User login
Merkel Cell Carcinoma in a Vein Graft Donor Site
Case Report
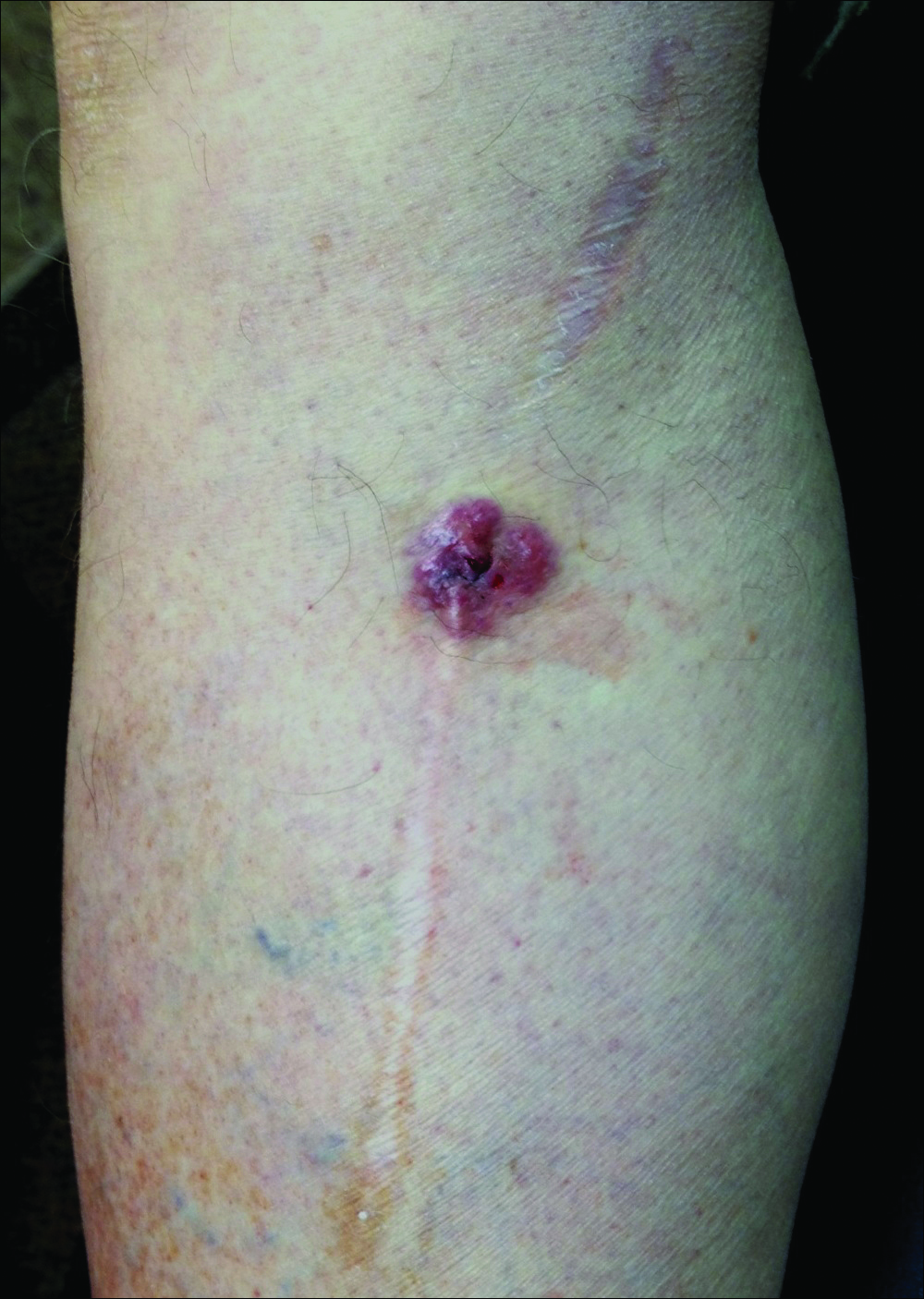
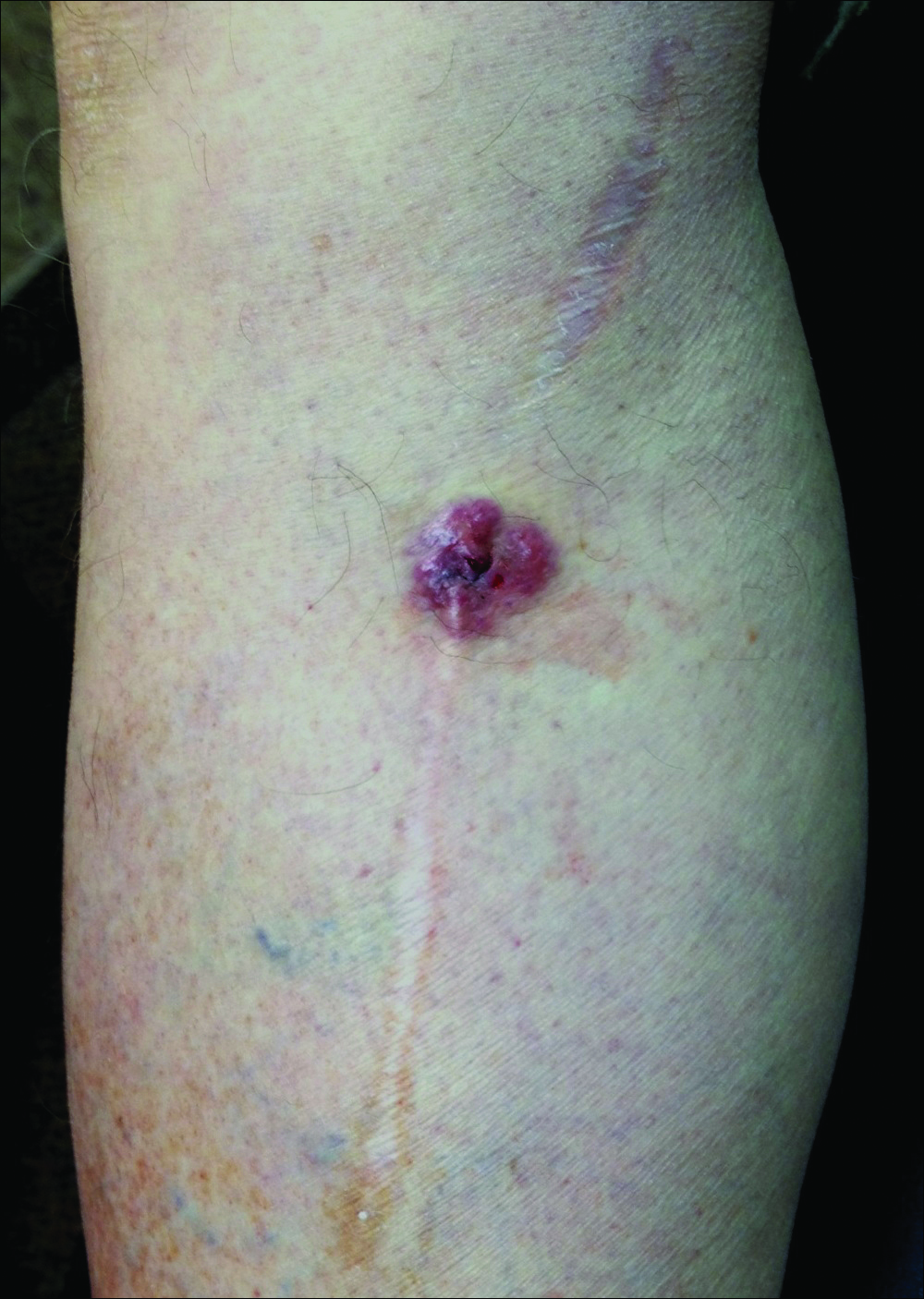
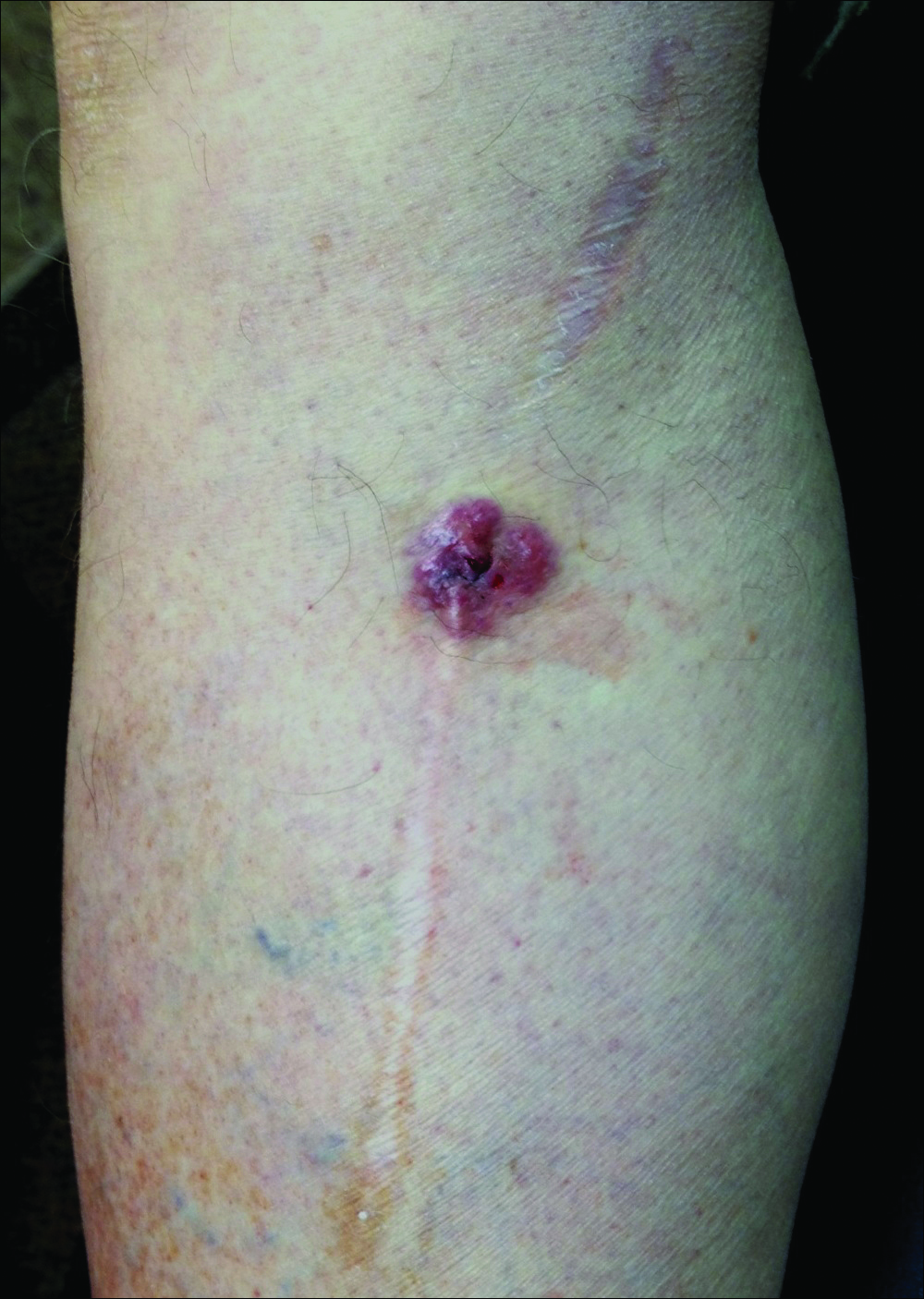
A 70-year-old man with history of coronary artery disease presented with a growing lesion on the right leg of 1 year’s duration. The lesion developed at a vein graft donor site for a coronary artery bypass that had been performed 18 years prior to presentation. The patient reported that the lesion was sensitive to touch. Physical examination revealed a 27-mm, firm, violaceous plaque on the medial aspect of the right upper shin (Figure 1). Mild pitting edema also was noted on both lower legs but was more prominent on the right leg. A 6-mm punch biopsy was performed.
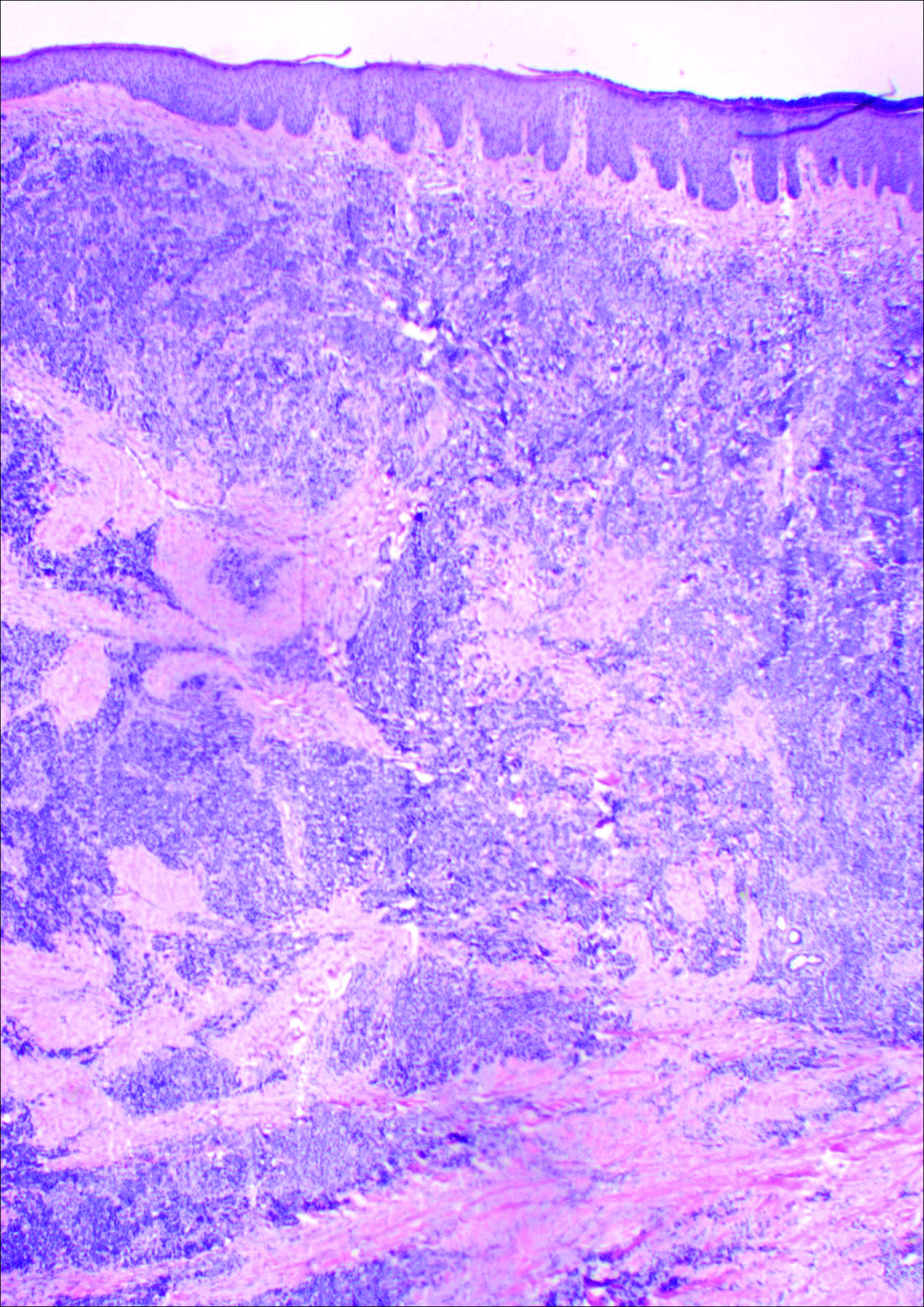
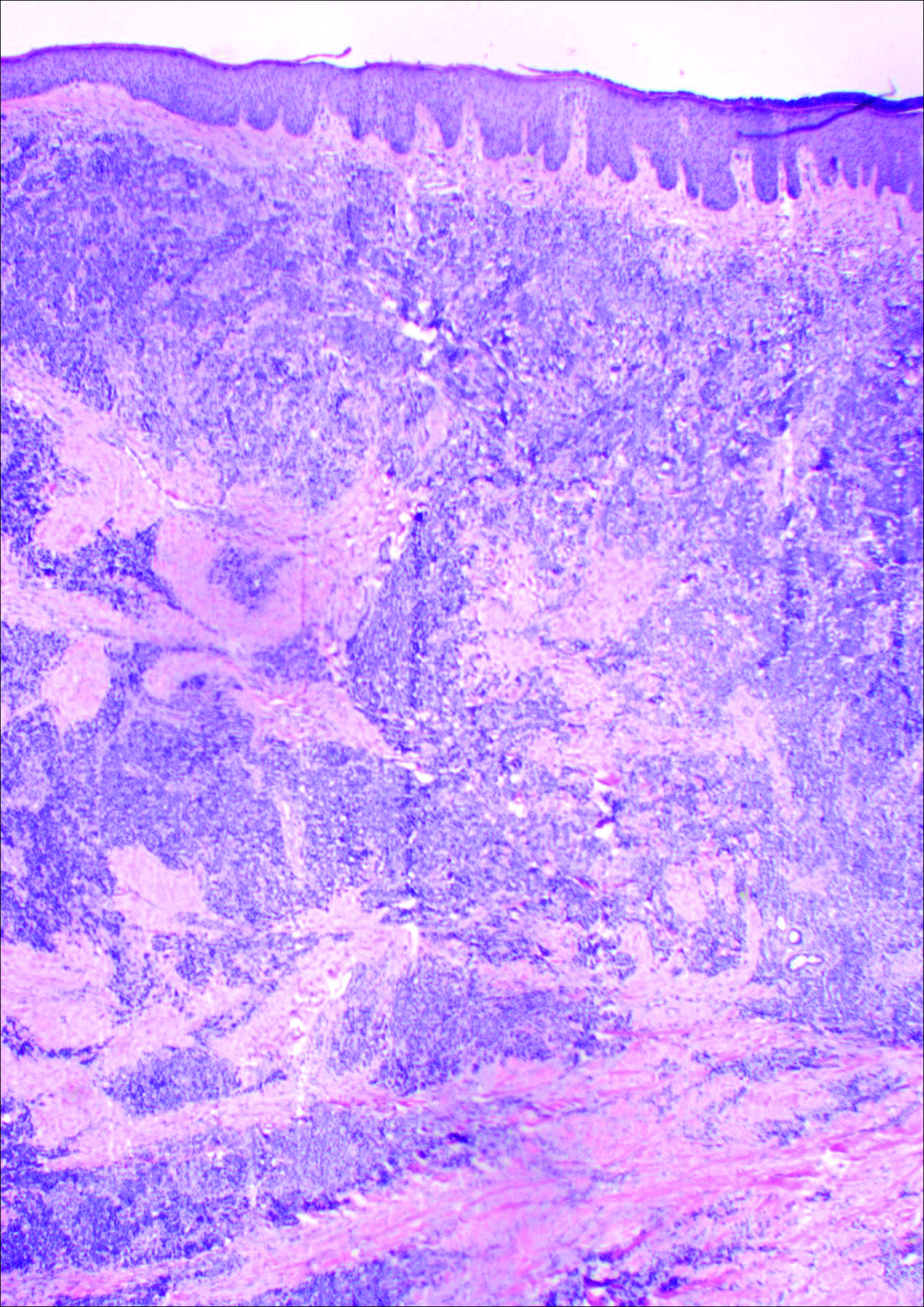
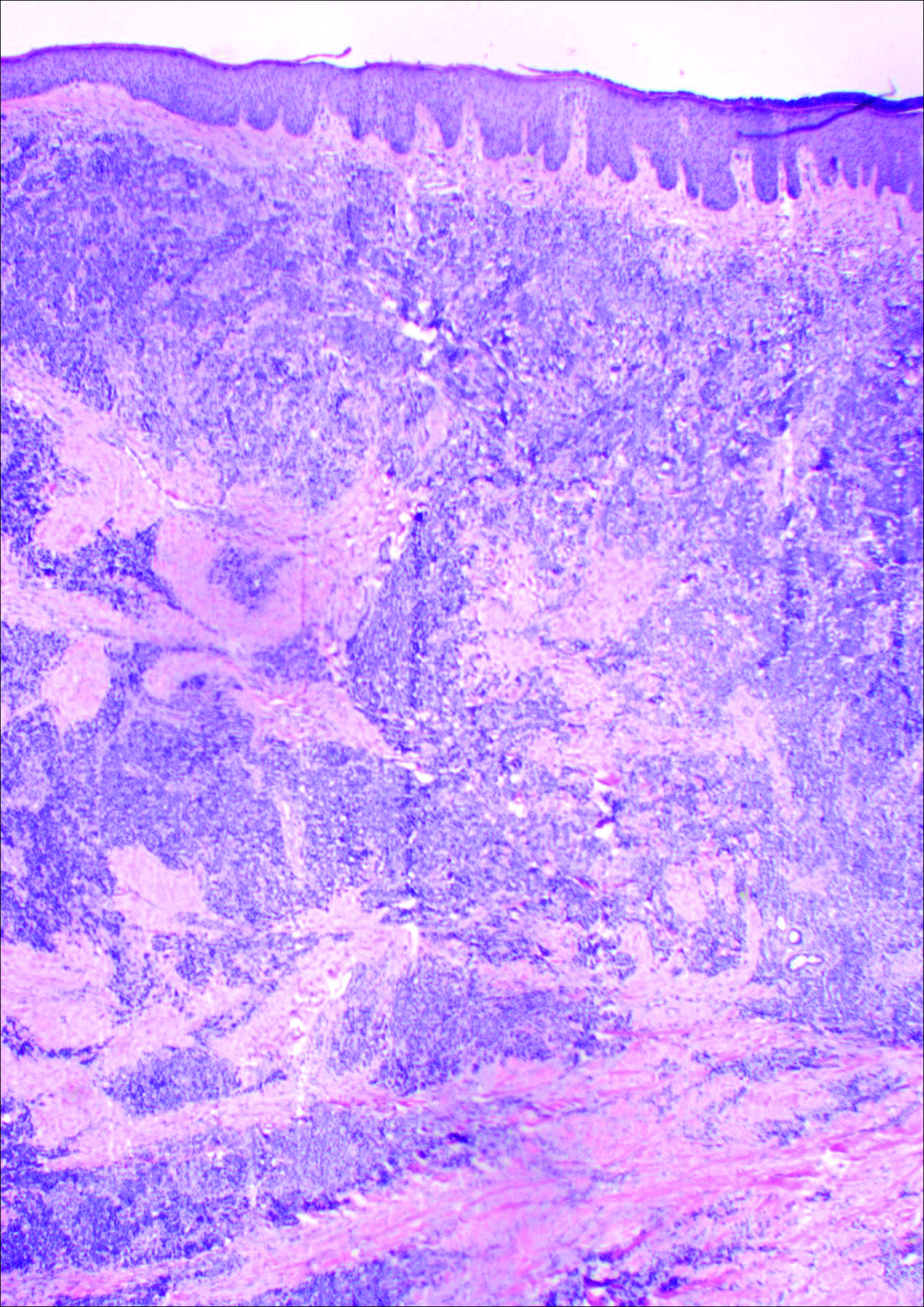
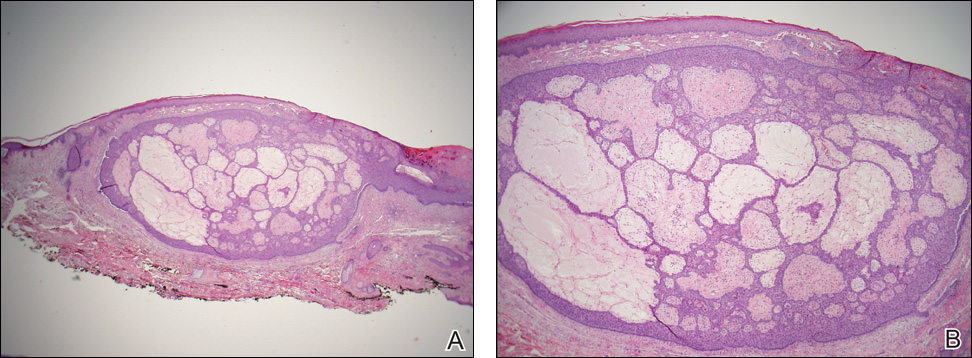
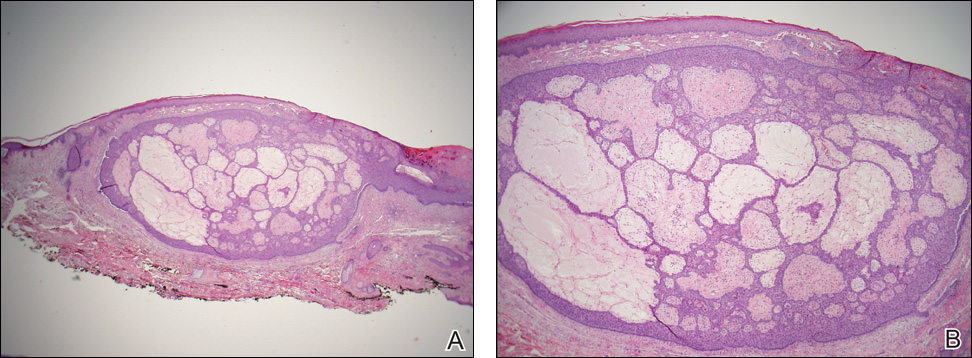
Histology showed diffuse infiltration of the dermis and subcutaneous fat by intermediate-sized atypical blue cells with scant cytoplasm (Figure 2). The tumor exhibited moderate cytologic atypia with occasional mitotic figures, and lymphovascular invasion was present. Staining for CD3 was negative within the tumor, but a few reactive lymphocytes were highlighted at the periphery. Staining for CD20 and CD30 was negative. Strong and diffuse staining for cyto-keratin 20 and pan-cytokeratin was noted within the tumor with the distinctive perinuclear pattern characteristic of Merkel cell carcinoma (MCC). Staining for cytokeratin 7 was negative. Synaptophysin and chromogranin were strongly and diffusely positive within the tumor, consistent with a diagnosis of MCC.
The patient was found to have stage IIA (T2N0M0) MCC. Computed tomography completed for staging showed no evidence of metastasis. Wide local excision of the lesion was performed. Margins were negative, as was a right inguinal sentinel lymph node dissection. Because of the size of the tumor and the presence of lymphovascular invasion, radiation therapy at the primary tumor site was recommended. Local radiation treatment (200 cGy daily) was administered for a total dose of 5000 cGy over 5 weeks. The patient currently is free of recurrence or metastases and is being followed by the oncology, surgery, and dermatology departments.
Comment
Merkel cell carcinoma is a rare aggressive cutaneous malignancy. The exact pathogenesis is unknown, but immunosuppression and UV radiation, possibly through its immunosuppressive effects, appear to be contributing factors. More recently, the Merkel cell polyomavirus has been linked to MCC in approximately 80% of cases.1,2
Merkel cell carcinoma is more common in individuals with fair skin, and the average age at diagnosis is 69 years.1 Patients typically present with an asymptomatic, firm, erythematous or violaceous, dome-shaped nodule or a small indurated plaque, most commonly on sun-exposed areas of the head and neck followed by the upper and lower extremities including the hands, feet, ankles, and wrists. Fifteen percent to 20% of MCCs develop on the legs and feet.1 Our patient presented with an MCC that developed on the right shin at a vein graft donor site.
The development of a cutaneous malignancy in a chronic wound (also known as a Marjolin ulcer) is a rare but well-recognized process. These malignancies occur in previously traumatized or chronically inflamed wounds and have been found to occur most commonly in chronic burn wounds, especially in ungrafted full-thickness burns. Squamous cell carcinomas (SCCs) are the most common malignancies to arise in chronic wounds, but basal cell carcinomas, adenocarcinomas, melanomas, malignant fibrous histiocytomas, adenoacanthomas, liposarcomas, and osteosarcomas also have been reported.3 There also have been a few reports of MCC associated with Bowen disease that developed in burn wounds.4 These malignancies generally occur years after injury (average, 35.5 years), but there have been reports of keratoacanthomas developing as early as 3 weeks after injury.5,6
In some reports, malignancies in skin graft donor sites are differentiated from Marjolin ulcers, as the former appear in healed surgical wounds rather than in chronic unstable wounds and tend to occur sooner (ie, in weeks to months after graft harvesting).7,8 The development of these malignancies in graft donor sites is not as well recognized and has been reported in donor sites for split-thickness skin grafts (STSGs), full-thickness skin grafts, tendon grafts, and bone grafts. In addition to malignancies that arise de novo, some develop due to metastatic and iatrogenic spread. The majority of reported malignancies in tendon and bone graft donor sites have been due to metastasis or iatrogenic spread.9-14
Iatrogenic implantation of tumor cells is a well-recognized phenomenon. Hussain et al10 reported a case of implantation of SCC in an STSG donor site, most likely due to direct seeding from a hollow needle used to infiltrate local anesthetic in the tumor area and the STSG. In this case, metastasis could not be completely ruled out.10 There also have been reports of osteosarcoma, ameloblastoma, scirrhous carcinoma of the breast, and malignant fibrous histiocytoma thought to be implanted at bone graft donor sites.14-17 Iatrogenic spread of malignancies can occur through seeding from contaminated gloves or instruments such as hollow bore needles or trocar placement in laparoscopic surgery.11 Airborne spread also may be possible, as viable melanoma cells have been detected in electrocautery plume in mice.13
Metastatic malignancies including metastases from SCC, adenocarcinoma, melanoma, malignant fibrous histiocytoma, angiosarcoma, and osteosarcoma also have been reported to develop in graft donor sites.11,13,18,19 Many malignancies thought to have developed from iatrogenic seeding may actually be from metastasis either by hematogenous or lymphatic spread. A possible contributing factor may be surgery-induced immunosuppression, which has been linked to increased tumor metastasis formation.20 Surgery or trauma have been shown to have an effect on cellular components of the immune system, causing changes such as a shift in T lymphocytes toward immune-suppressive T lymphocytes and impaired function of natural killer cells, neutrophils, and macrophages.20 The suppression of cell-mediated immunity has been shown to decrease over days to weeks in the postoperative period.21 In addition to surgery- or trauma-induced immunosuppression, the risk for metastasis may increase due to increased vascular, including lymphatic, flow toward a skin graft donor site.13,16 Furthermore, trauma predisposes areas to a hypercoagulable state with increased sludging as well as increased platelet counts and fibrinogen levels, which may lead to localization of metastatic lesions.22 All of these factors could potentially work simultaneously to induce the development of metastasis in graft donor sites.
We found that SCCs and keratoacanthomas, which may be a variant of SCC, are among the only primary malignancies that have been reported to develop in skin graft donor sites.6-8 Malignancies in these donor sites appear to develop sooner than those found in chronic wounds and are reported to develop within weeks to several months postoperatively, even in as few as 2 weeks.6,8 Tamir et al6 reported 2 keratoacanthomas that developed simultaneously in a burn scar and STSG donor site. The investigators believed it could be a sign of reduced immune surveillance in the 2 affected areas.6 It has been hypothesized that one cause of local immune suppression in Marjolin ulcers could be due to poor lymphatic regeneration in scar tissue, which would prevent delivery of antigens and stimulated lymphocytes.23 Haik et al7 considered this possibility when discussing a case of SCC that developed at the site of an STSG. The authors did not feel it applied, however, as the donor site had only undergone a single skin harvesting procedure.7 Ponnuvelu et al8 felt that inflammation was the underlying etiology behind the 2 cases they reported of SCCs that developed in STSG donor sites. The inflammation associated with tumors has many of the same processes involved in wound healing (eg, cellular proliferation, angiogenesis). Ponnuvelu et al8 hypothesized that the local inflammation caused by graft harvesting produced an ideal environment for early carcinogenesis. Although in chronic wounds it is believed that continual repair and regeneration in recurrent ulceration contributes to neoplastic initiation, it is thought that even a single injury may lead to malignant change, which may be because prior actinic damage or another cause has made the area more susceptible to these changes.24,25 Surgery-induced immunosuppression also may play a role in development of primary malignancies in graft donor sites.
There have been a few reports of SCCs and basal cell carcinomas occurring in other surgical scars that healed without complications.24,26-28 Similar to the malignancies in graft donor sites, some authors differentiate malignancies that occur in surgical scars that heal without complications from Marjolin ulcers, as they do not occur in chronically irritated wounds. These malignancies have been reported in scars from sternotomies, an infertility procedure, hair transplantation, thyroidectomy, colostomy, cleft lip repair, inguinal hernia repair, and paraumbilical laparoscopic port site. The time between surgery and diagnosis of malignancy ranged from 9 months to 67 years.24,26-28 The development of malignancies in these surgical scars may be due to local immunosuppression, possibly from decreased lymphatic flow; additionally, the inflammation in wound healing may provide the ideal environment for carcinogenesis. Trauma in areas already susceptible to malignant change could be a contributing factor.
Conclusion
Our patient developed an MCC in a vein graft donor site 18 years after vein harvesting. It was likely a primary tumor, as vein harvesting was done for coronary artery bypass graft. There was no evidence of any other lesions on physical examination or computed tomography, making it doubtful that an MCC serving as a primary lesion for seeding or metastasis was present. If such a lesion had been present at that time, it would likely have spread well before the time of presentation to our clinic due to the fast doubling time and high rate of metastasis characteristic of MCCs, further lessening the possibility of metastasis or implantation.
The extended length of time from procedure to lesion development in our patient is much longer than for other reported malignancies in graft donor sites, but the reported time for malignancies in other postsurgical scars is more varied. Regardless of whether the MCC in our patient is classified as a Marjolin ulcer, the pathogenesis is unclear. It is thought that a single injury could lead to malignant change in predisposed skin. Our patient’s legs did not have any evidence of prior actinic damage; however, it is likely that he had local immune suppression, which may have made him more susceptible to these changes. It is unlikely that surgery-induced immunosuppression played a role in our patient, as specific cellular components of the immune system only appear to be affected over days to weeks in the postoperative period. Although poor lymphatic regeneration in scar tissue leading to decreased immune surveillance is not generally thought to contribute to malignancies in most surgical scars, our patient underwent vein harvesting. Chronic edema commonly occurs after vein harvesting and is believed to be due to trauma to the lymphatics. Local immune suppression also may have led to increased susceptibility to infection by the MCC polyomavirus, which has been found to be associated with many MCCs. In addition, the area may have been more susceptible to carcinogenesis due to changes from inflammation from wound healing. We suspect together these factors contributed to the development of our patient’s MCC. Although rare, graft donor sites should be examined periodically for the development of malignancy.
- Swann MH, Yoon J. Merkel cell carcinoma. Semin Oncol. 2007;34:51-56.
- Schrama D, Ugurel S, Becker JC. Merkel cell carcinoma: recent insights and new treatment options. Curr Opin Oncol. 2012;24:141-149.
- Kadir AR. Burn scar neoplasm. Ann Burns Fire Disasters. 2007;20:185-188.
- Walsh NM. Primary neuroendocrine (Merkel cell) carcinoma of the skin: morphologic diversity and implications thereof. Hum Pathol. 2001;32:680-689.
- Guenther N, Menenakos C, Braumann C, et al. Squamous cell carcinoma arising on a skin graft 64 years after primary injury. Dermatol Online J. 2007;13:27.
- Tamir G, Morgenstern S, Ben-Amitay D, et al. Synchronous appearance of keratoacanthomas in burn scar and skin graft donor site shortly after injury. J Am Acad Dermatol. 1999;40:870-871.
- Haik J, Georgiou I, Farber N, et al. Squamous cell carcinoma arising in a split-thickness skin graft donor site. Burns. 2008;34:891-893.
- Ponnuvelu G, Ng MF, Connolly CM, et al. Inflammation to skin malignancy, time to rethink the link: SCC in skin graft donor sites. Surgeon. 2011;9:168-169.
- Bekar A, Kahveci R, Tolunay S, et al. Metastatic gliosarcoma mass extension to a donor fascia lata graft harvest site by tumor cell contamination. World Neurosurg. 2010;73:719-721.
- Hussain A, Ekwobi C, Watson S. Metastatic implantation squamous cell carcinoma in a split-thickness skin graft donor site. J Plast Reconstr Aesthet Surg. 2011;64:690-692.
- May JT, Patil YJ. Keratoacanthoma-type squamous cell carcinoma developing in a skin graft donor site after tumor extirpation at a distant site. Ear Nose Throat J. 2010;89:E11-E13.
- Serrano-Ortega S, Buendia-Eisman A, Ortega del Olmo RM, et al. Melanoma metastasis in donor site of full-thickness skin graft. Dermatology. 2000;201:377-378.
- Wright H, McKinnell TH, Dunkin C. Recurrence of cutaneous squamous cell carcinoma at remote limb donor site. J Plast Reconstr Aesthet Surg. 2012;65:1265-1266.
- Yip KM, Lin J, Kumta SM. A pelvic osteosarcoma with metastasis to the donor site of the bone graft. a case report. Int Orthop. 1996;20:389-391.
- Dias RG, Abudu A, Carter SR, et al. Tumour transfer to bone graft donor site: a case report and review of the literature of the mechanism of seeding. Sarcoma. 2000;4:57-59.
- Neilson D, Emerson DJ, Dunn L. Squamous cell carcinoma of skin developing in a skin graft donor site. Br J Plast Surg. 1988;41:417-419.
- Singh C, Ibrahim S, Pang KS, et al. Implantation metastasis in a 13-year-old girl: a case report. J Orthop Surg (Hong Kong). 2003;11:94-96.
- Enion DS, Scott MJ, Gouldesbrough D. Cutaneous metastasis from a malignant fibrous histiocytoma to a limb skin graft donor site. Br J Surg. 1993;80:366.
- Yamasaki O, Terao K, Asagoe K, et al. Koebner phenomenon on skin graft donor site in cutaneous angiosarcoma. Eur J Dermatol. 2001;11:584-586.
- Hogan BV, Peter MB, Shenoy HG, et al. Surgery induced immunosuppression. Surgeon. 2011;9:38-43.
- Neeman E, Ben-Eliyahu S. The perioperative period and promotion of cancer metastasis: new outlooks on mediating mechanisms and immune involvement. Brain Behav Immun. 2013;30(suppl):32-40.
- Agostino D, Cliffton EE. Trauma as a cause of localization of blood-borne metastases: preventive effect of heparin and fibrinolysin. Ann Surg. 1965;161:97-102.
- Hammond JS, Thomsen S, Ward CG. Scar carcinoma arising acutely in a skin graft donor site. J Trauma. 1987;27:681-683.
- Korula R, Hughes CF. Squamous cell carcinoma arising in a sternotomy scar. Ann Thorac Surg. 1991;51:667-669.
- Kennedy CTC, Burd DAR, Creamer D. Mechanical and thermal injury. In: Burns T, Breathnach S, Cox N, et al, eds. Rook’s Textbook of Dermatology. Vol 2. 8th ed. Hoboken, NJ: Wiley-Blackwell; 2010:28.1-28.94.
- Durrani AJ, Miller RJ, Davies M. Basal cell carcinoma arising in a laparoscopic port site scar at the umbilicus. Plast Reconstr Surg. 2005;116:348-350.
- Kotwal S, Madaan S, Prescott S, et al. Unusual squamous cell carcinoma of the scrotum arising from a well healed, innocuous scar of an infertility procedure: a case report. Ann R Coll Surg Engl. 2007;89:17-19.
- Ozyazgan I, Kontas O. Previous injuries or scars as risk factors for the development of basal cell carcinoma. Scand J Plast Reconstr Surg Hand Surg. 2004;38:11-15.
Case Report
A 70-year-old man with history of coronary artery disease presented with a growing lesion on the right leg of 1 year’s duration. The lesion developed at a vein graft donor site for a coronary artery bypass that had been performed 18 years prior to presentation. The patient reported that the lesion was sensitive to touch. Physical examination revealed a 27-mm, firm, violaceous plaque on the medial aspect of the right upper shin (Figure 1). Mild pitting edema also was noted on both lower legs but was more prominent on the right leg. A 6-mm punch biopsy was performed.
Histology showed diffuse infiltration of the dermis and subcutaneous fat by intermediate-sized atypical blue cells with scant cytoplasm (Figure 2). The tumor exhibited moderate cytologic atypia with occasional mitotic figures, and lymphovascular invasion was present. Staining for CD3 was negative within the tumor, but a few reactive lymphocytes were highlighted at the periphery. Staining for CD20 and CD30 was negative. Strong and diffuse staining for cyto-keratin 20 and pan-cytokeratin was noted within the tumor with the distinctive perinuclear pattern characteristic of Merkel cell carcinoma (MCC). Staining for cytokeratin 7 was negative. Synaptophysin and chromogranin were strongly and diffusely positive within the tumor, consistent with a diagnosis of MCC.
The patient was found to have stage IIA (T2N0M0) MCC. Computed tomography completed for staging showed no evidence of metastasis. Wide local excision of the lesion was performed. Margins were negative, as was a right inguinal sentinel lymph node dissection. Because of the size of the tumor and the presence of lymphovascular invasion, radiation therapy at the primary tumor site was recommended. Local radiation treatment (200 cGy daily) was administered for a total dose of 5000 cGy over 5 weeks. The patient currently is free of recurrence or metastases and is being followed by the oncology, surgery, and dermatology departments.
Comment
Merkel cell carcinoma is a rare aggressive cutaneous malignancy. The exact pathogenesis is unknown, but immunosuppression and UV radiation, possibly through its immunosuppressive effects, appear to be contributing factors. More recently, the Merkel cell polyomavirus has been linked to MCC in approximately 80% of cases.1,2
Merkel cell carcinoma is more common in individuals with fair skin, and the average age at diagnosis is 69 years.1 Patients typically present with an asymptomatic, firm, erythematous or violaceous, dome-shaped nodule or a small indurated plaque, most commonly on sun-exposed areas of the head and neck followed by the upper and lower extremities including the hands, feet, ankles, and wrists. Fifteen percent to 20% of MCCs develop on the legs and feet.1 Our patient presented with an MCC that developed on the right shin at a vein graft donor site.
The development of a cutaneous malignancy in a chronic wound (also known as a Marjolin ulcer) is a rare but well-recognized process. These malignancies occur in previously traumatized or chronically inflamed wounds and have been found to occur most commonly in chronic burn wounds, especially in ungrafted full-thickness burns. Squamous cell carcinomas (SCCs) are the most common malignancies to arise in chronic wounds, but basal cell carcinomas, adenocarcinomas, melanomas, malignant fibrous histiocytomas, adenoacanthomas, liposarcomas, and osteosarcomas also have been reported.3 There also have been a few reports of MCC associated with Bowen disease that developed in burn wounds.4 These malignancies generally occur years after injury (average, 35.5 years), but there have been reports of keratoacanthomas developing as early as 3 weeks after injury.5,6
In some reports, malignancies in skin graft donor sites are differentiated from Marjolin ulcers, as the former appear in healed surgical wounds rather than in chronic unstable wounds and tend to occur sooner (ie, in weeks to months after graft harvesting).7,8 The development of these malignancies in graft donor sites is not as well recognized and has been reported in donor sites for split-thickness skin grafts (STSGs), full-thickness skin grafts, tendon grafts, and bone grafts. In addition to malignancies that arise de novo, some develop due to metastatic and iatrogenic spread. The majority of reported malignancies in tendon and bone graft donor sites have been due to metastasis or iatrogenic spread.9-14
Iatrogenic implantation of tumor cells is a well-recognized phenomenon. Hussain et al10 reported a case of implantation of SCC in an STSG donor site, most likely due to direct seeding from a hollow needle used to infiltrate local anesthetic in the tumor area and the STSG. In this case, metastasis could not be completely ruled out.10 There also have been reports of osteosarcoma, ameloblastoma, scirrhous carcinoma of the breast, and malignant fibrous histiocytoma thought to be implanted at bone graft donor sites.14-17 Iatrogenic spread of malignancies can occur through seeding from contaminated gloves or instruments such as hollow bore needles or trocar placement in laparoscopic surgery.11 Airborne spread also may be possible, as viable melanoma cells have been detected in electrocautery plume in mice.13
Metastatic malignancies including metastases from SCC, adenocarcinoma, melanoma, malignant fibrous histiocytoma, angiosarcoma, and osteosarcoma also have been reported to develop in graft donor sites.11,13,18,19 Many malignancies thought to have developed from iatrogenic seeding may actually be from metastasis either by hematogenous or lymphatic spread. A possible contributing factor may be surgery-induced immunosuppression, which has been linked to increased tumor metastasis formation.20 Surgery or trauma have been shown to have an effect on cellular components of the immune system, causing changes such as a shift in T lymphocytes toward immune-suppressive T lymphocytes and impaired function of natural killer cells, neutrophils, and macrophages.20 The suppression of cell-mediated immunity has been shown to decrease over days to weeks in the postoperative period.21 In addition to surgery- or trauma-induced immunosuppression, the risk for metastasis may increase due to increased vascular, including lymphatic, flow toward a skin graft donor site.13,16 Furthermore, trauma predisposes areas to a hypercoagulable state with increased sludging as well as increased platelet counts and fibrinogen levels, which may lead to localization of metastatic lesions.22 All of these factors could potentially work simultaneously to induce the development of metastasis in graft donor sites.
We found that SCCs and keratoacanthomas, which may be a variant of SCC, are among the only primary malignancies that have been reported to develop in skin graft donor sites.6-8 Malignancies in these donor sites appear to develop sooner than those found in chronic wounds and are reported to develop within weeks to several months postoperatively, even in as few as 2 weeks.6,8 Tamir et al6 reported 2 keratoacanthomas that developed simultaneously in a burn scar and STSG donor site. The investigators believed it could be a sign of reduced immune surveillance in the 2 affected areas.6 It has been hypothesized that one cause of local immune suppression in Marjolin ulcers could be due to poor lymphatic regeneration in scar tissue, which would prevent delivery of antigens and stimulated lymphocytes.23 Haik et al7 considered this possibility when discussing a case of SCC that developed at the site of an STSG. The authors did not feel it applied, however, as the donor site had only undergone a single skin harvesting procedure.7 Ponnuvelu et al8 felt that inflammation was the underlying etiology behind the 2 cases they reported of SCCs that developed in STSG donor sites. The inflammation associated with tumors has many of the same processes involved in wound healing (eg, cellular proliferation, angiogenesis). Ponnuvelu et al8 hypothesized that the local inflammation caused by graft harvesting produced an ideal environment for early carcinogenesis. Although in chronic wounds it is believed that continual repair and regeneration in recurrent ulceration contributes to neoplastic initiation, it is thought that even a single injury may lead to malignant change, which may be because prior actinic damage or another cause has made the area more susceptible to these changes.24,25 Surgery-induced immunosuppression also may play a role in development of primary malignancies in graft donor sites.
There have been a few reports of SCCs and basal cell carcinomas occurring in other surgical scars that healed without complications.24,26-28 Similar to the malignancies in graft donor sites, some authors differentiate malignancies that occur in surgical scars that heal without complications from Marjolin ulcers, as they do not occur in chronically irritated wounds. These malignancies have been reported in scars from sternotomies, an infertility procedure, hair transplantation, thyroidectomy, colostomy, cleft lip repair, inguinal hernia repair, and paraumbilical laparoscopic port site. The time between surgery and diagnosis of malignancy ranged from 9 months to 67 years.24,26-28 The development of malignancies in these surgical scars may be due to local immunosuppression, possibly from decreased lymphatic flow; additionally, the inflammation in wound healing may provide the ideal environment for carcinogenesis. Trauma in areas already susceptible to malignant change could be a contributing factor.
Conclusion
Our patient developed an MCC in a vein graft donor site 18 years after vein harvesting. It was likely a primary tumor, as vein harvesting was done for coronary artery bypass graft. There was no evidence of any other lesions on physical examination or computed tomography, making it doubtful that an MCC serving as a primary lesion for seeding or metastasis was present. If such a lesion had been present at that time, it would likely have spread well before the time of presentation to our clinic due to the fast doubling time and high rate of metastasis characteristic of MCCs, further lessening the possibility of metastasis or implantation.
The extended length of time from procedure to lesion development in our patient is much longer than for other reported malignancies in graft donor sites, but the reported time for malignancies in other postsurgical scars is more varied. Regardless of whether the MCC in our patient is classified as a Marjolin ulcer, the pathogenesis is unclear. It is thought that a single injury could lead to malignant change in predisposed skin. Our patient’s legs did not have any evidence of prior actinic damage; however, it is likely that he had local immune suppression, which may have made him more susceptible to these changes. It is unlikely that surgery-induced immunosuppression played a role in our patient, as specific cellular components of the immune system only appear to be affected over days to weeks in the postoperative period. Although poor lymphatic regeneration in scar tissue leading to decreased immune surveillance is not generally thought to contribute to malignancies in most surgical scars, our patient underwent vein harvesting. Chronic edema commonly occurs after vein harvesting and is believed to be due to trauma to the lymphatics. Local immune suppression also may have led to increased susceptibility to infection by the MCC polyomavirus, which has been found to be associated with many MCCs. In addition, the area may have been more susceptible to carcinogenesis due to changes from inflammation from wound healing. We suspect together these factors contributed to the development of our patient’s MCC. Although rare, graft donor sites should be examined periodically for the development of malignancy.
Case Report
A 70-year-old man with history of coronary artery disease presented with a growing lesion on the right leg of 1 year’s duration. The lesion developed at a vein graft donor site for a coronary artery bypass that had been performed 18 years prior to presentation. The patient reported that the lesion was sensitive to touch. Physical examination revealed a 27-mm, firm, violaceous plaque on the medial aspect of the right upper shin (Figure 1). Mild pitting edema also was noted on both lower legs but was more prominent on the right leg. A 6-mm punch biopsy was performed.
Histology showed diffuse infiltration of the dermis and subcutaneous fat by intermediate-sized atypical blue cells with scant cytoplasm (Figure 2). The tumor exhibited moderate cytologic atypia with occasional mitotic figures, and lymphovascular invasion was present. Staining for CD3 was negative within the tumor, but a few reactive lymphocytes were highlighted at the periphery. Staining for CD20 and CD30 was negative. Strong and diffuse staining for cyto-keratin 20 and pan-cytokeratin was noted within the tumor with the distinctive perinuclear pattern characteristic of Merkel cell carcinoma (MCC). Staining for cytokeratin 7 was negative. Synaptophysin and chromogranin were strongly and diffusely positive within the tumor, consistent with a diagnosis of MCC.
The patient was found to have stage IIA (T2N0M0) MCC. Computed tomography completed for staging showed no evidence of metastasis. Wide local excision of the lesion was performed. Margins were negative, as was a right inguinal sentinel lymph node dissection. Because of the size of the tumor and the presence of lymphovascular invasion, radiation therapy at the primary tumor site was recommended. Local radiation treatment (200 cGy daily) was administered for a total dose of 5000 cGy over 5 weeks. The patient currently is free of recurrence or metastases and is being followed by the oncology, surgery, and dermatology departments.
Comment
Merkel cell carcinoma is a rare aggressive cutaneous malignancy. The exact pathogenesis is unknown, but immunosuppression and UV radiation, possibly through its immunosuppressive effects, appear to be contributing factors. More recently, the Merkel cell polyomavirus has been linked to MCC in approximately 80% of cases.1,2
Merkel cell carcinoma is more common in individuals with fair skin, and the average age at diagnosis is 69 years.1 Patients typically present with an asymptomatic, firm, erythematous or violaceous, dome-shaped nodule or a small indurated plaque, most commonly on sun-exposed areas of the head and neck followed by the upper and lower extremities including the hands, feet, ankles, and wrists. Fifteen percent to 20% of MCCs develop on the legs and feet.1 Our patient presented with an MCC that developed on the right shin at a vein graft donor site.
The development of a cutaneous malignancy in a chronic wound (also known as a Marjolin ulcer) is a rare but well-recognized process. These malignancies occur in previously traumatized or chronically inflamed wounds and have been found to occur most commonly in chronic burn wounds, especially in ungrafted full-thickness burns. Squamous cell carcinomas (SCCs) are the most common malignancies to arise in chronic wounds, but basal cell carcinomas, adenocarcinomas, melanomas, malignant fibrous histiocytomas, adenoacanthomas, liposarcomas, and osteosarcomas also have been reported.3 There also have been a few reports of MCC associated with Bowen disease that developed in burn wounds.4 These malignancies generally occur years after injury (average, 35.5 years), but there have been reports of keratoacanthomas developing as early as 3 weeks after injury.5,6
In some reports, malignancies in skin graft donor sites are differentiated from Marjolin ulcers, as the former appear in healed surgical wounds rather than in chronic unstable wounds and tend to occur sooner (ie, in weeks to months after graft harvesting).7,8 The development of these malignancies in graft donor sites is not as well recognized and has been reported in donor sites for split-thickness skin grafts (STSGs), full-thickness skin grafts, tendon grafts, and bone grafts. In addition to malignancies that arise de novo, some develop due to metastatic and iatrogenic spread. The majority of reported malignancies in tendon and bone graft donor sites have been due to metastasis or iatrogenic spread.9-14
Iatrogenic implantation of tumor cells is a well-recognized phenomenon. Hussain et al10 reported a case of implantation of SCC in an STSG donor site, most likely due to direct seeding from a hollow needle used to infiltrate local anesthetic in the tumor area and the STSG. In this case, metastasis could not be completely ruled out.10 There also have been reports of osteosarcoma, ameloblastoma, scirrhous carcinoma of the breast, and malignant fibrous histiocytoma thought to be implanted at bone graft donor sites.14-17 Iatrogenic spread of malignancies can occur through seeding from contaminated gloves or instruments such as hollow bore needles or trocar placement in laparoscopic surgery.11 Airborne spread also may be possible, as viable melanoma cells have been detected in electrocautery plume in mice.13
Metastatic malignancies including metastases from SCC, adenocarcinoma, melanoma, malignant fibrous histiocytoma, angiosarcoma, and osteosarcoma also have been reported to develop in graft donor sites.11,13,18,19 Many malignancies thought to have developed from iatrogenic seeding may actually be from metastasis either by hematogenous or lymphatic spread. A possible contributing factor may be surgery-induced immunosuppression, which has been linked to increased tumor metastasis formation.20 Surgery or trauma have been shown to have an effect on cellular components of the immune system, causing changes such as a shift in T lymphocytes toward immune-suppressive T lymphocytes and impaired function of natural killer cells, neutrophils, and macrophages.20 The suppression of cell-mediated immunity has been shown to decrease over days to weeks in the postoperative period.21 In addition to surgery- or trauma-induced immunosuppression, the risk for metastasis may increase due to increased vascular, including lymphatic, flow toward a skin graft donor site.13,16 Furthermore, trauma predisposes areas to a hypercoagulable state with increased sludging as well as increased platelet counts and fibrinogen levels, which may lead to localization of metastatic lesions.22 All of these factors could potentially work simultaneously to induce the development of metastasis in graft donor sites.
We found that SCCs and keratoacanthomas, which may be a variant of SCC, are among the only primary malignancies that have been reported to develop in skin graft donor sites.6-8 Malignancies in these donor sites appear to develop sooner than those found in chronic wounds and are reported to develop within weeks to several months postoperatively, even in as few as 2 weeks.6,8 Tamir et al6 reported 2 keratoacanthomas that developed simultaneously in a burn scar and STSG donor site. The investigators believed it could be a sign of reduced immune surveillance in the 2 affected areas.6 It has been hypothesized that one cause of local immune suppression in Marjolin ulcers could be due to poor lymphatic regeneration in scar tissue, which would prevent delivery of antigens and stimulated lymphocytes.23 Haik et al7 considered this possibility when discussing a case of SCC that developed at the site of an STSG. The authors did not feel it applied, however, as the donor site had only undergone a single skin harvesting procedure.7 Ponnuvelu et al8 felt that inflammation was the underlying etiology behind the 2 cases they reported of SCCs that developed in STSG donor sites. The inflammation associated with tumors has many of the same processes involved in wound healing (eg, cellular proliferation, angiogenesis). Ponnuvelu et al8 hypothesized that the local inflammation caused by graft harvesting produced an ideal environment for early carcinogenesis. Although in chronic wounds it is believed that continual repair and regeneration in recurrent ulceration contributes to neoplastic initiation, it is thought that even a single injury may lead to malignant change, which may be because prior actinic damage or another cause has made the area more susceptible to these changes.24,25 Surgery-induced immunosuppression also may play a role in development of primary malignancies in graft donor sites.
There have been a few reports of SCCs and basal cell carcinomas occurring in other surgical scars that healed without complications.24,26-28 Similar to the malignancies in graft donor sites, some authors differentiate malignancies that occur in surgical scars that heal without complications from Marjolin ulcers, as they do not occur in chronically irritated wounds. These malignancies have been reported in scars from sternotomies, an infertility procedure, hair transplantation, thyroidectomy, colostomy, cleft lip repair, inguinal hernia repair, and paraumbilical laparoscopic port site. The time between surgery and diagnosis of malignancy ranged from 9 months to 67 years.24,26-28 The development of malignancies in these surgical scars may be due to local immunosuppression, possibly from decreased lymphatic flow; additionally, the inflammation in wound healing may provide the ideal environment for carcinogenesis. Trauma in areas already susceptible to malignant change could be a contributing factor.
Conclusion
Our patient developed an MCC in a vein graft donor site 18 years after vein harvesting. It was likely a primary tumor, as vein harvesting was done for coronary artery bypass graft. There was no evidence of any other lesions on physical examination or computed tomography, making it doubtful that an MCC serving as a primary lesion for seeding or metastasis was present. If such a lesion had been present at that time, it would likely have spread well before the time of presentation to our clinic due to the fast doubling time and high rate of metastasis characteristic of MCCs, further lessening the possibility of metastasis or implantation.
The extended length of time from procedure to lesion development in our patient is much longer than for other reported malignancies in graft donor sites, but the reported time for malignancies in other postsurgical scars is more varied. Regardless of whether the MCC in our patient is classified as a Marjolin ulcer, the pathogenesis is unclear. It is thought that a single injury could lead to malignant change in predisposed skin. Our patient’s legs did not have any evidence of prior actinic damage; however, it is likely that he had local immune suppression, which may have made him more susceptible to these changes. It is unlikely that surgery-induced immunosuppression played a role in our patient, as specific cellular components of the immune system only appear to be affected over days to weeks in the postoperative period. Although poor lymphatic regeneration in scar tissue leading to decreased immune surveillance is not generally thought to contribute to malignancies in most surgical scars, our patient underwent vein harvesting. Chronic edema commonly occurs after vein harvesting and is believed to be due to trauma to the lymphatics. Local immune suppression also may have led to increased susceptibility to infection by the MCC polyomavirus, which has been found to be associated with many MCCs. In addition, the area may have been more susceptible to carcinogenesis due to changes from inflammation from wound healing. We suspect together these factors contributed to the development of our patient’s MCC. Although rare, graft donor sites should be examined periodically for the development of malignancy.
- Swann MH, Yoon J. Merkel cell carcinoma. Semin Oncol. 2007;34:51-56.
- Schrama D, Ugurel S, Becker JC. Merkel cell carcinoma: recent insights and new treatment options. Curr Opin Oncol. 2012;24:141-149.
- Kadir AR. Burn scar neoplasm. Ann Burns Fire Disasters. 2007;20:185-188.
- Walsh NM. Primary neuroendocrine (Merkel cell) carcinoma of the skin: morphologic diversity and implications thereof. Hum Pathol. 2001;32:680-689.
- Guenther N, Menenakos C, Braumann C, et al. Squamous cell carcinoma arising on a skin graft 64 years after primary injury. Dermatol Online J. 2007;13:27.
- Tamir G, Morgenstern S, Ben-Amitay D, et al. Synchronous appearance of keratoacanthomas in burn scar and skin graft donor site shortly after injury. J Am Acad Dermatol. 1999;40:870-871.
- Haik J, Georgiou I, Farber N, et al. Squamous cell carcinoma arising in a split-thickness skin graft donor site. Burns. 2008;34:891-893.
- Ponnuvelu G, Ng MF, Connolly CM, et al. Inflammation to skin malignancy, time to rethink the link: SCC in skin graft donor sites. Surgeon. 2011;9:168-169.
- Bekar A, Kahveci R, Tolunay S, et al. Metastatic gliosarcoma mass extension to a donor fascia lata graft harvest site by tumor cell contamination. World Neurosurg. 2010;73:719-721.
- Hussain A, Ekwobi C, Watson S. Metastatic implantation squamous cell carcinoma in a split-thickness skin graft donor site. J Plast Reconstr Aesthet Surg. 2011;64:690-692.
- May JT, Patil YJ. Keratoacanthoma-type squamous cell carcinoma developing in a skin graft donor site after tumor extirpation at a distant site. Ear Nose Throat J. 2010;89:E11-E13.
- Serrano-Ortega S, Buendia-Eisman A, Ortega del Olmo RM, et al. Melanoma metastasis in donor site of full-thickness skin graft. Dermatology. 2000;201:377-378.
- Wright H, McKinnell TH, Dunkin C. Recurrence of cutaneous squamous cell carcinoma at remote limb donor site. J Plast Reconstr Aesthet Surg. 2012;65:1265-1266.
- Yip KM, Lin J, Kumta SM. A pelvic osteosarcoma with metastasis to the donor site of the bone graft. a case report. Int Orthop. 1996;20:389-391.
- Dias RG, Abudu A, Carter SR, et al. Tumour transfer to bone graft donor site: a case report and review of the literature of the mechanism of seeding. Sarcoma. 2000;4:57-59.
- Neilson D, Emerson DJ, Dunn L. Squamous cell carcinoma of skin developing in a skin graft donor site. Br J Plast Surg. 1988;41:417-419.
- Singh C, Ibrahim S, Pang KS, et al. Implantation metastasis in a 13-year-old girl: a case report. J Orthop Surg (Hong Kong). 2003;11:94-96.
- Enion DS, Scott MJ, Gouldesbrough D. Cutaneous metastasis from a malignant fibrous histiocytoma to a limb skin graft donor site. Br J Surg. 1993;80:366.
- Yamasaki O, Terao K, Asagoe K, et al. Koebner phenomenon on skin graft donor site in cutaneous angiosarcoma. Eur J Dermatol. 2001;11:584-586.
- Hogan BV, Peter MB, Shenoy HG, et al. Surgery induced immunosuppression. Surgeon. 2011;9:38-43.
- Neeman E, Ben-Eliyahu S. The perioperative period and promotion of cancer metastasis: new outlooks on mediating mechanisms and immune involvement. Brain Behav Immun. 2013;30(suppl):32-40.
- Agostino D, Cliffton EE. Trauma as a cause of localization of blood-borne metastases: preventive effect of heparin and fibrinolysin. Ann Surg. 1965;161:97-102.
- Hammond JS, Thomsen S, Ward CG. Scar carcinoma arising acutely in a skin graft donor site. J Trauma. 1987;27:681-683.
- Korula R, Hughes CF. Squamous cell carcinoma arising in a sternotomy scar. Ann Thorac Surg. 1991;51:667-669.
- Kennedy CTC, Burd DAR, Creamer D. Mechanical and thermal injury. In: Burns T, Breathnach S, Cox N, et al, eds. Rook’s Textbook of Dermatology. Vol 2. 8th ed. Hoboken, NJ: Wiley-Blackwell; 2010:28.1-28.94.
- Durrani AJ, Miller RJ, Davies M. Basal cell carcinoma arising in a laparoscopic port site scar at the umbilicus. Plast Reconstr Surg. 2005;116:348-350.
- Kotwal S, Madaan S, Prescott S, et al. Unusual squamous cell carcinoma of the scrotum arising from a well healed, innocuous scar of an infertility procedure: a case report. Ann R Coll Surg Engl. 2007;89:17-19.
- Ozyazgan I, Kontas O. Previous injuries or scars as risk factors for the development of basal cell carcinoma. Scand J Plast Reconstr Surg Hand Surg. 2004;38:11-15.
- Swann MH, Yoon J. Merkel cell carcinoma. Semin Oncol. 2007;34:51-56.
- Schrama D, Ugurel S, Becker JC. Merkel cell carcinoma: recent insights and new treatment options. Curr Opin Oncol. 2012;24:141-149.
- Kadir AR. Burn scar neoplasm. Ann Burns Fire Disasters. 2007;20:185-188.
- Walsh NM. Primary neuroendocrine (Merkel cell) carcinoma of the skin: morphologic diversity and implications thereof. Hum Pathol. 2001;32:680-689.
- Guenther N, Menenakos C, Braumann C, et al. Squamous cell carcinoma arising on a skin graft 64 years after primary injury. Dermatol Online J. 2007;13:27.
- Tamir G, Morgenstern S, Ben-Amitay D, et al. Synchronous appearance of keratoacanthomas in burn scar and skin graft donor site shortly after injury. J Am Acad Dermatol. 1999;40:870-871.
- Haik J, Georgiou I, Farber N, et al. Squamous cell carcinoma arising in a split-thickness skin graft donor site. Burns. 2008;34:891-893.
- Ponnuvelu G, Ng MF, Connolly CM, et al. Inflammation to skin malignancy, time to rethink the link: SCC in skin graft donor sites. Surgeon. 2011;9:168-169.
- Bekar A, Kahveci R, Tolunay S, et al. Metastatic gliosarcoma mass extension to a donor fascia lata graft harvest site by tumor cell contamination. World Neurosurg. 2010;73:719-721.
- Hussain A, Ekwobi C, Watson S. Metastatic implantation squamous cell carcinoma in a split-thickness skin graft donor site. J Plast Reconstr Aesthet Surg. 2011;64:690-692.
- May JT, Patil YJ. Keratoacanthoma-type squamous cell carcinoma developing in a skin graft donor site after tumor extirpation at a distant site. Ear Nose Throat J. 2010;89:E11-E13.
- Serrano-Ortega S, Buendia-Eisman A, Ortega del Olmo RM, et al. Melanoma metastasis in donor site of full-thickness skin graft. Dermatology. 2000;201:377-378.
- Wright H, McKinnell TH, Dunkin C. Recurrence of cutaneous squamous cell carcinoma at remote limb donor site. J Plast Reconstr Aesthet Surg. 2012;65:1265-1266.
- Yip KM, Lin J, Kumta SM. A pelvic osteosarcoma with metastasis to the donor site of the bone graft. a case report. Int Orthop. 1996;20:389-391.
- Dias RG, Abudu A, Carter SR, et al. Tumour transfer to bone graft donor site: a case report and review of the literature of the mechanism of seeding. Sarcoma. 2000;4:57-59.
- Neilson D, Emerson DJ, Dunn L. Squamous cell carcinoma of skin developing in a skin graft donor site. Br J Plast Surg. 1988;41:417-419.
- Singh C, Ibrahim S, Pang KS, et al. Implantation metastasis in a 13-year-old girl: a case report. J Orthop Surg (Hong Kong). 2003;11:94-96.
- Enion DS, Scott MJ, Gouldesbrough D. Cutaneous metastasis from a malignant fibrous histiocytoma to a limb skin graft donor site. Br J Surg. 1993;80:366.
- Yamasaki O, Terao K, Asagoe K, et al. Koebner phenomenon on skin graft donor site in cutaneous angiosarcoma. Eur J Dermatol. 2001;11:584-586.
- Hogan BV, Peter MB, Shenoy HG, et al. Surgery induced immunosuppression. Surgeon. 2011;9:38-43.
- Neeman E, Ben-Eliyahu S. The perioperative period and promotion of cancer metastasis: new outlooks on mediating mechanisms and immune involvement. Brain Behav Immun. 2013;30(suppl):32-40.
- Agostino D, Cliffton EE. Trauma as a cause of localization of blood-borne metastases: preventive effect of heparin and fibrinolysin. Ann Surg. 1965;161:97-102.
- Hammond JS, Thomsen S, Ward CG. Scar carcinoma arising acutely in a skin graft donor site. J Trauma. 1987;27:681-683.
- Korula R, Hughes CF. Squamous cell carcinoma arising in a sternotomy scar. Ann Thorac Surg. 1991;51:667-669.
- Kennedy CTC, Burd DAR, Creamer D. Mechanical and thermal injury. In: Burns T, Breathnach S, Cox N, et al, eds. Rook’s Textbook of Dermatology. Vol 2. 8th ed. Hoboken, NJ: Wiley-Blackwell; 2010:28.1-28.94.
- Durrani AJ, Miller RJ, Davies M. Basal cell carcinoma arising in a laparoscopic port site scar at the umbilicus. Plast Reconstr Surg. 2005;116:348-350.
- Kotwal S, Madaan S, Prescott S, et al. Unusual squamous cell carcinoma of the scrotum arising from a well healed, innocuous scar of an infertility procedure: a case report. Ann R Coll Surg Engl. 2007;89:17-19.
- Ozyazgan I, Kontas O. Previous injuries or scars as risk factors for the development of basal cell carcinoma. Scand J Plast Reconstr Surg Hand Surg. 2004;38:11-15.
Practice Points
- Malignancies (both primary and metastatic) can develop in graft donor sites including donor sites for split-thickness skin, full-thickness skin, tendon, bone, and vein grafts.
- Primary malignancies that develop in graft donor sites may be distinct from malignancies that develop in chronic wounds, as the former occur in healed surgical wounds and tend to occur sooner after injury (ie, weeks to months after graft harvesting versus years).
- Although the occurrence is rare, graft donor sites should be examined periodically for development of malignancies.
Highlights From the 2016 AAN Annual Meeting
Click here to download the digital edition.
Click here to download the digital edition.
Click here to download the digital edition.
Irregular, Smooth, Pink Plaque on the Back
The Diagnosis: Fibroepithelioma of Pinkus
Fibroepithelioma of Pinkus (FeP) was first described in 19531 and was thought to be premalignant as evidenced by the proposed name premalignant fibroepithelial tumor of the skin. This neoplasm now is largely believed to represent a rare form of basal cell carcinoma (BCC). Typical presentation is a smooth, flesh-colored or pink plaque or nodule.2 Fibroepithelioma of Pinkus has a predilection for the lumbosacral back, though the groin also has been reported as a common site of incidence.1,3 Similar to other BCCs, it is seen in older individuals, typically those older than 50 years.3,4
Clinical diagnosis of FeP can be difficult. The differential diagnosis of FeP can include acrochordon, amelanotic melanoma, compound nevus, hemangioma, neurofibroma, nevus sebaceous, pyogenic granuloma, and seborrheic keratosis.5 Dermoscopic evaluation can aid in the diagnosis. A vascular network composed of fine arborizing vessels with or without dotted vessels and white streaks are characteristic findings of FeP. Patients with pigment also demonstrate structureless gray-brown areas and gray-blue dots.6
Biopsy with subsequent histopathologic evaluation confirms the diagnosis of FeP. The characteristic microscopic findings of thin eosinophilic epithelial strands with eccrine ducts anastomosing in an abundant fibromyxoid stroma with collections of basophilic cells located at the ends of the epithelial strands were demonstrated in our patient’s histopathologic specimen (Figure). The histologic appearance is similar to syringofibroadenoma of Mascaro. Recognition of basaloid nests, which often demonstrate retraction, and mitotic activity can differentiate FeP from syringofibroadenoma of Mascaro.7
Treatment of FeP is largely the same as other BCCs including destruction by electrodesiccation and curettage or complete removal by surgical excision. Several studies have demonstrated effective treatment of nonaggressive BCCs with curettage alone and subjectively reported improved cosmesis compared to electrodesiccation and curettage.8-10 Although methyl aminolevulinate photodynamic therapy has demonstrated some therapeutic efficacy for superficial and nodular BCCs,11 a case report utilizing the same modality for FeP did not provide adequate response.12 However, adequate data are not available to assess potential use of this less invasive therapy.
- Pinkus H. Premalignant fibroepithelial tumors of skin. AMA Arch Derm Syphilol. 1953;67:598-615.
- Bolognia J, Jorizzo JL, Schaffer JV. Dermatology. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012.
- Barr RJ, Herten RJ, Stone OJ. Multiple premalignant fibroepitheliomas of Pinkus: a case report and review of the literature. Cutis. 1978;21:335-337.
- Betti R, Inselvini E, Carducci M, et al. Age and site prevalence of histologic subtypes of basal cell carcinomas. Int J Dermatol. 1995;34:174-176.
- Cohen PR, Tschen JA. Fibroepithelioma of Pinkus presenting as a sessile thigh nodule. Skinmed. 2003;2:385-387.
- Zalaudek I, Ferrara G, Broganelli P, et al. Dermoscopy patterns of fibroepithelioma of Pinkus. Arch Dermatol. 2006;142:1318-1322.
- Schadt CR, Boyd AS. Eccrine syringofibroadenoma with co-existent squamous cell carcinoma. J Cutan Pathol. 2007;34(suppl 1):71-74.
- Barlow JO, Zalla MJ, Kyle A, et al. Treatment of basal cell carcinoma with curettage alone. J Am Acad Dermatol. 2006;54:1039-1045.
- McDaniel WE. Therapy for basal cell epitheliomas by curettage only. further study. Arch Dermatol. 1983;119:901-903.
- Reymann F. 15 Years’ experience with treatment of basal cell carcinomas of the skin with curettage. Acta Derm Venereol Suppl (Stockh). 1985;120:56-59.
- Fai D, Arpaia N, Romano I, et al. Methyl-aminolevulinate photodynamic therapy for the treatment of actinic keratoses and non-melanoma skin cancers: a retrospective analysis of response in 462 patients. G Ital Dermatol Venereol. 2009;144:281-285.
- Park MY, Kim YC. Fibroepithelioma of Pinkus: poor response to topical photodynamic therapy. Eur J Dermatol. 2010;20:133-134.
The Diagnosis: Fibroepithelioma of Pinkus
Fibroepithelioma of Pinkus (FeP) was first described in 19531 and was thought to be premalignant as evidenced by the proposed name premalignant fibroepithelial tumor of the skin. This neoplasm now is largely believed to represent a rare form of basal cell carcinoma (BCC). Typical presentation is a smooth, flesh-colored or pink plaque or nodule.2 Fibroepithelioma of Pinkus has a predilection for the lumbosacral back, though the groin also has been reported as a common site of incidence.1,3 Similar to other BCCs, it is seen in older individuals, typically those older than 50 years.3,4
Clinical diagnosis of FeP can be difficult. The differential diagnosis of FeP can include acrochordon, amelanotic melanoma, compound nevus, hemangioma, neurofibroma, nevus sebaceous, pyogenic granuloma, and seborrheic keratosis.5 Dermoscopic evaluation can aid in the diagnosis. A vascular network composed of fine arborizing vessels with or without dotted vessels and white streaks are characteristic findings of FeP. Patients with pigment also demonstrate structureless gray-brown areas and gray-blue dots.6
Biopsy with subsequent histopathologic evaluation confirms the diagnosis of FeP. The characteristic microscopic findings of thin eosinophilic epithelial strands with eccrine ducts anastomosing in an abundant fibromyxoid stroma with collections of basophilic cells located at the ends of the epithelial strands were demonstrated in our patient’s histopathologic specimen (Figure). The histologic appearance is similar to syringofibroadenoma of Mascaro. Recognition of basaloid nests, which often demonstrate retraction, and mitotic activity can differentiate FeP from syringofibroadenoma of Mascaro.7
Treatment of FeP is largely the same as other BCCs including destruction by electrodesiccation and curettage or complete removal by surgical excision. Several studies have demonstrated effective treatment of nonaggressive BCCs with curettage alone and subjectively reported improved cosmesis compared to electrodesiccation and curettage.8-10 Although methyl aminolevulinate photodynamic therapy has demonstrated some therapeutic efficacy for superficial and nodular BCCs,11 a case report utilizing the same modality for FeP did not provide adequate response.12 However, adequate data are not available to assess potential use of this less invasive therapy.
The Diagnosis: Fibroepithelioma of Pinkus
Fibroepithelioma of Pinkus (FeP) was first described in 19531 and was thought to be premalignant as evidenced by the proposed name premalignant fibroepithelial tumor of the skin. This neoplasm now is largely believed to represent a rare form of basal cell carcinoma (BCC). Typical presentation is a smooth, flesh-colored or pink plaque or nodule.2 Fibroepithelioma of Pinkus has a predilection for the lumbosacral back, though the groin also has been reported as a common site of incidence.1,3 Similar to other BCCs, it is seen in older individuals, typically those older than 50 years.3,4
Clinical diagnosis of FeP can be difficult. The differential diagnosis of FeP can include acrochordon, amelanotic melanoma, compound nevus, hemangioma, neurofibroma, nevus sebaceous, pyogenic granuloma, and seborrheic keratosis.5 Dermoscopic evaluation can aid in the diagnosis. A vascular network composed of fine arborizing vessels with or without dotted vessels and white streaks are characteristic findings of FeP. Patients with pigment also demonstrate structureless gray-brown areas and gray-blue dots.6
Biopsy with subsequent histopathologic evaluation confirms the diagnosis of FeP. The characteristic microscopic findings of thin eosinophilic epithelial strands with eccrine ducts anastomosing in an abundant fibromyxoid stroma with collections of basophilic cells located at the ends of the epithelial strands were demonstrated in our patient’s histopathologic specimen (Figure). The histologic appearance is similar to syringofibroadenoma of Mascaro. Recognition of basaloid nests, which often demonstrate retraction, and mitotic activity can differentiate FeP from syringofibroadenoma of Mascaro.7
Treatment of FeP is largely the same as other BCCs including destruction by electrodesiccation and curettage or complete removal by surgical excision. Several studies have demonstrated effective treatment of nonaggressive BCCs with curettage alone and subjectively reported improved cosmesis compared to electrodesiccation and curettage.8-10 Although methyl aminolevulinate photodynamic therapy has demonstrated some therapeutic efficacy for superficial and nodular BCCs,11 a case report utilizing the same modality for FeP did not provide adequate response.12 However, adequate data are not available to assess potential use of this less invasive therapy.
- Pinkus H. Premalignant fibroepithelial tumors of skin. AMA Arch Derm Syphilol. 1953;67:598-615.
- Bolognia J, Jorizzo JL, Schaffer JV. Dermatology. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012.
- Barr RJ, Herten RJ, Stone OJ. Multiple premalignant fibroepitheliomas of Pinkus: a case report and review of the literature. Cutis. 1978;21:335-337.
- Betti R, Inselvini E, Carducci M, et al. Age and site prevalence of histologic subtypes of basal cell carcinomas. Int J Dermatol. 1995;34:174-176.
- Cohen PR, Tschen JA. Fibroepithelioma of Pinkus presenting as a sessile thigh nodule. Skinmed. 2003;2:385-387.
- Zalaudek I, Ferrara G, Broganelli P, et al. Dermoscopy patterns of fibroepithelioma of Pinkus. Arch Dermatol. 2006;142:1318-1322.
- Schadt CR, Boyd AS. Eccrine syringofibroadenoma with co-existent squamous cell carcinoma. J Cutan Pathol. 2007;34(suppl 1):71-74.
- Barlow JO, Zalla MJ, Kyle A, et al. Treatment of basal cell carcinoma with curettage alone. J Am Acad Dermatol. 2006;54:1039-1045.
- McDaniel WE. Therapy for basal cell epitheliomas by curettage only. further study. Arch Dermatol. 1983;119:901-903.
- Reymann F. 15 Years’ experience with treatment of basal cell carcinomas of the skin with curettage. Acta Derm Venereol Suppl (Stockh). 1985;120:56-59.
- Fai D, Arpaia N, Romano I, et al. Methyl-aminolevulinate photodynamic therapy for the treatment of actinic keratoses and non-melanoma skin cancers: a retrospective analysis of response in 462 patients. G Ital Dermatol Venereol. 2009;144:281-285.
- Park MY, Kim YC. Fibroepithelioma of Pinkus: poor response to topical photodynamic therapy. Eur J Dermatol. 2010;20:133-134.
- Pinkus H. Premalignant fibroepithelial tumors of skin. AMA Arch Derm Syphilol. 1953;67:598-615.
- Bolognia J, Jorizzo JL, Schaffer JV. Dermatology. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012.
- Barr RJ, Herten RJ, Stone OJ. Multiple premalignant fibroepitheliomas of Pinkus: a case report and review of the literature. Cutis. 1978;21:335-337.
- Betti R, Inselvini E, Carducci M, et al. Age and site prevalence of histologic subtypes of basal cell carcinomas. Int J Dermatol. 1995;34:174-176.
- Cohen PR, Tschen JA. Fibroepithelioma of Pinkus presenting as a sessile thigh nodule. Skinmed. 2003;2:385-387.
- Zalaudek I, Ferrara G, Broganelli P, et al. Dermoscopy patterns of fibroepithelioma of Pinkus. Arch Dermatol. 2006;142:1318-1322.
- Schadt CR, Boyd AS. Eccrine syringofibroadenoma with co-existent squamous cell carcinoma. J Cutan Pathol. 2007;34(suppl 1):71-74.
- Barlow JO, Zalla MJ, Kyle A, et al. Treatment of basal cell carcinoma with curettage alone. J Am Acad Dermatol. 2006;54:1039-1045.
- McDaniel WE. Therapy for basal cell epitheliomas by curettage only. further study. Arch Dermatol. 1983;119:901-903.
- Reymann F. 15 Years’ experience with treatment of basal cell carcinomas of the skin with curettage. Acta Derm Venereol Suppl (Stockh). 1985;120:56-59.
- Fai D, Arpaia N, Romano I, et al. Methyl-aminolevulinate photodynamic therapy for the treatment of actinic keratoses and non-melanoma skin cancers: a retrospective analysis of response in 462 patients. G Ital Dermatol Venereol. 2009;144:281-285.
- Park MY, Kim YC. Fibroepithelioma of Pinkus: poor response to topical photodynamic therapy. Eur J Dermatol. 2010;20:133-134.

If a Chronic Wound Does Not Heal, Biopsy It: A Clinical Lesson on Underlying Malignancies
To the Editor:
Experience, subjective opinion, and relationships with patients are cornerstones of general practice but also can be pitfalls. It is common for a late-presenting patient to offer a seemingly rational explanation for a long-standing lesion. Unless an objective analysis of the clinical problem is undertaken, it can be easy to embark on an incorrect treatment pathway for the patient’s condition.
One of the luxuries of specialist hospital medicine or surgery is the ability to focus on a narrow range of clinical problems, which makes it easier to spot the anomaly, as long as it is within the purview of the practitioner. We report 2 cases of skin malignancies that were assumed to be chronic wounds of benign etiology.
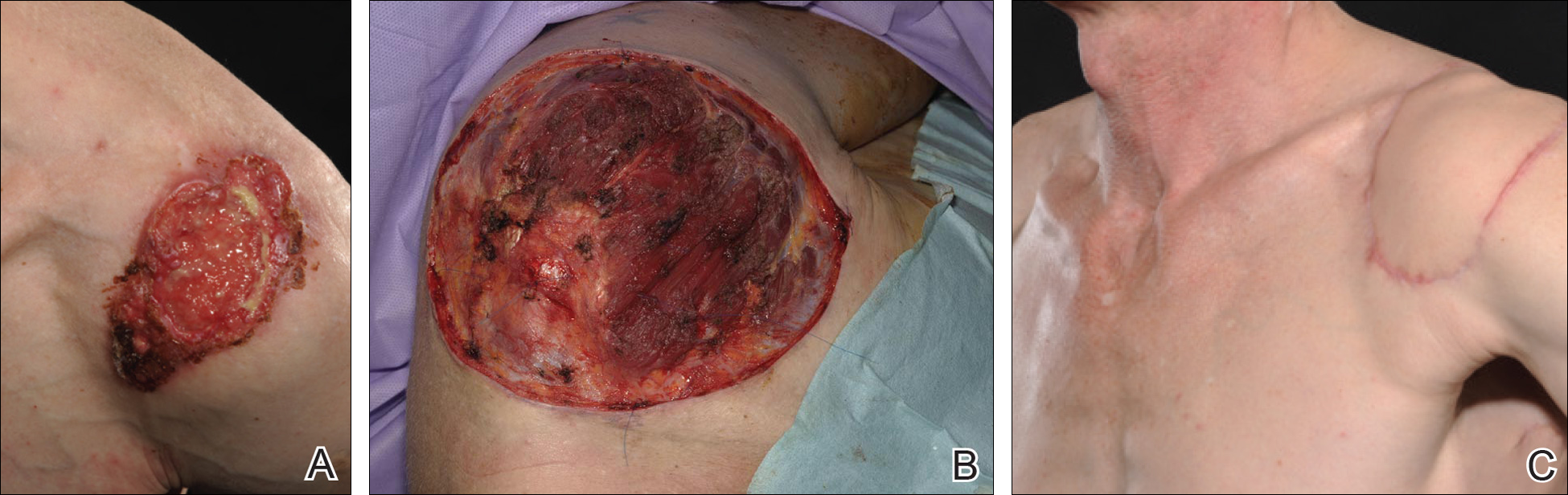
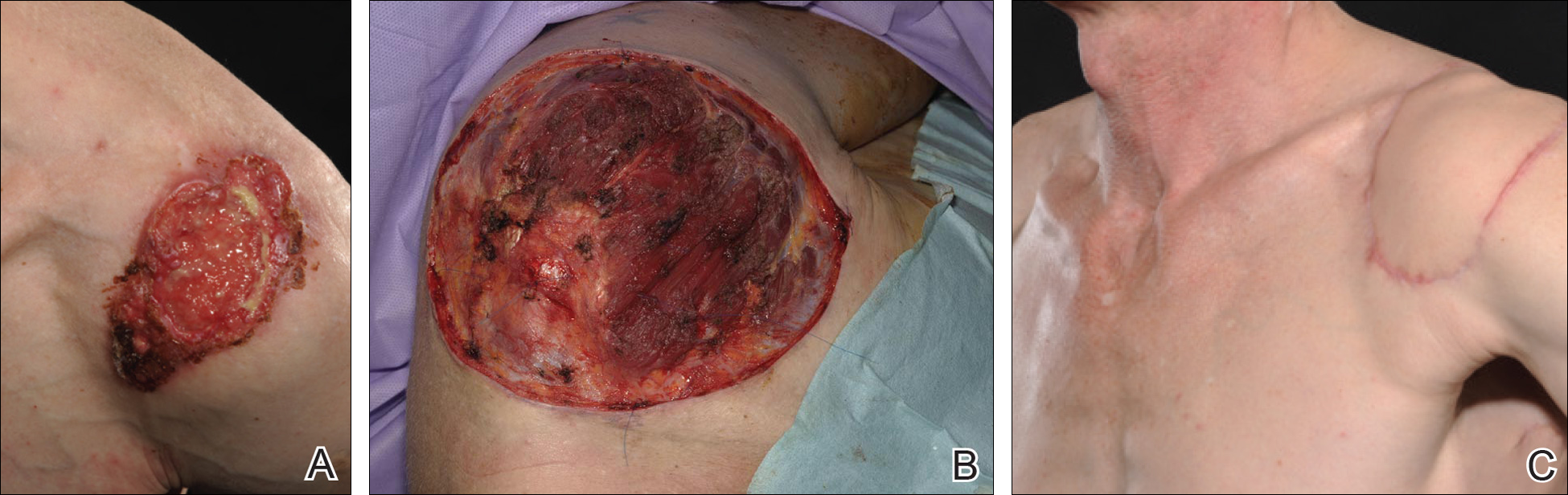
A 63-year-old builder was referred by his general practitioner with a chronic wound on the right forearm of 4 years’ duration. His medical history included psoriasis, and he did not have a history of diabetes mellitus or use of immunosuppressants. The general practitioner suggested possible incidental origin following a prior trauma or a psoriatic-related lesion. The patient reported that the lesion did not resemble prior psoriatic lesions and it had deteriorated substantially over the last 2 years. Furthermore, a small ulcer was starting to develop on the left forearm. Further advice was requested by the general practitioner regarding wound dressings. On examination a sloughy ulcer measuring 8.5×7.5 cm had eroded to expose necrotic tendons with surrounding induration and cellulitis (Figure 1A). In addition, a psoriatic lesion was found on the left forearm (Figure 1B). There were no palpable axillary lymph nodes. Clinical suspicion, incision biopsies, and subsequent histology confirmed cutaneous CD4+ T-cell lymphoma. This case was reviewed at a multidisciplinary team meeting and referred to the hematology-oncology department. The patient subsequently underwent chemotherapy with liposomal doxorubicin and radiotherapy over a period of 5 months. An elective right forearm amputation was planned due to erosion of the ulcer through tendons down to bone (Figure 2).


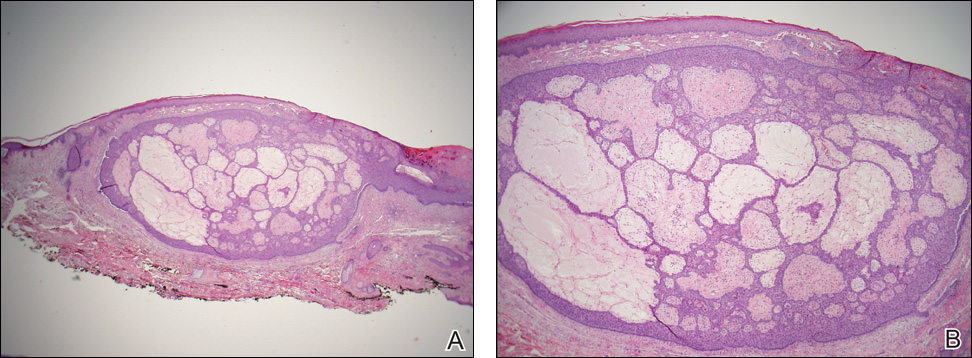
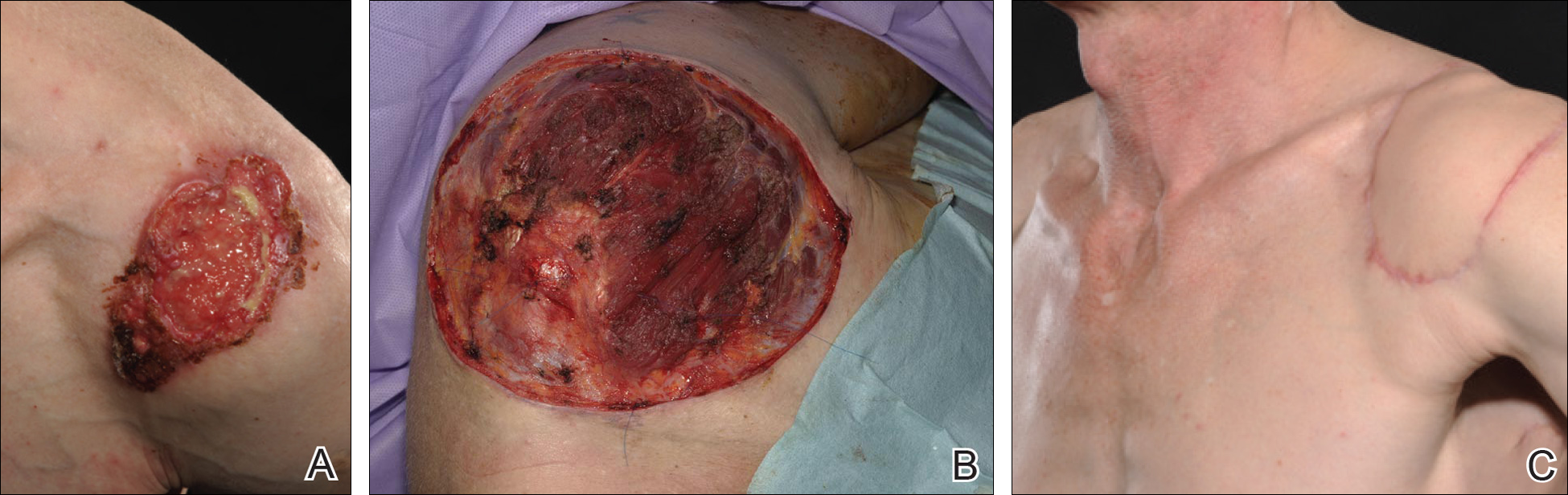
A 48-year-old Latvian lorry driver was referred by his general practitioner with a chronic wound on the left shoulder of 6 years’ duration. His medical history included a partial gastrectomy for a peptic ulcer 18 years prior, and he did not have a history of diabetes mellitus or use of immunosuppressants. The general practitioner included a partial gastrectomy for a peptic ulcer 18 years prior, and he did not have a history of diabetes mellitus or use of immunosuppressants. The general practitioner suggested the etiology was a burn from a hot metal rod 6 years prior. Advice was sought regarding dressings and suitability for a possible skin graft. Physical examination showed a 4.5×10-cm ulcer fixed to the underlying tissue on the anterior aspect of the left shoulder with no evidence of infection or presence of a foreign body (Figure 3A). Clinical suspicion, incision biopsies, and subsequent histology confirmed a highly infiltrative/morphoeic, partly nodular, and partly diffuse basal cell carcinoma (BCC) that measured 92 mm in diameter extending to the subcutis with no involvement of muscle or perineural or vascular invasion. The patient underwent wide local excision of the BCC with frozen section control. The BCC had eroded into the deltoid muscle and to the periosteum of the clavicle (Figure 3B). The defect was reconstructed with a pedicled muscle-sparing latissimus dorsi musculocutaneous flap. The patient presented for follow-up months following reconstruction with an uneventful recovery (Figure 3C).
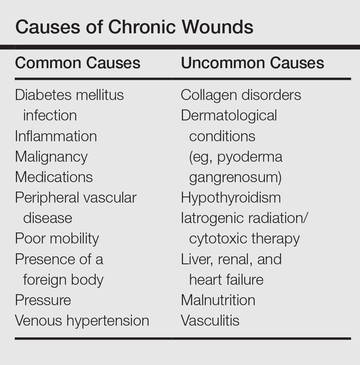
These 2 cases highlight easy pitfalls for an unsuspecting clinician. Although both cases had alternative plausible explanations, they proved to be cutaneous malignancies. The powerful message these cases send is that long-standing chronic wounds should be biopsied to exclude malignancy. Some of the other common underlying causes of wounds that may prevent healing are highlighted in the Table. Vascular insufficiency usually presents in characteristic patterns with a good clinical history and associated signs and findings on investigation. A foreign body, which can be anything from an orthopedic metal implant to a retained stitch from surgery or nonmedical material, may be the culprit and may be identified from a thorough medical history or appropriate imaging.
Infection is another possible explanation of a nonhealing wound. On the face, an underlying dental abscess with a sinus tracking from the root of the tooth to the skin of the cheek or jaw may be the source. Elsewhere on the body, chronic osteomyelitis may be the cause, which may be from any infective origin from Staphylococcus aureus to tuberculosis, and will most commonly present with a discharging sinus but also may present with a nonspecific ulcer.
Chronic wounds also may not heal because of a multitude of patient factors such as poor nutrition, diabetes mellitus, medication (eg, steroids, nonsteroidal anti-inflammatory drugs), other inflammatory causes, and poor mobility. Chronic wounds represent a substantial burden to patients, health care professionals, and the health care system. In the United States alone, they affect 5.7 million patients and cost an estimated $20 billion.1 Approximately 1% of the Western population will present with leg ulceration at some point in their lives.2
Physical examination of ulcers in any clinical setting can be difficult. We postulate that it can be made more difficult at times in primary care because the patient may add confounding elements for consideration or seemingly plausible explanations. However, whenever possible, a physician should ask, “Could there possibly be an underlying malignancy here?” If there is any chance of malignancy despite plausible explanations being offered, the lesion should be biopsied.
- Branski LK, Gauglitz GG, Herndon DN, et al. A review of gene and stem cell therapy in cutaneous wound healing [published online July 7, 2008]. Burns. 2009;35:171-180.
- Callam MJ. Prevalence of chronic leg ulceration and severe chronic venous disease in western countries. Phlebology. 1992;7(suppl 1):6-12.
To the Editor:
Experience, subjective opinion, and relationships with patients are cornerstones of general practice but also can be pitfalls. It is common for a late-presenting patient to offer a seemingly rational explanation for a long-standing lesion. Unless an objective analysis of the clinical problem is undertaken, it can be easy to embark on an incorrect treatment pathway for the patient’s condition.
One of the luxuries of specialist hospital medicine or surgery is the ability to focus on a narrow range of clinical problems, which makes it easier to spot the anomaly, as long as it is within the purview of the practitioner. We report 2 cases of skin malignancies that were assumed to be chronic wounds of benign etiology.
A 63-year-old builder was referred by his general practitioner with a chronic wound on the right forearm of 4 years’ duration. His medical history included psoriasis, and he did not have a history of diabetes mellitus or use of immunosuppressants. The general practitioner suggested possible incidental origin following a prior trauma or a psoriatic-related lesion. The patient reported that the lesion did not resemble prior psoriatic lesions and it had deteriorated substantially over the last 2 years. Furthermore, a small ulcer was starting to develop on the left forearm. Further advice was requested by the general practitioner regarding wound dressings. On examination a sloughy ulcer measuring 8.5×7.5 cm had eroded to expose necrotic tendons with surrounding induration and cellulitis (Figure 1A). In addition, a psoriatic lesion was found on the left forearm (Figure 1B). There were no palpable axillary lymph nodes. Clinical suspicion, incision biopsies, and subsequent histology confirmed cutaneous CD4+ T-cell lymphoma. This case was reviewed at a multidisciplinary team meeting and referred to the hematology-oncology department. The patient subsequently underwent chemotherapy with liposomal doxorubicin and radiotherapy over a period of 5 months. An elective right forearm amputation was planned due to erosion of the ulcer through tendons down to bone (Figure 2).


A 48-year-old Latvian lorry driver was referred by his general practitioner with a chronic wound on the left shoulder of 6 years’ duration. His medical history included a partial gastrectomy for a peptic ulcer 18 years prior, and he did not have a history of diabetes mellitus or use of immunosuppressants. The general practitioner included a partial gastrectomy for a peptic ulcer 18 years prior, and he did not have a history of diabetes mellitus or use of immunosuppressants. The general practitioner suggested the etiology was a burn from a hot metal rod 6 years prior. Advice was sought regarding dressings and suitability for a possible skin graft. Physical examination showed a 4.5×10-cm ulcer fixed to the underlying tissue on the anterior aspect of the left shoulder with no evidence of infection or presence of a foreign body (Figure 3A). Clinical suspicion, incision biopsies, and subsequent histology confirmed a highly infiltrative/morphoeic, partly nodular, and partly diffuse basal cell carcinoma (BCC) that measured 92 mm in diameter extending to the subcutis with no involvement of muscle or perineural or vascular invasion. The patient underwent wide local excision of the BCC with frozen section control. The BCC had eroded into the deltoid muscle and to the periosteum of the clavicle (Figure 3B). The defect was reconstructed with a pedicled muscle-sparing latissimus dorsi musculocutaneous flap. The patient presented for follow-up months following reconstruction with an uneventful recovery (Figure 3C).
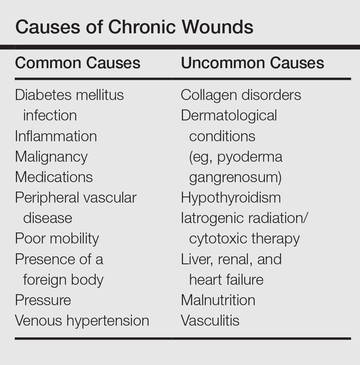
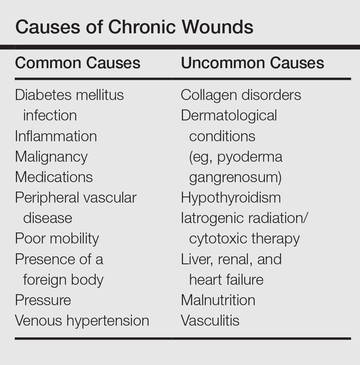
These 2 cases highlight easy pitfalls for an unsuspecting clinician. Although both cases had alternative plausible explanations, they proved to be cutaneous malignancies. The powerful message these cases send is that long-standing chronic wounds should be biopsied to exclude malignancy. Some of the other common underlying causes of wounds that may prevent healing are highlighted in the Table. Vascular insufficiency usually presents in characteristic patterns with a good clinical history and associated signs and findings on investigation. A foreign body, which can be anything from an orthopedic metal implant to a retained stitch from surgery or nonmedical material, may be the culprit and may be identified from a thorough medical history or appropriate imaging.
Infection is another possible explanation of a nonhealing wound. On the face, an underlying dental abscess with a sinus tracking from the root of the tooth to the skin of the cheek or jaw may be the source. Elsewhere on the body, chronic osteomyelitis may be the cause, which may be from any infective origin from Staphylococcus aureus to tuberculosis, and will most commonly present with a discharging sinus but also may present with a nonspecific ulcer.
Chronic wounds also may not heal because of a multitude of patient factors such as poor nutrition, diabetes mellitus, medication (eg, steroids, nonsteroidal anti-inflammatory drugs), other inflammatory causes, and poor mobility. Chronic wounds represent a substantial burden to patients, health care professionals, and the health care system. In the United States alone, they affect 5.7 million patients and cost an estimated $20 billion.1 Approximately 1% of the Western population will present with leg ulceration at some point in their lives.2
Physical examination of ulcers in any clinical setting can be difficult. We postulate that it can be made more difficult at times in primary care because the patient may add confounding elements for consideration or seemingly plausible explanations. However, whenever possible, a physician should ask, “Could there possibly be an underlying malignancy here?” If there is any chance of malignancy despite plausible explanations being offered, the lesion should be biopsied.
To the Editor:
Experience, subjective opinion, and relationships with patients are cornerstones of general practice but also can be pitfalls. It is common for a late-presenting patient to offer a seemingly rational explanation for a long-standing lesion. Unless an objective analysis of the clinical problem is undertaken, it can be easy to embark on an incorrect treatment pathway for the patient’s condition.
One of the luxuries of specialist hospital medicine or surgery is the ability to focus on a narrow range of clinical problems, which makes it easier to spot the anomaly, as long as it is within the purview of the practitioner. We report 2 cases of skin malignancies that were assumed to be chronic wounds of benign etiology.
A 63-year-old builder was referred by his general practitioner with a chronic wound on the right forearm of 4 years’ duration. His medical history included psoriasis, and he did not have a history of diabetes mellitus or use of immunosuppressants. The general practitioner suggested possible incidental origin following a prior trauma or a psoriatic-related lesion. The patient reported that the lesion did not resemble prior psoriatic lesions and it had deteriorated substantially over the last 2 years. Furthermore, a small ulcer was starting to develop on the left forearm. Further advice was requested by the general practitioner regarding wound dressings. On examination a sloughy ulcer measuring 8.5×7.5 cm had eroded to expose necrotic tendons with surrounding induration and cellulitis (Figure 1A). In addition, a psoriatic lesion was found on the left forearm (Figure 1B). There were no palpable axillary lymph nodes. Clinical suspicion, incision biopsies, and subsequent histology confirmed cutaneous CD4+ T-cell lymphoma. This case was reviewed at a multidisciplinary team meeting and referred to the hematology-oncology department. The patient subsequently underwent chemotherapy with liposomal doxorubicin and radiotherapy over a period of 5 months. An elective right forearm amputation was planned due to erosion of the ulcer through tendons down to bone (Figure 2).


A 48-year-old Latvian lorry driver was referred by his general practitioner with a chronic wound on the left shoulder of 6 years’ duration. His medical history included a partial gastrectomy for a peptic ulcer 18 years prior, and he did not have a history of diabetes mellitus or use of immunosuppressants. The general practitioner included a partial gastrectomy for a peptic ulcer 18 years prior, and he did not have a history of diabetes mellitus or use of immunosuppressants. The general practitioner suggested the etiology was a burn from a hot metal rod 6 years prior. Advice was sought regarding dressings and suitability for a possible skin graft. Physical examination showed a 4.5×10-cm ulcer fixed to the underlying tissue on the anterior aspect of the left shoulder with no evidence of infection or presence of a foreign body (Figure 3A). Clinical suspicion, incision biopsies, and subsequent histology confirmed a highly infiltrative/morphoeic, partly nodular, and partly diffuse basal cell carcinoma (BCC) that measured 92 mm in diameter extending to the subcutis with no involvement of muscle or perineural or vascular invasion. The patient underwent wide local excision of the BCC with frozen section control. The BCC had eroded into the deltoid muscle and to the periosteum of the clavicle (Figure 3B). The defect was reconstructed with a pedicled muscle-sparing latissimus dorsi musculocutaneous flap. The patient presented for follow-up months following reconstruction with an uneventful recovery (Figure 3C).
These 2 cases highlight easy pitfalls for an unsuspecting clinician. Although both cases had alternative plausible explanations, they proved to be cutaneous malignancies. The powerful message these cases send is that long-standing chronic wounds should be biopsied to exclude malignancy. Some of the other common underlying causes of wounds that may prevent healing are highlighted in the Table. Vascular insufficiency usually presents in characteristic patterns with a good clinical history and associated signs and findings on investigation. A foreign body, which can be anything from an orthopedic metal implant to a retained stitch from surgery or nonmedical material, may be the culprit and may be identified from a thorough medical history or appropriate imaging.
Infection is another possible explanation of a nonhealing wound. On the face, an underlying dental abscess with a sinus tracking from the root of the tooth to the skin of the cheek or jaw may be the source. Elsewhere on the body, chronic osteomyelitis may be the cause, which may be from any infective origin from Staphylococcus aureus to tuberculosis, and will most commonly present with a discharging sinus but also may present with a nonspecific ulcer.
Chronic wounds also may not heal because of a multitude of patient factors such as poor nutrition, diabetes mellitus, medication (eg, steroids, nonsteroidal anti-inflammatory drugs), other inflammatory causes, and poor mobility. Chronic wounds represent a substantial burden to patients, health care professionals, and the health care system. In the United States alone, they affect 5.7 million patients and cost an estimated $20 billion.1 Approximately 1% of the Western population will present with leg ulceration at some point in their lives.2
Physical examination of ulcers in any clinical setting can be difficult. We postulate that it can be made more difficult at times in primary care because the patient may add confounding elements for consideration or seemingly plausible explanations. However, whenever possible, a physician should ask, “Could there possibly be an underlying malignancy here?” If there is any chance of malignancy despite plausible explanations being offered, the lesion should be biopsied.
- Branski LK, Gauglitz GG, Herndon DN, et al. A review of gene and stem cell therapy in cutaneous wound healing [published online July 7, 2008]. Burns. 2009;35:171-180.
- Callam MJ. Prevalence of chronic leg ulceration and severe chronic venous disease in western countries. Phlebology. 1992;7(suppl 1):6-12.
- Branski LK, Gauglitz GG, Herndon DN, et al. A review of gene and stem cell therapy in cutaneous wound healing [published online July 7, 2008]. Burns. 2009;35:171-180.
- Callam MJ. Prevalence of chronic leg ulceration and severe chronic venous disease in western countries. Phlebology. 1992;7(suppl 1):6-12.
Practice Points
- Patients with chronic wounds should have a thorough history and examination, appropriate laboratory tests, and purposeful search to determine etiology.
- Long-standing chronic wounds should be biopsied to exclude malignancy.
Benefits of Hospital-Wide Mortality Reviews
Most divisions within a hospital will have a morbidity or mortality round where they review deaths that occurred in that department, but doing that on an institution-wide level is unusual and important. “It gives a totally different viewpoint,” he says. “When it’s a couple highly selected patients whose cases you examine, you really don’t have an idea at the end if the problems you identified are systemwide issues in your institution.”
The major issue the study identified was an inadequate discussion of goals of care. “This was often a patient who was dying, and in retrospect, it was clear that they were at high risk for death, but there had been no discussion with the patient about prognosis or about symptom management,” Dr. Kobewka says. “It seemed that care was directed at prolonging life. When we looked back at the case, that wasn’t realistic. That accounted for 25% of the quality issues that we identified: The discussion of prognosis and goals of care was inadequate or even absent all together. I think every hospital needs to think about those discussions and how and where and when we have them.”
Another revelation from the study: Errors in care are common but also underdiscussed. “When a physician is aware that maybe there was an error in care, it’s easy for there to be guilt and secrecy,” Dr. Kobewka says. “This is just a reminder that it’s common, and we need an open discussion about it. We need high-level, institution-wide systems to help us with this, but even at the individual provider level, this discussion needs to happen. Any quality improvement process needs engagement of frontline staff.”
Reference
- Kobewka DM, van Walraven C, Turnbull J, Worthington J, Calder L, Forster A. Quality gaps identified through mortality review [published online ahead of print February 8, 2016]. BMJ Qual Saf. doi:10.1136/bmjqs-2015-004735.
Most divisions within a hospital will have a morbidity or mortality round where they review deaths that occurred in that department, but doing that on an institution-wide level is unusual and important. “It gives a totally different viewpoint,” he says. “When it’s a couple highly selected patients whose cases you examine, you really don’t have an idea at the end if the problems you identified are systemwide issues in your institution.”
The major issue the study identified was an inadequate discussion of goals of care. “This was often a patient who was dying, and in retrospect, it was clear that they were at high risk for death, but there had been no discussion with the patient about prognosis or about symptom management,” Dr. Kobewka says. “It seemed that care was directed at prolonging life. When we looked back at the case, that wasn’t realistic. That accounted for 25% of the quality issues that we identified: The discussion of prognosis and goals of care was inadequate or even absent all together. I think every hospital needs to think about those discussions and how and where and when we have them.”
Another revelation from the study: Errors in care are common but also underdiscussed. “When a physician is aware that maybe there was an error in care, it’s easy for there to be guilt and secrecy,” Dr. Kobewka says. “This is just a reminder that it’s common, and we need an open discussion about it. We need high-level, institution-wide systems to help us with this, but even at the individual provider level, this discussion needs to happen. Any quality improvement process needs engagement of frontline staff.”
Reference
- Kobewka DM, van Walraven C, Turnbull J, Worthington J, Calder L, Forster A. Quality gaps identified through mortality review [published online ahead of print February 8, 2016]. BMJ Qual Saf. doi:10.1136/bmjqs-2015-004735.
Most divisions within a hospital will have a morbidity or mortality round where they review deaths that occurred in that department, but doing that on an institution-wide level is unusual and important. “It gives a totally different viewpoint,” he says. “When it’s a couple highly selected patients whose cases you examine, you really don’t have an idea at the end if the problems you identified are systemwide issues in your institution.”
The major issue the study identified was an inadequate discussion of goals of care. “This was often a patient who was dying, and in retrospect, it was clear that they were at high risk for death, but there had been no discussion with the patient about prognosis or about symptom management,” Dr. Kobewka says. “It seemed that care was directed at prolonging life. When we looked back at the case, that wasn’t realistic. That accounted for 25% of the quality issues that we identified: The discussion of prognosis and goals of care was inadequate or even absent all together. I think every hospital needs to think about those discussions and how and where and when we have them.”
Another revelation from the study: Errors in care are common but also underdiscussed. “When a physician is aware that maybe there was an error in care, it’s easy for there to be guilt and secrecy,” Dr. Kobewka says. “This is just a reminder that it’s common, and we need an open discussion about it. We need high-level, institution-wide systems to help us with this, but even at the individual provider level, this discussion needs to happen. Any quality improvement process needs engagement of frontline staff.”
Reference
- Kobewka DM, van Walraven C, Turnbull J, Worthington J, Calder L, Forster A. Quality gaps identified through mortality review [published online ahead of print February 8, 2016]. BMJ Qual Saf. doi:10.1136/bmjqs-2015-004735.
SHM Seats Its First Non-Physician Board Member
New Society of Hospital Medicine board member Tracy Cardin, ACNP-BC, SFHM, isn’t on the board because she’s a nurse practitioner (NP). But that doesn’t make her election as the first NP or physician assistant (PA) as a voting member of SHM’s oversight panel any less momentous.
“I can’t describe to you how passionately I believe that [NPs and PAs] have a huge role moving forward,” Cardin says. “I think our representation, our visibility, has sort of been flabby and kind of under the wire for a long time. We can really impact the design of care models at the bedside in a way that’s innovative and more efficient and in a way that’s really huge. I think there’s a transformation that’s going to be coming, and we’re going to be a huge part of it.”
Cardin officially started her new position as a board member in March at HM16 in San Diego. She previously—and fittingly—was chair of SHM’s Nurse Practitioner/Physician Assistant Committee. Last year, she received the society’s Award in Excellence in Hospital Medicine for NPs and PAs. She has worked at the University of Chicago for about 10 years.
SHM Past President Robert Harrington Jr., MD, SFHM, who pushed for her inclusion on the board, says that the value of bringing different perspectives to the society’s board can’t be overstated.
“I’m a family medicine–trained hospitalist, and so from firsthand experience, it was important to me before I ever thought about running for the board that there was some representation of our constituency whether that was at the committee level or at the board level,” Dr. Harrington says. “I think that is part of what drew me to seek a higher voice within SHM. … I thought it was important that somebody represent those growing constituencies.”
Dr. Harrington, who among others refers to SHM as a “big tent organization,” says Cardin’s appointment is evidence of that. He believes that his background in family medicine and her background as an NP show healthcare professionals that SHM is not just a group for doctors.
“It does send a message to the rest of our membership that SHM values those other constituencies and that this is not a physician membership organization but rather a membership organization comprised of people who are interested in improving healthcare for our hospitalized patients,” he says.
In fact, Dr. Harrington says one of the first official actions he took as president was to name Cardin an ex officio member of the board. While that meant she could not vote on issues, her perspective alone helped shape conversations.
“Over the course of the last year, she has proven herself to be exactly what I would have hoped she would be: a voice of an important constituency within our membership,” he says. “And as a result of that, [she] ended up being voted into the board.”
Cardin says the time is perfect for her to bring an added viewpoint to the board. First, the number of NPs and PAs is growing.
“NPs and PAs are such a huge part of all acute-care practices,” says Cardin, a past member of Team Hospitalist, the volunteer editorial advisory group for The Hospitalist. “The State of Hospital Medicine surveys showed that 83% of hospitalist groups are utilizing NPs and PAs. I think that is going to be reflected not only in hospitalist practices but in all acute-care practices—there is going to be more deployment and integration of NPs and PAs into practice.
“[SHM] is ahead of the curve recognizing that value.”
Second, healthcare is undergoing payment reform unseen since the introduction of Medicare and Medicaid. Technology is revamping bedside manner, care delivery, and everything in between. And quality of care is more important than ever as doctors will be increasingly paid for how well patients get, not for services provided to them.
“NP and PA providers can have a great impact on care design and throughput as well as other contributions in the hospital environment,” she adds.
Cardin says there can’t be too many educated viewpoints on complicated issues that will affect care delivery in the United States for decades to come. And the first NP/PA voice might be, gulp, just what the doctors ordered.
“We’re at a pivotal time for this organization and also for healthcare in general with the shifts in how we’re paid and what we’re paid for and the complexity of electronic medical records and fragmented healthcare and billing and quality metrics—there’s just so many challenges right now,” she says. “It’s just hugely humbling to be a part of that and try to anticipate what direction that we as a society should go into.” TH
Richard Quinn is a freelance writer based in New Jersey.
New Society of Hospital Medicine board member Tracy Cardin, ACNP-BC, SFHM, isn’t on the board because she’s a nurse practitioner (NP). But that doesn’t make her election as the first NP or physician assistant (PA) as a voting member of SHM’s oversight panel any less momentous.
“I can’t describe to you how passionately I believe that [NPs and PAs] have a huge role moving forward,” Cardin says. “I think our representation, our visibility, has sort of been flabby and kind of under the wire for a long time. We can really impact the design of care models at the bedside in a way that’s innovative and more efficient and in a way that’s really huge. I think there’s a transformation that’s going to be coming, and we’re going to be a huge part of it.”
Cardin officially started her new position as a board member in March at HM16 in San Diego. She previously—and fittingly—was chair of SHM’s Nurse Practitioner/Physician Assistant Committee. Last year, she received the society’s Award in Excellence in Hospital Medicine for NPs and PAs. She has worked at the University of Chicago for about 10 years.
SHM Past President Robert Harrington Jr., MD, SFHM, who pushed for her inclusion on the board, says that the value of bringing different perspectives to the society’s board can’t be overstated.
“I’m a family medicine–trained hospitalist, and so from firsthand experience, it was important to me before I ever thought about running for the board that there was some representation of our constituency whether that was at the committee level or at the board level,” Dr. Harrington says. “I think that is part of what drew me to seek a higher voice within SHM. … I thought it was important that somebody represent those growing constituencies.”
Dr. Harrington, who among others refers to SHM as a “big tent organization,” says Cardin’s appointment is evidence of that. He believes that his background in family medicine and her background as an NP show healthcare professionals that SHM is not just a group for doctors.
“It does send a message to the rest of our membership that SHM values those other constituencies and that this is not a physician membership organization but rather a membership organization comprised of people who are interested in improving healthcare for our hospitalized patients,” he says.
In fact, Dr. Harrington says one of the first official actions he took as president was to name Cardin an ex officio member of the board. While that meant she could not vote on issues, her perspective alone helped shape conversations.
“Over the course of the last year, she has proven herself to be exactly what I would have hoped she would be: a voice of an important constituency within our membership,” he says. “And as a result of that, [she] ended up being voted into the board.”
Cardin says the time is perfect for her to bring an added viewpoint to the board. First, the number of NPs and PAs is growing.
“NPs and PAs are such a huge part of all acute-care practices,” says Cardin, a past member of Team Hospitalist, the volunteer editorial advisory group for The Hospitalist. “The State of Hospital Medicine surveys showed that 83% of hospitalist groups are utilizing NPs and PAs. I think that is going to be reflected not only in hospitalist practices but in all acute-care practices—there is going to be more deployment and integration of NPs and PAs into practice.
“[SHM] is ahead of the curve recognizing that value.”
Second, healthcare is undergoing payment reform unseen since the introduction of Medicare and Medicaid. Technology is revamping bedside manner, care delivery, and everything in between. And quality of care is more important than ever as doctors will be increasingly paid for how well patients get, not for services provided to them.
“NP and PA providers can have a great impact on care design and throughput as well as other contributions in the hospital environment,” she adds.
Cardin says there can’t be too many educated viewpoints on complicated issues that will affect care delivery in the United States for decades to come. And the first NP/PA voice might be, gulp, just what the doctors ordered.
“We’re at a pivotal time for this organization and also for healthcare in general with the shifts in how we’re paid and what we’re paid for and the complexity of electronic medical records and fragmented healthcare and billing and quality metrics—there’s just so many challenges right now,” she says. “It’s just hugely humbling to be a part of that and try to anticipate what direction that we as a society should go into.” TH
Richard Quinn is a freelance writer based in New Jersey.
New Society of Hospital Medicine board member Tracy Cardin, ACNP-BC, SFHM, isn’t on the board because she’s a nurse practitioner (NP). But that doesn’t make her election as the first NP or physician assistant (PA) as a voting member of SHM’s oversight panel any less momentous.
“I can’t describe to you how passionately I believe that [NPs and PAs] have a huge role moving forward,” Cardin says. “I think our representation, our visibility, has sort of been flabby and kind of under the wire for a long time. We can really impact the design of care models at the bedside in a way that’s innovative and more efficient and in a way that’s really huge. I think there’s a transformation that’s going to be coming, and we’re going to be a huge part of it.”
Cardin officially started her new position as a board member in March at HM16 in San Diego. She previously—and fittingly—was chair of SHM’s Nurse Practitioner/Physician Assistant Committee. Last year, she received the society’s Award in Excellence in Hospital Medicine for NPs and PAs. She has worked at the University of Chicago for about 10 years.
SHM Past President Robert Harrington Jr., MD, SFHM, who pushed for her inclusion on the board, says that the value of bringing different perspectives to the society’s board can’t be overstated.
“I’m a family medicine–trained hospitalist, and so from firsthand experience, it was important to me before I ever thought about running for the board that there was some representation of our constituency whether that was at the committee level or at the board level,” Dr. Harrington says. “I think that is part of what drew me to seek a higher voice within SHM. … I thought it was important that somebody represent those growing constituencies.”
Dr. Harrington, who among others refers to SHM as a “big tent organization,” says Cardin’s appointment is evidence of that. He believes that his background in family medicine and her background as an NP show healthcare professionals that SHM is not just a group for doctors.
“It does send a message to the rest of our membership that SHM values those other constituencies and that this is not a physician membership organization but rather a membership organization comprised of people who are interested in improving healthcare for our hospitalized patients,” he says.
In fact, Dr. Harrington says one of the first official actions he took as president was to name Cardin an ex officio member of the board. While that meant she could not vote on issues, her perspective alone helped shape conversations.
“Over the course of the last year, she has proven herself to be exactly what I would have hoped she would be: a voice of an important constituency within our membership,” he says. “And as a result of that, [she] ended up being voted into the board.”
Cardin says the time is perfect for her to bring an added viewpoint to the board. First, the number of NPs and PAs is growing.
“NPs and PAs are such a huge part of all acute-care practices,” says Cardin, a past member of Team Hospitalist, the volunteer editorial advisory group for The Hospitalist. “The State of Hospital Medicine surveys showed that 83% of hospitalist groups are utilizing NPs and PAs. I think that is going to be reflected not only in hospitalist practices but in all acute-care practices—there is going to be more deployment and integration of NPs and PAs into practice.
“[SHM] is ahead of the curve recognizing that value.”
Second, healthcare is undergoing payment reform unseen since the introduction of Medicare and Medicaid. Technology is revamping bedside manner, care delivery, and everything in between. And quality of care is more important than ever as doctors will be increasingly paid for how well patients get, not for services provided to them.
“NP and PA providers can have a great impact on care design and throughput as well as other contributions in the hospital environment,” she adds.
Cardin says there can’t be too many educated viewpoints on complicated issues that will affect care delivery in the United States for decades to come. And the first NP/PA voice might be, gulp, just what the doctors ordered.
“We’re at a pivotal time for this organization and also for healthcare in general with the shifts in how we’re paid and what we’re paid for and the complexity of electronic medical records and fragmented healthcare and billing and quality metrics—there’s just so many challenges right now,” she says. “It’s just hugely humbling to be a part of that and try to anticipate what direction that we as a society should go into.” TH
Richard Quinn is a freelance writer based in New Jersey.
Helicobacter Pylori Treatment is Associated with a Short-term Increase in the Risk of Neuropsychiatic Events
NEW YORK (Reuters Health) - Helicobacter pylori treatment containing clarithromycin is associated with a short-term increase in the risk of neuropsychiatric events, according to a study from Hong Kong.
Neuropsychiatric events following clarithromycin therapy have been reported previously, but no population-based study had assessed the neuropsychiatric risk associated with clarithromycin.
Dr. Esther W. Chan, from Li Ka Shing Faculty of Medicine, University of Hong Kong, and colleagues used data from the University of Hong Kong Clinical Data Analysis and Reporting System to investigate the association between H. pylori therapy containing clarithromycin and acute neuropsychiatric events.
Current use of clarithromycin as part of the H. pylori regimen was associated with a 4.12-fold increased risk of neuropsychiatric events, including a 5.42-fold increase in psychotic events and a 2.63-fold increase in cognitive impairment, compared with baseline.
These increased risks appear to be limited to days 2 to 14 since the prescription start date, according to the May 2 online report in JAMA Internal Medicine.
The crude absolute risks per 1000 prescriptions were 0.45 for neuropsychiatric events, 0.12 for psychotic events, and 0.12 for cognitive impairment during current use of therapy.
"Given the low absolute neuropsychiatric risk, an abrupt change in prescribing practice based on the observed increase in neuropsychiatric events is not suggested, particularly in the absence of better treatment alternatives," the researchers conclude.
"Such transient neuropsychiatric events will usually resolve spontaneously after treatment cessation and psychiatric interventions can be avoided," the authors note.
"Because we investigated H. pylori therapy as the exposure, we could not pinpoint which drug in the regimen contributed to the neuropsychiatric events in our study," they caution. "We hypothesized that clarithromycin is the most probable drug because very limited evidence suggested that neuropsychiatric
events are associated with amoxicillin or proton pump inhibitors."
Dr. Chan was unable to provide comments in time for publication.
The authors reported no funding or disclosures.
NEW YORK (Reuters Health) - Helicobacter pylori treatment containing clarithromycin is associated with a short-term increase in the risk of neuropsychiatric events, according to a study from Hong Kong.
Neuropsychiatric events following clarithromycin therapy have been reported previously, but no population-based study had assessed the neuropsychiatric risk associated with clarithromycin.
Dr. Esther W. Chan, from Li Ka Shing Faculty of Medicine, University of Hong Kong, and colleagues used data from the University of Hong Kong Clinical Data Analysis and Reporting System to investigate the association between H. pylori therapy containing clarithromycin and acute neuropsychiatric events.
Current use of clarithromycin as part of the H. pylori regimen was associated with a 4.12-fold increased risk of neuropsychiatric events, including a 5.42-fold increase in psychotic events and a 2.63-fold increase in cognitive impairment, compared with baseline.
These increased risks appear to be limited to days 2 to 14 since the prescription start date, according to the May 2 online report in JAMA Internal Medicine.
The crude absolute risks per 1000 prescriptions were 0.45 for neuropsychiatric events, 0.12 for psychotic events, and 0.12 for cognitive impairment during current use of therapy.
"Given the low absolute neuropsychiatric risk, an abrupt change in prescribing practice based on the observed increase in neuropsychiatric events is not suggested, particularly in the absence of better treatment alternatives," the researchers conclude.
"Such transient neuropsychiatric events will usually resolve spontaneously after treatment cessation and psychiatric interventions can be avoided," the authors note.
"Because we investigated H. pylori therapy as the exposure, we could not pinpoint which drug in the regimen contributed to the neuropsychiatric events in our study," they caution. "We hypothesized that clarithromycin is the most probable drug because very limited evidence suggested that neuropsychiatric
events are associated with amoxicillin or proton pump inhibitors."
Dr. Chan was unable to provide comments in time for publication.
The authors reported no funding or disclosures.
NEW YORK (Reuters Health) - Helicobacter pylori treatment containing clarithromycin is associated with a short-term increase in the risk of neuropsychiatric events, according to a study from Hong Kong.
Neuropsychiatric events following clarithromycin therapy have been reported previously, but no population-based study had assessed the neuropsychiatric risk associated with clarithromycin.
Dr. Esther W. Chan, from Li Ka Shing Faculty of Medicine, University of Hong Kong, and colleagues used data from the University of Hong Kong Clinical Data Analysis and Reporting System to investigate the association between H. pylori therapy containing clarithromycin and acute neuropsychiatric events.
Current use of clarithromycin as part of the H. pylori regimen was associated with a 4.12-fold increased risk of neuropsychiatric events, including a 5.42-fold increase in psychotic events and a 2.63-fold increase in cognitive impairment, compared with baseline.
These increased risks appear to be limited to days 2 to 14 since the prescription start date, according to the May 2 online report in JAMA Internal Medicine.
The crude absolute risks per 1000 prescriptions were 0.45 for neuropsychiatric events, 0.12 for psychotic events, and 0.12 for cognitive impairment during current use of therapy.
"Given the low absolute neuropsychiatric risk, an abrupt change in prescribing practice based on the observed increase in neuropsychiatric events is not suggested, particularly in the absence of better treatment alternatives," the researchers conclude.
"Such transient neuropsychiatric events will usually resolve spontaneously after treatment cessation and psychiatric interventions can be avoided," the authors note.
"Because we investigated H. pylori therapy as the exposure, we could not pinpoint which drug in the regimen contributed to the neuropsychiatric events in our study," they caution. "We hypothesized that clarithromycin is the most probable drug because very limited evidence suggested that neuropsychiatric
events are associated with amoxicillin or proton pump inhibitors."
Dr. Chan was unable to provide comments in time for publication.
The authors reported no funding or disclosures.
Group isolates Tregs to treat GVHD

Image by Kathryn T. Iacono
Researchers say they have devised a method for harvesting regulatory T cells (Tregs) on a large scale, and they are currently testing these Tregs in a trial of patients with graft-versus-host disease (GVHD).
The team described the harvesting method in the Journal of Immunotherapy.
“A Tregs-based therapy could help reduce the risk of GVHD, but Tregs are a very rare population amongst blood cells,” said study author Sebastian Bertin-Maghit, PhD, of the Agency for Science, Technology and Research (A*STAR) in Singapore.
“For our therapy to work, we needed a large supply of pure, ‘untouched’ Tregs that are uncontaminated with other cell types.”
However, when it came to isolating pure Tregs on a large scale, the researchers found existing isolation methods inefficient.
So rather than isolating the cells by “plucking” them out of a donor sample—a method that comes with the risk of unwanted modification or activation of some cells—the team devised a depletion method for selecting Tregs in their pure, untouched state.
“We depleted all unwanted cells in donor samples using isolation reagents,” Dr Bertin-Maghit said. “This allowed us to harvest Tregs in their natural state. We took great care to wash out the isolation reagents in the final product.”
The researchers have since proven that this single-step depletion process can be scaled up to harvest highly pure Tregs at levels suitable for clinical trials, and their procedure complies with current trial standards.
Furthermore, while previous attempts to collect Tregs produced a final product with 60% pure Tregs, this new method generates over 90% pure Tregs.
“The first clinical trial using our Treg product is currently ongoing at the Singapore General Hospital,” Dr Bertin-Maghit said. “We are assessing the safety of Tregs in the treatment of GVHD in 12 leukemia patients. We believe our procedure will open doors to a new era in cell therapy.” ![]()

Image by Kathryn T. Iacono
Researchers say they have devised a method for harvesting regulatory T cells (Tregs) on a large scale, and they are currently testing these Tregs in a trial of patients with graft-versus-host disease (GVHD).
The team described the harvesting method in the Journal of Immunotherapy.
“A Tregs-based therapy could help reduce the risk of GVHD, but Tregs are a very rare population amongst blood cells,” said study author Sebastian Bertin-Maghit, PhD, of the Agency for Science, Technology and Research (A*STAR) in Singapore.
“For our therapy to work, we needed a large supply of pure, ‘untouched’ Tregs that are uncontaminated with other cell types.”
However, when it came to isolating pure Tregs on a large scale, the researchers found existing isolation methods inefficient.
So rather than isolating the cells by “plucking” them out of a donor sample—a method that comes with the risk of unwanted modification or activation of some cells—the team devised a depletion method for selecting Tregs in their pure, untouched state.
“We depleted all unwanted cells in donor samples using isolation reagents,” Dr Bertin-Maghit said. “This allowed us to harvest Tregs in their natural state. We took great care to wash out the isolation reagents in the final product.”
The researchers have since proven that this single-step depletion process can be scaled up to harvest highly pure Tregs at levels suitable for clinical trials, and their procedure complies with current trial standards.
Furthermore, while previous attempts to collect Tregs produced a final product with 60% pure Tregs, this new method generates over 90% pure Tregs.
“The first clinical trial using our Treg product is currently ongoing at the Singapore General Hospital,” Dr Bertin-Maghit said. “We are assessing the safety of Tregs in the treatment of GVHD in 12 leukemia patients. We believe our procedure will open doors to a new era in cell therapy.” ![]()

Image by Kathryn T. Iacono
Researchers say they have devised a method for harvesting regulatory T cells (Tregs) on a large scale, and they are currently testing these Tregs in a trial of patients with graft-versus-host disease (GVHD).
The team described the harvesting method in the Journal of Immunotherapy.
“A Tregs-based therapy could help reduce the risk of GVHD, but Tregs are a very rare population amongst blood cells,” said study author Sebastian Bertin-Maghit, PhD, of the Agency for Science, Technology and Research (A*STAR) in Singapore.
“For our therapy to work, we needed a large supply of pure, ‘untouched’ Tregs that are uncontaminated with other cell types.”
However, when it came to isolating pure Tregs on a large scale, the researchers found existing isolation methods inefficient.
So rather than isolating the cells by “plucking” them out of a donor sample—a method that comes with the risk of unwanted modification or activation of some cells—the team devised a depletion method for selecting Tregs in their pure, untouched state.
“We depleted all unwanted cells in donor samples using isolation reagents,” Dr Bertin-Maghit said. “This allowed us to harvest Tregs in their natural state. We took great care to wash out the isolation reagents in the final product.”
The researchers have since proven that this single-step depletion process can be scaled up to harvest highly pure Tregs at levels suitable for clinical trials, and their procedure complies with current trial standards.
Furthermore, while previous attempts to collect Tregs produced a final product with 60% pure Tregs, this new method generates over 90% pure Tregs.
“The first clinical trial using our Treg product is currently ongoing at the Singapore General Hospital,” Dr Bertin-Maghit said. “We are assessing the safety of Tregs in the treatment of GVHD in 12 leukemia patients. We believe our procedure will open doors to a new era in cell therapy.” ![]()
Warfarin indication, TTR linked to dementia risk

Photo courtesy of NIGMS
SAN FRANCISCO—Patients with atrial fibrillation (AF) who are on warfarin long-term have a higher risk of dementia than non-AF patients on long-term warfarin therapy, according to a new study.
The AF patients studied had higher rates of dementia, Alzheimer’s disease, and vascular dementia than their non-AF counterparts.
However, both groups of patients had a greater risk of dementia if they had lower percentages of time in therapeutic range (TTR).
“Our study results are the first to show that there are significant cognitive risk factors for patients treated with warfarin over a long period of time, regardless of the indication for anticoagulation,” said T. Jared Bunch, MD, of the Intermountain Medical Center Heart Institute in Salt Lake City, Utah.
Dr Bunch and his colleagues presented this research at the Heart Rhythm Society’s 37th Annual Scientific Sessions (abstract MP01-04).
The researchers enrolled 10,537 patients, age 18 and older, with no history of dementia prior to the study. They were receiving long-term warfarin for AF (n=4460), thromboembolism (n=5868), or mechanical heart valves (n=209).
The AF patients were older and had higher rates of hypertension, diabetes, heart failure, and stroke than the non-AF patients.
During a follow-up of approximately 7 years, the researchers found that all types of dementia increased in the AF group more than the non-AF group.
AF patients experienced higher rates of total dementia (5.8% vs 1.6%, P<0.0001), Alzheimer’s disease (2.8% vs 0.9%, P<0.0001), and vascular dementia (1.0% vs 0.2%, P<0.0001).
The researchers performed a propensity analysis of 6030 patients to account for the differences in baseline characteristics. And the risk of dementia remained significantly higher in AF patients than non-AF patients.
The hazard ratio (HR) was 2.42 for all types of dementia (P<0.0001), 2.04 for Alzheimer’s disease (P<0.0001), and 2.46 for senility (P<0.0001).
However, both AF and non-AF patients saw an increase in the risk of dementia if they had a low percent TTR.
In multivariate analysis, with the TTR >75% group as the reference, the HR for dementia in AF patients was:
- 1.30 for the 51%-75% TTR group (P=0.10)
- 1.57 for the 26%-50% TTR group (P=0.02)
- 1.92 for the ≤25% TTR group (P=0.005).
The HR for dementia in non-AF patients was:
- 1.57 for the 51%-75% TTR group (P=0.13)
- 2.69 for the 26%-50% TTR group (P=0.002)
- 3.87 for the ≤25% TTR group (P<0.0001).
Dr Bunch and his colleagues believe these findings have implications for treatment.
“First, as physicians, we have to understand that, although we need to use anticoagulants for many reasons, including to prevent stroke in AF patients, at that same time, there are risks that need to be considered, some of which we are only right now beginning to understand,” Dr Bunch said.
“In this regard, only those that absolutely need blood thinners should be placed on them long-term. Second, other medications like aspirin that may increase the blood thinner’s effect should be avoided unless there is a specific medical need. Finally, in people that are on warfarin in which the levels are erratic or difficult to control, switching to newer agents that are more predictable may lower risk.” ![]()

Photo courtesy of NIGMS
SAN FRANCISCO—Patients with atrial fibrillation (AF) who are on warfarin long-term have a higher risk of dementia than non-AF patients on long-term warfarin therapy, according to a new study.
The AF patients studied had higher rates of dementia, Alzheimer’s disease, and vascular dementia than their non-AF counterparts.
However, both groups of patients had a greater risk of dementia if they had lower percentages of time in therapeutic range (TTR).
“Our study results are the first to show that there are significant cognitive risk factors for patients treated with warfarin over a long period of time, regardless of the indication for anticoagulation,” said T. Jared Bunch, MD, of the Intermountain Medical Center Heart Institute in Salt Lake City, Utah.
Dr Bunch and his colleagues presented this research at the Heart Rhythm Society’s 37th Annual Scientific Sessions (abstract MP01-04).
The researchers enrolled 10,537 patients, age 18 and older, with no history of dementia prior to the study. They were receiving long-term warfarin for AF (n=4460), thromboembolism (n=5868), or mechanical heart valves (n=209).
The AF patients were older and had higher rates of hypertension, diabetes, heart failure, and stroke than the non-AF patients.
During a follow-up of approximately 7 years, the researchers found that all types of dementia increased in the AF group more than the non-AF group.
AF patients experienced higher rates of total dementia (5.8% vs 1.6%, P<0.0001), Alzheimer’s disease (2.8% vs 0.9%, P<0.0001), and vascular dementia (1.0% vs 0.2%, P<0.0001).
The researchers performed a propensity analysis of 6030 patients to account for the differences in baseline characteristics. And the risk of dementia remained significantly higher in AF patients than non-AF patients.
The hazard ratio (HR) was 2.42 for all types of dementia (P<0.0001), 2.04 for Alzheimer’s disease (P<0.0001), and 2.46 for senility (P<0.0001).
However, both AF and non-AF patients saw an increase in the risk of dementia if they had a low percent TTR.
In multivariate analysis, with the TTR >75% group as the reference, the HR for dementia in AF patients was:
- 1.30 for the 51%-75% TTR group (P=0.10)
- 1.57 for the 26%-50% TTR group (P=0.02)
- 1.92 for the ≤25% TTR group (P=0.005).
The HR for dementia in non-AF patients was:
- 1.57 for the 51%-75% TTR group (P=0.13)
- 2.69 for the 26%-50% TTR group (P=0.002)
- 3.87 for the ≤25% TTR group (P<0.0001).
Dr Bunch and his colleagues believe these findings have implications for treatment.
“First, as physicians, we have to understand that, although we need to use anticoagulants for many reasons, including to prevent stroke in AF patients, at that same time, there are risks that need to be considered, some of which we are only right now beginning to understand,” Dr Bunch said.
“In this regard, only those that absolutely need blood thinners should be placed on them long-term. Second, other medications like aspirin that may increase the blood thinner’s effect should be avoided unless there is a specific medical need. Finally, in people that are on warfarin in which the levels are erratic or difficult to control, switching to newer agents that are more predictable may lower risk.” ![]()

Photo courtesy of NIGMS
SAN FRANCISCO—Patients with atrial fibrillation (AF) who are on warfarin long-term have a higher risk of dementia than non-AF patients on long-term warfarin therapy, according to a new study.
The AF patients studied had higher rates of dementia, Alzheimer’s disease, and vascular dementia than their non-AF counterparts.
However, both groups of patients had a greater risk of dementia if they had lower percentages of time in therapeutic range (TTR).
“Our study results are the first to show that there are significant cognitive risk factors for patients treated with warfarin over a long period of time, regardless of the indication for anticoagulation,” said T. Jared Bunch, MD, of the Intermountain Medical Center Heart Institute in Salt Lake City, Utah.
Dr Bunch and his colleagues presented this research at the Heart Rhythm Society’s 37th Annual Scientific Sessions (abstract MP01-04).
The researchers enrolled 10,537 patients, age 18 and older, with no history of dementia prior to the study. They were receiving long-term warfarin for AF (n=4460), thromboembolism (n=5868), or mechanical heart valves (n=209).
The AF patients were older and had higher rates of hypertension, diabetes, heart failure, and stroke than the non-AF patients.
During a follow-up of approximately 7 years, the researchers found that all types of dementia increased in the AF group more than the non-AF group.
AF patients experienced higher rates of total dementia (5.8% vs 1.6%, P<0.0001), Alzheimer’s disease (2.8% vs 0.9%, P<0.0001), and vascular dementia (1.0% vs 0.2%, P<0.0001).
The researchers performed a propensity analysis of 6030 patients to account for the differences in baseline characteristics. And the risk of dementia remained significantly higher in AF patients than non-AF patients.
The hazard ratio (HR) was 2.42 for all types of dementia (P<0.0001), 2.04 for Alzheimer’s disease (P<0.0001), and 2.46 for senility (P<0.0001).
However, both AF and non-AF patients saw an increase in the risk of dementia if they had a low percent TTR.
In multivariate analysis, with the TTR >75% group as the reference, the HR for dementia in AF patients was:
- 1.30 for the 51%-75% TTR group (P=0.10)
- 1.57 for the 26%-50% TTR group (P=0.02)
- 1.92 for the ≤25% TTR group (P=0.005).
The HR for dementia in non-AF patients was:
- 1.57 for the 51%-75% TTR group (P=0.13)
- 2.69 for the 26%-50% TTR group (P=0.002)
- 3.87 for the ≤25% TTR group (P<0.0001).
Dr Bunch and his colleagues believe these findings have implications for treatment.
“First, as physicians, we have to understand that, although we need to use anticoagulants for many reasons, including to prevent stroke in AF patients, at that same time, there are risks that need to be considered, some of which we are only right now beginning to understand,” Dr Bunch said.
“In this regard, only those that absolutely need blood thinners should be placed on them long-term. Second, other medications like aspirin that may increase the blood thinner’s effect should be avoided unless there is a specific medical need. Finally, in people that are on warfarin in which the levels are erratic or difficult to control, switching to newer agents that are more predictable may lower risk.” ![]()
E-cigarettes fuel increase in nicotine exposures in young children
The incidence of exposure to nicotine and tobacco products in children less than 6 years old increased significantly from 2012 to 2015, according to Alisha Kamboj and her associates.
From January 2012 to April 2015, the National Poison Data System received 29,141 reports of nicotine and tobacco product exposure in children under 6 years of age, averaging 729 children per month. The annual rate of exposure increased from 3.0/100,000 children in 2012 to 4.2/100,000 in 2014. A dramatic increase in exposure to e-cigarettes drove the overall increase, with monthly reports of e-cigarette use rising nearly 1,500% from January 2012 to April 2015.
Nearly 80% of children exposed were younger than 2 years old, and the median age of exposed children was 1.1 years. Children younger than 2 accounted for 44.1% of e-cigarette exposures, 91.6% of cigarette exposures, and 75.4% of exposures to other tobacco products, the investigators noted.
Children exposed to e-cigarettes were significantly more likely to be admitted to a health care facility and to have severe outcomes than were children exposed to cigarettes, with odds ratios of 5.19 and 2.6, respectively. One death – of a 1-year-old child – was associated with nicotine liquid.
“Educating child caregivers about potential clinical effects and outcomes associated with nicotine exposure may help motivate adoption of safety behaviors and aid in identification of symptoms in the event of an exposure. Adults in households with children [younger than] 6 years should be counseled on vaping cessation and strongly encouraged not to use or store e-cigarettes, e-liquid, and related products in the home,” the investigators recommended.
Find the full study in Pediatrics (doi: 10.1542/peds.2016-0041).
The incidence of exposure to nicotine and tobacco products in children less than 6 years old increased significantly from 2012 to 2015, according to Alisha Kamboj and her associates.
From January 2012 to April 2015, the National Poison Data System received 29,141 reports of nicotine and tobacco product exposure in children under 6 years of age, averaging 729 children per month. The annual rate of exposure increased from 3.0/100,000 children in 2012 to 4.2/100,000 in 2014. A dramatic increase in exposure to e-cigarettes drove the overall increase, with monthly reports of e-cigarette use rising nearly 1,500% from January 2012 to April 2015.
Nearly 80% of children exposed were younger than 2 years old, and the median age of exposed children was 1.1 years. Children younger than 2 accounted for 44.1% of e-cigarette exposures, 91.6% of cigarette exposures, and 75.4% of exposures to other tobacco products, the investigators noted.
Children exposed to e-cigarettes were significantly more likely to be admitted to a health care facility and to have severe outcomes than were children exposed to cigarettes, with odds ratios of 5.19 and 2.6, respectively. One death – of a 1-year-old child – was associated with nicotine liquid.
“Educating child caregivers about potential clinical effects and outcomes associated with nicotine exposure may help motivate adoption of safety behaviors and aid in identification of symptoms in the event of an exposure. Adults in households with children [younger than] 6 years should be counseled on vaping cessation and strongly encouraged not to use or store e-cigarettes, e-liquid, and related products in the home,” the investigators recommended.
Find the full study in Pediatrics (doi: 10.1542/peds.2016-0041).
The incidence of exposure to nicotine and tobacco products in children less than 6 years old increased significantly from 2012 to 2015, according to Alisha Kamboj and her associates.
From January 2012 to April 2015, the National Poison Data System received 29,141 reports of nicotine and tobacco product exposure in children under 6 years of age, averaging 729 children per month. The annual rate of exposure increased from 3.0/100,000 children in 2012 to 4.2/100,000 in 2014. A dramatic increase in exposure to e-cigarettes drove the overall increase, with monthly reports of e-cigarette use rising nearly 1,500% from January 2012 to April 2015.
Nearly 80% of children exposed were younger than 2 years old, and the median age of exposed children was 1.1 years. Children younger than 2 accounted for 44.1% of e-cigarette exposures, 91.6% of cigarette exposures, and 75.4% of exposures to other tobacco products, the investigators noted.
Children exposed to e-cigarettes were significantly more likely to be admitted to a health care facility and to have severe outcomes than were children exposed to cigarettes, with odds ratios of 5.19 and 2.6, respectively. One death – of a 1-year-old child – was associated with nicotine liquid.
“Educating child caregivers about potential clinical effects and outcomes associated with nicotine exposure may help motivate adoption of safety behaviors and aid in identification of symptoms in the event of an exposure. Adults in households with children [younger than] 6 years should be counseled on vaping cessation and strongly encouraged not to use or store e-cigarettes, e-liquid, and related products in the home,” the investigators recommended.
Find the full study in Pediatrics (doi: 10.1542/peds.2016-0041).
FROM PEDIATRICS