User login
Nominate Yourself or a Colleague for the SHM Board of Directors
Interested in becoming a leader in hospital medicine? Know someone who would be a great leader? SHM is seeking nominations for three open seats for its board of directors. These positions serve a three-year term beginning in May 2013.
Take this opportunity to help determine the course of this rapidly growing specialty.
Send all nominations—including a one-page nomination letter, CV, and recent headshot—no later than Oct. 31 to Joy Barnosky at [email protected]. For full eligibility and nomination requirements, visit www.hospitalmedicine.org and click on “About SHM,” then “Election Information.”
If you have questions, email [email protected] or call 267-702-2614.
Interested in becoming a leader in hospital medicine? Know someone who would be a great leader? SHM is seeking nominations for three open seats for its board of directors. These positions serve a three-year term beginning in May 2013.
Take this opportunity to help determine the course of this rapidly growing specialty.
Send all nominations—including a one-page nomination letter, CV, and recent headshot—no later than Oct. 31 to Joy Barnosky at [email protected]. For full eligibility and nomination requirements, visit www.hospitalmedicine.org and click on “About SHM,” then “Election Information.”
If you have questions, email [email protected] or call 267-702-2614.
Interested in becoming a leader in hospital medicine? Know someone who would be a great leader? SHM is seeking nominations for three open seats for its board of directors. These positions serve a three-year term beginning in May 2013.
Take this opportunity to help determine the course of this rapidly growing specialty.
Send all nominations—including a one-page nomination letter, CV, and recent headshot—no later than Oct. 31 to Joy Barnosky at [email protected]. For full eligibility and nomination requirements, visit www.hospitalmedicine.org and click on “About SHM,” then “Election Information.”
If you have questions, email [email protected] or call 267-702-2614.
Hospitalists' Evolving Scope of Practice
Last month The Hospitalist reported new 2012 State of Hospital Medicine survey data showing that 57% of those adult medicine hospitalist groups providing surgical comanagement services typically do so as admitting/attending physician, as opposed to serving in a consultant role. For groups providing medical subspecialty comanagement, the admitting/attending rate was a whopping 85%.
But just how common is comanagement these days, and what else do we know about hospitalists’ evolving scope of practice? It’s hard to compare this year’s survey results with those presented in last year’s report because previously this information was reported for all HM groups combined while this year adult and pediatric groups are reported separately. In addition, the survey population was different this year since MGMA survey participants were no longer included. But if you ask almost anyone working in HM today, they probably will tell you that the pressure to assume increased comanagement responsibilities for more and more types of patients is intense.
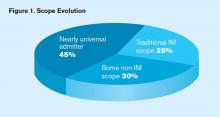
One of the new questions this year asked respondents to characterize their scope of services by selecting one of the following three options:
- We maintain a scope of practice that resembles traditional hospital-based internal medicine (or pediatrics, if applicable).
- Our practice scope has evolved to include some services that are outside of traditional internal medicine practice (or pediatrics, if applicable), e.g., admitting/managing patients with intracranial hemorrhage, small bowel obstruction or hip fracture.
- Our practice scope has evolved to encompass admitting a full range of hospital patients in the age group for which we are responsible, with the exception of OB and emergency surgery patients (i.e. nearly “universal admitter”).
A remarkable 45% of adult medicine hospitalist groups reported that their scope has evolved toward a nearly universal admitter role, while only a quarter of such groups reported maintaining a traditional internal medicine scope (see Figure 1, below). The broader scope of practice was more common in the Midwest, among private hospitalist-only groups and those employed by management companies, and in non-teaching hospitals. Not surprisingly, academic hospital medicine groups and those employed by university/medical schools tended to maintain narrower internal medicine-focused scopes.
As to the prevalence of comanagement, this year 94% of groups serving adults only reported providing surgical comanagement services (either admitting or consulting), while 70% reported providing comanagement for medical subspecialty patients. Seven years ago, SHM’s 2005 survey found that 87% of adult medicine groups provided surgical comanagement (SHM didn’t ask about medical comanagement).
So yes, the proportion of groups providing surgical comanagement has increased, but not dramatically.
Although we don’t know for sure since the question wasn’t asked in 2005, I suspect we’d find that most groups providing surgical (and probably medical subspecialty) comanagement in 2005 served as consultants; today the preponderance serve as admitting/attending physician for such patients. That’s a significant scope evolution that’s not obvious from just looking at the percent of groups that provide comanagement.
A comprehensive list of services routinely provided by HM groups is available in the new 2012 State of Hospital Medicine report, with breakdowns by group type, geographic region, employment model, and academic/teaching status. Hopefully, SHM will continue to survey this important topic so that scope evolution can be tracked going forward.
Last month The Hospitalist reported new 2012 State of Hospital Medicine survey data showing that 57% of those adult medicine hospitalist groups providing surgical comanagement services typically do so as admitting/attending physician, as opposed to serving in a consultant role. For groups providing medical subspecialty comanagement, the admitting/attending rate was a whopping 85%.
But just how common is comanagement these days, and what else do we know about hospitalists’ evolving scope of practice? It’s hard to compare this year’s survey results with those presented in last year’s report because previously this information was reported for all HM groups combined while this year adult and pediatric groups are reported separately. In addition, the survey population was different this year since MGMA survey participants were no longer included. But if you ask almost anyone working in HM today, they probably will tell you that the pressure to assume increased comanagement responsibilities for more and more types of patients is intense.
One of the new questions this year asked respondents to characterize their scope of services by selecting one of the following three options:
- We maintain a scope of practice that resembles traditional hospital-based internal medicine (or pediatrics, if applicable).
- Our practice scope has evolved to include some services that are outside of traditional internal medicine practice (or pediatrics, if applicable), e.g., admitting/managing patients with intracranial hemorrhage, small bowel obstruction or hip fracture.
- Our practice scope has evolved to encompass admitting a full range of hospital patients in the age group for which we are responsible, with the exception of OB and emergency surgery patients (i.e. nearly “universal admitter”).
A remarkable 45% of adult medicine hospitalist groups reported that their scope has evolved toward a nearly universal admitter role, while only a quarter of such groups reported maintaining a traditional internal medicine scope (see Figure 1, below). The broader scope of practice was more common in the Midwest, among private hospitalist-only groups and those employed by management companies, and in non-teaching hospitals. Not surprisingly, academic hospital medicine groups and those employed by university/medical schools tended to maintain narrower internal medicine-focused scopes.
As to the prevalence of comanagement, this year 94% of groups serving adults only reported providing surgical comanagement services (either admitting or consulting), while 70% reported providing comanagement for medical subspecialty patients. Seven years ago, SHM’s 2005 survey found that 87% of adult medicine groups provided surgical comanagement (SHM didn’t ask about medical comanagement).
So yes, the proportion of groups providing surgical comanagement has increased, but not dramatically.
Although we don’t know for sure since the question wasn’t asked in 2005, I suspect we’d find that most groups providing surgical (and probably medical subspecialty) comanagement in 2005 served as consultants; today the preponderance serve as admitting/attending physician for such patients. That’s a significant scope evolution that’s not obvious from just looking at the percent of groups that provide comanagement.
A comprehensive list of services routinely provided by HM groups is available in the new 2012 State of Hospital Medicine report, with breakdowns by group type, geographic region, employment model, and academic/teaching status. Hopefully, SHM will continue to survey this important topic so that scope evolution can be tracked going forward.
Last month The Hospitalist reported new 2012 State of Hospital Medicine survey data showing that 57% of those adult medicine hospitalist groups providing surgical comanagement services typically do so as admitting/attending physician, as opposed to serving in a consultant role. For groups providing medical subspecialty comanagement, the admitting/attending rate was a whopping 85%.
But just how common is comanagement these days, and what else do we know about hospitalists’ evolving scope of practice? It’s hard to compare this year’s survey results with those presented in last year’s report because previously this information was reported for all HM groups combined while this year adult and pediatric groups are reported separately. In addition, the survey population was different this year since MGMA survey participants were no longer included. But if you ask almost anyone working in HM today, they probably will tell you that the pressure to assume increased comanagement responsibilities for more and more types of patients is intense.
One of the new questions this year asked respondents to characterize their scope of services by selecting one of the following three options:
- We maintain a scope of practice that resembles traditional hospital-based internal medicine (or pediatrics, if applicable).
- Our practice scope has evolved to include some services that are outside of traditional internal medicine practice (or pediatrics, if applicable), e.g., admitting/managing patients with intracranial hemorrhage, small bowel obstruction or hip fracture.
- Our practice scope has evolved to encompass admitting a full range of hospital patients in the age group for which we are responsible, with the exception of OB and emergency surgery patients (i.e. nearly “universal admitter”).
A remarkable 45% of adult medicine hospitalist groups reported that their scope has evolved toward a nearly universal admitter role, while only a quarter of such groups reported maintaining a traditional internal medicine scope (see Figure 1, below). The broader scope of practice was more common in the Midwest, among private hospitalist-only groups and those employed by management companies, and in non-teaching hospitals. Not surprisingly, academic hospital medicine groups and those employed by university/medical schools tended to maintain narrower internal medicine-focused scopes.
As to the prevalence of comanagement, this year 94% of groups serving adults only reported providing surgical comanagement services (either admitting or consulting), while 70% reported providing comanagement for medical subspecialty patients. Seven years ago, SHM’s 2005 survey found that 87% of adult medicine groups provided surgical comanagement (SHM didn’t ask about medical comanagement).
So yes, the proportion of groups providing surgical comanagement has increased, but not dramatically.
Although we don’t know for sure since the question wasn’t asked in 2005, I suspect we’d find that most groups providing surgical (and probably medical subspecialty) comanagement in 2005 served as consultants; today the preponderance serve as admitting/attending physician for such patients. That’s a significant scope evolution that’s not obvious from just looking at the percent of groups that provide comanagement.
A comprehensive list of services routinely provided by HM groups is available in the new 2012 State of Hospital Medicine report, with breakdowns by group type, geographic region, employment model, and academic/teaching status. Hopefully, SHM will continue to survey this important topic so that scope evolution can be tracked going forward.
ITL: Physician Reviews of HM-Relevant Research
In This Edition
Literature At A Glance
A guide to this month’s studies
- Prediction tool for neurological outcomes after in-hospital cardiac arrest
- Radiation exposure in integrated healthcare systems, 1996-2010
- Postoperative troponin predicts 30-day mortality
- Clinical prediction model of mortality in acute heart failure
- Indwelling pleural catheter vs. talc pleurodesis via chest tube
- Early surgery for high-risk, native-valve endocarditis patients
- Risk factors after ED visit for syncope
- Acute hyperglycemia in CAP patients
- Hospital delirium associated with cognitive decline, institutionalization, and death
- Seven-day ciprofloxacin effective against acute pyelonephritis
- Advance directives in community patients with heart failure
- Chlorhexidine bathing effective against CVC-associated bloodstream infections
- Simulation training improves lumbar puncture skills
- PCP referrals to hospitals and publicly reported data
- Medication reconciliation best practices
Prediction Tool Validated for Prognosticating Favorable Neurological Outcome after In-Hospital Cardiac Arrest
Clinical question: Does the Cardiac Arrest Survival Post Resuscitation In-Hospital (CASPRI) score accurately predict favorable neurological outcomes?
Background: Previous cardiac arrest prediction models have been focused on survival to discharge without consideration of neurological status and have not been translated into valid bedside prognostication tools. Neurologic prognosis can assist patients, families, and physicians in decisions about continued goals of care post-arrest.
Study design: Retrospective cohort study.
Setting: Acute-care hospitals.
Synopsis: Using the Get with the Guidelines Resuscitation Registry, 551 hospitals identified 42,957 patients who were successfully resuscitated from an in-hospital cardiac arrest from January 2000 to October 2009. Researchers developed a simple prediction tool for favorable neurological outcomes (defined as “no” or “moderate” neurological disability) at discharge. The 11 predictors used to calculate the CASPRI score are age; time to defibrillation; pre-arrest neurological status; hospital location; duration of resuscitation; and pre-arrest comorbidities: mechanical ventilation, renal insufficiency, hepatic insufficiency, sepsis, malignancy,
and hypotension.
Rates of favorable neurological outcome were similar between derivation cohort (24.6%) and validation cohort (24.5%). The model had excellent discrimination with a C score of 0.80. Probability of favorable neurological survival ranged from 70.7% in the top decile of patients (CASPRI <10) and 2.8% in bottom decile (CASPRI ≥ 28).
This tool is not generalizable to patients with out-of-hospital arrest or undergoing therapeutic hypothermia.
Bottom line: CASPRI is a simple bedside tool validated to estimate probability of favorable neurological outcome after in-hospital cardiac arrest.
Citation: Chan PS, Spertus JA, Krumholz HA, et al. A validated prediction tool for initial survivors in in-hospital cardiac arrest. Arch Intern Med. 2012;172(12):947-953.
Increased Use of Radiologic Imaging and Associated Radiation Exposure in Integrated Healthcare Systems, 1996-2010
Clinical question: How much has imaging utilization and associated radiation exposure increased over 15 years in integrated healthcare systems independent of financial incentives in a fee-for-service system?
Background: Use of diagnostic imaging has increased significantly within fee-for-service healthcare models. The associated radiation exposure has increased the risk of radiation-induced malignancies. Little is known about the pattern of imaging use in integrated healthcare systems without the financial incentives seen in other models of care.
Study design: Retrospective cohort study.
Setting: Six integrated healthcare systems in the U.S.
Synopsis: The number of diagnostic imaging studies performed and estimated radiation exposure were determined from analysis of electronic medical records from member patients enrolled in health systems in the HMO Research Network from 1996 to 2010. Annual increases in use of advanced diagnostics were noted in CT (7.8% annual growth), MRI (10%), ultrasound (3.9%), and PET (57%) studies.
Increased CT use over the 15-year study period resulted in increased radiation exposure, doubling mean per capita effective dose (1.2 mSv to 2.3 mSv), as well as those receiving high exposure (1.2% to 2.5%) and very high exposure (0.6% to 1.4%).
The increased imaging use and radiation exposure among HMO enrollees was similar to that of fee-for-service Medicare patients in previous studies.
Bottom line: There is a significant increase in use of diagnostic imaging studies and associated radiation exposure among integrated healthcare system enrollees from 1996 to 2010, similar to patients in fee-for-service health plans.
Citation: Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA. 2012;307(22):2400-2409.
Postoperative Troponin Predicts 30-Day Mortality
Clinical question: Does postoperative peak troponin level predict 30-day mortality in patients undergoing noncardiac surgery?
Background: The use of postoperative peak troponin levels in predicting 30-day mortality for patients undergoing noncardiac surgery has not been studied extensively. Identifying patients at high risk for death following noncardiac surgery could facilitate appropriate postoperative care and improve survival.
Study design: Prospective cohort study.
Setting: International university and nonuniversity hospitals.
Synopsis: The Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) Study is a large, international, multicenter, prospective cohort study designed to evaluate the major complications of noncardiac surgery. More than 15,100 patients ages 45 and older requiring at least an overnight hospitalization were enrolled following noncardiac surgery.
Peak troponin measurements during the first three postoperative days of 0.01 ng/ml or less, 0.02 ng/ml, 0.03 ng/ml to 0.29 ng/ml, and 0.3 ng/ml or greater had 30-day mortality rates of 1.0%, 4.0%, 9.3%, and 16.9%, respectively.
This study demonstrates the sensitivity of troponin measurement for predicting postoperative 30-day mortality in patients undergoing noncardiac surgery. The study does not address interventions based on an increased postoperative troponin level. Future studies might investigate postoperative modifiable risk factors.
Bottom line: Postoperative peak troponin level predicts 30-day mortality in patients undergoing noncardiac surgery.
Citation: Devereaux PJ, Chan MT, Alonso-Coello P, et al. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2012;307(21):2295-2304.
Clinical Prediction Model of Mortality in Acute Heart Failure
Clinical question: Can a clinical prediction model accurately risk-stratify patients presenting to the ED with acute heart failure?
Background: Accurately prognosticating mortality is essential when determining whether to hospitalize or discharge patients presenting to the ED with acute heart failure. Evidence-based clinical prediction models enable physicians to risk-stratify patients and optimize care.
Study design: Retrospective cohort study.
Setting: Multicenter study of 86 hospitals in Ontario, Canada.
Synopsis: Data collected from 12,591 patients who presented to EDs with acute heart failure in Ontario were analyzed. A clinical prediction model of seven-day mortality of discharged and hospitalized patients was derived and validated. The Emergency Heart Failure Mortality Risk Grade (EHMRG) found an increased mortality based on higher triage heart rate, lower triage systolic blood pressure, initial oxygen saturation, and elevated troponin levels. This model uses readily available data collected in ED visits. The high-risk EHMRG score predicted about 8% seven-day mortality versus 0.3% in the low-risk score.
This model was not applied to chronic heart failure, did not utilize left ventricular function, and does not differentiate between systolic and diastolic heart failure.
Bottom line: The Emergency Heart Failure Mortality Risk Grade predicts seven-day mortality in acute heart failure in the emergent setting.
Citation: Lee DS, Stitt A, Austin PC, et al. Prediction of heart failure mortality in emergent care: a cohort study. Ann Intern Med. 2012;156(11):767-775.
Indwelling Pleural Catheter Is as Effective as Talc Pleurodesis Via Chest Tube in Relieving Dyspnea in Patients with Malignant Pleural Effusion
Clinical question: Is indwelling pleural catheter (IPC) as effective as chest tube and talc pleurodesis (talc) in improving dyspnea from malignant pleural effusion in patients who had no previous pleurodesis?
Background: Despite guidelines recommending chest tube insertion with pleurodesis as a first-line treatment for symptom palliation from malignant pleural effusion, there has been no randomized trial comparing indwelling pleural catheter with chest tube and talc pleurodesis.
Study design: Open-label, randomized controlled trial.
Setting: Seven hospitals in the United Kingdom.
Synopsis: One hundred six patients with malignant pleural effusion were randomized to undergo either IPC or talc treatment, and their daily mean dyspnea was measured. There was a clinically significant improvement of dyspnea in both IPC and talc groups over the first 42 days of the trial, without any significant difference in dyspnea between the two groups. After six months, researchers found a clinically significant decrease in dyspnea in the IPC group compared with the talc group. Chest pain and global quality of life were improved and were similar in both groups throughout the trial period. Length of hospital stay was significantly shorter in the IPC group compared with the talc group, but more patients in the IPC group experienced adverse events.
Bottom line: Indwelling pleural catheter is as effective as talc pleurodesis in reliving dyspnea from malignant pleural effusion; however, IPC is associated with increased adverse events despite shorter length of hospital stay.
Citation: Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs. chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion: the TIME2 randomized controlled trial. JAMA. 2012;307(22):2383-2389.
Early Surgery Better than Conventional Treatment in High-Risk Native-Valve Endocarditis
Clinical question: Is early cardiac surgery better than conventional treatment for patients with left-sided, native-valve, infective endocarditis?
Background: Although guidelines strongly recommend early surgery for patients with infective endocarditis and congestive heart failure, the timing of surgery for patients with large vegetations and high risk of embolism without heart failure symptoms remains controversial.
Study design: Prospective, randomized trial.
Setting: Two medical centers in South Korea.
Synopsis: Seventy-six patients with left-sided, native-valve, infective endocarditis with a high risk of embolism (defined as vegetation with a diameter greater than 10 mm or severe mitral or aortic valve disease) were randomized to undergo early surgery (within 48 hours of enrollment) or conventional treatment (antibiotic therapy and surgery only if complications required urgent surgery). The primary outcome of composite in-hospital death or
clinical embolic events within six weeks of the trial occurred in only one patient in the early surgery group, compared with nine patients in the conventional group (hazard ratio 0.10, 95% CI, 0.01-0.82, P=0.03).
There was no difference in all-cause mortality at six months between the two groups, but the rate of composite endpoint of death from any cause, embolic events, or recurrence of infective endocarditis at six months was significantly lower in the early surgery group compared with the conventional group.
Bottom line: Early cardiac surgery for patients with left-sided, native-valve infective endocarditis with a high risk of embolism significantly improved the composite outcome of all-cause mortality, embolic events, or recurrence of endocarditis compared with the conventional therapy.
Citation: Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366(26):2466-2473.
Risk Factors for Short-Term Mortality after Emergency Department Visit for Syncope
Clinical question: What are the risk factors for short-term mortality after an ED evaluation for syncope or near-syncope?
Background: Syncope accounts for 1% to 2% of all ED visits and an equal number of hospital admissions. The risk of death after an ED visit for syncope is poorly understood, resulting in frequent hospital admissions.
Study design: Retrospective cohort study.
Setting: EDs in Southern California.
Synopsis: Authors evaluated 23,951 ED visits resulting in syncope as sole primary diagnosis. Age was identified as the most significant risk factor for short-term mortality. Cumulative survival data revealed that more than 1% of patients 60 or older died by 30 days. There were 215 deaths (2.84%) in patients hospitalized from the ED and 66 deaths (0.45%) among patients not hospitalized.
Pre-existing comorbidities significantly associated with increased mortality included heart failure (HR=14.3 in ages 18-53; HR=3.09 in ages 60-79; HR=2.34 in ages 80-plus), diabetes (HR=1.49), seizure (HR=1.65), dementia (HR=1.41), and a recent prior visit for syncope (HR=1.86). The risk of death by 30 days was less than 0.2% in patients under 60 without heart failure and more than 2.5% in patients of all ages with heart failure.
Bottom line: After an ED visit for syncope, patients with a history of heart failure and patients 60 and older have a significantly increased risk of short-term mortality.
Citation: Derose SF, Gabayan GZ, Chiu VY, Sun BC. Patterns and preexisting risk factors of 30-day mortality after a primary discharge diagnosis of syncope or near syncope. Acad Emerg Med. 2012;19(5):488-496.
Acute Hyperglycemia Associated with Increased Mortality in Community-Acquired Pneumonia
Clinical question: In patients admitted to the hospital for community-acquired pneumonia, is serum glucose level on admission associated with mortality?
Background: Some retrospective studies have shown an association between alterations in serum glucose levels or pre-existing diabetes and higher mortality due to infections, while other studies have shown no clear association.
Study design: Multicenter, prospective cohort study.
Setting: Hospitals and private practices in Germany, Switzerland, and Austria.
Synopsis: Prospective data from 6,891 patients were included in the analysis. Patients without diabetes and normal serum glucose levels had the lowest mortality after 90 days. Patients without diabetes but with mild acute hyperglycemia (108 mg/dL to 198 mg/dL) had a significantly increased risk of death at 90 days (HR 1.56), and patients without diabetes but with more severe acute hyperglycemia (over 252 mg/dL) had an even higher risk of death at 90 days (HR 2.37).
The 90-day mortality rate was significantly higher in patients with pre-existing diabetes (HR 2.47), although this was not affected by serum glucose levels on admission.
Bottom line: Acute hyperglycemia, as well as pre-existing diabetes, was associated with an increased risk of 90-day mortality in patients with community acquired pneumonia.
Citation: Lepper PM, Ott S, Nüesch E, et al. Serum glucose levels for predicting death in patients admitted to hospital for community acquired pneumonia: prospective cohort study. BMJ. 2012;344:e3397.
Hospital Delirium Associated with Cognitive Decline, Institutionalization, and Death
Clinical question: What is the risk of subsequent cognitive decline, institutionalization, or death due to delirium in patients with dementia?
Background: Patients suffering delirium during hospitalization can suffer additional cognitive decline. Whether this is due to additional damage from the delirium state or reflects pre-existing cognitive vulnerability remains uncertain.
Study design: Prospective analysis of a cohort of Alzheimer’s patients.
Setting: Massachusetts community-based disease registry.
Synopsis: The analysis compared nonhospitalized individuals to patients hospitalized with, and without, delirium. In 771 individuals with dementia, at least one adverse outcome (including cognitive decline, institutionalization, or death) occurred in 32% of those not hospitalized, 55% of those hospitalized without delirium, and 79% of those hospitalized with delirium. Even after adjusting for confounders, hospitalization increased the risk for each of the adverse outcomes; the highest risk was in those with delirium.
Among hospitalized patients, the authors estimated 1 in 5 cases of cognitive decline, 1 in 7 institutionalizations, and 1 in 16 deaths were attributable to delirium. Some of the attributed risk could be the result of residual confounding from unmeasured variables, limiting conclusions of causality. Despite these limitations, this study supports the hypothesis that delirium prevention measures could improve important patient outcomes.
Bottom line: Hospitalization is associated with high rates of adverse outcomes in elderly patients with dementia, the worst of which occurs in those who experience delirium.
Citation: Fong TG, Jones RN, Marcantonio ER, et al. Adverse outcomes after hospitalization and delirium in persons with Alzheimer disease. Ann Int Med. 2012;156:848-856.
In Acute Pyelonephritis, a Seven-Day Course of Ciprofloxacin is Effective in Obtaining Clinical Cure
Clinical question: What is the efficacy of ciprofloxacin for seven days compared with 14 days in women with community-acquired acute pyelonephritis?
Background: Community-acquired acute pyelonephritis is a common and sometimes serious infection in women. In an era of increasing antibiotic resistance worldwide, it is prudent to reduce antibiotic utilization. There are limited controlled trials to assess the optimum duration of antibiotic treatment for this common infection.
Study design: Prospective, randomized, double-blind, noninferiority trial.
Setting: Twenty-one infectious-disease centers in Sweden.
Synopsis: Researchers randomly assigned 284 women 18 or older with a presumptive diagnosis of acute pyelonephritis to ciprofloxacin treatment for seven or 14 days. The primary endpoint was clinical and bacteriological cure 10 to 14 days after the completion of the treatment regimen. Short-term clinical cure occurred in 97% of the patients treated for seven days and 96% treated for 14 days. Long-term follow-up showed cumulative efficacy of 93% in each group. Both regimens were well tolerated.
Patients in this study had a low occurrence of complicated (9%) and recurrent (13%) infections. Whether short courses of antibiotics are effective in more complicated infections cannot be ascertained from this study. Also, the high cure rate obtained with a seven-day course of ciprofloxacin should not be extrapolated to other classes of antibiotics. Fluoroquinolones, such as ciprofloxacin, are recommended as first-line agents for empiric oral treatment of acute pyelonephritis if the resistance rate of the uropathogens remains lower than 10%; however, there is growing evidence that E. coli strains are becoming increasingly resistant to ciprofloxacin, limiting its usefulness.
Bottom line: Acute pyelonephritis in women can be treated successfully and safely with a seven-day course of ciprofloxacin, in areas with low ciprofloxacin resistance.
Citation: Sandberg T, Skoog G, Hermansson AB, et al. Ciprofloxacin for 7 days versus 14 days in women with acute pyelonephritis: a randomized, open-label and double-blind, placebo-controlled, non-inferiority trial. Lancet. 2012;380:484-490.
Advance Directives in Community Patients with Heart Failure
Clinical question: How prevalent are advance directives in heart-failure patients, and does a completed advance directive decrease end-of-life resource use (hospitalizations, ICU admissions, mechanical ventilation)?
Background: Heart failure is a common chronic and fatal disease. End-of-life care in heart-failure patients is associated with extremely high healthcare utilization. Heart failure guidelines recommend completing advance directives in all patients.
Study design: Population-based longitudinal cohort study.
Setting: Rochester Epidemiology Project in Olmstead County, Minn.
Synopsis: Investigators enrolled 608 patients presenting with heart failure between October 2007 and October 2011. At the time of enrollment, only 41% of the patients had existing advance directives. Independent predictors of advance directive completion included older age, history of malignancy, and renal dysfunction.
After a mean follow-up of 1.8 years, 164 patients (27%) had died. Among those patients, 106 had an advance directive (64.6%) at time of death—75 had an advance directive at the time of enrollment and another 31 completed an advance directive after enrollment.
Twenty-five patients (23.6%) specified DNR/DNI and another 39 (36.8%) denoted limitations on aggressiveness of care if death was imminent. Among the patients who died, 88 (53.7%) were hospitalized in the last month of their life and 50 (30.5%) died in the hospital. There was no difference in hospitalizations between those with an advance directive specifying limits and those who did not specify limits (OR 1.26, 95% CI 0.64-2.48). However, those with an advance directive specifying limits were less frequently mechanically ventilated (OR 0.26, 95% CI 0.06-0.88), and there was a trend toward them being less frequently admitted into the ICU (OR 0.45, 95% CI 0.16-1.29).
Bottom line: Less than half of community patients with heart failure had an advance directive, and many of these failed to address end-of-life decisions. Patients with an advance directive that specified limits in care were less likely to receive mechanical ventilation.
Citation: Dunlay SM, Swetz KM, Mueller PS, Roger VL. Advance directives in community patients with heart failure. Circ Cardiovasc Qual Outcomes. 2012;5:283-289.
Chlorhexidine Bathing Associated with Significant, Sustainable Reductions in Central-Venous-Catheter-Associated Bloodstream Infection
Clinical question: What is the impact, and sustainability, of chlorhexidine bathing on central-venous-catheter-associated bloodstream infections?
Background: Chlorhexidine bathing has been associated with reductions in healthcare-associated bloodstream infections, including vancomycin-resistant enterococci and methicillin-resistant Staphylococcus aureus. No prospective studies have evaluated the impact and sustainability of chlorhexidine bathing.
Study design: Prospective, three-phase study.
Setting: Medical-surgical ICUs and respiratory-care units at five New York hospitals.
Synopsis: In the pre-intervention phase (six to nine months, 1,808 admissions), patients were bathed with soap and water or nonmedicated bathing cloths. In the intervention phase (eight months, 1,832 admissions), patients were bathed with 2% chlorhexidine cloths. In the post-intervention phase (12 months, 2,834 admissions), chlorhexidine bathing was continued without oversight by researchers.
During the intervention phase, there were significantly fewer central-venous-catheter-associated bloodstream infections (2.6/1,000 catheter days vs. 6.4/1,000 pre-intervention). The reductions in bloodstream infections were sustained during the post-intervention period (2.9/1,000 catheter days). Compliance with chlorhexidine bathing was 82% and 88% during the intervention and post-intervention phases, and was well tolerated by the patients.
Limitations of this study include lack of patient-specific data and severity of illness data, as well as lack of randomization and blinding. Although not evaluated in this study, the savings associated with decreased bloodstream infections likely outweigh the cost of chlorhexidine bathing.
Bottom line: Chlorhexidine bathing is a well-tolerated, sustainable intervention that significantly reduces central-venous-catheter-associated bloodstream infections.
Citation: Montecalvo MA, McKenna D, Yarrish R, et al. Chlorhexidine bathing to reduce central venous catheter-associated bloodstream infection: impact and sustainability. Am J Med. 2012;125(5):505-511.
Simulation Training Improves Lumbar Puncture Skills
Clinical question: What effect does simulation have on lumbar puncture (LP) skills of PGY1 internal-medicine (IM) residents compared with PGY2-4 neurology residents who have not received simulation training?
Background: LPs are common procedures. The American College of General Medical Education does not define competency; neither do the internal-medicine (IM) or neurology board certifications. Simulation can improve skills in many areas but has not been well studied in LPs.
Study design: Pre-test-post-test.
Setting: Northwestern University’s Feinberg School of Medicine in Chicago.
Synopsis: The intervention group included 58 PGY1 IM residents, while the control group was 49 PGY2-to-PGY4 neurology residents. The pre-test consisted of a 21-point checklist. IM residents watched a three-hour video, performed LPs on simulators, and received feedback. The post-test was a clinical skills examination using the checklist. If this exam was failed, the participant practiced and was retested. Neurology residents completed the pre-test and demonstrated an LP using the simulator.
Pre-test passing was achieved by only 2% of IM residents and 6% of neurology residents. Post-test passing was achieved by 95% of the IM residents on the first trial and 100% of IM residents after an hour of additional training. IM mean scores increased to 95.7% from 46.3%, while the mean score of neurology residents was 65.4%.
This study is limited by its single-center nature, as education is variable from center to center. The study evaluated the proficiency on simulators only, and it did not evaluate the proficiency of the participants on patients.
Bottom line: Simulation training improves lumbar puncture skills.
Citation: Barsuk JH, Cohen ER, Caprio T, McGaghie WC, Simuni T, Wayne DB. Simulation-based education with mastery learning improves residents’ lumbar puncture skills. Neurology. 2012;79(2):132-137.
Primary-Care Physicians Do Not Use Publicly Reported Data When Referring Patients to Hospitals
Clinical question: When referring patients with pneumonia to the hospital, what factors do primary-care physicians (PCPs) consider?
Background: Publicly reported data are widely available. Pneumonia has publicly reported quality measures and is a common reason for hospitalization. Fewer PCPs are attending in the hospital due to the hospitalist movement; therefore, PCPs refer patients to a hospital when the need arises.
Study design: Online survey.
Setting: PCPs within 10 miles of Springfield, Mass.
Synopsis: A total of 92 PCPs responded to the survey, which included presentation of a case regarding a patient with pneumonia. PCPs were asked the importance of multiple factors leading to their decision to refer to a hospital. Familiarity with the hospital (70%), patient preference (62%), and admitting arrangements with a hospitalist group (62%) were considered to be very important to the PCPs that responded to the survey. Publicly reported data were very important to only 18% of respondents, and zero reported using publicly reported data when referring patients.
Importance of specific quality measures also was queried; antibiotics given within six hours of arrival (66%), appropriate choice of antibiotics (63%), and blood cultures prior to antibiotic administration (51%) were very important to respondents. Prestige, such as magnet status and U.S. News and World Report “Best Hospital” status, were deemed important by about 40% of PCPs.
Bottom line: Despite the availability of publicly reported data, PCPs do not use this information to refer patients to the hospital.
Citation: Morsi E, Lindenauer PK, Rothberg MB. Primary care physicians’ use of publicly reported quality data in hospital referral decisions. J Hosp Med. 2012;7(5):370-375.
What Works for Medication Reconciliation?
Clinical question: What are the most effective practices for medication reconciliation in the hospital setting?
Background: Medication discrepancies are common, occurring in as many as 70% of patients at hospital admission or discharge. Up to a third of these discrepancies have potential to cause patient harm, including prolonged hospital stays, ED visits, hospital recidivism, and use of other healthcare resources. Medication reconciliation (“med rec”) is a strategy for reducing these errors, though previous literature has not systematically reviewed best practices for hospital-based med rec.
Study design: Systematic review of literature.
Setting: Controlled studies from the U.S., Canada, Australia, New Zealand, Northern Ireland, United Kingdom, Belgium, Denmark, the Netherlands, and Sweden.
Synopsis: Investigators identified 26 controlled studies using a systematic search of English-language articles on med rec during inpatient hospitalizations published between Jan. 1, 1966, and Oct. 31, 2010. Fifteen studies reported on pharmacist-related interventions; six reported on technology-specific interventions; and five reported on other types of interventions, including staff education and use of standardized med-rec tools.
Analysis of these studies revealed that all of these interventions successfully decreased medication discrepancies and potential adverse drug events, but there was inconsistent benefit with regard to adverse drug events and healthcare utilization compared with usual care. The literature was most supportive of pharmacist-related interventions, including but not limited to comprehensive medication history at admission, med rec at discharge, patient counseling, discharge communication with outpatient providers, and post-discharge communication with the patient and post-hospital providers.
Bottom line: Successful med rec requires multiple interventions at various transitions of care and involves a variety of medical professionals. Patient-targeted interventions, including pharmacists, have the potential to decrease errors and adverse events.
Citation: Mueller S, Sponsler K, Kripalani S, Schnipper J. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med. 2012;172(14):1057-1069.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Prediction tool for neurological outcomes after in-hospital cardiac arrest
- Radiation exposure in integrated healthcare systems, 1996-2010
- Postoperative troponin predicts 30-day mortality
- Clinical prediction model of mortality in acute heart failure
- Indwelling pleural catheter vs. talc pleurodesis via chest tube
- Early surgery for high-risk, native-valve endocarditis patients
- Risk factors after ED visit for syncope
- Acute hyperglycemia in CAP patients
- Hospital delirium associated with cognitive decline, institutionalization, and death
- Seven-day ciprofloxacin effective against acute pyelonephritis
- Advance directives in community patients with heart failure
- Chlorhexidine bathing effective against CVC-associated bloodstream infections
- Simulation training improves lumbar puncture skills
- PCP referrals to hospitals and publicly reported data
- Medication reconciliation best practices
Prediction Tool Validated for Prognosticating Favorable Neurological Outcome after In-Hospital Cardiac Arrest
Clinical question: Does the Cardiac Arrest Survival Post Resuscitation In-Hospital (CASPRI) score accurately predict favorable neurological outcomes?
Background: Previous cardiac arrest prediction models have been focused on survival to discharge without consideration of neurological status and have not been translated into valid bedside prognostication tools. Neurologic prognosis can assist patients, families, and physicians in decisions about continued goals of care post-arrest.
Study design: Retrospective cohort study.
Setting: Acute-care hospitals.
Synopsis: Using the Get with the Guidelines Resuscitation Registry, 551 hospitals identified 42,957 patients who were successfully resuscitated from an in-hospital cardiac arrest from January 2000 to October 2009. Researchers developed a simple prediction tool for favorable neurological outcomes (defined as “no” or “moderate” neurological disability) at discharge. The 11 predictors used to calculate the CASPRI score are age; time to defibrillation; pre-arrest neurological status; hospital location; duration of resuscitation; and pre-arrest comorbidities: mechanical ventilation, renal insufficiency, hepatic insufficiency, sepsis, malignancy,
and hypotension.
Rates of favorable neurological outcome were similar between derivation cohort (24.6%) and validation cohort (24.5%). The model had excellent discrimination with a C score of 0.80. Probability of favorable neurological survival ranged from 70.7% in the top decile of patients (CASPRI <10) and 2.8% in bottom decile (CASPRI ≥ 28).
This tool is not generalizable to patients with out-of-hospital arrest or undergoing therapeutic hypothermia.
Bottom line: CASPRI is a simple bedside tool validated to estimate probability of favorable neurological outcome after in-hospital cardiac arrest.
Citation: Chan PS, Spertus JA, Krumholz HA, et al. A validated prediction tool for initial survivors in in-hospital cardiac arrest. Arch Intern Med. 2012;172(12):947-953.
Increased Use of Radiologic Imaging and Associated Radiation Exposure in Integrated Healthcare Systems, 1996-2010
Clinical question: How much has imaging utilization and associated radiation exposure increased over 15 years in integrated healthcare systems independent of financial incentives in a fee-for-service system?
Background: Use of diagnostic imaging has increased significantly within fee-for-service healthcare models. The associated radiation exposure has increased the risk of radiation-induced malignancies. Little is known about the pattern of imaging use in integrated healthcare systems without the financial incentives seen in other models of care.
Study design: Retrospective cohort study.
Setting: Six integrated healthcare systems in the U.S.
Synopsis: The number of diagnostic imaging studies performed and estimated radiation exposure were determined from analysis of electronic medical records from member patients enrolled in health systems in the HMO Research Network from 1996 to 2010. Annual increases in use of advanced diagnostics were noted in CT (7.8% annual growth), MRI (10%), ultrasound (3.9%), and PET (57%) studies.
Increased CT use over the 15-year study period resulted in increased radiation exposure, doubling mean per capita effective dose (1.2 mSv to 2.3 mSv), as well as those receiving high exposure (1.2% to 2.5%) and very high exposure (0.6% to 1.4%).
The increased imaging use and radiation exposure among HMO enrollees was similar to that of fee-for-service Medicare patients in previous studies.
Bottom line: There is a significant increase in use of diagnostic imaging studies and associated radiation exposure among integrated healthcare system enrollees from 1996 to 2010, similar to patients in fee-for-service health plans.
Citation: Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA. 2012;307(22):2400-2409.
Postoperative Troponin Predicts 30-Day Mortality
Clinical question: Does postoperative peak troponin level predict 30-day mortality in patients undergoing noncardiac surgery?
Background: The use of postoperative peak troponin levels in predicting 30-day mortality for patients undergoing noncardiac surgery has not been studied extensively. Identifying patients at high risk for death following noncardiac surgery could facilitate appropriate postoperative care and improve survival.
Study design: Prospective cohort study.
Setting: International university and nonuniversity hospitals.
Synopsis: The Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) Study is a large, international, multicenter, prospective cohort study designed to evaluate the major complications of noncardiac surgery. More than 15,100 patients ages 45 and older requiring at least an overnight hospitalization were enrolled following noncardiac surgery.
Peak troponin measurements during the first three postoperative days of 0.01 ng/ml or less, 0.02 ng/ml, 0.03 ng/ml to 0.29 ng/ml, and 0.3 ng/ml or greater had 30-day mortality rates of 1.0%, 4.0%, 9.3%, and 16.9%, respectively.
This study demonstrates the sensitivity of troponin measurement for predicting postoperative 30-day mortality in patients undergoing noncardiac surgery. The study does not address interventions based on an increased postoperative troponin level. Future studies might investigate postoperative modifiable risk factors.
Bottom line: Postoperative peak troponin level predicts 30-day mortality in patients undergoing noncardiac surgery.
Citation: Devereaux PJ, Chan MT, Alonso-Coello P, et al. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2012;307(21):2295-2304.
Clinical Prediction Model of Mortality in Acute Heart Failure
Clinical question: Can a clinical prediction model accurately risk-stratify patients presenting to the ED with acute heart failure?
Background: Accurately prognosticating mortality is essential when determining whether to hospitalize or discharge patients presenting to the ED with acute heart failure. Evidence-based clinical prediction models enable physicians to risk-stratify patients and optimize care.
Study design: Retrospective cohort study.
Setting: Multicenter study of 86 hospitals in Ontario, Canada.
Synopsis: Data collected from 12,591 patients who presented to EDs with acute heart failure in Ontario were analyzed. A clinical prediction model of seven-day mortality of discharged and hospitalized patients was derived and validated. The Emergency Heart Failure Mortality Risk Grade (EHMRG) found an increased mortality based on higher triage heart rate, lower triage systolic blood pressure, initial oxygen saturation, and elevated troponin levels. This model uses readily available data collected in ED visits. The high-risk EHMRG score predicted about 8% seven-day mortality versus 0.3% in the low-risk score.
This model was not applied to chronic heart failure, did not utilize left ventricular function, and does not differentiate between systolic and diastolic heart failure.
Bottom line: The Emergency Heart Failure Mortality Risk Grade predicts seven-day mortality in acute heart failure in the emergent setting.
Citation: Lee DS, Stitt A, Austin PC, et al. Prediction of heart failure mortality in emergent care: a cohort study. Ann Intern Med. 2012;156(11):767-775.
Indwelling Pleural Catheter Is as Effective as Talc Pleurodesis Via Chest Tube in Relieving Dyspnea in Patients with Malignant Pleural Effusion
Clinical question: Is indwelling pleural catheter (IPC) as effective as chest tube and talc pleurodesis (talc) in improving dyspnea from malignant pleural effusion in patients who had no previous pleurodesis?
Background: Despite guidelines recommending chest tube insertion with pleurodesis as a first-line treatment for symptom palliation from malignant pleural effusion, there has been no randomized trial comparing indwelling pleural catheter with chest tube and talc pleurodesis.
Study design: Open-label, randomized controlled trial.
Setting: Seven hospitals in the United Kingdom.
Synopsis: One hundred six patients with malignant pleural effusion were randomized to undergo either IPC or talc treatment, and their daily mean dyspnea was measured. There was a clinically significant improvement of dyspnea in both IPC and talc groups over the first 42 days of the trial, without any significant difference in dyspnea between the two groups. After six months, researchers found a clinically significant decrease in dyspnea in the IPC group compared with the talc group. Chest pain and global quality of life were improved and were similar in both groups throughout the trial period. Length of hospital stay was significantly shorter in the IPC group compared with the talc group, but more patients in the IPC group experienced adverse events.
Bottom line: Indwelling pleural catheter is as effective as talc pleurodesis in reliving dyspnea from malignant pleural effusion; however, IPC is associated with increased adverse events despite shorter length of hospital stay.
Citation: Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs. chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion: the TIME2 randomized controlled trial. JAMA. 2012;307(22):2383-2389.
Early Surgery Better than Conventional Treatment in High-Risk Native-Valve Endocarditis
Clinical question: Is early cardiac surgery better than conventional treatment for patients with left-sided, native-valve, infective endocarditis?
Background: Although guidelines strongly recommend early surgery for patients with infective endocarditis and congestive heart failure, the timing of surgery for patients with large vegetations and high risk of embolism without heart failure symptoms remains controversial.
Study design: Prospective, randomized trial.
Setting: Two medical centers in South Korea.
Synopsis: Seventy-six patients with left-sided, native-valve, infective endocarditis with a high risk of embolism (defined as vegetation with a diameter greater than 10 mm or severe mitral or aortic valve disease) were randomized to undergo early surgery (within 48 hours of enrollment) or conventional treatment (antibiotic therapy and surgery only if complications required urgent surgery). The primary outcome of composite in-hospital death or
clinical embolic events within six weeks of the trial occurred in only one patient in the early surgery group, compared with nine patients in the conventional group (hazard ratio 0.10, 95% CI, 0.01-0.82, P=0.03).
There was no difference in all-cause mortality at six months between the two groups, but the rate of composite endpoint of death from any cause, embolic events, or recurrence of infective endocarditis at six months was significantly lower in the early surgery group compared with the conventional group.
Bottom line: Early cardiac surgery for patients with left-sided, native-valve infective endocarditis with a high risk of embolism significantly improved the composite outcome of all-cause mortality, embolic events, or recurrence of endocarditis compared with the conventional therapy.
Citation: Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366(26):2466-2473.
Risk Factors for Short-Term Mortality after Emergency Department Visit for Syncope
Clinical question: What are the risk factors for short-term mortality after an ED evaluation for syncope or near-syncope?
Background: Syncope accounts for 1% to 2% of all ED visits and an equal number of hospital admissions. The risk of death after an ED visit for syncope is poorly understood, resulting in frequent hospital admissions.
Study design: Retrospective cohort study.
Setting: EDs in Southern California.
Synopsis: Authors evaluated 23,951 ED visits resulting in syncope as sole primary diagnosis. Age was identified as the most significant risk factor for short-term mortality. Cumulative survival data revealed that more than 1% of patients 60 or older died by 30 days. There were 215 deaths (2.84%) in patients hospitalized from the ED and 66 deaths (0.45%) among patients not hospitalized.
Pre-existing comorbidities significantly associated with increased mortality included heart failure (HR=14.3 in ages 18-53; HR=3.09 in ages 60-79; HR=2.34 in ages 80-plus), diabetes (HR=1.49), seizure (HR=1.65), dementia (HR=1.41), and a recent prior visit for syncope (HR=1.86). The risk of death by 30 days was less than 0.2% in patients under 60 without heart failure and more than 2.5% in patients of all ages with heart failure.
Bottom line: After an ED visit for syncope, patients with a history of heart failure and patients 60 and older have a significantly increased risk of short-term mortality.
Citation: Derose SF, Gabayan GZ, Chiu VY, Sun BC. Patterns and preexisting risk factors of 30-day mortality after a primary discharge diagnosis of syncope or near syncope. Acad Emerg Med. 2012;19(5):488-496.
Acute Hyperglycemia Associated with Increased Mortality in Community-Acquired Pneumonia
Clinical question: In patients admitted to the hospital for community-acquired pneumonia, is serum glucose level on admission associated with mortality?
Background: Some retrospective studies have shown an association between alterations in serum glucose levels or pre-existing diabetes and higher mortality due to infections, while other studies have shown no clear association.
Study design: Multicenter, prospective cohort study.
Setting: Hospitals and private practices in Germany, Switzerland, and Austria.
Synopsis: Prospective data from 6,891 patients were included in the analysis. Patients without diabetes and normal serum glucose levels had the lowest mortality after 90 days. Patients without diabetes but with mild acute hyperglycemia (108 mg/dL to 198 mg/dL) had a significantly increased risk of death at 90 days (HR 1.56), and patients without diabetes but with more severe acute hyperglycemia (over 252 mg/dL) had an even higher risk of death at 90 days (HR 2.37).
The 90-day mortality rate was significantly higher in patients with pre-existing diabetes (HR 2.47), although this was not affected by serum glucose levels on admission.
Bottom line: Acute hyperglycemia, as well as pre-existing diabetes, was associated with an increased risk of 90-day mortality in patients with community acquired pneumonia.
Citation: Lepper PM, Ott S, Nüesch E, et al. Serum glucose levels for predicting death in patients admitted to hospital for community acquired pneumonia: prospective cohort study. BMJ. 2012;344:e3397.
Hospital Delirium Associated with Cognitive Decline, Institutionalization, and Death
Clinical question: What is the risk of subsequent cognitive decline, institutionalization, or death due to delirium in patients with dementia?
Background: Patients suffering delirium during hospitalization can suffer additional cognitive decline. Whether this is due to additional damage from the delirium state or reflects pre-existing cognitive vulnerability remains uncertain.
Study design: Prospective analysis of a cohort of Alzheimer’s patients.
Setting: Massachusetts community-based disease registry.
Synopsis: The analysis compared nonhospitalized individuals to patients hospitalized with, and without, delirium. In 771 individuals with dementia, at least one adverse outcome (including cognitive decline, institutionalization, or death) occurred in 32% of those not hospitalized, 55% of those hospitalized without delirium, and 79% of those hospitalized with delirium. Even after adjusting for confounders, hospitalization increased the risk for each of the adverse outcomes; the highest risk was in those with delirium.
Among hospitalized patients, the authors estimated 1 in 5 cases of cognitive decline, 1 in 7 institutionalizations, and 1 in 16 deaths were attributable to delirium. Some of the attributed risk could be the result of residual confounding from unmeasured variables, limiting conclusions of causality. Despite these limitations, this study supports the hypothesis that delirium prevention measures could improve important patient outcomes.
Bottom line: Hospitalization is associated with high rates of adverse outcomes in elderly patients with dementia, the worst of which occurs in those who experience delirium.
Citation: Fong TG, Jones RN, Marcantonio ER, et al. Adverse outcomes after hospitalization and delirium in persons with Alzheimer disease. Ann Int Med. 2012;156:848-856.
In Acute Pyelonephritis, a Seven-Day Course of Ciprofloxacin is Effective in Obtaining Clinical Cure
Clinical question: What is the efficacy of ciprofloxacin for seven days compared with 14 days in women with community-acquired acute pyelonephritis?
Background: Community-acquired acute pyelonephritis is a common and sometimes serious infection in women. In an era of increasing antibiotic resistance worldwide, it is prudent to reduce antibiotic utilization. There are limited controlled trials to assess the optimum duration of antibiotic treatment for this common infection.
Study design: Prospective, randomized, double-blind, noninferiority trial.
Setting: Twenty-one infectious-disease centers in Sweden.
Synopsis: Researchers randomly assigned 284 women 18 or older with a presumptive diagnosis of acute pyelonephritis to ciprofloxacin treatment for seven or 14 days. The primary endpoint was clinical and bacteriological cure 10 to 14 days after the completion of the treatment regimen. Short-term clinical cure occurred in 97% of the patients treated for seven days and 96% treated for 14 days. Long-term follow-up showed cumulative efficacy of 93% in each group. Both regimens were well tolerated.
Patients in this study had a low occurrence of complicated (9%) and recurrent (13%) infections. Whether short courses of antibiotics are effective in more complicated infections cannot be ascertained from this study. Also, the high cure rate obtained with a seven-day course of ciprofloxacin should not be extrapolated to other classes of antibiotics. Fluoroquinolones, such as ciprofloxacin, are recommended as first-line agents for empiric oral treatment of acute pyelonephritis if the resistance rate of the uropathogens remains lower than 10%; however, there is growing evidence that E. coli strains are becoming increasingly resistant to ciprofloxacin, limiting its usefulness.
Bottom line: Acute pyelonephritis in women can be treated successfully and safely with a seven-day course of ciprofloxacin, in areas with low ciprofloxacin resistance.
Citation: Sandberg T, Skoog G, Hermansson AB, et al. Ciprofloxacin for 7 days versus 14 days in women with acute pyelonephritis: a randomized, open-label and double-blind, placebo-controlled, non-inferiority trial. Lancet. 2012;380:484-490.
Advance Directives in Community Patients with Heart Failure
Clinical question: How prevalent are advance directives in heart-failure patients, and does a completed advance directive decrease end-of-life resource use (hospitalizations, ICU admissions, mechanical ventilation)?
Background: Heart failure is a common chronic and fatal disease. End-of-life care in heart-failure patients is associated with extremely high healthcare utilization. Heart failure guidelines recommend completing advance directives in all patients.
Study design: Population-based longitudinal cohort study.
Setting: Rochester Epidemiology Project in Olmstead County, Minn.
Synopsis: Investigators enrolled 608 patients presenting with heart failure between October 2007 and October 2011. At the time of enrollment, only 41% of the patients had existing advance directives. Independent predictors of advance directive completion included older age, history of malignancy, and renal dysfunction.
After a mean follow-up of 1.8 years, 164 patients (27%) had died. Among those patients, 106 had an advance directive (64.6%) at time of death—75 had an advance directive at the time of enrollment and another 31 completed an advance directive after enrollment.
Twenty-five patients (23.6%) specified DNR/DNI and another 39 (36.8%) denoted limitations on aggressiveness of care if death was imminent. Among the patients who died, 88 (53.7%) were hospitalized in the last month of their life and 50 (30.5%) died in the hospital. There was no difference in hospitalizations between those with an advance directive specifying limits and those who did not specify limits (OR 1.26, 95% CI 0.64-2.48). However, those with an advance directive specifying limits were less frequently mechanically ventilated (OR 0.26, 95% CI 0.06-0.88), and there was a trend toward them being less frequently admitted into the ICU (OR 0.45, 95% CI 0.16-1.29).
Bottom line: Less than half of community patients with heart failure had an advance directive, and many of these failed to address end-of-life decisions. Patients with an advance directive that specified limits in care were less likely to receive mechanical ventilation.
Citation: Dunlay SM, Swetz KM, Mueller PS, Roger VL. Advance directives in community patients with heart failure. Circ Cardiovasc Qual Outcomes. 2012;5:283-289.
Chlorhexidine Bathing Associated with Significant, Sustainable Reductions in Central-Venous-Catheter-Associated Bloodstream Infection
Clinical question: What is the impact, and sustainability, of chlorhexidine bathing on central-venous-catheter-associated bloodstream infections?
Background: Chlorhexidine bathing has been associated with reductions in healthcare-associated bloodstream infections, including vancomycin-resistant enterococci and methicillin-resistant Staphylococcus aureus. No prospective studies have evaluated the impact and sustainability of chlorhexidine bathing.
Study design: Prospective, three-phase study.
Setting: Medical-surgical ICUs and respiratory-care units at five New York hospitals.
Synopsis: In the pre-intervention phase (six to nine months, 1,808 admissions), patients were bathed with soap and water or nonmedicated bathing cloths. In the intervention phase (eight months, 1,832 admissions), patients were bathed with 2% chlorhexidine cloths. In the post-intervention phase (12 months, 2,834 admissions), chlorhexidine bathing was continued without oversight by researchers.
During the intervention phase, there were significantly fewer central-venous-catheter-associated bloodstream infections (2.6/1,000 catheter days vs. 6.4/1,000 pre-intervention). The reductions in bloodstream infections were sustained during the post-intervention period (2.9/1,000 catheter days). Compliance with chlorhexidine bathing was 82% and 88% during the intervention and post-intervention phases, and was well tolerated by the patients.
Limitations of this study include lack of patient-specific data and severity of illness data, as well as lack of randomization and blinding. Although not evaluated in this study, the savings associated with decreased bloodstream infections likely outweigh the cost of chlorhexidine bathing.
Bottom line: Chlorhexidine bathing is a well-tolerated, sustainable intervention that significantly reduces central-venous-catheter-associated bloodstream infections.
Citation: Montecalvo MA, McKenna D, Yarrish R, et al. Chlorhexidine bathing to reduce central venous catheter-associated bloodstream infection: impact and sustainability. Am J Med. 2012;125(5):505-511.
Simulation Training Improves Lumbar Puncture Skills
Clinical question: What effect does simulation have on lumbar puncture (LP) skills of PGY1 internal-medicine (IM) residents compared with PGY2-4 neurology residents who have not received simulation training?
Background: LPs are common procedures. The American College of General Medical Education does not define competency; neither do the internal-medicine (IM) or neurology board certifications. Simulation can improve skills in many areas but has not been well studied in LPs.
Study design: Pre-test-post-test.
Setting: Northwestern University’s Feinberg School of Medicine in Chicago.
Synopsis: The intervention group included 58 PGY1 IM residents, while the control group was 49 PGY2-to-PGY4 neurology residents. The pre-test consisted of a 21-point checklist. IM residents watched a three-hour video, performed LPs on simulators, and received feedback. The post-test was a clinical skills examination using the checklist. If this exam was failed, the participant practiced and was retested. Neurology residents completed the pre-test and demonstrated an LP using the simulator.
Pre-test passing was achieved by only 2% of IM residents and 6% of neurology residents. Post-test passing was achieved by 95% of the IM residents on the first trial and 100% of IM residents after an hour of additional training. IM mean scores increased to 95.7% from 46.3%, while the mean score of neurology residents was 65.4%.
This study is limited by its single-center nature, as education is variable from center to center. The study evaluated the proficiency on simulators only, and it did not evaluate the proficiency of the participants on patients.
Bottom line: Simulation training improves lumbar puncture skills.
Citation: Barsuk JH, Cohen ER, Caprio T, McGaghie WC, Simuni T, Wayne DB. Simulation-based education with mastery learning improves residents’ lumbar puncture skills. Neurology. 2012;79(2):132-137.
Primary-Care Physicians Do Not Use Publicly Reported Data When Referring Patients to Hospitals
Clinical question: When referring patients with pneumonia to the hospital, what factors do primary-care physicians (PCPs) consider?
Background: Publicly reported data are widely available. Pneumonia has publicly reported quality measures and is a common reason for hospitalization. Fewer PCPs are attending in the hospital due to the hospitalist movement; therefore, PCPs refer patients to a hospital when the need arises.
Study design: Online survey.
Setting: PCPs within 10 miles of Springfield, Mass.
Synopsis: A total of 92 PCPs responded to the survey, which included presentation of a case regarding a patient with pneumonia. PCPs were asked the importance of multiple factors leading to their decision to refer to a hospital. Familiarity with the hospital (70%), patient preference (62%), and admitting arrangements with a hospitalist group (62%) were considered to be very important to the PCPs that responded to the survey. Publicly reported data were very important to only 18% of respondents, and zero reported using publicly reported data when referring patients.
Importance of specific quality measures also was queried; antibiotics given within six hours of arrival (66%), appropriate choice of antibiotics (63%), and blood cultures prior to antibiotic administration (51%) were very important to respondents. Prestige, such as magnet status and U.S. News and World Report “Best Hospital” status, were deemed important by about 40% of PCPs.
Bottom line: Despite the availability of publicly reported data, PCPs do not use this information to refer patients to the hospital.
Citation: Morsi E, Lindenauer PK, Rothberg MB. Primary care physicians’ use of publicly reported quality data in hospital referral decisions. J Hosp Med. 2012;7(5):370-375.
What Works for Medication Reconciliation?
Clinical question: What are the most effective practices for medication reconciliation in the hospital setting?
Background: Medication discrepancies are common, occurring in as many as 70% of patients at hospital admission or discharge. Up to a third of these discrepancies have potential to cause patient harm, including prolonged hospital stays, ED visits, hospital recidivism, and use of other healthcare resources. Medication reconciliation (“med rec”) is a strategy for reducing these errors, though previous literature has not systematically reviewed best practices for hospital-based med rec.
Study design: Systematic review of literature.
Setting: Controlled studies from the U.S., Canada, Australia, New Zealand, Northern Ireland, United Kingdom, Belgium, Denmark, the Netherlands, and Sweden.
Synopsis: Investigators identified 26 controlled studies using a systematic search of English-language articles on med rec during inpatient hospitalizations published between Jan. 1, 1966, and Oct. 31, 2010. Fifteen studies reported on pharmacist-related interventions; six reported on technology-specific interventions; and five reported on other types of interventions, including staff education and use of standardized med-rec tools.
Analysis of these studies revealed that all of these interventions successfully decreased medication discrepancies and potential adverse drug events, but there was inconsistent benefit with regard to adverse drug events and healthcare utilization compared with usual care. The literature was most supportive of pharmacist-related interventions, including but not limited to comprehensive medication history at admission, med rec at discharge, patient counseling, discharge communication with outpatient providers, and post-discharge communication with the patient and post-hospital providers.
Bottom line: Successful med rec requires multiple interventions at various transitions of care and involves a variety of medical professionals. Patient-targeted interventions, including pharmacists, have the potential to decrease errors and adverse events.
Citation: Mueller S, Sponsler K, Kripalani S, Schnipper J. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med. 2012;172(14):1057-1069.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Prediction tool for neurological outcomes after in-hospital cardiac arrest
- Radiation exposure in integrated healthcare systems, 1996-2010
- Postoperative troponin predicts 30-day mortality
- Clinical prediction model of mortality in acute heart failure
- Indwelling pleural catheter vs. talc pleurodesis via chest tube
- Early surgery for high-risk, native-valve endocarditis patients
- Risk factors after ED visit for syncope
- Acute hyperglycemia in CAP patients
- Hospital delirium associated with cognitive decline, institutionalization, and death
- Seven-day ciprofloxacin effective against acute pyelonephritis
- Advance directives in community patients with heart failure
- Chlorhexidine bathing effective against CVC-associated bloodstream infections
- Simulation training improves lumbar puncture skills
- PCP referrals to hospitals and publicly reported data
- Medication reconciliation best practices
Prediction Tool Validated for Prognosticating Favorable Neurological Outcome after In-Hospital Cardiac Arrest
Clinical question: Does the Cardiac Arrest Survival Post Resuscitation In-Hospital (CASPRI) score accurately predict favorable neurological outcomes?
Background: Previous cardiac arrest prediction models have been focused on survival to discharge without consideration of neurological status and have not been translated into valid bedside prognostication tools. Neurologic prognosis can assist patients, families, and physicians in decisions about continued goals of care post-arrest.
Study design: Retrospective cohort study.
Setting: Acute-care hospitals.
Synopsis: Using the Get with the Guidelines Resuscitation Registry, 551 hospitals identified 42,957 patients who were successfully resuscitated from an in-hospital cardiac arrest from January 2000 to October 2009. Researchers developed a simple prediction tool for favorable neurological outcomes (defined as “no” or “moderate” neurological disability) at discharge. The 11 predictors used to calculate the CASPRI score are age; time to defibrillation; pre-arrest neurological status; hospital location; duration of resuscitation; and pre-arrest comorbidities: mechanical ventilation, renal insufficiency, hepatic insufficiency, sepsis, malignancy,
and hypotension.
Rates of favorable neurological outcome were similar between derivation cohort (24.6%) and validation cohort (24.5%). The model had excellent discrimination with a C score of 0.80. Probability of favorable neurological survival ranged from 70.7% in the top decile of patients (CASPRI <10) and 2.8% in bottom decile (CASPRI ≥ 28).
This tool is not generalizable to patients with out-of-hospital arrest or undergoing therapeutic hypothermia.
Bottom line: CASPRI is a simple bedside tool validated to estimate probability of favorable neurological outcome after in-hospital cardiac arrest.
Citation: Chan PS, Spertus JA, Krumholz HA, et al. A validated prediction tool for initial survivors in in-hospital cardiac arrest. Arch Intern Med. 2012;172(12):947-953.
Increased Use of Radiologic Imaging and Associated Radiation Exposure in Integrated Healthcare Systems, 1996-2010
Clinical question: How much has imaging utilization and associated radiation exposure increased over 15 years in integrated healthcare systems independent of financial incentives in a fee-for-service system?
Background: Use of diagnostic imaging has increased significantly within fee-for-service healthcare models. The associated radiation exposure has increased the risk of radiation-induced malignancies. Little is known about the pattern of imaging use in integrated healthcare systems without the financial incentives seen in other models of care.
Study design: Retrospective cohort study.
Setting: Six integrated healthcare systems in the U.S.
Synopsis: The number of diagnostic imaging studies performed and estimated radiation exposure were determined from analysis of electronic medical records from member patients enrolled in health systems in the HMO Research Network from 1996 to 2010. Annual increases in use of advanced diagnostics were noted in CT (7.8% annual growth), MRI (10%), ultrasound (3.9%), and PET (57%) studies.
Increased CT use over the 15-year study period resulted in increased radiation exposure, doubling mean per capita effective dose (1.2 mSv to 2.3 mSv), as well as those receiving high exposure (1.2% to 2.5%) and very high exposure (0.6% to 1.4%).
The increased imaging use and radiation exposure among HMO enrollees was similar to that of fee-for-service Medicare patients in previous studies.
Bottom line: There is a significant increase in use of diagnostic imaging studies and associated radiation exposure among integrated healthcare system enrollees from 1996 to 2010, similar to patients in fee-for-service health plans.
Citation: Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA. 2012;307(22):2400-2409.
Postoperative Troponin Predicts 30-Day Mortality
Clinical question: Does postoperative peak troponin level predict 30-day mortality in patients undergoing noncardiac surgery?
Background: The use of postoperative peak troponin levels in predicting 30-day mortality for patients undergoing noncardiac surgery has not been studied extensively. Identifying patients at high risk for death following noncardiac surgery could facilitate appropriate postoperative care and improve survival.
Study design: Prospective cohort study.
Setting: International university and nonuniversity hospitals.
Synopsis: The Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) Study is a large, international, multicenter, prospective cohort study designed to evaluate the major complications of noncardiac surgery. More than 15,100 patients ages 45 and older requiring at least an overnight hospitalization were enrolled following noncardiac surgery.
Peak troponin measurements during the first three postoperative days of 0.01 ng/ml or less, 0.02 ng/ml, 0.03 ng/ml to 0.29 ng/ml, and 0.3 ng/ml or greater had 30-day mortality rates of 1.0%, 4.0%, 9.3%, and 16.9%, respectively.
This study demonstrates the sensitivity of troponin measurement for predicting postoperative 30-day mortality in patients undergoing noncardiac surgery. The study does not address interventions based on an increased postoperative troponin level. Future studies might investigate postoperative modifiable risk factors.
Bottom line: Postoperative peak troponin level predicts 30-day mortality in patients undergoing noncardiac surgery.
Citation: Devereaux PJ, Chan MT, Alonso-Coello P, et al. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2012;307(21):2295-2304.
Clinical Prediction Model of Mortality in Acute Heart Failure
Clinical question: Can a clinical prediction model accurately risk-stratify patients presenting to the ED with acute heart failure?
Background: Accurately prognosticating mortality is essential when determining whether to hospitalize or discharge patients presenting to the ED with acute heart failure. Evidence-based clinical prediction models enable physicians to risk-stratify patients and optimize care.
Study design: Retrospective cohort study.
Setting: Multicenter study of 86 hospitals in Ontario, Canada.
Synopsis: Data collected from 12,591 patients who presented to EDs with acute heart failure in Ontario were analyzed. A clinical prediction model of seven-day mortality of discharged and hospitalized patients was derived and validated. The Emergency Heart Failure Mortality Risk Grade (EHMRG) found an increased mortality based on higher triage heart rate, lower triage systolic blood pressure, initial oxygen saturation, and elevated troponin levels. This model uses readily available data collected in ED visits. The high-risk EHMRG score predicted about 8% seven-day mortality versus 0.3% in the low-risk score.
This model was not applied to chronic heart failure, did not utilize left ventricular function, and does not differentiate between systolic and diastolic heart failure.
Bottom line: The Emergency Heart Failure Mortality Risk Grade predicts seven-day mortality in acute heart failure in the emergent setting.
Citation: Lee DS, Stitt A, Austin PC, et al. Prediction of heart failure mortality in emergent care: a cohort study. Ann Intern Med. 2012;156(11):767-775.
Indwelling Pleural Catheter Is as Effective as Talc Pleurodesis Via Chest Tube in Relieving Dyspnea in Patients with Malignant Pleural Effusion
Clinical question: Is indwelling pleural catheter (IPC) as effective as chest tube and talc pleurodesis (talc) in improving dyspnea from malignant pleural effusion in patients who had no previous pleurodesis?
Background: Despite guidelines recommending chest tube insertion with pleurodesis as a first-line treatment for symptom palliation from malignant pleural effusion, there has been no randomized trial comparing indwelling pleural catheter with chest tube and talc pleurodesis.
Study design: Open-label, randomized controlled trial.
Setting: Seven hospitals in the United Kingdom.
Synopsis: One hundred six patients with malignant pleural effusion were randomized to undergo either IPC or talc treatment, and their daily mean dyspnea was measured. There was a clinically significant improvement of dyspnea in both IPC and talc groups over the first 42 days of the trial, without any significant difference in dyspnea between the two groups. After six months, researchers found a clinically significant decrease in dyspnea in the IPC group compared with the talc group. Chest pain and global quality of life were improved and were similar in both groups throughout the trial period. Length of hospital stay was significantly shorter in the IPC group compared with the talc group, but more patients in the IPC group experienced adverse events.
Bottom line: Indwelling pleural catheter is as effective as talc pleurodesis in reliving dyspnea from malignant pleural effusion; however, IPC is associated with increased adverse events despite shorter length of hospital stay.
Citation: Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs. chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion: the TIME2 randomized controlled trial. JAMA. 2012;307(22):2383-2389.
Early Surgery Better than Conventional Treatment in High-Risk Native-Valve Endocarditis
Clinical question: Is early cardiac surgery better than conventional treatment for patients with left-sided, native-valve, infective endocarditis?
Background: Although guidelines strongly recommend early surgery for patients with infective endocarditis and congestive heart failure, the timing of surgery for patients with large vegetations and high risk of embolism without heart failure symptoms remains controversial.
Study design: Prospective, randomized trial.
Setting: Two medical centers in South Korea.
Synopsis: Seventy-six patients with left-sided, native-valve, infective endocarditis with a high risk of embolism (defined as vegetation with a diameter greater than 10 mm or severe mitral or aortic valve disease) were randomized to undergo early surgery (within 48 hours of enrollment) or conventional treatment (antibiotic therapy and surgery only if complications required urgent surgery). The primary outcome of composite in-hospital death or
clinical embolic events within six weeks of the trial occurred in only one patient in the early surgery group, compared with nine patients in the conventional group (hazard ratio 0.10, 95% CI, 0.01-0.82, P=0.03).
There was no difference in all-cause mortality at six months between the two groups, but the rate of composite endpoint of death from any cause, embolic events, or recurrence of infective endocarditis at six months was significantly lower in the early surgery group compared with the conventional group.
Bottom line: Early cardiac surgery for patients with left-sided, native-valve infective endocarditis with a high risk of embolism significantly improved the composite outcome of all-cause mortality, embolic events, or recurrence of endocarditis compared with the conventional therapy.
Citation: Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366(26):2466-2473.
Risk Factors for Short-Term Mortality after Emergency Department Visit for Syncope
Clinical question: What are the risk factors for short-term mortality after an ED evaluation for syncope or near-syncope?
Background: Syncope accounts for 1% to 2% of all ED visits and an equal number of hospital admissions. The risk of death after an ED visit for syncope is poorly understood, resulting in frequent hospital admissions.
Study design: Retrospective cohort study.
Setting: EDs in Southern California.
Synopsis: Authors evaluated 23,951 ED visits resulting in syncope as sole primary diagnosis. Age was identified as the most significant risk factor for short-term mortality. Cumulative survival data revealed that more than 1% of patients 60 or older died by 30 days. There were 215 deaths (2.84%) in patients hospitalized from the ED and 66 deaths (0.45%) among patients not hospitalized.
Pre-existing comorbidities significantly associated with increased mortality included heart failure (HR=14.3 in ages 18-53; HR=3.09 in ages 60-79; HR=2.34 in ages 80-plus), diabetes (HR=1.49), seizure (HR=1.65), dementia (HR=1.41), and a recent prior visit for syncope (HR=1.86). The risk of death by 30 days was less than 0.2% in patients under 60 without heart failure and more than 2.5% in patients of all ages with heart failure.
Bottom line: After an ED visit for syncope, patients with a history of heart failure and patients 60 and older have a significantly increased risk of short-term mortality.
Citation: Derose SF, Gabayan GZ, Chiu VY, Sun BC. Patterns and preexisting risk factors of 30-day mortality after a primary discharge diagnosis of syncope or near syncope. Acad Emerg Med. 2012;19(5):488-496.
Acute Hyperglycemia Associated with Increased Mortality in Community-Acquired Pneumonia
Clinical question: In patients admitted to the hospital for community-acquired pneumonia, is serum glucose level on admission associated with mortality?
Background: Some retrospective studies have shown an association between alterations in serum glucose levels or pre-existing diabetes and higher mortality due to infections, while other studies have shown no clear association.
Study design: Multicenter, prospective cohort study.
Setting: Hospitals and private practices in Germany, Switzerland, and Austria.
Synopsis: Prospective data from 6,891 patients were included in the analysis. Patients without diabetes and normal serum glucose levels had the lowest mortality after 90 days. Patients without diabetes but with mild acute hyperglycemia (108 mg/dL to 198 mg/dL) had a significantly increased risk of death at 90 days (HR 1.56), and patients without diabetes but with more severe acute hyperglycemia (over 252 mg/dL) had an even higher risk of death at 90 days (HR 2.37).
The 90-day mortality rate was significantly higher in patients with pre-existing diabetes (HR 2.47), although this was not affected by serum glucose levels on admission.
Bottom line: Acute hyperglycemia, as well as pre-existing diabetes, was associated with an increased risk of 90-day mortality in patients with community acquired pneumonia.
Citation: Lepper PM, Ott S, Nüesch E, et al. Serum glucose levels for predicting death in patients admitted to hospital for community acquired pneumonia: prospective cohort study. BMJ. 2012;344:e3397.
Hospital Delirium Associated with Cognitive Decline, Institutionalization, and Death
Clinical question: What is the risk of subsequent cognitive decline, institutionalization, or death due to delirium in patients with dementia?
Background: Patients suffering delirium during hospitalization can suffer additional cognitive decline. Whether this is due to additional damage from the delirium state or reflects pre-existing cognitive vulnerability remains uncertain.
Study design: Prospective analysis of a cohort of Alzheimer’s patients.
Setting: Massachusetts community-based disease registry.
Synopsis: The analysis compared nonhospitalized individuals to patients hospitalized with, and without, delirium. In 771 individuals with dementia, at least one adverse outcome (including cognitive decline, institutionalization, or death) occurred in 32% of those not hospitalized, 55% of those hospitalized without delirium, and 79% of those hospitalized with delirium. Even after adjusting for confounders, hospitalization increased the risk for each of the adverse outcomes; the highest risk was in those with delirium.
Among hospitalized patients, the authors estimated 1 in 5 cases of cognitive decline, 1 in 7 institutionalizations, and 1 in 16 deaths were attributable to delirium. Some of the attributed risk could be the result of residual confounding from unmeasured variables, limiting conclusions of causality. Despite these limitations, this study supports the hypothesis that delirium prevention measures could improve important patient outcomes.
Bottom line: Hospitalization is associated with high rates of adverse outcomes in elderly patients with dementia, the worst of which occurs in those who experience delirium.
Citation: Fong TG, Jones RN, Marcantonio ER, et al. Adverse outcomes after hospitalization and delirium in persons with Alzheimer disease. Ann Int Med. 2012;156:848-856.
In Acute Pyelonephritis, a Seven-Day Course of Ciprofloxacin is Effective in Obtaining Clinical Cure
Clinical question: What is the efficacy of ciprofloxacin for seven days compared with 14 days in women with community-acquired acute pyelonephritis?
Background: Community-acquired acute pyelonephritis is a common and sometimes serious infection in women. In an era of increasing antibiotic resistance worldwide, it is prudent to reduce antibiotic utilization. There are limited controlled trials to assess the optimum duration of antibiotic treatment for this common infection.
Study design: Prospective, randomized, double-blind, noninferiority trial.
Setting: Twenty-one infectious-disease centers in Sweden.
Synopsis: Researchers randomly assigned 284 women 18 or older with a presumptive diagnosis of acute pyelonephritis to ciprofloxacin treatment for seven or 14 days. The primary endpoint was clinical and bacteriological cure 10 to 14 days after the completion of the treatment regimen. Short-term clinical cure occurred in 97% of the patients treated for seven days and 96% treated for 14 days. Long-term follow-up showed cumulative efficacy of 93% in each group. Both regimens were well tolerated.
Patients in this study had a low occurrence of complicated (9%) and recurrent (13%) infections. Whether short courses of antibiotics are effective in more complicated infections cannot be ascertained from this study. Also, the high cure rate obtained with a seven-day course of ciprofloxacin should not be extrapolated to other classes of antibiotics. Fluoroquinolones, such as ciprofloxacin, are recommended as first-line agents for empiric oral treatment of acute pyelonephritis if the resistance rate of the uropathogens remains lower than 10%; however, there is growing evidence that E. coli strains are becoming increasingly resistant to ciprofloxacin, limiting its usefulness.
Bottom line: Acute pyelonephritis in women can be treated successfully and safely with a seven-day course of ciprofloxacin, in areas with low ciprofloxacin resistance.
Citation: Sandberg T, Skoog G, Hermansson AB, et al. Ciprofloxacin for 7 days versus 14 days in women with acute pyelonephritis: a randomized, open-label and double-blind, placebo-controlled, non-inferiority trial. Lancet. 2012;380:484-490.
Advance Directives in Community Patients with Heart Failure
Clinical question: How prevalent are advance directives in heart-failure patients, and does a completed advance directive decrease end-of-life resource use (hospitalizations, ICU admissions, mechanical ventilation)?
Background: Heart failure is a common chronic and fatal disease. End-of-life care in heart-failure patients is associated with extremely high healthcare utilization. Heart failure guidelines recommend completing advance directives in all patients.
Study design: Population-based longitudinal cohort study.
Setting: Rochester Epidemiology Project in Olmstead County, Minn.
Synopsis: Investigators enrolled 608 patients presenting with heart failure between October 2007 and October 2011. At the time of enrollment, only 41% of the patients had existing advance directives. Independent predictors of advance directive completion included older age, history of malignancy, and renal dysfunction.
After a mean follow-up of 1.8 years, 164 patients (27%) had died. Among those patients, 106 had an advance directive (64.6%) at time of death—75 had an advance directive at the time of enrollment and another 31 completed an advance directive after enrollment.
Twenty-five patients (23.6%) specified DNR/DNI and another 39 (36.8%) denoted limitations on aggressiveness of care if death was imminent. Among the patients who died, 88 (53.7%) were hospitalized in the last month of their life and 50 (30.5%) died in the hospital. There was no difference in hospitalizations between those with an advance directive specifying limits and those who did not specify limits (OR 1.26, 95% CI 0.64-2.48). However, those with an advance directive specifying limits were less frequently mechanically ventilated (OR 0.26, 95% CI 0.06-0.88), and there was a trend toward them being less frequently admitted into the ICU (OR 0.45, 95% CI 0.16-1.29).
Bottom line: Less than half of community patients with heart failure had an advance directive, and many of these failed to address end-of-life decisions. Patients with an advance directive that specified limits in care were less likely to receive mechanical ventilation.
Citation: Dunlay SM, Swetz KM, Mueller PS, Roger VL. Advance directives in community patients with heart failure. Circ Cardiovasc Qual Outcomes. 2012;5:283-289.
Chlorhexidine Bathing Associated with Significant, Sustainable Reductions in Central-Venous-Catheter-Associated Bloodstream Infection
Clinical question: What is the impact, and sustainability, of chlorhexidine bathing on central-venous-catheter-associated bloodstream infections?
Background: Chlorhexidine bathing has been associated with reductions in healthcare-associated bloodstream infections, including vancomycin-resistant enterococci and methicillin-resistant Staphylococcus aureus. No prospective studies have evaluated the impact and sustainability of chlorhexidine bathing.
Study design: Prospective, three-phase study.
Setting: Medical-surgical ICUs and respiratory-care units at five New York hospitals.
Synopsis: In the pre-intervention phase (six to nine months, 1,808 admissions), patients were bathed with soap and water or nonmedicated bathing cloths. In the intervention phase (eight months, 1,832 admissions), patients were bathed with 2% chlorhexidine cloths. In the post-intervention phase (12 months, 2,834 admissions), chlorhexidine bathing was continued without oversight by researchers.
During the intervention phase, there were significantly fewer central-venous-catheter-associated bloodstream infections (2.6/1,000 catheter days vs. 6.4/1,000 pre-intervention). The reductions in bloodstream infections were sustained during the post-intervention period (2.9/1,000 catheter days). Compliance with chlorhexidine bathing was 82% and 88% during the intervention and post-intervention phases, and was well tolerated by the patients.
Limitations of this study include lack of patient-specific data and severity of illness data, as well as lack of randomization and blinding. Although not evaluated in this study, the savings associated with decreased bloodstream infections likely outweigh the cost of chlorhexidine bathing.
Bottom line: Chlorhexidine bathing is a well-tolerated, sustainable intervention that significantly reduces central-venous-catheter-associated bloodstream infections.
Citation: Montecalvo MA, McKenna D, Yarrish R, et al. Chlorhexidine bathing to reduce central venous catheter-associated bloodstream infection: impact and sustainability. Am J Med. 2012;125(5):505-511.
Simulation Training Improves Lumbar Puncture Skills
Clinical question: What effect does simulation have on lumbar puncture (LP) skills of PGY1 internal-medicine (IM) residents compared with PGY2-4 neurology residents who have not received simulation training?
Background: LPs are common procedures. The American College of General Medical Education does not define competency; neither do the internal-medicine (IM) or neurology board certifications. Simulation can improve skills in many areas but has not been well studied in LPs.
Study design: Pre-test-post-test.
Setting: Northwestern University’s Feinberg School of Medicine in Chicago.
Synopsis: The intervention group included 58 PGY1 IM residents, while the control group was 49 PGY2-to-PGY4 neurology residents. The pre-test consisted of a 21-point checklist. IM residents watched a three-hour video, performed LPs on simulators, and received feedback. The post-test was a clinical skills examination using the checklist. If this exam was failed, the participant practiced and was retested. Neurology residents completed the pre-test and demonstrated an LP using the simulator.
Pre-test passing was achieved by only 2% of IM residents and 6% of neurology residents. Post-test passing was achieved by 95% of the IM residents on the first trial and 100% of IM residents after an hour of additional training. IM mean scores increased to 95.7% from 46.3%, while the mean score of neurology residents was 65.4%.
This study is limited by its single-center nature, as education is variable from center to center. The study evaluated the proficiency on simulators only, and it did not evaluate the proficiency of the participants on patients.
Bottom line: Simulation training improves lumbar puncture skills.
Citation: Barsuk JH, Cohen ER, Caprio T, McGaghie WC, Simuni T, Wayne DB. Simulation-based education with mastery learning improves residents’ lumbar puncture skills. Neurology. 2012;79(2):132-137.
Primary-Care Physicians Do Not Use Publicly Reported Data When Referring Patients to Hospitals
Clinical question: When referring patients with pneumonia to the hospital, what factors do primary-care physicians (PCPs) consider?
Background: Publicly reported data are widely available. Pneumonia has publicly reported quality measures and is a common reason for hospitalization. Fewer PCPs are attending in the hospital due to the hospitalist movement; therefore, PCPs refer patients to a hospital when the need arises.
Study design: Online survey.
Setting: PCPs within 10 miles of Springfield, Mass.
Synopsis: A total of 92 PCPs responded to the survey, which included presentation of a case regarding a patient with pneumonia. PCPs were asked the importance of multiple factors leading to their decision to refer to a hospital. Familiarity with the hospital (70%), patient preference (62%), and admitting arrangements with a hospitalist group (62%) were considered to be very important to the PCPs that responded to the survey. Publicly reported data were very important to only 18% of respondents, and zero reported using publicly reported data when referring patients.
Importance of specific quality measures also was queried; antibiotics given within six hours of arrival (66%), appropriate choice of antibiotics (63%), and blood cultures prior to antibiotic administration (51%) were very important to respondents. Prestige, such as magnet status and U.S. News and World Report “Best Hospital” status, were deemed important by about 40% of PCPs.
Bottom line: Despite the availability of publicly reported data, PCPs do not use this information to refer patients to the hospital.
Citation: Morsi E, Lindenauer PK, Rothberg MB. Primary care physicians’ use of publicly reported quality data in hospital referral decisions. J Hosp Med. 2012;7(5):370-375.
What Works for Medication Reconciliation?
Clinical question: What are the most effective practices for medication reconciliation in the hospital setting?
Background: Medication discrepancies are common, occurring in as many as 70% of patients at hospital admission or discharge. Up to a third of these discrepancies have potential to cause patient harm, including prolonged hospital stays, ED visits, hospital recidivism, and use of other healthcare resources. Medication reconciliation (“med rec”) is a strategy for reducing these errors, though previous literature has not systematically reviewed best practices for hospital-based med rec.
Study design: Systematic review of literature.
Setting: Controlled studies from the U.S., Canada, Australia, New Zealand, Northern Ireland, United Kingdom, Belgium, Denmark, the Netherlands, and Sweden.
Synopsis: Investigators identified 26 controlled studies using a systematic search of English-language articles on med rec during inpatient hospitalizations published between Jan. 1, 1966, and Oct. 31, 2010. Fifteen studies reported on pharmacist-related interventions; six reported on technology-specific interventions; and five reported on other types of interventions, including staff education and use of standardized med-rec tools.
Analysis of these studies revealed that all of these interventions successfully decreased medication discrepancies and potential adverse drug events, but there was inconsistent benefit with regard to adverse drug events and healthcare utilization compared with usual care. The literature was most supportive of pharmacist-related interventions, including but not limited to comprehensive medication history at admission, med rec at discharge, patient counseling, discharge communication with outpatient providers, and post-discharge communication with the patient and post-hospital providers.
Bottom line: Successful med rec requires multiple interventions at various transitions of care and involves a variety of medical professionals. Patient-targeted interventions, including pharmacists, have the potential to decrease errors and adverse events.
Citation: Mueller S, Sponsler K, Kripalani S, Schnipper J. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med. 2012;172(14):1057-1069.
Evidence-Based Care Process Model for Febrile Infants Saves $2 Million
Clinical question: What is the impact of an evidence-based care process model (EB-CPM) on outcomes and costs in febrile infants?
Background: The care of febrile infants <90 days of age is common, and national guidelines have been in existence for nearly 20 years. However, variation in practice has been noted surrounding management of these infants, and there are limited reports of outcomes and costs related to implementation of local guidelines and quality-improvement (QI) projects.
Study design: Retrospective review of QI project.
Setting: Intermountain Healthcare System in Utah.
Synopsis: Over a period of five years, 8,044 infants with 8,431 febrile episodes were evaluated within the Intermountain Healthcare System, an integrated healthcare network that provides care for about 85% of the children in Utah. The EB-CPM was implemented in the middle of this five-year span and applied modified Rochester criteria to risk-stratify infants. Low-risk infants were eligible for discharge to home; high-risk infants were admitted and received viral testing. Infants with negative bacterial cultures and positive viral studies were eligible for discharge at 24 hours. For the remainder of admitted infants, discharge was recommended after 36 hours of negative bacterial cultures.
The review showed no statistically significant differences in readmissions or admission rates for serious bacterial infection before and after the implementation. There were significant reductions in mean hospital length of stay (60 to 44 hours, P<0.001) and cost per admitted infant ($7,178 to $5,979, P<0.001) after the EB-CPM was released. Cost savings were estimated at $1.9 million during the five-year study period.
Several limitations of this study are relevant. First, this QI project occurred within the confines of an integrated healthcare delivery system, a context that is uncommon in most of the country. Compliance with recommendations was not universal, which suggests that there is potential for improvement upon these results, or that clinical judgment played a significant role in decision-making.
Nonetheless, this report demonstrates that there is significant potential for cost savings with focused recommendations for discharge of febrile infants.
Bottom line: Standardized recommendations for discharge in febrile infants could result in substantial cost savings.
Citation: Byington CL, Reynolds CC, Korgenski K, et al. Cost and infant outcomes after implementation of a care process model for febrile infants. Pediatrics. 2012;130:e16-e24.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Clinical question: What is the impact of an evidence-based care process model (EB-CPM) on outcomes and costs in febrile infants?
Background: The care of febrile infants <90 days of age is common, and national guidelines have been in existence for nearly 20 years. However, variation in practice has been noted surrounding management of these infants, and there are limited reports of outcomes and costs related to implementation of local guidelines and quality-improvement (QI) projects.
Study design: Retrospective review of QI project.
Setting: Intermountain Healthcare System in Utah.
Synopsis: Over a period of five years, 8,044 infants with 8,431 febrile episodes were evaluated within the Intermountain Healthcare System, an integrated healthcare network that provides care for about 85% of the children in Utah. The EB-CPM was implemented in the middle of this five-year span and applied modified Rochester criteria to risk-stratify infants. Low-risk infants were eligible for discharge to home; high-risk infants were admitted and received viral testing. Infants with negative bacterial cultures and positive viral studies were eligible for discharge at 24 hours. For the remainder of admitted infants, discharge was recommended after 36 hours of negative bacterial cultures.
The review showed no statistically significant differences in readmissions or admission rates for serious bacterial infection before and after the implementation. There were significant reductions in mean hospital length of stay (60 to 44 hours, P<0.001) and cost per admitted infant ($7,178 to $5,979, P<0.001) after the EB-CPM was released. Cost savings were estimated at $1.9 million during the five-year study period.
Several limitations of this study are relevant. First, this QI project occurred within the confines of an integrated healthcare delivery system, a context that is uncommon in most of the country. Compliance with recommendations was not universal, which suggests that there is potential for improvement upon these results, or that clinical judgment played a significant role in decision-making.
Nonetheless, this report demonstrates that there is significant potential for cost savings with focused recommendations for discharge of febrile infants.
Bottom line: Standardized recommendations for discharge in febrile infants could result in substantial cost savings.
Citation: Byington CL, Reynolds CC, Korgenski K, et al. Cost and infant outcomes after implementation of a care process model for febrile infants. Pediatrics. 2012;130:e16-e24.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Clinical question: What is the impact of an evidence-based care process model (EB-CPM) on outcomes and costs in febrile infants?
Background: The care of febrile infants <90 days of age is common, and national guidelines have been in existence for nearly 20 years. However, variation in practice has been noted surrounding management of these infants, and there are limited reports of outcomes and costs related to implementation of local guidelines and quality-improvement (QI) projects.
Study design: Retrospective review of QI project.
Setting: Intermountain Healthcare System in Utah.
Synopsis: Over a period of five years, 8,044 infants with 8,431 febrile episodes were evaluated within the Intermountain Healthcare System, an integrated healthcare network that provides care for about 85% of the children in Utah. The EB-CPM was implemented in the middle of this five-year span and applied modified Rochester criteria to risk-stratify infants. Low-risk infants were eligible for discharge to home; high-risk infants were admitted and received viral testing. Infants with negative bacterial cultures and positive viral studies were eligible for discharge at 24 hours. For the remainder of admitted infants, discharge was recommended after 36 hours of negative bacterial cultures.
The review showed no statistically significant differences in readmissions or admission rates for serious bacterial infection before and after the implementation. There were significant reductions in mean hospital length of stay (60 to 44 hours, P<0.001) and cost per admitted infant ($7,178 to $5,979, P<0.001) after the EB-CPM was released. Cost savings were estimated at $1.9 million during the five-year study period.
Several limitations of this study are relevant. First, this QI project occurred within the confines of an integrated healthcare delivery system, a context that is uncommon in most of the country. Compliance with recommendations was not universal, which suggests that there is potential for improvement upon these results, or that clinical judgment played a significant role in decision-making.
Nonetheless, this report demonstrates that there is significant potential for cost savings with focused recommendations for discharge of febrile infants.
Bottom line: Standardized recommendations for discharge in febrile infants could result in substantial cost savings.
Citation: Byington CL, Reynolds CC, Korgenski K, et al. Cost and infant outcomes after implementation of a care process model for febrile infants. Pediatrics. 2012;130:e16-e24.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
When Is Testing for Thrombophilia Indicated?
The Case
A healthy 42-year-old woman presents to the hospital with acute-onset pleuritic chest pain and shortness of breath. She has not had any recent surgeries, takes no medications, and is very active. A lung ventilation-perfusion scan reveals a high probability of pulmonary embolism (PE). The patient’s history is notable for two second-trimester pregnancy losses. The patient is started on low-molecular heparin and warfarin (LMHW).
Should this patient be tested for thrombophilia?
Background
Thrombophilia can now be identified in more than half of all patients presenting with VTE, and testing for underlying causes of thrombophilia has become widespread.1 Physicians believe that thrombophilia testing frequently changes management of patients with VTE.2
Thrombophilias can be classified into three major categories: deficiency of natural inhibitors of coagulation, abnormal function or elevated level of coagulation factors, and acquired thrombophilias (see Table 1).
The prevalence of specific thrombophilias varies widely. For example, the prevalence of activated protein C resistance (the factor V Leiden mutation) is 3% to 7%. In comparison, the prevalence of antithrombin deficiency is estimated at 0.02%. Each thrombophilia is associated with an increased VTE risk, but the level of risk associated with a given thrombophilia varies greatly.1
Before testing for thrombophilia in acute VTE, assess the risk of recurrent VTE by determining if the thrombosis was provoked or unprovoked. A VTE event is considered provoked if it occurs in the setting of pregnancy within the previous three months; estrogen therapy; immobility from acute illness for more than one week; travel lasting for more than six hours; leg trauma, fracture, or surgery within the previous three months; or active malignancy (see Table 2,).3 Unprovoked VTE has a recurrence rate of 7.4% per patient year, compared with 3.3% per patient year for a provoked VTE; the risk is even lower (0.7% per patient year) if the risk factor for the provoked VTE was surgical.4
Testing for thrombophilia is indicated if the results would add significant prognostic information beyond the clinical history, or if it would change patient management—in particular, the intensity or the duration of anticoagulation.
Review of the Data
Does presence of thrombophilia alter the intensity of anticoagulation for VTE?
If thrombophilia increases the risk of VTE recurrence while on anticoagulation, then a more intense level of anticoagulation might prevent future VTE. There are no studies investigating higher intensity of anticoagulation, but if standard anticoagulation were insufficient for patients with identifiable thrombophilia, one might expect to observe increased recurrence rates among patients with thrombophilia treated with standard warfarin therapy.
In a substudy of the Extended Low-Intensity Anticoagulation for Unprovoked Venous ThromboEmbolism (ELATE) trial, the risk of recurrence of VTE among treated subjects was very low overall, and the presence of thrombophilic abnormalities was not associated with significantly higher risk.5 Observational studies have found VTE recurrence rates are low in patients treated with warfarin, with or without thrombophilia.6-8
The impact of the initial level of anticoagulation on recurrence after the completion of the treatment period has been evaluated. Although one study suggested that patients with substandard levels of anticoagulation were at an increased risk of subsequent VTE, this was not confirmed in the Leiden Thrombophilia Study (LETS). 9,10
In sum, the majority of data do not suggest a significantly increased risk of recurrent VTE in patients with thrombophilia treated with standard anticoagulation. Therefore, treatment with warfarin to a goal INR of 2 to 3 is sufficient.
Does presence of thrombophilia alter duration of VTE treatment?
A major decision clinicians face when caring for VTE patients is the duration of anticoagulation treatment. The current ACCP recommendation for treatment of a provoked VTE is three months, with treatment for an unprovoked VTE three months or lifelong.11 If the presence of thrombophilia increases the risk of recurrence after cessation of anticoagulation treatment, longer duration of treatment might be indicated. One of the goals of thrombophilia testing should be to identify those patients.
Overall, the recurrence rate after first VTE is high, with a cumulative incidence of 25% at five years, 30% at eight years, and 56% at 20 years.12,13
Deficiency of natural inhibitors of coagulation.
Deficiency of a natural inhibitor of coagulation has been associated with a risk of recurrence of VTE of as much as 10% per year, according to some studies.6,14 However, the estimates are based on studies that include individuals from thrombosis-prone families, and selection bias might have contributed to the high recurrence rates.1 In the unselected population represented in the LETS study, only a modest elevation was seen in the estimated risk of recurrence for patients with inhibitor deficiencies.15
Testing for deficiency of inhibitors offers little prognostic information beyond that obtained when determining whether a VTE event is provoked or unprovoked. In studies that have separately examined subjects with provoked vs. unprovoked VTE, deficiency of an inhibitor is not associated with increased risk of recurrence.15,16
Abnormal function or level of anticoagulation factors.
Factor V Leiden (FVL) is the most common cause of inherited thrombophilia and is associated with as much as a sixfold increase in VTE risk, while the prothrombin gene mutation is associated with a twofold increase.17,18
In contrast, the evidence associating these mutations with recurrent VTE risk is not as consistent. Although a study conducted at a referral center in Italy found an increased risk of recurrence with either Factor V Leiden or prothrombin gene mutation, a large meta-analysis of 23 studies found increased risk only with Factor V Leiden.19,20 Another meta-analysis demonstrated only a modest increased risk of recurrence in subjects with Factor V Leiden or prothrombin gene mutation, and a prospective study from Austria found no increased risk of recurrence with Factor V Leiden two years after discontinuation of anticoagulation.18,21 Additionally, when using patients with unprovoked VTE as reference, there was no increased risk of recurrence among patients homozygous for Factor V Leiden or the prothrombin gene mutation.22
In summary, although Factor V Leiden and prothrombin gene defects are associated with increased risk of recurrent VTE, the magnitude of the risk increase is modest and, therefore, should not alter duration of therapy.
Acquired thrombophilia.
It appears that the only thrombophilic state that might have a significant impact on the risk of recurrence is the antiphospholipid syndrome. The cessation of warfarin therapy in patients with thrombosis associated with antiphospholipid antibodies carries a 69% risk of recurrent thrombosis within a year.23 Some studies have suggested that the presence of specific antibodies (i.e. anticardiolipin antibodies) is associated with increased risk in patients with antiphospholipid syndrome.24
However, at present, all patients with VTE and antiphospholipid syndrome should be candidates for lifelong anticoagulation. Antiphospholipid antibody testing should be performed in patients with a suggestive history, including those with recurrent fetal loss or a single fetal loss after 10 weeks, or known collagen vascular disease.25
The role of provoked vs. unprovoked VTE.
Identifying whether a VTE is provoked or unprovoked has been shown to be an important predictor of recurrence. For example, one prospective, cohort study found two-year recurrence rates of zero in patients with a surgery or pregnancy-related VTE, 9% with other provoked VTE, and 19% with unprovoked VTE.26 In the same study, thrombophilia testing failed to reliably predict recurrence risk. Patients with unprovoked VTE who were tested and found to not have a defect were at equally high risk of recurrent VTE as those found to have a thrombophilia.27
The most significant predictor for VTE recurrence is whether the first event was provoked, and thrombophilia testing offers little additional prognostic information.28
VTE as a multifactorial disorder.
It is becoming increasingly clear that VTE is multifactorial disorder, caused by the interactions of genotypic, phenotypic, and environmental factors. In the case of an unprovoked VTE, the patient already carries a significantly elevated risk for recurrence, and further testing for known causes of thrombophilia appears to add very little additional information. The optimal duration of anticoagulation for unprovoked VTE is unclear, but current guidelines suggest at least three months—and clinicians should consider lifelong treatment.
In the vast majority of cases, testing for thrombophilia has no impact on the management of VTE and is not warranted. In patients with antiphospholipid-antibody syndrome, given the high risk of recurrence, long-term anticoagulation after a first VTE might be indicated. In select patients with a clinical picture suggestive of antiphospholipid-antibody syndrome, or a strong family history, testing should be considered.
Back to the Case
Our patient appears to have an unprovoked VTE. She should receive regular anticoagulation with warfarin, with a goal INR of 2 to 3, for at least three months. Lifelong anticoagulation therapy should be considered. Testing for heritable thrombophilia will not change the current management or treatment duration and, hence, is not indicated. However, the patient’s history is suggestive of antiphospholipid-antibody syndrome, so she should be tested. If the diagnosis of antiphospholipid syndrome is made, lifelong anticoagulation should be considered.
Bottom Line
Unprovoked VTE provides the strongest predictor for recurrence. Thrombophilia testing adds little in predicting recurrence and rarely is indicated.
Dr. Stehlikova is a clinical hospitalist in the division of hospital medicine, department of medicine, at Albert Einstein College of Medicine and Montefiore Medical Center in Bronx, N.Y. Dr. Martin is director of the Einstein Hospitalist Service. Dr. Janakiram is a fellow in the department of hematology at Einstein, and Dr. Korcak is an instructor at Einstein in the department of medicine and director of the Weiler Medical Service. Dr. Galhotra is associate director for inpatient quality in the department of medicine at Einstein; Dr. Averbukh is an academic hospitalist; and Dr. Southern is chief of the division of hospital medicine at Einstein.
References
- Middeldorp S, van Hylckama Vlieg A. Does thrombophilia testing help in the clinical management of patients? Br J Haematol. 2008;143:321-335.
- Coppens M, van Mourik JA, Eckmann CM, Büller HR, Middeldorp S. Current practise of testing for inherited thrombophilia. J Thromb Haemost. 2007;5:1979-1981.
- Prandoni P, Noventa F, Ghirarduzzi A, et al. The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica. 2007;92:199-205.
- Iorio A, Kearon C, Filippucci E, et al. Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review. Arch Intern Med. 2010;170:1710-1716.
- Kearon C, Julian JA, Kovacs MJ, et al. Influence of thrombophilia on risk of recurrent venous thromboembolism while on warfarin: results from a randomized trial. Blood. 2008;112:4432-4436.
- Vossen CY, Walker ID, Svensson P, et al. Recurrence rate after a first venous thrombosis in patients with familial thrombophilia. Arterioscler Thromb Vasc Biol. 2005;25:1992-1997.
- Brown K, Luddington R, Williamson D, Baker P, Baglin T. Risk of venous thromboembolism associated with a G to A transition at position 20210 in the 3'-untranslated region of the prothrombin gene. Br J Haematol. 1997;98:907-909.
- Schulman S, Tengborn L. Treatment of venous thromboembolism in patients with congenital deficiency of antithrombin III. Thromb Haemost. 1992;68:634-636.
- Palareti G, Legnani C, Cosmi B, Guazzaloca G, Cini M, Mattarozzi S. Poor anticoagulation quality in the first 3 months after unprovoked venous thromboembolism is a risk factor for long-term recurrence. J Thromb Haemost. 2005;3:955-961.
- Gadisseur AP, Christiansen SC, van der Meer FJ, Rosendaal FR. The quality of oral anticoagulant therapy and recurrent venous thrombotic events in the Leiden Thrombophilia Study. J Thromb Haemost. 2007;5:931-936.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:454S-545S.
- Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1-7.
- Laczkovics C, Grafenhofer H, Kaider A, et al. Risk of recurrence after a first venous thromboembolic event in young women. Haematologica. 2007;92:1201-1207.
- Brouwer JL, Lijfering WM, Ten Kate MK, Kluin-Nelemans HC, Veeger NJ, van der Meer J. High long-term absolute risk of recurrent venous thromboembolism in patients with hereditary deficiencies of protein S, protein C or antithrombin. Thromb Haemost. 2009;101:93-99.
- Christiansen SC, Cannegieter SC, Koster T, Vandenbroucke JP, Rosendaal FR. Thrombophilia, clinical factors, and recurrent venous thrombotic events. JAMA. 2005;293:2352-2361.
- De Stefano V, Simioni P, Rossi E, et al. The risk of recurrent venous thromboembolism in patients with inherited deficiency of natural anticoagulants antithrombin, protein C and protein S. Haematologica. 2006;91:695-698.
- Price DT, Ridker PM. Factor V Leiden mutation and the risks for thromboembolic disease: a clinical perspective. Ann Intern Med. 1997;127:895-903.
- Ho WK, Hankey GJ, Quinlan DJ, Eikelboom JW. Risk of recurrent venous thromboembolism in patients with common thrombophilia: a systematic review. Arch Intern Med. 2006;166:729-736.
- Simioni P, Prandoni P, Lensing AW, et al. Risk for subsequent venous thromboembolic complications in carriers of the prothrombin or the factor V gene mutation with a first episode of deep-vein thrombosis. Blood. 2000;96:3329-3333.
- Segal JB, Brotman DJ, Necochea AJ, et al. Predictive value of factor V Leiden and prothrombin G20210A in adults with venous thromboembolism and in family members of those with a mutation: a systematic review. JAMA. 2009;301:2472-2485.
- Eichinger S, Pabinger I, Stumpflen A, et al. The risk of recurrent venous thromboembolism in patients with and without factor V Leiden. Thromb Haemost. 1997;77:624-628.
- Lijfering WM, Middeldorp S, Veeger NJ, et al. Risk of recurrent venous thrombosis in homozygous carriers and double heterozygous carriers of factor V Leiden and prothrombin G20210A. Circulation. 2010;121(15):1706-1712.
- Khamashta MA, Cuadrado MJ, Mujic F, Taub NA, Hunt BJ, Hughes GR. The management of thrombosis in the antiphospholipid-antibody syndrome. N Engl J Med. 1995;332:993-997.
- Schulman S, Svenungsson E, Granqvist S. Anticardiolipin antibodies predict early recurrence of thromboembolism and death among patients with venous thromboembolism following anticoagulant therapy. Duration of Anticoagulation Study Group. Am J Med. 1998;104:332-338.
- Pengo V, Tripodi A, Reber G, et al. Update of the guidelines for lupus anticoagulant detection. Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2009;7:1737-1740.
- Baglin T, Luddington R, Brown K, Baglin C. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: prospective cohort study. Lancet. 2003;362:523-526.
- Rosendaal FR. Once and only once. Circulation. 2010;121:1688-1690.
- Dalen JE. Should patients with venous thromboembolism be screened for thrombophilia? Am J Med. 2008;121:458-463.
The Case
A healthy 42-year-old woman presents to the hospital with acute-onset pleuritic chest pain and shortness of breath. She has not had any recent surgeries, takes no medications, and is very active. A lung ventilation-perfusion scan reveals a high probability of pulmonary embolism (PE). The patient’s history is notable for two second-trimester pregnancy losses. The patient is started on low-molecular heparin and warfarin (LMHW).
Should this patient be tested for thrombophilia?
Background
Thrombophilia can now be identified in more than half of all patients presenting with VTE, and testing for underlying causes of thrombophilia has become widespread.1 Physicians believe that thrombophilia testing frequently changes management of patients with VTE.2
Thrombophilias can be classified into three major categories: deficiency of natural inhibitors of coagulation, abnormal function or elevated level of coagulation factors, and acquired thrombophilias (see Table 1).
The prevalence of specific thrombophilias varies widely. For example, the prevalence of activated protein C resistance (the factor V Leiden mutation) is 3% to 7%. In comparison, the prevalence of antithrombin deficiency is estimated at 0.02%. Each thrombophilia is associated with an increased VTE risk, but the level of risk associated with a given thrombophilia varies greatly.1
Before testing for thrombophilia in acute VTE, assess the risk of recurrent VTE by determining if the thrombosis was provoked or unprovoked. A VTE event is considered provoked if it occurs in the setting of pregnancy within the previous three months; estrogen therapy; immobility from acute illness for more than one week; travel lasting for more than six hours; leg trauma, fracture, or surgery within the previous three months; or active malignancy (see Table 2,).3 Unprovoked VTE has a recurrence rate of 7.4% per patient year, compared with 3.3% per patient year for a provoked VTE; the risk is even lower (0.7% per patient year) if the risk factor for the provoked VTE was surgical.4
Testing for thrombophilia is indicated if the results would add significant prognostic information beyond the clinical history, or if it would change patient management—in particular, the intensity or the duration of anticoagulation.
Review of the Data
Does presence of thrombophilia alter the intensity of anticoagulation for VTE?
If thrombophilia increases the risk of VTE recurrence while on anticoagulation, then a more intense level of anticoagulation might prevent future VTE. There are no studies investigating higher intensity of anticoagulation, but if standard anticoagulation were insufficient for patients with identifiable thrombophilia, one might expect to observe increased recurrence rates among patients with thrombophilia treated with standard warfarin therapy.
In a substudy of the Extended Low-Intensity Anticoagulation for Unprovoked Venous ThromboEmbolism (ELATE) trial, the risk of recurrence of VTE among treated subjects was very low overall, and the presence of thrombophilic abnormalities was not associated with significantly higher risk.5 Observational studies have found VTE recurrence rates are low in patients treated with warfarin, with or without thrombophilia.6-8
The impact of the initial level of anticoagulation on recurrence after the completion of the treatment period has been evaluated. Although one study suggested that patients with substandard levels of anticoagulation were at an increased risk of subsequent VTE, this was not confirmed in the Leiden Thrombophilia Study (LETS). 9,10
In sum, the majority of data do not suggest a significantly increased risk of recurrent VTE in patients with thrombophilia treated with standard anticoagulation. Therefore, treatment with warfarin to a goal INR of 2 to 3 is sufficient.
Does presence of thrombophilia alter duration of VTE treatment?
A major decision clinicians face when caring for VTE patients is the duration of anticoagulation treatment. The current ACCP recommendation for treatment of a provoked VTE is three months, with treatment for an unprovoked VTE three months or lifelong.11 If the presence of thrombophilia increases the risk of recurrence after cessation of anticoagulation treatment, longer duration of treatment might be indicated. One of the goals of thrombophilia testing should be to identify those patients.
Overall, the recurrence rate after first VTE is high, with a cumulative incidence of 25% at five years, 30% at eight years, and 56% at 20 years.12,13
Deficiency of natural inhibitors of coagulation.
Deficiency of a natural inhibitor of coagulation has been associated with a risk of recurrence of VTE of as much as 10% per year, according to some studies.6,14 However, the estimates are based on studies that include individuals from thrombosis-prone families, and selection bias might have contributed to the high recurrence rates.1 In the unselected population represented in the LETS study, only a modest elevation was seen in the estimated risk of recurrence for patients with inhibitor deficiencies.15
Testing for deficiency of inhibitors offers little prognostic information beyond that obtained when determining whether a VTE event is provoked or unprovoked. In studies that have separately examined subjects with provoked vs. unprovoked VTE, deficiency of an inhibitor is not associated with increased risk of recurrence.15,16
Abnormal function or level of anticoagulation factors.
Factor V Leiden (FVL) is the most common cause of inherited thrombophilia and is associated with as much as a sixfold increase in VTE risk, while the prothrombin gene mutation is associated with a twofold increase.17,18
In contrast, the evidence associating these mutations with recurrent VTE risk is not as consistent. Although a study conducted at a referral center in Italy found an increased risk of recurrence with either Factor V Leiden or prothrombin gene mutation, a large meta-analysis of 23 studies found increased risk only with Factor V Leiden.19,20 Another meta-analysis demonstrated only a modest increased risk of recurrence in subjects with Factor V Leiden or prothrombin gene mutation, and a prospective study from Austria found no increased risk of recurrence with Factor V Leiden two years after discontinuation of anticoagulation.18,21 Additionally, when using patients with unprovoked VTE as reference, there was no increased risk of recurrence among patients homozygous for Factor V Leiden or the prothrombin gene mutation.22
In summary, although Factor V Leiden and prothrombin gene defects are associated with increased risk of recurrent VTE, the magnitude of the risk increase is modest and, therefore, should not alter duration of therapy.
Acquired thrombophilia.
It appears that the only thrombophilic state that might have a significant impact on the risk of recurrence is the antiphospholipid syndrome. The cessation of warfarin therapy in patients with thrombosis associated with antiphospholipid antibodies carries a 69% risk of recurrent thrombosis within a year.23 Some studies have suggested that the presence of specific antibodies (i.e. anticardiolipin antibodies) is associated with increased risk in patients with antiphospholipid syndrome.24
However, at present, all patients with VTE and antiphospholipid syndrome should be candidates for lifelong anticoagulation. Antiphospholipid antibody testing should be performed in patients with a suggestive history, including those with recurrent fetal loss or a single fetal loss after 10 weeks, or known collagen vascular disease.25
The role of provoked vs. unprovoked VTE.
Identifying whether a VTE is provoked or unprovoked has been shown to be an important predictor of recurrence. For example, one prospective, cohort study found two-year recurrence rates of zero in patients with a surgery or pregnancy-related VTE, 9% with other provoked VTE, and 19% with unprovoked VTE.26 In the same study, thrombophilia testing failed to reliably predict recurrence risk. Patients with unprovoked VTE who were tested and found to not have a defect were at equally high risk of recurrent VTE as those found to have a thrombophilia.27
The most significant predictor for VTE recurrence is whether the first event was provoked, and thrombophilia testing offers little additional prognostic information.28
VTE as a multifactorial disorder.
It is becoming increasingly clear that VTE is multifactorial disorder, caused by the interactions of genotypic, phenotypic, and environmental factors. In the case of an unprovoked VTE, the patient already carries a significantly elevated risk for recurrence, and further testing for known causes of thrombophilia appears to add very little additional information. The optimal duration of anticoagulation for unprovoked VTE is unclear, but current guidelines suggest at least three months—and clinicians should consider lifelong treatment.
In the vast majority of cases, testing for thrombophilia has no impact on the management of VTE and is not warranted. In patients with antiphospholipid-antibody syndrome, given the high risk of recurrence, long-term anticoagulation after a first VTE might be indicated. In select patients with a clinical picture suggestive of antiphospholipid-antibody syndrome, or a strong family history, testing should be considered.
Back to the Case
Our patient appears to have an unprovoked VTE. She should receive regular anticoagulation with warfarin, with a goal INR of 2 to 3, for at least three months. Lifelong anticoagulation therapy should be considered. Testing for heritable thrombophilia will not change the current management or treatment duration and, hence, is not indicated. However, the patient’s history is suggestive of antiphospholipid-antibody syndrome, so she should be tested. If the diagnosis of antiphospholipid syndrome is made, lifelong anticoagulation should be considered.
Bottom Line
Unprovoked VTE provides the strongest predictor for recurrence. Thrombophilia testing adds little in predicting recurrence and rarely is indicated.
Dr. Stehlikova is a clinical hospitalist in the division of hospital medicine, department of medicine, at Albert Einstein College of Medicine and Montefiore Medical Center in Bronx, N.Y. Dr. Martin is director of the Einstein Hospitalist Service. Dr. Janakiram is a fellow in the department of hematology at Einstein, and Dr. Korcak is an instructor at Einstein in the department of medicine and director of the Weiler Medical Service. Dr. Galhotra is associate director for inpatient quality in the department of medicine at Einstein; Dr. Averbukh is an academic hospitalist; and Dr. Southern is chief of the division of hospital medicine at Einstein.
References
- Middeldorp S, van Hylckama Vlieg A. Does thrombophilia testing help in the clinical management of patients? Br J Haematol. 2008;143:321-335.
- Coppens M, van Mourik JA, Eckmann CM, Büller HR, Middeldorp S. Current practise of testing for inherited thrombophilia. J Thromb Haemost. 2007;5:1979-1981.
- Prandoni P, Noventa F, Ghirarduzzi A, et al. The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica. 2007;92:199-205.
- Iorio A, Kearon C, Filippucci E, et al. Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review. Arch Intern Med. 2010;170:1710-1716.
- Kearon C, Julian JA, Kovacs MJ, et al. Influence of thrombophilia on risk of recurrent venous thromboembolism while on warfarin: results from a randomized trial. Blood. 2008;112:4432-4436.
- Vossen CY, Walker ID, Svensson P, et al. Recurrence rate after a first venous thrombosis in patients with familial thrombophilia. Arterioscler Thromb Vasc Biol. 2005;25:1992-1997.
- Brown K, Luddington R, Williamson D, Baker P, Baglin T. Risk of venous thromboembolism associated with a G to A transition at position 20210 in the 3'-untranslated region of the prothrombin gene. Br J Haematol. 1997;98:907-909.
- Schulman S, Tengborn L. Treatment of venous thromboembolism in patients with congenital deficiency of antithrombin III. Thromb Haemost. 1992;68:634-636.
- Palareti G, Legnani C, Cosmi B, Guazzaloca G, Cini M, Mattarozzi S. Poor anticoagulation quality in the first 3 months after unprovoked venous thromboembolism is a risk factor for long-term recurrence. J Thromb Haemost. 2005;3:955-961.
- Gadisseur AP, Christiansen SC, van der Meer FJ, Rosendaal FR. The quality of oral anticoagulant therapy and recurrent venous thrombotic events in the Leiden Thrombophilia Study. J Thromb Haemost. 2007;5:931-936.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:454S-545S.
- Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1-7.
- Laczkovics C, Grafenhofer H, Kaider A, et al. Risk of recurrence after a first venous thromboembolic event in young women. Haematologica. 2007;92:1201-1207.
- Brouwer JL, Lijfering WM, Ten Kate MK, Kluin-Nelemans HC, Veeger NJ, van der Meer J. High long-term absolute risk of recurrent venous thromboembolism in patients with hereditary deficiencies of protein S, protein C or antithrombin. Thromb Haemost. 2009;101:93-99.
- Christiansen SC, Cannegieter SC, Koster T, Vandenbroucke JP, Rosendaal FR. Thrombophilia, clinical factors, and recurrent venous thrombotic events. JAMA. 2005;293:2352-2361.
- De Stefano V, Simioni P, Rossi E, et al. The risk of recurrent venous thromboembolism in patients with inherited deficiency of natural anticoagulants antithrombin, protein C and protein S. Haematologica. 2006;91:695-698.
- Price DT, Ridker PM. Factor V Leiden mutation and the risks for thromboembolic disease: a clinical perspective. Ann Intern Med. 1997;127:895-903.
- Ho WK, Hankey GJ, Quinlan DJ, Eikelboom JW. Risk of recurrent venous thromboembolism in patients with common thrombophilia: a systematic review. Arch Intern Med. 2006;166:729-736.
- Simioni P, Prandoni P, Lensing AW, et al. Risk for subsequent venous thromboembolic complications in carriers of the prothrombin or the factor V gene mutation with a first episode of deep-vein thrombosis. Blood. 2000;96:3329-3333.
- Segal JB, Brotman DJ, Necochea AJ, et al. Predictive value of factor V Leiden and prothrombin G20210A in adults with venous thromboembolism and in family members of those with a mutation: a systematic review. JAMA. 2009;301:2472-2485.
- Eichinger S, Pabinger I, Stumpflen A, et al. The risk of recurrent venous thromboembolism in patients with and without factor V Leiden. Thromb Haemost. 1997;77:624-628.
- Lijfering WM, Middeldorp S, Veeger NJ, et al. Risk of recurrent venous thrombosis in homozygous carriers and double heterozygous carriers of factor V Leiden and prothrombin G20210A. Circulation. 2010;121(15):1706-1712.
- Khamashta MA, Cuadrado MJ, Mujic F, Taub NA, Hunt BJ, Hughes GR. The management of thrombosis in the antiphospholipid-antibody syndrome. N Engl J Med. 1995;332:993-997.
- Schulman S, Svenungsson E, Granqvist S. Anticardiolipin antibodies predict early recurrence of thromboembolism and death among patients with venous thromboembolism following anticoagulant therapy. Duration of Anticoagulation Study Group. Am J Med. 1998;104:332-338.
- Pengo V, Tripodi A, Reber G, et al. Update of the guidelines for lupus anticoagulant detection. Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2009;7:1737-1740.
- Baglin T, Luddington R, Brown K, Baglin C. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: prospective cohort study. Lancet. 2003;362:523-526.
- Rosendaal FR. Once and only once. Circulation. 2010;121:1688-1690.
- Dalen JE. Should patients with venous thromboembolism be screened for thrombophilia? Am J Med. 2008;121:458-463.
The Case
A healthy 42-year-old woman presents to the hospital with acute-onset pleuritic chest pain and shortness of breath. She has not had any recent surgeries, takes no medications, and is very active. A lung ventilation-perfusion scan reveals a high probability of pulmonary embolism (PE). The patient’s history is notable for two second-trimester pregnancy losses. The patient is started on low-molecular heparin and warfarin (LMHW).
Should this patient be tested for thrombophilia?
Background
Thrombophilia can now be identified in more than half of all patients presenting with VTE, and testing for underlying causes of thrombophilia has become widespread.1 Physicians believe that thrombophilia testing frequently changes management of patients with VTE.2
Thrombophilias can be classified into three major categories: deficiency of natural inhibitors of coagulation, abnormal function or elevated level of coagulation factors, and acquired thrombophilias (see Table 1).
The prevalence of specific thrombophilias varies widely. For example, the prevalence of activated protein C resistance (the factor V Leiden mutation) is 3% to 7%. In comparison, the prevalence of antithrombin deficiency is estimated at 0.02%. Each thrombophilia is associated with an increased VTE risk, but the level of risk associated with a given thrombophilia varies greatly.1
Before testing for thrombophilia in acute VTE, assess the risk of recurrent VTE by determining if the thrombosis was provoked or unprovoked. A VTE event is considered provoked if it occurs in the setting of pregnancy within the previous three months; estrogen therapy; immobility from acute illness for more than one week; travel lasting for more than six hours; leg trauma, fracture, or surgery within the previous three months; or active malignancy (see Table 2,).3 Unprovoked VTE has a recurrence rate of 7.4% per patient year, compared with 3.3% per patient year for a provoked VTE; the risk is even lower (0.7% per patient year) if the risk factor for the provoked VTE was surgical.4
Testing for thrombophilia is indicated if the results would add significant prognostic information beyond the clinical history, or if it would change patient management—in particular, the intensity or the duration of anticoagulation.
Review of the Data
Does presence of thrombophilia alter the intensity of anticoagulation for VTE?
If thrombophilia increases the risk of VTE recurrence while on anticoagulation, then a more intense level of anticoagulation might prevent future VTE. There are no studies investigating higher intensity of anticoagulation, but if standard anticoagulation were insufficient for patients with identifiable thrombophilia, one might expect to observe increased recurrence rates among patients with thrombophilia treated with standard warfarin therapy.
In a substudy of the Extended Low-Intensity Anticoagulation for Unprovoked Venous ThromboEmbolism (ELATE) trial, the risk of recurrence of VTE among treated subjects was very low overall, and the presence of thrombophilic abnormalities was not associated with significantly higher risk.5 Observational studies have found VTE recurrence rates are low in patients treated with warfarin, with or without thrombophilia.6-8
The impact of the initial level of anticoagulation on recurrence after the completion of the treatment period has been evaluated. Although one study suggested that patients with substandard levels of anticoagulation were at an increased risk of subsequent VTE, this was not confirmed in the Leiden Thrombophilia Study (LETS). 9,10
In sum, the majority of data do not suggest a significantly increased risk of recurrent VTE in patients with thrombophilia treated with standard anticoagulation. Therefore, treatment with warfarin to a goal INR of 2 to 3 is sufficient.
Does presence of thrombophilia alter duration of VTE treatment?
A major decision clinicians face when caring for VTE patients is the duration of anticoagulation treatment. The current ACCP recommendation for treatment of a provoked VTE is three months, with treatment for an unprovoked VTE three months or lifelong.11 If the presence of thrombophilia increases the risk of recurrence after cessation of anticoagulation treatment, longer duration of treatment might be indicated. One of the goals of thrombophilia testing should be to identify those patients.
Overall, the recurrence rate after first VTE is high, with a cumulative incidence of 25% at five years, 30% at eight years, and 56% at 20 years.12,13
Deficiency of natural inhibitors of coagulation.
Deficiency of a natural inhibitor of coagulation has been associated with a risk of recurrence of VTE of as much as 10% per year, according to some studies.6,14 However, the estimates are based on studies that include individuals from thrombosis-prone families, and selection bias might have contributed to the high recurrence rates.1 In the unselected population represented in the LETS study, only a modest elevation was seen in the estimated risk of recurrence for patients with inhibitor deficiencies.15
Testing for deficiency of inhibitors offers little prognostic information beyond that obtained when determining whether a VTE event is provoked or unprovoked. In studies that have separately examined subjects with provoked vs. unprovoked VTE, deficiency of an inhibitor is not associated with increased risk of recurrence.15,16
Abnormal function or level of anticoagulation factors.
Factor V Leiden (FVL) is the most common cause of inherited thrombophilia and is associated with as much as a sixfold increase in VTE risk, while the prothrombin gene mutation is associated with a twofold increase.17,18
In contrast, the evidence associating these mutations with recurrent VTE risk is not as consistent. Although a study conducted at a referral center in Italy found an increased risk of recurrence with either Factor V Leiden or prothrombin gene mutation, a large meta-analysis of 23 studies found increased risk only with Factor V Leiden.19,20 Another meta-analysis demonstrated only a modest increased risk of recurrence in subjects with Factor V Leiden or prothrombin gene mutation, and a prospective study from Austria found no increased risk of recurrence with Factor V Leiden two years after discontinuation of anticoagulation.18,21 Additionally, when using patients with unprovoked VTE as reference, there was no increased risk of recurrence among patients homozygous for Factor V Leiden or the prothrombin gene mutation.22
In summary, although Factor V Leiden and prothrombin gene defects are associated with increased risk of recurrent VTE, the magnitude of the risk increase is modest and, therefore, should not alter duration of therapy.
Acquired thrombophilia.
It appears that the only thrombophilic state that might have a significant impact on the risk of recurrence is the antiphospholipid syndrome. The cessation of warfarin therapy in patients with thrombosis associated with antiphospholipid antibodies carries a 69% risk of recurrent thrombosis within a year.23 Some studies have suggested that the presence of specific antibodies (i.e. anticardiolipin antibodies) is associated with increased risk in patients with antiphospholipid syndrome.24
However, at present, all patients with VTE and antiphospholipid syndrome should be candidates for lifelong anticoagulation. Antiphospholipid antibody testing should be performed in patients with a suggestive history, including those with recurrent fetal loss or a single fetal loss after 10 weeks, or known collagen vascular disease.25
The role of provoked vs. unprovoked VTE.
Identifying whether a VTE is provoked or unprovoked has been shown to be an important predictor of recurrence. For example, one prospective, cohort study found two-year recurrence rates of zero in patients with a surgery or pregnancy-related VTE, 9% with other provoked VTE, and 19% with unprovoked VTE.26 In the same study, thrombophilia testing failed to reliably predict recurrence risk. Patients with unprovoked VTE who were tested and found to not have a defect were at equally high risk of recurrent VTE as those found to have a thrombophilia.27
The most significant predictor for VTE recurrence is whether the first event was provoked, and thrombophilia testing offers little additional prognostic information.28
VTE as a multifactorial disorder.
It is becoming increasingly clear that VTE is multifactorial disorder, caused by the interactions of genotypic, phenotypic, and environmental factors. In the case of an unprovoked VTE, the patient already carries a significantly elevated risk for recurrence, and further testing for known causes of thrombophilia appears to add very little additional information. The optimal duration of anticoagulation for unprovoked VTE is unclear, but current guidelines suggest at least three months—and clinicians should consider lifelong treatment.
In the vast majority of cases, testing for thrombophilia has no impact on the management of VTE and is not warranted. In patients with antiphospholipid-antibody syndrome, given the high risk of recurrence, long-term anticoagulation after a first VTE might be indicated. In select patients with a clinical picture suggestive of antiphospholipid-antibody syndrome, or a strong family history, testing should be considered.
Back to the Case
Our patient appears to have an unprovoked VTE. She should receive regular anticoagulation with warfarin, with a goal INR of 2 to 3, for at least three months. Lifelong anticoagulation therapy should be considered. Testing for heritable thrombophilia will not change the current management or treatment duration and, hence, is not indicated. However, the patient’s history is suggestive of antiphospholipid-antibody syndrome, so she should be tested. If the diagnosis of antiphospholipid syndrome is made, lifelong anticoagulation should be considered.
Bottom Line
Unprovoked VTE provides the strongest predictor for recurrence. Thrombophilia testing adds little in predicting recurrence and rarely is indicated.
Dr. Stehlikova is a clinical hospitalist in the division of hospital medicine, department of medicine, at Albert Einstein College of Medicine and Montefiore Medical Center in Bronx, N.Y. Dr. Martin is director of the Einstein Hospitalist Service. Dr. Janakiram is a fellow in the department of hematology at Einstein, and Dr. Korcak is an instructor at Einstein in the department of medicine and director of the Weiler Medical Service. Dr. Galhotra is associate director for inpatient quality in the department of medicine at Einstein; Dr. Averbukh is an academic hospitalist; and Dr. Southern is chief of the division of hospital medicine at Einstein.
References
- Middeldorp S, van Hylckama Vlieg A. Does thrombophilia testing help in the clinical management of patients? Br J Haematol. 2008;143:321-335.
- Coppens M, van Mourik JA, Eckmann CM, Büller HR, Middeldorp S. Current practise of testing for inherited thrombophilia. J Thromb Haemost. 2007;5:1979-1981.
- Prandoni P, Noventa F, Ghirarduzzi A, et al. The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica. 2007;92:199-205.
- Iorio A, Kearon C, Filippucci E, et al. Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review. Arch Intern Med. 2010;170:1710-1716.
- Kearon C, Julian JA, Kovacs MJ, et al. Influence of thrombophilia on risk of recurrent venous thromboembolism while on warfarin: results from a randomized trial. Blood. 2008;112:4432-4436.
- Vossen CY, Walker ID, Svensson P, et al. Recurrence rate after a first venous thrombosis in patients with familial thrombophilia. Arterioscler Thromb Vasc Biol. 2005;25:1992-1997.
- Brown K, Luddington R, Williamson D, Baker P, Baglin T. Risk of venous thromboembolism associated with a G to A transition at position 20210 in the 3'-untranslated region of the prothrombin gene. Br J Haematol. 1997;98:907-909.
- Schulman S, Tengborn L. Treatment of venous thromboembolism in patients with congenital deficiency of antithrombin III. Thromb Haemost. 1992;68:634-636.
- Palareti G, Legnani C, Cosmi B, Guazzaloca G, Cini M, Mattarozzi S. Poor anticoagulation quality in the first 3 months after unprovoked venous thromboembolism is a risk factor for long-term recurrence. J Thromb Haemost. 2005;3:955-961.
- Gadisseur AP, Christiansen SC, van der Meer FJ, Rosendaal FR. The quality of oral anticoagulant therapy and recurrent venous thrombotic events in the Leiden Thrombophilia Study. J Thromb Haemost. 2007;5:931-936.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:454S-545S.
- Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1-7.
- Laczkovics C, Grafenhofer H, Kaider A, et al. Risk of recurrence after a first venous thromboembolic event in young women. Haematologica. 2007;92:1201-1207.
- Brouwer JL, Lijfering WM, Ten Kate MK, Kluin-Nelemans HC, Veeger NJ, van der Meer J. High long-term absolute risk of recurrent venous thromboembolism in patients with hereditary deficiencies of protein S, protein C or antithrombin. Thromb Haemost. 2009;101:93-99.
- Christiansen SC, Cannegieter SC, Koster T, Vandenbroucke JP, Rosendaal FR. Thrombophilia, clinical factors, and recurrent venous thrombotic events. JAMA. 2005;293:2352-2361.
- De Stefano V, Simioni P, Rossi E, et al. The risk of recurrent venous thromboembolism in patients with inherited deficiency of natural anticoagulants antithrombin, protein C and protein S. Haematologica. 2006;91:695-698.
- Price DT, Ridker PM. Factor V Leiden mutation and the risks for thromboembolic disease: a clinical perspective. Ann Intern Med. 1997;127:895-903.
- Ho WK, Hankey GJ, Quinlan DJ, Eikelboom JW. Risk of recurrent venous thromboembolism in patients with common thrombophilia: a systematic review. Arch Intern Med. 2006;166:729-736.
- Simioni P, Prandoni P, Lensing AW, et al. Risk for subsequent venous thromboembolic complications in carriers of the prothrombin or the factor V gene mutation with a first episode of deep-vein thrombosis. Blood. 2000;96:3329-3333.
- Segal JB, Brotman DJ, Necochea AJ, et al. Predictive value of factor V Leiden and prothrombin G20210A in adults with venous thromboembolism and in family members of those with a mutation: a systematic review. JAMA. 2009;301:2472-2485.
- Eichinger S, Pabinger I, Stumpflen A, et al. The risk of recurrent venous thromboembolism in patients with and without factor V Leiden. Thromb Haemost. 1997;77:624-628.
- Lijfering WM, Middeldorp S, Veeger NJ, et al. Risk of recurrent venous thrombosis in homozygous carriers and double heterozygous carriers of factor V Leiden and prothrombin G20210A. Circulation. 2010;121(15):1706-1712.
- Khamashta MA, Cuadrado MJ, Mujic F, Taub NA, Hunt BJ, Hughes GR. The management of thrombosis in the antiphospholipid-antibody syndrome. N Engl J Med. 1995;332:993-997.
- Schulman S, Svenungsson E, Granqvist S. Anticardiolipin antibodies predict early recurrence of thromboembolism and death among patients with venous thromboembolism following anticoagulant therapy. Duration of Anticoagulation Study Group. Am J Med. 1998;104:332-338.
- Pengo V, Tripodi A, Reber G, et al. Update of the guidelines for lupus anticoagulant detection. Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2009;7:1737-1740.
- Baglin T, Luddington R, Brown K, Baglin C. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: prospective cohort study. Lancet. 2003;362:523-526.
- Rosendaal FR. Once and only once. Circulation. 2010;121:1688-1690.
- Dalen JE. Should patients with venous thromboembolism be screened for thrombophilia? Am J Med. 2008;121:458-463.
Contracts Need to Ensure Physicians are Free Agents
Physicians often have medical interests other than clinical practice. A restrictive employment agreement could quash those endeavors. Physician employment agreements play an integral role in establishing the legal, financial, and operational structure of the relationship between employer and physician/employee.
One clause of particular interest to many physicians is the clause defining what a physician can and cannot do outside of providing medical services on behalf of their employer—meaning, can the physician engage in such outside activities as moonlighting, volunteering, or serving as an expert witness? Moreover, if income is generated from these outside activities, who does that income belong to—the physician or the employer?
These questions should be clearly answered in the employment agreement. And if the answers in the employment agreement do not mirror the physician’s wishes, then these terms should be negotiated with the employer and memorialized in the employment agreement.
Consult Your Contract
The first question is whether the physician is even permitted under their employment agreement to participate in activities or perform services outside of employment. Some employers prohibit engagement in outside activities and services altogether, while other employers permit certain activities that do not interfere with the physician’s day-to-day responsibilities. Physicians should be aware of requirements that give the employer the right to approve or reject outside activities. If the physician wants to be able to engage in moonlighting, expert witness consultations and testimony, speaking opportunities, volunteer efforts, teaching, research, or publishing, the physician’s desired activities should be specifically identified in the employment agreement as permitted activities.
For example: Dr. A was joining a medical practice and was presented with the group’s template employment agreement. The draft agreement precluded Dr. A from participating in any medically related outside activities. In the past, Dr. A had served as a volunteer doctor for the local marathon, a medical expert witness, and was a frequent paid speaker at conferences. For Dr. A, a prohibition on outside medical activities did not align with his interests. With minimal discussion, the practice permitted Dr. A to identify the outside activities that he could conduct without violating his employment agreement:
If a physician is permitted to engage in outside activities or services, the second question is whether income generated from such activities belongs to the physician or the employer. This often is a topic of negotiation. Physician and employer frequently do not see eye to eye on this issue. Physicians, on the one hand, often view the income generated from permitted outside activities to be separate and apart from his or her services on behalf of the employer, and thus are outside the reach of the practice. This position is strengthened if the activity occurs on the physician’s own time and outside of the employer’s hours of operation. Employers, on the other hand, often view income from outside activities as part of the employment relationship with the physician. Some employers are of the belief that the physician would not have had the opportunity to participate in the outside activity but for the physician’s employment with the particular employer.
Dr. A’s employer felt that it already was conceding by allowing Dr. A to engage in outside activities and insisted that any payment received by him for these services should be remitted to the practice. Dr. A agreed to this and negotiated for the outside activity monies to be included in his collection amounts, which was a factor in calculating Dr. A’s compensation:
The last question is whether outside activities are covered by the physician’s malpractice insurance policy. If the employer provides the policy for the benefit of the physician, the employer—and the malpractice insurance carrier—may exclude activities performed by the physician outside of his or her employment with that employer. This often is an issue for physicians who want to moonlight, as moonlighting for a third party frequently is excluded from coverage. It is important that the physician consult the malpractice insurance carrier to confirm whether certain activities are covered under the policy. It may be the case that a separate policy is required to insure the physician’s outside activities, even those activities that are unpaid.
Contract clauses describing what the physician can and cannot do outside of the employment relationship are of key importance. These clauses should mirror the individual physician’s medically related and extracurricular interests, and the financial benefits of these activities—if any—should be addressed in the employment agreement. Don’t forget to check with the insurance carrier to ensure that the activity is covered by the policy, as even volunteering medical services could expose a physician. It is best to address these issues at the onset of the employer-employee relationship. That way, all parties are on the same page from the beginning.
Steven Harris is a nationally recognized healthcare attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
Physicians often have medical interests other than clinical practice. A restrictive employment agreement could quash those endeavors. Physician employment agreements play an integral role in establishing the legal, financial, and operational structure of the relationship between employer and physician/employee.
One clause of particular interest to many physicians is the clause defining what a physician can and cannot do outside of providing medical services on behalf of their employer—meaning, can the physician engage in such outside activities as moonlighting, volunteering, or serving as an expert witness? Moreover, if income is generated from these outside activities, who does that income belong to—the physician or the employer?
These questions should be clearly answered in the employment agreement. And if the answers in the employment agreement do not mirror the physician’s wishes, then these terms should be negotiated with the employer and memorialized in the employment agreement.
Consult Your Contract
The first question is whether the physician is even permitted under their employment agreement to participate in activities or perform services outside of employment. Some employers prohibit engagement in outside activities and services altogether, while other employers permit certain activities that do not interfere with the physician’s day-to-day responsibilities. Physicians should be aware of requirements that give the employer the right to approve or reject outside activities. If the physician wants to be able to engage in moonlighting, expert witness consultations and testimony, speaking opportunities, volunteer efforts, teaching, research, or publishing, the physician’s desired activities should be specifically identified in the employment agreement as permitted activities.
For example: Dr. A was joining a medical practice and was presented with the group’s template employment agreement. The draft agreement precluded Dr. A from participating in any medically related outside activities. In the past, Dr. A had served as a volunteer doctor for the local marathon, a medical expert witness, and was a frequent paid speaker at conferences. For Dr. A, a prohibition on outside medical activities did not align with his interests. With minimal discussion, the practice permitted Dr. A to identify the outside activities that he could conduct without violating his employment agreement:
If a physician is permitted to engage in outside activities or services, the second question is whether income generated from such activities belongs to the physician or the employer. This often is a topic of negotiation. Physician and employer frequently do not see eye to eye on this issue. Physicians, on the one hand, often view the income generated from permitted outside activities to be separate and apart from his or her services on behalf of the employer, and thus are outside the reach of the practice. This position is strengthened if the activity occurs on the physician’s own time and outside of the employer’s hours of operation. Employers, on the other hand, often view income from outside activities as part of the employment relationship with the physician. Some employers are of the belief that the physician would not have had the opportunity to participate in the outside activity but for the physician’s employment with the particular employer.
Dr. A’s employer felt that it already was conceding by allowing Dr. A to engage in outside activities and insisted that any payment received by him for these services should be remitted to the practice. Dr. A agreed to this and negotiated for the outside activity monies to be included in his collection amounts, which was a factor in calculating Dr. A’s compensation:
The last question is whether outside activities are covered by the physician’s malpractice insurance policy. If the employer provides the policy for the benefit of the physician, the employer—and the malpractice insurance carrier—may exclude activities performed by the physician outside of his or her employment with that employer. This often is an issue for physicians who want to moonlight, as moonlighting for a third party frequently is excluded from coverage. It is important that the physician consult the malpractice insurance carrier to confirm whether certain activities are covered under the policy. It may be the case that a separate policy is required to insure the physician’s outside activities, even those activities that are unpaid.
Contract clauses describing what the physician can and cannot do outside of the employment relationship are of key importance. These clauses should mirror the individual physician’s medically related and extracurricular interests, and the financial benefits of these activities—if any—should be addressed in the employment agreement. Don’t forget to check with the insurance carrier to ensure that the activity is covered by the policy, as even volunteering medical services could expose a physician. It is best to address these issues at the onset of the employer-employee relationship. That way, all parties are on the same page from the beginning.
Steven Harris is a nationally recognized healthcare attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
Physicians often have medical interests other than clinical practice. A restrictive employment agreement could quash those endeavors. Physician employment agreements play an integral role in establishing the legal, financial, and operational structure of the relationship between employer and physician/employee.
One clause of particular interest to many physicians is the clause defining what a physician can and cannot do outside of providing medical services on behalf of their employer—meaning, can the physician engage in such outside activities as moonlighting, volunteering, or serving as an expert witness? Moreover, if income is generated from these outside activities, who does that income belong to—the physician or the employer?
These questions should be clearly answered in the employment agreement. And if the answers in the employment agreement do not mirror the physician’s wishes, then these terms should be negotiated with the employer and memorialized in the employment agreement.
Consult Your Contract
The first question is whether the physician is even permitted under their employment agreement to participate in activities or perform services outside of employment. Some employers prohibit engagement in outside activities and services altogether, while other employers permit certain activities that do not interfere with the physician’s day-to-day responsibilities. Physicians should be aware of requirements that give the employer the right to approve or reject outside activities. If the physician wants to be able to engage in moonlighting, expert witness consultations and testimony, speaking opportunities, volunteer efforts, teaching, research, or publishing, the physician’s desired activities should be specifically identified in the employment agreement as permitted activities.
For example: Dr. A was joining a medical practice and was presented with the group’s template employment agreement. The draft agreement precluded Dr. A from participating in any medically related outside activities. In the past, Dr. A had served as a volunteer doctor for the local marathon, a medical expert witness, and was a frequent paid speaker at conferences. For Dr. A, a prohibition on outside medical activities did not align with his interests. With minimal discussion, the practice permitted Dr. A to identify the outside activities that he could conduct without violating his employment agreement:
If a physician is permitted to engage in outside activities or services, the second question is whether income generated from such activities belongs to the physician or the employer. This often is a topic of negotiation. Physician and employer frequently do not see eye to eye on this issue. Physicians, on the one hand, often view the income generated from permitted outside activities to be separate and apart from his or her services on behalf of the employer, and thus are outside the reach of the practice. This position is strengthened if the activity occurs on the physician’s own time and outside of the employer’s hours of operation. Employers, on the other hand, often view income from outside activities as part of the employment relationship with the physician. Some employers are of the belief that the physician would not have had the opportunity to participate in the outside activity but for the physician’s employment with the particular employer.
Dr. A’s employer felt that it already was conceding by allowing Dr. A to engage in outside activities and insisted that any payment received by him for these services should be remitted to the practice. Dr. A agreed to this and negotiated for the outside activity monies to be included in his collection amounts, which was a factor in calculating Dr. A’s compensation:
The last question is whether outside activities are covered by the physician’s malpractice insurance policy. If the employer provides the policy for the benefit of the physician, the employer—and the malpractice insurance carrier—may exclude activities performed by the physician outside of his or her employment with that employer. This often is an issue for physicians who want to moonlight, as moonlighting for a third party frequently is excluded from coverage. It is important that the physician consult the malpractice insurance carrier to confirm whether certain activities are covered under the policy. It may be the case that a separate policy is required to insure the physician’s outside activities, even those activities that are unpaid.
Contract clauses describing what the physician can and cannot do outside of the employment relationship are of key importance. These clauses should mirror the individual physician’s medically related and extracurricular interests, and the financial benefits of these activities—if any—should be addressed in the employment agreement. Don’t forget to check with the insurance carrier to ensure that the activity is covered by the policy, as even volunteering medical services could expose a physician. It is best to address these issues at the onset of the employer-employee relationship. That way, all parties are on the same page from the beginning.
Steven Harris is a nationally recognized healthcare attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
Patient Satisfaction Critical to Hospital Value-Based Purchasing Program
Should patient satisfaction factor prominently into healthcare pay-for-performance incentives? That question recently became moot as the Centers for Medicare & Medicaid Services (CMS) began withholding 1% of hospitals’ Medicare reimbursement as part of its Hospital Value-Based Purchasing Program, restoring it to institutions based upon their quality performance. Thirty percent of the program’s financial incentive is based upon how well hospitals score on patient satisfaction, as measured by the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey.
Despite those data having been collected and reported for years, their use as a healthcare performance indicator continues to be controversial. To win back reimbursement withholds, hospitals must earn perfect scores: The only winners are the ones for whom patients respond “always satisfied” to such questions as “How often did doctors treat you with courtesy and respect?” or “How often did doctors explain things in a way you could understand?” or “How often did hospital staff tell you what the medicine was for?”
A perfectly happy patient, skeptics say, isn’t necessarily one who has received the best medical care, and several analyses suggest that HCAHPS has unintended biases, making it a flawed accountability tool. Some of the nation’s most prestigious hospitals, for example, receive bad patient reviews despite getting high scores on clinical quality metrics.1
Conversely, many hospitals that receive high patient ratings have low clinical quality marks (e.g. significantly worse mortality rates than the national average for heart attacks, heart failure, or pneumonia).2
Safety-net hospitals perform more poorly than other hospitals on nearly every HCAHPS measure of patient experience, with gaps that are sizable and persistent. These institutions have the most fragile operating margins and are the least able to absorb the additional reimbursement cuts that will result from their low scores.3
Teaching hospitals and other large hospitals also score more poorly, on average, than do small community hospitals.4
Unexplained geographic disparities persist, with hospitals in cities and certain regions, such as the Northeast and California, scoring lower than other regions.1
Quality Requires Clarity
“These are valid criticisms. Just because someone receives the best medical care doesn’t mean they are the happiest—and vice versa,” says Peter Short, MD, senior vice president of medical affairs for Northeast Hospital Corp. in Massachusetts. “Are there biases [in the way patient satisfaction is measured]?
Absolutely. But we’re all being held accountable and we can’t wait for a perfect system.
“Any definition of high-quality medical care must take into consideration how it is perceived by patients,” he adds, particularly when “value” in healthcare means delivering high-quality, patient-friendly care at the lowest cost.
James Merlino, MD, FACS, FASCRS, chief experience officer for Cleveland Clinic, says little peer-reviewed research exists to show that HCAHPS is a robust process of measuring patient satisfaction, but he says CMS is “focusing on the right areas.”
“It’s hard to say that paying attention to the patient experience is not something we should do. And yet, many physicians and hospitals have not done a good job focusing on patient satisfaction,” Dr. Merlino says. “How well we communicate with patients goes to the heart of the patient-provider interaction: It’s crucial that patients are clearly informed what to do while they are in a hospital and after they are discharged. Poor communication can drive confusion, noncompliance, and complications.”

—John Wasson, MD, emeritus professor of community and family medicine at Dartmouth Medical School
Proven Improvements
Hospitalists will be leaders in driving patient satisfaction, Dr. Merlino says, given their central role in managing patients across the continuum of care. That role gives them great responsibility—and opportunity—to champion practices at their institutions that improve the hospital experience of their patients, many of whom have complicated illnesses requiring a potentially bewildering array of tests and procedures.
Several “best practices” have proven successful in boosting patient-satisfaction scores and can be readily adapted to a variety of local hospital settings, says Dr. Short, who is a speaker in SHM’s Hospital Value-Based Program Toolkit webinar series (see “Best Practices,”).
Cleveland Clinic has greatly boosted its physician communication scores by sharing HCAHPS performance data with physicians and by gleaning best practices from its high-scoring physicians, which include, for example, ensuring that residents and fellows speak with attendings before rounding with patients to ensure staff alignment and care coordination, Dr. Merlino explains.
Cleveland Clinic also is rolling out to its entire medical staff a communication training program taught by a carefully selected team of peer physicians, which Dr. Merlino says is proving to be very effective in boosting patient satisfaction and improving care by enhancing patient-physician conversations. The program features Kaiser Permanente’s “Four Habits” model to help organize medical interviews with patients:
- Invest in the beginning by creating rapport quickly, and let the patient know what to expect.
- Get the patient’s perspective by asking for their ideas concerning the meaning of symptoms and the request for care.
- Demonstrate empathy by being open to the patient’s emotions and conveying empathy verbally and nonverbally.
- Invest in the end by delivering diagnostic information, explaining the rationale for tests and treatments, involving the patient in decision-making, and reviewing the next steps.5
“Organizations have to evolve in an increasingly value-based healthcare environment by developing a culture that can adapt to any set of questions or regulations that CMS mandates,” Dr. Merlino adds.
Next-Generation Patient Satisfaction Measures
Tools to guide patients and healthcare/hospitalist teams toward more satisfying dialogues with patients—as well as tools to improve their outcomes—are becoming increasingly available, says John Wasson, MD, emeritus professor of community and family medicine at Dartmouth Medical School and a member of The Dartmouth Institute Patient-Reported Measure Trust, which is developing and testing next-generation, patient-reported healthcare measures.
One example is Howsyourhealth.org, a family of communication-enhancement tools designed to build patient confidence in managing and controlling their health problems by helping them “get what they want and need exactly when and how they want and need it,” Dr. Wasson says.
“Hospitalists and their teams might begin to think about processes that enhance a patient’s health confidence, which is very strongly associated with many outcomes,” he notes. The hospital version of the tool—at Howsyourcare.org—immediately provides information tailored to patients’ needs, as well as a summary hospitalists can review with their teams in order to improve patient/caregiver confidence for successful management of conditions when discharged, Dr. Wasson says.
“Overall patient satisfaction is not particularly useful for predicting health confidence,” he says. “Information quality tailored to patient need is what boosts patients’ health confidence—and has real power to improve patients’ clinical outcomes.”
Christopher Guadagnino is a freelance medical journalist in Philadelphia.
References
- Rau J. When TLC doesn't satisfy patients, elite hospitals may pay a price. Kaiser Health News website. Available at: http://www.kaiserhealthnews.org/stories/2011/november/08/patient-ratings-hospital-medicare-reimbursements.aspx. Accessed Aug. 15, 2012.
- Sternberg S, Schnaars C. Medicare data can help patients fill perception gap. USA Today website. Available at: http://www.usatoday.com/yourlife/health/healthcare/hospitals/2011-08-04-hospitals-patients-death-rates-Medicare_n.htm. Accessed Aug. 15, 2012.
- Chatterjee P, Joynt KE, Orav EJ, Jha AK. Patient experience in safety-net hospitals: implications for improving care and value-based purchasing. Arch Intern Med. 2012 Jul 16:1-7. doi: 10.1001/archinternmed.2012.3158 [Epub ahead of print].
- Rau J, Medicare to begin basing hospital payments on patient-satisfaction scores. Kaiser Health News website.. Available at: http://www.kaiserhealthnews.org/stories/2011/april/28/medicare-hospital-patient-satisfaction.aspx. Accessed Aug. 15, 2011.
- Frankel RM, Stein T. Getting the most out of the clinical encounter: the four habits model. The Permanente Journal website. Available at: http://xnet.kp.org/permanentejournal/fall99pj/habits.html. Accessed Aug. 15, 2012.
Should patient satisfaction factor prominently into healthcare pay-for-performance incentives? That question recently became moot as the Centers for Medicare & Medicaid Services (CMS) began withholding 1% of hospitals’ Medicare reimbursement as part of its Hospital Value-Based Purchasing Program, restoring it to institutions based upon their quality performance. Thirty percent of the program’s financial incentive is based upon how well hospitals score on patient satisfaction, as measured by the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey.
Despite those data having been collected and reported for years, their use as a healthcare performance indicator continues to be controversial. To win back reimbursement withholds, hospitals must earn perfect scores: The only winners are the ones for whom patients respond “always satisfied” to such questions as “How often did doctors treat you with courtesy and respect?” or “How often did doctors explain things in a way you could understand?” or “How often did hospital staff tell you what the medicine was for?”
A perfectly happy patient, skeptics say, isn’t necessarily one who has received the best medical care, and several analyses suggest that HCAHPS has unintended biases, making it a flawed accountability tool. Some of the nation’s most prestigious hospitals, for example, receive bad patient reviews despite getting high scores on clinical quality metrics.1
Conversely, many hospitals that receive high patient ratings have low clinical quality marks (e.g. significantly worse mortality rates than the national average for heart attacks, heart failure, or pneumonia).2
Safety-net hospitals perform more poorly than other hospitals on nearly every HCAHPS measure of patient experience, with gaps that are sizable and persistent. These institutions have the most fragile operating margins and are the least able to absorb the additional reimbursement cuts that will result from their low scores.3
Teaching hospitals and other large hospitals also score more poorly, on average, than do small community hospitals.4
Unexplained geographic disparities persist, with hospitals in cities and certain regions, such as the Northeast and California, scoring lower than other regions.1
Quality Requires Clarity
“These are valid criticisms. Just because someone receives the best medical care doesn’t mean they are the happiest—and vice versa,” says Peter Short, MD, senior vice president of medical affairs for Northeast Hospital Corp. in Massachusetts. “Are there biases [in the way patient satisfaction is measured]?
Absolutely. But we’re all being held accountable and we can’t wait for a perfect system.
“Any definition of high-quality medical care must take into consideration how it is perceived by patients,” he adds, particularly when “value” in healthcare means delivering high-quality, patient-friendly care at the lowest cost.
James Merlino, MD, FACS, FASCRS, chief experience officer for Cleveland Clinic, says little peer-reviewed research exists to show that HCAHPS is a robust process of measuring patient satisfaction, but he says CMS is “focusing on the right areas.”
“It’s hard to say that paying attention to the patient experience is not something we should do. And yet, many physicians and hospitals have not done a good job focusing on patient satisfaction,” Dr. Merlino says. “How well we communicate with patients goes to the heart of the patient-provider interaction: It’s crucial that patients are clearly informed what to do while they are in a hospital and after they are discharged. Poor communication can drive confusion, noncompliance, and complications.”

—John Wasson, MD, emeritus professor of community and family medicine at Dartmouth Medical School
Proven Improvements
Hospitalists will be leaders in driving patient satisfaction, Dr. Merlino says, given their central role in managing patients across the continuum of care. That role gives them great responsibility—and opportunity—to champion practices at their institutions that improve the hospital experience of their patients, many of whom have complicated illnesses requiring a potentially bewildering array of tests and procedures.
Several “best practices” have proven successful in boosting patient-satisfaction scores and can be readily adapted to a variety of local hospital settings, says Dr. Short, who is a speaker in SHM’s Hospital Value-Based Program Toolkit webinar series (see “Best Practices,”).
Cleveland Clinic has greatly boosted its physician communication scores by sharing HCAHPS performance data with physicians and by gleaning best practices from its high-scoring physicians, which include, for example, ensuring that residents and fellows speak with attendings before rounding with patients to ensure staff alignment and care coordination, Dr. Merlino explains.
Cleveland Clinic also is rolling out to its entire medical staff a communication training program taught by a carefully selected team of peer physicians, which Dr. Merlino says is proving to be very effective in boosting patient satisfaction and improving care by enhancing patient-physician conversations. The program features Kaiser Permanente’s “Four Habits” model to help organize medical interviews with patients:
- Invest in the beginning by creating rapport quickly, and let the patient know what to expect.
- Get the patient’s perspective by asking for their ideas concerning the meaning of symptoms and the request for care.
- Demonstrate empathy by being open to the patient’s emotions and conveying empathy verbally and nonverbally.
- Invest in the end by delivering diagnostic information, explaining the rationale for tests and treatments, involving the patient in decision-making, and reviewing the next steps.5
“Organizations have to evolve in an increasingly value-based healthcare environment by developing a culture that can adapt to any set of questions or regulations that CMS mandates,” Dr. Merlino adds.
Next-Generation Patient Satisfaction Measures
Tools to guide patients and healthcare/hospitalist teams toward more satisfying dialogues with patients—as well as tools to improve their outcomes—are becoming increasingly available, says John Wasson, MD, emeritus professor of community and family medicine at Dartmouth Medical School and a member of The Dartmouth Institute Patient-Reported Measure Trust, which is developing and testing next-generation, patient-reported healthcare measures.
One example is Howsyourhealth.org, a family of communication-enhancement tools designed to build patient confidence in managing and controlling their health problems by helping them “get what they want and need exactly when and how they want and need it,” Dr. Wasson says.
“Hospitalists and their teams might begin to think about processes that enhance a patient’s health confidence, which is very strongly associated with many outcomes,” he notes. The hospital version of the tool—at Howsyourcare.org—immediately provides information tailored to patients’ needs, as well as a summary hospitalists can review with their teams in order to improve patient/caregiver confidence for successful management of conditions when discharged, Dr. Wasson says.
“Overall patient satisfaction is not particularly useful for predicting health confidence,” he says. “Information quality tailored to patient need is what boosts patients’ health confidence—and has real power to improve patients’ clinical outcomes.”
Christopher Guadagnino is a freelance medical journalist in Philadelphia.
References
- Rau J. When TLC doesn't satisfy patients, elite hospitals may pay a price. Kaiser Health News website. Available at: http://www.kaiserhealthnews.org/stories/2011/november/08/patient-ratings-hospital-medicare-reimbursements.aspx. Accessed Aug. 15, 2012.
- Sternberg S, Schnaars C. Medicare data can help patients fill perception gap. USA Today website. Available at: http://www.usatoday.com/yourlife/health/healthcare/hospitals/2011-08-04-hospitals-patients-death-rates-Medicare_n.htm. Accessed Aug. 15, 2012.
- Chatterjee P, Joynt KE, Orav EJ, Jha AK. Patient experience in safety-net hospitals: implications for improving care and value-based purchasing. Arch Intern Med. 2012 Jul 16:1-7. doi: 10.1001/archinternmed.2012.3158 [Epub ahead of print].
- Rau J, Medicare to begin basing hospital payments on patient-satisfaction scores. Kaiser Health News website.. Available at: http://www.kaiserhealthnews.org/stories/2011/april/28/medicare-hospital-patient-satisfaction.aspx. Accessed Aug. 15, 2011.
- Frankel RM, Stein T. Getting the most out of the clinical encounter: the four habits model. The Permanente Journal website. Available at: http://xnet.kp.org/permanentejournal/fall99pj/habits.html. Accessed Aug. 15, 2012.
Should patient satisfaction factor prominently into healthcare pay-for-performance incentives? That question recently became moot as the Centers for Medicare & Medicaid Services (CMS) began withholding 1% of hospitals’ Medicare reimbursement as part of its Hospital Value-Based Purchasing Program, restoring it to institutions based upon their quality performance. Thirty percent of the program’s financial incentive is based upon how well hospitals score on patient satisfaction, as measured by the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey.
Despite those data having been collected and reported for years, their use as a healthcare performance indicator continues to be controversial. To win back reimbursement withholds, hospitals must earn perfect scores: The only winners are the ones for whom patients respond “always satisfied” to such questions as “How often did doctors treat you with courtesy and respect?” or “How often did doctors explain things in a way you could understand?” or “How often did hospital staff tell you what the medicine was for?”
A perfectly happy patient, skeptics say, isn’t necessarily one who has received the best medical care, and several analyses suggest that HCAHPS has unintended biases, making it a flawed accountability tool. Some of the nation’s most prestigious hospitals, for example, receive bad patient reviews despite getting high scores on clinical quality metrics.1
Conversely, many hospitals that receive high patient ratings have low clinical quality marks (e.g. significantly worse mortality rates than the national average for heart attacks, heart failure, or pneumonia).2
Safety-net hospitals perform more poorly than other hospitals on nearly every HCAHPS measure of patient experience, with gaps that are sizable and persistent. These institutions have the most fragile operating margins and are the least able to absorb the additional reimbursement cuts that will result from their low scores.3
Teaching hospitals and other large hospitals also score more poorly, on average, than do small community hospitals.4
Unexplained geographic disparities persist, with hospitals in cities and certain regions, such as the Northeast and California, scoring lower than other regions.1
Quality Requires Clarity
“These are valid criticisms. Just because someone receives the best medical care doesn’t mean they are the happiest—and vice versa,” says Peter Short, MD, senior vice president of medical affairs for Northeast Hospital Corp. in Massachusetts. “Are there biases [in the way patient satisfaction is measured]?
Absolutely. But we’re all being held accountable and we can’t wait for a perfect system.
“Any definition of high-quality medical care must take into consideration how it is perceived by patients,” he adds, particularly when “value” in healthcare means delivering high-quality, patient-friendly care at the lowest cost.
James Merlino, MD, FACS, FASCRS, chief experience officer for Cleveland Clinic, says little peer-reviewed research exists to show that HCAHPS is a robust process of measuring patient satisfaction, but he says CMS is “focusing on the right areas.”
“It’s hard to say that paying attention to the patient experience is not something we should do. And yet, many physicians and hospitals have not done a good job focusing on patient satisfaction,” Dr. Merlino says. “How well we communicate with patients goes to the heart of the patient-provider interaction: It’s crucial that patients are clearly informed what to do while they are in a hospital and after they are discharged. Poor communication can drive confusion, noncompliance, and complications.”

—John Wasson, MD, emeritus professor of community and family medicine at Dartmouth Medical School
Proven Improvements
Hospitalists will be leaders in driving patient satisfaction, Dr. Merlino says, given their central role in managing patients across the continuum of care. That role gives them great responsibility—and opportunity—to champion practices at their institutions that improve the hospital experience of their patients, many of whom have complicated illnesses requiring a potentially bewildering array of tests and procedures.
Several “best practices” have proven successful in boosting patient-satisfaction scores and can be readily adapted to a variety of local hospital settings, says Dr. Short, who is a speaker in SHM’s Hospital Value-Based Program Toolkit webinar series (see “Best Practices,”).
Cleveland Clinic has greatly boosted its physician communication scores by sharing HCAHPS performance data with physicians and by gleaning best practices from its high-scoring physicians, which include, for example, ensuring that residents and fellows speak with attendings before rounding with patients to ensure staff alignment and care coordination, Dr. Merlino explains.
Cleveland Clinic also is rolling out to its entire medical staff a communication training program taught by a carefully selected team of peer physicians, which Dr. Merlino says is proving to be very effective in boosting patient satisfaction and improving care by enhancing patient-physician conversations. The program features Kaiser Permanente’s “Four Habits” model to help organize medical interviews with patients:
- Invest in the beginning by creating rapport quickly, and let the patient know what to expect.
- Get the patient’s perspective by asking for their ideas concerning the meaning of symptoms and the request for care.
- Demonstrate empathy by being open to the patient’s emotions and conveying empathy verbally and nonverbally.
- Invest in the end by delivering diagnostic information, explaining the rationale for tests and treatments, involving the patient in decision-making, and reviewing the next steps.5
“Organizations have to evolve in an increasingly value-based healthcare environment by developing a culture that can adapt to any set of questions or regulations that CMS mandates,” Dr. Merlino adds.
Next-Generation Patient Satisfaction Measures
Tools to guide patients and healthcare/hospitalist teams toward more satisfying dialogues with patients—as well as tools to improve their outcomes—are becoming increasingly available, says John Wasson, MD, emeritus professor of community and family medicine at Dartmouth Medical School and a member of The Dartmouth Institute Patient-Reported Measure Trust, which is developing and testing next-generation, patient-reported healthcare measures.
One example is Howsyourhealth.org, a family of communication-enhancement tools designed to build patient confidence in managing and controlling their health problems by helping them “get what they want and need exactly when and how they want and need it,” Dr. Wasson says.
“Hospitalists and their teams might begin to think about processes that enhance a patient’s health confidence, which is very strongly associated with many outcomes,” he notes. The hospital version of the tool—at Howsyourcare.org—immediately provides information tailored to patients’ needs, as well as a summary hospitalists can review with their teams in order to improve patient/caregiver confidence for successful management of conditions when discharged, Dr. Wasson says.
“Overall patient satisfaction is not particularly useful for predicting health confidence,” he says. “Information quality tailored to patient need is what boosts patients’ health confidence—and has real power to improve patients’ clinical outcomes.”
Christopher Guadagnino is a freelance medical journalist in Philadelphia.
References
- Rau J. When TLC doesn't satisfy patients, elite hospitals may pay a price. Kaiser Health News website. Available at: http://www.kaiserhealthnews.org/stories/2011/november/08/patient-ratings-hospital-medicare-reimbursements.aspx. Accessed Aug. 15, 2012.
- Sternberg S, Schnaars C. Medicare data can help patients fill perception gap. USA Today website. Available at: http://www.usatoday.com/yourlife/health/healthcare/hospitals/2011-08-04-hospitals-patients-death-rates-Medicare_n.htm. Accessed Aug. 15, 2012.
- Chatterjee P, Joynt KE, Orav EJ, Jha AK. Patient experience in safety-net hospitals: implications for improving care and value-based purchasing. Arch Intern Med. 2012 Jul 16:1-7. doi: 10.1001/archinternmed.2012.3158 [Epub ahead of print].
- Rau J, Medicare to begin basing hospital payments on patient-satisfaction scores. Kaiser Health News website.. Available at: http://www.kaiserhealthnews.org/stories/2011/april/28/medicare-hospital-patient-satisfaction.aspx. Accessed Aug. 15, 2011.
- Frankel RM, Stein T. Getting the most out of the clinical encounter: the four habits model. The Permanente Journal website. Available at: http://xnet.kp.org/permanentejournal/fall99pj/habits.html. Accessed Aug. 15, 2012.
ICU Hospitalist Model Improves Quality of Care for Critically Ill Patients
Despite calls for board-certified intensivists to manage all critically ill patients, only a third of hospitalized ICU patients currently are seen by such a specialist—mostly because there are not enough of them to go around.1,2 More and more hospitalists, especially those in community hospitals, are working in ICUs (see “The Critical-Care Debate,”). With the proper training, that can be a good thing for patients and hospitalists, according to a Research, Innovations, and Clinical Vignettes (RIV) abstract presented at HM12 in San Diego.3
Lead author and hospitalist Mark Krivopal, MD, SFHM, formerly with TeamHealth in California and now vice president and medical director of clinical integration and hospital medicine at Steward Health Care in Boston, outlined a program at California’s Lodi Memorial Hospital that identified a group of hospitalists who had experience in caring for critically ill patients and credentials to perform such procedures as central-line placements, intubations, and ventilator management. The select group of TeamHealth hospitalists completed a two-day “Fundamentals of Critical Care Support” course offered by the Society of Critical Care Medicine (www.sccm.org), then began covering the ICU in shifts from 7 a.m. to 7 p.m. The program was so successful early on that hospital administration requested that it expand to a 24-hour service.
An ICU hospitalist program needs to be a partnership, Dr. Krivopal says. Essential oversight at Lodi Memorial is provided by the hospital’s sole pulmonologist.
Preliminary data showed a 35% reduction in ventilator days and 22% reduction in ICU stays, Dr. Krivopal says. The hospital also reports high satisfaction from nurses and other staff. Additional metrics, such as cost savings and patient satisfaction, are under review.
“So long as the level of training is sufficient, this is an approach that definitely should be explored,” he says, adding that young internists have many of the skills needed for ICU work. “But if you don’t keep those skills up [with practice] after residency, you lose them.”
References
- The Leapfrog Group. ICU physician staffing fact sheet. The Leapfrog Group website. Available at: http://www.leapfroggroup.org/media/file/Leapfrog-ICU_Physician_Staffing_Fact_Sheet.pdf. Accessed Aug. 29, 2012.
- Health Resources & Services Administration. Report to Congress: The critical care workforce: a study of the supply and demand for critical care physicians. U.S. Department of Health & Human Services website. Available at: http://bhpr.hrsa.gov/healthworkforce/reports/studycriticalcarephys.pdf. Accessed Aug. 29, 2012.
- Krivopal M, Hlaing M, Felber R, Himebaugh R. ICU hospitalist: a novel method of care for the critically ill patients in economically lean times. J Hosp Med. 2012;7(Suppl 2):192.
Despite calls for board-certified intensivists to manage all critically ill patients, only a third of hospitalized ICU patients currently are seen by such a specialist—mostly because there are not enough of them to go around.1,2 More and more hospitalists, especially those in community hospitals, are working in ICUs (see “The Critical-Care Debate,”). With the proper training, that can be a good thing for patients and hospitalists, according to a Research, Innovations, and Clinical Vignettes (RIV) abstract presented at HM12 in San Diego.3
Lead author and hospitalist Mark Krivopal, MD, SFHM, formerly with TeamHealth in California and now vice president and medical director of clinical integration and hospital medicine at Steward Health Care in Boston, outlined a program at California’s Lodi Memorial Hospital that identified a group of hospitalists who had experience in caring for critically ill patients and credentials to perform such procedures as central-line placements, intubations, and ventilator management. The select group of TeamHealth hospitalists completed a two-day “Fundamentals of Critical Care Support” course offered by the Society of Critical Care Medicine (www.sccm.org), then began covering the ICU in shifts from 7 a.m. to 7 p.m. The program was so successful early on that hospital administration requested that it expand to a 24-hour service.
An ICU hospitalist program needs to be a partnership, Dr. Krivopal says. Essential oversight at Lodi Memorial is provided by the hospital’s sole pulmonologist.
Preliminary data showed a 35% reduction in ventilator days and 22% reduction in ICU stays, Dr. Krivopal says. The hospital also reports high satisfaction from nurses and other staff. Additional metrics, such as cost savings and patient satisfaction, are under review.
“So long as the level of training is sufficient, this is an approach that definitely should be explored,” he says, adding that young internists have many of the skills needed for ICU work. “But if you don’t keep those skills up [with practice] after residency, you lose them.”
References
- The Leapfrog Group. ICU physician staffing fact sheet. The Leapfrog Group website. Available at: http://www.leapfroggroup.org/media/file/Leapfrog-ICU_Physician_Staffing_Fact_Sheet.pdf. Accessed Aug. 29, 2012.
- Health Resources & Services Administration. Report to Congress: The critical care workforce: a study of the supply and demand for critical care physicians. U.S. Department of Health & Human Services website. Available at: http://bhpr.hrsa.gov/healthworkforce/reports/studycriticalcarephys.pdf. Accessed Aug. 29, 2012.
- Krivopal M, Hlaing M, Felber R, Himebaugh R. ICU hospitalist: a novel method of care for the critically ill patients in economically lean times. J Hosp Med. 2012;7(Suppl 2):192.
Despite calls for board-certified intensivists to manage all critically ill patients, only a third of hospitalized ICU patients currently are seen by such a specialist—mostly because there are not enough of them to go around.1,2 More and more hospitalists, especially those in community hospitals, are working in ICUs (see “The Critical-Care Debate,”). With the proper training, that can be a good thing for patients and hospitalists, according to a Research, Innovations, and Clinical Vignettes (RIV) abstract presented at HM12 in San Diego.3
Lead author and hospitalist Mark Krivopal, MD, SFHM, formerly with TeamHealth in California and now vice president and medical director of clinical integration and hospital medicine at Steward Health Care in Boston, outlined a program at California’s Lodi Memorial Hospital that identified a group of hospitalists who had experience in caring for critically ill patients and credentials to perform such procedures as central-line placements, intubations, and ventilator management. The select group of TeamHealth hospitalists completed a two-day “Fundamentals of Critical Care Support” course offered by the Society of Critical Care Medicine (www.sccm.org), then began covering the ICU in shifts from 7 a.m. to 7 p.m. The program was so successful early on that hospital administration requested that it expand to a 24-hour service.
An ICU hospitalist program needs to be a partnership, Dr. Krivopal says. Essential oversight at Lodi Memorial is provided by the hospital’s sole pulmonologist.
Preliminary data showed a 35% reduction in ventilator days and 22% reduction in ICU stays, Dr. Krivopal says. The hospital also reports high satisfaction from nurses and other staff. Additional metrics, such as cost savings and patient satisfaction, are under review.
“So long as the level of training is sufficient, this is an approach that definitely should be explored,” he says, adding that young internists have many of the skills needed for ICU work. “But if you don’t keep those skills up [with practice] after residency, you lose them.”
References
- The Leapfrog Group. ICU physician staffing fact sheet. The Leapfrog Group website. Available at: http://www.leapfroggroup.org/media/file/Leapfrog-ICU_Physician_Staffing_Fact_Sheet.pdf. Accessed Aug. 29, 2012.
- Health Resources & Services Administration. Report to Congress: The critical care workforce: a study of the supply and demand for critical care physicians. U.S. Department of Health & Human Services website. Available at: http://bhpr.hrsa.gov/healthworkforce/reports/studycriticalcarephys.pdf. Accessed Aug. 29, 2012.
- Krivopal M, Hlaing M, Felber R, Himebaugh R. ICU hospitalist: a novel method of care for the critically ill patients in economically lean times. J Hosp Med. 2012;7(Suppl 2):192.
Sharp Rise in Imaging Test Rates has Slowed
A new study tracking the growth of advanced diagnostic imaging techniques found that the rate of growth for such tests is slowing dramatically, even as the total number of tests performed continues to grow.1 Starting in 2007, the rate of growth dropped sharply to about 1% to 3% from more than 6% per year during the previous decade.
Frank Levy, PhD, professor of urban economics at Massachusetts Institute of Technology in Cambridge, Mass., and one of the study’s authors, suggests that the previous growth of the technology could have been partly attributable to such nonmedical factors as profitability for hospitals and fear of malpractice by physicians. The slowdown, Dr. Levy says, also might reflect increased pushback from insurers, recognition of the cost and waste issues, and growing concerns about radiation exposure.
“There are many medical reasons for using these procedures—and many nonmedical reasons,” Dr. Levy says. “To use healthcare resources more efficiently, you should make sure your reason for ordering these tests is medical.”
SHM is working on a short list of sometimes unnecessary but commonly performed medical procedures, which it plans to submit to the American Board of Internal Medicine’s Choosing Wisely campaign this fall. One of the tests being considered for this list is serial chest X-rays for hospitalized patients outside of the ICU who are clinically stable, says Wendy Nickel, associate vice president of SHM’s Center for Hospital Innovation and Improvement. Unnecessary imaging tests are both a safety and a waste issue, she adds.
In related news, a study in the Journal of the National Cancer Institute found that 95.9% of patients 65 and older who have Stage IV cancer received at least one high-cost advanced imaging procedure (e.g. PET or nuclear medicine), with their utilization rates rising more rapidly than for earlier stages of disease.2 Such tests can lead to appropriate palliative measures but also can “distract patients from focusing on achievable end-of-life goals,” explain researchers from the Dana-Farber Cancer Institute in Boston.
References
- Lee D, Levy F. The sharp slowdown in growth of medical imaging: an early analysis suggests combination of policies was the cause. Health Affairs website. Available at: http://www.healthaffairs.org/alert_link.php?url=http://content.healthaffairs.org/content/early/2012/07/24/hlthaff.2011.1034&t=h&id=1590. Accessed Aug. 29, 2012.
- Hu YY, Kwok AC, Jiang W, et al. High-cost imaging in elderly patients with Stage IV cancer. J Natl Cancer Inst. 2012;104(15):1165-1173.
A new study tracking the growth of advanced diagnostic imaging techniques found that the rate of growth for such tests is slowing dramatically, even as the total number of tests performed continues to grow.1 Starting in 2007, the rate of growth dropped sharply to about 1% to 3% from more than 6% per year during the previous decade.
Frank Levy, PhD, professor of urban economics at Massachusetts Institute of Technology in Cambridge, Mass., and one of the study’s authors, suggests that the previous growth of the technology could have been partly attributable to such nonmedical factors as profitability for hospitals and fear of malpractice by physicians. The slowdown, Dr. Levy says, also might reflect increased pushback from insurers, recognition of the cost and waste issues, and growing concerns about radiation exposure.
“There are many medical reasons for using these procedures—and many nonmedical reasons,” Dr. Levy says. “To use healthcare resources more efficiently, you should make sure your reason for ordering these tests is medical.”
SHM is working on a short list of sometimes unnecessary but commonly performed medical procedures, which it plans to submit to the American Board of Internal Medicine’s Choosing Wisely campaign this fall. One of the tests being considered for this list is serial chest X-rays for hospitalized patients outside of the ICU who are clinically stable, says Wendy Nickel, associate vice president of SHM’s Center for Hospital Innovation and Improvement. Unnecessary imaging tests are both a safety and a waste issue, she adds.
In related news, a study in the Journal of the National Cancer Institute found that 95.9% of patients 65 and older who have Stage IV cancer received at least one high-cost advanced imaging procedure (e.g. PET or nuclear medicine), with their utilization rates rising more rapidly than for earlier stages of disease.2 Such tests can lead to appropriate palliative measures but also can “distract patients from focusing on achievable end-of-life goals,” explain researchers from the Dana-Farber Cancer Institute in Boston.
References
- Lee D, Levy F. The sharp slowdown in growth of medical imaging: an early analysis suggests combination of policies was the cause. Health Affairs website. Available at: http://www.healthaffairs.org/alert_link.php?url=http://content.healthaffairs.org/content/early/2012/07/24/hlthaff.2011.1034&t=h&id=1590. Accessed Aug. 29, 2012.
- Hu YY, Kwok AC, Jiang W, et al. High-cost imaging in elderly patients with Stage IV cancer. J Natl Cancer Inst. 2012;104(15):1165-1173.
A new study tracking the growth of advanced diagnostic imaging techniques found that the rate of growth for such tests is slowing dramatically, even as the total number of tests performed continues to grow.1 Starting in 2007, the rate of growth dropped sharply to about 1% to 3% from more than 6% per year during the previous decade.
Frank Levy, PhD, professor of urban economics at Massachusetts Institute of Technology in Cambridge, Mass., and one of the study’s authors, suggests that the previous growth of the technology could have been partly attributable to such nonmedical factors as profitability for hospitals and fear of malpractice by physicians. The slowdown, Dr. Levy says, also might reflect increased pushback from insurers, recognition of the cost and waste issues, and growing concerns about radiation exposure.
“There are many medical reasons for using these procedures—and many nonmedical reasons,” Dr. Levy says. “To use healthcare resources more efficiently, you should make sure your reason for ordering these tests is medical.”
SHM is working on a short list of sometimes unnecessary but commonly performed medical procedures, which it plans to submit to the American Board of Internal Medicine’s Choosing Wisely campaign this fall. One of the tests being considered for this list is serial chest X-rays for hospitalized patients outside of the ICU who are clinically stable, says Wendy Nickel, associate vice president of SHM’s Center for Hospital Innovation and Improvement. Unnecessary imaging tests are both a safety and a waste issue, she adds.
In related news, a study in the Journal of the National Cancer Institute found that 95.9% of patients 65 and older who have Stage IV cancer received at least one high-cost advanced imaging procedure (e.g. PET or nuclear medicine), with their utilization rates rising more rapidly than for earlier stages of disease.2 Such tests can lead to appropriate palliative measures but also can “distract patients from focusing on achievable end-of-life goals,” explain researchers from the Dana-Farber Cancer Institute in Boston.
References
- Lee D, Levy F. The sharp slowdown in growth of medical imaging: an early analysis suggests combination of policies was the cause. Health Affairs website. Available at: http://www.healthaffairs.org/alert_link.php?url=http://content.healthaffairs.org/content/early/2012/07/24/hlthaff.2011.1034&t=h&id=1590. Accessed Aug. 29, 2012.
- Hu YY, Kwok AC, Jiang W, et al. High-cost imaging in elderly patients with Stage IV cancer. J Natl Cancer Inst. 2012;104(15):1165-1173.
Noisy Hospitals Impede Sleep
Sleep-disturbing noise in the hospital is a big problem “that can really compromise a patient’s recovery process,” according to Orfeu Buxton, PhD, associate neuroscientist in the Division of Sleep Medicine at Brigham & Women’s Hospital in Boston.1
Researchers exposed a dozen healthy volunteers to typical nocturnal hospital noise while monitoring their sleep patterns and heart rates, systematically quantifying the disruptive capacity of a range of hospital sounds on sleep. Hospitalized patients routinely cite noise as a major factor that negatively affects quality of care, the researchers note. An Aug. 2 New York Times blog post by Pauline Chen, MD, suggests that government policies linking hospital reimbursement to patient satisfaction might finally turn hospital administrators’ focus on the need to bring this noise under better control.2
References
- Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170-179.
- Chen P. The clatter of the hospital room. New York Times website. Available at: http://well.blogs.nytimes.com/2012/08/02/the-clatter-of-the-hospital-room/. Accessed Aug. 29, 2012.
Sleep-disturbing noise in the hospital is a big problem “that can really compromise a patient’s recovery process,” according to Orfeu Buxton, PhD, associate neuroscientist in the Division of Sleep Medicine at Brigham & Women’s Hospital in Boston.1
Researchers exposed a dozen healthy volunteers to typical nocturnal hospital noise while monitoring their sleep patterns and heart rates, systematically quantifying the disruptive capacity of a range of hospital sounds on sleep. Hospitalized patients routinely cite noise as a major factor that negatively affects quality of care, the researchers note. An Aug. 2 New York Times blog post by Pauline Chen, MD, suggests that government policies linking hospital reimbursement to patient satisfaction might finally turn hospital administrators’ focus on the need to bring this noise under better control.2
References
- Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170-179.
- Chen P. The clatter of the hospital room. New York Times website. Available at: http://well.blogs.nytimes.com/2012/08/02/the-clatter-of-the-hospital-room/. Accessed Aug. 29, 2012.
Sleep-disturbing noise in the hospital is a big problem “that can really compromise a patient’s recovery process,” according to Orfeu Buxton, PhD, associate neuroscientist in the Division of Sleep Medicine at Brigham & Women’s Hospital in Boston.1
Researchers exposed a dozen healthy volunteers to typical nocturnal hospital noise while monitoring their sleep patterns and heart rates, systematically quantifying the disruptive capacity of a range of hospital sounds on sleep. Hospitalized patients routinely cite noise as a major factor that negatively affects quality of care, the researchers note. An Aug. 2 New York Times blog post by Pauline Chen, MD, suggests that government policies linking hospital reimbursement to patient satisfaction might finally turn hospital administrators’ focus on the need to bring this noise under better control.2
References
- Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170-179.
- Chen P. The clatter of the hospital room. New York Times website. Available at: http://well.blogs.nytimes.com/2012/08/02/the-clatter-of-the-hospital-room/. Accessed Aug. 29, 2012.