User login
Polydoctoring: The case against fragmented psychiatric care
How many providers does it take to depersonalize a patient? Nine? 1. A psychiatrist for transcranial magnetic stimulation (TMS). 2. A psychiatrist for ketamine. 3. A psychiatrist who specializes in substance use disorder medication. 4. A psychiatrist for the rest of the psychotropic medication. 5. An alternative medicine provider who prescribes supplements. 6. A therapist for depression who uses cognitive-behavioral therapy. 7. A therapist for posttraumatic stress disorder who uses eye movement desensitization and reprocessing. 8. An addiction counselor. 9. An equine therapist.
This doesn’t include other providers and professionals who likely contribute to one’s mental well-being, including yoga instructors and personal trainers. In addition, any one of those psychiatrists may have one or more nurse practitioners who routinely step in to attend to appointments.
In our uncertain and lonely times, the value of human contact and interaction has become exponentially more precious. I long to see my patients in my private practice office. I am now much more aware of their grounding effect on my life, and I suspect I had a similar grounding effect on theirs. Few things provide me more comfort than sitting on my lounge chair with a curious gaze waiting for the patient to start the visit. I often wonder what makes a patient choose to go see a private practice physician. Yet a common reason offered is, “Wait! You do everything? Therapy and meds if I need them? You’ll see me every week?”
While I am realistic about the need and use of split-care, I have never been enamored with the concept. I think that few medical students choose psychiatry with the goal of referring all psychotherapeutic needs and intervention to “allied mental health providers” as my prior managed care organization liked to refer to psychologists, social workers, marriage and family therapists, and other counselors. I remember particularly as a chief resident being bombarded by complaints of therapists complaining about psychiatry residents. All of their patients’ symptoms allegedly required medication adjustment and residents were supposedly dismissing them. In return, residents would complain that the therapists did not address the psychological manifestations of the patient’s ailments. Herein lies my problem with split-care, it encourages psychotherapy to be about medication management, and medication management to be about psychotherapy.
However, this is not an article against split-treatment. Psychiatrists, for a variety of reasons, are not suited to perform psychotherapy in most management care models. The main reason being that psychiatrists’ time is too expensive to justify the expense, and psychiatrists are (for the most part), the only ones able to prescribe medications for which the wait-list is already long enough. This article is about the absurd levels at which we have fragmented care of certain patients. Split-treatment is relevant in that its negative side effects, we are almost all familiar with, exemplify the problem of the fragmentation of modern psychiatry. In many ways this fragmentation of care is similar to polypharmacy – the premise for each psychotropic intervention may be sound, but the end result is often incoherent.
My main concern with the fragmentation of modern psychiatry stems from my belief that the most important facet of our work is our relationship with our patients. It is the duty we owe them, the attention we give them, the unique nature of interactions. Who among the nine providers is responsible for writing a discharge summary? Who is responsible for calling an emergency contact in a critical situation? Who communicates with the new provider when someone is taken off an insurance panel? Who makes the patient feel cared for? I am often confronted by this situation when TMS or ketamine providers say, “I just give the procedure/medication that was ordered by the referring psychiatrist.” This response disturbs me in that I could not imagine myself being so hands off in the care of a patient. There is an implication of projected immunity and lack of responsibility that bothers me.
But my concerns are also practical. From my forensic experience, I am well aware that the larger the number of providers treating a patient, the larger the number of inconsistent diagnoses, the more likely medication reconciliations are not kept up to date or incorrect, and the more likely intervention recommendations are contrary to one another. A disengaged ketamine provider may not realize that the patient was more recently enrolled in a substance use disorder program, a potential contraindication for ketamine, if not well-abreast of the patient’s continued evolution. A substance use disorder psychiatric specialist may be at odds with a substance use disorder counselor who worries about the message of treating psychiatric symptoms with chemical substances if they don’t communicate.
As with polypharmacy, “polydoctoring” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to specialize, patients still desire and benefit from an intimate and close relationship with one provider who is warm, concerned, and hopeful. Those traits can theoretically be provided by anyone and there is not something inherently wrong with having more than one provider. However, psychiatry would be wise to recognize this concerning trend, especially at a time when we all feel lonely, disconnected, and depersonalized.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
How many providers does it take to depersonalize a patient? Nine? 1. A psychiatrist for transcranial magnetic stimulation (TMS). 2. A psychiatrist for ketamine. 3. A psychiatrist who specializes in substance use disorder medication. 4. A psychiatrist for the rest of the psychotropic medication. 5. An alternative medicine provider who prescribes supplements. 6. A therapist for depression who uses cognitive-behavioral therapy. 7. A therapist for posttraumatic stress disorder who uses eye movement desensitization and reprocessing. 8. An addiction counselor. 9. An equine therapist.
This doesn’t include other providers and professionals who likely contribute to one’s mental well-being, including yoga instructors and personal trainers. In addition, any one of those psychiatrists may have one or more nurse practitioners who routinely step in to attend to appointments.
In our uncertain and lonely times, the value of human contact and interaction has become exponentially more precious. I long to see my patients in my private practice office. I am now much more aware of their grounding effect on my life, and I suspect I had a similar grounding effect on theirs. Few things provide me more comfort than sitting on my lounge chair with a curious gaze waiting for the patient to start the visit. I often wonder what makes a patient choose to go see a private practice physician. Yet a common reason offered is, “Wait! You do everything? Therapy and meds if I need them? You’ll see me every week?”
While I am realistic about the need and use of split-care, I have never been enamored with the concept. I think that few medical students choose psychiatry with the goal of referring all psychotherapeutic needs and intervention to “allied mental health providers” as my prior managed care organization liked to refer to psychologists, social workers, marriage and family therapists, and other counselors. I remember particularly as a chief resident being bombarded by complaints of therapists complaining about psychiatry residents. All of their patients’ symptoms allegedly required medication adjustment and residents were supposedly dismissing them. In return, residents would complain that the therapists did not address the psychological manifestations of the patient’s ailments. Herein lies my problem with split-care, it encourages psychotherapy to be about medication management, and medication management to be about psychotherapy.
However, this is not an article against split-treatment. Psychiatrists, for a variety of reasons, are not suited to perform psychotherapy in most management care models. The main reason being that psychiatrists’ time is too expensive to justify the expense, and psychiatrists are (for the most part), the only ones able to prescribe medications for which the wait-list is already long enough. This article is about the absurd levels at which we have fragmented care of certain patients. Split-treatment is relevant in that its negative side effects, we are almost all familiar with, exemplify the problem of the fragmentation of modern psychiatry. In many ways this fragmentation of care is similar to polypharmacy – the premise for each psychotropic intervention may be sound, but the end result is often incoherent.
My main concern with the fragmentation of modern psychiatry stems from my belief that the most important facet of our work is our relationship with our patients. It is the duty we owe them, the attention we give them, the unique nature of interactions. Who among the nine providers is responsible for writing a discharge summary? Who is responsible for calling an emergency contact in a critical situation? Who communicates with the new provider when someone is taken off an insurance panel? Who makes the patient feel cared for? I am often confronted by this situation when TMS or ketamine providers say, “I just give the procedure/medication that was ordered by the referring psychiatrist.” This response disturbs me in that I could not imagine myself being so hands off in the care of a patient. There is an implication of projected immunity and lack of responsibility that bothers me.
But my concerns are also practical. From my forensic experience, I am well aware that the larger the number of providers treating a patient, the larger the number of inconsistent diagnoses, the more likely medication reconciliations are not kept up to date or incorrect, and the more likely intervention recommendations are contrary to one another. A disengaged ketamine provider may not realize that the patient was more recently enrolled in a substance use disorder program, a potential contraindication for ketamine, if not well-abreast of the patient’s continued evolution. A substance use disorder psychiatric specialist may be at odds with a substance use disorder counselor who worries about the message of treating psychiatric symptoms with chemical substances if they don’t communicate.
As with polypharmacy, “polydoctoring” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to specialize, patients still desire and benefit from an intimate and close relationship with one provider who is warm, concerned, and hopeful. Those traits can theoretically be provided by anyone and there is not something inherently wrong with having more than one provider. However, psychiatry would be wise to recognize this concerning trend, especially at a time when we all feel lonely, disconnected, and depersonalized.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
How many providers does it take to depersonalize a patient? Nine? 1. A psychiatrist for transcranial magnetic stimulation (TMS). 2. A psychiatrist for ketamine. 3. A psychiatrist who specializes in substance use disorder medication. 4. A psychiatrist for the rest of the psychotropic medication. 5. An alternative medicine provider who prescribes supplements. 6. A therapist for depression who uses cognitive-behavioral therapy. 7. A therapist for posttraumatic stress disorder who uses eye movement desensitization and reprocessing. 8. An addiction counselor. 9. An equine therapist.
This doesn’t include other providers and professionals who likely contribute to one’s mental well-being, including yoga instructors and personal trainers. In addition, any one of those psychiatrists may have one or more nurse practitioners who routinely step in to attend to appointments.
In our uncertain and lonely times, the value of human contact and interaction has become exponentially more precious. I long to see my patients in my private practice office. I am now much more aware of their grounding effect on my life, and I suspect I had a similar grounding effect on theirs. Few things provide me more comfort than sitting on my lounge chair with a curious gaze waiting for the patient to start the visit. I often wonder what makes a patient choose to go see a private practice physician. Yet a common reason offered is, “Wait! You do everything? Therapy and meds if I need them? You’ll see me every week?”
While I am realistic about the need and use of split-care, I have never been enamored with the concept. I think that few medical students choose psychiatry with the goal of referring all psychotherapeutic needs and intervention to “allied mental health providers” as my prior managed care organization liked to refer to psychologists, social workers, marriage and family therapists, and other counselors. I remember particularly as a chief resident being bombarded by complaints of therapists complaining about psychiatry residents. All of their patients’ symptoms allegedly required medication adjustment and residents were supposedly dismissing them. In return, residents would complain that the therapists did not address the psychological manifestations of the patient’s ailments. Herein lies my problem with split-care, it encourages psychotherapy to be about medication management, and medication management to be about psychotherapy.
However, this is not an article against split-treatment. Psychiatrists, for a variety of reasons, are not suited to perform psychotherapy in most management care models. The main reason being that psychiatrists’ time is too expensive to justify the expense, and psychiatrists are (for the most part), the only ones able to prescribe medications for which the wait-list is already long enough. This article is about the absurd levels at which we have fragmented care of certain patients. Split-treatment is relevant in that its negative side effects, we are almost all familiar with, exemplify the problem of the fragmentation of modern psychiatry. In many ways this fragmentation of care is similar to polypharmacy – the premise for each psychotropic intervention may be sound, but the end result is often incoherent.
My main concern with the fragmentation of modern psychiatry stems from my belief that the most important facet of our work is our relationship with our patients. It is the duty we owe them, the attention we give them, the unique nature of interactions. Who among the nine providers is responsible for writing a discharge summary? Who is responsible for calling an emergency contact in a critical situation? Who communicates with the new provider when someone is taken off an insurance panel? Who makes the patient feel cared for? I am often confronted by this situation when TMS or ketamine providers say, “I just give the procedure/medication that was ordered by the referring psychiatrist.” This response disturbs me in that I could not imagine myself being so hands off in the care of a patient. There is an implication of projected immunity and lack of responsibility that bothers me.
But my concerns are also practical. From my forensic experience, I am well aware that the larger the number of providers treating a patient, the larger the number of inconsistent diagnoses, the more likely medication reconciliations are not kept up to date or incorrect, and the more likely intervention recommendations are contrary to one another. A disengaged ketamine provider may not realize that the patient was more recently enrolled in a substance use disorder program, a potential contraindication for ketamine, if not well-abreast of the patient’s continued evolution. A substance use disorder psychiatric specialist may be at odds with a substance use disorder counselor who worries about the message of treating psychiatric symptoms with chemical substances if they don’t communicate.
As with polypharmacy, “polydoctoring” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to specialize, patients still desire and benefit from an intimate and close relationship with one provider who is warm, concerned, and hopeful. Those traits can theoretically be provided by anyone and there is not something inherently wrong with having more than one provider. However, psychiatry would be wise to recognize this concerning trend, especially at a time when we all feel lonely, disconnected, and depersonalized.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
AMA president: Biden team must create national pandemic strategy
The incoming Biden administration must formulate an effective national strategy for the COVID-19 pandemic, Susan R. Bailey, MD, president of the American Medical Association (AMA), said in a speech delivered Jan. 12 at the National Press Club in Washington.
Dr. Bailey noted that America’s fight against the pandemic is in a critical phase, as evidenced by the escalation in cases, hospitalizations, and deaths in recent weeks. Emergency departments and ICUs are overwhelmed; many frontline clinicians are burned out; and the state- and local-level mechanisms for vaccine distribution have been slow and inconsistent, she said.
“The most important lesson for this moment, and for the year ahead, is that leaving state and local officials to shoulder this burden alone without adequate support from the federal government is not going to work,” Dr. Bailey emphasized.
She called on the Biden administration, which takes over on Jan. 20, to “provide states and local jurisdictions with additional resources, guidance, and support to enable rapid distribution and administration of vaccines.”
In addition, she said, the incoming administration needs to develop a more robust, national strategy for continued COVID-19 testing and PPE production “by tapping into the full powers of the Defense Production Act.”
Biden vaccine distribution policy
In a question-and-answer period following her speech, however, Dr. Bailey said she opposed the president-elect’s decision to release nearly all available vaccine supplies immediately, rather than hold back some doses for the second shots that the Pfizer and Moderna vaccines require. On Jan. 12, the Trump administration announced that it plans to do the same thing.
“We’re a little bit concerned about the announcement that [the Department of Health and Human Services] will not hold back vaccine doses to make sure that everyone who’s gotten their first dose will have a second dose in reserve,” Dr. Bailey said. “We don’t have adequate data to tell us that one dose is sufficient – we don’t think it is – and how long you can wait for the second dose without losing the benefits of the first dose.”
She added that it’s not recommended that people mix the two vaccines in the first and second doses. “Since the Pfizer vaccine has such rigid storage requirements, I want to make sure there’s plenty of vaccine for frontline health care workers who got the Pfizer vaccine because it was the first one to come out in December. I want to make sure they get their second dose on time and [do] not have to wait.”
Dr. Bailey said she hoped there will be plenty of vaccine supply. But she suggested that state and local health authorities be in communication with the federal government about whether there will be enough vaccine to guarantee people can get both doses.
Bolstering public health
In her speech, Dr. Bailey outlined five areas in which steps should be taken to improve the health system so that it isn’t overwhelmed the next time the United States has a public health crisis:
- Restore trust in science and science-based decision making. Make sure that scientific institutions such as the Centers for Disease Control and Prevention and the Food and Drug Administration are “free from political pressure, and that their actions are guided by the best available scientific evidence.”
- Ensure that the health system provides all Americans with affordable access to comprehensive health care. Dr. Bailey wasn’t talking about Medicare for All; she suggested that perhaps there be a second enrollment period for the Affordable Care Act’s individual insurance exchanges.
- Work to remove health care inequities that have hurt communities of color, who have been disproportionately impacted by the pandemic. She referred to a recent AMA that recognized racism as a public health threat.
- Improve public health domestically and globally. Among other things, she noted, the public health infrastructure needs to be revitalized after “decades of disinvestment and neglect,” which has contributed to the slow vaccine rollout.
- Recognize the global health community and restore America’s leadership in global efforts to combat disease, which are critical to preventing future threats. She praised President-Elect Biden for his promise that the United States will rejoin the World Health Organization.
At several points in her presentation, Dr. Bailey rejected political interference with science and health care. Among other things, she said public health could be improved by protecting the doctor-patient relationship from political interference.
Answering a question about how to separate politics from the pandemic, she replied, “The key is in sticking to the science and listening to our public health authorities. They all have to deliver the same message. Also, leaders at all levels, including in our communities, our schools, churches and college campuses, should wear masks and socially distance. This isn’t about anything other than the desire to get out of the pandemic and get our country on the right track again. Masks shouldn’t be political. Going back to school shouldn’t be political. Taking a certain medication or not shouldn’t be political. We need to stick to the science and listen to our public health authorities. That’s the quickest way out.”
Asked when she thought that life might get back to normal again in the United States, Dr. Bailey said a lot depends on the extent of vaccine uptake and how much self-discipline people exhibit in following public health advice. “I think we’re looking at the end of this year. I’m hopeful that by fall, things will have opened up quite a bit as the Venn diagrams of those who’ve gotten vaccines grow larger.”
A version of this article first appeared on Medscape.com.
The incoming Biden administration must formulate an effective national strategy for the COVID-19 pandemic, Susan R. Bailey, MD, president of the American Medical Association (AMA), said in a speech delivered Jan. 12 at the National Press Club in Washington.
Dr. Bailey noted that America’s fight against the pandemic is in a critical phase, as evidenced by the escalation in cases, hospitalizations, and deaths in recent weeks. Emergency departments and ICUs are overwhelmed; many frontline clinicians are burned out; and the state- and local-level mechanisms for vaccine distribution have been slow and inconsistent, she said.
“The most important lesson for this moment, and for the year ahead, is that leaving state and local officials to shoulder this burden alone without adequate support from the federal government is not going to work,” Dr. Bailey emphasized.
She called on the Biden administration, which takes over on Jan. 20, to “provide states and local jurisdictions with additional resources, guidance, and support to enable rapid distribution and administration of vaccines.”
In addition, she said, the incoming administration needs to develop a more robust, national strategy for continued COVID-19 testing and PPE production “by tapping into the full powers of the Defense Production Act.”
Biden vaccine distribution policy
In a question-and-answer period following her speech, however, Dr. Bailey said she opposed the president-elect’s decision to release nearly all available vaccine supplies immediately, rather than hold back some doses for the second shots that the Pfizer and Moderna vaccines require. On Jan. 12, the Trump administration announced that it plans to do the same thing.
“We’re a little bit concerned about the announcement that [the Department of Health and Human Services] will not hold back vaccine doses to make sure that everyone who’s gotten their first dose will have a second dose in reserve,” Dr. Bailey said. “We don’t have adequate data to tell us that one dose is sufficient – we don’t think it is – and how long you can wait for the second dose without losing the benefits of the first dose.”
She added that it’s not recommended that people mix the two vaccines in the first and second doses. “Since the Pfizer vaccine has such rigid storage requirements, I want to make sure there’s plenty of vaccine for frontline health care workers who got the Pfizer vaccine because it was the first one to come out in December. I want to make sure they get their second dose on time and [do] not have to wait.”
Dr. Bailey said she hoped there will be plenty of vaccine supply. But she suggested that state and local health authorities be in communication with the federal government about whether there will be enough vaccine to guarantee people can get both doses.
Bolstering public health
In her speech, Dr. Bailey outlined five areas in which steps should be taken to improve the health system so that it isn’t overwhelmed the next time the United States has a public health crisis:
- Restore trust in science and science-based decision making. Make sure that scientific institutions such as the Centers for Disease Control and Prevention and the Food and Drug Administration are “free from political pressure, and that their actions are guided by the best available scientific evidence.”
- Ensure that the health system provides all Americans with affordable access to comprehensive health care. Dr. Bailey wasn’t talking about Medicare for All; she suggested that perhaps there be a second enrollment period for the Affordable Care Act’s individual insurance exchanges.
- Work to remove health care inequities that have hurt communities of color, who have been disproportionately impacted by the pandemic. She referred to a recent AMA that recognized racism as a public health threat.
- Improve public health domestically and globally. Among other things, she noted, the public health infrastructure needs to be revitalized after “decades of disinvestment and neglect,” which has contributed to the slow vaccine rollout.
- Recognize the global health community and restore America’s leadership in global efforts to combat disease, which are critical to preventing future threats. She praised President-Elect Biden for his promise that the United States will rejoin the World Health Organization.
At several points in her presentation, Dr. Bailey rejected political interference with science and health care. Among other things, she said public health could be improved by protecting the doctor-patient relationship from political interference.
Answering a question about how to separate politics from the pandemic, she replied, “The key is in sticking to the science and listening to our public health authorities. They all have to deliver the same message. Also, leaders at all levels, including in our communities, our schools, churches and college campuses, should wear masks and socially distance. This isn’t about anything other than the desire to get out of the pandemic and get our country on the right track again. Masks shouldn’t be political. Going back to school shouldn’t be political. Taking a certain medication or not shouldn’t be political. We need to stick to the science and listen to our public health authorities. That’s the quickest way out.”
Asked when she thought that life might get back to normal again in the United States, Dr. Bailey said a lot depends on the extent of vaccine uptake and how much self-discipline people exhibit in following public health advice. “I think we’re looking at the end of this year. I’m hopeful that by fall, things will have opened up quite a bit as the Venn diagrams of those who’ve gotten vaccines grow larger.”
A version of this article first appeared on Medscape.com.
The incoming Biden administration must formulate an effective national strategy for the COVID-19 pandemic, Susan R. Bailey, MD, president of the American Medical Association (AMA), said in a speech delivered Jan. 12 at the National Press Club in Washington.
Dr. Bailey noted that America’s fight against the pandemic is in a critical phase, as evidenced by the escalation in cases, hospitalizations, and deaths in recent weeks. Emergency departments and ICUs are overwhelmed; many frontline clinicians are burned out; and the state- and local-level mechanisms for vaccine distribution have been slow and inconsistent, she said.
“The most important lesson for this moment, and for the year ahead, is that leaving state and local officials to shoulder this burden alone without adequate support from the federal government is not going to work,” Dr. Bailey emphasized.
She called on the Biden administration, which takes over on Jan. 20, to “provide states and local jurisdictions with additional resources, guidance, and support to enable rapid distribution and administration of vaccines.”
In addition, she said, the incoming administration needs to develop a more robust, national strategy for continued COVID-19 testing and PPE production “by tapping into the full powers of the Defense Production Act.”
Biden vaccine distribution policy
In a question-and-answer period following her speech, however, Dr. Bailey said she opposed the president-elect’s decision to release nearly all available vaccine supplies immediately, rather than hold back some doses for the second shots that the Pfizer and Moderna vaccines require. On Jan. 12, the Trump administration announced that it plans to do the same thing.
“We’re a little bit concerned about the announcement that [the Department of Health and Human Services] will not hold back vaccine doses to make sure that everyone who’s gotten their first dose will have a second dose in reserve,” Dr. Bailey said. “We don’t have adequate data to tell us that one dose is sufficient – we don’t think it is – and how long you can wait for the second dose without losing the benefits of the first dose.”
She added that it’s not recommended that people mix the two vaccines in the first and second doses. “Since the Pfizer vaccine has such rigid storage requirements, I want to make sure there’s plenty of vaccine for frontline health care workers who got the Pfizer vaccine because it was the first one to come out in December. I want to make sure they get their second dose on time and [do] not have to wait.”
Dr. Bailey said she hoped there will be plenty of vaccine supply. But she suggested that state and local health authorities be in communication with the federal government about whether there will be enough vaccine to guarantee people can get both doses.
Bolstering public health
In her speech, Dr. Bailey outlined five areas in which steps should be taken to improve the health system so that it isn’t overwhelmed the next time the United States has a public health crisis:
- Restore trust in science and science-based decision making. Make sure that scientific institutions such as the Centers for Disease Control and Prevention and the Food and Drug Administration are “free from political pressure, and that their actions are guided by the best available scientific evidence.”
- Ensure that the health system provides all Americans with affordable access to comprehensive health care. Dr. Bailey wasn’t talking about Medicare for All; she suggested that perhaps there be a second enrollment period for the Affordable Care Act’s individual insurance exchanges.
- Work to remove health care inequities that have hurt communities of color, who have been disproportionately impacted by the pandemic. She referred to a recent AMA that recognized racism as a public health threat.
- Improve public health domestically and globally. Among other things, she noted, the public health infrastructure needs to be revitalized after “decades of disinvestment and neglect,” which has contributed to the slow vaccine rollout.
- Recognize the global health community and restore America’s leadership in global efforts to combat disease, which are critical to preventing future threats. She praised President-Elect Biden for his promise that the United States will rejoin the World Health Organization.
At several points in her presentation, Dr. Bailey rejected political interference with science and health care. Among other things, she said public health could be improved by protecting the doctor-patient relationship from political interference.
Answering a question about how to separate politics from the pandemic, she replied, “The key is in sticking to the science and listening to our public health authorities. They all have to deliver the same message. Also, leaders at all levels, including in our communities, our schools, churches and college campuses, should wear masks and socially distance. This isn’t about anything other than the desire to get out of the pandemic and get our country on the right track again. Masks shouldn’t be political. Going back to school shouldn’t be political. Taking a certain medication or not shouldn’t be political. We need to stick to the science and listen to our public health authorities. That’s the quickest way out.”
Asked when she thought that life might get back to normal again in the United States, Dr. Bailey said a lot depends on the extent of vaccine uptake and how much self-discipline people exhibit in following public health advice. “I think we’re looking at the end of this year. I’m hopeful that by fall, things will have opened up quite a bit as the Venn diagrams of those who’ve gotten vaccines grow larger.”
A version of this article first appeared on Medscape.com.
A 67-year-old White woman presented with 2 weeks of bullae on her lower feet
Bullous arthropod assault
Insect-bite reactions are commonly seen in dermatology practice. Most often, they present as pruritic papules. Vesicles and bullae can be seen as well but are less common. Flea bites are the most likely to cause blisters.1 Lesions may be grouped or in a linear pattern. Children tend to have more severe reactions than adults. Body temperature and odor may make some people more susceptible than others to bites. Of note, patients with chronic lymphocytic leukemia tend to have more severe, bullous reactions.2 The differential diagnosis includes bullous pemphigoid, bullous impetigo, bullous tinea, bullous fixed drug, and bullous diabeticorum.
In general, bullous arthropod reactions begin as intraepidermal vesicles that can progress to subepidermal blisters. Eosinophils can be present. Flame figures are often seen in patients with chronic lymphocytic leukemia.3 Histopathology in this patient revealed a subepidermal vesicular dermatitis with minimal inflammation. Periodic acid–Schiff (PAS) stain was negative. Direct immunofluorescence was negative for IgG, C3, IgA, IgM, and fibrinogen. Of note, systemic steroids may alter histologic and immunologic findings.
Bullous pemphigoid is an autoimmune blistering disorder where patients develop widespread tense bullae. Histopathology revealed a subepidermal blister with numerous eosinophils. Direct immunofluorescence study of perilesional skin showed linear IgG and C3 deposits at the basal membrane level. Systemic steroids, tetracyclines, and immunosuppressive medications are a mainstay of treatment. In bullous impetigo, the toxin of Staphylococcus aureus causes blister formation. It is treated with antistaphylococcal antibiotics. Bullous tinea reveals hyphae with PAS staining. Topical or systemic antifungals are used for treatment.
In severe cases, systemic steroids can be used as well. Bacterial culture was negative in this patient. The patient was treated with 1 week of oral prednisone prior to biopsy and topical betamethasone ointment. Her lesions subsequently resolved with no recurrence.
This case and photo were submitted by Brooke Resh Sateesh, MD, San Diego Family Dermatology.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1-3. “Dermatology” 2nd ed. (Maryland Heights, Mo.: Mosby, 2008).
Bullous arthropod assault
Insect-bite reactions are commonly seen in dermatology practice. Most often, they present as pruritic papules. Vesicles and bullae can be seen as well but are less common. Flea bites are the most likely to cause blisters.1 Lesions may be grouped or in a linear pattern. Children tend to have more severe reactions than adults. Body temperature and odor may make some people more susceptible than others to bites. Of note, patients with chronic lymphocytic leukemia tend to have more severe, bullous reactions.2 The differential diagnosis includes bullous pemphigoid, bullous impetigo, bullous tinea, bullous fixed drug, and bullous diabeticorum.
In general, bullous arthropod reactions begin as intraepidermal vesicles that can progress to subepidermal blisters. Eosinophils can be present. Flame figures are often seen in patients with chronic lymphocytic leukemia.3 Histopathology in this patient revealed a subepidermal vesicular dermatitis with minimal inflammation. Periodic acid–Schiff (PAS) stain was negative. Direct immunofluorescence was negative for IgG, C3, IgA, IgM, and fibrinogen. Of note, systemic steroids may alter histologic and immunologic findings.
Bullous pemphigoid is an autoimmune blistering disorder where patients develop widespread tense bullae. Histopathology revealed a subepidermal blister with numerous eosinophils. Direct immunofluorescence study of perilesional skin showed linear IgG and C3 deposits at the basal membrane level. Systemic steroids, tetracyclines, and immunosuppressive medications are a mainstay of treatment. In bullous impetigo, the toxin of Staphylococcus aureus causes blister formation. It is treated with antistaphylococcal antibiotics. Bullous tinea reveals hyphae with PAS staining. Topical or systemic antifungals are used for treatment.
In severe cases, systemic steroids can be used as well. Bacterial culture was negative in this patient. The patient was treated with 1 week of oral prednisone prior to biopsy and topical betamethasone ointment. Her lesions subsequently resolved with no recurrence.
This case and photo were submitted by Brooke Resh Sateesh, MD, San Diego Family Dermatology.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1-3. “Dermatology” 2nd ed. (Maryland Heights, Mo.: Mosby, 2008).
Bullous arthropod assault
Insect-bite reactions are commonly seen in dermatology practice. Most often, they present as pruritic papules. Vesicles and bullae can be seen as well but are less common. Flea bites are the most likely to cause blisters.1 Lesions may be grouped or in a linear pattern. Children tend to have more severe reactions than adults. Body temperature and odor may make some people more susceptible than others to bites. Of note, patients with chronic lymphocytic leukemia tend to have more severe, bullous reactions.2 The differential diagnosis includes bullous pemphigoid, bullous impetigo, bullous tinea, bullous fixed drug, and bullous diabeticorum.
In general, bullous arthropod reactions begin as intraepidermal vesicles that can progress to subepidermal blisters. Eosinophils can be present. Flame figures are often seen in patients with chronic lymphocytic leukemia.3 Histopathology in this patient revealed a subepidermal vesicular dermatitis with minimal inflammation. Periodic acid–Schiff (PAS) stain was negative. Direct immunofluorescence was negative for IgG, C3, IgA, IgM, and fibrinogen. Of note, systemic steroids may alter histologic and immunologic findings.
Bullous pemphigoid is an autoimmune blistering disorder where patients develop widespread tense bullae. Histopathology revealed a subepidermal blister with numerous eosinophils. Direct immunofluorescence study of perilesional skin showed linear IgG and C3 deposits at the basal membrane level. Systemic steroids, tetracyclines, and immunosuppressive medications are a mainstay of treatment. In bullous impetigo, the toxin of Staphylococcus aureus causes blister formation. It is treated with antistaphylococcal antibiotics. Bullous tinea reveals hyphae with PAS staining. Topical or systemic antifungals are used for treatment.
In severe cases, systemic steroids can be used as well. Bacterial culture was negative in this patient. The patient was treated with 1 week of oral prednisone prior to biopsy and topical betamethasone ointment. Her lesions subsequently resolved with no recurrence.
This case and photo were submitted by Brooke Resh Sateesh, MD, San Diego Family Dermatology.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1-3. “Dermatology” 2nd ed. (Maryland Heights, Mo.: Mosby, 2008).
Feds to states: Give COVID-19 vaccine to 65+ and those with comorbidities
Federal health officials are urging states to vaccinate all Americans over age 65 and those aged 16-64 who have a documented underlying health condition that makes them more vulnerable to COVID-19.
U.S. Department of Health and Human Services (HHS) Secretary Alex Azar and Centers for Disease Control and Prevention Director Robert Redfield, MD, made the recommendation in a briefing with reporters on Jan. 12, saying that the current vaccine supply was sufficient to meet demand for the next phase of immunization as recommended by the CDC’s Advisory Committee on Immunization Practices.
“We are ready for a transition that we outlined last September in the playbook we sent to states,” Mr. Azar said. Both he and U.S. Army General Gustave F. Perna, chief operations officer for Operation Warp Speed, said that confidence in the distribution system had led to the decision to urge wider access.
The federal government will also increase the number of sites eligible to receive vaccine – including some 13,000 federally qualified community health centers – and will not keep doses in reserve as insurance against issues that might prevent people from receiving a second dose on a timely basis.
“We don’t need to hold back reserve doses,” Mr. Azar said, noting that if there were any “glitches in production” the federal government would move to fulfill obligations for second doses first and delay initial doses.
Azar: Use it or lose it
In a move that is sure to generate pushback, Mr. Azar said that states that don’t quickly administer vaccines will receive fewer doses in the future. That policy will not go into effect until later in February, which leaves open the possibility that it could be reversed by the incoming Biden administration.
“We have too much vaccine sitting in freezers at hospitals with hospitals not using it,” said Mr. Azar, who also blamed the slow administration process on a reporting lag and states being what he called “overly prescriptive” in who has been eligible to receive a shot.
“I would rather have people working to get appointments to get vaccinated than having vaccine going to waste sitting in freezers,” he told reporters.
Mr. Azar had already been pushing for broader vaccination, telling states to do so in an Operation Warp Speed briefing on Jan. 6. At that briefing, he also said that the federal government would be stepping up vaccination through an “early launch” of a federal partnership with 19 pharmacy chains, which will let states allocate vaccines directly to some 40,000 pharmacy sites.
Gen. Perna said during the Jan. 12 briefing that the aim is to further expand that to some 70,000 locations total.
The CDC reported that as of Jan. 11 some 25.4 million doses have been distributed, with 8.9 million administered. An additional 4.2 million doses were distributed to long-term care facilities, and 937,000 residents and staff have received a dose.
“Pace of administration”
Alaska, Connecticut, North Dakota, South Dakota, the District of Columbia, West Virginia, and the Northern Mariana Islands have administered the most vaccines per capita, according to the CDC. But even these locations have immunized only 4%-5% of their populations, the New York Times reports. At the bottom: Alabama, Arizona, Arkansas, Georgia, Mississippi, and South Carolina.
The federal government can encourage but not require states to move on to new phases of vaccination.
“States ultimately determine how they will proceed with vaccination,” said Marcus Plescia, MD, MPH, chief medical officer for the Association of State and Territorial Health Officials. “Most will be cautious about assuring there are doses for those needing a second dose,” he said in an interview.
Dr. Plescia said that ensuring a second dose is available is especially important for health care workers “who need to be confident that they are protected and not inadvertently transmitting the disease themselves.”
He added that “once we reach a steady state of supply and administration, the rate-limiting factor will be supply of vaccine.”
That supply could now be threatened if states don’t comply with a just-announced federal action that will change how doses are allocated.
Beginning in late February, vaccine allocations to states will be based on “the pace of administration reported by states,” and the size of the 65-and-older population, said Mr. Azar, who has previously criticized New York Governor Andrew Cuomo for fining hospitals that didn’t use up vaccine supply within a week.
“This new system gives states a strong incentive to ensure that all vaccinations are being promptly reported, which they currently are not,” he said.
Currently, allocations are based on a state’s or territory’s population.
Prepandemic, states were required to report vaccinations within 30 days. Since COVID-19 vaccines became available, the CDC has required reporting of shots within 72 hours.
Dr. Redfield said the requirement has caused some difficulty, and that the CDC is investigating why some states have reported using only 15% of doses while others have used 80%.
States have been scrambling to ramp up vaccinations.
Just ahead of the federal briefing, Gov. Cuomo tweeted that New York would be opening up vaccinations to anyone older than 65.
The Associated Press is reporting that some states have started mass vaccination sites.
Arizona has begun operating a 24/7 appointment-only vaccination program at State Farm Stadium outside of Phoenix, with the aim of immunizing 6,000 people each day, according to local radio station KJZZ.
California and Florida have also taken steps to use stadiums, while Michigan, New Jersey, New York, and Texas will use convention centers and fairgrounds, Axios has reported.
In Florida, Palm Beach County Health Director Alina Alonso, MD, told county commissioners on Jan. 12 that there isn’t enough vaccine to meet demand, WPTV reported. “We need to realize that there’s a shortage of vaccine. So it’s not the plan, it’s not our ability to do it. It’s simply supply and demand at this point,” Dr. Alonso said, according to the TV station report.
A version of this article first appeared on Medscape.com.
Federal health officials are urging states to vaccinate all Americans over age 65 and those aged 16-64 who have a documented underlying health condition that makes them more vulnerable to COVID-19.
U.S. Department of Health and Human Services (HHS) Secretary Alex Azar and Centers for Disease Control and Prevention Director Robert Redfield, MD, made the recommendation in a briefing with reporters on Jan. 12, saying that the current vaccine supply was sufficient to meet demand for the next phase of immunization as recommended by the CDC’s Advisory Committee on Immunization Practices.
“We are ready for a transition that we outlined last September in the playbook we sent to states,” Mr. Azar said. Both he and U.S. Army General Gustave F. Perna, chief operations officer for Operation Warp Speed, said that confidence in the distribution system had led to the decision to urge wider access.
The federal government will also increase the number of sites eligible to receive vaccine – including some 13,000 federally qualified community health centers – and will not keep doses in reserve as insurance against issues that might prevent people from receiving a second dose on a timely basis.
“We don’t need to hold back reserve doses,” Mr. Azar said, noting that if there were any “glitches in production” the federal government would move to fulfill obligations for second doses first and delay initial doses.
Azar: Use it or lose it
In a move that is sure to generate pushback, Mr. Azar said that states that don’t quickly administer vaccines will receive fewer doses in the future. That policy will not go into effect until later in February, which leaves open the possibility that it could be reversed by the incoming Biden administration.
“We have too much vaccine sitting in freezers at hospitals with hospitals not using it,” said Mr. Azar, who also blamed the slow administration process on a reporting lag and states being what he called “overly prescriptive” in who has been eligible to receive a shot.
“I would rather have people working to get appointments to get vaccinated than having vaccine going to waste sitting in freezers,” he told reporters.
Mr. Azar had already been pushing for broader vaccination, telling states to do so in an Operation Warp Speed briefing on Jan. 6. At that briefing, he also said that the federal government would be stepping up vaccination through an “early launch” of a federal partnership with 19 pharmacy chains, which will let states allocate vaccines directly to some 40,000 pharmacy sites.
Gen. Perna said during the Jan. 12 briefing that the aim is to further expand that to some 70,000 locations total.
The CDC reported that as of Jan. 11 some 25.4 million doses have been distributed, with 8.9 million administered. An additional 4.2 million doses were distributed to long-term care facilities, and 937,000 residents and staff have received a dose.
“Pace of administration”
Alaska, Connecticut, North Dakota, South Dakota, the District of Columbia, West Virginia, and the Northern Mariana Islands have administered the most vaccines per capita, according to the CDC. But even these locations have immunized only 4%-5% of their populations, the New York Times reports. At the bottom: Alabama, Arizona, Arkansas, Georgia, Mississippi, and South Carolina.
The federal government can encourage but not require states to move on to new phases of vaccination.
“States ultimately determine how they will proceed with vaccination,” said Marcus Plescia, MD, MPH, chief medical officer for the Association of State and Territorial Health Officials. “Most will be cautious about assuring there are doses for those needing a second dose,” he said in an interview.
Dr. Plescia said that ensuring a second dose is available is especially important for health care workers “who need to be confident that they are protected and not inadvertently transmitting the disease themselves.”
He added that “once we reach a steady state of supply and administration, the rate-limiting factor will be supply of vaccine.”
That supply could now be threatened if states don’t comply with a just-announced federal action that will change how doses are allocated.
Beginning in late February, vaccine allocations to states will be based on “the pace of administration reported by states,” and the size of the 65-and-older population, said Mr. Azar, who has previously criticized New York Governor Andrew Cuomo for fining hospitals that didn’t use up vaccine supply within a week.
“This new system gives states a strong incentive to ensure that all vaccinations are being promptly reported, which they currently are not,” he said.
Currently, allocations are based on a state’s or territory’s population.
Prepandemic, states were required to report vaccinations within 30 days. Since COVID-19 vaccines became available, the CDC has required reporting of shots within 72 hours.
Dr. Redfield said the requirement has caused some difficulty, and that the CDC is investigating why some states have reported using only 15% of doses while others have used 80%.
States have been scrambling to ramp up vaccinations.
Just ahead of the federal briefing, Gov. Cuomo tweeted that New York would be opening up vaccinations to anyone older than 65.
The Associated Press is reporting that some states have started mass vaccination sites.
Arizona has begun operating a 24/7 appointment-only vaccination program at State Farm Stadium outside of Phoenix, with the aim of immunizing 6,000 people each day, according to local radio station KJZZ.
California and Florida have also taken steps to use stadiums, while Michigan, New Jersey, New York, and Texas will use convention centers and fairgrounds, Axios has reported.
In Florida, Palm Beach County Health Director Alina Alonso, MD, told county commissioners on Jan. 12 that there isn’t enough vaccine to meet demand, WPTV reported. “We need to realize that there’s a shortage of vaccine. So it’s not the plan, it’s not our ability to do it. It’s simply supply and demand at this point,” Dr. Alonso said, according to the TV station report.
A version of this article first appeared on Medscape.com.
Federal health officials are urging states to vaccinate all Americans over age 65 and those aged 16-64 who have a documented underlying health condition that makes them more vulnerable to COVID-19.
U.S. Department of Health and Human Services (HHS) Secretary Alex Azar and Centers for Disease Control and Prevention Director Robert Redfield, MD, made the recommendation in a briefing with reporters on Jan. 12, saying that the current vaccine supply was sufficient to meet demand for the next phase of immunization as recommended by the CDC’s Advisory Committee on Immunization Practices.
“We are ready for a transition that we outlined last September in the playbook we sent to states,” Mr. Azar said. Both he and U.S. Army General Gustave F. Perna, chief operations officer for Operation Warp Speed, said that confidence in the distribution system had led to the decision to urge wider access.
The federal government will also increase the number of sites eligible to receive vaccine – including some 13,000 federally qualified community health centers – and will not keep doses in reserve as insurance against issues that might prevent people from receiving a second dose on a timely basis.
“We don’t need to hold back reserve doses,” Mr. Azar said, noting that if there were any “glitches in production” the federal government would move to fulfill obligations for second doses first and delay initial doses.
Azar: Use it or lose it
In a move that is sure to generate pushback, Mr. Azar said that states that don’t quickly administer vaccines will receive fewer doses in the future. That policy will not go into effect until later in February, which leaves open the possibility that it could be reversed by the incoming Biden administration.
“We have too much vaccine sitting in freezers at hospitals with hospitals not using it,” said Mr. Azar, who also blamed the slow administration process on a reporting lag and states being what he called “overly prescriptive” in who has been eligible to receive a shot.
“I would rather have people working to get appointments to get vaccinated than having vaccine going to waste sitting in freezers,” he told reporters.
Mr. Azar had already been pushing for broader vaccination, telling states to do so in an Operation Warp Speed briefing on Jan. 6. At that briefing, he also said that the federal government would be stepping up vaccination through an “early launch” of a federal partnership with 19 pharmacy chains, which will let states allocate vaccines directly to some 40,000 pharmacy sites.
Gen. Perna said during the Jan. 12 briefing that the aim is to further expand that to some 70,000 locations total.
The CDC reported that as of Jan. 11 some 25.4 million doses have been distributed, with 8.9 million administered. An additional 4.2 million doses were distributed to long-term care facilities, and 937,000 residents and staff have received a dose.
“Pace of administration”
Alaska, Connecticut, North Dakota, South Dakota, the District of Columbia, West Virginia, and the Northern Mariana Islands have administered the most vaccines per capita, according to the CDC. But even these locations have immunized only 4%-5% of their populations, the New York Times reports. At the bottom: Alabama, Arizona, Arkansas, Georgia, Mississippi, and South Carolina.
The federal government can encourage but not require states to move on to new phases of vaccination.
“States ultimately determine how they will proceed with vaccination,” said Marcus Plescia, MD, MPH, chief medical officer for the Association of State and Territorial Health Officials. “Most will be cautious about assuring there are doses for those needing a second dose,” he said in an interview.
Dr. Plescia said that ensuring a second dose is available is especially important for health care workers “who need to be confident that they are protected and not inadvertently transmitting the disease themselves.”
He added that “once we reach a steady state of supply and administration, the rate-limiting factor will be supply of vaccine.”
That supply could now be threatened if states don’t comply with a just-announced federal action that will change how doses are allocated.
Beginning in late February, vaccine allocations to states will be based on “the pace of administration reported by states,” and the size of the 65-and-older population, said Mr. Azar, who has previously criticized New York Governor Andrew Cuomo for fining hospitals that didn’t use up vaccine supply within a week.
“This new system gives states a strong incentive to ensure that all vaccinations are being promptly reported, which they currently are not,” he said.
Currently, allocations are based on a state’s or territory’s population.
Prepandemic, states were required to report vaccinations within 30 days. Since COVID-19 vaccines became available, the CDC has required reporting of shots within 72 hours.
Dr. Redfield said the requirement has caused some difficulty, and that the CDC is investigating why some states have reported using only 15% of doses while others have used 80%.
States have been scrambling to ramp up vaccinations.
Just ahead of the federal briefing, Gov. Cuomo tweeted that New York would be opening up vaccinations to anyone older than 65.
The Associated Press is reporting that some states have started mass vaccination sites.
Arizona has begun operating a 24/7 appointment-only vaccination program at State Farm Stadium outside of Phoenix, with the aim of immunizing 6,000 people each day, according to local radio station KJZZ.
California and Florida have also taken steps to use stadiums, while Michigan, New Jersey, New York, and Texas will use convention centers and fairgrounds, Axios has reported.
In Florida, Palm Beach County Health Director Alina Alonso, MD, told county commissioners on Jan. 12 that there isn’t enough vaccine to meet demand, WPTV reported. “We need to realize that there’s a shortage of vaccine. So it’s not the plan, it’s not our ability to do it. It’s simply supply and demand at this point,” Dr. Alonso said, according to the TV station report.
A version of this article first appeared on Medscape.com.
Neck papules in a young man

The findings of follicular-based papules, pustules, and scars led to the diagnosis of early folliculitis keloidalis nuchae (FKN).
FKN, also called acne keloidalis nuchae, is more common in patients with darker skin types (Fitzpatrick skin types IV-VI) and is the most common form of scarring alopecia in men of African descent. The pathogenesis is unclear, but the condition may arise from mechanical occlusion with a retained short hair that leads to follicular destruction. Patients should lengthen their hair to at least a quarter of an inch to minimize this process. Military personnel may receive a waiver from standard grooming requirements. FKN may also occur as a primary disorder arising from bacterial infection and subsequent vigorous inflammation.
For early disease, topical therapy with either clindamycin 1% lotion or chlorhexidine solution are acceptable options. Should these options and hair lengthening fail over 3 to 4 months, consider a 6- to 12-week course of doxycycline or minocycline 100 mg once or twice daily. Intralesional triamcinolone with 5 to 10 mg/mL injected into fixed papules every 4 to 8 weeks is another option to reduce scar formation. The most severe cases may require combination oral antibiotics, isotretinoin, or plastic surgery.
In this case, the patient grew out his hair and applied clindamycin 1% lotion twice daily for a year. As a result, he had no further disease.
Text and photos courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. (Photo copyright retained.)

The findings of follicular-based papules, pustules, and scars led to the diagnosis of early folliculitis keloidalis nuchae (FKN).
FKN, also called acne keloidalis nuchae, is more common in patients with darker skin types (Fitzpatrick skin types IV-VI) and is the most common form of scarring alopecia in men of African descent. The pathogenesis is unclear, but the condition may arise from mechanical occlusion with a retained short hair that leads to follicular destruction. Patients should lengthen their hair to at least a quarter of an inch to minimize this process. Military personnel may receive a waiver from standard grooming requirements. FKN may also occur as a primary disorder arising from bacterial infection and subsequent vigorous inflammation.
For early disease, topical therapy with either clindamycin 1% lotion or chlorhexidine solution are acceptable options. Should these options and hair lengthening fail over 3 to 4 months, consider a 6- to 12-week course of doxycycline or minocycline 100 mg once or twice daily. Intralesional triamcinolone with 5 to 10 mg/mL injected into fixed papules every 4 to 8 weeks is another option to reduce scar formation. The most severe cases may require combination oral antibiotics, isotretinoin, or plastic surgery.
In this case, the patient grew out his hair and applied clindamycin 1% lotion twice daily for a year. As a result, he had no further disease.
Text and photos courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. (Photo copyright retained.)

The findings of follicular-based papules, pustules, and scars led to the diagnosis of early folliculitis keloidalis nuchae (FKN).
FKN, also called acne keloidalis nuchae, is more common in patients with darker skin types (Fitzpatrick skin types IV-VI) and is the most common form of scarring alopecia in men of African descent. The pathogenesis is unclear, but the condition may arise from mechanical occlusion with a retained short hair that leads to follicular destruction. Patients should lengthen their hair to at least a quarter of an inch to minimize this process. Military personnel may receive a waiver from standard grooming requirements. FKN may also occur as a primary disorder arising from bacterial infection and subsequent vigorous inflammation.
For early disease, topical therapy with either clindamycin 1% lotion or chlorhexidine solution are acceptable options. Should these options and hair lengthening fail over 3 to 4 months, consider a 6- to 12-week course of doxycycline or minocycline 100 mg once or twice daily. Intralesional triamcinolone with 5 to 10 mg/mL injected into fixed papules every 4 to 8 weeks is another option to reduce scar formation. The most severe cases may require combination oral antibiotics, isotretinoin, or plastic surgery.
In this case, the patient grew out his hair and applied clindamycin 1% lotion twice daily for a year. As a result, he had no further disease.
Text and photos courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. (Photo copyright retained.)
Arguing with doctors
They think people should accept what experts advise. After all, experts work hard to learn accurate facts to promote the public’s best interests.
Those who disagree and justify their reluctance – to be vaccinated against COVID-19, for instance – are unrepentant. First of all, they are not so sure experts are public spirited. Perhaps doctors have something to gain from illness and approve vaccines for political reasons, or assign certain diagnoses to get higher reimbursement.
In this contentious climate, peculiar treatments and unproved “cures” are claimed to deserve more respect than so-called experts are willing to grant them: hydroxychloroquine, bleach, and so on.
From my perspective, what is notable about such public disputes with medical experts is not that they exist but that they are public. In private, people have always argued with doctors. Most of those arguments don’t reach public notice. They are not interesting enough.
For instance, as I think back over the years, I can recall:
- A man who preferred to treat his eczema using topical yogurt. And not just any yogurt: only low-fat, plain Market Basket. He had tried them all.
- The woman with perioral scarring. She had let an unlicensed practitioner apply a painful acid on her face – he never told her what the acid was, and she hadn’t asked – as she lay on a neighbor’s living room floor to have her “skin cancer” treated.
- The man with an obvious melanoma on his chest. He did not want to treat it, because his faith healer in Milwaukee, whom he had never met in person, assured him that “it’s all taken care of.”
I could go on.
I cite these examples only because they are striking. They are far from unique.
People argue with doctors for the same reason they argue with anybody – because they think they know better. They may have heard otherwise from a friend, a magazine article, a blog, a different kind of practitioner.
Many such disagreements are never spoken out loud, because people who expect to argue usually don’t show up at their doctors’ offices. They either stay home or see a different kind of healer. If they do visit a doctor whose point of view differs from their own, most keep disagreements to themselves, because few people relish in-person confrontation. Instead they go home and ignore medical advice there.
Even when overt disagreements do erupt at a medical visit, the doctor can often find a way to convince the patient to reconsider, or somehow deflect the clash. The physician has to at least try to convince a patient who thinks his melanoma has “been taken care of” to have it removed. Whereas if someone really prefers low-fat yogurt to topical steroids, there is no need to win the argument. If the patient decides at some point that his eczema is out of control, he can call and request a prescription. He usually won’t.
For dermatologists, medical arguments rarely involve stakes high enough to force the doctor to try changing patients’ minds or discharging them from the practice. Had I stayed in my original field of pediatrics, I would have confronted patients who refused to vaccinate their children. I would have had to negotiate a compromise – vaccinate “more slowly” – or else part ways with the family.
I always advised medical students, when they found themselves argued with, to separate patients’ needs from their own egos. Being challenged in a small room can be challenging. Still, what matters is how the patient fares, not how the doctor feels.
Public disputes with scientists during the COVID-19 pandemic strike me as being motivated by the same factors behind private disputes in physicians’ offices: skepticism, resentment, suspicion, and – often underlying all these – fear.
Public disputes carried out over social media allow for posturing and aggression. A tweet is a better medium behind which to cloak opinions in the mantle of a noble cause, such as personal freedom. It is also easier to express derision and hostility toward opponents, expert or otherwise, from behind the screen of a Twitter handle.
Fortunately, in everyday medical practice, in-your-face disputes don’t happen very often.
You do remember them, though.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at online. Write to him at [email protected].
They think people should accept what experts advise. After all, experts work hard to learn accurate facts to promote the public’s best interests.
Those who disagree and justify their reluctance – to be vaccinated against COVID-19, for instance – are unrepentant. First of all, they are not so sure experts are public spirited. Perhaps doctors have something to gain from illness and approve vaccines for political reasons, or assign certain diagnoses to get higher reimbursement.
In this contentious climate, peculiar treatments and unproved “cures” are claimed to deserve more respect than so-called experts are willing to grant them: hydroxychloroquine, bleach, and so on.
From my perspective, what is notable about such public disputes with medical experts is not that they exist but that they are public. In private, people have always argued with doctors. Most of those arguments don’t reach public notice. They are not interesting enough.
For instance, as I think back over the years, I can recall:
- A man who preferred to treat his eczema using topical yogurt. And not just any yogurt: only low-fat, plain Market Basket. He had tried them all.
- The woman with perioral scarring. She had let an unlicensed practitioner apply a painful acid on her face – he never told her what the acid was, and she hadn’t asked – as she lay on a neighbor’s living room floor to have her “skin cancer” treated.
- The man with an obvious melanoma on his chest. He did not want to treat it, because his faith healer in Milwaukee, whom he had never met in person, assured him that “it’s all taken care of.”
I could go on.
I cite these examples only because they are striking. They are far from unique.
People argue with doctors for the same reason they argue with anybody – because they think they know better. They may have heard otherwise from a friend, a magazine article, a blog, a different kind of practitioner.
Many such disagreements are never spoken out loud, because people who expect to argue usually don’t show up at their doctors’ offices. They either stay home or see a different kind of healer. If they do visit a doctor whose point of view differs from their own, most keep disagreements to themselves, because few people relish in-person confrontation. Instead they go home and ignore medical advice there.
Even when overt disagreements do erupt at a medical visit, the doctor can often find a way to convince the patient to reconsider, or somehow deflect the clash. The physician has to at least try to convince a patient who thinks his melanoma has “been taken care of” to have it removed. Whereas if someone really prefers low-fat yogurt to topical steroids, there is no need to win the argument. If the patient decides at some point that his eczema is out of control, he can call and request a prescription. He usually won’t.
For dermatologists, medical arguments rarely involve stakes high enough to force the doctor to try changing patients’ minds or discharging them from the practice. Had I stayed in my original field of pediatrics, I would have confronted patients who refused to vaccinate their children. I would have had to negotiate a compromise – vaccinate “more slowly” – or else part ways with the family.
I always advised medical students, when they found themselves argued with, to separate patients’ needs from their own egos. Being challenged in a small room can be challenging. Still, what matters is how the patient fares, not how the doctor feels.
Public disputes with scientists during the COVID-19 pandemic strike me as being motivated by the same factors behind private disputes in physicians’ offices: skepticism, resentment, suspicion, and – often underlying all these – fear.
Public disputes carried out over social media allow for posturing and aggression. A tweet is a better medium behind which to cloak opinions in the mantle of a noble cause, such as personal freedom. It is also easier to express derision and hostility toward opponents, expert or otherwise, from behind the screen of a Twitter handle.
Fortunately, in everyday medical practice, in-your-face disputes don’t happen very often.
You do remember them, though.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at online. Write to him at [email protected].
They think people should accept what experts advise. After all, experts work hard to learn accurate facts to promote the public’s best interests.
Those who disagree and justify their reluctance – to be vaccinated against COVID-19, for instance – are unrepentant. First of all, they are not so sure experts are public spirited. Perhaps doctors have something to gain from illness and approve vaccines for political reasons, or assign certain diagnoses to get higher reimbursement.
In this contentious climate, peculiar treatments and unproved “cures” are claimed to deserve more respect than so-called experts are willing to grant them: hydroxychloroquine, bleach, and so on.
From my perspective, what is notable about such public disputes with medical experts is not that they exist but that they are public. In private, people have always argued with doctors. Most of those arguments don’t reach public notice. They are not interesting enough.
For instance, as I think back over the years, I can recall:
- A man who preferred to treat his eczema using topical yogurt. And not just any yogurt: only low-fat, plain Market Basket. He had tried them all.
- The woman with perioral scarring. She had let an unlicensed practitioner apply a painful acid on her face – he never told her what the acid was, and she hadn’t asked – as she lay on a neighbor’s living room floor to have her “skin cancer” treated.
- The man with an obvious melanoma on his chest. He did not want to treat it, because his faith healer in Milwaukee, whom he had never met in person, assured him that “it’s all taken care of.”
I could go on.
I cite these examples only because they are striking. They are far from unique.
People argue with doctors for the same reason they argue with anybody – because they think they know better. They may have heard otherwise from a friend, a magazine article, a blog, a different kind of practitioner.
Many such disagreements are never spoken out loud, because people who expect to argue usually don’t show up at their doctors’ offices. They either stay home or see a different kind of healer. If they do visit a doctor whose point of view differs from their own, most keep disagreements to themselves, because few people relish in-person confrontation. Instead they go home and ignore medical advice there.
Even when overt disagreements do erupt at a medical visit, the doctor can often find a way to convince the patient to reconsider, or somehow deflect the clash. The physician has to at least try to convince a patient who thinks his melanoma has “been taken care of” to have it removed. Whereas if someone really prefers low-fat yogurt to topical steroids, there is no need to win the argument. If the patient decides at some point that his eczema is out of control, he can call and request a prescription. He usually won’t.
For dermatologists, medical arguments rarely involve stakes high enough to force the doctor to try changing patients’ minds or discharging them from the practice. Had I stayed in my original field of pediatrics, I would have confronted patients who refused to vaccinate their children. I would have had to negotiate a compromise – vaccinate “more slowly” – or else part ways with the family.
I always advised medical students, when they found themselves argued with, to separate patients’ needs from their own egos. Being challenged in a small room can be challenging. Still, what matters is how the patient fares, not how the doctor feels.
Public disputes with scientists during the COVID-19 pandemic strike me as being motivated by the same factors behind private disputes in physicians’ offices: skepticism, resentment, suspicion, and – often underlying all these – fear.
Public disputes carried out over social media allow for posturing and aggression. A tweet is a better medium behind which to cloak opinions in the mantle of a noble cause, such as personal freedom. It is also easier to express derision and hostility toward opponents, expert or otherwise, from behind the screen of a Twitter handle.
Fortunately, in everyday medical practice, in-your-face disputes don’t happen very often.
You do remember them, though.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at online. Write to him at [email protected].
Averting COVID hospitalizations with monoclonal antibodies
The United States has allocated more than 641,000 monoclonal antibody treatments for outpatients to ease pressure on strained hospitals, but officials from Operation Warp Speed report that more than half of that reserve sits unused as clinicians grapple with best practices.
There are space and personnel limitations in hospitals right now, Janet Woodcock, MD, therapeutics lead on Operation Warp Speed, acknowledges in an interview with this news organization. “Special areas and procedures must be set up.” And the operation is in the process of broadening availability beyond hospitals, she points out.
But for frontline clinicians, questions about treatment efficacy and the logistics of administering intravenous drugs to infectious outpatients loom large.
More than 50 monoclonal antibody products that target SARS-CoV-2 are now in development. The U.S. Food and Drug Administration has already issued Emergency Use Authorization (EUA) for two such drugs on the basis of phase 2 trial data – bamlanivimab, made by Eli Lilly, and a cocktail of casirivimab plus imdevimab, made by Regeneron – and another two-antibody cocktail from AstraZeneca, AZD7442, has started phase 3 clinical trials. The Regeneron combination was used to treat President Donald Trump when he contracted COVID-19 in October.
Monoclonal antibody drugs are based on the natural antibodies that the body uses to fight infections. They work by binding to a specific target and then blocking its action or flagging it for destruction by other parts of the immune system. Both bamlanivimab and the casirivimab plus imdevimab combination target the spike protein of the virus and stop it from attaching to and entering human cells.
Targeting the spike protein out of the hospital
The antibody drugs covered by EUAs do not cure COVID-19, but they have been shown to reduce hospitalizations and visits to the emergency department for patients at high risk for disease progression. They are approved to treat patients older than 12 years with mild to moderate COVID-19 who are at high risk of progressing to severe disease or hospitalization. They are not authorized for use in patients who have been hospitalized or who are on ventilators. The hope is that antibody drugs will reduce the number of severe cases of COVID-19 and ease pressure on overstretched hospitals.
Most COVID-19 patients are outpatients, so we need something to keep them from getting worse.
This is important because it targets the greatest need in COVID-19 therapeutics, says Rajesh Gandhi, MD, an infectious disease physician at Harvard Medical School in Boston, who is a member of two panels evaluating COVID-19 treatments: one for the Infectious Disease Society of America and the other for the National Institutes of Health. “Up to now, most of the focus has been on hospitalized patients,” he says, but “most COVID-19 patients are outpatients, so we need something to keep them from getting worse.”
Both panels have said that, despite the EUAs, more evidence is needed to be sure of the efficacy of the drugs and to determine which patients will benefit the most from them.
These aren’t the mature data from drug development that guideline groups are accustomed to working with, Dr. Woodcock points out. “But this is an emergency and the data taken as a whole are pretty convincing,” she says. “As I look at the totality of the evidence, monoclonal antibodies will have a big effect in keeping people out of the hospital and helping them recover faster.”
High-risk patients are eligible for treatment, especially those older than 65 years and those with comorbidities who are younger. Access to the drugs is increasing for clinicians who are able to infuse safely or work with a site that will.
In the Boston area, several hospitals, including Massachusetts General where Dr. Gandhi works, have set up infusion centers where newly diagnosed patients can get the antibody treatment if their doctor thinks it will benefit them. And Coram, a provider of at-home infusion therapy owned by the CVS pharmacy chain, is running a pilot program offering the Eli Lilly drug to people in seven cities – including Boston, Chicago, Los Angeles, and Tampa – and their surrounding communities with a physician referral.
Getting that referral could be tricky, however, for patients without a primary care physician or for those whose doctor isn’t already connected to one of the institutions providing the infusions. The hospitals are sending out communications on how patients and physicians can get the therapy, but Dr. Gandhi says that making information about access available should be a priority. The window for the effective treatment is small – the drugs appear to work best before patients begin to make their own antibodies, says Dr. Gandhi – so it’s vital that doctors act quickly if they have a patient who is eligible.
And rolling out the new therapies to patients around the world will be a major logistical undertaking.
The first hurdle will be making enough of them to go around. Case numbers are skyrocketing around the globe, and producing the drugs is a complex time- and labor-intensive process that requires specialized facilities. Antibodies are produced by cell lines in bioreactors, so a plant that churns out generic aspirin tablets can’t simply be converted into an antibody factory.
“These types of drugs are manufactured in a sterile injectables plant, which is different from a plant where oral solids are made,” says Kim Crabtree, senior director of pharma portfolio management for Henry Schein Medical, a medical supplies distributor. “Those are not as plentiful as a standard pill factory.”
The doses required are also relatively high – 1.2 g of each antibody in Regeneron’s cocktail – which will further strain production capacity. Leah Lipsich, PhD, vice president of strategic program direction at Regeneron, says the company is prepared for high demand and has been able to respond, thanks to its rapid development and manufacturing technology, known as VelociSuite, which allows it to rapidly scale-up from discovery to productions in weeks instead of months.
“We knew supply would be a huge problem for COVID-19, but because we had such confidence in our technology, we went immediately from research-scale to our largest-scale manufacturing,” she says. “We’ve been manufacturing our cocktail for months now.”
The company has also partnered with Roche, the biggest manufacturer and vendor of monoclonal antibodies in the world, to manufacture and supply the drugs. Once full manufacturing capacity is reached in 2021, the companies expect to produce at least 2 million doses a year.
Then there is the issue of getting the drugs from the factories to the places they will be used.
Antibodies are temperature sensitive and need to be refrigerated during transport and storage, so a cold-chain-compliant supply chain is required. Fortunately, they can be kept at standard refrigerator temperatures, ranging from 2° C to 8° C, rather than the ultra-low temperatures required by some COVID-19 vaccines.
Two million doses a year
Medical logistics companies have a lot of experience dealing with products like these and are well prepared to handle the new antibody drugs. “There are quite a few products like these on the market, and the supply chain is used to shipping them,” Ms. Crabtree says.
They will be shipped to distribution centers in refrigerated trucks, repacked into smaller lots that can sustain the correct temperature for 24 hours, and then sent to their final destination, often in something as simple as a Styrofoam cooler filled with dry ice.
The expected rise in demand shouldn’t be too much of an issue for distributors either, says Ms. Crabtree; they have built systems that can deal with short-term surges in volume. The annual flu vaccine, for example, involves shipping a lot of product in a very short time, usually from August to November. “The distribution system is used to seasonal variations and peaks in demand,” she says.
The next question is how the treatments will be administered. Although most patients who will receive monoclonal antibodies will be ambulatory and not hospitalized, the administration requires intravenous infusion. Hospitals, of course, have a lot of experience with intravenous drugs, but typically give them only to inpatients. Most other monoclonal antibody drugs – such as those for cancer and autoimmune disorders – are given in specialized suites in doctor’s offices or in stand-alone infusion clinics.
That means that the places best suited to treat COVID-19 patients with antibodies are those that regularly deal with people who are immunocompromised, and such patients should not be interacting with people who have an infectious disease. “How do we protect the staff and other patients?” Dr. Gandhi asks.
Protecting staff and other patients
This is not an insurmountable obstacle, he points out, but it is one that requires careful thought and planning to accommodate COVID-19 patients without unduly disrupting life-saving treatments for other patients. It might involve, for example, treating COVID-19 patients in sequestered parts of the clinic or at different times of day, with even greater attention paid to cleaning, he explains. “We now have many months of experience with infection control, so we know how to do this; it’s just a question of logistics.”
But even once all the details around manufacturing, transporting, and administering the drugs are sorted out, there is still the issue of how they will be distributed fairly and equitably.
Despite multiple companies working to produce an array of different antibody drugs, demand is still expected to exceed supply for many months. “With more than 200,000 new cases a day in the United States, there won’t be enough antibodies to treat all of the high-risk patients,” says Dr. Gandhi. “Most of us are worried that demand will far outstrip supply. People are talking about lotteries to determine who gets them.”
The Department of Health and Human Services will continue to distribute the drugs to states on the basis of their COVID-19 burdens, and the states will then decide how much to provide to each health care facility.
Although the HHS goal is to ensure that the drugs reach as many patients as possible, no matter where they live and regardless of their income, there are still concerns that larger facilities serving more affluent areas will end up being favored, if only because they are the ones best equipped to deal with the drugs right now.
“We are all aware that this has affected certain communities more, so we need to make sure that the drugs are used equitably and made available to the communities that were hardest hit,” says Dr. Gandhi. The ability to monitor drug distribution should be built into the rollout, so that institutions and governments will have some sense of whether they are being doled out evenly, he adds.
Equity in distribution will be an issue for the rest of the world as well. Currently, 80% of monoclonal antibodies are sold in Canada, Europe, and the United States; few, if any, are available in low- and middle-income countries. The treatments are expensive: the cost of producing one g of marketed monoclonal antibodies is between $95 and $200, which does not include the cost of R&D, packaging, shipping, or administration. The median price for antibody treatment not related to COVID-19 runs from $15,000 to $200,000 per year in the United States.
Regeneron’s Dr. Lipsich says that the company has not yet set a price for its antibody cocktail. The government paid $450 million for its 300,000 doses, but that price includes the costs of research, manufacturing, and distribution, so is not a useful indicator of the eventual per-dose price. “We’re not in a position to talk about how it will be priced yet, but we will do our best to make it affordable and accessible to all,” she says.
There are some projects underway to ensure that the drugs are made available in poorer countries. In April, the COVID-19 Therapeutics Accelerator – an initiative launched by the Bill & Melinda Gates Foundation, Wellcome, and Mastercard to speed-up the response to the global pandemic – reserved manufacturing capacity with Fujifilm Diosynth Biotechnologies in Denmark for future monoclonal antibody therapies that will supply low- and middle-income countries. In October, the initiative announced that Eli Lilly would use that reserved capacity to produce its antibody drug starting in April 2021.
In the meantime, Lilly will make some of its product manufactured in other facilities available to lower-income countries. To help keep costs down, the company’s collaborators have agreed to waive their royalties on antibodies distributed in low- and middle-income countries.
“Everyone is looking carefully at how the drugs are distributed to ensure all will get access,” said Dr. Lipsich.
A version of this article first appeared on Medscape.com.
The United States has allocated more than 641,000 monoclonal antibody treatments for outpatients to ease pressure on strained hospitals, but officials from Operation Warp Speed report that more than half of that reserve sits unused as clinicians grapple with best practices.
There are space and personnel limitations in hospitals right now, Janet Woodcock, MD, therapeutics lead on Operation Warp Speed, acknowledges in an interview with this news organization. “Special areas and procedures must be set up.” And the operation is in the process of broadening availability beyond hospitals, she points out.
But for frontline clinicians, questions about treatment efficacy and the logistics of administering intravenous drugs to infectious outpatients loom large.
More than 50 monoclonal antibody products that target SARS-CoV-2 are now in development. The U.S. Food and Drug Administration has already issued Emergency Use Authorization (EUA) for two such drugs on the basis of phase 2 trial data – bamlanivimab, made by Eli Lilly, and a cocktail of casirivimab plus imdevimab, made by Regeneron – and another two-antibody cocktail from AstraZeneca, AZD7442, has started phase 3 clinical trials. The Regeneron combination was used to treat President Donald Trump when he contracted COVID-19 in October.
Monoclonal antibody drugs are based on the natural antibodies that the body uses to fight infections. They work by binding to a specific target and then blocking its action or flagging it for destruction by other parts of the immune system. Both bamlanivimab and the casirivimab plus imdevimab combination target the spike protein of the virus and stop it from attaching to and entering human cells.
Targeting the spike protein out of the hospital
The antibody drugs covered by EUAs do not cure COVID-19, but they have been shown to reduce hospitalizations and visits to the emergency department for patients at high risk for disease progression. They are approved to treat patients older than 12 years with mild to moderate COVID-19 who are at high risk of progressing to severe disease or hospitalization. They are not authorized for use in patients who have been hospitalized or who are on ventilators. The hope is that antibody drugs will reduce the number of severe cases of COVID-19 and ease pressure on overstretched hospitals.
Most COVID-19 patients are outpatients, so we need something to keep them from getting worse.
This is important because it targets the greatest need in COVID-19 therapeutics, says Rajesh Gandhi, MD, an infectious disease physician at Harvard Medical School in Boston, who is a member of two panels evaluating COVID-19 treatments: one for the Infectious Disease Society of America and the other for the National Institutes of Health. “Up to now, most of the focus has been on hospitalized patients,” he says, but “most COVID-19 patients are outpatients, so we need something to keep them from getting worse.”
Both panels have said that, despite the EUAs, more evidence is needed to be sure of the efficacy of the drugs and to determine which patients will benefit the most from them.
These aren’t the mature data from drug development that guideline groups are accustomed to working with, Dr. Woodcock points out. “But this is an emergency and the data taken as a whole are pretty convincing,” she says. “As I look at the totality of the evidence, monoclonal antibodies will have a big effect in keeping people out of the hospital and helping them recover faster.”
High-risk patients are eligible for treatment, especially those older than 65 years and those with comorbidities who are younger. Access to the drugs is increasing for clinicians who are able to infuse safely or work with a site that will.
In the Boston area, several hospitals, including Massachusetts General where Dr. Gandhi works, have set up infusion centers where newly diagnosed patients can get the antibody treatment if their doctor thinks it will benefit them. And Coram, a provider of at-home infusion therapy owned by the CVS pharmacy chain, is running a pilot program offering the Eli Lilly drug to people in seven cities – including Boston, Chicago, Los Angeles, and Tampa – and their surrounding communities with a physician referral.
Getting that referral could be tricky, however, for patients without a primary care physician or for those whose doctor isn’t already connected to one of the institutions providing the infusions. The hospitals are sending out communications on how patients and physicians can get the therapy, but Dr. Gandhi says that making information about access available should be a priority. The window for the effective treatment is small – the drugs appear to work best before patients begin to make their own antibodies, says Dr. Gandhi – so it’s vital that doctors act quickly if they have a patient who is eligible.
And rolling out the new therapies to patients around the world will be a major logistical undertaking.
The first hurdle will be making enough of them to go around. Case numbers are skyrocketing around the globe, and producing the drugs is a complex time- and labor-intensive process that requires specialized facilities. Antibodies are produced by cell lines in bioreactors, so a plant that churns out generic aspirin tablets can’t simply be converted into an antibody factory.
“These types of drugs are manufactured in a sterile injectables plant, which is different from a plant where oral solids are made,” says Kim Crabtree, senior director of pharma portfolio management for Henry Schein Medical, a medical supplies distributor. “Those are not as plentiful as a standard pill factory.”
The doses required are also relatively high – 1.2 g of each antibody in Regeneron’s cocktail – which will further strain production capacity. Leah Lipsich, PhD, vice president of strategic program direction at Regeneron, says the company is prepared for high demand and has been able to respond, thanks to its rapid development and manufacturing technology, known as VelociSuite, which allows it to rapidly scale-up from discovery to productions in weeks instead of months.
“We knew supply would be a huge problem for COVID-19, but because we had such confidence in our technology, we went immediately from research-scale to our largest-scale manufacturing,” she says. “We’ve been manufacturing our cocktail for months now.”
The company has also partnered with Roche, the biggest manufacturer and vendor of monoclonal antibodies in the world, to manufacture and supply the drugs. Once full manufacturing capacity is reached in 2021, the companies expect to produce at least 2 million doses a year.
Then there is the issue of getting the drugs from the factories to the places they will be used.
Antibodies are temperature sensitive and need to be refrigerated during transport and storage, so a cold-chain-compliant supply chain is required. Fortunately, they can be kept at standard refrigerator temperatures, ranging from 2° C to 8° C, rather than the ultra-low temperatures required by some COVID-19 vaccines.
Two million doses a year
Medical logistics companies have a lot of experience dealing with products like these and are well prepared to handle the new antibody drugs. “There are quite a few products like these on the market, and the supply chain is used to shipping them,” Ms. Crabtree says.
They will be shipped to distribution centers in refrigerated trucks, repacked into smaller lots that can sustain the correct temperature for 24 hours, and then sent to their final destination, often in something as simple as a Styrofoam cooler filled with dry ice.
The expected rise in demand shouldn’t be too much of an issue for distributors either, says Ms. Crabtree; they have built systems that can deal with short-term surges in volume. The annual flu vaccine, for example, involves shipping a lot of product in a very short time, usually from August to November. “The distribution system is used to seasonal variations and peaks in demand,” she says.
The next question is how the treatments will be administered. Although most patients who will receive monoclonal antibodies will be ambulatory and not hospitalized, the administration requires intravenous infusion. Hospitals, of course, have a lot of experience with intravenous drugs, but typically give them only to inpatients. Most other monoclonal antibody drugs – such as those for cancer and autoimmune disorders – are given in specialized suites in doctor’s offices or in stand-alone infusion clinics.
That means that the places best suited to treat COVID-19 patients with antibodies are those that regularly deal with people who are immunocompromised, and such patients should not be interacting with people who have an infectious disease. “How do we protect the staff and other patients?” Dr. Gandhi asks.
Protecting staff and other patients
This is not an insurmountable obstacle, he points out, but it is one that requires careful thought and planning to accommodate COVID-19 patients without unduly disrupting life-saving treatments for other patients. It might involve, for example, treating COVID-19 patients in sequestered parts of the clinic or at different times of day, with even greater attention paid to cleaning, he explains. “We now have many months of experience with infection control, so we know how to do this; it’s just a question of logistics.”
But even once all the details around manufacturing, transporting, and administering the drugs are sorted out, there is still the issue of how they will be distributed fairly and equitably.
Despite multiple companies working to produce an array of different antibody drugs, demand is still expected to exceed supply for many months. “With more than 200,000 new cases a day in the United States, there won’t be enough antibodies to treat all of the high-risk patients,” says Dr. Gandhi. “Most of us are worried that demand will far outstrip supply. People are talking about lotteries to determine who gets them.”
The Department of Health and Human Services will continue to distribute the drugs to states on the basis of their COVID-19 burdens, and the states will then decide how much to provide to each health care facility.
Although the HHS goal is to ensure that the drugs reach as many patients as possible, no matter where they live and regardless of their income, there are still concerns that larger facilities serving more affluent areas will end up being favored, if only because they are the ones best equipped to deal with the drugs right now.
“We are all aware that this has affected certain communities more, so we need to make sure that the drugs are used equitably and made available to the communities that were hardest hit,” says Dr. Gandhi. The ability to monitor drug distribution should be built into the rollout, so that institutions and governments will have some sense of whether they are being doled out evenly, he adds.
Equity in distribution will be an issue for the rest of the world as well. Currently, 80% of monoclonal antibodies are sold in Canada, Europe, and the United States; few, if any, are available in low- and middle-income countries. The treatments are expensive: the cost of producing one g of marketed monoclonal antibodies is between $95 and $200, which does not include the cost of R&D, packaging, shipping, or administration. The median price for antibody treatment not related to COVID-19 runs from $15,000 to $200,000 per year in the United States.
Regeneron’s Dr. Lipsich says that the company has not yet set a price for its antibody cocktail. The government paid $450 million for its 300,000 doses, but that price includes the costs of research, manufacturing, and distribution, so is not a useful indicator of the eventual per-dose price. “We’re not in a position to talk about how it will be priced yet, but we will do our best to make it affordable and accessible to all,” she says.
There are some projects underway to ensure that the drugs are made available in poorer countries. In April, the COVID-19 Therapeutics Accelerator – an initiative launched by the Bill & Melinda Gates Foundation, Wellcome, and Mastercard to speed-up the response to the global pandemic – reserved manufacturing capacity with Fujifilm Diosynth Biotechnologies in Denmark for future monoclonal antibody therapies that will supply low- and middle-income countries. In October, the initiative announced that Eli Lilly would use that reserved capacity to produce its antibody drug starting in April 2021.
In the meantime, Lilly will make some of its product manufactured in other facilities available to lower-income countries. To help keep costs down, the company’s collaborators have agreed to waive their royalties on antibodies distributed in low- and middle-income countries.
“Everyone is looking carefully at how the drugs are distributed to ensure all will get access,” said Dr. Lipsich.
A version of this article first appeared on Medscape.com.
The United States has allocated more than 641,000 monoclonal antibody treatments for outpatients to ease pressure on strained hospitals, but officials from Operation Warp Speed report that more than half of that reserve sits unused as clinicians grapple with best practices.
There are space and personnel limitations in hospitals right now, Janet Woodcock, MD, therapeutics lead on Operation Warp Speed, acknowledges in an interview with this news organization. “Special areas and procedures must be set up.” And the operation is in the process of broadening availability beyond hospitals, she points out.
But for frontline clinicians, questions about treatment efficacy and the logistics of administering intravenous drugs to infectious outpatients loom large.
More than 50 monoclonal antibody products that target SARS-CoV-2 are now in development. The U.S. Food and Drug Administration has already issued Emergency Use Authorization (EUA) for two such drugs on the basis of phase 2 trial data – bamlanivimab, made by Eli Lilly, and a cocktail of casirivimab plus imdevimab, made by Regeneron – and another two-antibody cocktail from AstraZeneca, AZD7442, has started phase 3 clinical trials. The Regeneron combination was used to treat President Donald Trump when he contracted COVID-19 in October.
Monoclonal antibody drugs are based on the natural antibodies that the body uses to fight infections. They work by binding to a specific target and then blocking its action or flagging it for destruction by other parts of the immune system. Both bamlanivimab and the casirivimab plus imdevimab combination target the spike protein of the virus and stop it from attaching to and entering human cells.
Targeting the spike protein out of the hospital
The antibody drugs covered by EUAs do not cure COVID-19, but they have been shown to reduce hospitalizations and visits to the emergency department for patients at high risk for disease progression. They are approved to treat patients older than 12 years with mild to moderate COVID-19 who are at high risk of progressing to severe disease or hospitalization. They are not authorized for use in patients who have been hospitalized or who are on ventilators. The hope is that antibody drugs will reduce the number of severe cases of COVID-19 and ease pressure on overstretched hospitals.
Most COVID-19 patients are outpatients, so we need something to keep them from getting worse.
This is important because it targets the greatest need in COVID-19 therapeutics, says Rajesh Gandhi, MD, an infectious disease physician at Harvard Medical School in Boston, who is a member of two panels evaluating COVID-19 treatments: one for the Infectious Disease Society of America and the other for the National Institutes of Health. “Up to now, most of the focus has been on hospitalized patients,” he says, but “most COVID-19 patients are outpatients, so we need something to keep them from getting worse.”
Both panels have said that, despite the EUAs, more evidence is needed to be sure of the efficacy of the drugs and to determine which patients will benefit the most from them.
These aren’t the mature data from drug development that guideline groups are accustomed to working with, Dr. Woodcock points out. “But this is an emergency and the data taken as a whole are pretty convincing,” she says. “As I look at the totality of the evidence, monoclonal antibodies will have a big effect in keeping people out of the hospital and helping them recover faster.”
High-risk patients are eligible for treatment, especially those older than 65 years and those with comorbidities who are younger. Access to the drugs is increasing for clinicians who are able to infuse safely or work with a site that will.
In the Boston area, several hospitals, including Massachusetts General where Dr. Gandhi works, have set up infusion centers where newly diagnosed patients can get the antibody treatment if their doctor thinks it will benefit them. And Coram, a provider of at-home infusion therapy owned by the CVS pharmacy chain, is running a pilot program offering the Eli Lilly drug to people in seven cities – including Boston, Chicago, Los Angeles, and Tampa – and their surrounding communities with a physician referral.
Getting that referral could be tricky, however, for patients without a primary care physician or for those whose doctor isn’t already connected to one of the institutions providing the infusions. The hospitals are sending out communications on how patients and physicians can get the therapy, but Dr. Gandhi says that making information about access available should be a priority. The window for the effective treatment is small – the drugs appear to work best before patients begin to make their own antibodies, says Dr. Gandhi – so it’s vital that doctors act quickly if they have a patient who is eligible.
And rolling out the new therapies to patients around the world will be a major logistical undertaking.
The first hurdle will be making enough of them to go around. Case numbers are skyrocketing around the globe, and producing the drugs is a complex time- and labor-intensive process that requires specialized facilities. Antibodies are produced by cell lines in bioreactors, so a plant that churns out generic aspirin tablets can’t simply be converted into an antibody factory.
“These types of drugs are manufactured in a sterile injectables plant, which is different from a plant where oral solids are made,” says Kim Crabtree, senior director of pharma portfolio management for Henry Schein Medical, a medical supplies distributor. “Those are not as plentiful as a standard pill factory.”
The doses required are also relatively high – 1.2 g of each antibody in Regeneron’s cocktail – which will further strain production capacity. Leah Lipsich, PhD, vice president of strategic program direction at Regeneron, says the company is prepared for high demand and has been able to respond, thanks to its rapid development and manufacturing technology, known as VelociSuite, which allows it to rapidly scale-up from discovery to productions in weeks instead of months.
“We knew supply would be a huge problem for COVID-19, but because we had such confidence in our technology, we went immediately from research-scale to our largest-scale manufacturing,” she says. “We’ve been manufacturing our cocktail for months now.”
The company has also partnered with Roche, the biggest manufacturer and vendor of monoclonal antibodies in the world, to manufacture and supply the drugs. Once full manufacturing capacity is reached in 2021, the companies expect to produce at least 2 million doses a year.
Then there is the issue of getting the drugs from the factories to the places they will be used.
Antibodies are temperature sensitive and need to be refrigerated during transport and storage, so a cold-chain-compliant supply chain is required. Fortunately, they can be kept at standard refrigerator temperatures, ranging from 2° C to 8° C, rather than the ultra-low temperatures required by some COVID-19 vaccines.
Two million doses a year
Medical logistics companies have a lot of experience dealing with products like these and are well prepared to handle the new antibody drugs. “There are quite a few products like these on the market, and the supply chain is used to shipping them,” Ms. Crabtree says.
They will be shipped to distribution centers in refrigerated trucks, repacked into smaller lots that can sustain the correct temperature for 24 hours, and then sent to their final destination, often in something as simple as a Styrofoam cooler filled with dry ice.
The expected rise in demand shouldn’t be too much of an issue for distributors either, says Ms. Crabtree; they have built systems that can deal with short-term surges in volume. The annual flu vaccine, for example, involves shipping a lot of product in a very short time, usually from August to November. “The distribution system is used to seasonal variations and peaks in demand,” she says.
The next question is how the treatments will be administered. Although most patients who will receive monoclonal antibodies will be ambulatory and not hospitalized, the administration requires intravenous infusion. Hospitals, of course, have a lot of experience with intravenous drugs, but typically give them only to inpatients. Most other monoclonal antibody drugs – such as those for cancer and autoimmune disorders – are given in specialized suites in doctor’s offices or in stand-alone infusion clinics.
That means that the places best suited to treat COVID-19 patients with antibodies are those that regularly deal with people who are immunocompromised, and such patients should not be interacting with people who have an infectious disease. “How do we protect the staff and other patients?” Dr. Gandhi asks.
Protecting staff and other patients
This is not an insurmountable obstacle, he points out, but it is one that requires careful thought and planning to accommodate COVID-19 patients without unduly disrupting life-saving treatments for other patients. It might involve, for example, treating COVID-19 patients in sequestered parts of the clinic or at different times of day, with even greater attention paid to cleaning, he explains. “We now have many months of experience with infection control, so we know how to do this; it’s just a question of logistics.”
But even once all the details around manufacturing, transporting, and administering the drugs are sorted out, there is still the issue of how they will be distributed fairly and equitably.
Despite multiple companies working to produce an array of different antibody drugs, demand is still expected to exceed supply for many months. “With more than 200,000 new cases a day in the United States, there won’t be enough antibodies to treat all of the high-risk patients,” says Dr. Gandhi. “Most of us are worried that demand will far outstrip supply. People are talking about lotteries to determine who gets them.”
The Department of Health and Human Services will continue to distribute the drugs to states on the basis of their COVID-19 burdens, and the states will then decide how much to provide to each health care facility.
Although the HHS goal is to ensure that the drugs reach as many patients as possible, no matter where they live and regardless of their income, there are still concerns that larger facilities serving more affluent areas will end up being favored, if only because they are the ones best equipped to deal with the drugs right now.
“We are all aware that this has affected certain communities more, so we need to make sure that the drugs are used equitably and made available to the communities that were hardest hit,” says Dr. Gandhi. The ability to monitor drug distribution should be built into the rollout, so that institutions and governments will have some sense of whether they are being doled out evenly, he adds.
Equity in distribution will be an issue for the rest of the world as well. Currently, 80% of monoclonal antibodies are sold in Canada, Europe, and the United States; few, if any, are available in low- and middle-income countries. The treatments are expensive: the cost of producing one g of marketed monoclonal antibodies is between $95 and $200, which does not include the cost of R&D, packaging, shipping, or administration. The median price for antibody treatment not related to COVID-19 runs from $15,000 to $200,000 per year in the United States.
Regeneron’s Dr. Lipsich says that the company has not yet set a price for its antibody cocktail. The government paid $450 million for its 300,000 doses, but that price includes the costs of research, manufacturing, and distribution, so is not a useful indicator of the eventual per-dose price. “We’re not in a position to talk about how it will be priced yet, but we will do our best to make it affordable and accessible to all,” she says.
There are some projects underway to ensure that the drugs are made available in poorer countries. In April, the COVID-19 Therapeutics Accelerator – an initiative launched by the Bill & Melinda Gates Foundation, Wellcome, and Mastercard to speed-up the response to the global pandemic – reserved manufacturing capacity with Fujifilm Diosynth Biotechnologies in Denmark for future monoclonal antibody therapies that will supply low- and middle-income countries. In October, the initiative announced that Eli Lilly would use that reserved capacity to produce its antibody drug starting in April 2021.
In the meantime, Lilly will make some of its product manufactured in other facilities available to lower-income countries. To help keep costs down, the company’s collaborators have agreed to waive their royalties on antibodies distributed in low- and middle-income countries.
“Everyone is looking carefully at how the drugs are distributed to ensure all will get access,” said Dr. Lipsich.
A version of this article first appeared on Medscape.com.
COVID-19 in children: Weekly cases trending downward
The United States added over 171,000 new COVID-19 cases in children during the week ending Jan. 7, but that figure is lower than 3 of the previous 4 weeks, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
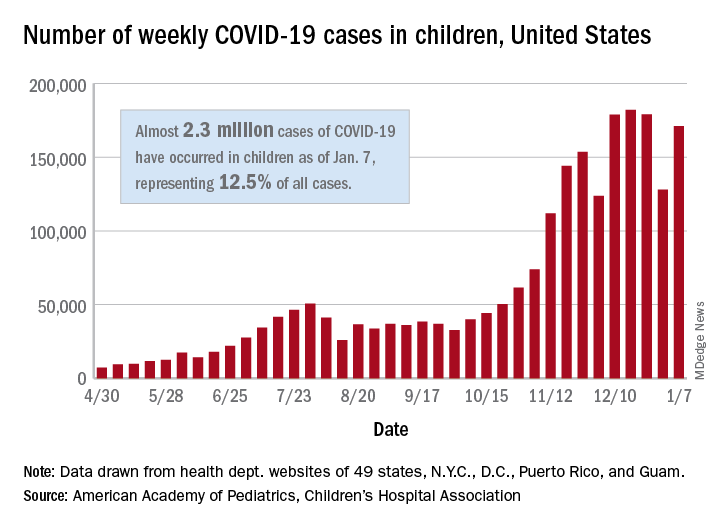
Despite an increase compared with the week ending Dec. 31, the most recent weekly total is down from the high of 182,000 cases reported for the week ending Dec. 17, based on data collected from the health department websites of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
Those jurisdictions have recorded a total of almost 2.3 million COVID-19 cases in children since the beginning of the pandemic, which amounts to 12.5% of reported cases among all ages. The 171,000 child cases for the most recent week represented 12.9% of the more than 1.3 million cases nationwide, the AAP and CHA said in their latest weekly update.
The United States now has a rate of 3,055 COVID-19 cases per 100,000 children in the population, the report shows, with 31 states above that figure and 14 states reporting rates above 4,500 per 100,000 children.
Severe illness, however, continues to be rare among children. So far, children represent 1.8% of all hospitalizations in the jurisdictions reporting such data (24 states and New York City), and just 0.9% of infected children have been hospitalized. There have been 188 deaths among children in 42 states and New York City, which makes up just 0.06% of the total for all ages in those jurisdictions, the AAP and CHA reported.
There are 13 states that have reported no coronavirus-related deaths in children, while Texas (34), New York City (21), Arizona (17), and Illinois (11) are the only jurisdictions with 10 or more. Nevada has the highest proportion of child deaths to all deaths at 0.2%, with Arizona and Nebraska next at 0.18%, according to the AAP/CHA report.
The United States added over 171,000 new COVID-19 cases in children during the week ending Jan. 7, but that figure is lower than 3 of the previous 4 weeks, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
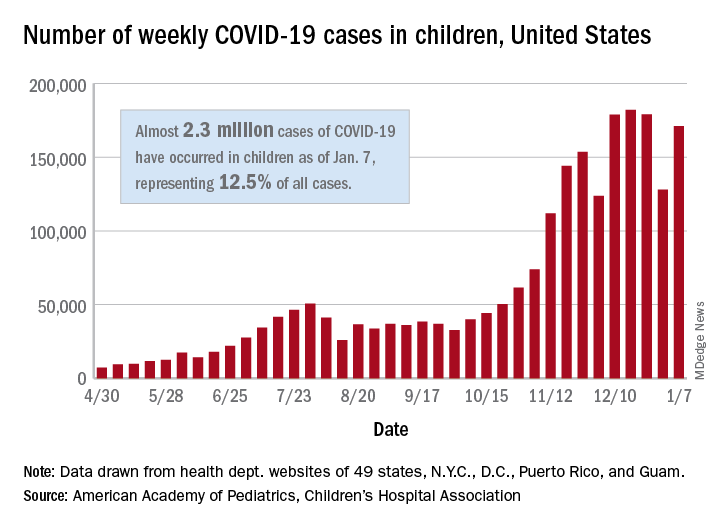
Despite an increase compared with the week ending Dec. 31, the most recent weekly total is down from the high of 182,000 cases reported for the week ending Dec. 17, based on data collected from the health department websites of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
Those jurisdictions have recorded a total of almost 2.3 million COVID-19 cases in children since the beginning of the pandemic, which amounts to 12.5% of reported cases among all ages. The 171,000 child cases for the most recent week represented 12.9% of the more than 1.3 million cases nationwide, the AAP and CHA said in their latest weekly update.
The United States now has a rate of 3,055 COVID-19 cases per 100,000 children in the population, the report shows, with 31 states above that figure and 14 states reporting rates above 4,500 per 100,000 children.
Severe illness, however, continues to be rare among children. So far, children represent 1.8% of all hospitalizations in the jurisdictions reporting such data (24 states and New York City), and just 0.9% of infected children have been hospitalized. There have been 188 deaths among children in 42 states and New York City, which makes up just 0.06% of the total for all ages in those jurisdictions, the AAP and CHA reported.
There are 13 states that have reported no coronavirus-related deaths in children, while Texas (34), New York City (21), Arizona (17), and Illinois (11) are the only jurisdictions with 10 or more. Nevada has the highest proportion of child deaths to all deaths at 0.2%, with Arizona and Nebraska next at 0.18%, according to the AAP/CHA report.
The United States added over 171,000 new COVID-19 cases in children during the week ending Jan. 7, but that figure is lower than 3 of the previous 4 weeks, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
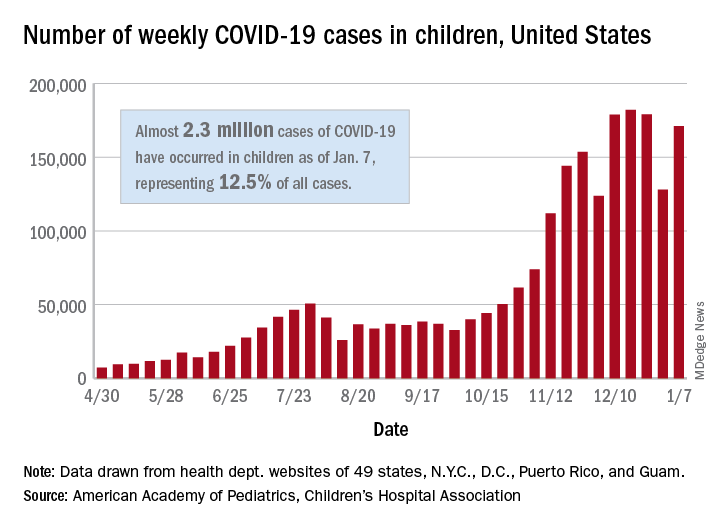
Despite an increase compared with the week ending Dec. 31, the most recent weekly total is down from the high of 182,000 cases reported for the week ending Dec. 17, based on data collected from the health department websites of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
Those jurisdictions have recorded a total of almost 2.3 million COVID-19 cases in children since the beginning of the pandemic, which amounts to 12.5% of reported cases among all ages. The 171,000 child cases for the most recent week represented 12.9% of the more than 1.3 million cases nationwide, the AAP and CHA said in their latest weekly update.
The United States now has a rate of 3,055 COVID-19 cases per 100,000 children in the population, the report shows, with 31 states above that figure and 14 states reporting rates above 4,500 per 100,000 children.
Severe illness, however, continues to be rare among children. So far, children represent 1.8% of all hospitalizations in the jurisdictions reporting such data (24 states and New York City), and just 0.9% of infected children have been hospitalized. There have been 188 deaths among children in 42 states and New York City, which makes up just 0.06% of the total for all ages in those jurisdictions, the AAP and CHA reported.
There are 13 states that have reported no coronavirus-related deaths in children, while Texas (34), New York City (21), Arizona (17), and Illinois (11) are the only jurisdictions with 10 or more. Nevada has the highest proportion of child deaths to all deaths at 0.2%, with Arizona and Nebraska next at 0.18%, according to the AAP/CHA report.
Left atrial appendage occlusion, DOAC comparable for AFib
Left atrial appendage occlusion (LAAO) for high-risk atrial fibrillation seems to prevent stroke as well as direct oral anticoagulation (DOAC) with a lower risk of major bleeding, according to results of a European study.
And although some experts question the strength of the conclusions, a lead researcher contends the study may provide enough support for interventional cardiologists to consider LAAO in selected patients until randomized clinical trials yield stronger evidence.
“The results suggest LAAO to be superior to DOAC in AF patients who have a predicted high risk of stroke and bleeding and adds to the evidence that LAAO is a promising stroke prevention strategy in selected AF patients,” said lead investigator Jens Erik Nielsen-Kudsk, MD, DMSc, a cardiologist at Aarhus University Hospital in Denmark.
Dr. Nielsen-Kudsk and colleagues wrote in JACC: Cardiovascular Interventions that this is the largest comparative study of LAAO vs. DOAC to date, but they also acknowledged the study limitations: its observational design, unaccounted confounders, potential selection bias, and disparities in the nature of the comparative datasets (a multination cohort vs. a single national registry).
Observational registry study shows 43% reduction in primary outcome
The study compared outcomes of 1,078 patients from the Amulet Observational Study who had LAAO during June 2015–September 2016 with 1,184 patients on DOAC therapy selected by propensity score matching from two Danish national registries. The LAAO population was prospectively enrolled at 61 centers in 17 countries. The study population had a high risk of stroke and bleeding; about one-third had a previous stroke and about three-quarters had a prior bleeding episode. The average age was 75 years.
The LAAO group had almost half the rate of the primary outcome – either stroke, major bleeding, or all-cause death – 256 vs. 461 events in the DOAC group with median follow-up of 2 years. The annualized event rate was significantly lower for the LAAO group: 14.5 vs. 25.7 per 100 patient years in the DOAC group. The researchers calculated the LAAO group had a relative 43% reduction risk.
Of the LAAO group, 155 patients (14.5%) died in the follow-up period, 35% of them from a cardiovascular cause, whereas 308 (26%) of patients in the DOAC group died, with a similar percentage, 36%, from a cardiovascular cause.
Using data from the Danish Cause of Death Registry, the study determined cause of death in the DOAC patients on a more granular level: 9.5% of the deaths were from vascular disease and 4.5% from stroke (the remainder in both groups were from noncardiovascular events).
Stroke incidence was similar between the two groups: 39 in the LAAO group vs. 37 in DOAC patients, conferring an 11% greater risk in the former. The risk of major bleeding and all-cause mortality were significantly lower in LAAO patients, 37% and 47%, respectively. However, 50% of DOAC patients had discontinued therapy after a year of follow-up, and 58% had done so after 2 years.
Dr. Nielsen-Kudsk noted that the findings line up with those from the smaller PRAQUE-17 study comparing LAAO and DOAC. He added that his group is participating in two larger RCTs, CATALYST and CHAMPION-AF, evaluating LAAO and medical therapy in about 6,000 patients combined.
“It will take at least 2 to 5 years before we have data from these randomized LAAO trials,” Dr. Nielsen-Kudsk said. “Meanwhile, based on data from three prior randomized clinical trials, propensity-score matched studies and data from large registries, LAAO should be considered in clinical practice for patients who have a high risk of bleeding or who for any other reason are unsuitable for long-term DOAC treatment.”
Noncompliance to DOAC therapy a concern
In an invited commentary, Mohamad Alkhouli, MD, of the Mayo Medical School, Rochester, Minn., wrote, “These findings provide reassuring evidence supporting the efficacy of LAAO despite the remaining challenges with this therapy.”
However, Dr. Alkhouli pointed out that the high rate of noncompliance among AF patients on DOAC can be a confounding factor for interpreting the efficacy of therapy. “This highlights the challenges of comparing LAAO to DOAC, considering that many patients are actually not on effective anticoagulation, but also suggests a possible real important role for LAAO in addressing the unmet need in stroke prevention in nonvalvular atrial fibrillation,” he said in an interview.
“The study showed a very good safety profile for LAAO,” Dr. Alkhouli added. “However, we should remember that this was an observational study without routine temporal imaging and a relatively short-term follow- up.”
Methods ‘severely flawed’
John Mandrola, MD, an electrophysiologist at Baptist Health in Louisville, Ky., said the study methodology was “severely flawed,” citing its nonrandomized nature and enrollment of only patients with successful implants in the LAAO group. “You have to take all patients who had attempted implants,” he said. Further, the study may be subject to selection bias based on how patients were recruited for the Ampulet Observational Study.
“Comparing LAAO to DOAC is a vital clinical question,” said Dr. Mandrola. “It simply cannot be answered with observational methods like this. It requires a properly powered RCT.”
Dr. Alkhouli said he’s looking forward to results from five large RCTS evaluating LAAO due in 3-5 years. “Until the results of those trials are out, careful patient selection and shared decision-making should continue to govern the rational dissipation of LAAO as a stroke prevention strategy,” he said.
Novo Nordisk Research Foundation supported the study and Abbott provided a grant. Dr. Nielsen-Kudsk disclosed financial relationships with Abbott and Boston Scientific. Coauthors disclosed relationships with Abbott, Boston Scientific, Bayer Vital, Bristol Myers Squibb, Boehringer Ingelheim, Daiichi-Sankyo, Medtronic, Pfizer, Portolo, and Sanofi.
Dr. Alkhouli disclosed a relationship with Boston Scientific. Dr. Mandrola has no relevant disclosures. He is chief cardiology correspondent for Medscape.com. MDedge is a member of the Medscape Professional Network.
Left atrial appendage occlusion (LAAO) for high-risk atrial fibrillation seems to prevent stroke as well as direct oral anticoagulation (DOAC) with a lower risk of major bleeding, according to results of a European study.
And although some experts question the strength of the conclusions, a lead researcher contends the study may provide enough support for interventional cardiologists to consider LAAO in selected patients until randomized clinical trials yield stronger evidence.
“The results suggest LAAO to be superior to DOAC in AF patients who have a predicted high risk of stroke and bleeding and adds to the evidence that LAAO is a promising stroke prevention strategy in selected AF patients,” said lead investigator Jens Erik Nielsen-Kudsk, MD, DMSc, a cardiologist at Aarhus University Hospital in Denmark.
Dr. Nielsen-Kudsk and colleagues wrote in JACC: Cardiovascular Interventions that this is the largest comparative study of LAAO vs. DOAC to date, but they also acknowledged the study limitations: its observational design, unaccounted confounders, potential selection bias, and disparities in the nature of the comparative datasets (a multination cohort vs. a single national registry).
Observational registry study shows 43% reduction in primary outcome
The study compared outcomes of 1,078 patients from the Amulet Observational Study who had LAAO during June 2015–September 2016 with 1,184 patients on DOAC therapy selected by propensity score matching from two Danish national registries. The LAAO population was prospectively enrolled at 61 centers in 17 countries. The study population had a high risk of stroke and bleeding; about one-third had a previous stroke and about three-quarters had a prior bleeding episode. The average age was 75 years.
The LAAO group had almost half the rate of the primary outcome – either stroke, major bleeding, or all-cause death – 256 vs. 461 events in the DOAC group with median follow-up of 2 years. The annualized event rate was significantly lower for the LAAO group: 14.5 vs. 25.7 per 100 patient years in the DOAC group. The researchers calculated the LAAO group had a relative 43% reduction risk.
Of the LAAO group, 155 patients (14.5%) died in the follow-up period, 35% of them from a cardiovascular cause, whereas 308 (26%) of patients in the DOAC group died, with a similar percentage, 36%, from a cardiovascular cause.
Using data from the Danish Cause of Death Registry, the study determined cause of death in the DOAC patients on a more granular level: 9.5% of the deaths were from vascular disease and 4.5% from stroke (the remainder in both groups were from noncardiovascular events).
Stroke incidence was similar between the two groups: 39 in the LAAO group vs. 37 in DOAC patients, conferring an 11% greater risk in the former. The risk of major bleeding and all-cause mortality were significantly lower in LAAO patients, 37% and 47%, respectively. However, 50% of DOAC patients had discontinued therapy after a year of follow-up, and 58% had done so after 2 years.
Dr. Nielsen-Kudsk noted that the findings line up with those from the smaller PRAQUE-17 study comparing LAAO and DOAC. He added that his group is participating in two larger RCTs, CATALYST and CHAMPION-AF, evaluating LAAO and medical therapy in about 6,000 patients combined.
“It will take at least 2 to 5 years before we have data from these randomized LAAO trials,” Dr. Nielsen-Kudsk said. “Meanwhile, based on data from three prior randomized clinical trials, propensity-score matched studies and data from large registries, LAAO should be considered in clinical practice for patients who have a high risk of bleeding or who for any other reason are unsuitable for long-term DOAC treatment.”
Noncompliance to DOAC therapy a concern
In an invited commentary, Mohamad Alkhouli, MD, of the Mayo Medical School, Rochester, Minn., wrote, “These findings provide reassuring evidence supporting the efficacy of LAAO despite the remaining challenges with this therapy.”
However, Dr. Alkhouli pointed out that the high rate of noncompliance among AF patients on DOAC can be a confounding factor for interpreting the efficacy of therapy. “This highlights the challenges of comparing LAAO to DOAC, considering that many patients are actually not on effective anticoagulation, but also suggests a possible real important role for LAAO in addressing the unmet need in stroke prevention in nonvalvular atrial fibrillation,” he said in an interview.
“The study showed a very good safety profile for LAAO,” Dr. Alkhouli added. “However, we should remember that this was an observational study without routine temporal imaging and a relatively short-term follow- up.”
Methods ‘severely flawed’
John Mandrola, MD, an electrophysiologist at Baptist Health in Louisville, Ky., said the study methodology was “severely flawed,” citing its nonrandomized nature and enrollment of only patients with successful implants in the LAAO group. “You have to take all patients who had attempted implants,” he said. Further, the study may be subject to selection bias based on how patients were recruited for the Ampulet Observational Study.
“Comparing LAAO to DOAC is a vital clinical question,” said Dr. Mandrola. “It simply cannot be answered with observational methods like this. It requires a properly powered RCT.”
Dr. Alkhouli said he’s looking forward to results from five large RCTS evaluating LAAO due in 3-5 years. “Until the results of those trials are out, careful patient selection and shared decision-making should continue to govern the rational dissipation of LAAO as a stroke prevention strategy,” he said.
Novo Nordisk Research Foundation supported the study and Abbott provided a grant. Dr. Nielsen-Kudsk disclosed financial relationships with Abbott and Boston Scientific. Coauthors disclosed relationships with Abbott, Boston Scientific, Bayer Vital, Bristol Myers Squibb, Boehringer Ingelheim, Daiichi-Sankyo, Medtronic, Pfizer, Portolo, and Sanofi.
Dr. Alkhouli disclosed a relationship with Boston Scientific. Dr. Mandrola has no relevant disclosures. He is chief cardiology correspondent for Medscape.com. MDedge is a member of the Medscape Professional Network.
Left atrial appendage occlusion (LAAO) for high-risk atrial fibrillation seems to prevent stroke as well as direct oral anticoagulation (DOAC) with a lower risk of major bleeding, according to results of a European study.
And although some experts question the strength of the conclusions, a lead researcher contends the study may provide enough support for interventional cardiologists to consider LAAO in selected patients until randomized clinical trials yield stronger evidence.
“The results suggest LAAO to be superior to DOAC in AF patients who have a predicted high risk of stroke and bleeding and adds to the evidence that LAAO is a promising stroke prevention strategy in selected AF patients,” said lead investigator Jens Erik Nielsen-Kudsk, MD, DMSc, a cardiologist at Aarhus University Hospital in Denmark.
Dr. Nielsen-Kudsk and colleagues wrote in JACC: Cardiovascular Interventions that this is the largest comparative study of LAAO vs. DOAC to date, but they also acknowledged the study limitations: its observational design, unaccounted confounders, potential selection bias, and disparities in the nature of the comparative datasets (a multination cohort vs. a single national registry).
Observational registry study shows 43% reduction in primary outcome
The study compared outcomes of 1,078 patients from the Amulet Observational Study who had LAAO during June 2015–September 2016 with 1,184 patients on DOAC therapy selected by propensity score matching from two Danish national registries. The LAAO population was prospectively enrolled at 61 centers in 17 countries. The study population had a high risk of stroke and bleeding; about one-third had a previous stroke and about three-quarters had a prior bleeding episode. The average age was 75 years.
The LAAO group had almost half the rate of the primary outcome – either stroke, major bleeding, or all-cause death – 256 vs. 461 events in the DOAC group with median follow-up of 2 years. The annualized event rate was significantly lower for the LAAO group: 14.5 vs. 25.7 per 100 patient years in the DOAC group. The researchers calculated the LAAO group had a relative 43% reduction risk.
Of the LAAO group, 155 patients (14.5%) died in the follow-up period, 35% of them from a cardiovascular cause, whereas 308 (26%) of patients in the DOAC group died, with a similar percentage, 36%, from a cardiovascular cause.
Using data from the Danish Cause of Death Registry, the study determined cause of death in the DOAC patients on a more granular level: 9.5% of the deaths were from vascular disease and 4.5% from stroke (the remainder in both groups were from noncardiovascular events).
Stroke incidence was similar between the two groups: 39 in the LAAO group vs. 37 in DOAC patients, conferring an 11% greater risk in the former. The risk of major bleeding and all-cause mortality were significantly lower in LAAO patients, 37% and 47%, respectively. However, 50% of DOAC patients had discontinued therapy after a year of follow-up, and 58% had done so after 2 years.
Dr. Nielsen-Kudsk noted that the findings line up with those from the smaller PRAQUE-17 study comparing LAAO and DOAC. He added that his group is participating in two larger RCTs, CATALYST and CHAMPION-AF, evaluating LAAO and medical therapy in about 6,000 patients combined.
“It will take at least 2 to 5 years before we have data from these randomized LAAO trials,” Dr. Nielsen-Kudsk said. “Meanwhile, based on data from three prior randomized clinical trials, propensity-score matched studies and data from large registries, LAAO should be considered in clinical practice for patients who have a high risk of bleeding or who for any other reason are unsuitable for long-term DOAC treatment.”
Noncompliance to DOAC therapy a concern
In an invited commentary, Mohamad Alkhouli, MD, of the Mayo Medical School, Rochester, Minn., wrote, “These findings provide reassuring evidence supporting the efficacy of LAAO despite the remaining challenges with this therapy.”
However, Dr. Alkhouli pointed out that the high rate of noncompliance among AF patients on DOAC can be a confounding factor for interpreting the efficacy of therapy. “This highlights the challenges of comparing LAAO to DOAC, considering that many patients are actually not on effective anticoagulation, but also suggests a possible real important role for LAAO in addressing the unmet need in stroke prevention in nonvalvular atrial fibrillation,” he said in an interview.
“The study showed a very good safety profile for LAAO,” Dr. Alkhouli added. “However, we should remember that this was an observational study without routine temporal imaging and a relatively short-term follow- up.”
Methods ‘severely flawed’
John Mandrola, MD, an electrophysiologist at Baptist Health in Louisville, Ky., said the study methodology was “severely flawed,” citing its nonrandomized nature and enrollment of only patients with successful implants in the LAAO group. “You have to take all patients who had attempted implants,” he said. Further, the study may be subject to selection bias based on how patients were recruited for the Ampulet Observational Study.
“Comparing LAAO to DOAC is a vital clinical question,” said Dr. Mandrola. “It simply cannot be answered with observational methods like this. It requires a properly powered RCT.”
Dr. Alkhouli said he’s looking forward to results from five large RCTS evaluating LAAO due in 3-5 years. “Until the results of those trials are out, careful patient selection and shared decision-making should continue to govern the rational dissipation of LAAO as a stroke prevention strategy,” he said.
Novo Nordisk Research Foundation supported the study and Abbott provided a grant. Dr. Nielsen-Kudsk disclosed financial relationships with Abbott and Boston Scientific. Coauthors disclosed relationships with Abbott, Boston Scientific, Bayer Vital, Bristol Myers Squibb, Boehringer Ingelheim, Daiichi-Sankyo, Medtronic, Pfizer, Portolo, and Sanofi.
Dr. Alkhouli disclosed a relationship with Boston Scientific. Dr. Mandrola has no relevant disclosures. He is chief cardiology correspondent for Medscape.com. MDedge is a member of the Medscape Professional Network.
FROM JACC CARDIOVASCULAR INTERVENTION
Setting the Stage for Major Depressive Disorder Recovery: Strategies for the Busy Primary Care Provider
Click here to read this supplement
CME/CE CREDITS: 1.5 CREDITS
After reviewing the learning objectives and reading the supplement, please complete the Activity Evaluation/Credit Request form online at www.cmesurvey.site/MDDJFP
Click here to read this supplement
CME/CE CREDITS: 1.5 CREDITS
After reviewing the learning objectives and reading the supplement, please complete the Activity Evaluation/Credit Request form online at www.cmesurvey.site/MDDJFP
Click here to read this supplement
CME/CE CREDITS: 1.5 CREDITS
After reviewing the learning objectives and reading the supplement, please complete the Activity Evaluation/Credit Request form online at www.cmesurvey.site/MDDJFP