User login
President’s report
As I write, it is 1 degree Fahrenheit and dreary in Kansas City, where I live. That’s minus 17 degrees Celsius for many of you. I hope that it is cheerier and bordering on springtime when you’re reading. You’ll understand, though, why I say Happy 2021! 2020 was a humdinger in many ways.
One of those ways, of course, was the COVID-19 pandemic, which wrought so many things – face masks, social distancing, steep learning curves, over 300,000 excess deaths, and new vaccines. For CHEST, it meant that two of our most important educational opportunities of the year, board review and the annual meeting, were held virtually. Dr. Levine has already written about the board reviews, so I’ll focus on the annual meeting, held in late October.
In many ways, the meeting was a success. We had over 6,800 attendees. There were 88 live online sessions, 22 that were semi-live, and 160 prerecorded sessions. For presenters, this was simultaneously both easy and difficult. They had to ensure that their recording equipment and their Internet access were of sufficient quality, and if prerecorded, the sessions had to be finished weeks ahead of time. But the presentations could be given from presenters’ homes or from their normal work offices. For attendees, the ability for nonsimultaneous playback allowed for fitting the meeting into a work-life schedule. In fact, at least one friend related that he watched sessions with a grandchild on his lap. However, it meant a lack of opportunities to ask clarifying questions of the presenters, which is a common activity at the end of a session, and the opportunity to see and catch up with old friends and colleagues was missing. Simulations, of course, could not be hands-on, but virtual educational games matured significantly. The satisfaction scores from both attendees and faculty were good, if slightly below our usual scores for live meetings. They told us that we all prefer our in-person meetings, but that content is deliverable and receivable in an online format. Overall, we have to consider the CHEST 2020 online platform to be a successful endeavor.
Which brings me to our plans for future meetings. The Board of Regents discussed the alternatives for CHEST 2021. Should we hold a live meeting in Vancouver, as planned? Should we hold another online meeting like the one we just discussed? None of us has the crystal ball that tells us exactly how COVID-19 is going to develop. We don’t know exactly how many people will be vaccinated either north or south of the U.S.-Canada border. While those of us who care for patients in the United States have had the opportunity to be vaccinated, we don’t know if the professional staff from CHEST headquarters who travel to the annual meeting will be vaccinated, even though that prospect is currently looking very reasonable. We don’t know if the Canadian government will be allowing U.S. residents to visit Canada without quarantine. There are just quite a few things that we can’t know. However, convention centers need to know if we will be there, and we needed to decide.
In the end, a couple of things swayed us—the unexpected availability of a U.S. convention center and uncertainty about travel to Canada. We are planning to hold CHEST 2021 in Orlando, Florida, during our usual late October time frame. CHEST 2021 is slated to be the first in-person pulmonary, critical care, and sleep conference to be held in the United States in 2 years. The Executive Program Committee has met, and program selections have been made. Very soon, invitations will go to our prospective faculty, and we will be underway. We are planning CHEST 2021 as what we call a “hybrid” meeting, a meeting that will provide an excellent experience whether one attends in person at the Orlando Convention Center or partakes of the meeting from home. Some sessions will be broadcast live and others will be prerecorded. Needless to say, the experience will not be equal for in-person and at-home learners, but it will be equitable. Regardless of how you choose to partake, CHEST 2021 will have excellent content to suit your needs. This plan also allows us the ability to convert to a fully online meeting, should the COVID-19 circumstances dictate that we must. Having sat in on the program committee meetings, I am excited about what we have to offer. So, dig around and find your old mouse ears or your red forehead scar. CHEST 2021 will be a dynamite experience for us all to share.
Our board review sessions, which are also among the most highly valued of CHEST activities, will be different out of necessity. Again, decisions had to be made many months ahead of time, and we have chosen to hold our board reviews online again this year. COVID-19 uncertainties certainly play into our decision to not put attendees in a room together. However, the ability to play and replay, slow down and speed up video content, and ability to watch any session any time are all well suited to reviewing for an examination. We think this is the appropriate decision for 2021, but we may be back together again for future sessions. Frankly, we are listening to hear which format our attendees like more. And, we are plotting how to make the online platform review even better.
The Board of Regents has been hard at work on a lot of fronts, but I want to focus on one of them, for now. It is important to the Board of Regents and to me, personally, that CHEST be the single most inclusive and diverse professional medical society, bar none. It is of utmost importance that we remove any barriers that might have inadvertently been put into place that would hamper the success of any of our members or their patients. In other words, we hope to find any implicit biases in attitude and behavior and to illuminate and remedy them. We have begun the process by focusing on what CHEST is all about – making a difference with our patients and corporate self and being an inclusive and diverse professional organization.
We believe that we must look at ourselves in three separate, but related, ways. We must examine our patient-facing side and the ways in which we help our members to serve their patients. We must examine our headquarters and our hiring, working, and promoting practices to ensure an inclusive and welcoming environment for the staff who do our day to day business. Finally, we must examine ourselves and our member-based organization, to ensure that all can participate freely in CHEST opportunities and, for those who aspire to lead our organization, to ensure that there are no implicit biases that hold them back.
We began the process with a series of regional listening sessions across the United States, sponsored by the CHEST Foundation, in which we heard from both patients and community leaders of color. We learned of challenges that our patients face in accessing care, communicating with their doctors, and obtaining the medications they need for their illness. Our professional staff has organized an anti-racism task force and is working to ensure that we can be proud of a diverse and inclusive work environment. For our members, we have held two board development sessions, so that our Board of Regents can examine us and our attitudes toward race and toward inclusiveness in our organization. We will soon be holding a listening session with CHEST members of color with the express purpose of allowing those of us who are not persons of color to better understand the challenges faced by our members and to understand where organizational changes could be necessary to help make their professional lives better. As a long time CHEST member, I believe that CHEST is not purposefully exclusive of anyone. We are, nevertheless, a part of the larger fabric of society, and because of that, we are subject to having implicit biases and practices as an organization. Our best path to be aware of them and to deal with them is to hear from our members who experience them, and we shall.
I will end on a note that is somber but important. In the past year, we have all lost friends and colleagues with whom we worked side by side, to COVID-19. Many of them have been CHEST members. Because of the pandemic, we have often not been able to mourn those we have cared about in the same ways that we normally would, in the company of friends and family. Yet, it is important for us to remember our colleagues and to share our memories. So, we established CHEST Remembers, a memorial wall on the CHEST website where we can post the news of our friends’ passing, along with our remembrances of them. If your friend or colleague has died of COVID-19, please feel free to share with the CHEST community. You can find the link to do that at www.chestnet.org.
As I write, it is 1 degree Fahrenheit and dreary in Kansas City, where I live. That’s minus 17 degrees Celsius for many of you. I hope that it is cheerier and bordering on springtime when you’re reading. You’ll understand, though, why I say Happy 2021! 2020 was a humdinger in many ways.
One of those ways, of course, was the COVID-19 pandemic, which wrought so many things – face masks, social distancing, steep learning curves, over 300,000 excess deaths, and new vaccines. For CHEST, it meant that two of our most important educational opportunities of the year, board review and the annual meeting, were held virtually. Dr. Levine has already written about the board reviews, so I’ll focus on the annual meeting, held in late October.
In many ways, the meeting was a success. We had over 6,800 attendees. There were 88 live online sessions, 22 that were semi-live, and 160 prerecorded sessions. For presenters, this was simultaneously both easy and difficult. They had to ensure that their recording equipment and their Internet access were of sufficient quality, and if prerecorded, the sessions had to be finished weeks ahead of time. But the presentations could be given from presenters’ homes or from their normal work offices. For attendees, the ability for nonsimultaneous playback allowed for fitting the meeting into a work-life schedule. In fact, at least one friend related that he watched sessions with a grandchild on his lap. However, it meant a lack of opportunities to ask clarifying questions of the presenters, which is a common activity at the end of a session, and the opportunity to see and catch up with old friends and colleagues was missing. Simulations, of course, could not be hands-on, but virtual educational games matured significantly. The satisfaction scores from both attendees and faculty were good, if slightly below our usual scores for live meetings. They told us that we all prefer our in-person meetings, but that content is deliverable and receivable in an online format. Overall, we have to consider the CHEST 2020 online platform to be a successful endeavor.
Which brings me to our plans for future meetings. The Board of Regents discussed the alternatives for CHEST 2021. Should we hold a live meeting in Vancouver, as planned? Should we hold another online meeting like the one we just discussed? None of us has the crystal ball that tells us exactly how COVID-19 is going to develop. We don’t know exactly how many people will be vaccinated either north or south of the U.S.-Canada border. While those of us who care for patients in the United States have had the opportunity to be vaccinated, we don’t know if the professional staff from CHEST headquarters who travel to the annual meeting will be vaccinated, even though that prospect is currently looking very reasonable. We don’t know if the Canadian government will be allowing U.S. residents to visit Canada without quarantine. There are just quite a few things that we can’t know. However, convention centers need to know if we will be there, and we needed to decide.
In the end, a couple of things swayed us—the unexpected availability of a U.S. convention center and uncertainty about travel to Canada. We are planning to hold CHEST 2021 in Orlando, Florida, during our usual late October time frame. CHEST 2021 is slated to be the first in-person pulmonary, critical care, and sleep conference to be held in the United States in 2 years. The Executive Program Committee has met, and program selections have been made. Very soon, invitations will go to our prospective faculty, and we will be underway. We are planning CHEST 2021 as what we call a “hybrid” meeting, a meeting that will provide an excellent experience whether one attends in person at the Orlando Convention Center or partakes of the meeting from home. Some sessions will be broadcast live and others will be prerecorded. Needless to say, the experience will not be equal for in-person and at-home learners, but it will be equitable. Regardless of how you choose to partake, CHEST 2021 will have excellent content to suit your needs. This plan also allows us the ability to convert to a fully online meeting, should the COVID-19 circumstances dictate that we must. Having sat in on the program committee meetings, I am excited about what we have to offer. So, dig around and find your old mouse ears or your red forehead scar. CHEST 2021 will be a dynamite experience for us all to share.
Our board review sessions, which are also among the most highly valued of CHEST activities, will be different out of necessity. Again, decisions had to be made many months ahead of time, and we have chosen to hold our board reviews online again this year. COVID-19 uncertainties certainly play into our decision to not put attendees in a room together. However, the ability to play and replay, slow down and speed up video content, and ability to watch any session any time are all well suited to reviewing for an examination. We think this is the appropriate decision for 2021, but we may be back together again for future sessions. Frankly, we are listening to hear which format our attendees like more. And, we are plotting how to make the online platform review even better.
The Board of Regents has been hard at work on a lot of fronts, but I want to focus on one of them, for now. It is important to the Board of Regents and to me, personally, that CHEST be the single most inclusive and diverse professional medical society, bar none. It is of utmost importance that we remove any barriers that might have inadvertently been put into place that would hamper the success of any of our members or their patients. In other words, we hope to find any implicit biases in attitude and behavior and to illuminate and remedy them. We have begun the process by focusing on what CHEST is all about – making a difference with our patients and corporate self and being an inclusive and diverse professional organization.
We believe that we must look at ourselves in three separate, but related, ways. We must examine our patient-facing side and the ways in which we help our members to serve their patients. We must examine our headquarters and our hiring, working, and promoting practices to ensure an inclusive and welcoming environment for the staff who do our day to day business. Finally, we must examine ourselves and our member-based organization, to ensure that all can participate freely in CHEST opportunities and, for those who aspire to lead our organization, to ensure that there are no implicit biases that hold them back.
We began the process with a series of regional listening sessions across the United States, sponsored by the CHEST Foundation, in which we heard from both patients and community leaders of color. We learned of challenges that our patients face in accessing care, communicating with their doctors, and obtaining the medications they need for their illness. Our professional staff has organized an anti-racism task force and is working to ensure that we can be proud of a diverse and inclusive work environment. For our members, we have held two board development sessions, so that our Board of Regents can examine us and our attitudes toward race and toward inclusiveness in our organization. We will soon be holding a listening session with CHEST members of color with the express purpose of allowing those of us who are not persons of color to better understand the challenges faced by our members and to understand where organizational changes could be necessary to help make their professional lives better. As a long time CHEST member, I believe that CHEST is not purposefully exclusive of anyone. We are, nevertheless, a part of the larger fabric of society, and because of that, we are subject to having implicit biases and practices as an organization. Our best path to be aware of them and to deal with them is to hear from our members who experience them, and we shall.
I will end on a note that is somber but important. In the past year, we have all lost friends and colleagues with whom we worked side by side, to COVID-19. Many of them have been CHEST members. Because of the pandemic, we have often not been able to mourn those we have cared about in the same ways that we normally would, in the company of friends and family. Yet, it is important for us to remember our colleagues and to share our memories. So, we established CHEST Remembers, a memorial wall on the CHEST website where we can post the news of our friends’ passing, along with our remembrances of them. If your friend or colleague has died of COVID-19, please feel free to share with the CHEST community. You can find the link to do that at www.chestnet.org.
As I write, it is 1 degree Fahrenheit and dreary in Kansas City, where I live. That’s minus 17 degrees Celsius for many of you. I hope that it is cheerier and bordering on springtime when you’re reading. You’ll understand, though, why I say Happy 2021! 2020 was a humdinger in many ways.
One of those ways, of course, was the COVID-19 pandemic, which wrought so many things – face masks, social distancing, steep learning curves, over 300,000 excess deaths, and new vaccines. For CHEST, it meant that two of our most important educational opportunities of the year, board review and the annual meeting, were held virtually. Dr. Levine has already written about the board reviews, so I’ll focus on the annual meeting, held in late October.
In many ways, the meeting was a success. We had over 6,800 attendees. There were 88 live online sessions, 22 that were semi-live, and 160 prerecorded sessions. For presenters, this was simultaneously both easy and difficult. They had to ensure that their recording equipment and their Internet access were of sufficient quality, and if prerecorded, the sessions had to be finished weeks ahead of time. But the presentations could be given from presenters’ homes or from their normal work offices. For attendees, the ability for nonsimultaneous playback allowed for fitting the meeting into a work-life schedule. In fact, at least one friend related that he watched sessions with a grandchild on his lap. However, it meant a lack of opportunities to ask clarifying questions of the presenters, which is a common activity at the end of a session, and the opportunity to see and catch up with old friends and colleagues was missing. Simulations, of course, could not be hands-on, but virtual educational games matured significantly. The satisfaction scores from both attendees and faculty were good, if slightly below our usual scores for live meetings. They told us that we all prefer our in-person meetings, but that content is deliverable and receivable in an online format. Overall, we have to consider the CHEST 2020 online platform to be a successful endeavor.
Which brings me to our plans for future meetings. The Board of Regents discussed the alternatives for CHEST 2021. Should we hold a live meeting in Vancouver, as planned? Should we hold another online meeting like the one we just discussed? None of us has the crystal ball that tells us exactly how COVID-19 is going to develop. We don’t know exactly how many people will be vaccinated either north or south of the U.S.-Canada border. While those of us who care for patients in the United States have had the opportunity to be vaccinated, we don’t know if the professional staff from CHEST headquarters who travel to the annual meeting will be vaccinated, even though that prospect is currently looking very reasonable. We don’t know if the Canadian government will be allowing U.S. residents to visit Canada without quarantine. There are just quite a few things that we can’t know. However, convention centers need to know if we will be there, and we needed to decide.
In the end, a couple of things swayed us—the unexpected availability of a U.S. convention center and uncertainty about travel to Canada. We are planning to hold CHEST 2021 in Orlando, Florida, during our usual late October time frame. CHEST 2021 is slated to be the first in-person pulmonary, critical care, and sleep conference to be held in the United States in 2 years. The Executive Program Committee has met, and program selections have been made. Very soon, invitations will go to our prospective faculty, and we will be underway. We are planning CHEST 2021 as what we call a “hybrid” meeting, a meeting that will provide an excellent experience whether one attends in person at the Orlando Convention Center or partakes of the meeting from home. Some sessions will be broadcast live and others will be prerecorded. Needless to say, the experience will not be equal for in-person and at-home learners, but it will be equitable. Regardless of how you choose to partake, CHEST 2021 will have excellent content to suit your needs. This plan also allows us the ability to convert to a fully online meeting, should the COVID-19 circumstances dictate that we must. Having sat in on the program committee meetings, I am excited about what we have to offer. So, dig around and find your old mouse ears or your red forehead scar. CHEST 2021 will be a dynamite experience for us all to share.
Our board review sessions, which are also among the most highly valued of CHEST activities, will be different out of necessity. Again, decisions had to be made many months ahead of time, and we have chosen to hold our board reviews online again this year. COVID-19 uncertainties certainly play into our decision to not put attendees in a room together. However, the ability to play and replay, slow down and speed up video content, and ability to watch any session any time are all well suited to reviewing for an examination. We think this is the appropriate decision for 2021, but we may be back together again for future sessions. Frankly, we are listening to hear which format our attendees like more. And, we are plotting how to make the online platform review even better.
The Board of Regents has been hard at work on a lot of fronts, but I want to focus on one of them, for now. It is important to the Board of Regents and to me, personally, that CHEST be the single most inclusive and diverse professional medical society, bar none. It is of utmost importance that we remove any barriers that might have inadvertently been put into place that would hamper the success of any of our members or their patients. In other words, we hope to find any implicit biases in attitude and behavior and to illuminate and remedy them. We have begun the process by focusing on what CHEST is all about – making a difference with our patients and corporate self and being an inclusive and diverse professional organization.
We believe that we must look at ourselves in three separate, but related, ways. We must examine our patient-facing side and the ways in which we help our members to serve their patients. We must examine our headquarters and our hiring, working, and promoting practices to ensure an inclusive and welcoming environment for the staff who do our day to day business. Finally, we must examine ourselves and our member-based organization, to ensure that all can participate freely in CHEST opportunities and, for those who aspire to lead our organization, to ensure that there are no implicit biases that hold them back.
We began the process with a series of regional listening sessions across the United States, sponsored by the CHEST Foundation, in which we heard from both patients and community leaders of color. We learned of challenges that our patients face in accessing care, communicating with their doctors, and obtaining the medications they need for their illness. Our professional staff has organized an anti-racism task force and is working to ensure that we can be proud of a diverse and inclusive work environment. For our members, we have held two board development sessions, so that our Board of Regents can examine us and our attitudes toward race and toward inclusiveness in our organization. We will soon be holding a listening session with CHEST members of color with the express purpose of allowing those of us who are not persons of color to better understand the challenges faced by our members and to understand where organizational changes could be necessary to help make their professional lives better. As a long time CHEST member, I believe that CHEST is not purposefully exclusive of anyone. We are, nevertheless, a part of the larger fabric of society, and because of that, we are subject to having implicit biases and practices as an organization. Our best path to be aware of them and to deal with them is to hear from our members who experience them, and we shall.
I will end on a note that is somber but important. In the past year, we have all lost friends and colleagues with whom we worked side by side, to COVID-19. Many of them have been CHEST members. Because of the pandemic, we have often not been able to mourn those we have cared about in the same ways that we normally would, in the company of friends and family. Yet, it is important for us to remember our colleagues and to share our memories. So, we established CHEST Remembers, a memorial wall on the CHEST website where we can post the news of our friends’ passing, along with our remembrances of them. If your friend or colleague has died of COVID-19, please feel free to share with the CHEST community. You can find the link to do that at www.chestnet.org.
CHEST to offer research matching service
CHEST Analytics has announced its new resource for members interested in serving as investigators in industry-sponsored clinical trials.
The new program, CHEST Clinical Trials Solutions, will pair members who have indicated their interest in specific research topics with companies seeking investigators. According to CHEST President Steven Q. Simpson, MD, FCCP: “For members who would like to be involved in research and for companies that have defined distinct criteria for their studies, CHEST Analytics can pair qualifying parties to facilitate communication between researcher and sponsor. It’s a great way for young investigators to get started or accomplished members to share their experience while helping industry expedite introducing new products that improve patient care.” More information regarding enrollment will be available at info.chestnet.org/clinical-trials.
CHEST Analytics has announced its new resource for members interested in serving as investigators in industry-sponsored clinical trials.
The new program, CHEST Clinical Trials Solutions, will pair members who have indicated their interest in specific research topics with companies seeking investigators. According to CHEST President Steven Q. Simpson, MD, FCCP: “For members who would like to be involved in research and for companies that have defined distinct criteria for their studies, CHEST Analytics can pair qualifying parties to facilitate communication between researcher and sponsor. It’s a great way for young investigators to get started or accomplished members to share their experience while helping industry expedite introducing new products that improve patient care.” More information regarding enrollment will be available at info.chestnet.org/clinical-trials.
CHEST Analytics has announced its new resource for members interested in serving as investigators in industry-sponsored clinical trials.
The new program, CHEST Clinical Trials Solutions, will pair members who have indicated their interest in specific research topics with companies seeking investigators. According to CHEST President Steven Q. Simpson, MD, FCCP: “For members who would like to be involved in research and for companies that have defined distinct criteria for their studies, CHEST Analytics can pair qualifying parties to facilitate communication between researcher and sponsor. It’s a great way for young investigators to get started or accomplished members to share their experience while helping industry expedite introducing new products that improve patient care.” More information regarding enrollment will be available at info.chestnet.org/clinical-trials.
President-Designate: Doreen J. Addrizzo-Harris, MD, FCCP
Doreen J. Addrizzo-Harris, MD, FCCP, is a pulmonary/critical care physician with an extensive background in bronchiectasis and non-tuberculous mycobacterial infection and medical education.
Dr. Addrizzo-Harris is currently a Professor of Medicine at the NYU Grossman School of Medicine. She serves as the Associate Division Director for Clinical and Faculty Affairs, is the Director of the NYU Bronchiectasis and NTM Program, and is Co-Director of the NYU Pulmonary Faculty Practice. She is now serving in her 20th year as the Program Director of NYU's Pulmonary and Critical Care Medicine Fellowship. Dr. Addrizzo-Harris received her medical degree and completed her residency and fellowship training at New York University School of Medicine. Since completing her training, she was recruited to stay as a faculty member at NYU, where she has been a critical presence over the past 25 years. She has been instrumental in educating the next generation of pulmonary/critical care physicians and has won a number of awards for her teaching skills, most recently, the 2021 Outstanding Educator Award from the APCCMPD. Dr. Addrizzo-Harris has served on the board of the Association of Pulmonary and Critical Care Medicine Program Directors (APCCMPD), including serving as President from 2006-2007. Academically, she authored 44 peer-reviewed publications and 57 scientific abstracts presented at international conferences. She has participated in numerous clinical trials, many as PI. Dr. Addrizzo-Harris has been recognized as a Distinguished CHEST Educator each year since its inception in 2017 and received the Distinguished Service Award in 2019.
During her leadership tenure with CHEST, Dr. Addrizzo-Harris has served on the Marketing Committee, the Health and Science Policy Committee (Chair from 2007-2009), Government Relations Committee, Scientific Program Committee, Education Committee, Governance Committee, Editorial Board for CHEST Physician, Professional Standards Committee (Chair 2016-2018), Board of Regents, and CHEST Foundation Board of Trustees. Most recently, Dr. Addrizzo-Harris served as the President of the CHEST Foundation from 2018-2019 and Co-Chair of the Foundation Awards Committee from 2015-2020. She will serve as the sixth woman to lead the American College of Chest Physicians.
Doreen J. Addrizzo-Harris, MD, FCCP, is a pulmonary/critical care physician with an extensive background in bronchiectasis and non-tuberculous mycobacterial infection and medical education.
Dr. Addrizzo-Harris is currently a Professor of Medicine at the NYU Grossman School of Medicine. She serves as the Associate Division Director for Clinical and Faculty Affairs, is the Director of the NYU Bronchiectasis and NTM Program, and is Co-Director of the NYU Pulmonary Faculty Practice. She is now serving in her 20th year as the Program Director of NYU's Pulmonary and Critical Care Medicine Fellowship. Dr. Addrizzo-Harris received her medical degree and completed her residency and fellowship training at New York University School of Medicine. Since completing her training, she was recruited to stay as a faculty member at NYU, where she has been a critical presence over the past 25 years. She has been instrumental in educating the next generation of pulmonary/critical care physicians and has won a number of awards for her teaching skills, most recently, the 2021 Outstanding Educator Award from the APCCMPD. Dr. Addrizzo-Harris has served on the board of the Association of Pulmonary and Critical Care Medicine Program Directors (APCCMPD), including serving as President from 2006-2007. Academically, she authored 44 peer-reviewed publications and 57 scientific abstracts presented at international conferences. She has participated in numerous clinical trials, many as PI. Dr. Addrizzo-Harris has been recognized as a Distinguished CHEST Educator each year since its inception in 2017 and received the Distinguished Service Award in 2019.
During her leadership tenure with CHEST, Dr. Addrizzo-Harris has served on the Marketing Committee, the Health and Science Policy Committee (Chair from 2007-2009), Government Relations Committee, Scientific Program Committee, Education Committee, Governance Committee, Editorial Board for CHEST Physician, Professional Standards Committee (Chair 2016-2018), Board of Regents, and CHEST Foundation Board of Trustees. Most recently, Dr. Addrizzo-Harris served as the President of the CHEST Foundation from 2018-2019 and Co-Chair of the Foundation Awards Committee from 2015-2020. She will serve as the sixth woman to lead the American College of Chest Physicians.
Doreen J. Addrizzo-Harris, MD, FCCP, is a pulmonary/critical care physician with an extensive background in bronchiectasis and non-tuberculous mycobacterial infection and medical education.
Dr. Addrizzo-Harris is currently a Professor of Medicine at the NYU Grossman School of Medicine. She serves as the Associate Division Director for Clinical and Faculty Affairs, is the Director of the NYU Bronchiectasis and NTM Program, and is Co-Director of the NYU Pulmonary Faculty Practice. She is now serving in her 20th year as the Program Director of NYU's Pulmonary and Critical Care Medicine Fellowship. Dr. Addrizzo-Harris received her medical degree and completed her residency and fellowship training at New York University School of Medicine. Since completing her training, she was recruited to stay as a faculty member at NYU, where she has been a critical presence over the past 25 years. She has been instrumental in educating the next generation of pulmonary/critical care physicians and has won a number of awards for her teaching skills, most recently, the 2021 Outstanding Educator Award from the APCCMPD. Dr. Addrizzo-Harris has served on the board of the Association of Pulmonary and Critical Care Medicine Program Directors (APCCMPD), including serving as President from 2006-2007. Academically, she authored 44 peer-reviewed publications and 57 scientific abstracts presented at international conferences. She has participated in numerous clinical trials, many as PI. Dr. Addrizzo-Harris has been recognized as a Distinguished CHEST Educator each year since its inception in 2017 and received the Distinguished Service Award in 2019.
During her leadership tenure with CHEST, Dr. Addrizzo-Harris has served on the Marketing Committee, the Health and Science Policy Committee (Chair from 2007-2009), Government Relations Committee, Scientific Program Committee, Education Committee, Governance Committee, Editorial Board for CHEST Physician, Professional Standards Committee (Chair 2016-2018), Board of Regents, and CHEST Foundation Board of Trustees. Most recently, Dr. Addrizzo-Harris served as the President of the CHEST Foundation from 2018-2019 and Co-Chair of the Foundation Awards Committee from 2015-2020. She will serve as the sixth woman to lead the American College of Chest Physicians.
Two popular screening tests for gestational diabetes clinically equivalent
Broadening the diagnosis of gestational diabetes mellitus (GDM) with a one-step screening approach does not lead to significant differences in maternal or perinatal outcomes, compared with a two-step approach. Investigators reported these findings in the New England Journal of Medicine after testing the two screening methods in more than 23,000 pregnant women.
GDM affects 6%-25% of pregnant women, increasing the risk of neonatal death and stillborn births. It can also lead to serious complications such as fetal overgrowth. Clinical guidelines recommend GDM screening between 24 and 28 weeks’ gestation to improve outcomes in mothers and infants. However, the scientific community has struggled to reach a consensus on testing approach.
For decades, clinicians used a two-step screening approach: a nonfasting 1-hour glucose challenge test and a longer 3-hour fasting oral glucose tolerance test to diagnose GDM; roughly 20% who test positive on this glucose challenge test require the second step. Results of a large study led to new diagnostic criteria on a one-step 75-g oral glucose tolerance test. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study “found a linear relationship with hyperglycemia and outcomes – the higher the glucose, the worse the outcomes,” said Teresa Hillier, MD, MS, an endocrinologist and investigator with Kaiser Permanente Center for Health Research Northwest and CHR-Hawaii. The International Association of the Diabetes and Pregnancy Study Groups (IADPSG) made a clinical recommendation on the one-step approach, now a common screening tool in the United States.
A focus on rare GDM outcomes
The IADPSG fasting one-step criteria typically identifies women with milder symptoms as having gestational diabetes, a factor expected to increase diagnosis rates by two- or threefold, said Dr. Hillier. “The unknown question was whether diagnosing and treating more women would be associated with any differences in any of the multiple GDM-associated outcomes for mother and baby.”
She and her colleagues conducted a large-scale randomized trial at two Kaiser sites to assess multiple maternal and perinatal outcomes including rare but important GDM-associated outcomes such as stillbirth and neonatal death between the two screening methods.
They randomized 23,792 pregnant women 1:1 to the one- or two-step gestational diabetes test at their first prenatal visit. Primary outcomes included diagnosis of gestational diabetes; large-for-gestational-age infants; primary cesarean section, and gestational hypertension or preeclampsia; and a composite perinatal outcome of any stillbirth, neonatal death, shoulder dystocia, bone fracture, or arm or hand nerve palsy related to birth injury.
Most participants (94%) completed screening, although there was lower adherence to screening in the one-step approach. The reasons for this aren’t entirely clear, said Dr. Hillier. Convenience may be a factor; patients have to fast for several hours to complete the one-step test, whereas the first test of the two-step screening approach can be done at any time of day, and most patients pass this test.
Corroborating HAPO’s results, twice as many women in the one-step group (16.5%) received a GDM diagnosis, compared with 8.5% in the two-step group (unadjusted relative risk, 1.94; 97.5% confidence interval, 1.79-2.11). However, for the other primary outcomes, investigators found no significant differences in incidences or unadjusted risks. Perinatal composite outcomes for the one- and two-step groups were 3.1% and 3.0%, respectively, and primary cesarean section outcomes were 24.0% and 24.6%.
In the one-step group, 8.9% experienced large-for-gestational-age infants outcomes, compared with 9.2% in the two-step group (RR, 0.95; 97.5% CI, 0.87-1.05). Among those diagnosed with gestational diabetes, similar percentages of women in the one- and two-step groups received insulin or hypoglycemic medication (42.6% and 45.6%, respectively).
Dr. Hillier and colleagues also reported comparable results among the two groups on safety outcomes and secondary outcomes such as macrosomia incidence, small-for-gestational-age infants, and factors such as neonatal hypoglycemia and respiratory distress.
“Although we did not find increased harms associated with the diagnosis and treatment of gestational diabetes in many more women with the one-step approach, some retrospective observational cohort studies have shown higher incidences of primary cesarean delivery and neonatal hypoglycemia with one-step screening after conversion from two-step protocols, with no substantive improvement in outcomes,” Dr. Hillier and colleagues noted.
The trial had several limitations. Adjustments made to address lower adherence to the one-step approach might not have accounted for all nonadherence differences. Another issue is the two sites didn’t use identical thresholds for the glucose challenge test in the two-step cohort. Demographically, the study lacked Black and American Indian representation.
“Moreover, the potential long-term benefits of increased diagnoses of gestational diabetes – such as the identification of more women at high risk for subsequent diabetes who might benefit from risk-reduction strategies – were not addressed by the trial,” Brian Casey, MD, wrote in a related editorial. Based on the study’s findings, “the perinatal benefits of the diagnosis of gestational diabetes with the use of the IADPSG single-step approach appear to be insufficient to justify the associated patient and health care costs of broadening the diagnosis” of GDM, added Dr. Casey, a professor with the department of obstetrics and gynecology at the University of Alabama at Birmingham.
U.S. doctors unlikely to change behaviors
Most U.S. physicians favor the two-step method. This has been a huge controversy worldwide, with other countries pushing the United States to use the one-step method, Vincenzo Berghella, MD, a professor with Thomas Jefferson University, Philadelphia, said in an interview. “I expect this study will increase the divide between the U.S. and the rest of the world,” since U.S. physicians will see no benefit to the one-step method, and continue to use the two-step method.
It’s not surprising that GDM diagnosis incidence went up to 16.5% with the inclusion of the one-step test, compared with 8.5% with the two-step test, Dr. Berghella continued. What’s less clear, are the details of treatment among the 8% diagnosed to have GDM with the one-step test, but not the two-step test.
These women were likely to have milder degrees of insulin resistance or GDM. Dr. Berghella, who has advocated in the past for the one-step approach, said it would be important to find out if these women, who test positive at the one-step test but would test negative at the two-step test, were treated properly with diet, exercise, and possibly insulin or other hypoglycemic agents for their mild degree of insulin resistance. The researchers concluded that expanding the definition of GDM through the one-step test didn’t make a difference. However, “it’s not just the test that will make the difference in maternal and baby outcomes, but the aggressive management of diabetes with diet, exercise, and medications as needed once that test comes back abnormal,” he said.
The randomized trial was a massive undertaking, said Dr. Hillier.
“We are still evaluating our future plans,” she added. Forthcoming subgroup analyses from the trial could further help inform clinical practice guidelines.
Dr. Hillier received a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development to support this study. The investigators reported no potential conflict of interest relevant to this article.
Broadening the diagnosis of gestational diabetes mellitus (GDM) with a one-step screening approach does not lead to significant differences in maternal or perinatal outcomes, compared with a two-step approach. Investigators reported these findings in the New England Journal of Medicine after testing the two screening methods in more than 23,000 pregnant women.
GDM affects 6%-25% of pregnant women, increasing the risk of neonatal death and stillborn births. It can also lead to serious complications such as fetal overgrowth. Clinical guidelines recommend GDM screening between 24 and 28 weeks’ gestation to improve outcomes in mothers and infants. However, the scientific community has struggled to reach a consensus on testing approach.
For decades, clinicians used a two-step screening approach: a nonfasting 1-hour glucose challenge test and a longer 3-hour fasting oral glucose tolerance test to diagnose GDM; roughly 20% who test positive on this glucose challenge test require the second step. Results of a large study led to new diagnostic criteria on a one-step 75-g oral glucose tolerance test. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study “found a linear relationship with hyperglycemia and outcomes – the higher the glucose, the worse the outcomes,” said Teresa Hillier, MD, MS, an endocrinologist and investigator with Kaiser Permanente Center for Health Research Northwest and CHR-Hawaii. The International Association of the Diabetes and Pregnancy Study Groups (IADPSG) made a clinical recommendation on the one-step approach, now a common screening tool in the United States.
A focus on rare GDM outcomes
The IADPSG fasting one-step criteria typically identifies women with milder symptoms as having gestational diabetes, a factor expected to increase diagnosis rates by two- or threefold, said Dr. Hillier. “The unknown question was whether diagnosing and treating more women would be associated with any differences in any of the multiple GDM-associated outcomes for mother and baby.”
She and her colleagues conducted a large-scale randomized trial at two Kaiser sites to assess multiple maternal and perinatal outcomes including rare but important GDM-associated outcomes such as stillbirth and neonatal death between the two screening methods.
They randomized 23,792 pregnant women 1:1 to the one- or two-step gestational diabetes test at their first prenatal visit. Primary outcomes included diagnosis of gestational diabetes; large-for-gestational-age infants; primary cesarean section, and gestational hypertension or preeclampsia; and a composite perinatal outcome of any stillbirth, neonatal death, shoulder dystocia, bone fracture, or arm or hand nerve palsy related to birth injury.
Most participants (94%) completed screening, although there was lower adherence to screening in the one-step approach. The reasons for this aren’t entirely clear, said Dr. Hillier. Convenience may be a factor; patients have to fast for several hours to complete the one-step test, whereas the first test of the two-step screening approach can be done at any time of day, and most patients pass this test.
Corroborating HAPO’s results, twice as many women in the one-step group (16.5%) received a GDM diagnosis, compared with 8.5% in the two-step group (unadjusted relative risk, 1.94; 97.5% confidence interval, 1.79-2.11). However, for the other primary outcomes, investigators found no significant differences in incidences or unadjusted risks. Perinatal composite outcomes for the one- and two-step groups were 3.1% and 3.0%, respectively, and primary cesarean section outcomes were 24.0% and 24.6%.
In the one-step group, 8.9% experienced large-for-gestational-age infants outcomes, compared with 9.2% in the two-step group (RR, 0.95; 97.5% CI, 0.87-1.05). Among those diagnosed with gestational diabetes, similar percentages of women in the one- and two-step groups received insulin or hypoglycemic medication (42.6% and 45.6%, respectively).
Dr. Hillier and colleagues also reported comparable results among the two groups on safety outcomes and secondary outcomes such as macrosomia incidence, small-for-gestational-age infants, and factors such as neonatal hypoglycemia and respiratory distress.
“Although we did not find increased harms associated with the diagnosis and treatment of gestational diabetes in many more women with the one-step approach, some retrospective observational cohort studies have shown higher incidences of primary cesarean delivery and neonatal hypoglycemia with one-step screening after conversion from two-step protocols, with no substantive improvement in outcomes,” Dr. Hillier and colleagues noted.
The trial had several limitations. Adjustments made to address lower adherence to the one-step approach might not have accounted for all nonadherence differences. Another issue is the two sites didn’t use identical thresholds for the glucose challenge test in the two-step cohort. Demographically, the study lacked Black and American Indian representation.
“Moreover, the potential long-term benefits of increased diagnoses of gestational diabetes – such as the identification of more women at high risk for subsequent diabetes who might benefit from risk-reduction strategies – were not addressed by the trial,” Brian Casey, MD, wrote in a related editorial. Based on the study’s findings, “the perinatal benefits of the diagnosis of gestational diabetes with the use of the IADPSG single-step approach appear to be insufficient to justify the associated patient and health care costs of broadening the diagnosis” of GDM, added Dr. Casey, a professor with the department of obstetrics and gynecology at the University of Alabama at Birmingham.
U.S. doctors unlikely to change behaviors
Most U.S. physicians favor the two-step method. This has been a huge controversy worldwide, with other countries pushing the United States to use the one-step method, Vincenzo Berghella, MD, a professor with Thomas Jefferson University, Philadelphia, said in an interview. “I expect this study will increase the divide between the U.S. and the rest of the world,” since U.S. physicians will see no benefit to the one-step method, and continue to use the two-step method.
It’s not surprising that GDM diagnosis incidence went up to 16.5% with the inclusion of the one-step test, compared with 8.5% with the two-step test, Dr. Berghella continued. What’s less clear, are the details of treatment among the 8% diagnosed to have GDM with the one-step test, but not the two-step test.
These women were likely to have milder degrees of insulin resistance or GDM. Dr. Berghella, who has advocated in the past for the one-step approach, said it would be important to find out if these women, who test positive at the one-step test but would test negative at the two-step test, were treated properly with diet, exercise, and possibly insulin or other hypoglycemic agents for their mild degree of insulin resistance. The researchers concluded that expanding the definition of GDM through the one-step test didn’t make a difference. However, “it’s not just the test that will make the difference in maternal and baby outcomes, but the aggressive management of diabetes with diet, exercise, and medications as needed once that test comes back abnormal,” he said.
The randomized trial was a massive undertaking, said Dr. Hillier.
“We are still evaluating our future plans,” she added. Forthcoming subgroup analyses from the trial could further help inform clinical practice guidelines.
Dr. Hillier received a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development to support this study. The investigators reported no potential conflict of interest relevant to this article.
Broadening the diagnosis of gestational diabetes mellitus (GDM) with a one-step screening approach does not lead to significant differences in maternal or perinatal outcomes, compared with a two-step approach. Investigators reported these findings in the New England Journal of Medicine after testing the two screening methods in more than 23,000 pregnant women.
GDM affects 6%-25% of pregnant women, increasing the risk of neonatal death and stillborn births. It can also lead to serious complications such as fetal overgrowth. Clinical guidelines recommend GDM screening between 24 and 28 weeks’ gestation to improve outcomes in mothers and infants. However, the scientific community has struggled to reach a consensus on testing approach.
For decades, clinicians used a two-step screening approach: a nonfasting 1-hour glucose challenge test and a longer 3-hour fasting oral glucose tolerance test to diagnose GDM; roughly 20% who test positive on this glucose challenge test require the second step. Results of a large study led to new diagnostic criteria on a one-step 75-g oral glucose tolerance test. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study “found a linear relationship with hyperglycemia and outcomes – the higher the glucose, the worse the outcomes,” said Teresa Hillier, MD, MS, an endocrinologist and investigator with Kaiser Permanente Center for Health Research Northwest and CHR-Hawaii. The International Association of the Diabetes and Pregnancy Study Groups (IADPSG) made a clinical recommendation on the one-step approach, now a common screening tool in the United States.
A focus on rare GDM outcomes
The IADPSG fasting one-step criteria typically identifies women with milder symptoms as having gestational diabetes, a factor expected to increase diagnosis rates by two- or threefold, said Dr. Hillier. “The unknown question was whether diagnosing and treating more women would be associated with any differences in any of the multiple GDM-associated outcomes for mother and baby.”
She and her colleagues conducted a large-scale randomized trial at two Kaiser sites to assess multiple maternal and perinatal outcomes including rare but important GDM-associated outcomes such as stillbirth and neonatal death between the two screening methods.
They randomized 23,792 pregnant women 1:1 to the one- or two-step gestational diabetes test at their first prenatal visit. Primary outcomes included diagnosis of gestational diabetes; large-for-gestational-age infants; primary cesarean section, and gestational hypertension or preeclampsia; and a composite perinatal outcome of any stillbirth, neonatal death, shoulder dystocia, bone fracture, or arm or hand nerve palsy related to birth injury.
Most participants (94%) completed screening, although there was lower adherence to screening in the one-step approach. The reasons for this aren’t entirely clear, said Dr. Hillier. Convenience may be a factor; patients have to fast for several hours to complete the one-step test, whereas the first test of the two-step screening approach can be done at any time of day, and most patients pass this test.
Corroborating HAPO’s results, twice as many women in the one-step group (16.5%) received a GDM diagnosis, compared with 8.5% in the two-step group (unadjusted relative risk, 1.94; 97.5% confidence interval, 1.79-2.11). However, for the other primary outcomes, investigators found no significant differences in incidences or unadjusted risks. Perinatal composite outcomes for the one- and two-step groups were 3.1% and 3.0%, respectively, and primary cesarean section outcomes were 24.0% and 24.6%.
In the one-step group, 8.9% experienced large-for-gestational-age infants outcomes, compared with 9.2% in the two-step group (RR, 0.95; 97.5% CI, 0.87-1.05). Among those diagnosed with gestational diabetes, similar percentages of women in the one- and two-step groups received insulin or hypoglycemic medication (42.6% and 45.6%, respectively).
Dr. Hillier and colleagues also reported comparable results among the two groups on safety outcomes and secondary outcomes such as macrosomia incidence, small-for-gestational-age infants, and factors such as neonatal hypoglycemia and respiratory distress.
“Although we did not find increased harms associated with the diagnosis and treatment of gestational diabetes in many more women with the one-step approach, some retrospective observational cohort studies have shown higher incidences of primary cesarean delivery and neonatal hypoglycemia with one-step screening after conversion from two-step protocols, with no substantive improvement in outcomes,” Dr. Hillier and colleagues noted.
The trial had several limitations. Adjustments made to address lower adherence to the one-step approach might not have accounted for all nonadherence differences. Another issue is the two sites didn’t use identical thresholds for the glucose challenge test in the two-step cohort. Demographically, the study lacked Black and American Indian representation.
“Moreover, the potential long-term benefits of increased diagnoses of gestational diabetes – such as the identification of more women at high risk for subsequent diabetes who might benefit from risk-reduction strategies – were not addressed by the trial,” Brian Casey, MD, wrote in a related editorial. Based on the study’s findings, “the perinatal benefits of the diagnosis of gestational diabetes with the use of the IADPSG single-step approach appear to be insufficient to justify the associated patient and health care costs of broadening the diagnosis” of GDM, added Dr. Casey, a professor with the department of obstetrics and gynecology at the University of Alabama at Birmingham.
U.S. doctors unlikely to change behaviors
Most U.S. physicians favor the two-step method. This has been a huge controversy worldwide, with other countries pushing the United States to use the one-step method, Vincenzo Berghella, MD, a professor with Thomas Jefferson University, Philadelphia, said in an interview. “I expect this study will increase the divide between the U.S. and the rest of the world,” since U.S. physicians will see no benefit to the one-step method, and continue to use the two-step method.
It’s not surprising that GDM diagnosis incidence went up to 16.5% with the inclusion of the one-step test, compared with 8.5% with the two-step test, Dr. Berghella continued. What’s less clear, are the details of treatment among the 8% diagnosed to have GDM with the one-step test, but not the two-step test.
These women were likely to have milder degrees of insulin resistance or GDM. Dr. Berghella, who has advocated in the past for the one-step approach, said it would be important to find out if these women, who test positive at the one-step test but would test negative at the two-step test, were treated properly with diet, exercise, and possibly insulin or other hypoglycemic agents for their mild degree of insulin resistance. The researchers concluded that expanding the definition of GDM through the one-step test didn’t make a difference. However, “it’s not just the test that will make the difference in maternal and baby outcomes, but the aggressive management of diabetes with diet, exercise, and medications as needed once that test comes back abnormal,” he said.
The randomized trial was a massive undertaking, said Dr. Hillier.
“We are still evaluating our future plans,” she added. Forthcoming subgroup analyses from the trial could further help inform clinical practice guidelines.
Dr. Hillier received a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development to support this study. The investigators reported no potential conflict of interest relevant to this article.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
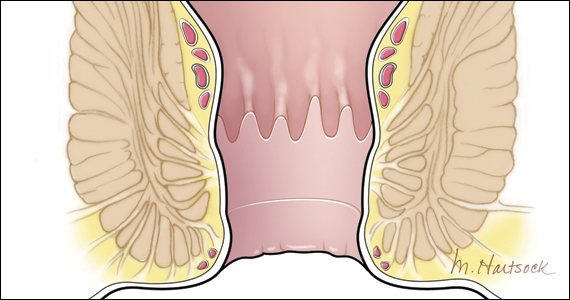
PPIs improve functional dyspepsia via anti-inflammatory effects
Proton pump inhibitors (PPIs) improve functional dyspepsia (FD) by reducing duodenal eosinophils and mast cells, according to a prospective study.
This suggests that the anti-inflammatory effects of PPIs are responsible for symptom improvement, and not barrier-protective or acid-suppressive effects, a finding that may guide future therapies and biomarkers, reported lead author Lucas Wauters, PhD, of University Hospitals Leuven (Belgium), and colleagues reported in Gastroenterology.
“FD is a common and unexplained disorder with unknown pathophysiology, hampering a conclusive diagnosis and the development of effective drugs,” the investigators wrote.
Although PPIs are currently used as first-line FD therapy, ostensibly for acid suppression, “the exact mechanism of action of PPIs in FD is unknown,” the investigators noted.
According to Dr. Wauters and colleagues, previous FD studies, such as a 2020 study published in Gut, have reported a variety of pathophysiological findings in the duodenum, including increased eosinophils and mast cells, as well as activation of duodenogastric reflexes, which suggests “a primary role for duodenal pathology in FD symptom generation.” Several drivers of this pathology have been proposed. Some, such as aberrations in bile salts and acidity, point to local, luminal changes, whereas others, such as dysregulated hypothalamic-pituitary-adrenal axis responsiveness and psychosocial factors, implicate a broader set of drivers, the investigators wrote.
The present study explored this landscape through a prospective trial that enrolled 30 healthy volunteers and 47 patients with FD (2 patients with FD did not complete the study).
Patients with FD were subgrouped into “FD-starters” who had not taken PPIs and/or acid suppression for at least 3 months leading up to the trial (n = 28) and “FD-stoppers” who had refractory symptoms after at least 1 month of daily PPI usage (n = 19). Among participants with FD, 25 had postprandial distress syndrome (PDS), 9 had epigastric pain syndrome (EPS), and 13 had subtype overlap.
For the trial, FD-starters and healthy volunteers took 4 weeks of pantoprazole 40 mg once daily, whereas FD-stoppers ceased PPI therapy for 8 weeks. Before and after these respective periods, certain study procedures were conducted, including duodenal biopsy collection, duodenal fluid aspiration, and questionnaires for symptoms and stress. The study also included use of Ussing chambers for biopsies, immunohistochemistry, and bile salt measurements.
FD-starters were significantly more symptomatic than healthy volunteers were at baseline. After starting PPIs, those with FD had symptom improvements, confirming “clinical efficacy of a standard course of PPIs in all FD subtypes,” whereas healthy volunteers showed no significant change in symptoms.
Similarly, baseline duodenal eosinophil counts were higher in FD-starters than in healthy volunteers. On starting PPIs, however, eosinophil counts in these two groups moved in opposite directions: FD-starters’ counts dropped from a mean of 331 to 183 eosinophils/mm2, whereas healthy volunteers’ counts rose from a mean of 115 to 229 eosinophils/mm2 (P < .0001). Changes in mast cells and paracellular passage followed the same pattern, falling in FD-starters and rising in healthy volunteers. On the other hand, symptoms actually improved in the FD-stoppers after they went off PPIs, although they did not reach symptom levels of the healthy volunteers.
“Differential effects of PPIs in healthy volunteers point to the role of luminal changes in determining low-grade mucosal immune activation in the duodenum, which can also occur in FD after long-term use and provide arguments against continued use in refractory patients,” the investigators wrote.
Dr. Wauters and colleagues suggested that their findings could guide future approaches to FD management.
“Our results suggest that quantification of duodenal eosinophils has the potential to become part of diagnostic workup and guide therapeutic decisions in FD,” they wrote. “Additional study of the underlying mediators might lead to the discovery of new potential biomarkers or novel therapeutic targets, potentially allowing the identification of subgroups responding to biologically targeted rather than symptom-based treatments.”
The study was supported by the clinical research fund of the University Hospitals Leuven. The investigators reported no conflicts of interest.
Functional dyspepsia (FD) is a commonly encountered diagnosis among primary care and gastroenterology clinics with estimated prevalence of 5%-11% worldwide. However, the pathophysiology of this entity is not well understood, and most of the patients who undergo upper endoscopy for dyspepsia tend to have normal findings.
The differential effects of PPIs on duodenal inflammation among the groups in this study are perplexing and the findings are limited by the short duration of follow-up testing and lack of a placebo group. Duodenal eosinophils, mast cells, and permeability were higher in treatment-naive FD, and a 4-week course of PPIs reduced this inflammation in FD but apparently increased it in healthy volunteers. Furthermore, when patients with PPI-refractory FD were studied, withdrawal of the PPI lead to improvement in symptoms and trends toward less duodenal inflammation.
The discordant impact of PPIs among these groups on duodenal inflammation raises questions regarding the true effect from PPIs or changes driven by other systemic factors (brain-gut axis). This is hard to differentiate without a placebo group. Focus in future studies should be placed on how to clinically phenotype and predict PPI responders versus nonresponders along with use of longer durations to see if even PPI responders tend to lose response over time, regardless of changes in the duodenal inflammation and permeability.
Dhyanesh A. Patel, MD, is an assistant professor of medicine at the center for esophageal disorders, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
Functional dyspepsia (FD) is a commonly encountered diagnosis among primary care and gastroenterology clinics with estimated prevalence of 5%-11% worldwide. However, the pathophysiology of this entity is not well understood, and most of the patients who undergo upper endoscopy for dyspepsia tend to have normal findings.
The differential effects of PPIs on duodenal inflammation among the groups in this study are perplexing and the findings are limited by the short duration of follow-up testing and lack of a placebo group. Duodenal eosinophils, mast cells, and permeability were higher in treatment-naive FD, and a 4-week course of PPIs reduced this inflammation in FD but apparently increased it in healthy volunteers. Furthermore, when patients with PPI-refractory FD were studied, withdrawal of the PPI lead to improvement in symptoms and trends toward less duodenal inflammation.
The discordant impact of PPIs among these groups on duodenal inflammation raises questions regarding the true effect from PPIs or changes driven by other systemic factors (brain-gut axis). This is hard to differentiate without a placebo group. Focus in future studies should be placed on how to clinically phenotype and predict PPI responders versus nonresponders along with use of longer durations to see if even PPI responders tend to lose response over time, regardless of changes in the duodenal inflammation and permeability.
Dhyanesh A. Patel, MD, is an assistant professor of medicine at the center for esophageal disorders, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
Functional dyspepsia (FD) is a commonly encountered diagnosis among primary care and gastroenterology clinics with estimated prevalence of 5%-11% worldwide. However, the pathophysiology of this entity is not well understood, and most of the patients who undergo upper endoscopy for dyspepsia tend to have normal findings.
The differential effects of PPIs on duodenal inflammation among the groups in this study are perplexing and the findings are limited by the short duration of follow-up testing and lack of a placebo group. Duodenal eosinophils, mast cells, and permeability were higher in treatment-naive FD, and a 4-week course of PPIs reduced this inflammation in FD but apparently increased it in healthy volunteers. Furthermore, when patients with PPI-refractory FD were studied, withdrawal of the PPI lead to improvement in symptoms and trends toward less duodenal inflammation.
The discordant impact of PPIs among these groups on duodenal inflammation raises questions regarding the true effect from PPIs or changes driven by other systemic factors (brain-gut axis). This is hard to differentiate without a placebo group. Focus in future studies should be placed on how to clinically phenotype and predict PPI responders versus nonresponders along with use of longer durations to see if even PPI responders tend to lose response over time, regardless of changes in the duodenal inflammation and permeability.
Dhyanesh A. Patel, MD, is an assistant professor of medicine at the center for esophageal disorders, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
Proton pump inhibitors (PPIs) improve functional dyspepsia (FD) by reducing duodenal eosinophils and mast cells, according to a prospective study.
This suggests that the anti-inflammatory effects of PPIs are responsible for symptom improvement, and not barrier-protective or acid-suppressive effects, a finding that may guide future therapies and biomarkers, reported lead author Lucas Wauters, PhD, of University Hospitals Leuven (Belgium), and colleagues reported in Gastroenterology.
“FD is a common and unexplained disorder with unknown pathophysiology, hampering a conclusive diagnosis and the development of effective drugs,” the investigators wrote.
Although PPIs are currently used as first-line FD therapy, ostensibly for acid suppression, “the exact mechanism of action of PPIs in FD is unknown,” the investigators noted.
According to Dr. Wauters and colleagues, previous FD studies, such as a 2020 study published in Gut, have reported a variety of pathophysiological findings in the duodenum, including increased eosinophils and mast cells, as well as activation of duodenogastric reflexes, which suggests “a primary role for duodenal pathology in FD symptom generation.” Several drivers of this pathology have been proposed. Some, such as aberrations in bile salts and acidity, point to local, luminal changes, whereas others, such as dysregulated hypothalamic-pituitary-adrenal axis responsiveness and psychosocial factors, implicate a broader set of drivers, the investigators wrote.
The present study explored this landscape through a prospective trial that enrolled 30 healthy volunteers and 47 patients with FD (2 patients with FD did not complete the study).
Patients with FD were subgrouped into “FD-starters” who had not taken PPIs and/or acid suppression for at least 3 months leading up to the trial (n = 28) and “FD-stoppers” who had refractory symptoms after at least 1 month of daily PPI usage (n = 19). Among participants with FD, 25 had postprandial distress syndrome (PDS), 9 had epigastric pain syndrome (EPS), and 13 had subtype overlap.
For the trial, FD-starters and healthy volunteers took 4 weeks of pantoprazole 40 mg once daily, whereas FD-stoppers ceased PPI therapy for 8 weeks. Before and after these respective periods, certain study procedures were conducted, including duodenal biopsy collection, duodenal fluid aspiration, and questionnaires for symptoms and stress. The study also included use of Ussing chambers for biopsies, immunohistochemistry, and bile salt measurements.
FD-starters were significantly more symptomatic than healthy volunteers were at baseline. After starting PPIs, those with FD had symptom improvements, confirming “clinical efficacy of a standard course of PPIs in all FD subtypes,” whereas healthy volunteers showed no significant change in symptoms.
Similarly, baseline duodenal eosinophil counts were higher in FD-starters than in healthy volunteers. On starting PPIs, however, eosinophil counts in these two groups moved in opposite directions: FD-starters’ counts dropped from a mean of 331 to 183 eosinophils/mm2, whereas healthy volunteers’ counts rose from a mean of 115 to 229 eosinophils/mm2 (P < .0001). Changes in mast cells and paracellular passage followed the same pattern, falling in FD-starters and rising in healthy volunteers. On the other hand, symptoms actually improved in the FD-stoppers after they went off PPIs, although they did not reach symptom levels of the healthy volunteers.
“Differential effects of PPIs in healthy volunteers point to the role of luminal changes in determining low-grade mucosal immune activation in the duodenum, which can also occur in FD after long-term use and provide arguments against continued use in refractory patients,” the investigators wrote.
Dr. Wauters and colleagues suggested that their findings could guide future approaches to FD management.
“Our results suggest that quantification of duodenal eosinophils has the potential to become part of diagnostic workup and guide therapeutic decisions in FD,” they wrote. “Additional study of the underlying mediators might lead to the discovery of new potential biomarkers or novel therapeutic targets, potentially allowing the identification of subgroups responding to biologically targeted rather than symptom-based treatments.”
The study was supported by the clinical research fund of the University Hospitals Leuven. The investigators reported no conflicts of interest.
Proton pump inhibitors (PPIs) improve functional dyspepsia (FD) by reducing duodenal eosinophils and mast cells, according to a prospective study.
This suggests that the anti-inflammatory effects of PPIs are responsible for symptom improvement, and not barrier-protective or acid-suppressive effects, a finding that may guide future therapies and biomarkers, reported lead author Lucas Wauters, PhD, of University Hospitals Leuven (Belgium), and colleagues reported in Gastroenterology.
“FD is a common and unexplained disorder with unknown pathophysiology, hampering a conclusive diagnosis and the development of effective drugs,” the investigators wrote.
Although PPIs are currently used as first-line FD therapy, ostensibly for acid suppression, “the exact mechanism of action of PPIs in FD is unknown,” the investigators noted.
According to Dr. Wauters and colleagues, previous FD studies, such as a 2020 study published in Gut, have reported a variety of pathophysiological findings in the duodenum, including increased eosinophils and mast cells, as well as activation of duodenogastric reflexes, which suggests “a primary role for duodenal pathology in FD symptom generation.” Several drivers of this pathology have been proposed. Some, such as aberrations in bile salts and acidity, point to local, luminal changes, whereas others, such as dysregulated hypothalamic-pituitary-adrenal axis responsiveness and psychosocial factors, implicate a broader set of drivers, the investigators wrote.
The present study explored this landscape through a prospective trial that enrolled 30 healthy volunteers and 47 patients with FD (2 patients with FD did not complete the study).
Patients with FD were subgrouped into “FD-starters” who had not taken PPIs and/or acid suppression for at least 3 months leading up to the trial (n = 28) and “FD-stoppers” who had refractory symptoms after at least 1 month of daily PPI usage (n = 19). Among participants with FD, 25 had postprandial distress syndrome (PDS), 9 had epigastric pain syndrome (EPS), and 13 had subtype overlap.
For the trial, FD-starters and healthy volunteers took 4 weeks of pantoprazole 40 mg once daily, whereas FD-stoppers ceased PPI therapy for 8 weeks. Before and after these respective periods, certain study procedures were conducted, including duodenal biopsy collection, duodenal fluid aspiration, and questionnaires for symptoms and stress. The study also included use of Ussing chambers for biopsies, immunohistochemistry, and bile salt measurements.
FD-starters were significantly more symptomatic than healthy volunteers were at baseline. After starting PPIs, those with FD had symptom improvements, confirming “clinical efficacy of a standard course of PPIs in all FD subtypes,” whereas healthy volunteers showed no significant change in symptoms.
Similarly, baseline duodenal eosinophil counts were higher in FD-starters than in healthy volunteers. On starting PPIs, however, eosinophil counts in these two groups moved in opposite directions: FD-starters’ counts dropped from a mean of 331 to 183 eosinophils/mm2, whereas healthy volunteers’ counts rose from a mean of 115 to 229 eosinophils/mm2 (P < .0001). Changes in mast cells and paracellular passage followed the same pattern, falling in FD-starters and rising in healthy volunteers. On the other hand, symptoms actually improved in the FD-stoppers after they went off PPIs, although they did not reach symptom levels of the healthy volunteers.
“Differential effects of PPIs in healthy volunteers point to the role of luminal changes in determining low-grade mucosal immune activation in the duodenum, which can also occur in FD after long-term use and provide arguments against continued use in refractory patients,” the investigators wrote.
Dr. Wauters and colleagues suggested that their findings could guide future approaches to FD management.
“Our results suggest that quantification of duodenal eosinophils has the potential to become part of diagnostic workup and guide therapeutic decisions in FD,” they wrote. “Additional study of the underlying mediators might lead to the discovery of new potential biomarkers or novel therapeutic targets, potentially allowing the identification of subgroups responding to biologically targeted rather than symptom-based treatments.”
The study was supported by the clinical research fund of the University Hospitals Leuven. The investigators reported no conflicts of interest.
FROM GASTROENTEROLOGY
Is there liability if you don’t test for BRCA?
CASE Young woman with family history of breast cancer detects lump
Two weeks after noting a lump on her breast when her cat happened to jump on her in that spot, a 28-year-old woman (G0) went to her primary care provider. She was referred to her gynecologist; breast imaging, ultrasonography, and mammography were obtained, with microcalcifications noted. A fine needle aspiration diagnosed intraductal malignancy. The surgical breast tissue specimen was estrogen receptor (ER)- and progestogen receptor (PR)-positive and HER2-negative. Other tumor markers were obtained, including carcinoembryonic antigen, and tissue polypeptide specific antigen, p53, cathepsin D, cyclin E, and nestin, but results were not available.
With regard to family history, the woman’s mother and maternal grandmother had a history of breast cancer. The patient and her family underwent gene testing. The patient was found to be BRCA1- and BRCA2-positive; her mother was BRCA1-positive, an older sister was BRCA2-positive, and her grandmother was not tested.
The question arose in light of her family history as to why she was not tested for BRCA and appropriately counseled by her gynecologist prior to the cancer diagnosis. Litigation was initiated. While the case did not go forward regarding litigation, it is indeed a case in point. (Please note that this is a hypothetical case. It is based on a composite of several cases.)
Medical considerations
Breast cancer is the most common type of cancer affecting women in the Western world.1 Advances in clinical testing for gene mutations have escalated and allowed for identification of patients at increased risk for breast and ovarian cancer. Along with these advances come professional liability risk. After looking at the medical considerations for BRCA1 and 2 testing, we will consider a number of important legal issues. In the view of some commentators, the failure to diagnose genetic mutations in patients predisposed to cancer is “poised to become the next wave of medical professional liability lawsuits.”2
BRCA1 and BRCA2 genes provide tumor suppressor proteins, and assessment for mutations is recommended for individuals at high risk for breast and/or ovarian cancer; mutations in BRCA genes cause DNA damage, which increases the chance of developing cancer. The other way to look at it is, BRCA1 and 2 are tumor suppressor genes that are integrally involved with DNA damage control. Once there is a mutation, it adversely affects the beneficial effects of the gene. Mutations in these genes account for 5% to 10% of all hereditary breast cancers.3 Of note, men with BRCA2 are at increased risk for prostate cancer.
A patient who presents to her gynecologist stating that there is a family history of breast cancer, without knowledge of genetic components, presents a challenge (and a medicolegal risk) for the provider to assess. Prediction models have been used to determine specific patient risk for carrying a genetic mutation with resultant breast cancer development.4 Risk prediction models do not appear to be a good answer to predicting who is more likely to develop breast or ovarian cancer, however. A Mayo model may assist (FIGURE).5 Clinicians should also be aware of other models of risk assessment, including the Gail Model (TABLE 1).6
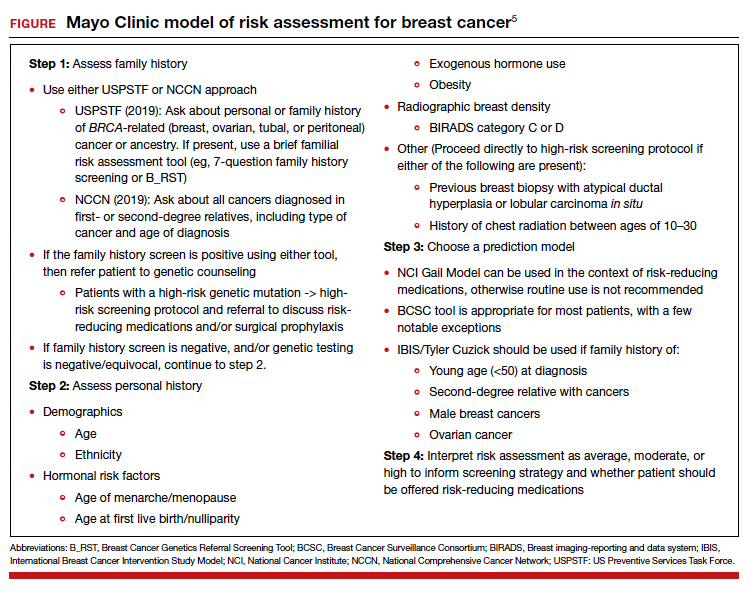
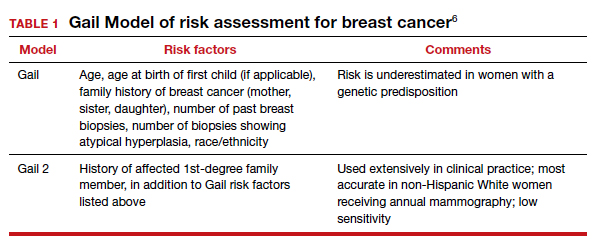
Continue to: Guidelines for genetic testing...
Guidelines for genetic testing
The American College of Obstetricians and Gynecologists states that patient medical history and family history are paramount in obtaining information regarding risk for breast and ovarian cancer. First- and second-degree relatives are allocated to this category. Information regarding age of diagnosis, maternal and paternal lineage, and ethnic background can imply a need for genetic testing (TABLE 2).7,8 A number of genetics national organizations have participated in recommendations and include the American College of Medical Genetics and Genomics, the National Society for Genetic Counselors, and the Society of Gynecologic Oncology.7
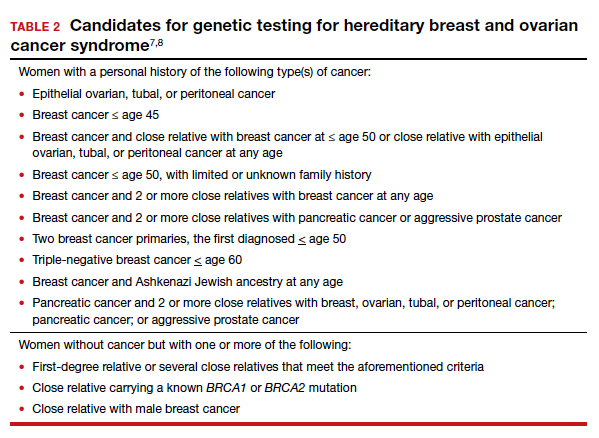
The question always surfaces, could the clinical outcome of the cancer when diagnosed have been changed if screening were undertaken, with earlier diagnosis, or prevented with prophylactic mastectomy, and changed the end result. In addition, it is well known that breast augmentation mammoplasty alters the ability to accurately evaluate mammograms. Patients considering this type of plastic surgery, ideally, should be counselled accordingly.9
Bottom line, we as clinicians must be cognizant of both ACOG and United States Preventive Services Task Force (USPSTF) recommendations regarding screening and gene testing for women considered high risk for breast cancer based on family history.7
Legal considerations
The case presented demonstrates that the discovery of the BRCA1 and BRCA2 genes, and reliable tests for determining the existence of the genes, brought with them legal issues as well as medical advantages. We look at professional liability (malpractice) questions this technology raises, and then consider the outcome of the hypothetical case. (BRCA is used here to apply broadly—not only to BRCA1 and 2 but also to PALB2, CHEK2, and similar genetic abnormalities.)
To date, the most visible BRCA legal issues covered in cases and law reviews have focused more on patent law than malpractice. The most important of these was a decision of the US Supreme Court in Association for Molecular Pathology v Myriad Genetics.10 The US Patent Office was granting patents to companies finding useful, naturally occurring segments of human DNA, and had granted Myriad several patents on BRCA1 and BRCA2 genes. This patent policy had the potential to seriously interfere with broad scientific use of these genes.11 Fortunately, the Supreme Court stepped in and unanimously invalidated such patents. It held that a “naturally occurring DNA segment is a product of nature and not patent eligible merely because it has been isolated.” The Court noted, “Finding the location of the BRCA1 and BRCA2 genes does not render the genes patent eligible ‘new . . . composition[s] of matter.’”8 The Court did allow the patenting of tests for specific gene structures, and artificial changes in naturally occurring genes.
Malpractice and BRCA
While the BRCA patent wars have lingered, the potential for a significant increase in BRCA-related malpractice cases is of increasing concern. Like most malpractice liability, these new claims are based on very old principles of negligence.12 To prevail, the plaintiff (ordinarily, an injured patient) must demonstrate 4 things:
- A duty. That is, the physician owed a duty to the injured party. Usually (but not always) that requires a professional relationship between the physician and the person injured.
- A breach of that duty. Malpractice liability is based on the fact that the physician did something that a reasonably careful physician (generally, of the same specialty) would not have done, or that the physician failed to do something that a reasonable physician would have done. This usually means that the profession itself sees what the physician did (or did not do) as medically inappropriate. In medical malpractice cases, that is ordinarily measured by what the usual or common practice is among prudent physicians. In rare circumstances, courts have found the standard practice of a profession to be negligent. Where, for example, it was custom for a professional not to give an eye pressure test to anyone under age 40, a court found that common standard to be inappropriate.13 In the words of Judge Learned Hand (speaking about a different case), “a whole calling may have unduly lagged in the adoption of new and available devices. It never may set its own tests.”14 Underlying negligence is a cost-benefit analysis (discussed below).
- Damages. There must have been some damage that courts recognize, usually loss of money or opportunity to work, the cost of care, pain and suffering, or loss of enjoyment/quality of life. In malpractice, many states now recognize the “loss of chance” or the “loss of a chance.” That means, if a “physician negligently fails to diagnose a curable disease, and the patient is harmed by the disease, the physician should be liable for causing the ‘loss of a chance of a cure.’”15 (Delay in diagnosis is the most common reason for claims in breast cancer care.)16
- Causation. The breach of duty (negligence) must have caused the damages. The causation must have been reasonably close. If a driver drives through a stop sign, or a physician misreads a test, and someone is injured but there is no connection between the negligence and the injury, there is not tort liability.
The 4 elements of malpractice just described are raised in some way in the possible liability associated with BRCA testing. We next look at the ways in which liability may arise from that testing (or lack of it).
Underlying much of the following discussion is the “cost-benefit” consideration noted above. This concept is that the total cost (financial and health) of testing should be compared with the value of the benefits of testing, taking into account the probabilities that the testing will result in better health outcomes. BRCA testing, for example, is essentially cost-free in terms of physical risk. Its financial cost, while not trivial, is not great, and it is commonly covered by health insurance.17 In terms of benefits, the testing has the potential for providing critical information in making treatment decisions for a meaningful percentage of patients and their families. There are many ways of analyzing the liability risks of genetic malpractice,7,18 and the following is intended to discuss some of the greatest risks related to BRCA testing.
Continue to: Areas of liability...
Areas of liability
The failure to recommend a test. The circumstances in which BRCA testing should be undertaken are set out by professional organizations (noted above). These recommendations are not static, however. They change from time to time. Given the potential harm caused by the failure to test in relevant circumstances, malpractice liability is certainly a possibility when the failure to recommend a test to a patient results in a cancer that might have been prevented had the genetic problem been identified in a timely manner. The circumstances in which testing should be considered continue to change, placing an obligation on clinicians to stay well informed of changing genetic understandings. Another risk is that one specialist may assume that it is the job of another specialist to order the test. Whatever the cause of the failure to test, or unnecessary delay in testing, it appears to be the primary basis for BRCA liability.
The failure to properly interpret a test. Any test that is misinterpreted may lead to harm for the patient. A false negative, of course, may mean that preventive treatment that could have been undertaken will be foregone, as a “loss of a chance.” On the other hand, a false positive can lead to radical, unnecessary surgery or treatment. If a misinterpretation occurred because of carelessness by the testing organization, or confusion by a practitioner, there is a likelihood of negligence.19
A different form of “misinterpretation” could be reasonable—and not negligent. Advances in scientific-medical understanding may result in the outcome of tests being reconsidered and changed. That has been the case with genetic testing and breast cancer. The availability of multiple breast cancer SNPs (single nucleotide polymorphisms), and combining this information with other risk factors for example, results in a polygenic risk score that may be at odds with the level of risk from earlier testing.20,21 This naturally leads to the question of when later, updated testing should be recommended to look for a better current interpretation.22,23
The failure to act on BRCA test results. Testing is of no value, of course, if the results are not used properly. Test results or analyses that are not sent to the proper physicians, or are somehow ignored when properly directed, is a “never” event—it should never happen. It almost always would be considered negligence, and if the patient were injured, could lead to liability. Amazingly, one study found that, in genetic testing liability cases, nearly 20% of the claims arose from failure to return test results to patients.24 In addition, when a patient is found to be BRCA-positive, there is an obligation to discuss the options for dealing with the increased risk associated with the gene mutation(s), as well as to recommend the prudent course of action or to refer the patient to someone who will have that discussion.
Informed consent to the patient. BRCA testing requires informed consent. The physical risks of the testing process are minimal, of course, but it carries a number of other emotional and family risks. The informed consent process is an invitation to an honest discussion between clinicians and patients. It should be an opportunity to discuss what the testing is, and is not, and what the test may mean for treatment. It may also be an opportunity to discuss the implications for other members of the patient’s family (noted below).
One element of informed consent is a discussion of the consequences of failure to consent, or to undertake one of the alternatives. In the case of BRCA testing, this is especially important in cases in which a patient expresses a hesitancy to be tested with an “I’d rather not know philosophy.” Although clinicians should not practice law, some patient concerns about discrimination may be addressed by the protection that the federal Genetic Information Nondiscrimination Act (GINA) and other laws provide (which prohibit insurance and employment discrimination based on genetic information). A good source of information about GINA and related nondiscrimination laws is provided by the National Human Genome Research Institute.25 In addition, the National Institutes of Health has a website that may be helpful to many patients26 (and a much more complex site for health professionals).27 At the same time, courts have resisted plaintiffs/patients who have tried to use informed consent as a way of suing for failure to offer genetic testing.28,29
The failure to refer. In some cases, a patient should be formally referred for genetics consultation. The considerations here are similar to other circumstances in modern, fast developing medical practice that require special sensitivity to those occasions in which a patient will benefit from additional expertise. It is a principle that the AMA Council on Ethical and Judicial Affairs has expressed this way: “In the absence of adequate expertise in pretest and posttest counseling, a physician should refer the patient to an appropriate specialist.”30 The failure to refer, when that deviates from acceptable practice, may result in liability.
Informing others. BRCA testing is an area of medicine in which results may be of great significance not only to the patient but also to the patient’s family.31 Physicians should counsel patients on the importance of informing relatives about relevant results and “should make themselves available to assist patients in communicating with relatives to discuss opportunities for counseling and testing, as appropriate.”30 The question may arise, however, of whether in some circumstances physicians should go a step further in ensuring relatives receive important information regarding their loved one’s health.32 The law has been reluctant to impose liability to “third parties” (someone not a patient). Duties usually arise through the physician-patient relationship. There are exceptions. Perhaps the best known has been the obligation of mental health professionals to take action to protect third parties from patients who have made believable threats against identifiable victims.33 There are indications that some courts could find, in extreme circumstances, a “duty to warn” nonpatients in some instances where it is essential to inform third parties that they should receive a specific form of genetic testing.34,35 Such a duty would, of course, have to protect the privacy rights of the patient to the maximum extent possible. A general duty of this type has not been established widely, but may be part of the future.
Continue to: Was there liability in our example case?...
Was there liability in our example case?
The hypothetical case provided above suggests that there could be liability. Routine medical history by the primary care physician would have produced the fact that the patient’s mother, sister, and maternal grandmother had breast cancer. That would clearly have put her in a category of those who should have received genetic testing. Yet, she was not tested until after her cancer was found. From the limited facts we have, it appears that this timeline of events would have been outside accepted practice—and negligent. The case was not pursued by the patient, however, and this may represent the current state of liability for BRCA issues.
The extent of liability seems to be significant
Our discussion of liability suggests that there is significant potential for BRCA testing negligence within practice, and that the damages in these cases could be substantial. Yet the predicted “tsunami” of malpractice lawsuits related to genetic testing has not appeared.36,37 One study of cases in the United States (through 2016) found a “slowly rising tide” of liability cases instead of a tsunami,24 as the number of claims made was low. On the other hand, the payments where damages were awarded were an order of magnitude larger than other malpractice cases—a mean of $5.3 million and median of $2 million. This is compared with mean values in the range of $275,000 to $600,000 in other areas of malpractice.
The majority of the genetic malpractice cases involve prenatal and newborn testing, and diagnosis/susceptibility/pharmacogenomic accounting for about 25% of cases. In terms of type of errors claimed, approximately 50% were diagnostic-interpretation errors, 30% failure to offer testing, nearly 20% failure to return test results to the patients, and a few remaining cases of failure to properly treat in light of genetic testing.24
Despite a few very large payments, however, the fact remains that there is a surprisingly low number of genetics malpractice cases. Gary Marchant and colleagues suggest that several reasons may account for this:
- the clinical implementation of genetic science has been slower than expected
- the lack of expertise of many physicians in genetic science
- expert witnesses have sometimes been hard to find
- the lack of understanding by plaintiffs’ attorneys of genetic malpractice
- potential plaintiffs’ lack of understanding of the nature of genetic testing and the harms resulting from genetic negligence.17,24,37
The tide is slowly coming in
By all appearances, there is every reason to think that genetic malpractice will be increasing, and that the recent past of much higher damages per claim paid in the genetics area will be part of that tide. The National Human Genome Research LawSeq project has suggested a number of useful ways of dealing with the liability issues.18 In addition to the BRCA issues that we have considered in this article for ObGyns, there are other critical issues of prenatal and newborn genetic testing.38 But those are topics for another day. ●
- Sevilla C, Moatti JP, Reynier CJ, et al. Testing for BRCA1 mutations: a cost-effective analysis. Europ J Human Genetics. 2002;10:599-606.
- Cotton V, Kirkpatrick D. Failure to recommend genetic counseling in breast cancer: is the next wave of medical professional liability lawsuits? Contemp OB/GYN. June 1, 2017.
- Suryavanshi M, Kumar D, Panigrahi M, et al. Detection of false positive mutations in BRCA gene by next generation sequencing. Fam Cancer. 2017;16:311-317.
- Black L, Knoppers B, Avard D, et al. Legal liability and the uncertain nature of risk prediction: the case of breast cancer risk prediction models. Public Health Genomics. 2012;15:335-340.
- McClintock A, Gollab A, Laya M. Breast cancer risk assessment, a step-wise approach for primary care physicians on the front lines of shared decision making. Mayo Clin Proc. 2020;95:1268-1275.
- National Cancer Institute. The Breast Cancer Risk Assessment Tool. https://bcrisktool.cancer.gov/. Accessed February 25, 2021.
- Neff J, Richardson G, Phelps J. Legal liabilities associated with hereditary breast and ovarian cancers. J Reprod Med. 2020;65:227-230.
- American College of Obstetricians and Gynecologists. Practice Bulletin No 182: hereditary breast and ovarian cancer syndrome. Obstet Gynecol. 2017;130:e110-e126.
- Sá dos Reis C, Gremion I, and Meystre NR. Study of breast implants mammography examinations for identification of suitable image quality criteria. Insights Imaging. 2020;11:3.
- Association for Molecular Pathology v Myriad Genetics, 569 U.S. 576 (2013).
- Smith SR. The Supreme Court 2012-2013: dogs, DNA, and DOMA. Register Rep. 2013;39(Fall):26-33.
- Bal BS. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467:339-347.
- Helling v Carey, 83 Wn.2d 514, 519 P.2d 981 (1974).
- The T.J. Hooper, 60 F.2d 737, 740 (2d Cir.1932), cert. denied 287 U.S. 662 (1932).
- Fischer DA. Tort recovery for loss of a chance. Wake Forest L Rev. 2001;36:605-655.
- Murphy BL, Ray-Zack MD, Reddy PN, et al. Breast cancer litigation in the 21st century. Ann Surg Oncol. 2018;25:2939- 2947.
- Prince AE. Prevention for those who can pay: insurance reimbursement of genetic-based preventive interventions in the liminal state between health and disease. J Law Biosci. 2015;2:365-395.
- Marchant G, Barnes M, Evans JP, et al; LawSeq Liability Task Force. From genetics to genomics: facing the liability implications in clinical care. J Law Med Ethics. 2020;48:11-43.
- Complaint, Held v Ambry Genetics Corp., No. 15-CV-8683, 2015 WL 6750024 (S.D.N.Y. Nov. 4, 2015); Order of Dismissal, Held v Ambry Genetics Corp., No. 15-CV-8683, (S.D.N.Y. Dec. 6, 2016).
- Pederson HJ. Breast cancer risk assessment and treatment: current concepts in genetics and genomics. Contemp OB/ GYN. 2017; 62:A1-A4.
- Pederson HJ. Who needs breast cancer genetics testing? OBG Manag. 2018;30:34-39.
- Roberts JL, Foulkes A. Genetic duties. William Mary L Rev. 2020;62:143-212.
- Thorogood A, Cook-Deegan R, Knoppers B. Public variant databases: liability? Genet Med. 2017;19:838–841.
- Marchant G, Lindor R. Genomic malpractice: an emerging tide or gentle ripple? Food Drug Law J. 2018;73:1-37.
- National Human Genome Research Institute. Genetic discrimination. https://www.genome.gov/about-genomics /policy-issues/Genetic-Discrimination. Updated September 16, 2020. Accessed February 25, 2021.
- National Cancer Institute. BRCA mutations: cancer risk and genetic testing. https://www.cancer.gov/about-cancer /causes-prevention/genetics/brca-fact-sheet. Reviewed November 19, 2020. Accessed February 25, 2021.
- National Cancer Institute. Genetics of breast and gynecologic cancers (PDQ®)–Health Professional Version. https://www .cancer.gov/types/breast/hp/breast-ovarian-genetics-pdq. Updated February 12, 2021. Accessed February 25, 2021.
- Reed v Campagnolo, 630 A.2d 1145, 1152–54 (Md. 1993).
- Munro v Regents of Univ. of Cal.,263 Cal. Rptr. 878, 885, 988 (1989).
- AMA Council on Ethical and Judicial Affairs. AMA Code of Medical Ethics’ opinions on genetic testing. Opinion 2.131. 2009;11:683-685. https://journalofethics.ama-assn .org/article/ama-code-medical-ethics-opinions-genetictesting/2009-09.
- Gilbar R, Barnoy S. Disclosing genetic test results to the patient’ relatives: how does the law influence clinical practice? J Law Technol Policy. 2019;125-168.
- Song K. Warning third parties of genetic risks in the era of personalized medicine. U.C. Davis L Rev. 2016;49:1987-2018.
- Tarasoff v Regents of the University of California, 551 P.2d 334, 131 Cal. Rptr. 14 (Cal. 1976).
- Safer v Estate of Pack, 677 A.2d 1188 (N.J. App. 1996), cert. denied, 683 A.2d 1163 (N.J. 1996).
- Pate v Threlkel, 661 So.2d 278 (Fla. 1995).
- Rothstein MA. Liability issues in pharmacogenomics. Louisiana L Rev. 2005;66:117-124.
- Marchant G, Lindor R. Personalized medicine and genetic malpractice. Genet Med. 2013;15:921-922.
- Westbrook M. Transforming the physician’s standard of care in the context of whole genome sequencing technologies: finding guidance in best practice standards. Saint Louis U J Health Law Policy. 2015;9:111-148.
CASE Young woman with family history of breast cancer detects lump
Two weeks after noting a lump on her breast when her cat happened to jump on her in that spot, a 28-year-old woman (G0) went to her primary care provider. She was referred to her gynecologist; breast imaging, ultrasonography, and mammography were obtained, with microcalcifications noted. A fine needle aspiration diagnosed intraductal malignancy. The surgical breast tissue specimen was estrogen receptor (ER)- and progestogen receptor (PR)-positive and HER2-negative. Other tumor markers were obtained, including carcinoembryonic antigen, and tissue polypeptide specific antigen, p53, cathepsin D, cyclin E, and nestin, but results were not available.
With regard to family history, the woman’s mother and maternal grandmother had a history of breast cancer. The patient and her family underwent gene testing. The patient was found to be BRCA1- and BRCA2-positive; her mother was BRCA1-positive, an older sister was BRCA2-positive, and her grandmother was not tested.
The question arose in light of her family history as to why she was not tested for BRCA and appropriately counseled by her gynecologist prior to the cancer diagnosis. Litigation was initiated. While the case did not go forward regarding litigation, it is indeed a case in point. (Please note that this is a hypothetical case. It is based on a composite of several cases.)
Medical considerations
Breast cancer is the most common type of cancer affecting women in the Western world.1 Advances in clinical testing for gene mutations have escalated and allowed for identification of patients at increased risk for breast and ovarian cancer. Along with these advances come professional liability risk. After looking at the medical considerations for BRCA1 and 2 testing, we will consider a number of important legal issues. In the view of some commentators, the failure to diagnose genetic mutations in patients predisposed to cancer is “poised to become the next wave of medical professional liability lawsuits.”2
BRCA1 and BRCA2 genes provide tumor suppressor proteins, and assessment for mutations is recommended for individuals at high risk for breast and/or ovarian cancer; mutations in BRCA genes cause DNA damage, which increases the chance of developing cancer. The other way to look at it is, BRCA1 and 2 are tumor suppressor genes that are integrally involved with DNA damage control. Once there is a mutation, it adversely affects the beneficial effects of the gene. Mutations in these genes account for 5% to 10% of all hereditary breast cancers.3 Of note, men with BRCA2 are at increased risk for prostate cancer.
A patient who presents to her gynecologist stating that there is a family history of breast cancer, without knowledge of genetic components, presents a challenge (and a medicolegal risk) for the provider to assess. Prediction models have been used to determine specific patient risk for carrying a genetic mutation with resultant breast cancer development.4 Risk prediction models do not appear to be a good answer to predicting who is more likely to develop breast or ovarian cancer, however. A Mayo model may assist (FIGURE).5 Clinicians should also be aware of other models of risk assessment, including the Gail Model (TABLE 1).6
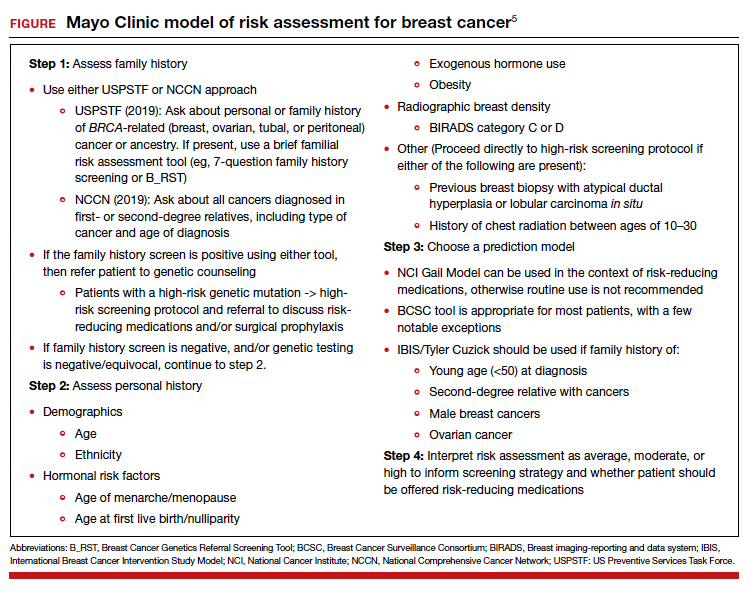
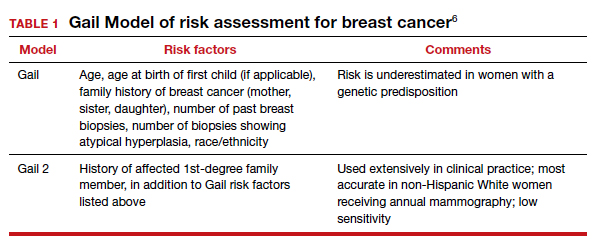
Continue to: Guidelines for genetic testing...
Guidelines for genetic testing
The American College of Obstetricians and Gynecologists states that patient medical history and family history are paramount in obtaining information regarding risk for breast and ovarian cancer. First- and second-degree relatives are allocated to this category. Information regarding age of diagnosis, maternal and paternal lineage, and ethnic background can imply a need for genetic testing (TABLE 2).7,8 A number of genetics national organizations have participated in recommendations and include the American College of Medical Genetics and Genomics, the National Society for Genetic Counselors, and the Society of Gynecologic Oncology.7
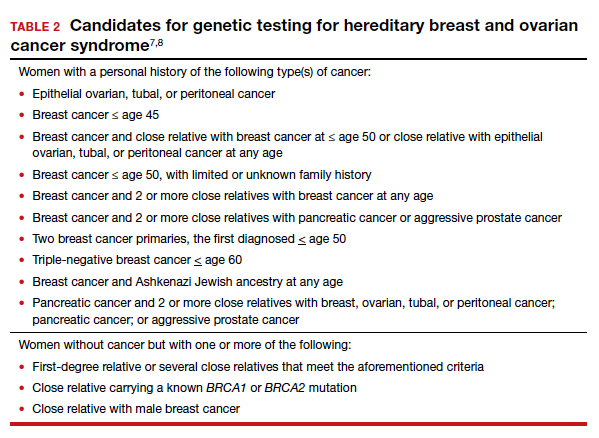
The question always surfaces, could the clinical outcome of the cancer when diagnosed have been changed if screening were undertaken, with earlier diagnosis, or prevented with prophylactic mastectomy, and changed the end result. In addition, it is well known that breast augmentation mammoplasty alters the ability to accurately evaluate mammograms. Patients considering this type of plastic surgery, ideally, should be counselled accordingly.9
Bottom line, we as clinicians must be cognizant of both ACOG and United States Preventive Services Task Force (USPSTF) recommendations regarding screening and gene testing for women considered high risk for breast cancer based on family history.7
Legal considerations
The case presented demonstrates that the discovery of the BRCA1 and BRCA2 genes, and reliable tests for determining the existence of the genes, brought with them legal issues as well as medical advantages. We look at professional liability (malpractice) questions this technology raises, and then consider the outcome of the hypothetical case. (BRCA is used here to apply broadly—not only to BRCA1 and 2 but also to PALB2, CHEK2, and similar genetic abnormalities.)
To date, the most visible BRCA legal issues covered in cases and law reviews have focused more on patent law than malpractice. The most important of these was a decision of the US Supreme Court in Association for Molecular Pathology v Myriad Genetics.10 The US Patent Office was granting patents to companies finding useful, naturally occurring segments of human DNA, and had granted Myriad several patents on BRCA1 and BRCA2 genes. This patent policy had the potential to seriously interfere with broad scientific use of these genes.11 Fortunately, the Supreme Court stepped in and unanimously invalidated such patents. It held that a “naturally occurring DNA segment is a product of nature and not patent eligible merely because it has been isolated.” The Court noted, “Finding the location of the BRCA1 and BRCA2 genes does not render the genes patent eligible ‘new . . . composition[s] of matter.’”8 The Court did allow the patenting of tests for specific gene structures, and artificial changes in naturally occurring genes.
Malpractice and BRCA
While the BRCA patent wars have lingered, the potential for a significant increase in BRCA-related malpractice cases is of increasing concern. Like most malpractice liability, these new claims are based on very old principles of negligence.12 To prevail, the plaintiff (ordinarily, an injured patient) must demonstrate 4 things:
- A duty. That is, the physician owed a duty to the injured party. Usually (but not always) that requires a professional relationship between the physician and the person injured.
- A breach of that duty. Malpractice liability is based on the fact that the physician did something that a reasonably careful physician (generally, of the same specialty) would not have done, or that the physician failed to do something that a reasonable physician would have done. This usually means that the profession itself sees what the physician did (or did not do) as medically inappropriate. In medical malpractice cases, that is ordinarily measured by what the usual or common practice is among prudent physicians. In rare circumstances, courts have found the standard practice of a profession to be negligent. Where, for example, it was custom for a professional not to give an eye pressure test to anyone under age 40, a court found that common standard to be inappropriate.13 In the words of Judge Learned Hand (speaking about a different case), “a whole calling may have unduly lagged in the adoption of new and available devices. It never may set its own tests.”14 Underlying negligence is a cost-benefit analysis (discussed below).
- Damages. There must have been some damage that courts recognize, usually loss of money or opportunity to work, the cost of care, pain and suffering, or loss of enjoyment/quality of life. In malpractice, many states now recognize the “loss of chance” or the “loss of a chance.” That means, if a “physician negligently fails to diagnose a curable disease, and the patient is harmed by the disease, the physician should be liable for causing the ‘loss of a chance of a cure.’”15 (Delay in diagnosis is the most common reason for claims in breast cancer care.)16
- Causation. The breach of duty (negligence) must have caused the damages. The causation must have been reasonably close. If a driver drives through a stop sign, or a physician misreads a test, and someone is injured but there is no connection between the negligence and the injury, there is not tort liability.
The 4 elements of malpractice just described are raised in some way in the possible liability associated with BRCA testing. We next look at the ways in which liability may arise from that testing (or lack of it).
Underlying much of the following discussion is the “cost-benefit” consideration noted above. This concept is that the total cost (financial and health) of testing should be compared with the value of the benefits of testing, taking into account the probabilities that the testing will result in better health outcomes. BRCA testing, for example, is essentially cost-free in terms of physical risk. Its financial cost, while not trivial, is not great, and it is commonly covered by health insurance.17 In terms of benefits, the testing has the potential for providing critical information in making treatment decisions for a meaningful percentage of patients and their families. There are many ways of analyzing the liability risks of genetic malpractice,7,18 and the following is intended to discuss some of the greatest risks related to BRCA testing.
Continue to: Areas of liability...
Areas of liability
The failure to recommend a test. The circumstances in which BRCA testing should be undertaken are set out by professional organizations (noted above). These recommendations are not static, however. They change from time to time. Given the potential harm caused by the failure to test in relevant circumstances, malpractice liability is certainly a possibility when the failure to recommend a test to a patient results in a cancer that might have been prevented had the genetic problem been identified in a timely manner. The circumstances in which testing should be considered continue to change, placing an obligation on clinicians to stay well informed of changing genetic understandings. Another risk is that one specialist may assume that it is the job of another specialist to order the test. Whatever the cause of the failure to test, or unnecessary delay in testing, it appears to be the primary basis for BRCA liability.
The failure to properly interpret a test. Any test that is misinterpreted may lead to harm for the patient. A false negative, of course, may mean that preventive treatment that could have been undertaken will be foregone, as a “loss of a chance.” On the other hand, a false positive can lead to radical, unnecessary surgery or treatment. If a misinterpretation occurred because of carelessness by the testing organization, or confusion by a practitioner, there is a likelihood of negligence.19
A different form of “misinterpretation” could be reasonable—and not negligent. Advances in scientific-medical understanding may result in the outcome of tests being reconsidered and changed. That has been the case with genetic testing and breast cancer. The availability of multiple breast cancer SNPs (single nucleotide polymorphisms), and combining this information with other risk factors for example, results in a polygenic risk score that may be at odds with the level of risk from earlier testing.20,21 This naturally leads to the question of when later, updated testing should be recommended to look for a better current interpretation.22,23
The failure to act on BRCA test results. Testing is of no value, of course, if the results are not used properly. Test results or analyses that are not sent to the proper physicians, or are somehow ignored when properly directed, is a “never” event—it should never happen. It almost always would be considered negligence, and if the patient were injured, could lead to liability. Amazingly, one study found that, in genetic testing liability cases, nearly 20% of the claims arose from failure to return test results to patients.24 In addition, when a patient is found to be BRCA-positive, there is an obligation to discuss the options for dealing with the increased risk associated with the gene mutation(s), as well as to recommend the prudent course of action or to refer the patient to someone who will have that discussion.
Informed consent to the patient. BRCA testing requires informed consent. The physical risks of the testing process are minimal, of course, but it carries a number of other emotional and family risks. The informed consent process is an invitation to an honest discussion between clinicians and patients. It should be an opportunity to discuss what the testing is, and is not, and what the test may mean for treatment. It may also be an opportunity to discuss the implications for other members of the patient’s family (noted below).
One element of informed consent is a discussion of the consequences of failure to consent, or to undertake one of the alternatives. In the case of BRCA testing, this is especially important in cases in which a patient expresses a hesitancy to be tested with an “I’d rather not know philosophy.” Although clinicians should not practice law, some patient concerns about discrimination may be addressed by the protection that the federal Genetic Information Nondiscrimination Act (GINA) and other laws provide (which prohibit insurance and employment discrimination based on genetic information). A good source of information about GINA and related nondiscrimination laws is provided by the National Human Genome Research Institute.25 In addition, the National Institutes of Health has a website that may be helpful to many patients26 (and a much more complex site for health professionals).27 At the same time, courts have resisted plaintiffs/patients who have tried to use informed consent as a way of suing for failure to offer genetic testing.28,29
The failure to refer. In some cases, a patient should be formally referred for genetics consultation. The considerations here are similar to other circumstances in modern, fast developing medical practice that require special sensitivity to those occasions in which a patient will benefit from additional expertise. It is a principle that the AMA Council on Ethical and Judicial Affairs has expressed this way: “In the absence of adequate expertise in pretest and posttest counseling, a physician should refer the patient to an appropriate specialist.”30 The failure to refer, when that deviates from acceptable practice, may result in liability.
Informing others. BRCA testing is an area of medicine in which results may be of great significance not only to the patient but also to the patient’s family.31 Physicians should counsel patients on the importance of informing relatives about relevant results and “should make themselves available to assist patients in communicating with relatives to discuss opportunities for counseling and testing, as appropriate.”30 The question may arise, however, of whether in some circumstances physicians should go a step further in ensuring relatives receive important information regarding their loved one’s health.32 The law has been reluctant to impose liability to “third parties” (someone not a patient). Duties usually arise through the physician-patient relationship. There are exceptions. Perhaps the best known has been the obligation of mental health professionals to take action to protect third parties from patients who have made believable threats against identifiable victims.33 There are indications that some courts could find, in extreme circumstances, a “duty to warn” nonpatients in some instances where it is essential to inform third parties that they should receive a specific form of genetic testing.34,35 Such a duty would, of course, have to protect the privacy rights of the patient to the maximum extent possible. A general duty of this type has not been established widely, but may be part of the future.
Continue to: Was there liability in our example case?...
Was there liability in our example case?
The hypothetical case provided above suggests that there could be liability. Routine medical history by the primary care physician would have produced the fact that the patient’s mother, sister, and maternal grandmother had breast cancer. That would clearly have put her in a category of those who should have received genetic testing. Yet, she was not tested until after her cancer was found. From the limited facts we have, it appears that this timeline of events would have been outside accepted practice—and negligent. The case was not pursued by the patient, however, and this may represent the current state of liability for BRCA issues.
The extent of liability seems to be significant
Our discussion of liability suggests that there is significant potential for BRCA testing negligence within practice, and that the damages in these cases could be substantial. Yet the predicted “tsunami” of malpractice lawsuits related to genetic testing has not appeared.36,37 One study of cases in the United States (through 2016) found a “slowly rising tide” of liability cases instead of a tsunami,24 as the number of claims made was low. On the other hand, the payments where damages were awarded were an order of magnitude larger than other malpractice cases—a mean of $5.3 million and median of $2 million. This is compared with mean values in the range of $275,000 to $600,000 in other areas of malpractice.
The majority of the genetic malpractice cases involve prenatal and newborn testing, and diagnosis/susceptibility/pharmacogenomic accounting for about 25% of cases. In terms of type of errors claimed, approximately 50% were diagnostic-interpretation errors, 30% failure to offer testing, nearly 20% failure to return test results to the patients, and a few remaining cases of failure to properly treat in light of genetic testing.24
Despite a few very large payments, however, the fact remains that there is a surprisingly low number of genetics malpractice cases. Gary Marchant and colleagues suggest that several reasons may account for this:
- the clinical implementation of genetic science has been slower than expected
- the lack of expertise of many physicians in genetic science
- expert witnesses have sometimes been hard to find
- the lack of understanding by plaintiffs’ attorneys of genetic malpractice
- potential plaintiffs’ lack of understanding of the nature of genetic testing and the harms resulting from genetic negligence.17,24,37
The tide is slowly coming in
By all appearances, there is every reason to think that genetic malpractice will be increasing, and that the recent past of much higher damages per claim paid in the genetics area will be part of that tide. The National Human Genome Research LawSeq project has suggested a number of useful ways of dealing with the liability issues.18 In addition to the BRCA issues that we have considered in this article for ObGyns, there are other critical issues of prenatal and newborn genetic testing.38 But those are topics for another day. ●
CASE Young woman with family history of breast cancer detects lump
Two weeks after noting a lump on her breast when her cat happened to jump on her in that spot, a 28-year-old woman (G0) went to her primary care provider. She was referred to her gynecologist; breast imaging, ultrasonography, and mammography were obtained, with microcalcifications noted. A fine needle aspiration diagnosed intraductal malignancy. The surgical breast tissue specimen was estrogen receptor (ER)- and progestogen receptor (PR)-positive and HER2-negative. Other tumor markers were obtained, including carcinoembryonic antigen, and tissue polypeptide specific antigen, p53, cathepsin D, cyclin E, and nestin, but results were not available.
With regard to family history, the woman’s mother and maternal grandmother had a history of breast cancer. The patient and her family underwent gene testing. The patient was found to be BRCA1- and BRCA2-positive; her mother was BRCA1-positive, an older sister was BRCA2-positive, and her grandmother was not tested.
The question arose in light of her family history as to why she was not tested for BRCA and appropriately counseled by her gynecologist prior to the cancer diagnosis. Litigation was initiated. While the case did not go forward regarding litigation, it is indeed a case in point. (Please note that this is a hypothetical case. It is based on a composite of several cases.)
Medical considerations
Breast cancer is the most common type of cancer affecting women in the Western world.1 Advances in clinical testing for gene mutations have escalated and allowed for identification of patients at increased risk for breast and ovarian cancer. Along with these advances come professional liability risk. After looking at the medical considerations for BRCA1 and 2 testing, we will consider a number of important legal issues. In the view of some commentators, the failure to diagnose genetic mutations in patients predisposed to cancer is “poised to become the next wave of medical professional liability lawsuits.”2
BRCA1 and BRCA2 genes provide tumor suppressor proteins, and assessment for mutations is recommended for individuals at high risk for breast and/or ovarian cancer; mutations in BRCA genes cause DNA damage, which increases the chance of developing cancer. The other way to look at it is, BRCA1 and 2 are tumor suppressor genes that are integrally involved with DNA damage control. Once there is a mutation, it adversely affects the beneficial effects of the gene. Mutations in these genes account for 5% to 10% of all hereditary breast cancers.3 Of note, men with BRCA2 are at increased risk for prostate cancer.
A patient who presents to her gynecologist stating that there is a family history of breast cancer, without knowledge of genetic components, presents a challenge (and a medicolegal risk) for the provider to assess. Prediction models have been used to determine specific patient risk for carrying a genetic mutation with resultant breast cancer development.4 Risk prediction models do not appear to be a good answer to predicting who is more likely to develop breast or ovarian cancer, however. A Mayo model may assist (FIGURE).5 Clinicians should also be aware of other models of risk assessment, including the Gail Model (TABLE 1).6
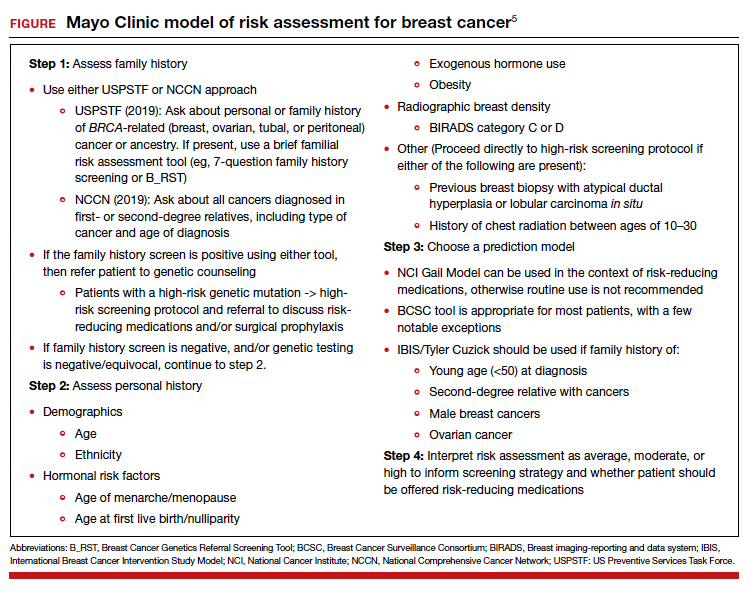
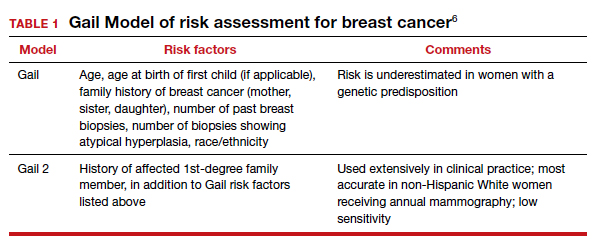
Continue to: Guidelines for genetic testing...
Guidelines for genetic testing
The American College of Obstetricians and Gynecologists states that patient medical history and family history are paramount in obtaining information regarding risk for breast and ovarian cancer. First- and second-degree relatives are allocated to this category. Information regarding age of diagnosis, maternal and paternal lineage, and ethnic background can imply a need for genetic testing (TABLE 2).7,8 A number of genetics national organizations have participated in recommendations and include the American College of Medical Genetics and Genomics, the National Society for Genetic Counselors, and the Society of Gynecologic Oncology.7
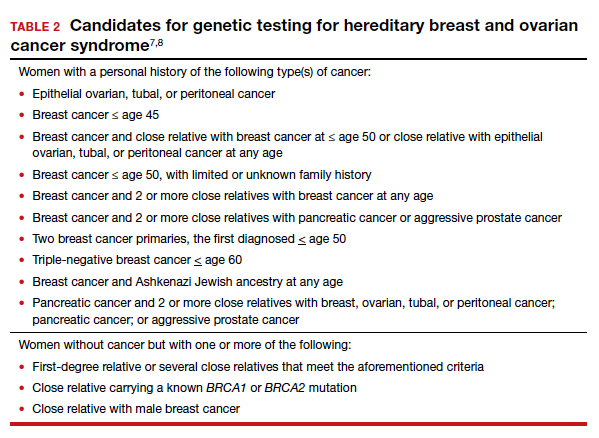
The question always surfaces, could the clinical outcome of the cancer when diagnosed have been changed if screening were undertaken, with earlier diagnosis, or prevented with prophylactic mastectomy, and changed the end result. In addition, it is well known that breast augmentation mammoplasty alters the ability to accurately evaluate mammograms. Patients considering this type of plastic surgery, ideally, should be counselled accordingly.9
Bottom line, we as clinicians must be cognizant of both ACOG and United States Preventive Services Task Force (USPSTF) recommendations regarding screening and gene testing for women considered high risk for breast cancer based on family history.7
Legal considerations
The case presented demonstrates that the discovery of the BRCA1 and BRCA2 genes, and reliable tests for determining the existence of the genes, brought with them legal issues as well as medical advantages. We look at professional liability (malpractice) questions this technology raises, and then consider the outcome of the hypothetical case. (BRCA is used here to apply broadly—not only to BRCA1 and 2 but also to PALB2, CHEK2, and similar genetic abnormalities.)
To date, the most visible BRCA legal issues covered in cases and law reviews have focused more on patent law than malpractice. The most important of these was a decision of the US Supreme Court in Association for Molecular Pathology v Myriad Genetics.10 The US Patent Office was granting patents to companies finding useful, naturally occurring segments of human DNA, and had granted Myriad several patents on BRCA1 and BRCA2 genes. This patent policy had the potential to seriously interfere with broad scientific use of these genes.11 Fortunately, the Supreme Court stepped in and unanimously invalidated such patents. It held that a “naturally occurring DNA segment is a product of nature and not patent eligible merely because it has been isolated.” The Court noted, “Finding the location of the BRCA1 and BRCA2 genes does not render the genes patent eligible ‘new . . . composition[s] of matter.’”8 The Court did allow the patenting of tests for specific gene structures, and artificial changes in naturally occurring genes.
Malpractice and BRCA
While the BRCA patent wars have lingered, the potential for a significant increase in BRCA-related malpractice cases is of increasing concern. Like most malpractice liability, these new claims are based on very old principles of negligence.12 To prevail, the plaintiff (ordinarily, an injured patient) must demonstrate 4 things:
- A duty. That is, the physician owed a duty to the injured party. Usually (but not always) that requires a professional relationship between the physician and the person injured.
- A breach of that duty. Malpractice liability is based on the fact that the physician did something that a reasonably careful physician (generally, of the same specialty) would not have done, or that the physician failed to do something that a reasonable physician would have done. This usually means that the profession itself sees what the physician did (or did not do) as medically inappropriate. In medical malpractice cases, that is ordinarily measured by what the usual or common practice is among prudent physicians. In rare circumstances, courts have found the standard practice of a profession to be negligent. Where, for example, it was custom for a professional not to give an eye pressure test to anyone under age 40, a court found that common standard to be inappropriate.13 In the words of Judge Learned Hand (speaking about a different case), “a whole calling may have unduly lagged in the adoption of new and available devices. It never may set its own tests.”14 Underlying negligence is a cost-benefit analysis (discussed below).
- Damages. There must have been some damage that courts recognize, usually loss of money or opportunity to work, the cost of care, pain and suffering, or loss of enjoyment/quality of life. In malpractice, many states now recognize the “loss of chance” or the “loss of a chance.” That means, if a “physician negligently fails to diagnose a curable disease, and the patient is harmed by the disease, the physician should be liable for causing the ‘loss of a chance of a cure.’”15 (Delay in diagnosis is the most common reason for claims in breast cancer care.)16
- Causation. The breach of duty (negligence) must have caused the damages. The causation must have been reasonably close. If a driver drives through a stop sign, or a physician misreads a test, and someone is injured but there is no connection between the negligence and the injury, there is not tort liability.
The 4 elements of malpractice just described are raised in some way in the possible liability associated with BRCA testing. We next look at the ways in which liability may arise from that testing (or lack of it).
Underlying much of the following discussion is the “cost-benefit” consideration noted above. This concept is that the total cost (financial and health) of testing should be compared with the value of the benefits of testing, taking into account the probabilities that the testing will result in better health outcomes. BRCA testing, for example, is essentially cost-free in terms of physical risk. Its financial cost, while not trivial, is not great, and it is commonly covered by health insurance.17 In terms of benefits, the testing has the potential for providing critical information in making treatment decisions for a meaningful percentage of patients and their families. There are many ways of analyzing the liability risks of genetic malpractice,7,18 and the following is intended to discuss some of the greatest risks related to BRCA testing.
Continue to: Areas of liability...
Areas of liability
The failure to recommend a test. The circumstances in which BRCA testing should be undertaken are set out by professional organizations (noted above). These recommendations are not static, however. They change from time to time. Given the potential harm caused by the failure to test in relevant circumstances, malpractice liability is certainly a possibility when the failure to recommend a test to a patient results in a cancer that might have been prevented had the genetic problem been identified in a timely manner. The circumstances in which testing should be considered continue to change, placing an obligation on clinicians to stay well informed of changing genetic understandings. Another risk is that one specialist may assume that it is the job of another specialist to order the test. Whatever the cause of the failure to test, or unnecessary delay in testing, it appears to be the primary basis for BRCA liability.
The failure to properly interpret a test. Any test that is misinterpreted may lead to harm for the patient. A false negative, of course, may mean that preventive treatment that could have been undertaken will be foregone, as a “loss of a chance.” On the other hand, a false positive can lead to radical, unnecessary surgery or treatment. If a misinterpretation occurred because of carelessness by the testing organization, or confusion by a practitioner, there is a likelihood of negligence.19
A different form of “misinterpretation” could be reasonable—and not negligent. Advances in scientific-medical understanding may result in the outcome of tests being reconsidered and changed. That has been the case with genetic testing and breast cancer. The availability of multiple breast cancer SNPs (single nucleotide polymorphisms), and combining this information with other risk factors for example, results in a polygenic risk score that may be at odds with the level of risk from earlier testing.20,21 This naturally leads to the question of when later, updated testing should be recommended to look for a better current interpretation.22,23
The failure to act on BRCA test results. Testing is of no value, of course, if the results are not used properly. Test results or analyses that are not sent to the proper physicians, or are somehow ignored when properly directed, is a “never” event—it should never happen. It almost always would be considered negligence, and if the patient were injured, could lead to liability. Amazingly, one study found that, in genetic testing liability cases, nearly 20% of the claims arose from failure to return test results to patients.24 In addition, when a patient is found to be BRCA-positive, there is an obligation to discuss the options for dealing with the increased risk associated with the gene mutation(s), as well as to recommend the prudent course of action or to refer the patient to someone who will have that discussion.
Informed consent to the patient. BRCA testing requires informed consent. The physical risks of the testing process are minimal, of course, but it carries a number of other emotional and family risks. The informed consent process is an invitation to an honest discussion between clinicians and patients. It should be an opportunity to discuss what the testing is, and is not, and what the test may mean for treatment. It may also be an opportunity to discuss the implications for other members of the patient’s family (noted below).
One element of informed consent is a discussion of the consequences of failure to consent, or to undertake one of the alternatives. In the case of BRCA testing, this is especially important in cases in which a patient expresses a hesitancy to be tested with an “I’d rather not know philosophy.” Although clinicians should not practice law, some patient concerns about discrimination may be addressed by the protection that the federal Genetic Information Nondiscrimination Act (GINA) and other laws provide (which prohibit insurance and employment discrimination based on genetic information). A good source of information about GINA and related nondiscrimination laws is provided by the National Human Genome Research Institute.25 In addition, the National Institutes of Health has a website that may be helpful to many patients26 (and a much more complex site for health professionals).27 At the same time, courts have resisted plaintiffs/patients who have tried to use informed consent as a way of suing for failure to offer genetic testing.28,29
The failure to refer. In some cases, a patient should be formally referred for genetics consultation. The considerations here are similar to other circumstances in modern, fast developing medical practice that require special sensitivity to those occasions in which a patient will benefit from additional expertise. It is a principle that the AMA Council on Ethical and Judicial Affairs has expressed this way: “In the absence of adequate expertise in pretest and posttest counseling, a physician should refer the patient to an appropriate specialist.”30 The failure to refer, when that deviates from acceptable practice, may result in liability.
Informing others. BRCA testing is an area of medicine in which results may be of great significance not only to the patient but also to the patient’s family.31 Physicians should counsel patients on the importance of informing relatives about relevant results and “should make themselves available to assist patients in communicating with relatives to discuss opportunities for counseling and testing, as appropriate.”30 The question may arise, however, of whether in some circumstances physicians should go a step further in ensuring relatives receive important information regarding their loved one’s health.32 The law has been reluctant to impose liability to “third parties” (someone not a patient). Duties usually arise through the physician-patient relationship. There are exceptions. Perhaps the best known has been the obligation of mental health professionals to take action to protect third parties from patients who have made believable threats against identifiable victims.33 There are indications that some courts could find, in extreme circumstances, a “duty to warn” nonpatients in some instances where it is essential to inform third parties that they should receive a specific form of genetic testing.34,35 Such a duty would, of course, have to protect the privacy rights of the patient to the maximum extent possible. A general duty of this type has not been established widely, but may be part of the future.
Continue to: Was there liability in our example case?...
Was there liability in our example case?
The hypothetical case provided above suggests that there could be liability. Routine medical history by the primary care physician would have produced the fact that the patient’s mother, sister, and maternal grandmother had breast cancer. That would clearly have put her in a category of those who should have received genetic testing. Yet, she was not tested until after her cancer was found. From the limited facts we have, it appears that this timeline of events would have been outside accepted practice—and negligent. The case was not pursued by the patient, however, and this may represent the current state of liability for BRCA issues.
The extent of liability seems to be significant
Our discussion of liability suggests that there is significant potential for BRCA testing negligence within practice, and that the damages in these cases could be substantial. Yet the predicted “tsunami” of malpractice lawsuits related to genetic testing has not appeared.36,37 One study of cases in the United States (through 2016) found a “slowly rising tide” of liability cases instead of a tsunami,24 as the number of claims made was low. On the other hand, the payments where damages were awarded were an order of magnitude larger than other malpractice cases—a mean of $5.3 million and median of $2 million. This is compared with mean values in the range of $275,000 to $600,000 in other areas of malpractice.
The majority of the genetic malpractice cases involve prenatal and newborn testing, and diagnosis/susceptibility/pharmacogenomic accounting for about 25% of cases. In terms of type of errors claimed, approximately 50% were diagnostic-interpretation errors, 30% failure to offer testing, nearly 20% failure to return test results to the patients, and a few remaining cases of failure to properly treat in light of genetic testing.24
Despite a few very large payments, however, the fact remains that there is a surprisingly low number of genetics malpractice cases. Gary Marchant and colleagues suggest that several reasons may account for this:
- the clinical implementation of genetic science has been slower than expected
- the lack of expertise of many physicians in genetic science
- expert witnesses have sometimes been hard to find
- the lack of understanding by plaintiffs’ attorneys of genetic malpractice
- potential plaintiffs’ lack of understanding of the nature of genetic testing and the harms resulting from genetic negligence.17,24,37
The tide is slowly coming in
By all appearances, there is every reason to think that genetic malpractice will be increasing, and that the recent past of much higher damages per claim paid in the genetics area will be part of that tide. The National Human Genome Research LawSeq project has suggested a number of useful ways of dealing with the liability issues.18 In addition to the BRCA issues that we have considered in this article for ObGyns, there are other critical issues of prenatal and newborn genetic testing.38 But those are topics for another day. ●
- Sevilla C, Moatti JP, Reynier CJ, et al. Testing for BRCA1 mutations: a cost-effective analysis. Europ J Human Genetics. 2002;10:599-606.
- Cotton V, Kirkpatrick D. Failure to recommend genetic counseling in breast cancer: is the next wave of medical professional liability lawsuits? Contemp OB/GYN. June 1, 2017.
- Suryavanshi M, Kumar D, Panigrahi M, et al. Detection of false positive mutations in BRCA gene by next generation sequencing. Fam Cancer. 2017;16:311-317.
- Black L, Knoppers B, Avard D, et al. Legal liability and the uncertain nature of risk prediction: the case of breast cancer risk prediction models. Public Health Genomics. 2012;15:335-340.
- McClintock A, Gollab A, Laya M. Breast cancer risk assessment, a step-wise approach for primary care physicians on the front lines of shared decision making. Mayo Clin Proc. 2020;95:1268-1275.
- National Cancer Institute. The Breast Cancer Risk Assessment Tool. https://bcrisktool.cancer.gov/. Accessed February 25, 2021.
- Neff J, Richardson G, Phelps J. Legal liabilities associated with hereditary breast and ovarian cancers. J Reprod Med. 2020;65:227-230.
- American College of Obstetricians and Gynecologists. Practice Bulletin No 182: hereditary breast and ovarian cancer syndrome. Obstet Gynecol. 2017;130:e110-e126.
- Sá dos Reis C, Gremion I, and Meystre NR. Study of breast implants mammography examinations for identification of suitable image quality criteria. Insights Imaging. 2020;11:3.
- Association for Molecular Pathology v Myriad Genetics, 569 U.S. 576 (2013).
- Smith SR. The Supreme Court 2012-2013: dogs, DNA, and DOMA. Register Rep. 2013;39(Fall):26-33.
- Bal BS. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467:339-347.
- Helling v Carey, 83 Wn.2d 514, 519 P.2d 981 (1974).
- The T.J. Hooper, 60 F.2d 737, 740 (2d Cir.1932), cert. denied 287 U.S. 662 (1932).
- Fischer DA. Tort recovery for loss of a chance. Wake Forest L Rev. 2001;36:605-655.
- Murphy BL, Ray-Zack MD, Reddy PN, et al. Breast cancer litigation in the 21st century. Ann Surg Oncol. 2018;25:2939- 2947.
- Prince AE. Prevention for those who can pay: insurance reimbursement of genetic-based preventive interventions in the liminal state between health and disease. J Law Biosci. 2015;2:365-395.
- Marchant G, Barnes M, Evans JP, et al; LawSeq Liability Task Force. From genetics to genomics: facing the liability implications in clinical care. J Law Med Ethics. 2020;48:11-43.
- Complaint, Held v Ambry Genetics Corp., No. 15-CV-8683, 2015 WL 6750024 (S.D.N.Y. Nov. 4, 2015); Order of Dismissal, Held v Ambry Genetics Corp., No. 15-CV-8683, (S.D.N.Y. Dec. 6, 2016).
- Pederson HJ. Breast cancer risk assessment and treatment: current concepts in genetics and genomics. Contemp OB/ GYN. 2017; 62:A1-A4.
- Pederson HJ. Who needs breast cancer genetics testing? OBG Manag. 2018;30:34-39.
- Roberts JL, Foulkes A. Genetic duties. William Mary L Rev. 2020;62:143-212.
- Thorogood A, Cook-Deegan R, Knoppers B. Public variant databases: liability? Genet Med. 2017;19:838–841.
- Marchant G, Lindor R. Genomic malpractice: an emerging tide or gentle ripple? Food Drug Law J. 2018;73:1-37.
- National Human Genome Research Institute. Genetic discrimination. https://www.genome.gov/about-genomics /policy-issues/Genetic-Discrimination. Updated September 16, 2020. Accessed February 25, 2021.
- National Cancer Institute. BRCA mutations: cancer risk and genetic testing. https://www.cancer.gov/about-cancer /causes-prevention/genetics/brca-fact-sheet. Reviewed November 19, 2020. Accessed February 25, 2021.
- National Cancer Institute. Genetics of breast and gynecologic cancers (PDQ®)–Health Professional Version. https://www .cancer.gov/types/breast/hp/breast-ovarian-genetics-pdq. Updated February 12, 2021. Accessed February 25, 2021.
- Reed v Campagnolo, 630 A.2d 1145, 1152–54 (Md. 1993).
- Munro v Regents of Univ. of Cal.,263 Cal. Rptr. 878, 885, 988 (1989).
- AMA Council on Ethical and Judicial Affairs. AMA Code of Medical Ethics’ opinions on genetic testing. Opinion 2.131. 2009;11:683-685. https://journalofethics.ama-assn .org/article/ama-code-medical-ethics-opinions-genetictesting/2009-09.
- Gilbar R, Barnoy S. Disclosing genetic test results to the patient’ relatives: how does the law influence clinical practice? J Law Technol Policy. 2019;125-168.
- Song K. Warning third parties of genetic risks in the era of personalized medicine. U.C. Davis L Rev. 2016;49:1987-2018.
- Tarasoff v Regents of the University of California, 551 P.2d 334, 131 Cal. Rptr. 14 (Cal. 1976).
- Safer v Estate of Pack, 677 A.2d 1188 (N.J. App. 1996), cert. denied, 683 A.2d 1163 (N.J. 1996).
- Pate v Threlkel, 661 So.2d 278 (Fla. 1995).
- Rothstein MA. Liability issues in pharmacogenomics. Louisiana L Rev. 2005;66:117-124.
- Marchant G, Lindor R. Personalized medicine and genetic malpractice. Genet Med. 2013;15:921-922.
- Westbrook M. Transforming the physician’s standard of care in the context of whole genome sequencing technologies: finding guidance in best practice standards. Saint Louis U J Health Law Policy. 2015;9:111-148.
- Sevilla C, Moatti JP, Reynier CJ, et al. Testing for BRCA1 mutations: a cost-effective analysis. Europ J Human Genetics. 2002;10:599-606.
- Cotton V, Kirkpatrick D. Failure to recommend genetic counseling in breast cancer: is the next wave of medical professional liability lawsuits? Contemp OB/GYN. June 1, 2017.
- Suryavanshi M, Kumar D, Panigrahi M, et al. Detection of false positive mutations in BRCA gene by next generation sequencing. Fam Cancer. 2017;16:311-317.
- Black L, Knoppers B, Avard D, et al. Legal liability and the uncertain nature of risk prediction: the case of breast cancer risk prediction models. Public Health Genomics. 2012;15:335-340.
- McClintock A, Gollab A, Laya M. Breast cancer risk assessment, a step-wise approach for primary care physicians on the front lines of shared decision making. Mayo Clin Proc. 2020;95:1268-1275.
- National Cancer Institute. The Breast Cancer Risk Assessment Tool. https://bcrisktool.cancer.gov/. Accessed February 25, 2021.
- Neff J, Richardson G, Phelps J. Legal liabilities associated with hereditary breast and ovarian cancers. J Reprod Med. 2020;65:227-230.
- American College of Obstetricians and Gynecologists. Practice Bulletin No 182: hereditary breast and ovarian cancer syndrome. Obstet Gynecol. 2017;130:e110-e126.
- Sá dos Reis C, Gremion I, and Meystre NR. Study of breast implants mammography examinations for identification of suitable image quality criteria. Insights Imaging. 2020;11:3.
- Association for Molecular Pathology v Myriad Genetics, 569 U.S. 576 (2013).
- Smith SR. The Supreme Court 2012-2013: dogs, DNA, and DOMA. Register Rep. 2013;39(Fall):26-33.
- Bal BS. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467:339-347.
- Helling v Carey, 83 Wn.2d 514, 519 P.2d 981 (1974).
- The T.J. Hooper, 60 F.2d 737, 740 (2d Cir.1932), cert. denied 287 U.S. 662 (1932).
- Fischer DA. Tort recovery for loss of a chance. Wake Forest L Rev. 2001;36:605-655.
- Murphy BL, Ray-Zack MD, Reddy PN, et al. Breast cancer litigation in the 21st century. Ann Surg Oncol. 2018;25:2939- 2947.
- Prince AE. Prevention for those who can pay: insurance reimbursement of genetic-based preventive interventions in the liminal state between health and disease. J Law Biosci. 2015;2:365-395.
- Marchant G, Barnes M, Evans JP, et al; LawSeq Liability Task Force. From genetics to genomics: facing the liability implications in clinical care. J Law Med Ethics. 2020;48:11-43.
- Complaint, Held v Ambry Genetics Corp., No. 15-CV-8683, 2015 WL 6750024 (S.D.N.Y. Nov. 4, 2015); Order of Dismissal, Held v Ambry Genetics Corp., No. 15-CV-8683, (S.D.N.Y. Dec. 6, 2016).
- Pederson HJ. Breast cancer risk assessment and treatment: current concepts in genetics and genomics. Contemp OB/ GYN. 2017; 62:A1-A4.
- Pederson HJ. Who needs breast cancer genetics testing? OBG Manag. 2018;30:34-39.
- Roberts JL, Foulkes A. Genetic duties. William Mary L Rev. 2020;62:143-212.
- Thorogood A, Cook-Deegan R, Knoppers B. Public variant databases: liability? Genet Med. 2017;19:838–841.
- Marchant G, Lindor R. Genomic malpractice: an emerging tide or gentle ripple? Food Drug Law J. 2018;73:1-37.
- National Human Genome Research Institute. Genetic discrimination. https://www.genome.gov/about-genomics /policy-issues/Genetic-Discrimination. Updated September 16, 2020. Accessed February 25, 2021.
- National Cancer Institute. BRCA mutations: cancer risk and genetic testing. https://www.cancer.gov/about-cancer /causes-prevention/genetics/brca-fact-sheet. Reviewed November 19, 2020. Accessed February 25, 2021.
- National Cancer Institute. Genetics of breast and gynecologic cancers (PDQ®)–Health Professional Version. https://www .cancer.gov/types/breast/hp/breast-ovarian-genetics-pdq. Updated February 12, 2021. Accessed February 25, 2021.
- Reed v Campagnolo, 630 A.2d 1145, 1152–54 (Md. 1993).
- Munro v Regents of Univ. of Cal.,263 Cal. Rptr. 878, 885, 988 (1989).
- AMA Council on Ethical and Judicial Affairs. AMA Code of Medical Ethics’ opinions on genetic testing. Opinion 2.131. 2009;11:683-685. https://journalofethics.ama-assn .org/article/ama-code-medical-ethics-opinions-genetictesting/2009-09.
- Gilbar R, Barnoy S. Disclosing genetic test results to the patient’ relatives: how does the law influence clinical practice? J Law Technol Policy. 2019;125-168.
- Song K. Warning third parties of genetic risks in the era of personalized medicine. U.C. Davis L Rev. 2016;49:1987-2018.
- Tarasoff v Regents of the University of California, 551 P.2d 334, 131 Cal. Rptr. 14 (Cal. 1976).
- Safer v Estate of Pack, 677 A.2d 1188 (N.J. App. 1996), cert. denied, 683 A.2d 1163 (N.J. 1996).
- Pate v Threlkel, 661 So.2d 278 (Fla. 1995).
- Rothstein MA. Liability issues in pharmacogenomics. Louisiana L Rev. 2005;66:117-124.
- Marchant G, Lindor R. Personalized medicine and genetic malpractice. Genet Med. 2013;15:921-922.
- Westbrook M. Transforming the physician’s standard of care in the context of whole genome sequencing technologies: finding guidance in best practice standards. Saint Louis U J Health Law Policy. 2015;9:111-148.
2021 Update on gynecologic cancer
Gynecologic malignancies continue to be a major cause of cancer-related mortality in women. In 2020, a number of developments changed practice in gynecologic oncology. In this Update, we highlight 3 important articles. The first showed that human papillomavirus (HPV) vaccination reduced the rate of cervical cancer. The next evaluated a novel targeted therapeutic approach using the combination of pembrolizumab and lenvatinib in women with recurrent endometrial carcinoma that progressed after prior systemic therapy. Finally, the third article showed that talcum powder was not associated with an increased risk of ovarian cancer. We provide here a brief overview of the major findings of these studies and how these results are influencing practice.
Evidence establishes that HPV vaccination cuts risk of invasive cervical cancer
Lei J, Ploner A, Elfström KM, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med. 2020;383:1340-1348.
HPV infection is associated with 99% of cervical cancers, and approximately 65% to 75% of cases involve HPV 16 or 18.1,2 The quadrivalent HPV (6, 11, 16, 18) vaccine was approved by the US Food and Drug Administration in 2006 for the prevention of cervical intraepithelial lesions and genital warts associated with HPV.3-5 Previous studies of the HPV vaccine showed it to be effective in preventing HPV infection, genital warts, and high-grade precancerous cervical lesions, such as cervical intraepithelial neoplasia grade 2 (CIN2) and grade 3 (CIN3).6-8 While the vaccine offers a number of advantages, the long-term goal of the vaccine—to reduce the incidence of invasive cervical cancer—was not shown until recently.
Large study followed HPV vaccinated and unvaccinated women
Lei and colleagues conducted a registry based cohort study from 2006 through 2017 of women aged 10 to 30 years who were living in Sweden.9 They followed the women from their 10th birthday until they were diagnosed with cervical cancer, died, emigrated from Sweden, were lost to follow-up, or turned 31 years of age. In the study, the unique personal identity numbers assigned to all Swedish residents were linked to a number of large national administrative databases. Beginning in 2007 in Sweden, the quadrivalent vaccine was subsidized for use in girls aged 13 to 17, and a subsequent catch-up period that started in 2012 incorporated women who had not been vaccinated.
Continue to: Cervical cancer rates were lowest in women vaccinated before age 17...
Cervical cancer rates were lowest in women vaccinated before age 17
A total of 1,672,983 women were included in the study; 527,871 received at least one dose of the HPV vaccine. During the study period, cervical cancer was diagnosed in 19 women who had received the quadrivalent HPV vaccine and in 538 women who had not received the vaccine. Women who initiated vaccination before age 17 had the lowest rates of cervical cancer (4 cases per 100,000 persons), followed by women vaccinated after age 17 (54 cases per 100,000 persons) and then those who were not vaccinated (94 cases per 100,000 persons).
After adjusting for confounders, the incidence rate ratio (RR) of cervical cancer was significantly lower among vaccinated women compared with unvaccinated women (RR, 0.37; 95% confidence interval [CI], 0.21– 0.57) (FIGURE 1).9 In addition, women who were vaccinated before age 17 demonstrated the greatest benefit. For those vaccinated before age 17 versus those who were unvaccinated, the RR was 0.12 (95% CI, 0.00–0.34). For women vaccinated between age 17 and 30 versus unvaccinated women, the RR was 0.47 (95% CI, 0.27–0.75).
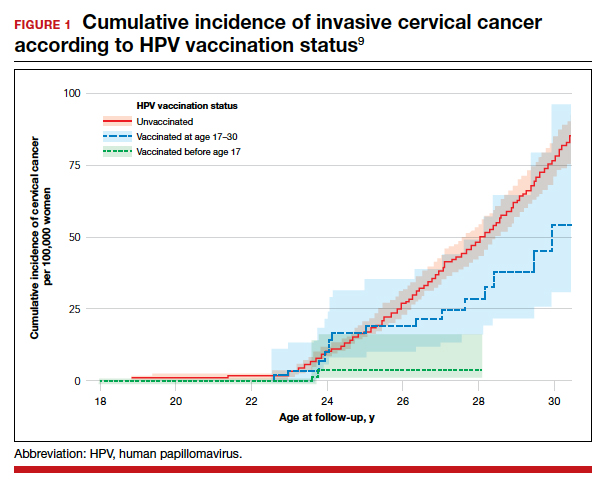
The study by Lei and colleagues showed that HPV vaccination was associated with a substantially lower risk of invasive cervical cancer. While all women who received the vaccine had reduced rates of invasive cervical cancer, those who received the vaccine earlier (before age 17) showed the greatest reduction in invasive cervical cancer. On a population level, this study demonstrates that a program of HPV vaccination can reduce the burden of cervical cancer.
Promising option for patients with advanced endometrial cancer: Lenvatinib plus pembrolizumab
Makker V, Taylor MH, Aghajanian C, et al. Lenvatinib plus pembrolizumab in patients with advanced endometrial cancer. J Clin Oncol. 2020;38:2981-2992.
Advanced stage endometrial cancer is associated with a 17% 5-year survival rate.10 Paclitaxel with carboplatin is the standard first-line treatment for advanced, recurrent, and metastatic endometrial cancer; for women who do not respond to this regimen, effective treatment options are limited.11,12
The immunotherapy approach
Immunotherapy is a more recently developed treatment, an approach in which the immune system is activated to target cancer cells. Pembrolizumab is a commonly used agent for many solid tumors.13 This drug binds to the programmed cell death receptor 1 (PD-1) or PD-ligand 1 (PD-L1), a component of the immune checkpoint, which then allows the immune system to target and destroy cancer cells.14
Prembrolizumab is FDA approved for use in the treatment of microsatellite instability-high (MSI-H)/mismatch repair deficient (dMMR) solid tumors that have progressed after prior therapy and for which there are no satisfactory alternative treatment options.15 Endometrial cancers frequently display microsatellite instability and mismatch repair defects.16
Lenvatinib is an oral multikinase inhibitor that targets vascular endothelial growth factor receptors 1, 2, and 3; fibroblast growth factor receptors 1, 2, 3, and 4; and platelet derived growth factor receptor alpha, RET, and KIT.17-19 In a phase 2 study of lenvatinib monotherapy for advanced previously treated endometrial cancer, the response rate was 14.3%.20
While some preclinical studies have examined the combination of immune checkpoint inhibitors with lenvatinib,21-23 a recent study is the first to evaluate this combination in patients with advanced tumors.24
Continue to: Prembrolizumab-lenvatinib combination therapy...
Prembrolizumab-lenvatinib combination therapy
Makker and colleagues conducted an ongoing multinational, open-label, phase 1B/2 study of lenvatinib 20 mg daily orally plus pembrolizumab 200 mg intravenously once every 3 weeks in patients with select solid tumors.24 Women with previously treated endometrial carcinoma (N = 125) were included. Of the study participants, 49% were PD-L1 positive and 10% were MSI-H/dMMR. The primary end point was objective response rate (ORR) at 24 weeks, which was 38.0% (95% CI, 28.8%–47.8%).
The median duration of response was 21.2 months (95% CI, 7.6 months to not estimable). The ORR was similar in patients with PD-L1 expressing tumors (35.8%; 95% CI, 23.1%–50.2%), who are more likely to respond to immunotherapy, compared with those without PD-L1 expression (39.5%; 95% CI, 25.0%–55.6%). For patients with MSI-H/dMMR, there was a higher ORR (63.6%; 95% CI, 30.8%–89.1%, versus 36.2%; 95% CI, 26.5%–46.7%).
Median progression-free survival was 7.4 months (95% CI, 5.3–8.7 months) and median overall survival was 16.7 months (15 months to not estimable). Moderate to severe treatment-related adverse events occurred in 83 patients (66.9%), and 22 patients (17.7%) discontinued 1 or both study drugs because of adverse effects. Two deaths were judged to be treatment related.
This study showed promising results for the combination of pembrolizumab with lenvatinib in women with advanced endometrial carcinoma who have progressed after prior systemic therapy. These data led to an accelerated approval by the FDA for the treatment of women with advanced endometrial carcinoma that is not MSI-H/dMMR, who have disease progression after prior systemic therapy, and who are not candidates for curative surgery or radiation therapy.25 Currently, 2 phase 3 trials of lenvatinib plus pembrolizumab in advanced endometrial carcinoma are underway, which will shed further light on this combination therapy
What is the risk of ovarian cancer in women who use powder in the genital area?
O’Brien KM, Tworoger SS, Harris HR, et al. Association of powder use in the genital area with risk of ovarian cancer. JAMA. 2020;323:49-59.
Women apply talcum powder to their genital area to keep skin dry and to prevent rashes. Powder can be applied by direct application, sanitary napkins, diaphragms, or tampons. Most powder products contain the mineral talc. Because it often is found in nature with asbestos, a known carcinogen, talc’s carcinogenic effects have been investigated.26,27
Talc also might ascend through the genital tract and irritate the epithelial lining of the fallopian tubes or ovaries, possibly triggering an inflammatory response that may promote carcinogenesis.28,29 Case-control studies have reported a possible association between genital powder use and ovarian cancer.30,31 Since these studies, talc-related lawsuits and media coverage have increased.32,33
Large prospective cohorts provide data for analysis
In a pooled analysis of 4 large US-based observational cohorts between 1976 and 2017, O’Brien and colleagues noted that 38% of the 252,745 women included in the study self-reported the use of powder in the genital area.34 With a median of 11.2 years of follow-up, 2,168 women developed ovarian cancer (58 cases/100,000 person-years). Among women who reported using genital powder, the incidence of ovarian cancer was 61 cases/100,000 person-years, while for women who reported never using genital powder, the incidence was 55 cases/100,000 person-years. This corresponded to an estimated hazard ratio (HR) of 1.08 (95% CI, 0.99–1.17).
Frequent powder use, long-term use, and never use. Similar findings were seen for those with frequent use versus never use (HR, 1.09; 95% CI, 0.97–1.23) and long-term use versus never use (HR, 1.01; 95% CI, 0.82– 1.25). When restricting the group to women with a patent reproductive tract at baseline, the HR was 1.13 (95% CI, 1.01–1.26), but the P value for interaction comparing women with versus women without a patent reproductive tract was 0.15 (FIGURE 2).34
Bottom line. In contrast to a prior meta-analysis, in this study there was no statistically significant association between the self-reported use of powder in the genital area and the incidence of ovarian cancer. ●
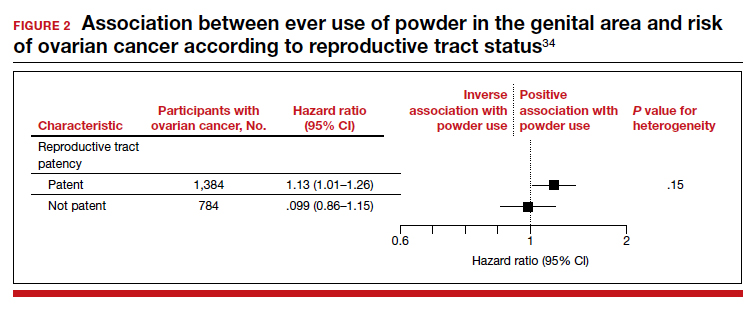
The study by O’Brien and colleagues is the largest study to date with the longest follow-up that examines the possible association between talc-based powder use and ovarian cancer. A strength of this study is the avoidance of recall bias by the selection of administrative data sets that had gathered information on talcum powder use from patients prior to the diagnosis of ovarian cancer. While these findings are reassuring, the study may have been underpowered to identify a small increase in ovarian cancer risk with talc use.
- de Sanjose S, Quint WG, Alemany L, et al; Retrospective International Survey and HPV Time Trends Study Group. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11:1048-1056.
- Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12-19.
- Ault KA; Future II Study Group. Effect of prophylactic human papillomavirus L1 virus-like-particle vaccine on risk of cervical intraepithelial neoplasia grade 2, grade 3, and adenocarcinoma in situ: a combined analysis of four randomised clinical trials. Lancet. 2007;369:1861-1868.
- Garland SM, Hernandez-Avila M, Wheeler CM, et al; Females United to Unilaterally Reduce Endo/Ectocervical disease (FUTURE) I Investigators. Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med. 2007;356:1928-1943.
- Joura EA, Leodolter S, Hernandez-Avila M, et al. Efficacy of a quadrivalent prophylactic human papillomavirus (types 6, 11, 16, and 18) L1 virus-like-particle vaccine against highgrade vulval and vaginal lesions: a combined analysis of three randomised clinical trials. Lancet. 2007;369:1693-1702.
- Arbyn M, Xu L, Simoens C, et al. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst Rev. 2018;5(5):CD009069.
- Paavonen J, Naud P, Salmerón J, et al; HPV PATRICIA Study Group. Efficacy of human papillomavirus (HPV)-16/18 AS04- adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet. 2009;374:301-314.
- FUTURE II Study Group. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med. 2007;356:1915-1927.
- Lei J, Ploner A, Elfström KM, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med. 2020;383:1340-1348.
- American Cancer Society. Survival rates for endometrial cancer. https://www.cancer.org/cancer/endometrial-cancer/ detection-diagnosis-staging/survival-rates.html. Accessed February 9, 2021.
- Miller D, Filiaci V, Fleming G, et al. Late-breaking abstract 1: Randomized phase III noninferiority trial of first line chemotherapy for metastatic or recurrent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol. 2012;125:771.
- National Comprehensive Cancer Network. Clinical practice guidelines in oncology: uterine neoplasms. Version 3.2019. https://www.nccn.org/professionals/physician_gls/pdf /uterine.pdf. Accessed February 9, 2021.
- Marcus L, Lemery SJ, Keegan P, et al. FDA approval summary: pembrolizumab for the treatment of microsatellite instabilityhigh solid tumors. Clin Cancer Res. 2019;25:3753-3758.
- Arora E, Masab M, Mittar P, et al. Role of immune checkpoint inhibitors in advanced or recurrent endometrial cancer. Cureus. 2018;10:e2521.
- Keytruda (pembrolizumab). Package insert. Merck Sharp & Dohme; 2018.
- Cancer Genome Atlas Research Network; Kandoth C, Schultz N, Cherniak AD, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67-73.
- Matsui J, Yamamoto Y, Funahashi Y, et al. E7080, a novel inhibitor that targets multiple kinases, has potent antitumor activities against stem cell factor producing human small cell lung cancer H146, based on angiogenesis inhibition. Int J Cancer. 2008;122:664-671.
- Okamoto K, Kodama K, Takase K, et al. Antitumor activities of the targeted multi-tyrosine kinase inhibitor lenvatinib (E7080) against RET gene fusion-driven tumor models. Cancer Lett. 2013;340:97-103.
- Tohyama O, Matsui J, Kodama K, et al. Antitumor activity of lenvatinib (E7080): an angiogenesis inhibitor that targets multiple receptor tyrosine kinases in preclinical human thyroid cancer models. J Thyroid Res. 2014;2014: 638747.
- Vergote I, Teneriello M, Powell MA, et al. A phase II trial of lenvatinib in patients with advanced or recurrent endometrial cancer: angiopoietin-2 as a predictive marker for clinical outcomes. J Clin Oncol. 2013;31(15 suppl): abstract 5520.
- Kimura T, Kato Y, Ozawa Y, et al. Immunomodulatory activity of lenvatinib contributes to antitumor activity in the Hepa1-6 hepatocellular carcinoma model. Cancer Sci. 2018;109:3993-4002.
- Kato Y, Tabata K, Hori Y, et al. Effects of lenvatinib on tumorassociated macrophages enhance antitumor activity of PD-1 signal inhibitors. Mol Cancer Ther. 2015;14(12 suppl 2): abstract A92.
- Kato Y, Bao X, Macgrath S, et al. Lenvatinib mesilate (LEN) enhanced antitumor activity of a PD-1 blockade agent by potentiating Th1 immune response. Ann Oncol. 2016;27(suppl 6): abstract 2PD.
- Makker V, Taylor MH, Aghajanian C, et al. Lenvatinib plus pembrolizumab in patients with advanced endometrial cancer. J Clin Oncol. 2020;38:2981-2992.
- Lenvima (lenvatinib). Package insert. Woodcliff Lake, NJ: Eisai; 2019.
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Carbon black, titanium dioxide, and talc. IARC Monogr Eval Carcinog Risks Hum. 2010;93:1-413.
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Arsenic, metals, fibres, and dusts. IARC Monogr Eval Carcinog Risks Hum. 2012;100(pt C):11-465.
- Erickson BK, Conner MG, Landen CN Jr. The role of the fallopian tube in the origin of ovarian cancer. Am J Obstet Gynecol. 2013;209:409-414.
- Ness RB, Cottreau C. Possible role of ovarian epithelial inflammation in ovarian cancer. J Natl Cancer Inst. 1999;91:1459-1467.
- Terry KL, Karageorgi S, Shvetsov YB, et al; Ovarian Cancer Association Consortium. Genital powder use and risk of ovarian cancer: a pooled analysis of 8,525 cases and 9,859 controls. Cancer Prev Res. 2013;6:811-821.
- Penninkilampi R, Eslick GD. Perineal talc use and ovarian cancer: a systematic review and meta-analysis. Epidemiology. 2018;29:41-49.
- Hsu T. Johnson & Johnson told to pay $4.7 billion in baby powder lawsuit. New York Times. July 12, 2018. Accessed February 18, 2021. https://www.nytimes.com/2018/07/12 /business/johnson-johnson-talcum-powder.html.
- McGinley L. Does talcum powder cause ovarian cancer? Washington Post. August 25, 2017. Accessed February 18, 2021. https://www.washingtonpost.com/news/to-your -health/wp/2017/08/23/does-talcum-powder-cause -ovarian-cancer-experts-are-divided/.
- O’Brien KM, Tworoger SS, Harris HR, et al. Association of powder use in the genital area with risk of ovarian cancer. JAMA. 2020;323:49-59.
Gynecologic malignancies continue to be a major cause of cancer-related mortality in women. In 2020, a number of developments changed practice in gynecologic oncology. In this Update, we highlight 3 important articles. The first showed that human papillomavirus (HPV) vaccination reduced the rate of cervical cancer. The next evaluated a novel targeted therapeutic approach using the combination of pembrolizumab and lenvatinib in women with recurrent endometrial carcinoma that progressed after prior systemic therapy. Finally, the third article showed that talcum powder was not associated with an increased risk of ovarian cancer. We provide here a brief overview of the major findings of these studies and how these results are influencing practice.
Evidence establishes that HPV vaccination cuts risk of invasive cervical cancer
Lei J, Ploner A, Elfström KM, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med. 2020;383:1340-1348.
HPV infection is associated with 99% of cervical cancers, and approximately 65% to 75% of cases involve HPV 16 or 18.1,2 The quadrivalent HPV (6, 11, 16, 18) vaccine was approved by the US Food and Drug Administration in 2006 for the prevention of cervical intraepithelial lesions and genital warts associated with HPV.3-5 Previous studies of the HPV vaccine showed it to be effective in preventing HPV infection, genital warts, and high-grade precancerous cervical lesions, such as cervical intraepithelial neoplasia grade 2 (CIN2) and grade 3 (CIN3).6-8 While the vaccine offers a number of advantages, the long-term goal of the vaccine—to reduce the incidence of invasive cervical cancer—was not shown until recently.
Large study followed HPV vaccinated and unvaccinated women
Lei and colleagues conducted a registry based cohort study from 2006 through 2017 of women aged 10 to 30 years who were living in Sweden.9 They followed the women from their 10th birthday until they were diagnosed with cervical cancer, died, emigrated from Sweden, were lost to follow-up, or turned 31 years of age. In the study, the unique personal identity numbers assigned to all Swedish residents were linked to a number of large national administrative databases. Beginning in 2007 in Sweden, the quadrivalent vaccine was subsidized for use in girls aged 13 to 17, and a subsequent catch-up period that started in 2012 incorporated women who had not been vaccinated.
Continue to: Cervical cancer rates were lowest in women vaccinated before age 17...
Cervical cancer rates were lowest in women vaccinated before age 17
A total of 1,672,983 women were included in the study; 527,871 received at least one dose of the HPV vaccine. During the study period, cervical cancer was diagnosed in 19 women who had received the quadrivalent HPV vaccine and in 538 women who had not received the vaccine. Women who initiated vaccination before age 17 had the lowest rates of cervical cancer (4 cases per 100,000 persons), followed by women vaccinated after age 17 (54 cases per 100,000 persons) and then those who were not vaccinated (94 cases per 100,000 persons).
After adjusting for confounders, the incidence rate ratio (RR) of cervical cancer was significantly lower among vaccinated women compared with unvaccinated women (RR, 0.37; 95% confidence interval [CI], 0.21– 0.57) (FIGURE 1).9 In addition, women who were vaccinated before age 17 demonstrated the greatest benefit. For those vaccinated before age 17 versus those who were unvaccinated, the RR was 0.12 (95% CI, 0.00–0.34). For women vaccinated between age 17 and 30 versus unvaccinated women, the RR was 0.47 (95% CI, 0.27–0.75).
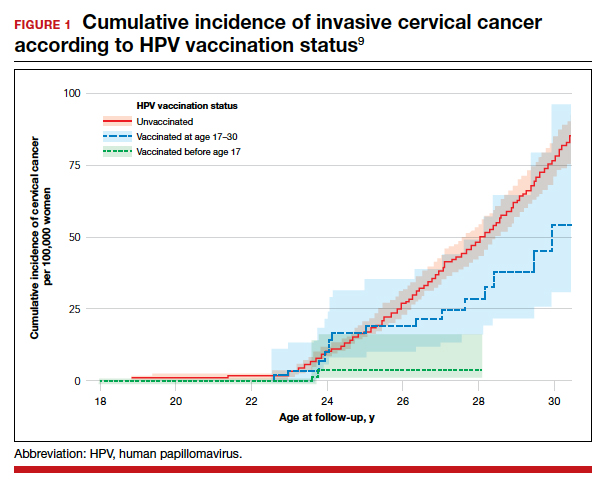
The study by Lei and colleagues showed that HPV vaccination was associated with a substantially lower risk of invasive cervical cancer. While all women who received the vaccine had reduced rates of invasive cervical cancer, those who received the vaccine earlier (before age 17) showed the greatest reduction in invasive cervical cancer. On a population level, this study demonstrates that a program of HPV vaccination can reduce the burden of cervical cancer.
Promising option for patients with advanced endometrial cancer: Lenvatinib plus pembrolizumab
Makker V, Taylor MH, Aghajanian C, et al. Lenvatinib plus pembrolizumab in patients with advanced endometrial cancer. J Clin Oncol. 2020;38:2981-2992.
Advanced stage endometrial cancer is associated with a 17% 5-year survival rate.10 Paclitaxel with carboplatin is the standard first-line treatment for advanced, recurrent, and metastatic endometrial cancer; for women who do not respond to this regimen, effective treatment options are limited.11,12
The immunotherapy approach
Immunotherapy is a more recently developed treatment, an approach in which the immune system is activated to target cancer cells. Pembrolizumab is a commonly used agent for many solid tumors.13 This drug binds to the programmed cell death receptor 1 (PD-1) or PD-ligand 1 (PD-L1), a component of the immune checkpoint, which then allows the immune system to target and destroy cancer cells.14
Prembrolizumab is FDA approved for use in the treatment of microsatellite instability-high (MSI-H)/mismatch repair deficient (dMMR) solid tumors that have progressed after prior therapy and for which there are no satisfactory alternative treatment options.15 Endometrial cancers frequently display microsatellite instability and mismatch repair defects.16
Lenvatinib is an oral multikinase inhibitor that targets vascular endothelial growth factor receptors 1, 2, and 3; fibroblast growth factor receptors 1, 2, 3, and 4; and platelet derived growth factor receptor alpha, RET, and KIT.17-19 In a phase 2 study of lenvatinib monotherapy for advanced previously treated endometrial cancer, the response rate was 14.3%.20
While some preclinical studies have examined the combination of immune checkpoint inhibitors with lenvatinib,21-23 a recent study is the first to evaluate this combination in patients with advanced tumors.24
Continue to: Prembrolizumab-lenvatinib combination therapy...
Prembrolizumab-lenvatinib combination therapy
Makker and colleagues conducted an ongoing multinational, open-label, phase 1B/2 study of lenvatinib 20 mg daily orally plus pembrolizumab 200 mg intravenously once every 3 weeks in patients with select solid tumors.24 Women with previously treated endometrial carcinoma (N = 125) were included. Of the study participants, 49% were PD-L1 positive and 10% were MSI-H/dMMR. The primary end point was objective response rate (ORR) at 24 weeks, which was 38.0% (95% CI, 28.8%–47.8%).
The median duration of response was 21.2 months (95% CI, 7.6 months to not estimable). The ORR was similar in patients with PD-L1 expressing tumors (35.8%; 95% CI, 23.1%–50.2%), who are more likely to respond to immunotherapy, compared with those without PD-L1 expression (39.5%; 95% CI, 25.0%–55.6%). For patients with MSI-H/dMMR, there was a higher ORR (63.6%; 95% CI, 30.8%–89.1%, versus 36.2%; 95% CI, 26.5%–46.7%).
Median progression-free survival was 7.4 months (95% CI, 5.3–8.7 months) and median overall survival was 16.7 months (15 months to not estimable). Moderate to severe treatment-related adverse events occurred in 83 patients (66.9%), and 22 patients (17.7%) discontinued 1 or both study drugs because of adverse effects. Two deaths were judged to be treatment related.
This study showed promising results for the combination of pembrolizumab with lenvatinib in women with advanced endometrial carcinoma who have progressed after prior systemic therapy. These data led to an accelerated approval by the FDA for the treatment of women with advanced endometrial carcinoma that is not MSI-H/dMMR, who have disease progression after prior systemic therapy, and who are not candidates for curative surgery or radiation therapy.25 Currently, 2 phase 3 trials of lenvatinib plus pembrolizumab in advanced endometrial carcinoma are underway, which will shed further light on this combination therapy
What is the risk of ovarian cancer in women who use powder in the genital area?
O’Brien KM, Tworoger SS, Harris HR, et al. Association of powder use in the genital area with risk of ovarian cancer. JAMA. 2020;323:49-59.
Women apply talcum powder to their genital area to keep skin dry and to prevent rashes. Powder can be applied by direct application, sanitary napkins, diaphragms, or tampons. Most powder products contain the mineral talc. Because it often is found in nature with asbestos, a known carcinogen, talc’s carcinogenic effects have been investigated.26,27
Talc also might ascend through the genital tract and irritate the epithelial lining of the fallopian tubes or ovaries, possibly triggering an inflammatory response that may promote carcinogenesis.28,29 Case-control studies have reported a possible association between genital powder use and ovarian cancer.30,31 Since these studies, talc-related lawsuits and media coverage have increased.32,33
Large prospective cohorts provide data for analysis
In a pooled analysis of 4 large US-based observational cohorts between 1976 and 2017, O’Brien and colleagues noted that 38% of the 252,745 women included in the study self-reported the use of powder in the genital area.34 With a median of 11.2 years of follow-up, 2,168 women developed ovarian cancer (58 cases/100,000 person-years). Among women who reported using genital powder, the incidence of ovarian cancer was 61 cases/100,000 person-years, while for women who reported never using genital powder, the incidence was 55 cases/100,000 person-years. This corresponded to an estimated hazard ratio (HR) of 1.08 (95% CI, 0.99–1.17).
Frequent powder use, long-term use, and never use. Similar findings were seen for those with frequent use versus never use (HR, 1.09; 95% CI, 0.97–1.23) and long-term use versus never use (HR, 1.01; 95% CI, 0.82– 1.25). When restricting the group to women with a patent reproductive tract at baseline, the HR was 1.13 (95% CI, 1.01–1.26), but the P value for interaction comparing women with versus women without a patent reproductive tract was 0.15 (FIGURE 2).34
Bottom line. In contrast to a prior meta-analysis, in this study there was no statistically significant association between the self-reported use of powder in the genital area and the incidence of ovarian cancer. ●
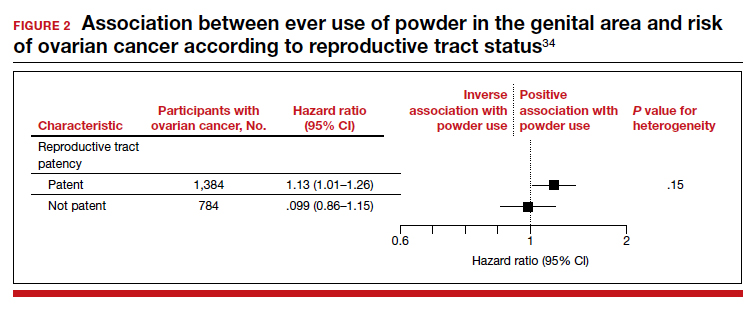
The study by O’Brien and colleagues is the largest study to date with the longest follow-up that examines the possible association between talc-based powder use and ovarian cancer. A strength of this study is the avoidance of recall bias by the selection of administrative data sets that had gathered information on talcum powder use from patients prior to the diagnosis of ovarian cancer. While these findings are reassuring, the study may have been underpowered to identify a small increase in ovarian cancer risk with talc use.
Gynecologic malignancies continue to be a major cause of cancer-related mortality in women. In 2020, a number of developments changed practice in gynecologic oncology. In this Update, we highlight 3 important articles. The first showed that human papillomavirus (HPV) vaccination reduced the rate of cervical cancer. The next evaluated a novel targeted therapeutic approach using the combination of pembrolizumab and lenvatinib in women with recurrent endometrial carcinoma that progressed after prior systemic therapy. Finally, the third article showed that talcum powder was not associated with an increased risk of ovarian cancer. We provide here a brief overview of the major findings of these studies and how these results are influencing practice.
Evidence establishes that HPV vaccination cuts risk of invasive cervical cancer
Lei J, Ploner A, Elfström KM, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med. 2020;383:1340-1348.
HPV infection is associated with 99% of cervical cancers, and approximately 65% to 75% of cases involve HPV 16 or 18.1,2 The quadrivalent HPV (6, 11, 16, 18) vaccine was approved by the US Food and Drug Administration in 2006 for the prevention of cervical intraepithelial lesions and genital warts associated with HPV.3-5 Previous studies of the HPV vaccine showed it to be effective in preventing HPV infection, genital warts, and high-grade precancerous cervical lesions, such as cervical intraepithelial neoplasia grade 2 (CIN2) and grade 3 (CIN3).6-8 While the vaccine offers a number of advantages, the long-term goal of the vaccine—to reduce the incidence of invasive cervical cancer—was not shown until recently.
Large study followed HPV vaccinated and unvaccinated women
Lei and colleagues conducted a registry based cohort study from 2006 through 2017 of women aged 10 to 30 years who were living in Sweden.9 They followed the women from their 10th birthday until they were diagnosed with cervical cancer, died, emigrated from Sweden, were lost to follow-up, or turned 31 years of age. In the study, the unique personal identity numbers assigned to all Swedish residents were linked to a number of large national administrative databases. Beginning in 2007 in Sweden, the quadrivalent vaccine was subsidized for use in girls aged 13 to 17, and a subsequent catch-up period that started in 2012 incorporated women who had not been vaccinated.
Continue to: Cervical cancer rates were lowest in women vaccinated before age 17...
Cervical cancer rates were lowest in women vaccinated before age 17
A total of 1,672,983 women were included in the study; 527,871 received at least one dose of the HPV vaccine. During the study period, cervical cancer was diagnosed in 19 women who had received the quadrivalent HPV vaccine and in 538 women who had not received the vaccine. Women who initiated vaccination before age 17 had the lowest rates of cervical cancer (4 cases per 100,000 persons), followed by women vaccinated after age 17 (54 cases per 100,000 persons) and then those who were not vaccinated (94 cases per 100,000 persons).
After adjusting for confounders, the incidence rate ratio (RR) of cervical cancer was significantly lower among vaccinated women compared with unvaccinated women (RR, 0.37; 95% confidence interval [CI], 0.21– 0.57) (FIGURE 1).9 In addition, women who were vaccinated before age 17 demonstrated the greatest benefit. For those vaccinated before age 17 versus those who were unvaccinated, the RR was 0.12 (95% CI, 0.00–0.34). For women vaccinated between age 17 and 30 versus unvaccinated women, the RR was 0.47 (95% CI, 0.27–0.75).
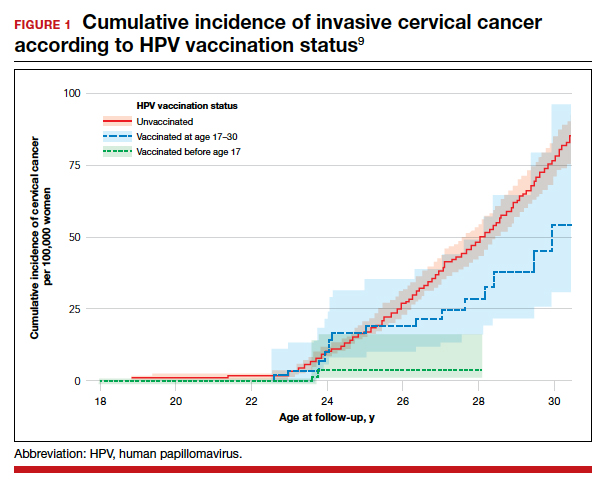
The study by Lei and colleagues showed that HPV vaccination was associated with a substantially lower risk of invasive cervical cancer. While all women who received the vaccine had reduced rates of invasive cervical cancer, those who received the vaccine earlier (before age 17) showed the greatest reduction in invasive cervical cancer. On a population level, this study demonstrates that a program of HPV vaccination can reduce the burden of cervical cancer.
Promising option for patients with advanced endometrial cancer: Lenvatinib plus pembrolizumab
Makker V, Taylor MH, Aghajanian C, et al. Lenvatinib plus pembrolizumab in patients with advanced endometrial cancer. J Clin Oncol. 2020;38:2981-2992.
Advanced stage endometrial cancer is associated with a 17% 5-year survival rate.10 Paclitaxel with carboplatin is the standard first-line treatment for advanced, recurrent, and metastatic endometrial cancer; for women who do not respond to this regimen, effective treatment options are limited.11,12
The immunotherapy approach
Immunotherapy is a more recently developed treatment, an approach in which the immune system is activated to target cancer cells. Pembrolizumab is a commonly used agent for many solid tumors.13 This drug binds to the programmed cell death receptor 1 (PD-1) or PD-ligand 1 (PD-L1), a component of the immune checkpoint, which then allows the immune system to target and destroy cancer cells.14
Prembrolizumab is FDA approved for use in the treatment of microsatellite instability-high (MSI-H)/mismatch repair deficient (dMMR) solid tumors that have progressed after prior therapy and for which there are no satisfactory alternative treatment options.15 Endometrial cancers frequently display microsatellite instability and mismatch repair defects.16
Lenvatinib is an oral multikinase inhibitor that targets vascular endothelial growth factor receptors 1, 2, and 3; fibroblast growth factor receptors 1, 2, 3, and 4; and platelet derived growth factor receptor alpha, RET, and KIT.17-19 In a phase 2 study of lenvatinib monotherapy for advanced previously treated endometrial cancer, the response rate was 14.3%.20
While some preclinical studies have examined the combination of immune checkpoint inhibitors with lenvatinib,21-23 a recent study is the first to evaluate this combination in patients with advanced tumors.24
Continue to: Prembrolizumab-lenvatinib combination therapy...
Prembrolizumab-lenvatinib combination therapy
Makker and colleagues conducted an ongoing multinational, open-label, phase 1B/2 study of lenvatinib 20 mg daily orally plus pembrolizumab 200 mg intravenously once every 3 weeks in patients with select solid tumors.24 Women with previously treated endometrial carcinoma (N = 125) were included. Of the study participants, 49% were PD-L1 positive and 10% were MSI-H/dMMR. The primary end point was objective response rate (ORR) at 24 weeks, which was 38.0% (95% CI, 28.8%–47.8%).
The median duration of response was 21.2 months (95% CI, 7.6 months to not estimable). The ORR was similar in patients with PD-L1 expressing tumors (35.8%; 95% CI, 23.1%–50.2%), who are more likely to respond to immunotherapy, compared with those without PD-L1 expression (39.5%; 95% CI, 25.0%–55.6%). For patients with MSI-H/dMMR, there was a higher ORR (63.6%; 95% CI, 30.8%–89.1%, versus 36.2%; 95% CI, 26.5%–46.7%).
Median progression-free survival was 7.4 months (95% CI, 5.3–8.7 months) and median overall survival was 16.7 months (15 months to not estimable). Moderate to severe treatment-related adverse events occurred in 83 patients (66.9%), and 22 patients (17.7%) discontinued 1 or both study drugs because of adverse effects. Two deaths were judged to be treatment related.
This study showed promising results for the combination of pembrolizumab with lenvatinib in women with advanced endometrial carcinoma who have progressed after prior systemic therapy. These data led to an accelerated approval by the FDA for the treatment of women with advanced endometrial carcinoma that is not MSI-H/dMMR, who have disease progression after prior systemic therapy, and who are not candidates for curative surgery or radiation therapy.25 Currently, 2 phase 3 trials of lenvatinib plus pembrolizumab in advanced endometrial carcinoma are underway, which will shed further light on this combination therapy
What is the risk of ovarian cancer in women who use powder in the genital area?
O’Brien KM, Tworoger SS, Harris HR, et al. Association of powder use in the genital area with risk of ovarian cancer. JAMA. 2020;323:49-59.
Women apply talcum powder to their genital area to keep skin dry and to prevent rashes. Powder can be applied by direct application, sanitary napkins, diaphragms, or tampons. Most powder products contain the mineral talc. Because it often is found in nature with asbestos, a known carcinogen, talc’s carcinogenic effects have been investigated.26,27
Talc also might ascend through the genital tract and irritate the epithelial lining of the fallopian tubes or ovaries, possibly triggering an inflammatory response that may promote carcinogenesis.28,29 Case-control studies have reported a possible association between genital powder use and ovarian cancer.30,31 Since these studies, talc-related lawsuits and media coverage have increased.32,33
Large prospective cohorts provide data for analysis
In a pooled analysis of 4 large US-based observational cohorts between 1976 and 2017, O’Brien and colleagues noted that 38% of the 252,745 women included in the study self-reported the use of powder in the genital area.34 With a median of 11.2 years of follow-up, 2,168 women developed ovarian cancer (58 cases/100,000 person-years). Among women who reported using genital powder, the incidence of ovarian cancer was 61 cases/100,000 person-years, while for women who reported never using genital powder, the incidence was 55 cases/100,000 person-years. This corresponded to an estimated hazard ratio (HR) of 1.08 (95% CI, 0.99–1.17).
Frequent powder use, long-term use, and never use. Similar findings were seen for those with frequent use versus never use (HR, 1.09; 95% CI, 0.97–1.23) and long-term use versus never use (HR, 1.01; 95% CI, 0.82– 1.25). When restricting the group to women with a patent reproductive tract at baseline, the HR was 1.13 (95% CI, 1.01–1.26), but the P value for interaction comparing women with versus women without a patent reproductive tract was 0.15 (FIGURE 2).34
Bottom line. In contrast to a prior meta-analysis, in this study there was no statistically significant association between the self-reported use of powder in the genital area and the incidence of ovarian cancer. ●
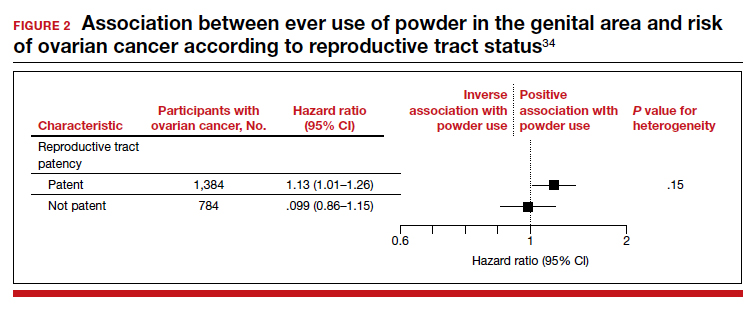
The study by O’Brien and colleagues is the largest study to date with the longest follow-up that examines the possible association between talc-based powder use and ovarian cancer. A strength of this study is the avoidance of recall bias by the selection of administrative data sets that had gathered information on talcum powder use from patients prior to the diagnosis of ovarian cancer. While these findings are reassuring, the study may have been underpowered to identify a small increase in ovarian cancer risk with talc use.
- de Sanjose S, Quint WG, Alemany L, et al; Retrospective International Survey and HPV Time Trends Study Group. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11:1048-1056.
- Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12-19.
- Ault KA; Future II Study Group. Effect of prophylactic human papillomavirus L1 virus-like-particle vaccine on risk of cervical intraepithelial neoplasia grade 2, grade 3, and adenocarcinoma in situ: a combined analysis of four randomised clinical trials. Lancet. 2007;369:1861-1868.
- Garland SM, Hernandez-Avila M, Wheeler CM, et al; Females United to Unilaterally Reduce Endo/Ectocervical disease (FUTURE) I Investigators. Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med. 2007;356:1928-1943.
- Joura EA, Leodolter S, Hernandez-Avila M, et al. Efficacy of a quadrivalent prophylactic human papillomavirus (types 6, 11, 16, and 18) L1 virus-like-particle vaccine against highgrade vulval and vaginal lesions: a combined analysis of three randomised clinical trials. Lancet. 2007;369:1693-1702.
- Arbyn M, Xu L, Simoens C, et al. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst Rev. 2018;5(5):CD009069.
- Paavonen J, Naud P, Salmerón J, et al; HPV PATRICIA Study Group. Efficacy of human papillomavirus (HPV)-16/18 AS04- adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet. 2009;374:301-314.
- FUTURE II Study Group. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med. 2007;356:1915-1927.
- Lei J, Ploner A, Elfström KM, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med. 2020;383:1340-1348.
- American Cancer Society. Survival rates for endometrial cancer. https://www.cancer.org/cancer/endometrial-cancer/ detection-diagnosis-staging/survival-rates.html. Accessed February 9, 2021.
- Miller D, Filiaci V, Fleming G, et al. Late-breaking abstract 1: Randomized phase III noninferiority trial of first line chemotherapy for metastatic or recurrent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol. 2012;125:771.
- National Comprehensive Cancer Network. Clinical practice guidelines in oncology: uterine neoplasms. Version 3.2019. https://www.nccn.org/professionals/physician_gls/pdf /uterine.pdf. Accessed February 9, 2021.
- Marcus L, Lemery SJ, Keegan P, et al. FDA approval summary: pembrolizumab for the treatment of microsatellite instabilityhigh solid tumors. Clin Cancer Res. 2019;25:3753-3758.
- Arora E, Masab M, Mittar P, et al. Role of immune checkpoint inhibitors in advanced or recurrent endometrial cancer. Cureus. 2018;10:e2521.
- Keytruda (pembrolizumab). Package insert. Merck Sharp & Dohme; 2018.
- Cancer Genome Atlas Research Network; Kandoth C, Schultz N, Cherniak AD, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67-73.
- Matsui J, Yamamoto Y, Funahashi Y, et al. E7080, a novel inhibitor that targets multiple kinases, has potent antitumor activities against stem cell factor producing human small cell lung cancer H146, based on angiogenesis inhibition. Int J Cancer. 2008;122:664-671.
- Okamoto K, Kodama K, Takase K, et al. Antitumor activities of the targeted multi-tyrosine kinase inhibitor lenvatinib (E7080) against RET gene fusion-driven tumor models. Cancer Lett. 2013;340:97-103.
- Tohyama O, Matsui J, Kodama K, et al. Antitumor activity of lenvatinib (E7080): an angiogenesis inhibitor that targets multiple receptor tyrosine kinases in preclinical human thyroid cancer models. J Thyroid Res. 2014;2014: 638747.
- Vergote I, Teneriello M, Powell MA, et al. A phase II trial of lenvatinib in patients with advanced or recurrent endometrial cancer: angiopoietin-2 as a predictive marker for clinical outcomes. J Clin Oncol. 2013;31(15 suppl): abstract 5520.
- Kimura T, Kato Y, Ozawa Y, et al. Immunomodulatory activity of lenvatinib contributes to antitumor activity in the Hepa1-6 hepatocellular carcinoma model. Cancer Sci. 2018;109:3993-4002.
- Kato Y, Tabata K, Hori Y, et al. Effects of lenvatinib on tumorassociated macrophages enhance antitumor activity of PD-1 signal inhibitors. Mol Cancer Ther. 2015;14(12 suppl 2): abstract A92.
- Kato Y, Bao X, Macgrath S, et al. Lenvatinib mesilate (LEN) enhanced antitumor activity of a PD-1 blockade agent by potentiating Th1 immune response. Ann Oncol. 2016;27(suppl 6): abstract 2PD.
- Makker V, Taylor MH, Aghajanian C, et al. Lenvatinib plus pembrolizumab in patients with advanced endometrial cancer. J Clin Oncol. 2020;38:2981-2992.
- Lenvima (lenvatinib). Package insert. Woodcliff Lake, NJ: Eisai; 2019.
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Carbon black, titanium dioxide, and talc. IARC Monogr Eval Carcinog Risks Hum. 2010;93:1-413.
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Arsenic, metals, fibres, and dusts. IARC Monogr Eval Carcinog Risks Hum. 2012;100(pt C):11-465.
- Erickson BK, Conner MG, Landen CN Jr. The role of the fallopian tube in the origin of ovarian cancer. Am J Obstet Gynecol. 2013;209:409-414.
- Ness RB, Cottreau C. Possible role of ovarian epithelial inflammation in ovarian cancer. J Natl Cancer Inst. 1999;91:1459-1467.
- Terry KL, Karageorgi S, Shvetsov YB, et al; Ovarian Cancer Association Consortium. Genital powder use and risk of ovarian cancer: a pooled analysis of 8,525 cases and 9,859 controls. Cancer Prev Res. 2013;6:811-821.
- Penninkilampi R, Eslick GD. Perineal talc use and ovarian cancer: a systematic review and meta-analysis. Epidemiology. 2018;29:41-49.
- Hsu T. Johnson & Johnson told to pay $4.7 billion in baby powder lawsuit. New York Times. July 12, 2018. Accessed February 18, 2021. https://www.nytimes.com/2018/07/12 /business/johnson-johnson-talcum-powder.html.
- McGinley L. Does talcum powder cause ovarian cancer? Washington Post. August 25, 2017. Accessed February 18, 2021. https://www.washingtonpost.com/news/to-your -health/wp/2017/08/23/does-talcum-powder-cause -ovarian-cancer-experts-are-divided/.
- O’Brien KM, Tworoger SS, Harris HR, et al. Association of powder use in the genital area with risk of ovarian cancer. JAMA. 2020;323:49-59.
- de Sanjose S, Quint WG, Alemany L, et al; Retrospective International Survey and HPV Time Trends Study Group. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11:1048-1056.
- Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12-19.
- Ault KA; Future II Study Group. Effect of prophylactic human papillomavirus L1 virus-like-particle vaccine on risk of cervical intraepithelial neoplasia grade 2, grade 3, and adenocarcinoma in situ: a combined analysis of four randomised clinical trials. Lancet. 2007;369:1861-1868.
- Garland SM, Hernandez-Avila M, Wheeler CM, et al; Females United to Unilaterally Reduce Endo/Ectocervical disease (FUTURE) I Investigators. Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med. 2007;356:1928-1943.
- Joura EA, Leodolter S, Hernandez-Avila M, et al. Efficacy of a quadrivalent prophylactic human papillomavirus (types 6, 11, 16, and 18) L1 virus-like-particle vaccine against highgrade vulval and vaginal lesions: a combined analysis of three randomised clinical trials. Lancet. 2007;369:1693-1702.
- Arbyn M, Xu L, Simoens C, et al. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst Rev. 2018;5(5):CD009069.
- Paavonen J, Naud P, Salmerón J, et al; HPV PATRICIA Study Group. Efficacy of human papillomavirus (HPV)-16/18 AS04- adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet. 2009;374:301-314.
- FUTURE II Study Group. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med. 2007;356:1915-1927.
- Lei J, Ploner A, Elfström KM, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med. 2020;383:1340-1348.
- American Cancer Society. Survival rates for endometrial cancer. https://www.cancer.org/cancer/endometrial-cancer/ detection-diagnosis-staging/survival-rates.html. Accessed February 9, 2021.
- Miller D, Filiaci V, Fleming G, et al. Late-breaking abstract 1: Randomized phase III noninferiority trial of first line chemotherapy for metastatic or recurrent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol. 2012;125:771.
- National Comprehensive Cancer Network. Clinical practice guidelines in oncology: uterine neoplasms. Version 3.2019. https://www.nccn.org/professionals/physician_gls/pdf /uterine.pdf. Accessed February 9, 2021.
- Marcus L, Lemery SJ, Keegan P, et al. FDA approval summary: pembrolizumab for the treatment of microsatellite instabilityhigh solid tumors. Clin Cancer Res. 2019;25:3753-3758.
- Arora E, Masab M, Mittar P, et al. Role of immune checkpoint inhibitors in advanced or recurrent endometrial cancer. Cureus. 2018;10:e2521.
- Keytruda (pembrolizumab). Package insert. Merck Sharp & Dohme; 2018.
- Cancer Genome Atlas Research Network; Kandoth C, Schultz N, Cherniak AD, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67-73.
- Matsui J, Yamamoto Y, Funahashi Y, et al. E7080, a novel inhibitor that targets multiple kinases, has potent antitumor activities against stem cell factor producing human small cell lung cancer H146, based on angiogenesis inhibition. Int J Cancer. 2008;122:664-671.
- Okamoto K, Kodama K, Takase K, et al. Antitumor activities of the targeted multi-tyrosine kinase inhibitor lenvatinib (E7080) against RET gene fusion-driven tumor models. Cancer Lett. 2013;340:97-103.
- Tohyama O, Matsui J, Kodama K, et al. Antitumor activity of lenvatinib (E7080): an angiogenesis inhibitor that targets multiple receptor tyrosine kinases in preclinical human thyroid cancer models. J Thyroid Res. 2014;2014: 638747.
- Vergote I, Teneriello M, Powell MA, et al. A phase II trial of lenvatinib in patients with advanced or recurrent endometrial cancer: angiopoietin-2 as a predictive marker for clinical outcomes. J Clin Oncol. 2013;31(15 suppl): abstract 5520.
- Kimura T, Kato Y, Ozawa Y, et al. Immunomodulatory activity of lenvatinib contributes to antitumor activity in the Hepa1-6 hepatocellular carcinoma model. Cancer Sci. 2018;109:3993-4002.
- Kato Y, Tabata K, Hori Y, et al. Effects of lenvatinib on tumorassociated macrophages enhance antitumor activity of PD-1 signal inhibitors. Mol Cancer Ther. 2015;14(12 suppl 2): abstract A92.
- Kato Y, Bao X, Macgrath S, et al. Lenvatinib mesilate (LEN) enhanced antitumor activity of a PD-1 blockade agent by potentiating Th1 immune response. Ann Oncol. 2016;27(suppl 6): abstract 2PD.
- Makker V, Taylor MH, Aghajanian C, et al. Lenvatinib plus pembrolizumab in patients with advanced endometrial cancer. J Clin Oncol. 2020;38:2981-2992.
- Lenvima (lenvatinib). Package insert. Woodcliff Lake, NJ: Eisai; 2019.
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Carbon black, titanium dioxide, and talc. IARC Monogr Eval Carcinog Risks Hum. 2010;93:1-413.
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Arsenic, metals, fibres, and dusts. IARC Monogr Eval Carcinog Risks Hum. 2012;100(pt C):11-465.
- Erickson BK, Conner MG, Landen CN Jr. The role of the fallopian tube in the origin of ovarian cancer. Am J Obstet Gynecol. 2013;209:409-414.
- Ness RB, Cottreau C. Possible role of ovarian epithelial inflammation in ovarian cancer. J Natl Cancer Inst. 1999;91:1459-1467.
- Terry KL, Karageorgi S, Shvetsov YB, et al; Ovarian Cancer Association Consortium. Genital powder use and risk of ovarian cancer: a pooled analysis of 8,525 cases and 9,859 controls. Cancer Prev Res. 2013;6:811-821.
- Penninkilampi R, Eslick GD. Perineal talc use and ovarian cancer: a systematic review and meta-analysis. Epidemiology. 2018;29:41-49.
- Hsu T. Johnson & Johnson told to pay $4.7 billion in baby powder lawsuit. New York Times. July 12, 2018. Accessed February 18, 2021. https://www.nytimes.com/2018/07/12 /business/johnson-johnson-talcum-powder.html.
- McGinley L. Does talcum powder cause ovarian cancer? Washington Post. August 25, 2017. Accessed February 18, 2021. https://www.washingtonpost.com/news/to-your -health/wp/2017/08/23/does-talcum-powder-cause -ovarian-cancer-experts-are-divided/.
- O’Brien KM, Tworoger SS, Harris HR, et al. Association of powder use in the genital area with risk of ovarian cancer. JAMA. 2020;323:49-59.
Testosterone supplementation in women: When, why, and how
There are no currently US Food and Drug Administration (FDA)-approved therapies for testosterone use in women. Its use by clinicians is through dose modification of FDA-approved therapies for men, or preparations created by compounding pharmacies. Recently, several professional organizations, including the American College of Obstetricians and Gynecologists (ACOG), North American Menopause Society, International Society for the Study of Women’s Sexual Health, and the International Society for Sexual Medicine, convened an expert panel to develop a global position statement on testosterone therapy for women.1 In this roundtable for OBG Management, moderated by Mickey Karram, MD, several experts discuss this position statement as well as the overall clinical advantages and drawbacks of using testosterone in women.
Testosterone indications
Mickey Karram, MD: For which indications do you prescribe testosterone supplementation in women?
Lauren Streicher, MD: I offer systemic testosterone therapy to postmenopausal women who have hypoactive sexual desire disorder (HSDD) and low serum testosterone levels, with one caveat—it is important that the patient’s reported distressing lack of libido is not explained by another condition or circumstance. Many women present reporting low libido but, on further questioning, it is typically revealed that dyspareunia precipitated their loss of interest in sex. It is normal to not want to do something that is painful. In addition, low libido can often be explained by chronic disease, such as diabetes, cancer, or clinical depression.
Some medications, including selective serotonin reuptake inhibitors (SSRIs), frequently cause a decline in sexual interest. Finally, psychosocial and partner issues may be the culprit.
James Simon, MD, CCP, NCMP, IF: Much of the beneficial data for testosterone’s use is for sexual function in postmenopausal women.2 Female sexual dysfunction is highly prevalent among women during the postmenopause.3 Androgen levels progressively decrease throughout adult life in all women, so the postmenopausal additional lack of estrogen has a recognized effect on genitourinary health. There is evidence that the insufficiency of androgens as well as estrogens after menopause can lead to genitourinary symptoms of menopause (GSM).4
Testosterone also is used for increasing strength, lean muscle mass, bone mineral density, and sense of well-being.5
Rebecca Glaser, MD: I consider testosterone supplementation in my clinical practice in both premenopausal and postmenopausal women for symptoms of androgen/hormone deficiency, including diminished sense of well-being; dysphoric mood; anxiety; irritability; fatigue; decreased libido, sexual activity, or pleasure; vasomotor instability; bone loss; decreased muscle strength; insomnia; changes in cognition; memory loss; urinary symptoms; incontinence; vaginal atrophy and dryness; and joint and muscular pain. We also have shown through preliminary and short-term data and case studies that testosterone therapy has a potential beneficial effect on migraine headaches, as well as active breast cancers in both premenopausal and postmenopausal women.6-10
Continue to: What is appropriate bloodwork?...
What is appropriate bloodwork?
Dr. Karram: Do you obtain blood work before initiating testosterone treatment? If so, what tests do you order and what testosterone levels are considered to be normal for premenopausal and postmenopausal women?
Dr. Streicher: Unlike estrogen, which is predictably low in a postmenopausal woman, serum testosterone (T) levels are highly variable because of the adrenal component. Ovarian testosterone production does not cease at the same time as estrogen production. So I do obtain total and free T levels, prior to initiating treatment. Having said that, it has been well established that T levels correlate poorly with level of sexual interest, and there is no specific blood level that can be used to differentiate women with and without sexual dysfunction. We all have patients who have nonexistent T levels and have a very healthy libido, and other women with sky-high levels who have no libido. But it is useful to know levels prior to initiating therapy to be able to monitor levels throughout treatment. Also, if levels are in the premenopausal physiologic range, not only is she unlikely to respond but she is also at risk for developing androgenic adverse effects, such as acne and hair growth. In general, a low free T level (even if it is in the normal postmenopausal range) in a clinical setting of HSDD supports supplementation.
The assessment and interpretation of T levels can be challenging, particularly as the majority of testosterone is protein-bound and biologically inactive. Free T levels (the biologically active testosterone) in many labs are unreliable and need to be calculated.
In addition to total and free T, I check levels of sex hormone-binding globulin (SHBG), the protein that binds testosterone and renders it biologically inactive. If someone has high SHBG levels and is taking an oral estrogen, simply switching to a transdermal estrogen will result in decreased SHBG and increased free T.
Levels of total and free T vary from lab to lab, so it is best to be familiar with those ranges and then be consistent in which lab you choose.
Dr. Glaser: Although I personally do order blood work on most patients (T, free T, estradiol, complete blood count, thyroid-stimulating hormone, and follicle-stimulating hormone), after 15 years of research and publishing data on testosterone implants, I do not believe that T levels are absolutely necessary or even beneficial in most cases. It rarely changes management in my patients.
As Lauren said, it is well known that T levels do not correlate with androgen deficiency symptoms or clinical conditions caused by androgen deficiency. If a patient has symptoms of androgen deficiency, a trial of testosterone therapy should be given.
T levels are not a valid marker of tissue exposure in women, reflecting less than 20% of total androgen activity. The major source of testosterone in pre and postmenopausal women is the local intracrine production of testosterone from the adrenal precursor steroids dehydroepiandrosterone (DHEA) and androstenedione, which would not be reflected in T levels.
In our study involving 300 women, we found no relationship between baseline T levels, presenting symptoms, or response to therapy.6 Premenopausal and postmenopausal women had similar baseline T levels and similar response to therapy. Even women with baseline T levels in the mid-range responded to therapy.
Some of the most controversial topics in treating women with testosterone are related to dosing and T levels throughout therapy. Guideline authors often use the terms ‘physiologic dosing’ and ‘physiologic ranges’ when making recommendations for therapy. Although “physiologic” sounds appropriate/ scientific, these rigid opinions/recommendations are not evidence based. There are no data supporting the use of endogenous T ranges to guide dosing or monitor testosterone therapy.
The decision to initiate testosterone therapy is a clinical decision between the doctor and the patient based on the patient’s symptomatology, which is the therapeutic endpoint. Testosterone therapy must be done with adequate doses determined by clinical effect (benefits) versus side effects or adverse events (risks). T levels may be helpful, along with clinical evaluation when troubleshooting.
Utilizing data from thousands of patients, we have developed serum ranges for testosterone implants.11 Even so, no two patients are the same, nor do they respond to therapy the same. It is always a clinical decision.
Continue to: Dr. Simon...
Dr. Simon: In the recent global consensus statement on testosterone use,1 the experts were in agreement that “no cut-off blood level can be used for any measured circulating androgen to differentiate women with and without sexual dysfunction.” They give their recommendation a C, and I agree that testosterone supplementation, with specific dosage levels, are a clinical decision.
Before initiating testosterone therapy, it is recommended that liver function and fasting lipids are assessed, as liver disease and hyperlipidemia are contraindications to treatment. These levels should be monitored twice in the first year and annually thereafter while the patient is taking testosterone. Breast and pelvic examinations, mammography, and evaluation for abnormal bleeding should be performed as well as the blood tests.12 These recommendations are focused on safety not efficacy.
Administration route
Dr. Karram: How do you administer testosterone, and why?
Dr. Streicher: As there are no FDA approved testosterone products for women, clinicians must determine the dosage and route of delivery based on published clinical trials.
Dr. Glaser: I treat patients with subcutaneous pellet implants. The implants provide consistent and continuous delivery of therapeutic amounts of testosterone. There is a reason testosterone pellets have been used for more than 80 years and are more popular now than ever—they work. The insertion procedure is simple and takes about 2 minutes. The treatment is cost-effective, avoids first pass, has no adverse effect on the liver or clotting factors, and there is no transference. Decades of data support both the efficacy and safety of testosterone implants.6 However, testosterone implants are not regulated by the FDA and all patients are required to sign a consent informing them of off-label use, benefits, and risks of testosterone implant therapy.
Dr. Simon: I think the consent is important, as there is no package labeling to warn of possible side effects.
Dr. Streicher: Oral testosterone therapy, because of its first pass through the liver and association with adverse lipid profiles with negative effects on high- and low-density lipoprotein cholesterol levels, is not recommended. I prefer a transdermal approach. Pellets, implants, and injections have the potential to result in supraphysiologic blood concentrations. It must be emphasized that the goal of treatment is to approximate premenopausal physiologic levels. More is not better; excessive levels do not demonstrate a greater sexual response and are in fact more likely to have a negative impact due to androgenic side effects.
In most clinical trials, a 300 mg/d testosterone patch was effective, but these patches are not commercially available so I rely on transdermal gel from a compounding pharmacy. The typical dose needed to raise levels into the high to normal range for most women is 2.5 mg up to 5 mg per day of testosterone 1%, which translates to roughly 1 mL. Many pharmacies provide a dispenser, which allots the appropriate dose. Alternatively, I instruct the patient to place a dollop on her thigh (roughly in size of a single M&M candy).
I always tell my patients that the response is not immediate, typically taking 8 to 12 weeks for the effect to become clinically significant. I generally see a patient back 8 weeks after initiation of treatment to check T levels and evaluate response.
Dr. Simon: There are some data demonstrating that intravaginal testosterone can be a potential treatment for GSM. Intravaginal testosterone coupled with aromatase inhibitor therapy used for breast cancer treatment resulted in supraphysiologic T levels and reportedly improved vaginal maturation index and reduced dyspareunia. More study is needed.13
Dr. Streicher: Agreed. The lower third of the vagina and the vestibule is rich in testosterone receptors. Like Dr. Simon, in some cases of vaginal atrophy I prescribe a compounded local vaginal testosterone.
Continue to: Testosterone and premenopausal women...
Testosterone and premenopausal women
Dr. Karram: Is there a role for testosterone supplementation in premenopausal women with normal estrogen production?
Dr. Glaser: Yes. In fact, in our study, more than one-third of the patients were premenopausal, which makes sense.6 There is a marked decline of T levels and the adrenal precursor steroids (DHEA and androstenedione) in women between the ages of 20–30 years and around age 50. As we said, symptoms of androgen deficiency often occur prior to menopause and are not related to estrogen levels. In our study, testosterone implant therapy relieved symptoms of hormone (androgen) deficiency, including vasomotor symptoms, sleep problems, depressive mood, irritability, anxiety, physical and mental exhaustion (fatigue, memory issues), sexual problems, bladder problems (incontinence, frequency), vaginal dryness, and joint and muscular pain. Premenopausal and postmenopausal patients reported similar hormone deficiency symptoms. Premenopausal women did report a higher incidence of psychological complaints (depressive mood, anxiety, and irritability), while postmenopausal women reported more hot flashes, vaginal dryness, and urologic symptoms. Both groups demonstrated similar improvement in symptoms.
In addition, we have seen relief of severe migraine headache in premenopausal (as well as postmenopausal) women treated with testosterone implant therapy.6,7
Dr. Streicher: The goal of testosterone supplementation is to approximate physiological testosterone concentrations for premenopausal women. While testosterone may improve well-being and sexual function in premenopausal women, the data are limited and really inconclusive. More study is needed given that there is likely a wide therapeutic range with many variables. Having said that, there are some data that indicate that testosterone in premenopausal women may enhance general sense of well-being.14
Why is there no FDA-approved agent?
Dr. Karram: Why do you think the FDA has been reluctant to approve a testosterone agent for women?
Dr. Simon: Three potential testosterone drugs for use in women have been unsuccessfully brought to market after the FDA did not approve them. There are 31 approved products for men, each of which were approved because they safely restored normal testosterone concentrations in men with reduced levels and an associated medical condition. Unlike this scenario for men, for women, the FDA has required products to show clinical effectiveness in trials. For instance, Estratest, a combination estrogen-testosterone product, was in use in the 1960s—approved for women with estrogen-resistant hot flushes, and used in practice for sexual dysfunction. After the FDA implemented its Drug Efficacy Study and Implementation regulation system after 2000, which required safety and efficacy trial(s) before drug approval, the manufacturer removed the drug from market when presented efficacy study data for the added testosterone in the drug were deemed inadequate.15
Dr. Streicher: We have yet another example of the disparity between the FDA approval processes for sexual function drugs for men versus women. Take Intrinsia as another example. It was a 300-mg testosterone patch that underwent clinical trials in women who were post-oophorectomy with HSDD. The patch had demonstrated efficacy with minimal adverse effects and no statistically significant dangerous effects. However, the FDA declined approval, citing “safety considerations” and requested longer-term clinical trials to evaluate potential cardiovascular or breast problems. Given that Intrinsia supplementation simply restored normal physiologic testosterone levels, and there was no such requirement in men who received supplementation post-orchiectomy, this requirement was nonsensical and unjustified.
Compounded formulations
Dr. Karram: Are compounding pharmacies appropriately regulated, and how can you be assured that the source of your testosterone is appropriate?
Dr. Glaser: Compounding pharmacies are regulated by the State Boards of Pharmacy, Drug Enforcement Agency, Occupational Safety and Health Administration, National Institute for Occupational Safety and Health, State Bureaus of Narcotics and Dangerous Drugs, and Departments of Health (in some states).
Compounding is a highly regulated profession that is constantly under scrutiny by agencies, patients, and physicians. Any additional regulations could adversely impact the accessibility of patients to individually compounded medications including intravenous and oncology medications. Over the past 20 years, I have treated hundreds of patients with breast cancer with compounded vaginal testosterone (with or without estriol) and subcutaneous testosterone (with or without anastrozole), greatly improving quality of life in women suffering from severe symptoms. Without the availability of compounded medications, there would have been no or limited alternatives for adequate and much needed therapy. Notably, there have been no adverse events or safety-related issues in more than 20 years.
Regarding whether or not “the source of your testosterone is appropriate,” pharmacists can only use United States Pharmacopeia (USP) grades of testosterone. Testosterone used in compounding is required by the FDA to be of USP grade from an FDA registered and compliant facility. In addition, compounding support companies run additional USP tests to confirm their products meet USP standards prior to being delivered to individual compounding pharmacies.
Dr. Streicher: However, there potentially can be substantial variability between formulations and batches. Product purity can also be an issue. It is reassuring if the compounding pharmacy is compliant with purity of Active Pharmaceutical Ingredients and Good Manufacturing Practice rules and guidelines that assure the minimum requirements to assure high quality and batch-to-batch consistency. I find it helpful to always work with the same pharmacy once you have established uniformity and reliability. If there is concern, it is appropriate to check a patient’s serum level 2 weeks after initiation of therapy.
Dr. Simon: I think the problem with some compounding pharmacies is that there may be incentives back and forth with the clinician to use a certain outlet, whereby the patient’s best interest may not be served. I do believe that there is a role for compounding pharmacies, however. We also use them because some women may have strange reactions or be allergic to the preservatives, formulating agents, or even lactose, in various pills and patches, gels, and creams.
Continue to: Testosterone for aging and cognition?...
Testosterone for aging and cognition?
Dr. Karram: Do you think that testosterone supplementation in the elderly can have a positive impact on aging, Alzheimer disease, and dementia?
Dr. Streicher: The jury is still out on the cognitive effects of postmenopausal androgen supplementation. There is currently insufficient evidence to support the use of testosterone to enhance cognitive performance, or to delay cognitive decline. I prescribe testosterone only to treat HSDD, but I do tell my patient that she may possibly also benefit in terms of cognitive function, musculoskeletal parameters, and well-being. Large RCTs are needed in those areas to justify prescribing for those benefits alone.
Dr. Simon: I would say this is the place for future development, but where there is very likely to be a benefit is on sarcopenia.
Dr. Glaser: There is some evidence that testosterone is neuroprotective.16 In my clinical practice I have seen “self-reported” memory issues improved on therapy, often returning toward the end of the testosterone implant cycle. Adequate amounts of bioavailable testosterone at the androgen receptor are critical for optimal health, immune function, and disease prevention.
Dr. Karram: In conclusion, this expert panel agrees that testosterone supplementation is beneficial for sexual dysfunction in postmenopausal women, with also many other potential benefits that require further investigation. Route of administration preferred by Dr. Simon and Dr. Streicher is transdermal or a transvaginal cream. Dr. Glaser uses a subcutaneous pellet approach. Thank you all for an engaging and informative discussion. ●
Dr. Karram: How would you treat the following patient? She is 56, postmenopausal, and taking estrogen. She reports decreased libido, fatigue, lack of sleep, and lack of focus. Would you consider testosterone supplementation?
Dr. Simon: For her libido, yes. I would not give it to her for the fatigue if it were simply lack of sleep and without an associated medical condition. For her lack of focus, the testosterone could be beneficial. The central nervous system effects of testosterone are thought to be related to the conversion of testosterone to estrogen in the brain; if a person’s getting enough estrogen, they shouldn’t have lack of focus. Since some women may not want more estrogen, administering a little testosterone for libido also offers focus because it adds to the estrogen in the brain. If after giving her adequate amounts of testosterone her libido is not better in 8 weeks, it wasn’t a testosterone problem. If she does report improvement, however, I would keep her on the agent as long as she is healthy. But most 56-year-old women who already met the criteria for going on estrogen should be fine with testosterone.
If this same patient were not reporting low libido but did report lack of strength, energy, or well-being I also would say, “Sure, give testosterone a try.”
Dr. Glaser: I also would treat her with testosterone—with pellet implants. The dose would depend on her body weight. I usually start with an approximate dose of 1 mg of testosterone per pound of body weight. This amount of testosterone delivered continuously from the implant also supplies estradiol (via aromatization) locally at the cellular level.
I would treat her for as long as she chooses to continue testosterone therapy. There is no end- or stop-date where a person no longer benefits from therapy or adverse events occur. Testosterone does not increase the risk of breast cancer and it has a positive effect on many of the adverse signs and symptoms of aging, including mental and physical deterioration.
- Davis SR, Baber R, Panay N, et al. Global Consensus Position Statement on the Use of Testosterone Therapy for Women. Climacteric. 2019;22:429-434.
- Islam RM, Bell RJ, Green S, et al. Safety and efficacy of testosterone for women: a systematic review and meta-analysis of randomised controlled trial data. Diabetes Endocrinol. 2019;S2213-8587:30189-30195.
- Simon JA, Davis SR, Althof SE, et al. Sexual well-being after menopause: an International Menopause Society White Paper. Climacteric. 2018;21:415-427.
- Traish AM, Vignozzi L, Simon JA, et al. Role of androgens in female genitourinary tissue structure and function: implications in the genitourinary syndrome of menopause. Sex Med Rev. 2018;6:558-571.
- Panay N. British Menopause Society tools for clinicians: testosterone replacement in menopause. Post Reprod Health. 2019;25:40-42.
- Glaser R, York AE, Dimitrakakis C. Beneficial effects of testosterone therapy in women measured by the validated Menopause Rating Scale (MRS). Maturitas. 2011;68:355-361.
- Glaser R, Dimitrakakis C, Trimble N, et al. Testosterone pellet implants and migraine headaches: a pilot study. Maturitas. 2012;71:385-388.
- Glaser RL, York AE, Dimitrakakis C. Efficacy of subcutaneous testosterone on menopausal symptoms in breast cancer survivors. J Clin Oncol. 2014;32(suppl):109-109.
- Glaser RL, Dimitrakakis C. Rapid response of breast cancer to neoadjuvant intramammary testosterone-anastrozole therapy: neoadjuvant hormone therapy in breast cancer. Menopause. 2014;21:673.
- Glaser RL, York AE, Dimitrakakis C. Subcutaneous testosterone-letrozole therapy before and concurrent with neoadjuvant breast chemotherapy: clinical response and therapeutic implications. Menopause. 2017;24:859-864.
- Glaser R, Kalantaridou S, Dimitrakakis C, et al. Testosterone implants in women: pharmacological dosing for a physiologic effect. Maturitas. 2013;74:179-184.
- International Society for the Study of Women’s Sexual Health (ISSWSH) clinical practice guideline for the use of systemic testosterone for hypoactive sexual desire disorder in women. J Sex Med. In press.
- Simon JA, Goldstein I, Kim NN, et al. The role of androgens in the treatment of genitourinary syndrome of menopause (GSM): International Society for the Study of Women’s Sexual Health (ISSWSH) expert consensus panel review. Menopause. 2018;25:837-847.
- Goldstat R, Briganti E, Tran J, et al. Transdermal testosterone therapy improves well-being, mood, and sexual function in premenopausal women. Menopause. 2003;10:390-398.
- Simon JA, Kapner MD. The saga of testosterone for menopausal women at the Food and Drug Administration (FDA). J Sex Med. 2020;17:826-829.
- Davis SR, Wahlin-Jacobsen S. Testosterone in women—the clinical significance. Lancet Diabetes Endocrinol. 2015;3: 980-992.
There are no currently US Food and Drug Administration (FDA)-approved therapies for testosterone use in women. Its use by clinicians is through dose modification of FDA-approved therapies for men, or preparations created by compounding pharmacies. Recently, several professional organizations, including the American College of Obstetricians and Gynecologists (ACOG), North American Menopause Society, International Society for the Study of Women’s Sexual Health, and the International Society for Sexual Medicine, convened an expert panel to develop a global position statement on testosterone therapy for women.1 In this roundtable for OBG Management, moderated by Mickey Karram, MD, several experts discuss this position statement as well as the overall clinical advantages and drawbacks of using testosterone in women.
Testosterone indications
Mickey Karram, MD: For which indications do you prescribe testosterone supplementation in women?
Lauren Streicher, MD: I offer systemic testosterone therapy to postmenopausal women who have hypoactive sexual desire disorder (HSDD) and low serum testosterone levels, with one caveat—it is important that the patient’s reported distressing lack of libido is not explained by another condition or circumstance. Many women present reporting low libido but, on further questioning, it is typically revealed that dyspareunia precipitated their loss of interest in sex. It is normal to not want to do something that is painful. In addition, low libido can often be explained by chronic disease, such as diabetes, cancer, or clinical depression.
Some medications, including selective serotonin reuptake inhibitors (SSRIs), frequently cause a decline in sexual interest. Finally, psychosocial and partner issues may be the culprit.
James Simon, MD, CCP, NCMP, IF: Much of the beneficial data for testosterone’s use is for sexual function in postmenopausal women.2 Female sexual dysfunction is highly prevalent among women during the postmenopause.3 Androgen levels progressively decrease throughout adult life in all women, so the postmenopausal additional lack of estrogen has a recognized effect on genitourinary health. There is evidence that the insufficiency of androgens as well as estrogens after menopause can lead to genitourinary symptoms of menopause (GSM).4
Testosterone also is used for increasing strength, lean muscle mass, bone mineral density, and sense of well-being.5
Rebecca Glaser, MD: I consider testosterone supplementation in my clinical practice in both premenopausal and postmenopausal women for symptoms of androgen/hormone deficiency, including diminished sense of well-being; dysphoric mood; anxiety; irritability; fatigue; decreased libido, sexual activity, or pleasure; vasomotor instability; bone loss; decreased muscle strength; insomnia; changes in cognition; memory loss; urinary symptoms; incontinence; vaginal atrophy and dryness; and joint and muscular pain. We also have shown through preliminary and short-term data and case studies that testosterone therapy has a potential beneficial effect on migraine headaches, as well as active breast cancers in both premenopausal and postmenopausal women.6-10
Continue to: What is appropriate bloodwork?...
What is appropriate bloodwork?
Dr. Karram: Do you obtain blood work before initiating testosterone treatment? If so, what tests do you order and what testosterone levels are considered to be normal for premenopausal and postmenopausal women?
Dr. Streicher: Unlike estrogen, which is predictably low in a postmenopausal woman, serum testosterone (T) levels are highly variable because of the adrenal component. Ovarian testosterone production does not cease at the same time as estrogen production. So I do obtain total and free T levels, prior to initiating treatment. Having said that, it has been well established that T levels correlate poorly with level of sexual interest, and there is no specific blood level that can be used to differentiate women with and without sexual dysfunction. We all have patients who have nonexistent T levels and have a very healthy libido, and other women with sky-high levels who have no libido. But it is useful to know levels prior to initiating therapy to be able to monitor levels throughout treatment. Also, if levels are in the premenopausal physiologic range, not only is she unlikely to respond but she is also at risk for developing androgenic adverse effects, such as acne and hair growth. In general, a low free T level (even if it is in the normal postmenopausal range) in a clinical setting of HSDD supports supplementation.
The assessment and interpretation of T levels can be challenging, particularly as the majority of testosterone is protein-bound and biologically inactive. Free T levels (the biologically active testosterone) in many labs are unreliable and need to be calculated.
In addition to total and free T, I check levels of sex hormone-binding globulin (SHBG), the protein that binds testosterone and renders it biologically inactive. If someone has high SHBG levels and is taking an oral estrogen, simply switching to a transdermal estrogen will result in decreased SHBG and increased free T.
Levels of total and free T vary from lab to lab, so it is best to be familiar with those ranges and then be consistent in which lab you choose.
Dr. Glaser: Although I personally do order blood work on most patients (T, free T, estradiol, complete blood count, thyroid-stimulating hormone, and follicle-stimulating hormone), after 15 years of research and publishing data on testosterone implants, I do not believe that T levels are absolutely necessary or even beneficial in most cases. It rarely changes management in my patients.
As Lauren said, it is well known that T levels do not correlate with androgen deficiency symptoms or clinical conditions caused by androgen deficiency. If a patient has symptoms of androgen deficiency, a trial of testosterone therapy should be given.
T levels are not a valid marker of tissue exposure in women, reflecting less than 20% of total androgen activity. The major source of testosterone in pre and postmenopausal women is the local intracrine production of testosterone from the adrenal precursor steroids dehydroepiandrosterone (DHEA) and androstenedione, which would not be reflected in T levels.
In our study involving 300 women, we found no relationship between baseline T levels, presenting symptoms, or response to therapy.6 Premenopausal and postmenopausal women had similar baseline T levels and similar response to therapy. Even women with baseline T levels in the mid-range responded to therapy.
Some of the most controversial topics in treating women with testosterone are related to dosing and T levels throughout therapy. Guideline authors often use the terms ‘physiologic dosing’ and ‘physiologic ranges’ when making recommendations for therapy. Although “physiologic” sounds appropriate/ scientific, these rigid opinions/recommendations are not evidence based. There are no data supporting the use of endogenous T ranges to guide dosing or monitor testosterone therapy.
The decision to initiate testosterone therapy is a clinical decision between the doctor and the patient based on the patient’s symptomatology, which is the therapeutic endpoint. Testosterone therapy must be done with adequate doses determined by clinical effect (benefits) versus side effects or adverse events (risks). T levels may be helpful, along with clinical evaluation when troubleshooting.
Utilizing data from thousands of patients, we have developed serum ranges for testosterone implants.11 Even so, no two patients are the same, nor do they respond to therapy the same. It is always a clinical decision.
Continue to: Dr. Simon...
Dr. Simon: In the recent global consensus statement on testosterone use,1 the experts were in agreement that “no cut-off blood level can be used for any measured circulating androgen to differentiate women with and without sexual dysfunction.” They give their recommendation a C, and I agree that testosterone supplementation, with specific dosage levels, are a clinical decision.
Before initiating testosterone therapy, it is recommended that liver function and fasting lipids are assessed, as liver disease and hyperlipidemia are contraindications to treatment. These levels should be monitored twice in the first year and annually thereafter while the patient is taking testosterone. Breast and pelvic examinations, mammography, and evaluation for abnormal bleeding should be performed as well as the blood tests.12 These recommendations are focused on safety not efficacy.
Administration route
Dr. Karram: How do you administer testosterone, and why?
Dr. Streicher: As there are no FDA approved testosterone products for women, clinicians must determine the dosage and route of delivery based on published clinical trials.
Dr. Glaser: I treat patients with subcutaneous pellet implants. The implants provide consistent and continuous delivery of therapeutic amounts of testosterone. There is a reason testosterone pellets have been used for more than 80 years and are more popular now than ever—they work. The insertion procedure is simple and takes about 2 minutes. The treatment is cost-effective, avoids first pass, has no adverse effect on the liver or clotting factors, and there is no transference. Decades of data support both the efficacy and safety of testosterone implants.6 However, testosterone implants are not regulated by the FDA and all patients are required to sign a consent informing them of off-label use, benefits, and risks of testosterone implant therapy.
Dr. Simon: I think the consent is important, as there is no package labeling to warn of possible side effects.
Dr. Streicher: Oral testosterone therapy, because of its first pass through the liver and association with adverse lipid profiles with negative effects on high- and low-density lipoprotein cholesterol levels, is not recommended. I prefer a transdermal approach. Pellets, implants, and injections have the potential to result in supraphysiologic blood concentrations. It must be emphasized that the goal of treatment is to approximate premenopausal physiologic levels. More is not better; excessive levels do not demonstrate a greater sexual response and are in fact more likely to have a negative impact due to androgenic side effects.
In most clinical trials, a 300 mg/d testosterone patch was effective, but these patches are not commercially available so I rely on transdermal gel from a compounding pharmacy. The typical dose needed to raise levels into the high to normal range for most women is 2.5 mg up to 5 mg per day of testosterone 1%, which translates to roughly 1 mL. Many pharmacies provide a dispenser, which allots the appropriate dose. Alternatively, I instruct the patient to place a dollop on her thigh (roughly in size of a single M&M candy).
I always tell my patients that the response is not immediate, typically taking 8 to 12 weeks for the effect to become clinically significant. I generally see a patient back 8 weeks after initiation of treatment to check T levels and evaluate response.
Dr. Simon: There are some data demonstrating that intravaginal testosterone can be a potential treatment for GSM. Intravaginal testosterone coupled with aromatase inhibitor therapy used for breast cancer treatment resulted in supraphysiologic T levels and reportedly improved vaginal maturation index and reduced dyspareunia. More study is needed.13
Dr. Streicher: Agreed. The lower third of the vagina and the vestibule is rich in testosterone receptors. Like Dr. Simon, in some cases of vaginal atrophy I prescribe a compounded local vaginal testosterone.
Continue to: Testosterone and premenopausal women...
Testosterone and premenopausal women
Dr. Karram: Is there a role for testosterone supplementation in premenopausal women with normal estrogen production?
Dr. Glaser: Yes. In fact, in our study, more than one-third of the patients were premenopausal, which makes sense.6 There is a marked decline of T levels and the adrenal precursor steroids (DHEA and androstenedione) in women between the ages of 20–30 years and around age 50. As we said, symptoms of androgen deficiency often occur prior to menopause and are not related to estrogen levels. In our study, testosterone implant therapy relieved symptoms of hormone (androgen) deficiency, including vasomotor symptoms, sleep problems, depressive mood, irritability, anxiety, physical and mental exhaustion (fatigue, memory issues), sexual problems, bladder problems (incontinence, frequency), vaginal dryness, and joint and muscular pain. Premenopausal and postmenopausal patients reported similar hormone deficiency symptoms. Premenopausal women did report a higher incidence of psychological complaints (depressive mood, anxiety, and irritability), while postmenopausal women reported more hot flashes, vaginal dryness, and urologic symptoms. Both groups demonstrated similar improvement in symptoms.
In addition, we have seen relief of severe migraine headache in premenopausal (as well as postmenopausal) women treated with testosterone implant therapy.6,7
Dr. Streicher: The goal of testosterone supplementation is to approximate physiological testosterone concentrations for premenopausal women. While testosterone may improve well-being and sexual function in premenopausal women, the data are limited and really inconclusive. More study is needed given that there is likely a wide therapeutic range with many variables. Having said that, there are some data that indicate that testosterone in premenopausal women may enhance general sense of well-being.14
Why is there no FDA-approved agent?
Dr. Karram: Why do you think the FDA has been reluctant to approve a testosterone agent for women?
Dr. Simon: Three potential testosterone drugs for use in women have been unsuccessfully brought to market after the FDA did not approve them. There are 31 approved products for men, each of which were approved because they safely restored normal testosterone concentrations in men with reduced levels and an associated medical condition. Unlike this scenario for men, for women, the FDA has required products to show clinical effectiveness in trials. For instance, Estratest, a combination estrogen-testosterone product, was in use in the 1960s—approved for women with estrogen-resistant hot flushes, and used in practice for sexual dysfunction. After the FDA implemented its Drug Efficacy Study and Implementation regulation system after 2000, which required safety and efficacy trial(s) before drug approval, the manufacturer removed the drug from market when presented efficacy study data for the added testosterone in the drug were deemed inadequate.15
Dr. Streicher: We have yet another example of the disparity between the FDA approval processes for sexual function drugs for men versus women. Take Intrinsia as another example. It was a 300-mg testosterone patch that underwent clinical trials in women who were post-oophorectomy with HSDD. The patch had demonstrated efficacy with minimal adverse effects and no statistically significant dangerous effects. However, the FDA declined approval, citing “safety considerations” and requested longer-term clinical trials to evaluate potential cardiovascular or breast problems. Given that Intrinsia supplementation simply restored normal physiologic testosterone levels, and there was no such requirement in men who received supplementation post-orchiectomy, this requirement was nonsensical and unjustified.
Compounded formulations
Dr. Karram: Are compounding pharmacies appropriately regulated, and how can you be assured that the source of your testosterone is appropriate?
Dr. Glaser: Compounding pharmacies are regulated by the State Boards of Pharmacy, Drug Enforcement Agency, Occupational Safety and Health Administration, National Institute for Occupational Safety and Health, State Bureaus of Narcotics and Dangerous Drugs, and Departments of Health (in some states).
Compounding is a highly regulated profession that is constantly under scrutiny by agencies, patients, and physicians. Any additional regulations could adversely impact the accessibility of patients to individually compounded medications including intravenous and oncology medications. Over the past 20 years, I have treated hundreds of patients with breast cancer with compounded vaginal testosterone (with or without estriol) and subcutaneous testosterone (with or without anastrozole), greatly improving quality of life in women suffering from severe symptoms. Without the availability of compounded medications, there would have been no or limited alternatives for adequate and much needed therapy. Notably, there have been no adverse events or safety-related issues in more than 20 years.
Regarding whether or not “the source of your testosterone is appropriate,” pharmacists can only use United States Pharmacopeia (USP) grades of testosterone. Testosterone used in compounding is required by the FDA to be of USP grade from an FDA registered and compliant facility. In addition, compounding support companies run additional USP tests to confirm their products meet USP standards prior to being delivered to individual compounding pharmacies.
Dr. Streicher: However, there potentially can be substantial variability between formulations and batches. Product purity can also be an issue. It is reassuring if the compounding pharmacy is compliant with purity of Active Pharmaceutical Ingredients and Good Manufacturing Practice rules and guidelines that assure the minimum requirements to assure high quality and batch-to-batch consistency. I find it helpful to always work with the same pharmacy once you have established uniformity and reliability. If there is concern, it is appropriate to check a patient’s serum level 2 weeks after initiation of therapy.
Dr. Simon: I think the problem with some compounding pharmacies is that there may be incentives back and forth with the clinician to use a certain outlet, whereby the patient’s best interest may not be served. I do believe that there is a role for compounding pharmacies, however. We also use them because some women may have strange reactions or be allergic to the preservatives, formulating agents, or even lactose, in various pills and patches, gels, and creams.
Continue to: Testosterone for aging and cognition?...
Testosterone for aging and cognition?
Dr. Karram: Do you think that testosterone supplementation in the elderly can have a positive impact on aging, Alzheimer disease, and dementia?
Dr. Streicher: The jury is still out on the cognitive effects of postmenopausal androgen supplementation. There is currently insufficient evidence to support the use of testosterone to enhance cognitive performance, or to delay cognitive decline. I prescribe testosterone only to treat HSDD, but I do tell my patient that she may possibly also benefit in terms of cognitive function, musculoskeletal parameters, and well-being. Large RCTs are needed in those areas to justify prescribing for those benefits alone.
Dr. Simon: I would say this is the place for future development, but where there is very likely to be a benefit is on sarcopenia.
Dr. Glaser: There is some evidence that testosterone is neuroprotective.16 In my clinical practice I have seen “self-reported” memory issues improved on therapy, often returning toward the end of the testosterone implant cycle. Adequate amounts of bioavailable testosterone at the androgen receptor are critical for optimal health, immune function, and disease prevention.
Dr. Karram: In conclusion, this expert panel agrees that testosterone supplementation is beneficial for sexual dysfunction in postmenopausal women, with also many other potential benefits that require further investigation. Route of administration preferred by Dr. Simon and Dr. Streicher is transdermal or a transvaginal cream. Dr. Glaser uses a subcutaneous pellet approach. Thank you all for an engaging and informative discussion. ●
Dr. Karram: How would you treat the following patient? She is 56, postmenopausal, and taking estrogen. She reports decreased libido, fatigue, lack of sleep, and lack of focus. Would you consider testosterone supplementation?
Dr. Simon: For her libido, yes. I would not give it to her for the fatigue if it were simply lack of sleep and without an associated medical condition. For her lack of focus, the testosterone could be beneficial. The central nervous system effects of testosterone are thought to be related to the conversion of testosterone to estrogen in the brain; if a person’s getting enough estrogen, they shouldn’t have lack of focus. Since some women may not want more estrogen, administering a little testosterone for libido also offers focus because it adds to the estrogen in the brain. If after giving her adequate amounts of testosterone her libido is not better in 8 weeks, it wasn’t a testosterone problem. If she does report improvement, however, I would keep her on the agent as long as she is healthy. But most 56-year-old women who already met the criteria for going on estrogen should be fine with testosterone.
If this same patient were not reporting low libido but did report lack of strength, energy, or well-being I also would say, “Sure, give testosterone a try.”
Dr. Glaser: I also would treat her with testosterone—with pellet implants. The dose would depend on her body weight. I usually start with an approximate dose of 1 mg of testosterone per pound of body weight. This amount of testosterone delivered continuously from the implant also supplies estradiol (via aromatization) locally at the cellular level.
I would treat her for as long as she chooses to continue testosterone therapy. There is no end- or stop-date where a person no longer benefits from therapy or adverse events occur. Testosterone does not increase the risk of breast cancer and it has a positive effect on many of the adverse signs and symptoms of aging, including mental and physical deterioration.
There are no currently US Food and Drug Administration (FDA)-approved therapies for testosterone use in women. Its use by clinicians is through dose modification of FDA-approved therapies for men, or preparations created by compounding pharmacies. Recently, several professional organizations, including the American College of Obstetricians and Gynecologists (ACOG), North American Menopause Society, International Society for the Study of Women’s Sexual Health, and the International Society for Sexual Medicine, convened an expert panel to develop a global position statement on testosterone therapy for women.1 In this roundtable for OBG Management, moderated by Mickey Karram, MD, several experts discuss this position statement as well as the overall clinical advantages and drawbacks of using testosterone in women.
Testosterone indications
Mickey Karram, MD: For which indications do you prescribe testosterone supplementation in women?
Lauren Streicher, MD: I offer systemic testosterone therapy to postmenopausal women who have hypoactive sexual desire disorder (HSDD) and low serum testosterone levels, with one caveat—it is important that the patient’s reported distressing lack of libido is not explained by another condition or circumstance. Many women present reporting low libido but, on further questioning, it is typically revealed that dyspareunia precipitated their loss of interest in sex. It is normal to not want to do something that is painful. In addition, low libido can often be explained by chronic disease, such as diabetes, cancer, or clinical depression.
Some medications, including selective serotonin reuptake inhibitors (SSRIs), frequently cause a decline in sexual interest. Finally, psychosocial and partner issues may be the culprit.
James Simon, MD, CCP, NCMP, IF: Much of the beneficial data for testosterone’s use is for sexual function in postmenopausal women.2 Female sexual dysfunction is highly prevalent among women during the postmenopause.3 Androgen levels progressively decrease throughout adult life in all women, so the postmenopausal additional lack of estrogen has a recognized effect on genitourinary health. There is evidence that the insufficiency of androgens as well as estrogens after menopause can lead to genitourinary symptoms of menopause (GSM).4
Testosterone also is used for increasing strength, lean muscle mass, bone mineral density, and sense of well-being.5
Rebecca Glaser, MD: I consider testosterone supplementation in my clinical practice in both premenopausal and postmenopausal women for symptoms of androgen/hormone deficiency, including diminished sense of well-being; dysphoric mood; anxiety; irritability; fatigue; decreased libido, sexual activity, or pleasure; vasomotor instability; bone loss; decreased muscle strength; insomnia; changes in cognition; memory loss; urinary symptoms; incontinence; vaginal atrophy and dryness; and joint and muscular pain. We also have shown through preliminary and short-term data and case studies that testosterone therapy has a potential beneficial effect on migraine headaches, as well as active breast cancers in both premenopausal and postmenopausal women.6-10
Continue to: What is appropriate bloodwork?...
What is appropriate bloodwork?
Dr. Karram: Do you obtain blood work before initiating testosterone treatment? If so, what tests do you order and what testosterone levels are considered to be normal for premenopausal and postmenopausal women?
Dr. Streicher: Unlike estrogen, which is predictably low in a postmenopausal woman, serum testosterone (T) levels are highly variable because of the adrenal component. Ovarian testosterone production does not cease at the same time as estrogen production. So I do obtain total and free T levels, prior to initiating treatment. Having said that, it has been well established that T levels correlate poorly with level of sexual interest, and there is no specific blood level that can be used to differentiate women with and without sexual dysfunction. We all have patients who have nonexistent T levels and have a very healthy libido, and other women with sky-high levels who have no libido. But it is useful to know levels prior to initiating therapy to be able to monitor levels throughout treatment. Also, if levels are in the premenopausal physiologic range, not only is she unlikely to respond but she is also at risk for developing androgenic adverse effects, such as acne and hair growth. In general, a low free T level (even if it is in the normal postmenopausal range) in a clinical setting of HSDD supports supplementation.
The assessment and interpretation of T levels can be challenging, particularly as the majority of testosterone is protein-bound and biologically inactive. Free T levels (the biologically active testosterone) in many labs are unreliable and need to be calculated.
In addition to total and free T, I check levels of sex hormone-binding globulin (SHBG), the protein that binds testosterone and renders it biologically inactive. If someone has high SHBG levels and is taking an oral estrogen, simply switching to a transdermal estrogen will result in decreased SHBG and increased free T.
Levels of total and free T vary from lab to lab, so it is best to be familiar with those ranges and then be consistent in which lab you choose.
Dr. Glaser: Although I personally do order blood work on most patients (T, free T, estradiol, complete blood count, thyroid-stimulating hormone, and follicle-stimulating hormone), after 15 years of research and publishing data on testosterone implants, I do not believe that T levels are absolutely necessary or even beneficial in most cases. It rarely changes management in my patients.
As Lauren said, it is well known that T levels do not correlate with androgen deficiency symptoms or clinical conditions caused by androgen deficiency. If a patient has symptoms of androgen deficiency, a trial of testosterone therapy should be given.
T levels are not a valid marker of tissue exposure in women, reflecting less than 20% of total androgen activity. The major source of testosterone in pre and postmenopausal women is the local intracrine production of testosterone from the adrenal precursor steroids dehydroepiandrosterone (DHEA) and androstenedione, which would not be reflected in T levels.
In our study involving 300 women, we found no relationship between baseline T levels, presenting symptoms, or response to therapy.6 Premenopausal and postmenopausal women had similar baseline T levels and similar response to therapy. Even women with baseline T levels in the mid-range responded to therapy.
Some of the most controversial topics in treating women with testosterone are related to dosing and T levels throughout therapy. Guideline authors often use the terms ‘physiologic dosing’ and ‘physiologic ranges’ when making recommendations for therapy. Although “physiologic” sounds appropriate/ scientific, these rigid opinions/recommendations are not evidence based. There are no data supporting the use of endogenous T ranges to guide dosing or monitor testosterone therapy.
The decision to initiate testosterone therapy is a clinical decision between the doctor and the patient based on the patient’s symptomatology, which is the therapeutic endpoint. Testosterone therapy must be done with adequate doses determined by clinical effect (benefits) versus side effects or adverse events (risks). T levels may be helpful, along with clinical evaluation when troubleshooting.
Utilizing data from thousands of patients, we have developed serum ranges for testosterone implants.11 Even so, no two patients are the same, nor do they respond to therapy the same. It is always a clinical decision.
Continue to: Dr. Simon...
Dr. Simon: In the recent global consensus statement on testosterone use,1 the experts were in agreement that “no cut-off blood level can be used for any measured circulating androgen to differentiate women with and without sexual dysfunction.” They give their recommendation a C, and I agree that testosterone supplementation, with specific dosage levels, are a clinical decision.
Before initiating testosterone therapy, it is recommended that liver function and fasting lipids are assessed, as liver disease and hyperlipidemia are contraindications to treatment. These levels should be monitored twice in the first year and annually thereafter while the patient is taking testosterone. Breast and pelvic examinations, mammography, and evaluation for abnormal bleeding should be performed as well as the blood tests.12 These recommendations are focused on safety not efficacy.
Administration route
Dr. Karram: How do you administer testosterone, and why?
Dr. Streicher: As there are no FDA approved testosterone products for women, clinicians must determine the dosage and route of delivery based on published clinical trials.
Dr. Glaser: I treat patients with subcutaneous pellet implants. The implants provide consistent and continuous delivery of therapeutic amounts of testosterone. There is a reason testosterone pellets have been used for more than 80 years and are more popular now than ever—they work. The insertion procedure is simple and takes about 2 minutes. The treatment is cost-effective, avoids first pass, has no adverse effect on the liver or clotting factors, and there is no transference. Decades of data support both the efficacy and safety of testosterone implants.6 However, testosterone implants are not regulated by the FDA and all patients are required to sign a consent informing them of off-label use, benefits, and risks of testosterone implant therapy.
Dr. Simon: I think the consent is important, as there is no package labeling to warn of possible side effects.
Dr. Streicher: Oral testosterone therapy, because of its first pass through the liver and association with adverse lipid profiles with negative effects on high- and low-density lipoprotein cholesterol levels, is not recommended. I prefer a transdermal approach. Pellets, implants, and injections have the potential to result in supraphysiologic blood concentrations. It must be emphasized that the goal of treatment is to approximate premenopausal physiologic levels. More is not better; excessive levels do not demonstrate a greater sexual response and are in fact more likely to have a negative impact due to androgenic side effects.
In most clinical trials, a 300 mg/d testosterone patch was effective, but these patches are not commercially available so I rely on transdermal gel from a compounding pharmacy. The typical dose needed to raise levels into the high to normal range for most women is 2.5 mg up to 5 mg per day of testosterone 1%, which translates to roughly 1 mL. Many pharmacies provide a dispenser, which allots the appropriate dose. Alternatively, I instruct the patient to place a dollop on her thigh (roughly in size of a single M&M candy).
I always tell my patients that the response is not immediate, typically taking 8 to 12 weeks for the effect to become clinically significant. I generally see a patient back 8 weeks after initiation of treatment to check T levels and evaluate response.
Dr. Simon: There are some data demonstrating that intravaginal testosterone can be a potential treatment for GSM. Intravaginal testosterone coupled with aromatase inhibitor therapy used for breast cancer treatment resulted in supraphysiologic T levels and reportedly improved vaginal maturation index and reduced dyspareunia. More study is needed.13
Dr. Streicher: Agreed. The lower third of the vagina and the vestibule is rich in testosterone receptors. Like Dr. Simon, in some cases of vaginal atrophy I prescribe a compounded local vaginal testosterone.
Continue to: Testosterone and premenopausal women...
Testosterone and premenopausal women
Dr. Karram: Is there a role for testosterone supplementation in premenopausal women with normal estrogen production?
Dr. Glaser: Yes. In fact, in our study, more than one-third of the patients were premenopausal, which makes sense.6 There is a marked decline of T levels and the adrenal precursor steroids (DHEA and androstenedione) in women between the ages of 20–30 years and around age 50. As we said, symptoms of androgen deficiency often occur prior to menopause and are not related to estrogen levels. In our study, testosterone implant therapy relieved symptoms of hormone (androgen) deficiency, including vasomotor symptoms, sleep problems, depressive mood, irritability, anxiety, physical and mental exhaustion (fatigue, memory issues), sexual problems, bladder problems (incontinence, frequency), vaginal dryness, and joint and muscular pain. Premenopausal and postmenopausal patients reported similar hormone deficiency symptoms. Premenopausal women did report a higher incidence of psychological complaints (depressive mood, anxiety, and irritability), while postmenopausal women reported more hot flashes, vaginal dryness, and urologic symptoms. Both groups demonstrated similar improvement in symptoms.
In addition, we have seen relief of severe migraine headache in premenopausal (as well as postmenopausal) women treated with testosterone implant therapy.6,7
Dr. Streicher: The goal of testosterone supplementation is to approximate physiological testosterone concentrations for premenopausal women. While testosterone may improve well-being and sexual function in premenopausal women, the data are limited and really inconclusive. More study is needed given that there is likely a wide therapeutic range with many variables. Having said that, there are some data that indicate that testosterone in premenopausal women may enhance general sense of well-being.14
Why is there no FDA-approved agent?
Dr. Karram: Why do you think the FDA has been reluctant to approve a testosterone agent for women?
Dr. Simon: Three potential testosterone drugs for use in women have been unsuccessfully brought to market after the FDA did not approve them. There are 31 approved products for men, each of which were approved because they safely restored normal testosterone concentrations in men with reduced levels and an associated medical condition. Unlike this scenario for men, for women, the FDA has required products to show clinical effectiveness in trials. For instance, Estratest, a combination estrogen-testosterone product, was in use in the 1960s—approved for women with estrogen-resistant hot flushes, and used in practice for sexual dysfunction. After the FDA implemented its Drug Efficacy Study and Implementation regulation system after 2000, which required safety and efficacy trial(s) before drug approval, the manufacturer removed the drug from market when presented efficacy study data for the added testosterone in the drug were deemed inadequate.15
Dr. Streicher: We have yet another example of the disparity between the FDA approval processes for sexual function drugs for men versus women. Take Intrinsia as another example. It was a 300-mg testosterone patch that underwent clinical trials in women who were post-oophorectomy with HSDD. The patch had demonstrated efficacy with minimal adverse effects and no statistically significant dangerous effects. However, the FDA declined approval, citing “safety considerations” and requested longer-term clinical trials to evaluate potential cardiovascular or breast problems. Given that Intrinsia supplementation simply restored normal physiologic testosterone levels, and there was no such requirement in men who received supplementation post-orchiectomy, this requirement was nonsensical and unjustified.
Compounded formulations
Dr. Karram: Are compounding pharmacies appropriately regulated, and how can you be assured that the source of your testosterone is appropriate?
Dr. Glaser: Compounding pharmacies are regulated by the State Boards of Pharmacy, Drug Enforcement Agency, Occupational Safety and Health Administration, National Institute for Occupational Safety and Health, State Bureaus of Narcotics and Dangerous Drugs, and Departments of Health (in some states).
Compounding is a highly regulated profession that is constantly under scrutiny by agencies, patients, and physicians. Any additional regulations could adversely impact the accessibility of patients to individually compounded medications including intravenous and oncology medications. Over the past 20 years, I have treated hundreds of patients with breast cancer with compounded vaginal testosterone (with or without estriol) and subcutaneous testosterone (with or without anastrozole), greatly improving quality of life in women suffering from severe symptoms. Without the availability of compounded medications, there would have been no or limited alternatives for adequate and much needed therapy. Notably, there have been no adverse events or safety-related issues in more than 20 years.
Regarding whether or not “the source of your testosterone is appropriate,” pharmacists can only use United States Pharmacopeia (USP) grades of testosterone. Testosterone used in compounding is required by the FDA to be of USP grade from an FDA registered and compliant facility. In addition, compounding support companies run additional USP tests to confirm their products meet USP standards prior to being delivered to individual compounding pharmacies.
Dr. Streicher: However, there potentially can be substantial variability between formulations and batches. Product purity can also be an issue. It is reassuring if the compounding pharmacy is compliant with purity of Active Pharmaceutical Ingredients and Good Manufacturing Practice rules and guidelines that assure the minimum requirements to assure high quality and batch-to-batch consistency. I find it helpful to always work with the same pharmacy once you have established uniformity and reliability. If there is concern, it is appropriate to check a patient’s serum level 2 weeks after initiation of therapy.
Dr. Simon: I think the problem with some compounding pharmacies is that there may be incentives back and forth with the clinician to use a certain outlet, whereby the patient’s best interest may not be served. I do believe that there is a role for compounding pharmacies, however. We also use them because some women may have strange reactions or be allergic to the preservatives, formulating agents, or even lactose, in various pills and patches, gels, and creams.
Continue to: Testosterone for aging and cognition?...
Testosterone for aging and cognition?
Dr. Karram: Do you think that testosterone supplementation in the elderly can have a positive impact on aging, Alzheimer disease, and dementia?
Dr. Streicher: The jury is still out on the cognitive effects of postmenopausal androgen supplementation. There is currently insufficient evidence to support the use of testosterone to enhance cognitive performance, or to delay cognitive decline. I prescribe testosterone only to treat HSDD, but I do tell my patient that she may possibly also benefit in terms of cognitive function, musculoskeletal parameters, and well-being. Large RCTs are needed in those areas to justify prescribing for those benefits alone.
Dr. Simon: I would say this is the place for future development, but where there is very likely to be a benefit is on sarcopenia.
Dr. Glaser: There is some evidence that testosterone is neuroprotective.16 In my clinical practice I have seen “self-reported” memory issues improved on therapy, often returning toward the end of the testosterone implant cycle. Adequate amounts of bioavailable testosterone at the androgen receptor are critical for optimal health, immune function, and disease prevention.
Dr. Karram: In conclusion, this expert panel agrees that testosterone supplementation is beneficial for sexual dysfunction in postmenopausal women, with also many other potential benefits that require further investigation. Route of administration preferred by Dr. Simon and Dr. Streicher is transdermal or a transvaginal cream. Dr. Glaser uses a subcutaneous pellet approach. Thank you all for an engaging and informative discussion. ●
Dr. Karram: How would you treat the following patient? She is 56, postmenopausal, and taking estrogen. She reports decreased libido, fatigue, lack of sleep, and lack of focus. Would you consider testosterone supplementation?
Dr. Simon: For her libido, yes. I would not give it to her for the fatigue if it were simply lack of sleep and without an associated medical condition. For her lack of focus, the testosterone could be beneficial. The central nervous system effects of testosterone are thought to be related to the conversion of testosterone to estrogen in the brain; if a person’s getting enough estrogen, they shouldn’t have lack of focus. Since some women may not want more estrogen, administering a little testosterone for libido also offers focus because it adds to the estrogen in the brain. If after giving her adequate amounts of testosterone her libido is not better in 8 weeks, it wasn’t a testosterone problem. If she does report improvement, however, I would keep her on the agent as long as she is healthy. But most 56-year-old women who already met the criteria for going on estrogen should be fine with testosterone.
If this same patient were not reporting low libido but did report lack of strength, energy, or well-being I also would say, “Sure, give testosterone a try.”
Dr. Glaser: I also would treat her with testosterone—with pellet implants. The dose would depend on her body weight. I usually start with an approximate dose of 1 mg of testosterone per pound of body weight. This amount of testosterone delivered continuously from the implant also supplies estradiol (via aromatization) locally at the cellular level.
I would treat her for as long as she chooses to continue testosterone therapy. There is no end- or stop-date where a person no longer benefits from therapy or adverse events occur. Testosterone does not increase the risk of breast cancer and it has a positive effect on many of the adverse signs and symptoms of aging, including mental and physical deterioration.
- Davis SR, Baber R, Panay N, et al. Global Consensus Position Statement on the Use of Testosterone Therapy for Women. Climacteric. 2019;22:429-434.
- Islam RM, Bell RJ, Green S, et al. Safety and efficacy of testosterone for women: a systematic review and meta-analysis of randomised controlled trial data. Diabetes Endocrinol. 2019;S2213-8587:30189-30195.
- Simon JA, Davis SR, Althof SE, et al. Sexual well-being after menopause: an International Menopause Society White Paper. Climacteric. 2018;21:415-427.
- Traish AM, Vignozzi L, Simon JA, et al. Role of androgens in female genitourinary tissue structure and function: implications in the genitourinary syndrome of menopause. Sex Med Rev. 2018;6:558-571.
- Panay N. British Menopause Society tools for clinicians: testosterone replacement in menopause. Post Reprod Health. 2019;25:40-42.
- Glaser R, York AE, Dimitrakakis C. Beneficial effects of testosterone therapy in women measured by the validated Menopause Rating Scale (MRS). Maturitas. 2011;68:355-361.
- Glaser R, Dimitrakakis C, Trimble N, et al. Testosterone pellet implants and migraine headaches: a pilot study. Maturitas. 2012;71:385-388.
- Glaser RL, York AE, Dimitrakakis C. Efficacy of subcutaneous testosterone on menopausal symptoms in breast cancer survivors. J Clin Oncol. 2014;32(suppl):109-109.
- Glaser RL, Dimitrakakis C. Rapid response of breast cancer to neoadjuvant intramammary testosterone-anastrozole therapy: neoadjuvant hormone therapy in breast cancer. Menopause. 2014;21:673.
- Glaser RL, York AE, Dimitrakakis C. Subcutaneous testosterone-letrozole therapy before and concurrent with neoadjuvant breast chemotherapy: clinical response and therapeutic implications. Menopause. 2017;24:859-864.
- Glaser R, Kalantaridou S, Dimitrakakis C, et al. Testosterone implants in women: pharmacological dosing for a physiologic effect. Maturitas. 2013;74:179-184.
- International Society for the Study of Women’s Sexual Health (ISSWSH) clinical practice guideline for the use of systemic testosterone for hypoactive sexual desire disorder in women. J Sex Med. In press.
- Simon JA, Goldstein I, Kim NN, et al. The role of androgens in the treatment of genitourinary syndrome of menopause (GSM): International Society for the Study of Women’s Sexual Health (ISSWSH) expert consensus panel review. Menopause. 2018;25:837-847.
- Goldstat R, Briganti E, Tran J, et al. Transdermal testosterone therapy improves well-being, mood, and sexual function in premenopausal women. Menopause. 2003;10:390-398.
- Simon JA, Kapner MD. The saga of testosterone for menopausal women at the Food and Drug Administration (FDA). J Sex Med. 2020;17:826-829.
- Davis SR, Wahlin-Jacobsen S. Testosterone in women—the clinical significance. Lancet Diabetes Endocrinol. 2015;3: 980-992.
- Davis SR, Baber R, Panay N, et al. Global Consensus Position Statement on the Use of Testosterone Therapy for Women. Climacteric. 2019;22:429-434.
- Islam RM, Bell RJ, Green S, et al. Safety and efficacy of testosterone for women: a systematic review and meta-analysis of randomised controlled trial data. Diabetes Endocrinol. 2019;S2213-8587:30189-30195.
- Simon JA, Davis SR, Althof SE, et al. Sexual well-being after menopause: an International Menopause Society White Paper. Climacteric. 2018;21:415-427.
- Traish AM, Vignozzi L, Simon JA, et al. Role of androgens in female genitourinary tissue structure and function: implications in the genitourinary syndrome of menopause. Sex Med Rev. 2018;6:558-571.
- Panay N. British Menopause Society tools for clinicians: testosterone replacement in menopause. Post Reprod Health. 2019;25:40-42.
- Glaser R, York AE, Dimitrakakis C. Beneficial effects of testosterone therapy in women measured by the validated Menopause Rating Scale (MRS). Maturitas. 2011;68:355-361.
- Glaser R, Dimitrakakis C, Trimble N, et al. Testosterone pellet implants and migraine headaches: a pilot study. Maturitas. 2012;71:385-388.
- Glaser RL, York AE, Dimitrakakis C. Efficacy of subcutaneous testosterone on menopausal symptoms in breast cancer survivors. J Clin Oncol. 2014;32(suppl):109-109.
- Glaser RL, Dimitrakakis C. Rapid response of breast cancer to neoadjuvant intramammary testosterone-anastrozole therapy: neoadjuvant hormone therapy in breast cancer. Menopause. 2014;21:673.
- Glaser RL, York AE, Dimitrakakis C. Subcutaneous testosterone-letrozole therapy before and concurrent with neoadjuvant breast chemotherapy: clinical response and therapeutic implications. Menopause. 2017;24:859-864.
- Glaser R, Kalantaridou S, Dimitrakakis C, et al. Testosterone implants in women: pharmacological dosing for a physiologic effect. Maturitas. 2013;74:179-184.
- International Society for the Study of Women’s Sexual Health (ISSWSH) clinical practice guideline for the use of systemic testosterone for hypoactive sexual desire disorder in women. J Sex Med. In press.
- Simon JA, Goldstein I, Kim NN, et al. The role of androgens in the treatment of genitourinary syndrome of menopause (GSM): International Society for the Study of Women’s Sexual Health (ISSWSH) expert consensus panel review. Menopause. 2018;25:837-847.
- Goldstat R, Briganti E, Tran J, et al. Transdermal testosterone therapy improves well-being, mood, and sexual function in premenopausal women. Menopause. 2003;10:390-398.
- Simon JA, Kapner MD. The saga of testosterone for menopausal women at the Food and Drug Administration (FDA). J Sex Med. 2020;17:826-829.
- Davis SR, Wahlin-Jacobsen S. Testosterone in women—the clinical significance. Lancet Diabetes Endocrinol. 2015;3: 980-992.
Caring for women with pelvic floor disorders during pregnancy and postpartum: Expert guidance
Pelvic floor disorders (PFDs) affect many pregnant and newly postpartum women. These conditions, including urinary incontinence, anal incontinence, and pelvic organ prolapse (POP), can be overshadowed by common pregnancy and postpartum concerns (TABLE 1).1 With the use of a few quick screening questions, however, PFDs easily can be identified in this at-risk population. Active management need not be delayed until after delivery for women experiencing bother, as options exist for women with PFDs during pregnancy as well as postpartum.
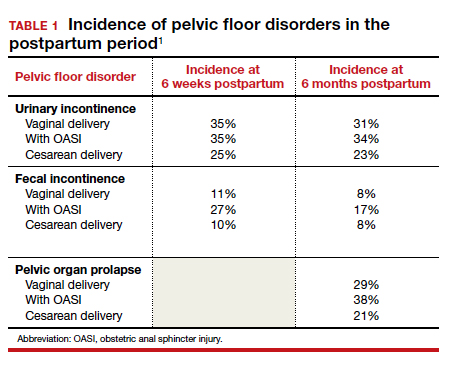
In this article, we discuss the common PFDs that obstetric clinicians face in the context of case scenarios and review how you can be better equipped to care for affected individuals.
CASE 1 Screening
A 30-year-old woman (G1P1) presents for her routine postpartum visit after an operative vaginal delivery with a second-degree laceration.
How would you screen this patient for PFDs?
Why screening for PFDs matters
While there are no validated PFD screening tools for this patient population, clinicians can ask a series of brief open-ended questions as part of the review of systems to efficiently evaluate for the common PFDs in peripartum patients (see “Screening questions to evaluate patients for peripartum pelvic floor disorders” below).
Pelvic floor disorders in the peripartum period can have a significant negative impact. In pregnancy, nearly half of women report psychological strain due to the presence of bowel, bladder, prolapse, or sexual dysfunction symptoms.2 Postpartum, PFDs have negative effects on overall health, well-being, and self-esteem, with significantly increased rates of postpartum depression in women who experience urinary incontinence.3,4 Proactively inquiring about PFD symptoms, providing anticipatory guidance, and recommending treatment options can positively impact a patient in multiple domains.
Sometimes during pregnancy or after having a baby, a woman experiences pelvic floor symptoms. Do you have any of the following?
- leakage with coughing, laughing, sneezing, or physical activity
- urgency to urinate or leakage due to urgency
- bulging or pressure within the vagina
- pain with intercourse
- accidental bowel leakage of stool or flatus
CASE 2 Stress urinary incontinence
A 27-year-old woman (G1P1) presents 2 months following spontaneous vaginal delivery with symptoms of urine leakage with laughing and running. Her urinary incontinence has been improving since delivery, but it continues to be bothersome.
What would you recommend for this patient?
Conservative SUI management strategies in pregnancy
Urinary tract symptoms are common in pregnancy, with up to 41.8% of women reporting urinary symptom distress in the third trimester.5 During pregnancy, estrogen and progesterone decrease urethral pressure that, together with increased intra-abdominal pressure from the gravid uterus, can cause or worsen stress urinary incontinence (SUI).6
During pregnancy, women should be offered conservative therapies for SUI. For women who can perform a pelvic floor contraction (a Kegel exercise), self-guided pelvic floor muscle exercises (PFMEs) may be helpful (see “Pelvic floor muscle exercises” below). We recommend that women start with 1 to 2 sets of 10 Kegel exercises per day and that they hold the squeeze for 2 to 3 seconds, working up to holding for 10 seconds. The goal is to strengthen and improve muscle control so that the Kegel squeeze can be paired with activities that cause SUI.
For women who are unable to perform a Kegel exercise or are not improving with a home PFME regimen, referral to pelvic floor physical therapy (PFPT) can be considered. While data support the efficacy of PFPT for SUI treatment in nonpregnant women,7 data are lacking on PFME in pregnancy.
In women without urinary incontinence, PFME in early pregnancy can prevent the onset of incontinence in late pregnancy and the postpartum period.8 By contrast, the same 2020 Cochrane Review found no evidence that antenatal pelvic floor muscle therapy in incontinent women decreases incontinence in mid- or late-pregnancy or in the postpartum period.8 As the quality of this evidence is very low and there is no evidence of harm with PFME, we continue to recommend it for women with bothersome SUI.
Incontinence pessaries or vaginal inserts (such as Poise Impressa bladder supports) can be helpful for SUI treatment. An incontinence pessary can be fitted in the office, and fitting kits are available for both. Pessaries can safely be used in pregnancy, but there are no data on the efficacy of pessaries for treating SUI in pregnancy. In nonpregnant women, evidence demonstrates 63% satisfaction 3 months post–pessary placement for SUI.7
We do not recommend invasive procedures for the treatment of SUI during pregnancy or in the first 6 months following delivery. There is no evidence that elective cesarean delivery prevents persistent SUI postpartum.9
To identify and engage the proper pelvic floor muscles:
- Insert a finger in the vagina and squeeze the vaginal muscles around your finger.
- Imagine you are sitting on a marble and have to pick it up with the vaginal muscles.
- Squeeze the muscles you would use to stop the flow of urine or hold back flatulence.
Perform sets of 10, 2 to 3 times per day as follows:
- Squeeze: Engage the pelvic floor muscles as described above; avoid performing Kegels while voiding.
- Hold: For 2 to 10 seconds; increase the duration to 10 seconds as able.
- Relax: Completely relax muscles before initating the next squeeze.
Reference
1. UpToDate. Patient education: pelvic muscle (Kegel) exercises (the basics). 2018. https://uptodatefree.ir/topic.htm?path=pelvic-muscle-kegel-exercises-the-basics. Accessed February 24, 2021.
Continue to: Managing SUI in the postpartum period...
Managing SUI in the postpartum period
After the first 6 months postpartum and exhaustion of conservative measures, we offer surgical interventions for women with persistent, bothersome incontinence. Surgery for SUI typically is not recommended until childbearing is complete, but it can be considered if the patient’s bother is significant.
For women with bothersome SUI who still desire future pregnancy, management options include periurethral bulking, a retropubic urethropexy (Burch procedure), or a midurethral sling procedure. Women who undergo an anti-incontinence procedure have an increased risk for urinary retention during a subsequent pregnancy.10 Most women with a midurethral sling will continue to be continent following an obstetric delivery.
Anticipatory guidance
At 3 months postpartum, the incidence of urinary incontinence is 6% to 40%, depending on parity and delivery type. Postpartum urinary incontinence is most common after instrumented vaginal delivery (32%) followed by spontaneous vaginal delivery (28%) and cesarean delivery (15%). The mean prevalence of any type of urinary incontinence is 33% at 3 months postpartum, and only small changes in the rate of urinary incontinence occur over the first postpartum year.11 While urinary incontinence is common postpartum, it should not be considered normal. We counsel that symptoms may improve spontaneously, but treatment can be initiated if the patient experiences significant bother.
A longitudinal cohort study that followed women from 3 months to 12 years postpartum found that, of women with urinary incontinence at 3 months postpartum, 76% continued to report incontinence at 12 years postpartum.12 We recommend that women be counseled that, even when symptoms resolve, they remain at increased risk for urinary incontinence in the future. Invasive therapies should be used to treat bothersome urinary incontinence, not to prevent future incontinence.
CASE 3 Fecal incontinence
A 24-year-old woman (G1P1) presents 3 weeks postpartum following a forceps-assisted vaginal delivery complicated by a 3c laceration. She reports fecal urgency, inability to control flatus, and once-daily fecal incontinence.
How would you evaluate these symptoms?
Steps in evaluation
The initial evaluation should include an inquiry regarding the patient’s stool consistency and bowel regimen. The Bristol stool form scale can be used to help patients describe their typical bowel movements (TABLE 2).13 During healing, the goal is to achieve a Bristol type 4 stool, both to avoid straining and to improve continence, as loose stool is the most difficult to control.
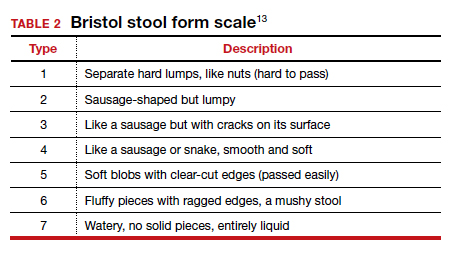
A physical examination can evaluate healing and sphincter integrity; it should include inspection of the distal vagina and perineal body and a digital rectal exam. Anal canal resting tone and squeeze strength should be evaluated, and the digital rectal examination scoring system (DRESS) can be useful for quantification (TABLE 3).14 Lack of tone at rest in the anterolateral portion of the sphincter complex can indicate an internal anal sphincter defect, as 80% of the resting tone comes from this muscle (FIGURE).15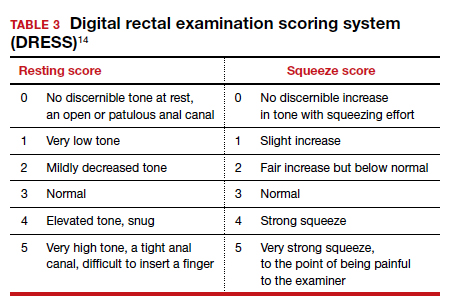
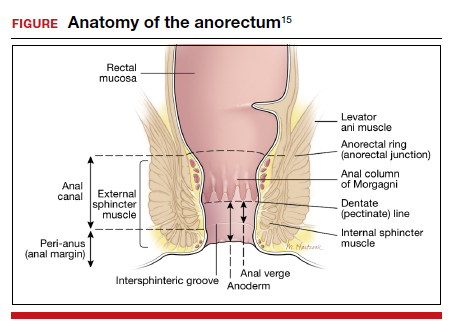
The rectovaginal septum should be assessed given the increased risk of rectovaginal fistula in women with obstetric anal sphincter injury (OASI). The patient should be instructed to contract the anal sphincter, allowing evaluation of muscular contraction. Lack of contraction anteriolaterally may indicate external anal sphincter separation.
Continue to: Conservative options for improving fecal incontinence symptoms...
Conservative options for improving fecal incontinence symptoms
The patient can be counseled regarding stool bulking, first with insoluble fiber supplementation and cessation of stool softeners if she is incontinent of liquid stool. If these measures are not effective, use of a constipating agent, such as loperamide, can improve stool consistency and thereby decrease incontinence episodes. PFPT with biofeedback can be offered as well. While typically we do not recommend initiating PFPT before 6 weeks postpartum, so the initial phases of healing can occur, early referral enables the patient to avoid a delay in access to care.
The patient also can be counseled about a referral to a pelvic floor specialist for further evaluation. A variety of peripartum pelvic floor disorder clinics are being established by Female Pelvic Medicine and Reconstructive Surgery (FPMRS) physicians. These clinics provide the benefit of comprehensive care for pelvic floor disorders in this unique population.
When conservative measures fail. If a patient has persistent bowel control issues despite conservative measures, a referral to an FPMRS physician should be initiated.
Delivery route in future pregnancies
The risk of a subsequent OASI is low. While this means that many women can safely pursue a future vaginal delivery, a scheduled cesarean delivery is indicated for women with persistent bowel control issues, wound healing complications, and those who experienced psychological trauma from their delivery.16 We recommend a shared-decision making approach, reviewing modifiable and nonmodifiable risk factors to help determine whether or not a future vaginal birth is appropriate. It is important to highlight that a cesarean delivery does not protect against fecal incontinence in women with a history of OASI; however, there is benefit in preventing worsening of anal incontinence, if present.17
CASE 4 Uterovaginal prolapse
A 36-year-old woman (G3P3) presents for her routine postpartum visit at 6 weeks after a spontaneous vaginal delivery without lacerations. She reports a persistent feeling of vaginal pressure and fullness. She thinks she felt a bulge with wiping after a bowel movement.
What options are available for this patient?
Prolapse in the peripartum population
Previous studies have revealed an increased prevalence of POP in pregnant women on examination compared with their nulligravid counterparts (47.6% vs 0%).18 With the changes in the hormonal milieu in pregnancy, as well as the weight of the gravid uterus on the pelvic floor, it is not surprising that pregnancy may be the inciting event to expose even transient defects in pelvic organ support.19
It is well established that increasing parity and, to a lesser extent, larger babies are associated with increased risk for future POP and surgery for prolapse. In the first year postpartum, nearly one-third of women have stage 2 or greater prolapse on exam, with studies demonstrating an increased prevalence of postpartum POP in women who delivered vaginally compared with those who delivered by cesarean.20,21
Initial evaluation
Diagnosis can be made during a routine pelvic exam by having the patient perform a Valsalva maneuver while in the lithotomy position. Using half of a speculum permits evaluation of the anterior and posterior vaginal walls separately, and Valsalva during a bimanual exam can aid in evaluating descensus of the uterus and cervix.
Excellent free patient education resources available online through the American Urogynecologic Society and the International Urogynecological Association can be used to direct counseling.
Continue to: Treatments you can offer for POP...
Treatments you can offer for POP
For pregnant or postpartum patients with bothersome prolapse, initial management options include pessary fitting and/or PFPT referral. In pregnancy, women often can be successfully fitted with a pessary for POP; however, as expulsion is a common issue, selection of a stiffer or space-occupying device may be more efficacious.
Often, early onset POP in pregnancy resolves as the gravid uterus lifts out of the pelvis in the second trimester, at which time the pessary can be discontinued. In the postpartum period, a pessary fitting can be undertaken similarly to that in nonpregnant patients. While data are lacking in the peripartum population, evidence supports the positive impact of PFPT on improving POP symptom bother.22 Additionally, for postpartum women who experience OASI, PFPT can produce significant improvement in subjective POP and associated bother.23
Impact of future childbearing wishes on treatment
The desire for future childbearing does not preclude treatment of patients experiencing bother from POP after conservative management options have failed. Both vaginal native tissue and mesh-augmented uterine-sparing repairs are performed by many FPMRS specialists and are associated with good outcomes. As with SUI, we do not recommend invasive treatment for POP during pregnancy or before 6 months postpartum.
In conclusion
Obstetric specialists play an essential role in caring for women with PFDs in the peripartum period. Basic evaluation, counseling, and management can be initiated using many of the resources already available in an obstetric ambulatory practice. Important adjunctive resources include those available for both providers and patients through the American Urogynecologic Society and the International Urogynecological Association. In addition, clinicians can partner with pelvic floor specialists through the growing number of FPMRS-run peripartum pelvic floor disorder clinics across the country and pelvic floor physical therapists.
If these specialty clinics and therapists are not available in your area, FPMRS specialists, urologists, gastroenterologists, and/or colorectal surgeons can aid in patient diagnosis and management to reach the ultimate goal of improving PFDs in this at-risk population. ●
- Madsen AM, Hickman LC, Propst K. Recognition and management of pelvic floor disorders in pregnancy and the postpartum period. Obstet Gynecol Clin North Am. Forthcoming 2021.
- Bodner-Adler B, Kimberger O, Laml T, et al. Prevalence and risk factors for pelvic floor disorders during early and late pregnancy in a cohort of Austrian women. Arch Gynecol Obstet. 2019;300:1325-1330.
- Swenson CW, DePorre JA, Haefner JK, et al. Postpartum depression screening and pelvic floor symptoms among women referred to a specialty postpartum perineal clinic. Am J Obstet Gynecol. 2018;218:335.e1-335.e6.
- Skinner EM, Dietz HP. Psychological and somatic sequelae of traumatic vaginal delivery: a literature review. Aust N Z J Obstet Gynaecol. 2015;55:309-314.
- Yohay D, Weintraub AY, Mauer-Perry N, et al. Prevalence and trends of pelvic floor disorders in late pregnancy and after delivery in a cohort of Israeli women using the PFDI-20. Eur J Obstet Gynecol Reprod Biol. 2016;200:35-39.
- Gregory WT, Sibai BM. Obstetrics and pelvic floor disorders. In: Walters M, Karram M, eds. Urogynecology and Reconstructive Pelvic Surgery. 4th ed. Philadelphia, PA: Saunders; 2015:224-237.
- Richter HE, Burgio KL, Brubaker L, et al; Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115:609-617.
- Woodley SJ, Lawrenson P, Boyle R, et al. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2020;6:CD007471.
- Foldspang A, Hvidman L, Mommsen S, et al. Risk of postpartum urinary incontinence associated with pregnancy and mode of delivery. Acta Obstet Gynecol Scand. 2004;83:923-927.
- Wieslander CK, Weinstein MM, Handa V, et al. Pregnancy in women with prior treatments for pelvic floor disorders. Female Pelvic Med Reconstr Surg. 2020;26:299-305.
- Thom DH, Rortveit G. Prevalence of postpartum urinary incontinence: a systematic review. Acta Obstet Gynecol Scand. 2010;89:1511-1522.
- MacArthur C, Wilson D, Herbison P, et al; Prolong Study Group. Urinary incontinence persisting after childbirth: extent, delivery history, and effects in a 12-year longitudinal cohort study. BJOG. 2016;123:1022-1029.
- Blake MR, Raker JM, Whelan K. Validity and reliability of the Bristol Stool Form Scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44:693-703
- Orkin BA, Sinykin SB, Lloyd PC. The digital rectal examination scoring system (DRESS). Dis Colon Rectum. 2010;53:1656-1660.
- UpToDate. Repair of episiotomy and perineal lacerations associated with childbirth. 2020. https://www-uptodate-com .ccmain.ohionet.org/contents/repair-of-perineal-and-other -lacerations-associated-with-childbirth?search=repair%20 episiotomy&source=search_result&selectedTitle=1~150&usa ge_type=default&display_rank=1. Accessed February 28, 2021.
- Committee on Practice Bulletins–Obstetrics. ACOG practice bulletin no. 198: prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2018;132:e87-e102.
- Jangö H, Langhoff-Roos J, Rosthøj S, et al. Long-term anal incontinence after obstetric anal sphincter injury—does grade of tear matter? Am J Obstet Gynecol. 2018;218:232.e1-232.e10.
- O’Boyle AL, Woodman PJ, O’Boyle JD, et al. Pelvic organ support in nulliparous pregnant and nonpregnant women: a case control study. Am J Obstet Gynecol. 2002;187:99-102.
- Handa VL, Blomquist JL, McDermott KC, et al. Pelvic floor disorders after vaginal birth. Obstet Gynecol. 2012;119 (2, pt 1):233-239.
- Handa VL, Nygaard I, Kenton K, et al; Pelvic Floor Disorders Network. Pelvic organ support among primiparous women in the first year after childbirth. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:1407-1411.
- O’Boyle AL, O’Boyle JD, Calhoun B, et al. Pelvic organ support in pregnancy and postpartum. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:69-72.
- Hagen S, Stark D, Glazener C, et al; POPPY Trial Collaborators. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. Lancet. 2014;383:796-806.
- Von Bargen E, Haviland MJ, Chang OH, et al. Evaluation of postpartum pelvic floor physical therapy on obstetrical anal sphincter injury: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2020. doi: 10.1097/SPV.0000000000000849.
Pelvic floor disorders (PFDs) affect many pregnant and newly postpartum women. These conditions, including urinary incontinence, anal incontinence, and pelvic organ prolapse (POP), can be overshadowed by common pregnancy and postpartum concerns (TABLE 1).1 With the use of a few quick screening questions, however, PFDs easily can be identified in this at-risk population. Active management need not be delayed until after delivery for women experiencing bother, as options exist for women with PFDs during pregnancy as well as postpartum.
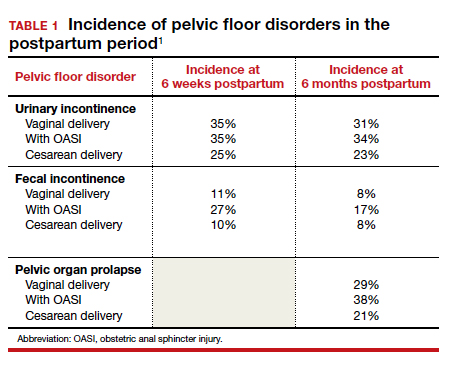
In this article, we discuss the common PFDs that obstetric clinicians face in the context of case scenarios and review how you can be better equipped to care for affected individuals.
CASE 1 Screening
A 30-year-old woman (G1P1) presents for her routine postpartum visit after an operative vaginal delivery with a second-degree laceration.
How would you screen this patient for PFDs?
Why screening for PFDs matters
While there are no validated PFD screening tools for this patient population, clinicians can ask a series of brief open-ended questions as part of the review of systems to efficiently evaluate for the common PFDs in peripartum patients (see “Screening questions to evaluate patients for peripartum pelvic floor disorders” below).
Pelvic floor disorders in the peripartum period can have a significant negative impact. In pregnancy, nearly half of women report psychological strain due to the presence of bowel, bladder, prolapse, or sexual dysfunction symptoms.2 Postpartum, PFDs have negative effects on overall health, well-being, and self-esteem, with significantly increased rates of postpartum depression in women who experience urinary incontinence.3,4 Proactively inquiring about PFD symptoms, providing anticipatory guidance, and recommending treatment options can positively impact a patient in multiple domains.
Sometimes during pregnancy or after having a baby, a woman experiences pelvic floor symptoms. Do you have any of the following?
- leakage with coughing, laughing, sneezing, or physical activity
- urgency to urinate or leakage due to urgency
- bulging or pressure within the vagina
- pain with intercourse
- accidental bowel leakage of stool or flatus
CASE 2 Stress urinary incontinence
A 27-year-old woman (G1P1) presents 2 months following spontaneous vaginal delivery with symptoms of urine leakage with laughing and running. Her urinary incontinence has been improving since delivery, but it continues to be bothersome.
What would you recommend for this patient?
Conservative SUI management strategies in pregnancy
Urinary tract symptoms are common in pregnancy, with up to 41.8% of women reporting urinary symptom distress in the third trimester.5 During pregnancy, estrogen and progesterone decrease urethral pressure that, together with increased intra-abdominal pressure from the gravid uterus, can cause or worsen stress urinary incontinence (SUI).6
During pregnancy, women should be offered conservative therapies for SUI. For women who can perform a pelvic floor contraction (a Kegel exercise), self-guided pelvic floor muscle exercises (PFMEs) may be helpful (see “Pelvic floor muscle exercises” below). We recommend that women start with 1 to 2 sets of 10 Kegel exercises per day and that they hold the squeeze for 2 to 3 seconds, working up to holding for 10 seconds. The goal is to strengthen and improve muscle control so that the Kegel squeeze can be paired with activities that cause SUI.
For women who are unable to perform a Kegel exercise or are not improving with a home PFME regimen, referral to pelvic floor physical therapy (PFPT) can be considered. While data support the efficacy of PFPT for SUI treatment in nonpregnant women,7 data are lacking on PFME in pregnancy.
In women without urinary incontinence, PFME in early pregnancy can prevent the onset of incontinence in late pregnancy and the postpartum period.8 By contrast, the same 2020 Cochrane Review found no evidence that antenatal pelvic floor muscle therapy in incontinent women decreases incontinence in mid- or late-pregnancy or in the postpartum period.8 As the quality of this evidence is very low and there is no evidence of harm with PFME, we continue to recommend it for women with bothersome SUI.
Incontinence pessaries or vaginal inserts (such as Poise Impressa bladder supports) can be helpful for SUI treatment. An incontinence pessary can be fitted in the office, and fitting kits are available for both. Pessaries can safely be used in pregnancy, but there are no data on the efficacy of pessaries for treating SUI in pregnancy. In nonpregnant women, evidence demonstrates 63% satisfaction 3 months post–pessary placement for SUI.7
We do not recommend invasive procedures for the treatment of SUI during pregnancy or in the first 6 months following delivery. There is no evidence that elective cesarean delivery prevents persistent SUI postpartum.9
To identify and engage the proper pelvic floor muscles:
- Insert a finger in the vagina and squeeze the vaginal muscles around your finger.
- Imagine you are sitting on a marble and have to pick it up with the vaginal muscles.
- Squeeze the muscles you would use to stop the flow of urine or hold back flatulence.
Perform sets of 10, 2 to 3 times per day as follows:
- Squeeze: Engage the pelvic floor muscles as described above; avoid performing Kegels while voiding.
- Hold: For 2 to 10 seconds; increase the duration to 10 seconds as able.
- Relax: Completely relax muscles before initating the next squeeze.
Reference
1. UpToDate. Patient education: pelvic muscle (Kegel) exercises (the basics). 2018. https://uptodatefree.ir/topic.htm?path=pelvic-muscle-kegel-exercises-the-basics. Accessed February 24, 2021.
Continue to: Managing SUI in the postpartum period...
Managing SUI in the postpartum period
After the first 6 months postpartum and exhaustion of conservative measures, we offer surgical interventions for women with persistent, bothersome incontinence. Surgery for SUI typically is not recommended until childbearing is complete, but it can be considered if the patient’s bother is significant.
For women with bothersome SUI who still desire future pregnancy, management options include periurethral bulking, a retropubic urethropexy (Burch procedure), or a midurethral sling procedure. Women who undergo an anti-incontinence procedure have an increased risk for urinary retention during a subsequent pregnancy.10 Most women with a midurethral sling will continue to be continent following an obstetric delivery.
Anticipatory guidance
At 3 months postpartum, the incidence of urinary incontinence is 6% to 40%, depending on parity and delivery type. Postpartum urinary incontinence is most common after instrumented vaginal delivery (32%) followed by spontaneous vaginal delivery (28%) and cesarean delivery (15%). The mean prevalence of any type of urinary incontinence is 33% at 3 months postpartum, and only small changes in the rate of urinary incontinence occur over the first postpartum year.11 While urinary incontinence is common postpartum, it should not be considered normal. We counsel that symptoms may improve spontaneously, but treatment can be initiated if the patient experiences significant bother.
A longitudinal cohort study that followed women from 3 months to 12 years postpartum found that, of women with urinary incontinence at 3 months postpartum, 76% continued to report incontinence at 12 years postpartum.12 We recommend that women be counseled that, even when symptoms resolve, they remain at increased risk for urinary incontinence in the future. Invasive therapies should be used to treat bothersome urinary incontinence, not to prevent future incontinence.
CASE 3 Fecal incontinence
A 24-year-old woman (G1P1) presents 3 weeks postpartum following a forceps-assisted vaginal delivery complicated by a 3c laceration. She reports fecal urgency, inability to control flatus, and once-daily fecal incontinence.
How would you evaluate these symptoms?
Steps in evaluation
The initial evaluation should include an inquiry regarding the patient’s stool consistency and bowel regimen. The Bristol stool form scale can be used to help patients describe their typical bowel movements (TABLE 2).13 During healing, the goal is to achieve a Bristol type 4 stool, both to avoid straining and to improve continence, as loose stool is the most difficult to control.
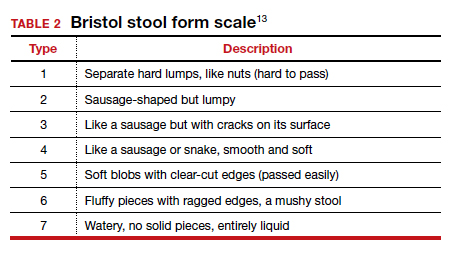
A physical examination can evaluate healing and sphincter integrity; it should include inspection of the distal vagina and perineal body and a digital rectal exam. Anal canal resting tone and squeeze strength should be evaluated, and the digital rectal examination scoring system (DRESS) can be useful for quantification (TABLE 3).14 Lack of tone at rest in the anterolateral portion of the sphincter complex can indicate an internal anal sphincter defect, as 80% of the resting tone comes from this muscle (FIGURE).15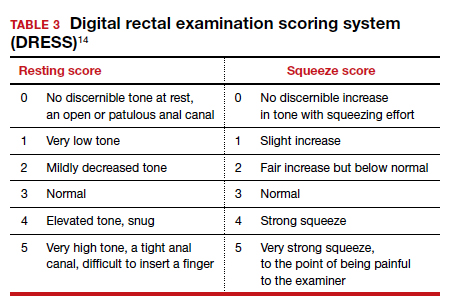
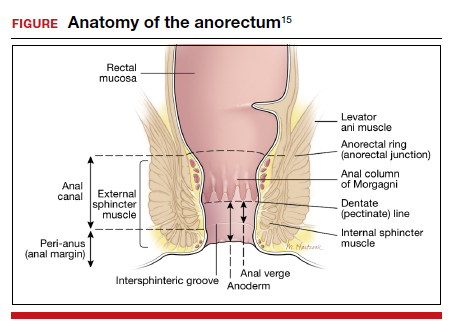
The rectovaginal septum should be assessed given the increased risk of rectovaginal fistula in women with obstetric anal sphincter injury (OASI). The patient should be instructed to contract the anal sphincter, allowing evaluation of muscular contraction. Lack of contraction anteriolaterally may indicate external anal sphincter separation.
Continue to: Conservative options for improving fecal incontinence symptoms...
Conservative options for improving fecal incontinence symptoms
The patient can be counseled regarding stool bulking, first with insoluble fiber supplementation and cessation of stool softeners if she is incontinent of liquid stool. If these measures are not effective, use of a constipating agent, such as loperamide, can improve stool consistency and thereby decrease incontinence episodes. PFPT with biofeedback can be offered as well. While typically we do not recommend initiating PFPT before 6 weeks postpartum, so the initial phases of healing can occur, early referral enables the patient to avoid a delay in access to care.
The patient also can be counseled about a referral to a pelvic floor specialist for further evaluation. A variety of peripartum pelvic floor disorder clinics are being established by Female Pelvic Medicine and Reconstructive Surgery (FPMRS) physicians. These clinics provide the benefit of comprehensive care for pelvic floor disorders in this unique population.
When conservative measures fail. If a patient has persistent bowel control issues despite conservative measures, a referral to an FPMRS physician should be initiated.
Delivery route in future pregnancies
The risk of a subsequent OASI is low. While this means that many women can safely pursue a future vaginal delivery, a scheduled cesarean delivery is indicated for women with persistent bowel control issues, wound healing complications, and those who experienced psychological trauma from their delivery.16 We recommend a shared-decision making approach, reviewing modifiable and nonmodifiable risk factors to help determine whether or not a future vaginal birth is appropriate. It is important to highlight that a cesarean delivery does not protect against fecal incontinence in women with a history of OASI; however, there is benefit in preventing worsening of anal incontinence, if present.17
CASE 4 Uterovaginal prolapse
A 36-year-old woman (G3P3) presents for her routine postpartum visit at 6 weeks after a spontaneous vaginal delivery without lacerations. She reports a persistent feeling of vaginal pressure and fullness. She thinks she felt a bulge with wiping after a bowel movement.
What options are available for this patient?
Prolapse in the peripartum population
Previous studies have revealed an increased prevalence of POP in pregnant women on examination compared with their nulligravid counterparts (47.6% vs 0%).18 With the changes in the hormonal milieu in pregnancy, as well as the weight of the gravid uterus on the pelvic floor, it is not surprising that pregnancy may be the inciting event to expose even transient defects in pelvic organ support.19
It is well established that increasing parity and, to a lesser extent, larger babies are associated with increased risk for future POP and surgery for prolapse. In the first year postpartum, nearly one-third of women have stage 2 or greater prolapse on exam, with studies demonstrating an increased prevalence of postpartum POP in women who delivered vaginally compared with those who delivered by cesarean.20,21
Initial evaluation
Diagnosis can be made during a routine pelvic exam by having the patient perform a Valsalva maneuver while in the lithotomy position. Using half of a speculum permits evaluation of the anterior and posterior vaginal walls separately, and Valsalva during a bimanual exam can aid in evaluating descensus of the uterus and cervix.
Excellent free patient education resources available online through the American Urogynecologic Society and the International Urogynecological Association can be used to direct counseling.
Continue to: Treatments you can offer for POP...
Treatments you can offer for POP
For pregnant or postpartum patients with bothersome prolapse, initial management options include pessary fitting and/or PFPT referral. In pregnancy, women often can be successfully fitted with a pessary for POP; however, as expulsion is a common issue, selection of a stiffer or space-occupying device may be more efficacious.
Often, early onset POP in pregnancy resolves as the gravid uterus lifts out of the pelvis in the second trimester, at which time the pessary can be discontinued. In the postpartum period, a pessary fitting can be undertaken similarly to that in nonpregnant patients. While data are lacking in the peripartum population, evidence supports the positive impact of PFPT on improving POP symptom bother.22 Additionally, for postpartum women who experience OASI, PFPT can produce significant improvement in subjective POP and associated bother.23
Impact of future childbearing wishes on treatment
The desire for future childbearing does not preclude treatment of patients experiencing bother from POP after conservative management options have failed. Both vaginal native tissue and mesh-augmented uterine-sparing repairs are performed by many FPMRS specialists and are associated with good outcomes. As with SUI, we do not recommend invasive treatment for POP during pregnancy or before 6 months postpartum.
In conclusion
Obstetric specialists play an essential role in caring for women with PFDs in the peripartum period. Basic evaluation, counseling, and management can be initiated using many of the resources already available in an obstetric ambulatory practice. Important adjunctive resources include those available for both providers and patients through the American Urogynecologic Society and the International Urogynecological Association. In addition, clinicians can partner with pelvic floor specialists through the growing number of FPMRS-run peripartum pelvic floor disorder clinics across the country and pelvic floor physical therapists.
If these specialty clinics and therapists are not available in your area, FPMRS specialists, urologists, gastroenterologists, and/or colorectal surgeons can aid in patient diagnosis and management to reach the ultimate goal of improving PFDs in this at-risk population. ●
Pelvic floor disorders (PFDs) affect many pregnant and newly postpartum women. These conditions, including urinary incontinence, anal incontinence, and pelvic organ prolapse (POP), can be overshadowed by common pregnancy and postpartum concerns (TABLE 1).1 With the use of a few quick screening questions, however, PFDs easily can be identified in this at-risk population. Active management need not be delayed until after delivery for women experiencing bother, as options exist for women with PFDs during pregnancy as well as postpartum.
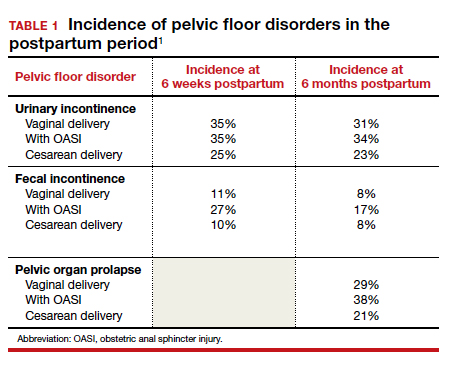
In this article, we discuss the common PFDs that obstetric clinicians face in the context of case scenarios and review how you can be better equipped to care for affected individuals.
CASE 1 Screening
A 30-year-old woman (G1P1) presents for her routine postpartum visit after an operative vaginal delivery with a second-degree laceration.
How would you screen this patient for PFDs?
Why screening for PFDs matters
While there are no validated PFD screening tools for this patient population, clinicians can ask a series of brief open-ended questions as part of the review of systems to efficiently evaluate for the common PFDs in peripartum patients (see “Screening questions to evaluate patients for peripartum pelvic floor disorders” below).
Pelvic floor disorders in the peripartum period can have a significant negative impact. In pregnancy, nearly half of women report psychological strain due to the presence of bowel, bladder, prolapse, or sexual dysfunction symptoms.2 Postpartum, PFDs have negative effects on overall health, well-being, and self-esteem, with significantly increased rates of postpartum depression in women who experience urinary incontinence.3,4 Proactively inquiring about PFD symptoms, providing anticipatory guidance, and recommending treatment options can positively impact a patient in multiple domains.
Sometimes during pregnancy or after having a baby, a woman experiences pelvic floor symptoms. Do you have any of the following?
- leakage with coughing, laughing, sneezing, or physical activity
- urgency to urinate or leakage due to urgency
- bulging or pressure within the vagina
- pain with intercourse
- accidental bowel leakage of stool or flatus
CASE 2 Stress urinary incontinence
A 27-year-old woman (G1P1) presents 2 months following spontaneous vaginal delivery with symptoms of urine leakage with laughing and running. Her urinary incontinence has been improving since delivery, but it continues to be bothersome.
What would you recommend for this patient?
Conservative SUI management strategies in pregnancy
Urinary tract symptoms are common in pregnancy, with up to 41.8% of women reporting urinary symptom distress in the third trimester.5 During pregnancy, estrogen and progesterone decrease urethral pressure that, together with increased intra-abdominal pressure from the gravid uterus, can cause or worsen stress urinary incontinence (SUI).6
During pregnancy, women should be offered conservative therapies for SUI. For women who can perform a pelvic floor contraction (a Kegel exercise), self-guided pelvic floor muscle exercises (PFMEs) may be helpful (see “Pelvic floor muscle exercises” below). We recommend that women start with 1 to 2 sets of 10 Kegel exercises per day and that they hold the squeeze for 2 to 3 seconds, working up to holding for 10 seconds. The goal is to strengthen and improve muscle control so that the Kegel squeeze can be paired with activities that cause SUI.
For women who are unable to perform a Kegel exercise or are not improving with a home PFME regimen, referral to pelvic floor physical therapy (PFPT) can be considered. While data support the efficacy of PFPT for SUI treatment in nonpregnant women,7 data are lacking on PFME in pregnancy.
In women without urinary incontinence, PFME in early pregnancy can prevent the onset of incontinence in late pregnancy and the postpartum period.8 By contrast, the same 2020 Cochrane Review found no evidence that antenatal pelvic floor muscle therapy in incontinent women decreases incontinence in mid- or late-pregnancy or in the postpartum period.8 As the quality of this evidence is very low and there is no evidence of harm with PFME, we continue to recommend it for women with bothersome SUI.
Incontinence pessaries or vaginal inserts (such as Poise Impressa bladder supports) can be helpful for SUI treatment. An incontinence pessary can be fitted in the office, and fitting kits are available for both. Pessaries can safely be used in pregnancy, but there are no data on the efficacy of pessaries for treating SUI in pregnancy. In nonpregnant women, evidence demonstrates 63% satisfaction 3 months post–pessary placement for SUI.7
We do not recommend invasive procedures for the treatment of SUI during pregnancy or in the first 6 months following delivery. There is no evidence that elective cesarean delivery prevents persistent SUI postpartum.9
To identify and engage the proper pelvic floor muscles:
- Insert a finger in the vagina and squeeze the vaginal muscles around your finger.
- Imagine you are sitting on a marble and have to pick it up with the vaginal muscles.
- Squeeze the muscles you would use to stop the flow of urine or hold back flatulence.
Perform sets of 10, 2 to 3 times per day as follows:
- Squeeze: Engage the pelvic floor muscles as described above; avoid performing Kegels while voiding.
- Hold: For 2 to 10 seconds; increase the duration to 10 seconds as able.
- Relax: Completely relax muscles before initating the next squeeze.
Reference
1. UpToDate. Patient education: pelvic muscle (Kegel) exercises (the basics). 2018. https://uptodatefree.ir/topic.htm?path=pelvic-muscle-kegel-exercises-the-basics. Accessed February 24, 2021.
Continue to: Managing SUI in the postpartum period...
Managing SUI in the postpartum period
After the first 6 months postpartum and exhaustion of conservative measures, we offer surgical interventions for women with persistent, bothersome incontinence. Surgery for SUI typically is not recommended until childbearing is complete, but it can be considered if the patient’s bother is significant.
For women with bothersome SUI who still desire future pregnancy, management options include periurethral bulking, a retropubic urethropexy (Burch procedure), or a midurethral sling procedure. Women who undergo an anti-incontinence procedure have an increased risk for urinary retention during a subsequent pregnancy.10 Most women with a midurethral sling will continue to be continent following an obstetric delivery.
Anticipatory guidance
At 3 months postpartum, the incidence of urinary incontinence is 6% to 40%, depending on parity and delivery type. Postpartum urinary incontinence is most common after instrumented vaginal delivery (32%) followed by spontaneous vaginal delivery (28%) and cesarean delivery (15%). The mean prevalence of any type of urinary incontinence is 33% at 3 months postpartum, and only small changes in the rate of urinary incontinence occur over the first postpartum year.11 While urinary incontinence is common postpartum, it should not be considered normal. We counsel that symptoms may improve spontaneously, but treatment can be initiated if the patient experiences significant bother.
A longitudinal cohort study that followed women from 3 months to 12 years postpartum found that, of women with urinary incontinence at 3 months postpartum, 76% continued to report incontinence at 12 years postpartum.12 We recommend that women be counseled that, even when symptoms resolve, they remain at increased risk for urinary incontinence in the future. Invasive therapies should be used to treat bothersome urinary incontinence, not to prevent future incontinence.
CASE 3 Fecal incontinence
A 24-year-old woman (G1P1) presents 3 weeks postpartum following a forceps-assisted vaginal delivery complicated by a 3c laceration. She reports fecal urgency, inability to control flatus, and once-daily fecal incontinence.
How would you evaluate these symptoms?
Steps in evaluation
The initial evaluation should include an inquiry regarding the patient’s stool consistency and bowel regimen. The Bristol stool form scale can be used to help patients describe their typical bowel movements (TABLE 2).13 During healing, the goal is to achieve a Bristol type 4 stool, both to avoid straining and to improve continence, as loose stool is the most difficult to control.
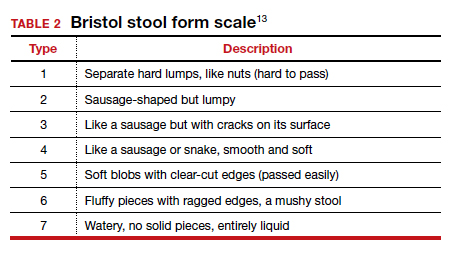
A physical examination can evaluate healing and sphincter integrity; it should include inspection of the distal vagina and perineal body and a digital rectal exam. Anal canal resting tone and squeeze strength should be evaluated, and the digital rectal examination scoring system (DRESS) can be useful for quantification (TABLE 3).14 Lack of tone at rest in the anterolateral portion of the sphincter complex can indicate an internal anal sphincter defect, as 80% of the resting tone comes from this muscle (FIGURE).15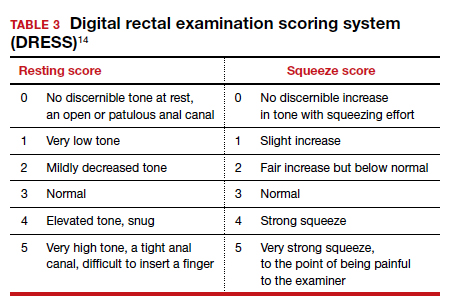
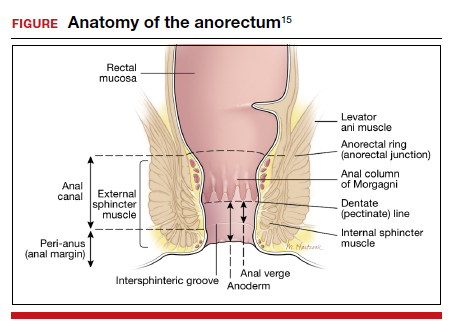
The rectovaginal septum should be assessed given the increased risk of rectovaginal fistula in women with obstetric anal sphincter injury (OASI). The patient should be instructed to contract the anal sphincter, allowing evaluation of muscular contraction. Lack of contraction anteriolaterally may indicate external anal sphincter separation.
Continue to: Conservative options for improving fecal incontinence symptoms...
Conservative options for improving fecal incontinence symptoms
The patient can be counseled regarding stool bulking, first with insoluble fiber supplementation and cessation of stool softeners if she is incontinent of liquid stool. If these measures are not effective, use of a constipating agent, such as loperamide, can improve stool consistency and thereby decrease incontinence episodes. PFPT with biofeedback can be offered as well. While typically we do not recommend initiating PFPT before 6 weeks postpartum, so the initial phases of healing can occur, early referral enables the patient to avoid a delay in access to care.
The patient also can be counseled about a referral to a pelvic floor specialist for further evaluation. A variety of peripartum pelvic floor disorder clinics are being established by Female Pelvic Medicine and Reconstructive Surgery (FPMRS) physicians. These clinics provide the benefit of comprehensive care for pelvic floor disorders in this unique population.
When conservative measures fail. If a patient has persistent bowel control issues despite conservative measures, a referral to an FPMRS physician should be initiated.
Delivery route in future pregnancies
The risk of a subsequent OASI is low. While this means that many women can safely pursue a future vaginal delivery, a scheduled cesarean delivery is indicated for women with persistent bowel control issues, wound healing complications, and those who experienced psychological trauma from their delivery.16 We recommend a shared-decision making approach, reviewing modifiable and nonmodifiable risk factors to help determine whether or not a future vaginal birth is appropriate. It is important to highlight that a cesarean delivery does not protect against fecal incontinence in women with a history of OASI; however, there is benefit in preventing worsening of anal incontinence, if present.17
CASE 4 Uterovaginal prolapse
A 36-year-old woman (G3P3) presents for her routine postpartum visit at 6 weeks after a spontaneous vaginal delivery without lacerations. She reports a persistent feeling of vaginal pressure and fullness. She thinks she felt a bulge with wiping after a bowel movement.
What options are available for this patient?
Prolapse in the peripartum population
Previous studies have revealed an increased prevalence of POP in pregnant women on examination compared with their nulligravid counterparts (47.6% vs 0%).18 With the changes in the hormonal milieu in pregnancy, as well as the weight of the gravid uterus on the pelvic floor, it is not surprising that pregnancy may be the inciting event to expose even transient defects in pelvic organ support.19
It is well established that increasing parity and, to a lesser extent, larger babies are associated with increased risk for future POP and surgery for prolapse. In the first year postpartum, nearly one-third of women have stage 2 or greater prolapse on exam, with studies demonstrating an increased prevalence of postpartum POP in women who delivered vaginally compared with those who delivered by cesarean.20,21
Initial evaluation
Diagnosis can be made during a routine pelvic exam by having the patient perform a Valsalva maneuver while in the lithotomy position. Using half of a speculum permits evaluation of the anterior and posterior vaginal walls separately, and Valsalva during a bimanual exam can aid in evaluating descensus of the uterus and cervix.
Excellent free patient education resources available online through the American Urogynecologic Society and the International Urogynecological Association can be used to direct counseling.
Continue to: Treatments you can offer for POP...
Treatments you can offer for POP
For pregnant or postpartum patients with bothersome prolapse, initial management options include pessary fitting and/or PFPT referral. In pregnancy, women often can be successfully fitted with a pessary for POP; however, as expulsion is a common issue, selection of a stiffer or space-occupying device may be more efficacious.
Often, early onset POP in pregnancy resolves as the gravid uterus lifts out of the pelvis in the second trimester, at which time the pessary can be discontinued. In the postpartum period, a pessary fitting can be undertaken similarly to that in nonpregnant patients. While data are lacking in the peripartum population, evidence supports the positive impact of PFPT on improving POP symptom bother.22 Additionally, for postpartum women who experience OASI, PFPT can produce significant improvement in subjective POP and associated bother.23
Impact of future childbearing wishes on treatment
The desire for future childbearing does not preclude treatment of patients experiencing bother from POP after conservative management options have failed. Both vaginal native tissue and mesh-augmented uterine-sparing repairs are performed by many FPMRS specialists and are associated with good outcomes. As with SUI, we do not recommend invasive treatment for POP during pregnancy or before 6 months postpartum.
In conclusion
Obstetric specialists play an essential role in caring for women with PFDs in the peripartum period. Basic evaluation, counseling, and management can be initiated using many of the resources already available in an obstetric ambulatory practice. Important adjunctive resources include those available for both providers and patients through the American Urogynecologic Society and the International Urogynecological Association. In addition, clinicians can partner with pelvic floor specialists through the growing number of FPMRS-run peripartum pelvic floor disorder clinics across the country and pelvic floor physical therapists.
If these specialty clinics and therapists are not available in your area, FPMRS specialists, urologists, gastroenterologists, and/or colorectal surgeons can aid in patient diagnosis and management to reach the ultimate goal of improving PFDs in this at-risk population. ●
- Madsen AM, Hickman LC, Propst K. Recognition and management of pelvic floor disorders in pregnancy and the postpartum period. Obstet Gynecol Clin North Am. Forthcoming 2021.
- Bodner-Adler B, Kimberger O, Laml T, et al. Prevalence and risk factors for pelvic floor disorders during early and late pregnancy in a cohort of Austrian women. Arch Gynecol Obstet. 2019;300:1325-1330.
- Swenson CW, DePorre JA, Haefner JK, et al. Postpartum depression screening and pelvic floor symptoms among women referred to a specialty postpartum perineal clinic. Am J Obstet Gynecol. 2018;218:335.e1-335.e6.
- Skinner EM, Dietz HP. Psychological and somatic sequelae of traumatic vaginal delivery: a literature review. Aust N Z J Obstet Gynaecol. 2015;55:309-314.
- Yohay D, Weintraub AY, Mauer-Perry N, et al. Prevalence and trends of pelvic floor disorders in late pregnancy and after delivery in a cohort of Israeli women using the PFDI-20. Eur J Obstet Gynecol Reprod Biol. 2016;200:35-39.
- Gregory WT, Sibai BM. Obstetrics and pelvic floor disorders. In: Walters M, Karram M, eds. Urogynecology and Reconstructive Pelvic Surgery. 4th ed. Philadelphia, PA: Saunders; 2015:224-237.
- Richter HE, Burgio KL, Brubaker L, et al; Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115:609-617.
- Woodley SJ, Lawrenson P, Boyle R, et al. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2020;6:CD007471.
- Foldspang A, Hvidman L, Mommsen S, et al. Risk of postpartum urinary incontinence associated with pregnancy and mode of delivery. Acta Obstet Gynecol Scand. 2004;83:923-927.
- Wieslander CK, Weinstein MM, Handa V, et al. Pregnancy in women with prior treatments for pelvic floor disorders. Female Pelvic Med Reconstr Surg. 2020;26:299-305.
- Thom DH, Rortveit G. Prevalence of postpartum urinary incontinence: a systematic review. Acta Obstet Gynecol Scand. 2010;89:1511-1522.
- MacArthur C, Wilson D, Herbison P, et al; Prolong Study Group. Urinary incontinence persisting after childbirth: extent, delivery history, and effects in a 12-year longitudinal cohort study. BJOG. 2016;123:1022-1029.
- Blake MR, Raker JM, Whelan K. Validity and reliability of the Bristol Stool Form Scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44:693-703
- Orkin BA, Sinykin SB, Lloyd PC. The digital rectal examination scoring system (DRESS). Dis Colon Rectum. 2010;53:1656-1660.
- UpToDate. Repair of episiotomy and perineal lacerations associated with childbirth. 2020. https://www-uptodate-com .ccmain.ohionet.org/contents/repair-of-perineal-and-other -lacerations-associated-with-childbirth?search=repair%20 episiotomy&source=search_result&selectedTitle=1~150&usa ge_type=default&display_rank=1. Accessed February 28, 2021.
- Committee on Practice Bulletins–Obstetrics. ACOG practice bulletin no. 198: prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2018;132:e87-e102.
- Jangö H, Langhoff-Roos J, Rosthøj S, et al. Long-term anal incontinence after obstetric anal sphincter injury—does grade of tear matter? Am J Obstet Gynecol. 2018;218:232.e1-232.e10.
- O’Boyle AL, Woodman PJ, O’Boyle JD, et al. Pelvic organ support in nulliparous pregnant and nonpregnant women: a case control study. Am J Obstet Gynecol. 2002;187:99-102.
- Handa VL, Blomquist JL, McDermott KC, et al. Pelvic floor disorders after vaginal birth. Obstet Gynecol. 2012;119 (2, pt 1):233-239.
- Handa VL, Nygaard I, Kenton K, et al; Pelvic Floor Disorders Network. Pelvic organ support among primiparous women in the first year after childbirth. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:1407-1411.
- O’Boyle AL, O’Boyle JD, Calhoun B, et al. Pelvic organ support in pregnancy and postpartum. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:69-72.
- Hagen S, Stark D, Glazener C, et al; POPPY Trial Collaborators. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. Lancet. 2014;383:796-806.
- Von Bargen E, Haviland MJ, Chang OH, et al. Evaluation of postpartum pelvic floor physical therapy on obstetrical anal sphincter injury: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2020. doi: 10.1097/SPV.0000000000000849.
- Madsen AM, Hickman LC, Propst K. Recognition and management of pelvic floor disorders in pregnancy and the postpartum period. Obstet Gynecol Clin North Am. Forthcoming 2021.
- Bodner-Adler B, Kimberger O, Laml T, et al. Prevalence and risk factors for pelvic floor disorders during early and late pregnancy in a cohort of Austrian women. Arch Gynecol Obstet. 2019;300:1325-1330.
- Swenson CW, DePorre JA, Haefner JK, et al. Postpartum depression screening and pelvic floor symptoms among women referred to a specialty postpartum perineal clinic. Am J Obstet Gynecol. 2018;218:335.e1-335.e6.
- Skinner EM, Dietz HP. Psychological and somatic sequelae of traumatic vaginal delivery: a literature review. Aust N Z J Obstet Gynaecol. 2015;55:309-314.
- Yohay D, Weintraub AY, Mauer-Perry N, et al. Prevalence and trends of pelvic floor disorders in late pregnancy and after delivery in a cohort of Israeli women using the PFDI-20. Eur J Obstet Gynecol Reprod Biol. 2016;200:35-39.
- Gregory WT, Sibai BM. Obstetrics and pelvic floor disorders. In: Walters M, Karram M, eds. Urogynecology and Reconstructive Pelvic Surgery. 4th ed. Philadelphia, PA: Saunders; 2015:224-237.
- Richter HE, Burgio KL, Brubaker L, et al; Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115:609-617.
- Woodley SJ, Lawrenson P, Boyle R, et al. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2020;6:CD007471.
- Foldspang A, Hvidman L, Mommsen S, et al. Risk of postpartum urinary incontinence associated with pregnancy and mode of delivery. Acta Obstet Gynecol Scand. 2004;83:923-927.
- Wieslander CK, Weinstein MM, Handa V, et al. Pregnancy in women with prior treatments for pelvic floor disorders. Female Pelvic Med Reconstr Surg. 2020;26:299-305.
- Thom DH, Rortveit G. Prevalence of postpartum urinary incontinence: a systematic review. Acta Obstet Gynecol Scand. 2010;89:1511-1522.
- MacArthur C, Wilson D, Herbison P, et al; Prolong Study Group. Urinary incontinence persisting after childbirth: extent, delivery history, and effects in a 12-year longitudinal cohort study. BJOG. 2016;123:1022-1029.
- Blake MR, Raker JM, Whelan K. Validity and reliability of the Bristol Stool Form Scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44:693-703
- Orkin BA, Sinykin SB, Lloyd PC. The digital rectal examination scoring system (DRESS). Dis Colon Rectum. 2010;53:1656-1660.
- UpToDate. Repair of episiotomy and perineal lacerations associated with childbirth. 2020. https://www-uptodate-com .ccmain.ohionet.org/contents/repair-of-perineal-and-other -lacerations-associated-with-childbirth?search=repair%20 episiotomy&source=search_result&selectedTitle=1~150&usa ge_type=default&display_rank=1. Accessed February 28, 2021.
- Committee on Practice Bulletins–Obstetrics. ACOG practice bulletin no. 198: prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2018;132:e87-e102.
- Jangö H, Langhoff-Roos J, Rosthøj S, et al. Long-term anal incontinence after obstetric anal sphincter injury—does grade of tear matter? Am J Obstet Gynecol. 2018;218:232.e1-232.e10.
- O’Boyle AL, Woodman PJ, O’Boyle JD, et al. Pelvic organ support in nulliparous pregnant and nonpregnant women: a case control study. Am J Obstet Gynecol. 2002;187:99-102.
- Handa VL, Blomquist JL, McDermott KC, et al. Pelvic floor disorders after vaginal birth. Obstet Gynecol. 2012;119 (2, pt 1):233-239.
- Handa VL, Nygaard I, Kenton K, et al; Pelvic Floor Disorders Network. Pelvic organ support among primiparous women in the first year after childbirth. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:1407-1411.
- O’Boyle AL, O’Boyle JD, Calhoun B, et al. Pelvic organ support in pregnancy and postpartum. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:69-72.
- Hagen S, Stark D, Glazener C, et al; POPPY Trial Collaborators. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. Lancet. 2014;383:796-806.
- Von Bargen E, Haviland MJ, Chang OH, et al. Evaluation of postpartum pelvic floor physical therapy on obstetrical anal sphincter injury: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2020. doi: 10.1097/SPV.0000000000000849.
For which patients is maternal oxygen supplementation of value?
Raghuraman N, Temming LA, Doering MM, et al. Maternal oxygen supplementation compared with room air for intrauterine resuscitation: a systematic review and meta-analysis. JAMA Pediatr. January 4, 2021. doi:10.1001/jamapediatrics.2020.5351.
EXPERT COMMENTARY
Maternal oxygen supplementation is widely used in labor for nonreassuring fetal heart rate (FHR) tracings, although its efficacy is uncertain for preventing fetal acidosis, operative intervention, or sequelae of neonatal encephalopathy. Recently, Raghuraman and colleagues reported the results of a systematic review and meta-analysis that included 16 randomized controlled trials. A total of 1,078 women were included in the oxygen group and 974 in the room air group. The primary outcome was umbilical artery pH; 14 trials reported on this outcome.
After analyzing the pooled and stratified results of the effect of maternal oxygen supplementation versus room air on umbilical artery gas measures, the authors concluded that peripartum oxygen supplementation is not associated with clinically relevant improvement in umbilical artery pH. They acknowledged, however, that the published studies were heterogeneous, lacked data on the association of oxygen supplementation with neonatal outcome, and did not assess oxygen use for abnormal FHR tracings, except for one trial with category II FHR tracings.
Effects of O2 supplementation
As maternal arterial hemoglobin is nearly saturated under normal conditions, maternal hyperoxia produces only modest increases in umbilical vein P
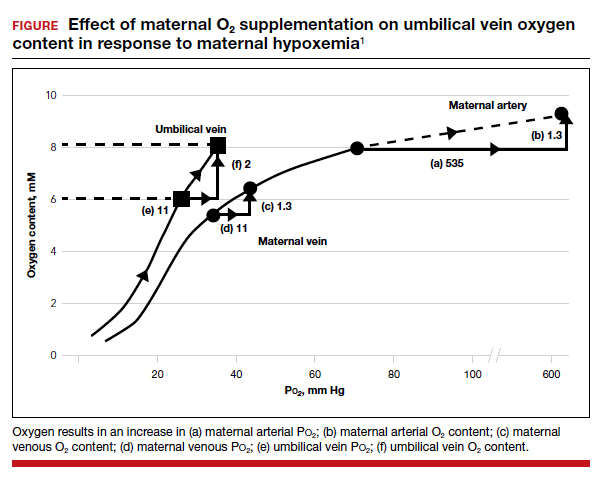
Fetal hypoxemia and acidosis can result from an interruption or an impairment of the mother-to-placenta-to-fetus oxygen pathway. With some interruptions of the oxygen pathway, such as placental abruption and complete cord occlusion–induced bradycardia, there would be less impact of maternal hyperoxia. By contrast, with other oxygen pathway impairments, such as reduced oxygen transfer with placental insufficiency, maternal hyperoxia can be of greater value by increasing maternal uterine artery and vein P
Continue to: Circumstances that may benefit from O2 supplementation...
Circumstances that may benefit from O2 supplementation
Late FHR decelerations reflect impairment of oxygen transfer and thus represent the heart rate pattern that is most likely to benefit from maternal hyperoxia. However, recurrent late decelerations occur in less than 2% of low-risk patients in labor,3 and severe levels of acidosis (umbilical artery pH <7.0 or base deficit [BD] ≥12 mmol/L) occur in only 1% to 2% of near-term or term deliveries.4,5
Variable decelerations also reflect fetal hypoxia and are much more common than late decelerations, so they also may benefit from O2 supplementation. Regardless, O2 supplementation should be seen only as a temporizing strategy while other resuscitative actions are initiated, including preparation for operative delivery, if indicated.
In a prior study by Raghuraman and colleagues (1 of only 4 studies that met selection criteria of oxygen supplementation for patients in labor), newborns of patients not receiving oxygen demonstrated 95% confidence limits of umbilical artery pH (7.24–7.28) and BD (2.9–4.3) well within the normal range.6 Thus, the low prevalence of cases in which a benefit might be anticipated and the low incidence of severe acidosis challenges the design of prospective studies to detect statistically and clinically significant changes in blood gas measures and newborn outcomes.
The normal mild fetal acidosis that develops during labor is likely a result of recurrent interruption of uterine placental blood flow during uterine contractions7 and is unlikely to benefit from maternal hyperoxia. Similarly, as placental oxygen transfer is predominantly flow rather than diffusion limited,8 oxygen supplementation is unlikely to improve severe variable FHR decelerations. Thus, a randomized study of hyperoxia in unselected laboring patients is unlikely to have a measurable effect on clinically significant acidosis.
Oxygen transport pathway guides treatment
For the present, an understanding of oxygen transport can guide clinical oxygen use. Thus, mothers with relative hypoxemia will unquestionably benefit with supplemental oxygen administration. Similarly, fetuses at risk for placental dysfunction (for example, growth restriction, postterm) and particularly those manifesting evidence of impaired oxygen transport (that is, late decelerations) may be most likely to benefit from the increased O2 gradient. For patients with reduced maternal uterine perfusion (such as hypotension or hypovolemia), pressors and/or fluid volume are likely to be more effective, while amnioinfusion is of greater value for umbilical cord compression patterns. A reduction in uterine activity may be of benefit to all fetuses exhibiting compromise. Due to the modest impact on fetal oxygen content, maternal hyperoxia does not produce significant fetal oxidative stress as measured by fetal malondialdehyde levels.
In view of the lack of demonstrated adverse effects of maternal supplemental oxygen, clinicians should not hesitate to use it. However, clinicians should recognize that supplemental oxygen is likely to be of value only in patients with significant impairment in the oxygen pathway, and they should choose additional intrauterine resuscitative measures focused on the etiology.
MICHAEL G. ROSS, MD, MPH,
AND BRYAN S. RICHARDSON, MD
- McNanley T, Woods J. Placental physiology. Glob Libr Women’s Med. (ISSN: 1756-2228). 2008. doi: 10.3843 /GLOWM.10195.
- Richardson BS. Fetal adaptive responses to asphyxia. Clin Perinatol. 1989;16:595-611.
- Sameshima H, Ikenoue T. Predictive value of late decelerations of fetal acidemia in unselective low-risk pregnancies. Am J Perinatol. 2005;22:19-23.
- Yeh P, Emary K, Impey L. The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51,519 consecutive validated samples. BJOG. 2012;119:824-831.
- Kelly R, Ramaiah SM, Sheridan H, et al. Dose-dependent relationship between acidosis at birth and likelihood of death or cerebral palsy. Arch Dis Child Fetal Neonatal Ed. 2018;103:F567-F572.
- Raghuraman N, Wan L, Temming LA, et al. Effect of oxygen vs room air on intrauterine fetal resuscitation: a randomized noninferiority clinical trial. JAMA Pediatr. 2018;172:818-823.
- Ramsey EM, Corner JW Jr, Donner MW. Serial and cineradioangiographic visualization of maternal circulation in the primate (hemochorial) placenta. Am J Obstet Gynecol. 1963;86:213-225.
- Nye GA, Ingram E, Johnstone ED, et al. Human placental oxygenation in late gestation: experimental and theoretical approaches. J Physiol. 2018;596:5523-5534.
Raghuraman N, Temming LA, Doering MM, et al. Maternal oxygen supplementation compared with room air for intrauterine resuscitation: a systematic review and meta-analysis. JAMA Pediatr. January 4, 2021. doi:10.1001/jamapediatrics.2020.5351.
EXPERT COMMENTARY
Maternal oxygen supplementation is widely used in labor for nonreassuring fetal heart rate (FHR) tracings, although its efficacy is uncertain for preventing fetal acidosis, operative intervention, or sequelae of neonatal encephalopathy. Recently, Raghuraman and colleagues reported the results of a systematic review and meta-analysis that included 16 randomized controlled trials. A total of 1,078 women were included in the oxygen group and 974 in the room air group. The primary outcome was umbilical artery pH; 14 trials reported on this outcome.
After analyzing the pooled and stratified results of the effect of maternal oxygen supplementation versus room air on umbilical artery gas measures, the authors concluded that peripartum oxygen supplementation is not associated with clinically relevant improvement in umbilical artery pH. They acknowledged, however, that the published studies were heterogeneous, lacked data on the association of oxygen supplementation with neonatal outcome, and did not assess oxygen use for abnormal FHR tracings, except for one trial with category II FHR tracings.
Effects of O2 supplementation
As maternal arterial hemoglobin is nearly saturated under normal conditions, maternal hyperoxia produces only modest increases in umbilical vein P
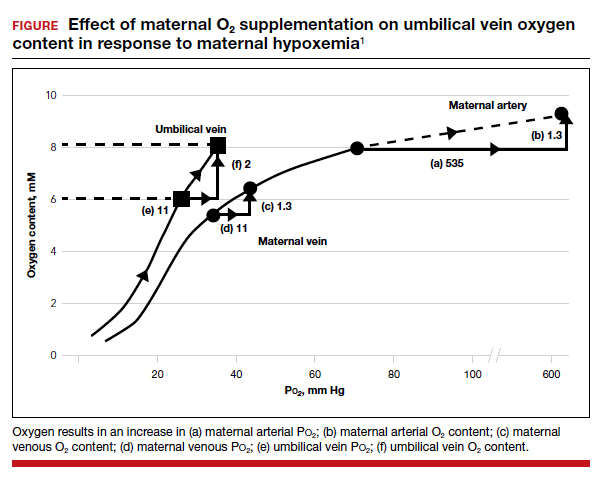
Fetal hypoxemia and acidosis can result from an interruption or an impairment of the mother-to-placenta-to-fetus oxygen pathway. With some interruptions of the oxygen pathway, such as placental abruption and complete cord occlusion–induced bradycardia, there would be less impact of maternal hyperoxia. By contrast, with other oxygen pathway impairments, such as reduced oxygen transfer with placental insufficiency, maternal hyperoxia can be of greater value by increasing maternal uterine artery and vein P
Continue to: Circumstances that may benefit from O2 supplementation...
Circumstances that may benefit from O2 supplementation
Late FHR decelerations reflect impairment of oxygen transfer and thus represent the heart rate pattern that is most likely to benefit from maternal hyperoxia. However, recurrent late decelerations occur in less than 2% of low-risk patients in labor,3 and severe levels of acidosis (umbilical artery pH <7.0 or base deficit [BD] ≥12 mmol/L) occur in only 1% to 2% of near-term or term deliveries.4,5
Variable decelerations also reflect fetal hypoxia and are much more common than late decelerations, so they also may benefit from O2 supplementation. Regardless, O2 supplementation should be seen only as a temporizing strategy while other resuscitative actions are initiated, including preparation for operative delivery, if indicated.
In a prior study by Raghuraman and colleagues (1 of only 4 studies that met selection criteria of oxygen supplementation for patients in labor), newborns of patients not receiving oxygen demonstrated 95% confidence limits of umbilical artery pH (7.24–7.28) and BD (2.9–4.3) well within the normal range.6 Thus, the low prevalence of cases in which a benefit might be anticipated and the low incidence of severe acidosis challenges the design of prospective studies to detect statistically and clinically significant changes in blood gas measures and newborn outcomes.
The normal mild fetal acidosis that develops during labor is likely a result of recurrent interruption of uterine placental blood flow during uterine contractions7 and is unlikely to benefit from maternal hyperoxia. Similarly, as placental oxygen transfer is predominantly flow rather than diffusion limited,8 oxygen supplementation is unlikely to improve severe variable FHR decelerations. Thus, a randomized study of hyperoxia in unselected laboring patients is unlikely to have a measurable effect on clinically significant acidosis.
Oxygen transport pathway guides treatment
For the present, an understanding of oxygen transport can guide clinical oxygen use. Thus, mothers with relative hypoxemia will unquestionably benefit with supplemental oxygen administration. Similarly, fetuses at risk for placental dysfunction (for example, growth restriction, postterm) and particularly those manifesting evidence of impaired oxygen transport (that is, late decelerations) may be most likely to benefit from the increased O2 gradient. For patients with reduced maternal uterine perfusion (such as hypotension or hypovolemia), pressors and/or fluid volume are likely to be more effective, while amnioinfusion is of greater value for umbilical cord compression patterns. A reduction in uterine activity may be of benefit to all fetuses exhibiting compromise. Due to the modest impact on fetal oxygen content, maternal hyperoxia does not produce significant fetal oxidative stress as measured by fetal malondialdehyde levels.
In view of the lack of demonstrated adverse effects of maternal supplemental oxygen, clinicians should not hesitate to use it. However, clinicians should recognize that supplemental oxygen is likely to be of value only in patients with significant impairment in the oxygen pathway, and they should choose additional intrauterine resuscitative measures focused on the etiology.
MICHAEL G. ROSS, MD, MPH,
AND BRYAN S. RICHARDSON, MD
Raghuraman N, Temming LA, Doering MM, et al. Maternal oxygen supplementation compared with room air for intrauterine resuscitation: a systematic review and meta-analysis. JAMA Pediatr. January 4, 2021. doi:10.1001/jamapediatrics.2020.5351.
EXPERT COMMENTARY
Maternal oxygen supplementation is widely used in labor for nonreassuring fetal heart rate (FHR) tracings, although its efficacy is uncertain for preventing fetal acidosis, operative intervention, or sequelae of neonatal encephalopathy. Recently, Raghuraman and colleagues reported the results of a systematic review and meta-analysis that included 16 randomized controlled trials. A total of 1,078 women were included in the oxygen group and 974 in the room air group. The primary outcome was umbilical artery pH; 14 trials reported on this outcome.
After analyzing the pooled and stratified results of the effect of maternal oxygen supplementation versus room air on umbilical artery gas measures, the authors concluded that peripartum oxygen supplementation is not associated with clinically relevant improvement in umbilical artery pH. They acknowledged, however, that the published studies were heterogeneous, lacked data on the association of oxygen supplementation with neonatal outcome, and did not assess oxygen use for abnormal FHR tracings, except for one trial with category II FHR tracings.
Effects of O2 supplementation
As maternal arterial hemoglobin is nearly saturated under normal conditions, maternal hyperoxia produces only modest increases in umbilical vein P
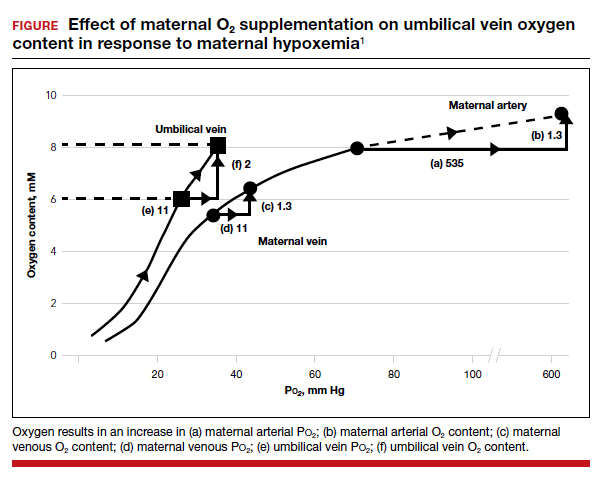
Fetal hypoxemia and acidosis can result from an interruption or an impairment of the mother-to-placenta-to-fetus oxygen pathway. With some interruptions of the oxygen pathway, such as placental abruption and complete cord occlusion–induced bradycardia, there would be less impact of maternal hyperoxia. By contrast, with other oxygen pathway impairments, such as reduced oxygen transfer with placental insufficiency, maternal hyperoxia can be of greater value by increasing maternal uterine artery and vein P
Continue to: Circumstances that may benefit from O2 supplementation...
Circumstances that may benefit from O2 supplementation
Late FHR decelerations reflect impairment of oxygen transfer and thus represent the heart rate pattern that is most likely to benefit from maternal hyperoxia. However, recurrent late decelerations occur in less than 2% of low-risk patients in labor,3 and severe levels of acidosis (umbilical artery pH <7.0 or base deficit [BD] ≥12 mmol/L) occur in only 1% to 2% of near-term or term deliveries.4,5
Variable decelerations also reflect fetal hypoxia and are much more common than late decelerations, so they also may benefit from O2 supplementation. Regardless, O2 supplementation should be seen only as a temporizing strategy while other resuscitative actions are initiated, including preparation for operative delivery, if indicated.
In a prior study by Raghuraman and colleagues (1 of only 4 studies that met selection criteria of oxygen supplementation for patients in labor), newborns of patients not receiving oxygen demonstrated 95% confidence limits of umbilical artery pH (7.24–7.28) and BD (2.9–4.3) well within the normal range.6 Thus, the low prevalence of cases in which a benefit might be anticipated and the low incidence of severe acidosis challenges the design of prospective studies to detect statistically and clinically significant changes in blood gas measures and newborn outcomes.
The normal mild fetal acidosis that develops during labor is likely a result of recurrent interruption of uterine placental blood flow during uterine contractions7 and is unlikely to benefit from maternal hyperoxia. Similarly, as placental oxygen transfer is predominantly flow rather than diffusion limited,8 oxygen supplementation is unlikely to improve severe variable FHR decelerations. Thus, a randomized study of hyperoxia in unselected laboring patients is unlikely to have a measurable effect on clinically significant acidosis.
Oxygen transport pathway guides treatment
For the present, an understanding of oxygen transport can guide clinical oxygen use. Thus, mothers with relative hypoxemia will unquestionably benefit with supplemental oxygen administration. Similarly, fetuses at risk for placental dysfunction (for example, growth restriction, postterm) and particularly those manifesting evidence of impaired oxygen transport (that is, late decelerations) may be most likely to benefit from the increased O2 gradient. For patients with reduced maternal uterine perfusion (such as hypotension or hypovolemia), pressors and/or fluid volume are likely to be more effective, while amnioinfusion is of greater value for umbilical cord compression patterns. A reduction in uterine activity may be of benefit to all fetuses exhibiting compromise. Due to the modest impact on fetal oxygen content, maternal hyperoxia does not produce significant fetal oxidative stress as measured by fetal malondialdehyde levels.
In view of the lack of demonstrated adverse effects of maternal supplemental oxygen, clinicians should not hesitate to use it. However, clinicians should recognize that supplemental oxygen is likely to be of value only in patients with significant impairment in the oxygen pathway, and they should choose additional intrauterine resuscitative measures focused on the etiology.
MICHAEL G. ROSS, MD, MPH,
AND BRYAN S. RICHARDSON, MD
- McNanley T, Woods J. Placental physiology. Glob Libr Women’s Med. (ISSN: 1756-2228). 2008. doi: 10.3843 /GLOWM.10195.
- Richardson BS. Fetal adaptive responses to asphyxia. Clin Perinatol. 1989;16:595-611.
- Sameshima H, Ikenoue T. Predictive value of late decelerations of fetal acidemia in unselective low-risk pregnancies. Am J Perinatol. 2005;22:19-23.
- Yeh P, Emary K, Impey L. The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51,519 consecutive validated samples. BJOG. 2012;119:824-831.
- Kelly R, Ramaiah SM, Sheridan H, et al. Dose-dependent relationship between acidosis at birth and likelihood of death or cerebral palsy. Arch Dis Child Fetal Neonatal Ed. 2018;103:F567-F572.
- Raghuraman N, Wan L, Temming LA, et al. Effect of oxygen vs room air on intrauterine fetal resuscitation: a randomized noninferiority clinical trial. JAMA Pediatr. 2018;172:818-823.
- Ramsey EM, Corner JW Jr, Donner MW. Serial and cineradioangiographic visualization of maternal circulation in the primate (hemochorial) placenta. Am J Obstet Gynecol. 1963;86:213-225.
- Nye GA, Ingram E, Johnstone ED, et al. Human placental oxygenation in late gestation: experimental and theoretical approaches. J Physiol. 2018;596:5523-5534.
- McNanley T, Woods J. Placental physiology. Glob Libr Women’s Med. (ISSN: 1756-2228). 2008. doi: 10.3843 /GLOWM.10195.
- Richardson BS. Fetal adaptive responses to asphyxia. Clin Perinatol. 1989;16:595-611.
- Sameshima H, Ikenoue T. Predictive value of late decelerations of fetal acidemia in unselective low-risk pregnancies. Am J Perinatol. 2005;22:19-23.
- Yeh P, Emary K, Impey L. The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51,519 consecutive validated samples. BJOG. 2012;119:824-831.
- Kelly R, Ramaiah SM, Sheridan H, et al. Dose-dependent relationship between acidosis at birth and likelihood of death or cerebral palsy. Arch Dis Child Fetal Neonatal Ed. 2018;103:F567-F572.
- Raghuraman N, Wan L, Temming LA, et al. Effect of oxygen vs room air on intrauterine fetal resuscitation: a randomized noninferiority clinical trial. JAMA Pediatr. 2018;172:818-823.
- Ramsey EM, Corner JW Jr, Donner MW. Serial and cineradioangiographic visualization of maternal circulation in the primate (hemochorial) placenta. Am J Obstet Gynecol. 1963;86:213-225.
- Nye GA, Ingram E, Johnstone ED, et al. Human placental oxygenation in late gestation: experimental and theoretical approaches. J Physiol. 2018;596:5523-5534.