant/advisor for Genentech, Novartis, and Food Allergy Research and Education. Dr. Swanson serves as chief medical officer for SpoonfulONE.
A version of this article first appeared on Medscape.com.
Four years after new infant feeding guidelines were issued to prevent allergies to peanut and other foods, 70% of surveyed parents and caregivers in the United States said they had never heard about the new recommendation.
Food allergies in developed countries have doubled in each of the last decades and now affect 7.6% of U.S. children. About 1 in 50 are allergic to peanut. Data from the 2015 LEAP study and other research has convincingly shown that early, sustained feeding of peanuts, eggs, and other allergens can prevent babies from developing allergies to these foods.
Based on those findings, the National Institute of Allergy and Infectious Diseases (NIAID) updated its feeding guidelines in 2017, urging parents to introduce these foods to babies around 4-6 months of age rather than wait until 1-3 years of age, as previously recommended. The American Academy of Pediatrics approved those guidelines too, and in 2019 changed its own feeding recommendations.
To assess awareness of this new guidance and to what extent these recommendations are being translated into clinical practice, researchers surveyed a demographically representative U.S. sample of 3,062 parents and caregivers with children between 7 months and 3½ years old. The survey was conducted in English and Spanish over the web or by phone.
More than one-third reported that their child’s primary care physician never discussed when to start feeding peanut-containing foods. And among those whose doctors did offer guidance, fewer than 1 in 4 specifically recommended introducing peanut by 6 months of age.
These data show that “despite strong evidence that early introduction of peanut within the first year of life can prevent the development of peanut allergy, this evidence is simply not making its way to parents of infants,” said Christopher Warren, PhD, assistant professor of preventive medicine at the Northwestern University Feinberg School of Medicine, Chicago. Dr. Warren led the study and presented the findings on a poster at this year’s American College of Allergy, Asthma & Immunology annual meeting in New Orleans.
In addition to caregivers, the Northwestern team surveyed U.S. allergists and pediatricians about the new feeding guidelines. Uptake was fairly good among allergists, with 65% reporting full implementation. On the other hand, while most pediatricians seemed familiar with the 2017 recommendations, fewer than one-third said they were following them.
“What’s unique about this challenge is that it’s not just a guideline change – it’s a guideline reversal,” said Wendy Sue Swanson, MD, chief medical officer for SpoonfulONE, a company that makes mix-ins and other products for multi-allergen feeding. After telling families for years to avoid these allergens in early life because food allergies were rising, “it’s harder advice to say, actually, we were wrong. Not only should you not wait, you should get peanut in while your baby’s immune system has this critical moment to learn and develop, and you should keep getting it in,” Dr. Swanson said in an interview.
Making matters worse, pediatricians are time pressed. Typically, at 4- to 6-month-old well-check visits, “they’re talking about sleep and development and feeding and milestones,” said Ruchi Gupta, MD, MPH, professor of pediatrics and medicine at Northwestern Feinberg, who led the allergist and pediatrician analyses.
Another challenge: Guidelines differ depending on the child’s level of food allergy risk, so it’s hard to explain them clearly and quickly. Babies at highest risk – as judged by having severe eczema, egg allergy, or both – should get peanut IgE blood testing and, if negative, begin regular consumption of peanut by 4-6 months. Intermediate-risk babies who have mild-to-moderate eczema are recommended to start peanut-containing foods by 6 months. And for low-risk babies with no eczema or known food allergies, the guidance is simply to introduce peanut-containing foods “in accordance with family preferences and cultural practices.”
As for pediatricians who say it’s hard to distinguish mild-to-moderate from severe eczema, “any eczema puts you at some risk,” Dr. Gupta told this news organization. “If they’ve required steroid creams to clear up their skin, or if you look at their skin, and you think it’s severe, don’t hesitate. Go ahead and draw the IgE and send them to an allergist.”
Australia, which has the highest rate of confirmed food allergy, has had more success implementing early feeding guidelines, said Dr. Swanson. Unlike the United States’ tiered approach, she said, they “had a national guideline that very crisply, years ago, told parents what to do.” Australia also has nurse educators that follow up with new moms to make sure they understand and follow the recommendations.
Dr. Gupta receives research support from the National Institutes of Health, Food Allergy Research and Education, the Melchiorre Family Foundation, the Sunshine Charitable Foundation, the Walder Foundation, the UnitedHealth Group, Thermo Fisher Scientific, and Genentech. She serves as a medical consultant/advisor for Genentech, Novartis, and Food Allergy Research and Education. Dr. Swanson serves as chief medical officer for SpoonfulONE.
A version of this article first appeared on Medscape.com.
Four years after new infant feeding guidelines were issued to prevent allergies to peanut and other foods, 70% of surveyed parents and caregivers in the United States said they had never heard about the new recommendation.
Food allergies in developed countries have doubled in each of the last decades and now affect 7.6% of U.S. children. About 1 in 50 are allergic to peanut. Data from the 2015 LEAP study and other research has convincingly shown that early, sustained feeding of peanuts, eggs, and other allergens can prevent babies from developing allergies to these foods.
Based on those findings, the National Institute of Allergy and Infectious Diseases (NIAID) updated its feeding guidelines in 2017, urging parents to introduce these foods to babies around 4-6 months of age rather than wait until 1-3 years of age, as previously recommended. The American Academy of Pediatrics approved those guidelines too, and in 2019 changed its own feeding recommendations.
To assess awareness of this new guidance and to what extent these recommendations are being translated into clinical practice, researchers surveyed a demographically representative U.S. sample of 3,062 parents and caregivers with children between 7 months and 3½ years old. The survey was conducted in English and Spanish over the web or by phone.
More than one-third reported that their child’s primary care physician never discussed when to start feeding peanut-containing foods. And among those whose doctors did offer guidance, fewer than 1 in 4 specifically recommended introducing peanut by 6 months of age.
These data show that “despite strong evidence that early introduction of peanut within the first year of life can prevent the development of peanut allergy, this evidence is simply not making its way to parents of infants,” said Christopher Warren, PhD, assistant professor of preventive medicine at the Northwestern University Feinberg School of Medicine, Chicago. Dr. Warren led the study and presented the findings on a poster at this year’s American College of Allergy, Asthma & Immunology annual meeting in New Orleans.
In addition to caregivers, the Northwestern team surveyed U.S. allergists and pediatricians about the new feeding guidelines. Uptake was fairly good among allergists, with 65% reporting full implementation. On the other hand, while most pediatricians seemed familiar with the 2017 recommendations, fewer than one-third said they were following them.
“What’s unique about this challenge is that it’s not just a guideline change – it’s a guideline reversal,” said Wendy Sue Swanson, MD, chief medical officer for SpoonfulONE, a company that makes mix-ins and other products for multi-allergen feeding. After telling families for years to avoid these allergens in early life because food allergies were rising, “it’s harder advice to say, actually, we were wrong. Not only should you not wait, you should get peanut in while your baby’s immune system has this critical moment to learn and develop, and you should keep getting it in,” Dr. Swanson said in an interview.
Making matters worse, pediatricians are time pressed. Typically, at 4- to 6-month-old well-check visits, “they’re talking about sleep and development and feeding and milestones,” said Ruchi Gupta, MD, MPH, professor of pediatrics and medicine at Northwestern Feinberg, who led the allergist and pediatrician analyses.
Another challenge: Guidelines differ depending on the child’s level of food allergy risk, so it’s hard to explain them clearly and quickly. Babies at highest risk – as judged by having severe eczema, egg allergy, or both – should get peanut IgE blood testing and, if negative, begin regular consumption of peanut by 4-6 months. Intermediate-risk babies who have mild-to-moderate eczema are recommended to start peanut-containing foods by 6 months. And for low-risk babies with no eczema or known food allergies, the guidance is simply to introduce peanut-containing foods “in accordance with family preferences and cultural practices.”
As for pediatricians who say it’s hard to distinguish mild-to-moderate from severe eczema, “any eczema puts you at some risk,” Dr. Gupta told this news organization. “If they’ve required steroid creams to clear up their skin, or if you look at their skin, and you think it’s severe, don’t hesitate. Go ahead and draw the IgE and send them to an allergist.”
Australia, which has the highest rate of confirmed food allergy, has had more success implementing early feeding guidelines, said Dr. Swanson. Unlike the United States’ tiered approach, she said, they “had a national guideline that very crisply, years ago, told parents what to do.” Australia also has nurse educators that follow up with new moms to make sure they understand and follow the recommendations.
Dr. Gupta receives research support from the National Institutes of Health, Food Allergy Research and Education, the Melchiorre Family Foundation, the Sunshine Charitable Foundation, the Walder Foundation, the UnitedHealth Group, Thermo Fisher Scientific, and Genentech. She serves as a medical consultant/advisor for Genentech, Novartis, and Food Allergy Research and Education. Dr. Swanson serves as chief medical officer for SpoonfulONE.
A version of this article first appeared on Medscape.com.
FAVOR III China: QFR-guided PCI shows advantage over angiography
Percutaneous coronary intervention (PCI) guided by quantitative flow ratio (QFR) lesion assessment provided better clinical outcomes than visual assessment of the angiogram in the sham-controlled FAVOR III China study.
PCI success rates were about 95% with both strategies; however, QFR guidance was associated with fewer major adverse cardiac events (MACE) at 1 year, use of fewer stents, less contrast medium exposure, and fewer procedural complications.
“The simplicity and safety of QFR compared with wire-based physiologic measurements should facilitate the adoption of physiologic lesion assessment into routine clinical practice,” co–primary investigator Bo Xu, MBBS, Fuwai Hospital, Beijing, said.
The results were presented at Transcatheter Cardiovascular Therapeutics (TCT) 2021, held online and in Orlando, and published simultaneously in The Lancet.
Although pressure wire–based physiological assessment with fractional flow reserve (FFR) and instantaneous wave-free ratio (IFR) more accurately identify flow-limiting lesions than standard angiography and have been shown to improve outcomes after PCI, the authors note that it’s underused in practice because of prolonged procedural time, potential pressure wire complications, and side effects from hyperemic agents.
QFR, however, is derived from 3-dimensional coronary artery reconstruction and computational fluid dynamics from the angiogram, so FFR can be estimated without the need for a pressure wire or hyperemic drugs.
FAVOR III China was designed statistically for superiority and enrolled 3,847 patients with stable or unstable angina or a myocardial infarction (MI) at least 72 hours before screening if they had at least one coronary lesion with a diameter stenosis of 50% to 90% and a reference vessel diameter of at least 2.5 mm. The intention-to-treat population included 3,825 patients (mean age, 62.7 years; 29.4% female).
In the QFR group, QFR was measured in all coronary arteries with a lesion but PCI performed only in lesions with a QFR of at least 0.80 or diameter stenosis greater than 90%. Two angiographic imaging runs were taken and the data transmitted to the AngioPlus system (Pulse Medical Imaging Technology) by a local network of sites for QFR calculation.
PCI in the angiography-guided group was performed on the basis of visual angiographic assessment only. A 10-minute delay was used in both groups to preserve masking.
The primary endpoint of 1-year MACE, a composite of all-cause death, MI, or ischemia-driven revascularization, occurred in 5.8% of the QFR-guided group and 8.8% of the angiography-guided group (hazard ratio, 0.65; 95% CI, 0.51-0.83; P = .0004).
The curves separated within 48 hours, driven largely by fewer MIs (3.4% vs. 5.7%; P = .0008) and ischemia-driven revascularizations (2.0% vs. 3.1%; P = .0078) in the QFR-guided group, Mr. Xu said.
The major secondary endpoint of MACE excluding periprocedural MI occurred in 3.1% of QFR-guided patients and 4.8% of angiography-guided patients (HR, 0.64; 95% CI, 0.46-0.89; P = .0073).
The prerandomization revascularization plan was changed in 23.3% of patients with QFR and only 6.2% in the angiography group (P < .0001), mainly due to deferral of treatment of at least one vessel originally planned for PCI (19.6% vs. 5.2%; P < .0001).
“I think in the next guideline they will change the recommendation, not just to include FFR and IFR, but also to include QFR,” Giuseppe Tarantini, MD, PhD, University of Padua, Italy, said during a press briefing on the study.
“This is a milestone in our community, not only because it is easier to use compared to the other lesion-specific indexes like FFR, IFR, but also for the need to expand the use of physiology in the setting of interventional cardiology,” he added.
In an accompanying commentary, Robert A. Byrne, MBBCh, PhD, and Laurna McGovern, MBBCh, both from the Cardiovascular Research Institute Dublin, say the results are “relevant for cardiovascular disease researchers and clinicians and an important step forward for the field of angiography-derived flow measurements for guidance of PCI.”
They point out, however, that the control group did not receive pressure wire–guided PCI, which is the standard of care in contemporary practice and out of step with clinical practice guidelines, thus limiting external validity.
They also note that experiences to date suggest that up to 20% of patients may be unsuitable for the algorithm analysis because of coronary anatomy, presence of overlapping vessels, and insufficient image quality.
Commenting for this news organization, David E. Kandzari, MD, chief of the Piedmont Heart Institute, Atlanta, said “the technology isn’t readily available in catheterization labs today. Could it be assimilated into the cath labs at one point in the near term? I think absolutely, and that would be a welcome addition to expedite the procedure itself.”
Nevertheless, he said the results “need to be externally validated too, with what is the gold standard today of FFR in a larger experience.”
Session moderator Gregg W. Stone, MD, Icahn School of Medicine at Mount Sinai, New York, said FAVOR III China has “advanced our knowledge” but pointed out that the ongoing randomized FAVOR III Europe Japan study is directly comparing QFR with invasive pressure-wire assessed FFR. The estimated primary completion date for that study is Dec. 31.
The study was supported by grants from the Beijing Municipal Science and Technology Commission, Chinese Academy of Medical Sciences, and the National Clinical Research Center for Cardiovascular Diseases, Fuwai Hospital. Dr. Byrne reported institutional research or educational funding from Abbott Vascular, Biosensors, Biotronik, and Boston Scientific. Ms. McGovern has disclosed no relevant financial relationships. Dr. Kandzari reported minor consulting honoraria from the interventional device industry and institutional research grant support.
A version of this article first appeared on Medscape.com.
Percutaneous coronary intervention (PCI) guided by quantitative flow ratio (QFR) lesion assessment provided better clinical outcomes than visual assessment of the angiogram in the sham-controlled FAVOR III China study.
PCI success rates were about 95% with both strategies; however, QFR guidance was associated with fewer major adverse cardiac events (MACE) at 1 year, use of fewer stents, less contrast medium exposure, and fewer procedural complications.
“The simplicity and safety of QFR compared with wire-based physiologic measurements should facilitate the adoption of physiologic lesion assessment into routine clinical practice,” co–primary investigator Bo Xu, MBBS, Fuwai Hospital, Beijing, said.
The results were presented at Transcatheter Cardiovascular Therapeutics (TCT) 2021, held online and in Orlando, and published simultaneously in The Lancet.
Although pressure wire–based physiological assessment with fractional flow reserve (FFR) and instantaneous wave-free ratio (IFR) more accurately identify flow-limiting lesions than standard angiography and have been shown to improve outcomes after PCI, the authors note that it’s underused in practice because of prolonged procedural time, potential pressure wire complications, and side effects from hyperemic agents.
QFR, however, is derived from 3-dimensional coronary artery reconstruction and computational fluid dynamics from the angiogram, so FFR can be estimated without the need for a pressure wire or hyperemic drugs.
FAVOR III China was designed statistically for superiority and enrolled 3,847 patients with stable or unstable angina or a myocardial infarction (MI) at least 72 hours before screening if they had at least one coronary lesion with a diameter stenosis of 50% to 90% and a reference vessel diameter of at least 2.5 mm. The intention-to-treat population included 3,825 patients (mean age, 62.7 years; 29.4% female).
In the QFR group, QFR was measured in all coronary arteries with a lesion but PCI performed only in lesions with a QFR of at least 0.80 or diameter stenosis greater than 90%. Two angiographic imaging runs were taken and the data transmitted to the AngioPlus system (Pulse Medical Imaging Technology) by a local network of sites for QFR calculation.
PCI in the angiography-guided group was performed on the basis of visual angiographic assessment only. A 10-minute delay was used in both groups to preserve masking.
The primary endpoint of 1-year MACE, a composite of all-cause death, MI, or ischemia-driven revascularization, occurred in 5.8% of the QFR-guided group and 8.8% of the angiography-guided group (hazard ratio, 0.65; 95% CI, 0.51-0.83; P = .0004).
The curves separated within 48 hours, driven largely by fewer MIs (3.4% vs. 5.7%; P = .0008) and ischemia-driven revascularizations (2.0% vs. 3.1%; P = .0078) in the QFR-guided group, Mr. Xu said.
The major secondary endpoint of MACE excluding periprocedural MI occurred in 3.1% of QFR-guided patients and 4.8% of angiography-guided patients (HR, 0.64; 95% CI, 0.46-0.89; P = .0073).
The prerandomization revascularization plan was changed in 23.3% of patients with QFR and only 6.2% in the angiography group (P < .0001), mainly due to deferral of treatment of at least one vessel originally planned for PCI (19.6% vs. 5.2%; P < .0001).
“I think in the next guideline they will change the recommendation, not just to include FFR and IFR, but also to include QFR,” Giuseppe Tarantini, MD, PhD, University of Padua, Italy, said during a press briefing on the study.
“This is a milestone in our community, not only because it is easier to use compared to the other lesion-specific indexes like FFR, IFR, but also for the need to expand the use of physiology in the setting of interventional cardiology,” he added.
In an accompanying commentary, Robert A. Byrne, MBBCh, PhD, and Laurna McGovern, MBBCh, both from the Cardiovascular Research Institute Dublin, say the results are “relevant for cardiovascular disease researchers and clinicians and an important step forward for the field of angiography-derived flow measurements for guidance of PCI.”
They point out, however, that the control group did not receive pressure wire–guided PCI, which is the standard of care in contemporary practice and out of step with clinical practice guidelines, thus limiting external validity.
They also note that experiences to date suggest that up to 20% of patients may be unsuitable for the algorithm analysis because of coronary anatomy, presence of overlapping vessels, and insufficient image quality.
Commenting for this news organization, David E. Kandzari, MD, chief of the Piedmont Heart Institute, Atlanta, said “the technology isn’t readily available in catheterization labs today. Could it be assimilated into the cath labs at one point in the near term? I think absolutely, and that would be a welcome addition to expedite the procedure itself.”
Nevertheless, he said the results “need to be externally validated too, with what is the gold standard today of FFR in a larger experience.”
Session moderator Gregg W. Stone, MD, Icahn School of Medicine at Mount Sinai, New York, said FAVOR III China has “advanced our knowledge” but pointed out that the ongoing randomized FAVOR III Europe Japan study is directly comparing QFR with invasive pressure-wire assessed FFR. The estimated primary completion date for that study is Dec. 31.
The study was supported by grants from the Beijing Municipal Science and Technology Commission, Chinese Academy of Medical Sciences, and the National Clinical Research Center for Cardiovascular Diseases, Fuwai Hospital. Dr. Byrne reported institutional research or educational funding from Abbott Vascular, Biosensors, Biotronik, and Boston Scientific. Ms. McGovern has disclosed no relevant financial relationships. Dr. Kandzari reported minor consulting honoraria from the interventional device industry and institutional research grant support.
A version of this article first appeared on Medscape.com.
Percutaneous coronary intervention (PCI) guided by quantitative flow ratio (QFR) lesion assessment provided better clinical outcomes than visual assessment of the angiogram in the sham-controlled FAVOR III China study.
PCI success rates were about 95% with both strategies; however, QFR guidance was associated with fewer major adverse cardiac events (MACE) at 1 year, use of fewer stents, less contrast medium exposure, and fewer procedural complications.
“The simplicity and safety of QFR compared with wire-based physiologic measurements should facilitate the adoption of physiologic lesion assessment into routine clinical practice,” co–primary investigator Bo Xu, MBBS, Fuwai Hospital, Beijing, said.
The results were presented at Transcatheter Cardiovascular Therapeutics (TCT) 2021, held online and in Orlando, and published simultaneously in The Lancet.
Although pressure wire–based physiological assessment with fractional flow reserve (FFR) and instantaneous wave-free ratio (IFR) more accurately identify flow-limiting lesions than standard angiography and have been shown to improve outcomes after PCI, the authors note that it’s underused in practice because of prolonged procedural time, potential pressure wire complications, and side effects from hyperemic agents.
QFR, however, is derived from 3-dimensional coronary artery reconstruction and computational fluid dynamics from the angiogram, so FFR can be estimated without the need for a pressure wire or hyperemic drugs.
FAVOR III China was designed statistically for superiority and enrolled 3,847 patients with stable or unstable angina or a myocardial infarction (MI) at least 72 hours before screening if they had at least one coronary lesion with a diameter stenosis of 50% to 90% and a reference vessel diameter of at least 2.5 mm. The intention-to-treat population included 3,825 patients (mean age, 62.7 years; 29.4% female).
In the QFR group, QFR was measured in all coronary arteries with a lesion but PCI performed only in lesions with a QFR of at least 0.80 or diameter stenosis greater than 90%. Two angiographic imaging runs were taken and the data transmitted to the AngioPlus system (Pulse Medical Imaging Technology) by a local network of sites for QFR calculation.
PCI in the angiography-guided group was performed on the basis of visual angiographic assessment only. A 10-minute delay was used in both groups to preserve masking.
The primary endpoint of 1-year MACE, a composite of all-cause death, MI, or ischemia-driven revascularization, occurred in 5.8% of the QFR-guided group and 8.8% of the angiography-guided group (hazard ratio, 0.65; 95% CI, 0.51-0.83; P = .0004).
The curves separated within 48 hours, driven largely by fewer MIs (3.4% vs. 5.7%; P = .0008) and ischemia-driven revascularizations (2.0% vs. 3.1%; P = .0078) in the QFR-guided group, Mr. Xu said.
The major secondary endpoint of MACE excluding periprocedural MI occurred in 3.1% of QFR-guided patients and 4.8% of angiography-guided patients (HR, 0.64; 95% CI, 0.46-0.89; P = .0073).
The prerandomization revascularization plan was changed in 23.3% of patients with QFR and only 6.2% in the angiography group (P < .0001), mainly due to deferral of treatment of at least one vessel originally planned for PCI (19.6% vs. 5.2%; P < .0001).
“I think in the next guideline they will change the recommendation, not just to include FFR and IFR, but also to include QFR,” Giuseppe Tarantini, MD, PhD, University of Padua, Italy, said during a press briefing on the study.
“This is a milestone in our community, not only because it is easier to use compared to the other lesion-specific indexes like FFR, IFR, but also for the need to expand the use of physiology in the setting of interventional cardiology,” he added.
In an accompanying commentary, Robert A. Byrne, MBBCh, PhD, and Laurna McGovern, MBBCh, both from the Cardiovascular Research Institute Dublin, say the results are “relevant for cardiovascular disease researchers and clinicians and an important step forward for the field of angiography-derived flow measurements for guidance of PCI.”
They point out, however, that the control group did not receive pressure wire–guided PCI, which is the standard of care in contemporary practice and out of step with clinical practice guidelines, thus limiting external validity.
They also note that experiences to date suggest that up to 20% of patients may be unsuitable for the algorithm analysis because of coronary anatomy, presence of overlapping vessels, and insufficient image quality.
Commenting for this news organization, David E. Kandzari, MD, chief of the Piedmont Heart Institute, Atlanta, said “the technology isn’t readily available in catheterization labs today. Could it be assimilated into the cath labs at one point in the near term? I think absolutely, and that would be a welcome addition to expedite the procedure itself.”
Nevertheless, he said the results “need to be externally validated too, with what is the gold standard today of FFR in a larger experience.”
Session moderator Gregg W. Stone, MD, Icahn School of Medicine at Mount Sinai, New York, said FAVOR III China has “advanced our knowledge” but pointed out that the ongoing randomized FAVOR III Europe Japan study is directly comparing QFR with invasive pressure-wire assessed FFR. The estimated primary completion date for that study is Dec. 31.
The study was supported by grants from the Beijing Municipal Science and Technology Commission, Chinese Academy of Medical Sciences, and the National Clinical Research Center for Cardiovascular Diseases, Fuwai Hospital. Dr. Byrne reported institutional research or educational funding from Abbott Vascular, Biosensors, Biotronik, and Boston Scientific. Ms. McGovern has disclosed no relevant financial relationships. Dr. Kandzari reported minor consulting honoraria from the interventional device industry and institutional research grant support.
A version of this article first appeared on Medscape.com.
Tolerability doesn’t explain why kids do better than adults on ALL regimens
The study team found that “an intensive pediatric ALL induction protocol can be delivered in an AYA [adolescent and young adult] cohort in a similar time frame to a pediatric population, suggesting that the inferior outcomes seen in AYA patients are more likely related to the biology of AYA ALL rather than intolerance of more intensive therapy,” said investigators led by Matthew Greenwood, MBBS, director of the stem cell transplant at the Royal North Shore Hospital, outside of Sydney
It’s been a long-standing question why intensive ALL regimens, which can be curative in children, don’t work as well in adolescents and young adults.
To see if tolerability and lack of adherence were issues, the investigators compared the treatment time lines of 82 AYA subjects with a median age of 22 years to the time lines of 608 children aged 1-17 years who were treated with the same intensive regimen (the ANZCHOG Study 8 protocol).
Induction/consolidation was equally deliverable in both populations. In the AYA group, 41.5% of subjects started the next phase of treatment – protocol M or high-risk (HR) therapy based on minimal residual disease (MRD) response to initial treatment – by day 94 versus 39.3% in the previous pediatric study (P = 0.77). The median time to protocol M/HR treatment was 96 days in AYAs and 98 days in children (P = .80).
About 52% of AYA subjects proceeded to HR therapy following induction/consolidation, versus just 10.7% in the pediatric study.
The investigators also found that a body mass index at or above 30 kg/m2 and the presence of MRD were both associated with worse disease-free and overall survival. “By addressing the factors predicting poorer outcomes from this study, we hope to significantly improve the outcomes for patients,” they said.
They noted that their work is the first to “report of the safety and efficacy of an MRD-stratified approach utilizing [Berlin-Frankfurt-Munich] HR therapy in an AYA cohort and show that this is a moderately efficacious strategy in patients who would otherwise be considered at high risk of relapse and death.”
Over a median follow-up of 44 months, estimated 3-year disease-free survival was 72.8% and estimated 3-year overall survival 74.9% in the AYA population.
The work was funded by the Australasian Leukaemia and Lymphoma Group. Several investigators had industry ties, including Dr. Greenwood, an adviser and/or researcher for Amgen, Pfizer, Servier, and Jazz.
The study team found that “an intensive pediatric ALL induction protocol can be delivered in an AYA [adolescent and young adult] cohort in a similar time frame to a pediatric population, suggesting that the inferior outcomes seen in AYA patients are more likely related to the biology of AYA ALL rather than intolerance of more intensive therapy,” said investigators led by Matthew Greenwood, MBBS, director of the stem cell transplant at the Royal North Shore Hospital, outside of Sydney
It’s been a long-standing question why intensive ALL regimens, which can be curative in children, don’t work as well in adolescents and young adults.
To see if tolerability and lack of adherence were issues, the investigators compared the treatment time lines of 82 AYA subjects with a median age of 22 years to the time lines of 608 children aged 1-17 years who were treated with the same intensive regimen (the ANZCHOG Study 8 protocol).
Induction/consolidation was equally deliverable in both populations. In the AYA group, 41.5% of subjects started the next phase of treatment – protocol M or high-risk (HR) therapy based on minimal residual disease (MRD) response to initial treatment – by day 94 versus 39.3% in the previous pediatric study (P = 0.77). The median time to protocol M/HR treatment was 96 days in AYAs and 98 days in children (P = .80).
About 52% of AYA subjects proceeded to HR therapy following induction/consolidation, versus just 10.7% in the pediatric study.
The investigators also found that a body mass index at or above 30 kg/m2 and the presence of MRD were both associated with worse disease-free and overall survival. “By addressing the factors predicting poorer outcomes from this study, we hope to significantly improve the outcomes for patients,” they said.
They noted that their work is the first to “report of the safety and efficacy of an MRD-stratified approach utilizing [Berlin-Frankfurt-Munich] HR therapy in an AYA cohort and show that this is a moderately efficacious strategy in patients who would otherwise be considered at high risk of relapse and death.”
Over a median follow-up of 44 months, estimated 3-year disease-free survival was 72.8% and estimated 3-year overall survival 74.9% in the AYA population.
The work was funded by the Australasian Leukaemia and Lymphoma Group. Several investigators had industry ties, including Dr. Greenwood, an adviser and/or researcher for Amgen, Pfizer, Servier, and Jazz.
The study team found that “an intensive pediatric ALL induction protocol can be delivered in an AYA [adolescent and young adult] cohort in a similar time frame to a pediatric population, suggesting that the inferior outcomes seen in AYA patients are more likely related to the biology of AYA ALL rather than intolerance of more intensive therapy,” said investigators led by Matthew Greenwood, MBBS, director of the stem cell transplant at the Royal North Shore Hospital, outside of Sydney
It’s been a long-standing question why intensive ALL regimens, which can be curative in children, don’t work as well in adolescents and young adults.
To see if tolerability and lack of adherence were issues, the investigators compared the treatment time lines of 82 AYA subjects with a median age of 22 years to the time lines of 608 children aged 1-17 years who were treated with the same intensive regimen (the ANZCHOG Study 8 protocol).
Induction/consolidation was equally deliverable in both populations. In the AYA group, 41.5% of subjects started the next phase of treatment – protocol M or high-risk (HR) therapy based on minimal residual disease (MRD) response to initial treatment – by day 94 versus 39.3% in the previous pediatric study (P = 0.77). The median time to protocol M/HR treatment was 96 days in AYAs and 98 days in children (P = .80).
About 52% of AYA subjects proceeded to HR therapy following induction/consolidation, versus just 10.7% in the pediatric study.
The investigators also found that a body mass index at or above 30 kg/m2 and the presence of MRD were both associated with worse disease-free and overall survival. “By addressing the factors predicting poorer outcomes from this study, we hope to significantly improve the outcomes for patients,” they said.
They noted that their work is the first to “report of the safety and efficacy of an MRD-stratified approach utilizing [Berlin-Frankfurt-Munich] HR therapy in an AYA cohort and show that this is a moderately efficacious strategy in patients who would otherwise be considered at high risk of relapse and death.”
Over a median follow-up of 44 months, estimated 3-year disease-free survival was 72.8% and estimated 3-year overall survival 74.9% in the AYA population.
The work was funded by the Australasian Leukaemia and Lymphoma Group. Several investigators had industry ties, including Dr. Greenwood, an adviser and/or researcher for Amgen, Pfizer, Servier, and Jazz.
FROM BLOOD ADVANCES
More than half of people living with HIV have coronary plaque
More than half of people living with HIV and suppressed viral loads nonetheless had imaging-confirmed coronary artery disease – and despite longtime use of HIV drugs that have been associated with cardiovascular trouble, none of those drugs were implicated in disease risk in this study.
“Traditional risk factors and duration of HIV infection were associated with severe coronary artery disease,” said Andreas Knudsen, MD, PhD, an infectious disease provider at Copenhagen University Hospital, Hvidovre, Denmark, during his presentation at the 18th European AIDS Conference. “When we adjusted for time since diagnosis of HIV, none of the drugs remained associated with the severity of coronary artery disease.”
Notably, that included abacavir, which was found in another EACS presentation and in past research to be associated with increased rates of heart attacks. Abacavir is sold individually as a generic as well as a component of Epzicom (abacavir/lamivudine) and the single-drug regimen Triumeq (dolutegravir/abacavir/lamivudine).
The Copenhagen Comorbidity in HIV Infection (COCOMO) study enrolled 1,099 people living with HIV in the Danish capital beginning in 2015, and 705 of them had angiographies via CT available to include in the results. The participants were almost all male (89%), at a healthy weight (BMI of 25), and 96% had undetectable viral loads.
Large minorities of participants also had traditional risk factors for coronary artery disease. More than one in four smoked, one in five had high cholesterol, and 42% had high blood pressure. In addition, many had used drugs that have been associated with cardiovascular trouble, including abacavir, which 26% of participants had used; indinavir, used by 17% of participants; zidovudine/AZT, used by 47%; and didanosine, which 14% used. (While abacavir is still in use, the other three drugs are considered legacy drugs and are not in current use.)
In addition, nearly one in three (29%) were currently using a protease inhibitor, which has been associated with heart failure.
When the investigators looked at participants’ CTs, they found that, by the Coronary Artery Disease-Reporting and Data Systems (CAD-RAMS) scoring system, close to half (46%) had clear arteries with no signs of coronary artery disease. But that also meant that 54% had some blockage or stiffening of the arteries. The good news is that 27% of those people had minimal or mild coronary artery disease.
But a full 17% had confirmed obstructive coronary artery disease, and another 1 in 10 participants had the highest level of blockages. When they broke the data down by traditional and HIV medication–related risk factors for coronary artery disease, they found something interesting. Although obesity was associated with the presence of atherosclerosis, it wasn’t associated with severe disease. But diabetes was the reverse of that: It wasn’t associated with the presence of the disease, but it was associated with more severe disease.
And when they looked at abacavir, they found no relationship between the drug and atherosclerosis. “Abacavir was not associated with the presence of atherosclerosis and was also not associated with severity of disease,” said Dr. Knudsen.
Although past use of AZT, indinavir, and didanosine were associated with severity of atherosclerosis, that association went away when Dr. Knudsen and team adjusted the findings for time since diagnosis. What was associated atherosclerosis was length of time living with HIV itself. For every 5 years a person lived with HIV, the study found the risk of having any atherosclerosis increased 20% and severity increased 23%. In addition, being a man was associated with a nearly 2.5-times increased risk of having any atherosclerosis and a 96% increased chance of having more severe atherosclerosis. Having diabetes was associated with a nearly threefold increased risk of atherosclerosis, as was every additional decade of life for a person who was living with HIV.
The findings confirm the baseline data of the REPRIEVE trial, which recently released data showing similarly high rates of atherosclerotic plaque in people living with HIV who didn’t register as “at risk” for cardiovascular disease using traditional scoring methods.
“It’s important in that it’s a huge study that’s confirmatory [of] what we know, which is that there are high levels of subclinical coronary artery disease in people living with HIV,” said Steven Grinspoon, MD, professor at Harvard Medical School in Boston, Massachusetts, and principal investigator of REPRIEVE.
As for the lack of association between abacavir and cardiovascular risk, he said he’s taking the findings with a grain of salt.
“It’s hard to make a lot out of that,” he said. “It’s hard to know in a cross-sectional study. People put people on different things.”
In Spain, where Jose Ignacio Bernardino, MD, treats people living with HIV at La Paz University Hospital in Madrid, abacavir is mostly a moot point, as clinicians have long since moved away from maintaining people living with HIV on any abacavir-containing regimens. What’s more important in the study, he told this news organization, is that “worrisome” high level of risk. REPRIEVE will test whether statins can reduce heart disease events in people living with HIV. But in the meantime, he said the take-away for clinicians from the study is the primary importance of traditional cardiovascular risk factors.
“We have to acknowledge that the major cardiovascular risk factor is age,” he said. “When patients are approaching their 50s, I usually try to stress a lot about cardiovascular risk factors in general. I stress healthy lifestyle – get physical exercise, hypertension, glucose, lipids – in every single patient.”
Dr. Knudsen and Dr. Bernardino have disclosed no relevant financial relationships. Dr. Grinspoon reports receiving personal and consulting fees from Theratechnologies and ViiV Healthcare.
A version of this article first appeared on Medscape.com.
More than half of people living with HIV and suppressed viral loads nonetheless had imaging-confirmed coronary artery disease – and despite longtime use of HIV drugs that have been associated with cardiovascular trouble, none of those drugs were implicated in disease risk in this study.
“Traditional risk factors and duration of HIV infection were associated with severe coronary artery disease,” said Andreas Knudsen, MD, PhD, an infectious disease provider at Copenhagen University Hospital, Hvidovre, Denmark, during his presentation at the 18th European AIDS Conference. “When we adjusted for time since diagnosis of HIV, none of the drugs remained associated with the severity of coronary artery disease.”
Notably, that included abacavir, which was found in another EACS presentation and in past research to be associated with increased rates of heart attacks. Abacavir is sold individually as a generic as well as a component of Epzicom (abacavir/lamivudine) and the single-drug regimen Triumeq (dolutegravir/abacavir/lamivudine).
The Copenhagen Comorbidity in HIV Infection (COCOMO) study enrolled 1,099 people living with HIV in the Danish capital beginning in 2015, and 705 of them had angiographies via CT available to include in the results. The participants were almost all male (89%), at a healthy weight (BMI of 25), and 96% had undetectable viral loads.
Large minorities of participants also had traditional risk factors for coronary artery disease. More than one in four smoked, one in five had high cholesterol, and 42% had high blood pressure. In addition, many had used drugs that have been associated with cardiovascular trouble, including abacavir, which 26% of participants had used; indinavir, used by 17% of participants; zidovudine/AZT, used by 47%; and didanosine, which 14% used. (While abacavir is still in use, the other three drugs are considered legacy drugs and are not in current use.)
In addition, nearly one in three (29%) were currently using a protease inhibitor, which has been associated with heart failure.
When the investigators looked at participants’ CTs, they found that, by the Coronary Artery Disease-Reporting and Data Systems (CAD-RAMS) scoring system, close to half (46%) had clear arteries with no signs of coronary artery disease. But that also meant that 54% had some blockage or stiffening of the arteries. The good news is that 27% of those people had minimal or mild coronary artery disease.
But a full 17% had confirmed obstructive coronary artery disease, and another 1 in 10 participants had the highest level of blockages. When they broke the data down by traditional and HIV medication–related risk factors for coronary artery disease, they found something interesting. Although obesity was associated with the presence of atherosclerosis, it wasn’t associated with severe disease. But diabetes was the reverse of that: It wasn’t associated with the presence of the disease, but it was associated with more severe disease.
And when they looked at abacavir, they found no relationship between the drug and atherosclerosis. “Abacavir was not associated with the presence of atherosclerosis and was also not associated with severity of disease,” said Dr. Knudsen.
Although past use of AZT, indinavir, and didanosine were associated with severity of atherosclerosis, that association went away when Dr. Knudsen and team adjusted the findings for time since diagnosis. What was associated atherosclerosis was length of time living with HIV itself. For every 5 years a person lived with HIV, the study found the risk of having any atherosclerosis increased 20% and severity increased 23%. In addition, being a man was associated with a nearly 2.5-times increased risk of having any atherosclerosis and a 96% increased chance of having more severe atherosclerosis. Having diabetes was associated with a nearly threefold increased risk of atherosclerosis, as was every additional decade of life for a person who was living with HIV.
The findings confirm the baseline data of the REPRIEVE trial, which recently released data showing similarly high rates of atherosclerotic plaque in people living with HIV who didn’t register as “at risk” for cardiovascular disease using traditional scoring methods.
“It’s important in that it’s a huge study that’s confirmatory [of] what we know, which is that there are high levels of subclinical coronary artery disease in people living with HIV,” said Steven Grinspoon, MD, professor at Harvard Medical School in Boston, Massachusetts, and principal investigator of REPRIEVE.
As for the lack of association between abacavir and cardiovascular risk, he said he’s taking the findings with a grain of salt.
“It’s hard to make a lot out of that,” he said. “It’s hard to know in a cross-sectional study. People put people on different things.”
In Spain, where Jose Ignacio Bernardino, MD, treats people living with HIV at La Paz University Hospital in Madrid, abacavir is mostly a moot point, as clinicians have long since moved away from maintaining people living with HIV on any abacavir-containing regimens. What’s more important in the study, he told this news organization, is that “worrisome” high level of risk. REPRIEVE will test whether statins can reduce heart disease events in people living with HIV. But in the meantime, he said the take-away for clinicians from the study is the primary importance of traditional cardiovascular risk factors.
“We have to acknowledge that the major cardiovascular risk factor is age,” he said. “When patients are approaching their 50s, I usually try to stress a lot about cardiovascular risk factors in general. I stress healthy lifestyle – get physical exercise, hypertension, glucose, lipids – in every single patient.”
Dr. Knudsen and Dr. Bernardino have disclosed no relevant financial relationships. Dr. Grinspoon reports receiving personal and consulting fees from Theratechnologies and ViiV Healthcare.
A version of this article first appeared on Medscape.com.
More than half of people living with HIV and suppressed viral loads nonetheless had imaging-confirmed coronary artery disease – and despite longtime use of HIV drugs that have been associated with cardiovascular trouble, none of those drugs were implicated in disease risk in this study.
“Traditional risk factors and duration of HIV infection were associated with severe coronary artery disease,” said Andreas Knudsen, MD, PhD, an infectious disease provider at Copenhagen University Hospital, Hvidovre, Denmark, during his presentation at the 18th European AIDS Conference. “When we adjusted for time since diagnosis of HIV, none of the drugs remained associated with the severity of coronary artery disease.”
Notably, that included abacavir, which was found in another EACS presentation and in past research to be associated with increased rates of heart attacks. Abacavir is sold individually as a generic as well as a component of Epzicom (abacavir/lamivudine) and the single-drug regimen Triumeq (dolutegravir/abacavir/lamivudine).
The Copenhagen Comorbidity in HIV Infection (COCOMO) study enrolled 1,099 people living with HIV in the Danish capital beginning in 2015, and 705 of them had angiographies via CT available to include in the results. The participants were almost all male (89%), at a healthy weight (BMI of 25), and 96% had undetectable viral loads.
Large minorities of participants also had traditional risk factors for coronary artery disease. More than one in four smoked, one in five had high cholesterol, and 42% had high blood pressure. In addition, many had used drugs that have been associated with cardiovascular trouble, including abacavir, which 26% of participants had used; indinavir, used by 17% of participants; zidovudine/AZT, used by 47%; and didanosine, which 14% used. (While abacavir is still in use, the other three drugs are considered legacy drugs and are not in current use.)
In addition, nearly one in three (29%) were currently using a protease inhibitor, which has been associated with heart failure.
When the investigators looked at participants’ CTs, they found that, by the Coronary Artery Disease-Reporting and Data Systems (CAD-RAMS) scoring system, close to half (46%) had clear arteries with no signs of coronary artery disease. But that also meant that 54% had some blockage or stiffening of the arteries. The good news is that 27% of those people had minimal or mild coronary artery disease.
But a full 17% had confirmed obstructive coronary artery disease, and another 1 in 10 participants had the highest level of blockages. When they broke the data down by traditional and HIV medication–related risk factors for coronary artery disease, they found something interesting. Although obesity was associated with the presence of atherosclerosis, it wasn’t associated with severe disease. But diabetes was the reverse of that: It wasn’t associated with the presence of the disease, but it was associated with more severe disease.
And when they looked at abacavir, they found no relationship between the drug and atherosclerosis. “Abacavir was not associated with the presence of atherosclerosis and was also not associated with severity of disease,” said Dr. Knudsen.
Although past use of AZT, indinavir, and didanosine were associated with severity of atherosclerosis, that association went away when Dr. Knudsen and team adjusted the findings for time since diagnosis. What was associated atherosclerosis was length of time living with HIV itself. For every 5 years a person lived with HIV, the study found the risk of having any atherosclerosis increased 20% and severity increased 23%. In addition, being a man was associated with a nearly 2.5-times increased risk of having any atherosclerosis and a 96% increased chance of having more severe atherosclerosis. Having diabetes was associated with a nearly threefold increased risk of atherosclerosis, as was every additional decade of life for a person who was living with HIV.
The findings confirm the baseline data of the REPRIEVE trial, which recently released data showing similarly high rates of atherosclerotic plaque in people living with HIV who didn’t register as “at risk” for cardiovascular disease using traditional scoring methods.
“It’s important in that it’s a huge study that’s confirmatory [of] what we know, which is that there are high levels of subclinical coronary artery disease in people living with HIV,” said Steven Grinspoon, MD, professor at Harvard Medical School in Boston, Massachusetts, and principal investigator of REPRIEVE.
As for the lack of association between abacavir and cardiovascular risk, he said he’s taking the findings with a grain of salt.
“It’s hard to make a lot out of that,” he said. “It’s hard to know in a cross-sectional study. People put people on different things.”
In Spain, where Jose Ignacio Bernardino, MD, treats people living with HIV at La Paz University Hospital in Madrid, abacavir is mostly a moot point, as clinicians have long since moved away from maintaining people living with HIV on any abacavir-containing regimens. What’s more important in the study, he told this news organization, is that “worrisome” high level of risk. REPRIEVE will test whether statins can reduce heart disease events in people living with HIV. But in the meantime, he said the take-away for clinicians from the study is the primary importance of traditional cardiovascular risk factors.
“We have to acknowledge that the major cardiovascular risk factor is age,” he said. “When patients are approaching their 50s, I usually try to stress a lot about cardiovascular risk factors in general. I stress healthy lifestyle – get physical exercise, hypertension, glucose, lipids – in every single patient.”
Dr. Knudsen and Dr. Bernardino have disclosed no relevant financial relationships. Dr. Grinspoon reports receiving personal and consulting fees from Theratechnologies and ViiV Healthcare.
A version of this article first appeared on Medscape.com.
SBRT on oligoprogressive lesions: Benefit in lung cancer
Patients treated with SBRT had a median PFS of 44 weeks, compared with 9 weeks for those who received standard care.
However, no benefit was observed in patients with metastatic breast cancer. There was no significant difference in PFS between the two groups (18 weeks with SBRT vs. 19 weeks with standard care).
“In this preplanned interim analysis, we demonstrated the benefit of SBRT to sites of oligoprogression on overall progression-free survival, which was the primary endpoint,” said lead author C. Jillian Tsai, MD, PhD, a radiation oncologist and director of metastatic disease radiation oncology research at Memorial Sloan Kettering Cancer Center in New York. “The difference was driven by the substantial response in [this] NSCLC cohort.”
There was no benefit of SBRT seen in the breast cohort, she noted, and most breast patients developed new lesions upon further progression.
Dr. Tsai and colleagues are planning to close the trial early, after the interim analysis established the benefit of SBRT. They are now investigating why SBRT was beneficial in NSCLC but not in breast cancer.
The findings were presented at the American Society for Radiation Oncology (ASTRO) annual meeting.
Dr. Tsai explained that the current standard of care for patients with oligoprogressive metastatic NSCLC is to switch to a different targeted therapy or chemotherapy following progression, but options may be limited. Efficacy for second-line therapy can be poor, with PFS ranging from about 4 months to 10 months for NSCLC, “and after second line, efficacy for third and fourth lines is even poorer,” she said.
Similarly, for breast cancer, PFS ranges from about 9 months to 20 months for estrogen-receptor positive patients. “But for triple negative patients, there really is no standard of care and PFS is poor,” Dr. Tsai said.
SBRT superior to standard of care
The authors hypothesized that there is an oligoprogressive state in metastatic cancer, in which disease control can be improved by applying local therapy to progressive lesions only.
The cohort included 102 patients with metastatic NSCLC or breast cancer who had received one or more lines of systemic therapy and had oligoprogressive lesions amenable to SBRT. There was no upper limit of nonprogressive lesions.
Oligoprogression was defined as Response Evaluation or Positron Emission Tomography Response Criteria in Solid Tumors documented progression ≤5 individual lesions.
Patients were randomly assigned to receive either SBRT to all progressive sites plus palliative standard of care or systemic SOC only. Systemic therapy was per physician’s discretion.
There were 58 patients with NSCLC (30 in the SBRT group) and 44 patients with breast cancer (22 in each group).
Most patients (75%) had more than one site of oligoprogression and 47% had more than 5 total metastatic lesions. About half of patients (54%) had received immunotherapy and the majority of those with NSCLC (86%) did not harbor an actionable driver mutation. About one-third (32%) of the breast cancer cohort were triple negative.
Patients were followed for a median of 45 weeks (58 weeks for living patients), by which time 78 (74%) had experienced further tumor progression and 39 (37%) had died.
Median progression-free survival for the entire cohort was 31 weeks for SBRT and 11 weeks for palliative SOC (P = .002).
In multivariable analysis that stratified for factors including age, sex, lines of systemic therapy, and change of systemic therapy, the progression-free survival benefit of SBRT continued to remain substantial in the NSCLC cohort (hazard ratio: 0.38; P = .007).
Adverse events were higher in the SBRT group. Grade 2 or higher adverse events occurred in 23 (61%) of SBRT patients, and 15 (40%) of SOC patients (P = .13).
Hoped-for results, with a few caveats
Approached for comment on the new findings, Clifford Robinson, MD, professor of radiation oncology, chief of SBRT service, and director of clinical trials and informatics at Washington University, St. Louis, said the results tie in with previous findings.
There are multiple published or presented prospective randomized phase 2 and 3 trials in various disease sites that have explored the role of local therapy, including SBRT, for patients who present with oligometastatic disease.
“These studies have nearly uniformly shown improvements in progression-free and/or overall survival with the inclusion of local therapy,” he told this news organization. Dr. Robinson was not involved with the study.
He explained that relatively few patients present with oligometastatic disease. However, many patients present with more advanced disease, but after an initial course of systemic therapy, develop oligoprogression.
“There is tremendous appeal to using local therapy at the time of oligoprogression in lieu of switching systemic therapy,” said Dr. Robinson. “It allows patients to stay on systemic therapy that is otherwise effective for the remainder of their disease.”
First-line systemic therapies are the most effective and the most tolerable, he continued, and switching systemic therapy introduces the potential for more toxicity and less efficacy. Therefore, it has become increasingly popular to offer SBRT to one or a few sites of oligoprogressive disease based on the results of oligometastatic disease.
“However, there is no established prospective data to guide this practice,” he said. “This trial is the first to examine this carefully in lung and breast cancer patients, and this trial shows what we hoped to see – that use of SBRT after oligoprogression results in improved progression-free survival as compared with standard of care alone. And this was accomplished with limited toxicity.”
There are a few caveats, though, he pointed out. “Progression-free survival is defined as time to first progression or death,” he said. “Since we don’t know what the overall survival is in this abstract, it’s entirely possible that patients live for the same length of time, but just take longer to progress.”
Another caveat is that this was a planned interim analysis. “Typically, planned interim analyses occur to see if the trial should be stopped or to adjust the study based on results,” he said. “It’s unclear what the investigators will do with this information.”
“But overall, these are very exciting data and lend support to the increasingly common practice of treating oligoprogressive disease,” Dr. Robinson added. “Since most of the serious adverse events of SBRT occur later, longer follow-up is needed, although the median survival of patients may not reach that timepoint.”
“For now, practice should not be altered based on these interim results,” he added.
Dr. Tsai reported acting as a consultant/advisor for Varian and Galera and also receiving research funding from Varian. Dr. Robinson reports stock/ownership in Radialogica, acting as a consultant/advisor for Varian, AstraZeneca, EMD Serono, Quantitative Radiology Solutions, research funding from Varian and Merck, and owning patents on systems for cardiac arrhythmias and ablation.
A version of this article first appeared on Medscape.com.
Patients treated with SBRT had a median PFS of 44 weeks, compared with 9 weeks for those who received standard care.
However, no benefit was observed in patients with metastatic breast cancer. There was no significant difference in PFS between the two groups (18 weeks with SBRT vs. 19 weeks with standard care).
“In this preplanned interim analysis, we demonstrated the benefit of SBRT to sites of oligoprogression on overall progression-free survival, which was the primary endpoint,” said lead author C. Jillian Tsai, MD, PhD, a radiation oncologist and director of metastatic disease radiation oncology research at Memorial Sloan Kettering Cancer Center in New York. “The difference was driven by the substantial response in [this] NSCLC cohort.”
There was no benefit of SBRT seen in the breast cohort, she noted, and most breast patients developed new lesions upon further progression.
Dr. Tsai and colleagues are planning to close the trial early, after the interim analysis established the benefit of SBRT. They are now investigating why SBRT was beneficial in NSCLC but not in breast cancer.
The findings were presented at the American Society for Radiation Oncology (ASTRO) annual meeting.
Dr. Tsai explained that the current standard of care for patients with oligoprogressive metastatic NSCLC is to switch to a different targeted therapy or chemotherapy following progression, but options may be limited. Efficacy for second-line therapy can be poor, with PFS ranging from about 4 months to 10 months for NSCLC, “and after second line, efficacy for third and fourth lines is even poorer,” she said.
Similarly, for breast cancer, PFS ranges from about 9 months to 20 months for estrogen-receptor positive patients. “But for triple negative patients, there really is no standard of care and PFS is poor,” Dr. Tsai said.
SBRT superior to standard of care
The authors hypothesized that there is an oligoprogressive state in metastatic cancer, in which disease control can be improved by applying local therapy to progressive lesions only.
The cohort included 102 patients with metastatic NSCLC or breast cancer who had received one or more lines of systemic therapy and had oligoprogressive lesions amenable to SBRT. There was no upper limit of nonprogressive lesions.
Oligoprogression was defined as Response Evaluation or Positron Emission Tomography Response Criteria in Solid Tumors documented progression ≤5 individual lesions.
Patients were randomly assigned to receive either SBRT to all progressive sites plus palliative standard of care or systemic SOC only. Systemic therapy was per physician’s discretion.
There were 58 patients with NSCLC (30 in the SBRT group) and 44 patients with breast cancer (22 in each group).
Most patients (75%) had more than one site of oligoprogression and 47% had more than 5 total metastatic lesions. About half of patients (54%) had received immunotherapy and the majority of those with NSCLC (86%) did not harbor an actionable driver mutation. About one-third (32%) of the breast cancer cohort were triple negative.
Patients were followed for a median of 45 weeks (58 weeks for living patients), by which time 78 (74%) had experienced further tumor progression and 39 (37%) had died.
Median progression-free survival for the entire cohort was 31 weeks for SBRT and 11 weeks for palliative SOC (P = .002).
In multivariable analysis that stratified for factors including age, sex, lines of systemic therapy, and change of systemic therapy, the progression-free survival benefit of SBRT continued to remain substantial in the NSCLC cohort (hazard ratio: 0.38; P = .007).
Adverse events were higher in the SBRT group. Grade 2 or higher adverse events occurred in 23 (61%) of SBRT patients, and 15 (40%) of SOC patients (P = .13).
Hoped-for results, with a few caveats
Approached for comment on the new findings, Clifford Robinson, MD, professor of radiation oncology, chief of SBRT service, and director of clinical trials and informatics at Washington University, St. Louis, said the results tie in with previous findings.
There are multiple published or presented prospective randomized phase 2 and 3 trials in various disease sites that have explored the role of local therapy, including SBRT, for patients who present with oligometastatic disease.
“These studies have nearly uniformly shown improvements in progression-free and/or overall survival with the inclusion of local therapy,” he told this news organization. Dr. Robinson was not involved with the study.
He explained that relatively few patients present with oligometastatic disease. However, many patients present with more advanced disease, but after an initial course of systemic therapy, develop oligoprogression.
“There is tremendous appeal to using local therapy at the time of oligoprogression in lieu of switching systemic therapy,” said Dr. Robinson. “It allows patients to stay on systemic therapy that is otherwise effective for the remainder of their disease.”
First-line systemic therapies are the most effective and the most tolerable, he continued, and switching systemic therapy introduces the potential for more toxicity and less efficacy. Therefore, it has become increasingly popular to offer SBRT to one or a few sites of oligoprogressive disease based on the results of oligometastatic disease.
“However, there is no established prospective data to guide this practice,” he said. “This trial is the first to examine this carefully in lung and breast cancer patients, and this trial shows what we hoped to see – that use of SBRT after oligoprogression results in improved progression-free survival as compared with standard of care alone. And this was accomplished with limited toxicity.”
There are a few caveats, though, he pointed out. “Progression-free survival is defined as time to first progression or death,” he said. “Since we don’t know what the overall survival is in this abstract, it’s entirely possible that patients live for the same length of time, but just take longer to progress.”
Another caveat is that this was a planned interim analysis. “Typically, planned interim analyses occur to see if the trial should be stopped or to adjust the study based on results,” he said. “It’s unclear what the investigators will do with this information.”
“But overall, these are very exciting data and lend support to the increasingly common practice of treating oligoprogressive disease,” Dr. Robinson added. “Since most of the serious adverse events of SBRT occur later, longer follow-up is needed, although the median survival of patients may not reach that timepoint.”
“For now, practice should not be altered based on these interim results,” he added.
Dr. Tsai reported acting as a consultant/advisor for Varian and Galera and also receiving research funding from Varian. Dr. Robinson reports stock/ownership in Radialogica, acting as a consultant/advisor for Varian, AstraZeneca, EMD Serono, Quantitative Radiology Solutions, research funding from Varian and Merck, and owning patents on systems for cardiac arrhythmias and ablation.
A version of this article first appeared on Medscape.com.
Patients treated with SBRT had a median PFS of 44 weeks, compared with 9 weeks for those who received standard care.
However, no benefit was observed in patients with metastatic breast cancer. There was no significant difference in PFS between the two groups (18 weeks with SBRT vs. 19 weeks with standard care).
“In this preplanned interim analysis, we demonstrated the benefit of SBRT to sites of oligoprogression on overall progression-free survival, which was the primary endpoint,” said lead author C. Jillian Tsai, MD, PhD, a radiation oncologist and director of metastatic disease radiation oncology research at Memorial Sloan Kettering Cancer Center in New York. “The difference was driven by the substantial response in [this] NSCLC cohort.”
There was no benefit of SBRT seen in the breast cohort, she noted, and most breast patients developed new lesions upon further progression.
Dr. Tsai and colleagues are planning to close the trial early, after the interim analysis established the benefit of SBRT. They are now investigating why SBRT was beneficial in NSCLC but not in breast cancer.
The findings were presented at the American Society for Radiation Oncology (ASTRO) annual meeting.
Dr. Tsai explained that the current standard of care for patients with oligoprogressive metastatic NSCLC is to switch to a different targeted therapy or chemotherapy following progression, but options may be limited. Efficacy for second-line therapy can be poor, with PFS ranging from about 4 months to 10 months for NSCLC, “and after second line, efficacy for third and fourth lines is even poorer,” she said.
Similarly, for breast cancer, PFS ranges from about 9 months to 20 months for estrogen-receptor positive patients. “But for triple negative patients, there really is no standard of care and PFS is poor,” Dr. Tsai said.
SBRT superior to standard of care
The authors hypothesized that there is an oligoprogressive state in metastatic cancer, in which disease control can be improved by applying local therapy to progressive lesions only.
The cohort included 102 patients with metastatic NSCLC or breast cancer who had received one or more lines of systemic therapy and had oligoprogressive lesions amenable to SBRT. There was no upper limit of nonprogressive lesions.
Oligoprogression was defined as Response Evaluation or Positron Emission Tomography Response Criteria in Solid Tumors documented progression ≤5 individual lesions.
Patients were randomly assigned to receive either SBRT to all progressive sites plus palliative standard of care or systemic SOC only. Systemic therapy was per physician’s discretion.
There were 58 patients with NSCLC (30 in the SBRT group) and 44 patients with breast cancer (22 in each group).
Most patients (75%) had more than one site of oligoprogression and 47% had more than 5 total metastatic lesions. About half of patients (54%) had received immunotherapy and the majority of those with NSCLC (86%) did not harbor an actionable driver mutation. About one-third (32%) of the breast cancer cohort were triple negative.
Patients were followed for a median of 45 weeks (58 weeks for living patients), by which time 78 (74%) had experienced further tumor progression and 39 (37%) had died.
Median progression-free survival for the entire cohort was 31 weeks for SBRT and 11 weeks for palliative SOC (P = .002).
In multivariable analysis that stratified for factors including age, sex, lines of systemic therapy, and change of systemic therapy, the progression-free survival benefit of SBRT continued to remain substantial in the NSCLC cohort (hazard ratio: 0.38; P = .007).
Adverse events were higher in the SBRT group. Grade 2 or higher adverse events occurred in 23 (61%) of SBRT patients, and 15 (40%) of SOC patients (P = .13).
Hoped-for results, with a few caveats
Approached for comment on the new findings, Clifford Robinson, MD, professor of radiation oncology, chief of SBRT service, and director of clinical trials and informatics at Washington University, St. Louis, said the results tie in with previous findings.
There are multiple published or presented prospective randomized phase 2 and 3 trials in various disease sites that have explored the role of local therapy, including SBRT, for patients who present with oligometastatic disease.
“These studies have nearly uniformly shown improvements in progression-free and/or overall survival with the inclusion of local therapy,” he told this news organization. Dr. Robinson was not involved with the study.
He explained that relatively few patients present with oligometastatic disease. However, many patients present with more advanced disease, but after an initial course of systemic therapy, develop oligoprogression.
“There is tremendous appeal to using local therapy at the time of oligoprogression in lieu of switching systemic therapy,” said Dr. Robinson. “It allows patients to stay on systemic therapy that is otherwise effective for the remainder of their disease.”
First-line systemic therapies are the most effective and the most tolerable, he continued, and switching systemic therapy introduces the potential for more toxicity and less efficacy. Therefore, it has become increasingly popular to offer SBRT to one or a few sites of oligoprogressive disease based on the results of oligometastatic disease.
“However, there is no established prospective data to guide this practice,” he said. “This trial is the first to examine this carefully in lung and breast cancer patients, and this trial shows what we hoped to see – that use of SBRT after oligoprogression results in improved progression-free survival as compared with standard of care alone. And this was accomplished with limited toxicity.”
There are a few caveats, though, he pointed out. “Progression-free survival is defined as time to first progression or death,” he said. “Since we don’t know what the overall survival is in this abstract, it’s entirely possible that patients live for the same length of time, but just take longer to progress.”
Another caveat is that this was a planned interim analysis. “Typically, planned interim analyses occur to see if the trial should be stopped or to adjust the study based on results,” he said. “It’s unclear what the investigators will do with this information.”
“But overall, these are very exciting data and lend support to the increasingly common practice of treating oligoprogressive disease,” Dr. Robinson added. “Since most of the serious adverse events of SBRT occur later, longer follow-up is needed, although the median survival of patients may not reach that timepoint.”
“For now, practice should not be altered based on these interim results,” he added.
Dr. Tsai reported acting as a consultant/advisor for Varian and Galera and also receiving research funding from Varian. Dr. Robinson reports stock/ownership in Radialogica, acting as a consultant/advisor for Varian, AstraZeneca, EMD Serono, Quantitative Radiology Solutions, research funding from Varian and Merck, and owning patents on systems for cardiac arrhythmias and ablation.
A version of this article first appeared on Medscape.com.
NCI mammography trial mostly a ‘waste,’ says expert
Funding for this trial is largely misspent money, it may produce misleading results, and it should be abandoned, he says.
Dr. Kopans has been an outspoken critic of the trial, describing it as a “huge waste of money” in comments made last year. Now he has set out his criticisms of the trial in an essay published in the October issue of Clinical Imaging, which outlines his objections and concerns for the first time in a peer-reviewed journal.
The Tomosynthesis Mammographic Imaging Screening Trial (TMIST) is comparing digital breast tomosynthesis (DBT), also known as 3-D mammography, with the older 2-D technology or full-field digital mammography (FFDM).
Dr. Kopans coined the term DBT and formerly held a now-expired patent on the first version of this technology.
“It could be argued that the imaging part of TMIST is a waste of valuable resources,” he writes in the essay.
The “imaging part” of the trial refers to the primary outcome measure and driving purpose of the trial, which is designed to learn which technology is better at finding – and reducing the rate of – potentially lethal “advanced” cancers.
These cancers include larger HER2-positive and triple-negative malignancies; those associated with positive nodes; and metastatic disease. These malignancies correlate with breast cancer mortality, TMIST’s principal investigator Etta Pisano, MD, of the American College of Radiology, has said in the past.
However, Dr. Kopans says that this surrogate endpoint is problematic. “TMIST will only investigate whether or not digital breast tomography results in a decline in advanced cancers, ignoring the fact that many women still die from cancers that are not advanced at the time of diagnosis,” he writes.
“Clearly reducing the rate of advanced cancers is not the only way that early detection saves lives. Lives are also saved by finding cancers at a smaller size within stages,” Dr. Kopans writes. He adds that DBT has been proven in observational cohort studies to find more smaller breast cancers than FFDM.
Dr. Kopans’ opinion that TMIST is largely a waste of resources is not shared by the National Cancer Institute. “We feel strongly that TMIST is a critical study,” an NCI spokesperson told this news organization.
Study power concerns
Another concern is that TMIST “may be underpowered,” Dr. Kopans writes. That concern arises in part from a recent review of TMIST by an advisory committee (that was prompted by low patient accrual rates), which proposed reducing the size of the trial. Dr. Kopans says this would result in “a reduction of the planned power of the trial.”
The NCI says that reducing the study size has been discussed but has not yet been implemented. “Any reduction in size would, of course, have appropriate statistical considerations in mind,” according to the NCI spokesperson.
Dr. Kopans’ concern about statistical power extends beyond downsizing the trial. An advanced cancer in TMIST is counted “if it occurs at any time while the participant is on study,” according to the NCI. Dr. Kopans says that is a problem.
“Since DBT cannot have any effect on advanced cancers in the prevalence year (they are already there), data from the first year (prevalence cancers are likely the largest number) will be unusable, and if used will, inappropriately, dilute the results,” he writes.
Dr. Kopans hopes that the investigators address the statistical power issues with the trial because, if not, “its results may be grossly misleading.”
American radiology practice
Dr. Kopans praises one aspect of TMIST – the trial’s effort to create a repository of blood and oral swab specimens, along with participant genetic data. The goal, say TMIST investigators, is to individualize or optimize screening strategies by tying molecular data to clinical outcomes in the trial.
However, apart from that one aspect, Dr. Kopans is highly critical of the trial.
It is now too late to compare the two technologies, he suggests, as DBT is already replacing FFDM for breast cancer screening in the U.S.
He notes that 76% of mammography facilities in the United States have 3-D devices (as of April 2021). That percentage has climbed steadily in recent years. “By the time the TMIST study is completed, DBT will, almost certainly, have become the ‘standard of care,’” he asserts, echoing others who have commented on the trial, including some participating physicians.
The money being spent on TMIST “should not be used for looking backwards,” says Dr. Kopans.
The NCI responded to that criticism. “TMIST is looking to clarify the best screening for women based on the science and is not solely about access. We are seeking to determine which technology is better and [are] providing access to the trial across the country in diverse practices and populations,” the NCI said in an email.
In his essay, Dr. Kopans says it is time to stop TMIST and put the money into other pressing breast cancer issues and questions. “... it makes no sense to continue this flawed trial whose results will be obsolete by the time they become available,” he writes.
Dr. Kopans reports consulting with DART Imaging in China, which is developing a digital breast tomosynthesis machine.
A version of this article first appeared on Medscape.com.
Funding for this trial is largely misspent money, it may produce misleading results, and it should be abandoned, he says.
Dr. Kopans has been an outspoken critic of the trial, describing it as a “huge waste of money” in comments made last year. Now he has set out his criticisms of the trial in an essay published in the October issue of Clinical Imaging, which outlines his objections and concerns for the first time in a peer-reviewed journal.
The Tomosynthesis Mammographic Imaging Screening Trial (TMIST) is comparing digital breast tomosynthesis (DBT), also known as 3-D mammography, with the older 2-D technology or full-field digital mammography (FFDM).
Dr. Kopans coined the term DBT and formerly held a now-expired patent on the first version of this technology.
“It could be argued that the imaging part of TMIST is a waste of valuable resources,” he writes in the essay.
The “imaging part” of the trial refers to the primary outcome measure and driving purpose of the trial, which is designed to learn which technology is better at finding – and reducing the rate of – potentially lethal “advanced” cancers.
These cancers include larger HER2-positive and triple-negative malignancies; those associated with positive nodes; and metastatic disease. These malignancies correlate with breast cancer mortality, TMIST’s principal investigator Etta Pisano, MD, of the American College of Radiology, has said in the past.
However, Dr. Kopans says that this surrogate endpoint is problematic. “TMIST will only investigate whether or not digital breast tomography results in a decline in advanced cancers, ignoring the fact that many women still die from cancers that are not advanced at the time of diagnosis,” he writes.
“Clearly reducing the rate of advanced cancers is not the only way that early detection saves lives. Lives are also saved by finding cancers at a smaller size within stages,” Dr. Kopans writes. He adds that DBT has been proven in observational cohort studies to find more smaller breast cancers than FFDM.
Dr. Kopans’ opinion that TMIST is largely a waste of resources is not shared by the National Cancer Institute. “We feel strongly that TMIST is a critical study,” an NCI spokesperson told this news organization.
Study power concerns
Another concern is that TMIST “may be underpowered,” Dr. Kopans writes. That concern arises in part from a recent review of TMIST by an advisory committee (that was prompted by low patient accrual rates), which proposed reducing the size of the trial. Dr. Kopans says this would result in “a reduction of the planned power of the trial.”
The NCI says that reducing the study size has been discussed but has not yet been implemented. “Any reduction in size would, of course, have appropriate statistical considerations in mind,” according to the NCI spokesperson.
Dr. Kopans’ concern about statistical power extends beyond downsizing the trial. An advanced cancer in TMIST is counted “if it occurs at any time while the participant is on study,” according to the NCI. Dr. Kopans says that is a problem.
“Since DBT cannot have any effect on advanced cancers in the prevalence year (they are already there), data from the first year (prevalence cancers are likely the largest number) will be unusable, and if used will, inappropriately, dilute the results,” he writes.
Dr. Kopans hopes that the investigators address the statistical power issues with the trial because, if not, “its results may be grossly misleading.”
American radiology practice
Dr. Kopans praises one aspect of TMIST – the trial’s effort to create a repository of blood and oral swab specimens, along with participant genetic data. The goal, say TMIST investigators, is to individualize or optimize screening strategies by tying molecular data to clinical outcomes in the trial.
However, apart from that one aspect, Dr. Kopans is highly critical of the trial.
It is now too late to compare the two technologies, he suggests, as DBT is already replacing FFDM for breast cancer screening in the U.S.
He notes that 76% of mammography facilities in the United States have 3-D devices (as of April 2021). That percentage has climbed steadily in recent years. “By the time the TMIST study is completed, DBT will, almost certainly, have become the ‘standard of care,’” he asserts, echoing others who have commented on the trial, including some participating physicians.
The money being spent on TMIST “should not be used for looking backwards,” says Dr. Kopans.
The NCI responded to that criticism. “TMIST is looking to clarify the best screening for women based on the science and is not solely about access. We are seeking to determine which technology is better and [are] providing access to the trial across the country in diverse practices and populations,” the NCI said in an email.
In his essay, Dr. Kopans says it is time to stop TMIST and put the money into other pressing breast cancer issues and questions. “... it makes no sense to continue this flawed trial whose results will be obsolete by the time they become available,” he writes.
Dr. Kopans reports consulting with DART Imaging in China, which is developing a digital breast tomosynthesis machine.
A version of this article first appeared on Medscape.com.
Funding for this trial is largely misspent money, it may produce misleading results, and it should be abandoned, he says.
Dr. Kopans has been an outspoken critic of the trial, describing it as a “huge waste of money” in comments made last year. Now he has set out his criticisms of the trial in an essay published in the October issue of Clinical Imaging, which outlines his objections and concerns for the first time in a peer-reviewed journal.
The Tomosynthesis Mammographic Imaging Screening Trial (TMIST) is comparing digital breast tomosynthesis (DBT), also known as 3-D mammography, with the older 2-D technology or full-field digital mammography (FFDM).
Dr. Kopans coined the term DBT and formerly held a now-expired patent on the first version of this technology.
“It could be argued that the imaging part of TMIST is a waste of valuable resources,” he writes in the essay.
The “imaging part” of the trial refers to the primary outcome measure and driving purpose of the trial, which is designed to learn which technology is better at finding – and reducing the rate of – potentially lethal “advanced” cancers.
These cancers include larger HER2-positive and triple-negative malignancies; those associated with positive nodes; and metastatic disease. These malignancies correlate with breast cancer mortality, TMIST’s principal investigator Etta Pisano, MD, of the American College of Radiology, has said in the past.
However, Dr. Kopans says that this surrogate endpoint is problematic. “TMIST will only investigate whether or not digital breast tomography results in a decline in advanced cancers, ignoring the fact that many women still die from cancers that are not advanced at the time of diagnosis,” he writes.
“Clearly reducing the rate of advanced cancers is not the only way that early detection saves lives. Lives are also saved by finding cancers at a smaller size within stages,” Dr. Kopans writes. He adds that DBT has been proven in observational cohort studies to find more smaller breast cancers than FFDM.
Dr. Kopans’ opinion that TMIST is largely a waste of resources is not shared by the National Cancer Institute. “We feel strongly that TMIST is a critical study,” an NCI spokesperson told this news organization.
Study power concerns
Another concern is that TMIST “may be underpowered,” Dr. Kopans writes. That concern arises in part from a recent review of TMIST by an advisory committee (that was prompted by low patient accrual rates), which proposed reducing the size of the trial. Dr. Kopans says this would result in “a reduction of the planned power of the trial.”
The NCI says that reducing the study size has been discussed but has not yet been implemented. “Any reduction in size would, of course, have appropriate statistical considerations in mind,” according to the NCI spokesperson.
Dr. Kopans’ concern about statistical power extends beyond downsizing the trial. An advanced cancer in TMIST is counted “if it occurs at any time while the participant is on study,” according to the NCI. Dr. Kopans says that is a problem.
“Since DBT cannot have any effect on advanced cancers in the prevalence year (they are already there), data from the first year (prevalence cancers are likely the largest number) will be unusable, and if used will, inappropriately, dilute the results,” he writes.
Dr. Kopans hopes that the investigators address the statistical power issues with the trial because, if not, “its results may be grossly misleading.”
American radiology practice
Dr. Kopans praises one aspect of TMIST – the trial’s effort to create a repository of blood and oral swab specimens, along with participant genetic data. The goal, say TMIST investigators, is to individualize or optimize screening strategies by tying molecular data to clinical outcomes in the trial.
However, apart from that one aspect, Dr. Kopans is highly critical of the trial.
It is now too late to compare the two technologies, he suggests, as DBT is already replacing FFDM for breast cancer screening in the U.S.
He notes that 76% of mammography facilities in the United States have 3-D devices (as of April 2021). That percentage has climbed steadily in recent years. “By the time the TMIST study is completed, DBT will, almost certainly, have become the ‘standard of care,’” he asserts, echoing others who have commented on the trial, including some participating physicians.
The money being spent on TMIST “should not be used for looking backwards,” says Dr. Kopans.
The NCI responded to that criticism. “TMIST is looking to clarify the best screening for women based on the science and is not solely about access. We are seeking to determine which technology is better and [are] providing access to the trial across the country in diverse practices and populations,” the NCI said in an email.
In his essay, Dr. Kopans says it is time to stop TMIST and put the money into other pressing breast cancer issues and questions. “... it makes no sense to continue this flawed trial whose results will be obsolete by the time they become available,” he writes.
Dr. Kopans reports consulting with DART Imaging in China, which is developing a digital breast tomosynthesis machine.
A version of this article first appeared on Medscape.com.
Prostate cancer risk higher with Lynch syndrome variants
Men who carry certain pathogenic variants in mismatch repair genes that characterize Lynch syndrome may have a higher risk of prostate cancer, shows a new study. However, for men who carry MSH2 and MSH6 variants, the risk of contracting cancer rises significantly.
Called IMPACT, the study, which was published online in The Lancet Oncology, is an international, prospective study of 828 men aged between 40 and 69 years who were prostate cancer free, but they carried germline pathogenic variants in one of the mismatch repair genes MLH1, MSH2, or MSH6.
The researchers, who were led by Rosalind A. Eeles, PhD, a specialist in oncogenetics with the Institute of Cancer Research, London, found that after one screening “a higher incidence of prostate cancer was detected in men with MSH2 and MHS6 pathogenic variants, compared with age-matched noncarrier controls.”
She and her team also found that MSH2 carriers “were diagnosed at a nonsignificantly younger age and had more clinically significant disease at diagnosis, compared with noncarriers. These data add evidence that prostate screening in this higher-risk context has potential to detect tumors that are highly likely to need treatment.”
The findings suggest that targeted prostate-specific antigen (PSA) screening in men with mismatch repair gene pathogenic variants is justifiable. “Testing for mismatch repair variants will likely become routine practice at diagnosis over the coming years,” the authors wrote.
Lynch syndrome can increase the risk of prostate cancer by 2-10 times, yet there is no international consensus for screening. The 2019 National Comprehensive Cancer Network guidelines recommend considering tumor testing for deficient mismatch repair in men with regional or metastatic prostate cancer. The NCCN also recommends germline testing for all newly diagnosed men with high-risk, very-high-risk, regional, or metastatic prostate cancer.
Currently, the PSA test is the most commonly used test, however, it is not recommended as a routine screening tool because of the negative consequences of overdetection. The American Cancer Society and European Association of Urology recommend PSA screening for men with a strong family history of prostate cancer. The EAU also supports annual PSA screening for men with BRCA2 variants.
“From a treatment perspective, knowledge of mismatch repair pathogenic variant status is increasingly important because of the evidence that mismatch repair-deficient prostate tumors can be sensitive to immune checkpoint inhibitors,” the investigators wrote.
NCCN guidelines support the use of the progressive death–1 inhibitor pembrolizumab (Keytruda, Merck) in these patients, among others.
Although immune checkpoint inhibitors are predominantly used to treat metastatic disease, “this field is rapidly evolving and we will likely see these treatments move earlier in the treatment pathway,” the authors predicted.
The findings in detail
The IMPACT study was established in 2005 to assess targeted PSA screening in men with BRCA1 or BRCA2 pathogenic variants. It was extended in 2012 to include men from families with MLH1, MSH2, and MSH6 pathogenic variants.
In this new report, within the first round of screening, 6% of the cohort had a PSA concentration higher than 3.0 ng/mL and the overall incidence of prostate cancer was 1.9%, the investigators noted.
MSH2 carriers were diagnosed at 58 years old on average, compared with 66 years old for the control group. MSH2-positive men had more clinically significant disease, compared with noncarriers. The incidence of prostate cancer was higher at 4.3% in MSH2 carriers than in controls at 0.5%. In MSH6 carriers, the incidence of prostate cancer was 3.0%, compared with 0% for controls.
Only 4% of men underwent a biopsy and only one cancer was found among the MSH2 noncarriers while no cancers were found in MLH1 carriers, MLH1 noncarriers, or MSH6 noncarriers.
The overall positive predictive value of using a PSA threshold of 3.0 ng/mL was 51.4%; separated by genetic status, the PPV in MSH2 carriers was higher at 72.2% and in MSH6 carriers, the PPV was 80%, the researchers noted.
Limitations of the study include the fact that the number of cancers detected in the study was relatively small, thus requiring further data from subsequent screening rounds.
One study coauthor disclosed a potential conflict of interest by holding a PSA test patent.
Men who carry certain pathogenic variants in mismatch repair genes that characterize Lynch syndrome may have a higher risk of prostate cancer, shows a new study. However, for men who carry MSH2 and MSH6 variants, the risk of contracting cancer rises significantly.
Called IMPACT, the study, which was published online in The Lancet Oncology, is an international, prospective study of 828 men aged between 40 and 69 years who were prostate cancer free, but they carried germline pathogenic variants in one of the mismatch repair genes MLH1, MSH2, or MSH6.
The researchers, who were led by Rosalind A. Eeles, PhD, a specialist in oncogenetics with the Institute of Cancer Research, London, found that after one screening “a higher incidence of prostate cancer was detected in men with MSH2 and MHS6 pathogenic variants, compared with age-matched noncarrier controls.”
She and her team also found that MSH2 carriers “were diagnosed at a nonsignificantly younger age and had more clinically significant disease at diagnosis, compared with noncarriers. These data add evidence that prostate screening in this higher-risk context has potential to detect tumors that are highly likely to need treatment.”
The findings suggest that targeted prostate-specific antigen (PSA) screening in men with mismatch repair gene pathogenic variants is justifiable. “Testing for mismatch repair variants will likely become routine practice at diagnosis over the coming years,” the authors wrote.
Lynch syndrome can increase the risk of prostate cancer by 2-10 times, yet there is no international consensus for screening. The 2019 National Comprehensive Cancer Network guidelines recommend considering tumor testing for deficient mismatch repair in men with regional or metastatic prostate cancer. The NCCN also recommends germline testing for all newly diagnosed men with high-risk, very-high-risk, regional, or metastatic prostate cancer.
Currently, the PSA test is the most commonly used test, however, it is not recommended as a routine screening tool because of the negative consequences of overdetection. The American Cancer Society and European Association of Urology recommend PSA screening for men with a strong family history of prostate cancer. The EAU also supports annual PSA screening for men with BRCA2 variants.
“From a treatment perspective, knowledge of mismatch repair pathogenic variant status is increasingly important because of the evidence that mismatch repair-deficient prostate tumors can be sensitive to immune checkpoint inhibitors,” the investigators wrote.
NCCN guidelines support the use of the progressive death–1 inhibitor pembrolizumab (Keytruda, Merck) in these patients, among others.
Although immune checkpoint inhibitors are predominantly used to treat metastatic disease, “this field is rapidly evolving and we will likely see these treatments move earlier in the treatment pathway,” the authors predicted.
The findings in detail
The IMPACT study was established in 2005 to assess targeted PSA screening in men with BRCA1 or BRCA2 pathogenic variants. It was extended in 2012 to include men from families with MLH1, MSH2, and MSH6 pathogenic variants.
In this new report, within the first round of screening, 6% of the cohort had a PSA concentration higher than 3.0 ng/mL and the overall incidence of prostate cancer was 1.9%, the investigators noted.
MSH2 carriers were diagnosed at 58 years old on average, compared with 66 years old for the control group. MSH2-positive men had more clinically significant disease, compared with noncarriers. The incidence of prostate cancer was higher at 4.3% in MSH2 carriers than in controls at 0.5%. In MSH6 carriers, the incidence of prostate cancer was 3.0%, compared with 0% for controls.
Only 4% of men underwent a biopsy and only one cancer was found among the MSH2 noncarriers while no cancers were found in MLH1 carriers, MLH1 noncarriers, or MSH6 noncarriers.
The overall positive predictive value of using a PSA threshold of 3.0 ng/mL was 51.4%; separated by genetic status, the PPV in MSH2 carriers was higher at 72.2% and in MSH6 carriers, the PPV was 80%, the researchers noted.
Limitations of the study include the fact that the number of cancers detected in the study was relatively small, thus requiring further data from subsequent screening rounds.
One study coauthor disclosed a potential conflict of interest by holding a PSA test patent.
Men who carry certain pathogenic variants in mismatch repair genes that characterize Lynch syndrome may have a higher risk of prostate cancer, shows a new study. However, for men who carry MSH2 and MSH6 variants, the risk of contracting cancer rises significantly.
Called IMPACT, the study, which was published online in The Lancet Oncology, is an international, prospective study of 828 men aged between 40 and 69 years who were prostate cancer free, but they carried germline pathogenic variants in one of the mismatch repair genes MLH1, MSH2, or MSH6.
The researchers, who were led by Rosalind A. Eeles, PhD, a specialist in oncogenetics with the Institute of Cancer Research, London, found that after one screening “a higher incidence of prostate cancer was detected in men with MSH2 and MHS6 pathogenic variants, compared with age-matched noncarrier controls.”
She and her team also found that MSH2 carriers “were diagnosed at a nonsignificantly younger age and had more clinically significant disease at diagnosis, compared with noncarriers. These data add evidence that prostate screening in this higher-risk context has potential to detect tumors that are highly likely to need treatment.”
The findings suggest that targeted prostate-specific antigen (PSA) screening in men with mismatch repair gene pathogenic variants is justifiable. “Testing for mismatch repair variants will likely become routine practice at diagnosis over the coming years,” the authors wrote.
Lynch syndrome can increase the risk of prostate cancer by 2-10 times, yet there is no international consensus for screening. The 2019 National Comprehensive Cancer Network guidelines recommend considering tumor testing for deficient mismatch repair in men with regional or metastatic prostate cancer. The NCCN also recommends germline testing for all newly diagnosed men with high-risk, very-high-risk, regional, or metastatic prostate cancer.
Currently, the PSA test is the most commonly used test, however, it is not recommended as a routine screening tool because of the negative consequences of overdetection. The American Cancer Society and European Association of Urology recommend PSA screening for men with a strong family history of prostate cancer. The EAU also supports annual PSA screening for men with BRCA2 variants.
“From a treatment perspective, knowledge of mismatch repair pathogenic variant status is increasingly important because of the evidence that mismatch repair-deficient prostate tumors can be sensitive to immune checkpoint inhibitors,” the investigators wrote.
NCCN guidelines support the use of the progressive death–1 inhibitor pembrolizumab (Keytruda, Merck) in these patients, among others.
Although immune checkpoint inhibitors are predominantly used to treat metastatic disease, “this field is rapidly evolving and we will likely see these treatments move earlier in the treatment pathway,” the authors predicted.
The findings in detail
The IMPACT study was established in 2005 to assess targeted PSA screening in men with BRCA1 or BRCA2 pathogenic variants. It was extended in 2012 to include men from families with MLH1, MSH2, and MSH6 pathogenic variants.
In this new report, within the first round of screening, 6% of the cohort had a PSA concentration higher than 3.0 ng/mL and the overall incidence of prostate cancer was 1.9%, the investigators noted.
MSH2 carriers were diagnosed at 58 years old on average, compared with 66 years old for the control group. MSH2-positive men had more clinically significant disease, compared with noncarriers. The incidence of prostate cancer was higher at 4.3% in MSH2 carriers than in controls at 0.5%. In MSH6 carriers, the incidence of prostate cancer was 3.0%, compared with 0% for controls.
Only 4% of men underwent a biopsy and only one cancer was found among the MSH2 noncarriers while no cancers were found in MLH1 carriers, MLH1 noncarriers, or MSH6 noncarriers.
The overall positive predictive value of using a PSA threshold of 3.0 ng/mL was 51.4%; separated by genetic status, the PPV in MSH2 carriers was higher at 72.2% and in MSH6 carriers, the PPV was 80%, the researchers noted.
Limitations of the study include the fact that the number of cancers detected in the study was relatively small, thus requiring further data from subsequent screening rounds.
One study coauthor disclosed a potential conflict of interest by holding a PSA test patent.
FROM LANCET ONCOLOGY
AGA Clinical Practice Update: Managing pain in gut-brain interaction disorders
An American Gastroenterological Association clinical practice update for gastrointestinal pain in disorders of gut-brain interaction (DGBI), published in Clinical Gastroenterology and Hepatology, emphasizes patient-physician collaboration and improvement of patient understanding of the pathways and mechanisms of pain sensations. It is aimed at management of patients in whom pain persists after first-line therapies fail to resolve visceral causes of pain.
DGBIs include irritable bowel syndrome, functional dyspepsia, and centrally mediated abdominal pain syndrome, according to Laurie Keefer, PhD, AGAF, of the division of gastroenterology at Icahn School of Medicine at Mount Sinai, New York, and colleagues. Initial treatment usually focuses on visceral triggers of pain such as food and bowel movements, but this approach is ineffective for many.
Cognitive, affective, and behavioral factors can impact the treatment of these patients, making it a complex clinical problem that calls for a collaborative approach between the patient and clinician. Opioids and other drugs that could be misused should be avoided, according to the authors. Both pharmacologic and nonpharmacologic approaches can be considered, but the update did not address use of marijuana or other complementary or alternative therapies.
Effective management requires empathy and collaboration. The patient has often seen various other clinicians with suboptimal results, which has left them dissatisfied with their care. Cultural sensitivity is crucial because the understanding and interpretation of pain, and preferred management approaches, vary across cultures.
The first step is a nonjudgmental patient history using open-ended questions. Examples include: “How do your symptoms interfere with your ability to do what you want in your daily life?” or “How are these symptoms impacting your life the most?” These types of questions may identify patients who could benefit from behavioral health interventions.
Questions about symptom-related anxiety can improve understanding of patient concerns and offer an opportunity to address fears. Additional understanding of the patient’s perspective can come from questions like: “What do you think is causing your symptoms,” “Why are you coming to see me now?” and “What are you most concerned about with your symptoms?”
The initial assessment should ideally result in shared goals and expectations for pain management.
Providers should educate the patient about the pathogenesis of pain and how it can be modified. Pain signals can result from innocuous signals from the gut that are misinterpreted by the vigilant brain as it scans for injury or illness. That model might explain why some patients with similar diagnoses have widely differing pain experiences, and offers hope that a change in how one approaches pain might lead to improvements. Patients should be encouraged to avoid too much focus on the cause or a solution to pain, because it can interfere with acceptance of pain or, when needed, treatment.
Opioids should not be prescribed for these patients, and if they are already taking them on referral, it’s important to manage them within a multidisciplinary framework until the opioids can be discontinued. Long-term use of opioids can lead to narcotic bowel syndrome, which results in chronic and often heightened abdominal pain even with escalating opioid doses. Opioid stoppage often must be accompanied by behavioral and psychiatric therapies to ensure success.
Nonpharmacological therapies such as brain-gut psychotherapies should be brought up as potential options early in treatment, even though many patients won’t require this type of care. Early mention is likely to keep the patient more open to trying them because they’re less likely to think of it as a sign of failure or a “last-ditch” approach. Cognitive-behavioral therapy works to improve pain management skills and bolster skill deficits, with attention to pain catastrophizing, pain hypervigilance, and visceral anxiety through different techniques.
Gut-directed hypnotherapy deals with somatic awareness and the use of imagery and suggestion to reduce pain sensations. Mindfulness-based stress reduction has been shown to be effective in inflammatory bowel disease and musculoskeletal pain syndromes. The provider should be familiar with these available methods, but should leave choice of interventions to partner mental health providers.
It’s important to distinguish between gastrointestinal pain with visceral causes and centrally mediated pain. Central sensitization can cause intermittent pain to become persistent even in the absence of ongoing peripheral causes of pain.
Peripheral acting agents affect gastrointestinal pain, and a network meta-analysis identified the top three drugs for pain relief in irritable bowel syndrome as tricyclic antidepressants, antispasmodics, and peppermint oil.
Neuromodulator drugs are an option for DGBI pain because the gut nervous system shares embryonic developmental pathways with the brain and spinal cord, which helps explains some of the benefits of low-dose antidepressants, now termed gut-brain neuromodulators. These drugs should be started at a low dose and gradually titrated according to symptom response and tolerability.
The authors have financial relationships with various pharmaceutical companies.
An American Gastroenterological Association clinical practice update for gastrointestinal pain in disorders of gut-brain interaction (DGBI), published in Clinical Gastroenterology and Hepatology, emphasizes patient-physician collaboration and improvement of patient understanding of the pathways and mechanisms of pain sensations. It is aimed at management of patients in whom pain persists after first-line therapies fail to resolve visceral causes of pain.
DGBIs include irritable bowel syndrome, functional dyspepsia, and centrally mediated abdominal pain syndrome, according to Laurie Keefer, PhD, AGAF, of the division of gastroenterology at Icahn School of Medicine at Mount Sinai, New York, and colleagues. Initial treatment usually focuses on visceral triggers of pain such as food and bowel movements, but this approach is ineffective for many.
Cognitive, affective, and behavioral factors can impact the treatment of these patients, making it a complex clinical problem that calls for a collaborative approach between the patient and clinician. Opioids and other drugs that could be misused should be avoided, according to the authors. Both pharmacologic and nonpharmacologic approaches can be considered, but the update did not address use of marijuana or other complementary or alternative therapies.
Effective management requires empathy and collaboration. The patient has often seen various other clinicians with suboptimal results, which has left them dissatisfied with their care. Cultural sensitivity is crucial because the understanding and interpretation of pain, and preferred management approaches, vary across cultures.
The first step is a nonjudgmental patient history using open-ended questions. Examples include: “How do your symptoms interfere with your ability to do what you want in your daily life?” or “How are these symptoms impacting your life the most?” These types of questions may identify patients who could benefit from behavioral health interventions.
Questions about symptom-related anxiety can improve understanding of patient concerns and offer an opportunity to address fears. Additional understanding of the patient’s perspective can come from questions like: “What do you think is causing your symptoms,” “Why are you coming to see me now?” and “What are you most concerned about with your symptoms?”
The initial assessment should ideally result in shared goals and expectations for pain management.
Providers should educate the patient about the pathogenesis of pain and how it can be modified. Pain signals can result from innocuous signals from the gut that are misinterpreted by the vigilant brain as it scans for injury or illness. That model might explain why some patients with similar diagnoses have widely differing pain experiences, and offers hope that a change in how one approaches pain might lead to improvements. Patients should be encouraged to avoid too much focus on the cause or a solution to pain, because it can interfere with acceptance of pain or, when needed, treatment.
Opioids should not be prescribed for these patients, and if they are already taking them on referral, it’s important to manage them within a multidisciplinary framework until the opioids can be discontinued. Long-term use of opioids can lead to narcotic bowel syndrome, which results in chronic and often heightened abdominal pain even with escalating opioid doses. Opioid stoppage often must be accompanied by behavioral and psychiatric therapies to ensure success.
Nonpharmacological therapies such as brain-gut psychotherapies should be brought up as potential options early in treatment, even though many patients won’t require this type of care. Early mention is likely to keep the patient more open to trying them because they’re less likely to think of it as a sign of failure or a “last-ditch” approach. Cognitive-behavioral therapy works to improve pain management skills and bolster skill deficits, with attention to pain catastrophizing, pain hypervigilance, and visceral anxiety through different techniques.
Gut-directed hypnotherapy deals with somatic awareness and the use of imagery and suggestion to reduce pain sensations. Mindfulness-based stress reduction has been shown to be effective in inflammatory bowel disease and musculoskeletal pain syndromes. The provider should be familiar with these available methods, but should leave choice of interventions to partner mental health providers.
It’s important to distinguish between gastrointestinal pain with visceral causes and centrally mediated pain. Central sensitization can cause intermittent pain to become persistent even in the absence of ongoing peripheral causes of pain.
Peripheral acting agents affect gastrointestinal pain, and a network meta-analysis identified the top three drugs for pain relief in irritable bowel syndrome as tricyclic antidepressants, antispasmodics, and peppermint oil.
Neuromodulator drugs are an option for DGBI pain because the gut nervous system shares embryonic developmental pathways with the brain and spinal cord, which helps explains some of the benefits of low-dose antidepressants, now termed gut-brain neuromodulators. These drugs should be started at a low dose and gradually titrated according to symptom response and tolerability.
The authors have financial relationships with various pharmaceutical companies.
An American Gastroenterological Association clinical practice update for gastrointestinal pain in disorders of gut-brain interaction (DGBI), published in Clinical Gastroenterology and Hepatology, emphasizes patient-physician collaboration and improvement of patient understanding of the pathways and mechanisms of pain sensations. It is aimed at management of patients in whom pain persists after first-line therapies fail to resolve visceral causes of pain.
DGBIs include irritable bowel syndrome, functional dyspepsia, and centrally mediated abdominal pain syndrome, according to Laurie Keefer, PhD, AGAF, of the division of gastroenterology at Icahn School of Medicine at Mount Sinai, New York, and colleagues. Initial treatment usually focuses on visceral triggers of pain such as food and bowel movements, but this approach is ineffective for many.
Cognitive, affective, and behavioral factors can impact the treatment of these patients, making it a complex clinical problem that calls for a collaborative approach between the patient and clinician. Opioids and other drugs that could be misused should be avoided, according to the authors. Both pharmacologic and nonpharmacologic approaches can be considered, but the update did not address use of marijuana or other complementary or alternative therapies.
Effective management requires empathy and collaboration. The patient has often seen various other clinicians with suboptimal results, which has left them dissatisfied with their care. Cultural sensitivity is crucial because the understanding and interpretation of pain, and preferred management approaches, vary across cultures.
The first step is a nonjudgmental patient history using open-ended questions. Examples include: “How do your symptoms interfere with your ability to do what you want in your daily life?” or “How are these symptoms impacting your life the most?” These types of questions may identify patients who could benefit from behavioral health interventions.
Questions about symptom-related anxiety can improve understanding of patient concerns and offer an opportunity to address fears. Additional understanding of the patient’s perspective can come from questions like: “What do you think is causing your symptoms,” “Why are you coming to see me now?” and “What are you most concerned about with your symptoms?”
The initial assessment should ideally result in shared goals and expectations for pain management.
Providers should educate the patient about the pathogenesis of pain and how it can be modified. Pain signals can result from innocuous signals from the gut that are misinterpreted by the vigilant brain as it scans for injury or illness. That model might explain why some patients with similar diagnoses have widely differing pain experiences, and offers hope that a change in how one approaches pain might lead to improvements. Patients should be encouraged to avoid too much focus on the cause or a solution to pain, because it can interfere with acceptance of pain or, when needed, treatment.
Opioids should not be prescribed for these patients, and if they are already taking them on referral, it’s important to manage them within a multidisciplinary framework until the opioids can be discontinued. Long-term use of opioids can lead to narcotic bowel syndrome, which results in chronic and often heightened abdominal pain even with escalating opioid doses. Opioid stoppage often must be accompanied by behavioral and psychiatric therapies to ensure success.
Nonpharmacological therapies such as brain-gut psychotherapies should be brought up as potential options early in treatment, even though many patients won’t require this type of care. Early mention is likely to keep the patient more open to trying them because they’re less likely to think of it as a sign of failure or a “last-ditch” approach. Cognitive-behavioral therapy works to improve pain management skills and bolster skill deficits, with attention to pain catastrophizing, pain hypervigilance, and visceral anxiety through different techniques.
Gut-directed hypnotherapy deals with somatic awareness and the use of imagery and suggestion to reduce pain sensations. Mindfulness-based stress reduction has been shown to be effective in inflammatory bowel disease and musculoskeletal pain syndromes. The provider should be familiar with these available methods, but should leave choice of interventions to partner mental health providers.
It’s important to distinguish between gastrointestinal pain with visceral causes and centrally mediated pain. Central sensitization can cause intermittent pain to become persistent even in the absence of ongoing peripheral causes of pain.
Peripheral acting agents affect gastrointestinal pain, and a network meta-analysis identified the top three drugs for pain relief in irritable bowel syndrome as tricyclic antidepressants, antispasmodics, and peppermint oil.
Neuromodulator drugs are an option for DGBI pain because the gut nervous system shares embryonic developmental pathways with the brain and spinal cord, which helps explains some of the benefits of low-dose antidepressants, now termed gut-brain neuromodulators. These drugs should be started at a low dose and gradually titrated according to symptom response and tolerability.
The authors have financial relationships with various pharmaceutical companies.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Expected spike in acute flaccid myelitis did not occur in 2020
suggested researchers at the Centers for Disease Control and Prevention.
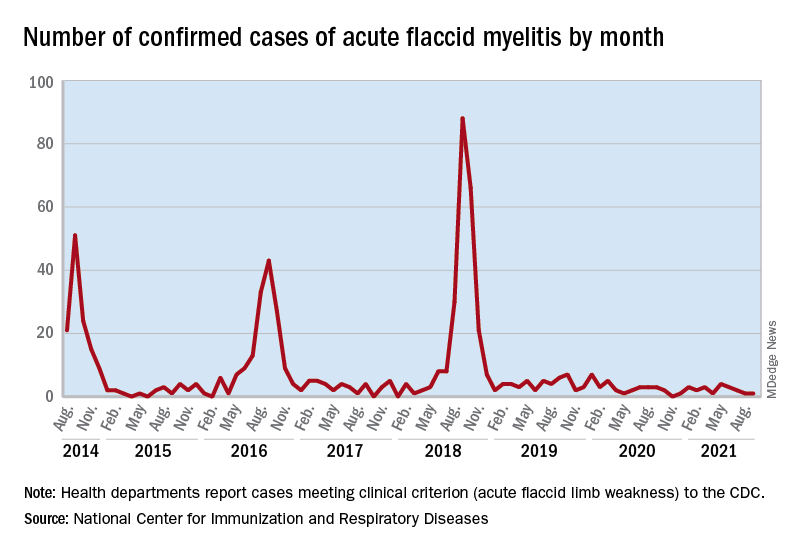
Acute flaccid myelitis (AFM) is an uncommon but serious complication of some viral infections, including West Nile virus and nonpolio enteroviruses. It is “characterized by sudden onset of limb weakness and lesions in the gray matter of the spinal cord,” they said, and more than 90% of cases occur in young children.
Cases of AFM, which can lead to respiratory insufficiency and permanent paralysis, spiked during the late summer and early fall in 2014, 2016, and 2018 and were expected to do so again in 2020, Sarah Kidd, MD, and associates at the division of viral diseases at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta, said in the Morbidity and Mortality Weekly Report.
Monthly peaks in those previous years – each occurring in September – reached 51 cases in 2014, 43 cases in 2016, and 88 cases in 2018, but in 2020 there was only 1 case reported in September, with a high of 4 coming in May, CDC data show. The total number of cases for 2020 (32) was, in fact, lower than in 2019, when 47 were reported.
The investigators’ main objective was to see if there were any differences between the 2018 and 2019-2020 cases. Reports from state health departments to the CDC showed that, in 2019-2020, “patients were older; more likely to have lower limb involvement; and less likely to have upper limb involvement, prodromal illness, [cerebrospinal fluid] pleocytosis, or specimens that tested positive for EV [enterovirus]-D68” than patients from 2018, Dr. Kidd and associates said.
Mask wearing and reduced in-school attendance may have decreased circulation of EV-D68 – the enterovirus type most often detected in the stool and respiratory specimens of AFM patients – as was seen with other respiratory viruses, such as influenza and respiratory syncytial virus, in 2020. Previous studies have suggested that EV-D68 drives the increases in cases during peak years, the researchers noted.
The absence of such an increase “in 2020 reflects a deviation from the previously observed biennial pattern, and it is unclear when the next increase in AFM should be expected. Clinicians should continue to maintain vigilance and suspect AFM in any child with acute flaccid limb weakness, particularly in the setting of recent febrile or respiratory illness,” they wrote.
suggested researchers at the Centers for Disease Control and Prevention.
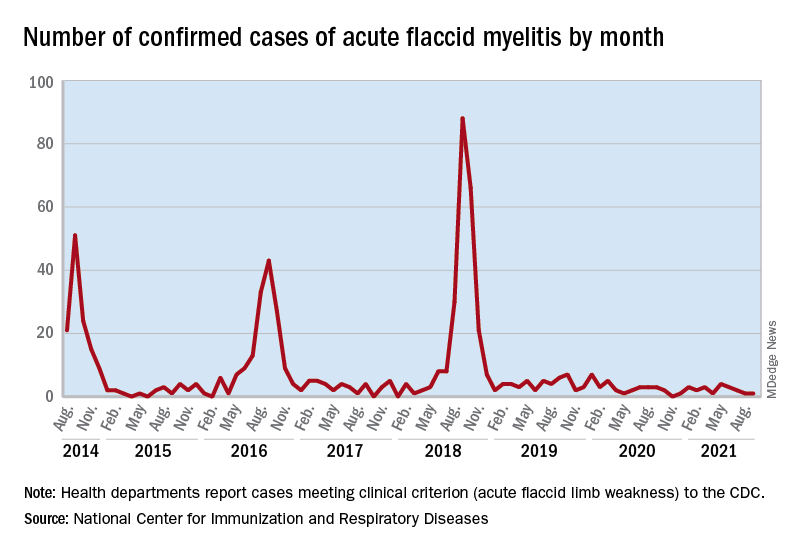
Acute flaccid myelitis (AFM) is an uncommon but serious complication of some viral infections, including West Nile virus and nonpolio enteroviruses. It is “characterized by sudden onset of limb weakness and lesions in the gray matter of the spinal cord,” they said, and more than 90% of cases occur in young children.
Cases of AFM, which can lead to respiratory insufficiency and permanent paralysis, spiked during the late summer and early fall in 2014, 2016, and 2018 and were expected to do so again in 2020, Sarah Kidd, MD, and associates at the division of viral diseases at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta, said in the Morbidity and Mortality Weekly Report.
Monthly peaks in those previous years – each occurring in September – reached 51 cases in 2014, 43 cases in 2016, and 88 cases in 2018, but in 2020 there was only 1 case reported in September, with a high of 4 coming in May, CDC data show. The total number of cases for 2020 (32) was, in fact, lower than in 2019, when 47 were reported.
The investigators’ main objective was to see if there were any differences between the 2018 and 2019-2020 cases. Reports from state health departments to the CDC showed that, in 2019-2020, “patients were older; more likely to have lower limb involvement; and less likely to have upper limb involvement, prodromal illness, [cerebrospinal fluid] pleocytosis, or specimens that tested positive for EV [enterovirus]-D68” than patients from 2018, Dr. Kidd and associates said.
Mask wearing and reduced in-school attendance may have decreased circulation of EV-D68 – the enterovirus type most often detected in the stool and respiratory specimens of AFM patients – as was seen with other respiratory viruses, such as influenza and respiratory syncytial virus, in 2020. Previous studies have suggested that EV-D68 drives the increases in cases during peak years, the researchers noted.
The absence of such an increase “in 2020 reflects a deviation from the previously observed biennial pattern, and it is unclear when the next increase in AFM should be expected. Clinicians should continue to maintain vigilance and suspect AFM in any child with acute flaccid limb weakness, particularly in the setting of recent febrile or respiratory illness,” they wrote.
suggested researchers at the Centers for Disease Control and Prevention.
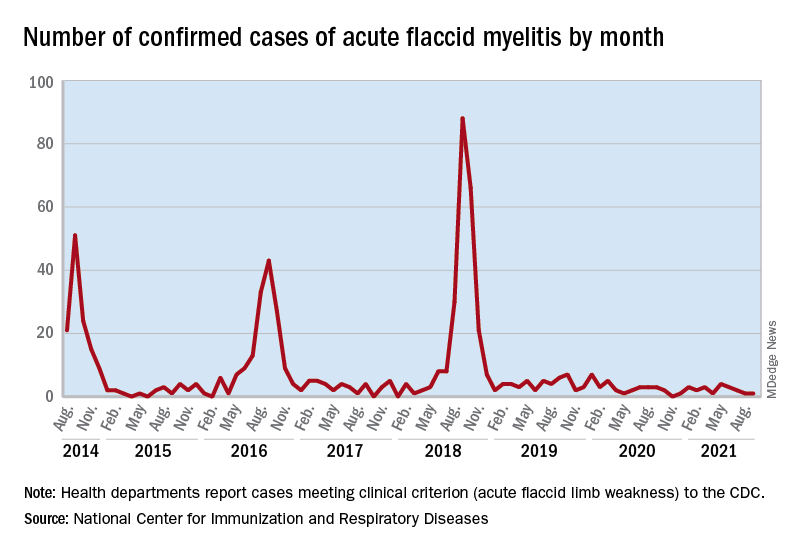
Acute flaccid myelitis (AFM) is an uncommon but serious complication of some viral infections, including West Nile virus and nonpolio enteroviruses. It is “characterized by sudden onset of limb weakness and lesions in the gray matter of the spinal cord,” they said, and more than 90% of cases occur in young children.
Cases of AFM, which can lead to respiratory insufficiency and permanent paralysis, spiked during the late summer and early fall in 2014, 2016, and 2018 and were expected to do so again in 2020, Sarah Kidd, MD, and associates at the division of viral diseases at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta, said in the Morbidity and Mortality Weekly Report.
Monthly peaks in those previous years – each occurring in September – reached 51 cases in 2014, 43 cases in 2016, and 88 cases in 2018, but in 2020 there was only 1 case reported in September, with a high of 4 coming in May, CDC data show. The total number of cases for 2020 (32) was, in fact, lower than in 2019, when 47 were reported.
The investigators’ main objective was to see if there were any differences between the 2018 and 2019-2020 cases. Reports from state health departments to the CDC showed that, in 2019-2020, “patients were older; more likely to have lower limb involvement; and less likely to have upper limb involvement, prodromal illness, [cerebrospinal fluid] pleocytosis, or specimens that tested positive for EV [enterovirus]-D68” than patients from 2018, Dr. Kidd and associates said.
Mask wearing and reduced in-school attendance may have decreased circulation of EV-D68 – the enterovirus type most often detected in the stool and respiratory specimens of AFM patients – as was seen with other respiratory viruses, such as influenza and respiratory syncytial virus, in 2020. Previous studies have suggested that EV-D68 drives the increases in cases during peak years, the researchers noted.
The absence of such an increase “in 2020 reflects a deviation from the previously observed biennial pattern, and it is unclear when the next increase in AFM should be expected. Clinicians should continue to maintain vigilance and suspect AFM in any child with acute flaccid limb weakness, particularly in the setting of recent febrile or respiratory illness,” they wrote.
FROM MMWR