User login
Energy-based devices: Expert shares treatment tips for rosacea, scars
, according to a 2020 international consensus publication that Jeremy B. Green, MD, reviewed during a virtual course on laser and aesthetic skin therapy.
During his presentation, he also reviewed laser treatment of scars. “Erythema is an indicator of scar activity,” said Dr. Green, a dermatologist in Coral Gables, Fla. “So, with flat, red scars, vascular devices are the first choice. If you’re going to treat with multiple lasers in a single session, use the vascular laser first, followed by a resurfacing laser if needed. If you treat with a resurfacing laser first, you’ll cause erythema and edema and you’ll obscure that blood vessel target.”
The manuscript, which was created by a panel of 26 dermatologists and plastic and reconstructive surgeons from 13 different countries, also calls for using scar treatment settings that are lower than those used for port wine stains, with mild purpura as the clinical endpoint to strive for.
Vascular lasers are also the expert panel’s first choice when a scar is painful or pruritic, while the second choice is an ablative fractional laser with intralesional triamcinolone and/or 5-fluorouracil (5-FU). “If the scar is hypertrophic, I will combine a vascular laser, then a nonablative or an ablative fractional laser, then intralesional triamcinolone mixed with 5-FU,” said Dr. Green, who was not involved in drafting the recommendations.
As for the first treatment of choice, 80% of the experts chose a pulsed dye laser, while others chose the KTP laser, intense pulsed light (IPL) and the neodymium yttrium aluminum garnet (Nd:YAG) laser. With regard to settings, when using a PDL and a 10-mm spot size, 41% of experts recommend a fluence of 5-6 J/cm2, 27% recommend a fluence of 4-5 J/cm2, and 27% recommend a fluence of 6-7 J/cm2. Pertaining to pulse duration, 50% favor 1.5 milliseconds, 18% use 3 milliseconds, and 18% use .45 milliseconds.
As for timing post surgery, 70% report treating less than 1 week after surgery and 90% report treating within 1 month post surgery. “I prefer to treat about 1 week after sutures are removed so the skin is re-epithelialized,” Dr. Green said. “The bottom line is, with postsurgical, posttraumatic scars, once the skin is healed, the sooner you get at it, the better.”
Rosacea
He also discussed the microvascular effects of PDL in combination with oxymetazoline 1% cream, an alpha1A adrenoceptor agonist, which is approved by the Food and Drug Administration for treatment of persistent facial erythema associated with rosacea. “This has been a hot topic lately,” Dr. Green said. “When the studies were done for FDA approval, there was an observation that vasodilation occurs 5 minutes after application of oxymetazoline, so the venule diameter increases. Sixty minutes after application, vasoconstriction happens, which is the desired clinical effect for patients with facial erythema.”
In a mouse study, researchers led by Bernard Choi, PhD, and Kristin M. Kelly, MD, of the Beckman Laser Institute and Medical Clinic, University of California, Irvine, found that the combination protocol of oxymetazoline application, followed 5 minutes later by PDL, induced persistent vascular shutdown 7 days after irradiation. Vascular shutdown occurred in 67% of vessels treated with oxymetazoline plus PDL at day 7 vs. 17% in those treated with saline plus PDL.
“This is fascinating,” Dr. Green said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “There is no publication I’m aware of in humans that has explored this timing, but I have used oxymetazoline in my clinic in patients with stubborn erythema and treated them with the vascular laser 5 minutes later.”
In a separate open-label study of 46 patients with moderate to severe facial erythema associated with rosacea, researchers found that oxymetazoline 1% as adjunctive therapy with energy-based therapy was safe and well tolerated, and reduced facial erythema in patients with moderate to severe persistent facial erythema associated with rosacea. Energy sources used were the PDL, KTP, or IPL.
In a study presented during the 2020 American Society for Laser Medicine & Surgery meeting, researchers led by Pooja Sodha, MD, of George Washington University, Washington, conducted a pilot trial of PDL plus oxymetazoline 1% cream for erythematotelangiectatic rosacea. Between baseline and 6 months’ follow-up the Clinician’s Erythema Assessment score fell from 4 to 2.
“Of note, I would also throw the kitchen sink at these patients medically, meaning I love topical ivermectin 1% cream,” Dr. Green said. “In some cases I’ll even use oral ivermectin and an oral tetracycline class antibiotic.”
He reported having received research funding and/or consulting fees from numerous device and pharmaceutical companies.
, according to a 2020 international consensus publication that Jeremy B. Green, MD, reviewed during a virtual course on laser and aesthetic skin therapy.
During his presentation, he also reviewed laser treatment of scars. “Erythema is an indicator of scar activity,” said Dr. Green, a dermatologist in Coral Gables, Fla. “So, with flat, red scars, vascular devices are the first choice. If you’re going to treat with multiple lasers in a single session, use the vascular laser first, followed by a resurfacing laser if needed. If you treat with a resurfacing laser first, you’ll cause erythema and edema and you’ll obscure that blood vessel target.”
The manuscript, which was created by a panel of 26 dermatologists and plastic and reconstructive surgeons from 13 different countries, also calls for using scar treatment settings that are lower than those used for port wine stains, with mild purpura as the clinical endpoint to strive for.
Vascular lasers are also the expert panel’s first choice when a scar is painful or pruritic, while the second choice is an ablative fractional laser with intralesional triamcinolone and/or 5-fluorouracil (5-FU). “If the scar is hypertrophic, I will combine a vascular laser, then a nonablative or an ablative fractional laser, then intralesional triamcinolone mixed with 5-FU,” said Dr. Green, who was not involved in drafting the recommendations.
As for the first treatment of choice, 80% of the experts chose a pulsed dye laser, while others chose the KTP laser, intense pulsed light (IPL) and the neodymium yttrium aluminum garnet (Nd:YAG) laser. With regard to settings, when using a PDL and a 10-mm spot size, 41% of experts recommend a fluence of 5-6 J/cm2, 27% recommend a fluence of 4-5 J/cm2, and 27% recommend a fluence of 6-7 J/cm2. Pertaining to pulse duration, 50% favor 1.5 milliseconds, 18% use 3 milliseconds, and 18% use .45 milliseconds.
As for timing post surgery, 70% report treating less than 1 week after surgery and 90% report treating within 1 month post surgery. “I prefer to treat about 1 week after sutures are removed so the skin is re-epithelialized,” Dr. Green said. “The bottom line is, with postsurgical, posttraumatic scars, once the skin is healed, the sooner you get at it, the better.”
Rosacea
He also discussed the microvascular effects of PDL in combination with oxymetazoline 1% cream, an alpha1A adrenoceptor agonist, which is approved by the Food and Drug Administration for treatment of persistent facial erythema associated with rosacea. “This has been a hot topic lately,” Dr. Green said. “When the studies were done for FDA approval, there was an observation that vasodilation occurs 5 minutes after application of oxymetazoline, so the venule diameter increases. Sixty minutes after application, vasoconstriction happens, which is the desired clinical effect for patients with facial erythema.”
In a mouse study, researchers led by Bernard Choi, PhD, and Kristin M. Kelly, MD, of the Beckman Laser Institute and Medical Clinic, University of California, Irvine, found that the combination protocol of oxymetazoline application, followed 5 minutes later by PDL, induced persistent vascular shutdown 7 days after irradiation. Vascular shutdown occurred in 67% of vessels treated with oxymetazoline plus PDL at day 7 vs. 17% in those treated with saline plus PDL.
“This is fascinating,” Dr. Green said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “There is no publication I’m aware of in humans that has explored this timing, but I have used oxymetazoline in my clinic in patients with stubborn erythema and treated them with the vascular laser 5 minutes later.”
In a separate open-label study of 46 patients with moderate to severe facial erythema associated with rosacea, researchers found that oxymetazoline 1% as adjunctive therapy with energy-based therapy was safe and well tolerated, and reduced facial erythema in patients with moderate to severe persistent facial erythema associated with rosacea. Energy sources used were the PDL, KTP, or IPL.
In a study presented during the 2020 American Society for Laser Medicine & Surgery meeting, researchers led by Pooja Sodha, MD, of George Washington University, Washington, conducted a pilot trial of PDL plus oxymetazoline 1% cream for erythematotelangiectatic rosacea. Between baseline and 6 months’ follow-up the Clinician’s Erythema Assessment score fell from 4 to 2.
“Of note, I would also throw the kitchen sink at these patients medically, meaning I love topical ivermectin 1% cream,” Dr. Green said. “In some cases I’ll even use oral ivermectin and an oral tetracycline class antibiotic.”
He reported having received research funding and/or consulting fees from numerous device and pharmaceutical companies.
, according to a 2020 international consensus publication that Jeremy B. Green, MD, reviewed during a virtual course on laser and aesthetic skin therapy.
During his presentation, he also reviewed laser treatment of scars. “Erythema is an indicator of scar activity,” said Dr. Green, a dermatologist in Coral Gables, Fla. “So, with flat, red scars, vascular devices are the first choice. If you’re going to treat with multiple lasers in a single session, use the vascular laser first, followed by a resurfacing laser if needed. If you treat with a resurfacing laser first, you’ll cause erythema and edema and you’ll obscure that blood vessel target.”
The manuscript, which was created by a panel of 26 dermatologists and plastic and reconstructive surgeons from 13 different countries, also calls for using scar treatment settings that are lower than those used for port wine stains, with mild purpura as the clinical endpoint to strive for.
Vascular lasers are also the expert panel’s first choice when a scar is painful or pruritic, while the second choice is an ablative fractional laser with intralesional triamcinolone and/or 5-fluorouracil (5-FU). “If the scar is hypertrophic, I will combine a vascular laser, then a nonablative or an ablative fractional laser, then intralesional triamcinolone mixed with 5-FU,” said Dr. Green, who was not involved in drafting the recommendations.
As for the first treatment of choice, 80% of the experts chose a pulsed dye laser, while others chose the KTP laser, intense pulsed light (IPL) and the neodymium yttrium aluminum garnet (Nd:YAG) laser. With regard to settings, when using a PDL and a 10-mm spot size, 41% of experts recommend a fluence of 5-6 J/cm2, 27% recommend a fluence of 4-5 J/cm2, and 27% recommend a fluence of 6-7 J/cm2. Pertaining to pulse duration, 50% favor 1.5 milliseconds, 18% use 3 milliseconds, and 18% use .45 milliseconds.
As for timing post surgery, 70% report treating less than 1 week after surgery and 90% report treating within 1 month post surgery. “I prefer to treat about 1 week after sutures are removed so the skin is re-epithelialized,” Dr. Green said. “The bottom line is, with postsurgical, posttraumatic scars, once the skin is healed, the sooner you get at it, the better.”
Rosacea
He also discussed the microvascular effects of PDL in combination with oxymetazoline 1% cream, an alpha1A adrenoceptor agonist, which is approved by the Food and Drug Administration for treatment of persistent facial erythema associated with rosacea. “This has been a hot topic lately,” Dr. Green said. “When the studies were done for FDA approval, there was an observation that vasodilation occurs 5 minutes after application of oxymetazoline, so the venule diameter increases. Sixty minutes after application, vasoconstriction happens, which is the desired clinical effect for patients with facial erythema.”
In a mouse study, researchers led by Bernard Choi, PhD, and Kristin M. Kelly, MD, of the Beckman Laser Institute and Medical Clinic, University of California, Irvine, found that the combination protocol of oxymetazoline application, followed 5 minutes later by PDL, induced persistent vascular shutdown 7 days after irradiation. Vascular shutdown occurred in 67% of vessels treated with oxymetazoline plus PDL at day 7 vs. 17% in those treated with saline plus PDL.
“This is fascinating,” Dr. Green said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “There is no publication I’m aware of in humans that has explored this timing, but I have used oxymetazoline in my clinic in patients with stubborn erythema and treated them with the vascular laser 5 minutes later.”
In a separate open-label study of 46 patients with moderate to severe facial erythema associated with rosacea, researchers found that oxymetazoline 1% as adjunctive therapy with energy-based therapy was safe and well tolerated, and reduced facial erythema in patients with moderate to severe persistent facial erythema associated with rosacea. Energy sources used were the PDL, KTP, or IPL.
In a study presented during the 2020 American Society for Laser Medicine & Surgery meeting, researchers led by Pooja Sodha, MD, of George Washington University, Washington, conducted a pilot trial of PDL plus oxymetazoline 1% cream for erythematotelangiectatic rosacea. Between baseline and 6 months’ follow-up the Clinician’s Erythema Assessment score fell from 4 to 2.
“Of note, I would also throw the kitchen sink at these patients medically, meaning I love topical ivermectin 1% cream,” Dr. Green said. “In some cases I’ll even use oral ivermectin and an oral tetracycline class antibiotic.”
He reported having received research funding and/or consulting fees from numerous device and pharmaceutical companies.
EXPERT ANALYSIS FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Sleep apnea and cognitive impairment are common bedfellows
“The study shows obstructive sleep apnea is common in patients with cognitive impairment. The results suggest that people with cognitive impairment should be assessed for sleep apnea if they have difficulty with sleep or if they demonstrate sleep-related symptoms,” said study investigator David Colelli, MSc, research coordinator at Sunnybrook Health Sciences Centre in Toronto.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology..
Linked to cognitive impairment
OSA is a common sleep disorder and is associated with an increased risk of developing cognitive impairment. It is also prevalent in the general population, but even more common among patients with dementia.
However, the investigators noted, the frequency and predictors of OSA have not been well established in Alzheimer’s disease and other related conditions such as vascular dementia.
The investigators had conducted a previous feasibility study investigating a home sleep monitor as an OSA screening tool. The current research examined potential correlations between OSA detected by this monitor and cognitive impairment.
The study included 67 patients with cognitive impairment due to neurodegenerative or vascular disease. The range of disorders included Alzheimer’s disease, mild cognitive impairment caused by Alzheimer’s disease, dementia caused by Parkinson’s or Lewy body disease, and vascular conditions.
Participants had a mean age of 72.8 years and 44.8% were male. The mean body mass index (BMI) was 25.6 kg/m2.
These participants completed a home sleep apnea test, which is an alternative to polysomnography for the detection of OSA.
Researchers identified OSA in 52.2% of the study population. This, Mr. Colelli said, “is in the range” of other research investigating sleep and cognitive impairment.
“In the general population, however, this number is a lot lower – in the 10%-20% range depending on the population or country you’re looking at,” Mr. Colelli said.
He emphasized that, without an objective sleep test, some patients may be unaware of their sleep issues. Those with cognitive impairment may “misjudge how they’re sleeping,” especially if they sleep without a partner, so it’s possible that sleep disorder symptoms often go undetected.
Bidirectional relationship?
Participants answered questionnaires on sleep, cognition, and mood. They also completed the 30-point Montreal Cognitive Assessment (MoCA) to assess language, visuospatial abilities, memory and recall, and abstract thinking.
Scores on this test range from 0 to 30, with a score of 26 or higher signifying normal, 18-25 indicating mild cognitive impairment, and 17 or lower indicating moderate to severe cognitive impairment. The average score for study participants with OSA was 20.5, compared with 23.6 for those without the sleep disorder.
Results showed OSA was significantly associated with a lower score on the MoCA scale (odds ratio, 0.40; P = .048). “This demonstrated an association of OSA with lower cognitive scores,” Mr. Colelli said.
The analysis also showed that OSA severity was correlated with actigraphy-derived sleep variables, including lower total sleep time, greater sleep onset latency, lower sleep efficiency, and more awakenings.
The study was too small to determine whether a specific diagnosis of cognitive impairment affected the link to OSA, Mr. Colelli said. “But definitely future research should be directed towards looking at this.”
Obesity is a risk factor for OSA, but the mean BMI in the study was not in the obese range of 30 and over. This, Mr. Colelli said, suggests that sleep apnea may present differently in those with cognitive impairment.
“Sleep apnea in this population might not present with the typical risk factors of obesity or snoring or feeling tired.”
While the new study “adds to the understanding that there’s a link between sleep and cognitive impairment, the direction of that link isn’t entirely clear,” Mr. Colelli said.
“It’s slowly becoming appreciated that the relationship might be bidirectionality, where sleep apnea might be contributing to the cognitive impairment and cognitive impairment could be contributing to the sleep issues.”
The study highlights how essential sleep is to mental health, Mr. Colelli said. “I feel, and I’m sure you do too, that if you don’t get good sleep, you feel tired during the day and you may not have the best concentration or memory.”
Identifying sleep issues in patients with cognitive impairment is important, as treatment and management of these issues could affect outcomes including cognition and quality of life, he added.
“Future research should be directed to see if treatment of sleep disorders with continuous positive airway pressure (CPAP), which is the gold standard, and various other treatments, can improve outcomes.” Future research should also examine OSA prevalence in larger cohorts.
Common, undertreated
Commenting on the resaerch, Lei Gao, MD, assistant professor of anesthesia at Harvard Medical School, Boston, whose areas of expertise include disorders of cognition, sleep, and circadian rhythm, believes the findings are important. “It highlights how common and potentially undertreated OSA is in this age group, and in particular, its link to cognitive impairment.”
OSA is often associated with significant comorbidities, as well as sleep disruption, Dr. Gao noted. One of the study’s strengths was including objective assessment of sleep using actigraphy. “It will be interesting to see to what extent the OSA link to cognitive impairment is via poor sleep or disrupted circadian rest/activity cycles.”
It would also be interesting “to tease out whether OSA is more linked to dementia of vascular etiologies due to common risk factors, or whether it is pervasive to all forms of dementia,” he added.
A version of this article first appeared on Medscape.com.
“The study shows obstructive sleep apnea is common in patients with cognitive impairment. The results suggest that people with cognitive impairment should be assessed for sleep apnea if they have difficulty with sleep or if they demonstrate sleep-related symptoms,” said study investigator David Colelli, MSc, research coordinator at Sunnybrook Health Sciences Centre in Toronto.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology..
Linked to cognitive impairment
OSA is a common sleep disorder and is associated with an increased risk of developing cognitive impairment. It is also prevalent in the general population, but even more common among patients with dementia.
However, the investigators noted, the frequency and predictors of OSA have not been well established in Alzheimer’s disease and other related conditions such as vascular dementia.
The investigators had conducted a previous feasibility study investigating a home sleep monitor as an OSA screening tool. The current research examined potential correlations between OSA detected by this monitor and cognitive impairment.
The study included 67 patients with cognitive impairment due to neurodegenerative or vascular disease. The range of disorders included Alzheimer’s disease, mild cognitive impairment caused by Alzheimer’s disease, dementia caused by Parkinson’s or Lewy body disease, and vascular conditions.
Participants had a mean age of 72.8 years and 44.8% were male. The mean body mass index (BMI) was 25.6 kg/m2.
These participants completed a home sleep apnea test, which is an alternative to polysomnography for the detection of OSA.
Researchers identified OSA in 52.2% of the study population. This, Mr. Colelli said, “is in the range” of other research investigating sleep and cognitive impairment.
“In the general population, however, this number is a lot lower – in the 10%-20% range depending on the population or country you’re looking at,” Mr. Colelli said.
He emphasized that, without an objective sleep test, some patients may be unaware of their sleep issues. Those with cognitive impairment may “misjudge how they’re sleeping,” especially if they sleep without a partner, so it’s possible that sleep disorder symptoms often go undetected.
Bidirectional relationship?
Participants answered questionnaires on sleep, cognition, and mood. They also completed the 30-point Montreal Cognitive Assessment (MoCA) to assess language, visuospatial abilities, memory and recall, and abstract thinking.
Scores on this test range from 0 to 30, with a score of 26 or higher signifying normal, 18-25 indicating mild cognitive impairment, and 17 or lower indicating moderate to severe cognitive impairment. The average score for study participants with OSA was 20.5, compared with 23.6 for those without the sleep disorder.
Results showed OSA was significantly associated with a lower score on the MoCA scale (odds ratio, 0.40; P = .048). “This demonstrated an association of OSA with lower cognitive scores,” Mr. Colelli said.
The analysis also showed that OSA severity was correlated with actigraphy-derived sleep variables, including lower total sleep time, greater sleep onset latency, lower sleep efficiency, and more awakenings.
The study was too small to determine whether a specific diagnosis of cognitive impairment affected the link to OSA, Mr. Colelli said. “But definitely future research should be directed towards looking at this.”
Obesity is a risk factor for OSA, but the mean BMI in the study was not in the obese range of 30 and over. This, Mr. Colelli said, suggests that sleep apnea may present differently in those with cognitive impairment.
“Sleep apnea in this population might not present with the typical risk factors of obesity or snoring or feeling tired.”
While the new study “adds to the understanding that there’s a link between sleep and cognitive impairment, the direction of that link isn’t entirely clear,” Mr. Colelli said.
“It’s slowly becoming appreciated that the relationship might be bidirectionality, where sleep apnea might be contributing to the cognitive impairment and cognitive impairment could be contributing to the sleep issues.”
The study highlights how essential sleep is to mental health, Mr. Colelli said. “I feel, and I’m sure you do too, that if you don’t get good sleep, you feel tired during the day and you may not have the best concentration or memory.”
Identifying sleep issues in patients with cognitive impairment is important, as treatment and management of these issues could affect outcomes including cognition and quality of life, he added.
“Future research should be directed to see if treatment of sleep disorders with continuous positive airway pressure (CPAP), which is the gold standard, and various other treatments, can improve outcomes.” Future research should also examine OSA prevalence in larger cohorts.
Common, undertreated
Commenting on the resaerch, Lei Gao, MD, assistant professor of anesthesia at Harvard Medical School, Boston, whose areas of expertise include disorders of cognition, sleep, and circadian rhythm, believes the findings are important. “It highlights how common and potentially undertreated OSA is in this age group, and in particular, its link to cognitive impairment.”
OSA is often associated with significant comorbidities, as well as sleep disruption, Dr. Gao noted. One of the study’s strengths was including objective assessment of sleep using actigraphy. “It will be interesting to see to what extent the OSA link to cognitive impairment is via poor sleep or disrupted circadian rest/activity cycles.”
It would also be interesting “to tease out whether OSA is more linked to dementia of vascular etiologies due to common risk factors, or whether it is pervasive to all forms of dementia,” he added.
A version of this article first appeared on Medscape.com.
“The study shows obstructive sleep apnea is common in patients with cognitive impairment. The results suggest that people with cognitive impairment should be assessed for sleep apnea if they have difficulty with sleep or if they demonstrate sleep-related symptoms,” said study investigator David Colelli, MSc, research coordinator at Sunnybrook Health Sciences Centre in Toronto.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology..
Linked to cognitive impairment
OSA is a common sleep disorder and is associated with an increased risk of developing cognitive impairment. It is also prevalent in the general population, but even more common among patients with dementia.
However, the investigators noted, the frequency and predictors of OSA have not been well established in Alzheimer’s disease and other related conditions such as vascular dementia.
The investigators had conducted a previous feasibility study investigating a home sleep monitor as an OSA screening tool. The current research examined potential correlations between OSA detected by this monitor and cognitive impairment.
The study included 67 patients with cognitive impairment due to neurodegenerative or vascular disease. The range of disorders included Alzheimer’s disease, mild cognitive impairment caused by Alzheimer’s disease, dementia caused by Parkinson’s or Lewy body disease, and vascular conditions.
Participants had a mean age of 72.8 years and 44.8% were male. The mean body mass index (BMI) was 25.6 kg/m2.
These participants completed a home sleep apnea test, which is an alternative to polysomnography for the detection of OSA.
Researchers identified OSA in 52.2% of the study population. This, Mr. Colelli said, “is in the range” of other research investigating sleep and cognitive impairment.
“In the general population, however, this number is a lot lower – in the 10%-20% range depending on the population or country you’re looking at,” Mr. Colelli said.
He emphasized that, without an objective sleep test, some patients may be unaware of their sleep issues. Those with cognitive impairment may “misjudge how they’re sleeping,” especially if they sleep without a partner, so it’s possible that sleep disorder symptoms often go undetected.
Bidirectional relationship?
Participants answered questionnaires on sleep, cognition, and mood. They also completed the 30-point Montreal Cognitive Assessment (MoCA) to assess language, visuospatial abilities, memory and recall, and abstract thinking.
Scores on this test range from 0 to 30, with a score of 26 or higher signifying normal, 18-25 indicating mild cognitive impairment, and 17 or lower indicating moderate to severe cognitive impairment. The average score for study participants with OSA was 20.5, compared with 23.6 for those without the sleep disorder.
Results showed OSA was significantly associated with a lower score on the MoCA scale (odds ratio, 0.40; P = .048). “This demonstrated an association of OSA with lower cognitive scores,” Mr. Colelli said.
The analysis also showed that OSA severity was correlated with actigraphy-derived sleep variables, including lower total sleep time, greater sleep onset latency, lower sleep efficiency, and more awakenings.
The study was too small to determine whether a specific diagnosis of cognitive impairment affected the link to OSA, Mr. Colelli said. “But definitely future research should be directed towards looking at this.”
Obesity is a risk factor for OSA, but the mean BMI in the study was not in the obese range of 30 and over. This, Mr. Colelli said, suggests that sleep apnea may present differently in those with cognitive impairment.
“Sleep apnea in this population might not present with the typical risk factors of obesity or snoring or feeling tired.”
While the new study “adds to the understanding that there’s a link between sleep and cognitive impairment, the direction of that link isn’t entirely clear,” Mr. Colelli said.
“It’s slowly becoming appreciated that the relationship might be bidirectionality, where sleep apnea might be contributing to the cognitive impairment and cognitive impairment could be contributing to the sleep issues.”
The study highlights how essential sleep is to mental health, Mr. Colelli said. “I feel, and I’m sure you do too, that if you don’t get good sleep, you feel tired during the day and you may not have the best concentration or memory.”
Identifying sleep issues in patients with cognitive impairment is important, as treatment and management of these issues could affect outcomes including cognition and quality of life, he added.
“Future research should be directed to see if treatment of sleep disorders with continuous positive airway pressure (CPAP), which is the gold standard, and various other treatments, can improve outcomes.” Future research should also examine OSA prevalence in larger cohorts.
Common, undertreated
Commenting on the resaerch, Lei Gao, MD, assistant professor of anesthesia at Harvard Medical School, Boston, whose areas of expertise include disorders of cognition, sleep, and circadian rhythm, believes the findings are important. “It highlights how common and potentially undertreated OSA is in this age group, and in particular, its link to cognitive impairment.”
OSA is often associated with significant comorbidities, as well as sleep disruption, Dr. Gao noted. One of the study’s strengths was including objective assessment of sleep using actigraphy. “It will be interesting to see to what extent the OSA link to cognitive impairment is via poor sleep or disrupted circadian rest/activity cycles.”
It would also be interesting “to tease out whether OSA is more linked to dementia of vascular etiologies due to common risk factors, or whether it is pervasive to all forms of dementia,” he added.
A version of this article first appeared on Medscape.com.
FROM AAN 2021
JAMA podcast on racism in medicine faces backlash
Published on Feb. 23, the episode is hosted on JAMA’s learning platform for doctors and is available for continuing medical education credits.
“No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast,” JAMA wrote in a Twitter post to promote the episode. That tweet has since been deleted.

The episode features host Ed Livingston, MD, deputy editor for clinical reviews and education at JAMA, and guest Mitchell Katz, MD, president and CEO for NYC Health + Hospitals and deputy editor for JAMA Internal Medicine. Dr. Livingston approaches the episode as “structural racism for skeptics,” and Dr. Katz tries to explain how structural racism deepens health disparities and what health systems can do about it.
“Many physicians are skeptical of structural racism, the idea that economic, educational, and other societal systems preferentially disadvantage Black Americans and other communities of color,” the episode description says.
In the podcast, Dr. Livingston and Dr. Katz speak about health care disparities and racial inequality. Dr. Livingston, who says he “didn’t understand the concept” going into the episode, suggests that racism was made illegal in the 1960s and that the discussion of “structural racism” should shift away from the term “racism” and focus on socioeconomic status instead.
“What you’re talking about isn’t so much racism ... it isn’t their race, it isn’t their color, it’s their socioeconomic status,” Dr. Livingston says. “Is that a fair statement?”
But Dr. Katz says that “acknowledging structural racism can be helpful to us. Structural racism refers to a system in which policies or practices or how we look at people perpetuates racial inequality.”
Dr. Katz points to the creation of a hospital in San Francisco in the 1880s to treat patients of Chinese ethnicity separately. Outside of health care, he talks about environmental racism between neighborhoods with inequalities in hospitals, schools, and social services.
“All of those things have an impact on that minority person,” Dr. Katz says. “The big thing we can all do is move away from trying to interrogate each other’s opinions and move to a place where we are looking at the policies of our institutions and making sure that they promote equality.”
Dr. Livingston concludes the episode by reemphasizing that “racism” should be taken out of the conversation and it should instead focus on the “structural” aspect of socioeconomics.
“Minorities ... aren’t [in those neighborhoods] because they’re not allowed to buy houses or they can’t get a job because they’re Black or Hispanic. That would be illegal,” Dr. Livingston says. “But disproportionality does exist.”
Efforts to reach Dr. Livingston were unsuccessful. Dr. Katz distanced himself from Dr. Livingston in a statement released on March 4.
“Systemic and interpersonal racism both still exist in our country — they must be rooted out. I do not share the JAMA host’s belief of doing away with the word ‘racism’ will help us be more successful in ending inequities that exists across racial and ethnic lines,” Dr. Katz said. “Further, I believe that we will only produce an equitable society when social and political structures do not continue to produce and perpetuate disparate results based on social race and ethnicity.”
Dr. Katz reiterated that both interpersonal and structural racism continue to exist in the United States, “and it is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it.”
He also recommended JAMA use this controversy “as a learning opportunity for continued dialogue and create another podcast series as an open conversation that invites diverse experts in the field to have an open discussion about structural racism in healthcare.”
The podcast and JAMA’s tweet promoting it were widely criticized on Twitter. In interviews with WebMD, many doctors expressed disbelief that such a respected journal would lend its name to this podcast episode.
B. Bobby Chiong, MD, a radiologist in New York, said although JAMA’s effort to engage with its audience about racism is laudable, it missed the mark.
“I think the backlash comes from how they tried to make a podcast about the subject and somehow made themselves an example of unconscious bias and unfamiliarity with just how embedded in our system is structural racism,” he said.
Perhaps the podcast’s worst offense was its failure to address the painful history of racial bias in this country that still permeates the medical community, says Tamara Saint-Surin, MD, assistant professor at the University of North Carolina at Chapel Hill.
“For physicians in leadership to have the belief that structural racism does not exist in medicine, they don’t really appreciate what affects their patients and what their patients were dealing with,” Dr. Saint-Surin said in an interview. “It was a very harmful podcast and goes to show we still have so much work to do.”
Along with a flawed premise, she says, the podcast was not nearly long enough to address such a nuanced issue. And Dr. Livingston focused on interpersonal racism rather than structural racism, she said, failing to address widespread problems such as higher rates of asthma among Black populations living in areas with poor air quality.
The number of Black doctors remains low and the lack of representation adds to an environment already rife with racism, according to many medical professionals.
Shirlene Obuobi, MD, an internal medicine doctor in Chicago, said JAMA failed to live up to its own standards by publishing material that lacked research and expertise.
“I can’t submit a clinical trial to JAMA without them combing through methods with a fine-tooth comb,” Dr. Obuobi said. “They didn’t uphold the standards they normally apply to anyone else.”
Both the editor of JAMA and the head of the American Medical Association issued statements criticizing the episode and the tweet that promoted it.
JAMA Editor-in-Chief Howard Bauchner, MD, said, “The language of the tweet, and some portions of the podcast, do not reflect my commitment as editorial leader of JAMA and JAMA Network to call out and discuss the adverse effects of injustice, inequity, and racism in society and medicine as JAMA has done for many years.” He said JAMA will schedule a future podcast to address the concerns raised about the recent episode.
AMA CEO James L. Madara, MD, said, “The AMA’s House of Delegates passed policy stating that racism is structural, systemic, cultural, and interpersonal, and we are deeply disturbed – and angered – by a recent JAMA podcast that questioned the existence of structural racism and the affiliated tweet that promoted the podcast and stated ‘no physician is racist, so how can there be structural racism in health care?’ ”
He continued: “JAMA has editorial independence from AMA, but this tweet and podcast are inconsistent with the policies and views of AMA, and I’m concerned about and acknowledge the harms they have caused. Structural racism in health care and our society exists, and it is incumbent on all of us to fix it.”
This article was updated 3/5/21.
A version of this article first appeared on WebMD.com.
Published on Feb. 23, the episode is hosted on JAMA’s learning platform for doctors and is available for continuing medical education credits.
“No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast,” JAMA wrote in a Twitter post to promote the episode. That tweet has since been deleted.

The episode features host Ed Livingston, MD, deputy editor for clinical reviews and education at JAMA, and guest Mitchell Katz, MD, president and CEO for NYC Health + Hospitals and deputy editor for JAMA Internal Medicine. Dr. Livingston approaches the episode as “structural racism for skeptics,” and Dr. Katz tries to explain how structural racism deepens health disparities and what health systems can do about it.
“Many physicians are skeptical of structural racism, the idea that economic, educational, and other societal systems preferentially disadvantage Black Americans and other communities of color,” the episode description says.
In the podcast, Dr. Livingston and Dr. Katz speak about health care disparities and racial inequality. Dr. Livingston, who says he “didn’t understand the concept” going into the episode, suggests that racism was made illegal in the 1960s and that the discussion of “structural racism” should shift away from the term “racism” and focus on socioeconomic status instead.
“What you’re talking about isn’t so much racism ... it isn’t their race, it isn’t their color, it’s their socioeconomic status,” Dr. Livingston says. “Is that a fair statement?”
But Dr. Katz says that “acknowledging structural racism can be helpful to us. Structural racism refers to a system in which policies or practices or how we look at people perpetuates racial inequality.”
Dr. Katz points to the creation of a hospital in San Francisco in the 1880s to treat patients of Chinese ethnicity separately. Outside of health care, he talks about environmental racism between neighborhoods with inequalities in hospitals, schools, and social services.
“All of those things have an impact on that minority person,” Dr. Katz says. “The big thing we can all do is move away from trying to interrogate each other’s opinions and move to a place where we are looking at the policies of our institutions and making sure that they promote equality.”
Dr. Livingston concludes the episode by reemphasizing that “racism” should be taken out of the conversation and it should instead focus on the “structural” aspect of socioeconomics.
“Minorities ... aren’t [in those neighborhoods] because they’re not allowed to buy houses or they can’t get a job because they’re Black or Hispanic. That would be illegal,” Dr. Livingston says. “But disproportionality does exist.”
Efforts to reach Dr. Livingston were unsuccessful. Dr. Katz distanced himself from Dr. Livingston in a statement released on March 4.
“Systemic and interpersonal racism both still exist in our country — they must be rooted out. I do not share the JAMA host’s belief of doing away with the word ‘racism’ will help us be more successful in ending inequities that exists across racial and ethnic lines,” Dr. Katz said. “Further, I believe that we will only produce an equitable society when social and political structures do not continue to produce and perpetuate disparate results based on social race and ethnicity.”
Dr. Katz reiterated that both interpersonal and structural racism continue to exist in the United States, “and it is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it.”
He also recommended JAMA use this controversy “as a learning opportunity for continued dialogue and create another podcast series as an open conversation that invites diverse experts in the field to have an open discussion about structural racism in healthcare.”
The podcast and JAMA’s tweet promoting it were widely criticized on Twitter. In interviews with WebMD, many doctors expressed disbelief that such a respected journal would lend its name to this podcast episode.
B. Bobby Chiong, MD, a radiologist in New York, said although JAMA’s effort to engage with its audience about racism is laudable, it missed the mark.
“I think the backlash comes from how they tried to make a podcast about the subject and somehow made themselves an example of unconscious bias and unfamiliarity with just how embedded in our system is structural racism,” he said.
Perhaps the podcast’s worst offense was its failure to address the painful history of racial bias in this country that still permeates the medical community, says Tamara Saint-Surin, MD, assistant professor at the University of North Carolina at Chapel Hill.
“For physicians in leadership to have the belief that structural racism does not exist in medicine, they don’t really appreciate what affects their patients and what their patients were dealing with,” Dr. Saint-Surin said in an interview. “It was a very harmful podcast and goes to show we still have so much work to do.”
Along with a flawed premise, she says, the podcast was not nearly long enough to address such a nuanced issue. And Dr. Livingston focused on interpersonal racism rather than structural racism, she said, failing to address widespread problems such as higher rates of asthma among Black populations living in areas with poor air quality.
The number of Black doctors remains low and the lack of representation adds to an environment already rife with racism, according to many medical professionals.
Shirlene Obuobi, MD, an internal medicine doctor in Chicago, said JAMA failed to live up to its own standards by publishing material that lacked research and expertise.
“I can’t submit a clinical trial to JAMA without them combing through methods with a fine-tooth comb,” Dr. Obuobi said. “They didn’t uphold the standards they normally apply to anyone else.”
Both the editor of JAMA and the head of the American Medical Association issued statements criticizing the episode and the tweet that promoted it.
JAMA Editor-in-Chief Howard Bauchner, MD, said, “The language of the tweet, and some portions of the podcast, do not reflect my commitment as editorial leader of JAMA and JAMA Network to call out and discuss the adverse effects of injustice, inequity, and racism in society and medicine as JAMA has done for many years.” He said JAMA will schedule a future podcast to address the concerns raised about the recent episode.
AMA CEO James L. Madara, MD, said, “The AMA’s House of Delegates passed policy stating that racism is structural, systemic, cultural, and interpersonal, and we are deeply disturbed – and angered – by a recent JAMA podcast that questioned the existence of structural racism and the affiliated tweet that promoted the podcast and stated ‘no physician is racist, so how can there be structural racism in health care?’ ”
He continued: “JAMA has editorial independence from AMA, but this tweet and podcast are inconsistent with the policies and views of AMA, and I’m concerned about and acknowledge the harms they have caused. Structural racism in health care and our society exists, and it is incumbent on all of us to fix it.”
This article was updated 3/5/21.
A version of this article first appeared on WebMD.com.
Published on Feb. 23, the episode is hosted on JAMA’s learning platform for doctors and is available for continuing medical education credits.
“No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast,” JAMA wrote in a Twitter post to promote the episode. That tweet has since been deleted.

The episode features host Ed Livingston, MD, deputy editor for clinical reviews and education at JAMA, and guest Mitchell Katz, MD, president and CEO for NYC Health + Hospitals and deputy editor for JAMA Internal Medicine. Dr. Livingston approaches the episode as “structural racism for skeptics,” and Dr. Katz tries to explain how structural racism deepens health disparities and what health systems can do about it.
“Many physicians are skeptical of structural racism, the idea that economic, educational, and other societal systems preferentially disadvantage Black Americans and other communities of color,” the episode description says.
In the podcast, Dr. Livingston and Dr. Katz speak about health care disparities and racial inequality. Dr. Livingston, who says he “didn’t understand the concept” going into the episode, suggests that racism was made illegal in the 1960s and that the discussion of “structural racism” should shift away from the term “racism” and focus on socioeconomic status instead.
“What you’re talking about isn’t so much racism ... it isn’t their race, it isn’t their color, it’s their socioeconomic status,” Dr. Livingston says. “Is that a fair statement?”
But Dr. Katz says that “acknowledging structural racism can be helpful to us. Structural racism refers to a system in which policies or practices or how we look at people perpetuates racial inequality.”
Dr. Katz points to the creation of a hospital in San Francisco in the 1880s to treat patients of Chinese ethnicity separately. Outside of health care, he talks about environmental racism between neighborhoods with inequalities in hospitals, schools, and social services.
“All of those things have an impact on that minority person,” Dr. Katz says. “The big thing we can all do is move away from trying to interrogate each other’s opinions and move to a place where we are looking at the policies of our institutions and making sure that they promote equality.”
Dr. Livingston concludes the episode by reemphasizing that “racism” should be taken out of the conversation and it should instead focus on the “structural” aspect of socioeconomics.
“Minorities ... aren’t [in those neighborhoods] because they’re not allowed to buy houses or they can’t get a job because they’re Black or Hispanic. That would be illegal,” Dr. Livingston says. “But disproportionality does exist.”
Efforts to reach Dr. Livingston were unsuccessful. Dr. Katz distanced himself from Dr. Livingston in a statement released on March 4.
“Systemic and interpersonal racism both still exist in our country — they must be rooted out. I do not share the JAMA host’s belief of doing away with the word ‘racism’ will help us be more successful in ending inequities that exists across racial and ethnic lines,” Dr. Katz said. “Further, I believe that we will only produce an equitable society when social and political structures do not continue to produce and perpetuate disparate results based on social race and ethnicity.”
Dr. Katz reiterated that both interpersonal and structural racism continue to exist in the United States, “and it is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it.”
He also recommended JAMA use this controversy “as a learning opportunity for continued dialogue and create another podcast series as an open conversation that invites diverse experts in the field to have an open discussion about structural racism in healthcare.”
The podcast and JAMA’s tweet promoting it were widely criticized on Twitter. In interviews with WebMD, many doctors expressed disbelief that such a respected journal would lend its name to this podcast episode.
B. Bobby Chiong, MD, a radiologist in New York, said although JAMA’s effort to engage with its audience about racism is laudable, it missed the mark.
“I think the backlash comes from how they tried to make a podcast about the subject and somehow made themselves an example of unconscious bias and unfamiliarity with just how embedded in our system is structural racism,” he said.
Perhaps the podcast’s worst offense was its failure to address the painful history of racial bias in this country that still permeates the medical community, says Tamara Saint-Surin, MD, assistant professor at the University of North Carolina at Chapel Hill.
“For physicians in leadership to have the belief that structural racism does not exist in medicine, they don’t really appreciate what affects their patients and what their patients were dealing with,” Dr. Saint-Surin said in an interview. “It was a very harmful podcast and goes to show we still have so much work to do.”
Along with a flawed premise, she says, the podcast was not nearly long enough to address such a nuanced issue. And Dr. Livingston focused on interpersonal racism rather than structural racism, she said, failing to address widespread problems such as higher rates of asthma among Black populations living in areas with poor air quality.
The number of Black doctors remains low and the lack of representation adds to an environment already rife with racism, according to many medical professionals.
Shirlene Obuobi, MD, an internal medicine doctor in Chicago, said JAMA failed to live up to its own standards by publishing material that lacked research and expertise.
“I can’t submit a clinical trial to JAMA without them combing through methods with a fine-tooth comb,” Dr. Obuobi said. “They didn’t uphold the standards they normally apply to anyone else.”
Both the editor of JAMA and the head of the American Medical Association issued statements criticizing the episode and the tweet that promoted it.
JAMA Editor-in-Chief Howard Bauchner, MD, said, “The language of the tweet, and some portions of the podcast, do not reflect my commitment as editorial leader of JAMA and JAMA Network to call out and discuss the adverse effects of injustice, inequity, and racism in society and medicine as JAMA has done for many years.” He said JAMA will schedule a future podcast to address the concerns raised about the recent episode.
AMA CEO James L. Madara, MD, said, “The AMA’s House of Delegates passed policy stating that racism is structural, systemic, cultural, and interpersonal, and we are deeply disturbed – and angered – by a recent JAMA podcast that questioned the existence of structural racism and the affiliated tweet that promoted the podcast and stated ‘no physician is racist, so how can there be structural racism in health care?’ ”
He continued: “JAMA has editorial independence from AMA, but this tweet and podcast are inconsistent with the policies and views of AMA, and I’m concerned about and acknowledge the harms they have caused. Structural racism in health care and our society exists, and it is incumbent on all of us to fix it.”
This article was updated 3/5/21.
A version of this article first appeared on WebMD.com.
U.S. suicide rate in 2019 took first downturn in 14 years
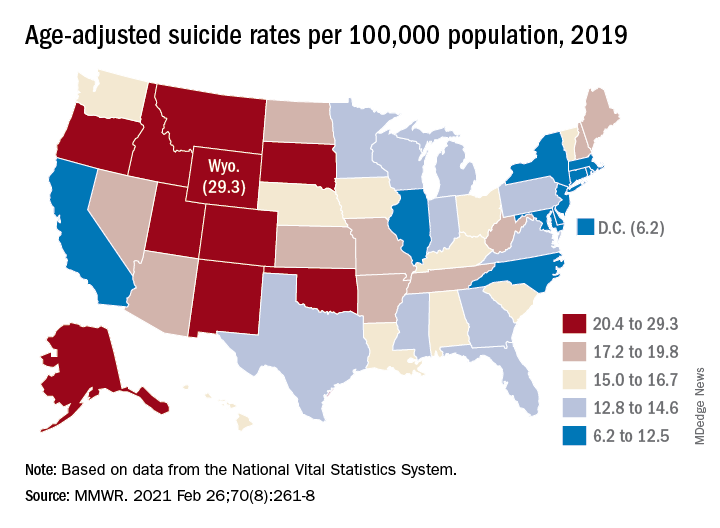
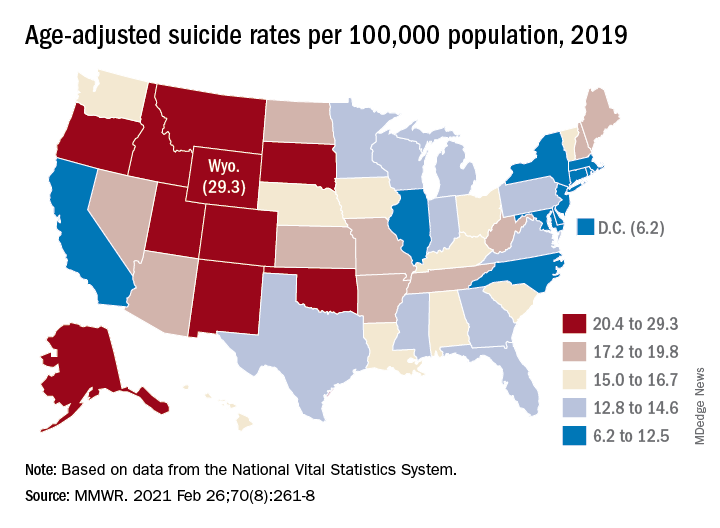
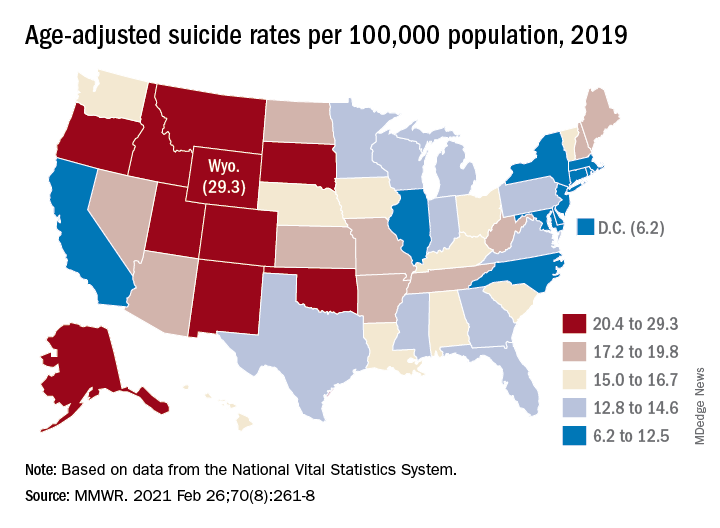
In 2019, the U.S. suicide rate dropped for the first time in 14 years, driven largely by a significant decline in firearm-related deaths, according to a new analysis of National Vital Statistics System data.
Since firearms are the “most common and most lethal” mechanism of suicide, the drop in deaths is “particularly encouraging,” Deborah M. Stone, ScD, MSW, MPH, and associates wrote in the Morbidity and Mortality Weekly Report.
The national suicide rate decreased from 14.2 per 100,000 population in 2018 to 13.9 per 100,000 in 2019, a statistically significant drop of 2.1% that reversed a 20-year trend that saw the rate increase by 33% since 1999, they said.
The rate for firearm use, which is involved in half of all suicides, declined from 7.0 per 100,000 to 6.8, for a significant change of 2.9%, said Dr. Stone and associates at the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
The only other method with a drop in suicide rate from 2018 to 2019 was suffocation – the second most common mechanism of injury – but the relative change of 2.3% was not significant, they noted.
Significant declines also occurred in several subgroups: Whites; those aged 15-24, 55-64, and 65-74 years; and those living in counties classified as large fringe metropolitan or micropolitan (urban cluster of ≥ 10,000 but less than 50,000 population), they said, based on data from the National Vital Statistics System.
the investigators wrote.
The states with significant increases were Hawaii (30.3%) and Nebraska (20.1%), while declines in the suicide rate were significant in five states – Idaho, Indiana, Massachusetts, North Carolina, and Virginia, Dr. Stone and associates reported. Altogether, the rate fell in 31 states, increased in 18, and did not change in 2.
The significance of those changes varied between males and females. Declines were significant for females in Indiana, Massachusetts, and Washington, and for males in Florida, Kentucky, Massachusetts, North Carolina, and West Virginia. Minnesota was the only state with a significant increase among females, with Hawaii and Wyoming posting increases for males, they said.
As the response to the COVID-19 pandemic continues, the investigators pointed out, “prevention is more important than ever. Past research indicates that suicide rates remain stable or decline during infrastructure disruption (e.g., natural disasters), only to rise afterwards as the longer-term sequelae unfold in persons, families, and communities.”
In 2019, the U.S. suicide rate dropped for the first time in 14 years, driven largely by a significant decline in firearm-related deaths, according to a new analysis of National Vital Statistics System data.
Since firearms are the “most common and most lethal” mechanism of suicide, the drop in deaths is “particularly encouraging,” Deborah M. Stone, ScD, MSW, MPH, and associates wrote in the Morbidity and Mortality Weekly Report.
The national suicide rate decreased from 14.2 per 100,000 population in 2018 to 13.9 per 100,000 in 2019, a statistically significant drop of 2.1% that reversed a 20-year trend that saw the rate increase by 33% since 1999, they said.
The rate for firearm use, which is involved in half of all suicides, declined from 7.0 per 100,000 to 6.8, for a significant change of 2.9%, said Dr. Stone and associates at the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
The only other method with a drop in suicide rate from 2018 to 2019 was suffocation – the second most common mechanism of injury – but the relative change of 2.3% was not significant, they noted.
Significant declines also occurred in several subgroups: Whites; those aged 15-24, 55-64, and 65-74 years; and those living in counties classified as large fringe metropolitan or micropolitan (urban cluster of ≥ 10,000 but less than 50,000 population), they said, based on data from the National Vital Statistics System.
the investigators wrote.
The states with significant increases were Hawaii (30.3%) and Nebraska (20.1%), while declines in the suicide rate were significant in five states – Idaho, Indiana, Massachusetts, North Carolina, and Virginia, Dr. Stone and associates reported. Altogether, the rate fell in 31 states, increased in 18, and did not change in 2.
The significance of those changes varied between males and females. Declines were significant for females in Indiana, Massachusetts, and Washington, and for males in Florida, Kentucky, Massachusetts, North Carolina, and West Virginia. Minnesota was the only state with a significant increase among females, with Hawaii and Wyoming posting increases for males, they said.
As the response to the COVID-19 pandemic continues, the investigators pointed out, “prevention is more important than ever. Past research indicates that suicide rates remain stable or decline during infrastructure disruption (e.g., natural disasters), only to rise afterwards as the longer-term sequelae unfold in persons, families, and communities.”
In 2019, the U.S. suicide rate dropped for the first time in 14 years, driven largely by a significant decline in firearm-related deaths, according to a new analysis of National Vital Statistics System data.
Since firearms are the “most common and most lethal” mechanism of suicide, the drop in deaths is “particularly encouraging,” Deborah M. Stone, ScD, MSW, MPH, and associates wrote in the Morbidity and Mortality Weekly Report.
The national suicide rate decreased from 14.2 per 100,000 population in 2018 to 13.9 per 100,000 in 2019, a statistically significant drop of 2.1% that reversed a 20-year trend that saw the rate increase by 33% since 1999, they said.
The rate for firearm use, which is involved in half of all suicides, declined from 7.0 per 100,000 to 6.8, for a significant change of 2.9%, said Dr. Stone and associates at the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
The only other method with a drop in suicide rate from 2018 to 2019 was suffocation – the second most common mechanism of injury – but the relative change of 2.3% was not significant, they noted.
Significant declines also occurred in several subgroups: Whites; those aged 15-24, 55-64, and 65-74 years; and those living in counties classified as large fringe metropolitan or micropolitan (urban cluster of ≥ 10,000 but less than 50,000 population), they said, based on data from the National Vital Statistics System.
the investigators wrote.
The states with significant increases were Hawaii (30.3%) and Nebraska (20.1%), while declines in the suicide rate were significant in five states – Idaho, Indiana, Massachusetts, North Carolina, and Virginia, Dr. Stone and associates reported. Altogether, the rate fell in 31 states, increased in 18, and did not change in 2.
The significance of those changes varied between males and females. Declines were significant for females in Indiana, Massachusetts, and Washington, and for males in Florida, Kentucky, Massachusetts, North Carolina, and West Virginia. Minnesota was the only state with a significant increase among females, with Hawaii and Wyoming posting increases for males, they said.
As the response to the COVID-19 pandemic continues, the investigators pointed out, “prevention is more important than ever. Past research indicates that suicide rates remain stable or decline during infrastructure disruption (e.g., natural disasters), only to rise afterwards as the longer-term sequelae unfold in persons, families, and communities.”
FROM MMWR
Do antidepressants increase the risk of brain bleeds?
Contrary to previous findings, results of a large observational study show. However, at least one expert urged caution in interpreting the finding.
“These findings are important, especially since depression is common after stroke and SSRIs are some of the first drugs considered for people,” Mithilesh Siddu, MD, of the University of Miami/Jackson Memorial Hospital, also in Miami, said in a statement.
However, Dr. Siddu said “more research is needed to confirm our findings and to also examine if SSRIs prescribed after a stroke may be linked to risk of a second stroke.”
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Widely prescribed
SSRIs, the most widely prescribed antidepressant in the United States, have previously been linked to an increased risk of ICH, possibly as a result of impaired platelet function.
To investigate further, the researchers analyzed data from the Florida Stroke Registry (FSR). They identified 127,915 patients who suffered ICH from January 2010 to December 2019 and for whom information on antidepressant use was available.
They analyzed the proportion of cases presenting with ICH among antidepressant users and the rate of SSRI prescription among stroke patients discharged on antidepressant therapy.
The researchers found that 11% of those who had been prescribed antidepressants had an ICH, compared with 14% of those who had not.
Antidepressant users were more likely to be female; non-Hispanic White; have hypertension; have diabetes; and use oral anticoagulants, antiplatelets, and statins prior to hospital presentation for ICH.
In multivariable analyses adjusting for age, race, prior history of hypertension, diabetes and prior oral anticoagulant, antiplatelet and statin use, antidepressant users were just as likely to present with spontaneous ICH as nonantidepressant users (odds ratio, 0.92; 95% confidence interval, 0.85-1.01).
A total of 3.4% of all ICH patients and 9% of those in whom specific antidepressant information was available were discharged home on an antidepressant, most commonly an SSRI (74%).
The authors noted a key limitation of the study: Some details regarding the length, dosage, and type of antidepressants were not available.
Interpret with caution
In a comment, Shaheen Lakhan, MD, PhD, a neurologist in Newton, Mass., and executive director of the Global Neuroscience Initiative Foundation, urged caution in making any firm conclusions based on this study.
“We have two questions here: One, is SSRI use a risk factor for first-time intracerebral hemorrhage, and two, is SSRI use after an ICH a risk factor for additional hemorrhages,” said Dr. Lakhan, who was not involved with the study.
“This study incompletely addresses the first because it is known that SSRIs have a variety of potencies. For instance, paroxetine is a strong inhibitor of serotonin reuptake, whereas bupropion is weak. Hypothetically, the former has a greater risk of ICH. Because this study did not stratify by type of antidepressant, it is not possible to tease these out,” Dr. Lakhan said.
“The second question is completely unaddressed by this study and is the real concern in clinical practice, because the chance of rebleed is much higher than the risk of first-time ICH in the general population,” he added.
The study had no specific funding. Dr. Siddu and Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Contrary to previous findings, results of a large observational study show. However, at least one expert urged caution in interpreting the finding.
“These findings are important, especially since depression is common after stroke and SSRIs are some of the first drugs considered for people,” Mithilesh Siddu, MD, of the University of Miami/Jackson Memorial Hospital, also in Miami, said in a statement.
However, Dr. Siddu said “more research is needed to confirm our findings and to also examine if SSRIs prescribed after a stroke may be linked to risk of a second stroke.”
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Widely prescribed
SSRIs, the most widely prescribed antidepressant in the United States, have previously been linked to an increased risk of ICH, possibly as a result of impaired platelet function.
To investigate further, the researchers analyzed data from the Florida Stroke Registry (FSR). They identified 127,915 patients who suffered ICH from January 2010 to December 2019 and for whom information on antidepressant use was available.
They analyzed the proportion of cases presenting with ICH among antidepressant users and the rate of SSRI prescription among stroke patients discharged on antidepressant therapy.
The researchers found that 11% of those who had been prescribed antidepressants had an ICH, compared with 14% of those who had not.
Antidepressant users were more likely to be female; non-Hispanic White; have hypertension; have diabetes; and use oral anticoagulants, antiplatelets, and statins prior to hospital presentation for ICH.
In multivariable analyses adjusting for age, race, prior history of hypertension, diabetes and prior oral anticoagulant, antiplatelet and statin use, antidepressant users were just as likely to present with spontaneous ICH as nonantidepressant users (odds ratio, 0.92; 95% confidence interval, 0.85-1.01).
A total of 3.4% of all ICH patients and 9% of those in whom specific antidepressant information was available were discharged home on an antidepressant, most commonly an SSRI (74%).
The authors noted a key limitation of the study: Some details regarding the length, dosage, and type of antidepressants were not available.
Interpret with caution
In a comment, Shaheen Lakhan, MD, PhD, a neurologist in Newton, Mass., and executive director of the Global Neuroscience Initiative Foundation, urged caution in making any firm conclusions based on this study.
“We have two questions here: One, is SSRI use a risk factor for first-time intracerebral hemorrhage, and two, is SSRI use after an ICH a risk factor for additional hemorrhages,” said Dr. Lakhan, who was not involved with the study.
“This study incompletely addresses the first because it is known that SSRIs have a variety of potencies. For instance, paroxetine is a strong inhibitor of serotonin reuptake, whereas bupropion is weak. Hypothetically, the former has a greater risk of ICH. Because this study did not stratify by type of antidepressant, it is not possible to tease these out,” Dr. Lakhan said.
“The second question is completely unaddressed by this study and is the real concern in clinical practice, because the chance of rebleed is much higher than the risk of first-time ICH in the general population,” he added.
The study had no specific funding. Dr. Siddu and Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Contrary to previous findings, results of a large observational study show. However, at least one expert urged caution in interpreting the finding.
“These findings are important, especially since depression is common after stroke and SSRIs are some of the first drugs considered for people,” Mithilesh Siddu, MD, of the University of Miami/Jackson Memorial Hospital, also in Miami, said in a statement.
However, Dr. Siddu said “more research is needed to confirm our findings and to also examine if SSRIs prescribed after a stroke may be linked to risk of a second stroke.”
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Widely prescribed
SSRIs, the most widely prescribed antidepressant in the United States, have previously been linked to an increased risk of ICH, possibly as a result of impaired platelet function.
To investigate further, the researchers analyzed data from the Florida Stroke Registry (FSR). They identified 127,915 patients who suffered ICH from January 2010 to December 2019 and for whom information on antidepressant use was available.
They analyzed the proportion of cases presenting with ICH among antidepressant users and the rate of SSRI prescription among stroke patients discharged on antidepressant therapy.
The researchers found that 11% of those who had been prescribed antidepressants had an ICH, compared with 14% of those who had not.
Antidepressant users were more likely to be female; non-Hispanic White; have hypertension; have diabetes; and use oral anticoagulants, antiplatelets, and statins prior to hospital presentation for ICH.
In multivariable analyses adjusting for age, race, prior history of hypertension, diabetes and prior oral anticoagulant, antiplatelet and statin use, antidepressant users were just as likely to present with spontaneous ICH as nonantidepressant users (odds ratio, 0.92; 95% confidence interval, 0.85-1.01).
A total of 3.4% of all ICH patients and 9% of those in whom specific antidepressant information was available were discharged home on an antidepressant, most commonly an SSRI (74%).
The authors noted a key limitation of the study: Some details regarding the length, dosage, and type of antidepressants were not available.
Interpret with caution
In a comment, Shaheen Lakhan, MD, PhD, a neurologist in Newton, Mass., and executive director of the Global Neuroscience Initiative Foundation, urged caution in making any firm conclusions based on this study.
“We have two questions here: One, is SSRI use a risk factor for first-time intracerebral hemorrhage, and two, is SSRI use after an ICH a risk factor for additional hemorrhages,” said Dr. Lakhan, who was not involved with the study.
“This study incompletely addresses the first because it is known that SSRIs have a variety of potencies. For instance, paroxetine is a strong inhibitor of serotonin reuptake, whereas bupropion is weak. Hypothetically, the former has a greater risk of ICH. Because this study did not stratify by type of antidepressant, it is not possible to tease these out,” Dr. Lakhan said.
“The second question is completely unaddressed by this study and is the real concern in clinical practice, because the chance of rebleed is much higher than the risk of first-time ICH in the general population,” he added.
The study had no specific funding. Dr. Siddu and Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAN 2021
Natalizumab postinfusion reactions rare; is monitoring necessary?
new studies show.
Collectively, the results suggest the need to rethink the drug’s mandatory 1-hour postinfusion observation period – particularly when unnecessarily spending time in medical settings is discouraged because of concerns regarding COVID-19, the researchers concluded.
Their findings “highlight a potential opportunity to improve and streamline the infusion and postinfusion monitoring process,” reported the authors of one of the studies. The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Infusion reactions were rare
“In this systematic review of almost 10,000 natalizumab infusions, all infusion-related adverse events were mild, and no clinically relevant safety concerns were associated with natalizumab infusions,” they said.
The 1-hour postinfusion observation period for natalizumab, approved for the treatment of relapsing remitting MS (RRMS), is mandated by the Food and Drug Administration, as well as the European Medicines Agency, and applies to each dose, regardless of treatment duration, owing to concerns of infusion reactions. However, previous evidence has indicated that reactions are rare and are usually mild.
In addition to adding burden to the treatment regimen for patients and providers alike, any extended time in an environment where there is concern of heightened risk for SARS-CoV-2 exposure is a concern.
To evaluate the frequency, severity, and timing of infusion reactions, Yujie Wang, MD, of the department of neurology at the University of Washington, Seattle, and colleagues reviewed medical records of all patients who received natalizumab at the University of Washington MS Center’s infusion suite between July 2012 and September 2020.
Among 333 patients with RRMS, 9,682 infusions of natalizumab were provided over the study period, with a mean of 27 infusions per patient (range, 1-174). The mean age of the patients was 41 years, and 87 (26%) were male.
Overall, 33 infusion-related adverse events were reported in 26 patients, representing 0.34% of total infusions and 7.8% of patients.
In 77% of cases, the adverse event occurred during the infusion. In 92% of cases, the adverse event occurred within the first 6 months of treatment.
All of the events were described as mild. The most common were itching, gastrointestinal problems, headache, and flushing.
None of the reactions required emergency care or hospitalization. Symptoms were either self-managed or were managed easily with standard care. The treatment was continued in all cases.
“For physicians and providers who care for patients with MS and are comfortable with infusible therapies, it is no surprise that rates of clinically significant infusion reactions were low,” Dr. Wang said. “It is indeed consistent with prior studies that reactions generally occur during rather than post infusion.”
The authors underscored the array of potential benefits in making changes to the requirement. “Anticipated benefits may include reducing SARS-CoV2 exposure risks for patients and staff, reducing patients’ treatment burden, increasing efficiency, as well as improving access to care without neglecting patient safety.”
Additional studies show consistent findings
Several other recent studies have shown similar results. In a study published in Multiple Sclerosis in October 2020, researchers with the Amsterdam University Medical Center found that, among 14,174 natalizumab infusions provided to 225 patients with RRMS between 2006 and 2018, 276 infusion-related adverse events occurred (1.95%) among 60 patients.
There were 11 severe infusion-related adverse events in nine patients (4.0%). All documented severe reactions occurred during the infusion. Among 19 moderate adverse events, 17 occurred during the infusion.
The researchers noted that the majority of patients who experienced severe infusion reactions had detectable antibodies against natalizumab. Such antibodies are associated with a higher risk for infusion-related adverse events.
Patients who did not have any symptoms of a reaction during the infusion had no clinically relevant moderate or severe reactions.
“Thus, the need for postinfusion observation will depend on the patients’ clinical status during the infusion,” they wrote. “Consequently, our data suggest that patients who do not have an infusion-related adverse event while receiving natalizumab treatment do not need to stay in the hospital for an additional observation hour.”
Rapid infusion protocol
In another recent study published in Multiple Sclerosis and Related Disorders in January 2021, researchers in Australia reported on the use of a rapid infusion protocol of natalizumab and ocrelizumab. The protocol was implemented to reduce the amount of time patients are required to spend in clinical settings during the COVID-19 pandemic.
In their analysis of 269 rapid infusions of natalizumab and 100 rapid infusions of ocrelizumab, there were two infusion-related reactions in the natalizumab group and eight in the ocrelizumab group.
All the reactions were mild to moderate, and no discontinuations were required. None of the reactions occurred during the postinfusion observation period.
“In the setting of COVID-19 pandemic, rapid infusion protocols could potentially save hospital resources and limit patient exposure to a high-risk clinical setting while still maintaining ongoing treatment of multiple sclerosis,” the authors wrote.
Under the rapid infusion protocol, patients receive three standard doses for 1 hour followed by 30 minutes of observation. In addition, infusions are reduced to 30 minutes, explained lead author Louise Rath, of clinical neurosciences, Alfred Health, in Melbourne.
“For our cohort of patients, the side effects were minimal,” she said.
“Rapid infusions allowed patients to have option of hospital in-home or office, ensuring work was not at risk by infusion,” she added. “Our governance has been very supportive, and we will be keeping rapid infusion post COVID.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new studies show.
Collectively, the results suggest the need to rethink the drug’s mandatory 1-hour postinfusion observation period – particularly when unnecessarily spending time in medical settings is discouraged because of concerns regarding COVID-19, the researchers concluded.
Their findings “highlight a potential opportunity to improve and streamline the infusion and postinfusion monitoring process,” reported the authors of one of the studies. The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Infusion reactions were rare
“In this systematic review of almost 10,000 natalizumab infusions, all infusion-related adverse events were mild, and no clinically relevant safety concerns were associated with natalizumab infusions,” they said.
The 1-hour postinfusion observation period for natalizumab, approved for the treatment of relapsing remitting MS (RRMS), is mandated by the Food and Drug Administration, as well as the European Medicines Agency, and applies to each dose, regardless of treatment duration, owing to concerns of infusion reactions. However, previous evidence has indicated that reactions are rare and are usually mild.
In addition to adding burden to the treatment regimen for patients and providers alike, any extended time in an environment where there is concern of heightened risk for SARS-CoV-2 exposure is a concern.
To evaluate the frequency, severity, and timing of infusion reactions, Yujie Wang, MD, of the department of neurology at the University of Washington, Seattle, and colleagues reviewed medical records of all patients who received natalizumab at the University of Washington MS Center’s infusion suite between July 2012 and September 2020.
Among 333 patients with RRMS, 9,682 infusions of natalizumab were provided over the study period, with a mean of 27 infusions per patient (range, 1-174). The mean age of the patients was 41 years, and 87 (26%) were male.
Overall, 33 infusion-related adverse events were reported in 26 patients, representing 0.34% of total infusions and 7.8% of patients.
In 77% of cases, the adverse event occurred during the infusion. In 92% of cases, the adverse event occurred within the first 6 months of treatment.
All of the events were described as mild. The most common were itching, gastrointestinal problems, headache, and flushing.
None of the reactions required emergency care or hospitalization. Symptoms were either self-managed or were managed easily with standard care. The treatment was continued in all cases.
“For physicians and providers who care for patients with MS and are comfortable with infusible therapies, it is no surprise that rates of clinically significant infusion reactions were low,” Dr. Wang said. “It is indeed consistent with prior studies that reactions generally occur during rather than post infusion.”
The authors underscored the array of potential benefits in making changes to the requirement. “Anticipated benefits may include reducing SARS-CoV2 exposure risks for patients and staff, reducing patients’ treatment burden, increasing efficiency, as well as improving access to care without neglecting patient safety.”
Additional studies show consistent findings
Several other recent studies have shown similar results. In a study published in Multiple Sclerosis in October 2020, researchers with the Amsterdam University Medical Center found that, among 14,174 natalizumab infusions provided to 225 patients with RRMS between 2006 and 2018, 276 infusion-related adverse events occurred (1.95%) among 60 patients.
There were 11 severe infusion-related adverse events in nine patients (4.0%). All documented severe reactions occurred during the infusion. Among 19 moderate adverse events, 17 occurred during the infusion.
The researchers noted that the majority of patients who experienced severe infusion reactions had detectable antibodies against natalizumab. Such antibodies are associated with a higher risk for infusion-related adverse events.
Patients who did not have any symptoms of a reaction during the infusion had no clinically relevant moderate or severe reactions.
“Thus, the need for postinfusion observation will depend on the patients’ clinical status during the infusion,” they wrote. “Consequently, our data suggest that patients who do not have an infusion-related adverse event while receiving natalizumab treatment do not need to stay in the hospital for an additional observation hour.”
Rapid infusion protocol
In another recent study published in Multiple Sclerosis and Related Disorders in January 2021, researchers in Australia reported on the use of a rapid infusion protocol of natalizumab and ocrelizumab. The protocol was implemented to reduce the amount of time patients are required to spend in clinical settings during the COVID-19 pandemic.
In their analysis of 269 rapid infusions of natalizumab and 100 rapid infusions of ocrelizumab, there were two infusion-related reactions in the natalizumab group and eight in the ocrelizumab group.
All the reactions were mild to moderate, and no discontinuations were required. None of the reactions occurred during the postinfusion observation period.
“In the setting of COVID-19 pandemic, rapid infusion protocols could potentially save hospital resources and limit patient exposure to a high-risk clinical setting while still maintaining ongoing treatment of multiple sclerosis,” the authors wrote.
Under the rapid infusion protocol, patients receive three standard doses for 1 hour followed by 30 minutes of observation. In addition, infusions are reduced to 30 minutes, explained lead author Louise Rath, of clinical neurosciences, Alfred Health, in Melbourne.
“For our cohort of patients, the side effects were minimal,” she said.
“Rapid infusions allowed patients to have option of hospital in-home or office, ensuring work was not at risk by infusion,” she added. “Our governance has been very supportive, and we will be keeping rapid infusion post COVID.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new studies show.
Collectively, the results suggest the need to rethink the drug’s mandatory 1-hour postinfusion observation period – particularly when unnecessarily spending time in medical settings is discouraged because of concerns regarding COVID-19, the researchers concluded.
Their findings “highlight a potential opportunity to improve and streamline the infusion and postinfusion monitoring process,” reported the authors of one of the studies. The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Infusion reactions were rare
“In this systematic review of almost 10,000 natalizumab infusions, all infusion-related adverse events were mild, and no clinically relevant safety concerns were associated with natalizumab infusions,” they said.
The 1-hour postinfusion observation period for natalizumab, approved for the treatment of relapsing remitting MS (RRMS), is mandated by the Food and Drug Administration, as well as the European Medicines Agency, and applies to each dose, regardless of treatment duration, owing to concerns of infusion reactions. However, previous evidence has indicated that reactions are rare and are usually mild.
In addition to adding burden to the treatment regimen for patients and providers alike, any extended time in an environment where there is concern of heightened risk for SARS-CoV-2 exposure is a concern.
To evaluate the frequency, severity, and timing of infusion reactions, Yujie Wang, MD, of the department of neurology at the University of Washington, Seattle, and colleagues reviewed medical records of all patients who received natalizumab at the University of Washington MS Center’s infusion suite between July 2012 and September 2020.
Among 333 patients with RRMS, 9,682 infusions of natalizumab were provided over the study period, with a mean of 27 infusions per patient (range, 1-174). The mean age of the patients was 41 years, and 87 (26%) were male.
Overall, 33 infusion-related adverse events were reported in 26 patients, representing 0.34% of total infusions and 7.8% of patients.
In 77% of cases, the adverse event occurred during the infusion. In 92% of cases, the adverse event occurred within the first 6 months of treatment.
All of the events were described as mild. The most common were itching, gastrointestinal problems, headache, and flushing.
None of the reactions required emergency care or hospitalization. Symptoms were either self-managed or were managed easily with standard care. The treatment was continued in all cases.
“For physicians and providers who care for patients with MS and are comfortable with infusible therapies, it is no surprise that rates of clinically significant infusion reactions were low,” Dr. Wang said. “It is indeed consistent with prior studies that reactions generally occur during rather than post infusion.”
The authors underscored the array of potential benefits in making changes to the requirement. “Anticipated benefits may include reducing SARS-CoV2 exposure risks for patients and staff, reducing patients’ treatment burden, increasing efficiency, as well as improving access to care without neglecting patient safety.”
Additional studies show consistent findings
Several other recent studies have shown similar results. In a study published in Multiple Sclerosis in October 2020, researchers with the Amsterdam University Medical Center found that, among 14,174 natalizumab infusions provided to 225 patients with RRMS between 2006 and 2018, 276 infusion-related adverse events occurred (1.95%) among 60 patients.
There were 11 severe infusion-related adverse events in nine patients (4.0%). All documented severe reactions occurred during the infusion. Among 19 moderate adverse events, 17 occurred during the infusion.
The researchers noted that the majority of patients who experienced severe infusion reactions had detectable antibodies against natalizumab. Such antibodies are associated with a higher risk for infusion-related adverse events.
Patients who did not have any symptoms of a reaction during the infusion had no clinically relevant moderate or severe reactions.
“Thus, the need for postinfusion observation will depend on the patients’ clinical status during the infusion,” they wrote. “Consequently, our data suggest that patients who do not have an infusion-related adverse event while receiving natalizumab treatment do not need to stay in the hospital for an additional observation hour.”
Rapid infusion protocol
In another recent study published in Multiple Sclerosis and Related Disorders in January 2021, researchers in Australia reported on the use of a rapid infusion protocol of natalizumab and ocrelizumab. The protocol was implemented to reduce the amount of time patients are required to spend in clinical settings during the COVID-19 pandemic.
In their analysis of 269 rapid infusions of natalizumab and 100 rapid infusions of ocrelizumab, there were two infusion-related reactions in the natalizumab group and eight in the ocrelizumab group.
All the reactions were mild to moderate, and no discontinuations were required. None of the reactions occurred during the postinfusion observation period.
“In the setting of COVID-19 pandemic, rapid infusion protocols could potentially save hospital resources and limit patient exposure to a high-risk clinical setting while still maintaining ongoing treatment of multiple sclerosis,” the authors wrote.
Under the rapid infusion protocol, patients receive three standard doses for 1 hour followed by 30 minutes of observation. In addition, infusions are reduced to 30 minutes, explained lead author Louise Rath, of clinical neurosciences, Alfred Health, in Melbourne.
“For our cohort of patients, the side effects were minimal,” she said.
“Rapid infusions allowed patients to have option of hospital in-home or office, ensuring work was not at risk by infusion,” she added. “Our governance has been very supportive, and we will be keeping rapid infusion post COVID.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACTRIMS 2021
Docs become dog groomers and warehouse workers after COVID-19 work loss
One of the biggest conundrums of the COVID-19 pandemic has been the simultaneous panic-hiring of medical professionals in hot spots and significant downsizing of staff across the country. From huge hospital systems to private practices, the stoppage of breast reductions and knee replacements, not to mention the drops in motor vehicle accidents and bar fights, have quieted operating rooms and emergency departments and put doctors’ jobs on the chopping block. A widely cited survey suggests that 21% of doctors have had a work reduction due to COVID-19.
For many American doctors, this is their first extended period of unemployment. Unlike engineers or those with MBAs who might see their fortunes rise and fall with the whims of recessions and boom times, physicians are not exactly accustomed to being laid off. However, doctors were already smarting for years due to falling salaries and decreased autonomy, punctuated by endless clicks on electronic medical records software.
Stephanie Eschenbach Morgan, MD, a breast radiologist in North Carolina, trained for 10 years after college before earning a true physician’s salary.
“Being furloughed was awful. Initially, it was only going to be 2 weeks, and then it turned into 2 months with no pay,” she reflected.
Dr. Eschenbach Morgan and her surgeon husband, who lost a full quarter’s salary, had to ask for grace periods on their credit card and mortgage payments because they had paid a large tax bill right before the pandemic began. “We couldn’t get any stimulus help, so that added insult to injury,” she said.
With her time spent waiting in a holding pattern, Dr. Eschenbach Morgan homeschooled her two young children and started putting a home gym together. She went on a home organizing spree, started a garden, and, perhaps most impressively, caught up with 5 years of photo albums.
A bonus she noted: “I didn’t set an alarm for 2 months.”
Shella Farooki, MD, a radiologist in California, was also focused on homeschooling, itself a demanding job, and veered toward retirement. When one of her work contracts furloughed her (“at one point, I made $30K a month for [their business]”), she started saving money at home, teaching the kids, and applied for a Paycheck Protection Program loan. Her husband, a hospitalist, had had his shifts cut. Dr. Farooki tried a radiology artificial intelligence firm but backed out when she was asked to read 9,200 studies for them for $2,000 per month.
Now, she thinks about leaving medicine “every day.”
Some doctors are questioning whether they should be in medicine in the first place. Family medicine physician Jonathan Polak, MD, faced with his own pink slip, turned to pink T-shirts instead. His girlfriend manages an outlet of the teen fashion retailer Justice. Dr. Polak, who finished his residency just 2 years ago, didn’t hesitate to take a $10-an-hour gig as a stock doc, once even finding himself delivering a shelving unit from the shuttering store to a physician fleeing the city for rural New Hampshire to “escape.”
There’s no escape for him – yet. Saddled with “astronomical” student loans, he had considered grocery store work as well. Dr. Polak knows he can’t work part time or go into teaching long term, as he might like.
Even so, he’s doing everything he can to not be in patient care for the long haul – it’s just not what he thought it would be.
“The culture of medicine, bureaucracy, endless paperwork and charting, and threat of litigation sucks a lot of the joy out of it to the point that I don’t see myself doing it forever when imagining myself 5-10 years into it.”
Still, he recently took an 18-month hospital contract that will force him to move to Florida, but he’s also been turning himself into a veritable Renaissance man; composing music, training for an ultramarathon, studying the latest medical findings, roadtripping, and launching a podcast about dog grooming with a master groomer. “We found parallels between medicine and dog grooming,” he says, somewhat convincingly.
Also working the ruff life is Jen Tserng, MD, a former forensic pathologist who landed on news websites in recent years for becoming a professional dogwalker and housesitter without a permanent home. Dr. Tserng knows doctors were restless and unhappy before COVID-19, their thoughts wandering where the grass might be greener.
As her profile grew, she found her inbox gathering messages from disaffected medical minions: students with a fear of failing or staring down residency application season and employed doctors sick of the constant grind. As she recounted those de facto life coach conversations (“What do you really enjoy?” “Do you really like dogs?”) by phone from New York, she said matter-of-factly, “They don’t call because of COVID. They call because they hate their lives.”
Michelle Mudge-Riley, MD, a physician in Texas, has been seeing this shift for some time as well. She recently held a virtual version of her Physicians Helping Physicians conference, where doctors hear from their peers working successfully in fields like pharmaceuticals and real estate investing.
When COVID-19 hit, Dr. Mudge-Riley quickly pivoted to a virtual platform, where the MDs and DOs huddled in breakout rooms having honest chats about their fears and tentative hopes about their new careers.
“There has been increased interest in nonclinical exploration into full- and part-time careers, as well as side hustles, since COVID began,” she said. “Many physicians have had their hours or pay cut, and some have been laid off. Others are furloughed. Some just want out of an environment where they don’t feel safe.”
An ear, nose, and throat surgeon, Maansi Doshi, MD, from central California, didn’t feel safe – so she left. She had returned from India sick with a mystery virus right as the pandemic began (she said her COVID-19 tests were all negative) and was waiting to get well enough to go back to her private practice job. However, she said she clashed with Trump-supporting colleagues she feared might not be taking the pandemic seriously enough.
Finally getting over a relapse of her mystery virus, Dr. Doshi emailed her resignation in May. Her husband, family practice doctor Mark Mangiapane, MD, gave his job notice weeks later in solidarity because he worked in the same building. Together, they have embraced gardening, a Peloton splurge, and learning business skills to open private practices – solo primary care for him; ENT with a focus on her favorite surgery, rhinoplasty, for her.
Dr. Mangiapane had considered editing medical brochures and also tried to apply for a job as a county public health officer in rural California, but he received his own shock when he learned the county intended to open schools in the midst of the pandemic despite advisement to the contrary by the former health officer.
He retreated from job listings altogether after hearing his would-be peers were getting death threats – targeting their children.
Both doctors felt COVID-19 pushed them beyond their comfort zones. “If COVID hadn’t happened, I would be working. ... Be ‘owned.’ In a weird way, COVID made me more independent and take a risk with my career.”
Obstetrician Kwandaa Roberts, MD, certainly did; she took a budding interest in decorating dollhouses straight to Instagram and national news fame, and she is now a TV-show expert on “Sell This House.”
Like Dr. Doshi and Dr. Mangiapane, Dr. Polak wants to be more in control of his future – even if selling T-shirts at a mall means a certain loss of status along the way.
“Aside from my passion to learn and to have that connection with people, I went into medicine ... because of the job security I thought existed,” he said. “I would say that my getting furloughed has changed my view of the United States in a dramatic way. I do not feel as confident in the U.S. economy and general way of life as I did a year ago. And I am taking a number of steps to put myself in a more fluid, adaptable position in case another crisis like this occurs or if the current state of things worsens.”
A version of this article first appeared on Medscape.com.
One of the biggest conundrums of the COVID-19 pandemic has been the simultaneous panic-hiring of medical professionals in hot spots and significant downsizing of staff across the country. From huge hospital systems to private practices, the stoppage of breast reductions and knee replacements, not to mention the drops in motor vehicle accidents and bar fights, have quieted operating rooms and emergency departments and put doctors’ jobs on the chopping block. A widely cited survey suggests that 21% of doctors have had a work reduction due to COVID-19.
For many American doctors, this is their first extended period of unemployment. Unlike engineers or those with MBAs who might see their fortunes rise and fall with the whims of recessions and boom times, physicians are not exactly accustomed to being laid off. However, doctors were already smarting for years due to falling salaries and decreased autonomy, punctuated by endless clicks on electronic medical records software.
Stephanie Eschenbach Morgan, MD, a breast radiologist in North Carolina, trained for 10 years after college before earning a true physician’s salary.
“Being furloughed was awful. Initially, it was only going to be 2 weeks, and then it turned into 2 months with no pay,” she reflected.
Dr. Eschenbach Morgan and her surgeon husband, who lost a full quarter’s salary, had to ask for grace periods on their credit card and mortgage payments because they had paid a large tax bill right before the pandemic began. “We couldn’t get any stimulus help, so that added insult to injury,” she said.
With her time spent waiting in a holding pattern, Dr. Eschenbach Morgan homeschooled her two young children and started putting a home gym together. She went on a home organizing spree, started a garden, and, perhaps most impressively, caught up with 5 years of photo albums.
A bonus she noted: “I didn’t set an alarm for 2 months.”
Shella Farooki, MD, a radiologist in California, was also focused on homeschooling, itself a demanding job, and veered toward retirement. When one of her work contracts furloughed her (“at one point, I made $30K a month for [their business]”), she started saving money at home, teaching the kids, and applied for a Paycheck Protection Program loan. Her husband, a hospitalist, had had his shifts cut. Dr. Farooki tried a radiology artificial intelligence firm but backed out when she was asked to read 9,200 studies for them for $2,000 per month.
Now, she thinks about leaving medicine “every day.”
Some doctors are questioning whether they should be in medicine in the first place. Family medicine physician Jonathan Polak, MD, faced with his own pink slip, turned to pink T-shirts instead. His girlfriend manages an outlet of the teen fashion retailer Justice. Dr. Polak, who finished his residency just 2 years ago, didn’t hesitate to take a $10-an-hour gig as a stock doc, once even finding himself delivering a shelving unit from the shuttering store to a physician fleeing the city for rural New Hampshire to “escape.”
There’s no escape for him – yet. Saddled with “astronomical” student loans, he had considered grocery store work as well. Dr. Polak knows he can’t work part time or go into teaching long term, as he might like.
Even so, he’s doing everything he can to not be in patient care for the long haul – it’s just not what he thought it would be.
“The culture of medicine, bureaucracy, endless paperwork and charting, and threat of litigation sucks a lot of the joy out of it to the point that I don’t see myself doing it forever when imagining myself 5-10 years into it.”
Still, he recently took an 18-month hospital contract that will force him to move to Florida, but he’s also been turning himself into a veritable Renaissance man; composing music, training for an ultramarathon, studying the latest medical findings, roadtripping, and launching a podcast about dog grooming with a master groomer. “We found parallels between medicine and dog grooming,” he says, somewhat convincingly.
Also working the ruff life is Jen Tserng, MD, a former forensic pathologist who landed on news websites in recent years for becoming a professional dogwalker and housesitter without a permanent home. Dr. Tserng knows doctors were restless and unhappy before COVID-19, their thoughts wandering where the grass might be greener.
As her profile grew, she found her inbox gathering messages from disaffected medical minions: students with a fear of failing or staring down residency application season and employed doctors sick of the constant grind. As she recounted those de facto life coach conversations (“What do you really enjoy?” “Do you really like dogs?”) by phone from New York, she said matter-of-factly, “They don’t call because of COVID. They call because they hate their lives.”
Michelle Mudge-Riley, MD, a physician in Texas, has been seeing this shift for some time as well. She recently held a virtual version of her Physicians Helping Physicians conference, where doctors hear from their peers working successfully in fields like pharmaceuticals and real estate investing.
When COVID-19 hit, Dr. Mudge-Riley quickly pivoted to a virtual platform, where the MDs and DOs huddled in breakout rooms having honest chats about their fears and tentative hopes about their new careers.
“There has been increased interest in nonclinical exploration into full- and part-time careers, as well as side hustles, since COVID began,” she said. “Many physicians have had their hours or pay cut, and some have been laid off. Others are furloughed. Some just want out of an environment where they don’t feel safe.”
An ear, nose, and throat surgeon, Maansi Doshi, MD, from central California, didn’t feel safe – so she left. She had returned from India sick with a mystery virus right as the pandemic began (she said her COVID-19 tests were all negative) and was waiting to get well enough to go back to her private practice job. However, she said she clashed with Trump-supporting colleagues she feared might not be taking the pandemic seriously enough.
Finally getting over a relapse of her mystery virus, Dr. Doshi emailed her resignation in May. Her husband, family practice doctor Mark Mangiapane, MD, gave his job notice weeks later in solidarity because he worked in the same building. Together, they have embraced gardening, a Peloton splurge, and learning business skills to open private practices – solo primary care for him; ENT with a focus on her favorite surgery, rhinoplasty, for her.
Dr. Mangiapane had considered editing medical brochures and also tried to apply for a job as a county public health officer in rural California, but he received his own shock when he learned the county intended to open schools in the midst of the pandemic despite advisement to the contrary by the former health officer.
He retreated from job listings altogether after hearing his would-be peers were getting death threats – targeting their children.
Both doctors felt COVID-19 pushed them beyond their comfort zones. “If COVID hadn’t happened, I would be working. ... Be ‘owned.’ In a weird way, COVID made me more independent and take a risk with my career.”
Obstetrician Kwandaa Roberts, MD, certainly did; she took a budding interest in decorating dollhouses straight to Instagram and national news fame, and she is now a TV-show expert on “Sell This House.”
Like Dr. Doshi and Dr. Mangiapane, Dr. Polak wants to be more in control of his future – even if selling T-shirts at a mall means a certain loss of status along the way.
“Aside from my passion to learn and to have that connection with people, I went into medicine ... because of the job security I thought existed,” he said. “I would say that my getting furloughed has changed my view of the United States in a dramatic way. I do not feel as confident in the U.S. economy and general way of life as I did a year ago. And I am taking a number of steps to put myself in a more fluid, adaptable position in case another crisis like this occurs or if the current state of things worsens.”
A version of this article first appeared on Medscape.com.
One of the biggest conundrums of the COVID-19 pandemic has been the simultaneous panic-hiring of medical professionals in hot spots and significant downsizing of staff across the country. From huge hospital systems to private practices, the stoppage of breast reductions and knee replacements, not to mention the drops in motor vehicle accidents and bar fights, have quieted operating rooms and emergency departments and put doctors’ jobs on the chopping block. A widely cited survey suggests that 21% of doctors have had a work reduction due to COVID-19.
For many American doctors, this is their first extended period of unemployment. Unlike engineers or those with MBAs who might see their fortunes rise and fall with the whims of recessions and boom times, physicians are not exactly accustomed to being laid off. However, doctors were already smarting for years due to falling salaries and decreased autonomy, punctuated by endless clicks on electronic medical records software.
Stephanie Eschenbach Morgan, MD, a breast radiologist in North Carolina, trained for 10 years after college before earning a true physician’s salary.
“Being furloughed was awful. Initially, it was only going to be 2 weeks, and then it turned into 2 months with no pay,” she reflected.
Dr. Eschenbach Morgan and her surgeon husband, who lost a full quarter’s salary, had to ask for grace periods on their credit card and mortgage payments because they had paid a large tax bill right before the pandemic began. “We couldn’t get any stimulus help, so that added insult to injury,” she said.
With her time spent waiting in a holding pattern, Dr. Eschenbach Morgan homeschooled her two young children and started putting a home gym together. She went on a home organizing spree, started a garden, and, perhaps most impressively, caught up with 5 years of photo albums.
A bonus she noted: “I didn’t set an alarm for 2 months.”
Shella Farooki, MD, a radiologist in California, was also focused on homeschooling, itself a demanding job, and veered toward retirement. When one of her work contracts furloughed her (“at one point, I made $30K a month for [their business]”), she started saving money at home, teaching the kids, and applied for a Paycheck Protection Program loan. Her husband, a hospitalist, had had his shifts cut. Dr. Farooki tried a radiology artificial intelligence firm but backed out when she was asked to read 9,200 studies for them for $2,000 per month.
Now, she thinks about leaving medicine “every day.”
Some doctors are questioning whether they should be in medicine in the first place. Family medicine physician Jonathan Polak, MD, faced with his own pink slip, turned to pink T-shirts instead. His girlfriend manages an outlet of the teen fashion retailer Justice. Dr. Polak, who finished his residency just 2 years ago, didn’t hesitate to take a $10-an-hour gig as a stock doc, once even finding himself delivering a shelving unit from the shuttering store to a physician fleeing the city for rural New Hampshire to “escape.”
There’s no escape for him – yet. Saddled with “astronomical” student loans, he had considered grocery store work as well. Dr. Polak knows he can’t work part time or go into teaching long term, as he might like.
Even so, he’s doing everything he can to not be in patient care for the long haul – it’s just not what he thought it would be.
“The culture of medicine, bureaucracy, endless paperwork and charting, and threat of litigation sucks a lot of the joy out of it to the point that I don’t see myself doing it forever when imagining myself 5-10 years into it.”
Still, he recently took an 18-month hospital contract that will force him to move to Florida, but he’s also been turning himself into a veritable Renaissance man; composing music, training for an ultramarathon, studying the latest medical findings, roadtripping, and launching a podcast about dog grooming with a master groomer. “We found parallels between medicine and dog grooming,” he says, somewhat convincingly.
Also working the ruff life is Jen Tserng, MD, a former forensic pathologist who landed on news websites in recent years for becoming a professional dogwalker and housesitter without a permanent home. Dr. Tserng knows doctors were restless and unhappy before COVID-19, their thoughts wandering where the grass might be greener.
As her profile grew, she found her inbox gathering messages from disaffected medical minions: students with a fear of failing or staring down residency application season and employed doctors sick of the constant grind. As she recounted those de facto life coach conversations (“What do you really enjoy?” “Do you really like dogs?”) by phone from New York, she said matter-of-factly, “They don’t call because of COVID. They call because they hate their lives.”
Michelle Mudge-Riley, MD, a physician in Texas, has been seeing this shift for some time as well. She recently held a virtual version of her Physicians Helping Physicians conference, where doctors hear from their peers working successfully in fields like pharmaceuticals and real estate investing.
When COVID-19 hit, Dr. Mudge-Riley quickly pivoted to a virtual platform, where the MDs and DOs huddled in breakout rooms having honest chats about their fears and tentative hopes about their new careers.
“There has been increased interest in nonclinical exploration into full- and part-time careers, as well as side hustles, since COVID began,” she said. “Many physicians have had their hours or pay cut, and some have been laid off. Others are furloughed. Some just want out of an environment where they don’t feel safe.”
An ear, nose, and throat surgeon, Maansi Doshi, MD, from central California, didn’t feel safe – so she left. She had returned from India sick with a mystery virus right as the pandemic began (she said her COVID-19 tests were all negative) and was waiting to get well enough to go back to her private practice job. However, she said she clashed with Trump-supporting colleagues she feared might not be taking the pandemic seriously enough.
Finally getting over a relapse of her mystery virus, Dr. Doshi emailed her resignation in May. Her husband, family practice doctor Mark Mangiapane, MD, gave his job notice weeks later in solidarity because he worked in the same building. Together, they have embraced gardening, a Peloton splurge, and learning business skills to open private practices – solo primary care for him; ENT with a focus on her favorite surgery, rhinoplasty, for her.
Dr. Mangiapane had considered editing medical brochures and also tried to apply for a job as a county public health officer in rural California, but he received his own shock when he learned the county intended to open schools in the midst of the pandemic despite advisement to the contrary by the former health officer.
He retreated from job listings altogether after hearing his would-be peers were getting death threats – targeting their children.
Both doctors felt COVID-19 pushed them beyond their comfort zones. “If COVID hadn’t happened, I would be working. ... Be ‘owned.’ In a weird way, COVID made me more independent and take a risk with my career.”
Obstetrician Kwandaa Roberts, MD, certainly did; she took a budding interest in decorating dollhouses straight to Instagram and national news fame, and she is now a TV-show expert on “Sell This House.”
Like Dr. Doshi and Dr. Mangiapane, Dr. Polak wants to be more in control of his future – even if selling T-shirts at a mall means a certain loss of status along the way.
“Aside from my passion to learn and to have that connection with people, I went into medicine ... because of the job security I thought existed,” he said. “I would say that my getting furloughed has changed my view of the United States in a dramatic way. I do not feel as confident in the U.S. economy and general way of life as I did a year ago. And I am taking a number of steps to put myself in a more fluid, adaptable position in case another crisis like this occurs or if the current state of things worsens.”
A version of this article first appeared on Medscape.com.
Novel oral agent effective in teens with atopic dermatitis
Abrocitinib, an investigational drug proven to be a safe and effective treatment for moderate to severe atopic dermatitis (AD) in adults 18 years and older, is also safe and effective in patients aged 12-17 years, according to a randomized trial of the oral, once-daily Janus kinase (JAK) 1 selective inhibitor, used in combination with medicated topical therapy.
The results, from the phase 3 JADE TEEN study, were presented during an oral abstract session at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“We’re very excited about the introduction of oral JAKs into our armamentarium for atopic dermatitis,” lead author Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and chief of pediatric and adolescent dermatology, Rady Children’s Hospital, also in San Diego, said in an interview.
AD ranges in severity, and there is a great deal of moderate to severe AD that has a tremendous negative impact on the individual, Dr. Eichenfield said. “Traditionally we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control.”
JAK inhibitors are effective mediators of the inflammation response that occurs in moderate to severe AD. They inhibit the stimulation of the JAK pathway and allow anti-inflammatory effects and therefore have potential, especially in more severe disease, Dr. Eichenfield said.
In the current study, which is a spin-off of the original study that looked at abrocitinib in adults, he and his team randomly assigned 285 teens (mean age, 14.9 years; 50.9% male; 56.1% White) with moderate to severe AD to receive one of the following treatments for 12 weeks: abrocitinib 200 mg plus topical therapy (95); abrocitinib 100 mg plus topical therapy (95); or placebo, which consisted of topical therapy alone (95).
The primary endpoints were an Investigator’s Global Assessment response of clear or almost clear (scores of 0 and 1, respectively), with an improvement of at least 2 points, and an improvement in Eczema Area and Severity Index score of at least 75% at week 12.
Secondary endpoints included an improvement in Peak Pruritus Numerical Rating Scale (PP-NRS) response of at least 4 points at week 12.
The teens who received abrocitinib along with medicated topical therapy showed significant improvement in the severity of their AD at the end of the 12-week period, compared with those in the placebo group.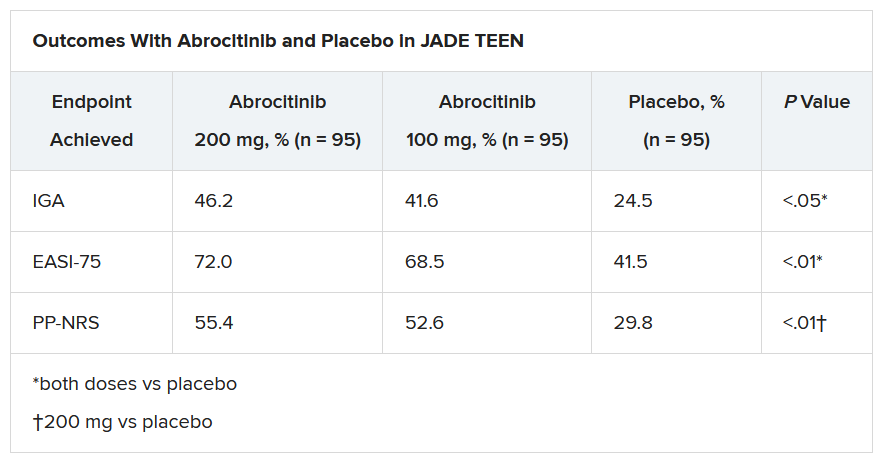
“The percentage of patients achieving essentially no itch, as captured in the fact that more than half of those on the higher dose of abrocitinib made it to no itch, is a new data point and is important to note,” Dr. Eichenfield said. “A lot of the other medicines don’t really get a significant percentage of the population to an itch score of 0 to 1. This drug brought about a rapid and profound itch relief.”
He added: “The results from JADE TEEN extend the drug’s utility in this younger population and show that abrocitinib performs the same with regard to efficacy and safety in the teenagers. Having atopic dermatitis that does not respond to treatment is especially hard for adolescents, but now we know that abrocitinib will be safe and effective and so we now have something to offer these kids.”
“Abrocitinib achieved a good response in this study that was statistically significant, compared to standard treatment,” Jonathan A. Bernstein, MD, professor of medicine at the University of Cincinnati, commented in an interview.
“JAK inhibitors are very promising, and this study adds to that promise. They play an important role in atopic dermatitis, so obviously, teenagers with AD represent an important population,” said Dr. Bernstein, who was not part of the study. “These results are very encouraging, and I think that we will probably see some of these JAK inhibitors approved by the FDA, if not this year, probably next.”
The study was sponsored by Pfizer. Dr. Eichenfield serves as an investigator, speaker, and consultant for Pfizer; and as an investigator, speaker, consultant, and/or is on a data safety monitoring board for AbbVie, Almirall, Amgen, Arcutis, Asana, Dermavant, Dermira, Forte, Galderma, Ichnos/Glenmark, Incyte, LEO, Lilly, L’Oreal, Novartis, Regeneron, Sanofi-Genzyme, and Verrica. Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Abrocitinib, an investigational drug proven to be a safe and effective treatment for moderate to severe atopic dermatitis (AD) in adults 18 years and older, is also safe and effective in patients aged 12-17 years, according to a randomized trial of the oral, once-daily Janus kinase (JAK) 1 selective inhibitor, used in combination with medicated topical therapy.
The results, from the phase 3 JADE TEEN study, were presented during an oral abstract session at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“We’re very excited about the introduction of oral JAKs into our armamentarium for atopic dermatitis,” lead author Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and chief of pediatric and adolescent dermatology, Rady Children’s Hospital, also in San Diego, said in an interview.
AD ranges in severity, and there is a great deal of moderate to severe AD that has a tremendous negative impact on the individual, Dr. Eichenfield said. “Traditionally we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control.”
JAK inhibitors are effective mediators of the inflammation response that occurs in moderate to severe AD. They inhibit the stimulation of the JAK pathway and allow anti-inflammatory effects and therefore have potential, especially in more severe disease, Dr. Eichenfield said.
In the current study, which is a spin-off of the original study that looked at abrocitinib in adults, he and his team randomly assigned 285 teens (mean age, 14.9 years; 50.9% male; 56.1% White) with moderate to severe AD to receive one of the following treatments for 12 weeks: abrocitinib 200 mg plus topical therapy (95); abrocitinib 100 mg plus topical therapy (95); or placebo, which consisted of topical therapy alone (95).
The primary endpoints were an Investigator’s Global Assessment response of clear or almost clear (scores of 0 and 1, respectively), with an improvement of at least 2 points, and an improvement in Eczema Area and Severity Index score of at least 75% at week 12.
Secondary endpoints included an improvement in Peak Pruritus Numerical Rating Scale (PP-NRS) response of at least 4 points at week 12.
The teens who received abrocitinib along with medicated topical therapy showed significant improvement in the severity of their AD at the end of the 12-week period, compared with those in the placebo group.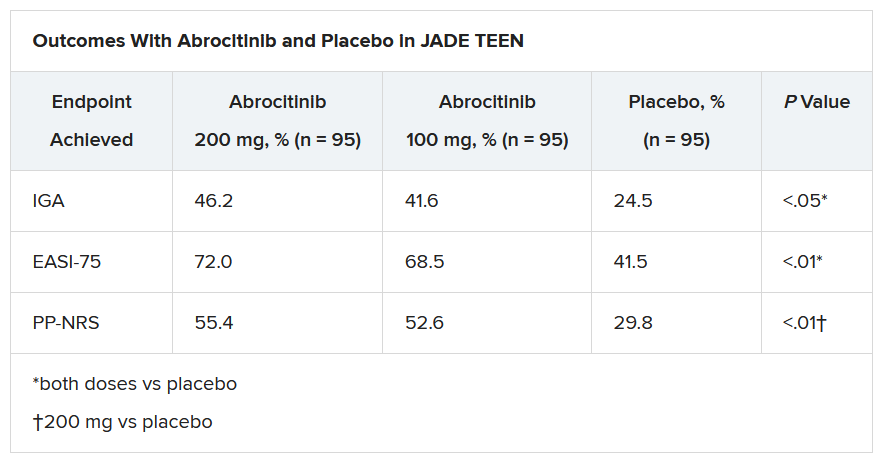
“The percentage of patients achieving essentially no itch, as captured in the fact that more than half of those on the higher dose of abrocitinib made it to no itch, is a new data point and is important to note,” Dr. Eichenfield said. “A lot of the other medicines don’t really get a significant percentage of the population to an itch score of 0 to 1. This drug brought about a rapid and profound itch relief.”
He added: “The results from JADE TEEN extend the drug’s utility in this younger population and show that abrocitinib performs the same with regard to efficacy and safety in the teenagers. Having atopic dermatitis that does not respond to treatment is especially hard for adolescents, but now we know that abrocitinib will be safe and effective and so we now have something to offer these kids.”
“Abrocitinib achieved a good response in this study that was statistically significant, compared to standard treatment,” Jonathan A. Bernstein, MD, professor of medicine at the University of Cincinnati, commented in an interview.
“JAK inhibitors are very promising, and this study adds to that promise. They play an important role in atopic dermatitis, so obviously, teenagers with AD represent an important population,” said Dr. Bernstein, who was not part of the study. “These results are very encouraging, and I think that we will probably see some of these JAK inhibitors approved by the FDA, if not this year, probably next.”
The study was sponsored by Pfizer. Dr. Eichenfield serves as an investigator, speaker, and consultant for Pfizer; and as an investigator, speaker, consultant, and/or is on a data safety monitoring board for AbbVie, Almirall, Amgen, Arcutis, Asana, Dermavant, Dermira, Forte, Galderma, Ichnos/Glenmark, Incyte, LEO, Lilly, L’Oreal, Novartis, Regeneron, Sanofi-Genzyme, and Verrica. Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Abrocitinib, an investigational drug proven to be a safe and effective treatment for moderate to severe atopic dermatitis (AD) in adults 18 years and older, is also safe and effective in patients aged 12-17 years, according to a randomized trial of the oral, once-daily Janus kinase (JAK) 1 selective inhibitor, used in combination with medicated topical therapy.
The results, from the phase 3 JADE TEEN study, were presented during an oral abstract session at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“We’re very excited about the introduction of oral JAKs into our armamentarium for atopic dermatitis,” lead author Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and chief of pediatric and adolescent dermatology, Rady Children’s Hospital, also in San Diego, said in an interview.
AD ranges in severity, and there is a great deal of moderate to severe AD that has a tremendous negative impact on the individual, Dr. Eichenfield said. “Traditionally we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control.”
JAK inhibitors are effective mediators of the inflammation response that occurs in moderate to severe AD. They inhibit the stimulation of the JAK pathway and allow anti-inflammatory effects and therefore have potential, especially in more severe disease, Dr. Eichenfield said.
In the current study, which is a spin-off of the original study that looked at abrocitinib in adults, he and his team randomly assigned 285 teens (mean age, 14.9 years; 50.9% male; 56.1% White) with moderate to severe AD to receive one of the following treatments for 12 weeks: abrocitinib 200 mg plus topical therapy (95); abrocitinib 100 mg plus topical therapy (95); or placebo, which consisted of topical therapy alone (95).
The primary endpoints were an Investigator’s Global Assessment response of clear or almost clear (scores of 0 and 1, respectively), with an improvement of at least 2 points, and an improvement in Eczema Area and Severity Index score of at least 75% at week 12.
Secondary endpoints included an improvement in Peak Pruritus Numerical Rating Scale (PP-NRS) response of at least 4 points at week 12.
The teens who received abrocitinib along with medicated topical therapy showed significant improvement in the severity of their AD at the end of the 12-week period, compared with those in the placebo group.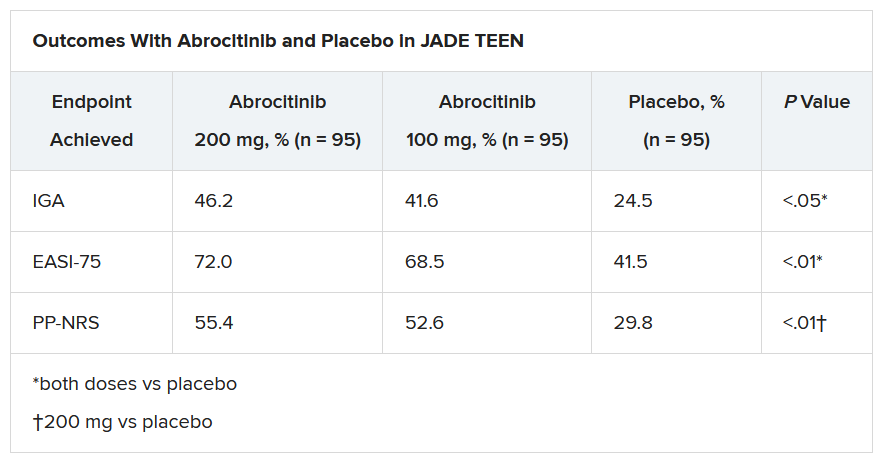
“The percentage of patients achieving essentially no itch, as captured in the fact that more than half of those on the higher dose of abrocitinib made it to no itch, is a new data point and is important to note,” Dr. Eichenfield said. “A lot of the other medicines don’t really get a significant percentage of the population to an itch score of 0 to 1. This drug brought about a rapid and profound itch relief.”
He added: “The results from JADE TEEN extend the drug’s utility in this younger population and show that abrocitinib performs the same with regard to efficacy and safety in the teenagers. Having atopic dermatitis that does not respond to treatment is especially hard for adolescents, but now we know that abrocitinib will be safe and effective and so we now have something to offer these kids.”
“Abrocitinib achieved a good response in this study that was statistically significant, compared to standard treatment,” Jonathan A. Bernstein, MD, professor of medicine at the University of Cincinnati, commented in an interview.
“JAK inhibitors are very promising, and this study adds to that promise. They play an important role in atopic dermatitis, so obviously, teenagers with AD represent an important population,” said Dr. Bernstein, who was not part of the study. “These results are very encouraging, and I think that we will probably see some of these JAK inhibitors approved by the FDA, if not this year, probably next.”
The study was sponsored by Pfizer. Dr. Eichenfield serves as an investigator, speaker, and consultant for Pfizer; and as an investigator, speaker, consultant, and/or is on a data safety monitoring board for AbbVie, Almirall, Amgen, Arcutis, Asana, Dermavant, Dermira, Forte, Galderma, Ichnos/Glenmark, Incyte, LEO, Lilly, L’Oreal, Novartis, Regeneron, Sanofi-Genzyme, and Verrica. Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Slow-growing lesion on eyebrow
A 51-year-old woman presented to the family medicine clinic for evaluation of a slightly tender skin lesion on her left eyebrow. The lesion had been slowly growing for a year.
The patient’s family history included multiple family members with colon or breast cancer and other relatives with pancreatic and prostate cancer. A colonoscopy performed a year earlier on the patient was negative. The patient’s past medical history included hypertension, major depressive disorder, hyperlipidemia, and venous insufficiency. She also had a colon polyp history.
Physical examination of the eyebrow showed a 3-mm papule that was firm on palpation. Dermoscopy of the lesion revealed a yellow papule with

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Sebaceous carcinoma
A rapid teledermatology consultation helped us to determine that this was a sebaceous lesion, but its location and the overlying telangiectasia raised concerns for malignancy. After shared decision-making with the patient, she agreed to proceed with a biopsy. We first made an incision into the lesion, which was hard, demonstrating that it was not cystic. A shave biopsy was then completed. The dermatopathology findings showed clear-cell change consisting of bubbly or foamy cytoplasm, with scalloping of the nuclei, which is characteristic of a sebaceous origin. There were tumor cells that were enlarged with pleomorphism, multiple nucleoli, and scattered mitotic figures. These findings pointed to a diagnosis of sebaceous carcinoma.
Sebaceous carcinomas most commonly manifest on the eyelids. They can originate from the Meibomian glands as well as from pilosebaceous glands at other sites on the body.1 They are rare, accounting for only 1% to 5% of eyelid malignancies, and occur in approximately 2 per 1 million people.1 Tumors can invade locally and metastasize, particularly to surrounding lymph nodes. Periocular pathology may sometimes lead to misdiagnosis, which contributes to a mortality rate that has been reported as high as 20%.1 Suspicion for malignancy may arise due to ulceration, bleeding, pain, or rapid growth.
A lesson in considering the full differential
While sebaceous lesions on the eyelid and eyebrow are often benign, this case underscored the importance of considering the more worrisome elements in the differential. The differential diagnosis for lesions in the area of the eye include the following:
Sebaceous hyperplasia is a common condition (typically among older patients) in which sebaceous glands increase in size and number.2 The classic clinical feature is yellow or skin-colored papules. The lesions typically manifest on the face—particularly on the forehead. They are benign and often have a central umbilication.2
Sebaceous adenomas are benign tumors that may manifest as tan, skin-colored, pink, or yellow papules or nodules.2 The lesions are usually asymptomatic, small, and slow growing.2
Continue to: Basal and squamous cell carcinomas
Basal and squamous cell carcinomas. Basal cell carcinomas often feature translucent lesions on areas of the skin that are exposed to sunlight. These lesions often have slightly rolled border edges or overlying branching telangiectasia and may be nodular.3 Squamous cell carcinomas often feature scaled, reddened patches that may become tender and ulcerate.4
Hordeolums and chalazions. A hordeolum (or stye) is a painful, acute, localized swelling of the eyelid.5 These often develop externally at the lid margin from infection of the follicle. A chalazion is characterized by a persistent, nontender mass that results from small, noninfectious obstruction of the Meibomian glands with secondary granulomatous inflammation.5
Dermoscopy can (and did) help with the Dx
Dermoscopy can help confirm whether a lesion has a sebaceous origin because it would show yellow globules with “crown vessel” telangiectasias that classically do not cross midline.6 Unfortunately, the findings of yellow globules and dermal vessels do not adequately differentiate benign from malignant lesions.6 Carcinomas can manifest in an undifferentiated way early in their course.
Sebaceous carcinomas can be associated with the autosomal dominant Muir-Torre syndrome, a subset of the Lynch syndrome.7,8 Colorectal and genitourinary carcinomas are the most common internal malignancies seen in patients with Muir-Torre syndrome.9
Patients benefit from Mohs surgery
Treatment outcomes for sebaceous carcinoma appear to be improved by Mohs surgery. In a recent review of 1265 patients with early-stage sebaceous carcinomas, Su et al found that 234 patients who were treated with Mohs surgery had improved overall survival, compared with 1031 who were treated with surgical excision.10
Continue to: Our patient
Our patient was referred to a Mohs surgeon who removed the lesion (FIGURES 2 and 3). Given the overall small tumor size, a sentinel lymph node biopsy was not necessary. Because of the patient’s family history, which was suggestive of a genetic predisposition to cancer, she requested a clinical genetics consultation for definitive testing. She went on to pursue genetic testing, which came back negative for Lynch syndrome genes.

The dermatologist recommended yearly skin examination for 5 years for the patient.

1. Kahana A, Pribila HT, Nelson CC, et al. Sebaceous cell carcinoma. In: Levin LA, Albert DM, eds. Ocular Disease: Mechanisms and Management. Saunders/Elsevier; 2010:396-407.
2. Iacobelli J, Harvey NT, Wood BA. Sebaceous lesions of the skin. Pathology. 2017;49:688-697.
3. Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167-179.
4. Smith H, Patel A. When to suspect a non-melanoma skin cancer. BMJ. 2020;368:m692.
5. Sun MT, Huang S, Huilgol SC, et al. Eyelid lesions in general practice. Aust J Gen Pract. 2019;48:509-514.
6. Kim NH, Zell DS, Kolm I, et al. The dermoscopic differential diagnosis of yellow lobularlike structures. Arch Dermatol. 2008;144:962.
7. EG, Bell AJY, Barlow KA. Multiple primary carcinomata of the colon, duodenum, and larynx associated with kerato-acanthomata of the face. Br J Surg. 1967;54:191-195.
8. Torre D. Multiple sebaceous tumors. Arch Dermatol. 1968;98:549-55.
9. Cohen PR, Kohn SR, Kurzrock R. Association of sebaceous gland tumors and internal malignancy: the Muir-Torre syndrome. Am J Med. 1991;90:606-613.
10. Su C, Nguyen KA, Bai HX, et al. Comparison of Mohs surgery and surgical excision in the treatment of localized sebaceous carcinoma. Dermatol Surg. 2019;45:1125-1135.
A 51-year-old woman presented to the family medicine clinic for evaluation of a slightly tender skin lesion on her left eyebrow. The lesion had been slowly growing for a year.
The patient’s family history included multiple family members with colon or breast cancer and other relatives with pancreatic and prostate cancer. A colonoscopy performed a year earlier on the patient was negative. The patient’s past medical history included hypertension, major depressive disorder, hyperlipidemia, and venous insufficiency. She also had a colon polyp history.
Physical examination of the eyebrow showed a 3-mm papule that was firm on palpation. Dermoscopy of the lesion revealed a yellow papule with

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Sebaceous carcinoma
A rapid teledermatology consultation helped us to determine that this was a sebaceous lesion, but its location and the overlying telangiectasia raised concerns for malignancy. After shared decision-making with the patient, she agreed to proceed with a biopsy. We first made an incision into the lesion, which was hard, demonstrating that it was not cystic. A shave biopsy was then completed. The dermatopathology findings showed clear-cell change consisting of bubbly or foamy cytoplasm, with scalloping of the nuclei, which is characteristic of a sebaceous origin. There were tumor cells that were enlarged with pleomorphism, multiple nucleoli, and scattered mitotic figures. These findings pointed to a diagnosis of sebaceous carcinoma.
Sebaceous carcinomas most commonly manifest on the eyelids. They can originate from the Meibomian glands as well as from pilosebaceous glands at other sites on the body.1 They are rare, accounting for only 1% to 5% of eyelid malignancies, and occur in approximately 2 per 1 million people.1 Tumors can invade locally and metastasize, particularly to surrounding lymph nodes. Periocular pathology may sometimes lead to misdiagnosis, which contributes to a mortality rate that has been reported as high as 20%.1 Suspicion for malignancy may arise due to ulceration, bleeding, pain, or rapid growth.
A lesson in considering the full differential
While sebaceous lesions on the eyelid and eyebrow are often benign, this case underscored the importance of considering the more worrisome elements in the differential. The differential diagnosis for lesions in the area of the eye include the following:
Sebaceous hyperplasia is a common condition (typically among older patients) in which sebaceous glands increase in size and number.2 The classic clinical feature is yellow or skin-colored papules. The lesions typically manifest on the face—particularly on the forehead. They are benign and often have a central umbilication.2
Sebaceous adenomas are benign tumors that may manifest as tan, skin-colored, pink, or yellow papules or nodules.2 The lesions are usually asymptomatic, small, and slow growing.2
Continue to: Basal and squamous cell carcinomas
Basal and squamous cell carcinomas. Basal cell carcinomas often feature translucent lesions on areas of the skin that are exposed to sunlight. These lesions often have slightly rolled border edges or overlying branching telangiectasia and may be nodular.3 Squamous cell carcinomas often feature scaled, reddened patches that may become tender and ulcerate.4
Hordeolums and chalazions. A hordeolum (or stye) is a painful, acute, localized swelling of the eyelid.5 These often develop externally at the lid margin from infection of the follicle. A chalazion is characterized by a persistent, nontender mass that results from small, noninfectious obstruction of the Meibomian glands with secondary granulomatous inflammation.5
Dermoscopy can (and did) help with the Dx
Dermoscopy can help confirm whether a lesion has a sebaceous origin because it would show yellow globules with “crown vessel” telangiectasias that classically do not cross midline.6 Unfortunately, the findings of yellow globules and dermal vessels do not adequately differentiate benign from malignant lesions.6 Carcinomas can manifest in an undifferentiated way early in their course.
Sebaceous carcinomas can be associated with the autosomal dominant Muir-Torre syndrome, a subset of the Lynch syndrome.7,8 Colorectal and genitourinary carcinomas are the most common internal malignancies seen in patients with Muir-Torre syndrome.9
Patients benefit from Mohs surgery
Treatment outcomes for sebaceous carcinoma appear to be improved by Mohs surgery. In a recent review of 1265 patients with early-stage sebaceous carcinomas, Su et al found that 234 patients who were treated with Mohs surgery had improved overall survival, compared with 1031 who were treated with surgical excision.10
Continue to: Our patient
Our patient was referred to a Mohs surgeon who removed the lesion (FIGURES 2 and 3). Given the overall small tumor size, a sentinel lymph node biopsy was not necessary. Because of the patient’s family history, which was suggestive of a genetic predisposition to cancer, she requested a clinical genetics consultation for definitive testing. She went on to pursue genetic testing, which came back negative for Lynch syndrome genes.

The dermatologist recommended yearly skin examination for 5 years for the patient.

A 51-year-old woman presented to the family medicine clinic for evaluation of a slightly tender skin lesion on her left eyebrow. The lesion had been slowly growing for a year.
The patient’s family history included multiple family members with colon or breast cancer and other relatives with pancreatic and prostate cancer. A colonoscopy performed a year earlier on the patient was negative. The patient’s past medical history included hypertension, major depressive disorder, hyperlipidemia, and venous insufficiency. She also had a colon polyp history.
Physical examination of the eyebrow showed a 3-mm papule that was firm on palpation. Dermoscopy of the lesion revealed a yellow papule with

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Sebaceous carcinoma
A rapid teledermatology consultation helped us to determine that this was a sebaceous lesion, but its location and the overlying telangiectasia raised concerns for malignancy. After shared decision-making with the patient, she agreed to proceed with a biopsy. We first made an incision into the lesion, which was hard, demonstrating that it was not cystic. A shave biopsy was then completed. The dermatopathology findings showed clear-cell change consisting of bubbly or foamy cytoplasm, with scalloping of the nuclei, which is characteristic of a sebaceous origin. There were tumor cells that were enlarged with pleomorphism, multiple nucleoli, and scattered mitotic figures. These findings pointed to a diagnosis of sebaceous carcinoma.
Sebaceous carcinomas most commonly manifest on the eyelids. They can originate from the Meibomian glands as well as from pilosebaceous glands at other sites on the body.1 They are rare, accounting for only 1% to 5% of eyelid malignancies, and occur in approximately 2 per 1 million people.1 Tumors can invade locally and metastasize, particularly to surrounding lymph nodes. Periocular pathology may sometimes lead to misdiagnosis, which contributes to a mortality rate that has been reported as high as 20%.1 Suspicion for malignancy may arise due to ulceration, bleeding, pain, or rapid growth.
A lesson in considering the full differential
While sebaceous lesions on the eyelid and eyebrow are often benign, this case underscored the importance of considering the more worrisome elements in the differential. The differential diagnosis for lesions in the area of the eye include the following:
Sebaceous hyperplasia is a common condition (typically among older patients) in which sebaceous glands increase in size and number.2 The classic clinical feature is yellow or skin-colored papules. The lesions typically manifest on the face—particularly on the forehead. They are benign and often have a central umbilication.2
Sebaceous adenomas are benign tumors that may manifest as tan, skin-colored, pink, or yellow papules or nodules.2 The lesions are usually asymptomatic, small, and slow growing.2
Continue to: Basal and squamous cell carcinomas
Basal and squamous cell carcinomas. Basal cell carcinomas often feature translucent lesions on areas of the skin that are exposed to sunlight. These lesions often have slightly rolled border edges or overlying branching telangiectasia and may be nodular.3 Squamous cell carcinomas often feature scaled, reddened patches that may become tender and ulcerate.4
Hordeolums and chalazions. A hordeolum (or stye) is a painful, acute, localized swelling of the eyelid.5 These often develop externally at the lid margin from infection of the follicle. A chalazion is characterized by a persistent, nontender mass that results from small, noninfectious obstruction of the Meibomian glands with secondary granulomatous inflammation.5
Dermoscopy can (and did) help with the Dx
Dermoscopy can help confirm whether a lesion has a sebaceous origin because it would show yellow globules with “crown vessel” telangiectasias that classically do not cross midline.6 Unfortunately, the findings of yellow globules and dermal vessels do not adequately differentiate benign from malignant lesions.6 Carcinomas can manifest in an undifferentiated way early in their course.
Sebaceous carcinomas can be associated with the autosomal dominant Muir-Torre syndrome, a subset of the Lynch syndrome.7,8 Colorectal and genitourinary carcinomas are the most common internal malignancies seen in patients with Muir-Torre syndrome.9
Patients benefit from Mohs surgery
Treatment outcomes for sebaceous carcinoma appear to be improved by Mohs surgery. In a recent review of 1265 patients with early-stage sebaceous carcinomas, Su et al found that 234 patients who were treated with Mohs surgery had improved overall survival, compared with 1031 who were treated with surgical excision.10
Continue to: Our patient
Our patient was referred to a Mohs surgeon who removed the lesion (FIGURES 2 and 3). Given the overall small tumor size, a sentinel lymph node biopsy was not necessary. Because of the patient’s family history, which was suggestive of a genetic predisposition to cancer, she requested a clinical genetics consultation for definitive testing. She went on to pursue genetic testing, which came back negative for Lynch syndrome genes.

The dermatologist recommended yearly skin examination for 5 years for the patient.

1. Kahana A, Pribila HT, Nelson CC, et al. Sebaceous cell carcinoma. In: Levin LA, Albert DM, eds. Ocular Disease: Mechanisms and Management. Saunders/Elsevier; 2010:396-407.
2. Iacobelli J, Harvey NT, Wood BA. Sebaceous lesions of the skin. Pathology. 2017;49:688-697.
3. Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167-179.
4. Smith H, Patel A. When to suspect a non-melanoma skin cancer. BMJ. 2020;368:m692.
5. Sun MT, Huang S, Huilgol SC, et al. Eyelid lesions in general practice. Aust J Gen Pract. 2019;48:509-514.
6. Kim NH, Zell DS, Kolm I, et al. The dermoscopic differential diagnosis of yellow lobularlike structures. Arch Dermatol. 2008;144:962.
7. EG, Bell AJY, Barlow KA. Multiple primary carcinomata of the colon, duodenum, and larynx associated with kerato-acanthomata of the face. Br J Surg. 1967;54:191-195.
8. Torre D. Multiple sebaceous tumors. Arch Dermatol. 1968;98:549-55.
9. Cohen PR, Kohn SR, Kurzrock R. Association of sebaceous gland tumors and internal malignancy: the Muir-Torre syndrome. Am J Med. 1991;90:606-613.
10. Su C, Nguyen KA, Bai HX, et al. Comparison of Mohs surgery and surgical excision in the treatment of localized sebaceous carcinoma. Dermatol Surg. 2019;45:1125-1135.
1. Kahana A, Pribila HT, Nelson CC, et al. Sebaceous cell carcinoma. In: Levin LA, Albert DM, eds. Ocular Disease: Mechanisms and Management. Saunders/Elsevier; 2010:396-407.
2. Iacobelli J, Harvey NT, Wood BA. Sebaceous lesions of the skin. Pathology. 2017;49:688-697.
3. Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167-179.
4. Smith H, Patel A. When to suspect a non-melanoma skin cancer. BMJ. 2020;368:m692.
5. Sun MT, Huang S, Huilgol SC, et al. Eyelid lesions in general practice. Aust J Gen Pract. 2019;48:509-514.
6. Kim NH, Zell DS, Kolm I, et al. The dermoscopic differential diagnosis of yellow lobularlike structures. Arch Dermatol. 2008;144:962.
7. EG, Bell AJY, Barlow KA. Multiple primary carcinomata of the colon, duodenum, and larynx associated with kerato-acanthomata of the face. Br J Surg. 1967;54:191-195.
8. Torre D. Multiple sebaceous tumors. Arch Dermatol. 1968;98:549-55.
9. Cohen PR, Kohn SR, Kurzrock R. Association of sebaceous gland tumors and internal malignancy: the Muir-Torre syndrome. Am J Med. 1991;90:606-613.
10. Su C, Nguyen KA, Bai HX, et al. Comparison of Mohs surgery and surgical excision in the treatment of localized sebaceous carcinoma. Dermatol Surg. 2019;45:1125-1135.
Is metformin effective for reducing weight in obese or overweight adolescents?
EVIDENCE SUMMARY
Metformin has modest effects on body weight
A large systematic review and meta-analysis (38 RCTs; n = 2199) published in 2020 evaluated metformin therapy in children and adolescents (including those with metabolic disease, growth problems, and psychological disorders in addition to obesity and overweight).1 Over an average of 6 months, metformin use modestly reduced BMI (weighted mean difference [WMD] = –1.07 kg/m2; 95% CI, –1.43 to –0.72 kg/m2) and body weight (WMD = –2.51 kg; 95% CI, –3.14 to –1.89 kg) for all participants.1
However, the authors also performed a meta-analysis of trials involving obese or overweight youth without other comorbidities. Participants in these trials ranged in age from 7 to 17 years (mean not supplied; most trials, 12-15 years), had a BMI greater than the 95th percentile for age, and took doses of metformin ranging from 1500 to 3000 mg (most trials, 1500-2000 mg/d for 24 weeks).1 In this analysis, metformin reduced body weight (8 trials; n = 616; WMD = –2.06 kg; 95% CI, –3.47 to –0.65 kg) and body fat mass (–1.9%; 95% CI, –3.25% to –0.56%). But it did not reduce BMI (12 trials; n = 826; WMD = –0.76 kg/m2; 95 % CI, –1.61 to 0.08 kg/m2) or improve lean body mass (2 trials; N = 98; WMD = –0.74 kg; 95% CI, –2.4 to 0.91 kg).1
The authors of this meta-analysis did not include an evaluation of the quality of the individual RCTs.
Metformin has benefits but also adverse effects
A 2016 Cochrane systematic review and meta-analysis assessed 8 trials (total n = 543) evaluating metformin vs placebo in adolescents prescribed exercise and lifestyle support.2 This meta-analysis included 4 trials (n = 294) with obese or overweight adolescents that were also included in the newer meta-analysis,1 as well as 4 trials involving obese adolescents with insulin resistance. The authors did not assess the effects of metformin on obese or overweight adolescents separately.
Over 6 months, metformin use reduced BMI (WMD = –1.35 kg/m2; 95% CI –2 to –0.69 kg/m2).2 Metformin commonly produced gastrointestinal symptoms: diarrhea, flatulence (rates not given), and nausea in 15% to 42% compared with 3% to 21% with placebo (no comparison statistic supplied), however rarely to the point of discontinuation (< 5%).2 Nine participants withdrew due to adverse effects: 5 in the metformin group and 4 in the placebo group. The authors rated the quality of the included trials as low to moderate.
An evidence report and systematic review (42 RCTs; total n = 6956) compared the efficacy of several approaches for weight loss in adolescents, including metformin (6 of the 8 RCTs included in the 2020 meta-analysis1) and lifestyle interventions.3 Interventions comprising exercise and diet counseling for > 26 hours over 6 to 12 months produced decreases in BMI (–0.86 kg/m2; 95% CI –1.44 to –0.29 kg/m2) but not weight (–2 kg; 95% CI –3.2 to 1.2 kg).3
Recommendations from others
The US Preventive Services Task Force states that metformin treatment in adolescents who are overweight or obese produces a small reduction in BMI when compared to placebo, but the clinical significance of this reduction is unclear.3
Editor’s takeaway
The idea of using medications for weight loss remains seductive, given how hard it can be for patients to achieve significant, lasting weight loss through lifestyle modification. Evidence suggests that metformin can help in this regard but not enough to recommend it. In addition, metformin therapy is associated with gastrointestinal adverse effects.
1. Sadeghi A, Mousavi SM, Mokhtari T, et al. Metformin therapy reduces obesity indices in children and adolescents: a systematic review and meta-analysis of randomized clinical trials. Child Obes. 2020;16:174-191.
2. Mead E, Atkinson G, Richter B, et al. Drug interventions for the treatment of obesity in children and adolescents. Cochrane Database Syst Rev. 2016;11:CD012436.
3. O’Connor EA, Evans CV, Burda BU, et al. Screening for obesity and intervention for weight management in children and adolescents: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2017;317:2427-2444.
EVIDENCE SUMMARY
Metformin has modest effects on body weight
A large systematic review and meta-analysis (38 RCTs; n = 2199) published in 2020 evaluated metformin therapy in children and adolescents (including those with metabolic disease, growth problems, and psychological disorders in addition to obesity and overweight).1 Over an average of 6 months, metformin use modestly reduced BMI (weighted mean difference [WMD] = –1.07 kg/m2; 95% CI, –1.43 to –0.72 kg/m2) and body weight (WMD = –2.51 kg; 95% CI, –3.14 to –1.89 kg) for all participants.1
However, the authors also performed a meta-analysis of trials involving obese or overweight youth without other comorbidities. Participants in these trials ranged in age from 7 to 17 years (mean not supplied; most trials, 12-15 years), had a BMI greater than the 95th percentile for age, and took doses of metformin ranging from 1500 to 3000 mg (most trials, 1500-2000 mg/d for 24 weeks).1 In this analysis, metformin reduced body weight (8 trials; n = 616; WMD = –2.06 kg; 95% CI, –3.47 to –0.65 kg) and body fat mass (–1.9%; 95% CI, –3.25% to –0.56%). But it did not reduce BMI (12 trials; n = 826; WMD = –0.76 kg/m2; 95 % CI, –1.61 to 0.08 kg/m2) or improve lean body mass (2 trials; N = 98; WMD = –0.74 kg; 95% CI, –2.4 to 0.91 kg).1
The authors of this meta-analysis did not include an evaluation of the quality of the individual RCTs.
Metformin has benefits but also adverse effects
A 2016 Cochrane systematic review and meta-analysis assessed 8 trials (total n = 543) evaluating metformin vs placebo in adolescents prescribed exercise and lifestyle support.2 This meta-analysis included 4 trials (n = 294) with obese or overweight adolescents that were also included in the newer meta-analysis,1 as well as 4 trials involving obese adolescents with insulin resistance. The authors did not assess the effects of metformin on obese or overweight adolescents separately.
Over 6 months, metformin use reduced BMI (WMD = –1.35 kg/m2; 95% CI –2 to –0.69 kg/m2).2 Metformin commonly produced gastrointestinal symptoms: diarrhea, flatulence (rates not given), and nausea in 15% to 42% compared with 3% to 21% with placebo (no comparison statistic supplied), however rarely to the point of discontinuation (< 5%).2 Nine participants withdrew due to adverse effects: 5 in the metformin group and 4 in the placebo group. The authors rated the quality of the included trials as low to moderate.
An evidence report and systematic review (42 RCTs; total n = 6956) compared the efficacy of several approaches for weight loss in adolescents, including metformin (6 of the 8 RCTs included in the 2020 meta-analysis1) and lifestyle interventions.3 Interventions comprising exercise and diet counseling for > 26 hours over 6 to 12 months produced decreases in BMI (–0.86 kg/m2; 95% CI –1.44 to –0.29 kg/m2) but not weight (–2 kg; 95% CI –3.2 to 1.2 kg).3
Recommendations from others
The US Preventive Services Task Force states that metformin treatment in adolescents who are overweight or obese produces a small reduction in BMI when compared to placebo, but the clinical significance of this reduction is unclear.3
Editor’s takeaway
The idea of using medications for weight loss remains seductive, given how hard it can be for patients to achieve significant, lasting weight loss through lifestyle modification. Evidence suggests that metformin can help in this regard but not enough to recommend it. In addition, metformin therapy is associated with gastrointestinal adverse effects.
EVIDENCE SUMMARY
Metformin has modest effects on body weight
A large systematic review and meta-analysis (38 RCTs; n = 2199) published in 2020 evaluated metformin therapy in children and adolescents (including those with metabolic disease, growth problems, and psychological disorders in addition to obesity and overweight).1 Over an average of 6 months, metformin use modestly reduced BMI (weighted mean difference [WMD] = –1.07 kg/m2; 95% CI, –1.43 to –0.72 kg/m2) and body weight (WMD = –2.51 kg; 95% CI, –3.14 to –1.89 kg) for all participants.1
However, the authors also performed a meta-analysis of trials involving obese or overweight youth without other comorbidities. Participants in these trials ranged in age from 7 to 17 years (mean not supplied; most trials, 12-15 years), had a BMI greater than the 95th percentile for age, and took doses of metformin ranging from 1500 to 3000 mg (most trials, 1500-2000 mg/d for 24 weeks).1 In this analysis, metformin reduced body weight (8 trials; n = 616; WMD = –2.06 kg; 95% CI, –3.47 to –0.65 kg) and body fat mass (–1.9%; 95% CI, –3.25% to –0.56%). But it did not reduce BMI (12 trials; n = 826; WMD = –0.76 kg/m2; 95 % CI, –1.61 to 0.08 kg/m2) or improve lean body mass (2 trials; N = 98; WMD = –0.74 kg; 95% CI, –2.4 to 0.91 kg).1
The authors of this meta-analysis did not include an evaluation of the quality of the individual RCTs.
Metformin has benefits but also adverse effects
A 2016 Cochrane systematic review and meta-analysis assessed 8 trials (total n = 543) evaluating metformin vs placebo in adolescents prescribed exercise and lifestyle support.2 This meta-analysis included 4 trials (n = 294) with obese or overweight adolescents that were also included in the newer meta-analysis,1 as well as 4 trials involving obese adolescents with insulin resistance. The authors did not assess the effects of metformin on obese or overweight adolescents separately.
Over 6 months, metformin use reduced BMI (WMD = –1.35 kg/m2; 95% CI –2 to –0.69 kg/m2).2 Metformin commonly produced gastrointestinal symptoms: diarrhea, flatulence (rates not given), and nausea in 15% to 42% compared with 3% to 21% with placebo (no comparison statistic supplied), however rarely to the point of discontinuation (< 5%).2 Nine participants withdrew due to adverse effects: 5 in the metformin group and 4 in the placebo group. The authors rated the quality of the included trials as low to moderate.
An evidence report and systematic review (42 RCTs; total n = 6956) compared the efficacy of several approaches for weight loss in adolescents, including metformin (6 of the 8 RCTs included in the 2020 meta-analysis1) and lifestyle interventions.3 Interventions comprising exercise and diet counseling for > 26 hours over 6 to 12 months produced decreases in BMI (–0.86 kg/m2; 95% CI –1.44 to –0.29 kg/m2) but not weight (–2 kg; 95% CI –3.2 to 1.2 kg).3
Recommendations from others
The US Preventive Services Task Force states that metformin treatment in adolescents who are overweight or obese produces a small reduction in BMI when compared to placebo, but the clinical significance of this reduction is unclear.3
Editor’s takeaway
The idea of using medications for weight loss remains seductive, given how hard it can be for patients to achieve significant, lasting weight loss through lifestyle modification. Evidence suggests that metformin can help in this regard but not enough to recommend it. In addition, metformin therapy is associated with gastrointestinal adverse effects.
1. Sadeghi A, Mousavi SM, Mokhtari T, et al. Metformin therapy reduces obesity indices in children and adolescents: a systematic review and meta-analysis of randomized clinical trials. Child Obes. 2020;16:174-191.
2. Mead E, Atkinson G, Richter B, et al. Drug interventions for the treatment of obesity in children and adolescents. Cochrane Database Syst Rev. 2016;11:CD012436.
3. O’Connor EA, Evans CV, Burda BU, et al. Screening for obesity and intervention for weight management in children and adolescents: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2017;317:2427-2444.
1. Sadeghi A, Mousavi SM, Mokhtari T, et al. Metformin therapy reduces obesity indices in children and adolescents: a systematic review and meta-analysis of randomized clinical trials. Child Obes. 2020;16:174-191.
2. Mead E, Atkinson G, Richter B, et al. Drug interventions for the treatment of obesity in children and adolescents. Cochrane Database Syst Rev. 2016;11:CD012436.
3. O’Connor EA, Evans CV, Burda BU, et al. Screening for obesity and intervention for weight management in children and adolescents: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2017;317:2427-2444.
EVIDENCE-BASED ANSWER:
Yes, to some degree—but it is of uncertain clinical significance. Over a period of 6 months, metformin modestly reduced weight (–2.1 kg) and body fat mass (–1.9%), but not body mass index (BMI) or lean body mass, in adolescents who were overweight or obese. This is comparable to lifestyle interventions (diet and exercise) supported with > 26 hours of counseling, which modestly improved BMI but not weight. (Strength of recommendation [SOR]: A, based on a large meta-analysis of randomized controlled trials [RCTs] of variable quality).





