User login
High-quality index colonoscopies pay off down the road for low-risk patients
CHARLOTTE, N.C.– Performing high-quality index colonoscopies may pay off later in your patients’ reduced risk for advanced neoplasia, investigators report.
A study of registry data on more than 2,200 patients who had an index colonoscopy showing no evidence of neoplasia found that, on repeat colonoscopy 10 years later, the absolute risk for advanced neoplasia outcomes was lower for those with a high-quality index exam, compared with those who had a lesser-quality index colonoscopy.
The adjusted odds ratio for patients who underwent high-quality index exams was 0.59%, reported Joseph Anderson, MD, from the Geisel School of Medicine at Dartmouth, Hanover, N.H.
“These data demonstrate that high-quality index colonoscopy provides better protection from interval lesions than low-quality exams with no polyps detected at that index exam,” he said in an oral abstract presentation at the annual meeting of the American College of Gastroenterology.
“These data support the importance of high-quality index exams in the prevention of interval colorectal cancer, and support the 10-year interval for normal exams,” Dr. Anderson added.
He recommended that endoscopists focus on the quality of their exams by using adequate scope withdrawal time – 8-10 minutes – to ensure optimal adenoma detection, and by ensuring the use of optimal bowel preparation in their practices.
Registry study
Dr. Anderson and colleagues studied how the quality of index colonoscopies could affect the risk of advanced outcomes in low-risk patients at the 10-year or later follow-up. They used records from the New Hampshire Colonoscopy Registry, which includes data from 2004 to the present on more than 250,000 exams performed by more than 150 endoscopists in more than 30 Granite State practices.
The investigators also looked at data on patients with less than 5 years of follow-up, and those with follow-up from 5 to less than 10 years.
The study sample included patients with no adenoma or significant serrated polyps on their index exams who had at least one follow-up exam 12 months or more after the index exams. Patients with inflammatory bowel disease or familial colon cancer syndromes were excluded.
They defined a high-quality colonoscopy as an exam complete to cecum, with adequate bowel preparation, and performed by an endoscopist with an adenoma detection rate of 25 or higher.
The adenoma detection rate is calculated as the number of screening colonoscopies with at least one adenoma divided by the total number of screening colonoscopies.
The definition of advanced outcomes included advanced adenomas, colorectal cancer, and/or large serrated polyps (1 cm or greater).
Of the 14,011 patients in the sample, 2,283 had a follow-up exam at 10 years. The absolute risk for advanced outcomes among patients who had a high quality index exam was 4.0% vs. 6.7% for those with lower quality exams.
Among patients with low-quality index exams – but not patients with high quality exams – there was a statistically significant increase in the absolute risk for advanced outcomes at all time periods, from 5.1% in the less than 5-year follow-up group, to 6.7% in the 10-years or more follow-up group.
Patients with initial high-quality exams also had a lower risk for postcolonoscopy colorectal cancer, compared with patients who had low-quality index exams: 0.4% vs. 0.8%. This difference translated into an adjusted hazard ratio for colorectal cancer after a high-quality exam of 0.53.
It’s getting better all the time
In an interview, Daniel J. Pambianco, MD, FACG from Charlottesville (Va.) Gastroenterology Associates, who was not involved in the study, commented that Dr. Anderson and colleagues highlighted the importance of the quality of the bowel prep and the quality of the examination itself.
He noted that the use of devices such as colonoscopy caps can help further improve adenoma detection rates and pointed to up-and-coming developments such as the use of artificial intelligence algorithms to aid human endoscopists.
Dr. Pambianco comoderated the session where the data were presented.
The investigators did not report a study funding source. Dr. Anderson and Dr. Pambianco reported having no relevant financial disclosures.
CHARLOTTE, N.C.– Performing high-quality index colonoscopies may pay off later in your patients’ reduced risk for advanced neoplasia, investigators report.
A study of registry data on more than 2,200 patients who had an index colonoscopy showing no evidence of neoplasia found that, on repeat colonoscopy 10 years later, the absolute risk for advanced neoplasia outcomes was lower for those with a high-quality index exam, compared with those who had a lesser-quality index colonoscopy.
The adjusted odds ratio for patients who underwent high-quality index exams was 0.59%, reported Joseph Anderson, MD, from the Geisel School of Medicine at Dartmouth, Hanover, N.H.
“These data demonstrate that high-quality index colonoscopy provides better protection from interval lesions than low-quality exams with no polyps detected at that index exam,” he said in an oral abstract presentation at the annual meeting of the American College of Gastroenterology.
“These data support the importance of high-quality index exams in the prevention of interval colorectal cancer, and support the 10-year interval for normal exams,” Dr. Anderson added.
He recommended that endoscopists focus on the quality of their exams by using adequate scope withdrawal time – 8-10 minutes – to ensure optimal adenoma detection, and by ensuring the use of optimal bowel preparation in their practices.
Registry study
Dr. Anderson and colleagues studied how the quality of index colonoscopies could affect the risk of advanced outcomes in low-risk patients at the 10-year or later follow-up. They used records from the New Hampshire Colonoscopy Registry, which includes data from 2004 to the present on more than 250,000 exams performed by more than 150 endoscopists in more than 30 Granite State practices.
The investigators also looked at data on patients with less than 5 years of follow-up, and those with follow-up from 5 to less than 10 years.
The study sample included patients with no adenoma or significant serrated polyps on their index exams who had at least one follow-up exam 12 months or more after the index exams. Patients with inflammatory bowel disease or familial colon cancer syndromes were excluded.
They defined a high-quality colonoscopy as an exam complete to cecum, with adequate bowel preparation, and performed by an endoscopist with an adenoma detection rate of 25 or higher.
The adenoma detection rate is calculated as the number of screening colonoscopies with at least one adenoma divided by the total number of screening colonoscopies.
The definition of advanced outcomes included advanced adenomas, colorectal cancer, and/or large serrated polyps (1 cm or greater).
Of the 14,011 patients in the sample, 2,283 had a follow-up exam at 10 years. The absolute risk for advanced outcomes among patients who had a high quality index exam was 4.0% vs. 6.7% for those with lower quality exams.
Among patients with low-quality index exams – but not patients with high quality exams – there was a statistically significant increase in the absolute risk for advanced outcomes at all time periods, from 5.1% in the less than 5-year follow-up group, to 6.7% in the 10-years or more follow-up group.
Patients with initial high-quality exams also had a lower risk for postcolonoscopy colorectal cancer, compared with patients who had low-quality index exams: 0.4% vs. 0.8%. This difference translated into an adjusted hazard ratio for colorectal cancer after a high-quality exam of 0.53.
It’s getting better all the time
In an interview, Daniel J. Pambianco, MD, FACG from Charlottesville (Va.) Gastroenterology Associates, who was not involved in the study, commented that Dr. Anderson and colleagues highlighted the importance of the quality of the bowel prep and the quality of the examination itself.
He noted that the use of devices such as colonoscopy caps can help further improve adenoma detection rates and pointed to up-and-coming developments such as the use of artificial intelligence algorithms to aid human endoscopists.
Dr. Pambianco comoderated the session where the data were presented.
The investigators did not report a study funding source. Dr. Anderson and Dr. Pambianco reported having no relevant financial disclosures.
CHARLOTTE, N.C.– Performing high-quality index colonoscopies may pay off later in your patients’ reduced risk for advanced neoplasia, investigators report.
A study of registry data on more than 2,200 patients who had an index colonoscopy showing no evidence of neoplasia found that, on repeat colonoscopy 10 years later, the absolute risk for advanced neoplasia outcomes was lower for those with a high-quality index exam, compared with those who had a lesser-quality index colonoscopy.
The adjusted odds ratio for patients who underwent high-quality index exams was 0.59%, reported Joseph Anderson, MD, from the Geisel School of Medicine at Dartmouth, Hanover, N.H.
“These data demonstrate that high-quality index colonoscopy provides better protection from interval lesions than low-quality exams with no polyps detected at that index exam,” he said in an oral abstract presentation at the annual meeting of the American College of Gastroenterology.
“These data support the importance of high-quality index exams in the prevention of interval colorectal cancer, and support the 10-year interval for normal exams,” Dr. Anderson added.
He recommended that endoscopists focus on the quality of their exams by using adequate scope withdrawal time – 8-10 minutes – to ensure optimal adenoma detection, and by ensuring the use of optimal bowel preparation in their practices.
Registry study
Dr. Anderson and colleagues studied how the quality of index colonoscopies could affect the risk of advanced outcomes in low-risk patients at the 10-year or later follow-up. They used records from the New Hampshire Colonoscopy Registry, which includes data from 2004 to the present on more than 250,000 exams performed by more than 150 endoscopists in more than 30 Granite State practices.
The investigators also looked at data on patients with less than 5 years of follow-up, and those with follow-up from 5 to less than 10 years.
The study sample included patients with no adenoma or significant serrated polyps on their index exams who had at least one follow-up exam 12 months or more after the index exams. Patients with inflammatory bowel disease or familial colon cancer syndromes were excluded.
They defined a high-quality colonoscopy as an exam complete to cecum, with adequate bowel preparation, and performed by an endoscopist with an adenoma detection rate of 25 or higher.
The adenoma detection rate is calculated as the number of screening colonoscopies with at least one adenoma divided by the total number of screening colonoscopies.
The definition of advanced outcomes included advanced adenomas, colorectal cancer, and/or large serrated polyps (1 cm or greater).
Of the 14,011 patients in the sample, 2,283 had a follow-up exam at 10 years. The absolute risk for advanced outcomes among patients who had a high quality index exam was 4.0% vs. 6.7% for those with lower quality exams.
Among patients with low-quality index exams – but not patients with high quality exams – there was a statistically significant increase in the absolute risk for advanced outcomes at all time periods, from 5.1% in the less than 5-year follow-up group, to 6.7% in the 10-years or more follow-up group.
Patients with initial high-quality exams also had a lower risk for postcolonoscopy colorectal cancer, compared with patients who had low-quality index exams: 0.4% vs. 0.8%. This difference translated into an adjusted hazard ratio for colorectal cancer after a high-quality exam of 0.53.
It’s getting better all the time
In an interview, Daniel J. Pambianco, MD, FACG from Charlottesville (Va.) Gastroenterology Associates, who was not involved in the study, commented that Dr. Anderson and colleagues highlighted the importance of the quality of the bowel prep and the quality of the examination itself.
He noted that the use of devices such as colonoscopy caps can help further improve adenoma detection rates and pointed to up-and-coming developments such as the use of artificial intelligence algorithms to aid human endoscopists.
Dr. Pambianco comoderated the session where the data were presented.
The investigators did not report a study funding source. Dr. Anderson and Dr. Pambianco reported having no relevant financial disclosures.
AT ACG 2022
Easier bowel prep recipe yields real-world results
CHARLOTTE, N.C. – In a real-world setting, a 1-liter polyethylene glycol and ascorbic acid combination produced a high level of adequate or better bowel cleansing for colonoscopy.
Among more than 13,000 patients who used the combination, abbreviated as 1L PEG+ASC (Plenvu), the overall rate of adequate quality bowel prep was 89.3%, reported Cátia Arieira, MD, from the Hospital da Senhora da Oliveira in Guimarães, Portugal.
The rate of adequate prep was significantly higher with a split-dose regimen (evening-morning) than with a same-day regimen, at 94.7% versus 86.7%, respectively.
“Results from this large study confirm the high cleansing effectiveness and good tolerability of 1 liter of polyethylene glycol and ascorbic acid in real-world settings,” she said in an oral abstract session during the annual meeting of the American College of Gastroenterology.
Designed for tolerability
The 1L PEG+ASC regimen is intended to make precolonoscopy bowel prep a little easier both to take, by reducing the volume of liquid patients need to ingest, and to reduce indigestion with two asymmetric doses, with the second dose having a high ascorbate content.
The 1-liter regimen has been shown to be safe and effective both in clinical trials and in smaller practice-based studies, Dr. Arieira said.
To see how well 1L PEG+ASC performs on a larger scale, the investigators conducted a retrospective observational study of patients underwent a colonoscopy from June 2019 to September 2021 at 12 centers in Spain and Portugal.
The sample included patients who had either a screening, diagnostic, or surveillance colonoscopy and used 1L PEG+ASC in either a split or same-day dose.
The investigators used the Boston Bowel Preparation Scale (BBPS) to evaluate the quality of cleansing. They defined an adequate cleansing as a total BBPS score of 6 or greater, with all segmental scores 2 or greater, and a high-quality cleansing as segmental scores of 3.
They enrolled a total of 13,169 patients, 6,406 men and 6,763 women. The same-day regimen was used by two-thirds of patients, and the split-dose regimen by one-third.
In all, 41.9% of procedures were for screening, 29.4% for diagnosis, 26.2% for surveillance, and 2.6% for other, unspecified reasons.
Results
As noted, the overall rate of adequate prep was 89.3%, with rates of 94.7% and 86.7% for the split and same-day doses, respectively.
A breakdown of cleansing by bowel segment showed that, for each segment, the split-dose regimen was numerically superior to the same-day regimen, with rates of 95.6% versus 89.5% for the right colon, 97.1% versus 91.9% for the left colon, and 97.8% versus 93.1% for the transverse colon, respectively.
Mean BBPS scores were significantly better with split dosing, at 8.02 versus 6.96. Higher scores were seen with split-dosing for each colon segment.
The incidence of adverse events was low, at 2.3% overall, 1.4% for same-day dosing, and 3.9% for split dosing, with nausea the most common.
Tolerability is key
Renee L. Williams, MD, MHPE, FACG, from New York University, who moderated the session but was not involved in the study, commented that the more convenient 1L PEG+ASC regimen may be helpful with improving compliance with bowel prep in underserved populations.
“My population of patients is very different from the one in this study,” she said in an interview. “Normally, if you’re looking at people who are not prepped, at least in the United States, people who have a lot of comorbidities, who are underserved, or have insurance uncertainty tend to have a lower level of bowel prep. So I’d be curious to see whether this would work in that population.”
Dr. Williams noted that she prefers split dosing for bowel prep because it offers better tolerability for patients, adding that when her center introduced split-dose prep, the percentage of adequate prep rose from around 60% to more than 90%.
Comoderator John R. Saltzman, MD, FACG, from Harvard Medical School and Brigham & Women’s Hospital, both in Boston, said that while he’s not familiar with this specific bowel prep formulation, “I’m looking for whatever is most palatable to patients and most effective in practice. Still, most of our patients tolerate these 2-liter overnight preps very well.”
The 1L-PEG+ASC regimen may be a suitable option for patients whose colonoscopies are scheduled for later in the day, Dr. Saltzman added.
The study was supported by Norgine and Xolomon Tree. Dr. Arieira, Dr. Williams, and Dr. Saltzman reported no relevant conflicts of interest.
CHARLOTTE, N.C. – In a real-world setting, a 1-liter polyethylene glycol and ascorbic acid combination produced a high level of adequate or better bowel cleansing for colonoscopy.
Among more than 13,000 patients who used the combination, abbreviated as 1L PEG+ASC (Plenvu), the overall rate of adequate quality bowel prep was 89.3%, reported Cátia Arieira, MD, from the Hospital da Senhora da Oliveira in Guimarães, Portugal.
The rate of adequate prep was significantly higher with a split-dose regimen (evening-morning) than with a same-day regimen, at 94.7% versus 86.7%, respectively.
“Results from this large study confirm the high cleansing effectiveness and good tolerability of 1 liter of polyethylene glycol and ascorbic acid in real-world settings,” she said in an oral abstract session during the annual meeting of the American College of Gastroenterology.
Designed for tolerability
The 1L PEG+ASC regimen is intended to make precolonoscopy bowel prep a little easier both to take, by reducing the volume of liquid patients need to ingest, and to reduce indigestion with two asymmetric doses, with the second dose having a high ascorbate content.
The 1-liter regimen has been shown to be safe and effective both in clinical trials and in smaller practice-based studies, Dr. Arieira said.
To see how well 1L PEG+ASC performs on a larger scale, the investigators conducted a retrospective observational study of patients underwent a colonoscopy from June 2019 to September 2021 at 12 centers in Spain and Portugal.
The sample included patients who had either a screening, diagnostic, or surveillance colonoscopy and used 1L PEG+ASC in either a split or same-day dose.
The investigators used the Boston Bowel Preparation Scale (BBPS) to evaluate the quality of cleansing. They defined an adequate cleansing as a total BBPS score of 6 or greater, with all segmental scores 2 or greater, and a high-quality cleansing as segmental scores of 3.
They enrolled a total of 13,169 patients, 6,406 men and 6,763 women. The same-day regimen was used by two-thirds of patients, and the split-dose regimen by one-third.
In all, 41.9% of procedures were for screening, 29.4% for diagnosis, 26.2% for surveillance, and 2.6% for other, unspecified reasons.
Results
As noted, the overall rate of adequate prep was 89.3%, with rates of 94.7% and 86.7% for the split and same-day doses, respectively.
A breakdown of cleansing by bowel segment showed that, for each segment, the split-dose regimen was numerically superior to the same-day regimen, with rates of 95.6% versus 89.5% for the right colon, 97.1% versus 91.9% for the left colon, and 97.8% versus 93.1% for the transverse colon, respectively.
Mean BBPS scores were significantly better with split dosing, at 8.02 versus 6.96. Higher scores were seen with split-dosing for each colon segment.
The incidence of adverse events was low, at 2.3% overall, 1.4% for same-day dosing, and 3.9% for split dosing, with nausea the most common.
Tolerability is key
Renee L. Williams, MD, MHPE, FACG, from New York University, who moderated the session but was not involved in the study, commented that the more convenient 1L PEG+ASC regimen may be helpful with improving compliance with bowel prep in underserved populations.
“My population of patients is very different from the one in this study,” she said in an interview. “Normally, if you’re looking at people who are not prepped, at least in the United States, people who have a lot of comorbidities, who are underserved, or have insurance uncertainty tend to have a lower level of bowel prep. So I’d be curious to see whether this would work in that population.”
Dr. Williams noted that she prefers split dosing for bowel prep because it offers better tolerability for patients, adding that when her center introduced split-dose prep, the percentage of adequate prep rose from around 60% to more than 90%.
Comoderator John R. Saltzman, MD, FACG, from Harvard Medical School and Brigham & Women’s Hospital, both in Boston, said that while he’s not familiar with this specific bowel prep formulation, “I’m looking for whatever is most palatable to patients and most effective in practice. Still, most of our patients tolerate these 2-liter overnight preps very well.”
The 1L-PEG+ASC regimen may be a suitable option for patients whose colonoscopies are scheduled for later in the day, Dr. Saltzman added.
The study was supported by Norgine and Xolomon Tree. Dr. Arieira, Dr. Williams, and Dr. Saltzman reported no relevant conflicts of interest.
CHARLOTTE, N.C. – In a real-world setting, a 1-liter polyethylene glycol and ascorbic acid combination produced a high level of adequate or better bowel cleansing for colonoscopy.
Among more than 13,000 patients who used the combination, abbreviated as 1L PEG+ASC (Plenvu), the overall rate of adequate quality bowel prep was 89.3%, reported Cátia Arieira, MD, from the Hospital da Senhora da Oliveira in Guimarães, Portugal.
The rate of adequate prep was significantly higher with a split-dose regimen (evening-morning) than with a same-day regimen, at 94.7% versus 86.7%, respectively.
“Results from this large study confirm the high cleansing effectiveness and good tolerability of 1 liter of polyethylene glycol and ascorbic acid in real-world settings,” she said in an oral abstract session during the annual meeting of the American College of Gastroenterology.
Designed for tolerability
The 1L PEG+ASC regimen is intended to make precolonoscopy bowel prep a little easier both to take, by reducing the volume of liquid patients need to ingest, and to reduce indigestion with two asymmetric doses, with the second dose having a high ascorbate content.
The 1-liter regimen has been shown to be safe and effective both in clinical trials and in smaller practice-based studies, Dr. Arieira said.
To see how well 1L PEG+ASC performs on a larger scale, the investigators conducted a retrospective observational study of patients underwent a colonoscopy from June 2019 to September 2021 at 12 centers in Spain and Portugal.
The sample included patients who had either a screening, diagnostic, or surveillance colonoscopy and used 1L PEG+ASC in either a split or same-day dose.
The investigators used the Boston Bowel Preparation Scale (BBPS) to evaluate the quality of cleansing. They defined an adequate cleansing as a total BBPS score of 6 or greater, with all segmental scores 2 or greater, and a high-quality cleansing as segmental scores of 3.
They enrolled a total of 13,169 patients, 6,406 men and 6,763 women. The same-day regimen was used by two-thirds of patients, and the split-dose regimen by one-third.
In all, 41.9% of procedures were for screening, 29.4% for diagnosis, 26.2% for surveillance, and 2.6% for other, unspecified reasons.
Results
As noted, the overall rate of adequate prep was 89.3%, with rates of 94.7% and 86.7% for the split and same-day doses, respectively.
A breakdown of cleansing by bowel segment showed that, for each segment, the split-dose regimen was numerically superior to the same-day regimen, with rates of 95.6% versus 89.5% for the right colon, 97.1% versus 91.9% for the left colon, and 97.8% versus 93.1% for the transverse colon, respectively.
Mean BBPS scores were significantly better with split dosing, at 8.02 versus 6.96. Higher scores were seen with split-dosing for each colon segment.
The incidence of adverse events was low, at 2.3% overall, 1.4% for same-day dosing, and 3.9% for split dosing, with nausea the most common.
Tolerability is key
Renee L. Williams, MD, MHPE, FACG, from New York University, who moderated the session but was not involved in the study, commented that the more convenient 1L PEG+ASC regimen may be helpful with improving compliance with bowel prep in underserved populations.
“My population of patients is very different from the one in this study,” she said in an interview. “Normally, if you’re looking at people who are not prepped, at least in the United States, people who have a lot of comorbidities, who are underserved, or have insurance uncertainty tend to have a lower level of bowel prep. So I’d be curious to see whether this would work in that population.”
Dr. Williams noted that she prefers split dosing for bowel prep because it offers better tolerability for patients, adding that when her center introduced split-dose prep, the percentage of adequate prep rose from around 60% to more than 90%.
Comoderator John R. Saltzman, MD, FACG, from Harvard Medical School and Brigham & Women’s Hospital, both in Boston, said that while he’s not familiar with this specific bowel prep formulation, “I’m looking for whatever is most palatable to patients and most effective in practice. Still, most of our patients tolerate these 2-liter overnight preps very well.”
The 1L-PEG+ASC regimen may be a suitable option for patients whose colonoscopies are scheduled for later in the day, Dr. Saltzman added.
The study was supported by Norgine and Xolomon Tree. Dr. Arieira, Dr. Williams, and Dr. Saltzman reported no relevant conflicts of interest.
AT ACG 2022
Has the pandemic affected babies’ brain development?
There’s some good overall news in a large analysis that looked at whether a mother’s COVID-19 infection or birth during the pandemic could affect a baby’s brain development.
Researchers studied 21,419 infants who had neurodevelopmental screening during the pandemic (from January 2020 to January 2021) and compared them with babies born before the pandemic (2015-2019).
They found in an analysis of eight studies that, generally, brain development in infants ages 6-12 months old was not changed by COVID-19.
Communication skill scores lower than prepandemic
However, one area did see a significant difference when they looked at answers to the Ages and Stages Questionnaire, 3rd edition (ASQ-3): Scores were lower in communication skills.
Compared with the prepandemic babies, the pandemic group of babies was more likely to have communication impairment (odds were 1.7 times higher).
Additionally, mothers’ SARS-CoV-2 infection was not associated with significant differences in any neurodevelopment sector in offspring, with one exception: Odds were 3.5 times higher for fine motor impairment in the pandemic baby group.
The babies in this study were either exposed in the womb to the SARS-CoV-2 infection or screened during the pandemic regardless of whether they were exposed to the virus.
The study, led by Kamran Hessami, MD, with the Maternal Fetal Care Center at Boston Children’s Hospital and Harvard Medical School in Boston, was published in JAMA Network Open.
Potential reasons for lower communication skills
The study points to some factors of the pandemic that may be tied to impaired communication skills.
“Higher levels of COVID-19–related stress were reported for both mothers and fathers of infants aged 0-6 months and were associated with insensitive parenting practices, including decreased emotional responsiveness in only mothers, which could lessen the reciprocal exchanges that support language development in early childhood,” they write. “Additionally, opportunities to promote language and social development through new experiences outside the home, including visits with extended family and friends or attendance at a child care center, were lessened for many during the pandemic.”
Viviana M. Fajardo Martinez, MD, with neonatal/perinatal medicine at University of California, Los Angeles, Health, told this publication her team is also studying child development before and after the pandemic over a 3-year period, and delayed communication skills is something she is seeing in clinic there.
She says some parents have been concerned, saying their babies aren’t talking enough or are behind in vocabulary.
Babies can catch up after 12 months
One thing she tells parents is that babies who are a bit delayed at 12 months can catch up.
Up to 18 months, they can catch up, she said, adding that they can be reevaluated then for improvement. If, at that point, the baby is not catching up, “that’s when we refer for early intervention,” she said.
Dr. Martinez also tells parents concerned about their infant’s communication skills that it’s important to talk, read, and sing to their child. She said amid pandemic stress, corners may have been cut in asking children to use language skills.
For instance, if a child points to an apple, a stressed parent may just give the child the apple instead of asking the child to request it by name and repeat the word several times.
She also said a limitation of this study is the use of the ASQ-3 questionnaire, which is filled out by parents. Answers are subjective, she notes, and sometimes differ between one child’s two parents. The questionnaire was commonly used during the pandemic because a more objective, professional evaluation has been more difficult.
However, a measure like the Bayley Scales of Infant and Toddler Development Screening Test adds objectivity and will likely give a better picture as research progresses, Dr. Martinez said.
Some information missing
Andréane Lavallée, PhD, and Dani Dumitriu, MD, PhD, both with the department of pediatrics at Columbia University, New York, write in an invited commentary that the overall positive message of the study “should not make researchers complacent” and results should be viewed with caution.
They point out that the precise effects of this novel virus are still unclear and the age group and variables studied may not tell the whole story.
“It should be noted that this systematic review did not consider timing of exposure during pregnancy, maternal infection severity, or exposure to various SARS-CoV-2 variants – all factors that could eventually be proven to contribute to subtle adverse neurodevelopmental outcomes,” they write.
Additionally, past pandemics “such as the 1918 Spanish flu, 1964 rubella, and 2009 H1N1” have taught researchers to watch for increases in diagnoses such as autism spectrum disorder (ASD) and schizophrenia in subsequent years.
“ASD is generally diagnosed at age 3-5 years (and often not until early teens), while schizophrenia is generally diagnosed in mid-to-late 20s,” the editorialists point out. The authors agree and emphasize the need for long-term studies.
Authors report no relevant financial relationships. Editorialist Dr. Dumitriu reports grants from National Institute of Mental Health, the U.S. Centers for Disease Control and Prevention, and the W. K. Kellogg Foundation; and has received gift funds from Einhorn Collaborative during the conduct of the study to the Nurture Science Program, for which Dr Dumitriu serves as director. Dr. Dumitriu received personal fees from Medela outside the submitted work; and is the corresponding author for one of the studies (Shuffrey et al., 2022) included in the systematic review conducted by Dr. Hessami et al. Dr. Lavallée reports grants from the Canadian Institutes of Health Research. Dr. Martinez reports no relevant financial relationships.
There’s some good overall news in a large analysis that looked at whether a mother’s COVID-19 infection or birth during the pandemic could affect a baby’s brain development.
Researchers studied 21,419 infants who had neurodevelopmental screening during the pandemic (from January 2020 to January 2021) and compared them with babies born before the pandemic (2015-2019).
They found in an analysis of eight studies that, generally, brain development in infants ages 6-12 months old was not changed by COVID-19.
Communication skill scores lower than prepandemic
However, one area did see a significant difference when they looked at answers to the Ages and Stages Questionnaire, 3rd edition (ASQ-3): Scores were lower in communication skills.
Compared with the prepandemic babies, the pandemic group of babies was more likely to have communication impairment (odds were 1.7 times higher).
Additionally, mothers’ SARS-CoV-2 infection was not associated with significant differences in any neurodevelopment sector in offspring, with one exception: Odds were 3.5 times higher for fine motor impairment in the pandemic baby group.
The babies in this study were either exposed in the womb to the SARS-CoV-2 infection or screened during the pandemic regardless of whether they were exposed to the virus.
The study, led by Kamran Hessami, MD, with the Maternal Fetal Care Center at Boston Children’s Hospital and Harvard Medical School in Boston, was published in JAMA Network Open.
Potential reasons for lower communication skills
The study points to some factors of the pandemic that may be tied to impaired communication skills.
“Higher levels of COVID-19–related stress were reported for both mothers and fathers of infants aged 0-6 months and were associated with insensitive parenting practices, including decreased emotional responsiveness in only mothers, which could lessen the reciprocal exchanges that support language development in early childhood,” they write. “Additionally, opportunities to promote language and social development through new experiences outside the home, including visits with extended family and friends or attendance at a child care center, were lessened for many during the pandemic.”
Viviana M. Fajardo Martinez, MD, with neonatal/perinatal medicine at University of California, Los Angeles, Health, told this publication her team is also studying child development before and after the pandemic over a 3-year period, and delayed communication skills is something she is seeing in clinic there.
She says some parents have been concerned, saying their babies aren’t talking enough or are behind in vocabulary.
Babies can catch up after 12 months
One thing she tells parents is that babies who are a bit delayed at 12 months can catch up.
Up to 18 months, they can catch up, she said, adding that they can be reevaluated then for improvement. If, at that point, the baby is not catching up, “that’s when we refer for early intervention,” she said.
Dr. Martinez also tells parents concerned about their infant’s communication skills that it’s important to talk, read, and sing to their child. She said amid pandemic stress, corners may have been cut in asking children to use language skills.
For instance, if a child points to an apple, a stressed parent may just give the child the apple instead of asking the child to request it by name and repeat the word several times.
She also said a limitation of this study is the use of the ASQ-3 questionnaire, which is filled out by parents. Answers are subjective, she notes, and sometimes differ between one child’s two parents. The questionnaire was commonly used during the pandemic because a more objective, professional evaluation has been more difficult.
However, a measure like the Bayley Scales of Infant and Toddler Development Screening Test adds objectivity and will likely give a better picture as research progresses, Dr. Martinez said.
Some information missing
Andréane Lavallée, PhD, and Dani Dumitriu, MD, PhD, both with the department of pediatrics at Columbia University, New York, write in an invited commentary that the overall positive message of the study “should not make researchers complacent” and results should be viewed with caution.
They point out that the precise effects of this novel virus are still unclear and the age group and variables studied may not tell the whole story.
“It should be noted that this systematic review did not consider timing of exposure during pregnancy, maternal infection severity, or exposure to various SARS-CoV-2 variants – all factors that could eventually be proven to contribute to subtle adverse neurodevelopmental outcomes,” they write.
Additionally, past pandemics “such as the 1918 Spanish flu, 1964 rubella, and 2009 H1N1” have taught researchers to watch for increases in diagnoses such as autism spectrum disorder (ASD) and schizophrenia in subsequent years.
“ASD is generally diagnosed at age 3-5 years (and often not until early teens), while schizophrenia is generally diagnosed in mid-to-late 20s,” the editorialists point out. The authors agree and emphasize the need for long-term studies.
Authors report no relevant financial relationships. Editorialist Dr. Dumitriu reports grants from National Institute of Mental Health, the U.S. Centers for Disease Control and Prevention, and the W. K. Kellogg Foundation; and has received gift funds from Einhorn Collaborative during the conduct of the study to the Nurture Science Program, for which Dr Dumitriu serves as director. Dr. Dumitriu received personal fees from Medela outside the submitted work; and is the corresponding author for one of the studies (Shuffrey et al., 2022) included in the systematic review conducted by Dr. Hessami et al. Dr. Lavallée reports grants from the Canadian Institutes of Health Research. Dr. Martinez reports no relevant financial relationships.
There’s some good overall news in a large analysis that looked at whether a mother’s COVID-19 infection or birth during the pandemic could affect a baby’s brain development.
Researchers studied 21,419 infants who had neurodevelopmental screening during the pandemic (from January 2020 to January 2021) and compared them with babies born before the pandemic (2015-2019).
They found in an analysis of eight studies that, generally, brain development in infants ages 6-12 months old was not changed by COVID-19.
Communication skill scores lower than prepandemic
However, one area did see a significant difference when they looked at answers to the Ages and Stages Questionnaire, 3rd edition (ASQ-3): Scores were lower in communication skills.
Compared with the prepandemic babies, the pandemic group of babies was more likely to have communication impairment (odds were 1.7 times higher).
Additionally, mothers’ SARS-CoV-2 infection was not associated with significant differences in any neurodevelopment sector in offspring, with one exception: Odds were 3.5 times higher for fine motor impairment in the pandemic baby group.
The babies in this study were either exposed in the womb to the SARS-CoV-2 infection or screened during the pandemic regardless of whether they were exposed to the virus.
The study, led by Kamran Hessami, MD, with the Maternal Fetal Care Center at Boston Children’s Hospital and Harvard Medical School in Boston, was published in JAMA Network Open.
Potential reasons for lower communication skills
The study points to some factors of the pandemic that may be tied to impaired communication skills.
“Higher levels of COVID-19–related stress were reported for both mothers and fathers of infants aged 0-6 months and were associated with insensitive parenting practices, including decreased emotional responsiveness in only mothers, which could lessen the reciprocal exchanges that support language development in early childhood,” they write. “Additionally, opportunities to promote language and social development through new experiences outside the home, including visits with extended family and friends or attendance at a child care center, were lessened for many during the pandemic.”
Viviana M. Fajardo Martinez, MD, with neonatal/perinatal medicine at University of California, Los Angeles, Health, told this publication her team is also studying child development before and after the pandemic over a 3-year period, and delayed communication skills is something she is seeing in clinic there.
She says some parents have been concerned, saying their babies aren’t talking enough or are behind in vocabulary.
Babies can catch up after 12 months
One thing she tells parents is that babies who are a bit delayed at 12 months can catch up.
Up to 18 months, they can catch up, she said, adding that they can be reevaluated then for improvement. If, at that point, the baby is not catching up, “that’s when we refer for early intervention,” she said.
Dr. Martinez also tells parents concerned about their infant’s communication skills that it’s important to talk, read, and sing to their child. She said amid pandemic stress, corners may have been cut in asking children to use language skills.
For instance, if a child points to an apple, a stressed parent may just give the child the apple instead of asking the child to request it by name and repeat the word several times.
She also said a limitation of this study is the use of the ASQ-3 questionnaire, which is filled out by parents. Answers are subjective, she notes, and sometimes differ between one child’s two parents. The questionnaire was commonly used during the pandemic because a more objective, professional evaluation has been more difficult.
However, a measure like the Bayley Scales of Infant and Toddler Development Screening Test adds objectivity and will likely give a better picture as research progresses, Dr. Martinez said.
Some information missing
Andréane Lavallée, PhD, and Dani Dumitriu, MD, PhD, both with the department of pediatrics at Columbia University, New York, write in an invited commentary that the overall positive message of the study “should not make researchers complacent” and results should be viewed with caution.
They point out that the precise effects of this novel virus are still unclear and the age group and variables studied may not tell the whole story.
“It should be noted that this systematic review did not consider timing of exposure during pregnancy, maternal infection severity, or exposure to various SARS-CoV-2 variants – all factors that could eventually be proven to contribute to subtle adverse neurodevelopmental outcomes,” they write.
Additionally, past pandemics “such as the 1918 Spanish flu, 1964 rubella, and 2009 H1N1” have taught researchers to watch for increases in diagnoses such as autism spectrum disorder (ASD) and schizophrenia in subsequent years.
“ASD is generally diagnosed at age 3-5 years (and often not until early teens), while schizophrenia is generally diagnosed in mid-to-late 20s,” the editorialists point out. The authors agree and emphasize the need for long-term studies.
Authors report no relevant financial relationships. Editorialist Dr. Dumitriu reports grants from National Institute of Mental Health, the U.S. Centers for Disease Control and Prevention, and the W. K. Kellogg Foundation; and has received gift funds from Einhorn Collaborative during the conduct of the study to the Nurture Science Program, for which Dr Dumitriu serves as director. Dr. Dumitriu received personal fees from Medela outside the submitted work; and is the corresponding author for one of the studies (Shuffrey et al., 2022) included in the systematic review conducted by Dr. Hessami et al. Dr. Lavallée reports grants from the Canadian Institutes of Health Research. Dr. Martinez reports no relevant financial relationships.
FROM JAMA NETWORK OPEN
Higher cardiovascular fitness may help preserve mobility in MS
Investigators found that over time, lower cardiorespiratory fitness predicts increased variability in stride time and could represent a biomarker for subtle neuromuscular decline in patients with MS.
Cardiorespiratory fitness “may exert neuroprotective effects on the central nervous system,” study investigator Syamala Buragadda, neurophysical therapist and PhD candidate, Memorial University, St. John’s, Nfld..
She reported her research at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
Gait changes
Gait is a complicated process involving coordination of multiple systems, but steps are almost always consistent and symmetric, said Ms. Buragadda. Patients with MS can experience subtle declines in gait quality even without relapses. Considering the neuroprotective properties of exercise, having higher fitness levels could prevent brain atrophy and protect against subtle gait changes.
Calculating stride time variability is a sensitive method to map changes in gait quality.
Ms. Buragadda, with co-investigator Michelle Ploughman, PhD, also with Memorial University, evaluated stride time variability over time in people with MS and explored whether cardiorespiratory fitness predicts stride time variability.
They recruited 49 adults with relapsing-remitting MS (63% women) and mild disability (Expanded Disability Status Scale [EDSS] score < 4; median, 2.0) from MS clinics in Canada. None required walking aids, and none had experienced relapses in the prior 3 months.
Gait quality was assessed on an instrumented walkway, and variability was measured as the coefficient of variation of stride time. Cardiorespiratory fitness was measured as maximal oxygen uptake (VO2max) during a graded exercise test using recumbent stepper. Tests were conducted 2 years apart.
There were no significant changes in EDSS scores over the study period. However, stride time variability increased from 7.3% at baseline to 8.3% at 2 years.
Cardiorespiratory fitness at baseline significantly correlated with stride time variability 2 years later (P = .016) and was a significant predictor of stride time variability at 2 years, accounting for 10% of its variance, Ms. Buragadda reported.
Stride time variability, measured on an instrumented walkway, could be a biomarker for subtle changes to walking and balance, she said.
Limitations of the study include a convenience sample that may not represent the diversity of MS. Also, assessments were made at only two time points, and more time points would likely yield better predictive power. In addition, the lack of MRI images limits correlating structural changes with clinical observations of gait changes.
A buffer against disability?
In a comment, Valerie Block, physical therapist and adjunct instructor, department of physical therapy and rehabilitation science, University of California, San Francisco, and UCSF Weill Institute for Neuroscience, said the findings in this study are not surprising and align with what she has observed, subjectively, in her work.
“In the general population, cardiovascular fitness has a wide array of benefits. Depending on what means the person uses to maintain or improve cardiovascular fitness (that is, running, walking, swimming, etc.), this would have the potential for neuroplastic effects on gait – even in MS and other neurological disorders,” Ms. Block said.
Also offering perspective, Brain Sandroff, PhD, senior research scientist, Kessler Foundation, West Orange, N.J., said the study provides “more evidence on the multisystemic benefits of exercise training and having better physical fitness in persons with MS. The evidence seems to be converging more and more on this, as research groups across countries and continents are reporting on similar themes,” said Dr. Sandroff.
He noted that the findings from this study coincide with some other data that showed that premorbid physical activity is associated with reduced mobility decline over time in persons with MS.
“Collectively, the data suggest that perhaps engaging in exercise training early in the disease (or having better cardiorespiratory fitness at diagnosis) provides a buffer against disability progression over time,” Dr. Sandroff said.
He said it would be interesting to see whether “physical fitness/premorbid physical activity provides such a buffer in those who already demonstrate mobility problems.”
The study had no specific funding. Ms. Buragadda, Dr. Ploughman, Ms. Block, and Dr. Sandroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators found that over time, lower cardiorespiratory fitness predicts increased variability in stride time and could represent a biomarker for subtle neuromuscular decline in patients with MS.
Cardiorespiratory fitness “may exert neuroprotective effects on the central nervous system,” study investigator Syamala Buragadda, neurophysical therapist and PhD candidate, Memorial University, St. John’s, Nfld..
She reported her research at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
Gait changes
Gait is a complicated process involving coordination of multiple systems, but steps are almost always consistent and symmetric, said Ms. Buragadda. Patients with MS can experience subtle declines in gait quality even without relapses. Considering the neuroprotective properties of exercise, having higher fitness levels could prevent brain atrophy and protect against subtle gait changes.
Calculating stride time variability is a sensitive method to map changes in gait quality.
Ms. Buragadda, with co-investigator Michelle Ploughman, PhD, also with Memorial University, evaluated stride time variability over time in people with MS and explored whether cardiorespiratory fitness predicts stride time variability.
They recruited 49 adults with relapsing-remitting MS (63% women) and mild disability (Expanded Disability Status Scale [EDSS] score < 4; median, 2.0) from MS clinics in Canada. None required walking aids, and none had experienced relapses in the prior 3 months.
Gait quality was assessed on an instrumented walkway, and variability was measured as the coefficient of variation of stride time. Cardiorespiratory fitness was measured as maximal oxygen uptake (VO2max) during a graded exercise test using recumbent stepper. Tests were conducted 2 years apart.
There were no significant changes in EDSS scores over the study period. However, stride time variability increased from 7.3% at baseline to 8.3% at 2 years.
Cardiorespiratory fitness at baseline significantly correlated with stride time variability 2 years later (P = .016) and was a significant predictor of stride time variability at 2 years, accounting for 10% of its variance, Ms. Buragadda reported.
Stride time variability, measured on an instrumented walkway, could be a biomarker for subtle changes to walking and balance, she said.
Limitations of the study include a convenience sample that may not represent the diversity of MS. Also, assessments were made at only two time points, and more time points would likely yield better predictive power. In addition, the lack of MRI images limits correlating structural changes with clinical observations of gait changes.
A buffer against disability?
In a comment, Valerie Block, physical therapist and adjunct instructor, department of physical therapy and rehabilitation science, University of California, San Francisco, and UCSF Weill Institute for Neuroscience, said the findings in this study are not surprising and align with what she has observed, subjectively, in her work.
“In the general population, cardiovascular fitness has a wide array of benefits. Depending on what means the person uses to maintain or improve cardiovascular fitness (that is, running, walking, swimming, etc.), this would have the potential for neuroplastic effects on gait – even in MS and other neurological disorders,” Ms. Block said.
Also offering perspective, Brain Sandroff, PhD, senior research scientist, Kessler Foundation, West Orange, N.J., said the study provides “more evidence on the multisystemic benefits of exercise training and having better physical fitness in persons with MS. The evidence seems to be converging more and more on this, as research groups across countries and continents are reporting on similar themes,” said Dr. Sandroff.
He noted that the findings from this study coincide with some other data that showed that premorbid physical activity is associated with reduced mobility decline over time in persons with MS.
“Collectively, the data suggest that perhaps engaging in exercise training early in the disease (or having better cardiorespiratory fitness at diagnosis) provides a buffer against disability progression over time,” Dr. Sandroff said.
He said it would be interesting to see whether “physical fitness/premorbid physical activity provides such a buffer in those who already demonstrate mobility problems.”
The study had no specific funding. Ms. Buragadda, Dr. Ploughman, Ms. Block, and Dr. Sandroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators found that over time, lower cardiorespiratory fitness predicts increased variability in stride time and could represent a biomarker for subtle neuromuscular decline in patients with MS.
Cardiorespiratory fitness “may exert neuroprotective effects on the central nervous system,” study investigator Syamala Buragadda, neurophysical therapist and PhD candidate, Memorial University, St. John’s, Nfld..
She reported her research at the annual meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
Gait changes
Gait is a complicated process involving coordination of multiple systems, but steps are almost always consistent and symmetric, said Ms. Buragadda. Patients with MS can experience subtle declines in gait quality even without relapses. Considering the neuroprotective properties of exercise, having higher fitness levels could prevent brain atrophy and protect against subtle gait changes.
Calculating stride time variability is a sensitive method to map changes in gait quality.
Ms. Buragadda, with co-investigator Michelle Ploughman, PhD, also with Memorial University, evaluated stride time variability over time in people with MS and explored whether cardiorespiratory fitness predicts stride time variability.
They recruited 49 adults with relapsing-remitting MS (63% women) and mild disability (Expanded Disability Status Scale [EDSS] score < 4; median, 2.0) from MS clinics in Canada. None required walking aids, and none had experienced relapses in the prior 3 months.
Gait quality was assessed on an instrumented walkway, and variability was measured as the coefficient of variation of stride time. Cardiorespiratory fitness was measured as maximal oxygen uptake (VO2max) during a graded exercise test using recumbent stepper. Tests were conducted 2 years apart.
There were no significant changes in EDSS scores over the study period. However, stride time variability increased from 7.3% at baseline to 8.3% at 2 years.
Cardiorespiratory fitness at baseline significantly correlated with stride time variability 2 years later (P = .016) and was a significant predictor of stride time variability at 2 years, accounting for 10% of its variance, Ms. Buragadda reported.
Stride time variability, measured on an instrumented walkway, could be a biomarker for subtle changes to walking and balance, she said.
Limitations of the study include a convenience sample that may not represent the diversity of MS. Also, assessments were made at only two time points, and more time points would likely yield better predictive power. In addition, the lack of MRI images limits correlating structural changes with clinical observations of gait changes.
A buffer against disability?
In a comment, Valerie Block, physical therapist and adjunct instructor, department of physical therapy and rehabilitation science, University of California, San Francisco, and UCSF Weill Institute for Neuroscience, said the findings in this study are not surprising and align with what she has observed, subjectively, in her work.
“In the general population, cardiovascular fitness has a wide array of benefits. Depending on what means the person uses to maintain or improve cardiovascular fitness (that is, running, walking, swimming, etc.), this would have the potential for neuroplastic effects on gait – even in MS and other neurological disorders,” Ms. Block said.
Also offering perspective, Brain Sandroff, PhD, senior research scientist, Kessler Foundation, West Orange, N.J., said the study provides “more evidence on the multisystemic benefits of exercise training and having better physical fitness in persons with MS. The evidence seems to be converging more and more on this, as research groups across countries and continents are reporting on similar themes,” said Dr. Sandroff.
He noted that the findings from this study coincide with some other data that showed that premorbid physical activity is associated with reduced mobility decline over time in persons with MS.
“Collectively, the data suggest that perhaps engaging in exercise training early in the disease (or having better cardiorespiratory fitness at diagnosis) provides a buffer against disability progression over time,” Dr. Sandroff said.
He said it would be interesting to see whether “physical fitness/premorbid physical activity provides such a buffer in those who already demonstrate mobility problems.”
The study had no specific funding. Ms. Buragadda, Dr. Ploughman, Ms. Block, and Dr. Sandroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ECTRIMS 2022
BMI and reproduction – weighing the evidence
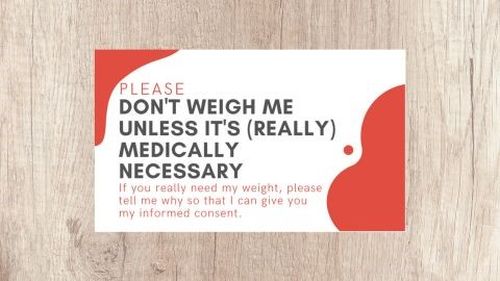
Arguably, no topic during an infertility consultation generates more of an emotional reaction than discussing body mass index (BMI), particularly when it is high. Patients have become increasingly sensitive to weight discussions with their physicians because of concerns about body shaming. Among patients with an elevated BMI, criticism on social media of health care professionals’ counseling and a preemptive presentation of “Don’t Weigh Me” cards have become popular responses. Despite the medical evidence on impaired reproduction with an abnormal BMI, patients are choosing to forgo the topic. Research has demonstrated “extensive evidence [of] strong weight bias” in a wide range of health staff.1 A “viral” TikTok study revealed that medical “gaslighting” founded in weight stigma and bias is harmful, as reported on KevinMD.com.2 This month, we review the effect of abnormal BMI, both high and low, on reproduction and pregnancy.
A method to assess relative weight was first described in 1832 as its ratio in kilograms divided by the square of the height in meters, or the Quetelet Index. The search for a functional assessment of relative body weight began after World War II when reports by actuaries noted the increased mortality of overweight policyholders. The relationship between weight and cardiovascular disease was further revealed in epidemiologic studies. The Quetelet Index became the BMI in 1972.3
Weight measurement is a mainstay in the assessment of a patient’s vital signs along with blood pressure, pulse rate, respiration rate, and temperature. Weight is vital to the calculation of medication dosage – for instance, administration of conscious sedative drugs, methotrexate, and gonadotropins. Some state boards of medicine, such as Florida, have a limitation on patient BMI at office-based surgery centers (40 kg/m2).
Obesity is a disease
As reported by the World Health Organization in 2022, the disease of obesity is an epidemic afflicting more than 1 billion people worldwide, or 1 in 8 individuals globally.4 The health implications of an elevated BMI include increased mortality, diabetes, heart disease, and stroke, physical limitations to activities of daily living, and complications affecting reproduction.
Female obesity is related to poorer outcomes in natural and assisted conception, including an increased risk of miscarriage. Compared with normal-weight women, those with obesity are three times more likely to have ovulatory dysfunction,5 infertility,6 a lower chance for conception,7 higher rate of miscarriage, and low birth weight.8,9During pregnancy, women with obesity have three to four times higher rates of gestational diabetes and preeclampsia,10 as well as likelihood of delivering preterm,11 having a fetus with macrosomia and birth defects, and a 1.3- to 2.1-times higher risk of stillbirth.12
Obesity is present in 40%-80% of women with polycystic ovary syndrome,13 the most common cause of ovulatory dysfunction from dysregulation of the hypothalamic-pituitary-ovarian axis. While PCOS is associated with reproductive and metabolic consequences, even in regularly ovulating women, increasing obesity appears to be associated with decreasing spontaneous pregnancy rates and increased time to pregnancy.14
Obesity and IVF
Women with obesity have reduced success with assisted reproductive technology, an increased number of canceled cycles, and poorer quality oocytes retrieved. A prospective cohort study of nearly 2,000 women reported that every 5 kg of body weight increase (from the patient’s baseline weight at age 18) was associated with a 5% increase in the mean duration of time required for conception (95% confidence interval, 3%-7%).15 Given that approximately 90% of these women had regular menstrual cycles, ovulatory dysfunction was not the suspected pathophysiology.
A meta-analysis of 21 cohort studies reported a lower likelihood of live birth following in vitro fertilization for women with obesity, compared with normal-weight women (risk ratio, 0.85; 95% CI, 0.82-0.87).16 A further subgroup analysis that evaluated only women with PCOS showed a reduction in the live birth rate following IVF for individuals with obesity, compared with normal-weight individuals (RR, 0.78; 95% CI, 0.74-0.82).
In a retrospective study of almost 500,000 fresh autologous IVF cycles, women with obesity had a 6% reduction in pregnancy rates and a 13% reduction in live birth rates, compared with normal-weight women. Both high and low BMI were associated with an increased risk of low birth weight and preterm delivery.17 The live birth rates per transfer for normal-weight and higher-weight women were 38% and 33%, respectively.
Contrarily, a randomized controlled trial showed that an intensive weight-reduction program resulted in a large weight loss but did not substantially affect live birth rates in women with obesity scheduled for IVF.18
Low BMI
A noteworthy cause of low BMI is functional hypothalamic amenorrhea (FHA), a disorder with low energy availability either from decreased caloric intake and/or excessive energy expenditure associated with eating disorders, excessive exercise, and stress. Consequently, a reduced GnRH drive results in a decreased pulse frequency and amplitude leading to low levels of follicle-stimulating hormone and luteinizing hormone, resulting in anovulation. Correction of lifestyle behaviors related to FHA can restore menstrual cycles. After normal weight is achieved, it appears unlikely that fertility is affected.19 In 47% of adolescent patients with anorexia, menses spontaneously returned within the first 12 months after admission, with an improved prognosis in secondary over primary amenorrhea.20,21 Interestingly, mildly and significantly underweight infertile women have pregnancy and live birth rates similar to normal-weight patients after IVF treatment.22
Pregnancy is complicated in underweight women, resulting in an increased risk of anemia, fetal growth retardation, and low birth weight, as well as preterm birth.21
Take-home message
The extremes of BMI both impair natural reproduction. Elevated BMI reduces success with IVF but rapid weight loss prior to IVF does not improve outcomes. A normal BMI is the goal for optimal reproductive and pregnancy health.
Dr. Trolice is director of the IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
References
1. Talumaa B et al. Obesity Rev. 2022;23:e13494.
2. https://bit.ly/3rHCivE.
3. Eknoyan G. Nephrol Dial Transplant. 2008;23:47-51.
4. Wells JCK. Dis Models Mech. 2012;5:595-607.
5. Brewer CJ and Balen AH. Reproduction. 2010;140:347-64.
6. Silvestris E et al. Reprod Biol Endocrinol. 2018;16:22.
7. Wise LA et al. Hum Reprod. 2010;25:253-64.
8. Bellver J. Curr Opin Obstet Gynecol. 2022;34:114-21.
9. Dickey RP et al. Am J Obstet Gynecol. 2013;209:349.e1.
10. Alwash SM et al. Obes Res Clin Pract. 2021;15:425-30.
11. Cnattingius S et al. JAMA. 2013;309:2362-70.
12. Aune D et al. JAMA. 2014;311:1536-46.
13. Sam S. Obes Manag. 2007;3:69-73.
14. van der Steeg JW et al. Hum Reprod. 2008;23:324-8.
15. Gaskins AJ et al. Obstet Gynecol. 2015;126:850-8.
16. Sermondade N et al. Hum Reprod Update. 2019;25:439-519.
17. Kawwass JF et al. Fertil Steril. 2016;106[7]:1742-50.
18. Einarsson S et al. Hum Reprod. 2017;32:1621-30.
19. Chaer R et al. Diseases. 2020;8:46.
20. Dempfle A et al. Psychiatry. 2013;13:308.
21. Verma A and Shrimali L. J Clin Diagn Res. 2012;6:1531-3.
22. Romanski PA et al. Reprod Biomed Online. 2020;42:366-74.
Arguably, no topic during an infertility consultation generates more of an emotional reaction than discussing body mass index (BMI), particularly when it is high. Patients have become increasingly sensitive to weight discussions with their physicians because of concerns about body shaming. Among patients with an elevated BMI, criticism on social media of health care professionals’ counseling and a preemptive presentation of “Don’t Weigh Me” cards have become popular responses. Despite the medical evidence on impaired reproduction with an abnormal BMI, patients are choosing to forgo the topic. Research has demonstrated “extensive evidence [of] strong weight bias” in a wide range of health staff.1 A “viral” TikTok study revealed that medical “gaslighting” founded in weight stigma and bias is harmful, as reported on KevinMD.com.2 This month, we review the effect of abnormal BMI, both high and low, on reproduction and pregnancy.
A method to assess relative weight was first described in 1832 as its ratio in kilograms divided by the square of the height in meters, or the Quetelet Index. The search for a functional assessment of relative body weight began after World War II when reports by actuaries noted the increased mortality of overweight policyholders. The relationship between weight and cardiovascular disease was further revealed in epidemiologic studies. The Quetelet Index became the BMI in 1972.3
Weight measurement is a mainstay in the assessment of a patient’s vital signs along with blood pressure, pulse rate, respiration rate, and temperature. Weight is vital to the calculation of medication dosage – for instance, administration of conscious sedative drugs, methotrexate, and gonadotropins. Some state boards of medicine, such as Florida, have a limitation on patient BMI at office-based surgery centers (40 kg/m2).
Obesity is a disease
As reported by the World Health Organization in 2022, the disease of obesity is an epidemic afflicting more than 1 billion people worldwide, or 1 in 8 individuals globally.4 The health implications of an elevated BMI include increased mortality, diabetes, heart disease, and stroke, physical limitations to activities of daily living, and complications affecting reproduction.
Female obesity is related to poorer outcomes in natural and assisted conception, including an increased risk of miscarriage. Compared with normal-weight women, those with obesity are three times more likely to have ovulatory dysfunction,5 infertility,6 a lower chance for conception,7 higher rate of miscarriage, and low birth weight.8,9During pregnancy, women with obesity have three to four times higher rates of gestational diabetes and preeclampsia,10 as well as likelihood of delivering preterm,11 having a fetus with macrosomia and birth defects, and a 1.3- to 2.1-times higher risk of stillbirth.12
Obesity is present in 40%-80% of women with polycystic ovary syndrome,13 the most common cause of ovulatory dysfunction from dysregulation of the hypothalamic-pituitary-ovarian axis. While PCOS is associated with reproductive and metabolic consequences, even in regularly ovulating women, increasing obesity appears to be associated with decreasing spontaneous pregnancy rates and increased time to pregnancy.14
Obesity and IVF
Women with obesity have reduced success with assisted reproductive technology, an increased number of canceled cycles, and poorer quality oocytes retrieved. A prospective cohort study of nearly 2,000 women reported that every 5 kg of body weight increase (from the patient’s baseline weight at age 18) was associated with a 5% increase in the mean duration of time required for conception (95% confidence interval, 3%-7%).15 Given that approximately 90% of these women had regular menstrual cycles, ovulatory dysfunction was not the suspected pathophysiology.
A meta-analysis of 21 cohort studies reported a lower likelihood of live birth following in vitro fertilization for women with obesity, compared with normal-weight women (risk ratio, 0.85; 95% CI, 0.82-0.87).16 A further subgroup analysis that evaluated only women with PCOS showed a reduction in the live birth rate following IVF for individuals with obesity, compared with normal-weight individuals (RR, 0.78; 95% CI, 0.74-0.82).
In a retrospective study of almost 500,000 fresh autologous IVF cycles, women with obesity had a 6% reduction in pregnancy rates and a 13% reduction in live birth rates, compared with normal-weight women. Both high and low BMI were associated with an increased risk of low birth weight and preterm delivery.17 The live birth rates per transfer for normal-weight and higher-weight women were 38% and 33%, respectively.
Contrarily, a randomized controlled trial showed that an intensive weight-reduction program resulted in a large weight loss but did not substantially affect live birth rates in women with obesity scheduled for IVF.18
Low BMI
A noteworthy cause of low BMI is functional hypothalamic amenorrhea (FHA), a disorder with low energy availability either from decreased caloric intake and/or excessive energy expenditure associated with eating disorders, excessive exercise, and stress. Consequently, a reduced GnRH drive results in a decreased pulse frequency and amplitude leading to low levels of follicle-stimulating hormone and luteinizing hormone, resulting in anovulation. Correction of lifestyle behaviors related to FHA can restore menstrual cycles. After normal weight is achieved, it appears unlikely that fertility is affected.19 In 47% of adolescent patients with anorexia, menses spontaneously returned within the first 12 months after admission, with an improved prognosis in secondary over primary amenorrhea.20,21 Interestingly, mildly and significantly underweight infertile women have pregnancy and live birth rates similar to normal-weight patients after IVF treatment.22
Pregnancy is complicated in underweight women, resulting in an increased risk of anemia, fetal growth retardation, and low birth weight, as well as preterm birth.21
Take-home message
The extremes of BMI both impair natural reproduction. Elevated BMI reduces success with IVF but rapid weight loss prior to IVF does not improve outcomes. A normal BMI is the goal for optimal reproductive and pregnancy health.
Dr. Trolice is director of the IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
References
1. Talumaa B et al. Obesity Rev. 2022;23:e13494.
2. https://bit.ly/3rHCivE.
3. Eknoyan G. Nephrol Dial Transplant. 2008;23:47-51.
4. Wells JCK. Dis Models Mech. 2012;5:595-607.
5. Brewer CJ and Balen AH. Reproduction. 2010;140:347-64.
6. Silvestris E et al. Reprod Biol Endocrinol. 2018;16:22.
7. Wise LA et al. Hum Reprod. 2010;25:253-64.
8. Bellver J. Curr Opin Obstet Gynecol. 2022;34:114-21.
9. Dickey RP et al. Am J Obstet Gynecol. 2013;209:349.e1.
10. Alwash SM et al. Obes Res Clin Pract. 2021;15:425-30.
11. Cnattingius S et al. JAMA. 2013;309:2362-70.
12. Aune D et al. JAMA. 2014;311:1536-46.
13. Sam S. Obes Manag. 2007;3:69-73.
14. van der Steeg JW et al. Hum Reprod. 2008;23:324-8.
15. Gaskins AJ et al. Obstet Gynecol. 2015;126:850-8.
16. Sermondade N et al. Hum Reprod Update. 2019;25:439-519.
17. Kawwass JF et al. Fertil Steril. 2016;106[7]:1742-50.
18. Einarsson S et al. Hum Reprod. 2017;32:1621-30.
19. Chaer R et al. Diseases. 2020;8:46.
20. Dempfle A et al. Psychiatry. 2013;13:308.
21. Verma A and Shrimali L. J Clin Diagn Res. 2012;6:1531-3.
22. Romanski PA et al. Reprod Biomed Online. 2020;42:366-74.
Arguably, no topic during an infertility consultation generates more of an emotional reaction than discussing body mass index (BMI), particularly when it is high. Patients have become increasingly sensitive to weight discussions with their physicians because of concerns about body shaming. Among patients with an elevated BMI, criticism on social media of health care professionals’ counseling and a preemptive presentation of “Don’t Weigh Me” cards have become popular responses. Despite the medical evidence on impaired reproduction with an abnormal BMI, patients are choosing to forgo the topic. Research has demonstrated “extensive evidence [of] strong weight bias” in a wide range of health staff.1 A “viral” TikTok study revealed that medical “gaslighting” founded in weight stigma and bias is harmful, as reported on KevinMD.com.2 This month, we review the effect of abnormal BMI, both high and low, on reproduction and pregnancy.
A method to assess relative weight was first described in 1832 as its ratio in kilograms divided by the square of the height in meters, or the Quetelet Index. The search for a functional assessment of relative body weight began after World War II when reports by actuaries noted the increased mortality of overweight policyholders. The relationship between weight and cardiovascular disease was further revealed in epidemiologic studies. The Quetelet Index became the BMI in 1972.3
Weight measurement is a mainstay in the assessment of a patient’s vital signs along with blood pressure, pulse rate, respiration rate, and temperature. Weight is vital to the calculation of medication dosage – for instance, administration of conscious sedative drugs, methotrexate, and gonadotropins. Some state boards of medicine, such as Florida, have a limitation on patient BMI at office-based surgery centers (40 kg/m2).
Obesity is a disease
As reported by the World Health Organization in 2022, the disease of obesity is an epidemic afflicting more than 1 billion people worldwide, or 1 in 8 individuals globally.4 The health implications of an elevated BMI include increased mortality, diabetes, heart disease, and stroke, physical limitations to activities of daily living, and complications affecting reproduction.
Female obesity is related to poorer outcomes in natural and assisted conception, including an increased risk of miscarriage. Compared with normal-weight women, those with obesity are three times more likely to have ovulatory dysfunction,5 infertility,6 a lower chance for conception,7 higher rate of miscarriage, and low birth weight.8,9During pregnancy, women with obesity have three to four times higher rates of gestational diabetes and preeclampsia,10 as well as likelihood of delivering preterm,11 having a fetus with macrosomia and birth defects, and a 1.3- to 2.1-times higher risk of stillbirth.12
Obesity is present in 40%-80% of women with polycystic ovary syndrome,13 the most common cause of ovulatory dysfunction from dysregulation of the hypothalamic-pituitary-ovarian axis. While PCOS is associated with reproductive and metabolic consequences, even in regularly ovulating women, increasing obesity appears to be associated with decreasing spontaneous pregnancy rates and increased time to pregnancy.14
Obesity and IVF
Women with obesity have reduced success with assisted reproductive technology, an increased number of canceled cycles, and poorer quality oocytes retrieved. A prospective cohort study of nearly 2,000 women reported that every 5 kg of body weight increase (from the patient’s baseline weight at age 18) was associated with a 5% increase in the mean duration of time required for conception (95% confidence interval, 3%-7%).15 Given that approximately 90% of these women had regular menstrual cycles, ovulatory dysfunction was not the suspected pathophysiology.
A meta-analysis of 21 cohort studies reported a lower likelihood of live birth following in vitro fertilization for women with obesity, compared with normal-weight women (risk ratio, 0.85; 95% CI, 0.82-0.87).16 A further subgroup analysis that evaluated only women with PCOS showed a reduction in the live birth rate following IVF for individuals with obesity, compared with normal-weight individuals (RR, 0.78; 95% CI, 0.74-0.82).
In a retrospective study of almost 500,000 fresh autologous IVF cycles, women with obesity had a 6% reduction in pregnancy rates and a 13% reduction in live birth rates, compared with normal-weight women. Both high and low BMI were associated with an increased risk of low birth weight and preterm delivery.17 The live birth rates per transfer for normal-weight and higher-weight women were 38% and 33%, respectively.
Contrarily, a randomized controlled trial showed that an intensive weight-reduction program resulted in a large weight loss but did not substantially affect live birth rates in women with obesity scheduled for IVF.18
Low BMI
A noteworthy cause of low BMI is functional hypothalamic amenorrhea (FHA), a disorder with low energy availability either from decreased caloric intake and/or excessive energy expenditure associated with eating disorders, excessive exercise, and stress. Consequently, a reduced GnRH drive results in a decreased pulse frequency and amplitude leading to low levels of follicle-stimulating hormone and luteinizing hormone, resulting in anovulation. Correction of lifestyle behaviors related to FHA can restore menstrual cycles. After normal weight is achieved, it appears unlikely that fertility is affected.19 In 47% of adolescent patients with anorexia, menses spontaneously returned within the first 12 months after admission, with an improved prognosis in secondary over primary amenorrhea.20,21 Interestingly, mildly and significantly underweight infertile women have pregnancy and live birth rates similar to normal-weight patients after IVF treatment.22
Pregnancy is complicated in underweight women, resulting in an increased risk of anemia, fetal growth retardation, and low birth weight, as well as preterm birth.21
Take-home message
The extremes of BMI both impair natural reproduction. Elevated BMI reduces success with IVF but rapid weight loss prior to IVF does not improve outcomes. A normal BMI is the goal for optimal reproductive and pregnancy health.
Dr. Trolice is director of the IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
References
1. Talumaa B et al. Obesity Rev. 2022;23:e13494.
2. https://bit.ly/3rHCivE.
3. Eknoyan G. Nephrol Dial Transplant. 2008;23:47-51.
4. Wells JCK. Dis Models Mech. 2012;5:595-607.
5. Brewer CJ and Balen AH. Reproduction. 2010;140:347-64.
6. Silvestris E et al. Reprod Biol Endocrinol. 2018;16:22.
7. Wise LA et al. Hum Reprod. 2010;25:253-64.
8. Bellver J. Curr Opin Obstet Gynecol. 2022;34:114-21.
9. Dickey RP et al. Am J Obstet Gynecol. 2013;209:349.e1.
10. Alwash SM et al. Obes Res Clin Pract. 2021;15:425-30.
11. Cnattingius S et al. JAMA. 2013;309:2362-70.
12. Aune D et al. JAMA. 2014;311:1536-46.
13. Sam S. Obes Manag. 2007;3:69-73.
14. van der Steeg JW et al. Hum Reprod. 2008;23:324-8.
15. Gaskins AJ et al. Obstet Gynecol. 2015;126:850-8.
16. Sermondade N et al. Hum Reprod Update. 2019;25:439-519.
17. Kawwass JF et al. Fertil Steril. 2016;106[7]:1742-50.
18. Einarsson S et al. Hum Reprod. 2017;32:1621-30.
19. Chaer R et al. Diseases. 2020;8:46.
20. Dempfle A et al. Psychiatry. 2013;13:308.
21. Verma A and Shrimali L. J Clin Diagn Res. 2012;6:1531-3.
22. Romanski PA et al. Reprod Biomed Online. 2020;42:366-74.
Would a national provider directory save docs’ time, help patients?
When a consumer uses a health plan provider directory to look up a physician, there’s a high probability that the entry for that doctor is incomplete or inaccurate. The Centers for Medicare & Medicaid Services would like to change that by creating a National Directory of Healthcare Providers and Services, which the agency believes would be more valuable to consumers.
In asking for public comments on whether and how it should establish the directory, CMS argues that this data repository would help patients locate physicians and could help with care coordination, health information exchange, and public health data reporting.
However, it’s not clear that such a directory would be any better than current insurance company listings or that people would use it. But a national directory could benefit physician practices by reducing their administrative work, according to observers.
In requesting public comment on the proposed national directory, CMS explains that provider organizations face “redundant and burdensome reporting requirements to multiple databases.” The directory could greatly reduce this challenge by requiring health care organizations to report provider information to a single database. Currently, physician practices have to submit these data to an average of 20 payers each, according to CMS.
“Right now, [physicians are] inundated with requests, and it takes a lot of time to update this stuff,” said David Zetter, a practice management consultant in Mechanicsburg, Pa.. “If there were one national repository of this information, that would be a good move.”
CMS envisions the National Directory as a central hub from which payers could obtain the latest provider data, which would be updated through a standardized application programming interface (API). Consequently, the insurers would no longer need to have providers submit this information to them separately.
CMS is soliciting input on what should be included in the directory. It notes that in addition to contact information, insurer directories also include a physicians’ specialties, health plan affiliations, and whether they accept new patients.
CMS’ 60-day public comment period ends Dec. 6. After that, the agency will decide what steps to take if it is decided that CMS has the legal authority to create the directory.
Terrible track record
In its annual reviews of health plan directories, CMS found that, from 2017 to 2022, only 47% of provider entries were complete. Only 73% of the providers could be matched to published directories. And only 28% of the provider names, addresses, and specialties in the directories matched those in the National Provider Identifier (NPI) registry.
Many of the mistakes in provider directories stem from errors made by practice staff, who have many other duties besides updating directory data. Yet an astonishing amount of time and effort is devoted to this task. A 2019 survey found that physician practices spend $2.76 billion annually on directory maintenance, or nearly $1000 per month per practice, on average.
The Council for Affordable Quality Healthcare, which conducted the survey, estimated that placing all directory data collection on a single platform could save the average practice $4,746 per year. For all practices in the United States, that works out to about $1.1 billion annually, CAQH said.
Pros and cons of national directory
For all the money spent on maintaining provider directories, consumers don’t use them very much. According to a 2021 Press Ganey survey, fewer than 5% of consumers seeking a primary care doctor get their information from an insurer or a benefits manager. About half search the internet first, and 24% seek a referral from a physician.
A national provider directory would be useful only if it were done right, Mr. Zetter said. Citing the inaccuracy and incompleteness of health plan directories, he said it was likely that a national directory would have similar problems. Data entered by practice staff would have to be automatically validated, perhaps through use of some kind of AI algorithm.
Effect on coordination of care
Mr. Zetter doubts the directory could improve care coordination, because primary care doctors usually refer patients to specialists they already know.
But Julia Adler-Milstein, PhD, professor of medicine and director of the Center for Clinical Informatics at the University of California, San Francisco, said that a national directory could improve communications among providers when patients select specialists outside of their primary care physician’s referral network.
“Especially if it’s not an established referral relationship, that’s where a national directory would be helpful, not only to locate the physicians but also to understand their preferences in how they’d like to receive information,” she said in an interview.
Dr. Adler-Milstein worries less than Mr. Zetter does about the challenge of ensuring the accuracy of data in the directory. She pointed out that the National Plan and Provider Enumeration System, which includes the NPI registry, has done a good job of validating provider name, address, and specialty information.
Dr. Adler-Milstein is more concerned about whether the proposed directory would address physician preferences as to how they wish to receive information. For example, while some physicians may prefer to be contacted directly, others may prefer or are required to communicate through their practices or health systems.
Efficiency in data exchange
The API used by the proposed directory would be based on the Fast Health Interoperability Resources standard that all electronic health record vendors must now include in their products. That raises the question of whether communications using contact information from the directory would be sent through a secure email system or through integrated EHR systems, Dr. Adler-Milstein said.
“I’m not sure whether the directory could support that [integration],” she said. “If it focuses on the concept of secure email exchange, that’s a relatively inefficient way of doing it,” because providers want clinical messages to pop up in their EHR workflow rather than their inboxes.
Nevertheless, Dr. Milstein-Adler added, the directory “would clearly take a lot of today’s manual work out of the system. I think organizations like UCSF would be very motivated to support the directory, knowing that people were going to a single source to find the updated information, including preferences in how we’d like people to communicate with us. There would be a lot of efficiency reasons for organizations to use this national directory.”
A version of this article first appeared on Medscape.com.
When a consumer uses a health plan provider directory to look up a physician, there’s a high probability that the entry for that doctor is incomplete or inaccurate. The Centers for Medicare & Medicaid Services would like to change that by creating a National Directory of Healthcare Providers and Services, which the agency believes would be more valuable to consumers.
In asking for public comments on whether and how it should establish the directory, CMS argues that this data repository would help patients locate physicians and could help with care coordination, health information exchange, and public health data reporting.
However, it’s not clear that such a directory would be any better than current insurance company listings or that people would use it. But a national directory could benefit physician practices by reducing their administrative work, according to observers.
In requesting public comment on the proposed national directory, CMS explains that provider organizations face “redundant and burdensome reporting requirements to multiple databases.” The directory could greatly reduce this challenge by requiring health care organizations to report provider information to a single database. Currently, physician practices have to submit these data to an average of 20 payers each, according to CMS.
“Right now, [physicians are] inundated with requests, and it takes a lot of time to update this stuff,” said David Zetter, a practice management consultant in Mechanicsburg, Pa.. “If there were one national repository of this information, that would be a good move.”
CMS envisions the National Directory as a central hub from which payers could obtain the latest provider data, which would be updated through a standardized application programming interface (API). Consequently, the insurers would no longer need to have providers submit this information to them separately.
CMS is soliciting input on what should be included in the directory. It notes that in addition to contact information, insurer directories also include a physicians’ specialties, health plan affiliations, and whether they accept new patients.
CMS’ 60-day public comment period ends Dec. 6. After that, the agency will decide what steps to take if it is decided that CMS has the legal authority to create the directory.
Terrible track record
In its annual reviews of health plan directories, CMS found that, from 2017 to 2022, only 47% of provider entries were complete. Only 73% of the providers could be matched to published directories. And only 28% of the provider names, addresses, and specialties in the directories matched those in the National Provider Identifier (NPI) registry.
Many of the mistakes in provider directories stem from errors made by practice staff, who have many other duties besides updating directory data. Yet an astonishing amount of time and effort is devoted to this task. A 2019 survey found that physician practices spend $2.76 billion annually on directory maintenance, or nearly $1000 per month per practice, on average.
The Council for Affordable Quality Healthcare, which conducted the survey, estimated that placing all directory data collection on a single platform could save the average practice $4,746 per year. For all practices in the United States, that works out to about $1.1 billion annually, CAQH said.
Pros and cons of national directory
For all the money spent on maintaining provider directories, consumers don’t use them very much. According to a 2021 Press Ganey survey, fewer than 5% of consumers seeking a primary care doctor get their information from an insurer or a benefits manager. About half search the internet first, and 24% seek a referral from a physician.
A national provider directory would be useful only if it were done right, Mr. Zetter said. Citing the inaccuracy and incompleteness of health plan directories, he said it was likely that a national directory would have similar problems. Data entered by practice staff would have to be automatically validated, perhaps through use of some kind of AI algorithm.
Effect on coordination of care
Mr. Zetter doubts the directory could improve care coordination, because primary care doctors usually refer patients to specialists they already know.
But Julia Adler-Milstein, PhD, professor of medicine and director of the Center for Clinical Informatics at the University of California, San Francisco, said that a national directory could improve communications among providers when patients select specialists outside of their primary care physician’s referral network.
“Especially if it’s not an established referral relationship, that’s where a national directory would be helpful, not only to locate the physicians but also to understand their preferences in how they’d like to receive information,” she said in an interview.
Dr. Adler-Milstein worries less than Mr. Zetter does about the challenge of ensuring the accuracy of data in the directory. She pointed out that the National Plan and Provider Enumeration System, which includes the NPI registry, has done a good job of validating provider name, address, and specialty information.
Dr. Adler-Milstein is more concerned about whether the proposed directory would address physician preferences as to how they wish to receive information. For example, while some physicians may prefer to be contacted directly, others may prefer or are required to communicate through their practices or health systems.
Efficiency in data exchange
The API used by the proposed directory would be based on the Fast Health Interoperability Resources standard that all electronic health record vendors must now include in their products. That raises the question of whether communications using contact information from the directory would be sent through a secure email system or through integrated EHR systems, Dr. Adler-Milstein said.
“I’m not sure whether the directory could support that [integration],” she said. “If it focuses on the concept of secure email exchange, that’s a relatively inefficient way of doing it,” because providers want clinical messages to pop up in their EHR workflow rather than their inboxes.
Nevertheless, Dr. Milstein-Adler added, the directory “would clearly take a lot of today’s manual work out of the system. I think organizations like UCSF would be very motivated to support the directory, knowing that people were going to a single source to find the updated information, including preferences in how we’d like people to communicate with us. There would be a lot of efficiency reasons for organizations to use this national directory.”
A version of this article first appeared on Medscape.com.
When a consumer uses a health plan provider directory to look up a physician, there’s a high probability that the entry for that doctor is incomplete or inaccurate. The Centers for Medicare & Medicaid Services would like to change that by creating a National Directory of Healthcare Providers and Services, which the agency believes would be more valuable to consumers.
In asking for public comments on whether and how it should establish the directory, CMS argues that this data repository would help patients locate physicians and could help with care coordination, health information exchange, and public health data reporting.
However, it’s not clear that such a directory would be any better than current insurance company listings or that people would use it. But a national directory could benefit physician practices by reducing their administrative work, according to observers.
In requesting public comment on the proposed national directory, CMS explains that provider organizations face “redundant and burdensome reporting requirements to multiple databases.” The directory could greatly reduce this challenge by requiring health care organizations to report provider information to a single database. Currently, physician practices have to submit these data to an average of 20 payers each, according to CMS.
“Right now, [physicians are] inundated with requests, and it takes a lot of time to update this stuff,” said David Zetter, a practice management consultant in Mechanicsburg, Pa.. “If there were one national repository of this information, that would be a good move.”
CMS envisions the National Directory as a central hub from which payers could obtain the latest provider data, which would be updated through a standardized application programming interface (API). Consequently, the insurers would no longer need to have providers submit this information to them separately.
CMS is soliciting input on what should be included in the directory. It notes that in addition to contact information, insurer directories also include a physicians’ specialties, health plan affiliations, and whether they accept new patients.
CMS’ 60-day public comment period ends Dec. 6. After that, the agency will decide what steps to take if it is decided that CMS has the legal authority to create the directory.
Terrible track record
In its annual reviews of health plan directories, CMS found that, from 2017 to 2022, only 47% of provider entries were complete. Only 73% of the providers could be matched to published directories. And only 28% of the provider names, addresses, and specialties in the directories matched those in the National Provider Identifier (NPI) registry.
Many of the mistakes in provider directories stem from errors made by practice staff, who have many other duties besides updating directory data. Yet an astonishing amount of time and effort is devoted to this task. A 2019 survey found that physician practices spend $2.76 billion annually on directory maintenance, or nearly $1000 per month per practice, on average.
The Council for Affordable Quality Healthcare, which conducted the survey, estimated that placing all directory data collection on a single platform could save the average practice $4,746 per year. For all practices in the United States, that works out to about $1.1 billion annually, CAQH said.
Pros and cons of national directory
For all the money spent on maintaining provider directories, consumers don’t use them very much. According to a 2021 Press Ganey survey, fewer than 5% of consumers seeking a primary care doctor get their information from an insurer or a benefits manager. About half search the internet first, and 24% seek a referral from a physician.
A national provider directory would be useful only if it were done right, Mr. Zetter said. Citing the inaccuracy and incompleteness of health plan directories, he said it was likely that a national directory would have similar problems. Data entered by practice staff would have to be automatically validated, perhaps through use of some kind of AI algorithm.
Effect on coordination of care
Mr. Zetter doubts the directory could improve care coordination, because primary care doctors usually refer patients to specialists they already know.
But Julia Adler-Milstein, PhD, professor of medicine and director of the Center for Clinical Informatics at the University of California, San Francisco, said that a national directory could improve communications among providers when patients select specialists outside of their primary care physician’s referral network.
“Especially if it’s not an established referral relationship, that’s where a national directory would be helpful, not only to locate the physicians but also to understand their preferences in how they’d like to receive information,” she said in an interview.
Dr. Adler-Milstein worries less than Mr. Zetter does about the challenge of ensuring the accuracy of data in the directory. She pointed out that the National Plan and Provider Enumeration System, which includes the NPI registry, has done a good job of validating provider name, address, and specialty information.
Dr. Adler-Milstein is more concerned about whether the proposed directory would address physician preferences as to how they wish to receive information. For example, while some physicians may prefer to be contacted directly, others may prefer or are required to communicate through their practices or health systems.
Efficiency in data exchange
The API used by the proposed directory would be based on the Fast Health Interoperability Resources standard that all electronic health record vendors must now include in their products. That raises the question of whether communications using contact information from the directory would be sent through a secure email system or through integrated EHR systems, Dr. Adler-Milstein said.
“I’m not sure whether the directory could support that [integration],” she said. “If it focuses on the concept of secure email exchange, that’s a relatively inefficient way of doing it,” because providers want clinical messages to pop up in their EHR workflow rather than their inboxes.
Nevertheless, Dr. Milstein-Adler added, the directory “would clearly take a lot of today’s manual work out of the system. I think organizations like UCSF would be very motivated to support the directory, knowing that people were going to a single source to find the updated information, including preferences in how we’d like people to communicate with us. There would be a lot of efficiency reasons for organizations to use this national directory.”
A version of this article first appeared on Medscape.com.
Safe to expand limits of active surveillance in thyroid cancer?
Expanding eligibility for active surveillance in low-risk papillary thyroid cancer appears to be safe, a new prospective trial indicates.
Researchers found that doubling the limits for tumor size to 2 cm and nearly doubling the limits for tumor growth in low-risk papillary thyroid cancer showed no increased risk of adverse outcomes or mortality for patients undergoing active surveillance versus surgery.
“The results of this nonrandomized controlled trial suggest the basis of a more permissive strategy for thyroid cancer management, strengthening the evidence for active surveillance and broadening potential candidacy to most diagnosed thyroid cancers,” the authors conclude. “By extending [tumor] size/growth limits, these study results potentially broaden the potential candidacy for active surveillance and reduce the likelihood of surgery by lengthening the window of observation.”
However, “the expanded parameters are quite controversial,” first author Allen S. Ho, MD, of Cedars-Sinai Medical Center, Los Angeles, told this news organization. Prior studies have only examined tumor size limits up to 1 cm and “clinicians rarely recommend active surveillance up to 2 cm,” Dr. Ho noted. “As far as we know, Cedars-Sinai is the only place that will consider it.”
In addition, the ultimate decision surrounding active surveillance versus surgery may depend on the patient’s level of anxiety, researchers found.
The research was published in JAMA Oncology.
The potential to expand criteria for thyroid cancer active surveillance comes amid ongoing concerns surrounding overtreatment. Advances in technology have led to increased detection of small, often indolent thyroid cancers that can likely be monitored safely through active surveillance but may present decision-making challenges for clinicians about whether to treat or watch and wait.
Similar challenges in prostate cancer have been addressed with tiered risk stratification, but such guidelines have not been as firmly established in thyroid cancer.
Guidelines from the American Thyroid Association in 2015 suggest active surveillance as an alternative for very low-risk tumors; however, studies in general have recommended the approach for initial tumor sizes of only up to 1 cm and with growth of less than 3 mm. And overall, active surveillance has not been broadly adopted as an option in thyroid cancer, the authors explained.
To determine if criteria for active surveillance can be safely expanded to tumors up to 2 cm and for those with growth up to 5 mm, Dr. Ho and colleagues compared outcomes among 222 patients with Bethesda 5 or 6 nodules of 2 cm or smaller who received either active surveillance or immediate surgery.
The patients were recruited from Cedars-Sinai Medical Center between 2014 and 2021. Patients were a median 46.8 years old; 76% were female.
The median size of tumors was 11 mm, with about 60% representing larger tumors (10.1 to 20 mm) and 20.6% measuring 15.1 to 20 mm.
About half of patients (n = 112) chose active surveillance. The median size of tumors in this group was smaller than those in the surgery group (10.1 mm vs. 12 mm). Tumor growth exceeded 5 mm in 3.6% of cases, and tumor volume increases of more than 100% occurred in 7% of cases.
With a mean follow-up of 37 months, 90% (101) of those on active surveillance continued with that approach. Notably, 41% of these patients demonstrated a decrease in tumor size, and no cases of metastatic lymph nodes or distant metastases emerged.
Of the 110 patients who elected to undergo immediate surgery, 19% (21) had equivocal-risk or undetermined features on final pathology, but the disease severity for these patients remained classified as stage I thyroid cancer.
The disease-specific survival and overall survival rates were the same in both groups, at 100%.
Although a general concern is that larger tumors may be more likely to grow, it’s important to note that “papillary thyroid cancer exists in a spectrum,” Dr. Ho explained. What that means is “some smaller cancers grow quickly, while some larger cancers are stable for decades.”
“We believe that a 1 cm cutoff is arbitrary,” Dr. Ho said, adding that 2 cm cancers that grow will still be within the therapeutic window for safe surgery.
However, a key factor in treatment decisions is patient fear. The authors also looked at the anxiety levels in both groups, using the 18-item Thyroid Cancer Modified Anxiety Scale.
Among the 59 patients who participated, those who chose immediate surgery had significantly higher baseline anxiety levels, compared with those who opted for active surveillance. Notably, these higher rates of anxiety endured over time, including after the intervention.
“It is unsurprising that patients choosing surgery possess a higher baseline level of worry,” Dr. Ho said. “However, we were astonished to find that such patients retained high levels of worry, even after surgery and presumed cure of their cancer.”
The role of the anxiety, however, underscores the need for clinicians to be mindful of the often profound psychological impacts of cancer, even low-risk disease.
“We always encourage clinicians to educate patients on active surveillance, especially as it gets highlighted more in official guidelines,” Dr. Ho noted. “However, we certainly acknowledge that cancer is a life-changing diagnosis, and the term can carry enormous psychological weight.”
The authors also acknowledged several study limitations, including the single-center, nonrandomized design and small sample size, and urge follow-up analyses to “independently verify our findings.”
In an accompanying editorial, Andrea L. Merrill, MD, from Boston Medical Center, and Priya H. Dedhia, MD, PhD, with Ohio State University Wexner Medical Center, said the findings have important clinical implications.
“This provocative study not only lays the groundwork for expanding active surveillance criteria for low-risk papillary thyroid cancer but may also improve use of current American Thyroid Association guidelines for active surveillance by demonstrating that use of active surveillance for Bethesda 5 or 6 nodules 20 mm or smaller was not associated with an increase in staging or disease-specific mortality,” they write.
The study is also notable for being among the first to assess the role of patient anxiety in the selection of immediate surgery versus active surveillance, Dr. Merrill and Dr. Dedhia added.
“These findings imply that patient anxiety should be an essential component of shared decision-making and selection of strategies for low-risk papillary thyroid cancer,” they say.
The study authors and editorial authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Expanding eligibility for active surveillance in low-risk papillary thyroid cancer appears to be safe, a new prospective trial indicates.
Researchers found that doubling the limits for tumor size to 2 cm and nearly doubling the limits for tumor growth in low-risk papillary thyroid cancer showed no increased risk of adverse outcomes or mortality for patients undergoing active surveillance versus surgery.
“The results of this nonrandomized controlled trial suggest the basis of a more permissive strategy for thyroid cancer management, strengthening the evidence for active surveillance and broadening potential candidacy to most diagnosed thyroid cancers,” the authors conclude. “By extending [tumor] size/growth limits, these study results potentially broaden the potential candidacy for active surveillance and reduce the likelihood of surgery by lengthening the window of observation.”
However, “the expanded parameters are quite controversial,” first author Allen S. Ho, MD, of Cedars-Sinai Medical Center, Los Angeles, told this news organization. Prior studies have only examined tumor size limits up to 1 cm and “clinicians rarely recommend active surveillance up to 2 cm,” Dr. Ho noted. “As far as we know, Cedars-Sinai is the only place that will consider it.”
In addition, the ultimate decision surrounding active surveillance versus surgery may depend on the patient’s level of anxiety, researchers found.
The research was published in JAMA Oncology.
The potential to expand criteria for thyroid cancer active surveillance comes amid ongoing concerns surrounding overtreatment. Advances in technology have led to increased detection of small, often indolent thyroid cancers that can likely be monitored safely through active surveillance but may present decision-making challenges for clinicians about whether to treat or watch and wait.
Similar challenges in prostate cancer have been addressed with tiered risk stratification, but such guidelines have not been as firmly established in thyroid cancer.
Guidelines from the American Thyroid Association in 2015 suggest active surveillance as an alternative for very low-risk tumors; however, studies in general have recommended the approach for initial tumor sizes of only up to 1 cm and with growth of less than 3 mm. And overall, active surveillance has not been broadly adopted as an option in thyroid cancer, the authors explained.
To determine if criteria for active surveillance can be safely expanded to tumors up to 2 cm and for those with growth up to 5 mm, Dr. Ho and colleagues compared outcomes among 222 patients with Bethesda 5 or 6 nodules of 2 cm or smaller who received either active surveillance or immediate surgery.
The patients were recruited from Cedars-Sinai Medical Center between 2014 and 2021. Patients were a median 46.8 years old; 76% were female.
The median size of tumors was 11 mm, with about 60% representing larger tumors (10.1 to 20 mm) and 20.6% measuring 15.1 to 20 mm.
About half of patients (n = 112) chose active surveillance. The median size of tumors in this group was smaller than those in the surgery group (10.1 mm vs. 12 mm). Tumor growth exceeded 5 mm in 3.6% of cases, and tumor volume increases of more than 100% occurred in 7% of cases.
With a mean follow-up of 37 months, 90% (101) of those on active surveillance continued with that approach. Notably, 41% of these patients demonstrated a decrease in tumor size, and no cases of metastatic lymph nodes or distant metastases emerged.
Of the 110 patients who elected to undergo immediate surgery, 19% (21) had equivocal-risk or undetermined features on final pathology, but the disease severity for these patients remained classified as stage I thyroid cancer.
The disease-specific survival and overall survival rates were the same in both groups, at 100%.
Although a general concern is that larger tumors may be more likely to grow, it’s important to note that “papillary thyroid cancer exists in a spectrum,” Dr. Ho explained. What that means is “some smaller cancers grow quickly, while some larger cancers are stable for decades.”
“We believe that a 1 cm cutoff is arbitrary,” Dr. Ho said, adding that 2 cm cancers that grow will still be within the therapeutic window for safe surgery.
However, a key factor in treatment decisions is patient fear. The authors also looked at the anxiety levels in both groups, using the 18-item Thyroid Cancer Modified Anxiety Scale.
Among the 59 patients who participated, those who chose immediate surgery had significantly higher baseline anxiety levels, compared with those who opted for active surveillance. Notably, these higher rates of anxiety endured over time, including after the intervention.
“It is unsurprising that patients choosing surgery possess a higher baseline level of worry,” Dr. Ho said. “However, we were astonished to find that such patients retained high levels of worry, even after surgery and presumed cure of their cancer.”
The role of the anxiety, however, underscores the need for clinicians to be mindful of the often profound psychological impacts of cancer, even low-risk disease.
“We always encourage clinicians to educate patients on active surveillance, especially as it gets highlighted more in official guidelines,” Dr. Ho noted. “However, we certainly acknowledge that cancer is a life-changing diagnosis, and the term can carry enormous psychological weight.”
The authors also acknowledged several study limitations, including the single-center, nonrandomized design and small sample size, and urge follow-up analyses to “independently verify our findings.”
In an accompanying editorial, Andrea L. Merrill, MD, from Boston Medical Center, and Priya H. Dedhia, MD, PhD, with Ohio State University Wexner Medical Center, said the findings have important clinical implications.
“This provocative study not only lays the groundwork for expanding active surveillance criteria for low-risk papillary thyroid cancer but may also improve use of current American Thyroid Association guidelines for active surveillance by demonstrating that use of active surveillance for Bethesda 5 or 6 nodules 20 mm or smaller was not associated with an increase in staging or disease-specific mortality,” they write.
The study is also notable for being among the first to assess the role of patient anxiety in the selection of immediate surgery versus active surveillance, Dr. Merrill and Dr. Dedhia added.
“These findings imply that patient anxiety should be an essential component of shared decision-making and selection of strategies for low-risk papillary thyroid cancer,” they say.
The study authors and editorial authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Expanding eligibility for active surveillance in low-risk papillary thyroid cancer appears to be safe, a new prospective trial indicates.
Researchers found that doubling the limits for tumor size to 2 cm and nearly doubling the limits for tumor growth in low-risk papillary thyroid cancer showed no increased risk of adverse outcomes or mortality for patients undergoing active surveillance versus surgery.
“The results of this nonrandomized controlled trial suggest the basis of a more permissive strategy for thyroid cancer management, strengthening the evidence for active surveillance and broadening potential candidacy to most diagnosed thyroid cancers,” the authors conclude. “By extending [tumor] size/growth limits, these study results potentially broaden the potential candidacy for active surveillance and reduce the likelihood of surgery by lengthening the window of observation.”
However, “the expanded parameters are quite controversial,” first author Allen S. Ho, MD, of Cedars-Sinai Medical Center, Los Angeles, told this news organization. Prior studies have only examined tumor size limits up to 1 cm and “clinicians rarely recommend active surveillance up to 2 cm,” Dr. Ho noted. “As far as we know, Cedars-Sinai is the only place that will consider it.”
In addition, the ultimate decision surrounding active surveillance versus surgery may depend on the patient’s level of anxiety, researchers found.
The research was published in JAMA Oncology.
The potential to expand criteria for thyroid cancer active surveillance comes amid ongoing concerns surrounding overtreatment. Advances in technology have led to increased detection of small, often indolent thyroid cancers that can likely be monitored safely through active surveillance but may present decision-making challenges for clinicians about whether to treat or watch and wait.
Similar challenges in prostate cancer have been addressed with tiered risk stratification, but such guidelines have not been as firmly established in thyroid cancer.
Guidelines from the American Thyroid Association in 2015 suggest active surveillance as an alternative for very low-risk tumors; however, studies in general have recommended the approach for initial tumor sizes of only up to 1 cm and with growth of less than 3 mm. And overall, active surveillance has not been broadly adopted as an option in thyroid cancer, the authors explained.
To determine if criteria for active surveillance can be safely expanded to tumors up to 2 cm and for those with growth up to 5 mm, Dr. Ho and colleagues compared outcomes among 222 patients with Bethesda 5 or 6 nodules of 2 cm or smaller who received either active surveillance or immediate surgery.
The patients were recruited from Cedars-Sinai Medical Center between 2014 and 2021. Patients were a median 46.8 years old; 76% were female.
The median size of tumors was 11 mm, with about 60% representing larger tumors (10.1 to 20 mm) and 20.6% measuring 15.1 to 20 mm.
About half of patients (n = 112) chose active surveillance. The median size of tumors in this group was smaller than those in the surgery group (10.1 mm vs. 12 mm). Tumor growth exceeded 5 mm in 3.6% of cases, and tumor volume increases of more than 100% occurred in 7% of cases.
With a mean follow-up of 37 months, 90% (101) of those on active surveillance continued with that approach. Notably, 41% of these patients demonstrated a decrease in tumor size, and no cases of metastatic lymph nodes or distant metastases emerged.
Of the 110 patients who elected to undergo immediate surgery, 19% (21) had equivocal-risk or undetermined features on final pathology, but the disease severity for these patients remained classified as stage I thyroid cancer.
The disease-specific survival and overall survival rates were the same in both groups, at 100%.
Although a general concern is that larger tumors may be more likely to grow, it’s important to note that “papillary thyroid cancer exists in a spectrum,” Dr. Ho explained. What that means is “some smaller cancers grow quickly, while some larger cancers are stable for decades.”
“We believe that a 1 cm cutoff is arbitrary,” Dr. Ho said, adding that 2 cm cancers that grow will still be within the therapeutic window for safe surgery.
However, a key factor in treatment decisions is patient fear. The authors also looked at the anxiety levels in both groups, using the 18-item Thyroid Cancer Modified Anxiety Scale.
Among the 59 patients who participated, those who chose immediate surgery had significantly higher baseline anxiety levels, compared with those who opted for active surveillance. Notably, these higher rates of anxiety endured over time, including after the intervention.
“It is unsurprising that patients choosing surgery possess a higher baseline level of worry,” Dr. Ho said. “However, we were astonished to find that such patients retained high levels of worry, even after surgery and presumed cure of their cancer.”
The role of the anxiety, however, underscores the need for clinicians to be mindful of the often profound psychological impacts of cancer, even low-risk disease.
“We always encourage clinicians to educate patients on active surveillance, especially as it gets highlighted more in official guidelines,” Dr. Ho noted. “However, we certainly acknowledge that cancer is a life-changing diagnosis, and the term can carry enormous psychological weight.”
The authors also acknowledged several study limitations, including the single-center, nonrandomized design and small sample size, and urge follow-up analyses to “independently verify our findings.”
In an accompanying editorial, Andrea L. Merrill, MD, from Boston Medical Center, and Priya H. Dedhia, MD, PhD, with Ohio State University Wexner Medical Center, said the findings have important clinical implications.
“This provocative study not only lays the groundwork for expanding active surveillance criteria for low-risk papillary thyroid cancer but may also improve use of current American Thyroid Association guidelines for active surveillance by demonstrating that use of active surveillance for Bethesda 5 or 6 nodules 20 mm or smaller was not associated with an increase in staging or disease-specific mortality,” they write.
The study is also notable for being among the first to assess the role of patient anxiety in the selection of immediate surgery versus active surveillance, Dr. Merrill and Dr. Dedhia added.
“These findings imply that patient anxiety should be an essential component of shared decision-making and selection of strategies for low-risk papillary thyroid cancer,” they say.
The study authors and editorial authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Children with low-risk thyroid cancer can skip radioactive iodine
MONTREAL – Pediatric patients with low-risk differentiated thyroid cancer (DTC) who are spared radioactive iodine (RAI) therapy show no increases in the risk of remission, compared with those who do receive it, supporting guidelines that recommend against use of RAI in such patients.
“In 2015, when the American Thyroid Association [ATA] created their pediatric guidelines [on RAI therapy in DTC], they were taking a leap of faith that these [pediatric DTC] patients would be able to achieve remission without RAI,” said first author Mya Bojarsky, Children’s Hospital of Philadelphia (CHOP), when presenting the findings at the American Thyroid Association annual meeting.
“This is the first study to validate those guidelines and support the sentiment that for ATA low-risk pediatric thyroid cancer patients, withholding RAI therapy is clinically beneficial as it reduces exposure to radiation while having no negative impact on remission,” she said.
Prior to 2015, thyroidectomy in combination with RAI was the standard treatment for DTC in pediatric patients. However, data showing that radiation exposure in children increases the risk of secondary hematologic malignancies by 51% and solid malignancies by 23% over a lifetime raised concerns and led to a push to change the treatment approach.
In response, the 2015 ATA pediatric guidelines recommended that patients not receive RAI for the treatment of DTC that was mostly confined to the thyroid (N0 or minimal N1a disease).
Senior author Andrew J. Bauer, MD, noted that, in addition to being the first study to confirm that withholding RAI in low-risk patients is associated with the same rate of achieving remission as patients treated with RAI, the study also endorses that assessments at 1 year can be reliable predictors of remission.
“For these patients, the 1-year mark post-initial treatment (thyroidectomy) is an early and accurate time point for initial assessment of remission, with increasing rates of remission with continued surveillance (at last clinical follow-up) of approximately 90% 2 years post initial treatment,” said Dr. Bauer, medical director, CHOP, and professor of pediatrics, Perelman School of Medicine, University of Pennsylvania, Philadelphia.
“This approach has recently been validated through a prospective study in adult patients,” he added. A large recent study of 730 patients, published in the New England Journal of Medicine, supported the omission of RAI in low-risk DTC in adults, showing that, compared with those who received RAI, the no-RAI group was noninferior in the occurrence of functional, structural, and biologic events at 3 years.
Safe to eliminate RAI therapy in low-risk DTC in children
With limited data on how or if the change in treatment had an impact on rates of remission in pediatric patients, Ms. Bojarsky and colleagues conducted a retrospective cohort study of patients under the age of 19 years with ATA low-risk DTC who had undergone a total thyroidectomy at CHOP between 2010 and 2020.
Overall, they identified 95 patients, including 50 who had been treated with RAI in addition to thyroidectomy and 45 who did not receive RAI. Among those who did receive RAI, 31 were treated prior to 2015, and 19 were treated after 2019.
For the study, remission was defined as having undetectable thyroglobulin levels as well as no evidence of disease by ultrasound, Ms. Bojarsky said.
“This is important to show, because we want to ensure that as we are reducing our RAI use in the pediatric population, we were not negatively impacting their ability to achieve remission,” she explained.
The percentage of low-risk pediatric patients with DTC treated with RAI had already dropped from 100% in 2010 down to 38% by 2015 when the guidelines were issued, and after a slight rise to 50% by 2018, the practice plummeted to 0% by 2020, the study shows.
In terms of remission, at 1 year post-treatment, 80% of patients who received RAI were in remission, and the rate was even slightly higher, at 84%, among those who did not receive RAI, for a difference that was not significant.
Further looking at disease status as of the last clinical evaluation, 90% in the group treated with RAI had no evidence of disease at a median of 4.9 years of follow-up, and the rate was 87% in the group not receiving RAI, which had a median of 2.7 years of follow-up.
“In ATA low-risk patients, there is no detriment in achieving remission if RAI therapy is withheld,” say investigators.
The median tumor size in the RAI group was larger (19.5 mm vs. 12.0 mm; P < .001), and the primary tumor was T1 in 44% of the RAI group but 82% in the no-RAI group (P < .001).
The lymph node status was N0 in 72% of those receiving RAI and 76% in the no RAI group, which was not significantly different.
The leading risk factors associated with treatment with RAI included larger primary tumor size (OR, 1.07; P = .003), lymph node metastasis (OR, 3.72; P = .036), and surgery pre-2015 (OR, 9.83; P < .001).
RAI administration, N1a disease, and surgery prior to 2015 were not independent risk factors for evidence of persistent disease or indeterminate status.
Ms. Bojarsky has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – Pediatric patients with low-risk differentiated thyroid cancer (DTC) who are spared radioactive iodine (RAI) therapy show no increases in the risk of remission, compared with those who do receive it, supporting guidelines that recommend against use of RAI in such patients.
“In 2015, when the American Thyroid Association [ATA] created their pediatric guidelines [on RAI therapy in DTC], they were taking a leap of faith that these [pediatric DTC] patients would be able to achieve remission without RAI,” said first author Mya Bojarsky, Children’s Hospital of Philadelphia (CHOP), when presenting the findings at the American Thyroid Association annual meeting.
“This is the first study to validate those guidelines and support the sentiment that for ATA low-risk pediatric thyroid cancer patients, withholding RAI therapy is clinically beneficial as it reduces exposure to radiation while having no negative impact on remission,” she said.
Prior to 2015, thyroidectomy in combination with RAI was the standard treatment for DTC in pediatric patients. However, data showing that radiation exposure in children increases the risk of secondary hematologic malignancies by 51% and solid malignancies by 23% over a lifetime raised concerns and led to a push to change the treatment approach.
In response, the 2015 ATA pediatric guidelines recommended that patients not receive RAI for the treatment of DTC that was mostly confined to the thyroid (N0 or minimal N1a disease).
Senior author Andrew J. Bauer, MD, noted that, in addition to being the first study to confirm that withholding RAI in low-risk patients is associated with the same rate of achieving remission as patients treated with RAI, the study also endorses that assessments at 1 year can be reliable predictors of remission.
“For these patients, the 1-year mark post-initial treatment (thyroidectomy) is an early and accurate time point for initial assessment of remission, with increasing rates of remission with continued surveillance (at last clinical follow-up) of approximately 90% 2 years post initial treatment,” said Dr. Bauer, medical director, CHOP, and professor of pediatrics, Perelman School of Medicine, University of Pennsylvania, Philadelphia.
“This approach has recently been validated through a prospective study in adult patients,” he added. A large recent study of 730 patients, published in the New England Journal of Medicine, supported the omission of RAI in low-risk DTC in adults, showing that, compared with those who received RAI, the no-RAI group was noninferior in the occurrence of functional, structural, and biologic events at 3 years.
Safe to eliminate RAI therapy in low-risk DTC in children
With limited data on how or if the change in treatment had an impact on rates of remission in pediatric patients, Ms. Bojarsky and colleagues conducted a retrospective cohort study of patients under the age of 19 years with ATA low-risk DTC who had undergone a total thyroidectomy at CHOP between 2010 and 2020.
Overall, they identified 95 patients, including 50 who had been treated with RAI in addition to thyroidectomy and 45 who did not receive RAI. Among those who did receive RAI, 31 were treated prior to 2015, and 19 were treated after 2019.
For the study, remission was defined as having undetectable thyroglobulin levels as well as no evidence of disease by ultrasound, Ms. Bojarsky said.
“This is important to show, because we want to ensure that as we are reducing our RAI use in the pediatric population, we were not negatively impacting their ability to achieve remission,” she explained.
The percentage of low-risk pediatric patients with DTC treated with RAI had already dropped from 100% in 2010 down to 38% by 2015 when the guidelines were issued, and after a slight rise to 50% by 2018, the practice plummeted to 0% by 2020, the study shows.
In terms of remission, at 1 year post-treatment, 80% of patients who received RAI were in remission, and the rate was even slightly higher, at 84%, among those who did not receive RAI, for a difference that was not significant.
Further looking at disease status as of the last clinical evaluation, 90% in the group treated with RAI had no evidence of disease at a median of 4.9 years of follow-up, and the rate was 87% in the group not receiving RAI, which had a median of 2.7 years of follow-up.
“In ATA low-risk patients, there is no detriment in achieving remission if RAI therapy is withheld,” say investigators.
The median tumor size in the RAI group was larger (19.5 mm vs. 12.0 mm; P < .001), and the primary tumor was T1 in 44% of the RAI group but 82% in the no-RAI group (P < .001).
The lymph node status was N0 in 72% of those receiving RAI and 76% in the no RAI group, which was not significantly different.
The leading risk factors associated with treatment with RAI included larger primary tumor size (OR, 1.07; P = .003), lymph node metastasis (OR, 3.72; P = .036), and surgery pre-2015 (OR, 9.83; P < .001).
RAI administration, N1a disease, and surgery prior to 2015 were not independent risk factors for evidence of persistent disease or indeterminate status.
Ms. Bojarsky has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – Pediatric patients with low-risk differentiated thyroid cancer (DTC) who are spared radioactive iodine (RAI) therapy show no increases in the risk of remission, compared with those who do receive it, supporting guidelines that recommend against use of RAI in such patients.
“In 2015, when the American Thyroid Association [ATA] created their pediatric guidelines [on RAI therapy in DTC], they were taking a leap of faith that these [pediatric DTC] patients would be able to achieve remission without RAI,” said first author Mya Bojarsky, Children’s Hospital of Philadelphia (CHOP), when presenting the findings at the American Thyroid Association annual meeting.
“This is the first study to validate those guidelines and support the sentiment that for ATA low-risk pediatric thyroid cancer patients, withholding RAI therapy is clinically beneficial as it reduces exposure to radiation while having no negative impact on remission,” she said.
Prior to 2015, thyroidectomy in combination with RAI was the standard treatment for DTC in pediatric patients. However, data showing that radiation exposure in children increases the risk of secondary hematologic malignancies by 51% and solid malignancies by 23% over a lifetime raised concerns and led to a push to change the treatment approach.
In response, the 2015 ATA pediatric guidelines recommended that patients not receive RAI for the treatment of DTC that was mostly confined to the thyroid (N0 or minimal N1a disease).
Senior author Andrew J. Bauer, MD, noted that, in addition to being the first study to confirm that withholding RAI in low-risk patients is associated with the same rate of achieving remission as patients treated with RAI, the study also endorses that assessments at 1 year can be reliable predictors of remission.
“For these patients, the 1-year mark post-initial treatment (thyroidectomy) is an early and accurate time point for initial assessment of remission, with increasing rates of remission with continued surveillance (at last clinical follow-up) of approximately 90% 2 years post initial treatment,” said Dr. Bauer, medical director, CHOP, and professor of pediatrics, Perelman School of Medicine, University of Pennsylvania, Philadelphia.
“This approach has recently been validated through a prospective study in adult patients,” he added. A large recent study of 730 patients, published in the New England Journal of Medicine, supported the omission of RAI in low-risk DTC in adults, showing that, compared with those who received RAI, the no-RAI group was noninferior in the occurrence of functional, structural, and biologic events at 3 years.
Safe to eliminate RAI therapy in low-risk DTC in children
With limited data on how or if the change in treatment had an impact on rates of remission in pediatric patients, Ms. Bojarsky and colleagues conducted a retrospective cohort study of patients under the age of 19 years with ATA low-risk DTC who had undergone a total thyroidectomy at CHOP between 2010 and 2020.
Overall, they identified 95 patients, including 50 who had been treated with RAI in addition to thyroidectomy and 45 who did not receive RAI. Among those who did receive RAI, 31 were treated prior to 2015, and 19 were treated after 2019.
For the study, remission was defined as having undetectable thyroglobulin levels as well as no evidence of disease by ultrasound, Ms. Bojarsky said.
“This is important to show, because we want to ensure that as we are reducing our RAI use in the pediatric population, we were not negatively impacting their ability to achieve remission,” she explained.
The percentage of low-risk pediatric patients with DTC treated with RAI had already dropped from 100% in 2010 down to 38% by 2015 when the guidelines were issued, and after a slight rise to 50% by 2018, the practice plummeted to 0% by 2020, the study shows.
In terms of remission, at 1 year post-treatment, 80% of patients who received RAI were in remission, and the rate was even slightly higher, at 84%, among those who did not receive RAI, for a difference that was not significant.
Further looking at disease status as of the last clinical evaluation, 90% in the group treated with RAI had no evidence of disease at a median of 4.9 years of follow-up, and the rate was 87% in the group not receiving RAI, which had a median of 2.7 years of follow-up.
“In ATA low-risk patients, there is no detriment in achieving remission if RAI therapy is withheld,” say investigators.
The median tumor size in the RAI group was larger (19.5 mm vs. 12.0 mm; P < .001), and the primary tumor was T1 in 44% of the RAI group but 82% in the no-RAI group (P < .001).
The lymph node status was N0 in 72% of those receiving RAI and 76% in the no RAI group, which was not significantly different.
The leading risk factors associated with treatment with RAI included larger primary tumor size (OR, 1.07; P = .003), lymph node metastasis (OR, 3.72; P = .036), and surgery pre-2015 (OR, 9.83; P < .001).
RAI administration, N1a disease, and surgery prior to 2015 were not independent risk factors for evidence of persistent disease or indeterminate status.
Ms. Bojarsky has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ATA 2022
Plant-based diet cut hot flashes 78%: WAVS study
Women eating a reduced-fat vegan diet combined with a daily serving of soybeans experienced a 78% reduction in frequency of menopausal hot flashes over 12 weeks, in a small, nonblinded, randomized-controlled trial.
“We do not fully understand yet why this combination works, but it seems that these three elements are key: avoiding animal products, reducing fat, and adding a serving of soybeans,” lead researcher Neal Barnard, MD, explained in a press release. “These new results suggest that a diet change should be considered as a first-line treatment for troublesome vasomotor symptoms, including night sweats and hot flashes,” added Dr. Barnard, who is president of the Physicians Committee for Responsible Medicine, and adjunct professor at George Washington University, Washington.
But, while “the findings from this very small study complement everything we know about the benefits of an excellent diet and the health benefits of soy,” they should be interpreted with some caution, commented Susan Reed, MD, president of the North American Menopause Society, and associate program director of the women’s reproductive research program at the University of Washington, Seattle.
For the trial, called WAVS (Women’s Study for the Alleviation of Vasomotor Symptoms), the researchers randomized 84 postmenopausal women with at least two moderate to severe hot flashes daily to either the intervention or usual diet, with a total of 71 subjects completing the 12-week study, published in Menopause. Criteria for exclusion included any cause of vasomotor symptoms other than natural menopause, current use of a low-fat, vegan diet that includes daily soy products, soy allergy, and body mass index < 18.5 kg/m2.
Participants in the intervention group were asked to avoid animal-derived foods, minimize their use of oils and fatty foods such as nuts and avocados, and include half a cup (86 g) of cooked soybeans daily in their diets. They were also offered 1-hour virtual group meetings each week, in which a registered dietitian or research staff provided information on food preparation and managing common dietary challenges.
Control group participants were asked to continue their usual diets and attend four 1-hour group sessions.
At baseline and then after the 12-week study period, dietary intake was self-recorded for 2 weekdays and 1 weekend day, hot flash frequency and severity was recorded for 1 week using a mobile app, and the effect of menopausal symptoms on quality of life was measured using the vasomotor, psychosocial, physical, and sexual domains of the Menopause-Specific Quality of Life (MENQOL) questionnaire.
Equol production was also assessed in a subset of 15 intervention and 12 control participants who had urinary isoflavone concentrations measured after eating half a cup (86 g) of soybeans twice daily for 3 days. This was based on the theory that diets such as the intervention in this study “seem to foster the growth of gut bacteria capable of converting daidzein to equol,” noted the authors. The ability to produce equol is detected more frequently in individuals following vegetarian diets than in omnivores and … has been proposed as a factor in soy’s apparent health benefits.”
The study found that total hot flash frequency decreased by 78% in the intervention group (P < .001) and 39% (P < .001) in the control group (between-group P = .003), and moderate to severe hot flashes decreased by 88% versus 34%, respectively (from 5.0 to 0.6 per day, P < .001 vs. from 4.4 to 2.9 per day, P < .001; between-group P < .001). Among participants with at least seven moderate to severe hot flashes per day at baseline, moderate to severe hot flashes decreased by 93% (from 10.6 to 0.7 per day) in the intervention group (P < .001) and 36% (from 9.0 to 5.8 per day) in the control group (P = .01, between-group P < .001). The changes in hot flashes were paralleled by changes in the MENQOL findings, with significant between-group differences in the vasomotor (P = 0.004), physical (P = 0.01), and sexual (P = 0.03) domains.
Changes in frequency of severe hot flashes correlated directly with changes in fat intake, and inversely with changes in carbohydrate and fiber intake, such that “the greater the reduction in fat intake and the greater the increases in carbohydrate and fiber consumption, the greater the reduction in severe hot flashes,” noted the researchers. Mean body weight also decreased by 3.6 kg in the intervention group and 0.2 kg in the control group (P < .001). “Equol-production status had no apparent effect on hot flashes,” they added.
The study is the second phase of WAVS, which comprises two parts, the first of which showed similar results, but was conducted in the fall, raising questions about whether cooler temperatures were partly responsible for the results. Phase 2 of WAVS enrolled participants in the spring “ruling out the effect of outside temperature,” noted the authors.
“Eating a healthy diet at midlife is so important for long-term health and a sense of well-being for peri- and postmenopausal women,” said Dr Reed, but she urged caution in interpreting the findings. “This was an unblinded study,” she told this news organization. “Women were recruited to this study anticipating that they would be in a study on a soy diet. Individuals who sign up for a study are hoping for benefit from the intervention. The controls who don’t get the soy diet are often disappointed, so there is no benefit from a nonblinded control arm for their hot flashes. And that is exactly what we saw here. Blinded studies can hide what you are getting, so everyone in the study (intervention and controls) has the same anticipated benefit. But you cannot blind a soy diet.”
Dr. Reed also noted that, while the biologic mechanism of benefit should be equol production, this was not shown – given that both equol producers and nonproducers in the soy intervention reported marked symptom reduction.
“Only prior studies with estrogen interventions have observed reductions of hot flashes of the amount reported here,” she concluded. “Hopefully future large studies will clarify the role of soy diet for decreasing hot flashes.”
Dr. Barnard writes books and articles and gives lectures related to nutrition and health and has received royalties and honoraria from these sources. Dr. Reed has no relevant disclosures.
Women eating a reduced-fat vegan diet combined with a daily serving of soybeans experienced a 78% reduction in frequency of menopausal hot flashes over 12 weeks, in a small, nonblinded, randomized-controlled trial.
“We do not fully understand yet why this combination works, but it seems that these three elements are key: avoiding animal products, reducing fat, and adding a serving of soybeans,” lead researcher Neal Barnard, MD, explained in a press release. “These new results suggest that a diet change should be considered as a first-line treatment for troublesome vasomotor symptoms, including night sweats and hot flashes,” added Dr. Barnard, who is president of the Physicians Committee for Responsible Medicine, and adjunct professor at George Washington University, Washington.
But, while “the findings from this very small study complement everything we know about the benefits of an excellent diet and the health benefits of soy,” they should be interpreted with some caution, commented Susan Reed, MD, president of the North American Menopause Society, and associate program director of the women’s reproductive research program at the University of Washington, Seattle.
For the trial, called WAVS (Women’s Study for the Alleviation of Vasomotor Symptoms), the researchers randomized 84 postmenopausal women with at least two moderate to severe hot flashes daily to either the intervention or usual diet, with a total of 71 subjects completing the 12-week study, published in Menopause. Criteria for exclusion included any cause of vasomotor symptoms other than natural menopause, current use of a low-fat, vegan diet that includes daily soy products, soy allergy, and body mass index < 18.5 kg/m2.
Participants in the intervention group were asked to avoid animal-derived foods, minimize their use of oils and fatty foods such as nuts and avocados, and include half a cup (86 g) of cooked soybeans daily in their diets. They were also offered 1-hour virtual group meetings each week, in which a registered dietitian or research staff provided information on food preparation and managing common dietary challenges.
Control group participants were asked to continue their usual diets and attend four 1-hour group sessions.
At baseline and then after the 12-week study period, dietary intake was self-recorded for 2 weekdays and 1 weekend day, hot flash frequency and severity was recorded for 1 week using a mobile app, and the effect of menopausal symptoms on quality of life was measured using the vasomotor, psychosocial, physical, and sexual domains of the Menopause-Specific Quality of Life (MENQOL) questionnaire.
Equol production was also assessed in a subset of 15 intervention and 12 control participants who had urinary isoflavone concentrations measured after eating half a cup (86 g) of soybeans twice daily for 3 days. This was based on the theory that diets such as the intervention in this study “seem to foster the growth of gut bacteria capable of converting daidzein to equol,” noted the authors. The ability to produce equol is detected more frequently in individuals following vegetarian diets than in omnivores and … has been proposed as a factor in soy’s apparent health benefits.”
The study found that total hot flash frequency decreased by 78% in the intervention group (P < .001) and 39% (P < .001) in the control group (between-group P = .003), and moderate to severe hot flashes decreased by 88% versus 34%, respectively (from 5.0 to 0.6 per day, P < .001 vs. from 4.4 to 2.9 per day, P < .001; between-group P < .001). Among participants with at least seven moderate to severe hot flashes per day at baseline, moderate to severe hot flashes decreased by 93% (from 10.6 to 0.7 per day) in the intervention group (P < .001) and 36% (from 9.0 to 5.8 per day) in the control group (P = .01, between-group P < .001). The changes in hot flashes were paralleled by changes in the MENQOL findings, with significant between-group differences in the vasomotor (P = 0.004), physical (P = 0.01), and sexual (P = 0.03) domains.
Changes in frequency of severe hot flashes correlated directly with changes in fat intake, and inversely with changes in carbohydrate and fiber intake, such that “the greater the reduction in fat intake and the greater the increases in carbohydrate and fiber consumption, the greater the reduction in severe hot flashes,” noted the researchers. Mean body weight also decreased by 3.6 kg in the intervention group and 0.2 kg in the control group (P < .001). “Equol-production status had no apparent effect on hot flashes,” they added.
The study is the second phase of WAVS, which comprises two parts, the first of which showed similar results, but was conducted in the fall, raising questions about whether cooler temperatures were partly responsible for the results. Phase 2 of WAVS enrolled participants in the spring “ruling out the effect of outside temperature,” noted the authors.
“Eating a healthy diet at midlife is so important for long-term health and a sense of well-being for peri- and postmenopausal women,” said Dr Reed, but she urged caution in interpreting the findings. “This was an unblinded study,” she told this news organization. “Women were recruited to this study anticipating that they would be in a study on a soy diet. Individuals who sign up for a study are hoping for benefit from the intervention. The controls who don’t get the soy diet are often disappointed, so there is no benefit from a nonblinded control arm for their hot flashes. And that is exactly what we saw here. Blinded studies can hide what you are getting, so everyone in the study (intervention and controls) has the same anticipated benefit. But you cannot blind a soy diet.”
Dr. Reed also noted that, while the biologic mechanism of benefit should be equol production, this was not shown – given that both equol producers and nonproducers in the soy intervention reported marked symptom reduction.
“Only prior studies with estrogen interventions have observed reductions of hot flashes of the amount reported here,” she concluded. “Hopefully future large studies will clarify the role of soy diet for decreasing hot flashes.”
Dr. Barnard writes books and articles and gives lectures related to nutrition and health and has received royalties and honoraria from these sources. Dr. Reed has no relevant disclosures.
Women eating a reduced-fat vegan diet combined with a daily serving of soybeans experienced a 78% reduction in frequency of menopausal hot flashes over 12 weeks, in a small, nonblinded, randomized-controlled trial.
“We do not fully understand yet why this combination works, but it seems that these three elements are key: avoiding animal products, reducing fat, and adding a serving of soybeans,” lead researcher Neal Barnard, MD, explained in a press release. “These new results suggest that a diet change should be considered as a first-line treatment for troublesome vasomotor symptoms, including night sweats and hot flashes,” added Dr. Barnard, who is president of the Physicians Committee for Responsible Medicine, and adjunct professor at George Washington University, Washington.
But, while “the findings from this very small study complement everything we know about the benefits of an excellent diet and the health benefits of soy,” they should be interpreted with some caution, commented Susan Reed, MD, president of the North American Menopause Society, and associate program director of the women’s reproductive research program at the University of Washington, Seattle.
For the trial, called WAVS (Women’s Study for the Alleviation of Vasomotor Symptoms), the researchers randomized 84 postmenopausal women with at least two moderate to severe hot flashes daily to either the intervention or usual diet, with a total of 71 subjects completing the 12-week study, published in Menopause. Criteria for exclusion included any cause of vasomotor symptoms other than natural menopause, current use of a low-fat, vegan diet that includes daily soy products, soy allergy, and body mass index < 18.5 kg/m2.
Participants in the intervention group were asked to avoid animal-derived foods, minimize their use of oils and fatty foods such as nuts and avocados, and include half a cup (86 g) of cooked soybeans daily in their diets. They were also offered 1-hour virtual group meetings each week, in which a registered dietitian or research staff provided information on food preparation and managing common dietary challenges.
Control group participants were asked to continue their usual diets and attend four 1-hour group sessions.
At baseline and then after the 12-week study period, dietary intake was self-recorded for 2 weekdays and 1 weekend day, hot flash frequency and severity was recorded for 1 week using a mobile app, and the effect of menopausal symptoms on quality of life was measured using the vasomotor, psychosocial, physical, and sexual domains of the Menopause-Specific Quality of Life (MENQOL) questionnaire.
Equol production was also assessed in a subset of 15 intervention and 12 control participants who had urinary isoflavone concentrations measured after eating half a cup (86 g) of soybeans twice daily for 3 days. This was based on the theory that diets such as the intervention in this study “seem to foster the growth of gut bacteria capable of converting daidzein to equol,” noted the authors. The ability to produce equol is detected more frequently in individuals following vegetarian diets than in omnivores and … has been proposed as a factor in soy’s apparent health benefits.”
The study found that total hot flash frequency decreased by 78% in the intervention group (P < .001) and 39% (P < .001) in the control group (between-group P = .003), and moderate to severe hot flashes decreased by 88% versus 34%, respectively (from 5.0 to 0.6 per day, P < .001 vs. from 4.4 to 2.9 per day, P < .001; between-group P < .001). Among participants with at least seven moderate to severe hot flashes per day at baseline, moderate to severe hot flashes decreased by 93% (from 10.6 to 0.7 per day) in the intervention group (P < .001) and 36% (from 9.0 to 5.8 per day) in the control group (P = .01, between-group P < .001). The changes in hot flashes were paralleled by changes in the MENQOL findings, with significant between-group differences in the vasomotor (P = 0.004), physical (P = 0.01), and sexual (P = 0.03) domains.
Changes in frequency of severe hot flashes correlated directly with changes in fat intake, and inversely with changes in carbohydrate and fiber intake, such that “the greater the reduction in fat intake and the greater the increases in carbohydrate and fiber consumption, the greater the reduction in severe hot flashes,” noted the researchers. Mean body weight also decreased by 3.6 kg in the intervention group and 0.2 kg in the control group (P < .001). “Equol-production status had no apparent effect on hot flashes,” they added.
The study is the second phase of WAVS, which comprises two parts, the first of which showed similar results, but was conducted in the fall, raising questions about whether cooler temperatures were partly responsible for the results. Phase 2 of WAVS enrolled participants in the spring “ruling out the effect of outside temperature,” noted the authors.
“Eating a healthy diet at midlife is so important for long-term health and a sense of well-being for peri- and postmenopausal women,” said Dr Reed, but she urged caution in interpreting the findings. “This was an unblinded study,” she told this news organization. “Women were recruited to this study anticipating that they would be in a study on a soy diet. Individuals who sign up for a study are hoping for benefit from the intervention. The controls who don’t get the soy diet are often disappointed, so there is no benefit from a nonblinded control arm for their hot flashes. And that is exactly what we saw here. Blinded studies can hide what you are getting, so everyone in the study (intervention and controls) has the same anticipated benefit. But you cannot blind a soy diet.”
Dr. Reed also noted that, while the biologic mechanism of benefit should be equol production, this was not shown – given that both equol producers and nonproducers in the soy intervention reported marked symptom reduction.
“Only prior studies with estrogen interventions have observed reductions of hot flashes of the amount reported here,” she concluded. “Hopefully future large studies will clarify the role of soy diet for decreasing hot flashes.”
Dr. Barnard writes books and articles and gives lectures related to nutrition and health and has received royalties and honoraria from these sources. Dr. Reed has no relevant disclosures.
Finerenone: ‘Striking’ cut in pneumonia, COVID-19 risks
The nonsteroidal mineralocorticoid receptor antagonist finerenone (Kerendia) unexpectedly showed that it might protect against incident infective pneumonia and COVID-19. The finding was based on secondary analyses run on more than 13,000 people enrolled in the two pivotal trials for finerenone.
Finerenone was approved by the Food and Drug Administration in 2021 for slowing progressive renal dysfunction and preventing cardiovascular events in adults with type 2 diabetes and chronic kidney disease (CKD).
‘Striking reduction in the risk of pneumonia’
The “striking reduction in risk of pneumonia” in a new analysis suggests that “the propagation of pulmonary infection into lobar or bronchial consolidation may be reduced by finerenone,” write Bertram Pitt, MD, and coauthors in a report published on October 26 in JAMA Network Open.
They also suggest that if further studies confirm that finerenone treatment reduces complications from pneumonia and COVID-19, it would have “significant medical implications,” especially because of the limited treatment options now available for complications from COVID-19.
The new analyses used the FIDELITY dataset, a prespecified merging of results from the FIDELIO-DKD and FIGARO-DKD trials, which together enrolled 13,026 people with type 2 diabetes and CKD, as determined on the basis of the patients’ having a urine albumin-to-creatinine ratio of at least 30 mg/g.
The primary outcomes of these trials showed that treatment with finerenone led to significant slowing of the progression of CKD and a significant reduction in the incidence of cardiovascular events, compared with placebo during median follow-up of 3 years.
The new, secondary analyses focused on the 6.0% of participants in whom there was evidence of pneumonia and the 1.6% in whom there was evidence of having COVID-19. Pneumonia was the most common serious adverse event in the two trials, a finding consistent with the documented risk for pneumonia faced by people with CKD.
Finerenone linked with a 29% relative reduction in pneumonia
When analyzed by treatment, the incidence of pneumonia was 4.7% among those who received finerenone and 6.7% among those who received placebo. This translated into a significant relative risk reduction of 29% associated with finerenone treatment.
Analysis of COVID-19 adverse events showed a 1.3% incidence among those who received finerenone and a 1.8% incidence among those in the placebo group, which translated into a significant 27% relative risk reduction linked with finerenone treatment.
In contrast, the data showed no reduced incidence of several other respiratory infections among the finerenone recipients, including nasopharyngitis, bronchitis, and influenza. The data also showed no signal that pneumonia or COVID-19 was more severe among the people who did not receive finerenone, nor did finerenone treatment appear to affect pneumonia recovery.
Analysis based on adverse events reports
These secondary analyses are far from definitive. The authors relied on pneumonia and COVID-19 being reported as adverse events. Each investigator diagnosed pneumonia at their discretion, and the trials did not specify diagnostic criteria. The authors also acknowledge that testing for COVID-19 was “not widespread” and that one of the two pivotal trials largely ran prior to the onset of the COVID-19 pandemic so that only 6 participants developed COVID-19 symptoms out of more than 5,700 enrolled.
The authors hypothesize that several actions of finerenone might potentially help mediate an effect on pneumonia and COVID-19: improvements in pulmonary inflammation and fibrosis, upregulation of expression of angiotensin converting enzyme 2, and amelioration of right heart pressure and pulmonary congestion. Also, antagonizing the mineralocorticoid receptor on monocytes and macrophages may block macrophage infiltration and accumulation of active macrophages, which can mediate the pulmonary tissue damage caused by COVID-19.
The FIDELIO-DKD and FIGARO-DKD trials and the FIDELITY combined database were sponsored by Bayer, the company that markets finerenone (Kerendia). Dr. Pitt has received personal fees from Bayer and personal fees and stock options from numerous other companies. Several coauthors reported having a financial relationship with Bayer, as well as with other companies.
A version of this article first appeared on Medscape.com.
The nonsteroidal mineralocorticoid receptor antagonist finerenone (Kerendia) unexpectedly showed that it might protect against incident infective pneumonia and COVID-19. The finding was based on secondary analyses run on more than 13,000 people enrolled in the two pivotal trials for finerenone.
Finerenone was approved by the Food and Drug Administration in 2021 for slowing progressive renal dysfunction and preventing cardiovascular events in adults with type 2 diabetes and chronic kidney disease (CKD).
‘Striking reduction in the risk of pneumonia’
The “striking reduction in risk of pneumonia” in a new analysis suggests that “the propagation of pulmonary infection into lobar or bronchial consolidation may be reduced by finerenone,” write Bertram Pitt, MD, and coauthors in a report published on October 26 in JAMA Network Open.
They also suggest that if further studies confirm that finerenone treatment reduces complications from pneumonia and COVID-19, it would have “significant medical implications,” especially because of the limited treatment options now available for complications from COVID-19.
The new analyses used the FIDELITY dataset, a prespecified merging of results from the FIDELIO-DKD and FIGARO-DKD trials, which together enrolled 13,026 people with type 2 diabetes and CKD, as determined on the basis of the patients’ having a urine albumin-to-creatinine ratio of at least 30 mg/g.
The primary outcomes of these trials showed that treatment with finerenone led to significant slowing of the progression of CKD and a significant reduction in the incidence of cardiovascular events, compared with placebo during median follow-up of 3 years.
The new, secondary analyses focused on the 6.0% of participants in whom there was evidence of pneumonia and the 1.6% in whom there was evidence of having COVID-19. Pneumonia was the most common serious adverse event in the two trials, a finding consistent with the documented risk for pneumonia faced by people with CKD.
Finerenone linked with a 29% relative reduction in pneumonia
When analyzed by treatment, the incidence of pneumonia was 4.7% among those who received finerenone and 6.7% among those who received placebo. This translated into a significant relative risk reduction of 29% associated with finerenone treatment.
Analysis of COVID-19 adverse events showed a 1.3% incidence among those who received finerenone and a 1.8% incidence among those in the placebo group, which translated into a significant 27% relative risk reduction linked with finerenone treatment.
In contrast, the data showed no reduced incidence of several other respiratory infections among the finerenone recipients, including nasopharyngitis, bronchitis, and influenza. The data also showed no signal that pneumonia or COVID-19 was more severe among the people who did not receive finerenone, nor did finerenone treatment appear to affect pneumonia recovery.
Analysis based on adverse events reports
These secondary analyses are far from definitive. The authors relied on pneumonia and COVID-19 being reported as adverse events. Each investigator diagnosed pneumonia at their discretion, and the trials did not specify diagnostic criteria. The authors also acknowledge that testing for COVID-19 was “not widespread” and that one of the two pivotal trials largely ran prior to the onset of the COVID-19 pandemic so that only 6 participants developed COVID-19 symptoms out of more than 5,700 enrolled.
The authors hypothesize that several actions of finerenone might potentially help mediate an effect on pneumonia and COVID-19: improvements in pulmonary inflammation and fibrosis, upregulation of expression of angiotensin converting enzyme 2, and amelioration of right heart pressure and pulmonary congestion. Also, antagonizing the mineralocorticoid receptor on monocytes and macrophages may block macrophage infiltration and accumulation of active macrophages, which can mediate the pulmonary tissue damage caused by COVID-19.
The FIDELIO-DKD and FIGARO-DKD trials and the FIDELITY combined database were sponsored by Bayer, the company that markets finerenone (Kerendia). Dr. Pitt has received personal fees from Bayer and personal fees and stock options from numerous other companies. Several coauthors reported having a financial relationship with Bayer, as well as with other companies.
A version of this article first appeared on Medscape.com.
The nonsteroidal mineralocorticoid receptor antagonist finerenone (Kerendia) unexpectedly showed that it might protect against incident infective pneumonia and COVID-19. The finding was based on secondary analyses run on more than 13,000 people enrolled in the two pivotal trials for finerenone.
Finerenone was approved by the Food and Drug Administration in 2021 for slowing progressive renal dysfunction and preventing cardiovascular events in adults with type 2 diabetes and chronic kidney disease (CKD).
‘Striking reduction in the risk of pneumonia’
The “striking reduction in risk of pneumonia” in a new analysis suggests that “the propagation of pulmonary infection into lobar or bronchial consolidation may be reduced by finerenone,” write Bertram Pitt, MD, and coauthors in a report published on October 26 in JAMA Network Open.
They also suggest that if further studies confirm that finerenone treatment reduces complications from pneumonia and COVID-19, it would have “significant medical implications,” especially because of the limited treatment options now available for complications from COVID-19.
The new analyses used the FIDELITY dataset, a prespecified merging of results from the FIDELIO-DKD and FIGARO-DKD trials, which together enrolled 13,026 people with type 2 diabetes and CKD, as determined on the basis of the patients’ having a urine albumin-to-creatinine ratio of at least 30 mg/g.
The primary outcomes of these trials showed that treatment with finerenone led to significant slowing of the progression of CKD and a significant reduction in the incidence of cardiovascular events, compared with placebo during median follow-up of 3 years.
The new, secondary analyses focused on the 6.0% of participants in whom there was evidence of pneumonia and the 1.6% in whom there was evidence of having COVID-19. Pneumonia was the most common serious adverse event in the two trials, a finding consistent with the documented risk for pneumonia faced by people with CKD.
Finerenone linked with a 29% relative reduction in pneumonia
When analyzed by treatment, the incidence of pneumonia was 4.7% among those who received finerenone and 6.7% among those who received placebo. This translated into a significant relative risk reduction of 29% associated with finerenone treatment.
Analysis of COVID-19 adverse events showed a 1.3% incidence among those who received finerenone and a 1.8% incidence among those in the placebo group, which translated into a significant 27% relative risk reduction linked with finerenone treatment.
In contrast, the data showed no reduced incidence of several other respiratory infections among the finerenone recipients, including nasopharyngitis, bronchitis, and influenza. The data also showed no signal that pneumonia or COVID-19 was more severe among the people who did not receive finerenone, nor did finerenone treatment appear to affect pneumonia recovery.
Analysis based on adverse events reports
These secondary analyses are far from definitive. The authors relied on pneumonia and COVID-19 being reported as adverse events. Each investigator diagnosed pneumonia at their discretion, and the trials did not specify diagnostic criteria. The authors also acknowledge that testing for COVID-19 was “not widespread” and that one of the two pivotal trials largely ran prior to the onset of the COVID-19 pandemic so that only 6 participants developed COVID-19 symptoms out of more than 5,700 enrolled.
The authors hypothesize that several actions of finerenone might potentially help mediate an effect on pneumonia and COVID-19: improvements in pulmonary inflammation and fibrosis, upregulation of expression of angiotensin converting enzyme 2, and amelioration of right heart pressure and pulmonary congestion. Also, antagonizing the mineralocorticoid receptor on monocytes and macrophages may block macrophage infiltration and accumulation of active macrophages, which can mediate the pulmonary tissue damage caused by COVID-19.
The FIDELIO-DKD and FIGARO-DKD trials and the FIDELITY combined database were sponsored by Bayer, the company that markets finerenone (Kerendia). Dr. Pitt has received personal fees from Bayer and personal fees and stock options from numerous other companies. Several coauthors reported having a financial relationship with Bayer, as well as with other companies.
A version of this article first appeared on Medscape.com.