User login
Medicaid Expansion and Veterans’ Reliance on the VA for Depression Care
The US Department of Veterans Affairs (VA) is the largest integrated health care system in the United States, providing care for more than 9 million veterans.1 With veterans experiencing mental health conditions like posttraumatic stress disorder (PTSD), substance use disorders, and other serious mental illnesses (SMI) at higher rates compared with the general population, the VA plays an important role in the provision of mental health services.2-5 Since the implementation of its Mental Health Strategic Plan in 2004, the VA has overseen the development of a wide array of mental health programs geared toward the complex needs of veterans. Research has demonstrated VA care outperforming Medicaid-reimbursed services in terms of the percentage of veterans filling antidepressants for at least 12 weeks after initiation of treatment for major depressive disorder (MDD), as well as posthospitalization follow-up.6
Eligible veterans enrolled in the VA often also seek non-VA care. Medicaid covers nearly 10% of all nonelderly veterans, and of these veterans, 39% rely solely on Medicaid for health care access.7 Today, Medicaid is the largest payer for mental health services in the US, providing coverage for approximately 27% of Americans who have SMI and helping fulfill unmet mental health needs.8,9 Understanding which of these systems veterans choose to use, and under which circumstances, is essential in guiding the allocation of limited health care resources.10
Beyond Medicaid, alternatives to VA care may include TRICARE, Medicare, Indian Health Services, and employer-based or self-purchased private insurance. While these options potentially increase convenience, choice, and access to health care practitioners (HCPs) and services not available at local VA systems, cross-system utilization with poor integration may cause care coordination and continuity problems, such as medication mismanagement and opioid overdose, unnecessary duplicate utilization, and possible increased mortality.11-15 As recent national legislative changes, such as the Patient Protection and Affordable Care Act (ACA), Veterans Access, Choice and Accountability Act, and the VA MISSION Act, continue to shift the health care landscape for veterans, questions surrounding how veterans are changing their health care use become significant.16,17
Here, we approach the impacts of Medicaid expansion on veterans’ reliance on the VA for mental health services with a unique lens. We leverage a difference-in-difference design to study 2 historical Medicaid expansions in Arizona (AZ) and New York (NY), which extended eligibility to childless adults in 2001. Prior Medicaid dual-eligible mental health research investigated reliance shifts during the immediate postenrollment year in a subset of veterans newly enrolled in Medicaid.18 However, this study took place in a period of relative policy stability. In contrast, we investigate the potential effects of a broad policy shift by analyzing state-level changes in veterans’ reliance over 6 years after a statewide Medicaid expansion. We match expansion states with demographically similar nonexpansion states to account for unobserved trends and confounding effects. Prior studies have used this method to evaluate post-Medicaid expansion mortality changes and changes in veteran dual enrollment and hospitalizations.10,19 While a study of ACA Medicaid expansion states would be ideal, Medicaid data from most states were only available through 2014 at the time of this analysis. Our study offers a quasi-experimental framework leveraging longitudinal data that can be applied as more post-ACA data become available.
Given the rising incidence of suicide among veterans, understanding care-seeking behaviors for depression among veterans is important as it is the most common psychiatric condition found in those who died by suicide.20,21 Furthermore, depression may be useful as a clinical proxy for mental health policy impacts, given that the Patient Health Questionnaire-9 (PHQ-9) screening tool is well validated and increasingly research accessible, and it is a chronic condition responsive to both well-managed pharmacologic treatment and psychotherapeutic interventions.22,23
In this study, we quantify the change in care-seeking behavior for depression among veterans after Medicaid expansion, using a quasi-experimental design. We hypothesize that new access to Medicaid would be associated with a shift away from using VA services for depression. Given the income-dependent eligibility requirements of Medicaid, we also hypothesize that veterans who qualified for VA coverage due to low income, determined by a regional means test (Priority group 5, “income-eligible”), would be more likely to shift care compared with those whose serviced-connected conditions related to their military service (Priority groups 1-4, “service-connected”) provide VA access.
Methods
To investigate the relative changes in veterans’ reliance on the VA for depression care after the 2001 NY and AZ Medicaid expansions We used a retrospective, difference-in-difference analysis. Our comparison pairings, based on prior demographic analyses were as follows: NY with Pennsylvania(PA); AZ with New Mexico and Nevada (NM/NV).19 The time frame of our analysis was 1999 to 2006, with pre- and postexpansion periods defined as 1999 to 2000 and 2001 to 2006, respectively.
Data
We included veterans aged 18 to 64 years, seeking care for depression from 1999 to 2006, who were also VA-enrolled and residing in our states of interest. We counted veterans as enrolled in Medicaid if they were enrolled at least 1 month in a given year.
Using similar methods like those used in prior studies, we selected patients with encounters documenting depression as the primary outpatient or inpatient diagnosis using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: 296.2x for a single episode of major depressive disorder, 296.3x for a recurrent episode of MDD, 300.4 for dysthymia, and 311.0 for depression not otherwise specified.18,24 We used data from the Medicaid Analytic eXtract files (MAX) for Medicaid data and the VA Corporate Data Warehouse (CDW) for VA data. We chose 1999 as the first study year because it was the earliest year MAX data were available.
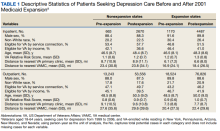
Our final sample included 1833 person-years pre-expansion and 7157 postexpansion in our inpatient analysis, as well as 31,767 person-years pre-expansion and 130,382 postexpansion in our outpatient analysis.
Outcomes and Variables
Our primary outcomes were comparative shifts in VA reliance between expansion and nonexpansion states after Medicaid expansion for both inpatient and outpatient depression care. For each year of study, we calculated a veteran’s VA reliance by aggregating the number of days with depression-related encounters at the VA and dividing by the total number of days with a VA or Medicaid depression-related encounters for the year. To provide context to these shifts in VA reliance, we further analyzed the changes in the proportion of annual VA-Medicaid dual users and annual per capita utilization of depression care across the VA and Medicaid.
We conducted subanalyses by income-eligible and service-connected veterans and adjusted our models for age, non-White race, sex, distances to the nearest inpatient and outpatient VA facilities, and VA Relative Risk Score, which is a measure of disease burden and clinical complexity validated specifically for veterans.25
Statistical Analysis
We used fractional logistic regression to model the adjusted effect of Medicaid expansion on VA reliance for depression care. In parallel, we leveraged ordered logit regression and negative binomial regression models to examine the proportion of VA-Medicaid dual users and the per capita utilization of Medicaid and VA depression care, respectively. To estimate the difference-in-difference effects, we used the interaction term of 2 categorical variables—expansion vs nonexpansion states and pre- vs postexpansion status—as the independent variable. We then calculated the average marginal effects with 95% CIs to estimate the differences in outcomes between expansion and nonexpansion states from pre- to postexpansion periods, as well as year-by-year shifts as a robustness check. We conducted these analyses using Stata MP, version 15.
Results
Baseline and postexpansion characteristics
VA Reliance
Overall, we observed postexpansion decreases in VA reliance for depression care
At the state level, reliance on the VA for inpatient depression care in NY decreased by 13.53 pp (95% CI, -22.58 to -4.49) for income-eligible veterans and 16.67 pp (95% CI, -24.53 to -8.80) for service-connected veterans. No relative differences were observed in the outpatient comparisons for both income-eligible (-0.58 pp; 95% CI, -2.13 to 0.98) and service-connected (0.05 pp; 95% CI, -1.00 to 1.10) veterans. In AZ, Medicaid expansion was associated with decreased VA reliance for outpatient depression care among income-eligible veterans (-8.60 pp; 95% CI, -10.60 to -6.61), greater than that for service-connected veterans (-2.89 pp; 95% CI, -4.02 to -1.77). This decrease in VA reliance was significant in the inpatient context only for service-connected veterans (-4.55 pp; 95% CI, -8.14 to -0.97), not income-eligible veterans (-8.38 pp; 95% CI, -17.91 to 1.16).
By applying the aggregate pp changes toward the postexpansion number of visits across both expansion and nonexpansion states, we found that expansion of Medicaid across all our study states would have resulted in 996 fewer hospitalizations and 10,109 fewer outpatient visits for depression at VA in the postexpansion period vs if no states had chosen to expand Medicaid.
Dual Use/Per Capita Utilization
Overall, Medicaid expansion was associated with greater dual use for inpatient depression care—a 0.97-pp (95% CI, 0.46 to 1.48) increase among service-connected veterans and a 0.64-pp (95% CI, 0.35 to 0.94) increase among income-eligible veterans.
At the state level, NY similarly showed increases in dual use among both service-connected (1.48 pp; 95% CI, 0.80 to 2.16) and income-eligible veterans (0.73 pp; 95% CI, 0.39 to 1.07) after Medicaid expansion. However, dual use in AZ increased significantly only among service-connected veterans (0.70 pp; 95% CI, 0.03 to 1.38), not income-eligible veterans (0.31 pp; 95% CI, -0.17 to 0.78).
Among outpatient visits, Medicaid expansion was associated with increased dual use only for income-eligible veterans (0.16 pp; 95% CI, 0.03-0.29), and not service-connected veterans (0.09 pp; 95% CI, -0.04 to 0.21). State-level analyses showed that Medicaid expansion in NY was not associated with changes in dual use for either service-connected (0.01 pp; 95% CI, -0.16 to 0.17) or income-eligible veterans (0.03 pp; 95% CI, -0.12 to 0.18), while expansion in AZ was associated with increases in dual use among both service-connected (0.42 pp; 95% CI, 0.23 to 0.61) and income-eligible veterans (0.83 pp; 95% CI, 0.59 to 1.07).
Concerning per capita utilization of depression care after Medicaid expansion, analyses showed no detectable changes for either inpatient or outpatient services, among both service-connected and income-eligible veterans. However, while this pattern held at the state level among hospitalizations, outpatient visit results showed divergent trends between AZ and NY. In NY, Medicaid expansion was associated with decreased per capita utilization of outpatient depression care among both service-connected (-0.25 visits annually; 95% CI, -0.48 to -0.01) and income-eligible veterans (-0.64 visits annually; 95% CI, -0.93 to -0.35). In AZ, Medicaid expansion was associated with increased per capita utilization of outpatient depression care among both service-connected (0.62 visits annually; 95% CI, 0.32-0.91) and income-eligible veterans (2.32 visits annually; 95% CI, 1.99-2.65).
Discussion
Our study quantified changes in depression-related health care utilization after Medicaid expansions in NY and AZ in 2001. Overall, the balance of evidence indicated that Medicaid expansion was associated with decreased reliance on the VA for depression-related services. There was an exception: income-eligible veterans in AZ did not shift their hospital care away from the VA in a statistically discernible way, although the point estimate was lower. More broadly, these findings concerning veterans’ reliance varied not only in inpatient vs outpatient services and income- vs service-connected eligibility, but also in the state-level contexts of veteran dual users and per capita utilization.
Given that the overall per capita utilization of depression care was unchanged from pre- to postexpansion periods, one might interpret the decreases in VA reliance and increases in Medicaid-VA dual users as a substitution effect from VA care to non-VA care. This could be plausible for hospitalizations where state-level analyses showed similarly stable levels of per capita utilization. However, state-level trends in our outpatient utilization analysis, especially with a substantial 2.32 pp increase in annual per capita visits among income-eligible veterans in AZ, leave open the possibility that in some cases veterans may be complementing VA care with Medicaid-reimbursed services.
The causes underlying these differences in reliance shifts between NY and AZ are likely also influenced by the policy contexts of their respective Medicaid expansions. For example, in 1999, NY passed Kendra’s Law, which established a procedure for obtaining court orders for assisted outpatient mental health treatment for individuals deemed unlikely to survive safely in the community.26 A reasonable inference is that there was less unfulfilled outpatient mental health need in NY under the existing accessibility provisioned by Kendra’s Law. In addition, while both states extended coverage to childless adults under 100% of the Federal Poverty level (FPL), the AZ Medicaid expansion was via a voters’ initiative and extended family coverage to 200% FPL vs 150% FPL for families in NY. Given that the AZ Medicaid expansion enjoyed both broader public participation and generosity in terms of eligibility, its uptake and therefore effect size may have been larger than in NY for nonacute outpatient care.
Our findings contribute to the growing body of literature surrounding the changes in health care utilization after Medicaid expansion, specifically for a newly dual-eligible population of veterans seeking mental health services for depression. While prior research concerning Medicare dual-enrolled veterans has shown high reliance on the VA for both mental health diagnoses and services, scholars have established the association of Medicaid enrollment with decreased VA reliance.27-29 Our analysis is the first to investigate state-level effects of Medicaid expansion on VA reliance for a single mental health condition using a natural experimental framework. We focus on a population that includes a large portion of veterans who are newly Medicaid-eligible due to a sweeping policy change and use demographically matched nonexpansion states to draw comparisons in VA reliance for depression care. Our findings of Medicaid expansion–associated decreases in VA reliance for depression care complement prior literature that describe Medicaid enrollment–associated decreases in VA reliance for overall mental health care.
Implications
From a systems-level perspective, the implications of shifting services away from the VA are complex and incompletely understood. The VA lacks interoperability with the electronic health records (EHRs) used by Medicaid clinicians. Consequently, significant issues of service duplication and incomplete clinical data exist for veterans seeking treatment outside of the VA system, posing health care quality and safety concerns.30 On one hand, Medicaid access is associated with increased health care utilization attributed to filling unmet needs for Medicare dual enrollees, as well as increased prescription filling for psychiatric medications.31,32 Furthermore, the only randomized control trial of Medicaid expansion to date was associated with a 9-pp decrease in positive screening rates for depression among those who received access at around 2 years postexpansion.33 On the other hand, the VA has developed a mental health system tailored to the particular needs of veterans, and health care practitioners at the VA have significantly greater rates of military cultural competency compared to those in nonmilitary settings (70% vs 24% in the TRICARE network and 8% among those with no military or TRICARE affiliation).34 Compared to individuals seeking mental health services with private insurance plans, veterans were about twice as likely to receive appropriate treatment for schizophrenia and depression at the VA.35 These documented strengths of VA mental health care may together help explain the small absolute number of visits that were associated with shifts away from VA overall after Medicaid expansion.
Finally, it is worth considering extrinsic factors that influence utilization among newly dual-eligible veterans. For example, hospitalizations are less likely to be planned than outpatient services, translating to a greater importance of proximity to a nearby medical facility than a veteran’s preference of where to seek care. In the same vein, major VA medical centers are fewer and more distant on average than VA outpatient clinics, therefore reducing the advantage of a Medicaid-reimbursed outpatient clinic in terms of distance.36 These realities may partially explain the proportionally larger shifts away from the VA for hospitalizations compared to outpatient care for depression.
Limitations and Future Directions
Our results should be interpreted within methodological and data limitations. With only 2 states in our sample, NY demonstrably skewed overall results, contributing 1.7 to 3 times more observations than AZ across subanalyses—a challenge also cited by Sommers and colleagues.19 Our veteran groupings were also unable to distinguish those veterans classified as service-connected who may also have qualified by income-eligible criteria (which would tend to understate the size of results) and those veterans who gained and then lost Medicaid coverage in a given year. Our study also faces limitations in generalizability and establishing causality. First, we included only 2 historical state Medicaid expansions, compared with the 38 states and Washington, DC, that have now expanded Medicaid to date under the ACA. Just in the 2 states from our study, we noted significant heterogeneity in the shifts associated with Medicaid expansion, which makes extrapolating specific trends difficult. Differences in underlying health care resources, legislation, and other external factors may limit the applicability of Medicaid expansion in the era of the ACA, as well as the Veterans Choice and MISSION acts. Second, while we leveraged a difference-in-difference analysis using demographically matched, neighboring comparison states, our findings are nevertheless drawn from observational data obviating causality. VA data for other sources of coverage such as private insurance are limited and not included in our study, and MAX datasets vary by quality across states, translating to potential gaps in our study cohort.28
Moving forward, our study demonstrates the potential for applying a natural experimental approach to studying dual-eligible veterans at the interface of Medicaid expansion. We focused on changes in VA reliance for the specific condition of depression and, in doing so, invite further inquiry into the impact of state mental health policy on outcomes more proximate to veterans’ outcomes. Clinical indicators, such as rates of antidepressant filling, utilization and duration of psychotherapy, and PHQ-9 scores, can similarly be investigated by natural experimental design. While current limits of administrative data and the siloing of EHRs may pose barriers to some of these avenues of research, multidisciplinary methodologies and data querying innovations such as natural language processing algorithms for clinical notes hold exciting opportunities to bridge the gap between policy and clinical efficacy.
Conclusions
This study applied a difference-in-difference analysis and found that Medicaid expansion is associated with decreases in VA reliance for both inpatient and outpatient services for depression. As additional data are generated from the Medicaid expansions of the ACA, similarly robust methods should be applied to further explore the impacts associated with such policy shifts and open the door to a better understanding of implications at the clinical level.
Acknowledgments
We acknowledge the efforts of Janine Wong, who proofread and formatted the manuscript.
1. US Department of Veterans Affairs, Veterans Health Administration. About VA. 2019. Updated September 27, 2022. Accessed September 29, 2022. https://www.va.gov/health/
2. Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. 2010;44(1):4-19. doi:10.3109/00048670903393597
3. Lan CW, Fiellin DA, Barry DT, et al. The epidemiology of substance use disorders in US veterans: a systematic review and analysis of assessment methods. Am J Addict. 2016;25(1):7-24. doi:10.1111/ajad.12319
4. Grant BF, Saha TD, June Ruan W, et al. Epidemiology of DSM-5 drug use disorder results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiat. 2016;73(1):39-47. doi:10.1001/jamapsychiatry.015.2132
5. Pemberton MR, Forman-Hoffman VL, Lipari RN, Ashley OS, Heller DC, Williams MR. Prevalence of past year substance use and mental illness by veteran status in a nationally representative sample. CBHSQ Data Review. Published November 9, 2016. Accessed October 6, 2022. https://www.samhsa.gov/data/report/prevalence-past-year-substance-use-and-mental-illness-veteran-status-nationally
6. Watkins KE, Pincus HA, Smith B, et al. Veterans Health Administration Mental Health Program Evaluation: Capstone Report. 2011. Accessed September 29, 2022. https://www.rand.org/pubs/technical_reports/TR956.html
7. Henry J. Kaiser Family Foundation. Medicaid’s role in covering veterans. June 29, 2017. Accessed September 29, 2022. https://www.kff.org/infographic/medicaids-role-in-covering-veterans
8. Substance Abuse and Mental Health Services Administration. Results from the 2016 National Survey on Drug Use and Health: detailed tables. September 7, 2017. Accessed September 29, 2022. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf
9. Wen H, Druss BG, Cummings JR. Effect of Medicaid expansions on health insurance coverage and access to care among low-income adults with behavioral health conditions. Health Serv Res. 2015;50:1787-1809. doi:10.1111/1475-6773.12411
10. O’Mahen PN, Petersen LA. Effects of state-level Medicaid expansion on Veterans Health Administration dual enrollment and utilization: potential implications for future coverage expansions. Med Care. 2020;58(6):526-533. doi:10.1097/MLR.0000000000001327
11. Ono SS, Dziak KM, Wittrock SM, et al. Treating dual-use patients across two health care systems: a qualitative study. Fed Pract. 2015;32(8):32-37.
12. Weeks WB, Mahar PJ, Wright SM. Utilization of VA and Medicare services by Medicare-eligible veterans: the impact of additional access points in a rural setting. J Healthc Manag. 2005;50(2):95-106.
13. Gellad WF, Thorpe JM, Zhao X, et al. Impact of dual use of Department of Veterans Affairs and Medicare part d drug benefits on potentially unsafe opioid use. Am J Public Health. 2018;108(2):248-255. doi:10.2105/AJPH.2017.304174
14. Coughlin SS, Young L. A review of dual health care system use by veterans with cardiometabolic disease. J Hosp Manag Health Policy. 2018;2:39. doi:10.21037/jhmhp.2018.07.05
15. Radomski TR, Zhao X, Thorpe CT, et al. The impact of medication-based risk adjustment on the association between veteran health outcomes and dual health system use. J Gen Intern Med. 2017;32(9):967-973. doi:10.1007/s11606-017-4064-4
16. Kullgren JT, Fagerlin A, Kerr EA. Completing the MISSION: a blueprint for helping veterans make the most of new choices. J Gen Intern Med. 2020;35(5):1567-1570. doi:10.1007/s11606-019-05404-w
17. VA MISSION Act of 2018, 38 USC §101 (2018). https://www.govinfo.gov/app/details/USCODE-2018-title38/USCODE-2018-title38-partI-chap1-sec101
18. Vanneman ME, Phibbs CS, Dally SK, Trivedi AN, Yoon J. The impact of Medicaid enrollment on Veterans Health Administration enrollees’ behavioral health services use. Health Serv Res. 2018;53(suppl 3):5238-5259. doi:10.1111/1475-6773.13062
19. Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367(11):1025-1034. doi:10.1056/NEJMsa1202099
20. US Department of Veterans Affairs Office of Mental Health. 2019 national veteran suicide prevention annual report. 2019. Accessed September 29, 2022. https://www.mentalhealth.va.gov/docs/data-sheets/2019/2019_National_Veteran_Suicide_Prevention_Annual_Report_508.pdf
21. Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147(1-3):17-28. doi:10.1016/j.jad.2013.01.004
22. Adekkanattu P, Sholle ET, DeFerio J, Pathak J, Johnson SB, Campion TR Jr. Ascertaining depression severity by extracting Patient Health Questionnaire-9 (PHQ-9) scores from clinical notes. AMIA Annu Symp Proc. 2018;2018:147-156.
23. DeRubeis RJ, Siegle GJ, Hollon SD. Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms. Nat Rev Neurosci. 2008;9(10):788-796. doi:10.1038/nrn2345
24. Cully JA, Zimmer M, Khan MM, Petersen LA. Quality of depression care and its impact on health service use and mortality among veterans. Psychiatr Serv. 2008;59(12):1399-1405. doi:10.1176/ps.2008.59.12.1399
25. Byrne MM, Kuebeler M, Pietz K, Petersen LA. Effect of using information from only one system for dually eligible health care users. Med Care. 2006;44(8):768-773. doi:10.1097/01.mlr.0000218786.44722.14
26. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396. doi:10.1176/appi.ps.201400537
27. Petersen LA, Byrne MM, Daw CN, Hasche J, Reis B, Pietz K. Relationship between clinical conditions and use of Veterans Affairs health care among Medicare-enrolled veterans. Health Serv Res. 2010;45(3):762-791. doi:10.1111/j.1475-6773.2010.01107.x
28. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Use of Veterans Affairs and Medicaid services for dually enrolled veterans. Health Serv Res. 2018;53(3):1539-1561. doi:10.1111/1475-6773.12727
29. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Veterans’ reliance on VA care by type of service and distance to VA for nonelderly VA-Medicaid dual enrollees. Med Care. 2019;57(3):225-229. doi:10.1097/MLR.0000000000001066
30. Gaglioti A, Cozad A, Wittrock S, et al. Non-VA primary care providers’ perspectives on comanagement for rural veterans. Mil Med. 2014;179(11):1236-1243. doi:10.7205/MILMED-D-13-00342
31. Moon S, Shin J. Health care utilization among Medicare-Medicaid dual eligibles: a count data analysis. BMC Public Health. 2006;6(1):88. doi:10.1186/1471-2458-6-88
32. Henry J. Kaiser Family Foundation. Facilitating access to mental health services: a look at Medicaid, private insurance, and the uninsured. November 27, 2017. Accessed September 29, 2022. https://www.kff.org/medicaid/fact-sheet/facilitating-access-to-mental-health-services-a-look-at-medicaid-private-insurance-and-the-uninsured
33. Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment - effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713-1722. doi:10.1056/NEJMsa1212321
34. Tanielian T, Farris C, Batka C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. 2014. Accessed September 29, 2022. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf
35. Kizer KW, Dudley RA. Extreme makeover: transformation of the Veterans Health Care System. Annu Rev Public Health. 2009;30(1):313-339. doi:10.1146/annurev.publhealth.29.020907.090940
36. Brennan KJ. Kendra’s Law: final report on the status of assisted outpatient treatment, appendix 2. 2002. Accessed September 29, 2022. https://omh.ny.gov/omhweb/kendra_web/finalreport/appendix2.htm
The US Department of Veterans Affairs (VA) is the largest integrated health care system in the United States, providing care for more than 9 million veterans.1 With veterans experiencing mental health conditions like posttraumatic stress disorder (PTSD), substance use disorders, and other serious mental illnesses (SMI) at higher rates compared with the general population, the VA plays an important role in the provision of mental health services.2-5 Since the implementation of its Mental Health Strategic Plan in 2004, the VA has overseen the development of a wide array of mental health programs geared toward the complex needs of veterans. Research has demonstrated VA care outperforming Medicaid-reimbursed services in terms of the percentage of veterans filling antidepressants for at least 12 weeks after initiation of treatment for major depressive disorder (MDD), as well as posthospitalization follow-up.6
Eligible veterans enrolled in the VA often also seek non-VA care. Medicaid covers nearly 10% of all nonelderly veterans, and of these veterans, 39% rely solely on Medicaid for health care access.7 Today, Medicaid is the largest payer for mental health services in the US, providing coverage for approximately 27% of Americans who have SMI and helping fulfill unmet mental health needs.8,9 Understanding which of these systems veterans choose to use, and under which circumstances, is essential in guiding the allocation of limited health care resources.10
Beyond Medicaid, alternatives to VA care may include TRICARE, Medicare, Indian Health Services, and employer-based or self-purchased private insurance. While these options potentially increase convenience, choice, and access to health care practitioners (HCPs) and services not available at local VA systems, cross-system utilization with poor integration may cause care coordination and continuity problems, such as medication mismanagement and opioid overdose, unnecessary duplicate utilization, and possible increased mortality.11-15 As recent national legislative changes, such as the Patient Protection and Affordable Care Act (ACA), Veterans Access, Choice and Accountability Act, and the VA MISSION Act, continue to shift the health care landscape for veterans, questions surrounding how veterans are changing their health care use become significant.16,17
Here, we approach the impacts of Medicaid expansion on veterans’ reliance on the VA for mental health services with a unique lens. We leverage a difference-in-difference design to study 2 historical Medicaid expansions in Arizona (AZ) and New York (NY), which extended eligibility to childless adults in 2001. Prior Medicaid dual-eligible mental health research investigated reliance shifts during the immediate postenrollment year in a subset of veterans newly enrolled in Medicaid.18 However, this study took place in a period of relative policy stability. In contrast, we investigate the potential effects of a broad policy shift by analyzing state-level changes in veterans’ reliance over 6 years after a statewide Medicaid expansion. We match expansion states with demographically similar nonexpansion states to account for unobserved trends and confounding effects. Prior studies have used this method to evaluate post-Medicaid expansion mortality changes and changes in veteran dual enrollment and hospitalizations.10,19 While a study of ACA Medicaid expansion states would be ideal, Medicaid data from most states were only available through 2014 at the time of this analysis. Our study offers a quasi-experimental framework leveraging longitudinal data that can be applied as more post-ACA data become available.
Given the rising incidence of suicide among veterans, understanding care-seeking behaviors for depression among veterans is important as it is the most common psychiatric condition found in those who died by suicide.20,21 Furthermore, depression may be useful as a clinical proxy for mental health policy impacts, given that the Patient Health Questionnaire-9 (PHQ-9) screening tool is well validated and increasingly research accessible, and it is a chronic condition responsive to both well-managed pharmacologic treatment and psychotherapeutic interventions.22,23
In this study, we quantify the change in care-seeking behavior for depression among veterans after Medicaid expansion, using a quasi-experimental design. We hypothesize that new access to Medicaid would be associated with a shift away from using VA services for depression. Given the income-dependent eligibility requirements of Medicaid, we also hypothesize that veterans who qualified for VA coverage due to low income, determined by a regional means test (Priority group 5, “income-eligible”), would be more likely to shift care compared with those whose serviced-connected conditions related to their military service (Priority groups 1-4, “service-connected”) provide VA access.
Methods
To investigate the relative changes in veterans’ reliance on the VA for depression care after the 2001 NY and AZ Medicaid expansions We used a retrospective, difference-in-difference analysis. Our comparison pairings, based on prior demographic analyses were as follows: NY with Pennsylvania(PA); AZ with New Mexico and Nevada (NM/NV).19 The time frame of our analysis was 1999 to 2006, with pre- and postexpansion periods defined as 1999 to 2000 and 2001 to 2006, respectively.
Data
We included veterans aged 18 to 64 years, seeking care for depression from 1999 to 2006, who were also VA-enrolled and residing in our states of interest. We counted veterans as enrolled in Medicaid if they were enrolled at least 1 month in a given year.
Using similar methods like those used in prior studies, we selected patients with encounters documenting depression as the primary outpatient or inpatient diagnosis using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: 296.2x for a single episode of major depressive disorder, 296.3x for a recurrent episode of MDD, 300.4 for dysthymia, and 311.0 for depression not otherwise specified.18,24 We used data from the Medicaid Analytic eXtract files (MAX) for Medicaid data and the VA Corporate Data Warehouse (CDW) for VA data. We chose 1999 as the first study year because it was the earliest year MAX data were available.
Our final sample included 1833 person-years pre-expansion and 7157 postexpansion in our inpatient analysis, as well as 31,767 person-years pre-expansion and 130,382 postexpansion in our outpatient analysis.
Outcomes and Variables
Our primary outcomes were comparative shifts in VA reliance between expansion and nonexpansion states after Medicaid expansion for both inpatient and outpatient depression care. For each year of study, we calculated a veteran’s VA reliance by aggregating the number of days with depression-related encounters at the VA and dividing by the total number of days with a VA or Medicaid depression-related encounters for the year. To provide context to these shifts in VA reliance, we further analyzed the changes in the proportion of annual VA-Medicaid dual users and annual per capita utilization of depression care across the VA and Medicaid.
We conducted subanalyses by income-eligible and service-connected veterans and adjusted our models for age, non-White race, sex, distances to the nearest inpatient and outpatient VA facilities, and VA Relative Risk Score, which is a measure of disease burden and clinical complexity validated specifically for veterans.25
Statistical Analysis
We used fractional logistic regression to model the adjusted effect of Medicaid expansion on VA reliance for depression care. In parallel, we leveraged ordered logit regression and negative binomial regression models to examine the proportion of VA-Medicaid dual users and the per capita utilization of Medicaid and VA depression care, respectively. To estimate the difference-in-difference effects, we used the interaction term of 2 categorical variables—expansion vs nonexpansion states and pre- vs postexpansion status—as the independent variable. We then calculated the average marginal effects with 95% CIs to estimate the differences in outcomes between expansion and nonexpansion states from pre- to postexpansion periods, as well as year-by-year shifts as a robustness check. We conducted these analyses using Stata MP, version 15.
Results
Baseline and postexpansion characteristics
VA Reliance
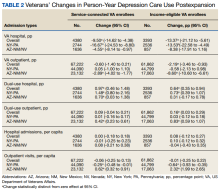
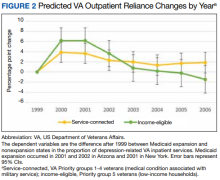
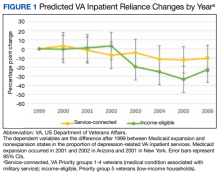
Overall, we observed postexpansion decreases in VA reliance for depression care
At the state level, reliance on the VA for inpatient depression care in NY decreased by 13.53 pp (95% CI, -22.58 to -4.49) for income-eligible veterans and 16.67 pp (95% CI, -24.53 to -8.80) for service-connected veterans. No relative differences were observed in the outpatient comparisons for both income-eligible (-0.58 pp; 95% CI, -2.13 to 0.98) and service-connected (0.05 pp; 95% CI, -1.00 to 1.10) veterans. In AZ, Medicaid expansion was associated with decreased VA reliance for outpatient depression care among income-eligible veterans (-8.60 pp; 95% CI, -10.60 to -6.61), greater than that for service-connected veterans (-2.89 pp; 95% CI, -4.02 to -1.77). This decrease in VA reliance was significant in the inpatient context only for service-connected veterans (-4.55 pp; 95% CI, -8.14 to -0.97), not income-eligible veterans (-8.38 pp; 95% CI, -17.91 to 1.16).
By applying the aggregate pp changes toward the postexpansion number of visits across both expansion and nonexpansion states, we found that expansion of Medicaid across all our study states would have resulted in 996 fewer hospitalizations and 10,109 fewer outpatient visits for depression at VA in the postexpansion period vs if no states had chosen to expand Medicaid.
Dual Use/Per Capita Utilization
Overall, Medicaid expansion was associated with greater dual use for inpatient depression care—a 0.97-pp (95% CI, 0.46 to 1.48) increase among service-connected veterans and a 0.64-pp (95% CI, 0.35 to 0.94) increase among income-eligible veterans.
At the state level, NY similarly showed increases in dual use among both service-connected (1.48 pp; 95% CI, 0.80 to 2.16) and income-eligible veterans (0.73 pp; 95% CI, 0.39 to 1.07) after Medicaid expansion. However, dual use in AZ increased significantly only among service-connected veterans (0.70 pp; 95% CI, 0.03 to 1.38), not income-eligible veterans (0.31 pp; 95% CI, -0.17 to 0.78).
Among outpatient visits, Medicaid expansion was associated with increased dual use only for income-eligible veterans (0.16 pp; 95% CI, 0.03-0.29), and not service-connected veterans (0.09 pp; 95% CI, -0.04 to 0.21). State-level analyses showed that Medicaid expansion in NY was not associated with changes in dual use for either service-connected (0.01 pp; 95% CI, -0.16 to 0.17) or income-eligible veterans (0.03 pp; 95% CI, -0.12 to 0.18), while expansion in AZ was associated with increases in dual use among both service-connected (0.42 pp; 95% CI, 0.23 to 0.61) and income-eligible veterans (0.83 pp; 95% CI, 0.59 to 1.07).
Concerning per capita utilization of depression care after Medicaid expansion, analyses showed no detectable changes for either inpatient or outpatient services, among both service-connected and income-eligible veterans. However, while this pattern held at the state level among hospitalizations, outpatient visit results showed divergent trends between AZ and NY. In NY, Medicaid expansion was associated with decreased per capita utilization of outpatient depression care among both service-connected (-0.25 visits annually; 95% CI, -0.48 to -0.01) and income-eligible veterans (-0.64 visits annually; 95% CI, -0.93 to -0.35). In AZ, Medicaid expansion was associated with increased per capita utilization of outpatient depression care among both service-connected (0.62 visits annually; 95% CI, 0.32-0.91) and income-eligible veterans (2.32 visits annually; 95% CI, 1.99-2.65).
Discussion
Our study quantified changes in depression-related health care utilization after Medicaid expansions in NY and AZ in 2001. Overall, the balance of evidence indicated that Medicaid expansion was associated with decreased reliance on the VA for depression-related services. There was an exception: income-eligible veterans in AZ did not shift their hospital care away from the VA in a statistically discernible way, although the point estimate was lower. More broadly, these findings concerning veterans’ reliance varied not only in inpatient vs outpatient services and income- vs service-connected eligibility, but also in the state-level contexts of veteran dual users and per capita utilization.
Given that the overall per capita utilization of depression care was unchanged from pre- to postexpansion periods, one might interpret the decreases in VA reliance and increases in Medicaid-VA dual users as a substitution effect from VA care to non-VA care. This could be plausible for hospitalizations where state-level analyses showed similarly stable levels of per capita utilization. However, state-level trends in our outpatient utilization analysis, especially with a substantial 2.32 pp increase in annual per capita visits among income-eligible veterans in AZ, leave open the possibility that in some cases veterans may be complementing VA care with Medicaid-reimbursed services.
The causes underlying these differences in reliance shifts between NY and AZ are likely also influenced by the policy contexts of their respective Medicaid expansions. For example, in 1999, NY passed Kendra’s Law, which established a procedure for obtaining court orders for assisted outpatient mental health treatment for individuals deemed unlikely to survive safely in the community.26 A reasonable inference is that there was less unfulfilled outpatient mental health need in NY under the existing accessibility provisioned by Kendra’s Law. In addition, while both states extended coverage to childless adults under 100% of the Federal Poverty level (FPL), the AZ Medicaid expansion was via a voters’ initiative and extended family coverage to 200% FPL vs 150% FPL for families in NY. Given that the AZ Medicaid expansion enjoyed both broader public participation and generosity in terms of eligibility, its uptake and therefore effect size may have been larger than in NY for nonacute outpatient care.
Our findings contribute to the growing body of literature surrounding the changes in health care utilization after Medicaid expansion, specifically for a newly dual-eligible population of veterans seeking mental health services for depression. While prior research concerning Medicare dual-enrolled veterans has shown high reliance on the VA for both mental health diagnoses and services, scholars have established the association of Medicaid enrollment with decreased VA reliance.27-29 Our analysis is the first to investigate state-level effects of Medicaid expansion on VA reliance for a single mental health condition using a natural experimental framework. We focus on a population that includes a large portion of veterans who are newly Medicaid-eligible due to a sweeping policy change and use demographically matched nonexpansion states to draw comparisons in VA reliance for depression care. Our findings of Medicaid expansion–associated decreases in VA reliance for depression care complement prior literature that describe Medicaid enrollment–associated decreases in VA reliance for overall mental health care.
Implications
From a systems-level perspective, the implications of shifting services away from the VA are complex and incompletely understood. The VA lacks interoperability with the electronic health records (EHRs) used by Medicaid clinicians. Consequently, significant issues of service duplication and incomplete clinical data exist for veterans seeking treatment outside of the VA system, posing health care quality and safety concerns.30 On one hand, Medicaid access is associated with increased health care utilization attributed to filling unmet needs for Medicare dual enrollees, as well as increased prescription filling for psychiatric medications.31,32 Furthermore, the only randomized control trial of Medicaid expansion to date was associated with a 9-pp decrease in positive screening rates for depression among those who received access at around 2 years postexpansion.33 On the other hand, the VA has developed a mental health system tailored to the particular needs of veterans, and health care practitioners at the VA have significantly greater rates of military cultural competency compared to those in nonmilitary settings (70% vs 24% in the TRICARE network and 8% among those with no military or TRICARE affiliation).34 Compared to individuals seeking mental health services with private insurance plans, veterans were about twice as likely to receive appropriate treatment for schizophrenia and depression at the VA.35 These documented strengths of VA mental health care may together help explain the small absolute number of visits that were associated with shifts away from VA overall after Medicaid expansion.
Finally, it is worth considering extrinsic factors that influence utilization among newly dual-eligible veterans. For example, hospitalizations are less likely to be planned than outpatient services, translating to a greater importance of proximity to a nearby medical facility than a veteran’s preference of where to seek care. In the same vein, major VA medical centers are fewer and more distant on average than VA outpatient clinics, therefore reducing the advantage of a Medicaid-reimbursed outpatient clinic in terms of distance.36 These realities may partially explain the proportionally larger shifts away from the VA for hospitalizations compared to outpatient care for depression.
Limitations and Future Directions
Our results should be interpreted within methodological and data limitations. With only 2 states in our sample, NY demonstrably skewed overall results, contributing 1.7 to 3 times more observations than AZ across subanalyses—a challenge also cited by Sommers and colleagues.19 Our veteran groupings were also unable to distinguish those veterans classified as service-connected who may also have qualified by income-eligible criteria (which would tend to understate the size of results) and those veterans who gained and then lost Medicaid coverage in a given year. Our study also faces limitations in generalizability and establishing causality. First, we included only 2 historical state Medicaid expansions, compared with the 38 states and Washington, DC, that have now expanded Medicaid to date under the ACA. Just in the 2 states from our study, we noted significant heterogeneity in the shifts associated with Medicaid expansion, which makes extrapolating specific trends difficult. Differences in underlying health care resources, legislation, and other external factors may limit the applicability of Medicaid expansion in the era of the ACA, as well as the Veterans Choice and MISSION acts. Second, while we leveraged a difference-in-difference analysis using demographically matched, neighboring comparison states, our findings are nevertheless drawn from observational data obviating causality. VA data for other sources of coverage such as private insurance are limited and not included in our study, and MAX datasets vary by quality across states, translating to potential gaps in our study cohort.28
Moving forward, our study demonstrates the potential for applying a natural experimental approach to studying dual-eligible veterans at the interface of Medicaid expansion. We focused on changes in VA reliance for the specific condition of depression and, in doing so, invite further inquiry into the impact of state mental health policy on outcomes more proximate to veterans’ outcomes. Clinical indicators, such as rates of antidepressant filling, utilization and duration of psychotherapy, and PHQ-9 scores, can similarly be investigated by natural experimental design. While current limits of administrative data and the siloing of EHRs may pose barriers to some of these avenues of research, multidisciplinary methodologies and data querying innovations such as natural language processing algorithms for clinical notes hold exciting opportunities to bridge the gap between policy and clinical efficacy.
Conclusions
This study applied a difference-in-difference analysis and found that Medicaid expansion is associated with decreases in VA reliance for both inpatient and outpatient services for depression. As additional data are generated from the Medicaid expansions of the ACA, similarly robust methods should be applied to further explore the impacts associated with such policy shifts and open the door to a better understanding of implications at the clinical level.
Acknowledgments
We acknowledge the efforts of Janine Wong, who proofread and formatted the manuscript.
The US Department of Veterans Affairs (VA) is the largest integrated health care system in the United States, providing care for more than 9 million veterans.1 With veterans experiencing mental health conditions like posttraumatic stress disorder (PTSD), substance use disorders, and other serious mental illnesses (SMI) at higher rates compared with the general population, the VA plays an important role in the provision of mental health services.2-5 Since the implementation of its Mental Health Strategic Plan in 2004, the VA has overseen the development of a wide array of mental health programs geared toward the complex needs of veterans. Research has demonstrated VA care outperforming Medicaid-reimbursed services in terms of the percentage of veterans filling antidepressants for at least 12 weeks after initiation of treatment for major depressive disorder (MDD), as well as posthospitalization follow-up.6
Eligible veterans enrolled in the VA often also seek non-VA care. Medicaid covers nearly 10% of all nonelderly veterans, and of these veterans, 39% rely solely on Medicaid for health care access.7 Today, Medicaid is the largest payer for mental health services in the US, providing coverage for approximately 27% of Americans who have SMI and helping fulfill unmet mental health needs.8,9 Understanding which of these systems veterans choose to use, and under which circumstances, is essential in guiding the allocation of limited health care resources.10
Beyond Medicaid, alternatives to VA care may include TRICARE, Medicare, Indian Health Services, and employer-based or self-purchased private insurance. While these options potentially increase convenience, choice, and access to health care practitioners (HCPs) and services not available at local VA systems, cross-system utilization with poor integration may cause care coordination and continuity problems, such as medication mismanagement and opioid overdose, unnecessary duplicate utilization, and possible increased mortality.11-15 As recent national legislative changes, such as the Patient Protection and Affordable Care Act (ACA), Veterans Access, Choice and Accountability Act, and the VA MISSION Act, continue to shift the health care landscape for veterans, questions surrounding how veterans are changing their health care use become significant.16,17
Here, we approach the impacts of Medicaid expansion on veterans’ reliance on the VA for mental health services with a unique lens. We leverage a difference-in-difference design to study 2 historical Medicaid expansions in Arizona (AZ) and New York (NY), which extended eligibility to childless adults in 2001. Prior Medicaid dual-eligible mental health research investigated reliance shifts during the immediate postenrollment year in a subset of veterans newly enrolled in Medicaid.18 However, this study took place in a period of relative policy stability. In contrast, we investigate the potential effects of a broad policy shift by analyzing state-level changes in veterans’ reliance over 6 years after a statewide Medicaid expansion. We match expansion states with demographically similar nonexpansion states to account for unobserved trends and confounding effects. Prior studies have used this method to evaluate post-Medicaid expansion mortality changes and changes in veteran dual enrollment and hospitalizations.10,19 While a study of ACA Medicaid expansion states would be ideal, Medicaid data from most states were only available through 2014 at the time of this analysis. Our study offers a quasi-experimental framework leveraging longitudinal data that can be applied as more post-ACA data become available.
Given the rising incidence of suicide among veterans, understanding care-seeking behaviors for depression among veterans is important as it is the most common psychiatric condition found in those who died by suicide.20,21 Furthermore, depression may be useful as a clinical proxy for mental health policy impacts, given that the Patient Health Questionnaire-9 (PHQ-9) screening tool is well validated and increasingly research accessible, and it is a chronic condition responsive to both well-managed pharmacologic treatment and psychotherapeutic interventions.22,23
In this study, we quantify the change in care-seeking behavior for depression among veterans after Medicaid expansion, using a quasi-experimental design. We hypothesize that new access to Medicaid would be associated with a shift away from using VA services for depression. Given the income-dependent eligibility requirements of Medicaid, we also hypothesize that veterans who qualified for VA coverage due to low income, determined by a regional means test (Priority group 5, “income-eligible”), would be more likely to shift care compared with those whose serviced-connected conditions related to their military service (Priority groups 1-4, “service-connected”) provide VA access.
Methods
To investigate the relative changes in veterans’ reliance on the VA for depression care after the 2001 NY and AZ Medicaid expansions We used a retrospective, difference-in-difference analysis. Our comparison pairings, based on prior demographic analyses were as follows: NY with Pennsylvania(PA); AZ with New Mexico and Nevada (NM/NV).19 The time frame of our analysis was 1999 to 2006, with pre- and postexpansion periods defined as 1999 to 2000 and 2001 to 2006, respectively.
Data
We included veterans aged 18 to 64 years, seeking care for depression from 1999 to 2006, who were also VA-enrolled and residing in our states of interest. We counted veterans as enrolled in Medicaid if they were enrolled at least 1 month in a given year.
Using similar methods like those used in prior studies, we selected patients with encounters documenting depression as the primary outpatient or inpatient diagnosis using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: 296.2x for a single episode of major depressive disorder, 296.3x for a recurrent episode of MDD, 300.4 for dysthymia, and 311.0 for depression not otherwise specified.18,24 We used data from the Medicaid Analytic eXtract files (MAX) for Medicaid data and the VA Corporate Data Warehouse (CDW) for VA data. We chose 1999 as the first study year because it was the earliest year MAX data were available.
Our final sample included 1833 person-years pre-expansion and 7157 postexpansion in our inpatient analysis, as well as 31,767 person-years pre-expansion and 130,382 postexpansion in our outpatient analysis.
Outcomes and Variables
Our primary outcomes were comparative shifts in VA reliance between expansion and nonexpansion states after Medicaid expansion for both inpatient and outpatient depression care. For each year of study, we calculated a veteran’s VA reliance by aggregating the number of days with depression-related encounters at the VA and dividing by the total number of days with a VA or Medicaid depression-related encounters for the year. To provide context to these shifts in VA reliance, we further analyzed the changes in the proportion of annual VA-Medicaid dual users and annual per capita utilization of depression care across the VA and Medicaid.
We conducted subanalyses by income-eligible and service-connected veterans and adjusted our models for age, non-White race, sex, distances to the nearest inpatient and outpatient VA facilities, and VA Relative Risk Score, which is a measure of disease burden and clinical complexity validated specifically for veterans.25
Statistical Analysis
We used fractional logistic regression to model the adjusted effect of Medicaid expansion on VA reliance for depression care. In parallel, we leveraged ordered logit regression and negative binomial regression models to examine the proportion of VA-Medicaid dual users and the per capita utilization of Medicaid and VA depression care, respectively. To estimate the difference-in-difference effects, we used the interaction term of 2 categorical variables—expansion vs nonexpansion states and pre- vs postexpansion status—as the independent variable. We then calculated the average marginal effects with 95% CIs to estimate the differences in outcomes between expansion and nonexpansion states from pre- to postexpansion periods, as well as year-by-year shifts as a robustness check. We conducted these analyses using Stata MP, version 15.
Results
Baseline and postexpansion characteristics
VA Reliance
Overall, we observed postexpansion decreases in VA reliance for depression care
At the state level, reliance on the VA for inpatient depression care in NY decreased by 13.53 pp (95% CI, -22.58 to -4.49) for income-eligible veterans and 16.67 pp (95% CI, -24.53 to -8.80) for service-connected veterans. No relative differences were observed in the outpatient comparisons for both income-eligible (-0.58 pp; 95% CI, -2.13 to 0.98) and service-connected (0.05 pp; 95% CI, -1.00 to 1.10) veterans. In AZ, Medicaid expansion was associated with decreased VA reliance for outpatient depression care among income-eligible veterans (-8.60 pp; 95% CI, -10.60 to -6.61), greater than that for service-connected veterans (-2.89 pp; 95% CI, -4.02 to -1.77). This decrease in VA reliance was significant in the inpatient context only for service-connected veterans (-4.55 pp; 95% CI, -8.14 to -0.97), not income-eligible veterans (-8.38 pp; 95% CI, -17.91 to 1.16).
By applying the aggregate pp changes toward the postexpansion number of visits across both expansion and nonexpansion states, we found that expansion of Medicaid across all our study states would have resulted in 996 fewer hospitalizations and 10,109 fewer outpatient visits for depression at VA in the postexpansion period vs if no states had chosen to expand Medicaid.
Dual Use/Per Capita Utilization
Overall, Medicaid expansion was associated with greater dual use for inpatient depression care—a 0.97-pp (95% CI, 0.46 to 1.48) increase among service-connected veterans and a 0.64-pp (95% CI, 0.35 to 0.94) increase among income-eligible veterans.
At the state level, NY similarly showed increases in dual use among both service-connected (1.48 pp; 95% CI, 0.80 to 2.16) and income-eligible veterans (0.73 pp; 95% CI, 0.39 to 1.07) after Medicaid expansion. However, dual use in AZ increased significantly only among service-connected veterans (0.70 pp; 95% CI, 0.03 to 1.38), not income-eligible veterans (0.31 pp; 95% CI, -0.17 to 0.78).
Among outpatient visits, Medicaid expansion was associated with increased dual use only for income-eligible veterans (0.16 pp; 95% CI, 0.03-0.29), and not service-connected veterans (0.09 pp; 95% CI, -0.04 to 0.21). State-level analyses showed that Medicaid expansion in NY was not associated with changes in dual use for either service-connected (0.01 pp; 95% CI, -0.16 to 0.17) or income-eligible veterans (0.03 pp; 95% CI, -0.12 to 0.18), while expansion in AZ was associated with increases in dual use among both service-connected (0.42 pp; 95% CI, 0.23 to 0.61) and income-eligible veterans (0.83 pp; 95% CI, 0.59 to 1.07).
Concerning per capita utilization of depression care after Medicaid expansion, analyses showed no detectable changes for either inpatient or outpatient services, among both service-connected and income-eligible veterans. However, while this pattern held at the state level among hospitalizations, outpatient visit results showed divergent trends between AZ and NY. In NY, Medicaid expansion was associated with decreased per capita utilization of outpatient depression care among both service-connected (-0.25 visits annually; 95% CI, -0.48 to -0.01) and income-eligible veterans (-0.64 visits annually; 95% CI, -0.93 to -0.35). In AZ, Medicaid expansion was associated with increased per capita utilization of outpatient depression care among both service-connected (0.62 visits annually; 95% CI, 0.32-0.91) and income-eligible veterans (2.32 visits annually; 95% CI, 1.99-2.65).
Discussion
Our study quantified changes in depression-related health care utilization after Medicaid expansions in NY and AZ in 2001. Overall, the balance of evidence indicated that Medicaid expansion was associated with decreased reliance on the VA for depression-related services. There was an exception: income-eligible veterans in AZ did not shift their hospital care away from the VA in a statistically discernible way, although the point estimate was lower. More broadly, these findings concerning veterans’ reliance varied not only in inpatient vs outpatient services and income- vs service-connected eligibility, but also in the state-level contexts of veteran dual users and per capita utilization.
Given that the overall per capita utilization of depression care was unchanged from pre- to postexpansion periods, one might interpret the decreases in VA reliance and increases in Medicaid-VA dual users as a substitution effect from VA care to non-VA care. This could be plausible for hospitalizations where state-level analyses showed similarly stable levels of per capita utilization. However, state-level trends in our outpatient utilization analysis, especially with a substantial 2.32 pp increase in annual per capita visits among income-eligible veterans in AZ, leave open the possibility that in some cases veterans may be complementing VA care with Medicaid-reimbursed services.
The causes underlying these differences in reliance shifts between NY and AZ are likely also influenced by the policy contexts of their respective Medicaid expansions. For example, in 1999, NY passed Kendra’s Law, which established a procedure for obtaining court orders for assisted outpatient mental health treatment for individuals deemed unlikely to survive safely in the community.26 A reasonable inference is that there was less unfulfilled outpatient mental health need in NY under the existing accessibility provisioned by Kendra’s Law. In addition, while both states extended coverage to childless adults under 100% of the Federal Poverty level (FPL), the AZ Medicaid expansion was via a voters’ initiative and extended family coverage to 200% FPL vs 150% FPL for families in NY. Given that the AZ Medicaid expansion enjoyed both broader public participation and generosity in terms of eligibility, its uptake and therefore effect size may have been larger than in NY for nonacute outpatient care.
Our findings contribute to the growing body of literature surrounding the changes in health care utilization after Medicaid expansion, specifically for a newly dual-eligible population of veterans seeking mental health services for depression. While prior research concerning Medicare dual-enrolled veterans has shown high reliance on the VA for both mental health diagnoses and services, scholars have established the association of Medicaid enrollment with decreased VA reliance.27-29 Our analysis is the first to investigate state-level effects of Medicaid expansion on VA reliance for a single mental health condition using a natural experimental framework. We focus on a population that includes a large portion of veterans who are newly Medicaid-eligible due to a sweeping policy change and use demographically matched nonexpansion states to draw comparisons in VA reliance for depression care. Our findings of Medicaid expansion–associated decreases in VA reliance for depression care complement prior literature that describe Medicaid enrollment–associated decreases in VA reliance for overall mental health care.
Implications
From a systems-level perspective, the implications of shifting services away from the VA are complex and incompletely understood. The VA lacks interoperability with the electronic health records (EHRs) used by Medicaid clinicians. Consequently, significant issues of service duplication and incomplete clinical data exist for veterans seeking treatment outside of the VA system, posing health care quality and safety concerns.30 On one hand, Medicaid access is associated with increased health care utilization attributed to filling unmet needs for Medicare dual enrollees, as well as increased prescription filling for psychiatric medications.31,32 Furthermore, the only randomized control trial of Medicaid expansion to date was associated with a 9-pp decrease in positive screening rates for depression among those who received access at around 2 years postexpansion.33 On the other hand, the VA has developed a mental health system tailored to the particular needs of veterans, and health care practitioners at the VA have significantly greater rates of military cultural competency compared to those in nonmilitary settings (70% vs 24% in the TRICARE network and 8% among those with no military or TRICARE affiliation).34 Compared to individuals seeking mental health services with private insurance plans, veterans were about twice as likely to receive appropriate treatment for schizophrenia and depression at the VA.35 These documented strengths of VA mental health care may together help explain the small absolute number of visits that were associated with shifts away from VA overall after Medicaid expansion.
Finally, it is worth considering extrinsic factors that influence utilization among newly dual-eligible veterans. For example, hospitalizations are less likely to be planned than outpatient services, translating to a greater importance of proximity to a nearby medical facility than a veteran’s preference of where to seek care. In the same vein, major VA medical centers are fewer and more distant on average than VA outpatient clinics, therefore reducing the advantage of a Medicaid-reimbursed outpatient clinic in terms of distance.36 These realities may partially explain the proportionally larger shifts away from the VA for hospitalizations compared to outpatient care for depression.
Limitations and Future Directions
Our results should be interpreted within methodological and data limitations. With only 2 states in our sample, NY demonstrably skewed overall results, contributing 1.7 to 3 times more observations than AZ across subanalyses—a challenge also cited by Sommers and colleagues.19 Our veteran groupings were also unable to distinguish those veterans classified as service-connected who may also have qualified by income-eligible criteria (which would tend to understate the size of results) and those veterans who gained and then lost Medicaid coverage in a given year. Our study also faces limitations in generalizability and establishing causality. First, we included only 2 historical state Medicaid expansions, compared with the 38 states and Washington, DC, that have now expanded Medicaid to date under the ACA. Just in the 2 states from our study, we noted significant heterogeneity in the shifts associated with Medicaid expansion, which makes extrapolating specific trends difficult. Differences in underlying health care resources, legislation, and other external factors may limit the applicability of Medicaid expansion in the era of the ACA, as well as the Veterans Choice and MISSION acts. Second, while we leveraged a difference-in-difference analysis using demographically matched, neighboring comparison states, our findings are nevertheless drawn from observational data obviating causality. VA data for other sources of coverage such as private insurance are limited and not included in our study, and MAX datasets vary by quality across states, translating to potential gaps in our study cohort.28
Moving forward, our study demonstrates the potential for applying a natural experimental approach to studying dual-eligible veterans at the interface of Medicaid expansion. We focused on changes in VA reliance for the specific condition of depression and, in doing so, invite further inquiry into the impact of state mental health policy on outcomes more proximate to veterans’ outcomes. Clinical indicators, such as rates of antidepressant filling, utilization and duration of psychotherapy, and PHQ-9 scores, can similarly be investigated by natural experimental design. While current limits of administrative data and the siloing of EHRs may pose barriers to some of these avenues of research, multidisciplinary methodologies and data querying innovations such as natural language processing algorithms for clinical notes hold exciting opportunities to bridge the gap between policy and clinical efficacy.
Conclusions
This study applied a difference-in-difference analysis and found that Medicaid expansion is associated with decreases in VA reliance for both inpatient and outpatient services for depression. As additional data are generated from the Medicaid expansions of the ACA, similarly robust methods should be applied to further explore the impacts associated with such policy shifts and open the door to a better understanding of implications at the clinical level.
Acknowledgments
We acknowledge the efforts of Janine Wong, who proofread and formatted the manuscript.
1. US Department of Veterans Affairs, Veterans Health Administration. About VA. 2019. Updated September 27, 2022. Accessed September 29, 2022. https://www.va.gov/health/
2. Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. 2010;44(1):4-19. doi:10.3109/00048670903393597
3. Lan CW, Fiellin DA, Barry DT, et al. The epidemiology of substance use disorders in US veterans: a systematic review and analysis of assessment methods. Am J Addict. 2016;25(1):7-24. doi:10.1111/ajad.12319
4. Grant BF, Saha TD, June Ruan W, et al. Epidemiology of DSM-5 drug use disorder results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiat. 2016;73(1):39-47. doi:10.1001/jamapsychiatry.015.2132
5. Pemberton MR, Forman-Hoffman VL, Lipari RN, Ashley OS, Heller DC, Williams MR. Prevalence of past year substance use and mental illness by veteran status in a nationally representative sample. CBHSQ Data Review. Published November 9, 2016. Accessed October 6, 2022. https://www.samhsa.gov/data/report/prevalence-past-year-substance-use-and-mental-illness-veteran-status-nationally
6. Watkins KE, Pincus HA, Smith B, et al. Veterans Health Administration Mental Health Program Evaluation: Capstone Report. 2011. Accessed September 29, 2022. https://www.rand.org/pubs/technical_reports/TR956.html
7. Henry J. Kaiser Family Foundation. Medicaid’s role in covering veterans. June 29, 2017. Accessed September 29, 2022. https://www.kff.org/infographic/medicaids-role-in-covering-veterans
8. Substance Abuse and Mental Health Services Administration. Results from the 2016 National Survey on Drug Use and Health: detailed tables. September 7, 2017. Accessed September 29, 2022. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf
9. Wen H, Druss BG, Cummings JR. Effect of Medicaid expansions on health insurance coverage and access to care among low-income adults with behavioral health conditions. Health Serv Res. 2015;50:1787-1809. doi:10.1111/1475-6773.12411
10. O’Mahen PN, Petersen LA. Effects of state-level Medicaid expansion on Veterans Health Administration dual enrollment and utilization: potential implications for future coverage expansions. Med Care. 2020;58(6):526-533. doi:10.1097/MLR.0000000000001327
11. Ono SS, Dziak KM, Wittrock SM, et al. Treating dual-use patients across two health care systems: a qualitative study. Fed Pract. 2015;32(8):32-37.
12. Weeks WB, Mahar PJ, Wright SM. Utilization of VA and Medicare services by Medicare-eligible veterans: the impact of additional access points in a rural setting. J Healthc Manag. 2005;50(2):95-106.
13. Gellad WF, Thorpe JM, Zhao X, et al. Impact of dual use of Department of Veterans Affairs and Medicare part d drug benefits on potentially unsafe opioid use. Am J Public Health. 2018;108(2):248-255. doi:10.2105/AJPH.2017.304174
14. Coughlin SS, Young L. A review of dual health care system use by veterans with cardiometabolic disease. J Hosp Manag Health Policy. 2018;2:39. doi:10.21037/jhmhp.2018.07.05
15. Radomski TR, Zhao X, Thorpe CT, et al. The impact of medication-based risk adjustment on the association between veteran health outcomes and dual health system use. J Gen Intern Med. 2017;32(9):967-973. doi:10.1007/s11606-017-4064-4
16. Kullgren JT, Fagerlin A, Kerr EA. Completing the MISSION: a blueprint for helping veterans make the most of new choices. J Gen Intern Med. 2020;35(5):1567-1570. doi:10.1007/s11606-019-05404-w
17. VA MISSION Act of 2018, 38 USC §101 (2018). https://www.govinfo.gov/app/details/USCODE-2018-title38/USCODE-2018-title38-partI-chap1-sec101
18. Vanneman ME, Phibbs CS, Dally SK, Trivedi AN, Yoon J. The impact of Medicaid enrollment on Veterans Health Administration enrollees’ behavioral health services use. Health Serv Res. 2018;53(suppl 3):5238-5259. doi:10.1111/1475-6773.13062
19. Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367(11):1025-1034. doi:10.1056/NEJMsa1202099
20. US Department of Veterans Affairs Office of Mental Health. 2019 national veteran suicide prevention annual report. 2019. Accessed September 29, 2022. https://www.mentalhealth.va.gov/docs/data-sheets/2019/2019_National_Veteran_Suicide_Prevention_Annual_Report_508.pdf
21. Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147(1-3):17-28. doi:10.1016/j.jad.2013.01.004
22. Adekkanattu P, Sholle ET, DeFerio J, Pathak J, Johnson SB, Campion TR Jr. Ascertaining depression severity by extracting Patient Health Questionnaire-9 (PHQ-9) scores from clinical notes. AMIA Annu Symp Proc. 2018;2018:147-156.
23. DeRubeis RJ, Siegle GJ, Hollon SD. Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms. Nat Rev Neurosci. 2008;9(10):788-796. doi:10.1038/nrn2345
24. Cully JA, Zimmer M, Khan MM, Petersen LA. Quality of depression care and its impact on health service use and mortality among veterans. Psychiatr Serv. 2008;59(12):1399-1405. doi:10.1176/ps.2008.59.12.1399
25. Byrne MM, Kuebeler M, Pietz K, Petersen LA. Effect of using information from only one system for dually eligible health care users. Med Care. 2006;44(8):768-773. doi:10.1097/01.mlr.0000218786.44722.14
26. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396. doi:10.1176/appi.ps.201400537
27. Petersen LA, Byrne MM, Daw CN, Hasche J, Reis B, Pietz K. Relationship between clinical conditions and use of Veterans Affairs health care among Medicare-enrolled veterans. Health Serv Res. 2010;45(3):762-791. doi:10.1111/j.1475-6773.2010.01107.x
28. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Use of Veterans Affairs and Medicaid services for dually enrolled veterans. Health Serv Res. 2018;53(3):1539-1561. doi:10.1111/1475-6773.12727
29. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Veterans’ reliance on VA care by type of service and distance to VA for nonelderly VA-Medicaid dual enrollees. Med Care. 2019;57(3):225-229. doi:10.1097/MLR.0000000000001066
30. Gaglioti A, Cozad A, Wittrock S, et al. Non-VA primary care providers’ perspectives on comanagement for rural veterans. Mil Med. 2014;179(11):1236-1243. doi:10.7205/MILMED-D-13-00342
31. Moon S, Shin J. Health care utilization among Medicare-Medicaid dual eligibles: a count data analysis. BMC Public Health. 2006;6(1):88. doi:10.1186/1471-2458-6-88
32. Henry J. Kaiser Family Foundation. Facilitating access to mental health services: a look at Medicaid, private insurance, and the uninsured. November 27, 2017. Accessed September 29, 2022. https://www.kff.org/medicaid/fact-sheet/facilitating-access-to-mental-health-services-a-look-at-medicaid-private-insurance-and-the-uninsured
33. Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment - effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713-1722. doi:10.1056/NEJMsa1212321
34. Tanielian T, Farris C, Batka C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. 2014. Accessed September 29, 2022. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf
35. Kizer KW, Dudley RA. Extreme makeover: transformation of the Veterans Health Care System. Annu Rev Public Health. 2009;30(1):313-339. doi:10.1146/annurev.publhealth.29.020907.090940
36. Brennan KJ. Kendra’s Law: final report on the status of assisted outpatient treatment, appendix 2. 2002. Accessed September 29, 2022. https://omh.ny.gov/omhweb/kendra_web/finalreport/appendix2.htm
1. US Department of Veterans Affairs, Veterans Health Administration. About VA. 2019. Updated September 27, 2022. Accessed September 29, 2022. https://www.va.gov/health/
2. Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. 2010;44(1):4-19. doi:10.3109/00048670903393597
3. Lan CW, Fiellin DA, Barry DT, et al. The epidemiology of substance use disorders in US veterans: a systematic review and analysis of assessment methods. Am J Addict. 2016;25(1):7-24. doi:10.1111/ajad.12319
4. Grant BF, Saha TD, June Ruan W, et al. Epidemiology of DSM-5 drug use disorder results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiat. 2016;73(1):39-47. doi:10.1001/jamapsychiatry.015.2132
5. Pemberton MR, Forman-Hoffman VL, Lipari RN, Ashley OS, Heller DC, Williams MR. Prevalence of past year substance use and mental illness by veteran status in a nationally representative sample. CBHSQ Data Review. Published November 9, 2016. Accessed October 6, 2022. https://www.samhsa.gov/data/report/prevalence-past-year-substance-use-and-mental-illness-veteran-status-nationally
6. Watkins KE, Pincus HA, Smith B, et al. Veterans Health Administration Mental Health Program Evaluation: Capstone Report. 2011. Accessed September 29, 2022. https://www.rand.org/pubs/technical_reports/TR956.html
7. Henry J. Kaiser Family Foundation. Medicaid’s role in covering veterans. June 29, 2017. Accessed September 29, 2022. https://www.kff.org/infographic/medicaids-role-in-covering-veterans
8. Substance Abuse and Mental Health Services Administration. Results from the 2016 National Survey on Drug Use and Health: detailed tables. September 7, 2017. Accessed September 29, 2022. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf
9. Wen H, Druss BG, Cummings JR. Effect of Medicaid expansions on health insurance coverage and access to care among low-income adults with behavioral health conditions. Health Serv Res. 2015;50:1787-1809. doi:10.1111/1475-6773.12411
10. O’Mahen PN, Petersen LA. Effects of state-level Medicaid expansion on Veterans Health Administration dual enrollment and utilization: potential implications for future coverage expansions. Med Care. 2020;58(6):526-533. doi:10.1097/MLR.0000000000001327
11. Ono SS, Dziak KM, Wittrock SM, et al. Treating dual-use patients across two health care systems: a qualitative study. Fed Pract. 2015;32(8):32-37.
12. Weeks WB, Mahar PJ, Wright SM. Utilization of VA and Medicare services by Medicare-eligible veterans: the impact of additional access points in a rural setting. J Healthc Manag. 2005;50(2):95-106.
13. Gellad WF, Thorpe JM, Zhao X, et al. Impact of dual use of Department of Veterans Affairs and Medicare part d drug benefits on potentially unsafe opioid use. Am J Public Health. 2018;108(2):248-255. doi:10.2105/AJPH.2017.304174
14. Coughlin SS, Young L. A review of dual health care system use by veterans with cardiometabolic disease. J Hosp Manag Health Policy. 2018;2:39. doi:10.21037/jhmhp.2018.07.05
15. Radomski TR, Zhao X, Thorpe CT, et al. The impact of medication-based risk adjustment on the association between veteran health outcomes and dual health system use. J Gen Intern Med. 2017;32(9):967-973. doi:10.1007/s11606-017-4064-4
16. Kullgren JT, Fagerlin A, Kerr EA. Completing the MISSION: a blueprint for helping veterans make the most of new choices. J Gen Intern Med. 2020;35(5):1567-1570. doi:10.1007/s11606-019-05404-w
17. VA MISSION Act of 2018, 38 USC §101 (2018). https://www.govinfo.gov/app/details/USCODE-2018-title38/USCODE-2018-title38-partI-chap1-sec101
18. Vanneman ME, Phibbs CS, Dally SK, Trivedi AN, Yoon J. The impact of Medicaid enrollment on Veterans Health Administration enrollees’ behavioral health services use. Health Serv Res. 2018;53(suppl 3):5238-5259. doi:10.1111/1475-6773.13062
19. Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367(11):1025-1034. doi:10.1056/NEJMsa1202099
20. US Department of Veterans Affairs Office of Mental Health. 2019 national veteran suicide prevention annual report. 2019. Accessed September 29, 2022. https://www.mentalhealth.va.gov/docs/data-sheets/2019/2019_National_Veteran_Suicide_Prevention_Annual_Report_508.pdf
21. Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147(1-3):17-28. doi:10.1016/j.jad.2013.01.004
22. Adekkanattu P, Sholle ET, DeFerio J, Pathak J, Johnson SB, Campion TR Jr. Ascertaining depression severity by extracting Patient Health Questionnaire-9 (PHQ-9) scores from clinical notes. AMIA Annu Symp Proc. 2018;2018:147-156.
23. DeRubeis RJ, Siegle GJ, Hollon SD. Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms. Nat Rev Neurosci. 2008;9(10):788-796. doi:10.1038/nrn2345
24. Cully JA, Zimmer M, Khan MM, Petersen LA. Quality of depression care and its impact on health service use and mortality among veterans. Psychiatr Serv. 2008;59(12):1399-1405. doi:10.1176/ps.2008.59.12.1399
25. Byrne MM, Kuebeler M, Pietz K, Petersen LA. Effect of using information from only one system for dually eligible health care users. Med Care. 2006;44(8):768-773. doi:10.1097/01.mlr.0000218786.44722.14
26. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396. doi:10.1176/appi.ps.201400537
27. Petersen LA, Byrne MM, Daw CN, Hasche J, Reis B, Pietz K. Relationship between clinical conditions and use of Veterans Affairs health care among Medicare-enrolled veterans. Health Serv Res. 2010;45(3):762-791. doi:10.1111/j.1475-6773.2010.01107.x
28. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Use of Veterans Affairs and Medicaid services for dually enrolled veterans. Health Serv Res. 2018;53(3):1539-1561. doi:10.1111/1475-6773.12727
29. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Veterans’ reliance on VA care by type of service and distance to VA for nonelderly VA-Medicaid dual enrollees. Med Care. 2019;57(3):225-229. doi:10.1097/MLR.0000000000001066
30. Gaglioti A, Cozad A, Wittrock S, et al. Non-VA primary care providers’ perspectives on comanagement for rural veterans. Mil Med. 2014;179(11):1236-1243. doi:10.7205/MILMED-D-13-00342
31. Moon S, Shin J. Health care utilization among Medicare-Medicaid dual eligibles: a count data analysis. BMC Public Health. 2006;6(1):88. doi:10.1186/1471-2458-6-88
32. Henry J. Kaiser Family Foundation. Facilitating access to mental health services: a look at Medicaid, private insurance, and the uninsured. November 27, 2017. Accessed September 29, 2022. https://www.kff.org/medicaid/fact-sheet/facilitating-access-to-mental-health-services-a-look-at-medicaid-private-insurance-and-the-uninsured
33. Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment - effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713-1722. doi:10.1056/NEJMsa1212321
34. Tanielian T, Farris C, Batka C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. 2014. Accessed September 29, 2022. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf
35. Kizer KW, Dudley RA. Extreme makeover: transformation of the Veterans Health Care System. Annu Rev Public Health. 2009;30(1):313-339. doi:10.1146/annurev.publhealth.29.020907.090940
36. Brennan KJ. Kendra’s Law: final report on the status of assisted outpatient treatment, appendix 2. 2002. Accessed September 29, 2022. https://omh.ny.gov/omhweb/kendra_web/finalreport/appendix2.htm
Traffic-related pollutant tied to increased dementia risk
Exposure to a traffic-related air pollutant significantly increases risk for dementia, new research suggests. Results from a meta-analysis, which included a total of more than 90 million people, showed
Particulate matter is a mixture of solid particles and liquid droplets from the burning of fossil fuels and nitrogen oxide, and also produced from road traffic exhaust.
While the research only showed an association between this type of air pollution and dementia risk, the estimates were consistent across the different analyses used.
“It’s rather sobering that there is this 3% relationship between incidence of dementia and the particulate matter and that it is such a precise estimate,” senior investigator Janet Martin, PharmD, MSc, associate professor of anesthesia & perioperative medicine and epidemiology & biostatistics at Western University’s, London, Ont., told this news organization.
The findings were published online in Neurology.
Conflicting results in past studies
Air pollution is a known risk factor for dementia, but studies attempting to pinpoint its exact impact have yielded conflicting results.
Researchers analyzed data from 17 studies with a total of 91.4 million individuals, 6% of whom had dementia. In addition to PM2.5, the investigators also assessed nitrogen oxides, which form smog, nitrogen dioxide, and ozone exposure.
After adjustments for other known risk factors, such as age and gender, results showed that dementia risk increased by 3% for every 1 m3 rise in PM2.5 exposure (adjusted hazard ratio, 1.03; 95% confidence interval, 1.02-1.05).
The associations between dementia and exposure to nitrogen oxides (HR, 1.05; 95% CI, 0.99-1.13), nitrogen dioxide (HR, 1.03; 95% CI, 1.00-1.07) and ozone (HR, 1.01; 95% CI, 0.91-1.11) did not reach statistical significance. However, the confidence intervals were wide enough that clinical relevance cannot be ruled out, Dr. Martin said.
The study did not examine how or if the duration of PM2.5 exposure affected dementia risk. In addition, the investigators were not able to identify a threshold above which dementia risk begins to rise.
The Environmental Pollution Agency considers average yearly exposures up to 12 mcg/m3 to be safe. The World Health Organization sets that limit lower, at 5 mcg/m3.
Dr. Martin noted that more studies are needed to explore those issues, as well as the mechanisms by which air pollutants contribute to the pathology of dementia. However, the clear link between fine particulate matter exposure and increased risk emphasizes the need to address air pollution as a modifiable risk factor for dementia.
“The rising tide of dementia is not something we can easily reverse,” Dr. Martin said. “The evidence has been so elusive for how to treat dementia once you have it, so our biggest opportunity is to prevent it.”
Results from a study published earlier in 2022 estimated that rates of dementia will triple worldwide and double in the United States by 2050 unless steps are taking to mitigate risk factors.
Research also suggests that improving air quality PM2.5 by just 10% results in a 14% decreased risk for dementia.
‘Impressive’ pattern
Paul Rosenberg, MD, codirector of the Memory and Alzheimer’s Treatment Center division of geriatric psychiatry at Johns Hopkins University, Baltimore, said that air pollution “is the most prominent environmental risk we’ve found” for dementia. It also “adds to many other lifestyle and comorbidity risks, such as lack of exercise, obesity, depression, hearing loss, etc,” said Dr. Rosenberg, who was not involved with the research.
He noted what was “most impressive” was that in most of the pooled studies, small particulate air pollution was associated with dementia. “The overall pattern is most impressive and the effect sizes quite consistent over most of the studies,” Dr. Rosenberg said.
The meta-analysis was unfunded. Dr. Martin and Dr. Rosenberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Exposure to a traffic-related air pollutant significantly increases risk for dementia, new research suggests. Results from a meta-analysis, which included a total of more than 90 million people, showed
Particulate matter is a mixture of solid particles and liquid droplets from the burning of fossil fuels and nitrogen oxide, and also produced from road traffic exhaust.
While the research only showed an association between this type of air pollution and dementia risk, the estimates were consistent across the different analyses used.
“It’s rather sobering that there is this 3% relationship between incidence of dementia and the particulate matter and that it is such a precise estimate,” senior investigator Janet Martin, PharmD, MSc, associate professor of anesthesia & perioperative medicine and epidemiology & biostatistics at Western University’s, London, Ont., told this news organization.
The findings were published online in Neurology.
Conflicting results in past studies
Air pollution is a known risk factor for dementia, but studies attempting to pinpoint its exact impact have yielded conflicting results.
Researchers analyzed data from 17 studies with a total of 91.4 million individuals, 6% of whom had dementia. In addition to PM2.5, the investigators also assessed nitrogen oxides, which form smog, nitrogen dioxide, and ozone exposure.
After adjustments for other known risk factors, such as age and gender, results showed that dementia risk increased by 3% for every 1 m3 rise in PM2.5 exposure (adjusted hazard ratio, 1.03; 95% confidence interval, 1.02-1.05).
The associations between dementia and exposure to nitrogen oxides (HR, 1.05; 95% CI, 0.99-1.13), nitrogen dioxide (HR, 1.03; 95% CI, 1.00-1.07) and ozone (HR, 1.01; 95% CI, 0.91-1.11) did not reach statistical significance. However, the confidence intervals were wide enough that clinical relevance cannot be ruled out, Dr. Martin said.
The study did not examine how or if the duration of PM2.5 exposure affected dementia risk. In addition, the investigators were not able to identify a threshold above which dementia risk begins to rise.
The Environmental Pollution Agency considers average yearly exposures up to 12 mcg/m3 to be safe. The World Health Organization sets that limit lower, at 5 mcg/m3.
Dr. Martin noted that more studies are needed to explore those issues, as well as the mechanisms by which air pollutants contribute to the pathology of dementia. However, the clear link between fine particulate matter exposure and increased risk emphasizes the need to address air pollution as a modifiable risk factor for dementia.
“The rising tide of dementia is not something we can easily reverse,” Dr. Martin said. “The evidence has been so elusive for how to treat dementia once you have it, so our biggest opportunity is to prevent it.”
Results from a study published earlier in 2022 estimated that rates of dementia will triple worldwide and double in the United States by 2050 unless steps are taking to mitigate risk factors.
Research also suggests that improving air quality PM2.5 by just 10% results in a 14% decreased risk for dementia.
‘Impressive’ pattern
Paul Rosenberg, MD, codirector of the Memory and Alzheimer’s Treatment Center division of geriatric psychiatry at Johns Hopkins University, Baltimore, said that air pollution “is the most prominent environmental risk we’ve found” for dementia. It also “adds to many other lifestyle and comorbidity risks, such as lack of exercise, obesity, depression, hearing loss, etc,” said Dr. Rosenberg, who was not involved with the research.
He noted what was “most impressive” was that in most of the pooled studies, small particulate air pollution was associated with dementia. “The overall pattern is most impressive and the effect sizes quite consistent over most of the studies,” Dr. Rosenberg said.
The meta-analysis was unfunded. Dr. Martin and Dr. Rosenberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Exposure to a traffic-related air pollutant significantly increases risk for dementia, new research suggests. Results from a meta-analysis, which included a total of more than 90 million people, showed
Particulate matter is a mixture of solid particles and liquid droplets from the burning of fossil fuels and nitrogen oxide, and also produced from road traffic exhaust.
While the research only showed an association between this type of air pollution and dementia risk, the estimates were consistent across the different analyses used.
“It’s rather sobering that there is this 3% relationship between incidence of dementia and the particulate matter and that it is such a precise estimate,” senior investigator Janet Martin, PharmD, MSc, associate professor of anesthesia & perioperative medicine and epidemiology & biostatistics at Western University’s, London, Ont., told this news organization.
The findings were published online in Neurology.
Conflicting results in past studies
Air pollution is a known risk factor for dementia, but studies attempting to pinpoint its exact impact have yielded conflicting results.
Researchers analyzed data from 17 studies with a total of 91.4 million individuals, 6% of whom had dementia. In addition to PM2.5, the investigators also assessed nitrogen oxides, which form smog, nitrogen dioxide, and ozone exposure.
After adjustments for other known risk factors, such as age and gender, results showed that dementia risk increased by 3% for every 1 m3 rise in PM2.5 exposure (adjusted hazard ratio, 1.03; 95% confidence interval, 1.02-1.05).
The associations between dementia and exposure to nitrogen oxides (HR, 1.05; 95% CI, 0.99-1.13), nitrogen dioxide (HR, 1.03; 95% CI, 1.00-1.07) and ozone (HR, 1.01; 95% CI, 0.91-1.11) did not reach statistical significance. However, the confidence intervals were wide enough that clinical relevance cannot be ruled out, Dr. Martin said.
The study did not examine how or if the duration of PM2.5 exposure affected dementia risk. In addition, the investigators were not able to identify a threshold above which dementia risk begins to rise.
The Environmental Pollution Agency considers average yearly exposures up to 12 mcg/m3 to be safe. The World Health Organization sets that limit lower, at 5 mcg/m3.
Dr. Martin noted that more studies are needed to explore those issues, as well as the mechanisms by which air pollutants contribute to the pathology of dementia. However, the clear link between fine particulate matter exposure and increased risk emphasizes the need to address air pollution as a modifiable risk factor for dementia.
“The rising tide of dementia is not something we can easily reverse,” Dr. Martin said. “The evidence has been so elusive for how to treat dementia once you have it, so our biggest opportunity is to prevent it.”
Results from a study published earlier in 2022 estimated that rates of dementia will triple worldwide and double in the United States by 2050 unless steps are taking to mitigate risk factors.
Research also suggests that improving air quality PM2.5 by just 10% results in a 14% decreased risk for dementia.
‘Impressive’ pattern
Paul Rosenberg, MD, codirector of the Memory and Alzheimer’s Treatment Center division of geriatric psychiatry at Johns Hopkins University, Baltimore, said that air pollution “is the most prominent environmental risk we’ve found” for dementia. It also “adds to many other lifestyle and comorbidity risks, such as lack of exercise, obesity, depression, hearing loss, etc,” said Dr. Rosenberg, who was not involved with the research.
He noted what was “most impressive” was that in most of the pooled studies, small particulate air pollution was associated with dementia. “The overall pattern is most impressive and the effect sizes quite consistent over most of the studies,” Dr. Rosenberg said.
The meta-analysis was unfunded. Dr. Martin and Dr. Rosenberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Is opioid abuse leading to pediatric head trauma?
As a physician in the heart of the opioid epidemic, Pavirthra R. Ellison, MD, has watched for years as her patients have lost parents to overdoses. More than 1,400 adults in West Virginia, where she practices, died of opioid abuse in 2021 alone, government statistics show.
The grim toll made Ellison wonder: What was happening to children in the state? The answer, according to a new study, is not reassuring.
Ellison and her colleagues have found a troubling link between a surge in critical head and neck injuries among youth in West Virginia and a spike in positive tests for opioids and benzodiazepines among children who arrive at emergency departments in the state. They don’t think the pattern is a coincidence.
“What we found was really kind of scary,” said Dr. Ellison, a professor of anesthesiology and pediatrics at West Virginia University, Morgantown. “Children in this region often get exposure to these drugs early on.”
A region in crisis
According to a 2020 report from the Department of Health & Human Services, about 9.9 million Americans abused prescription opioids in 2018. That same year, almost 47,000 died following an overdose of the painkillers. In 2017, Appalachian counties experienced a death rate from opioid overdoses that was 72% higher than that of the rest of the country.
Dr. Ellison and associates who presented their findings recently at the 2022 annual meeting of the American Society of Anesthesiologists, examined rates of pediatric trauma injuries, injury severity, and results of drug screenings throughout West Virginia between 2009 and 2019.
The study included 4,538 children and adolescents younger than 18 years who had been treated for head and neck trauma. The youth were divided into two groups: 3,356 who were treated from 2009 to 2016, and 1,182 who were treated between 2017 and 2019.
The incidence of critical head injuries increased from 3.7% in the period 2009-2016 to 7.2% in the period 2017-2019 (P = .007). The incidence of serious neck injuries increased from 12.2% to 27.1% (P = .007) during that period, according to the researchers. The number of days that these patients spent on ventilators more than doubled, from 3.1 to 6.3 (P < .001), they reported.
At the same time, the rate of positive urine drug tests rose sharply, from 0.8% to 1.8% (P < .001) for benzodiazepines and from 1% to 4.9% for opioids (P < .001).
Drug testing of children hospitalized for trauma rose more than threefold, from 6.9% to 23.2% (P < .001). Dr. Ellison’s group was unable to match positive drug screens with patients who came in with injuries.
Dr. Ellison said her research “warrants further evaluation of current policies and protocols targeting substance use in children and adolescents.” To that end, her team is planning to conduct a prospective study in mid 2023 to further illuminate the trends.
“I hope early next year we can put together a group of physicians, pediatric general surgeons, neurosurgeons, and anesthesiologists,” she said. “I want to look at what we can do to reduce the severity of injury.”
She also wants to reach the population that these findings directly affect.
“The next step that we are currently working on is community awareness of the issue,” Dr. Ellison said. “Our trauma institute is partnering with middle school and high school kids to create material to raise awareness.”
Rural Appalachia faces several other endemic problems that affect the health and well-being of children and families, including limited access to health care, poverty, and minimal community support, according to Dr. Ellison. Children and teens in the region who live with parents who abuse opioids are more likely to experience family conflict, mental health challenges, legal troubles, and negative health effects, including physical trauma.
A call to action
Toufic Jildeh, MD, assistant professor of orthopedics, Michigan State University Health Care, East Lansing, who has studied ways to reduce opioid use among surgery patients, called the new findings “alarming.”
After reviewing the study, Dr. Jildeh said that in his opinion, the results support standardized drug testing of children, particularly in the context of severe trauma.
Bruce Bassi, MD, an addiction psychiatrist and owner of TelepsychHealth, a private, online psychiatric practice, agreed. “The main take-home message is that drug screening should be the standard of care for pediatric patients in this region, because it changes the management of those individuals,” Dr. Bassi said.
But identifying these patients is just the first step. “We should continue to educate and raise awareness, not only in the health care system,” Dr. Bassi said. “We also need to let parents know that the possibility of children obtaining access to medications is high.”
The study was independently supported. Dr. Ellison and Dr. Jildeh reported no relevant financial relationships. Dr. Bassi owns a private psychiatry practice called Telepsychhealth but has no other relevant financial relationships.
A version of this article first appeared on Medscape.com.
As a physician in the heart of the opioid epidemic, Pavirthra R. Ellison, MD, has watched for years as her patients have lost parents to overdoses. More than 1,400 adults in West Virginia, where she practices, died of opioid abuse in 2021 alone, government statistics show.
The grim toll made Ellison wonder: What was happening to children in the state? The answer, according to a new study, is not reassuring.
Ellison and her colleagues have found a troubling link between a surge in critical head and neck injuries among youth in West Virginia and a spike in positive tests for opioids and benzodiazepines among children who arrive at emergency departments in the state. They don’t think the pattern is a coincidence.
“What we found was really kind of scary,” said Dr. Ellison, a professor of anesthesiology and pediatrics at West Virginia University, Morgantown. “Children in this region often get exposure to these drugs early on.”
A region in crisis
According to a 2020 report from the Department of Health & Human Services, about 9.9 million Americans abused prescription opioids in 2018. That same year, almost 47,000 died following an overdose of the painkillers. In 2017, Appalachian counties experienced a death rate from opioid overdoses that was 72% higher than that of the rest of the country.
Dr. Ellison and associates who presented their findings recently at the 2022 annual meeting of the American Society of Anesthesiologists, examined rates of pediatric trauma injuries, injury severity, and results of drug screenings throughout West Virginia between 2009 and 2019.
The study included 4,538 children and adolescents younger than 18 years who had been treated for head and neck trauma. The youth were divided into two groups: 3,356 who were treated from 2009 to 2016, and 1,182 who were treated between 2017 and 2019.
The incidence of critical head injuries increased from 3.7% in the period 2009-2016 to 7.2% in the period 2017-2019 (P = .007). The incidence of serious neck injuries increased from 12.2% to 27.1% (P = .007) during that period, according to the researchers. The number of days that these patients spent on ventilators more than doubled, from 3.1 to 6.3 (P < .001), they reported.
At the same time, the rate of positive urine drug tests rose sharply, from 0.8% to 1.8% (P < .001) for benzodiazepines and from 1% to 4.9% for opioids (P < .001).
Drug testing of children hospitalized for trauma rose more than threefold, from 6.9% to 23.2% (P < .001). Dr. Ellison’s group was unable to match positive drug screens with patients who came in with injuries.
Dr. Ellison said her research “warrants further evaluation of current policies and protocols targeting substance use in children and adolescents.” To that end, her team is planning to conduct a prospective study in mid 2023 to further illuminate the trends.
“I hope early next year we can put together a group of physicians, pediatric general surgeons, neurosurgeons, and anesthesiologists,” she said. “I want to look at what we can do to reduce the severity of injury.”
She also wants to reach the population that these findings directly affect.
“The next step that we are currently working on is community awareness of the issue,” Dr. Ellison said. “Our trauma institute is partnering with middle school and high school kids to create material to raise awareness.”
Rural Appalachia faces several other endemic problems that affect the health and well-being of children and families, including limited access to health care, poverty, and minimal community support, according to Dr. Ellison. Children and teens in the region who live with parents who abuse opioids are more likely to experience family conflict, mental health challenges, legal troubles, and negative health effects, including physical trauma.
A call to action
Toufic Jildeh, MD, assistant professor of orthopedics, Michigan State University Health Care, East Lansing, who has studied ways to reduce opioid use among surgery patients, called the new findings “alarming.”
After reviewing the study, Dr. Jildeh said that in his opinion, the results support standardized drug testing of children, particularly in the context of severe trauma.
Bruce Bassi, MD, an addiction psychiatrist and owner of TelepsychHealth, a private, online psychiatric practice, agreed. “The main take-home message is that drug screening should be the standard of care for pediatric patients in this region, because it changes the management of those individuals,” Dr. Bassi said.
But identifying these patients is just the first step. “We should continue to educate and raise awareness, not only in the health care system,” Dr. Bassi said. “We also need to let parents know that the possibility of children obtaining access to medications is high.”
The study was independently supported. Dr. Ellison and Dr. Jildeh reported no relevant financial relationships. Dr. Bassi owns a private psychiatry practice called Telepsychhealth but has no other relevant financial relationships.
A version of this article first appeared on Medscape.com.
As a physician in the heart of the opioid epidemic, Pavirthra R. Ellison, MD, has watched for years as her patients have lost parents to overdoses. More than 1,400 adults in West Virginia, where she practices, died of opioid abuse in 2021 alone, government statistics show.
The grim toll made Ellison wonder: What was happening to children in the state? The answer, according to a new study, is not reassuring.
Ellison and her colleagues have found a troubling link between a surge in critical head and neck injuries among youth in West Virginia and a spike in positive tests for opioids and benzodiazepines among children who arrive at emergency departments in the state. They don’t think the pattern is a coincidence.
“What we found was really kind of scary,” said Dr. Ellison, a professor of anesthesiology and pediatrics at West Virginia University, Morgantown. “Children in this region often get exposure to these drugs early on.”
A region in crisis
According to a 2020 report from the Department of Health & Human Services, about 9.9 million Americans abused prescription opioids in 2018. That same year, almost 47,000 died following an overdose of the painkillers. In 2017, Appalachian counties experienced a death rate from opioid overdoses that was 72% higher than that of the rest of the country.
Dr. Ellison and associates who presented their findings recently at the 2022 annual meeting of the American Society of Anesthesiologists, examined rates of pediatric trauma injuries, injury severity, and results of drug screenings throughout West Virginia between 2009 and 2019.
The study included 4,538 children and adolescents younger than 18 years who had been treated for head and neck trauma. The youth were divided into two groups: 3,356 who were treated from 2009 to 2016, and 1,182 who were treated between 2017 and 2019.
The incidence of critical head injuries increased from 3.7% in the period 2009-2016 to 7.2% in the period 2017-2019 (P = .007). The incidence of serious neck injuries increased from 12.2% to 27.1% (P = .007) during that period, according to the researchers. The number of days that these patients spent on ventilators more than doubled, from 3.1 to 6.3 (P < .001), they reported.
At the same time, the rate of positive urine drug tests rose sharply, from 0.8% to 1.8% (P < .001) for benzodiazepines and from 1% to 4.9% for opioids (P < .001).
Drug testing of children hospitalized for trauma rose more than threefold, from 6.9% to 23.2% (P < .001). Dr. Ellison’s group was unable to match positive drug screens with patients who came in with injuries.
Dr. Ellison said her research “warrants further evaluation of current policies and protocols targeting substance use in children and adolescents.” To that end, her team is planning to conduct a prospective study in mid 2023 to further illuminate the trends.
“I hope early next year we can put together a group of physicians, pediatric general surgeons, neurosurgeons, and anesthesiologists,” she said. “I want to look at what we can do to reduce the severity of injury.”
She also wants to reach the population that these findings directly affect.
“The next step that we are currently working on is community awareness of the issue,” Dr. Ellison said. “Our trauma institute is partnering with middle school and high school kids to create material to raise awareness.”
Rural Appalachia faces several other endemic problems that affect the health and well-being of children and families, including limited access to health care, poverty, and minimal community support, according to Dr. Ellison. Children and teens in the region who live with parents who abuse opioids are more likely to experience family conflict, mental health challenges, legal troubles, and negative health effects, including physical trauma.
A call to action
Toufic Jildeh, MD, assistant professor of orthopedics, Michigan State University Health Care, East Lansing, who has studied ways to reduce opioid use among surgery patients, called the new findings “alarming.”
After reviewing the study, Dr. Jildeh said that in his opinion, the results support standardized drug testing of children, particularly in the context of severe trauma.
Bruce Bassi, MD, an addiction psychiatrist and owner of TelepsychHealth, a private, online psychiatric practice, agreed. “The main take-home message is that drug screening should be the standard of care for pediatric patients in this region, because it changes the management of those individuals,” Dr. Bassi said.
But identifying these patients is just the first step. “We should continue to educate and raise awareness, not only in the health care system,” Dr. Bassi said. “We also need to let parents know that the possibility of children obtaining access to medications is high.”
The study was independently supported. Dr. Ellison and Dr. Jildeh reported no relevant financial relationships. Dr. Bassi owns a private psychiatry practice called Telepsychhealth but has no other relevant financial relationships.
A version of this article first appeared on Medscape.com.
Challenges and Considerations in Treating Negative and Cognitive Symptoms of Schizophrenia Spectrum Disorders
Schizophrenia spectrum disorders (SSDs) represent some of the most debilitating mental health disorders.1 While these disorders have myriad presentations, the prototypical patient with SSD is often thought to possess positive symptoms. More recently, clinicians and researchers are raising awareness of another presentation of SSD: predominantly negative and cognitive symptoms. This symptom profile is not a novel phenomenon; for many years this presentation was recognized as a “deficit” presentation, referring to negative symptoms as the prominent feature.2,3 However, it presents unique diagnostic and treatment considerations that are often underappreciated in clinical settings.
Negative symptoms (blunted/flat affect, avolition, alogia, anhedonia, asociality) have long been identified as key features of SSD and are widely recognized as predictive of poor prognostic outcomes for patients with SSDs.1 In many patients, negative symptoms may precede the development of positive symptoms and emerge as a more robust predictor of functional outcomes than positive symptoms.1 Negative symptoms also appear to be inextricably linked to cognitive symptoms. Specifically, patients with primary negative symptoms seem to perform poorly on measures of global cognitive functioning.1 Similar to negative symptoms, cognitive symptoms of SSDs are a primary source of functional impairment and persistent disability.1 Despite this, little attention is given in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) to the neurocognitive and social cognitive deficits seen in patients with SSDs. Previous research highlights broad deficits in a range of neurocognitive abilities, including attention, working memory, processing speed, executive functioning, learning and memory, and receptive and expressive language.4 Similarly, patients also display deficits in domains of social cognition, such as emotion processing, identifying and utilizing social cues, evaluating attributions of others, and perspective-taking.5
A predominantly negative and cognitive symptom presentation can present diagnostic and treatment challenges. We present a case of a patient with such a presentation and the unique considerations given to diagnostic clarification and her treatment.
Case Presentation
A 33-year-old female veteran presented to the emergency department (ED) at the Michael E. DeBakey Veterans Affairs Medical Center (MEDVAMC) in Houston, Texas, in 2020. She was brought to the ED by local police following an attempted assault of her neighbor. Per collateral information from the police, the veteran stated she “had the urge to hurt someone” but was unable to provide any other information about this event. The veteran demonstrated diminished speech output, providing 2- to 3-word responses before refusing to speak entirely. She also presented with markedly blunted affect and tangential speech. She was not oriented to situation, stating confusion as to how she was brought to the hospital, and appeared to be responding to internal stimuli. She was subsequently admitted to the inpatient mental health unit due to unspecified psychosis.
The veteran presented as an unreliable historian, and much of her medical history was obtained via a review of US Department of Defense (DoD) records and collateral interview with her parents. Before her hospitalization, the veteran had been diagnosed with major depressive disorder (MDD) and adjustment disorder while serving in the Navy. Her psychiatric history before her military career was otherwise unremarkable. At that time, she began a trial of sertraline 50 mg and completed 10 sessions of psychotherapy. After approximately 1 year, she elected to stop taking sertraline due to improved mental health. However, shortly after this she began experiencing significant depressive symptoms and was ultimately released early from the Navy due to her mental health concerns.
The veteran’s parents provided interim history between her discharge and establishing care at MEDVAMC as the veteran was reluctant to discuss this period of her life. According to her parents the veteran had prior diagnoses of borderline personality disorder and MDD and had difficulty adhering to her current medications (bupropion and duloxetine) for about 1 month before her hospitalization. During the previous month, her parents observed her staying in her room around the clock and “[going] mute.”
The veteran remained hospitalized for about 1 month, during which she was diagnosed with schizoaffective disorder and stabilized on injections of long-acting olanzapine 210 mg (administered every 2 weeks). She was referred for outpatient psychotherapy in a specialty clinic for veterans with SSDs. However, she did not attend her initial intake assessment.
About 2 weeks after discharge from the hospital, the veteran presented for her injection appointment. At this time, she was noted to be disorganized in her thinking and behavior, displaying thought blocking and catatonic behavior. Her parents also described concerning behavior since her discharge. They stated she went to a hotel after her discharge and spent all her available money. She then returned to her parents’ home, where she did not sleep or bathe for several days. She was observed wandering around the house aimlessly and in a confused manner and had become verbally aggressive and threatening toward her parents. The veteran was again psychiatrically admitted due to psychosis and concerns for her safety. She was discharged about 2 weeks later and continued olanzapine injections. She was also referred for outpatient psychotherapy; although she did not initially engage in psychotherapy, she was referred again about 5 months after discharge and began psychotherapy at that time.
The veteran began a course of weekly outpatient psychotherapy employing cognitive behavior therapy for psychosis (CBTp).6 During this time, she described her primary concerns as anxiety and feeling disconnected from others. She reported a history of depression but not of schizoaffective disorder. When asked about this, the veteran stated that she did not feel this diagnosis was accurate and instead believed she had severe depression. When asked why she was prescribed olanzapine, the veteran stated that this medication was for depression. As with her inpatient stays, the veteran demonstrated several negative symptoms during her course of psychotherapy. She presented with noticeably blunted affect, evidenced by lack of facial expression and monotonic speech. She also routinely displayed alogia (ie, lack of speech), often stating that she “did not feel like talking much.” She described difficulty finding motivation to initiate tasks (avolition) as well as a tendency toward social isolation (asociality).
The veteran also described concerns related to neurocognitive and social cognitive symptoms. She reported difficulties in processing speed, cognitive set-shifting (mentally switching between tasks), and inhibition, describing how these concerns interfered with her occupational functioning. She noted difficulty maintaining the expected pace of work at her previous positions, stating that she felt it took her longer to complete tasks compared with others. In addition, she displayed some difficulties with attention and memory. On more than one occasion, she seemed to have forgotten the previous day’s conversations with clinicians. Regarding social cognitive symptoms, she noted difficulties in emotion processing, indicating that it was difficult for her to identify and manage her emotions. This was especially prominent during times of depressed mood.
She also displayed a hostile attribution bias, or tendency to overattribute hostile intent to others’ ambiguous actions. For example, she described an instance where a family member sat too close to her on the couch, stating that she felt this behavior indicated the family member did not care about her. Relatedly, the veteran demonstrated difficulty with perspective taking, which became evident during cognitive restructuring regarding interpretations of her family’s behavior. Finally, the veteran displayed some deficits in social perception, or the ability to identify social context and rules based on nonverbal communication, verbal cues, and vocal intonation. She stated that she often felt conversing with others was difficult for her and indicated that she was “not good at conversations.” This may have in part been due to deficits in social perception.
During the first 2 months of psychotherapy, the veteran regularly attended sessions (conducted over telephone due to the COVID-19 pandemic) and was adherent to twice-weekly olanzapine injections. Despite this, she began experiencing an increase in depressive symptoms accompanied by a noticeable worsening of her blunted affect, alogia, and avolition. After about 2 months of psychotherapy, she described active suicidal ideation and requested to be voluntarily hospitalized. During this hospitalization, the veteran was consulted about the use of clozapine in treatment-refractory conditions and began a trial of clozapine 400 mg. She demonstrated marked improvement in her depressed mood after taking the medication and was discharged about 2 weeks after admission. The veteran completed 10 sessions of CBTp before electing to terminate due to an upcoming move. She was adherent to weekly blood draws per the requirements of clozapine and described intentions to engage in mental health care after her move. The patient’s mother contacted the clinic to inform the treatment team that the patient and her family had moved to a different city and the patient had started receiving care at the VAMC in that city.
Discussion
As the veteran’s case highlights, a predominantly negative and cognitive symptom presentation may present diagnostic challenges. Since this presentation may not be viewed as representative of SSDs, patients with this presentation may be misdiagnosed. This was evident in the current case, not only in the veteran’s prodromal phase of illness while in the Navy, but also in her reported previous diagnoses of borderline personality disorder and MDD. More than one clinician at the MEDVAMC provisionally considered a diagnosis of MDD before collecting collateral information from the veteran’s family regarding her clear psychotic symptoms. Unfortunately, such misdiagnoses may have prevented early intervention of the veteran’s schizoaffective disorder, which is found to be instrumental in reducing impairment and disability among patients with SSDs.7,8
These misdiagnoses are understandable given the considerable symptom overlap between SSDs and other mental health disorders. For instance, anhedonia and avolition are 2 key symptoms seen in depressive episodes. Both anhedonia and lack of positive emotion are often seen in posttraumatic stress disorder. Additionally, anxiety disorders may induce a lack of positive emotion, loss of interest in previously enjoyed activities, and lack of motivation secondary to primary symptoms of anxiety. Furthermore, schizoaffective disorder requires the presence of a major mood episode. In the absence of apparent positive symptoms (as is the case for patients with a predominantly negative symptom presentation), schizoaffective disorder may be easily misdiagnosed as a mood disorder.
Patients with predominantly negative or cognitive symptoms may also be less accepting of a diagnosis of SSD. A wealth of research points to the clear stigma of SSDs, with many suggesting that these disorders are among the most stigmatized mental health disorders.9 Therefore, patients with predominantly negative and cognitive symptoms may be more likely to attribute their symptoms to another, less stigmatized mental health disorder. This was seen in the current case, as the veteran repeatedly denied a diagnosis of schizoaffective disorder and instead claimed to have severe depression. This reluctance to accept a diagnosis of an SSD, coupled with the diagnostic ambiguity of negative symptoms, is likely to make it challenging for clinicians to accurately identify patients with a predominantly negative and cognitive symptom presentation of SSDs.
Clinicians working within a team-based setting may be less likely to misdiagnose patients as they can consult others. Diagnostic clarity in the current case was undoubtedly facilitated by the multidisciplinary team involved in the veteran’s care; clinicians involved in her care were able to consult with one another to determine that her symptoms were indicative of an SSD rather than a mood disorder. Mental health professionals in private practice are unlikely to have access to such multidisciplinary specialty services and may be particularly vulnerable to misdiagnoses.
Treatment Considerations
This case also highlights several psychotherapy and psychopharmacology treatment considerations for patients with a predominantly negative and cognitive symptom presentation. The veteran was initially difficult to engage in psychotherapy. Although patients with SSDs often have difficulty engaging in treatment, patients with a predominant negative and cognitive symptom profile may experience more difficulty doing so.10 Previous research suggests that both negative symptoms and cognitive symptoms are inversely related to treatment engagement.11,12
By their very nature, negative symptoms may make it difficult to fully engage in psychotherapy. First, avolition and amotivation likely make it difficult for patients to attend psychotherapy appointments. Furthermore, negative symptoms may make it difficult to emotionally engage with the content of psychotherapy, thus limiting the potential benefits. Cognitive symptoms may also make it more difficult for patients to fully reap the benefits of psychotherapy. Deficits in attention, memory, and abstract reasoning seen in other mental health and medical conditions are associated with poorer treatment outcomes in psychotherapy.13,14 Thus, it may be especially difficult to engage patients with primarily negative and cognitive symptoms of SSDs in psychotherapy. However, given the link between these symptoms and functional impairment, it is even more important to evaluate and address such barriers to treatment.
This case highlights the utility of clozapine in the treatment of SSDs. Many commonly prescribed antipsychotic medications have questionable efficacy in treating negative symptoms, and none of the currently available antipsychotics are approved for this indication.15 In our case, the veteran saw a limited reduction of her negative or cognitive symptoms from her use of olanzapine. However, case reports, naturalistic follow-up, and open-label studies suggest that clozapine may be efficacious in targeting negative symptoms of SSDs.16-19 Previous research also suggests clozapine is more effective than other antipsychotic medications, including olanzapine, quetiapine, and risperidone, in decreasing overall SSD symptoms.20,21 Additionally, there is initial evidence of the efficacy of clozapine in treating cognitive symptoms, suggesting that some areas of cognition may improve in response to this medication.22-24 On the other hand, a recent case study suggests high doses of clozapine may be associated with cognitive impairment, although cognitive impairment was still greater without medication than at this higher dose.25 Thus, further research is needed to refine our understanding of the impact of clozapine on cognitive symptoms in SSDs.
Despite the promising research behind clozapine, it remains widely underprescribed, likely due to concerns regarding the potential adverse effects.26,27 Clozapine has been associated with many adverse effects, the most concerning being neutropenia, which can lead to serious infection and death. Thus, one concern among clinicians may be the potential lethality of clozapine. However, a wealth of research indicates clozapine can be safely administered under medical supervision.26,28 In fact, clozapine has been linked to lower all-cause mortality rates and lower mortality rates by suicide compared with other antipsychotic medications.29-31 It may therefore be argued that clozapine lowers the overall risk of mortality. Prescribers may also be weary of adherence to regular blood tests that patients must undergo to monitor their risk for neutropenia. This is the most frequently cited anticipated barrier to beginning a trial of clozapine.27 These concerns may not be unfounded; indeed, if avolition and amotivation make it difficult to attend psychotherapy sessions, these factors may logically make it difficult to attend blood draw appointments. In response to such barriers, several solutions have been suggested regarding potential blood draw nonadherence, including the use of in-home treatment teams and point-of-care monitoring.32,33
Conclusions
Predominant negative and cognitive symptom presentations of SSDs require unique considerations to accurately identify and provide optimal treatment for patients with such presentations. As our case highlights, patients with such presentations may often be misdiagnosed, as negative and cognitive symptoms may be attributed to other disorders. Additionally, patients with this presentation may experience difficulty engaging in psychotherapy and may not see the same benefits from common antipsychotic medications as patients with predominantly positive symptoms. Clozapine emerges as a promising treatment for addressing negative and cognitive symptoms, although it remains widely underutilized. In cases where clinicians encounter patients with predominantly negative and cognitive symptoms, we strongly recommend consultation and referral to psychiatric care for medication management.
The current case highlights the need for individually tailored treatment plans for individuals seeking mental health care. Clinicians of patients with any mental disorder, but especially those with SSDs of predominantly negative and cognitive symptoms, should carefully formulate a treatment plan based on relevant case history, presentation, and current empirical literature. A singular, one-size-fits-all approach should not be universally implemented for such patients. Our case demonstrates how careful multidisciplinary evaluations, review of medical records, collateral information from patients’ family members, and other diagnostic and treatment considerations in patients with predominant negative and cognitive symptoms of SSDs can refine and enhance the clinical care offered to such patients.
Acknowledgments
A.K. is supported by the US Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Central Texas Veterans Affairs Health Care System, and the VISN 17 Center of Excellence for Research on Returning War Veterans.
1. Kantrowitz JT. Managing negative symptoms of schizophrenia: how far have we come? CNS Drugs. 2017;31(5):373-388. doi:10.1007/s40263-017-0428-x
2. Fenton WS, McGlashan TH. Antecedents, symptom progression, and long-term outcome of the deficit syndrome in schizophrenia. Am J Psychiatry. 1994;151(3):351-356. doi:10.1176/ajp.151.3.351
3. Kirkpatrick B, Buchanan RW, Ross DE, Carpenter WT. A separate disease within the syndrome of schizophrenia. Arch Gen Psychiatry. 2001;58(2):165. doi:10.1001/archpsyc.58.2.165
4. Kalkstein S, Hurford I, Gur RC. Neurocognition in schizophrenia. Curr Top Behav Neurosci. 2010;4:373-390. doi:10.1007/7854_2010_42
5. Green MF, Horan WP. Social cognition in schizophrenia. Curr Dir Psychol Sci. 2010;19(4):243-248. doi:10.1177/0963721410377600
6. Kingdon DG, Turkington D. Cognitive Therapy of Schizophrenia. Guilford Press; 2008.
7. Correll CU, Galling B, Pawar A, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry. 2018;75(6):555. doi:10.1001/jamapsychiatry.2018.0623
8. McGorry PD. Early intervention in psychosis: obvious, effective, overdue. J Nerv Ment Dis. 2015;203(5):310-318. doi:10.1097/NMD.0000000000000284
9. Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry. 2000;177(1):4-7. doi:10.1192/bjp.177.1.4
10. Dixon LB, Holoshitz Y, Nossel I. Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry. 2016;15(1):13-20. doi:10.1002/wps.20306
11. Kukla M, Davis LW, Lysaker PH. Cognitive behavioral therapy and work outcomes: correlates of treatment engagement and full and partial success in schizophrenia. Behav Cogn Psychother. 2014;42(5):577-592. doi:10.1017/S1352465813000428
12. Johansen R, Hestad K, Iversen VC, et al. Cognitive and clinical factors are associated with service engagement in early-phase schizophrenia spectrum disorders. J Nerv Ment Dis. 2011;199(3):176-182. doi:10.1097/NMD.0b013e31820bc2f9
13. Aharonovich E, Hasin DS, Brooks AC, Liu X, Bisaga A, Nunes EV. Cognitive deficits predict low treatment retention in cocaine dependent patients. Drug Alcohol Depend. 2006;81(3):313-322. doi:10.1016/j.drugalcdep.2005.08.003
14. Aarsland D, Taylor JP, Weintraub D. Psychiatric issues in cognitive impairment. Mov Disord. 2014;29(5):651-662. doi:10.1002/mds.25873
15. Leucht S, Cipriani A, Spineli L, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951-962. doi:10.1016/S0140-6736(13)60733-3
16. Khan AH, Zaidi S. Clozapine: Improvement of Negative Symptoms of Schizophrenia. Cureus. 2017;9(12):e1973. Published 2017 Dec 20. doi:10.7759/cureus.1973
17. Brar JS, Chengappa KN, Parepally H, et al. The effects of clozapine on negative symptoms in patients with schizophrenia with minimal positive symptoms. Ann Clin Psychiatry. 1997;9(4):227-234. doi:10.1023/a:1022352326334
18. Llorca PM, Lancon C, Farisse J, Scotto JC. Clozapine and negative symptoms. An open study. Prog Neuropsychopharmacol Biol Psychiatry. 2000;24(3):373-384. doi:10.1016/s0278-5846(99)00105-0
19. Siskind D, McCartney L, Goldschlager R, Kisely S. Clozapine v. first- and second-generation antipsychotics in treatment-refractory schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2016;209(5):385-392. doi:10.1192/bjp.bp.115.177261
20. McEvoy JP, Lieberman JA, Stroup TS, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163(4):600-610. doi:10.1176/appi.ajp.163.4.600
21. Stroup TS, Gerhard T, Crystal S, Huang C, Olfson M. Comparative Effectiveness of Clozapine and Standard Antipsychotic Treatment in Adults With Schizophrenia. Am J Psychiatry. 2016;173(2):166-173. doi:10.1176/appi.ajp.2015.15030332
22. Lee MA, Thompson PA, Meltzer HY. Effects of clozapine in cognitive function in schizophrenia. J Clin Psychiatry. 1994;55(suppl B):82-87.
23. Sharma T, Hughes C, Soni W, Kumari V. Cognitive effects of olanzapine and clozapine treatment in chronic schizophrenia. Psychopharmacology (Berl). 2003;169(3-4):398-403. doi:10.1007/s00213-003-1506-y
24. Spagna A, Dong Y, Mackie MA, et al. Clozapine improves the orienting of attention in schizophrenia. Schizophr Res. 2015;168(1-2):285-291. doi:10.1016/j.schres.2015.08.009
25. Savulich G, Mezquida G, Atkinson S, Bernardo M, Fernandez-Egea E. A case study of clozapine and cognition: friend or foe? J Clin Psychopharmacol. 2018;38(2):152-153. doi:10.1097/JCP.0000000000000847
26. Bogers JPAM, Schulte PFJ, Van Dijk D, Bakker B, Cohen D. Clozapine underutilization in the treatment of schizophrenia: how can clozapine prescription rates be improved? J Clin Psychopharmacol. 2016;36(2):109-111. doi:10.1097/JCP.0000000000000478
27. Kelly DL, Freudenreich O, Sayer MA, Love RC. Addressing Barriers to Clozapine Underutilization: A National Effort. Psychiatr Serv. 2018;69(2):224-227. doi:10.1176/appi.ps.201700162
28. Honigfeld G, Arellano F, Sethi J, Bianchini A, Schein J. Reducing clozapine-related morbidity and mortality: 5 years of experience with the Clozaril National Registry. J Clin Psychiatry. 1998;59(suppl 3):3-7.
29. Cho J, Hayes RD, Jewell A, et al. Clozapine and all-cause mortality in treatment-resistant schizophrenia: a historical cohort study. Acta Psychiatr Scand. 2019;139(3):237-247. doi:10.1111/acps.12989
30. Kane JM. Clozapine Reduces All-Cause Mortality. Am J Psychiatry. 2017;174(10):920-921. doi:10.1176/appi.ajp.2017.17070770
31. Taipale H, Lähteenvuo M, Tanskanen A, Mittendorfer-Rutz E, Tiihonen J. Comparative Effectiveness of Antipsychotics for Risk of Attempted or Completed Suicide Among Persons With Schizophrenia. Schizophr Bull. 2021;47(1):23-30. doi:10.1093/schbul/sbaa111
32. Love RC, Kelly DL, Freudenreich O, Sayer MA. Clozapine underutilization: addressing the barriers. National Association of State Mental Health Program Directors; 2016. Accessed October 6, 2022. https://www.nasmhpd.org/sites/default/files/Assessment%201_Clozapine%20Underutilization.pdf
33. Kelly DL, Ben-Yoav H, Payne GF, et al. Blood draw barriers for treatment with clozapine and development of a point-of-care monitoring device. Clin Schizophr Relat Psychoses. 2018;12(1):23-30. doi:10.3371/CSRP.KEBE.070415
Schizophrenia spectrum disorders (SSDs) represent some of the most debilitating mental health disorders.1 While these disorders have myriad presentations, the prototypical patient with SSD is often thought to possess positive symptoms. More recently, clinicians and researchers are raising awareness of another presentation of SSD: predominantly negative and cognitive symptoms. This symptom profile is not a novel phenomenon; for many years this presentation was recognized as a “deficit” presentation, referring to negative symptoms as the prominent feature.2,3 However, it presents unique diagnostic and treatment considerations that are often underappreciated in clinical settings.
Negative symptoms (blunted/flat affect, avolition, alogia, anhedonia, asociality) have long been identified as key features of SSD and are widely recognized as predictive of poor prognostic outcomes for patients with SSDs.1 In many patients, negative symptoms may precede the development of positive symptoms and emerge as a more robust predictor of functional outcomes than positive symptoms.1 Negative symptoms also appear to be inextricably linked to cognitive symptoms. Specifically, patients with primary negative symptoms seem to perform poorly on measures of global cognitive functioning.1 Similar to negative symptoms, cognitive symptoms of SSDs are a primary source of functional impairment and persistent disability.1 Despite this, little attention is given in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) to the neurocognitive and social cognitive deficits seen in patients with SSDs. Previous research highlights broad deficits in a range of neurocognitive abilities, including attention, working memory, processing speed, executive functioning, learning and memory, and receptive and expressive language.4 Similarly, patients also display deficits in domains of social cognition, such as emotion processing, identifying and utilizing social cues, evaluating attributions of others, and perspective-taking.5
A predominantly negative and cognitive symptom presentation can present diagnostic and treatment challenges. We present a case of a patient with such a presentation and the unique considerations given to diagnostic clarification and her treatment.
Case Presentation
A 33-year-old female veteran presented to the emergency department (ED) at the Michael E. DeBakey Veterans Affairs Medical Center (MEDVAMC) in Houston, Texas, in 2020. She was brought to the ED by local police following an attempted assault of her neighbor. Per collateral information from the police, the veteran stated she “had the urge to hurt someone” but was unable to provide any other information about this event. The veteran demonstrated diminished speech output, providing 2- to 3-word responses before refusing to speak entirely. She also presented with markedly blunted affect and tangential speech. She was not oriented to situation, stating confusion as to how she was brought to the hospital, and appeared to be responding to internal stimuli. She was subsequently admitted to the inpatient mental health unit due to unspecified psychosis.
The veteran presented as an unreliable historian, and much of her medical history was obtained via a review of US Department of Defense (DoD) records and collateral interview with her parents. Before her hospitalization, the veteran had been diagnosed with major depressive disorder (MDD) and adjustment disorder while serving in the Navy. Her psychiatric history before her military career was otherwise unremarkable. At that time, she began a trial of sertraline 50 mg and completed 10 sessions of psychotherapy. After approximately 1 year, she elected to stop taking sertraline due to improved mental health. However, shortly after this she began experiencing significant depressive symptoms and was ultimately released early from the Navy due to her mental health concerns.
The veteran’s parents provided interim history between her discharge and establishing care at MEDVAMC as the veteran was reluctant to discuss this period of her life. According to her parents the veteran had prior diagnoses of borderline personality disorder and MDD and had difficulty adhering to her current medications (bupropion and duloxetine) for about 1 month before her hospitalization. During the previous month, her parents observed her staying in her room around the clock and “[going] mute.”
The veteran remained hospitalized for about 1 month, during which she was diagnosed with schizoaffective disorder and stabilized on injections of long-acting olanzapine 210 mg (administered every 2 weeks). She was referred for outpatient psychotherapy in a specialty clinic for veterans with SSDs. However, she did not attend her initial intake assessment.
About 2 weeks after discharge from the hospital, the veteran presented for her injection appointment. At this time, she was noted to be disorganized in her thinking and behavior, displaying thought blocking and catatonic behavior. Her parents also described concerning behavior since her discharge. They stated she went to a hotel after her discharge and spent all her available money. She then returned to her parents’ home, where she did not sleep or bathe for several days. She was observed wandering around the house aimlessly and in a confused manner and had become verbally aggressive and threatening toward her parents. The veteran was again psychiatrically admitted due to psychosis and concerns for her safety. She was discharged about 2 weeks later and continued olanzapine injections. She was also referred for outpatient psychotherapy; although she did not initially engage in psychotherapy, she was referred again about 5 months after discharge and began psychotherapy at that time.
The veteran began a course of weekly outpatient psychotherapy employing cognitive behavior therapy for psychosis (CBTp).6 During this time, she described her primary concerns as anxiety and feeling disconnected from others. She reported a history of depression but not of schizoaffective disorder. When asked about this, the veteran stated that she did not feel this diagnosis was accurate and instead believed she had severe depression. When asked why she was prescribed olanzapine, the veteran stated that this medication was for depression. As with her inpatient stays, the veteran demonstrated several negative symptoms during her course of psychotherapy. She presented with noticeably blunted affect, evidenced by lack of facial expression and monotonic speech. She also routinely displayed alogia (ie, lack of speech), often stating that she “did not feel like talking much.” She described difficulty finding motivation to initiate tasks (avolition) as well as a tendency toward social isolation (asociality).
The veteran also described concerns related to neurocognitive and social cognitive symptoms. She reported difficulties in processing speed, cognitive set-shifting (mentally switching between tasks), and inhibition, describing how these concerns interfered with her occupational functioning. She noted difficulty maintaining the expected pace of work at her previous positions, stating that she felt it took her longer to complete tasks compared with others. In addition, she displayed some difficulties with attention and memory. On more than one occasion, she seemed to have forgotten the previous day’s conversations with clinicians. Regarding social cognitive symptoms, she noted difficulties in emotion processing, indicating that it was difficult for her to identify and manage her emotions. This was especially prominent during times of depressed mood.
She also displayed a hostile attribution bias, or tendency to overattribute hostile intent to others’ ambiguous actions. For example, she described an instance where a family member sat too close to her on the couch, stating that she felt this behavior indicated the family member did not care about her. Relatedly, the veteran demonstrated difficulty with perspective taking, which became evident during cognitive restructuring regarding interpretations of her family’s behavior. Finally, the veteran displayed some deficits in social perception, or the ability to identify social context and rules based on nonverbal communication, verbal cues, and vocal intonation. She stated that she often felt conversing with others was difficult for her and indicated that she was “not good at conversations.” This may have in part been due to deficits in social perception.
During the first 2 months of psychotherapy, the veteran regularly attended sessions (conducted over telephone due to the COVID-19 pandemic) and was adherent to twice-weekly olanzapine injections. Despite this, she began experiencing an increase in depressive symptoms accompanied by a noticeable worsening of her blunted affect, alogia, and avolition. After about 2 months of psychotherapy, she described active suicidal ideation and requested to be voluntarily hospitalized. During this hospitalization, the veteran was consulted about the use of clozapine in treatment-refractory conditions and began a trial of clozapine 400 mg. She demonstrated marked improvement in her depressed mood after taking the medication and was discharged about 2 weeks after admission. The veteran completed 10 sessions of CBTp before electing to terminate due to an upcoming move. She was adherent to weekly blood draws per the requirements of clozapine and described intentions to engage in mental health care after her move. The patient’s mother contacted the clinic to inform the treatment team that the patient and her family had moved to a different city and the patient had started receiving care at the VAMC in that city.
Discussion
As the veteran’s case highlights, a predominantly negative and cognitive symptom presentation may present diagnostic challenges. Since this presentation may not be viewed as representative of SSDs, patients with this presentation may be misdiagnosed. This was evident in the current case, not only in the veteran’s prodromal phase of illness while in the Navy, but also in her reported previous diagnoses of borderline personality disorder and MDD. More than one clinician at the MEDVAMC provisionally considered a diagnosis of MDD before collecting collateral information from the veteran’s family regarding her clear psychotic symptoms. Unfortunately, such misdiagnoses may have prevented early intervention of the veteran’s schizoaffective disorder, which is found to be instrumental in reducing impairment and disability among patients with SSDs.7,8
These misdiagnoses are understandable given the considerable symptom overlap between SSDs and other mental health disorders. For instance, anhedonia and avolition are 2 key symptoms seen in depressive episodes. Both anhedonia and lack of positive emotion are often seen in posttraumatic stress disorder. Additionally, anxiety disorders may induce a lack of positive emotion, loss of interest in previously enjoyed activities, and lack of motivation secondary to primary symptoms of anxiety. Furthermore, schizoaffective disorder requires the presence of a major mood episode. In the absence of apparent positive symptoms (as is the case for patients with a predominantly negative symptom presentation), schizoaffective disorder may be easily misdiagnosed as a mood disorder.
Patients with predominantly negative or cognitive symptoms may also be less accepting of a diagnosis of SSD. A wealth of research points to the clear stigma of SSDs, with many suggesting that these disorders are among the most stigmatized mental health disorders.9 Therefore, patients with predominantly negative and cognitive symptoms may be more likely to attribute their symptoms to another, less stigmatized mental health disorder. This was seen in the current case, as the veteran repeatedly denied a diagnosis of schizoaffective disorder and instead claimed to have severe depression. This reluctance to accept a diagnosis of an SSD, coupled with the diagnostic ambiguity of negative symptoms, is likely to make it challenging for clinicians to accurately identify patients with a predominantly negative and cognitive symptom presentation of SSDs.
Clinicians working within a team-based setting may be less likely to misdiagnose patients as they can consult others. Diagnostic clarity in the current case was undoubtedly facilitated by the multidisciplinary team involved in the veteran’s care; clinicians involved in her care were able to consult with one another to determine that her symptoms were indicative of an SSD rather than a mood disorder. Mental health professionals in private practice are unlikely to have access to such multidisciplinary specialty services and may be particularly vulnerable to misdiagnoses.
Treatment Considerations
This case also highlights several psychotherapy and psychopharmacology treatment considerations for patients with a predominantly negative and cognitive symptom presentation. The veteran was initially difficult to engage in psychotherapy. Although patients with SSDs often have difficulty engaging in treatment, patients with a predominant negative and cognitive symptom profile may experience more difficulty doing so.10 Previous research suggests that both negative symptoms and cognitive symptoms are inversely related to treatment engagement.11,12
By their very nature, negative symptoms may make it difficult to fully engage in psychotherapy. First, avolition and amotivation likely make it difficult for patients to attend psychotherapy appointments. Furthermore, negative symptoms may make it difficult to emotionally engage with the content of psychotherapy, thus limiting the potential benefits. Cognitive symptoms may also make it more difficult for patients to fully reap the benefits of psychotherapy. Deficits in attention, memory, and abstract reasoning seen in other mental health and medical conditions are associated with poorer treatment outcomes in psychotherapy.13,14 Thus, it may be especially difficult to engage patients with primarily negative and cognitive symptoms of SSDs in psychotherapy. However, given the link between these symptoms and functional impairment, it is even more important to evaluate and address such barriers to treatment.
This case highlights the utility of clozapine in the treatment of SSDs. Many commonly prescribed antipsychotic medications have questionable efficacy in treating negative symptoms, and none of the currently available antipsychotics are approved for this indication.15 In our case, the veteran saw a limited reduction of her negative or cognitive symptoms from her use of olanzapine. However, case reports, naturalistic follow-up, and open-label studies suggest that clozapine may be efficacious in targeting negative symptoms of SSDs.16-19 Previous research also suggests clozapine is more effective than other antipsychotic medications, including olanzapine, quetiapine, and risperidone, in decreasing overall SSD symptoms.20,21 Additionally, there is initial evidence of the efficacy of clozapine in treating cognitive symptoms, suggesting that some areas of cognition may improve in response to this medication.22-24 On the other hand, a recent case study suggests high doses of clozapine may be associated with cognitive impairment, although cognitive impairment was still greater without medication than at this higher dose.25 Thus, further research is needed to refine our understanding of the impact of clozapine on cognitive symptoms in SSDs.
Despite the promising research behind clozapine, it remains widely underprescribed, likely due to concerns regarding the potential adverse effects.26,27 Clozapine has been associated with many adverse effects, the most concerning being neutropenia, which can lead to serious infection and death. Thus, one concern among clinicians may be the potential lethality of clozapine. However, a wealth of research indicates clozapine can be safely administered under medical supervision.26,28 In fact, clozapine has been linked to lower all-cause mortality rates and lower mortality rates by suicide compared with other antipsychotic medications.29-31 It may therefore be argued that clozapine lowers the overall risk of mortality. Prescribers may also be weary of adherence to regular blood tests that patients must undergo to monitor their risk for neutropenia. This is the most frequently cited anticipated barrier to beginning a trial of clozapine.27 These concerns may not be unfounded; indeed, if avolition and amotivation make it difficult to attend psychotherapy sessions, these factors may logically make it difficult to attend blood draw appointments. In response to such barriers, several solutions have been suggested regarding potential blood draw nonadherence, including the use of in-home treatment teams and point-of-care monitoring.32,33
Conclusions
Predominant negative and cognitive symptom presentations of SSDs require unique considerations to accurately identify and provide optimal treatment for patients with such presentations. As our case highlights, patients with such presentations may often be misdiagnosed, as negative and cognitive symptoms may be attributed to other disorders. Additionally, patients with this presentation may experience difficulty engaging in psychotherapy and may not see the same benefits from common antipsychotic medications as patients with predominantly positive symptoms. Clozapine emerges as a promising treatment for addressing negative and cognitive symptoms, although it remains widely underutilized. In cases where clinicians encounter patients with predominantly negative and cognitive symptoms, we strongly recommend consultation and referral to psychiatric care for medication management.
The current case highlights the need for individually tailored treatment plans for individuals seeking mental health care. Clinicians of patients with any mental disorder, but especially those with SSDs of predominantly negative and cognitive symptoms, should carefully formulate a treatment plan based on relevant case history, presentation, and current empirical literature. A singular, one-size-fits-all approach should not be universally implemented for such patients. Our case demonstrates how careful multidisciplinary evaluations, review of medical records, collateral information from patients’ family members, and other diagnostic and treatment considerations in patients with predominant negative and cognitive symptoms of SSDs can refine and enhance the clinical care offered to such patients.
Acknowledgments
A.K. is supported by the US Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Central Texas Veterans Affairs Health Care System, and the VISN 17 Center of Excellence for Research on Returning War Veterans.
Schizophrenia spectrum disorders (SSDs) represent some of the most debilitating mental health disorders.1 While these disorders have myriad presentations, the prototypical patient with SSD is often thought to possess positive symptoms. More recently, clinicians and researchers are raising awareness of another presentation of SSD: predominantly negative and cognitive symptoms. This symptom profile is not a novel phenomenon; for many years this presentation was recognized as a “deficit” presentation, referring to negative symptoms as the prominent feature.2,3 However, it presents unique diagnostic and treatment considerations that are often underappreciated in clinical settings.
Negative symptoms (blunted/flat affect, avolition, alogia, anhedonia, asociality) have long been identified as key features of SSD and are widely recognized as predictive of poor prognostic outcomes for patients with SSDs.1 In many patients, negative symptoms may precede the development of positive symptoms and emerge as a more robust predictor of functional outcomes than positive symptoms.1 Negative symptoms also appear to be inextricably linked to cognitive symptoms. Specifically, patients with primary negative symptoms seem to perform poorly on measures of global cognitive functioning.1 Similar to negative symptoms, cognitive symptoms of SSDs are a primary source of functional impairment and persistent disability.1 Despite this, little attention is given in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) to the neurocognitive and social cognitive deficits seen in patients with SSDs. Previous research highlights broad deficits in a range of neurocognitive abilities, including attention, working memory, processing speed, executive functioning, learning and memory, and receptive and expressive language.4 Similarly, patients also display deficits in domains of social cognition, such as emotion processing, identifying and utilizing social cues, evaluating attributions of others, and perspective-taking.5
A predominantly negative and cognitive symptom presentation can present diagnostic and treatment challenges. We present a case of a patient with such a presentation and the unique considerations given to diagnostic clarification and her treatment.
Case Presentation
A 33-year-old female veteran presented to the emergency department (ED) at the Michael E. DeBakey Veterans Affairs Medical Center (MEDVAMC) in Houston, Texas, in 2020. She was brought to the ED by local police following an attempted assault of her neighbor. Per collateral information from the police, the veteran stated she “had the urge to hurt someone” but was unable to provide any other information about this event. The veteran demonstrated diminished speech output, providing 2- to 3-word responses before refusing to speak entirely. She also presented with markedly blunted affect and tangential speech. She was not oriented to situation, stating confusion as to how she was brought to the hospital, and appeared to be responding to internal stimuli. She was subsequently admitted to the inpatient mental health unit due to unspecified psychosis.
The veteran presented as an unreliable historian, and much of her medical history was obtained via a review of US Department of Defense (DoD) records and collateral interview with her parents. Before her hospitalization, the veteran had been diagnosed with major depressive disorder (MDD) and adjustment disorder while serving in the Navy. Her psychiatric history before her military career was otherwise unremarkable. At that time, she began a trial of sertraline 50 mg and completed 10 sessions of psychotherapy. After approximately 1 year, she elected to stop taking sertraline due to improved mental health. However, shortly after this she began experiencing significant depressive symptoms and was ultimately released early from the Navy due to her mental health concerns.
The veteran’s parents provided interim history between her discharge and establishing care at MEDVAMC as the veteran was reluctant to discuss this period of her life. According to her parents the veteran had prior diagnoses of borderline personality disorder and MDD and had difficulty adhering to her current medications (bupropion and duloxetine) for about 1 month before her hospitalization. During the previous month, her parents observed her staying in her room around the clock and “[going] mute.”
The veteran remained hospitalized for about 1 month, during which she was diagnosed with schizoaffective disorder and stabilized on injections of long-acting olanzapine 210 mg (administered every 2 weeks). She was referred for outpatient psychotherapy in a specialty clinic for veterans with SSDs. However, she did not attend her initial intake assessment.
About 2 weeks after discharge from the hospital, the veteran presented for her injection appointment. At this time, she was noted to be disorganized in her thinking and behavior, displaying thought blocking and catatonic behavior. Her parents also described concerning behavior since her discharge. They stated she went to a hotel after her discharge and spent all her available money. She then returned to her parents’ home, where she did not sleep or bathe for several days. She was observed wandering around the house aimlessly and in a confused manner and had become verbally aggressive and threatening toward her parents. The veteran was again psychiatrically admitted due to psychosis and concerns for her safety. She was discharged about 2 weeks later and continued olanzapine injections. She was also referred for outpatient psychotherapy; although she did not initially engage in psychotherapy, she was referred again about 5 months after discharge and began psychotherapy at that time.
The veteran began a course of weekly outpatient psychotherapy employing cognitive behavior therapy for psychosis (CBTp).6 During this time, she described her primary concerns as anxiety and feeling disconnected from others. She reported a history of depression but not of schizoaffective disorder. When asked about this, the veteran stated that she did not feel this diagnosis was accurate and instead believed she had severe depression. When asked why she was prescribed olanzapine, the veteran stated that this medication was for depression. As with her inpatient stays, the veteran demonstrated several negative symptoms during her course of psychotherapy. She presented with noticeably blunted affect, evidenced by lack of facial expression and monotonic speech. She also routinely displayed alogia (ie, lack of speech), often stating that she “did not feel like talking much.” She described difficulty finding motivation to initiate tasks (avolition) as well as a tendency toward social isolation (asociality).
The veteran also described concerns related to neurocognitive and social cognitive symptoms. She reported difficulties in processing speed, cognitive set-shifting (mentally switching between tasks), and inhibition, describing how these concerns interfered with her occupational functioning. She noted difficulty maintaining the expected pace of work at her previous positions, stating that she felt it took her longer to complete tasks compared with others. In addition, she displayed some difficulties with attention and memory. On more than one occasion, she seemed to have forgotten the previous day’s conversations with clinicians. Regarding social cognitive symptoms, she noted difficulties in emotion processing, indicating that it was difficult for her to identify and manage her emotions. This was especially prominent during times of depressed mood.
She also displayed a hostile attribution bias, or tendency to overattribute hostile intent to others’ ambiguous actions. For example, she described an instance where a family member sat too close to her on the couch, stating that she felt this behavior indicated the family member did not care about her. Relatedly, the veteran demonstrated difficulty with perspective taking, which became evident during cognitive restructuring regarding interpretations of her family’s behavior. Finally, the veteran displayed some deficits in social perception, or the ability to identify social context and rules based on nonverbal communication, verbal cues, and vocal intonation. She stated that she often felt conversing with others was difficult for her and indicated that she was “not good at conversations.” This may have in part been due to deficits in social perception.
During the first 2 months of psychotherapy, the veteran regularly attended sessions (conducted over telephone due to the COVID-19 pandemic) and was adherent to twice-weekly olanzapine injections. Despite this, she began experiencing an increase in depressive symptoms accompanied by a noticeable worsening of her blunted affect, alogia, and avolition. After about 2 months of psychotherapy, she described active suicidal ideation and requested to be voluntarily hospitalized. During this hospitalization, the veteran was consulted about the use of clozapine in treatment-refractory conditions and began a trial of clozapine 400 mg. She demonstrated marked improvement in her depressed mood after taking the medication and was discharged about 2 weeks after admission. The veteran completed 10 sessions of CBTp before electing to terminate due to an upcoming move. She was adherent to weekly blood draws per the requirements of clozapine and described intentions to engage in mental health care after her move. The patient’s mother contacted the clinic to inform the treatment team that the patient and her family had moved to a different city and the patient had started receiving care at the VAMC in that city.
Discussion
As the veteran’s case highlights, a predominantly negative and cognitive symptom presentation may present diagnostic challenges. Since this presentation may not be viewed as representative of SSDs, patients with this presentation may be misdiagnosed. This was evident in the current case, not only in the veteran’s prodromal phase of illness while in the Navy, but also in her reported previous diagnoses of borderline personality disorder and MDD. More than one clinician at the MEDVAMC provisionally considered a diagnosis of MDD before collecting collateral information from the veteran’s family regarding her clear psychotic symptoms. Unfortunately, such misdiagnoses may have prevented early intervention of the veteran’s schizoaffective disorder, which is found to be instrumental in reducing impairment and disability among patients with SSDs.7,8
These misdiagnoses are understandable given the considerable symptom overlap between SSDs and other mental health disorders. For instance, anhedonia and avolition are 2 key symptoms seen in depressive episodes. Both anhedonia and lack of positive emotion are often seen in posttraumatic stress disorder. Additionally, anxiety disorders may induce a lack of positive emotion, loss of interest in previously enjoyed activities, and lack of motivation secondary to primary symptoms of anxiety. Furthermore, schizoaffective disorder requires the presence of a major mood episode. In the absence of apparent positive symptoms (as is the case for patients with a predominantly negative symptom presentation), schizoaffective disorder may be easily misdiagnosed as a mood disorder.
Patients with predominantly negative or cognitive symptoms may also be less accepting of a diagnosis of SSD. A wealth of research points to the clear stigma of SSDs, with many suggesting that these disorders are among the most stigmatized mental health disorders.9 Therefore, patients with predominantly negative and cognitive symptoms may be more likely to attribute their symptoms to another, less stigmatized mental health disorder. This was seen in the current case, as the veteran repeatedly denied a diagnosis of schizoaffective disorder and instead claimed to have severe depression. This reluctance to accept a diagnosis of an SSD, coupled with the diagnostic ambiguity of negative symptoms, is likely to make it challenging for clinicians to accurately identify patients with a predominantly negative and cognitive symptom presentation of SSDs.
Clinicians working within a team-based setting may be less likely to misdiagnose patients as they can consult others. Diagnostic clarity in the current case was undoubtedly facilitated by the multidisciplinary team involved in the veteran’s care; clinicians involved in her care were able to consult with one another to determine that her symptoms were indicative of an SSD rather than a mood disorder. Mental health professionals in private practice are unlikely to have access to such multidisciplinary specialty services and may be particularly vulnerable to misdiagnoses.
Treatment Considerations
This case also highlights several psychotherapy and psychopharmacology treatment considerations for patients with a predominantly negative and cognitive symptom presentation. The veteran was initially difficult to engage in psychotherapy. Although patients with SSDs often have difficulty engaging in treatment, patients with a predominant negative and cognitive symptom profile may experience more difficulty doing so.10 Previous research suggests that both negative symptoms and cognitive symptoms are inversely related to treatment engagement.11,12
By their very nature, negative symptoms may make it difficult to fully engage in psychotherapy. First, avolition and amotivation likely make it difficult for patients to attend psychotherapy appointments. Furthermore, negative symptoms may make it difficult to emotionally engage with the content of psychotherapy, thus limiting the potential benefits. Cognitive symptoms may also make it more difficult for patients to fully reap the benefits of psychotherapy. Deficits in attention, memory, and abstract reasoning seen in other mental health and medical conditions are associated with poorer treatment outcomes in psychotherapy.13,14 Thus, it may be especially difficult to engage patients with primarily negative and cognitive symptoms of SSDs in psychotherapy. However, given the link between these symptoms and functional impairment, it is even more important to evaluate and address such barriers to treatment.
This case highlights the utility of clozapine in the treatment of SSDs. Many commonly prescribed antipsychotic medications have questionable efficacy in treating negative symptoms, and none of the currently available antipsychotics are approved for this indication.15 In our case, the veteran saw a limited reduction of her negative or cognitive symptoms from her use of olanzapine. However, case reports, naturalistic follow-up, and open-label studies suggest that clozapine may be efficacious in targeting negative symptoms of SSDs.16-19 Previous research also suggests clozapine is more effective than other antipsychotic medications, including olanzapine, quetiapine, and risperidone, in decreasing overall SSD symptoms.20,21 Additionally, there is initial evidence of the efficacy of clozapine in treating cognitive symptoms, suggesting that some areas of cognition may improve in response to this medication.22-24 On the other hand, a recent case study suggests high doses of clozapine may be associated with cognitive impairment, although cognitive impairment was still greater without medication than at this higher dose.25 Thus, further research is needed to refine our understanding of the impact of clozapine on cognitive symptoms in SSDs.
Despite the promising research behind clozapine, it remains widely underprescribed, likely due to concerns regarding the potential adverse effects.26,27 Clozapine has been associated with many adverse effects, the most concerning being neutropenia, which can lead to serious infection and death. Thus, one concern among clinicians may be the potential lethality of clozapine. However, a wealth of research indicates clozapine can be safely administered under medical supervision.26,28 In fact, clozapine has been linked to lower all-cause mortality rates and lower mortality rates by suicide compared with other antipsychotic medications.29-31 It may therefore be argued that clozapine lowers the overall risk of mortality. Prescribers may also be weary of adherence to regular blood tests that patients must undergo to monitor their risk for neutropenia. This is the most frequently cited anticipated barrier to beginning a trial of clozapine.27 These concerns may not be unfounded; indeed, if avolition and amotivation make it difficult to attend psychotherapy sessions, these factors may logically make it difficult to attend blood draw appointments. In response to such barriers, several solutions have been suggested regarding potential blood draw nonadherence, including the use of in-home treatment teams and point-of-care monitoring.32,33
Conclusions
Predominant negative and cognitive symptom presentations of SSDs require unique considerations to accurately identify and provide optimal treatment for patients with such presentations. As our case highlights, patients with such presentations may often be misdiagnosed, as negative and cognitive symptoms may be attributed to other disorders. Additionally, patients with this presentation may experience difficulty engaging in psychotherapy and may not see the same benefits from common antipsychotic medications as patients with predominantly positive symptoms. Clozapine emerges as a promising treatment for addressing negative and cognitive symptoms, although it remains widely underutilized. In cases where clinicians encounter patients with predominantly negative and cognitive symptoms, we strongly recommend consultation and referral to psychiatric care for medication management.
The current case highlights the need for individually tailored treatment plans for individuals seeking mental health care. Clinicians of patients with any mental disorder, but especially those with SSDs of predominantly negative and cognitive symptoms, should carefully formulate a treatment plan based on relevant case history, presentation, and current empirical literature. A singular, one-size-fits-all approach should not be universally implemented for such patients. Our case demonstrates how careful multidisciplinary evaluations, review of medical records, collateral information from patients’ family members, and other diagnostic and treatment considerations in patients with predominant negative and cognitive symptoms of SSDs can refine and enhance the clinical care offered to such patients.
Acknowledgments
A.K. is supported by the US Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Central Texas Veterans Affairs Health Care System, and the VISN 17 Center of Excellence for Research on Returning War Veterans.
1. Kantrowitz JT. Managing negative symptoms of schizophrenia: how far have we come? CNS Drugs. 2017;31(5):373-388. doi:10.1007/s40263-017-0428-x
2. Fenton WS, McGlashan TH. Antecedents, symptom progression, and long-term outcome of the deficit syndrome in schizophrenia. Am J Psychiatry. 1994;151(3):351-356. doi:10.1176/ajp.151.3.351
3. Kirkpatrick B, Buchanan RW, Ross DE, Carpenter WT. A separate disease within the syndrome of schizophrenia. Arch Gen Psychiatry. 2001;58(2):165. doi:10.1001/archpsyc.58.2.165
4. Kalkstein S, Hurford I, Gur RC. Neurocognition in schizophrenia. Curr Top Behav Neurosci. 2010;4:373-390. doi:10.1007/7854_2010_42
5. Green MF, Horan WP. Social cognition in schizophrenia. Curr Dir Psychol Sci. 2010;19(4):243-248. doi:10.1177/0963721410377600
6. Kingdon DG, Turkington D. Cognitive Therapy of Schizophrenia. Guilford Press; 2008.
7. Correll CU, Galling B, Pawar A, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry. 2018;75(6):555. doi:10.1001/jamapsychiatry.2018.0623
8. McGorry PD. Early intervention in psychosis: obvious, effective, overdue. J Nerv Ment Dis. 2015;203(5):310-318. doi:10.1097/NMD.0000000000000284
9. Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry. 2000;177(1):4-7. doi:10.1192/bjp.177.1.4
10. Dixon LB, Holoshitz Y, Nossel I. Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry. 2016;15(1):13-20. doi:10.1002/wps.20306
11. Kukla M, Davis LW, Lysaker PH. Cognitive behavioral therapy and work outcomes: correlates of treatment engagement and full and partial success in schizophrenia. Behav Cogn Psychother. 2014;42(5):577-592. doi:10.1017/S1352465813000428
12. Johansen R, Hestad K, Iversen VC, et al. Cognitive and clinical factors are associated with service engagement in early-phase schizophrenia spectrum disorders. J Nerv Ment Dis. 2011;199(3):176-182. doi:10.1097/NMD.0b013e31820bc2f9
13. Aharonovich E, Hasin DS, Brooks AC, Liu X, Bisaga A, Nunes EV. Cognitive deficits predict low treatment retention in cocaine dependent patients. Drug Alcohol Depend. 2006;81(3):313-322. doi:10.1016/j.drugalcdep.2005.08.003
14. Aarsland D, Taylor JP, Weintraub D. Psychiatric issues in cognitive impairment. Mov Disord. 2014;29(5):651-662. doi:10.1002/mds.25873
15. Leucht S, Cipriani A, Spineli L, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951-962. doi:10.1016/S0140-6736(13)60733-3
16. Khan AH, Zaidi S. Clozapine: Improvement of Negative Symptoms of Schizophrenia. Cureus. 2017;9(12):e1973. Published 2017 Dec 20. doi:10.7759/cureus.1973
17. Brar JS, Chengappa KN, Parepally H, et al. The effects of clozapine on negative symptoms in patients with schizophrenia with minimal positive symptoms. Ann Clin Psychiatry. 1997;9(4):227-234. doi:10.1023/a:1022352326334
18. Llorca PM, Lancon C, Farisse J, Scotto JC. Clozapine and negative symptoms. An open study. Prog Neuropsychopharmacol Biol Psychiatry. 2000;24(3):373-384. doi:10.1016/s0278-5846(99)00105-0
19. Siskind D, McCartney L, Goldschlager R, Kisely S. Clozapine v. first- and second-generation antipsychotics in treatment-refractory schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2016;209(5):385-392. doi:10.1192/bjp.bp.115.177261
20. McEvoy JP, Lieberman JA, Stroup TS, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163(4):600-610. doi:10.1176/appi.ajp.163.4.600
21. Stroup TS, Gerhard T, Crystal S, Huang C, Olfson M. Comparative Effectiveness of Clozapine and Standard Antipsychotic Treatment in Adults With Schizophrenia. Am J Psychiatry. 2016;173(2):166-173. doi:10.1176/appi.ajp.2015.15030332
22. Lee MA, Thompson PA, Meltzer HY. Effects of clozapine in cognitive function in schizophrenia. J Clin Psychiatry. 1994;55(suppl B):82-87.
23. Sharma T, Hughes C, Soni W, Kumari V. Cognitive effects of olanzapine and clozapine treatment in chronic schizophrenia. Psychopharmacology (Berl). 2003;169(3-4):398-403. doi:10.1007/s00213-003-1506-y
24. Spagna A, Dong Y, Mackie MA, et al. Clozapine improves the orienting of attention in schizophrenia. Schizophr Res. 2015;168(1-2):285-291. doi:10.1016/j.schres.2015.08.009
25. Savulich G, Mezquida G, Atkinson S, Bernardo M, Fernandez-Egea E. A case study of clozapine and cognition: friend or foe? J Clin Psychopharmacol. 2018;38(2):152-153. doi:10.1097/JCP.0000000000000847
26. Bogers JPAM, Schulte PFJ, Van Dijk D, Bakker B, Cohen D. Clozapine underutilization in the treatment of schizophrenia: how can clozapine prescription rates be improved? J Clin Psychopharmacol. 2016;36(2):109-111. doi:10.1097/JCP.0000000000000478
27. Kelly DL, Freudenreich O, Sayer MA, Love RC. Addressing Barriers to Clozapine Underutilization: A National Effort. Psychiatr Serv. 2018;69(2):224-227. doi:10.1176/appi.ps.201700162
28. Honigfeld G, Arellano F, Sethi J, Bianchini A, Schein J. Reducing clozapine-related morbidity and mortality: 5 years of experience with the Clozaril National Registry. J Clin Psychiatry. 1998;59(suppl 3):3-7.
29. Cho J, Hayes RD, Jewell A, et al. Clozapine and all-cause mortality in treatment-resistant schizophrenia: a historical cohort study. Acta Psychiatr Scand. 2019;139(3):237-247. doi:10.1111/acps.12989
30. Kane JM. Clozapine Reduces All-Cause Mortality. Am J Psychiatry. 2017;174(10):920-921. doi:10.1176/appi.ajp.2017.17070770
31. Taipale H, Lähteenvuo M, Tanskanen A, Mittendorfer-Rutz E, Tiihonen J. Comparative Effectiveness of Antipsychotics for Risk of Attempted or Completed Suicide Among Persons With Schizophrenia. Schizophr Bull. 2021;47(1):23-30. doi:10.1093/schbul/sbaa111
32. Love RC, Kelly DL, Freudenreich O, Sayer MA. Clozapine underutilization: addressing the barriers. National Association of State Mental Health Program Directors; 2016. Accessed October 6, 2022. https://www.nasmhpd.org/sites/default/files/Assessment%201_Clozapine%20Underutilization.pdf
33. Kelly DL, Ben-Yoav H, Payne GF, et al. Blood draw barriers for treatment with clozapine and development of a point-of-care monitoring device. Clin Schizophr Relat Psychoses. 2018;12(1):23-30. doi:10.3371/CSRP.KEBE.070415
1. Kantrowitz JT. Managing negative symptoms of schizophrenia: how far have we come? CNS Drugs. 2017;31(5):373-388. doi:10.1007/s40263-017-0428-x
2. Fenton WS, McGlashan TH. Antecedents, symptom progression, and long-term outcome of the deficit syndrome in schizophrenia. Am J Psychiatry. 1994;151(3):351-356. doi:10.1176/ajp.151.3.351
3. Kirkpatrick B, Buchanan RW, Ross DE, Carpenter WT. A separate disease within the syndrome of schizophrenia. Arch Gen Psychiatry. 2001;58(2):165. doi:10.1001/archpsyc.58.2.165
4. Kalkstein S, Hurford I, Gur RC. Neurocognition in schizophrenia. Curr Top Behav Neurosci. 2010;4:373-390. doi:10.1007/7854_2010_42
5. Green MF, Horan WP. Social cognition in schizophrenia. Curr Dir Psychol Sci. 2010;19(4):243-248. doi:10.1177/0963721410377600
6. Kingdon DG, Turkington D. Cognitive Therapy of Schizophrenia. Guilford Press; 2008.
7. Correll CU, Galling B, Pawar A, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry. 2018;75(6):555. doi:10.1001/jamapsychiatry.2018.0623
8. McGorry PD. Early intervention in psychosis: obvious, effective, overdue. J Nerv Ment Dis. 2015;203(5):310-318. doi:10.1097/NMD.0000000000000284
9. Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry. 2000;177(1):4-7. doi:10.1192/bjp.177.1.4
10. Dixon LB, Holoshitz Y, Nossel I. Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry. 2016;15(1):13-20. doi:10.1002/wps.20306
11. Kukla M, Davis LW, Lysaker PH. Cognitive behavioral therapy and work outcomes: correlates of treatment engagement and full and partial success in schizophrenia. Behav Cogn Psychother. 2014;42(5):577-592. doi:10.1017/S1352465813000428
12. Johansen R, Hestad K, Iversen VC, et al. Cognitive and clinical factors are associated with service engagement in early-phase schizophrenia spectrum disorders. J Nerv Ment Dis. 2011;199(3):176-182. doi:10.1097/NMD.0b013e31820bc2f9
13. Aharonovich E, Hasin DS, Brooks AC, Liu X, Bisaga A, Nunes EV. Cognitive deficits predict low treatment retention in cocaine dependent patients. Drug Alcohol Depend. 2006;81(3):313-322. doi:10.1016/j.drugalcdep.2005.08.003
14. Aarsland D, Taylor JP, Weintraub D. Psychiatric issues in cognitive impairment. Mov Disord. 2014;29(5):651-662. doi:10.1002/mds.25873
15. Leucht S, Cipriani A, Spineli L, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951-962. doi:10.1016/S0140-6736(13)60733-3
16. Khan AH, Zaidi S. Clozapine: Improvement of Negative Symptoms of Schizophrenia. Cureus. 2017;9(12):e1973. Published 2017 Dec 20. doi:10.7759/cureus.1973
17. Brar JS, Chengappa KN, Parepally H, et al. The effects of clozapine on negative symptoms in patients with schizophrenia with minimal positive symptoms. Ann Clin Psychiatry. 1997;9(4):227-234. doi:10.1023/a:1022352326334
18. Llorca PM, Lancon C, Farisse J, Scotto JC. Clozapine and negative symptoms. An open study. Prog Neuropsychopharmacol Biol Psychiatry. 2000;24(3):373-384. doi:10.1016/s0278-5846(99)00105-0
19. Siskind D, McCartney L, Goldschlager R, Kisely S. Clozapine v. first- and second-generation antipsychotics in treatment-refractory schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2016;209(5):385-392. doi:10.1192/bjp.bp.115.177261
20. McEvoy JP, Lieberman JA, Stroup TS, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163(4):600-610. doi:10.1176/appi.ajp.163.4.600
21. Stroup TS, Gerhard T, Crystal S, Huang C, Olfson M. Comparative Effectiveness of Clozapine and Standard Antipsychotic Treatment in Adults With Schizophrenia. Am J Psychiatry. 2016;173(2):166-173. doi:10.1176/appi.ajp.2015.15030332
22. Lee MA, Thompson PA, Meltzer HY. Effects of clozapine in cognitive function in schizophrenia. J Clin Psychiatry. 1994;55(suppl B):82-87.
23. Sharma T, Hughes C, Soni W, Kumari V. Cognitive effects of olanzapine and clozapine treatment in chronic schizophrenia. Psychopharmacology (Berl). 2003;169(3-4):398-403. doi:10.1007/s00213-003-1506-y
24. Spagna A, Dong Y, Mackie MA, et al. Clozapine improves the orienting of attention in schizophrenia. Schizophr Res. 2015;168(1-2):285-291. doi:10.1016/j.schres.2015.08.009
25. Savulich G, Mezquida G, Atkinson S, Bernardo M, Fernandez-Egea E. A case study of clozapine and cognition: friend or foe? J Clin Psychopharmacol. 2018;38(2):152-153. doi:10.1097/JCP.0000000000000847
26. Bogers JPAM, Schulte PFJ, Van Dijk D, Bakker B, Cohen D. Clozapine underutilization in the treatment of schizophrenia: how can clozapine prescription rates be improved? J Clin Psychopharmacol. 2016;36(2):109-111. doi:10.1097/JCP.0000000000000478
27. Kelly DL, Freudenreich O, Sayer MA, Love RC. Addressing Barriers to Clozapine Underutilization: A National Effort. Psychiatr Serv. 2018;69(2):224-227. doi:10.1176/appi.ps.201700162
28. Honigfeld G, Arellano F, Sethi J, Bianchini A, Schein J. Reducing clozapine-related morbidity and mortality: 5 years of experience with the Clozaril National Registry. J Clin Psychiatry. 1998;59(suppl 3):3-7.
29. Cho J, Hayes RD, Jewell A, et al. Clozapine and all-cause mortality in treatment-resistant schizophrenia: a historical cohort study. Acta Psychiatr Scand. 2019;139(3):237-247. doi:10.1111/acps.12989
30. Kane JM. Clozapine Reduces All-Cause Mortality. Am J Psychiatry. 2017;174(10):920-921. doi:10.1176/appi.ajp.2017.17070770
31. Taipale H, Lähteenvuo M, Tanskanen A, Mittendorfer-Rutz E, Tiihonen J. Comparative Effectiveness of Antipsychotics for Risk of Attempted or Completed Suicide Among Persons With Schizophrenia. Schizophr Bull. 2021;47(1):23-30. doi:10.1093/schbul/sbaa111
32. Love RC, Kelly DL, Freudenreich O, Sayer MA. Clozapine underutilization: addressing the barriers. National Association of State Mental Health Program Directors; 2016. Accessed October 6, 2022. https://www.nasmhpd.org/sites/default/files/Assessment%201_Clozapine%20Underutilization.pdf
33. Kelly DL, Ben-Yoav H, Payne GF, et al. Blood draw barriers for treatment with clozapine and development of a point-of-care monitoring device. Clin Schizophr Relat Psychoses. 2018;12(1):23-30. doi:10.3371/CSRP.KEBE.070415
Does subclinical hyperthyroidism raise fracture risk?
People with subclinical hyperthyroidism are at 34% greater risk of experiencing a fracture compared with those with normal thyroid function, new research shows.
The finding, from a study of nearly 11,000 middle-aged men and women followed for a median of 2 decades, “highlights a potential role for more aggressive screening and monitoring of patients with subclinical hyperthyroidism to prevent bone mineral disease,” the researchers wrote.
Primary care physicians “should be more aware of the risks for fracture among persons with subclinical hyperthyroidism in the ambulatory setting,” Natalie R. Daya, a PhD student in epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and first author of the study, told this news organization.
Ms. Daya and her colleagues published their findings in JAMA Network Open.
Building on earlier findings
The results agree with previous work, including a meta-analysis of 13 prospective cohort studies of 70,289 primarily White individuals with an average age of 64 years, which found that subclinical hyperthyroidism was associated with a modestly increased risk for fractures, the researchers noted.
“Our study extends these findings to a younger, community-based cohort that included both Black and White participants, included extensive adjustment for potential confounders, and had a longer follow-up period (median follow-up of 21 years vs. 12 years),” they wrote.
The study included 10,946 participants in the Atherosclerosis Risk in Communities Study who were recruited in Washington County, Maryland; Forsyth County, North Carolina; Jackson, Mississippi; and the suburbs of Minneapolis.
Baseline thyroid function was measured in blood samples collected during the second visit, which occurred between 1990 and 1992. No participants in the new analysis took thyroid medications or had a history of hospitalization for fractures at baseline, and all identified as Black or White. The mean age was 57 years, 24% were Black, and 54.3% were female.
Subclinical hyperthyroidism was defined as a thyrotropin level less than 0.56 mIU/L; subclinical hypothyroidism as a thyrotropin level greater than 5.1 mIU/L; and normal thyroid function as a thyrotropin level between 0.56 and 5.1 mIU/L, with normal free thyroxine levels of 0.85-1.4 ng/dL.
The vast majority (93%) of participants had normal thyroid function, 2.6% had subclinical hyperthyroidism, and 4.4% had subclinical hypothyroidism, according to the researchers.
Median follow-up was 21 years. The researchers identified 3,556 incident fractures, detected with hospitalization discharge codes through 2019 and inpatient and Medicare claims data through 2018, for a rate of 167.1 per 10,000 person-years.
Adjusted hazard ratios for fracture were 1.34 (95% confidence interval [CI], 1.09-1.65) for people with subclinical hyperthyroidism and 0.90 (95% CI, 0.77-1.05) for those with subclinical hypothyroidism, compared with those with normal thyroid function.
Most fractures occurred in either the hip (14.1%) or spine (13.8%), according to the researchers.
Limitations included a lack of thyroid function data during the follow-up period and lack of data on bone mineral density, the researchers wrote.
‘An important risk factor’
Endocrinologist Michael McClung, MD, founding and emeritus director of the Oregon Osteoporosis Center, Portland, who was not involved in the study, pointed out that both subclinical hypothyroidism and subclinical hyperthyroidism have been linked to greater risk for cardiovascular disease as well as fracture.
The new paper underscores that subclinical hyperthyroidism “should be included as an important risk factor” for fracture as well as cardiovascular risk, Dr. McClung said in an interview. In considering whether to treat osteoporosis, subclinical hyperthyroidism “may be enough to tip the balance in favor of pharmacological therapy,” he added.
Thyroid-stimulating hormone (TSH) tests to assess thyroid function are typically ordered only if a patient has symptoms of hyperthyroidism or hypothyroidism, Ms. Daya said. Depending on the cause and severity of a low TSH level, a physician may prescribe methimazole or radioactive iodine therapy to reduce the production of thyroxine, she said.
However, well-designed studies are needed to evaluate whether treatment of subclinical thyroid dysfunction reduces the risk for fracture or cardiovascular problems and assess downsides such as side effects, costs, and psychological harm, Dr. McClung noted.
The U.S. Preventive Services Task Force concluded in 2015 that the data were insufficient to recommend screening for thyroid dysfunction in adults without symptoms. As of a year ago, no new evidence has emerged to support an update, according to the task force’s website.
“Until those studies are available, selective screening of thyroid function should be considered in all patients undergoing risk assessment for cardiovascular disease or skeletal health,” Dr. McClung said.
The Atherosclerosis Risk in Communities Study has been funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH) and the U.S. Department of Health and Human Services. Ms. Daya and four study authors reported receiving NIH grants during the study period. Dr. McClung reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
People with subclinical hyperthyroidism are at 34% greater risk of experiencing a fracture compared with those with normal thyroid function, new research shows.
The finding, from a study of nearly 11,000 middle-aged men and women followed for a median of 2 decades, “highlights a potential role for more aggressive screening and monitoring of patients with subclinical hyperthyroidism to prevent bone mineral disease,” the researchers wrote.
Primary care physicians “should be more aware of the risks for fracture among persons with subclinical hyperthyroidism in the ambulatory setting,” Natalie R. Daya, a PhD student in epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and first author of the study, told this news organization.
Ms. Daya and her colleagues published their findings in JAMA Network Open.
Building on earlier findings
The results agree with previous work, including a meta-analysis of 13 prospective cohort studies of 70,289 primarily White individuals with an average age of 64 years, which found that subclinical hyperthyroidism was associated with a modestly increased risk for fractures, the researchers noted.
“Our study extends these findings to a younger, community-based cohort that included both Black and White participants, included extensive adjustment for potential confounders, and had a longer follow-up period (median follow-up of 21 years vs. 12 years),” they wrote.
The study included 10,946 participants in the Atherosclerosis Risk in Communities Study who were recruited in Washington County, Maryland; Forsyth County, North Carolina; Jackson, Mississippi; and the suburbs of Minneapolis.
Baseline thyroid function was measured in blood samples collected during the second visit, which occurred between 1990 and 1992. No participants in the new analysis took thyroid medications or had a history of hospitalization for fractures at baseline, and all identified as Black or White. The mean age was 57 years, 24% were Black, and 54.3% were female.
Subclinical hyperthyroidism was defined as a thyrotropin level less than 0.56 mIU/L; subclinical hypothyroidism as a thyrotropin level greater than 5.1 mIU/L; and normal thyroid function as a thyrotropin level between 0.56 and 5.1 mIU/L, with normal free thyroxine levels of 0.85-1.4 ng/dL.
The vast majority (93%) of participants had normal thyroid function, 2.6% had subclinical hyperthyroidism, and 4.4% had subclinical hypothyroidism, according to the researchers.
Median follow-up was 21 years. The researchers identified 3,556 incident fractures, detected with hospitalization discharge codes through 2019 and inpatient and Medicare claims data through 2018, for a rate of 167.1 per 10,000 person-years.
Adjusted hazard ratios for fracture were 1.34 (95% confidence interval [CI], 1.09-1.65) for people with subclinical hyperthyroidism and 0.90 (95% CI, 0.77-1.05) for those with subclinical hypothyroidism, compared with those with normal thyroid function.
Most fractures occurred in either the hip (14.1%) or spine (13.8%), according to the researchers.
Limitations included a lack of thyroid function data during the follow-up period and lack of data on bone mineral density, the researchers wrote.
‘An important risk factor’
Endocrinologist Michael McClung, MD, founding and emeritus director of the Oregon Osteoporosis Center, Portland, who was not involved in the study, pointed out that both subclinical hypothyroidism and subclinical hyperthyroidism have been linked to greater risk for cardiovascular disease as well as fracture.
The new paper underscores that subclinical hyperthyroidism “should be included as an important risk factor” for fracture as well as cardiovascular risk, Dr. McClung said in an interview. In considering whether to treat osteoporosis, subclinical hyperthyroidism “may be enough to tip the balance in favor of pharmacological therapy,” he added.
Thyroid-stimulating hormone (TSH) tests to assess thyroid function are typically ordered only if a patient has symptoms of hyperthyroidism or hypothyroidism, Ms. Daya said. Depending on the cause and severity of a low TSH level, a physician may prescribe methimazole or radioactive iodine therapy to reduce the production of thyroxine, she said.
However, well-designed studies are needed to evaluate whether treatment of subclinical thyroid dysfunction reduces the risk for fracture or cardiovascular problems and assess downsides such as side effects, costs, and psychological harm, Dr. McClung noted.
The U.S. Preventive Services Task Force concluded in 2015 that the data were insufficient to recommend screening for thyroid dysfunction in adults without symptoms. As of a year ago, no new evidence has emerged to support an update, according to the task force’s website.
“Until those studies are available, selective screening of thyroid function should be considered in all patients undergoing risk assessment for cardiovascular disease or skeletal health,” Dr. McClung said.
The Atherosclerosis Risk in Communities Study has been funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH) and the U.S. Department of Health and Human Services. Ms. Daya and four study authors reported receiving NIH grants during the study period. Dr. McClung reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
People with subclinical hyperthyroidism are at 34% greater risk of experiencing a fracture compared with those with normal thyroid function, new research shows.
The finding, from a study of nearly 11,000 middle-aged men and women followed for a median of 2 decades, “highlights a potential role for more aggressive screening and monitoring of patients with subclinical hyperthyroidism to prevent bone mineral disease,” the researchers wrote.
Primary care physicians “should be more aware of the risks for fracture among persons with subclinical hyperthyroidism in the ambulatory setting,” Natalie R. Daya, a PhD student in epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and first author of the study, told this news organization.
Ms. Daya and her colleagues published their findings in JAMA Network Open.
Building on earlier findings
The results agree with previous work, including a meta-analysis of 13 prospective cohort studies of 70,289 primarily White individuals with an average age of 64 years, which found that subclinical hyperthyroidism was associated with a modestly increased risk for fractures, the researchers noted.
“Our study extends these findings to a younger, community-based cohort that included both Black and White participants, included extensive adjustment for potential confounders, and had a longer follow-up period (median follow-up of 21 years vs. 12 years),” they wrote.
The study included 10,946 participants in the Atherosclerosis Risk in Communities Study who were recruited in Washington County, Maryland; Forsyth County, North Carolina; Jackson, Mississippi; and the suburbs of Minneapolis.
Baseline thyroid function was measured in blood samples collected during the second visit, which occurred between 1990 and 1992. No participants in the new analysis took thyroid medications or had a history of hospitalization for fractures at baseline, and all identified as Black or White. The mean age was 57 years, 24% were Black, and 54.3% were female.
Subclinical hyperthyroidism was defined as a thyrotropin level less than 0.56 mIU/L; subclinical hypothyroidism as a thyrotropin level greater than 5.1 mIU/L; and normal thyroid function as a thyrotropin level between 0.56 and 5.1 mIU/L, with normal free thyroxine levels of 0.85-1.4 ng/dL.
The vast majority (93%) of participants had normal thyroid function, 2.6% had subclinical hyperthyroidism, and 4.4% had subclinical hypothyroidism, according to the researchers.
Median follow-up was 21 years. The researchers identified 3,556 incident fractures, detected with hospitalization discharge codes through 2019 and inpatient and Medicare claims data through 2018, for a rate of 167.1 per 10,000 person-years.
Adjusted hazard ratios for fracture were 1.34 (95% confidence interval [CI], 1.09-1.65) for people with subclinical hyperthyroidism and 0.90 (95% CI, 0.77-1.05) for those with subclinical hypothyroidism, compared with those with normal thyroid function.
Most fractures occurred in either the hip (14.1%) or spine (13.8%), according to the researchers.
Limitations included a lack of thyroid function data during the follow-up period and lack of data on bone mineral density, the researchers wrote.
‘An important risk factor’
Endocrinologist Michael McClung, MD, founding and emeritus director of the Oregon Osteoporosis Center, Portland, who was not involved in the study, pointed out that both subclinical hypothyroidism and subclinical hyperthyroidism have been linked to greater risk for cardiovascular disease as well as fracture.
The new paper underscores that subclinical hyperthyroidism “should be included as an important risk factor” for fracture as well as cardiovascular risk, Dr. McClung said in an interview. In considering whether to treat osteoporosis, subclinical hyperthyroidism “may be enough to tip the balance in favor of pharmacological therapy,” he added.
Thyroid-stimulating hormone (TSH) tests to assess thyroid function are typically ordered only if a patient has symptoms of hyperthyroidism or hypothyroidism, Ms. Daya said. Depending on the cause and severity of a low TSH level, a physician may prescribe methimazole or radioactive iodine therapy to reduce the production of thyroxine, she said.
However, well-designed studies are needed to evaluate whether treatment of subclinical thyroid dysfunction reduces the risk for fracture or cardiovascular problems and assess downsides such as side effects, costs, and psychological harm, Dr. McClung noted.
The U.S. Preventive Services Task Force concluded in 2015 that the data were insufficient to recommend screening for thyroid dysfunction in adults without symptoms. As of a year ago, no new evidence has emerged to support an update, according to the task force’s website.
“Until those studies are available, selective screening of thyroid function should be considered in all patients undergoing risk assessment for cardiovascular disease or skeletal health,” Dr. McClung said.
The Atherosclerosis Risk in Communities Study has been funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH) and the U.S. Department of Health and Human Services. Ms. Daya and four study authors reported receiving NIH grants during the study period. Dr. McClung reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Four-drug combo gets BP down in one step: QUARTET-USA
Use of a combination antihypertensive product containing quarter doses of four different drugs could be an effective strategy to get patients to target blood pressures in one step, a new study suggests.
The study, QUARTET-USA, showed a reduction in BP of almost 5 mm Hg more than the comparator of one antihypertensive agent at standard dose over the 12-week follow-up period in patients with mild to moderate hypertension.
The QUARTET-USA study was presented at the American Heart Association scientific sessions by Mark Huffman, MD, professor of medicine at Washington University in St. Louis.
It builds on a previous trial, QUARTET, conducted in Australia, which first showed benefits with this approach.
In the new U.S. study, which was considerably smaller than the Australian trial, the four-drug combination, including candesartan, amlodipine, indapamide, and bisoprolol, led to a –4.8/–4.9 mm Hg greater reduction in BP from baseline to 12 weeks, compared with standard-dose candesartan monotherapy.
Differences in systolic BP were not statistically significant, which is likely because of limited power related to the sample size, Dr. Huffman noted.
Adverse events were more common in the four-drug intervention group, but the rate of discontinuation was higher in the comparator group. No severe adverse events were deemed related to the study drug.
“The direction and magnitude of [the] blood pressure–lowering effect were similar between the previous Australian study and this American study, despite different populations with lower baseline blood pressure in the current study, thus strengthening the case for this new approach,” Dr. Huffman concluded.
“The two studies together show that the approach of using four drugs in quarter doses is more effective in lowering blood pressure than a single standard dose antihypertensive agent and has an acceptable safely profile,” he said in an interview.
He said the four-drug combination could be an effective way of getting patients to target without multiple appointments.
“If you think about how many visits to the doctor’s office it takes to get patients to goal blood pressures, this combination gets patients down to new guideline target levels in one step, whereas in the SPRINT trial it took three or more visits to get down to these levels. And in practice we lose people – they don’t come back,” he said.
Dr. Huffman explained that the rationale for the study was the persistently low hypertension control rate, which demonstrates the need for a new approach.
The previous Australian QUARTET study suggested that ultra–low-dose combination therapy has a favorable balance between blood pressure–lowering effect, tolerability, and adherence.
That study, conducted in 591 patients and reported in 2021, demonstrated a greater BP-lowering effect with a four-drug combination at quarter doses (irbesartan 37.5 mg, amlodipine 1.25 mg, indapamide 0.625 mg, bisoprolol 2.5 mg) at 12 weeks, compared with irbesartan 150 mg daily. Systolic BP was reduced by more than 6.9 mm Hg and diastolic BP by 5.8 mm Hg than full-dose irbesartan alone, both significant differences.
The current study, QUARTET-USA, aimed to see if a similar strategy could produce comparable results in a U.S. population.
The U.S. study included 62 patients from the Access Community Health Network, Chicago, who were either treatment naive with BPs above 140/90 mm Hg, or already taking antihypertensive monotherapy with BPs above 130/85 mm Hg.
The mean systolic BP at baseline was 138 mm Hg and the mean diastolic pressure was 84 mm Hg.
Study participants were mainly from ethnic minorities (90% Hispanic or Black) and over half were from low-income households (annual household income less than $25,000).
They were randomly assigned to daily administration of a four-drug combination at quarter doses (candesartan 2 mg, amlodipine 1.25 mg, indapamide 0.625 mg, bisoprolol 2.5 mg) or a full dose of candesartan 8 mg (the comparator arm).
Amlodipine 5 mg daily could be added on to treatment if BP remained above 130/80 mm Hg at 6 weeks. This occurred in 18% of the study group versus 53% of the comparator group.
Results showed that at 12 weeks the adjusted mean change in systolic BP weeks was –4.8 mm Hg (95% CI,–10.7 to 1.2), and the adjusted mean change in diastolic BP was –4.9 mm Hg (95% CI, –8.6 to –1.1) in the four-drug combination group, compared with the comparator arm.
Average BPs at the end of 12-week study period were 121 mm Hg systolic and 73 mm Hg diastolic in the four-drug intervention group, compared with 124 mm Hg systolic and 77 mm Hg diastolic in the comparator group.
Any adverse events that were possibly related to drug therapy occurred in 25% of the intervention group versus 10% of the comparator group. But adverse events leading to discontinuation occurred in 6.3% of the study group versus 26.7% of patients in the comparator arm.
“New approaches are needed to achieve lower blood pressure targets, especially for patients and communities with a high burden of hypertension and hypertension-related diseases. QUARTET-USA was the first trial of a four-drug, ultra–low-dose, blood pressure–lowering combination therapy in the U.S.,” Dr. Huffman said.
“We showed reductions in blood pressure similar in magnitude to those in the Australian study. It is useful to know that the direction of the effect is similar across varied populations. Now that we have that signal of efficacy and tolerability, we can move to actually getting it into the hands of patients and providers,” he added.
Noting that further studies will be required to attain marketing authorization, Dr. Huffman suggested that a pharmaceutical company would need to complete that process.
“These are promising results for companies who may be interested in partnering,” he said.
‘A more efficient approach’
LaPrincess C. Brewer, MD, assistant professor of medicine at the Mayo Clinic, Rochester, Minn., and discussant of the study, said the QUARTET-USA study suggests the four-drug, low-dose combination shows promise in lowering BP, compared with the standard dose, and while the reduction in systolic BP was not quite significant, it was clinically meaningful.
“Most U.S. adults with hypertension do not have it under control. This is due to unfavorable social and structural determinants of health which limit adherence to antihypertensive medication,” Dr. Brewer noted.
From a patient point of view, the multiple visits needed to attain goals are a burden and there is also the issue of clinical inertia and lack of medication intensification by clinicians, she commented.
“Of patients with uncontrolled hypertension, 40% are taking just one antihypertensive medication, so up-front, low-dose combination therapy is likely a more efficient approach,” she said.
“This study builds the evidence base for the need for tailored interventions that address the social determinants of health and the intentional prioritization of diverse population in clinical trials,” Dr. Brewer concluded.
QUARTET was an investigator-initiated study, Dr. Huffman reported a pending patent for a heart failure polypill. The George Institute for Global Health, Sydney, Australia, where Huffman has a secondary appointment, has a patent, license, and has received investment funding with intent to commercialize fixed-dose combination therapy. Dr. Brewer reported research support from the National Institutes of Health, Centers for Disease Control and Prevention, American Heart Association, and Bristol-Meyers Squibb Foundation.
A version of this article first appeared on Medscape.com.
Use of a combination antihypertensive product containing quarter doses of four different drugs could be an effective strategy to get patients to target blood pressures in one step, a new study suggests.
The study, QUARTET-USA, showed a reduction in BP of almost 5 mm Hg more than the comparator of one antihypertensive agent at standard dose over the 12-week follow-up period in patients with mild to moderate hypertension.
The QUARTET-USA study was presented at the American Heart Association scientific sessions by Mark Huffman, MD, professor of medicine at Washington University in St. Louis.
It builds on a previous trial, QUARTET, conducted in Australia, which first showed benefits with this approach.
In the new U.S. study, which was considerably smaller than the Australian trial, the four-drug combination, including candesartan, amlodipine, indapamide, and bisoprolol, led to a –4.8/–4.9 mm Hg greater reduction in BP from baseline to 12 weeks, compared with standard-dose candesartan monotherapy.
Differences in systolic BP were not statistically significant, which is likely because of limited power related to the sample size, Dr. Huffman noted.
Adverse events were more common in the four-drug intervention group, but the rate of discontinuation was higher in the comparator group. No severe adverse events were deemed related to the study drug.
“The direction and magnitude of [the] blood pressure–lowering effect were similar between the previous Australian study and this American study, despite different populations with lower baseline blood pressure in the current study, thus strengthening the case for this new approach,” Dr. Huffman concluded.
“The two studies together show that the approach of using four drugs in quarter doses is more effective in lowering blood pressure than a single standard dose antihypertensive agent and has an acceptable safely profile,” he said in an interview.
He said the four-drug combination could be an effective way of getting patients to target without multiple appointments.
“If you think about how many visits to the doctor’s office it takes to get patients to goal blood pressures, this combination gets patients down to new guideline target levels in one step, whereas in the SPRINT trial it took three or more visits to get down to these levels. And in practice we lose people – they don’t come back,” he said.
Dr. Huffman explained that the rationale for the study was the persistently low hypertension control rate, which demonstrates the need for a new approach.
The previous Australian QUARTET study suggested that ultra–low-dose combination therapy has a favorable balance between blood pressure–lowering effect, tolerability, and adherence.
That study, conducted in 591 patients and reported in 2021, demonstrated a greater BP-lowering effect with a four-drug combination at quarter doses (irbesartan 37.5 mg, amlodipine 1.25 mg, indapamide 0.625 mg, bisoprolol 2.5 mg) at 12 weeks, compared with irbesartan 150 mg daily. Systolic BP was reduced by more than 6.9 mm Hg and diastolic BP by 5.8 mm Hg than full-dose irbesartan alone, both significant differences.
The current study, QUARTET-USA, aimed to see if a similar strategy could produce comparable results in a U.S. population.
The U.S. study included 62 patients from the Access Community Health Network, Chicago, who were either treatment naive with BPs above 140/90 mm Hg, or already taking antihypertensive monotherapy with BPs above 130/85 mm Hg.
The mean systolic BP at baseline was 138 mm Hg and the mean diastolic pressure was 84 mm Hg.
Study participants were mainly from ethnic minorities (90% Hispanic or Black) and over half were from low-income households (annual household income less than $25,000).
They were randomly assigned to daily administration of a four-drug combination at quarter doses (candesartan 2 mg, amlodipine 1.25 mg, indapamide 0.625 mg, bisoprolol 2.5 mg) or a full dose of candesartan 8 mg (the comparator arm).
Amlodipine 5 mg daily could be added on to treatment if BP remained above 130/80 mm Hg at 6 weeks. This occurred in 18% of the study group versus 53% of the comparator group.
Results showed that at 12 weeks the adjusted mean change in systolic BP weeks was –4.8 mm Hg (95% CI,–10.7 to 1.2), and the adjusted mean change in diastolic BP was –4.9 mm Hg (95% CI, –8.6 to –1.1) in the four-drug combination group, compared with the comparator arm.
Average BPs at the end of 12-week study period were 121 mm Hg systolic and 73 mm Hg diastolic in the four-drug intervention group, compared with 124 mm Hg systolic and 77 mm Hg diastolic in the comparator group.
Any adverse events that were possibly related to drug therapy occurred in 25% of the intervention group versus 10% of the comparator group. But adverse events leading to discontinuation occurred in 6.3% of the study group versus 26.7% of patients in the comparator arm.
“New approaches are needed to achieve lower blood pressure targets, especially for patients and communities with a high burden of hypertension and hypertension-related diseases. QUARTET-USA was the first trial of a four-drug, ultra–low-dose, blood pressure–lowering combination therapy in the U.S.,” Dr. Huffman said.
“We showed reductions in blood pressure similar in magnitude to those in the Australian study. It is useful to know that the direction of the effect is similar across varied populations. Now that we have that signal of efficacy and tolerability, we can move to actually getting it into the hands of patients and providers,” he added.
Noting that further studies will be required to attain marketing authorization, Dr. Huffman suggested that a pharmaceutical company would need to complete that process.
“These are promising results for companies who may be interested in partnering,” he said.
‘A more efficient approach’
LaPrincess C. Brewer, MD, assistant professor of medicine at the Mayo Clinic, Rochester, Minn., and discussant of the study, said the QUARTET-USA study suggests the four-drug, low-dose combination shows promise in lowering BP, compared with the standard dose, and while the reduction in systolic BP was not quite significant, it was clinically meaningful.
“Most U.S. adults with hypertension do not have it under control. This is due to unfavorable social and structural determinants of health which limit adherence to antihypertensive medication,” Dr. Brewer noted.
From a patient point of view, the multiple visits needed to attain goals are a burden and there is also the issue of clinical inertia and lack of medication intensification by clinicians, she commented.
“Of patients with uncontrolled hypertension, 40% are taking just one antihypertensive medication, so up-front, low-dose combination therapy is likely a more efficient approach,” she said.
“This study builds the evidence base for the need for tailored interventions that address the social determinants of health and the intentional prioritization of diverse population in clinical trials,” Dr. Brewer concluded.
QUARTET was an investigator-initiated study, Dr. Huffman reported a pending patent for a heart failure polypill. The George Institute for Global Health, Sydney, Australia, where Huffman has a secondary appointment, has a patent, license, and has received investment funding with intent to commercialize fixed-dose combination therapy. Dr. Brewer reported research support from the National Institutes of Health, Centers for Disease Control and Prevention, American Heart Association, and Bristol-Meyers Squibb Foundation.
A version of this article first appeared on Medscape.com.
Use of a combination antihypertensive product containing quarter doses of four different drugs could be an effective strategy to get patients to target blood pressures in one step, a new study suggests.
The study, QUARTET-USA, showed a reduction in BP of almost 5 mm Hg more than the comparator of one antihypertensive agent at standard dose over the 12-week follow-up period in patients with mild to moderate hypertension.
The QUARTET-USA study was presented at the American Heart Association scientific sessions by Mark Huffman, MD, professor of medicine at Washington University in St. Louis.
It builds on a previous trial, QUARTET, conducted in Australia, which first showed benefits with this approach.
In the new U.S. study, which was considerably smaller than the Australian trial, the four-drug combination, including candesartan, amlodipine, indapamide, and bisoprolol, led to a –4.8/–4.9 mm Hg greater reduction in BP from baseline to 12 weeks, compared with standard-dose candesartan monotherapy.
Differences in systolic BP were not statistically significant, which is likely because of limited power related to the sample size, Dr. Huffman noted.
Adverse events were more common in the four-drug intervention group, but the rate of discontinuation was higher in the comparator group. No severe adverse events were deemed related to the study drug.
“The direction and magnitude of [the] blood pressure–lowering effect were similar between the previous Australian study and this American study, despite different populations with lower baseline blood pressure in the current study, thus strengthening the case for this new approach,” Dr. Huffman concluded.
“The two studies together show that the approach of using four drugs in quarter doses is more effective in lowering blood pressure than a single standard dose antihypertensive agent and has an acceptable safely profile,” he said in an interview.
He said the four-drug combination could be an effective way of getting patients to target without multiple appointments.
“If you think about how many visits to the doctor’s office it takes to get patients to goal blood pressures, this combination gets patients down to new guideline target levels in one step, whereas in the SPRINT trial it took three or more visits to get down to these levels. And in practice we lose people – they don’t come back,” he said.
Dr. Huffman explained that the rationale for the study was the persistently low hypertension control rate, which demonstrates the need for a new approach.
The previous Australian QUARTET study suggested that ultra–low-dose combination therapy has a favorable balance between blood pressure–lowering effect, tolerability, and adherence.
That study, conducted in 591 patients and reported in 2021, demonstrated a greater BP-lowering effect with a four-drug combination at quarter doses (irbesartan 37.5 mg, amlodipine 1.25 mg, indapamide 0.625 mg, bisoprolol 2.5 mg) at 12 weeks, compared with irbesartan 150 mg daily. Systolic BP was reduced by more than 6.9 mm Hg and diastolic BP by 5.8 mm Hg than full-dose irbesartan alone, both significant differences.
The current study, QUARTET-USA, aimed to see if a similar strategy could produce comparable results in a U.S. population.
The U.S. study included 62 patients from the Access Community Health Network, Chicago, who were either treatment naive with BPs above 140/90 mm Hg, or already taking antihypertensive monotherapy with BPs above 130/85 mm Hg.
The mean systolic BP at baseline was 138 mm Hg and the mean diastolic pressure was 84 mm Hg.
Study participants were mainly from ethnic minorities (90% Hispanic or Black) and over half were from low-income households (annual household income less than $25,000).
They were randomly assigned to daily administration of a four-drug combination at quarter doses (candesartan 2 mg, amlodipine 1.25 mg, indapamide 0.625 mg, bisoprolol 2.5 mg) or a full dose of candesartan 8 mg (the comparator arm).
Amlodipine 5 mg daily could be added on to treatment if BP remained above 130/80 mm Hg at 6 weeks. This occurred in 18% of the study group versus 53% of the comparator group.
Results showed that at 12 weeks the adjusted mean change in systolic BP weeks was –4.8 mm Hg (95% CI,–10.7 to 1.2), and the adjusted mean change in diastolic BP was –4.9 mm Hg (95% CI, –8.6 to –1.1) in the four-drug combination group, compared with the comparator arm.
Average BPs at the end of 12-week study period were 121 mm Hg systolic and 73 mm Hg diastolic in the four-drug intervention group, compared with 124 mm Hg systolic and 77 mm Hg diastolic in the comparator group.
Any adverse events that were possibly related to drug therapy occurred in 25% of the intervention group versus 10% of the comparator group. But adverse events leading to discontinuation occurred in 6.3% of the study group versus 26.7% of patients in the comparator arm.
“New approaches are needed to achieve lower blood pressure targets, especially for patients and communities with a high burden of hypertension and hypertension-related diseases. QUARTET-USA was the first trial of a four-drug, ultra–low-dose, blood pressure–lowering combination therapy in the U.S.,” Dr. Huffman said.
“We showed reductions in blood pressure similar in magnitude to those in the Australian study. It is useful to know that the direction of the effect is similar across varied populations. Now that we have that signal of efficacy and tolerability, we can move to actually getting it into the hands of patients and providers,” he added.
Noting that further studies will be required to attain marketing authorization, Dr. Huffman suggested that a pharmaceutical company would need to complete that process.
“These are promising results for companies who may be interested in partnering,” he said.
‘A more efficient approach’
LaPrincess C. Brewer, MD, assistant professor of medicine at the Mayo Clinic, Rochester, Minn., and discussant of the study, said the QUARTET-USA study suggests the four-drug, low-dose combination shows promise in lowering BP, compared with the standard dose, and while the reduction in systolic BP was not quite significant, it was clinically meaningful.
“Most U.S. adults with hypertension do not have it under control. This is due to unfavorable social and structural determinants of health which limit adherence to antihypertensive medication,” Dr. Brewer noted.
From a patient point of view, the multiple visits needed to attain goals are a burden and there is also the issue of clinical inertia and lack of medication intensification by clinicians, she commented.
“Of patients with uncontrolled hypertension, 40% are taking just one antihypertensive medication, so up-front, low-dose combination therapy is likely a more efficient approach,” she said.
“This study builds the evidence base for the need for tailored interventions that address the social determinants of health and the intentional prioritization of diverse population in clinical trials,” Dr. Brewer concluded.
QUARTET was an investigator-initiated study, Dr. Huffman reported a pending patent for a heart failure polypill. The George Institute for Global Health, Sydney, Australia, where Huffman has a secondary appointment, has a patent, license, and has received investment funding with intent to commercialize fixed-dose combination therapy. Dr. Brewer reported research support from the National Institutes of Health, Centers for Disease Control and Prevention, American Heart Association, and Bristol-Meyers Squibb Foundation.
A version of this article first appeared on Medscape.com.
FROM AHA 2022
Physicians react: Climate change and other social issues
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
ACR introduces guideline for integrative interventions in RA
Exercise tops the list of 28 recommendations in a guideline for integrative interventions in patients with rheumatoid arthritis developed by the American College of Rheumatology.
The guideline is specific to RA and presents integrative interventions to accompany treatment with disease-modifying antirheumatic drugs (DMARDs), according to a summary statement issued by the ACR. The summary was approved by the ACR Board of Directors on Oct. 31, and the recommendations are part of a manuscript that will be submitted for publication in both Arthritis & Rheumatology and Arthritis Care & Research.
Consistent engagement in exercise earned the only strong recommendation; the other 27 were conditional. In the exercise category, the authors offered conditional recommendations for aerobic exercise, aquatic exercise, resistance exercise, and mind-body exercise.
Three recommendations focused on diet. Notably, the recommended diet is Mediterranean style. Two other recommendations were specifically against any other formal diet and against the use of dietary supplements. “The conditional recommendation for adhering to a Mediterranean-style diet, but not other formally defined diets, to improve RA-specific outcomes may be surprising to some clinicians,” said Bryant R. England, MD, PhD, of the University of Nebraska Medical Center, Omaha, and one of the guideline’s coprincipal investigators, in a press release. “The voting panel acknowledged, however, that other health indications may exist for alternative diet and dietary supplements, which makes it crucial for clinicians and patients to engage in shared decision-making,” Dr. England said.
Nearly half of the 28 recommendations (13) focused on rehabilitation, but all were conditional. These included comprehensive occupational and physical therapy and hand therapy, as well as the use of splinting, orthoses, compression, bracing, and taping of affected areas. Other conditional recommendations supported the use of joint protection techniques, assistive devices, adaptive equipment, and/or environmental adaptations. The authors also included a conditional recommendation for vocational rehabilitation and work-site evaluations and/or modifications.
A category of additional integrative interventions included recommendations against both electrotherapy and chiropractic care. However, conditional recommendations were positive for acupuncture, massage therapy, and thermal modalities. Conditional recommendations also supported cognitive-behavioral therapy and/or mind-body strategies, and a standardized self-management program.
The guideline was developed by an interprofessional voting panel of 20 individuals with expertise in epidemiology, exercise physiology, GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology, integrative medicine, nursing, nutrition, occupational therapy, physical therapy, rheumatology, and social work, as well as three individuals who have RA. The panel developed questions, conducted a literature review, and used the GRADE approach to rate the certainty of evidence.
“These recommendations are specific to RA management, understanding that other medical indications and general health benefits may exist for many of these interventions,” the authors write in the summary statement.
The range of interventions shows both the importance of an interprofessional team–based approach to RA management and the need to engage patients in shared decision-making, they said.
A version of this article first appeared on Medscape.com.
Exercise tops the list of 28 recommendations in a guideline for integrative interventions in patients with rheumatoid arthritis developed by the American College of Rheumatology.
The guideline is specific to RA and presents integrative interventions to accompany treatment with disease-modifying antirheumatic drugs (DMARDs), according to a summary statement issued by the ACR. The summary was approved by the ACR Board of Directors on Oct. 31, and the recommendations are part of a manuscript that will be submitted for publication in both Arthritis & Rheumatology and Arthritis Care & Research.
Consistent engagement in exercise earned the only strong recommendation; the other 27 were conditional. In the exercise category, the authors offered conditional recommendations for aerobic exercise, aquatic exercise, resistance exercise, and mind-body exercise.
Three recommendations focused on diet. Notably, the recommended diet is Mediterranean style. Two other recommendations were specifically against any other formal diet and against the use of dietary supplements. “The conditional recommendation for adhering to a Mediterranean-style diet, but not other formally defined diets, to improve RA-specific outcomes may be surprising to some clinicians,” said Bryant R. England, MD, PhD, of the University of Nebraska Medical Center, Omaha, and one of the guideline’s coprincipal investigators, in a press release. “The voting panel acknowledged, however, that other health indications may exist for alternative diet and dietary supplements, which makes it crucial for clinicians and patients to engage in shared decision-making,” Dr. England said.
Nearly half of the 28 recommendations (13) focused on rehabilitation, but all were conditional. These included comprehensive occupational and physical therapy and hand therapy, as well as the use of splinting, orthoses, compression, bracing, and taping of affected areas. Other conditional recommendations supported the use of joint protection techniques, assistive devices, adaptive equipment, and/or environmental adaptations. The authors also included a conditional recommendation for vocational rehabilitation and work-site evaluations and/or modifications.
A category of additional integrative interventions included recommendations against both electrotherapy and chiropractic care. However, conditional recommendations were positive for acupuncture, massage therapy, and thermal modalities. Conditional recommendations also supported cognitive-behavioral therapy and/or mind-body strategies, and a standardized self-management program.
The guideline was developed by an interprofessional voting panel of 20 individuals with expertise in epidemiology, exercise physiology, GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology, integrative medicine, nursing, nutrition, occupational therapy, physical therapy, rheumatology, and social work, as well as three individuals who have RA. The panel developed questions, conducted a literature review, and used the GRADE approach to rate the certainty of evidence.
“These recommendations are specific to RA management, understanding that other medical indications and general health benefits may exist for many of these interventions,” the authors write in the summary statement.
The range of interventions shows both the importance of an interprofessional team–based approach to RA management and the need to engage patients in shared decision-making, they said.
A version of this article first appeared on Medscape.com.
Exercise tops the list of 28 recommendations in a guideline for integrative interventions in patients with rheumatoid arthritis developed by the American College of Rheumatology.
The guideline is specific to RA and presents integrative interventions to accompany treatment with disease-modifying antirheumatic drugs (DMARDs), according to a summary statement issued by the ACR. The summary was approved by the ACR Board of Directors on Oct. 31, and the recommendations are part of a manuscript that will be submitted for publication in both Arthritis & Rheumatology and Arthritis Care & Research.
Consistent engagement in exercise earned the only strong recommendation; the other 27 were conditional. In the exercise category, the authors offered conditional recommendations for aerobic exercise, aquatic exercise, resistance exercise, and mind-body exercise.
Three recommendations focused on diet. Notably, the recommended diet is Mediterranean style. Two other recommendations were specifically against any other formal diet and against the use of dietary supplements. “The conditional recommendation for adhering to a Mediterranean-style diet, but not other formally defined diets, to improve RA-specific outcomes may be surprising to some clinicians,” said Bryant R. England, MD, PhD, of the University of Nebraska Medical Center, Omaha, and one of the guideline’s coprincipal investigators, in a press release. “The voting panel acknowledged, however, that other health indications may exist for alternative diet and dietary supplements, which makes it crucial for clinicians and patients to engage in shared decision-making,” Dr. England said.
Nearly half of the 28 recommendations (13) focused on rehabilitation, but all were conditional. These included comprehensive occupational and physical therapy and hand therapy, as well as the use of splinting, orthoses, compression, bracing, and taping of affected areas. Other conditional recommendations supported the use of joint protection techniques, assistive devices, adaptive equipment, and/or environmental adaptations. The authors also included a conditional recommendation for vocational rehabilitation and work-site evaluations and/or modifications.
A category of additional integrative interventions included recommendations against both electrotherapy and chiropractic care. However, conditional recommendations were positive for acupuncture, massage therapy, and thermal modalities. Conditional recommendations also supported cognitive-behavioral therapy and/or mind-body strategies, and a standardized self-management program.
The guideline was developed by an interprofessional voting panel of 20 individuals with expertise in epidemiology, exercise physiology, GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology, integrative medicine, nursing, nutrition, occupational therapy, physical therapy, rheumatology, and social work, as well as three individuals who have RA. The panel developed questions, conducted a literature review, and used the GRADE approach to rate the certainty of evidence.
“These recommendations are specific to RA management, understanding that other medical indications and general health benefits may exist for many of these interventions,” the authors write in the summary statement.
The range of interventions shows both the importance of an interprofessional team–based approach to RA management and the need to engage patients in shared decision-making, they said.
A version of this article first appeared on Medscape.com.
The danger when doctors don’t get mental health help
As medical professionals, you’re continually exposed to overwork, burnout, stressful situations, and challenging ethical decisions. Yet seeking help for mental health care may be last on your to-do list – or completely off your radar.
That’s sad and dangerous, since the American College of Emergency Physicians said 300-400 physicians die by suicide each year, and the stigma keeps 69% of female physicians from seeking mental health care, according to a prepandemic study.
In the 2022 Medscape Physician Suicide Report, 11% of female doctors and 9% of male doctors said they have had thoughts of suicide, and 64% experienced colloquial depression (feeling down, sad, or blue).
What’s more, physicians are typically seen as strong and capable and are often put on a pedestal by loved ones, patients, and the public and thought of as superhuman. No wonder it isn’t easy when you need to take time away to decompress and treat your mental well-being.
“There is a real fear for physicians when it comes to getting mental health care,” said Emil Tsai, MD, PhD, MAS, professor at the department of psychiatry and behavioral sciences at the University of California, Los Angeles, and an internationally reputed scientist in neurosciences and brain disorders.
The fear, said Dr. Tsai, comes from the stigma of mental health issues, potential repercussions to employment, and conceivable medical board suspension or revocation of your medical license.
Dr. Tsai said in an interview that to combat anxiety about “punishment” that many physicians fear when seeking care for their mental health, we must allow physicians to take time away from their day-to-day patient care for respite and treatment without reprisal.
Since the medical profession is high stress and has a high depression and suicide rate, finding solutions is imperative. And physicians must feel supported enough to seek treatment when needed. So how can we normalize seeking mental health care among physicians?
Get honest about stress and burnout
The only way to normalize any behavior is to be open and candid, Dr. Tsai said in an interview. The mental health conversation must occur across the board, not just within the medical profession.
“The greatest thing we can do to try and lift the burden that we place on physicians is to be willing to talk and be honest about the stress that physicians deal with and the importance of everyone feeling free to seek treatment and rest to strengthen their mental health,” said Dr. Tsai.
The more we talk about mental health and its treatment, the more we lessen the stigma, said Dr. Tsai. That could be more employer-employee check-ins, counseling as part of physician wellness, and programs structured so as not to construe a penal system.
“Mental health in the medical profession is a big issue and one that has to be met with the same compassion and care as it should be for any patient. We have annual physical checkups. Why don’t we offer annual mental health checkups for all, physicians included?” asked Dr. Tsai.
Evaluate the workload
Elizabeth Lombardo, PhD, psychologist, coach, and global keynote speaker, thinks that health care employers should reexamine their physicians’ workloads to see if they’re contributing to mental health issues.
The conversation on mental health in the workplace shouldn’t be about whether a certain person can handle stressors that are “normal” for health care settings. Instead, workplace managers in health care institutions should redefine workloads to ensure that physicians aren’t too heavily burdened with responsibilities that can cause overwork, burnout, and mental health problems,” she said.
Lessen the stigma
Even when physicians want to seek help for their psychological struggles, they may be weary of how their colleagues would react if they knew.
Raffaello Antonino, MD, clinical director at Therapy Central in London, said several underlying fears may exist at a physician’s core that prevent them from seeking care – being seen as weak, being judged as unfit to practice medicine, and the notion that “something is wrong with them.”
Dr. Antonino said we need to understand that physicians face challenges of bereavement and trauma derived from losing patients and the inability to save someone’s life. “These issues can easily develop into an accumulation of difficult, unprocessed emotions, later arising in symptoms and signs of PTSD, anxiety, and depression.”
Education is the best way to end this stigma, just like with any form of prejudice and stereotypes. For instance, we know that health care professionals are at risk of developing burnout. So, educating physicians on the symptoms and management of burnout and its consequences and prevention strategies is a must.
“Imagine what could happen if there were regular opportunities to work through the day’s events before signing out from a shift. The idea that individual weekly therapy is the only way to relieve mental distress is false,” said Lori McIsaac Bewsher, MSW, RSW, a trauma therapist and owner of a trauma-focused mental health clinic in New Brunswick.
“There are ways of integrating individual care into our doctor’s offices and hospitals that can be brief, effective, and confidential. The best way to introduce these interventions is early and collectively; no one is immune to the potential impact of exposure to trauma. The earlier these interventions can be accessed, the better the outcomes for everyone,” she said.
Dr. Antonino suggests, perhaps in the future, organizations can have “burnout checks” or mental health wellness checks for physicians akin to how we also have quick examinations for various physical ailments. What if physicians regularly answered a 10-question mental health survey as part of a burnout or trauma prevention strategy?
“Theirs is a profession and an identity which is often linked with a sense of strength, leadership and [benevolent] power: adjectives, which on the surface one might see as incompatible with what instead, unfortunately, and wrongly, may be associated with mental health issues,” said Dr. Antonino.
Keep it private
When it comes to removing the stigma from mental health care and treatment for physicians, privacy is top of mind. There needs to be some form of privacy protection for physicians who seek professional help for mental health reasons. Dr. Lombardo said physicians need to have the choice to keep their mental health journeys private. “Ideally, normalization should mean openly conversing about mental health, but for physicians, it can be a matter of life or death for their career, so the choice to remain private is something that should be afforded to them.”
Along those lines, the American Medical Association is pushing for system changes in legislative and regulatory arenas to support the mental health of practicing physicians, residents, and medical students. The organization is also urging health systems and state medical licensing bodies to remove questions on their applications that ask about prior treatment for mental health conditions.
Among many programs across the country, the Foundation of the Pennsylvania Medical Society has also created a Physicians’ Health Program, which provides confidential assessment, counseling, and referral services for physicians with mental health concerns.
“All of these initiatives are important in helping to destigmatize mental health issues among physicians,” said Harold Hong, MD, a board-certified psychiatrist in Raleigh, N.C.
Hail the benefits of treatment
Dr. Hong said to continue to destigmatize mental health among physicians and normalize its treatment, we not only have to emphasize how attending to mental health has individual benefits but also how it helps us help our patients.
“One key aspect that perhaps underpins this issue is the still present separation between mental and physical health, between mind and body, Dr. Hong said in an interview. “Feeling sad or angry or anxious should become a fact of life, a characteristic of being human, just like catching a cold or breaking a leg.”
It’s a normalization that, perhaps more than anything else, can lead the way for improving physicians’ mental health outcomes while also improving them for the rest of society. When society can finally see the health and well-being of someone in both their psychological and physical status, some of the stigmas may dissipate, and perhaps more physicians’ lives can be saved.
A version of this article first appeared on Medscape.com.
As medical professionals, you’re continually exposed to overwork, burnout, stressful situations, and challenging ethical decisions. Yet seeking help for mental health care may be last on your to-do list – or completely off your radar.
That’s sad and dangerous, since the American College of Emergency Physicians said 300-400 physicians die by suicide each year, and the stigma keeps 69% of female physicians from seeking mental health care, according to a prepandemic study.
In the 2022 Medscape Physician Suicide Report, 11% of female doctors and 9% of male doctors said they have had thoughts of suicide, and 64% experienced colloquial depression (feeling down, sad, or blue).
What’s more, physicians are typically seen as strong and capable and are often put on a pedestal by loved ones, patients, and the public and thought of as superhuman. No wonder it isn’t easy when you need to take time away to decompress and treat your mental well-being.
“There is a real fear for physicians when it comes to getting mental health care,” said Emil Tsai, MD, PhD, MAS, professor at the department of psychiatry and behavioral sciences at the University of California, Los Angeles, and an internationally reputed scientist in neurosciences and brain disorders.
The fear, said Dr. Tsai, comes from the stigma of mental health issues, potential repercussions to employment, and conceivable medical board suspension or revocation of your medical license.
Dr. Tsai said in an interview that to combat anxiety about “punishment” that many physicians fear when seeking care for their mental health, we must allow physicians to take time away from their day-to-day patient care for respite and treatment without reprisal.
Since the medical profession is high stress and has a high depression and suicide rate, finding solutions is imperative. And physicians must feel supported enough to seek treatment when needed. So how can we normalize seeking mental health care among physicians?
Get honest about stress and burnout
The only way to normalize any behavior is to be open and candid, Dr. Tsai said in an interview. The mental health conversation must occur across the board, not just within the medical profession.
“The greatest thing we can do to try and lift the burden that we place on physicians is to be willing to talk and be honest about the stress that physicians deal with and the importance of everyone feeling free to seek treatment and rest to strengthen their mental health,” said Dr. Tsai.
The more we talk about mental health and its treatment, the more we lessen the stigma, said Dr. Tsai. That could be more employer-employee check-ins, counseling as part of physician wellness, and programs structured so as not to construe a penal system.
“Mental health in the medical profession is a big issue and one that has to be met with the same compassion and care as it should be for any patient. We have annual physical checkups. Why don’t we offer annual mental health checkups for all, physicians included?” asked Dr. Tsai.
Evaluate the workload
Elizabeth Lombardo, PhD, psychologist, coach, and global keynote speaker, thinks that health care employers should reexamine their physicians’ workloads to see if they’re contributing to mental health issues.
The conversation on mental health in the workplace shouldn’t be about whether a certain person can handle stressors that are “normal” for health care settings. Instead, workplace managers in health care institutions should redefine workloads to ensure that physicians aren’t too heavily burdened with responsibilities that can cause overwork, burnout, and mental health problems,” she said.
Lessen the stigma
Even when physicians want to seek help for their psychological struggles, they may be weary of how their colleagues would react if they knew.
Raffaello Antonino, MD, clinical director at Therapy Central in London, said several underlying fears may exist at a physician’s core that prevent them from seeking care – being seen as weak, being judged as unfit to practice medicine, and the notion that “something is wrong with them.”
Dr. Antonino said we need to understand that physicians face challenges of bereavement and trauma derived from losing patients and the inability to save someone’s life. “These issues can easily develop into an accumulation of difficult, unprocessed emotions, later arising in symptoms and signs of PTSD, anxiety, and depression.”
Education is the best way to end this stigma, just like with any form of prejudice and stereotypes. For instance, we know that health care professionals are at risk of developing burnout. So, educating physicians on the symptoms and management of burnout and its consequences and prevention strategies is a must.
“Imagine what could happen if there were regular opportunities to work through the day’s events before signing out from a shift. The idea that individual weekly therapy is the only way to relieve mental distress is false,” said Lori McIsaac Bewsher, MSW, RSW, a trauma therapist and owner of a trauma-focused mental health clinic in New Brunswick.
“There are ways of integrating individual care into our doctor’s offices and hospitals that can be brief, effective, and confidential. The best way to introduce these interventions is early and collectively; no one is immune to the potential impact of exposure to trauma. The earlier these interventions can be accessed, the better the outcomes for everyone,” she said.
Dr. Antonino suggests, perhaps in the future, organizations can have “burnout checks” or mental health wellness checks for physicians akin to how we also have quick examinations for various physical ailments. What if physicians regularly answered a 10-question mental health survey as part of a burnout or trauma prevention strategy?
“Theirs is a profession and an identity which is often linked with a sense of strength, leadership and [benevolent] power: adjectives, which on the surface one might see as incompatible with what instead, unfortunately, and wrongly, may be associated with mental health issues,” said Dr. Antonino.
Keep it private
When it comes to removing the stigma from mental health care and treatment for physicians, privacy is top of mind. There needs to be some form of privacy protection for physicians who seek professional help for mental health reasons. Dr. Lombardo said physicians need to have the choice to keep their mental health journeys private. “Ideally, normalization should mean openly conversing about mental health, but for physicians, it can be a matter of life or death for their career, so the choice to remain private is something that should be afforded to them.”
Along those lines, the American Medical Association is pushing for system changes in legislative and regulatory arenas to support the mental health of practicing physicians, residents, and medical students. The organization is also urging health systems and state medical licensing bodies to remove questions on their applications that ask about prior treatment for mental health conditions.
Among many programs across the country, the Foundation of the Pennsylvania Medical Society has also created a Physicians’ Health Program, which provides confidential assessment, counseling, and referral services for physicians with mental health concerns.
“All of these initiatives are important in helping to destigmatize mental health issues among physicians,” said Harold Hong, MD, a board-certified psychiatrist in Raleigh, N.C.
Hail the benefits of treatment
Dr. Hong said to continue to destigmatize mental health among physicians and normalize its treatment, we not only have to emphasize how attending to mental health has individual benefits but also how it helps us help our patients.
“One key aspect that perhaps underpins this issue is the still present separation between mental and physical health, between mind and body, Dr. Hong said in an interview. “Feeling sad or angry or anxious should become a fact of life, a characteristic of being human, just like catching a cold or breaking a leg.”
It’s a normalization that, perhaps more than anything else, can lead the way for improving physicians’ mental health outcomes while also improving them for the rest of society. When society can finally see the health and well-being of someone in both their psychological and physical status, some of the stigmas may dissipate, and perhaps more physicians’ lives can be saved.
A version of this article first appeared on Medscape.com.
As medical professionals, you’re continually exposed to overwork, burnout, stressful situations, and challenging ethical decisions. Yet seeking help for mental health care may be last on your to-do list – or completely off your radar.
That’s sad and dangerous, since the American College of Emergency Physicians said 300-400 physicians die by suicide each year, and the stigma keeps 69% of female physicians from seeking mental health care, according to a prepandemic study.
In the 2022 Medscape Physician Suicide Report, 11% of female doctors and 9% of male doctors said they have had thoughts of suicide, and 64% experienced colloquial depression (feeling down, sad, or blue).
What’s more, physicians are typically seen as strong and capable and are often put on a pedestal by loved ones, patients, and the public and thought of as superhuman. No wonder it isn’t easy when you need to take time away to decompress and treat your mental well-being.
“There is a real fear for physicians when it comes to getting mental health care,” said Emil Tsai, MD, PhD, MAS, professor at the department of psychiatry and behavioral sciences at the University of California, Los Angeles, and an internationally reputed scientist in neurosciences and brain disorders.
The fear, said Dr. Tsai, comes from the stigma of mental health issues, potential repercussions to employment, and conceivable medical board suspension or revocation of your medical license.
Dr. Tsai said in an interview that to combat anxiety about “punishment” that many physicians fear when seeking care for their mental health, we must allow physicians to take time away from their day-to-day patient care for respite and treatment without reprisal.
Since the medical profession is high stress and has a high depression and suicide rate, finding solutions is imperative. And physicians must feel supported enough to seek treatment when needed. So how can we normalize seeking mental health care among physicians?
Get honest about stress and burnout
The only way to normalize any behavior is to be open and candid, Dr. Tsai said in an interview. The mental health conversation must occur across the board, not just within the medical profession.
“The greatest thing we can do to try and lift the burden that we place on physicians is to be willing to talk and be honest about the stress that physicians deal with and the importance of everyone feeling free to seek treatment and rest to strengthen their mental health,” said Dr. Tsai.
The more we talk about mental health and its treatment, the more we lessen the stigma, said Dr. Tsai. That could be more employer-employee check-ins, counseling as part of physician wellness, and programs structured so as not to construe a penal system.
“Mental health in the medical profession is a big issue and one that has to be met with the same compassion and care as it should be for any patient. We have annual physical checkups. Why don’t we offer annual mental health checkups for all, physicians included?” asked Dr. Tsai.
Evaluate the workload
Elizabeth Lombardo, PhD, psychologist, coach, and global keynote speaker, thinks that health care employers should reexamine their physicians’ workloads to see if they’re contributing to mental health issues.
The conversation on mental health in the workplace shouldn’t be about whether a certain person can handle stressors that are “normal” for health care settings. Instead, workplace managers in health care institutions should redefine workloads to ensure that physicians aren’t too heavily burdened with responsibilities that can cause overwork, burnout, and mental health problems,” she said.
Lessen the stigma
Even when physicians want to seek help for their psychological struggles, they may be weary of how their colleagues would react if they knew.
Raffaello Antonino, MD, clinical director at Therapy Central in London, said several underlying fears may exist at a physician’s core that prevent them from seeking care – being seen as weak, being judged as unfit to practice medicine, and the notion that “something is wrong with them.”
Dr. Antonino said we need to understand that physicians face challenges of bereavement and trauma derived from losing patients and the inability to save someone’s life. “These issues can easily develop into an accumulation of difficult, unprocessed emotions, later arising in symptoms and signs of PTSD, anxiety, and depression.”
Education is the best way to end this stigma, just like with any form of prejudice and stereotypes. For instance, we know that health care professionals are at risk of developing burnout. So, educating physicians on the symptoms and management of burnout and its consequences and prevention strategies is a must.
“Imagine what could happen if there were regular opportunities to work through the day’s events before signing out from a shift. The idea that individual weekly therapy is the only way to relieve mental distress is false,” said Lori McIsaac Bewsher, MSW, RSW, a trauma therapist and owner of a trauma-focused mental health clinic in New Brunswick.
“There are ways of integrating individual care into our doctor’s offices and hospitals that can be brief, effective, and confidential. The best way to introduce these interventions is early and collectively; no one is immune to the potential impact of exposure to trauma. The earlier these interventions can be accessed, the better the outcomes for everyone,” she said.
Dr. Antonino suggests, perhaps in the future, organizations can have “burnout checks” or mental health wellness checks for physicians akin to how we also have quick examinations for various physical ailments. What if physicians regularly answered a 10-question mental health survey as part of a burnout or trauma prevention strategy?
“Theirs is a profession and an identity which is often linked with a sense of strength, leadership and [benevolent] power: adjectives, which on the surface one might see as incompatible with what instead, unfortunately, and wrongly, may be associated with mental health issues,” said Dr. Antonino.
Keep it private
When it comes to removing the stigma from mental health care and treatment for physicians, privacy is top of mind. There needs to be some form of privacy protection for physicians who seek professional help for mental health reasons. Dr. Lombardo said physicians need to have the choice to keep their mental health journeys private. “Ideally, normalization should mean openly conversing about mental health, but for physicians, it can be a matter of life or death for their career, so the choice to remain private is something that should be afforded to them.”
Along those lines, the American Medical Association is pushing for system changes in legislative and regulatory arenas to support the mental health of practicing physicians, residents, and medical students. The organization is also urging health systems and state medical licensing bodies to remove questions on their applications that ask about prior treatment for mental health conditions.
Among many programs across the country, the Foundation of the Pennsylvania Medical Society has also created a Physicians’ Health Program, which provides confidential assessment, counseling, and referral services for physicians with mental health concerns.
“All of these initiatives are important in helping to destigmatize mental health issues among physicians,” said Harold Hong, MD, a board-certified psychiatrist in Raleigh, N.C.
Hail the benefits of treatment
Dr. Hong said to continue to destigmatize mental health among physicians and normalize its treatment, we not only have to emphasize how attending to mental health has individual benefits but also how it helps us help our patients.
“One key aspect that perhaps underpins this issue is the still present separation between mental and physical health, between mind and body, Dr. Hong said in an interview. “Feeling sad or angry or anxious should become a fact of life, a characteristic of being human, just like catching a cold or breaking a leg.”
It’s a normalization that, perhaps more than anything else, can lead the way for improving physicians’ mental health outcomes while also improving them for the rest of society. When society can finally see the health and well-being of someone in both their psychological and physical status, some of the stigmas may dissipate, and perhaps more physicians’ lives can be saved.
A version of this article first appeared on Medscape.com.
Med students dismayed that residency match process won’t change
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.